User login
Coding considerations in investigating chronic pelvic pain
Nonsurgical interventions for chronic pelvic pain may include evaluation and management visits for managing medications, trigger point injections, or pelvic floor physical therapy. However, while these management options can be coded, some of them may have limitations imposed by payers on the frequency of care and by whom the care may be rendered.
For encounters that involve the management of pain medications, it is important that documentation for each of these visits clearly spells out the progress the patient is making in setting goals for pain management. Frequent office visits may send a flag to the payer for overutilization; complete documentation will go a long way to support the medical necessity of each visit at the level billed.
Who renders treatment?
Sometimes, chronic pelvic pain management involves pelvic floor physical therapy, such as teaching pelvic floor exercises or using biofeedback to control certain aspects of the pain. The majority of payers have strict guidelines dictating who can render these services by way of licensure and training if performed by someone other than the physician, and at what frequency. Typically, the person performing the therapy must be, at minimum, a licensed physical therapist.
Frequency
Frequency is often limited to 1 to 2 times a week in increments of 4 weeks before additional authorization is granted. Again, careful and detailed documentation of the patient’s progress will be crucial to continued therapy.
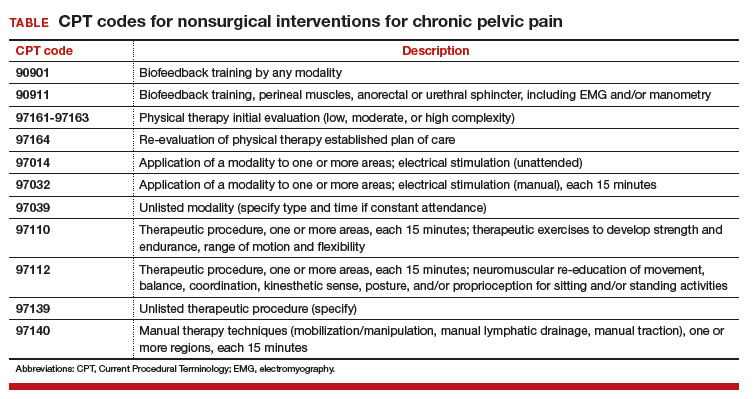
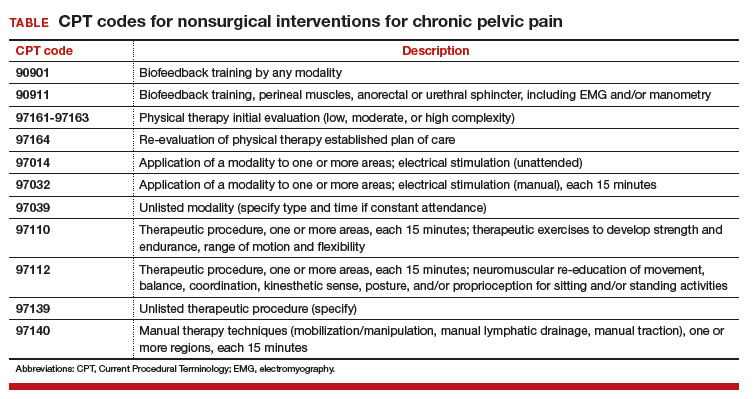
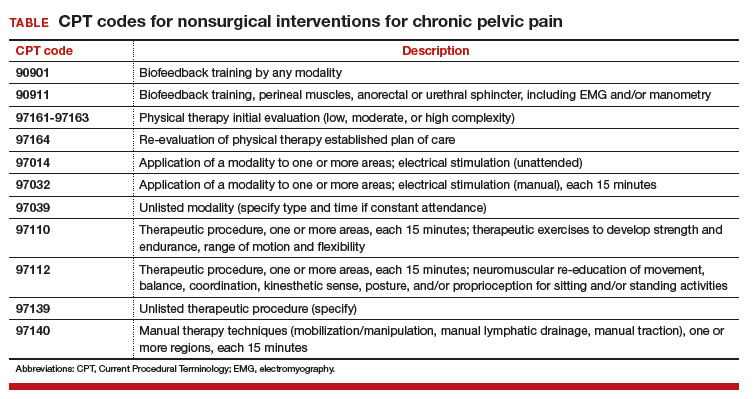
The TABLE shows typical Current Procedural Terminology (CPT) codes that might be authorized by the payer for this type of management.
Timed codes
Keep in mind that the “timed” codes listed above are based on the provider’s time spent one-on-one in direct contact with the patient. The time must have been used to provide skilled services and includes pre-, intra-, and posttreatment. CPT also has clarified that if “less than 15 minutes of service is provided, then the reduced services modifier -52 should be appended to the code to identify the reduction of service.” It will therefore be important that the provider accurately document the time involved in the therapy session for these codes.
Trigger point injections
Another treatment option is the use of trigger point injections to control pelvic pain. CPT provides 2 codes to report these:
- 20552, Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s)
- 20553, Injection(s); single or multiple trigger point(s), 3 or more muscles.
Notice that the choice of code depends on the number of muscles the anesthetic is injected into, not the number of injections given at that muscle site.
The relative values units assigned to these codes are based on the injection procedure alone. Normally, the anesthetic used (lidocaine or bupivacaine) can be billed in addition; however, there are no specific Healthcare Common Procedure Coding System (HCPCS) “J” codes for either. Code J2001, Injection, lidocaine HCl, can only be reported for an intravenous infusion, not intramuscular, and the only current code for bupivacaine is an “S” code that is only recognized by some Blue Cross/Blue Shield payers (S0020, Injection, bupivacaine HCl, 30 ml).
Some physicians also inject sodium bicarbonate, but this, too, has no specific “J” code. Because of this, the only correct J code to report these drugs will be J3490, Unclassified drugs. Be sure to include the National Drug Code (NDC) number (usually found on the package insert) for each drug, and an invoice showing your cost with the claim.
ICD-10-CM codes needed for support
Billing for services will not be complete without a supporting diagnostic code. For pelvic pain in particular, 1 or more of the following ICD-10-CM codes may provide the medical justification for the provided nonsurgical services so long as there are no identified psychological factors:
- G89.0, Central pain syndrome
- G89.29, Other chronic pain
- N94.10, Unspecified dyspareunia
- N94.11, Superficial (introital) dyspareunia
- N94.12, Deep dyspareunia
- N94.19, Other specified dyspareunia
- N94.2, Vaginismus
- N94.4, Primary dysmenorrhea
- N94.5, Secondary dysmenorrhea
- N94.6, Dysmenorrhea, unspecified
- N94.810, Vulvar vestibulitis
- N94.818, Other vulvodynia
- N94.819, Vulvodynia, unspecified
- R10.2, Pelvic and perineal pain.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Nonsurgical interventions for chronic pelvic pain may include evaluation and management visits for managing medications, trigger point injections, or pelvic floor physical therapy. However, while these management options can be coded, some of them may have limitations imposed by payers on the frequency of care and by whom the care may be rendered.
For encounters that involve the management of pain medications, it is important that documentation for each of these visits clearly spells out the progress the patient is making in setting goals for pain management. Frequent office visits may send a flag to the payer for overutilization; complete documentation will go a long way to support the medical necessity of each visit at the level billed.
Who renders treatment?
Sometimes, chronic pelvic pain management involves pelvic floor physical therapy, such as teaching pelvic floor exercises or using biofeedback to control certain aspects of the pain. The majority of payers have strict guidelines dictating who can render these services by way of licensure and training if performed by someone other than the physician, and at what frequency. Typically, the person performing the therapy must be, at minimum, a licensed physical therapist.
Frequency
Frequency is often limited to 1 to 2 times a week in increments of 4 weeks before additional authorization is granted. Again, careful and detailed documentation of the patient’s progress will be crucial to continued therapy.
The TABLE shows typical Current Procedural Terminology (CPT) codes that might be authorized by the payer for this type of management.
Timed codes
Keep in mind that the “timed” codes listed above are based on the provider’s time spent one-on-one in direct contact with the patient. The time must have been used to provide skilled services and includes pre-, intra-, and posttreatment. CPT also has clarified that if “less than 15 minutes of service is provided, then the reduced services modifier -52 should be appended to the code to identify the reduction of service.” It will therefore be important that the provider accurately document the time involved in the therapy session for these codes.
Trigger point injections
Another treatment option is the use of trigger point injections to control pelvic pain. CPT provides 2 codes to report these:
- 20552, Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s)
- 20553, Injection(s); single or multiple trigger point(s), 3 or more muscles.
Notice that the choice of code depends on the number of muscles the anesthetic is injected into, not the number of injections given at that muscle site.
The relative values units assigned to these codes are based on the injection procedure alone. Normally, the anesthetic used (lidocaine or bupivacaine) can be billed in addition; however, there are no specific Healthcare Common Procedure Coding System (HCPCS) “J” codes for either. Code J2001, Injection, lidocaine HCl, can only be reported for an intravenous infusion, not intramuscular, and the only current code for bupivacaine is an “S” code that is only recognized by some Blue Cross/Blue Shield payers (S0020, Injection, bupivacaine HCl, 30 ml).
Some physicians also inject sodium bicarbonate, but this, too, has no specific “J” code. Because of this, the only correct J code to report these drugs will be J3490, Unclassified drugs. Be sure to include the National Drug Code (NDC) number (usually found on the package insert) for each drug, and an invoice showing your cost with the claim.
ICD-10-CM codes needed for support
Billing for services will not be complete without a supporting diagnostic code. For pelvic pain in particular, 1 or more of the following ICD-10-CM codes may provide the medical justification for the provided nonsurgical services so long as there are no identified psychological factors:
- G89.0, Central pain syndrome
- G89.29, Other chronic pain
- N94.10, Unspecified dyspareunia
- N94.11, Superficial (introital) dyspareunia
- N94.12, Deep dyspareunia
- N94.19, Other specified dyspareunia
- N94.2, Vaginismus
- N94.4, Primary dysmenorrhea
- N94.5, Secondary dysmenorrhea
- N94.6, Dysmenorrhea, unspecified
- N94.810, Vulvar vestibulitis
- N94.818, Other vulvodynia
- N94.819, Vulvodynia, unspecified
- R10.2, Pelvic and perineal pain.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Nonsurgical interventions for chronic pelvic pain may include evaluation and management visits for managing medications, trigger point injections, or pelvic floor physical therapy. However, while these management options can be coded, some of them may have limitations imposed by payers on the frequency of care and by whom the care may be rendered.
For encounters that involve the management of pain medications, it is important that documentation for each of these visits clearly spells out the progress the patient is making in setting goals for pain management. Frequent office visits may send a flag to the payer for overutilization; complete documentation will go a long way to support the medical necessity of each visit at the level billed.
Who renders treatment?
Sometimes, chronic pelvic pain management involves pelvic floor physical therapy, such as teaching pelvic floor exercises or using biofeedback to control certain aspects of the pain. The majority of payers have strict guidelines dictating who can render these services by way of licensure and training if performed by someone other than the physician, and at what frequency. Typically, the person performing the therapy must be, at minimum, a licensed physical therapist.
Frequency
Frequency is often limited to 1 to 2 times a week in increments of 4 weeks before additional authorization is granted. Again, careful and detailed documentation of the patient’s progress will be crucial to continued therapy.
The TABLE shows typical Current Procedural Terminology (CPT) codes that might be authorized by the payer for this type of management.
Timed codes
Keep in mind that the “timed” codes listed above are based on the provider’s time spent one-on-one in direct contact with the patient. The time must have been used to provide skilled services and includes pre-, intra-, and posttreatment. CPT also has clarified that if “less than 15 minutes of service is provided, then the reduced services modifier -52 should be appended to the code to identify the reduction of service.” It will therefore be important that the provider accurately document the time involved in the therapy session for these codes.
Trigger point injections
Another treatment option is the use of trigger point injections to control pelvic pain. CPT provides 2 codes to report these:
- 20552, Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s)
- 20553, Injection(s); single or multiple trigger point(s), 3 or more muscles.
Notice that the choice of code depends on the number of muscles the anesthetic is injected into, not the number of injections given at that muscle site.
The relative values units assigned to these codes are based on the injection procedure alone. Normally, the anesthetic used (lidocaine or bupivacaine) can be billed in addition; however, there are no specific Healthcare Common Procedure Coding System (HCPCS) “J” codes for either. Code J2001, Injection, lidocaine HCl, can only be reported for an intravenous infusion, not intramuscular, and the only current code for bupivacaine is an “S” code that is only recognized by some Blue Cross/Blue Shield payers (S0020, Injection, bupivacaine HCl, 30 ml).
Some physicians also inject sodium bicarbonate, but this, too, has no specific “J” code. Because of this, the only correct J code to report these drugs will be J3490, Unclassified drugs. Be sure to include the National Drug Code (NDC) number (usually found on the package insert) for each drug, and an invoice showing your cost with the claim.
ICD-10-CM codes needed for support
Billing for services will not be complete without a supporting diagnostic code. For pelvic pain in particular, 1 or more of the following ICD-10-CM codes may provide the medical justification for the provided nonsurgical services so long as there are no identified psychological factors:
- G89.0, Central pain syndrome
- G89.29, Other chronic pain
- N94.10, Unspecified dyspareunia
- N94.11, Superficial (introital) dyspareunia
- N94.12, Deep dyspareunia
- N94.19, Other specified dyspareunia
- N94.2, Vaginismus
- N94.4, Primary dysmenorrhea
- N94.5, Secondary dysmenorrhea
- N94.6, Dysmenorrhea, unspecified
- N94.810, Vulvar vestibulitis
- N94.818, Other vulvodynia
- N94.819, Vulvodynia, unspecified
- R10.2, Pelvic and perineal pain.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
New Medicare cards
By now, you are probably aware that . The new, completely random number-letter combinations – dubbed Medicare Beneficiary Identifiers (MBI) – replace the old Social Security number–based Health Insurance Claim Numbers (HICN). The idea is to make citizens’ private information less vulnerable to identity thieves and other nefarious parties.
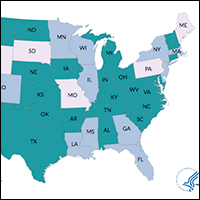
The switch began on April 1, and is expected to take about a year as the CMS processes about half a dozen states at a time. As I write this (at the beginning of May), the CMS is mailing out the first group of new cards to patients in Pennsylvania, Virginia, West Virginia, Maryland, Delaware, and the District of Columbia. But regardless of where you practice, you can expect to start seeing MBIs in your office soon – if you haven’t already – because people enrolling in Medicare for the first time are also receiving the new cards, no matter where they live.
Unlike the abrupt switch in 2015 from ICD-9 coding to ICD-10, this changeover has a transition period: Both HICNs and MBIs can be used on all billing and Medicare transactions from now until the end of 2019; after that, only claims with MBIs will be accepted. The last day of 2019 may sound like a long way off, but the time to get up to speed on everything MBI is now. That way, you can begin processing MBIs as soon as you start receiving them, and you will have time to solve any processing glitches well before the deadline.
First, you’ll need to make sure that your electronic health records and claims processing software will accept the new format, and that your electronic clearinghouse, if you use one, is geared up to accept and transmit the data on the new cards. Not all of them are. Some have been seduced by the year-and-a-half buffer – during which time HICNs can still be used – into dragging their feet on the MBI issue. Now is the time to find out if a vendor’s software is hard-wired to accept a maximum of 10 digits (MBIs have 11), not when your claims start bouncing.
Second, you will need to educate your front desk staff, so they will be able to recognize the new cards at a glance. Unfortunately, it looks a lot like the current card, though it is slightly smaller. It has the traditional red and blue colors with black printing, but there is no birthday or gender designation – again, in the interest of protecting patients’ identities. Knowing the difference will become particularly important after your state has been processed, when all of your Medicare patients should have the new card. Those who don’t will need to be identified and urged to get one before the December 2019 deadline.
Finally, once your staff and vendors are up to speed, you can begin educating your patients. Inevitably, some will not receive a new card, especially if they have moved and have not notified the CMS of the change; and some who are not expecting a new card will believe it is a duplicate, and throw it away. The CMS will be airing public service announcements and mailing education pieces to Medicare recipients, but a substantial portion of the education burden will fall on doctors and hospitals.
Have your front office staff remind patients to be sure their addresses are updated online with Medicare (www.Medicare.gov) or the Social Security Administration (www.ssa.gov). Encourage them to take advantage of the free resources available at www.cms.gov. These include both downloadable options and printed materials that illustrate what the new card will look like, explain how to update a mailing address with the Social Security Administration, and remind seniors to keep an eye out for their cards in the mail.
For the many Medicare-age patients who are not particularly computer savvy, the CMS has free resources for physicians as well. You will need to open an account at the agency’s Product Ordering website (productordering.cms.hhs.gov), which in turn needs to be approved by an administrator. The posters and other free literature can be displayed in your waiting room, exam rooms, and other “patient flow” areas. There is also a 1-minute video, downloadable from YouTube (https://youtu.be/DusRmgzQnLY), which can be looped in your waiting area.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
By now, you are probably aware that . The new, completely random number-letter combinations – dubbed Medicare Beneficiary Identifiers (MBI) – replace the old Social Security number–based Health Insurance Claim Numbers (HICN). The idea is to make citizens’ private information less vulnerable to identity thieves and other nefarious parties.
The switch began on April 1, and is expected to take about a year as the CMS processes about half a dozen states at a time. As I write this (at the beginning of May), the CMS is mailing out the first group of new cards to patients in Pennsylvania, Virginia, West Virginia, Maryland, Delaware, and the District of Columbia. But regardless of where you practice, you can expect to start seeing MBIs in your office soon – if you haven’t already – because people enrolling in Medicare for the first time are also receiving the new cards, no matter where they live.
Unlike the abrupt switch in 2015 from ICD-9 coding to ICD-10, this changeover has a transition period: Both HICNs and MBIs can be used on all billing and Medicare transactions from now until the end of 2019; after that, only claims with MBIs will be accepted. The last day of 2019 may sound like a long way off, but the time to get up to speed on everything MBI is now. That way, you can begin processing MBIs as soon as you start receiving them, and you will have time to solve any processing glitches well before the deadline.
First, you’ll need to make sure that your electronic health records and claims processing software will accept the new format, and that your electronic clearinghouse, if you use one, is geared up to accept and transmit the data on the new cards. Not all of them are. Some have been seduced by the year-and-a-half buffer – during which time HICNs can still be used – into dragging their feet on the MBI issue. Now is the time to find out if a vendor’s software is hard-wired to accept a maximum of 10 digits (MBIs have 11), not when your claims start bouncing.
Second, you will need to educate your front desk staff, so they will be able to recognize the new cards at a glance. Unfortunately, it looks a lot like the current card, though it is slightly smaller. It has the traditional red and blue colors with black printing, but there is no birthday or gender designation – again, in the interest of protecting patients’ identities. Knowing the difference will become particularly important after your state has been processed, when all of your Medicare patients should have the new card. Those who don’t will need to be identified and urged to get one before the December 2019 deadline.
Finally, once your staff and vendors are up to speed, you can begin educating your patients. Inevitably, some will not receive a new card, especially if they have moved and have not notified the CMS of the change; and some who are not expecting a new card will believe it is a duplicate, and throw it away. The CMS will be airing public service announcements and mailing education pieces to Medicare recipients, but a substantial portion of the education burden will fall on doctors and hospitals.
Have your front office staff remind patients to be sure their addresses are updated online with Medicare (www.Medicare.gov) or the Social Security Administration (www.ssa.gov). Encourage them to take advantage of the free resources available at www.cms.gov. These include both downloadable options and printed materials that illustrate what the new card will look like, explain how to update a mailing address with the Social Security Administration, and remind seniors to keep an eye out for their cards in the mail.
