User login
Neurogastroenterology and motility fellowships
“So you want to be a gastroenterologist? What do you really want to do?” This is not an uncommon question that a trainee is faced with when progressing through residency and gastroenterology fellowship.
The list of possibilities includes general gastroenterology, advanced endoscopy, transplant hepatology, and neurogastroenterology and motility. From there, each subspecialty can be broken down further into organ system or a specific procedure of interest. Another necessary question is whether to pursue a career in academics or private practice. The first is for the resident who is interested in gaining experience in gastroenterology prior to starting a general gastroenterology fellowship (there are two programs that currently allow for this pathway). The other track is for those who have completed a general gastroenterology fellowship and are looking to enhance their academic careers by pursuing additional training in neurogastroenterology and motility.
There is currently a need for gastroenterologists interested in neurogastroenterology and motility. Among the most common diagnoses in an ambulatory setting, based on International Classification of Disease (ICD) coding, are abdominal pain, gastroesophageal reflux disease, constipation, nausea and vomiting, irritable bowel syndrome, functional dyspepsia, and dysphagia.1,2 While many fellows are exposed to a wide range of motility patients during general gastroenterology fellowship, there is typically not a sufficient amount of training to attain “level 2” proficiency.2,3 In an effort to help standardize training there are recommended thresholds established and advanced training in neurogastroenterology and motility can help fellows to attain that proficiency.2,3 The extra year can also help you prepare to run a motility lab, train nurses, establish lab protocols and quality standards, and manage referrals, which are important skills as a neurogastroenterology and motility specialist.
Types of programs
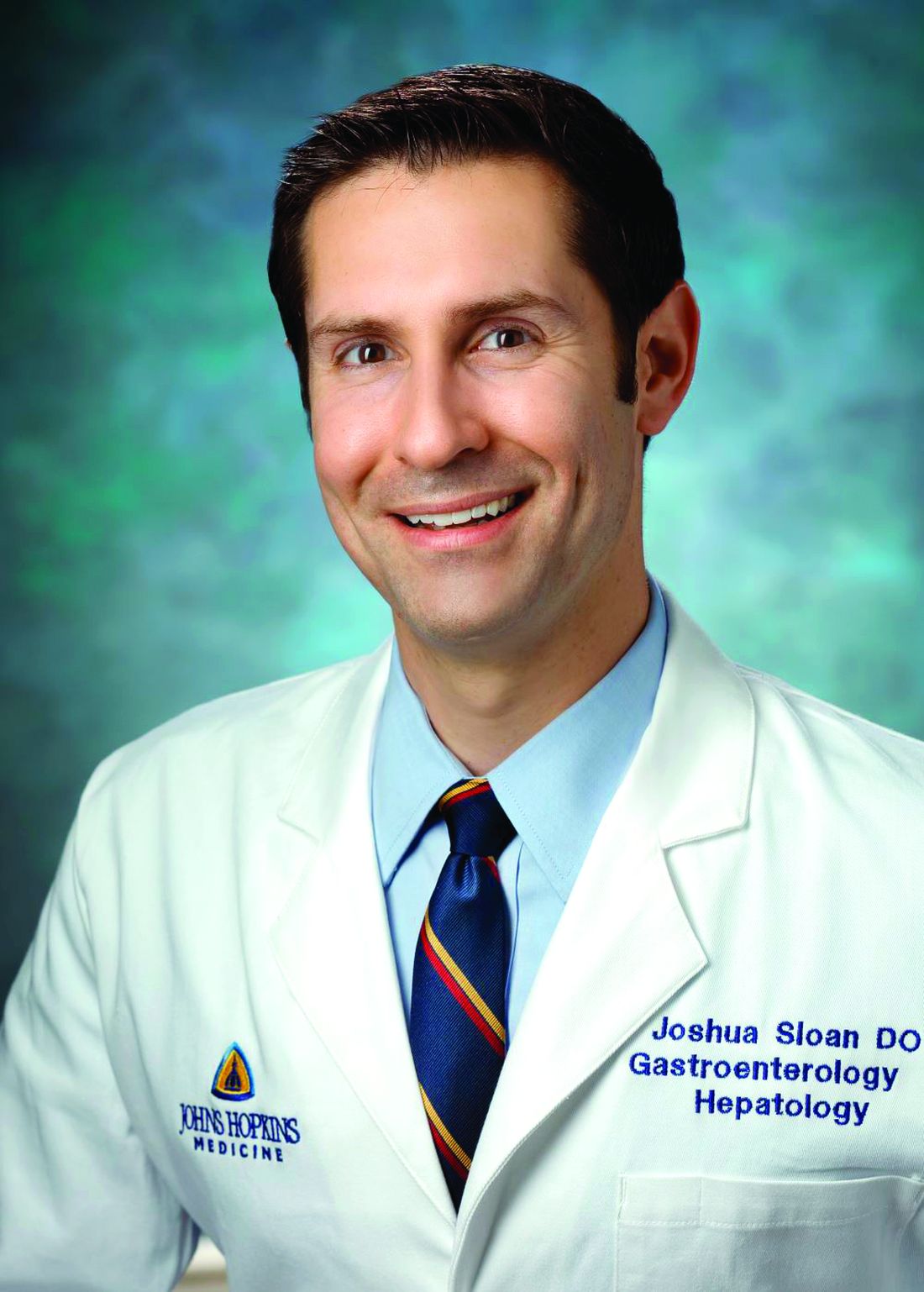
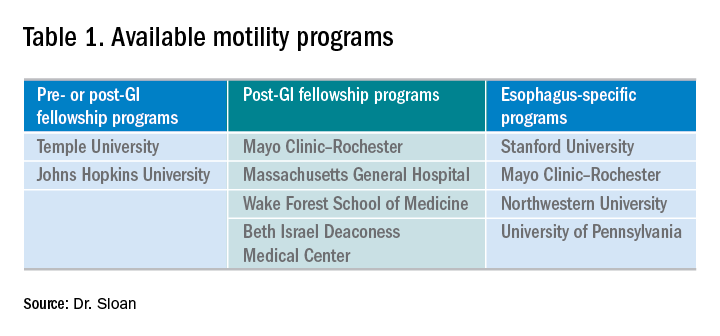
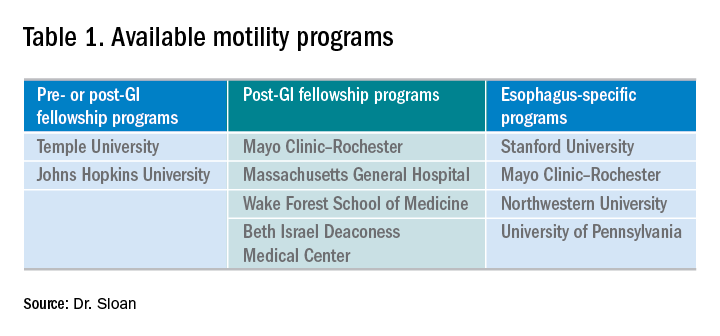
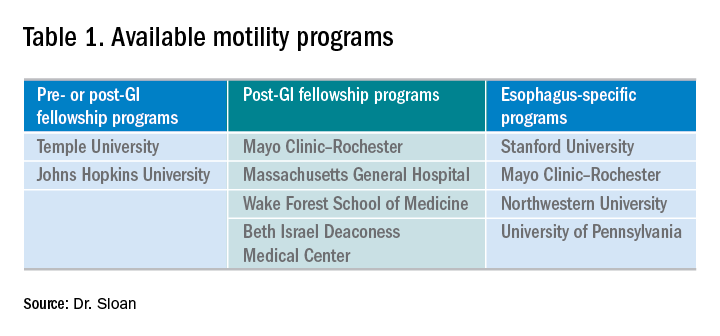
There are several different types of motility programs available. As mentioned previously, some programs afford individuals an opportunity to gain additional experience in gastroenterology before progressing to general gastroenterology fellowship. There are two programs that offer a 1-year fellowship in neurogastroenterology and motility, both prior to or after a general gastroenterology fellowship. Four programs offer 1-year neurogastroenterology and motility fellowships only after a general gastroenterology fellowship. While the neurogastroenterology and motility fellowships cover esophageal motility, there are four programs that specifically focus solely on the esophagus (Table 1).
In addition to pursuing an extra year of training, interested gastroenterology fellows may choose to explore a 1-month Clinical Training Program sponsored by the American Neurogastroenterology and Motility Society (ANMS) at 1 of 10 centers.
Where to find programs
Currently, there is not a singular list of neurogastroenterology and motility programs available for review as you might find with an Accreditation Council for Graduate Medical Education (ACGME) residency or fellowship. At present, the best way to identify the available programs is to search online. Motivation to select a specific program may be related to individual preference and can include geography and department expertise; this ultimately helps to create a focused list. With regard to the ANMS 1-month Clinical Training Program, the list of available programs is available on the society’s website and is for fellows currently in training who wish to incorporate neurogastroenterology and motility into their general GI fellowship.
How to apply
Advanced training in neurogastroenterology and motility is currently a non-ACGME pathway and does not offer a match process for its applicants. After identifying a program of interest, one can find specific instructions on how to apply at the programs’ websites. Typically the process involves reaching out to the program director, writing a letter of interest or personal statement, providing letters of recommendation, and interviewing. Each program has some variability in what is required and attention should be paid to the criteria listed on the specific website.
My experience
I was fortunate to have substantial exposure to esophageal motility in my general gastroenterology fellowship. Gaining this experience was invaluable and laid the foundation for my interest in neurogastroenterology and motility, and, specifically, esophageal dysmotility. My interest in neurogastroenterology and motility then collided with my desire to pursue a career in academics. Knowing the general trajectory for my future career, I began exploring the possibility of undergoing an additional 1-year fellowship early in my second year of GI fellowship. I worked closely with my program director to help define my future goals and to identify available places that would help me attain those goals. While I continued to have an interest in the esophagus, additional training in neurogastroenterology and motility would broaden my understanding and enhance my ability to manage complex patients and perform research at a tertiary care center. I investigated the different neurogastroenterology and motility fellowship programs online and followed the online application instructions. Utilizing national gastroenterology society conferences as networking opportunities, I was able to meet with the program director of my current neurogastroenterology and motility fellowship. In my third year of general gastroenterology fellowship I formally interviewed with the motility group at Johns Hopkins and was later accepted into the neurogastroenterology and motility fellowship program.
Now, nearing the end of my 1-year neurogastroenterology and motility fellowship, I reflect on my extremely positive experience. Throughout the course of the year I have been able to work with multiple GI providers — each with their own area of expertise within the field. There has been a profound exposure to a wide variety of patients with a spectrum of motility conditions covering the entire GI tract. There has been ample opportunity to read motility studies with the guidance and support of the motility faculty to further enhance my skills. The additional year has broadened my exposure to, and the management of, the biopsychosocial aspect of this specific patient population. In line with that, I have had the ability to grow with regard to my use of pharmacology and recognize which symptom might benefit from a particular neuromodulator. An emphasis was also placed on learning the gut-brain axis, and, through multidisciplinary clinics, I worked closely with other disciplines such as psychiatry and GI clinical psychology. Furthermore, the additional year has allowed me to be involved in several research projects within neurogastroenterology and motility that will undoubtedly enhance my future career.
Conclusion
Deciding to pursue an additional year in neurogastroenterology and motility has been one that has helped to give a solid direction to my budding career. It has left me confident in managing this diverse and complex patient population and has helped prepare me for a career in academic gastroenterology. For those who are interested in academic neurogastroenterology and motility, an additional fellowship can help define you as a gastroenterologist and help you to pursue the career of your dreams.
Dr. Sloan is a clinical instructor in the division of gastroenterology at Johns Hopkins in Baltimore.
References
1. Peery A. et al. Burden of gastrointestinal, liver, and pancreatic disease in the United States. Gastroenterology 2015;149:1731-41.e3.
2. Rao S., Parkman H. Advanced training in neurogastroenterology and gastrointestinal motility. Gastroenterology 2015;148:881-5.
3. American Association for the Study of Liver Diseases, American College of Gastroenterology, American Gastroenterological Association (AGA) Institute, and American Society for Gastrointestinal Endoscopy. The gastroenterology core curriculum, third edition. Gastroenterology 2007;132:2012-18.
“So you want to be a gastroenterologist? What do you really want to do?” This is not an uncommon question that a trainee is faced with when progressing through residency and gastroenterology fellowship.
The list of possibilities includes general gastroenterology, advanced endoscopy, transplant hepatology, and neurogastroenterology and motility. From there, each subspecialty can be broken down further into organ system or a specific procedure of interest. Another necessary question is whether to pursue a career in academics or private practice. The first is for the resident who is interested in gaining experience in gastroenterology prior to starting a general gastroenterology fellowship (there are two programs that currently allow for this pathway). The other track is for those who have completed a general gastroenterology fellowship and are looking to enhance their academic careers by pursuing additional training in neurogastroenterology and motility.
There is currently a need for gastroenterologists interested in neurogastroenterology and motility. Among the most common diagnoses in an ambulatory setting, based on International Classification of Disease (ICD) coding, are abdominal pain, gastroesophageal reflux disease, constipation, nausea and vomiting, irritable bowel syndrome, functional dyspepsia, and dysphagia.1,2 While many fellows are exposed to a wide range of motility patients during general gastroenterology fellowship, there is typically not a sufficient amount of training to attain “level 2” proficiency.2,3 In an effort to help standardize training there are recommended thresholds established and advanced training in neurogastroenterology and motility can help fellows to attain that proficiency.2,3 The extra year can also help you prepare to run a motility lab, train nurses, establish lab protocols and quality standards, and manage referrals, which are important skills as a neurogastroenterology and motility specialist.
Types of programs
There are several different types of motility programs available. As mentioned previously, some programs afford individuals an opportunity to gain additional experience in gastroenterology before progressing to general gastroenterology fellowship. There are two programs that offer a 1-year fellowship in neurogastroenterology and motility, both prior to or after a general gastroenterology fellowship. Four programs offer 1-year neurogastroenterology and motility fellowships only after a general gastroenterology fellowship. While the neurogastroenterology and motility fellowships cover esophageal motility, there are four programs that specifically focus solely on the esophagus (Table 1).
In addition to pursuing an extra year of training, interested gastroenterology fellows may choose to explore a 1-month Clinical Training Program sponsored by the American Neurogastroenterology and Motility Society (ANMS) at 1 of 10 centers.
Where to find programs
Currently, there is not a singular list of neurogastroenterology and motility programs available for review as you might find with an Accreditation Council for Graduate Medical Education (ACGME) residency or fellowship. At present, the best way to identify the available programs is to search online. Motivation to select a specific program may be related to individual preference and can include geography and department expertise; this ultimately helps to create a focused list. With regard to the ANMS 1-month Clinical Training Program, the list of available programs is available on the society’s website and is for fellows currently in training who wish to incorporate neurogastroenterology and motility into their general GI fellowship.
How to apply
Advanced training in neurogastroenterology and motility is currently a non-ACGME pathway and does not offer a match process for its applicants. After identifying a program of interest, one can find specific instructions on how to apply at the programs’ websites. Typically the process involves reaching out to the program director, writing a letter of interest or personal statement, providing letters of recommendation, and interviewing. Each program has some variability in what is required and attention should be paid to the criteria listed on the specific website.
My experience
I was fortunate to have substantial exposure to esophageal motility in my general gastroenterology fellowship. Gaining this experience was invaluable and laid the foundation for my interest in neurogastroenterology and motility, and, specifically, esophageal dysmotility. My interest in neurogastroenterology and motility then collided with my desire to pursue a career in academics. Knowing the general trajectory for my future career, I began exploring the possibility of undergoing an additional 1-year fellowship early in my second year of GI fellowship. I worked closely with my program director to help define my future goals and to identify available places that would help me attain those goals. While I continued to have an interest in the esophagus, additional training in neurogastroenterology and motility would broaden my understanding and enhance my ability to manage complex patients and perform research at a tertiary care center. I investigated the different neurogastroenterology and motility fellowship programs online and followed the online application instructions. Utilizing national gastroenterology society conferences as networking opportunities, I was able to meet with the program director of my current neurogastroenterology and motility fellowship. In my third year of general gastroenterology fellowship I formally interviewed with the motility group at Johns Hopkins and was later accepted into the neurogastroenterology and motility fellowship program.
Now, nearing the end of my 1-year neurogastroenterology and motility fellowship, I reflect on my extremely positive experience. Throughout the course of the year I have been able to work with multiple GI providers — each with their own area of expertise within the field. There has been a profound exposure to a wide variety of patients with a spectrum of motility conditions covering the entire GI tract. There has been ample opportunity to read motility studies with the guidance and support of the motility faculty to further enhance my skills. The additional year has broadened my exposure to, and the management of, the biopsychosocial aspect of this specific patient population. In line with that, I have had the ability to grow with regard to my use of pharmacology and recognize which symptom might benefit from a particular neuromodulator. An emphasis was also placed on learning the gut-brain axis, and, through multidisciplinary clinics, I worked closely with other disciplines such as psychiatry and GI clinical psychology. Furthermore, the additional year has allowed me to be involved in several research projects within neurogastroenterology and motility that will undoubtedly enhance my future career.
Conclusion
Deciding to pursue an additional year in neurogastroenterology and motility has been one that has helped to give a solid direction to my budding career. It has left me confident in managing this diverse and complex patient population and has helped prepare me for a career in academic gastroenterology. For those who are interested in academic neurogastroenterology and motility, an additional fellowship can help define you as a gastroenterologist and help you to pursue the career of your dreams.
Dr. Sloan is a clinical instructor in the division of gastroenterology at Johns Hopkins in Baltimore.
References
1. Peery A. et al. Burden of gastrointestinal, liver, and pancreatic disease in the United States. Gastroenterology 2015;149:1731-41.e3.
2. Rao S., Parkman H. Advanced training in neurogastroenterology and gastrointestinal motility. Gastroenterology 2015;148:881-5.
3. American Association for the Study of Liver Diseases, American College of Gastroenterology, American Gastroenterological Association (AGA) Institute, and American Society for Gastrointestinal Endoscopy. The gastroenterology core curriculum, third edition. Gastroenterology 2007;132:2012-18.
“So you want to be a gastroenterologist? What do you really want to do?” This is not an uncommon question that a trainee is faced with when progressing through residency and gastroenterology fellowship.
The list of possibilities includes general gastroenterology, advanced endoscopy, transplant hepatology, and neurogastroenterology and motility. From there, each subspecialty can be broken down further into organ system or a specific procedure of interest. Another necessary question is whether to pursue a career in academics or private practice. The first is for the resident who is interested in gaining experience in gastroenterology prior to starting a general gastroenterology fellowship (there are two programs that currently allow for this pathway). The other track is for those who have completed a general gastroenterology fellowship and are looking to enhance their academic careers by pursuing additional training in neurogastroenterology and motility.
There is currently a need for gastroenterologists interested in neurogastroenterology and motility. Among the most common diagnoses in an ambulatory setting, based on International Classification of Disease (ICD) coding, are abdominal pain, gastroesophageal reflux disease, constipation, nausea and vomiting, irritable bowel syndrome, functional dyspepsia, and dysphagia.1,2 While many fellows are exposed to a wide range of motility patients during general gastroenterology fellowship, there is typically not a sufficient amount of training to attain “level 2” proficiency.2,3 In an effort to help standardize training there are recommended thresholds established and advanced training in neurogastroenterology and motility can help fellows to attain that proficiency.2,3 The extra year can also help you prepare to run a motility lab, train nurses, establish lab protocols and quality standards, and manage referrals, which are important skills as a neurogastroenterology and motility specialist.
Types of programs
There are several different types of motility programs available. As mentioned previously, some programs afford individuals an opportunity to gain additional experience in gastroenterology before progressing to general gastroenterology fellowship. There are two programs that offer a 1-year fellowship in neurogastroenterology and motility, both prior to or after a general gastroenterology fellowship. Four programs offer 1-year neurogastroenterology and motility fellowships only after a general gastroenterology fellowship. While the neurogastroenterology and motility fellowships cover esophageal motility, there are four programs that specifically focus solely on the esophagus (Table 1).
In addition to pursuing an extra year of training, interested gastroenterology fellows may choose to explore a 1-month Clinical Training Program sponsored by the American Neurogastroenterology and Motility Society (ANMS) at 1 of 10 centers.
Where to find programs
Currently, there is not a singular list of neurogastroenterology and motility programs available for review as you might find with an Accreditation Council for Graduate Medical Education (ACGME) residency or fellowship. At present, the best way to identify the available programs is to search online. Motivation to select a specific program may be related to individual preference and can include geography and department expertise; this ultimately helps to create a focused list. With regard to the ANMS 1-month Clinical Training Program, the list of available programs is available on the society’s website and is for fellows currently in training who wish to incorporate neurogastroenterology and motility into their general GI fellowship.
How to apply
Advanced training in neurogastroenterology and motility is currently a non-ACGME pathway and does not offer a match process for its applicants. After identifying a program of interest, one can find specific instructions on how to apply at the programs’ websites. Typically the process involves reaching out to the program director, writing a letter of interest or personal statement, providing letters of recommendation, and interviewing. Each program has some variability in what is required and attention should be paid to the criteria listed on the specific website.
My experience
I was fortunate to have substantial exposure to esophageal motility in my general gastroenterology fellowship. Gaining this experience was invaluable and laid the foundation for my interest in neurogastroenterology and motility, and, specifically, esophageal dysmotility. My interest in neurogastroenterology and motility then collided with my desire to pursue a career in academics. Knowing the general trajectory for my future career, I began exploring the possibility of undergoing an additional 1-year fellowship early in my second year of GI fellowship. I worked closely with my program director to help define my future goals and to identify available places that would help me attain those goals. While I continued to have an interest in the esophagus, additional training in neurogastroenterology and motility would broaden my understanding and enhance my ability to manage complex patients and perform research at a tertiary care center. I investigated the different neurogastroenterology and motility fellowship programs online and followed the online application instructions. Utilizing national gastroenterology society conferences as networking opportunities, I was able to meet with the program director of my current neurogastroenterology and motility fellowship. In my third year of general gastroenterology fellowship I formally interviewed with the motility group at Johns Hopkins and was later accepted into the neurogastroenterology and motility fellowship program.