For the many Medicare-age patients who are not particularly computer savvy, the CMS has free resources for physicians as well. You will need to open an account at the agency’s Product Ordering website (productordering.cms.hhs.gov), which in turn needs to be approved by an administrator. The posters and other free literature can be displayed in your waiting room, exam rooms, and other “patient flow” areas. There is also a 1-minute video, downloadable from YouTube (https://youtu.be/DusRmgzQnLY), which can be looped in your waiting area.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
By now, you are probably aware that . The new, completely random number-letter combinations – dubbed Medicare Beneficiary Identifiers (MBI) – replace the old Social Security number–based Health Insurance Claim Numbers (HICN). The idea is to make citizens’ private information less vulnerable to identity thieves and other nefarious parties.
The switch began on April 1, and is expected to take about a year as the CMS processes about half a dozen states at a time. As I write this (at the beginning of May), the CMS is mailing out the first group of new cards to patients in Pennsylvania, Virginia, West Virginia, Maryland, Delaware, and the District of Columbia. But regardless of where you practice, you can expect to start seeing MBIs in your office soon – if you haven’t already – because people enrolling in Medicare for the first time are also receiving the new cards, no matter where they live.
Unlike the abrupt switch in 2015 from ICD-9 coding to ICD-10, this changeover has a transition period: Both HICNs and MBIs can be used on all billing and Medicare transactions from now until the end of 2019; after that, only claims with MBIs will be accepted. The last day of 2019 may sound like a long way off, but the time to get up to speed on everything MBI is now. That way, you can begin processing MBIs as soon as you start receiving them, and you will have time to solve any processing glitches well before the deadline.
First, you’ll need to make sure that your electronic health records and claims processing software will accept the new format, and that your electronic clearinghouse, if you use one, is geared up to accept and transmit the data on the new cards. Not all of them are. Some have been seduced by the year-and-a-half buffer – during which time HICNs can still be used – into dragging their feet on the MBI issue. Now is the time to find out if a vendor’s software is hard-wired to accept a maximum of 10 digits (MBIs have 11), not when your claims start bouncing.
Second, you will need to educate your front desk staff, so they will be able to recognize the new cards at a glance. Unfortunately, it looks a lot like the current card, though it is slightly smaller. It has the traditional red and blue colors with black printing, but there is no birthday or gender designation – again, in the interest of protecting patients’ identities. Knowing the difference will become particularly important after your state has been processed, when all of your Medicare patients should have the new card. Those who don’t will need to be identified and urged to get one before the December 2019 deadline.
Finally, once your staff and vendors are up to speed, you can begin educating your patients. Inevitably, some will not receive a new card, especially if they have moved and have not notified the CMS of the change; and some who are not expecting a new card will believe it is a duplicate, and throw it away. The CMS will be airing public service announcements and mailing education pieces to Medicare recipients, but a substantial portion of the education burden will fall on doctors and hospitals.
Have your front office staff remind patients to be sure their addresses are updated online with Medicare (www.Medicare.gov) or the Social Security Administration (www.ssa.gov). Encourage them to take advantage of the free resources available at www.cms.gov. These include both downloadable options and printed materials that illustrate what the new card will look like, explain how to update a mailing address with the Social Security Administration, and remind seniors to keep an eye out for their cards in the mail.
For the many Medicare-age patients who are not particularly computer savvy, the CMS has free resources for physicians as well. You will need to open an account at the agency’s Product Ordering website (productordering.cms.hhs.gov), which in turn needs to be approved by an administrator. The posters and other free literature can be displayed in your waiting room, exam rooms, and other “patient flow” areas. There is also a 1-minute video, downloadable from YouTube (https://youtu.be/DusRmgzQnLY), which can be looped in your waiting area.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
How to decide on purchasing new medical equipment
Providing state-of-the-art health care for women often requires the use of various types of medical equipment, and decisions regarding their purchase can be complicated. With rising costs and reduced reimbursements, capital expenditures must be made with great care. Some equipment may not generate revenue but is required at a basic care-giving level: examination tables, procedure instruments, autoclaves, etc. Conversely, other equipment may not be necessary but strongly desired to offer a full complement of care. Unfortunately, sometimes a decision to buy expensive equipment is based more on a sales representative's ability to rationalize the purchase as a sound investment than on its necessity or practicality. This article focuses on tools to help you make a decision to obtain revenue-generating medical equipment.
First consideration: Nonfinancial evaluation
Nonfinancial criteria should be your first concern. They may have a greater impact on your practice than any financial consideration.
Does this investment align with your overall goals?
If your focus is to provide the best and most efficient obstetric care in the community, it may not make sense to purchase urodynamic equipment, even if using the equipment could be profitable.1 If the equipment begins to distract the practice from its strategic focus, then complications from managing this new equipment might be more harmful than helpful.
What are the pros and cons of the investment?
Concern that the equipment may not be effective or may become obsolete in a few years would preclude having to consider the financial purchase in the first place.1
Consider a PESTLE analysis
Before starting a new project, use a PESTLE analysis to assess external factors that are political, economic, social, technological, legal, and environmental. Its purpose is to identify issues that are beyond the control of the organization and have some level of impact on the organization.2,3
If you are considering the purchase of a laser hair removal machine, what could be the political considerations, such as your reputation among peers or other physicians who refer patients to your practice? What are the economic (financial) considerations? How would the social (or marketing) message be communicated, and do you have the organizational skills to implement a marketing strategy? What are the technical challenges required for maintaining this machine, and how much skill and training would be required to safely use it? What are the legal ramifications for implementing this service? Does your malpractice insurance cover it? And finally, what kind of environment (physical space) would be required?
What alternative investment opportunities might compete?
When considering a significant investment, other opportunities may no longer be feasible. Think about other ways your practice could use the money and which investment prospects would be the best fit.1 For instance, purchasing equipment that is very time intensive may not necessarily be the most profitable decision, especially if it takes the provider away from other services with higher margins. Could investing in expensive equipment delay bringing in another provider who might have a higher financial impact?
Next stage: Financial evaluation
To begin a basic cash flow analysis of the new investment, gather your practice's financial data. Estimate the cash flow resulting from the equipment investment, including any additional expenses and revenues. Here are some steps:
- Identify the revenue generated by each use of the equipment.
- Estimate the variable costs (costs that increase with each incremental unit of activity). Variable costs include expenses associated with each use, such as disposable accessories. For a hysteroscope, the variable cost may be the tubing and fluid used. Some procedures, such as office hysteroscopic sterilization, require the purchase of intratubal occlusion devices.
Also consider the cost of your time. One way to determine this is to investigate the hourly rate you would be paid if you were hypothetically hired by a third party to perform the procedure.
- Estimate the step costs. Step costs are constant over a narrow range of activity but shift to a higher level with increased activity. One example is staffing costs. If the number of these procedures significantly increases, additional staffing will be required. Include the hourly pay for your medical assistants in the analysis.
- Determine the contribution margin. Subtract the revenue from the sum of the variable and step costs to find the contribution margin (dollar contribution per unit) to your practice.4,5
- Estimate the approximate volume of procedures. It is hard to predict future demand, but a good rule of thumb is to estimate the best, expected, and pessimistic volumes. Then average the 3 scenarios and use that figure as the anticipated volume. Multiply the volume by the contribution margin to calculate profit.
Additional financial tools
Once the basic cash flow analysis of the new investment is undertaken, add these methods to your analysis:
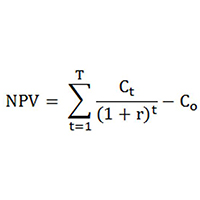
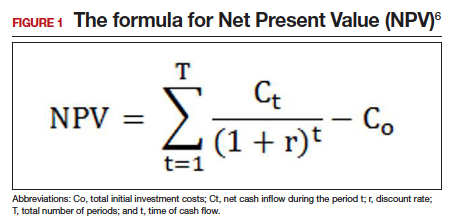
Net Present Value (NPV) is the difference between the present value of cash inflows and the present value of cash outflows (FIGURE 1).6 NPV takes into consideration the time value of money, where money in the present is worth more than the same value sometime in the future due to inflation and earning capacity. NPV is used in capital budgeting to analyze the profitability of a projected investment or project.1,4,5
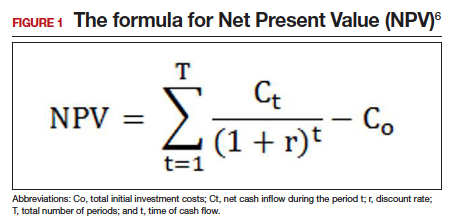
Consider the discount rate as the expected rate of return or cost of capital. By discounting the future cash flow each year by the discount rate, you can get the present value of cash flow. Subtract the present value of cash flow from the original investment to get the NPV for the equipment's investment. A positive value is a favorable analysis to purchase the equipment; a negative value may suggest that the equipment may be a poor investment.
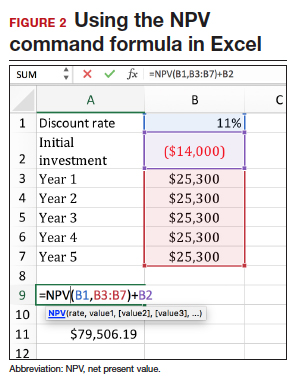
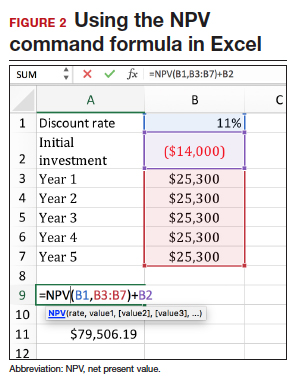
The NPV can be calculated in a spreadsheet using the following NPV command formula: NPV(rate,value1,[value2],...). This formula gives you the present value of cash inflows. The rate is the discount rate and the values are the series of cash flows occurring over a period of time. The NPV command formula in Excel, despite its misleading name, only gives the present value of cash flows.7 Therefore, it is important that the present value of cash inflows is subtracted from the initial capital investment to get the NPV.
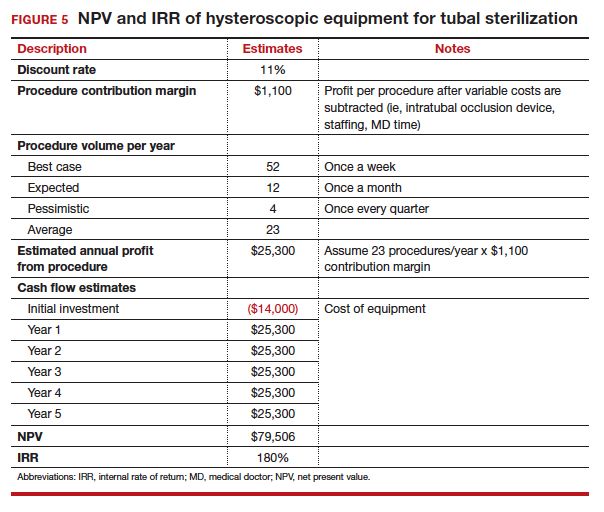
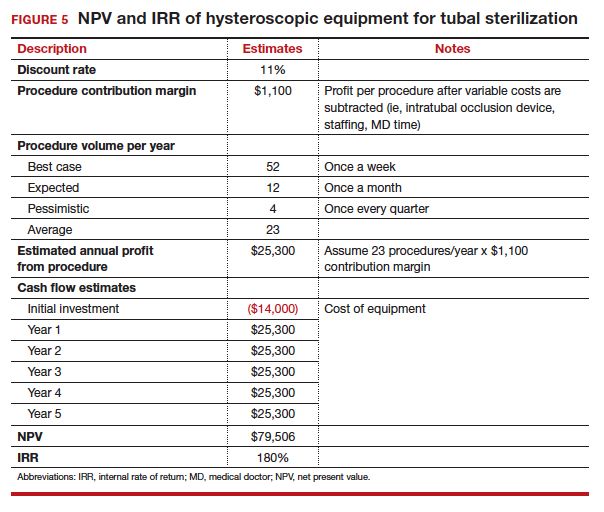
FIGURE 2 shows analysis of a piece of equipment that requires a $14,000 initial investment in Year 0. Each year the use of the equipment generates $25,300 per year through year 5. Assign a discount rate of 11%, about what you would expect for a stock market investment.
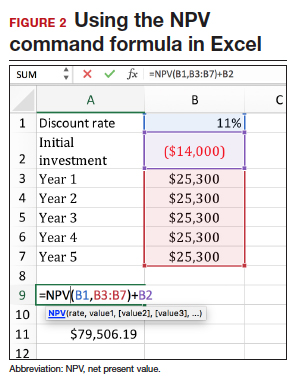
Consider other investment opportunities. The historical rate of return for a stock index fund is 11.5%.8 Using this discount rate, you can compare whether the money would be better invested in the medical equipment or stock.
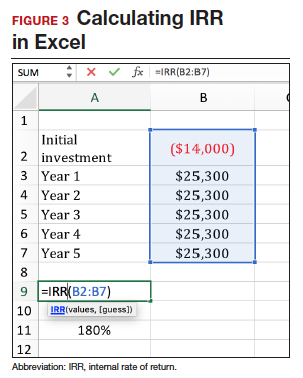
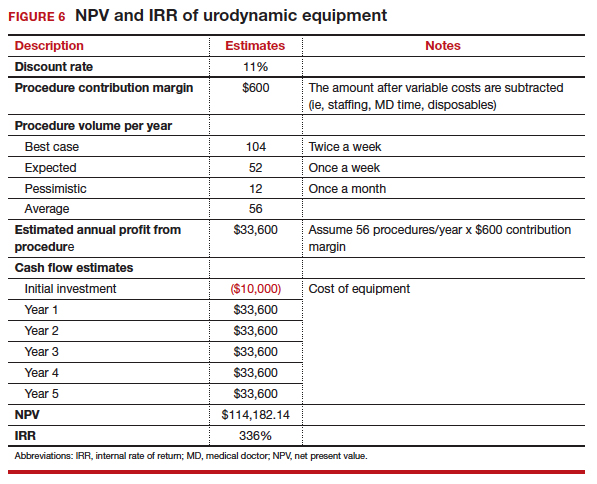
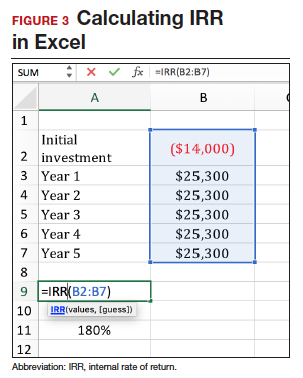
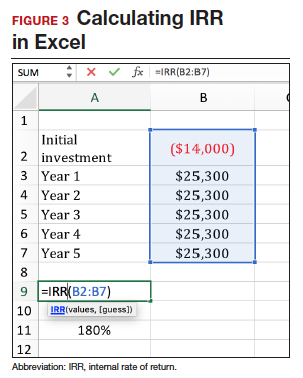
Internal rate of return (IRR) is a metric used in capital budgeting to measure the profitability of potential investments. The IRR determines if the discount rate at which the present value of expected net cash inflow is equal to the cash outlay. In other words, the IRR is the discount rate that makes the net present cash flows from a project equal zero. The decision rule related to the IRR criterion is to accept a project in which the IRR is greater than the required rate of return (cutoff rate). The formula for the IRR is the same as the NPV formula, except that the NPV is set at zero and the discount rate is calculated through iterative calculation. The IRR can be calculated in a spreadsheet using the following command formula: IRR(values, [guess]).1,5,9 In FIGURE 3, the IRR is 180%, far superior than the return you would find in other investments such as the stock market.
The IRR is somewhat different from return on investment (ROI). ROI is the percent of return on the initial investment over a period of time. Each piece of equipment has a different ROI over a different time period. ROI does not take into account the time value of money (TVM). Incorporating the IRR (or the TVM) allows for equal comparison between 2 pieces of equipment in the analysis.10
If you are not comparing 2 different types of equipment for purchase, then using the cutoff of 11.5% may be helpful (the historical average stock market return). If the IRR is less than 11.5%, then in theory, it would be better to put your money in the stock market than in new equipment.7
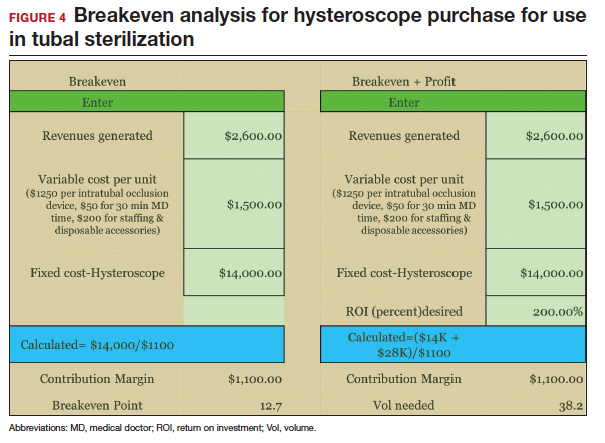
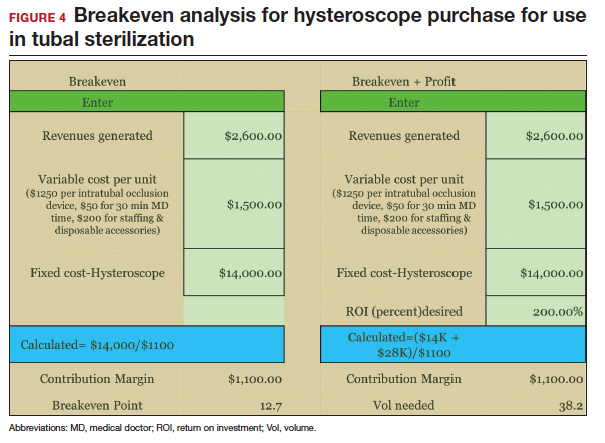
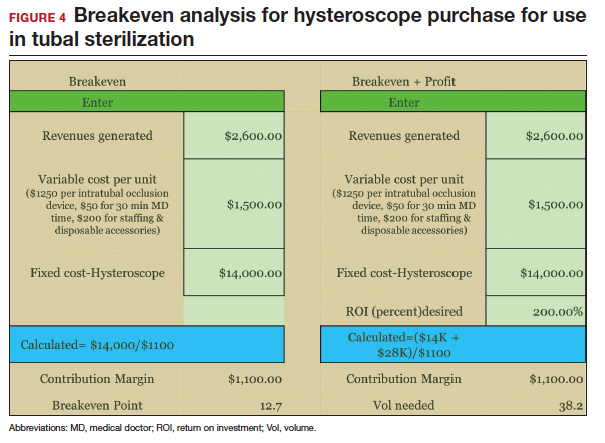
Breakeven analysis calculates the volume of procedures that would be needed to break even or make a profit. It can also determine if there is enough demand to meet the volume required to break even or profit. Unlike the first 2 methods, where you have to guess at future volume, this method calculates the volume required to break even, but does not specify a time period. Your practice would have to use subjective experience to determine how long it would take to reach that volume, given your patient population and the ability to reach the targeted market segment.
Fixed costs are costs that do not change with the varying volume of units of service or products sold. After calculating the contribution margin, divide the fixed costs of the equipment by the contribution margin. Then you will have the volume required to break even (FIGURE 4). Add the dollar amount of profit you would like to attain to the fixed costs, then divide that total by the contribution margin, and you'll have the volume required to meet those specifications.1,4,5
Even though the calculations described above relate to medical equipment, you can use this same method to analyze the cost of adding new providers or any other business development project to determine the required volume to break even on the capital outlay.
CASE New equipment requests
A new ObGyn in your practice requests that you purchase a hysteroscope so that she can start performing office-based hysteroscopic sterilization. Another partner would like to acquire urodynamic equipment instead of referring urinary incontinent patients to a urogynecologist. How do you decide what to purchase?
First calculate the contribution margins for each product. Next, since you do not know for certain the volume you might achieve for each procedure, create 3 scenarios for the best, expected, and pessimistic situations. Assume equal probability for each of these categories and average the volumes of the estimates. Even though you may keep the equipment longer, estimate the financial analysis over 5 years. In this example, we assume a discount rate of 11% for the NPV calculation for both pieces of equipment.
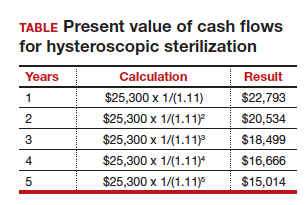
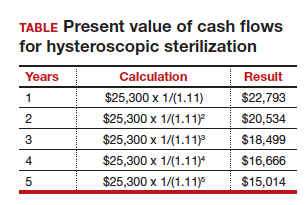
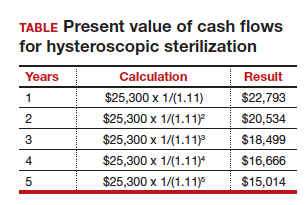
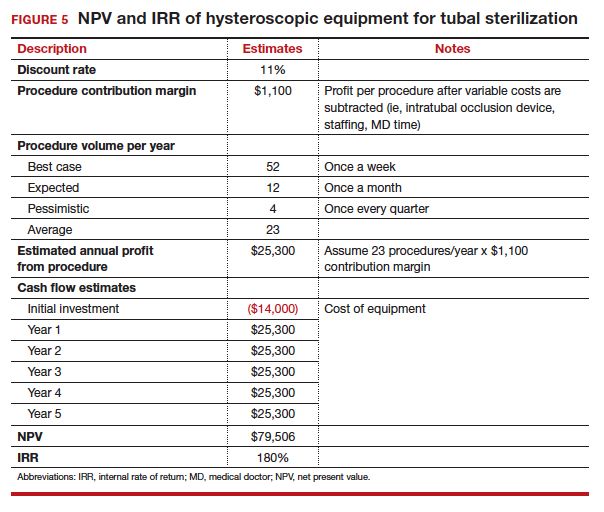
Calculate the IRR using a spreadsheet based on the cash flow for each piece of equipment. Say that the practice anticipates doing 23 hysteroscopic sterilizations per year. If the reimbursement is $2,600 per procedure, and the variable costs are $1,500, the contribution margin is $1,100. So 23 procedures multiplied by $1,100 equals an annual profit of $25,300. Then discount the $25,300 for each year. In this example, we use a discount rate of 11%. The TABLE shows the amount discounted each year.
The sum of the discounted cash flows is $93,506. However, we have to subtract the initial investment of $14,000, so the final NPV equals $79,506 (FIGURE 5).
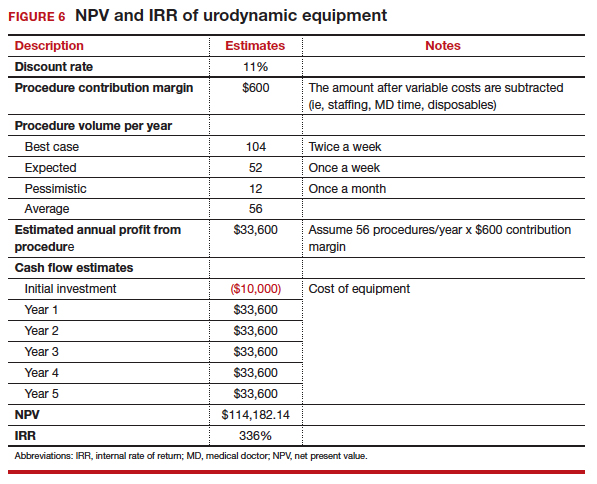
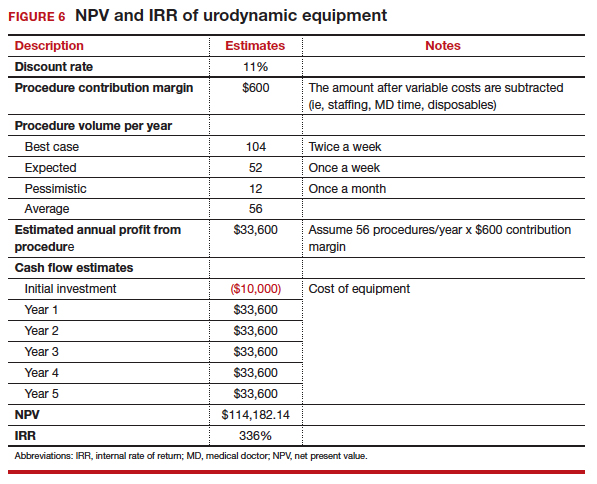
Apply the same financial NPV and IRR calculations used to assess the hysteroscope to the urodynamic equipment. From the analysis (FIGUREs 5 and 6), both purchases would be financially successful. However, it appears that the urodynamic equipment is a superior investment over the hysteroscope, with a higher NPV ($115,877 vs $81,880, respectively) and IRR (336% vs 180%, respectively). This is likely due to the higher anticipated volume of use with the urodynamic equipment and lower cost of initial investment, despite having a lower contribution margin than the hysteroscope.
Caveats
For simplicity, this analysis does not account for the fact that the hysteroscope could be used for other revenue-generating procedures such as diagnostic hysteroscopy. Factoring in these potential additional services using the same hysteroscope might change the decision analysis in favor of the hysteroscope.
Remember that, although the financial analysis is very helpful in decision making, nonfinancial evaluations should also influence your choice. In this example, while there may be a financial advantage to purchasing the urodynamic equipment over the hysteroscopic equipment, nonfinancial considerations can help you decide which purchase would be a better aligned with the goals and strategies of your practice.
These tools for nonfinancial and financial analysis can be used for any investment in your practice, whether it is in medical equipment, personnel, or development of other profit centers.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Willis DR. How to decide whether to buy new medical equipment. Fam Pract Manag. 2004;11(3):53−58.
- PESTLE Analysis Strategy Skills. http://www.free-management-ebooks.com/dldebk-pdf/fme-pestle-analysis.pdf. Published 2013. Accessed March 2, 2018.
- What is PESTLE analysis? A tool for business analysis. http://pestleanalysis.com/what-is-pestle-analysis/. Published 2018. Accessed March 2, 2018.
- Nowicki M, ed. Introduction to the Financial Management of Healthcare Organizations. 6th ed. Chicago, Illinois: Health Administration Press; 2014:150−151, 299−316.
- Ross SA, Westerfield RW, Jaffe J. Corporate Finance. 8th ed. New York, New York: McGraw Hill; 2008:271−288.
- Net Present Value - NPV. Investopia. https://www.investopedia.com/terms/n/npv.asp. Accessed April 10, 2018.
- NPV function. Microsoft Office Support. https://support.office.com/en-us/article/npv-function-8672cb67-2576-4d07-b67b-ac28acf2a568. Accessed April 10, 2018.
- Damodaran A. Annual Returns on Stock, T.Bonds and T.Bills: 1928 - Current. http://pages.stern.nyu.edu/~adamodar/New_Home_Page/datafile/histretSP.html. Updated January 5, 2018. Accessed March 2, 2018.
- IRR function. Microsoft Office Support. https://support.office.com/en-us/article/irr-function-64925eaa-9988-495b-b290-3ad0c163c1bc. Accessed April 10, 2018.
- Time Value of Money (TVM). Investopedia. https://www.investopedia.com/terms/t/timevalueofmoney.asp. Published 2018. Accessed March 2, 2018.
Providing state-of-the-art health care for women often requires the use of various types of medical equipment, and decisions regarding their purchase can be complicated. With rising costs and reduced reimbursements, capital expenditures must be made with great care. Some equipment may not generate revenue but is required at a basic care-giving level: examination tables, procedure instruments, autoclaves, etc. Conversely, other equipment may not be necessary but strongly desired to offer a full complement of care. Unfortunately, sometimes a decision to buy expensive equipment is based more on a sales representative's ability to rationalize the purchase as a sound investment than on its necessity or practicality. This article focuses on tools to help you make a decision to obtain revenue-generating medical equipment.
First consideration: Nonfinancial evaluation
Nonfinancial criteria should be your first concern. They may have a greater impact on your practice than any financial consideration.
Does this investment align with your overall goals?
If your focus is to provide the best and most efficient obstetric care in the community, it may not make sense to purchase urodynamic equipment, even if using the equipment could be profitable.1 If the equipment begins to distract the practice from its strategic focus, then complications from managing this new equipment might be more harmful than helpful.
What are the pros and cons of the investment?
Concern that the equipment may not be effective or may become obsolete in a few years would preclude having to consider the financial purchase in the first place.1
Consider a PESTLE analysis
Before starting a new project, use a PESTLE analysis to assess external factors that are political, economic, social, technological, legal, and environmental. Its purpose is to identify issues that are beyond the control of the organization and have some level of impact on the organization.2,3
If you are considering the purchase of a laser hair removal machine, what could be the political considerations, such as your reputation among peers or other physicians who refer patients to your practice? What are the economic (financial) considerations? How would the social (or marketing) message be communicated, and do you have the organizational skills to implement a marketing strategy? What are the technical challenges required for maintaining this machine, and how much skill and training would be required to safely use it? What are the legal ramifications for implementing this service? Does your malpractice insurance cover it? And finally, what kind of environment (physical space) would be required?
What alternative investment opportunities might compete?
When considering a significant investment, other opportunities may no longer be feasible. Think about other ways your practice could use the money and which investment prospects would be the best fit.1 For instance, purchasing equipment that is very time intensive may not necessarily be the most profitable decision, especially if it takes the provider away from other services with higher margins. Could investing in expensive equipment delay bringing in another provider who might have a higher financial impact?
Next stage: Financial evaluation
To begin a basic cash flow analysis of the new investment, gather your practice's financial data. Estimate the cash flow resulting from the equipment investment, including any additional expenses and revenues. Here are some steps:
- Identify the revenue generated by each use of the equipment.
- Estimate the variable costs (costs that increase with each incremental unit of activity). Variable costs include expenses associated with each use, such as disposable accessories. For a hysteroscope, the variable cost may be the tubing and fluid used. Some procedures, such as office hysteroscopic sterilization, require the purchase of intratubal occlusion devices.
Also consider the cost of your time. One way to determine this is to investigate the hourly rate you would be paid if you were hypothetically hired by a third party to perform the procedure.
- Estimate the step costs. Step costs are constant over a narrow range of activity but shift to a higher level with increased activity. One example is staffing costs. If the number of these procedures significantly increases, additional staffing will be required. Include the hourly pay for your medical assistants in the analysis.
- Determine the contribution margin. Subtract the revenue from the sum of the variable and step costs to find the contribution margin (dollar contribution per unit) to your practice.4,5
- Estimate the approximate volume of procedures. It is hard to predict future demand, but a good rule of thumb is to estimate the best, expected, and pessimistic volumes. Then average the 3 scenarios and use that figure as the anticipated volume. Multiply the volume by the contribution margin to calculate profit.
Additional financial tools
Once the basic cash flow analysis of the new investment is undertaken, add these methods to your analysis:
Net Present Value (NPV) is the difference between the present value of cash inflows and the present value of cash outflows (FIGURE 1).6 NPV takes into consideration the time value of money, where money in the present is worth more than the same value sometime in the future due to inflation and earning capacity. NPV is used in capital budgeting to analyze the profitability of a projected investment or project.1,4,5
Consider the discount rate as the expected rate of return or cost of capital. By discounting the future cash flow each year by the discount rate, you can get the present value of cash flow. Subtract the present value of cash flow from the original investment to get the NPV for the equipment's investment. A positive value is a favorable analysis to purchase the equipment; a negative value may suggest that the equipment may be a poor investment.
The NPV can be calculated in a spreadsheet using the following NPV command formula: NPV(rate,value1,[value2],...). This formula gives you the present value of cash inflows. The rate is the discount rate and the values are the series of cash flows occurring over a period of time. The NPV command formula in Excel, despite its misleading name, only gives the present value of cash flows.7 Therefore, it is important that the present value of cash inflows is subtracted from the initial capital investment to get the NPV.
FIGURE 2 shows analysis of a piece of equipment that requires a $14,000 initial investment in Year 0. Each year the use of the equipment generates $25,300 per year through year 5. Assign a discount rate of 11%, about what you would expect for a stock market investment.
Consider other investment opportunities. The historical rate of return for a stock index fund is 11.5%.8 Using this discount rate, you can compare whether the money would be better invested in the medical equipment or stock.
Internal rate of return (IRR) is a metric used in capital budgeting to measure the profitability of potential investments. The IRR determines if the discount rate at which the present value of expected net cash inflow is equal to the cash outlay. In other words, the IRR is the discount rate that makes the net present cash flows from a project equal zero. The decision rule related to the IRR criterion is to accept a project in which the IRR is greater than the required rate of return (cutoff rate). The formula for the IRR is the same as the NPV formula, except that the NPV is set at zero and the discount rate is calculated through iterative calculation. The IRR can be calculated in a spreadsheet using the following command formula: IRR(values, [guess]).1,5,9 In FIGURE 3, the IRR is 180%, far superior than the return you would find in other investments such as the stock market.
The IRR is somewhat different from return on investment (ROI). ROI is the percent of return on the initial investment over a period of time. Each piece of equipment has a different ROI over a different time period. ROI does not take into account the time value of money (TVM). Incorporating the IRR (or the TVM) allows for equal comparison between 2 pieces of equipment in the analysis.10
If you are not comparing 2 different types of equipment for purchase, then using the cutoff of 11.5% may be helpful (the historical average stock market return). If the IRR is less than 11.5%, then in theory, it would be better to put your money in the stock market than in new equipment.7
Breakeven analysis calculates the volume of procedures that would be needed to break even or make a profit. It can also determine if there is enough demand to meet the volume required to break even or profit. Unlike the first 2 methods, where you have to guess at future volume, this method calculates the volume required to break even, but does not specify a time period. Your practice would have to use subjective experience to determine how long it would take to reach that volume, given your patient population and the ability to reach the targeted market segment.
Fixed costs are costs that do not change with the varying volume of units of service or products sold. After calculating the contribution margin, divide the fixed costs of the equipment by the contribution margin. Then you will have the volume required to break even (FIGURE 4). Add the dollar amount of profit you would like to attain to the fixed costs, then divide that total by the contribution margin, and you'll have the volume required to meet those specifications.1,4,5
Even though the calculations described above relate to medical equipment, you can use this same method to analyze the cost of adding new providers or any other business development project to determine the required volume to break even on the capital outlay.
CASE New equipment requests
A new ObGyn in your practice requests that you purchase a hysteroscope so that she can start performing office-based hysteroscopic sterilization. Another partner would like to acquire urodynamic equipment instead of referring urinary incontinent patients to a urogynecologist. How do you decide what to purchase?
First calculate the contribution margins for each product. Next, since you do not know for certain the volume you might achieve for each procedure, create 3 scenarios for the best, expected, and pessimistic situations. Assume equal probability for each of these categories and average the volumes of the estimates. Even though you may keep the equipment longer, estimate the financial analysis over 5 years. In this example, we assume a discount rate of 11% for the NPV calculation for both pieces of equipment.
Calculate the IRR using a spreadsheet based on the cash flow for each piece of equipment. Say that the practice anticipates doing 23 hysteroscopic sterilizations per year. If the reimbursement is $2,600 per procedure, and the variable costs are $1,500, the contribution margin is $1,100. So 23 procedures multiplied by $1,100 equals an annual profit of $25,300. Then discount the $25,300 for each year. In this example, we use a discount rate of 11%. The TABLE shows the amount discounted each year.
The sum of the discounted cash flows is $93,506. However, we have to subtract the initial investment of $14,000, so the final NPV equals $79,506 (FIGURE 5).
Apply the same financial NPV and IRR calculations used to assess the hysteroscope to the urodynamic equipment. From the analysis (FIGUREs 5 and 6), both purchases would be financially successful. However, it appears that the urodynamic equipment is a superior investment over the hysteroscope, with a higher NPV ($115,877 vs $81,880, respectively) and IRR (336% vs 180%, respectively). This is likely due to the higher anticipated volume of use with the urodynamic equipment and lower cost of initial investment, despite having a lower contribution margin than the hysteroscope.
Caveats
For simplicity, this analysis does not account for the fact that the hysteroscope could be used for other revenue-generating procedures such as diagnostic hysteroscopy. Factoring in these potential additional services using the same hysteroscope might change the decision analysis in favor of the hysteroscope.
Remember that, although the financial analysis is very helpful in decision making, nonfinancial evaluations should also influence your choice. In this example, while there may be a financial advantage to purchasing the urodynamic equipment over the hysteroscopic equipment, nonfinancial considerations can help you decide which purchase would be a better aligned with the goals and strategies of your practice.
These tools for nonfinancial and financial analysis can be used for any investment in your practice, whether it is in medical equipment, personnel, or development of other profit centers.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Providing state-of-the-art health care for women often requires the use of various types of medical equipment, and decisions regarding their purchase can be complicated. With rising costs and reduced reimbursements, capital expenditures must be made with great care. Some equipment may not generate revenue but is required at a basic care-giving level: examination tables, procedure instruments, autoclaves, etc. Conversely, other equipment may not be necessary but strongly desired to offer a full complement of care. Unfortunately, sometimes a decision to buy expensive equipment is based more on a sales representative's ability to rationalize the purchase as a sound investment than on its necessity or practicality. This article focuses on tools to help you make a decision to obtain revenue-generating medical equipment.
First consideration: Nonfinancial evaluation
Nonfinancial criteria should be your first concern. They may have a greater impact on your practice than any financial consideration.
Does this investment align with your overall goals?
If your focus is to provide the best and most efficient obstetric care in the community, it may not make sense to purchase urodynamic equipment, even if using the equipment could be profitable.1 If the equipment begins to distract the practice from its strategic focus, then complications from managing this new equipment might be more harmful than helpful.
What are the pros and cons of the investment?
Concern that the equipment may not be effective or may become obsolete in a few years would preclude having to consider the financial purchase in the first place.1
Consider a PESTLE analysis
Before starting a new project, use a PESTLE analysis to assess external factors that are political, economic, social, technological, legal, and environmental. Its purpose is to identify issues that are beyond the control of the organization and have some level of impact on the organization.2,3
If you are considering the purchase of a laser hair removal machine, what could be the political considerations, such as your reputation among peers or other physicians who refer patients to your practice? What are the economic (financial) considerations? How would the social (or marketing) message be communicated, and do you have the organizational skills to implement a marketing strategy? What are the technical challenges required for maintaining this machine, and how much skill and training would be required to safely use it? What are the legal ramifications for implementing this service? Does your malpractice insurance cover it? And finally, what kind of environment (physical space) would be required?
What alternative investment opportunities might compete?
When considering a significant investment, other opportunities may no longer be feasible. Think about other ways your practice could use the money and which investment prospects would be the best fit.1 For instance, purchasing equipment that is very time intensive may not necessarily be the most profitable decision, especially if it takes the provider away from other services with higher margins. Could investing in expensive equipment delay bringing in another provider who might have a higher financial impact?
Next stage: Financial evaluation
To begin a basic cash flow analysis of the new investment, gather your practice's financial data. Estimate the cash flow resulting from the equipment investment, including any additional expenses and revenues. Here are some steps:
- Identify the revenue generated by each use of the equipment.
- Estimate the variable costs (costs that increase with each incremental unit of activity). Variable costs include expenses associated with each use, such as disposable accessories. For a hysteroscope, the variable cost may be the tubing and fluid used. Some procedures, such as office hysteroscopic sterilization, require the purchase of intratubal occlusion devices.
Also consider the cost of your time. One way to determine this is to investigate the hourly rate you would be paid if you were hypothetically hired by a third party to perform the procedure.
- Estimate the step costs. Step costs are constant over a narrow range of activity but shift to a higher level with increased activity. One example is staffing costs. If the number of these procedures significantly increases, additional staffing will be required. Include the hourly pay for your medical assistants in the analysis.
- Determine the contribution margin. Subtract the revenue from the sum of the variable and step costs to find the contribution margin (dollar contribution per unit) to your practice.4,5
- Estimate the approximate volume of procedures. It is hard to predict future demand, but a good rule of thumb is to estimate the best, expected, and pessimistic volumes. Then average the 3 scenarios and use that figure as the anticipated volume. Multiply the volume by the contribution margin to calculate profit.