Now, nearing the end of my 1-year neurogastroenterology and motility fellowship, I reflect on my extremely positive experience. Throughout the course of the year I have been able to work with multiple GI providers — each with their own area of expertise within the field. There has been a profound exposure to a wide variety of patients with a spectrum of motility conditions covering the entire GI tract. There has been ample opportunity to read motility studies with the guidance and support of the motility faculty to further enhance my skills. The additional year has broadened my exposure to, and the management of, the biopsychosocial aspect of this specific patient population. In line with that, I have had the ability to grow with regard to my use of pharmacology and recognize which symptom might benefit from a particular neuromodulator. An emphasis was also placed on learning the gut-brain axis, and, through multidisciplinary clinics, I worked closely with other disciplines such as psychiatry and GI clinical psychology. Furthermore, the additional year has allowed me to be involved in several research projects within neurogastroenterology and motility that will undoubtedly enhance my future career.
Conclusion
Deciding to pursue an additional year in neurogastroenterology and motility has been one that has helped to give a solid direction to my budding career. It has left me confident in managing this diverse and complex patient population and has helped prepare me for a career in academic gastroenterology. For those who are interested in academic neurogastroenterology and motility, an additional fellowship can help define you as a gastroenterologist and help you to pursue the career of your dreams.
Dr. Sloan is a clinical instructor in the division of gastroenterology at Johns Hopkins in Baltimore.
References
1. Peery A. et al. Burden of gastrointestinal, liver, and pancreatic disease in the United States. Gastroenterology 2015;149:1731-41.e3.
2. Rao S., Parkman H. Advanced training in neurogastroenterology and gastrointestinal motility. Gastroenterology 2015;148:881-5.
3. American Association for the Study of Liver Diseases, American College of Gastroenterology, American Gastroenterological Association (AGA) Institute, and American Society for Gastrointestinal Endoscopy. The gastroenterology core curriculum, third edition. Gastroenterology 2007;132:2012-18.
AGA Editorial Fellowship: Three lasting lessons
As a first-year gastroenterology fellow, banding my first patient with a variceal bleed was an exciting – but also stress-provoking – event. What if I banded incorrectly and caused more bleeding? With a successful band, a patient’s hemorrhagic shock is now controlled, hemodynamics improved, and euphoria takes over. Now, in my third year of a gastroenterology fellowship but my first year of the American Gastroenterological Association (AGA) Editorial Fellowship, preparing to present the first manuscript that I handled to the Board of Editors at our weekly meeting has now induced the same excitement and need for the same level of dedication. Have I researched the foundational literature that this current manuscript was built on? What is the trajectory of this research and will this project be interesting to our readers and lead to breakthroughs in the field?
Gastroenterology is the premier flagship journal of the AGA and, in this Editorial Fellowship, I was selected to spend a fully immersive 1-year experience working on all aspects of this journal. In its second year of inception, I echo Dr. Eric Shah’s insight into the transformative and immersive nature of this fellowship.1 In this role, I have made three developments, and each one has left me with a valuable lesson.
Mentorship
My first development was as a direct mentee under the leadership of the two editors in chief Richard Peek, MD, and Douglas Corley, MD, and associate editor John Inadomi, MD. In this role, I reviewed submitted manuscripts regarding outcome data of oncologic studies in the fields of colon, esophageal, and gastric cancer. I served as a reviewer for submitted manuscripts and discussed the impact, novelty, and decision for publication with the Board of Editors. In our weekly meetings, the associate editors discussed manuscripts that needed further review prior to acceptance, revision, or rejection. A few themes underpinned the discussion of these manuscripts:
- Is this science reproducible and is there scientific rigor for study design, validity, and analysis?
- How does this manuscript add to the current state of the literature?
- What is the trajectory of this research field?
- How will this manuscript lead to breakthroughs in this field?
- Are the advancements in this manuscript likely to lead to paradigm shifts in the field in its approach, design, or findings?
I also was fortunate to meet leaders in the field, including working daily in person with multiple members of the Board of Editors at Vanderbilt University Medical Center, Nashville, Tenn., as well as visiting professors, including Dr. Corley, Linda Rabeneck, MD, and T. Jake Liang, MD, who not only spoke on their scientific inquiries but also about their transitional path from gastroenterology fellows to pioneers in their respective fields. From these lessons, I have learned the scientific rigor of manuscript review for Gastroenterology and how to approach modern challenges in our field to directly improve patient care.
AGA’s commitment to early-career investigators
The Editorial Fellowship allowed me to expand a traditional third-year gastroenterology fellowship to dive deep into the intense path to get a manuscript published in Gastroenterology. Whereas 1 year prior, I had found dilating a complete esophageal stricture difficult, I now found myself learning to master clinical trial design, applying modern techniques of artificial intelligence, understanding organoid development, and navigating the impact of the microbiome. I was fortunate to be selected for Vanderbilt’s Master’s in Science in Clinical Investigation, which allowed me to apply my education not only to my own research but also to synergistically understand and deconstruct new submissions ranging from modern statistics with Bayesian modeling to analysis of large genetic data. All of this was built in the supportive framework of my mentoring committee.
As a fellow, I am inspired to see the multicenter, international collaboration to answer important questions in our field. Leveraging large databases and the expertise of multiple investigators, breakthroughs were made because of the collaborative nature of the science. This also was felt in the review process, where experts generously reviewed manuscripts to enhance the quality of the submission in order to advance knowledge in the field. Reading hundreds of these reviews this year has allowed me to refocus my current research studies and improve the way I write my current reviews. In the spirit of reproducible science and challenging the precision of study design, I was impressed by the time, effort, and dedication reviewers from our field spent to help improve the literature. Dr. Peek and Dr. Corley, our editors in chief, committed their time in discussing my innovations and critiques and displayed their level of interest in the opinions of early-career investigators and fostering the next generation of scientists and practitioners. In this lesson, I was invigorated by the depth of AGA opportunities for fellows and junior faculty in education, research, and involvement.
Self-reflection
Having the honor and privilege to review manuscripts upon submission also increased my critical view of my current practices. I now question the level of evidence for which current patient care practices are based, which allows me to better understand the research areas that need increased attention to improve the quality of our guidelines and evidence. For motivated fellows interested in a path of academic medicine, I would strongly advise applying for this prestigious fellowship. In no other training process could I have learned such a breadth of scientific skills and directly apply them to my patient care, my research, and my role as an educator. Furthermore, I was able to contribute to the reviewing and editing process, which allowed me to directly contribute to the field at an early stage of my career. In this final lesson, I exit this impactful Editorial Fellowship in self-reflection. I leave this fellowship humbled – by you – the reader who continues to learn to improve your patient care, the scientist as she works tirelessly to answer questions and contribute to the literature, the gastroenterology community for their willingness to teach and mentor fellows and early-career investigators and practitioners, and the patients who remind us that we all have a shared mission to advance scientific knowledge to improve patient care.
Dr. Naik is a gastroenterology fellow in the department of gastroenterology and hepatology at Vanderbilt University Medical Center in Nashville, Tenn.
Reference
1. Shah ED. Skills acquired during my 1-year AGA Editorial Fellowship. Gastroenterology. 2018;154(6):1563.
As a first-year gastroenterology fellow, banding my first patient with a variceal bleed was an exciting – but also stress-provoking – event. What if I banded incorrectly and caused more bleeding? With a successful band, a patient’s hemorrhagic shock is now controlled, hemodynamics improved, and euphoria takes over. Now, in my third year of a gastroenterology fellowship but my first year of the American Gastroenterological Association (AGA) Editorial Fellowship, preparing to present the first manuscript that I handled to the Board of Editors at our weekly meeting has now induced the same excitement and need for the same level of dedication. Have I researched the foundational literature that this current manuscript was built on? What is the trajectory of this research and will this project be interesting to our readers and lead to breakthroughs in the field?
Gastroenterology is the premier flagship journal of the AGA and, in this Editorial Fellowship, I was selected to spend a fully immersive 1-year experience working on all aspects of this journal. In its second year of inception, I echo Dr. Eric Shah’s insight into the transformative and immersive nature of this fellowship.1 In this role, I have made three developments, and each one has left me with a valuable lesson.
Mentorship
My first development was as a direct mentee under the leadership of the two editors in chief Richard Peek, MD, and Douglas Corley, MD, and associate editor John Inadomi, MD. In this role, I reviewed submitted manuscripts regarding outcome data of oncologic studies in the fields of colon, esophageal, and gastric cancer. I served as a reviewer for submitted manuscripts and discussed the impact, novelty, and decision for publication with the Board of Editors. In our weekly meetings, the associate editors discussed manuscripts that needed further review prior to acceptance, revision, or rejection. A few themes underpinned the discussion of these manuscripts:
- Is this science reproducible and is there scientific rigor for study design, validity, and analysis?
- How does this manuscript add to the current state of the literature?
- What is the trajectory of this research field?
- How will this manuscript lead to breakthroughs in this field?
- Are the advancements in this manuscript likely to lead to paradigm shifts in the field in its approach, design, or findings?
I also was fortunate to meet leaders in the field, including working daily in person with multiple members of the Board of Editors at Vanderbilt University Medical Center, Nashville, Tenn., as well as visiting professors, including Dr. Corley, Linda Rabeneck, MD, and T. Jake Liang, MD, who not only spoke on their scientific inquiries but also about their transitional path from gastroenterology fellows to pioneers in their respective fields. From these lessons, I have learned the scientific rigor of manuscript review for Gastroenterology and how to approach modern challenges in our field to directly improve patient care.
AGA’s commitment to early-career investigators
The Editorial Fellowship allowed me to expand a traditional third-year gastroenterology fellowship to dive deep into the intense path to get a manuscript published in Gastroenterology. Whereas 1 year prior, I had found dilating a complete esophageal stricture difficult, I now found myself learning to master clinical trial design, applying modern techniques of artificial intelligence, understanding organoid development, and navigating the impact of the microbiome. I was fortunate to be selected for Vanderbilt’s Master’s in Science in Clinical Investigation, which allowed me to apply my education not only to my own research but also to synergistically understand and deconstruct new submissions ranging from modern statistics with Bayesian modeling to analysis of large genetic data. All of this was built in the supportive framework of my mentoring committee.
As a fellow, I am inspired to see the multicenter, international collaboration to answer important questions in our field. Leveraging large databases and the expertise of multiple investigators, breakthroughs were made because of the collaborative nature of the science. This also was felt in the review process, where experts generously reviewed manuscripts to enhance the quality of the submission in order to advance knowledge in the field. Reading hundreds of these reviews this year has allowed me to refocus my current research studies and improve the way I write my current reviews. In the spirit of reproducible science and challenging the precision of study design, I was impressed by the time, effort, and dedication reviewers from our field spent to help improve the literature. Dr. Peek and Dr. Corley, our editors in chief, committed their time in discussing my innovations and critiques and displayed their level of interest in the opinions of early-career investigators and fostering the next generation of scientists and practitioners. In this lesson, I was invigorated by the depth of AGA opportunities for fellows and junior faculty in education, research, and involvement.
Self-reflection
Having the honor and privilege to review manuscripts upon submission also increased my critical view of my current practices. I now question the level of evidence for which current patient care practices are based, which allows me to better understand the research areas that need increased attention to improve the quality of our guidelines and evidence. For motivated fellows interested in a path of academic medicine, I would strongly advise applying for this prestigious fellowship. In no other training process could I have learned such a breadth of scientific skills and directly apply them to my patient care, my research, and my role as an educator. Furthermore, I was able to contribute to the reviewing and editing process, which allowed me to directly contribute to the field at an early stage of my career. In this final lesson, I exit this impactful Editorial Fellowship in self-reflection. I leave this fellowship humbled – by you – the reader who continues to learn to improve your patient care, the scientist as she works tirelessly to answer questions and contribute to the literature, the gastroenterology community for their willingness to teach and mentor fellows and early-career investigators and practitioners, and the patients who remind us that we all have a shared mission to advance scientific knowledge to improve patient care.
Dr. Naik is a gastroenterology fellow in the department of gastroenterology and hepatology at Vanderbilt University Medical Center in Nashville, Tenn.
Reference
1. Shah ED. Skills acquired during my 1-year AGA Editorial Fellowship. Gastroenterology. 2018;154(6):1563.
As a first-year gastroenterology fellow, banding my first patient with a variceal bleed was an exciting – but also stress-provoking – event. What if I banded incorrectly and caused more bleeding? With a successful band, a patient’s hemorrhagic shock is now controlled, hemodynamics improved, and euphoria takes over. Now, in my third year of a gastroenterology fellowship but my first year of the American Gastroenterological Association (AGA) Editorial Fellowship, preparing to present the first manuscript that I handled to the Board of Editors at our weekly meeting has now induced the same excitement and need for the same level of dedication. Have I researched the foundational literature that this current manuscript was built on? What is the trajectory of this research and will this project be interesting to our readers and lead to breakthroughs in the field?
Gastroenterology is the premier flagship journal of the AGA and, in this Editorial Fellowship, I was selected to spend a fully immersive 1-year experience working on all aspects of this journal. In its second year of inception, I echo Dr. Eric Shah’s insight into the transformative and immersive nature of this fellowship.1 In this role, I have made three developments, and each one has left me with a valuable lesson.
Mentorship
My first development was as a direct mentee under the leadership of the two editors in chief Richard Peek, MD, and Douglas Corley, MD, and associate editor John Inadomi, MD. In this role, I reviewed submitted manuscripts regarding outcome data of oncologic studies in the fields of colon, esophageal, and gastric cancer. I served as a reviewer for submitted manuscripts and discussed the impact, novelty, and decision for publication with the Board of Editors. In our weekly meetings, the associate editors discussed manuscripts that needed further review prior to acceptance, revision, or rejection. A few themes underpinned the discussion of these manuscripts:
- Is this science reproducible and is there scientific rigor for study design, validity, and analysis?
- How does this manuscript add to the current state of the literature?
- What is the trajectory of this research field?
- How will this manuscript lead to breakthroughs in this field?
- Are the advancements in this manuscript likely to lead to paradigm shifts in the field in its approach, design, or findings?
I also was fortunate to meet leaders in the field, including working daily in person with multiple members of the Board of Editors at Vanderbilt University Medical Center, Nashville, Tenn., as well as visiting professors, including Dr. Corley, Linda Rabeneck, MD, and T. Jake Liang, MD, who not only spoke on their scientific inquiries but also about their transitional path from gastroenterology fellows to pioneers in their respective fields. From these lessons, I have learned the scientific rigor of manuscript review for Gastroenterology and how to approach modern challenges in our field to directly improve patient care.
AGA’s commitment to early-career investigators
The Editorial Fellowship allowed me to expand a traditional third-year gastroenterology fellowship to dive deep into the intense path to get a manuscript published in Gastroenterology. Whereas 1 year prior, I had found dilating a complete esophageal stricture difficult, I now found myself learning to master clinical trial design, applying modern techniques of artificial intelligence, understanding organoid development, and navigating the impact of the microbiome. I was fortunate to be selected for Vanderbilt’s Master’s in Science in Clinical Investigation, which allowed me to apply my education not only to my own research but also to synergistically understand and deconstruct new submissions ranging from modern statistics with Bayesian modeling to analysis of large genetic data. All of this was built in the supportive framework of my mentoring committee.
As a fellow, I am inspired to see the multicenter, international collaboration to answer important questions in our field. Leveraging large databases and the expertise of multiple investigators, breakthroughs were made because of the collaborative nature of the science. This also was felt in the review process, where experts generously reviewed manuscripts to enhance the quality of the submission in order to advance knowledge in the field. Reading hundreds of these reviews this year has allowed me to refocus my current research studies and improve the way I write my current reviews. In the spirit of reproducible science and challenging the precision of study design, I was impressed by the time, effort, and dedication reviewers from our field spent to help improve the literature. Dr. Peek and Dr. Corley, our editors in chief, committed their time in discussing my innovations and critiques and displayed their level of interest in the opinions of early-career investigators and fostering the next generation of scientists and practitioners. In this lesson, I was invigorated by the depth of AGA opportunities for fellows and junior faculty in education, research, and involvement.
Self-reflection
Having the honor and privilege to review manuscripts upon submission also increased my critical view of my current practices. I now question the level of evidence for which current patient care practices are based, which allows me to better understand the research areas that need increased attention to improve the quality of our guidelines and evidence. For motivated fellows interested in a path of academic medicine, I would strongly advise applying for this prestigious fellowship. In no other training process could I have learned such a breadth of scientific skills and directly apply them to my patient care, my research, and my role as an educator. Furthermore, I was able to contribute to the reviewing and editing process, which allowed me to directly contribute to the field at an early stage of my career. In this final lesson, I exit this impactful Editorial Fellowship in self-reflection. I leave this fellowship humbled – by you – the reader who continues to learn to improve your patient care, the scientist as she works tirelessly to answer questions and contribute to the literature, the gastroenterology community for their willingness to teach and mentor fellows and early-career investigators and practitioners, and the patients who remind us that we all have a shared mission to advance scientific knowledge to improve patient care.
Dr. Naik is a gastroenterology fellow in the department of gastroenterology and hepatology at Vanderbilt University Medical Center in Nashville, Tenn.
Reference
1. Shah ED. Skills acquired during my 1-year AGA Editorial Fellowship. Gastroenterology. 2018;154(6):1563.
Estate planning: A must-do for all medical professionals
As medical professionals, you may have encountered patients with serious illnesses and asked yourself the following questions: What if I was in that situation? Where will my assets go when I die? What will happen to my loved ones, and will they be taken care of? Who would handle my affairs if I became ill? These important questions can only be addressed through effective estate planning.
Everyone needs an estate plan regardless of age, health, and financial or family situation. An effective estate plan provides for the orderly management and disposition of your assets upon your death. In addition, as medical professionals may appreciate, an effective estate plan appoints individuals to manage your financial affairs and make health care decisions for you in the event that you become physically or mentally incapacitated.
The most common estate planning tool is a will, which dictates how your assets pass at death. In addition, a will identifies the personal representative of your estate (that is, the person who will see that your assets pass in accordance with your wishes) and, in many states, identifies the guardian of any minor children. Although a court will make the ultimate determination of who is appointed as the guardian, courts typically give significant weight to the person named in a will.
If you die “intestate,” meaning that you died without a valid will, your assets will be distributed in accordance with your state’s intestacy statutes, and any interested person (as opposed to the individual of your choice) may be appointed as the personal representative of your estate. Therefore, to ensure that your property goes to the individuals of your choice and that your final affairs are handled by the person you trust, a will is essential.
In many states, a revocable living trust can be equally beneficial. Like a will, a revocable living trust will dictate how your property passes at death and appoints a trustee to see that the property is distributed in accordance with your wishes. Revocable living trusts can be great tools for incapacity planning and, unlike a will, are not required to be recorded, so the trust agreement can remain private. The assets that are held in a revocable living trust also avoid the often lengthy and expensive probate process, which generally includes the preparation and filing of a petition to open the estate, an inventory identifying the assets of the estate, and an accounting that details all assets received and distributed, followed by the payment of fees based upon the value of the probate estate.
In many situations, leaving assets to young, disabled, or troubled children would result in catastrophic consequences, such as disqualification for government benefits, dissipation of assets for inappropriate uses, or attachment by creditors. Further, for wealthy individuals, outright distributions to spouses could lead to unnecessary estate tax. Wills and revocable trusts can protect against these issues by requiring that, at death, the decedent’s assets are held in further trust for these individuals.
There are various types of trusts that can help ensure that your assets are used for the benefit of your loved one while avoiding any unintended consequences, some of which include the following:
- Special needs trusts, which allow the trustee to use the trust funds for the benefit of the disabled beneficiary without disqualifying the beneficiary from important government benefits.
- Spendthrift trusts, which can protect the trust assets from claims of creditors or property division in a divorce action.
- Marital trusts, which can be used to reduce taxes and ensure that property will be distributed pursuant to your wishes upon the death of your spouse.
- Dynasty trusts, which can be used to protect assets for many generations and, in doing so, reduce the amount of federal and state transfer taxes.
Whether you use a will or revocable living trust, it is critical to coordinate the beneficiary designations of assets such as retirement accounts and life insurance policies, as well as any other account that passes by beneficiary designation. These beneficiary designations trump the provisions of your will and revocable living trust. Likewise, property owned jointly with another person as joint tenants with the right of survivorship, or with a spouse as tenants by the entirety, will pass directly to the joint owner and not pursuant to the terms of your will or revocable trust.
An effective estate plan involves not just planning for death, but also for your incapacity. A durable power of attorney allows you to select an agent or agents to manage your property during your lifetime. The power of attorney can become effective immediately so that the agent can act on your behalf upon execution of the document or the power of attorney can become effective only if and when you become incapacitated.
A durable power of attorney for health care (or advance health care directive) permits you to appoint an agent to make health care decisions on your behalf in the event that you cannot make your own decisions. In addition, should you become permanently unconscious or in a terminal condition, it permits you to appoint an agent who can withhold or withdraw life-sustaining treatment. With a living will, you can express in writing the circumstances under which you do or do not want artificial life-sustaining measures.
With respect to these powers of attorney, the persons that you appoint as your agents should be people that you trust. It is also important to have conversations with your designated agents to ensure that they understand their responsibilities and your wishes. Without these powers of attorney, in the event of your incapacitation, a court will appoint a guardian. The guardian may not be the person you would have appointed, and it will result in annual, and burdensome, court filings.
As busy medical professionals, it may be difficult to find time to develop an estate plan and you may believe that there is plenty of time to do it in the future. It is important to begin thinking about your estate-planning goals and to speak with an attorney to help develop and draft your estate-planning documents. If you already have estate-planning documents, it is important to review those documents periodically to ensure that your estate-planning objectives have remained the same and, if they have changed, to update your documents.
No one knows what the future will hold, so it is important to consult with a local attorney to establish or review your estate plan now. If you do, you will be comforted by the fact that you and your loved ones will be taken care of in accordance with your wishes if you are unable to do so in the future.
Mr. D’Emilio is a managing member and Mr. Riley is an associate at McCollom D’Emilio Smith Uebler, Wilmington, Del.
As medical professionals, you may have encountered patients with serious illnesses and asked yourself the following questions: What if I was in that situation? Where will my assets go when I die? What will happen to my loved ones, and will they be taken care of? Who would handle my affairs if I became ill? These important questions can only be addressed through effective estate planning.
Everyone needs an estate plan regardless of age, health, and financial or family situation. An effective estate plan provides for the orderly management and disposition of your assets upon your death. In addition, as medical professionals may appreciate, an effective estate plan appoints individuals to manage your financial affairs and make health care decisions for you in the event that you become physically or mentally incapacitated.
The most common estate planning tool is a will, which dictates how your assets pass at death. In addition, a will identifies the personal representative of your estate (that is, the person who will see that your assets pass in accordance with your wishes) and, in many states, identifies the guardian of any minor children. Although a court will make the ultimate determination of who is appointed as the guardian, courts typically give significant weight to the person named in a will.
If you die “intestate,” meaning that you died without a valid will, your assets will be distributed in accordance with your state’s intestacy statutes, and any interested person (as opposed to the individual of your choice) may be appointed as the personal representative of your estate. Therefore, to ensure that your property goes to the individuals of your choice and that your final affairs are handled by the person you trust, a will is essential.
In many states, a revocable living trust can be equally beneficial. Like a will, a revocable living trust will dictate how your property passes at death and appoints a trustee to see that the property is distributed in accordance with your wishes. Revocable living trusts can be great tools for incapacity planning and, unlike a will, are not required to be recorded, so the trust agreement can remain private. The assets that are held in a revocable living trust also avoid the often lengthy and expensive probate process, which generally includes the preparation and filing of a petition to open the estate, an inventory identifying the assets of the estate, and an accounting that details all assets received and distributed, followed by the payment of fees based upon the value of the probate estate.
In many situations, leaving assets to young, disabled, or troubled children would result in catastrophic consequences, such as disqualification for government benefits, dissipation of assets for inappropriate uses, or attachment by creditors. Further, for wealthy individuals, outright distributions to spouses could lead to unnecessary estate tax. Wills and revocable trusts can protect against these issues by requiring that, at death, the decedent’s assets are held in further trust for these individuals.
There are various types of trusts that can help ensure that your assets are used for the benefit of your loved one while avoiding any unintended consequences, some of which include the following:
- Special needs trusts, which allow the trustee to use the trust funds for the benefit of the disabled beneficiary without disqualifying the beneficiary from important government benefits.
- Spendthrift trusts, which can protect the trust assets from claims of creditors or property division in a divorce action.
- Marital trusts, which can be used to reduce taxes and ensure that property will be distributed pursuant to your wishes upon the death of your spouse.
- Dynasty trusts, which can be used to protect assets for many generations and, in doing so, reduce the amount of federal and state transfer taxes.
Whether you use a will or revocable living trust, it is critical to coordinate the beneficiary designations of assets such as retirement accounts and life insurance policies, as well as any other account that passes by beneficiary designation. These beneficiary designations trump the provisions of your will and revocable living trust. Likewise, property owned jointly with another person as joint tenants with the right of survivorship, or with a spouse as tenants by the entirety, will pass directly to the joint owner and not pursuant to the terms of your will or revocable trust.
An effective estate plan involves not just planning for death, but also for your incapacity. A durable power of attorney allows you to select an agent or agents to manage your property during your lifetime. The power of attorney can become effective immediately so that the agent can act on your behalf upon execution of the document or the power of attorney can become effective only if and when you become incapacitated.
A durable power of attorney for health care (or advance health care directive) permits you to appoint an agent to make health care decisions on your behalf in the event that you cannot make your own decisions. In addition, should you become permanently unconscious or in a terminal condition, it permits you to appoint an agent who can withhold or withdraw life-sustaining treatment. With a living will, you can express in writing the circumstances under which you do or do not want artificial life-sustaining measures.
With respect to these powers of attorney, the persons that you appoint as your agents should be people that you trust. It is also important to have conversations with your designated agents to ensure that they understand their responsibilities and your wishes. Without these powers of attorney, in the event of your incapacitation, a court will appoint a guardian. The guardian may not be the person you would have appointed, and it will result in annual, and burdensome, court filings.
As busy medical professionals, it may be difficult to find time to develop an estate plan and you may believe that there is plenty of time to do it in the future. It is important to begin thinking about your estate-planning goals and to speak with an attorney to help develop and draft your estate-planning documents. If you already have estate-planning documents, it is important to review those documents periodically to ensure that your estate-planning objectives have remained the same and, if they have changed, to update your documents.
No one knows what the future will hold, so it is important to consult with a local attorney to establish or review your estate plan now. If you do, you will be comforted by the fact that you and your loved ones will be taken care of in accordance with your wishes if you are unable to do so in the future.
Mr. D’Emilio is a managing member and Mr. Riley is an associate at McCollom D’Emilio Smith Uebler, Wilmington, Del.
As medical professionals, you may have encountered patients with serious illnesses and asked yourself the following questions: What if I was in that situation? Where will my assets go when I die? What will happen to my loved ones, and will they be taken care of? Who would handle my affairs if I became ill? These important questions can only be addressed through effective estate planning.
Everyone needs an estate plan regardless of age, health, and financial or family situation. An effective estate plan provides for the orderly management and disposition of your assets upon your death. In addition, as medical professionals may appreciate, an effective estate plan appoints individuals to manage your financial affairs and make health care decisions for you in the event that you become physically or mentally incapacitated.
The most common estate planning tool is a will, which dictates how your assets pass at death. In addition, a will identifies the personal representative of your estate (that is, the person who will see that your assets pass in accordance with your wishes) and, in many states, identifies the guardian of any minor children. Although a court will make the ultimate determination of who is appointed as the guardian, courts typically give significant weight to the person named in a will.
If you die “intestate,” meaning that you died without a valid will, your assets will be distributed in accordance with your state’s intestacy statutes, and any interested person (as opposed to the individual of your choice) may be appointed as the personal representative of your estate. Therefore, to ensure that your property goes to the individuals of your choice and that your final affairs are handled by the person you trust, a will is essential.
In many states, a revocable living trust can be equally beneficial. Like a will, a revocable living trust will dictate how your property passes at death and appoints a trustee to see that the property is distributed in accordance with your wishes. Revocable living trusts can be great tools for incapacity planning and, unlike a will, are not required to be recorded, so the trust agreement can remain private. The assets that are held in a revocable living trust also avoid the often lengthy and expensive probate process, which generally includes the preparation and filing of a petition to open the estate, an inventory identifying the assets of the estate, and an accounting that details all assets received and distributed, followed by the payment of fees based upon the value of the probate estate.
In many situations, leaving assets to young, disabled, or troubled children would result in catastrophic consequences, such as disqualification for government benefits, dissipation of assets for inappropriate uses, or attachment by creditors. Further, for wealthy individuals, outright distributions to spouses could lead to unnecessary estate tax. Wills and revocable trusts can protect against these issues by requiring that, at death, the decedent’s assets are held in further trust for these individuals.
There are various types of trusts that can help ensure that your assets are used for the benefit of your loved one while avoiding any unintended consequences, some of which include the following:
- Special needs trusts, which allow the trustee to use the trust funds for the benefit of the disabled beneficiary without disqualifying the beneficiary from important government benefits.
- Spendthrift trusts, which can protect the trust assets from claims of creditors or property division in a divorce action.
- Marital trusts, which can be used to reduce taxes and ensure that property will be distributed pursuant to your wishes upon the death of your spouse.
- Dynasty trusts, which can be used to protect assets for many generations and, in doing so, reduce the amount of federal and state transfer taxes.
Whether you use a will or revocable living trust, it is critical to coordinate the beneficiary designations of assets such as retirement accounts and life insurance policies, as well as any other account that passes by beneficiary designation. These beneficiary designations trump the provisions of your will and revocable living trust. Likewise, property owned jointly with another person as joint tenants with the right of survivorship, or with a spouse as tenants by the entirety, will pass directly to the joint owner and not pursuant to the terms of your will or revocable trust.
An effective estate plan involves not just planning for death, but also for your incapacity. A durable power of attorney allows you to select an agent or agents to manage your property during your lifetime. The power of attorney can become effective immediately so that the agent can act on your behalf upon execution of the document or the power of attorney can become effective only if and when you become incapacitated.
A durable power of attorney for health care (or advance health care directive) permits you to appoint an agent to make health care decisions on your behalf in the event that you cannot make your own decisions. In addition, should you become permanently unconscious or in a terminal condition, it permits you to appoint an agent who can withhold or withdraw life-sustaining treatment. With a living will, you can express in writing the circumstances under which you do or do not want artificial life-sustaining measures.
With respect to these powers of attorney, the persons that you appoint as your agents should be people that you trust. It is also important to have conversations with your designated agents to ensure that they understand their responsibilities and your wishes. Without these powers of attorney, in the event of your incapacitation, a court will appoint a guardian. The guardian may not be the person you would have appointed, and it will result in annual, and burdensome, court filings.
As busy medical professionals, it may be difficult to find time to develop an estate plan and you may believe that there is plenty of time to do it in the future. It is important to begin thinking about your estate-planning goals and to speak with an attorney to help develop and draft your estate-planning documents. If you already have estate-planning documents, it is important to review those documents periodically to ensure that your estate-planning objectives have remained the same and, if they have changed, to update your documents.
No one knows what the future will hold, so it is important to consult with a local attorney to establish or review your estate plan now. If you do, you will be comforted by the fact that you and your loved ones will be taken care of in accordance with your wishes if you are unable to do so in the future.
Mr. D’Emilio is a managing member and Mr. Riley is an associate at McCollom D’Emilio Smith Uebler, Wilmington, Del.
Building an effective community gastroenterology practice
During my medical training and fellowship, I often heard that my education was not preparing me for the real world. After 3 years of internal medicine training with limited exposure to the outpatient arena and 3-4 years of specialty gastroenterology, hepatology, and advanced procedure training, you’ve probably heard the same thing. Most gastroenterologists who enter private practice have felt this way early on, and our experiences can help you navigate some of the major factors that influence clinical practice to build a thriving career in gastroenterology.
Conduct research on referrals
Once you’ve decided to join a practice, do some research about local dynamics between large hospital systems and private practice. Community clinical practice is unique and varies by region, location, and how the practice is set up. GIs working in rural, low-access areas face different challenges than those working in urban areas near major health care systems. In rural, low-access areas, some physicians have long wait lists for office appointments and procedures.
In urban settings, there may be a larger population of patients but more competition from hospital systems and other practices. In this case, you’ll have to figure out where most of the referrals come from and why – is it the group’s overall reputation or are there physicians in the practice with a highly needed specialty?
Determine if your specialty training can be a differentiator in your market. If you are multilingual and there is a large patient population that speaks the language(s) in which you are fluent, this can be a great way to bring new patients into a practice. This is especially true if there aren’t many (or any) physicians in the practice who are multilingual.
Meet with local physicians in health care systems. Make a connection with hospitalists, referring physicians, ED physicians, advanced practitioners, and surgeons while covering inpatient service. Volunteer for teaching activities – including for nursing staff, who are a great referral source.
Figure out what opportunities exist to have direct interactions with patients, such as health fairs. If possible, it might be smart to invest in marketing directly to patients in your community as well. Leverage opportunities provided by awareness months – such as providing patients with information about cancer screening – to establish a referral basis.
Medical practice is complex and at times can be confusing until you’ve practiced in a given location for some time. Look internally to learn about the community. It’s always a good idea to learn from those who have been practicing in the community for a long time. Don’t hesitate to ask questions and make suggestions, even if they seem naive. Develop relationships with staff members and gain their trust. Establishing a clear understanding of your specialty with your colleagues and staff also can be a good way to find referrals.
Learn the internal process
Schedules during early months are usually filled with urgent patients. Make yourself available for overflow referrals to other established physicians within the practice and for hospital discharge follow-ups. Reading through the charts of these patients can help you understand the various styles of other doctors and can help you familiarize yourself with referring physicians.
This also will help to clarify the process of how a patient moves through the system – from the time patients call the office to when they check out. This includes navigating through procedures, results reporting, and the recall system. While it will be hard to master all aspects of a practice right away, processes within practices are well established, and it is important for you to have a good understanding of how they function.
Focus on patient care and satisfaction
Learning internal processes also can be useful in increasing patient satisfaction, an important quality outcome indicator. As you’re starting out, keep the following things in mind that can help put your patients at ease and increase satisfaction.
- Understand how to communicate what a patient should expect when being seen. Being at ease with the process helps garner trust and confidence.
- Call patients the next day to check on their symptoms.
- Relay results personally. Make connections with family member(s).
- Remember that cultural competency is important. Do everything you can to ensure you’re meeting the social, cultural, and linguistic needs of patients in your community.
- Above all – continue to provide personalized and thorough care. Word of mouth is the best form of referral and is time tested.
Continue to grow
As you begin to understand the dynamics of local practice, it’s important to establish where you fit into the practice and start differentiating your expertise. Here are some ideas and suggestions for how you can continue to expand your patient base.
- Differentiate and establish a subspecialty within your practice: Motility, inflammatory bowel disease, Clostridium difficile/fecal microbiota transplantation, liver diseases, Celiac disease, and medical weight-loss programs are just a few.
- Establish connections with local medical societies as well as hospital and state committees. This is a great way to connect with other physicians of various specialties. If you have a specialty unique to the area, it may help establish a clear referral line.
- Establish a consistent conversation with referring physicians – get to know them and keep direct lines of communication, such as having their cell phone numbers.
- Look for public speaking engagements that reach patients directly. These are organized mostly through patient-based organization and foundations.
- Increase your reach through the local media and through social media platforms like Facebook, Instagram, and Twitter.
At this point, you should have plenty of patients to keep you busy, which could lead to other challenges in managing your various responsibilities and obligations. A key factor at this stage to help reduce stress is to lean on the effective and efficient support system your practice should have in place. Educating medical assistants or nurses on the most common GI diseases and conditions can help reduce the time involved in communicating results. Practice management software and patient portals can help create efficiencies to handle the increasing number of patient visits.
Remember, creating a referral process and patient base as a new gastroenterologist doesn’t have to be daunting. If you follow these tips, you’ll be on your way to establishing yourself within the community. No doubt you will have the same success as many physicians in my group and in the groups of my colleagues in the Digestive Health Physicians Association. And once you’re established, it will be your turn to help the next generation of physicians who want to enter private practice and thrive – so that independent community GI care remains strong well into the future.
Dr. Alaparthi is the director of committee operations at the Gastroenterology Center of Connecticut and serves as chair of the communications committee for the Digestive Health Physicians Association.
During my medical training and fellowship, I often heard that my education was not preparing me for the real world. After 3 years of internal medicine training with limited exposure to the outpatient arena and 3-4 years of specialty gastroenterology, hepatology, and advanced procedure training, you’ve probably heard the same thing. Most gastroenterologists who enter private practice have felt this way early on, and our experiences can help you navigate some of the major factors that influence clinical practice to build a thriving career in gastroenterology.
Conduct research on referrals
Once you’ve decided to join a practice, do some research about local dynamics between large hospital systems and private practice. Community clinical practice is unique and varies by region, location, and how the practice is set up. GIs working in rural, low-access areas face different challenges than those working in urban areas near major health care systems. In rural, low-access areas, some physicians have long wait lists for office appointments and procedures.
In urban settings, there may be a larger population of patients but more competition from hospital systems and other practices. In this case, you’ll have to figure out where most of the referrals come from and why – is it the group’s overall reputation or are there physicians in the practice with a highly needed specialty?
Determine if your specialty training can be a differentiator in your market. If you are multilingual and there is a large patient population that speaks the language(s) in which you are fluent, this can be a great way to bring new patients into a practice. This is especially true if there aren’t many (or any) physicians in the practice who are multilingual.
Meet with local physicians in health care systems. Make a connection with hospitalists, referring physicians, ED physicians, advanced practitioners, and surgeons while covering inpatient service. Volunteer for teaching activities – including for nursing staff, who are a great referral source.
Figure out what opportunities exist to have direct interactions with patients, such as health fairs. If possible, it might be smart to invest in marketing directly to patients in your community as well. Leverage opportunities provided by awareness months – such as providing patients with information about cancer screening – to establish a referral basis.
Medical practice is complex and at times can be confusing until you’ve practiced in a given location for some time. Look internally to learn about the community. It’s always a good idea to learn from those who have been practicing in the community for a long time. Don’t hesitate to ask questions and make suggestions, even if they seem naive. Develop relationships with staff members and gain their trust. Establishing a clear understanding of your specialty with your colleagues and staff also can be a good way to find referrals.
Learn the internal process
Schedules during early months are usually filled with urgent patients. Make yourself available for overflow referrals to other established physicians within the practice and for hospital discharge follow-ups. Reading through the charts of these patients can help you understand the various styles of other doctors and can help you familiarize yourself with referring physicians.
This also will help to clarify the process of how a patient moves through the system – from the time patients call the office to when they check out. This includes navigating through procedures, results reporting, and the recall system. While it will be hard to master all aspects of a practice right away, processes within practices are well established, and it is important for you to have a good understanding of how they function.
Focus on patient care and satisfaction
Learning internal processes also can be useful in increasing patient satisfaction, an important quality outcome indicator. As you’re starting out, keep the following things in mind that can help put your patients at ease and increase satisfaction.
- Understand how to communicate what a patient should expect when being seen. Being at ease with the process helps garner trust and confidence.
- Call patients the next day to check on their symptoms.
- Relay results personally. Make connections with family member(s).
- Remember that cultural competency is important. Do everything you can to ensure you’re meeting the social, cultural, and linguistic needs of patients in your community.
- Above all – continue to provide personalized and thorough care. Word of mouth is the best form of referral and is time tested.
Continue to grow
As you begin to understand the dynamics of local practice, it’s important to establish where you fit into the practice and start differentiating your expertise. Here are some ideas and suggestions for how you can continue to expand your patient base.
- Differentiate and establish a subspecialty within your practice: Motility, inflammatory bowel disease, Clostridium difficile/fecal microbiota transplantation, liver diseases, Celiac disease, and medical weight-loss programs are just a few.
- Establish connections with local medical societies as well as hospital and state committees. This is a great way to connect with other physicians of various specialties. If you have a specialty unique to the area, it may help establish a clear referral line.
- Establish a consistent conversation with referring physicians – get to know them and keep direct lines of communication, such as having their cell phone numbers.
- Look for public speaking engagements that reach patients directly. These are organized mostly through patient-based organization and foundations.
- Increase your reach through the local media and through social media platforms like Facebook, Instagram, and Twitter.
At this point, you should have plenty of patients to keep you busy, which could lead to other challenges in managing your various responsibilities and obligations. A key factor at this stage to help reduce stress is to lean on the effective and efficient support system your practice should have in place. Educating medical assistants or nurses on the most common GI diseases and conditions can help reduce the time involved in communicating results. Practice management software and patient portals can help create efficiencies to handle the increasing number of patient visits.
Remember, creating a referral process and patient base as a new gastroenterologist doesn’t have to be daunting. If you follow these tips, you’ll be on your way to establishing yourself within the community. No doubt you will have the same success as many physicians in my group and in the groups of my colleagues in the Digestive Health Physicians Association. And once you’re established, it will be your turn to help the next generation of physicians who want to enter private practice and thrive – so that independent community GI care remains strong well into the future.
Dr. Alaparthi is the director of committee operations at the Gastroenterology Center of Connecticut and serves as chair of the communications committee for the Digestive Health Physicians Association.
During my medical training and fellowship, I often heard that my education was not preparing me for the real world. After 3 years of internal medicine training with limited exposure to the outpatient arena and 3-4 years of specialty gastroenterology, hepatology, and advanced procedure training, you’ve probably heard the same thing. Most gastroenterologists who enter private practice have felt this way early on, and our experiences can help you navigate some of the major factors that influence clinical practice to build a thriving career in gastroenterology.
Conduct research on referrals
Once you’ve decided to join a practice, do some research about local dynamics between large hospital systems and private practice. Community clinical practice is unique and varies by region, location, and how the practice is set up. GIs working in rural, low-access areas face different challenges than those working in urban areas near major health care systems. In rural, low-access areas, some physicians have long wait lists for office appointments and procedures.
In urban settings, there may be a larger population of patients but more competition from hospital systems and other practices. In this case, you’ll have to figure out where most of the referrals come from and why – is it the group’s overall reputation or are there physicians in the practice with a highly needed specialty?
Determine if your specialty training can be a differentiator in your market. If you are multilingual and there is a large patient population that speaks the language(s) in which you are fluent, this can be a great way to bring new patients into a practice. This is especially true if there aren’t many (or any) physicians in the practice who are multilingual.
Meet with local physicians in health care systems. Make a connection with hospitalists, referring physicians, ED physicians, advanced practitioners, and surgeons while covering inpatient service. Volunteer for teaching activities – including for nursing staff, who are a great referral source.
Figure out what opportunities exist to have direct interactions with patients, such as health fairs. If possible, it might be smart to invest in marketing directly to patients in your community as well. Leverage opportunities provided by awareness months – such as providing patients with information about cancer screening – to establish a referral basis.
Medical practice is complex and at times can be confusing until you’ve practiced in a given location for some time. Look internally to learn about the community. It’s always a good idea to learn from those who have been practicing in the community for a long time. Don’t hesitate to ask questions and make suggestions, even if they seem naive. Develop relationships with staff members and gain their trust. Establishing a clear understanding of your specialty with your colleagues and staff also can be a good way to find referrals.
Learn the internal process
Schedules during early months are usually filled with urgent patients. Make yourself available for overflow referrals to other established physicians within the practice and for hospital discharge follow-ups. Reading through the charts of these patients can help you understand the various styles of other doctors and can help you familiarize yourself with referring physicians.
This also will help to clarify the process of how a patient moves through the system – from the time patients call the office to when they check out. This includes navigating through procedures, results reporting, and the recall system. While it will be hard to master all aspects of a practice right away, processes within practices are well established, and it is important for you to have a good understanding of how they function.
Focus on patient care and satisfaction
Learning internal processes also can be useful in increasing patient satisfaction, an important quality outcome indicator. As you’re starting out, keep the following things in mind that can help put your patients at ease and increase satisfaction.
- Understand how to communicate what a patient should expect when being seen. Being at ease with the process helps garner trust and confidence.
- Call patients the next day to check on their symptoms.
- Relay results personally. Make connections with family member(s).
- Remember that cultural competency is important. Do everything you can to ensure you’re meeting the social, cultural, and linguistic needs of patients in your community.
- Above all – continue to provide personalized and thorough care. Word of mouth is the best form of referral and is time tested.
Continue to grow
As you begin to understand the dynamics of local practice, it’s important to establish where you fit into the practice and start differentiating your expertise. Here are some ideas and suggestions for how you can continue to expand your patient base.