Additional financial tools
Once the basic cash flow analysis of the new investment is undertaken, add these methods to your analysis:
Net Present Value (NPV) is the difference between the present value of cash inflows and the present value of cash outflows (FIGURE 1).6 NPV takes into consideration the time value of money, where money in the present is worth more than the same value sometime in the future due to inflation and earning capacity. NPV is used in capital budgeting to analyze the profitability of a projected investment or project.1,4,5
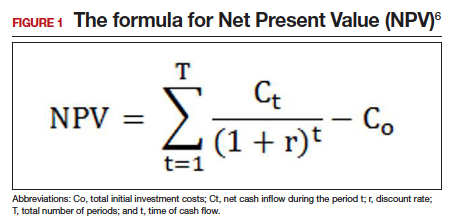
Consider the discount rate as the expected rate of return or cost of capital. By discounting the future cash flow each year by the discount rate, you can get the present value of cash flow. Subtract the present value of cash flow from the original investment to get the NPV for the equipment's investment. A positive value is a favorable analysis to purchase the equipment; a negative value may suggest that the equipment may be a poor investment.
The NPV can be calculated in a spreadsheet using the following NPV command formula: NPV(rate,value1,[value2],...). This formula gives you the present value of cash inflows. The rate is the discount rate and the values are the series of cash flows occurring over a period of time. The NPV command formula in Excel, despite its misleading name, only gives the present value of cash flows.7 Therefore, it is important that the present value of cash inflows is subtracted from the initial capital investment to get the NPV.
FIGURE 2 shows analysis of a piece of equipment that requires a $14,000 initial investment in Year 0. Each year the use of the equipment generates $25,300 per year through year 5. Assign a discount rate of 11%, about what you would expect for a stock market investment.
Consider other investment opportunities. The historical rate of return for a stock index fund is 11.5%.8 Using this discount rate, you can compare whether the money would be better invested in the medical equipment or stock.
Internal rate of return (IRR) is a metric used in capital budgeting to measure the profitability of potential investments. The IRR determines if the discount rate at which the present value of expected net cash inflow is equal to the cash outlay. In other words, the IRR is the discount rate that makes the net present cash flows from a project equal zero. The decision rule related to the IRR criterion is to accept a project in which the IRR is greater than the required rate of return (cutoff rate). The formula for the IRR is the same as the NPV formula, except that the NPV is set at zero and the discount rate is calculated through iterative calculation. The IRR can be calculated in a spreadsheet using the following command formula: IRR(values, [guess]).1,5,9 In FIGURE 3, the IRR is 180%, far superior than the return you would find in other investments such as the stock market.
The IRR is somewhat different from return on investment (ROI). ROI is the percent of return on the initial investment over a period of time. Each piece of equipment has a different ROI over a different time period. ROI does not take into account the time value of money (TVM). Incorporating the IRR (or the TVM) allows for equal comparison between 2 pieces of equipment in the analysis.10
If you are not comparing 2 different types of equipment for purchase, then using the cutoff of 11.5% may be helpful (the historical average stock market return). If the IRR is less than 11.5%, then in theory, it would be better to put your money in the stock market than in new equipment.7
Breakeven analysis calculates the volume of procedures that would be needed to break even or make a profit. It can also determine if there is enough demand to meet the volume required to break even or profit. Unlike the first 2 methods, where you have to guess at future volume, this method calculates the volume required to break even, but does not specify a time period. Your practice would have to use subjective experience to determine how long it would take to reach that volume, given your patient population and the ability to reach the targeted market segment.
Fixed costs are costs that do not change with the varying volume of units of service or products sold. After calculating the contribution margin, divide the fixed costs of the equipment by the contribution margin. Then you will have the volume required to break even (FIGURE 4). Add the dollar amount of profit you would like to attain to the fixed costs, then divide that total by the contribution margin, and you'll have the volume required to meet those specifications.1,4,5
Even though the calculations described above relate to medical equipment, you can use this same method to analyze the cost of adding new providers or any other business development project to determine the required volume to break even on the capital outlay.
CASE New equipment requests
A new ObGyn in your practice requests that you purchase a hysteroscope so that she can start performing office-based hysteroscopic sterilization. Another partner would like to acquire urodynamic equipment instead of referring urinary incontinent patients to a urogynecologist. How do you decide what to purchase?
First calculate the contribution margins for each product. Next, since you do not know for certain the volume you might achieve for each procedure, create 3 scenarios for the best, expected, and pessimistic situations. Assume equal probability for each of these categories and average the volumes of the estimates. Even though you may keep the equipment longer, estimate the financial analysis over 5 years. In this example, we assume a discount rate of 11% for the NPV calculation for both pieces of equipment.
Calculate the IRR using a spreadsheet based on the cash flow for each piece of equipment. Say that the practice anticipates doing 23 hysteroscopic sterilizations per year. If the reimbursement is $2,600 per procedure, and the variable costs are $1,500, the contribution margin is $1,100. So 23 procedures multiplied by $1,100 equals an annual profit of $25,300. Then discount the $25,300 for each year. In this example, we use a discount rate of 11%. The TABLE shows the amount discounted each year.
The sum of the discounted cash flows is $93,506. However, we have to subtract the initial investment of $14,000, so the final NPV equals $79,506 (FIGURE 5).
Apply the same financial NPV and IRR calculations used to assess the hysteroscope to the urodynamic equipment. From the analysis (FIGUREs 5 and 6), both purchases would be financially successful. However, it appears that the urodynamic equipment is a superior investment over the hysteroscope, with a higher NPV ($115,877 vs $81,880, respectively) and IRR (336% vs 180%, respectively). This is likely due to the higher anticipated volume of use with the urodynamic equipment and lower cost of initial investment, despite having a lower contribution margin than the hysteroscope.
Caveats
For simplicity, this analysis does not account for the fact that the hysteroscope could be used for other revenue-generating procedures such as diagnostic hysteroscopy. Factoring in these potential additional services using the same hysteroscope might change the decision analysis in favor of the hysteroscope.
Remember that, although the financial analysis is very helpful in decision making, nonfinancial evaluations should also influence your choice. In this example, while there may be a financial advantage to purchasing the urodynamic equipment over the hysteroscopic equipment, nonfinancial considerations can help you decide which purchase would be a better aligned with the goals and strategies of your practice.
These tools for nonfinancial and financial analysis can be used for any investment in your practice, whether it is in medical equipment, personnel, or development of other profit centers.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Willis DR. How to decide whether to buy new medical equipment. Fam Pract Manag. 2004;11(3):53−58.
- PESTLE Analysis Strategy Skills. http://www.free-management-ebooks.com/dldebk-pdf/fme-pestle-analysis.pdf. Published 2013. Accessed March 2, 2018.
- What is PESTLE analysis? A tool for business analysis. http://pestleanalysis.com/what-is-pestle-analysis/. Published 2018. Accessed March 2, 2018.
- Nowicki M, ed. Introduction to the Financial Management of Healthcare Organizations. 6th ed. Chicago, Illinois: Health Administration Press; 2014:150−151, 299−316.
- Ross SA, Westerfield RW, Jaffe J. Corporate Finance. 8th ed. New York, New York: McGraw Hill; 2008:271−288.
- Net Present Value - NPV. Investopia. https://www.investopedia.com/terms/n/npv.asp. Accessed April 10, 2018.
- NPV function. Microsoft Office Support. https://support.office.com/en-us/article/npv-function-8672cb67-2576-4d07-b67b-ac28acf2a568. Accessed April 10, 2018.
- Damodaran A. Annual Returns on Stock, T.Bonds and T.Bills: 1928 - Current. http://pages.stern.nyu.edu/~adamodar/New_Home_Page/datafile/histretSP.html. Updated January 5, 2018. Accessed March 2, 2018.
- IRR function. Microsoft Office Support. https://support.office.com/en-us/article/irr-function-64925eaa-9988-495b-b290-3ad0c163c1bc. Accessed April 10, 2018.
- Time Value of Money (TVM). Investopedia. https://www.investopedia.com/terms/t/timevalueofmoney.asp. Published 2018. Accessed March 2, 2018.
- Willis DR. How to decide whether to buy new medical equipment. Fam Pract Manag. 2004;11(3):53−58.
- PESTLE Analysis Strategy Skills. http://www.free-management-ebooks.com/dldebk-pdf/fme-pestle-analysis.pdf. Published 2013. Accessed March 2, 2018.
- What is PESTLE analysis? A tool for business analysis. http://pestleanalysis.com/what-is-pestle-analysis/. Published 2018. Accessed March 2, 2018.
- Nowicki M, ed. Introduction to the Financial Management of Healthcare Organizations. 6th ed. Chicago, Illinois: Health Administration Press; 2014:150−151, 299−316.
- Ross SA, Westerfield RW, Jaffe J. Corporate Finance. 8th ed. New York, New York: McGraw Hill; 2008:271−288.
- Net Present Value - NPV. Investopia. https://www.investopedia.com/terms/n/npv.asp. Accessed April 10, 2018.
- NPV function. Microsoft Office Support. https://support.office.com/en-us/article/npv-function-8672cb67-2576-4d07-b67b-ac28acf2a568. Accessed April 10, 2018.
- Damodaran A. Annual Returns on Stock, T.Bonds and T.Bills: 1928 - Current. http://pages.stern.nyu.edu/~adamodar/New_Home_Page/datafile/histretSP.html. Updated January 5, 2018. Accessed March 2, 2018.
- IRR function. Microsoft Office Support. https://support.office.com/en-us/article/irr-function-64925eaa-9988-495b-b290-3ad0c163c1bc. Accessed April 10, 2018.
- Time Value of Money (TVM). Investopedia. https://www.investopedia.com/terms/t/timevalueofmoney.asp. Published 2018. Accessed March 2, 2018.
IN THIS ARTICLE
- Financial evaluation steps
- Breakeven analysis
- Compare 2 investment opportunities
Take action to prevent maternal mortality
The facts
While other industrialized nations are seeing a decrease in their maternal mortality rates, the United States has noted a 26% increase over a 15-year period. This is especially true for women of color: black women are nearly 4 times as likely to die from pregnancy related causes as compared to non-Hispanic white women. Postpartum hemorrhage and preeclampsia are often the leading causes of maternal death; however, suicide and overdoses are becoming increasingly more common. This information is highlighted in the March 2018 OBG Management article “Factors critical to reducing US maternal mortality and morbidity,” by Lucia DiVenere, MA, Government and Political Affairs, at the American College of Obstetricians and Gynecologists (ACOG).1
Although there are efforts to improve these outcomes, programs vary by state. One initiative is the perinatal quality collaboratives (PQCs), state or multistate networks of teams working to improve the quality of care for mothers and babies (see “Has your state established a perinatal quality collaborative?”).
Currently, only 33 states have a maternal mortality review committee (MMRC) comprised of an interdisciplinary team of ObGyns, nurses, and other stakeholders. The MMRC reviews each maternal death in their state and provides recommendations and policy changes to help prevent further loss of life.
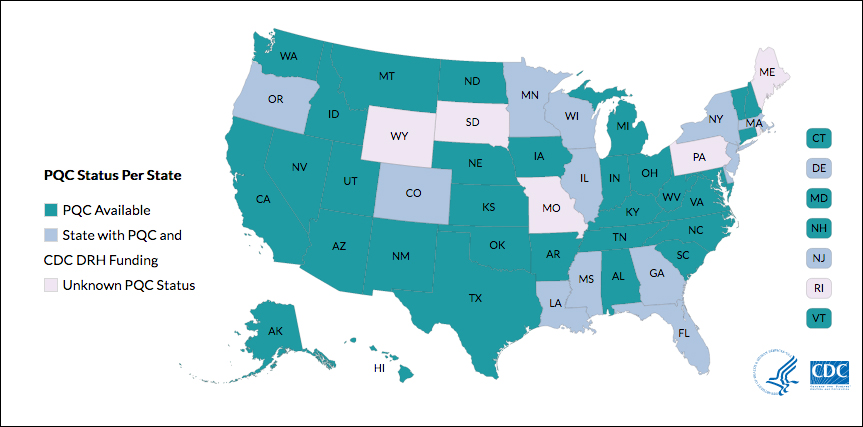
Many states currently have active collaboratives, and others are in development. The CDC’s Division of Reproductive Health (DRH) currently provides support for state-based PQCs in Colorado, Delaware, Florida, Georgia, Illinois, Louisiana, Massachusetts, Minnesota, Mississippi, New Jersey, New York, Oregon, and Wisconsin. The status of PQCs in Maine, Rhode Island, Pennsylvania, Missouri, South Dakota, and Wyoming is unknown.1
The CDC can help people establish a collaborative. Visit: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pqc-states.html.
Reference
- Centers for Disease Control and Prevention. Reproductive health: State Perinatal Quality Collaboratives. CDC website. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pqc-states.html Updated October 17, 2017. Accessed April 4, 2018.
The bill
Preventing Maternal Deaths Act/Maternal Health Accountability Act (H.R. 1318/S. 1112) is a bipartisan, bicameral effort to reduce maternal mortality and reduce health care disparities.
The bills authorize the Centers for Disease Control and Prevention (CDC) to help states create or expand state MMRCs through annual grant funding of $7 million through fiscal year 2022. Through the MMRCs, the CDC would have the ability to gather data on maternal mortality and health care disparities, allowing the agency to better understand leading causes of maternal death as well as a state’s successes and pitfalls in interventions.
Currently the House bill (H.R. 1318) has 102 cosponsors (https://cqrcengage.com/acog/app/bill/903056?0) and the Senate bill (S. 1112) has 17 cosponsors (https://cqrcengage.com/acog/app/bill/943204?1). Click these links to see if your representative is a cosponsor.
Not sure who your representative is? Click here to find out: http://cqrcengage.com/acog/app/lookup?1&m=29525.
Take action
Both the Senate and House bills have been referred to health committees. However, no advances have been made since March 2017. In order for the bills to move forward, your representatives need to hear from you.
If your representative is a cosponsor of the bill, thank them for their support, but also ask what we can do to ensure this bill becomes law.
If your representative is not a cosponsor, follow this link to email your representative: http://cqrcengage.com/acog/app/onestep-write-a-letter?0&engagementId=306574. You also can call your representative’s office and speak directly to a staff member.
When calling or emailing, highlight the following:
- I am an ObGyn and I am asking [your Representative/Senator] to support H.R. 1318 or S. 1112.
- While maternal mortality rates are decreasing in other parts of the world, they are increasing in the United States. We have the highest maternal mortality rate in the developing world.
- This bill gives all states the opportunity to have a maternal mortality review committee, allowing health care leaders to review each maternal death and analyze how further deaths can be prevented.
- Congress has invested in programs addressing infant mortality, birth defects, and preterm birth. It is time we put the same investment into saving our nation’s mothers.
- As an ObGyn, I urge you to support this bill.
More from ACOG
Want to know what other advocacy opportunities are available? Check out ACOG action at http://cqrcengage.com/acog/home?3.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- DiVenere L. Factors critical to reducing US maternal mortality and morbidity. OBG Manag. 2018;30(3):30−33.
The facts
While other industrialized nations are seeing a decrease in their maternal mortality rates, the United States has noted a 26% increase over a 15-year period. This is especially true for women of color: black women are nearly 4 times as likely to die from pregnancy related causes as compared to non-Hispanic white women. Postpartum hemorrhage and preeclampsia are often the leading causes of maternal death; however, suicide and overdoses are becoming increasingly more common. This information is highlighted in the March 2018 OBG Management article “Factors critical to reducing US maternal mortality and morbidity,” by Lucia DiVenere, MA, Government and Political Affairs, at the American College of Obstetricians and Gynecologists (ACOG).1
Although there are efforts to improve these outcomes, programs vary by state. One initiative is the perinatal quality collaboratives (PQCs), state or multistate networks of teams working to improve the quality of care for mothers and babies (see “Has your state established a perinatal quality collaborative?”).
Currently, only 33 states have a maternal mortality review committee (MMRC) comprised of an interdisciplinary team of ObGyns, nurses, and other stakeholders. The MMRC reviews each maternal death in their state and provides recommendations and policy changes to help prevent further loss of life.
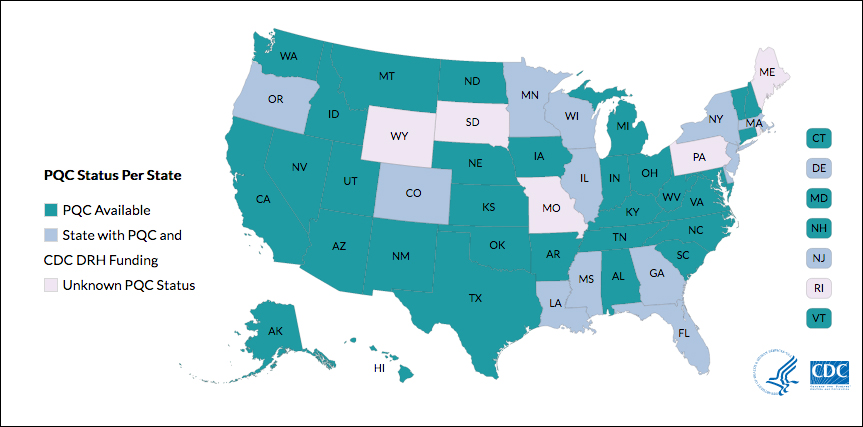
Many states currently have active collaboratives, and others are in development. The CDC’s Division of Reproductive Health (DRH) currently provides support for state-based PQCs in Colorado, Delaware, Florida, Georgia, Illinois, Louisiana, Massachusetts, Minnesota, Mississippi, New Jersey, New York, Oregon, and Wisconsin. The status of PQCs in Maine, Rhode Island, Pennsylvania, Missouri, South Dakota, and Wyoming is unknown.1
The CDC can help people establish a collaborative. Visit: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pqc-states.html.
Reference
- Centers for Disease Control and Prevention. Reproductive health: State Perinatal Quality Collaboratives. CDC website. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pqc-states.html Updated October 17, 2017. Accessed April 4, 2018.
The bill
Preventing Maternal Deaths Act/Maternal Health Accountability Act (H.R. 1318/S. 1112) is a bipartisan, bicameral effort to reduce maternal mortality and reduce health care disparities.
The bills authorize the Centers for Disease Control and Prevention (CDC) to help states create or expand state MMRCs through annual grant funding of $7 million through fiscal year 2022. Through the MMRCs, the CDC would have the ability to gather data on maternal mortality and health care disparities, allowing the agency to better understand leading causes of maternal death as well as a state’s successes and pitfalls in interventions.
Currently the House bill (H.R. 1318) has 102 cosponsors (https://cqrcengage.com/acog/app/bill/903056?0) and the Senate bill (S. 1112) has 17 cosponsors (https://cqrcengage.com/acog/app/bill/943204?1). Click these links to see if your representative is a cosponsor.
Not sure who your representative is? Click here to find out: http://cqrcengage.com/acog/app/lookup?1&m=29525.
Take action
Both the Senate and House bills have been referred to health committees. However, no advances have been made since March 2017. In order for the bills to move forward, your representatives need to hear from you.
If your representative is a cosponsor of the bill, thank them for their support, but also ask what we can do to ensure this bill becomes law.
If your representative is not a cosponsor, follow this link to email your representative: http://cqrcengage.com/acog/app/onestep-write-a-letter?0&engagementId=306574. You also can call your representative’s office and speak directly to a staff member.
When calling or emailing, highlight the following:
- I am an ObGyn and I am asking [your Representative/Senator] to support H.R. 1318 or S. 1112.
- While maternal mortality rates are decreasing in other parts of the world, they are increasing in the United States. We have the highest maternal mortality rate in the developing world.
- This bill gives all states the opportunity to have a maternal mortality review committee, allowing health care leaders to review each maternal death and analyze how further deaths can be prevented.
- Congress has invested in programs addressing infant mortality, birth defects, and preterm birth. It is time we put the same investment into saving our nation’s mothers.
- As an ObGyn, I urge you to support this bill.