- Differentiate and establish a subspecialty within your practice: Motility, inflammatory bowel disease, Clostridium difficile/fecal microbiota transplantation, liver diseases, Celiac disease, and medical weight-loss programs are just a few.
- Establish connections with local medical societies as well as hospital and state committees. This is a great way to connect with other physicians of various specialties. If you have a specialty unique to the area, it may help establish a clear referral line.
- Establish a consistent conversation with referring physicians – get to know them and keep direct lines of communication, such as having their cell phone numbers.
- Look for public speaking engagements that reach patients directly. These are organized mostly through patient-based organization and foundations.
- Increase your reach through the local media and through social media platforms like Facebook, Instagram, and Twitter.
At this point, you should have plenty of patients to keep you busy, which could lead to other challenges in managing your various responsibilities and obligations. A key factor at this stage to help reduce stress is to lean on the effective and efficient support system your practice should have in place. Educating medical assistants or nurses on the most common GI diseases and conditions can help reduce the time involved in communicating results. Practice management software and patient portals can help create efficiencies to handle the increasing number of patient visits.
Remember, creating a referral process and patient base as a new gastroenterologist doesn’t have to be daunting. If you follow these tips, you’ll be on your way to establishing yourself within the community. No doubt you will have the same success as many physicians in my group and in the groups of my colleagues in the Digestive Health Physicians Association. And once you’re established, it will be your turn to help the next generation of physicians who want to enter private practice and thrive – so that independent community GI care remains strong well into the future.
Dr. Alaparthi is the director of committee operations at the Gastroenterology Center of Connecticut and serves as chair of the communications committee for the Digestive Health Physicians Association.
Mentoring during fellowship to improve career fit, decrease burnout, and optimize career satisfaction among young gastroenterologists
Introduction
Burnout in physicians has received significant attention within the past several years, particularly among trainees and early-career physicians. The subspecialties of gastroenterology and hepatology are not immune to burnout, with multiple studies indicating that early career gastroenterologists may be disproportionately affected, compared with their more-established counterparts.1-4 Although the drivers of depersonalization, emotional exhaustion, and a reduced sense of personal accomplishment among trainees and early-career gastroenterologists are not fully understood, maximizing career fit during the transition from fellowship into the first posttraining position has been promoted as a potential method to decrease burnout in this population.4,5
While most trainees enter gastroenterology fellowships with a set of predefined career goals, mentorship during fellowship can provide critical guidance along with exposure to new areas and career tracks that were not previously considered. In a survey of gastroenterology and transplant hepatology fellows, 94% of participants with a mentor reported that the mentor significantly influenced their career decision.6 Effective mentoring also has been identified as one possible method to decrease burnout among trainees.7,8
Formal mentoring in gastroenterology fellowship programs might decrease burnout through effectively identifying risk factors such as work hour violations or a lack of social support. Additionally, when fellows are being prepared for transition to their first positions as attending gastroenterologists, there is a critical opportunity to improve career fit and decrease burnout rates among early-career gastroenterologists. Making the correct choice of subsequent career path after fellowship might be a source of stress, but this should allow early-career gastroenterologists to maximize the time spent doing those activities they feel are the most rewarding. A formal mentoring system and an accessible career mentor can be invaluable in allowing the mentee to identify and select that position.
Career fit
The concept of career fit has been described as the ability of individuals to focus their effort on the aspect or aspects of their work that they find most meaningful.5 Multiple specialties have recognized the importance of career fit and the need to choose appropriately when selecting a position and career path upon completing fellowship. In one evaluation of faculty members from the department of medicine at a large academic medical center, those individuals who spent less than 20% of their time working on the activity that they found most meaningful were significantly more likely to demonstrate burnout.5
In a relatively short time period, gastroenterology fellows are required to gather multiple new skill sets, including functioning as a consultant, performing endoscopic procedures, and potentially gaining formal training in clinical, basic, or translational research methods. During this same period, an intense phase of self-assessment should begin, with one critical aim of training being to identify those factors most likely to lead to a long, satisfying career. The growth that occurs during fellowship may allow for the identification of a career track that is likely to be the most rewarding, such as a career as a clinical investigator, clinician educator, or in clinical practice. Importantly, the trainee must decide which career track will most likely lead to self-fulfillment, even if the chosen path does not align with a mentor or advisor. Additionally, self-assessment also may aid in the identification of a niche that an individual finds most intellectually stimulating, which may lead to an area of research or clinical expertise.
While the demonstrated relationship between career fit and burnout is only an association without demonstrated causation, this does merit further consideration. For the first time in most trainees’ careers, the position after fellowship represents an opportunity to choose a job as opposed to going through a “match” process. Therefore, the trainee must strongly consider the factors that will ultimately lead to career satisfaction. If a large disconnect is present between self-identified career goals and the actual tasks required within daily workflow, this may lead to burnout relatively early in a career. Perhaps more importantly, if an individual did not perform adequate self-reflection when choosing a career path or did not receive effective guidance from career mentors, this also might lead to decreased career satisfaction, poor career fit, and an increased risk for burnout as an early-career gastroenterologist.
The mentor’s role
Although a structured career mentoring program is in place within many gastroenterology training programs, other fellowships encourage the mentee to select from a pool of potential mentors. In many cases, trainees and early career gastroenterologists will benefit from building a mentorship team, including career mentor or mentors, research mentors, and other advisors.9
While the mentor-mentee relationship can be an extremely rewarding experience for both parties, the effective mentor must meet a high standard. Several qualities have been identified that will maximize the benefit of the mentor-mentee relationship for the trainee, including the mentor taking a selfless approach to the relationship, working to assist the mentee in choosing a career path that will be the most rewarding, and then aiding the mentee in making helpful connections to promote growth along that chosen path.9 A good mentors should inspire a mentees, but also should be willing to provide honest and at times critical feedback to ensure that mentees maximizes their potential and ultimately assume the appropriate career trajectory. Unbiased mentorship, as well as continued reevaluations of strengths, weaknesses, and career goals by the mentor and mentee, will ultimately offer an opportunity to ensure the best combination of career fit,5 work-life balance,10 and satisfaction with career choice.11
The mentor-mentee relationship after training is complete
Once a trainee has completed gastroenterology fellowship, another stressful transition to the role of an attending physician commences. It is critical that early-career gastroenterologists not only have confidence in the guidance that their mentor has provided to ensure appropriate career fit in their new role but also maintain these critical mentor-mentee relationships during this transition. A good mentor does not disappear because one phase of training is complete. The need for effective mentoring at the junior faculty level also is well recognized,12 and early-career gastroenterologists should continue to rely on established mentoring relationships when new decision points are encountered.
Depending on the career track of an early-career gastroenterologist, formal mentoring also may be offered in the new role as a junior faculty member.12 Additionally, external mentoring can exist within foundations or other subspecialty groups. One example of extramural mentoring is the Career Connection Program offered through the Crohn’s & Colitis Foundation’s Rising Educators Academics and Clinicians Helping IBD (REACH-IBD) platform. In this program, early-career gastroenterologists are selected and paired with national opinion leaders for one-on-one mentoring relationships. Such a program offers further opportunities for career growth, establishing connections within a smaller subspecialty of gastroenterology, and maximizing career fit.
Conclusion
In an era where the toll of burnout and other influences on early-career gastroenterologists are increasingly being recognized, the importance of career fit during the transition into the role of an attending should not be underestimated. In conjunction with appropriate self-reflection, unbiased and critical mentorship during fellowship can promote significant growth among trainees and allow for the ultimate selection of a career track or career path that will promote happiness, work-life balance, and long-term success as defined by the mentee.
Edward L. Barnes, MD, MPH, is with the Multidisciplinary Center for Inflammatory Bowel Diseases and the Center for Gastrointestinal Biology and Disease in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. Dr. Barnes reports no relevant disclosures.
References
1. Keswani RN et al. Am J Gastroenterol. 2011;106(10):1734-40.
2. Burke C et al. Am J Gastroenterol. 2017;112:S593-4.
3. DeCross AJ. AGA Perspectives. 2017.
4. Barnes EL et al. Dig Dis Sci. 2019;64(2):302-6.
5. Shanafelt TD et al. Arch Intern Med. 2009;169(10):990-5.
6. Ordway SM et al. Hepatol Commun. 2017;1(4):347-53.
7. Janko MR, Smeds MR. J Vasc Surg. 2019;69(4):1233-42.
8. Eckleberry-Hunt J et al. Acad Med. 2009;84(2):269-77.
9. Lieberman D. Gastroenterology. 2016;151(1):17-9.
10. Shanafelt TD et al. Mayo Clin Proc. 2015;90(12):1600-13.
11. Shanafelt TD et al. Ann Surg. 2009;250(3):463-71.
12. Shaheen NJ, Sandler RS. Gastroenterology. 2018;155(5):1293-7.
Introduction
Burnout in physicians has received significant attention within the past several years, particularly among trainees and early-career physicians. The subspecialties of gastroenterology and hepatology are not immune to burnout, with multiple studies indicating that early career gastroenterologists may be disproportionately affected, compared with their more-established counterparts.1-4 Although the drivers of depersonalization, emotional exhaustion, and a reduced sense of personal accomplishment among trainees and early-career gastroenterologists are not fully understood, maximizing career fit during the transition from fellowship into the first posttraining position has been promoted as a potential method to decrease burnout in this population.4,5
While most trainees enter gastroenterology fellowships with a set of predefined career goals, mentorship during fellowship can provide critical guidance along with exposure to new areas and career tracks that were not previously considered. In a survey of gastroenterology and transplant hepatology fellows, 94% of participants with a mentor reported that the mentor significantly influenced their career decision.6 Effective mentoring also has been identified as one possible method to decrease burnout among trainees.7,8
Formal mentoring in gastroenterology fellowship programs might decrease burnout through effectively identifying risk factors such as work hour violations or a lack of social support. Additionally, when fellows are being prepared for transition to their first positions as attending gastroenterologists, there is a critical opportunity to improve career fit and decrease burnout rates among early-career gastroenterologists. Making the correct choice of subsequent career path after fellowship might be a source of stress, but this should allow early-career gastroenterologists to maximize the time spent doing those activities they feel are the most rewarding. A formal mentoring system and an accessible career mentor can be invaluable in allowing the mentee to identify and select that position.
Career fit
The concept of career fit has been described as the ability of individuals to focus their effort on the aspect or aspects of their work that they find most meaningful.5 Multiple specialties have recognized the importance of career fit and the need to choose appropriately when selecting a position and career path upon completing fellowship. In one evaluation of faculty members from the department of medicine at a large academic medical center, those individuals who spent less than 20% of their time working on the activity that they found most meaningful were significantly more likely to demonstrate burnout.5
In a relatively short time period, gastroenterology fellows are required to gather multiple new skill sets, including functioning as a consultant, performing endoscopic procedures, and potentially gaining formal training in clinical, basic, or translational research methods. During this same period, an intense phase of self-assessment should begin, with one critical aim of training being to identify those factors most likely to lead to a long, satisfying career. The growth that occurs during fellowship may allow for the identification of a career track that is likely to be the most rewarding, such as a career as a clinical investigator, clinician educator, or in clinical practice. Importantly, the trainee must decide which career track will most likely lead to self-fulfillment, even if the chosen path does not align with a mentor or advisor. Additionally, self-assessment also may aid in the identification of a niche that an individual finds most intellectually stimulating, which may lead to an area of research or clinical expertise.
While the demonstrated relationship between career fit and burnout is only an association without demonstrated causation, this does merit further consideration. For the first time in most trainees’ careers, the position after fellowship represents an opportunity to choose a job as opposed to going through a “match” process. Therefore, the trainee must strongly consider the factors that will ultimately lead to career satisfaction. If a large disconnect is present between self-identified career goals and the actual tasks required within daily workflow, this may lead to burnout relatively early in a career. Perhaps more importantly, if an individual did not perform adequate self-reflection when choosing a career path or did not receive effective guidance from career mentors, this also might lead to decreased career satisfaction, poor career fit, and an increased risk for burnout as an early-career gastroenterologist.
The mentor’s role
Although a structured career mentoring program is in place within many gastroenterology training programs, other fellowships encourage the mentee to select from a pool of potential mentors. In many cases, trainees and early career gastroenterologists will benefit from building a mentorship team, including career mentor or mentors, research mentors, and other advisors.9
While the mentor-mentee relationship can be an extremely rewarding experience for both parties, the effective mentor must meet a high standard. Several qualities have been identified that will maximize the benefit of the mentor-mentee relationship for the trainee, including the mentor taking a selfless approach to the relationship, working to assist the mentee in choosing a career path that will be the most rewarding, and then aiding the mentee in making helpful connections to promote growth along that chosen path.9 A good mentors should inspire a mentees, but also should be willing to provide honest and at times critical feedback to ensure that mentees maximizes their potential and ultimately assume the appropriate career trajectory. Unbiased mentorship, as well as continued reevaluations of strengths, weaknesses, and career goals by the mentor and mentee, will ultimately offer an opportunity to ensure the best combination of career fit,5 work-life balance,10 and satisfaction with career choice.11
The mentor-mentee relationship after training is complete
Once a trainee has completed gastroenterology fellowship, another stressful transition to the role of an attending physician commences. It is critical that early-career gastroenterologists not only have confidence in the guidance that their mentor has provided to ensure appropriate career fit in their new role but also maintain these critical mentor-mentee relationships during this transition. A good mentor does not disappear because one phase of training is complete. The need for effective mentoring at the junior faculty level also is well recognized,12 and early-career gastroenterologists should continue to rely on established mentoring relationships when new decision points are encountered.
Depending on the career track of an early-career gastroenterologist, formal mentoring also may be offered in the new role as a junior faculty member.12 Additionally, external mentoring can exist within foundations or other subspecialty groups. One example of extramural mentoring is the Career Connection Program offered through the Crohn’s & Colitis Foundation’s Rising Educators Academics and Clinicians Helping IBD (REACH-IBD) platform. In this program, early-career gastroenterologists are selected and paired with national opinion leaders for one-on-one mentoring relationships. Such a program offers further opportunities for career growth, establishing connections within a smaller subspecialty of gastroenterology, and maximizing career fit.
Conclusion
In an era where the toll of burnout and other influences on early-career gastroenterologists are increasingly being recognized, the importance of career fit during the transition into the role of an attending should not be underestimated. In conjunction with appropriate self-reflection, unbiased and critical mentorship during fellowship can promote significant growth among trainees and allow for the ultimate selection of a career track or career path that will promote happiness, work-life balance, and long-term success as defined by the mentee.
Edward L. Barnes, MD, MPH, is with the Multidisciplinary Center for Inflammatory Bowel Diseases and the Center for Gastrointestinal Biology and Disease in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. Dr. Barnes reports no relevant disclosures.
References
1. Keswani RN et al. Am J Gastroenterol. 2011;106(10):1734-40.
2. Burke C et al. Am J Gastroenterol. 2017;112:S593-4.
3. DeCross AJ. AGA Perspectives. 2017.
4. Barnes EL et al. Dig Dis Sci. 2019;64(2):302-6.
5. Shanafelt TD et al. Arch Intern Med. 2009;169(10):990-5.
6. Ordway SM et al. Hepatol Commun. 2017;1(4):347-53.
7. Janko MR, Smeds MR. J Vasc Surg. 2019;69(4):1233-42.
8. Eckleberry-Hunt J et al. Acad Med. 2009;84(2):269-77.
9. Lieberman D. Gastroenterology. 2016;151(1):17-9.
10. Shanafelt TD et al. Mayo Clin Proc. 2015;90(12):1600-13.
11. Shanafelt TD et al. Ann Surg. 2009;250(3):463-71.
12. Shaheen NJ, Sandler RS. Gastroenterology. 2018;155(5):1293-7.
Introduction
Burnout in physicians has received significant attention within the past several years, particularly among trainees and early-career physicians. The subspecialties of gastroenterology and hepatology are not immune to burnout, with multiple studies indicating that early career gastroenterologists may be disproportionately affected, compared with their more-established counterparts.1-4 Although the drivers of depersonalization, emotional exhaustion, and a reduced sense of personal accomplishment among trainees and early-career gastroenterologists are not fully understood, maximizing career fit during the transition from fellowship into the first posttraining position has been promoted as a potential method to decrease burnout in this population.4,5
While most trainees enter gastroenterology fellowships with a set of predefined career goals, mentorship during fellowship can provide critical guidance along with exposure to new areas and career tracks that were not previously considered. In a survey of gastroenterology and transplant hepatology fellows, 94% of participants with a mentor reported that the mentor significantly influenced their career decision.6 Effective mentoring also has been identified as one possible method to decrease burnout among trainees.7,8
Formal mentoring in gastroenterology fellowship programs might decrease burnout through effectively identifying risk factors such as work hour violations or a lack of social support. Additionally, when fellows are being prepared for transition to their first positions as attending gastroenterologists, there is a critical opportunity to improve career fit and decrease burnout rates among early-career gastroenterologists. Making the correct choice of subsequent career path after fellowship might be a source of stress, but this should allow early-career gastroenterologists to maximize the time spent doing those activities they feel are the most rewarding. A formal mentoring system and an accessible career mentor can be invaluable in allowing the mentee to identify and select that position.
Career fit
The concept of career fit has been described as the ability of individuals to focus their effort on the aspect or aspects of their work that they find most meaningful.5 Multiple specialties have recognized the importance of career fit and the need to choose appropriately when selecting a position and career path upon completing fellowship. In one evaluation of faculty members from the department of medicine at a large academic medical center, those individuals who spent less than 20% of their time working on the activity that they found most meaningful were significantly more likely to demonstrate burnout.5
In a relatively short time period, gastroenterology fellows are required to gather multiple new skill sets, including functioning as a consultant, performing endoscopic procedures, and potentially gaining formal training in clinical, basic, or translational research methods. During this same period, an intense phase of self-assessment should begin, with one critical aim of training being to identify those factors most likely to lead to a long, satisfying career. The growth that occurs during fellowship may allow for the identification of a career track that is likely to be the most rewarding, such as a career as a clinical investigator, clinician educator, or in clinical practice. Importantly, the trainee must decide which career track will most likely lead to self-fulfillment, even if the chosen path does not align with a mentor or advisor. Additionally, self-assessment also may aid in the identification of a niche that an individual finds most intellectually stimulating, which may lead to an area of research or clinical expertise.
While the demonstrated relationship between career fit and burnout is only an association without demonstrated causation, this does merit further consideration. For the first time in most trainees’ careers, the position after fellowship represents an opportunity to choose a job as opposed to going through a “match” process. Therefore, the trainee must strongly consider the factors that will ultimately lead to career satisfaction. If a large disconnect is present between self-identified career goals and the actual tasks required within daily workflow, this may lead to burnout relatively early in a career. Perhaps more importantly, if an individual did not perform adequate self-reflection when choosing a career path or did not receive effective guidance from career mentors, this also might lead to decreased career satisfaction, poor career fit, and an increased risk for burnout as an early-career gastroenterologist.
The mentor’s role
Although a structured career mentoring program is in place within many gastroenterology training programs, other fellowships encourage the mentee to select from a pool of potential mentors. In many cases, trainees and early career gastroenterologists will benefit from building a mentorship team, including career mentor or mentors, research mentors, and other advisors.9
While the mentor-mentee relationship can be an extremely rewarding experience for both parties, the effective mentor must meet a high standard. Several qualities have been identified that will maximize the benefit of the mentor-mentee relationship for the trainee, including the mentor taking a selfless approach to the relationship, working to assist the mentee in choosing a career path that will be the most rewarding, and then aiding the mentee in making helpful connections to promote growth along that chosen path.9 A good mentors should inspire a mentees, but also should be willing to provide honest and at times critical feedback to ensure that mentees maximizes their potential and ultimately assume the appropriate career trajectory. Unbiased mentorship, as well as continued reevaluations of strengths, weaknesses, and career goals by the mentor and mentee, will ultimately offer an opportunity to ensure the best combination of career fit,5 work-life balance,10 and satisfaction with career choice.11
The mentor-mentee relationship after training is complete
Once a trainee has completed gastroenterology fellowship, another stressful transition to the role of an attending physician commences. It is critical that early-career gastroenterologists not only have confidence in the guidance that their mentor has provided to ensure appropriate career fit in their new role but also maintain these critical mentor-mentee relationships during this transition. A good mentor does not disappear because one phase of training is complete. The need for effective mentoring at the junior faculty level also is well recognized,12 and early-career gastroenterologists should continue to rely on established mentoring relationships when new decision points are encountered.
Depending on the career track of an early-career gastroenterologist, formal mentoring also may be offered in the new role as a junior faculty member.12 Additionally, external mentoring can exist within foundations or other subspecialty groups. One example of extramural mentoring is the Career Connection Program offered through the Crohn’s & Colitis Foundation’s Rising Educators Academics and Clinicians Helping IBD (REACH-IBD) platform. In this program, early-career gastroenterologists are selected and paired with national opinion leaders for one-on-one mentoring relationships. Such a program offers further opportunities for career growth, establishing connections within a smaller subspecialty of gastroenterology, and maximizing career fit.
Conclusion
In an era where the toll of burnout and other influences on early-career gastroenterologists are increasingly being recognized, the importance of career fit during the transition into the role of an attending should not be underestimated. In conjunction with appropriate self-reflection, unbiased and critical mentorship during fellowship can promote significant growth among trainees and allow for the ultimate selection of a career track or career path that will promote happiness, work-life balance, and long-term success as defined by the mentee.
Edward L. Barnes, MD, MPH, is with the Multidisciplinary Center for Inflammatory Bowel Diseases and the Center for Gastrointestinal Biology and Disease in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. Dr. Barnes reports no relevant disclosures.
References
1. Keswani RN et al. Am J Gastroenterol. 2011;106(10):1734-40.
2. Burke C et al. Am J Gastroenterol. 2017;112:S593-4.
3. DeCross AJ. AGA Perspectives. 2017.
4. Barnes EL et al. Dig Dis Sci. 2019;64(2):302-6.
5. Shanafelt TD et al. Arch Intern Med. 2009;169(10):990-5.
6. Ordway SM et al. Hepatol Commun. 2017;1(4):347-53.
7. Janko MR, Smeds MR. J Vasc Surg. 2019;69(4):1233-42.
8. Eckleberry-Hunt J et al. Acad Med. 2009;84(2):269-77.
9. Lieberman D. Gastroenterology. 2016;151(1):17-9.
10. Shanafelt TD et al. Mayo Clin Proc. 2015;90(12):1600-13.
11. Shanafelt TD et al. Ann Surg. 2009;250(3):463-71.
12. Shaheen NJ, Sandler RS. Gastroenterology. 2018;155(5):1293-7.
AGA News
AGA journals select new editorial fellows
Congrats to the six GIs selected for this competitive program.
The AGA journals – Gastroenterology, Clinical Gastroenterology and Hepatology (CGH), and Cellular and Molecular Gastroenterology and Hepatology (CMGH) – are pleased to announce their 2019-2020 editorial fellows.
Gastroenterology
Feng Su, MD
University of Washington, Seattle
Victoria Weis, PhD
Wake Forest University, Winston-Salem, N.C.
CGH
Austin Chiang, MD, MPH
Jefferson Medical College, Philadelphia, Penn.
Jennifer Kolb, MD
University of Colorado at Denver, Aurora
CMGH
Cambrian Liu, PhD
The Saban Research Institute, Children’s Hospital Los Angeles, Calif.
Tirthadipa Pradhan-Sundd, PhD
University of Pittsburgh, Penn.
The editorial fellows will be mentored on their respective journals’ editorial processes, including peer review and the publication process from manuscript submission to acceptance. They will participate in discussions and conferences with the boards of editors and work closely with the AGA editorial staff. Additionally, the fellows will participate in AGA’s new reviewer education program and will also be offered the opportunity to contribute content to their respective journals. The newly expanded program builds on the success of the previous 2 years when Gastroenterology had an editorial fellow.
The journals’ board of editors and editorial staff congratulate the fellows and are excited to work with them over the next year.
Get to know this rock star IBS researcher and mom
AGA Research Foundation pilot awards are an invaluable tool for investigators – they provide seed funding to explore promising new lines of research and generate preliminary data for larger grants. So, when Meenakshi Rao, MD, PhD, received the 2016 AGA–Takeda Pharmaceuticals International Research Scholar Award in Neurogastroenterology, she was able to double down on a project to identify why men and women with irritable bowel syndrome (IBS), the most common but least understood of all digestive disorders, report different symptoms and respond differently to treatment. Based on her recent accomplishments, we’re excited for you to get to know Dr. Rao, assistant professor of pediatrics at Harvard Medical School, Boston, and our AGA Research Foundation researcher of the month.
The Rao lab AGA-funded project focused on building upon Dr. Rao’s previous findings, which showed that disrupting nerves in the bowel had vastly different effects on males and females. These surprising results led Dr. Rao to explore whether sex hormones, such as testosterone and estrogen, might regulate how well things move through the bowel. Dr. Rao believes that identifying the underlying causes for sex differences in bowel function could lead to more effective and personalized treatments for patients with IBS. You can read the specifics of Dr. Rao’s research in the October 2017 issue of Gastroenterology and the October 2018 issue of Journal of Neuroscience.
IBS symptoms in women more typically involve constipation while young men with IBS more commonly report diarrhea. Over time, as men age, however, they tend to experience more constipation, Dr. Rao said. “Sex hormones might be signaling directly to the nerves in our gut and playing a role in these sex differences,” Dr. Rao said. “It might mean we can’t think of this as one disorder. IBS in a male may be different than IBS in a female, and that could change how we approach diagnosis and treatment.”
The AGA grant laid the groundwork for Dr. Rao’s findings, which led to a new understanding of how different types of cells in the gut nervous system regulate bowel functions – and how this regulation is different in males and females. The AGA grant helped Dr. Rao secure funding from the National Institutes of Health to launch new projects focused on how disruption of the gut nervous system causes disease.
Dr. Rao received the AGA award in 2015, when her son, Avinash, was aged 2 years. She acknowledged the delicate balancing act of raising a family and advancing her research.
“A lot of things were happening at once,” she said. “As a young parent, having the support of this award and having a technician (made possible by the award) made a big difference.”
Her son, now 5 years old, is growing up in a science-centric household because Dr. Rao’s husband is also a scientist. Not surprisingly, Dr. Rao says, her son is becoming a budding scientist.
“He talks about experiments all the time,” she says. “He even articulated to me the other day why we work on mice to learn how to help people. I never taught him that. I was floored.”
Five new GI technologies to know
The AGA Tech Summit Shark Tank is our annual reminder that the field of GI is ripe for innovation. Continue reading for an overview of the five new technologies pitched to our panel of sharks.
The smart toilet seat. A toilet seat developed by Toi Labs, called TrueLoo, is equipped with lighting and cameras that capture images of bowel movements and urination for subsequent analysis. The company describes TrueLoo as a low-cost disease-screening tool that has major potential for early detection of conditions ranging from dehydration to gastrointestinal cancer.
AI to aid screening endoscopy. A new tool called Ultivision, being developed by the startup Docbot, was described as a strategy to employ artificial intelligence (AI) to aid endoscopists in screening for dysplasia in either screening colonoscopy or in surveillance of Barrett’s esophagus. The tool integrates with existing endoscopic tools. As tissue is visualized, the AI is programmed to highlight suspected dysplasia with a colored box to alert the endoscopist.
Obesity phenotyping tool. The Pheno Test, developed by Phenomix Sciences, applies “multi-omics” to a blood-based test to separate patients with obesity into four phenotypes: hungry brain (satiation signal is impaired), hungry gut (signals to eat are upregulated), emotional hunger (psychological reasons drive eating behavior), and slow metabolism (failure to burn fat at normal rates). With this knowledge, treatment can be tailored appropriately leading to better outcomes.
Capsule diagnostic tool. The Atmo Gas Capsule from Atmo Biosciences is an ingestible capsule that measures gases at the source, which can accelerate the diagnosis of diseases such as IBS and inflammatory bowel disease (IBD). According to the company, this technique is highly accurate and offers an alternative to more invasive and expensive diagnostic tools.
Winner: “all-in-one” IBD app. Our Shark Tank winner by both popular vote from AGA Tech Summit attendees and the six-member Shark Tank panel was Oshi Health, selected for its IBD app. The app allows patients to track symptoms, a first step in understanding personalized flare pattern, as well as find resources to learn about their disease and communicate with other patients about their experiences. In a future iteration, information gathered by the app will be made available to physicians to provide current information about disease status to better individualize therapy.
2020 Crohn’s & Colitis Congress now open for registration
Join the Crohn’s & Colitis Foundation and AGA next January in Austin, Tex., for the premier conference on IBD.
The Crohn’s & Colitis Congress combines the strengths of the nation’s leading IBD patient organization, the Crohn’s & Colitis Foundation, and the premier GI professional organization, AGA, to bring together IBD professionals, across all disciplines, to transform IBD care.
The 2020 Congress Committee Chair David T. Rubin, MD, AGAF, University of Chicago, and Cochair Uma Mahadevan, MD, AGAF, University of California, San Francisco, lead a faculty that includes thought leaders in the fields of GI, research investigation, surgery, pediatrics, advanced practice, IBD nursing, diet and nutrition, mental health, radiology, and pathology.
The congress’s agenda includes main sessions that will emphasize case studies and panel discussions. There will also be parallel sessions on basic and translational science for senior and junior investigators. In addition, opening breakout sessions, taking place Jan. 23, will be available for selection free of charge.
Attendees of the 2020 congress will be able to meet with IBD leaders, discover different perspectives, leave with practical information they can immediately implement to take care of their next IBD patient and hear what’s on the horizon in potential treatment.
There will also be plenty of social events and plenty of time to build a strong network, including a Friday night Welcome Reception that should not be missed.
In addition, the 2020 congress is taking place in Austin, Tex. The capital of Texas and the Live Music Capital of the World, Austin is famous for its inspiring and enticing entertainment, culture, cuisine, and outdoor settings. Make a week of it and enjoy all Austin has to offer.
Early-bird registration ends Sept. 18. General abstract submissions for basic, translational, and clinical research begin Aug. 28 and end Oct. 23. To learn more and register, visit www.crohnscolitiscongress.org.
AGA welcomes new president, Hashem B. El-Serag, MD, MPH, AGAF
Hashem B. El-Serag, MD, MPH, AGAF, began his term as the 114th president of the AGA Institute at Digestive Disease Week® (DDW 2019).
Dr. El-Serag is former editor in chief of Clinical Gastroenterology and Hepatology. He currently serves as chair of the department of medicine at Baylor College of Medicine, Houston, following a decade leading and expanding Baylor’s gastroenterology and hepatology section. He is one of the few academic gastroenterologists serving as a chair of a department of medicine in the United States.
Originally Palestinian, Dr. El-Serag became a U.S. citizen in the early 2000s after medical school in Libya. He completed his training at community hospitals in the United States. His path from Benghazi to Baylor is described in the May issue of Gastroenterology by Baylor colleague Dr. Fasiha Kanwal.
“I firmly believe that the success I achieved in the United States would not have been possible anywhere else in the world, and it is as much a testament to the accepting society and medical system as to whatever intrinsic ability or skill I have,” noted Dr. El-Serag.
The major focus of Dr. El-Serag’s scholarly work is the epidemiology and clinical outcomes of hepatocellular carcinoma. Much of the modern literature on this topic includes his more than 100 publications. Since 2014, Dr. El-Serag has been named by Thomson Reuter as among the top 1% of clinical scientists.
Dr. El-Serag “is an innovative scientist, a compassionate physician, and a gifted educator. He is a relentless advocate of science and training, with an astute political sense — all key to influencing and shaping policy,” said Dr. Kanwal.
Dr. El-Serag’s term as AGA president concludes May 2020. Follow him on twitter at @SeragHashem.
AGA journals select new editorial fellows
Congrats to the six GIs selected for this competitive program.
The AGA journals – Gastroenterology, Clinical Gastroenterology and Hepatology (CGH), and Cellular and Molecular Gastroenterology and Hepatology (CMGH) – are pleased to announce their 2019-2020 editorial fellows.
Gastroenterology
Feng Su, MD
University of Washington, Seattle
Victoria Weis, PhD
Wake Forest University, Winston-Salem, N.C.
CGH
Austin Chiang, MD, MPH
Jefferson Medical College, Philadelphia, Penn.
Jennifer Kolb, MD
University of Colorado at Denver, Aurora
CMGH
Cambrian Liu, PhD
The Saban Research Institute, Children’s Hospital Los Angeles, Calif.
Tirthadipa Pradhan-Sundd, PhD
University of Pittsburgh, Penn.
The editorial fellows will be mentored on their respective journals’ editorial processes, including peer review and the publication process from manuscript submission to acceptance. They will participate in discussions and conferences with the boards of editors and work closely with the AGA editorial staff. Additionally, the fellows will participate in AGA’s new reviewer education program and will also be offered the opportunity to contribute content to their respective journals. The newly expanded program builds on the success of the previous 2 years when Gastroenterology had an editorial fellow.
The journals’ board of editors and editorial staff congratulate the fellows and are excited to work with them over the next year.
Get to know this rock star IBS researcher and mom
AGA Research Foundation pilot awards are an invaluable tool for investigators – they provide seed funding to explore promising new lines of research and generate preliminary data for larger grants. So, when Meenakshi Rao, MD, PhD, received the 2016 AGA–Takeda Pharmaceuticals International Research Scholar Award in Neurogastroenterology, she was able to double down on a project to identify why men and women with irritable bowel syndrome (IBS), the most common but least understood of all digestive disorders, report different symptoms and respond differently to treatment. Based on her recent accomplishments, we’re excited for you to get to know Dr. Rao, assistant professor of pediatrics at Harvard Medical School, Boston, and our AGA Research Foundation researcher of the month.
The Rao lab AGA-funded project focused on building upon Dr. Rao’s previous findings, which showed that disrupting nerves in the bowel had vastly different effects on males and females. These surprising results led Dr. Rao to explore whether sex hormones, such as testosterone and estrogen, might regulate how well things move through the bowel. Dr. Rao believes that identifying the underlying causes for sex differences in bowel function could lead to more effective and personalized treatments for patients with IBS. You can read the specifics of Dr. Rao’s research in the October 2017 issue of Gastroenterology and the October 2018 issue of Journal of Neuroscience.
IBS symptoms in women more typically involve constipation while young men with IBS more commonly report diarrhea. Over time, as men age, however, they tend to experience more constipation, Dr. Rao said. “Sex hormones might be signaling directly to the nerves in our gut and playing a role in these sex differences,” Dr. Rao said. “It might mean we can’t think of this as one disorder. IBS in a male may be different than IBS in a female, and that could change how we approach diagnosis and treatment.”
The AGA grant laid the groundwork for Dr. Rao’s findings, which led to a new understanding of how different types of cells in the gut nervous system regulate bowel functions – and how this regulation is different in males and females. The AGA grant helped Dr. Rao secure funding from the National Institutes of Health to launch new projects focused on how disruption of the gut nervous system causes disease.
Dr. Rao received the AGA award in 2015, when her son, Avinash, was aged 2 years. She acknowledged the delicate balancing act of raising a family and advancing her research.
“A lot of things were happening at once,” she said. “As a young parent, having the support of this award and having a technician (made possible by the award) made a big difference.”
Her son, now 5 years old, is growing up in a science-centric household because Dr. Rao’s husband is also a scientist. Not surprisingly, Dr. Rao says, her son is becoming a budding scientist.
“He talks about experiments all the time,” she says. “He even articulated to me the other day why we work on mice to learn how to help people. I never taught him that. I was floored.”
Five new GI technologies to know
The AGA Tech Summit Shark Tank is our annual reminder that the field of GI is ripe for innovation. Continue reading for an overview of the five new technologies pitched to our panel of sharks.
The smart toilet seat. A toilet seat developed by Toi Labs, called TrueLoo, is equipped with lighting and cameras that capture images of bowel movements and urination for subsequent analysis. The company describes TrueLoo as a low-cost disease-screening tool that has major potential for early detection of conditions ranging from dehydration to gastrointestinal cancer.
AI to aid screening endoscopy. A new tool called Ultivision, being developed by the startup Docbot, was described as a strategy to employ artificial intelligence (AI) to aid endoscopists in screening for dysplasia in either screening colonoscopy or in surveillance of Barrett’s esophagus. The tool integrates with existing endoscopic tools. As tissue is visualized, the AI is programmed to highlight suspected dysplasia with a colored box to alert the endoscopist.
Obesity phenotyping tool. The Pheno Test, developed by Phenomix Sciences, applies “multi-omics” to a blood-based test to separate patients with obesity into four phenotypes: hungry brain (satiation signal is impaired), hungry gut (signals to eat are upregulated), emotional hunger (psychological reasons drive eating behavior), and slow metabolism (failure to burn fat at normal rates). With this knowledge, treatment can be tailored appropriately leading to better outcomes.
Capsule diagnostic tool. The Atmo Gas Capsule from Atmo Biosciences is an ingestible capsule that measures gases at the source, which can accelerate the diagnosis of diseases such as IBS and inflammatory bowel disease (IBD). According to the company, this technique is highly accurate and offers an alternative to more invasive and expensive diagnostic tools.
Winner: “all-in-one” IBD app. Our Shark Tank winner by both popular vote from AGA Tech Summit attendees and the six-member Shark Tank panel was Oshi Health, selected for its IBD app. The app allows patients to track symptoms, a first step in understanding personalized flare pattern, as well as find resources to learn about their disease and communicate with other patients about their experiences. In a future iteration, information gathered by the app will be made available to physicians to provide current information about disease status to better individualize therapy.
2020 Crohn’s & Colitis Congress now open for registration
Join the Crohn’s & Colitis Foundation and AGA next January in Austin, Tex., for the premier conference on IBD.
The Crohn’s & Colitis Congress combines the strengths of the nation’s leading IBD patient organization, the Crohn’s & Colitis Foundation, and the premier GI professional organization, AGA, to bring together IBD professionals, across all disciplines, to transform IBD care.
The 2020 Congress Committee Chair David T. Rubin, MD, AGAF, University of Chicago, and Cochair Uma Mahadevan, MD, AGAF, University of California, San Francisco, lead a faculty that includes thought leaders in the fields of GI, research investigation, surgery, pediatrics, advanced practice, IBD nursing, diet and nutrition, mental health, radiology, and pathology.
The congress’s agenda includes main sessions that will emphasize case studies and panel discussions. There will also be parallel sessions on basic and translational science for senior and junior investigators. In addition, opening breakout sessions, taking place Jan. 23, will be available for selection free of charge.
Attendees of the 2020 congress will be able to meet with IBD leaders, discover different perspectives, leave with practical information they can immediately implement to take care of their next IBD patient and hear what’s on the horizon in potential treatment.
There will also be plenty of social events and plenty of time to build a strong network, including a Friday night Welcome Reception that should not be missed.
In addition, the 2020 congress is taking place in Austin, Tex. The capital of Texas and the Live Music Capital of the World, Austin is famous for its inspiring and enticing entertainment, culture, cuisine, and outdoor settings. Make a week of it and enjoy all Austin has to offer.
Early-bird registration ends Sept. 18. General abstract submissions for basic, translational, and clinical research begin Aug. 28 and end Oct. 23. To learn more and register, visit www.crohnscolitiscongress.org.
AGA welcomes new president, Hashem B. El-Serag, MD, MPH, AGAF
Hashem B. El-Serag, MD, MPH, AGAF, began his term as the 114th president of the AGA Institute at Digestive Disease Week® (DDW 2019).
Dr. El-Serag is former editor in chief of Clinical Gastroenterology and Hepatology. He currently serves as chair of the department of medicine at Baylor College of Medicine, Houston, following a decade leading and expanding Baylor’s gastroenterology and hepatology section. He is one of the few academic gastroenterologists serving as a chair of a department of medicine in the United States.
Originally Palestinian, Dr. El-Serag became a U.S. citizen in the early 2000s after medical school in Libya. He completed his training at community hospitals in the United States. His path from Benghazi to Baylor is described in the May issue of Gastroenterology by Baylor colleague Dr. Fasiha Kanwal.
“I firmly believe that the success I achieved in the United States would not have been possible anywhere else in the world, and it is as much a testament to the accepting society and medical system as to whatever intrinsic ability or skill I have,” noted Dr. El-Serag.
The major focus of Dr. El-Serag’s scholarly work is the epidemiology and clinical outcomes of hepatocellular carcinoma. Much of the modern literature on this topic includes his more than 100 publications. Since 2014, Dr. El-Serag has been named by Thomson Reuter as among the top 1% of clinical scientists.
Dr. El-Serag “is an innovative scientist, a compassionate physician, and a gifted educator. He is a relentless advocate of science and training, with an astute political sense — all key to influencing and shaping policy,” said Dr. Kanwal.
Dr. El-Serag’s term as AGA president concludes May 2020. Follow him on twitter at @SeragHashem.
AGA journals select new editorial fellows
Congrats to the six GIs selected for this competitive program.
The AGA journals – Gastroenterology, Clinical Gastroenterology and Hepatology (CGH), and Cellular and Molecular Gastroenterology and Hepatology (CMGH) – are pleased to announce their 2019-2020 editorial fellows.
Gastroenterology
Feng Su, MD
University of Washington, Seattle
Victoria Weis, PhD
Wake Forest University, Winston-Salem, N.C.
CGH
Austin Chiang, MD, MPH
Jefferson Medical College, Philadelphia, Penn.
Jennifer Kolb, MD
University of Colorado at Denver, Aurora
CMGH
Cambrian Liu, PhD
The Saban Research Institute, Children’s Hospital Los Angeles, Calif.
Tirthadipa Pradhan-Sundd, PhD
University of Pittsburgh, Penn.
The editorial fellows will be mentored on their respective journals’ editorial processes, including peer review and the publication process from manuscript submission to acceptance. They will participate in discussions and conferences with the boards of editors and work closely with the AGA editorial staff. Additionally, the fellows will participate in AGA’s new reviewer education program and will also be offered the opportunity to contribute content to their respective journals. The newly expanded program builds on the success of the previous 2 years when Gastroenterology had an editorial fellow.
The journals’ board of editors and editorial staff congratulate the fellows and are excited to work with them over the next year.
Get to know this rock star IBS researcher and mom
AGA Research Foundation pilot awards are an invaluable tool for investigators – they provide seed funding to explore promising new lines of research and generate preliminary data for larger grants. So, when Meenakshi Rao, MD, PhD, received the 2016 AGA–Takeda Pharmaceuticals International Research Scholar Award in Neurogastroenterology, she was able to double down on a project to identify why men and women with irritable bowel syndrome (IBS), the most common but least understood of all digestive disorders, report different symptoms and respond differently to treatment. Based on her recent accomplishments, we’re excited for you to get to know Dr. Rao, assistant professor of pediatrics at Harvard Medical School, Boston, and our AGA Research Foundation researcher of the month.
The Rao lab AGA-funded project focused on building upon Dr. Rao’s previous findings, which showed that disrupting nerves in the bowel had vastly different effects on males and females. These surprising results led Dr. Rao to explore whether sex hormones, such as testosterone and estrogen, might regulate how well things move through the bowel. Dr. Rao believes that identifying the underlying causes for sex differences in bowel function could lead to more effective and personalized treatments for patients with IBS. You can read the specifics of Dr. Rao’s research in the October 2017 issue of Gastroenterology and the October 2018 issue of Journal of Neuroscience.
IBS symptoms in women more typically involve constipation while young men with IBS more commonly report diarrhea. Over time, as men age, however, they tend to experience more constipation, Dr. Rao said. “Sex hormones might be signaling directly to the nerves in our gut and playing a role in these sex differences,” Dr. Rao said. “It might mean we can’t think of this as one disorder. IBS in a male may be different than IBS in a female, and that could change how we approach diagnosis and treatment.”
The AGA grant laid the groundwork for Dr. Rao’s findings, which led to a new understanding of how different types of cells in the gut nervous system regulate bowel functions – and how this regulation is different in males and females. The AGA grant helped Dr. Rao secure funding from the National Institutes of Health to launch new projects focused on how disruption of the gut nervous system causes disease.
Dr. Rao received the AGA award in 2015, when her son, Avinash, was aged 2 years. She acknowledged the delicate balancing act of raising a family and advancing her research.
“A lot of things were happening at once,” she said. “As a young parent, having the support of this award and having a technician (made possible by the award) made a big difference.”
Her son, now 5 years old, is growing up in a science-centric household because Dr. Rao’s husband is also a scientist. Not surprisingly, Dr. Rao says, her son is becoming a budding scientist.