More from ACOG
Want to know what other advocacy opportunities are available? Check out ACOG action at http://cqrcengage.com/acog/home?3.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The facts
While other industrialized nations are seeing a decrease in their maternal mortality rates, the United States has noted a 26% increase over a 15-year period. This is especially true for women of color: black women are nearly 4 times as likely to die from pregnancy related causes as compared to non-Hispanic white women. Postpartum hemorrhage and preeclampsia are often the leading causes of maternal death; however, suicide and overdoses are becoming increasingly more common. This information is highlighted in the March 2018 OBG Management article “Factors critical to reducing US maternal mortality and morbidity,” by Lucia DiVenere, MA, Government and Political Affairs, at the American College of Obstetricians and Gynecologists (ACOG).1
Although there are efforts to improve these outcomes, programs vary by state. One initiative is the perinatal quality collaboratives (PQCs), state or multistate networks of teams working to improve the quality of care for mothers and babies (see “Has your state established a perinatal quality collaborative?”).
Currently, only 33 states have a maternal mortality review committee (MMRC) comprised of an interdisciplinary team of ObGyns, nurses, and other stakeholders. The MMRC reviews each maternal death in their state and provides recommendations and policy changes to help prevent further loss of life.
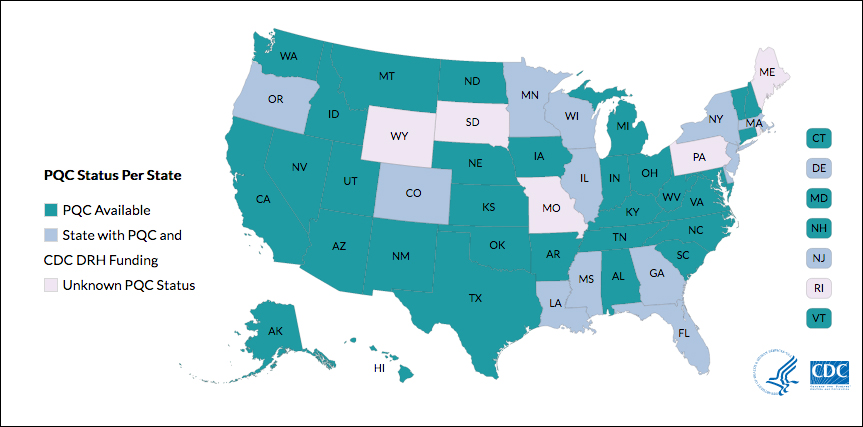
Many states currently have active collaboratives, and others are in development. The CDC’s Division of Reproductive Health (DRH) currently provides support for state-based PQCs in Colorado, Delaware, Florida, Georgia, Illinois, Louisiana, Massachusetts, Minnesota, Mississippi, New Jersey, New York, Oregon, and Wisconsin. The status of PQCs in Maine, Rhode Island, Pennsylvania, Missouri, South Dakota, and Wyoming is unknown.1
The CDC can help people establish a collaborative. Visit: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pqc-states.html.
Reference
- Centers for Disease Control and Prevention. Reproductive health: State Perinatal Quality Collaboratives. CDC website. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pqc-states.html Updated October 17, 2017. Accessed April 4, 2018.
The bill
Preventing Maternal Deaths Act/Maternal Health Accountability Act (H.R. 1318/S. 1112) is a bipartisan, bicameral effort to reduce maternal mortality and reduce health care disparities.
The bills authorize the Centers for Disease Control and Prevention (CDC) to help states create or expand state MMRCs through annual grant funding of $7 million through fiscal year 2022. Through the MMRCs, the CDC would have the ability to gather data on maternal mortality and health care disparities, allowing the agency to better understand leading causes of maternal death as well as a state’s successes and pitfalls in interventions.
Currently the House bill (H.R. 1318) has 102 cosponsors (https://cqrcengage.com/acog/app/bill/903056?0) and the Senate bill (S. 1112) has 17 cosponsors (https://cqrcengage.com/acog/app/bill/943204?1). Click these links to see if your representative is a cosponsor.
Not sure who your representative is? Click here to find out: http://cqrcengage.com/acog/app/lookup?1&m=29525.
Take action
Both the Senate and House bills have been referred to health committees. However, no advances have been made since March 2017. In order for the bills to move forward, your representatives need to hear from you.
If your representative is a cosponsor of the bill, thank them for their support, but also ask what we can do to ensure this bill becomes law.
If your representative is not a cosponsor, follow this link to email your representative: http://cqrcengage.com/acog/app/onestep-write-a-letter?0&engagementId=306574. You also can call your representative’s office and speak directly to a staff member.
When calling or emailing, highlight the following:
- I am an ObGyn and I am asking [your Representative/Senator] to support H.R. 1318 or S. 1112.
- While maternal mortality rates are decreasing in other parts of the world, they are increasing in the United States. We have the highest maternal mortality rate in the developing world.
- This bill gives all states the opportunity to have a maternal mortality review committee, allowing health care leaders to review each maternal death and analyze how further deaths can be prevented.
- Congress has invested in programs addressing infant mortality, birth defects, and preterm birth. It is time we put the same investment into saving our nation’s mothers.
- As an ObGyn, I urge you to support this bill.
More from ACOG
Want to know what other advocacy opportunities are available? Check out ACOG action at http://cqrcengage.com/acog/home?3.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- DiVenere L. Factors critical to reducing US maternal mortality and morbidity. OBG Manag. 2018;30(3):30−33.
- DiVenere L. Factors critical to reducing US maternal mortality and morbidity. OBG Manag. 2018;30(3):30−33.
Website improvements
Nowadays, almost half of all Americans (and nearly all millennials) seek out doctors online. But your practice website should be doing a lot more than simply describing your practice. How many visitors to your site actually schedule an appointment? With a few relatively simple but important modifications, you can convert casual website viewers to patients.
Start with a good title, one that not only describes your practice but also anticipates how prospective patients will search for you – usually by specialty plus geographic location. My site’s title, for example, is “Belleville Dermatology Center,” so when someone searches for a dermatologist near Belleville, N.J., my site will invariably rank near the top of their search results.
Follow with an understandable URL. Search engines use URLs to determine how well your site, or a portion of it, matches search criteria. URLs also need to make sense to searchers, especially when they link specific areas of expertise (more on that in a minute). For example, a URL like “bellevilledermatology[dot]com/?p=89021” is meaningless to anyone except programmers; but “bellevilledermatology[dot]com/psoriasistreatments” obviously leads to a page about psoriasis treatments. Search engines look for not only the most relevant, but also the most helpful and user-friendly, answers to a user’s query.
Incidentally, if the URL for your site is not your own name, you should register your name as a separate domain name – even if you never use it – to be sure that a trickster or troll, or someone with the same name but a bad reputation, doesn’t get it.
Continue with a good meta description. That’s the grayish text that follows the title and URL in search results. Searchers will read it to confirm that your site is what they seek, so make sure it describes exactly what you do, including any areas of special expertise. Aggressive marketers will sometimes pad their descriptions with a wide variety of other specialties, services, and locations, hoping to gain inclusion in a larger pool of search results. That tactic – “keyword stuffing” in IT parlance – is not only ineffective, but search engines tend to ignore sites that use it. An accurate, honest description works best.
Describe your principal services in detail. You never know which specific service a prospective patient is searching for, so describe everything you offer. Don’t try to summarize everything on a single page; relevance is determined by how deeply a topic is covered, so each principal service should have a detailed description on its own page. Not only will your skills become more visible to search engines, but you can also use the space to enumerate your qualifications and expertise in each area. Whenever possible, write your descriptions in question-and-answer form. Searchers tend to ask questions (“what is the best…?”), particularly in voice searches. Search engines increasingly value sites that ask and answer common questions.
How does your site look on small screens? More than half of all searches are now made on smartphones, so the more “mobile friendly” your site is, the higher it will be ranked. Besides, prospective patients who are forced to scroll forever, or zoom in to tap a link, are likely to become frustrated and move on. Mobile searchers prefer sites that provide the best experience for the least amount of effort, and rankings tend to reflect that preference.
Include photos. Especially yours; new patients are more comfortable when they know what you look like. Although some disagree, I feel family photos are also important; they help to present you as a person, as well as a doctor. Photos of your office – professional ones, not casual snapshots – will reassure prospective patients that they will be visiting a clean, modern, professional facility.
Provide online appointment scheduling. Once searchers make an appointment, they stop searching. If they have to wait until the next day to call your office, they may keep looking – and might find a competitor with online scheduling. You should also have a separate “contact” page, listing all of the ways people can reach you, along with a map. Finally, list which insurance plans you accept as a courtesy to patients and to decrease unnecessary calls for your staff.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Nowadays, almost half of all Americans (and nearly all millennials) seek out doctors online. But your practice website should be doing a lot more than simply describing your practice. How many visitors to your site actually schedule an appointment? With a few relatively simple but important modifications, you can convert casual website viewers to patients.
Start with a good title, one that not only describes your practice but also anticipates how prospective patients will search for you – usually by specialty plus geographic location. My site’s title, for example, is “Belleville Dermatology Center,” so when someone searches for a dermatologist near Belleville, N.J., my site will invariably rank near the top of their search results.
Follow with an understandable URL. Search engines use URLs to determine how well your site, or a portion of it, matches search criteria. URLs also need to make sense to searchers, especially when they link specific areas of expertise (more on that in a minute). For example, a URL like “bellevilledermatology[dot]com/?p=89021” is meaningless to anyone except programmers; but “bellevilledermatology[dot]com/psoriasistreatments” obviously leads to a page about psoriasis treatments. Search engines look for not only the most relevant, but also the most helpful and user-friendly, answers to a user’s query.
Incidentally, if the URL for your site is not your own name, you should register your name as a separate domain name – even if you never use it – to be sure that a trickster or troll, or someone with the same name but a bad reputation, doesn’t get it.
Continue with a good meta description. That’s the grayish text that follows the title and URL in search results. Searchers will read it to confirm that your site is what they seek, so make sure it describes exactly what you do, including any areas of special expertise. Aggressive marketers will sometimes pad their descriptions with a wide variety of other specialties, services, and locations, hoping to gain inclusion in a larger pool of search results. That tactic – “keyword stuffing” in IT parlance – is not only ineffective, but search engines tend to ignore sites that use it. An accurate, honest description works best.
Describe your principal services in detail. You never know which specific service a prospective patient is searching for, so describe everything you offer. Don’t try to summarize everything on a single page; relevance is determined by how deeply a topic is covered, so each principal service should have a detailed description on its own page. Not only will your skills become more visible to search engines, but you can also use the space to enumerate your qualifications and expertise in each area. Whenever possible, write your descriptions in question-and-answer form. Searchers tend to ask questions (“what is the best…?”), particularly in voice searches. Search engines increasingly value sites that ask and answer common questions.
How does your site look on small screens? More than half of all searches are now made on smartphones, so the more “mobile friendly” your site is, the higher it will be ranked. Besides, prospective patients who are forced to scroll forever, or zoom in to tap a link, are likely to become frustrated and move on. Mobile searchers prefer sites that provide the best experience for the least amount of effort, and rankings tend to reflect that preference.
Include photos. Especially yours; new patients are more comfortable when they know what you look like. Although some disagree, I feel family photos are also important; they help to present you as a person, as well as a doctor. Photos of your office – professional ones, not casual snapshots – will reassure prospective patients that they will be visiting a clean, modern, professional facility.
Provide online appointment scheduling. Once searchers make an appointment, they stop searching. If they have to wait until the next day to call your office, they may keep looking – and might find a competitor with online scheduling. You should also have a separate “contact” page, listing all of the ways people can reach you, along with a map. Finally, list which insurance plans you accept as a courtesy to patients and to decrease unnecessary calls for your staff.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Nowadays, almost half of all Americans (and nearly all millennials) seek out doctors online. But your practice website should be doing a lot more than simply describing your practice. How many visitors to your site actually schedule an appointment? With a few relatively simple but important modifications, you can convert casual website viewers to patients.
Start with a good title, one that not only describes your practice but also anticipates how prospective patients will search for you – usually by specialty plus geographic location. My site’s title, for example, is “Belleville Dermatology Center,” so when someone searches for a dermatologist near Belleville, N.J., my site will invariably rank near the top of their search results.
Follow with an understandable URL. Search engines use URLs to determine how well your site, or a portion of it, matches search criteria. URLs also need to make sense to searchers, especially when they link specific areas of expertise (more on that in a minute). For example, a URL like “bellevilledermatology[dot]com/?p=89021” is meaningless to anyone except programmers; but “bellevilledermatology[dot]com/psoriasistreatments” obviously leads to a page about psoriasis treatments. Search engines look for not only the most relevant, but also the most helpful and user-friendly, answers to a user’s query.
Incidentally, if the URL for your site is not your own name, you should register your name as a separate domain name – even if you never use it – to be sure that a trickster or troll, or someone with the same name but a bad reputation, doesn’t get it.
Continue with a good meta description. That’s the grayish text that follows the title and URL in search results. Searchers will read it to confirm that your site is what they seek, so make sure it describes exactly what you do, including any areas of special expertise. Aggressive marketers will sometimes pad their descriptions with a wide variety of other specialties, services, and locations, hoping to gain inclusion in a larger pool of search results. That tactic – “keyword stuffing” in IT parlance – is not only ineffective, but search engines tend to ignore sites that use it. An accurate, honest description works best.
Describe your principal services in detail. You never know which specific service a prospective patient is searching for, so describe everything you offer. Don’t try to summarize everything on a single page; relevance is determined by how deeply a topic is covered, so each principal service should have a detailed description on its own page. Not only will your skills become more visible to search engines, but you can also use the space to enumerate your qualifications and expertise in each area. Whenever possible, write your descriptions in question-and-answer form. Searchers tend to ask questions (“what is the best…?”), particularly in voice searches. Search engines increasingly value sites that ask and answer common questions.
How does your site look on small screens? More than half of all searches are now made on smartphones, so the more “mobile friendly” your site is, the higher it will be ranked. Besides, prospective patients who are forced to scroll forever, or zoom in to tap a link, are likely to become frustrated and move on. Mobile searchers prefer sites that provide the best experience for the least amount of effort, and rankings tend to reflect that preference.
Include photos. Especially yours; new patients are more comfortable when they know what you look like. Although some disagree, I feel family photos are also important; they help to present you as a person, as well as a doctor. Photos of your office – professional ones, not casual snapshots – will reassure prospective patients that they will be visiting a clean, modern, professional facility.
Provide online appointment scheduling. Once searchers make an appointment, they stop searching. If they have to wait until the next day to call your office, they may keep looking – and might find a competitor with online scheduling. You should also have a separate “contact” page, listing all of the ways people can reach you, along with a map. Finally, list which insurance plans you accept as a courtesy to patients and to decrease unnecessary calls for your staff.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Does measuring episiotomy rates really benefit the quality of care our patients receive?
Like most California institutions performing deliveries, St. Joseph Hospital in Orange, California, started releasing 2016 maternal quality metrics internally at first. Data for the first 9 months of 2016 were distributed in December 2016. These metrics depend on a denominator based on the number of deliveries attributed to each obstetrician.
- I was very pleased to see that I ranked first in the vaginal birth after cesarean (VBAC) rate at 36.8%.
- I also was pleased that I ranked the fourth lowest, at 15.9%, for my cesarean delivery rate in the low-risk, nulliparous term singleton vertex (NTSV) population.
- I was neither pleased nor displeased that I ranked number 29 of 31 physicians at 59.1% (39/66) for the episiotomy rate. The denominator range was 1 to 287. I knew I would hear about this! Sure enough, a medical director asked me how 2 of my metrics could be so good, yet the third be so abysmal.
After the release of the data and the somewhat humorous chastisement by the medical director, I decided to try complying with the new American College of Obstetricians and Gynecologists (ACOG) guidelines1 again beginning in January 2017.
A little personal history
Allow me to date myself. I completed my residency in 1981 and was Board Certified in 1984. My wife refers to me as a “Dinosaur!” As an ObGyn in solo practice, I take my own call.
During my training, episiotomies were commonly performed but were not always necessary. We were taught to not perform an episiotomy if the patient could safely and easily deliver without one. However, if clinically indicated, an episiotomy should be performed. If a 3rd- or 4th-degree laceration occurred, we were taught to anatomically repair it. Nowadays in my practice, these lacerations are rare in conjunction with an episiotomy, and with a controlled delivery of the fetal head.
Our nursing staff will tell you that I resist change. However, I usually attempt and often do adapt the latest national guidelines into my practice. Although I did not agree when restrictive episiotomies became a national goal a few years ago, I tried to adhere to the new national episiotomy recommendations.1 I am meticulous: a standard episiotomy repair that does not involve excessive bleeding usually takes 20 minutes to restore normal anatomy with a simple, straightforward, layered closure.
My episiotomy performance record
In 2015, I restricted my use of episiotomies. When I did not perform one, the patient usually experienced lacerations. These were labial or periurethral as well as complex 3-dimensional “Z” or “Y” shaped vaginal/perineal lacerations, not just the 1st- and 2nd-degree perineal lacerations to which the literature refers.
The problems associated with complex, geometric vaginal lacerations are multifactorial:
- Lacerations occur at multiple locations.
- Significant bleeding often occurs. Because the lacerations are in multiple locations, the bleeding cannot be addressed easily, quickly, or at once.
- Visualization is difficult because of the bleeding, thus further prolonging the repair.
- These lacerations are often deeper than an episiotomy would have been and are very friable as all the layers have been stretched to their breaking point before tearing.
- Sometimes the lacerations include avulsion of the hymen with extensive bleeding.
- Difficult-to-repair lacerations can tear upon suturing, requiring layer upon layer of sutures at the same site. Future scarring and vaginal stricture leading to sexual dysfunction are concerns.
- At times, the friability and bleeding is so brisk that once the bleeding is controlled and the episiotomy is partially repaired, I can see that it is has not been an anatomic repair. I then have to take it down and re-do the repair with an obscured field from bleeding again!
- Some repairs are so fragile that when I express retained blood from the uterus and upper vagina after completing the repair, the tissue tears, bleeds, and requires additional restoration.
- These tears usually require an hour to repair and achieve hemostasis. At times, an assistant and a retractor are necessary.
After 2015, when I spent the year complying with the new guidelines, I returned to my original protocol: I performed an episiotomy only when I thought the patient was going to experience a significant laceration. I did not perform an episiotomy if I thought the mother could deliver easily without one. That is how I attained the 59.1% episiotomy rate in 2016.
Another try
After the 2016 hospital data were released, I decided to comply with the new guidelines1 again beginning in January 2017. Here I share the details of 3 deliveries that occurred in 2017:
- A 30-year-old woman (G2P1) planned to have a repeat cesarean delivery. At 38 3/7 weeks’ gestation, she was admitted in active labor with the cervix dilated to 5 cm. She requested a VBAC. After successful vaginal delivery without episiotomy of a 7 lb 5 oz infant, there were bilateral periurethral and right labia minora abrasions/lacerations.
- A 21-year-old woman (G1P0) at 40 4/7 weeks’ gestation was admitted in early labor. The cervix was 2-cm dilated and 70% effaced after spontaneous rupture of membranes. I exercised my clinical judgment and performed a midline episiotomy. A 9 lb 3 oz infant was delivered by vaginal delivery.
- A 16-year-old woman (G1P0) at 41 weeks’ gestation was admitted for induction of labor with an unripe cervix. I was delayed, and the laborist performed a vaginal delivery after 1 attempt at vacuum extraction and no episiotomy. The 7 lb 3 oz baby had Apgar scores of 4 and 9 at 1 and 5 minutes, respectively. There was significant bleeding from bilateral vaginal lacerations with bilateral hymeneal avulsions.
What is the benefit?
Are we really benefitting our patients by restricting the use of episiotomy? Consider these questions:
- Should we delay the mother’s bonding with her baby for an hour’s complex repair versus 20 minutes for a simple, layered episiotomy repair?