“He talks about experiments all the time,” she says. “He even articulated to me the other day why we work on mice to learn how to help people. I never taught him that. I was floored.”
Five new GI technologies to know
The AGA Tech Summit Shark Tank is our annual reminder that the field of GI is ripe for innovation. Continue reading for an overview of the five new technologies pitched to our panel of sharks.
The smart toilet seat. A toilet seat developed by Toi Labs, called TrueLoo, is equipped with lighting and cameras that capture images of bowel movements and urination for subsequent analysis. The company describes TrueLoo as a low-cost disease-screening tool that has major potential for early detection of conditions ranging from dehydration to gastrointestinal cancer.
AI to aid screening endoscopy. A new tool called Ultivision, being developed by the startup Docbot, was described as a strategy to employ artificial intelligence (AI) to aid endoscopists in screening for dysplasia in either screening colonoscopy or in surveillance of Barrett’s esophagus. The tool integrates with existing endoscopic tools. As tissue is visualized, the AI is programmed to highlight suspected dysplasia with a colored box to alert the endoscopist.
Obesity phenotyping tool. The Pheno Test, developed by Phenomix Sciences, applies “multi-omics” to a blood-based test to separate patients with obesity into four phenotypes: hungry brain (satiation signal is impaired), hungry gut (signals to eat are upregulated), emotional hunger (psychological reasons drive eating behavior), and slow metabolism (failure to burn fat at normal rates). With this knowledge, treatment can be tailored appropriately leading to better outcomes.
Capsule diagnostic tool. The Atmo Gas Capsule from Atmo Biosciences is an ingestible capsule that measures gases at the source, which can accelerate the diagnosis of diseases such as IBS and inflammatory bowel disease (IBD). According to the company, this technique is highly accurate and offers an alternative to more invasive and expensive diagnostic tools.
Winner: “all-in-one” IBD app. Our Shark Tank winner by both popular vote from AGA Tech Summit attendees and the six-member Shark Tank panel was Oshi Health, selected for its IBD app. The app allows patients to track symptoms, a first step in understanding personalized flare pattern, as well as find resources to learn about their disease and communicate with other patients about their experiences. In a future iteration, information gathered by the app will be made available to physicians to provide current information about disease status to better individualize therapy.
2020 Crohn’s & Colitis Congress now open for registration
Join the Crohn’s & Colitis Foundation and AGA next January in Austin, Tex., for the premier conference on IBD.
The Crohn’s & Colitis Congress combines the strengths of the nation’s leading IBD patient organization, the Crohn’s & Colitis Foundation, and the premier GI professional organization, AGA, to bring together IBD professionals, across all disciplines, to transform IBD care.
The 2020 Congress Committee Chair David T. Rubin, MD, AGAF, University of Chicago, and Cochair Uma Mahadevan, MD, AGAF, University of California, San Francisco, lead a faculty that includes thought leaders in the fields of GI, research investigation, surgery, pediatrics, advanced practice, IBD nursing, diet and nutrition, mental health, radiology, and pathology.
The congress’s agenda includes main sessions that will emphasize case studies and panel discussions. There will also be parallel sessions on basic and translational science for senior and junior investigators. In addition, opening breakout sessions, taking place Jan. 23, will be available for selection free of charge.
Attendees of the 2020 congress will be able to meet with IBD leaders, discover different perspectives, leave with practical information they can immediately implement to take care of their next IBD patient and hear what’s on the horizon in potential treatment.
There will also be plenty of social events and plenty of time to build a strong network, including a Friday night Welcome Reception that should not be missed.
In addition, the 2020 congress is taking place in Austin, Tex. The capital of Texas and the Live Music Capital of the World, Austin is famous for its inspiring and enticing entertainment, culture, cuisine, and outdoor settings. Make a week of it and enjoy all Austin has to offer.
Early-bird registration ends Sept. 18. General abstract submissions for basic, translational, and clinical research begin Aug. 28 and end Oct. 23. To learn more and register, visit www.crohnscolitiscongress.org.
AGA welcomes new president, Hashem B. El-Serag, MD, MPH, AGAF
Hashem B. El-Serag, MD, MPH, AGAF, began his term as the 114th president of the AGA Institute at Digestive Disease Week® (DDW 2019).
Dr. El-Serag is former editor in chief of Clinical Gastroenterology and Hepatology. He currently serves as chair of the department of medicine at Baylor College of Medicine, Houston, following a decade leading and expanding Baylor’s gastroenterology and hepatology section. He is one of the few academic gastroenterologists serving as a chair of a department of medicine in the United States.
Originally Palestinian, Dr. El-Serag became a U.S. citizen in the early 2000s after medical school in Libya. He completed his training at community hospitals in the United States. His path from Benghazi to Baylor is described in the May issue of Gastroenterology by Baylor colleague Dr. Fasiha Kanwal.
“I firmly believe that the success I achieved in the United States would not have been possible anywhere else in the world, and it is as much a testament to the accepting society and medical system as to whatever intrinsic ability or skill I have,” noted Dr. El-Serag.
The major focus of Dr. El-Serag’s scholarly work is the epidemiology and clinical outcomes of hepatocellular carcinoma. Much of the modern literature on this topic includes his more than 100 publications. Since 2014, Dr. El-Serag has been named by Thomson Reuter as among the top 1% of clinical scientists.
Dr. El-Serag “is an innovative scientist, a compassionate physician, and a gifted educator. He is a relentless advocate of science and training, with an astute political sense — all key to influencing and shaping policy,” said Dr. Kanwal.
Dr. El-Serag’s term as AGA president concludes May 2020. Follow him on twitter at @SeragHashem.
Calendar
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Aug. 9-10, 2019
2019 Freston Conference: Food at the Intersection of Gut Health and Disease
GI clinicians and allied health professionals are increasingly focused on how nutrients influence GI physiology and how diet can promote sound gut health. In response to this growing body of knowledge, the 2019 James W. Freston Conference — Food at the Intersection of Gut Health and Disease, Aug. 9-10, 2019, in Chicago — will examine how nutrition management therapies can combat GI disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and celiac disease and how diet supports improvement across the care continuum.
Chicago, Illinois
Aug. 9–11, 2019
2019 Principles of GI for the NP and PA
The Principles of Gastroenterology for the Nurse Practitioner and Physician Assistant (NPPA) is the medical industry’s premiere course guiding and enabling nurse practitioners and physician assistants with the intricacies of identifying, treating, and managing GI disorders. Designed and taught by expert clinicians and advanced practice providers, NPPA provides the latest insights, knowledge, and research on how to improve GI patient care. Attendees will leave with stronger diagnostic and therapeutic skills, a more robust professional network, and an enhanced value for their practices.
Chicago, Illinois
Sept. 18-19, 2019; Oct. 9-10. 2019
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc.
Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Atlanta, GA (9/18-19); Las Vegas, NV (10/9-10)
Oct. 4, 2019
2019 AGA Partners in Value
Join GI trailblazers and leaders from AGA and DHPA to network and discuss strategies that will help your practice succeed in the changing business of health care. Leave equipped to make better decisions for the future.
Chicago, Illinois
May 2-5, 2020
Digestive Disease Week® (DDW)
Digestive Disease Week® (DDW) is the world’s leading educational forum for academicians, clinicians, researchers, students, and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery, and related fields. Whether you work in patient care, research, education, or administration, the DDW program offers something for you. Abstract submissions will be due on Dec. 1, and registration will open in January 2020.
Chicago, Illinois
AWARDS APPLICATION DEADLINES
AGA-Elsevier Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing research in gastroenterology- or hepatology-related areas.
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of inflammatory bowel disease (IBD).
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Nonalcoholic Fatty Liver Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of nonalcoholic fatty liver disease (NAFLD).
Application Deadline: Sept. 4, 2019
AGA-Pfizer Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to recipients at any career stage researching new directions focused on improving the diagnosis and treatment of inflammatory bowel disease.
Application Deadline: Sept. 4, 2019
AGA-Rome Foundation Functional GI and Motility Disorders Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing clinical or translational research pertaining to functional GI and motility disorders.
Application Deadline: Sept. 4, 2019
AGA Research Scholar Award (RSA)
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in digestive disease research.
Application Deadline: Nov. 13, 2019
AGA-Gastric Cancer Foundation Ben Feinstein Memorial Research Scholar Award in Gastric Cancer
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in gastric cancer research. Research involving precancerous lesions will be considered if relevance to gastric cancer is explicitly outlined.
Application Deadline: Nov. 13, 2019
AGA-Takeda Pharmaceuticals Research Scholar Award in Inflammatory Bowel Disease
This award provides $100,000 per year for 3 years (total $300,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in inflammatory bowel disease research.
Application Deadline: Nov. 13, 2019
AGA Fellow Abstract Award
This $500 travel award supports recipients who are MD, PhD or equivalent fellows giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW). The top-scoring abstract will be designated the Fellow Abstract of the Year and receive a $1,000 award.
Application Deadline: Feb. 26, 2020
AGA Student Abstract Award
This $500 travel award supports recipients who are graduate students, medical students, or medical residents (residents up to postgraduate year three) giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
AGA-Moti L. & Kamla Rustgi International Travel Awards
This $750 travel award supports recipients who are young (i.e., 35 years of age or younger at the time of DDW) basic, translational, or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Aug. 9-10, 2019
2019 Freston Conference: Food at the Intersection of Gut Health and Disease
GI clinicians and allied health professionals are increasingly focused on how nutrients influence GI physiology and how diet can promote sound gut health. In response to this growing body of knowledge, the 2019 James W. Freston Conference — Food at the Intersection of Gut Health and Disease, Aug. 9-10, 2019, in Chicago — will examine how nutrition management therapies can combat GI disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and celiac disease and how diet supports improvement across the care continuum.
Chicago, Illinois
Aug. 9–11, 2019
2019 Principles of GI for the NP and PA
The Principles of Gastroenterology for the Nurse Practitioner and Physician Assistant (NPPA) is the medical industry’s premiere course guiding and enabling nurse practitioners and physician assistants with the intricacies of identifying, treating, and managing GI disorders. Designed and taught by expert clinicians and advanced practice providers, NPPA provides the latest insights, knowledge, and research on how to improve GI patient care. Attendees will leave with stronger diagnostic and therapeutic skills, a more robust professional network, and an enhanced value for their practices.
Chicago, Illinois
Sept. 18-19, 2019; Oct. 9-10. 2019
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc.
Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Atlanta, GA (9/18-19); Las Vegas, NV (10/9-10)
Oct. 4, 2019
2019 AGA Partners in Value
Join GI trailblazers and leaders from AGA and DHPA to network and discuss strategies that will help your practice succeed in the changing business of health care. Leave equipped to make better decisions for the future.
Chicago, Illinois
May 2-5, 2020
Digestive Disease Week® (DDW)
Digestive Disease Week® (DDW) is the world’s leading educational forum for academicians, clinicians, researchers, students, and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery, and related fields. Whether you work in patient care, research, education, or administration, the DDW program offers something for you. Abstract submissions will be due on Dec. 1, and registration will open in January 2020.
Chicago, Illinois
AWARDS APPLICATION DEADLINES
AGA-Elsevier Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing research in gastroenterology- or hepatology-related areas.
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of inflammatory bowel disease (IBD).
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Nonalcoholic Fatty Liver Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of nonalcoholic fatty liver disease (NAFLD).
Application Deadline: Sept. 4, 2019
AGA-Pfizer Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to recipients at any career stage researching new directions focused on improving the diagnosis and treatment of inflammatory bowel disease.
Application Deadline: Sept. 4, 2019
AGA-Rome Foundation Functional GI and Motility Disorders Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing clinical or translational research pertaining to functional GI and motility disorders.
Application Deadline: Sept. 4, 2019
AGA Research Scholar Award (RSA)
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in digestive disease research.
Application Deadline: Nov. 13, 2019
AGA-Gastric Cancer Foundation Ben Feinstein Memorial Research Scholar Award in Gastric Cancer
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in gastric cancer research. Research involving precancerous lesions will be considered if relevance to gastric cancer is explicitly outlined.
Application Deadline: Nov. 13, 2019
AGA-Takeda Pharmaceuticals Research Scholar Award in Inflammatory Bowel Disease
This award provides $100,000 per year for 3 years (total $300,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in inflammatory bowel disease research.
Application Deadline: Nov. 13, 2019
AGA Fellow Abstract Award
This $500 travel award supports recipients who are MD, PhD or equivalent fellows giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW). The top-scoring abstract will be designated the Fellow Abstract of the Year and receive a $1,000 award.
Application Deadline: Feb. 26, 2020
AGA Student Abstract Award
This $500 travel award supports recipients who are graduate students, medical students, or medical residents (residents up to postgraduate year three) giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
AGA-Moti L. & Kamla Rustgi International Travel Awards
This $750 travel award supports recipients who are young (i.e., 35 years of age or younger at the time of DDW) basic, translational, or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Aug. 9-10, 2019
2019 Freston Conference: Food at the Intersection of Gut Health and Disease
GI clinicians and allied health professionals are increasingly focused on how nutrients influence GI physiology and how diet can promote sound gut health. In response to this growing body of knowledge, the 2019 James W. Freston Conference — Food at the Intersection of Gut Health and Disease, Aug. 9-10, 2019, in Chicago — will examine how nutrition management therapies can combat GI disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and celiac disease and how diet supports improvement across the care continuum.
Chicago, Illinois
Aug. 9–11, 2019
2019 Principles of GI for the NP and PA
The Principles of Gastroenterology for the Nurse Practitioner and Physician Assistant (NPPA) is the medical industry’s premiere course guiding and enabling nurse practitioners and physician assistants with the intricacies of identifying, treating, and managing GI disorders. Designed and taught by expert clinicians and advanced practice providers, NPPA provides the latest insights, knowledge, and research on how to improve GI patient care. Attendees will leave with stronger diagnostic and therapeutic skills, a more robust professional network, and an enhanced value for their practices.
Chicago, Illinois
Sept. 18-19, 2019; Oct. 9-10. 2019
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc.
Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Atlanta, GA (9/18-19); Las Vegas, NV (10/9-10)
Oct. 4, 2019
2019 AGA Partners in Value
Join GI trailblazers and leaders from AGA and DHPA to network and discuss strategies that will help your practice succeed in the changing business of health care. Leave equipped to make better decisions for the future.
Chicago, Illinois
May 2-5, 2020
Digestive Disease Week® (DDW)
Digestive Disease Week® (DDW) is the world’s leading educational forum for academicians, clinicians, researchers, students, and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery, and related fields. Whether you work in patient care, research, education, or administration, the DDW program offers something for you. Abstract submissions will be due on Dec. 1, and registration will open in January 2020.
Chicago, Illinois
AWARDS APPLICATION DEADLINES
AGA-Elsevier Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing research in gastroenterology- or hepatology-related areas.
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of inflammatory bowel disease (IBD).
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Nonalcoholic Fatty Liver Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of nonalcoholic fatty liver disease (NAFLD).
Application Deadline: Sept. 4, 2019
AGA-Pfizer Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to recipients at any career stage researching new directions focused on improving the diagnosis and treatment of inflammatory bowel disease.
Application Deadline: Sept. 4, 2019
AGA-Rome Foundation Functional GI and Motility Disorders Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing clinical or translational research pertaining to functional GI and motility disorders.
Application Deadline: Sept. 4, 2019
AGA Research Scholar Award (RSA)
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in digestive disease research.
Application Deadline: Nov. 13, 2019
AGA-Gastric Cancer Foundation Ben Feinstein Memorial Research Scholar Award in Gastric Cancer
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in gastric cancer research. Research involving precancerous lesions will be considered if relevance to gastric cancer is explicitly outlined.
Application Deadline: Nov. 13, 2019
AGA-Takeda Pharmaceuticals Research Scholar Award in Inflammatory Bowel Disease
This award provides $100,000 per year for 3 years (total $300,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in inflammatory bowel disease research.
Application Deadline: Nov. 13, 2019
AGA Fellow Abstract Award
This $500 travel award supports recipients who are MD, PhD or equivalent fellows giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW). The top-scoring abstract will be designated the Fellow Abstract of the Year and receive a $1,000 award.
Application Deadline: Feb. 26, 2020
AGA Student Abstract Award
This $500 travel award supports recipients who are graduate students, medical students, or medical residents (residents up to postgraduate year three) giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
AGA-Moti L. & Kamla Rustgi International Travel Awards
This $750 travel award supports recipients who are young (i.e., 35 years of age or younger at the time of DDW) basic, translational, or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
August 2019 – ICYMI
Gastroenterology
Promoting leadership by women in gastroenterology: Lessons learned and future directions. Pascua M et al. 2019 May;156(6):1548-52. doi. org/10.1053/j.gastro.2019.03.012.
How to incorporate esophageal manometry teaching in your fellowship program. Kraft C et al. 2019 June;156(8):2120-3. doi. org/10.1053/j.gastro.2019.04.024.
How to incorporate bariatric training into your fellowship program. Jirapinyo P et al. 2019 July;157(1):9-13. doi. org/10.1053/j.gastro.2019.05.034.
Clin Gastroenterol Hepatol.
Preparing for large-scale disruptions in health care delivery: Nursing strikes and beyond. Allen JI et al. 2019 July;17(8):1424-7. doi. org/10.1016/j.cgh.2019.02.001.
Optimal management of malignant polyps, from endoscopic assessment and resection to decisions about surgery. Rex DK et al. 2019 July;17(8):1428-37. doi. org/10.1016/j.cgh.2018.09.040.
Bowel cleansing strategies after suboptimal bowel preparation. Sharara AI et al. 2019 June;17(7):1239-41. doi. org/10.1016/j.cgh.2018.12.042.
Holding gastroenterologists accountable for colonoscopy through MACRA episode–based cost measure. Siddique SM et al. 2019 May;17(6):1015-8. doi. org/10.1016/j.cgh.2019.01.009.
Endoscopic mucosal resection vs endoscopic submucosal dissection for Barrett’s esophagus and colorectal neoplasia. Yang D et al. May;17(6):1019-28. doi. org/10.1016/j.cgh.2018.09.030.
Metal biliary stents in benign disease. Haseeb A et al. 2019 May;17(6):1029-32. doi. org/10.1016/j.cgh.2018.12.010.
Cell Mol Gastroenterol Hepatol.
Rigor, reproducibility, and responsibility: A quantum of solace. Turner JR. 2019;7(4):869-71. doi. org/10.1016/j.jcmgh.2019.03.006.
Gastroenterology
Promoting leadership by women in gastroenterology: Lessons learned and future directions. Pascua M et al. 2019 May;156(6):1548-52. doi. org/10.1053/j.gastro.2019.03.012.
How to incorporate esophageal manometry teaching in your fellowship program. Kraft C et al. 2019 June;156(8):2120-3. doi. org/10.1053/j.gastro.2019.04.024.
How to incorporate bariatric training into your fellowship program. Jirapinyo P et al. 2019 July;157(1):9-13. doi. org/10.1053/j.gastro.2019.05.034.
Clin Gastroenterol Hepatol.
Preparing for large-scale disruptions in health care delivery: Nursing strikes and beyond. Allen JI et al. 2019 July;17(8):1424-7. doi. org/10.1016/j.cgh.2019.02.001.
Optimal management of malignant polyps, from endoscopic assessment and resection to decisions about surgery. Rex DK et al. 2019 July;17(8):1428-37. doi. org/10.1016/j.cgh.2018.09.040.
Bowel cleansing strategies after suboptimal bowel preparation. Sharara AI et al. 2019 June;17(7):1239-41. doi. org/10.1016/j.cgh.2018.12.042.
Holding gastroenterologists accountable for colonoscopy through MACRA episode–based cost measure. Siddique SM et al. 2019 May;17(6):1015-8. doi. org/10.1016/j.cgh.2019.01.009.
Endoscopic mucosal resection vs endoscopic submucosal dissection for Barrett’s esophagus and colorectal neoplasia. Yang D et al. May;17(6):1019-28. doi. org/10.1016/j.cgh.2018.09.030.
Metal biliary stents in benign disease. Haseeb A et al. 2019 May;17(6):1029-32. doi. org/10.1016/j.cgh.2018.12.010.
Cell Mol Gastroenterol Hepatol.
Rigor, reproducibility, and responsibility: A quantum of solace. Turner JR. 2019;7(4):869-71. doi. org/10.1016/j.jcmgh.2019.03.006.
Gastroenterology
Promoting leadership by women in gastroenterology: Lessons learned and future directions. Pascua M et al. 2019 May;156(6):1548-52. doi. org/10.1053/j.gastro.2019.03.012.
How to incorporate esophageal manometry teaching in your fellowship program. Kraft C et al. 2019 June;156(8):2120-3. doi. org/10.1053/j.gastro.2019.04.024.
How to incorporate bariatric training into your fellowship program. Jirapinyo P et al. 2019 July;157(1):9-13. doi. org/10.1053/j.gastro.2019.05.034.
Clin Gastroenterol Hepatol.
Preparing for large-scale disruptions in health care delivery: Nursing strikes and beyond. Allen JI et al. 2019 July;17(8):1424-7. doi. org/10.1016/j.cgh.2019.02.001.
Optimal management of malignant polyps, from endoscopic assessment and resection to decisions about surgery. Rex DK et al. 2019 July;17(8):1428-37. doi. org/10.1016/j.cgh.2018.09.040.
Bowel cleansing strategies after suboptimal bowel preparation. Sharara AI et al. 2019 June;17(7):1239-41. doi. org/10.1016/j.cgh.2018.12.042.
Holding gastroenterologists accountable for colonoscopy through MACRA episode–based cost measure. Siddique SM et al. 2019 May;17(6):1015-8. doi. org/10.1016/j.cgh.2019.01.009.
Endoscopic mucosal resection vs endoscopic submucosal dissection for Barrett’s esophagus and colorectal neoplasia. Yang D et al. May;17(6):1019-28. doi. org/10.1016/j.cgh.2018.09.030.
Metal biliary stents in benign disease. Haseeb A et al. 2019 May;17(6):1029-32. doi. org/10.1016/j.cgh.2018.12.010.
Cell Mol Gastroenterol Hepatol.
Rigor, reproducibility, and responsibility: A quantum of solace. Turner JR. 2019;7(4):869-71. doi. org/10.1016/j.jcmgh.2019.03.006.
Chronic abdominal pain, career options in industry, coding basics, and more
As many of us see patients with abdominal pain on an almost daily basis, it becomes easy to overlook the substantial long-term effects this chronic pain can have on patients. In this quarter’s In Focus article, Emily Weaver and Eva Szigethy (UPMC) explore how to utilize a multidisciplinary approach to effectively treat chronic abdominal pain, and they also highlight how chronic abdominal pain can truly be a traumatic experience for patients. This article is definitely a must-read for all practitioners.
Also in this issue of The New Gastroenterologist, Matthew Whitson (Hofstra-Northwell) provides some advice on becoming an effective educator, which is critically important, especially when making the transition from being a trainee to now having to teach trainees. Additionally, Erica Cohen and Gil Melmed (Cedars-Sinai) provide some important lessons about attempting to start an investigator-led clinical trial, which is a difficult task regardless of what career stage you’re in.
In this quarter’s DHPA-cosponsored private practice perspective, Marc Sonenshine (Atlanta Gastroenterology Associates) provides some tips for how to develop a specialized niche in private practice. And in our postfellowship pathway section, Mark Sostek (Orphomed) provides an enlightening overview of some career options in industry.
Finally, Kathleen Mueller (AskMueller Consulting, LLC) gives an overview of some coding basics, which is important knowledge, especially for trainees, and Latha Alaparthi (Gastroenterology Center of Connecticut/Yale/Quinnipiac) provides an overview of some advanced degree programs you may consider when contemplating a career change.
Interested in contributing to The New Gastroenterologist? Have ideas for future issues? If so, please contact me at [email protected] or the managing editor, Ryan Farrell, at [email protected].
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an assistant professor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
As many of us see patients with abdominal pain on an almost daily basis, it becomes easy to overlook the substantial long-term effects this chronic pain can have on patients. In this quarter’s In Focus article, Emily Weaver and Eva Szigethy (UPMC) explore how to utilize a multidisciplinary approach to effectively treat chronic abdominal pain, and they also highlight how chronic abdominal pain can truly be a traumatic experience for patients. This article is definitely a must-read for all practitioners.
Also in this issue of The New Gastroenterologist, Matthew Whitson (Hofstra-Northwell) provides some advice on becoming an effective educator, which is critically important, especially when making the transition from being a trainee to now having to teach trainees. Additionally, Erica Cohen and Gil Melmed (Cedars-Sinai) provide some important lessons about attempting to start an investigator-led clinical trial, which is a difficult task regardless of what career stage you’re in.
In this quarter’s DHPA-cosponsored private practice perspective, Marc Sonenshine (Atlanta Gastroenterology Associates) provides some tips for how to develop a specialized niche in private practice. And in our postfellowship pathway section, Mark Sostek (Orphomed) provides an enlightening overview of some career options in industry.
Finally, Kathleen Mueller (AskMueller Consulting, LLC) gives an overview of some coding basics, which is important knowledge, especially for trainees, and Latha Alaparthi (Gastroenterology Center of Connecticut/Yale/Quinnipiac) provides an overview of some advanced degree programs you may consider when contemplating a career change.
Interested in contributing to The New Gastroenterologist? Have ideas for future issues? If so, please contact me at [email protected] or the managing editor, Ryan Farrell, at [email protected].
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an assistant professor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
As many of us see patients with abdominal pain on an almost daily basis, it becomes easy to overlook the substantial long-term effects this chronic pain can have on patients. In this quarter’s In Focus article, Emily Weaver and Eva Szigethy (UPMC) explore how to utilize a multidisciplinary approach to effectively treat chronic abdominal pain, and they also highlight how chronic abdominal pain can truly be a traumatic experience for patients. This article is definitely a must-read for all practitioners.
Also in this issue of The New Gastroenterologist, Matthew Whitson (Hofstra-Northwell) provides some advice on becoming an effective educator, which is critically important, especially when making the transition from being a trainee to now having to teach trainees. Additionally, Erica Cohen and Gil Melmed (Cedars-Sinai) provide some important lessons about attempting to start an investigator-led clinical trial, which is a difficult task regardless of what career stage you’re in.
In this quarter’s DHPA-cosponsored private practice perspective, Marc Sonenshine (Atlanta Gastroenterology Associates) provides some tips for how to develop a specialized niche in private practice. And in our postfellowship pathway section, Mark Sostek (Orphomed) provides an enlightening overview of some career options in industry.
Finally, Kathleen Mueller (AskMueller Consulting, LLC) gives an overview of some coding basics, which is important knowledge, especially for trainees, and Latha Alaparthi (Gastroenterology Center of Connecticut/Yale/Quinnipiac) provides an overview of some advanced degree programs you may consider when contemplating a career change.
Interested in contributing to The New Gastroenterologist? Have ideas for future issues? If so, please contact me at [email protected] or the managing editor, Ryan Farrell, at [email protected].
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an assistant professor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
Exploring multidisciplinary treatments in the traumatizing aspects of chronic abdominal pain
Introduction
Abdominal pain is a complex phenomenon that involves unpleasant sensory and emotional experiences caused by actual or potential visceral tissue damage. As pain becomes chronic, there is a functional reorganization of the brain involved in emotional and cognitive processing leading to amplification of pain perception and associated pain suffering.1,2 With the rising recognition of the complexity of pain management in the 1960s, the treatment of pain became a recognized field of study, leading to the formation of interdisciplinary teams to treat pain. However, although efficacious, this model lacked adequate reimbursement structures and eventually subsided as opioids (which at the time were widely believed to be nonaddictive) become more prevalent.3 Not only is there a lack of empirical evidence for opioids in the management of chronic abdominal pain, there is a growing list of adverse consequences of prolonged opioid use for both the brain and gastrointestinal tract.4
Recently, there has been more clinical focus on behavioral interventions that can modulate gut pain signals and associated behaviors by reversing maladaptive emotional and cognitive brain processes.5 One such psychological process that has received little attention is the traumatizing nature of chronic abdominal pain. Chronic pain, particularly when it feels uncontrollable to patients, activates the brain’s fear circuitry and drives hyperarousal, emotional numbing, and consolidation of painful somatic memories, which become habitual and further amplify negative visceral signals.6,7 These processes are identical to the symptom manifestations of posttraumatic stress disorder (PTSD) such as intrusiveness, avoidance, negative mood and cognitions, and hyperarousal from life events. In fact, individuals with a history of other traumatizing exposures have an even higher risk of developing chronic pain disorders.8 This review has two objectives: to provide a theoretical framework for understanding chronic pain as a traumatizing experience with posttraumatic manifestations and to discuss behavioral interventions and adjunctive nonopioid pharmacotherapy embedded in multidisciplinary care models essential to reversing this negative brain-gut cycle and reducing pain-related suffering.
Trauma and chronic abdominal pain
Trauma is defined as an individual’s response to a threat to safety. Traumatized patients or those with PTSD are at higher risk for chronic abdominal pain.9 Given the strong neurobiological connection between the brain and gut that has been phylogenetically preserved, emotional (e.g., fear, terror) or physical (e.g., pain) signals represent danger, and with chronicity, there can be a kindling-related consolidation of these maladaptive neurobiological pathways leading to suffering (e.g., hopelessness, sense of failure) and disability (Figure 1).
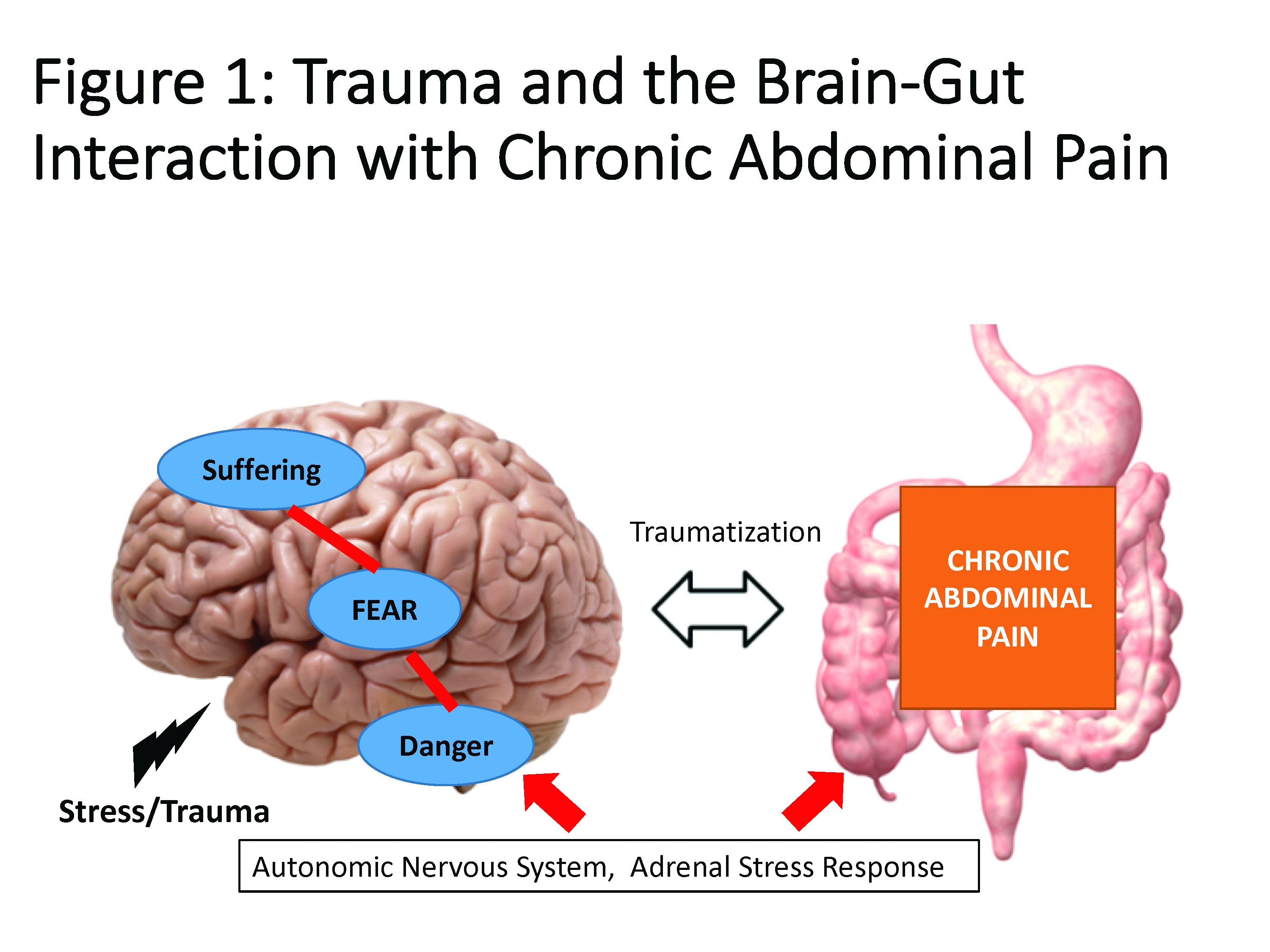
The interrelationship between chronic pain and trauma is multifaceted and is further complicated by the traumatizing nature of chronic pain itself, when pain is interpreted as a signal that the body is sick or even dangerously ill. Patients with chronic abdominal pain may seek multiple medical opinions and often undergo extensive, unnecessary, and sometimes harmful interventions to find the cause of their pain, with fear of disability and even death driving this search for answers.
The degree to which an individual with long-lasting pain interprets their discomfort as a risk to their well-being is related to the degree of trauma they experience because of their pain.10 Indeed, many of the negative symptoms associated with posttraumatic stress are also found in those with chronic abdominal pain. Trauma impacts the fear circuitry centers of the brain, leading to altered activation of the hypothalamic-pituitary-adrenal axis and the amygdala, as well as chronic activation of the sympathetic nervous system and stress-released hormones, all of which are potential pathways that dysregulate the brain-gut relationship.11-13 Worries for safety, which are reactivated by physiological cues (e.g., GI symptoms, pain), as well as avoidance of potential triggers of GI symptoms (e.g., food, exercise, medications, and situations such as travel or scheduled events, and fear of being trapped without bathroom access), are common. Traumatized individuals can experience a foreshortened sense of the future, which may lead to decreased investment in long-term determinants of health (e.g., balanced diet, exercise, social support) and have higher rates of functional impairment and higher health care utilization.14 Negative mood, including irritability, anxiety, depression, insomnia, and impaired concentration are common in those with trauma and chronic pain and can be accompanied by internalized blame (e.g., depression, substance abuse, suicidality) or externalized blame (e.g., negative relationships with health care providers, rejection from their support or faith system). These can be worsened by an impaired sense of trust, which impacts the patient-provider relationship and other sources of social support leading to lack of behavioral activation, anhedonia, and isolation.
Another commonality is hypervigilance, as those with chronic abdominal pain are often hyperaware of physical symptoms and always “on alert” for a signal indicative of a pain flare. Anxiety and depression frequently co-occur in populations with trauma and chronic pain; these diagnoses are associated with higher rates of catastrophizing and learned helplessness, which may be exacerbated by lack of a “cure” for functional gastrointestinal disorders (FGIDs) and chronic pain.15 These factors could potentially lead to lack of engagement with treatment or, alternatively, risky or destructive attempts to cure pain including dangerous complementary alternative treatments or substance abuse to numb sensations. Another feature of trauma in chronic pain is the sense of dissociation from and lack of control over the body, sometimes induced by negative medical experiences (e.g., unwanted physical examinations, medication side effects, traumatic procedures, or hospitalizations).16,17
The importance of treating trauma in the management of chronic pain
Behavioral treatment is increasingly being recognized as an essential component in the management of any chronic pain syndrome.18 The most studied psychosocial interventions for chronic abdominal pain are cognitive-behavioral therapy (CBT) and gut-focused hypnosis. CBT is usually a problem-focused, short-term intervention that can be delivered individually in the office, via group therapy, or through virtual platforms. CBT is most effective when cognitive distortions and ineffective behaviors create emotional distress, and the therapy targets patient’s stress reactivity, visceral anxiety, catastrophizing, and inflexible coping styles.5 Gut-focused hypnosis is the second most–studied behavioral treatment for chronic abdominal pain and utilizes the trance state to make positive suggestions leading to broad and lasting physiological and psychological improvement.19 In addition to pain management, both CBT and hypnosis are efficacious treatments for PTSD.20,21
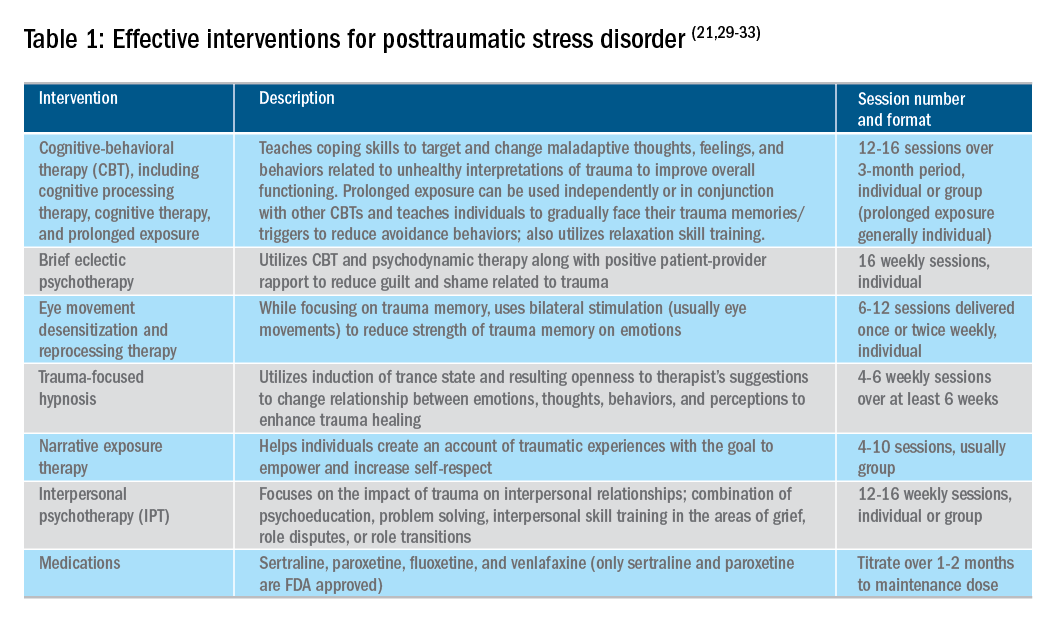
Utilizing a multidisciplinary medical team including integrated behavioral experts, such as in a patient-centered medical home, is considered the standard of care for treatment of chronic pain. The patient-provider relationship is essential, as is consistent follow-up to ensure effective symptom management and improvements in quality of life. Additionally, patient education, including a positive (i.e., clear) diagnosis and information on the brain-gut relationship, is associated with symptom improvement. In our subspecialty medical home for inflammatory bowel disease (IBD), we found that, in our patients who were on opioids for their chronic pain, engagement with our embedded behavioral and pain specialists resulted in significant reduction in opioid use and depression as well as improved self-reported quality of life.22 Gastroenterologists and advanced-practice providers operating without embedded behavioral therapists can consider referring patients to behavioral treatment (e.g., licensed clinical social workers, licensed professional counselors, marriage and family therapists, psychologists, and psychiatrists; the latter often specialize in medication management and may not offer behavioral therapy) for trauma if patients have undergone a traumatic event (e.g., exposure to any potentially life-threatening event, serious injury, or violence) at any point in their lifetime and are experiencing intrusive symptoms (e.g., memories, dreams, or flashbacks to trauma), avoidance of trauma reminders, and negative mood or hyperarousal related to traumatic events (Table 1).23
With the traumatization component of chronic abdominal pain, which can further drive maladaptive coping cycles, incorporation of trauma-informed treatment into gastroenterology clinics is an avenue toward more effective treatment. The core principles of trauma-informed care include safety, choice, collaboration, trustworthiness, and empowerment,24 and are easily aligned with patient-centered models of care such as the interdisciplinary medical home model. Incorporation of screening techniques, interdisciplinary training of clinicians, and use of behavioral providers with experience in evidenced-based treatments of trauma enhance a clinic’s ability to effectively identify and treat individuals who have trauma because of their abdominal pain.25 Additionally, the most common behavioral interventions for functional gastrointestinal disorders (FGIDs) are also efficacious in the treatment of trauma. CBT is a well-validated treatment for PTSD that utilizes exposure therapy to help individuals restructure negative beliefs shaped by their negative experience and develop relaxation skills. Hypnosis is also validated in the treatment of trauma, with the possible mechanism of action being the replacement of the negative or dissociated traumatic trance with a healthy, adaptive trance facilitated by the hypnotherapist.21
Adjunctive nonopioid medications for chronic abdominal pain
While there are few randomized controlled trials establishing efficacy of pharmacotherapy for sustained improvement of abdominal pain or related suffering, several small trials and consensus clinical expert opinion suggest partial improvement in these domains.26,27 Central neuromodulators that can attenuate chronic visceral pain include antidepressants, antipsychotics, and other central nervous system–targeted medications.26 Tricyclic antidepressants (e.g., amitriptyline, nortriptyline, imipramine, desipramine) are often first-line treatment for FGIDs.28 Serotonin noradrenergic reuptake inhibitors (e.g., duloxetine, venlafaxine, desvenlafaxine, milnacipran) are also effective in pain management. Selective serotonin reuptake inhibitors (e.g., paroxetine, fluoxetine, sertraline, citalopram, escitalopram) can be used, especially when comorbid depression, anxiety, and phobic disorders are present. Tetracyclic antidepressants (e.g., mirtazapine, mianserin, trazodone) are effective treatments for early satiety, nausea/vomiting, insomnia, and low weight. Augmenting agents are utilized when single agents do not provide maximum benefit, including quetiapine (disturbed sleep), bupropion (fatigue), aripiprazole, buspirone, and tandospirone (dyspeptic features and anxiety). Delta ligands including gabapentin and pregabalin are helpful for abdominal wall pain or fibromyalgia. Ketamine is a newer but promising pathway for treatment of pain and depression and is increasingly being utilized in outpatient settings. Additionally, partial opioid-receptor agonists including methadone and suboxone have been reported to decrease pain in addition to their efficacy in addiction recovery. Medical marijuana is another area of growing interest, and while research has yet to show a clear effect in pain management, it does appear helpful in nausea and appetite stimulation. Obtaining a therapeutic response is the first treatment goal, after which a patient should be monitored in at least 6-month intervals to ensure sustained benefits and tolerability, and if these are not met, enhancement of treatment or a slow taper is indicated. As in all treatments, a positive patient-provider relationship predicts improved treatment adherence and outcomes.26 However, while these pharmacological interventions can reduce symptom severity, there is little evidence that they reduce traumatization without adjunctive psychotherapy.29
Summary
Both behavioral and pharmacological treatment options are available for chronic abdominal pain and most useful if traumatic manifestations are assessed and included as treatment targets. A multidisciplinary approach to the treatment of chronic abdominal pain with increased screening and treatment of trauma is a promising pathway to improved care and management for patients with chronic pain. If trauma is left untreated, the benefits of otherwise effective treatments are likely to be significantly limited.
References
1. Apkarian AV et al. Prog Neurobiol. 2009 Feb;87(2):81-97.
2. Gallagher RM et al. Pain Med. 2011 Jan;12(1):1-2.
3. Collier R et al. CMAJ. 2018 Jan 8;190(1):E26-7. doi: 10.1503/cmaj.109-5523.
4. Szigethy E et al. Nature Reviews Gastroenterology & Hepatology, 2018;15:168-80.
5. Ballou S et al. Clin Transl Gastroenterol. 2017 Jan;8(1):e214.
6. Egloff N et al. J Pain Res. 2013 Nov 5;6:765-70.
7. Fashler S et al. J Pain Res. 2016 Aug 10;9:551-61.
8. McKernan LC et al. Clin J Pain. 2019 May;35(5):385-93.
9. Ju T et al. J Clin Gastroenterol. 2018 Dec 19. doi: 10.1097/MCG.0000000000001153.
10. Fishbain DA et al. Pain Med. 2017 Apr 1;18(4):711-35.
11. Martin CR et al. Cell Mol Gastroenterol Hepatol. 2018;6(2):133-48.
12. Osadchiy V et al. Clin Gastroenterol Hepatol. 2019 Jan;17(2):322-32.
13. Brzozowski B et al. Curr Neuropharmacol. 2016 Nov;14(8):892-900.
14. Outclat SD et al. Pain Med. 2014;15(11):1872-9.
15. Asmundson GJ et al. Can J Psychiatry. 2002;Dec;47(10):930-7.
16. Taft TH et al. Inflamm Bowel Dis. 2019 Mar 7. doi: 10.1093/ibd/izz032.
17. Duckworth MP et al. International Journal of Rehabilitation and Health, 2000 Apr;5(2):129-39.
18. Scascighini L et al. Rheumatology (Oxford). 2008 May;47(5):670-8.
19. Palsson O et al. European Gastroenterology & Hepatology Review. 2010;6(1):42-6.
20. Watkins LE et al. Frontiers in Behavioral Neuroscience. 2018;12:1-9.
21. O’Toole SK et al. J Trauma Stress. 2016 Feb;29(1):97-100.
22. Goldblum Y et al. Digestive Disease Week. San Diego. 2019. Abstract in press.
23. American Psychiatric Association. Diagnostic and Statistical Manual (of Mental Disorders), Fifth Edition. Arlington, Va: American Psychiatric Publishing, 2013.