- In a busy labor and delivery unit, should resources be tied up for this extra time? With all due respect to the national experts advocating this recommendation, are they in the trenches performing deliveries and spending hours repairing complex lacerations?
- Should we not use our clinical judgment instead of allowing the mother to experience an extensive vaginal/perineal laceration after a vaginal delivery of a 9- or 10-lb baby?
- Where are the long-term data showing that it is better for a woman to stretch and attenuate her perineal and vaginal muscles to the breaking point, and then tear?
- Do all the additional sutures lead to vaginal scarring, vaginal stricture, and sexual dysfunction in later years?
- Which protocol better enables the mother to maintain pelvic organ support and avoid pelvic organ prolapse and stress urinary incontinence?
In Williams Obstetrics, the authors state: “We are of the view that episiotomy should be applied selectively for the appropriate indications. The final rule is that there is no substitute for surgical judgment and common sense.”2
Consider other metrics
Patients might be better served by measuring quality and safety metrics other than episiotomy. These might include, for example, measuring:
- the use of prophylactic oxytocin after the anterior shoulder is delivered in order to decrease the risk of postpartum hemorrhage, as advocated by the California Maternal Quality Care Collaborative3
- the number of patients admitted before active labor and those receiving an epidural before active labor (with the aim of decreasing the primary cesarean rate in the NTSV population)
- the number of patients in an advanced stage of labor whose labor pattern has become dysfunctional, in whom no interventions have been instituted to improve the labor pattern, and who subsequently deliver by primary cesarean.
Recommendation
I recommend that performing an episiotomy should be an individual clinical decision for the individual patient by the individual obstetrician, and not a national mandate. We can provide quality care to our patients by performing selective episiotomies when clinically necessary, and not avoid them to an extreme that harms our patients. In my opinion, using the episiotomy rate as a quality metric should be abandoned.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- CambriaAmerican College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. Practice Bulletin No. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2016;128(1):e1Times New Roman MT Std–e15.
- Vaginal delivery. In: Cunnigham FG, Leveno KJ, Bloom SL, et al, eds. Williams Obstetrics. 24th ed. New York, NY: McGraw-Hill Medical; 2014:550.
- CMQCC: California Maternal Quality Care Collaborative website. https://www.cmqcc.org/. Accessed March 12, 2018.
Like most California institutions performing deliveries, St. Joseph Hospital in Orange, California, started releasing 2016 maternal quality metrics internally at first. Data for the first 9 months of 2016 were distributed in December 2016. These metrics depend on a denominator based on the number of deliveries attributed to each obstetrician.
- I was very pleased to see that I ranked first in the vaginal birth after cesarean (VBAC) rate at 36.8%.
- I also was pleased that I ranked the fourth lowest, at 15.9%, for my cesarean delivery rate in the low-risk, nulliparous term singleton vertex (NTSV) population.
- I was neither pleased nor displeased that I ranked number 29 of 31 physicians at 59.1% (39/66) for the episiotomy rate. The denominator range was 1 to 287. I knew I would hear about this! Sure enough, a medical director asked me how 2 of my metrics could be so good, yet the third be so abysmal.
After the release of the data and the somewhat humorous chastisement by the medical director, I decided to try complying with the new American College of Obstetricians and Gynecologists (ACOG) guidelines1 again beginning in January 2017.
A little personal history
Allow me to date myself. I completed my residency in 1981 and was Board Certified in 1984. My wife refers to me as a “Dinosaur!” As an ObGyn in solo practice, I take my own call.
During my training, episiotomies were commonly performed but were not always necessary. We were taught to not perform an episiotomy if the patient could safely and easily deliver without one. However, if clinically indicated, an episiotomy should be performed. If a 3rd- or 4th-degree laceration occurred, we were taught to anatomically repair it. Nowadays in my practice, these lacerations are rare in conjunction with an episiotomy, and with a controlled delivery of the fetal head.
Our nursing staff will tell you that I resist change. However, I usually attempt and often do adapt the latest national guidelines into my practice. Although I did not agree when restrictive episiotomies became a national goal a few years ago, I tried to adhere to the new national episiotomy recommendations.1 I am meticulous: a standard episiotomy repair that does not involve excessive bleeding usually takes 20 minutes to restore normal anatomy with a simple, straightforward, layered closure.
My episiotomy performance record
In 2015, I restricted my use of episiotomies. When I did not perform one, the patient usually experienced lacerations. These were labial or periurethral as well as complex 3-dimensional “Z” or “Y” shaped vaginal/perineal lacerations, not just the 1st- and 2nd-degree perineal lacerations to which the literature refers.
The problems associated with complex, geometric vaginal lacerations are multifactorial:
- Lacerations occur at multiple locations.
- Significant bleeding often occurs. Because the lacerations are in multiple locations, the bleeding cannot be addressed easily, quickly, or at once.
- Visualization is difficult because of the bleeding, thus further prolonging the repair.
- These lacerations are often deeper than an episiotomy would have been and are very friable as all the layers have been stretched to their breaking point before tearing.
- Sometimes the lacerations include avulsion of the hymen with extensive bleeding.
- Difficult-to-repair lacerations can tear upon suturing, requiring layer upon layer of sutures at the same site. Future scarring and vaginal stricture leading to sexual dysfunction are concerns.
- At times, the friability and bleeding is so brisk that once the bleeding is controlled and the episiotomy is partially repaired, I can see that it is has not been an anatomic repair. I then have to take it down and re-do the repair with an obscured field from bleeding again!
- Some repairs are so fragile that when I express retained blood from the uterus and upper vagina after completing the repair, the tissue tears, bleeds, and requires additional restoration.
- These tears usually require an hour to repair and achieve hemostasis. At times, an assistant and a retractor are necessary.
After 2015, when I spent the year complying with the new guidelines, I returned to my original protocol: I performed an episiotomy only when I thought the patient was going to experience a significant laceration. I did not perform an episiotomy if I thought the mother could deliver easily without one. That is how I attained the 59.1% episiotomy rate in 2016.
Another try
After the 2016 hospital data were released, I decided to comply with the new guidelines1 again beginning in January 2017. Here I share the details of 3 deliveries that occurred in 2017:
- A 30-year-old woman (G2P1) planned to have a repeat cesarean delivery. At 38 3/7 weeks’ gestation, she was admitted in active labor with the cervix dilated to 5 cm. She requested a VBAC. After successful vaginal delivery without episiotomy of a 7 lb 5 oz infant, there were bilateral periurethral and right labia minora abrasions/lacerations.
- A 21-year-old woman (G1P0) at 40 4/7 weeks’ gestation was admitted in early labor. The cervix was 2-cm dilated and 70% effaced after spontaneous rupture of membranes. I exercised my clinical judgment and performed a midline episiotomy. A 9 lb 3 oz infant was delivered by vaginal delivery.
- A 16-year-old woman (G1P0) at 41 weeks’ gestation was admitted for induction of labor with an unripe cervix. I was delayed, and the laborist performed a vaginal delivery after 1 attempt at vacuum extraction and no episiotomy. The 7 lb 3 oz baby had Apgar scores of 4 and 9 at 1 and 5 minutes, respectively. There was significant bleeding from bilateral vaginal lacerations with bilateral hymeneal avulsions.
What is the benefit?
Are we really benefitting our patients by restricting the use of episiotomy? Consider these questions:
- Should we delay the mother’s bonding with her baby for an hour’s complex repair versus 20 minutes for a simple, layered episiotomy repair?
- In a busy labor and delivery unit, should resources be tied up for this extra time? With all due respect to the national experts advocating this recommendation, are they in the trenches performing deliveries and spending hours repairing complex lacerations?
- Should we not use our clinical judgment instead of allowing the mother to experience an extensive vaginal/perineal laceration after a vaginal delivery of a 9- or 10-lb baby?
- Where are the long-term data showing that it is better for a woman to stretch and attenuate her perineal and vaginal muscles to the breaking point, and then tear?
- Do all the additional sutures lead to vaginal scarring, vaginal stricture, and sexual dysfunction in later years?
- Which protocol better enables the mother to maintain pelvic organ support and avoid pelvic organ prolapse and stress urinary incontinence?
In Williams Obstetrics, the authors state: “We are of the view that episiotomy should be applied selectively for the appropriate indications. The final rule is that there is no substitute for surgical judgment and common sense.”2
Consider other metrics
Patients might be better served by measuring quality and safety metrics other than episiotomy. These might include, for example, measuring:
- the use of prophylactic oxytocin after the anterior shoulder is delivered in order to decrease the risk of postpartum hemorrhage, as advocated by the California Maternal Quality Care Collaborative3
- the number of patients admitted before active labor and those receiving an epidural before active labor (with the aim of decreasing the primary cesarean rate in the NTSV population)
- the number of patients in an advanced stage of labor whose labor pattern has become dysfunctional, in whom no interventions have been instituted to improve the labor pattern, and who subsequently deliver by primary cesarean.
Recommendation
I recommend that performing an episiotomy should be an individual clinical decision for the individual patient by the individual obstetrician, and not a national mandate. We can provide quality care to our patients by performing selective episiotomies when clinically necessary, and not avoid them to an extreme that harms our patients. In my opinion, using the episiotomy rate as a quality metric should be abandoned.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Like most California institutions performing deliveries, St. Joseph Hospital in Orange, California, started releasing 2016 maternal quality metrics internally at first. Data for the first 9 months of 2016 were distributed in December 2016. These metrics depend on a denominator based on the number of deliveries attributed to each obstetrician.
- I was very pleased to see that I ranked first in the vaginal birth after cesarean (VBAC) rate at 36.8%.
- I also was pleased that I ranked the fourth lowest, at 15.9%, for my cesarean delivery rate in the low-risk, nulliparous term singleton vertex (NTSV) population.
- I was neither pleased nor displeased that I ranked number 29 of 31 physicians at 59.1% (39/66) for the episiotomy rate. The denominator range was 1 to 287. I knew I would hear about this! Sure enough, a medical director asked me how 2 of my metrics could be so good, yet the third be so abysmal.
After the release of the data and the somewhat humorous chastisement by the medical director, I decided to try complying with the new American College of Obstetricians and Gynecologists (ACOG) guidelines1 again beginning in January 2017.
A little personal history
Allow me to date myself. I completed my residency in 1981 and was Board Certified in 1984. My wife refers to me as a “Dinosaur!” As an ObGyn in solo practice, I take my own call.
During my training, episiotomies were commonly performed but were not always necessary. We were taught to not perform an episiotomy if the patient could safely and easily deliver without one. However, if clinically indicated, an episiotomy should be performed. If a 3rd- or 4th-degree laceration occurred, we were taught to anatomically repair it. Nowadays in my practice, these lacerations are rare in conjunction with an episiotomy, and with a controlled delivery of the fetal head.
Our nursing staff will tell you that I resist change. However, I usually attempt and often do adapt the latest national guidelines into my practice. Although I did not agree when restrictive episiotomies became a national goal a few years ago, I tried to adhere to the new national episiotomy recommendations.1 I am meticulous: a standard episiotomy repair that does not involve excessive bleeding usually takes 20 minutes to restore normal anatomy with a simple, straightforward, layered closure.
My episiotomy performance record
In 2015, I restricted my use of episiotomies. When I did not perform one, the patient usually experienced lacerations. These were labial or periurethral as well as complex 3-dimensional “Z” or “Y” shaped vaginal/perineal lacerations, not just the 1st- and 2nd-degree perineal lacerations to which the literature refers.
The problems associated with complex, geometric vaginal lacerations are multifactorial:
- Lacerations occur at multiple locations.
- Significant bleeding often occurs. Because the lacerations are in multiple locations, the bleeding cannot be addressed easily, quickly, or at once.
- Visualization is difficult because of the bleeding, thus further prolonging the repair.
- These lacerations are often deeper than an episiotomy would have been and are very friable as all the layers have been stretched to their breaking point before tearing.
- Sometimes the lacerations include avulsion of the hymen with extensive bleeding.
- Difficult-to-repair lacerations can tear upon suturing, requiring layer upon layer of sutures at the same site. Future scarring and vaginal stricture leading to sexual dysfunction are concerns.
- At times, the friability and bleeding is so brisk that once the bleeding is controlled and the episiotomy is partially repaired, I can see that it is has not been an anatomic repair. I then have to take it down and re-do the repair with an obscured field from bleeding again!
- Some repairs are so fragile that when I express retained blood from the uterus and upper vagina after completing the repair, the tissue tears, bleeds, and requires additional restoration.
- These tears usually require an hour to repair and achieve hemostasis. At times, an assistant and a retractor are necessary.
After 2015, when I spent the year complying with the new guidelines, I returned to my original protocol: I performed an episiotomy only when I thought the patient was going to experience a significant laceration. I did not perform an episiotomy if I thought the mother could deliver easily without one. That is how I attained the 59.1% episiotomy rate in 2016.
Another try
After the 2016 hospital data were released, I decided to comply with the new guidelines1 again beginning in January 2017. Here I share the details of 3 deliveries that occurred in 2017:
- A 30-year-old woman (G2P1) planned to have a repeat cesarean delivery. At 38 3/7 weeks’ gestation, she was admitted in active labor with the cervix dilated to 5 cm. She requested a VBAC. After successful vaginal delivery without episiotomy of a 7 lb 5 oz infant, there were bilateral periurethral and right labia minora abrasions/lacerations.
- A 21-year-old woman (G1P0) at 40 4/7 weeks’ gestation was admitted in early labor. The cervix was 2-cm dilated and 70% effaced after spontaneous rupture of membranes. I exercised my clinical judgment and performed a midline episiotomy. A 9 lb 3 oz infant was delivered by vaginal delivery.
- A 16-year-old woman (G1P0) at 41 weeks’ gestation was admitted for induction of labor with an unripe cervix. I was delayed, and the laborist performed a vaginal delivery after 1 attempt at vacuum extraction and no episiotomy. The 7 lb 3 oz baby had Apgar scores of 4 and 9 at 1 and 5 minutes, respectively. There was significant bleeding from bilateral vaginal lacerations with bilateral hymeneal avulsions.
What is the benefit?
Are we really benefitting our patients by restricting the use of episiotomy? Consider these questions:
- Should we delay the mother’s bonding with her baby for an hour’s complex repair versus 20 minutes for a simple, layered episiotomy repair?
- In a busy labor and delivery unit, should resources be tied up for this extra time? With all due respect to the national experts advocating this recommendation, are they in the trenches performing deliveries and spending hours repairing complex lacerations?
- Should we not use our clinical judgment instead of allowing the mother to experience an extensive vaginal/perineal laceration after a vaginal delivery of a 9- or 10-lb baby?
- Where are the long-term data showing that it is better for a woman to stretch and attenuate her perineal and vaginal muscles to the breaking point, and then tear?
- Do all the additional sutures lead to vaginal scarring, vaginal stricture, and sexual dysfunction in later years?
- Which protocol better enables the mother to maintain pelvic organ support and avoid pelvic organ prolapse and stress urinary incontinence?
In Williams Obstetrics, the authors state: “We are of the view that episiotomy should be applied selectively for the appropriate indications. The final rule is that there is no substitute for surgical judgment and common sense.”2
Consider other metrics
Patients might be better served by measuring quality and safety metrics other than episiotomy. These might include, for example, measuring:
- the use of prophylactic oxytocin after the anterior shoulder is delivered in order to decrease the risk of postpartum hemorrhage, as advocated by the California Maternal Quality Care Collaborative3
- the number of patients admitted before active labor and those receiving an epidural before active labor (with the aim of decreasing the primary cesarean rate in the NTSV population)
- the number of patients in an advanced stage of labor whose labor pattern has become dysfunctional, in whom no interventions have been instituted to improve the labor pattern, and who subsequently deliver by primary cesarean.
Recommendation
I recommend that performing an episiotomy should be an individual clinical decision for the individual patient by the individual obstetrician, and not a national mandate. We can provide quality care to our patients by performing selective episiotomies when clinically necessary, and not avoid them to an extreme that harms our patients. In my opinion, using the episiotomy rate as a quality metric should be abandoned.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- CambriaAmerican College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. Practice Bulletin No. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2016;128(1):e1Times New Roman MT Std–e15.
- Vaginal delivery. In: Cunnigham FG, Leveno KJ, Bloom SL, et al, eds. Williams Obstetrics. 24th ed. New York, NY: McGraw-Hill Medical; 2014:550.
- CMQCC: California Maternal Quality Care Collaborative website. https://www.cmqcc.org/. Accessed March 12, 2018.
- CambriaAmerican College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. Practice Bulletin No. 165: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2016;128(1):e1Times New Roman MT Std–e15.
- Vaginal delivery. In: Cunnigham FG, Leveno KJ, Bloom SL, et al, eds. Williams Obstetrics. 24th ed. New York, NY: McGraw-Hill Medical; 2014:550.
- CMQCC: California Maternal Quality Care Collaborative website. https://www.cmqcc.org/. Accessed March 12, 2018.
AHRQ Practice Toolbox: Practice facilitation
This is the eighth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Last month’s article discussed AHRQ’s tool and resources for practice transformation, or how to help make your practice ready for advances such as shared decision making, team-based care, and integrating behavioral health and primary care. Use of practice facilitation, an evidence-based approach to quality improvement, can be a key element to helping primary care practices make the necessary changes for transformation. Practice facilitators (also known as practice coaches, quality improvement coaches, or practice enhancement assistants) are specially trained individuals who assist primary care clinicians in research and quality improvement projects. They are distinguished from consultants through specialized training, broad scope of practice, and long-term relationships with an organization, its staff and clinicians, and its patients.
If you are wondering how a practice facilitator can help you, AHRQ offers How a Practice Facilitator Can Support Your Practice. This tip sheet provides ideas and techniques for primary care practices interested in getting started with quality improvement activities and describes the benefits of working with a practice facilitator. The tip sheet is distilled from a more extensive white paper on Engaging Primary Care Practices in Quality Improvement: Strategies for Practice Facilitators, which presents a framework for engaging primary care practices in quality improvement and provides strategies for sustained involvement in the undertaking.
For those with greater interest in implementation of practice facilitation, AHRQ offers the Practice Facilitation Handbook: Training Modules for New Facilitators and Their Trainers. The Handbook is designed to assist in the training of new practice facilitators as they begin to develop the knowledge and skills needed to support meaningful improvement in primary care practices. AHRQ built upon the modules in the Handbook with the Primary Care Practice Facilitation Curriculum. The Curriculum updates the modules in the Handbook and adds an additional twelve modules for a total of 32 modules. More importantly, some of the modules can be used by clinicians and staff as a sort of Quality Improvement 101. Modules on appreciative inquiry, approaches to quality improvement, redesigning work flow, root cause analysis, and measuring clinical performance can be useful to anyone interested in increasing their knowledge and skills for quality improvement.
Mr. McNellis is senior adviser for primary care at AHRQ and Dr. Ganiats is director of the National Center for Excellence in Primary Care Research at AHRQ.
Links from the AHRQ Web site:
How a Practice Facilitator Can Support Your Practice
Engaging Primary Care Practices in Quality Improvement: Strategies for Practice Facilitators
Primary Care Practice Facilitation Curriculum
Practice Facilitation Handbook
A How-To Guide on Developing and Running a Practice Facilitation Program
These and other tools can be found at the NCEPCR Web site.
This is the eighth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Last month’s article discussed AHRQ’s tool and resources for practice transformation, or how to help make your practice ready for advances such as shared decision making, team-based care, and integrating behavioral health and primary care. Use of practice facilitation, an evidence-based approach to quality improvement, can be a key element to helping primary care practices make the necessary changes for transformation. Practice facilitators (also known as practice coaches, quality improvement coaches, or practice enhancement assistants) are specially trained individuals who assist primary care clinicians in research and quality improvement projects. They are distinguished from consultants through specialized training, broad scope of practice, and long-term relationships with an organization, its staff and clinicians, and its patients.
If you are wondering how a practice facilitator can help you, AHRQ offers How a Practice Facilitator Can Support Your Practice. This tip sheet provides ideas and techniques for primary care practices interested in getting started with quality improvement activities and describes the benefits of working with a practice facilitator. The tip sheet is distilled from a more extensive white paper on Engaging Primary Care Practices in Quality Improvement: Strategies for Practice Facilitators, which presents a framework for engaging primary care practices in quality improvement and provides strategies for sustained involvement in the undertaking.
For those with greater interest in implementation of practice facilitation, AHRQ offers the Practice Facilitation Handbook: Training Modules for New Facilitators and Their Trainers. The Handbook is designed to assist in the training of new practice facilitators as they begin to develop the knowledge and skills needed to support meaningful improvement in primary care practices. AHRQ built upon the modules in the Handbook with the Primary Care Practice Facilitation Curriculum. The Curriculum updates the modules in the Handbook and adds an additional twelve modules for a total of 32 modules. More importantly, some of the modules can be used by clinicians and staff as a sort of Quality Improvement 101. Modules on appreciative inquiry, approaches to quality improvement, redesigning work flow, root cause analysis, and measuring clinical performance can be useful to anyone interested in increasing their knowledge and skills for quality improvement.
Mr. McNellis is senior adviser for primary care at AHRQ and Dr. Ganiats is director of the National Center for Excellence in Primary Care Research at AHRQ.
Links from the AHRQ Web site:
How a Practice Facilitator Can Support Your Practice
Engaging Primary Care Practices in Quality Improvement: Strategies for Practice Facilitators
Primary Care Practice Facilitation Curriculum
Practice Facilitation Handbook
A How-To Guide on Developing and Running a Practice Facilitation Program
These and other tools can be found at the NCEPCR Web site.
This is the eighth in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Last month’s article discussed AHRQ’s tool and resources for practice transformation, or how to help make your practice ready for advances such as shared decision making, team-based care, and integrating behavioral health and primary care. Use of practice facilitation, an evidence-based approach to quality improvement, can be a key element to helping primary care practices make the necessary changes for transformation. Practice facilitators (also known as practice coaches, quality improvement coaches, or practice enhancement assistants) are specially trained individuals who assist primary care clinicians in research and quality improvement projects. They are distinguished from consultants through specialized training, broad scope of practice, and long-term relationships with an organization, its staff and clinicians, and its patients.
If you are wondering how a practice facilitator can help you, AHRQ offers How a Practice Facilitator Can Support Your Practice. This tip sheet provides ideas and techniques for primary care practices interested in getting started with quality improvement activities and describes the benefits of working with a practice facilitator. The tip sheet is distilled from a more extensive white paper on Engaging Primary Care Practices in Quality Improvement: Strategies for Practice Facilitators, which presents a framework for engaging primary care practices in quality improvement and provides strategies for sustained involvement in the undertaking.
For those with greater interest in implementation of practice facilitation, AHRQ offers the Practice Facilitation Handbook: Training Modules for New Facilitators and Their Trainers. The Handbook is designed to assist in the training of new practice facilitators as they begin to develop the knowledge and skills needed to support meaningful improvement in primary care practices. AHRQ built upon the modules in the Handbook with the Primary Care Practice Facilitation Curriculum. The Curriculum updates the modules in the Handbook and adds an additional twelve modules for a total of 32 modules. More importantly, some of the modules can be used by clinicians and staff as a sort of Quality Improvement 101. Modules on appreciative inquiry, approaches to quality improvement, redesigning work flow, root cause analysis, and measuring clinical performance can be useful to anyone interested in increasing their knowledge and skills for quality improvement.
Mr. McNellis is senior adviser for primary care at AHRQ and Dr. Ganiats is director of the National Center for Excellence in Primary Care Research at AHRQ.
Links from the AHRQ Web site:
How a Practice Facilitator Can Support Your Practice
Engaging Primary Care Practices in Quality Improvement: Strategies for Practice Facilitators
Primary Care Practice Facilitation Curriculum
Practice Facilitation Handbook
A How-To Guide on Developing and Running a Practice Facilitation Program
These and other tools can be found at the NCEPCR Web site.
It costs what?! How we can educate residents and students on how much things cost
“Why are you ordering a CBC on the patient when her white blood cell count, hemoglobin, and platelets have been stable for the past 3 days?” sternly inquired the attending gynecologic oncologist. “Don’t order tests without any clinical indication. If she is infected or bleeding, there will be signs and thus an indication to order a CBC. The physical exam is your test.” There was an authoritative pause before he invoked the “value-based care” maxim.
For many residents who graduated in the past decade, education in value-based care and alternative payment models (APMs) was cobbled together from experience, demonstrated by attendings who labeled it as such, and from rare didactic education classroom sessions and inpatient environments.
In today’s health care environment, professional survival requires the ability to successfully deliver high-value care to patients. Attendings often illustrate and champion how to do this by using patient care to highlight the definition: Value = Quality ÷ Cost.
For residency education programs to create the ObGyns of the future, they must teach trainees what they will be evaluated on and held accountable for.1 Today’s clinicians will have to take responsibility for reigning in health care costs from the fee-for-service era, which in the United States have snowballed into one of the unhealthiest cost-to-outcomes ratios worldwide. Residents will be required to understand not only value but also areas in which they can influence the cost of care and how their outcome metrics are valued.
Modifiable factors in value-based care
As mentioned, value is defined by the equation, Value = Quality ÷ Cost. The granularity of these terms helps clarify the depth and the multitude of levels that clinicians can modify and influence to achieve the highest value.
Quality, as defined by the National Academy of Medicine, includes2:
- effectiveness: providing care processes and achieving outcomes as supported by scientific evidence
- efficiency: maximizing the quality of a comparable unit of health care delivered or unit of health benefit achieved for a given unit of health care resources used
- equity: providing health care of equal quality to those who may differ in personal characteristics other than their clinical condition or preferences for care
- patient-centeredness: meeting patient needs and preferences and providing education and support
- safety: actual or potential bodily harm
- timeliness: obtaining needed care while minimizing delays.
From electronic health records, which were mandated in the Patient Protection and Affordable Care Act of 2010, offices, hospitals, and medical systems have gained robust databases of mineable information. Even data abstraction from paper records has been made easier, allowing better reflection of practitioner-based delivery of care.
Understanding cost breakdown in the overall value equation
With regard to value-based care, cost is generally related to money. When broadly explored, however, cost can be broken down into cost to the patient, the health care system, and society this way:
- patient: time spent receiving evaluation and management from a clinician; money spent for family care needs while undergoing management; money spent for procedures and tests; wages lost due to appointments
- health system: preventive services versus costly emergency room visit; community-based interventions to improve population health
- society: cost to tax payers; equitable distribution of vital resources (for example, vaccines); prevention of iatrogenic antibiotic resistance.
To understand how physicians are paid, it is important to see how payers value our services. The Centers for Medicare and Medicaid Services states that it is “promoting value-based care as part of its larger quality strategy to reform how health care is delivered and paid for.” In 2018, the US Department of Health and Human Services is striving to have half of Medicare payments in APMs.3
It is the physician’s responsibility to recognize that costs to the patient, payer, health system, and society can compete with and directly influence the outcome of each other. For example, because the patient pays an insurance premium to participate in a risk pool where cost-sharing is the primary cost-containment strategy, poor-value interventions can directly translate into increased premiums, copayments, or deductibles for the entire pool.4
By clearly identifying the different variables involved in the value-based care equation, residents can better understand their responsibility in their day-to-day work in medicine to address value, not just quality or cost. Clarifying the tenets of value-based care will help guide educators in identifying “teaching moments” and organizing didactic sessions focused on practical implementation of value.
Less is more
In our opening anecdote, the attending shows how curbing overuse of resources can increase the value of care delivered. But that example illustrates only one of the many levels on which educators can help residents understand their impact on value. A multidisciplinary education that incorporates outpatient and inpatient pharmacists, social workers, occupational therapists, pelvic floor physiotherapists, office staff, billing specialists, operating room (OR) technologists, and others can be beneficial in learning how to deliver high-value care.
Read about selecting value-based interventions at work.
Value-based interventions at work
In the discussion that follows, we illustrate how residents can identify, evaluate, and put into practice value-based interventions that can occur at multiple levels.
Antibiotic selection. Resident choices for outpatient antibiotics can severely affect patient adherence. Subtle differences in the formulation of certain antibiotics affect the price and thus pose a significant potential obstacle. Judicious use of inexpensive drug formulations with fewer dosing frequencies can help patients engage in their own care.
Knowing the pharmacologic difference between doxycycline hyclate and doxycycline monohydrate, for example, is to know the difference between esoteric salts—undeniably worthless information with regard to successfully treating a patient’s infection. Knowing that one formula is on the bargain formulary at the patient’s local pharmacy, or that one drug requires twice-daily dosing versus 4-times-daily dosing, however, can mean the difference between the patient’s adherence or nonadherence to your expert recommendation.
Contraception options. Contraceptives pose a challenge with respect to value because of the myriad delivery systems, doses, and generic formulations available. There are dozens of oral contraceptive pills (OCPs) on the market that vary in their dosing, phasic nature (monophasic, multiphasic), iron content in the hormone-free week, and different progestogens for different conditions (such as drospirenone for androgen excess).
When weighing contraceptive options, the clinician must look at value not only from a cost perspective but also from an effectiveness perspective. The desired outcome in this scenario is preventing unwanted pregnancy with ideal or typical contraceptive use at the most inexpensive price point. When working within the value equation, the clinician must individualize the prescribed contraceptive to one that is most acceptable to the patient and that optimizes the various costs and quality measures. “Cost” can mean the cost of OCPs, menstrual control products, backup contraception, failed or unwanted pregnancy management, or suffering lost wages from missed days of work from, for example, dysmenorrhea. “Quality” can mean a low contraceptive failure rate, predictable cyclicality, the need for patient administration and the risk of forgetting, and the need for backup contraceptives.
In comparing the subdermal contraceptive implant (which can cost up to $1,300 every 3 years, equivalent to $36.11 per month) with OCPs (which can cost as low as $324 for 3 years for an ethinyl estradiol and norgestimate combination, or $9 per month), the OCPs significantly outweigh the implant in terms of cost. When comparing failure rates, the degree of patient intervention, and decreased use of menstrual control products due to amenorrhea, the subdermal contraceptive wins. As we know, long-acting reversible contraception (LARC), including the intrauterine device (IUD) and subdermal implant, is the most effective but often the most expensive contraceptive option.5 When cost is evaluated from a global perspective, as highlighted by the adage “an IUD is cheaper than a baby,” the LARC’s value is derived from its overall high effectiveness and low cost.
If the patient elects to choose OCPs, the clinician should direct the prescription to a pharmacy that has discounted generic pills on its formulary. Generic OCPs have a low- cost burden without loss of efficacy, thus providing maximal value.6 This requires an intimate knowledge of the local pharmacies and what their formularies provide. Sometimes the patient will need to drive out of her way to access cost-effective, quality medications, or the high-value option.
Surgery considerations. Judicious instrument selection in the OR can decrease overall operative costs. While most advanced sealing and cutting instrumentation is for single use, for example, it also can be reprocessed for reuse. Although the cost of reprocessed, single-use instruments is lower, studies evaluating the quality of these instruments “found a significant rate of physical defects, performance issues, or improper decontamination.”7
Marketing largely has driven physician choice in the use of certain vessel sealing and cutting devices, but there has yet to be evidence that using any one device actually improves performance or outcomes, such as length of surgery, blood loss, or postoperative complications. Technology companies that create these instruments likely will have to start designing studies to test performance and outcomes as they relate to their devices to persuade hospital systems that using their products improves outcomes and reduces costs.
While learning laparoscopic hysterectomy, residents may see that some attending surgeons can complete the entire procedure with monopolar scissors, bipolar forceps, and laparoscopic needle drivers, while other surgeons use those instruments plus others, such as a LigaSure instrument or a Harmonic scalpel. With outcomes being the same between these surgeons, it is reasonable for hospitals to audit each surgeon using the Value = Quality ÷ Cost equation and to seek data to describe why the latter surgeon requires additional instrumentation.
Residency training poses a unique opportunity for physicians to learn numerous ways to perform the same procedure so they can fill their armamentarium with various effective techniques. Residency also should be a time in which proficiency with basic surgical instrumentation is emphasized. Attending physicians can help residents improve their skills, for example, by having them use only one advanced sealing and cutting device, or no device at all. This practice will make the trainee better able to adapt to situations in which an advanced device may fail or be unavailable. Future performance metrics may evaluate the physician’s cost effectiveness with regard to single-use instruments during routine surgical procedures.
Standardized order sets. Evidence-based order sets help in the management of pneumonia, sepsis, deep vein thrombosis prophylaxis, and numerous other conditions. In the era of computerized physician order entry systems (CPOEs), a resident needs to enter just a few clicks to order all necessary tests, interventions, and imaging studies for a condition. In one fell swoop, orders are placed not only for admission but also for the patient’s entire hospitalization. The paradox of the order set is that it uses a template to deliver individualized patient-centered care.
In the age of enhanced recovery pathways after surgery, we see patients who undergo a hysterectomy being discharged home directly from the postoperative anesthesia care unit (PACU). Generally, follow-up laboratory testing is not ordered on an outpatient basis. If, however, the patient needs to remain in the hospital for social reasons (such as delayed PACU transfer, transportation, weather), she receives the standardized orders from the post hysterectomy order set: a morning complete blood count ($55) with a basic metabolic panel ($45). As an academic exercise, the order set may help residents learn which orders they must consider when admitting a postoperative hysterectomy patient, but overuse of order sets can be a setback for a value-based care system.
Read about evaluating competence and individualizing care.
Evaluating competence in value-based care
Research is an integral component of all residency programs accredited by the Accreditation Council for Graduate Medical Education (ACGME). The implementation of value-based care—with all its nuances, quality metrics, and cost parameters—creates a space for resident-led studies to contribute to peer education. The ACGME’s Obstetrics and Gynecology Milestones project was developed to assess the development of ObGyn residents’ competence as they progress through training. Despite national laws tying reimbursements to value-based care, there is no mention of value as it relates to the basic formula, Value = Quality ÷ Cost, in the project.
With the nuances that value-based care offers, it would behoove the Council on Resident Education in Obstetrics and Gynecology of the American College of Obstetricians and Gynecologists to incorporate a method of evaluation to determine competence in this evolving field.
Care also must be individualized
Academic ObGyns and instructors should focus their pedagogy not only on value-based care but also on individualized care that will maximize desired outcomes for each patient. Incorporating multidisciplinary didactics, focused research, and a 360-degree evaluation in the residency curriculum will create new ObGyns who are known for successfully delivering high-value care.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Wieand E, Lagrew DC Jr. Value-based payment: what does it mean, and how can ObGyns get out ahead? OBG Manag. 2018;30(1):17–19, 25–26.
- Agency for Healthcare Research and Quality. The six domains of health care quality. https://www.ahrq.gov/professionals/quality-patient-safety/talkingquality/create/sixdomains.html. Reviewed March 2016. Accessed March 22, 2018.
- Centers for Medicare and Medicaid Services. Better care. Smarter spending. Healthier people: paying providers for value, not volume. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-01-26-3.html. Published January 26, 2015. Accessed March 22, 2018.
- Society for Human Resource Management. Managing health care costs. https://www.shrm.org/resourcesandtools/tools-and-samples/toolkits/pages/managinghealthcarecosts.aspx. Published January 11, 2017. Accessed March 18, 2018.
- American College of Obstetricians and Gynecologists Committee on Gynecologic Practice, Long-Acting Reversible Contraception Working Group. ACOG Committee Opinion No. 642: Increasing access to contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet Gynecol. 2015;126(4):e44–e48.
- American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. ACOG Committee Opinion No. 375: Brand versus generic oral contraceptives. Obstet Gynecol. 2007;110(2 pt 1):447–448.
- American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. ACOG Committee Opinion No. 537: R
eprocessed single-use devices. Obstet Gynecol. 2012;120(4):974–976.
“Why are you ordering a CBC on the patient when her white blood cell count, hemoglobin, and platelets have been stable for the past 3 days?” sternly inquired the attending gynecologic oncologist. “Don’t order tests without any clinical indication. If she is infected or bleeding, there will be signs and thus an indication to order a CBC. The physical exam is your test.” There was an authoritative pause before he invoked the “value-based care” maxim.
For many residents who graduated in the past decade, education in value-based care and alternative payment models (APMs) was cobbled together from experience, demonstrated by attendings who labeled it as such, and from rare didactic education classroom sessions and inpatient environments.
In today’s health care environment, professional survival requires the ability to successfully deliver high-value care to patients. Attendings often illustrate and champion how to do this by using patient care to highlight the definition: Value = Quality ÷ Cost.
For residency education programs to create the ObGyns of the future, they must teach trainees what they will be evaluated on and held accountable for.1 Today’s clinicians will have to take responsibility for reigning in health care costs from the fee-for-service era, which in the United States have snowballed into one of the unhealthiest cost-to-outcomes ratios worldwide. Residents will be required to understand not only value but also areas in which they can influence the cost of care and how their outcome metrics are valued.
Modifiable factors in value-based care
As mentioned, value is defined by the equation, Value = Quality ÷ Cost. The granularity of these terms helps clarify the depth and the multitude of levels that clinicians can modify and influence to achieve the highest value.
Quality, as defined by the National Academy of Medicine, includes2:
- effectiveness: providing care processes and achieving outcomes as supported by scientific evidence
- efficiency: maximizing the quality of a comparable unit of health care delivered or unit of health benefit achieved for a given unit of health care resources used
- equity: providing health care of equal quality to those who may differ in personal characteristics other than their clinical condition or preferences for care
- patient-centeredness: meeting patient needs and preferences and providing education and support
- safety: actual or potential bodily harm
- timeliness: obtaining needed care while minimizing delays.
From electronic health records, which were mandated in the Patient Protection and Affordable Care Act of 2010, offices, hospitals, and medical systems have gained robust databases of mineable information. Even data abstraction from paper records has been made easier, allowing better reflection of practitioner-based delivery of care.
Understanding cost breakdown in the overall value equation
With regard to value-based care, cost is generally related to money. When broadly explored, however, cost can be broken down into cost to the patient, the health care system, and society this way:
- patient: time spent receiving evaluation and management from a clinician; money spent for family care needs while undergoing management; money spent for procedures and tests; wages lost due to appointments
- health system: preventive services versus costly emergency room visit; community-based interventions to improve population health
- society: cost to tax payers; equitable distribution of vital resources (for example, vaccines); prevention of iatrogenic antibiotic resistance.
To understand how physicians are paid, it is important to see how payers value our services. The Centers for Medicare and Medicaid Services states that it is “promoting value-based care as part of its larger quality strategy to reform how health care is delivered and paid for.” In 2018, the US Department of Health and Human Services is striving to have half of Medicare payments in APMs.3
It is the physician’s responsibility to recognize that costs to the patient, payer, health system, and society can compete with and directly influence the outcome of each other. For example, because the patient pays an insurance premium to participate in a risk pool where cost-sharing is the primary cost-containment strategy, poor-value interventions can directly translate into increased premiums, copayments, or deductibles for the entire pool.4
By clearly identifying the different variables involved in the value-based care equation, residents can better understand their responsibility in their day-to-day work in medicine to address value, not just quality or cost. Clarifying the tenets of value-based care will help guide educators in identifying “teaching moments” and organizing didactic sessions focused on practical implementation of value.
Less is more
In our opening anecdote, the attending shows how curbing overuse of resources can increase the value of care delivered. But that example illustrates only one of the many levels on which educators can help residents understand their impact on value. A multidisciplinary education that incorporates outpatient and inpatient pharmacists, social workers, occupational therapists, pelvic floor physiotherapists, office staff, billing specialists, operating room (OR) technologists, and others can be beneficial in learning how to deliver high-value care.
Read about selecting value-based interventions at work.
Value-based interventions at work
In the discussion that follows, we illustrate how residents can identify, evaluate, and put into practice value-based interventions that can occur at multiple levels.
Antibiotic selection. Resident choices for outpatient antibiotics can severely affect patient adherence. Subtle differences in the formulation of certain antibiotics affect the price and thus pose a significant potential obstacle. Judicious use of inexpensive drug formulations with fewer dosing frequencies can help patients engage in their own care.
Knowing the pharmacologic difference between doxycycline hyclate and doxycycline monohydrate, for example, is to know the difference between esoteric salts—undeniably worthless information with regard to successfully treating a patient’s infection. Knowing that one formula is on the bargain formulary at the patient’s local pharmacy, or that one drug requires twice-daily dosing versus 4-times-daily dosing, however, can mean the difference between the patient’s adherence or nonadherence to your expert recommendation.
Contraception options. Contraceptives pose a challenge with respect to value because of the myriad delivery systems, doses, and generic formulations available. There are dozens of oral contraceptive pills (OCPs) on the market that vary in their dosing, phasic nature (monophasic, multiphasic), iron content in the hormone-free week, and different progestogens for different conditions (such as drospirenone for androgen excess).
When weighing contraceptive options, the clinician must look at value not only from a cost perspective but also from an effectiveness perspective. The desired outcome in this scenario is preventing unwanted pregnancy with ideal or typical contraceptive use at the most inexpensive price point. When working within the value equation, the clinician must individualize the prescribed contraceptive to one that is most acceptable to the patient and that optimizes the various costs and quality measures. “Cost” can mean the cost of OCPs, menstrual control products, backup contraception, failed or unwanted pregnancy management, or suffering lost wages from missed days of work from, for example, dysmenorrhea. “Quality” can mean a low contraceptive failure rate, predictable cyclicality, the need for patient administration and the risk of forgetting, and the need for backup contraceptives.
In comparing the subdermal contraceptive implant (which can cost up to $1,300 every 3 years, equivalent to $36.11 per month) with OCPs (which can cost as low as $324 for 3 years for an ethinyl estradiol and norgestimate combination, or $9 per month), the OCPs significantly outweigh the implant in terms of cost. When comparing failure rates, the degree of patient intervention, and decreased use of menstrual control products due to amenorrhea, the subdermal contraceptive wins. As we know, long-acting reversible contraception (LARC), including the intrauterine device (IUD) and subdermal implant, is the most effective but often the most expensive contraceptive option.5 When cost is evaluated from a global perspective, as highlighted by the adage “an IUD is cheaper than a baby,” the LARC’s value is derived from its overall high effectiveness and low cost.
If the patient elects to choose OCPs, the clinician should direct the prescription to a pharmacy that has discounted generic pills on its formulary. Generic OCPs have a low- cost burden without loss of efficacy, thus providing maximal value.6 This requires an intimate knowledge of the local pharmacies and what their formularies provide. Sometimes the patient will need to drive out of her way to access cost-effective, quality medications, or the high-value option.
Surgery considerations. Judicious instrument selection in the OR can decrease overall operative costs. While most advanced sealing and cutting instrumentation is for single use, for example, it also can be reprocessed for reuse. Although the cost of reprocessed, single-use instruments is lower, studies evaluating the quality of these instruments “found a significant rate of physical defects, performance issues, or improper decontamination.”7
Marketing largely has driven physician choice in the use of certain vessel sealing and cutting devices, but there has yet to be evidence that using any one device actually improves performance or outcomes, such as length of surgery, blood loss, or postoperative complications. Technology companies that create these instruments likely will have to start designing studies to test performance and outcomes as they relate to their devices to persuade hospital systems that using their products improves outcomes and reduces costs.
While learning laparoscopic hysterectomy, residents may see that some attending surgeons can complete the entire procedure with monopolar scissors, bipolar forceps, and laparoscopic needle drivers, while other surgeons use those instruments plus others, such as a LigaSure instrument or a Harmonic scalpel. With outcomes being the same between these surgeons, it is reasonable for hospitals to audit each surgeon using the Value = Quality ÷ Cost equation and to seek data to describe why the latter surgeon requires additional instrumentation.
Residency training poses a unique opportunity for physicians to learn numerous ways to perform the same procedure so they can fill their armamentarium with various effective techniques. Residency also should be a time in which proficiency with basic surgical instrumentation is emphasized. Attending physicians can help residents improve their skills, for example, by having them use only one advanced sealing and cutting device, or no device at all. This practice will make the trainee better able to adapt to situations in which an advanced device may fail or be unavailable. Future performance metrics may evaluate the physician’s cost effectiveness with regard to single-use instruments during routine surgical procedures.
Standardized order sets. Evidence-based order sets help in the management of pneumonia, sepsis, deep vein thrombosis prophylaxis, and numerous other conditions. In the era of computerized physician order entry systems (CPOEs), a resident needs to enter just a few clicks to order all necessary tests, interventions, and imaging studies for a condition. In one fell swoop, orders are placed not only for admission but also for the patient’s entire hospitalization. The paradox of the order set is that it uses a template to deliver individualized patient-centered care.
In the age of enhanced recovery pathways after surgery, we see patients who undergo a hysterectomy being discharged home directly from the postoperative anesthesia care unit (PACU). Generally, follow-up laboratory testing is not ordered on an outpatient basis. If, however, the patient needs to remain in the hospital for social reasons (such as delayed PACU transfer, transportation, weather), she receives the standardized orders from the post hysterectomy order set: a morning complete blood count ($55) with a basic metabolic panel ($45). As an academic exercise, the order set may help residents learn which orders they must consider when admitting a postoperative hysterectomy patient, but overuse of order sets can be a setback for a value-based care system.
Read about evaluating competence and individualizing care.
Evaluating competence in value-based care
Research is an integral component of all residency programs accredited by the Accreditation Council for Graduate Medical Education (ACGME). The implementation of value-based care—with all its nuances, quality metrics, and cost parameters—creates a space for resident-led studies to contribute to peer education. The ACGME’s Obstetrics and Gynecology Milestones project was developed to assess the development of ObGyn residents’ competence as they progress through training. Despite national laws tying reimbursements to value-based care, there is no mention of value as it relates to the basic formula, Value = Quality ÷ Cost, in the project.
With the nuances that value-based care offers, it would behoove the Council on Resident Education in Obstetrics and Gynecology of the American College of Obstetricians and Gynecologists to incorporate a method of evaluation to determine competence in this evolving field.
Care also must be individualized
Academic ObGyns and instructors should focus their pedagogy not only on value-based care but also on individualized care that will maximize desired outcomes for each patient. Incorporating multidisciplinary didactics, focused research, and a 360-degree evaluation in the residency curriculum will create new ObGyns who are known for successfully delivering high-value care.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“Why are you ordering a CBC on the patient when her white blood cell count, hemoglobin, and platelets have been stable for the past 3 days?” sternly inquired the attending gynecologic oncologist. “Don’t order tests without any clinical indication. If she is infected or bleeding, there will be signs and thus an indication to order a CBC. The physical exam is your test.” There was an authoritative pause before he invoked the “value-based care” maxim.
For many residents who graduated in the past decade, education in value-based care and alternative payment models (APMs) was cobbled together from experience, demonstrated by attendings who labeled it as such, and from rare didactic education classroom sessions and inpatient environments.
In today’s health care environment, professional survival requires the ability to successfully deliver high-value care to patients. Attendings often illustrate and champion how to do this by using patient care to highlight the definition: Value = Quality ÷ Cost.
For residency education programs to create the ObGyns of the future, they must teach trainees what they will be evaluated on and held accountable for.1 Today’s clinicians will have to take responsibility for reigning in health care costs from the fee-for-service era, which in the United States have snowballed into one of the unhealthiest cost-to-outcomes ratios worldwide. Residents will be required to understand not only value but also areas in which they can influence the cost of care and how their outcome metrics are valued.
Modifiable factors in value-based care
As mentioned, value is defined by the equation, Value = Quality ÷ Cost. The granularity of these terms helps clarify the depth and the multitude of levels that clinicians can modify and influence to achieve the highest value.
Quality, as defined by the National Academy of Medicine, includes2:
- effectiveness: providing care processes and achieving outcomes as supported by scientific evidence
- efficiency: maximizing the quality of a comparable unit of health care delivered or unit of health benefit achieved for a given unit of health care resources used
- equity: providing health care of equal quality to those who may differ in personal characteristics other than their clinical condition or preferences for care
- patient-centeredness: meeting patient needs and preferences and providing education and support
- safety: actual or potential bodily harm
- timeliness: obtaining needed care while minimizing delays.
From electronic health records, which were mandated in the Patient Protection and Affordable Care Act of 2010, offices, hospitals, and medical systems have gained robust databases of mineable information. Even data abstraction from paper records has been made easier, allowing better reflection of practitioner-based delivery of care.
Understanding cost breakdown in the overall value equation
With regard to value-based care, cost is generally related to money. When broadly explored, however, cost can be broken down into cost to the patient, the health care system, and society this way:
- patient: time spent receiving evaluation and management from a clinician; money spent for family care needs while undergoing management; money spent for procedures and tests; wages lost due to appointments
- health system: preventive services versus costly emergency room visit; community-based interventions to improve population health
- society: cost to tax payers; equitable distribution of vital resources (for example, vaccines); prevention of iatrogenic antibiotic resistance.
To understand how physicians are paid, it is important to see how payers value our services. The Centers for Medicare and Medicaid Services states that it is “promoting value-based care as part of its larger quality strategy to reform how health care is delivered and paid for.” In 2018, the US Department of Health and Human Services is striving to have half of Medicare payments in APMs.3
It is the physician’s responsibility to recognize that costs to the patient, payer, health system, and society can compete with and directly influence the outcome of each other. For example, because the patient pays an insurance premium to participate in a risk pool where cost-sharing is the primary cost-containment strategy, poor-value interventions can directly translate into increased premiums, copayments, or deductibles for the entire pool.4
By clearly identifying the different variables involved in the value-based care equation, residents can better understand their responsibility in their day-to-day work in medicine to address value, not just quality or cost. Clarifying the tenets of value-based care will help guide educators in identifying “teaching moments” and organizing didactic sessions focused on practical implementation of value.
Less is more
In our opening anecdote, the attending shows how curbing overuse of resources can increase the value of care delivered. But that example illustrates only one of the many levels on which educators can help residents understand their impact on value. A multidisciplinary education that incorporates outpatient and inpatient pharmacists, social workers, occupational therapists, pelvic floor physiotherapists, office staff, billing specialists, operating room (OR) technologists, and others can be beneficial in learning how to deliver high-value care.
Read about selecting value-based interventions at work.
Value-based interventions at work
In the discussion that follows, we illustrate how residents can identify, evaluate, and put into practice value-based interventions that can occur at multiple levels.
Antibiotic selection. Resident choices for outpatient antibiotics can severely affect patient adherence. Subtle differences in the formulation of certain antibiotics affect the price and thus pose a significant potential obstacle. Judicious use of inexpensive drug formulations with fewer dosing frequencies can help patients engage in their own care.
Knowing the pharmacologic difference between doxycycline hyclate and doxycycline monohydrate, for example, is to know the difference between esoteric salts—undeniably worthless information with regard to successfully treating a patient’s infection. Knowing that one formula is on the bargain formulary at the patient’s local pharmacy, or that one drug requires twice-daily dosing versus 4-times-daily dosing, however, can mean the difference between the patient’s adherence or nonadherence to your expert recommendation.
Contraception options. Contraceptives pose a challenge with respect to value because of the myriad delivery systems, doses, and generic formulations available. There are dozens of oral contraceptive pills (OCPs) on the market that vary in their dosing, phasic nature (monophasic, multiphasic), iron content in the hormone-free week, and different progestogens for different conditions (such as drospirenone for androgen excess).
When weighing contraceptive options, the clinician must look at value not only from a cost perspective but also from an effectiveness perspective. The desired outcome in this scenario is preventing unwanted pregnancy with ideal or typical contraceptive use at the most inexpensive price point. When working within the value equation, the clinician must individualize the prescribed contraceptive to one that is most acceptable to the patient and that optimizes the various costs and quality measures. “Cost” can mean the cost of OCPs, menstrual control products, backup contraception, failed or unwanted pregnancy management, or suffering lost wages from missed days of work from, for example, dysmenorrhea. “Quality” can mean a low contraceptive failure rate, predictable cyclicality, the need for patient administration and the risk of forgetting, and the need for backup contraceptives.
In comparing the subdermal contraceptive implant (which can cost up to $1,300 every 3 years, equivalent to $36.11 per month) with OCPs (which can cost as low as $324 for 3 years for an ethinyl estradiol and norgestimate combination, or $9 per month), the OCPs significantly outweigh the implant in terms of cost. When comparing failure rates, the degree of patient intervention, and decreased use of menstrual control products due to amenorrhea, the subdermal contraceptive wins. As we know, long-acting reversible contraception (LARC), including the intrauterine device (IUD) and subdermal implant, is the most effective but often the most expensive contraceptive option.5 When cost is evaluated from a global perspective, as highlighted by the adage “an IUD is cheaper than a baby,” the LARC’s value is derived from its overall high effectiveness and low cost.
If the patient elects to choose OCPs, the clinician should direct the prescription to a pharmacy that has discounted generic pills on its formulary. Generic OCPs have a low- cost burden without loss of efficacy, thus providing maximal value.6 This requires an intimate knowledge of the local pharmacies and what their formularies provide. Sometimes the patient will need to drive out of her way to access cost-effective, quality medications, or the high-value option.
Surgery considerations. Judicious instrument selection in the OR can decrease overall operative costs. While most advanced sealing and cutting instrumentation is for single use, for example, it also can be reprocessed for reuse. Although the cost of reprocessed, single-use instruments is lower, studies evaluating the quality of these instruments “found a significant rate of physical defects, performance issues, or improper decontamination.”7
Marketing largely has driven physician choice in the use of certain vessel sealing and cutting devices, but there has yet to be evidence that using any one device actually improves performance or outcomes, such as length of surgery, blood loss, or postoperative complications. Technology companies that create these instruments likely will have to start designing studies to test performance and outcomes as they relate to their devices to persuade hospital systems that using their products improves outcomes and reduces costs.
While learning laparoscopic hysterectomy, residents may see that some attending surgeons can complete the entire procedure with monopolar scissors, bipolar forceps, and laparoscopic needle drivers, while other surgeons use those instruments plus others, such as a LigaSure instrument or a Harmonic scalpel. With outcomes being the same between these surgeons, it is reasonable for hospitals to audit each surgeon using the Value = Quality ÷ Cost equation and to seek data to describe why the latter surgeon requires additional instrumentation.
Residency training poses a unique opportunity for physicians to learn numerous ways to perform the same procedure so they can fill their armamentarium with various effective techniques. Residency also should be a time in which proficiency with basic surgical instrumentation is emphasized. Attending physicians can help residents improve their skills, for example, by having them use only one advanced sealing and cutting device, or no device at all. This practice will make the trainee better able to adapt to situations in which an advanced device may fail or be unavailable. Future performance metrics may evaluate the physician’s cost effectiveness with regard to single-use instruments during routine surgical procedures.
Standardized order sets. Evidence-based order sets help in the management of pneumonia, sepsis, deep vein thrombosis prophylaxis, and numerous other conditions. In the era of computerized physician order entry systems (CPOEs), a resident needs to enter just a few clicks to order all necessary tests, interventions, and imaging studies for a condition. In one fell swoop, orders are placed not only for admission but also for the patient’s entire hospitalization. The paradox of the order set is that it uses a template to deliver individualized patient-centered care.
In the age of enhanced recovery pathways after surgery, we see patients who undergo a hysterectomy being discharged home directly from the postoperative anesthesia care unit (PACU). Generally, follow-up laboratory testing is not ordered on an outpatient basis. If, however, the patient needs to remain in the hospital for social reasons (such as delayed PACU transfer, transportation, weather), she receives the standardized orders from the post hysterectomy order set: a morning complete blood count ($55) with a basic metabolic panel ($45). As an academic exercise, the order set may help residents learn which orders they must consider when admitting a postoperative hysterectomy patient, but overuse of order sets can be a setback for a value-based care system.
Read about evaluating competence and individualizing care.
Evaluating competence in value-based care
Research is an integral component of all residency programs accredited by the Accreditation Council for Graduate Medical Education (ACGME). The implementation of value-based care—with all its nuances, quality metrics, and cost parameters—creates a space for resident-led studies to contribute to peer education. The ACGME’s Obstetrics and Gynecology Milestones project was developed to assess the development of ObGyn residents’ competence as they progress through training. Despite national laws tying reimbursements to value-based care, there is no mention of value as it relates to the basic formula, Value = Quality ÷ Cost, in the project.
With the nuances that value-based care offers, it would behoove the Council on Resident Education in Obstetrics and Gynecology of the American College of Obstetricians and Gynecologists to incorporate a method of evaluation to determine competence in this evolving field.
Care also must be individualized
Academic ObGyns and instructors should focus their pedagogy not only on value-based care but also on individualized care that will maximize desired outcomes for each patient. Incorporating multidisciplinary didactics, focused research, and a 360-degree evaluation in the residency curriculum will create new ObGyns who are known for successfully delivering high-value care.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Wieand E, Lagrew DC Jr. Value-based payment: what does it mean, and how can ObGyns get out ahead? OBG Manag. 2018;30(1):17–19, 25–26.
- Agency for Healthcare Research and Quality. The six domains of health care quality. https://www.ahrq.gov/professionals/quality-patient-safety/talkingquality/create/sixdomains.html. Reviewed March 2016. Accessed March 22, 2018.
- Centers for Medicare and Medicaid Services. Better care. Smarter spending. Healthier people: paying providers for value, not volume. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-01-26-3.html. Published January 26, 2015. Accessed March 22, 2018.
- Society for Human Resource Management. Managing health care costs. https://www.shrm.org/resourcesandtools/tools-and-samples/toolkits/pages/managinghealthcarecosts.aspx. Published January 11, 2017. Accessed March 18, 2018.
- American College of Obstetricians and Gynecologists Committee on Gynecologic Practice, Long-Acting Reversible Contraception Working Group. ACOG Committee Opinion No. 642: Increasing access to contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet Gynecol. 2015;126(4):e44–e48.
- American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. ACOG Committee Opinion No. 375: Brand versus generic oral contraceptives. Obstet Gynecol. 2007;110(2 pt 1):447–448.
- American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. ACOG Committee Opinion No. 537: R
eprocessed single-use devices. Obstet Gynecol. 2012;120(4):974–976.
- Wieand E, Lagrew DC Jr. Value-based payment: what does it mean, and how can ObGyns get out ahead? OBG Manag. 2018;30(1):17–19, 25–26.
- Agency for Healthcare Research and Quality. The six domains of health care quality. https://www.ahrq.gov/professionals/quality-patient-safety/talkingquality/create/sixdomains.html. Reviewed March 2016. Accessed March 22, 2018.
- Centers for Medicare and Medicaid Services. Better care. Smarter spending. Healthier people: paying providers for value, not volume. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-01-26-3.html. Published January 26, 2015. Accessed March 22, 2018.
- Society for Human Resource Management. Managing health care costs. https://www.shrm.org/resourcesandtools/tools-and-samples/toolkits/pages/managinghealthcarecosts.aspx. Published January 11, 2017. Accessed March 18, 2018.
- American College of Obstetricians and Gynecologists Committee on Gynecologic Practice, Long-Acting Reversible Contraception Working Group. ACOG Committee Opinion No. 642: Increasing access to contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet Gynecol. 2015;126(4):e44–e48.
- American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. ACOG Committee Opinion No. 375: Brand versus generic oral contraceptives. Obstet Gynecol. 2007;110(2 pt 1):447–448.
- American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. ACOG Committee Opinion No. 537: R
eprocessed single-use devices. Obstet Gynecol. 2012;120(4):974–976.
Read all parts of this series
PART 1 Value-based payment: What does it mean and how can ObGyns get out ahead
PART 2 What makes a “quality” quality measure?
PART 3 The role of patient-reported outcomes in women’s health
PART 4 It costs what?! How we can educate residents and students on how much things cost