24. United States Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. 2018. Trauma-informed approach and trauma-specific interventions. Retrieved from samhsa.gov/nctic/trauma-interventions.
25. Click BH et al. Inflamm Bowel Dis. 2017;23(5):681-94.
26. Drossman DA et al. Gastroenterology. 2018 Mar;154(4):1140-71.
27. Thorkelson G et al. Inflamm Bowel Dis. 2016 Jun 1;22(6):1509-22.
28. Törnblom H et al. Current Gastroenterology Reports. 2018;20(12):58.
29. Watkins LE et al. Front Behav Neurosci. 2018;12:258.
30. American Psychiatric Association. Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults. 2017.
31. Bisson JI et al. Cochrane Database Syst Rev. 2013 Dec 13;(12):CD003388.
32. Department of Veterans Affairs and Department of Defense. VA/DOD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. 2017.
33. Karatzias T et al. Psychol Med. 2019 Mar 12:1-15. doi: 10.1017/S0033291719000436. Advance online publication.
Emily Weaver, LCSW, is a UPMC Total Care–IBD program senior social worker, Eva Szigethy, MD, PhD, is professor of psychiatry and medicine, codirector, IBD Total Care Medical Home, University of Pittsburgh Medical Center, departments of medicine and psychiatry.
Introduction
Abdominal pain is a complex phenomenon that involves unpleasant sensory and emotional experiences caused by actual or potential visceral tissue damage. As pain becomes chronic, there is a functional reorganization of the brain involved in emotional and cognitive processing leading to amplification of pain perception and associated pain suffering.1,2 With the rising recognition of the complexity of pain management in the 1960s, the treatment of pain became a recognized field of study, leading to the formation of interdisciplinary teams to treat pain. However, although efficacious, this model lacked adequate reimbursement structures and eventually subsided as opioids (which at the time were widely believed to be nonaddictive) become more prevalent.3 Not only is there a lack of empirical evidence for opioids in the management of chronic abdominal pain, there is a growing list of adverse consequences of prolonged opioid use for both the brain and gastrointestinal tract.4
Recently, there has been more clinical focus on behavioral interventions that can modulate gut pain signals and associated behaviors by reversing maladaptive emotional and cognitive brain processes.5 One such psychological process that has received little attention is the traumatizing nature of chronic abdominal pain. Chronic pain, particularly when it feels uncontrollable to patients, activates the brain’s fear circuitry and drives hyperarousal, emotional numbing, and consolidation of painful somatic memories, which become habitual and further amplify negative visceral signals.6,7 These processes are identical to the symptom manifestations of posttraumatic stress disorder (PTSD) such as intrusiveness, avoidance, negative mood and cognitions, and hyperarousal from life events. In fact, individuals with a history of other traumatizing exposures have an even higher risk of developing chronic pain disorders.8 This review has two objectives: to provide a theoretical framework for understanding chronic pain as a traumatizing experience with posttraumatic manifestations and to discuss behavioral interventions and adjunctive nonopioid pharmacotherapy embedded in multidisciplinary care models essential to reversing this negative brain-gut cycle and reducing pain-related suffering.
Trauma and chronic abdominal pain
Trauma is defined as an individual’s response to a threat to safety. Traumatized patients or those with PTSD are at higher risk for chronic abdominal pain.9 Given the strong neurobiological connection between the brain and gut that has been phylogenetically preserved, emotional (e.g., fear, terror) or physical (e.g., pain) signals represent danger, and with chronicity, there can be a kindling-related consolidation of these maladaptive neurobiological pathways leading to suffering (e.g., hopelessness, sense of failure) and disability (Figure 1).
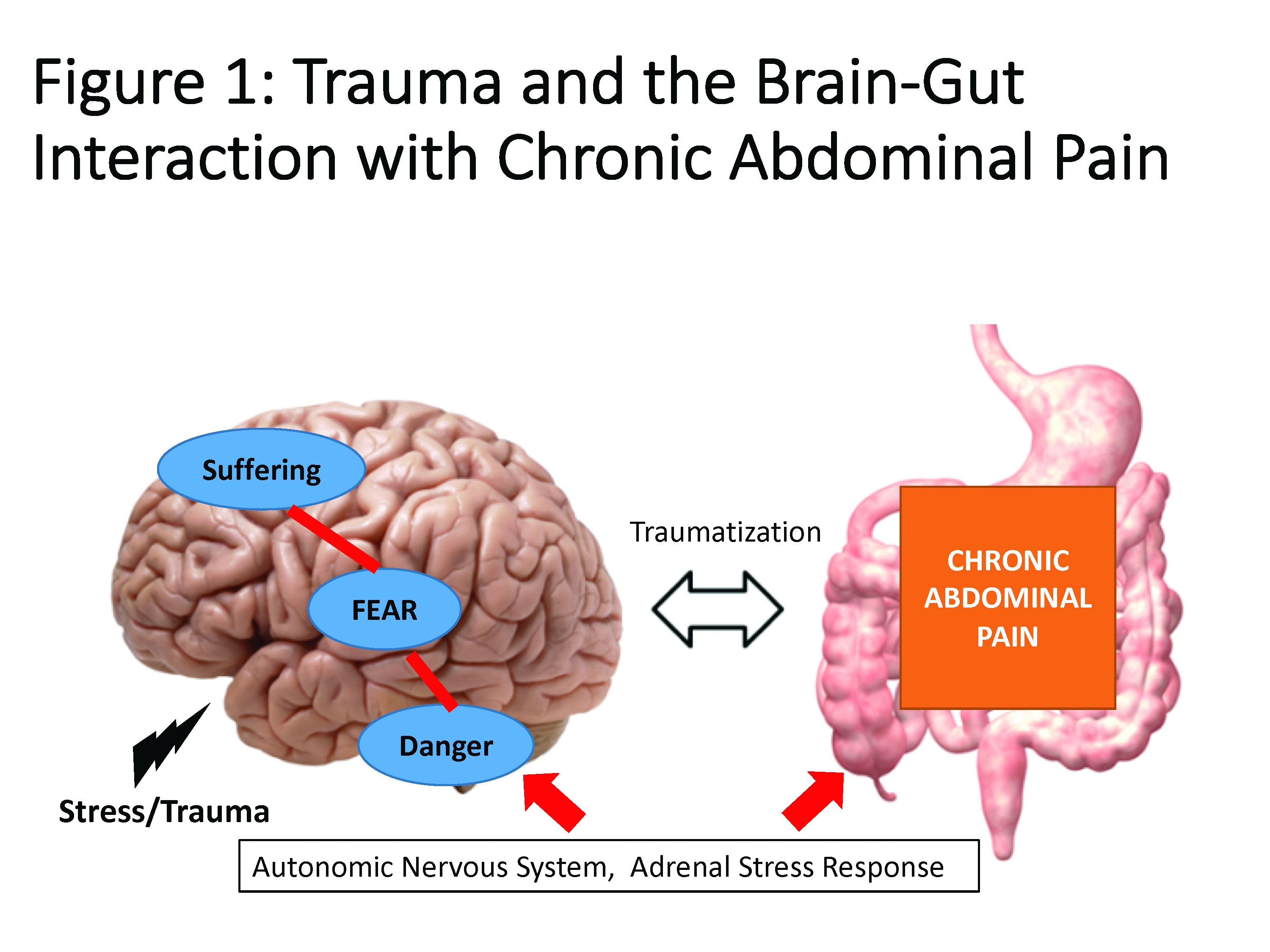
The interrelationship between chronic pain and trauma is multifaceted and is further complicated by the traumatizing nature of chronic pain itself, when pain is interpreted as a signal that the body is sick or even dangerously ill. Patients with chronic abdominal pain may seek multiple medical opinions and often undergo extensive, unnecessary, and sometimes harmful interventions to find the cause of their pain, with fear of disability and even death driving this search for answers.
The degree to which an individual with long-lasting pain interprets their discomfort as a risk to their well-being is related to the degree of trauma they experience because of their pain.10 Indeed, many of the negative symptoms associated with posttraumatic stress are also found in those with chronic abdominal pain. Trauma impacts the fear circuitry centers of the brain, leading to altered activation of the hypothalamic-pituitary-adrenal axis and the amygdala, as well as chronic activation of the sympathetic nervous system and stress-released hormones, all of which are potential pathways that dysregulate the brain-gut relationship.11-13 Worries for safety, which are reactivated by physiological cues (e.g., GI symptoms, pain), as well as avoidance of potential triggers of GI symptoms (e.g., food, exercise, medications, and situations such as travel or scheduled events, and fear of being trapped without bathroom access), are common. Traumatized individuals can experience a foreshortened sense of the future, which may lead to decreased investment in long-term determinants of health (e.g., balanced diet, exercise, social support) and have higher rates of functional impairment and higher health care utilization.14 Negative mood, including irritability, anxiety, depression, insomnia, and impaired concentration are common in those with trauma and chronic pain and can be accompanied by internalized blame (e.g., depression, substance abuse, suicidality) or externalized blame (e.g., negative relationships with health care providers, rejection from their support or faith system). These can be worsened by an impaired sense of trust, which impacts the patient-provider relationship and other sources of social support leading to lack of behavioral activation, anhedonia, and isolation.
Another commonality is hypervigilance, as those with chronic abdominal pain are often hyperaware of physical symptoms and always “on alert” for a signal indicative of a pain flare. Anxiety and depression frequently co-occur in populations with trauma and chronic pain; these diagnoses are associated with higher rates of catastrophizing and learned helplessness, which may be exacerbated by lack of a “cure” for functional gastrointestinal disorders (FGIDs) and chronic pain.15 These factors could potentially lead to lack of engagement with treatment or, alternatively, risky or destructive attempts to cure pain including dangerous complementary alternative treatments or substance abuse to numb sensations. Another feature of trauma in chronic pain is the sense of dissociation from and lack of control over the body, sometimes induced by negative medical experiences (e.g., unwanted physical examinations, medication side effects, traumatic procedures, or hospitalizations).16,17
The importance of treating trauma in the management of chronic pain
Behavioral treatment is increasingly being recognized as an essential component in the management of any chronic pain syndrome.18 The most studied psychosocial interventions for chronic abdominal pain are cognitive-behavioral therapy (CBT) and gut-focused hypnosis. CBT is usually a problem-focused, short-term intervention that can be delivered individually in the office, via group therapy, or through virtual platforms. CBT is most effective when cognitive distortions and ineffective behaviors create emotional distress, and the therapy targets patient’s stress reactivity, visceral anxiety, catastrophizing, and inflexible coping styles.5 Gut-focused hypnosis is the second most–studied behavioral treatment for chronic abdominal pain and utilizes the trance state to make positive suggestions leading to broad and lasting physiological and psychological improvement.19 In addition to pain management, both CBT and hypnosis are efficacious treatments for PTSD.20,21
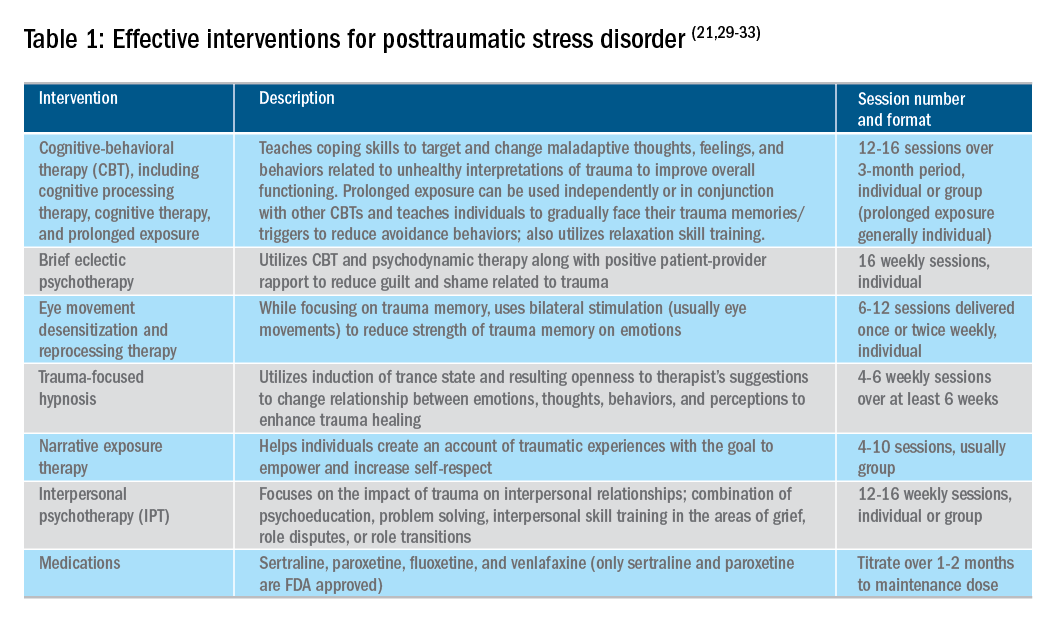
Utilizing a multidisciplinary medical team including integrated behavioral experts, such as in a patient-centered medical home, is considered the standard of care for treatment of chronic pain. The patient-provider relationship is essential, as is consistent follow-up to ensure effective symptom management and improvements in quality of life. Additionally, patient education, including a positive (i.e., clear) diagnosis and information on the brain-gut relationship, is associated with symptom improvement. In our subspecialty medical home for inflammatory bowel disease (IBD), we found that, in our patients who were on opioids for their chronic pain, engagement with our embedded behavioral and pain specialists resulted in significant reduction in opioid use and depression as well as improved self-reported quality of life.22 Gastroenterologists and advanced-practice providers operating without embedded behavioral therapists can consider referring patients to behavioral treatment (e.g., licensed clinical social workers, licensed professional counselors, marriage and family therapists, psychologists, and psychiatrists; the latter often specialize in medication management and may not offer behavioral therapy) for trauma if patients have undergone a traumatic event (e.g., exposure to any potentially life-threatening event, serious injury, or violence) at any point in their lifetime and are experiencing intrusive symptoms (e.g., memories, dreams, or flashbacks to trauma), avoidance of trauma reminders, and negative mood or hyperarousal related to traumatic events (Table 1).23
With the traumatization component of chronic abdominal pain, which can further drive maladaptive coping cycles, incorporation of trauma-informed treatment into gastroenterology clinics is an avenue toward more effective treatment. The core principles of trauma-informed care include safety, choice, collaboration, trustworthiness, and empowerment,24 and are easily aligned with patient-centered models of care such as the interdisciplinary medical home model. Incorporation of screening techniques, interdisciplinary training of clinicians, and use of behavioral providers with experience in evidenced-based treatments of trauma enhance a clinic’s ability to effectively identify and treat individuals who have trauma because of their abdominal pain.25 Additionally, the most common behavioral interventions for functional gastrointestinal disorders (FGIDs) are also efficacious in the treatment of trauma. CBT is a well-validated treatment for PTSD that utilizes exposure therapy to help individuals restructure negative beliefs shaped by their negative experience and develop relaxation skills. Hypnosis is also validated in the treatment of trauma, with the possible mechanism of action being the replacement of the negative or dissociated traumatic trance with a healthy, adaptive trance facilitated by the hypnotherapist.21
Adjunctive nonopioid medications for chronic abdominal pain
While there are few randomized controlled trials establishing efficacy of pharmacotherapy for sustained improvement of abdominal pain or related suffering, several small trials and consensus clinical expert opinion suggest partial improvement in these domains.26,27 Central neuromodulators that can attenuate chronic visceral pain include antidepressants, antipsychotics, and other central nervous system–targeted medications.26 Tricyclic antidepressants (e.g., amitriptyline, nortriptyline, imipramine, desipramine) are often first-line treatment for FGIDs.28 Serotonin noradrenergic reuptake inhibitors (e.g., duloxetine, venlafaxine, desvenlafaxine, milnacipran) are also effective in pain management. Selective serotonin reuptake inhibitors (e.g., paroxetine, fluoxetine, sertraline, citalopram, escitalopram) can be used, especially when comorbid depression, anxiety, and phobic disorders are present. Tetracyclic antidepressants (e.g., mirtazapine, mianserin, trazodone) are effective treatments for early satiety, nausea/vomiting, insomnia, and low weight. Augmenting agents are utilized when single agents do not provide maximum benefit, including quetiapine (disturbed sleep), bupropion (fatigue), aripiprazole, buspirone, and tandospirone (dyspeptic features and anxiety). Delta ligands including gabapentin and pregabalin are helpful for abdominal wall pain or fibromyalgia. Ketamine is a newer but promising pathway for treatment of pain and depression and is increasingly being utilized in outpatient settings. Additionally, partial opioid-receptor agonists including methadone and suboxone have been reported to decrease pain in addition to their efficacy in addiction recovery. Medical marijuana is another area of growing interest, and while research has yet to show a clear effect in pain management, it does appear helpful in nausea and appetite stimulation. Obtaining a therapeutic response is the first treatment goal, after which a patient should be monitored in at least 6-month intervals to ensure sustained benefits and tolerability, and if these are not met, enhancement of treatment or a slow taper is indicated. As in all treatments, a positive patient-provider relationship predicts improved treatment adherence and outcomes.26 However, while these pharmacological interventions can reduce symptom severity, there is little evidence that they reduce traumatization without adjunctive psychotherapy.29
Summary
Both behavioral and pharmacological treatment options are available for chronic abdominal pain and most useful if traumatic manifestations are assessed and included as treatment targets. A multidisciplinary approach to the treatment of chronic abdominal pain with increased screening and treatment of trauma is a promising pathway to improved care and management for patients with chronic pain. If trauma is left untreated, the benefits of otherwise effective treatments are likely to be significantly limited.
References
1. Apkarian AV et al. Prog Neurobiol. 2009 Feb;87(2):81-97.
2. Gallagher RM et al. Pain Med. 2011 Jan;12(1):1-2.
3. Collier R et al. CMAJ. 2018 Jan 8;190(1):E26-7. doi: 10.1503/cmaj.109-5523.
4. Szigethy E et al. Nature Reviews Gastroenterology & Hepatology, 2018;15:168-80.
5. Ballou S et al. Clin Transl Gastroenterol. 2017 Jan;8(1):e214.
6. Egloff N et al. J Pain Res. 2013 Nov 5;6:765-70.
7. Fashler S et al. J Pain Res. 2016 Aug 10;9:551-61.
8. McKernan LC et al. Clin J Pain. 2019 May;35(5):385-93.
9. Ju T et al. J Clin Gastroenterol. 2018 Dec 19. doi: 10.1097/MCG.0000000000001153.
10. Fishbain DA et al. Pain Med. 2017 Apr 1;18(4):711-35.
11. Martin CR et al. Cell Mol Gastroenterol Hepatol. 2018;6(2):133-48.
12. Osadchiy V et al. Clin Gastroenterol Hepatol. 2019 Jan;17(2):322-32.
13. Brzozowski B et al. Curr Neuropharmacol. 2016 Nov;14(8):892-900.
14. Outclat SD et al. Pain Med. 2014;15(11):1872-9.
15. Asmundson GJ et al. Can J Psychiatry. 2002;Dec;47(10):930-7.
16. Taft TH et al. Inflamm Bowel Dis. 2019 Mar 7. doi: 10.1093/ibd/izz032.
17. Duckworth MP et al. International Journal of Rehabilitation and Health, 2000 Apr;5(2):129-39.
18. Scascighini L et al. Rheumatology (Oxford). 2008 May;47(5):670-8.
19. Palsson O et al. European Gastroenterology & Hepatology Review. 2010;6(1):42-6.
20. Watkins LE et al. Frontiers in Behavioral Neuroscience. 2018;12:1-9.
21. O’Toole SK et al. J Trauma Stress. 2016 Feb;29(1):97-100.
22. Goldblum Y et al. Digestive Disease Week. San Diego. 2019. Abstract in press.
23. American Psychiatric Association. Diagnostic and Statistical Manual (of Mental Disorders), Fifth Edition. Arlington, Va: American Psychiatric Publishing, 2013.
24. United States Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. 2018. Trauma-informed approach and trauma-specific interventions. Retrieved from samhsa.gov/nctic/trauma-interventions.
25. Click BH et al. Inflamm Bowel Dis. 2017;23(5):681-94.
26. Drossman DA et al. Gastroenterology. 2018 Mar;154(4):1140-71.
27. Thorkelson G et al. Inflamm Bowel Dis. 2016 Jun 1;22(6):1509-22.
28. Törnblom H et al. Current Gastroenterology Reports. 2018;20(12):58.
29. Watkins LE et al. Front Behav Neurosci. 2018;12:258.
30. American Psychiatric Association. Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults. 2017.
31. Bisson JI et al. Cochrane Database Syst Rev. 2013 Dec 13;(12):CD003388.
32. Department of Veterans Affairs and Department of Defense. VA/DOD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. 2017.
33. Karatzias T et al. Psychol Med. 2019 Mar 12:1-15. doi: 10.1017/S0033291719000436. Advance online publication.
Emily Weaver, LCSW, is a UPMC Total Care–IBD program senior social worker, Eva Szigethy, MD, PhD, is professor of psychiatry and medicine, codirector, IBD Total Care Medical Home, University of Pittsburgh Medical Center, departments of medicine and psychiatry.
Introduction
Abdominal pain is a complex phenomenon that involves unpleasant sensory and emotional experiences caused by actual or potential visceral tissue damage. As pain becomes chronic, there is a functional reorganization of the brain involved in emotional and cognitive processing leading to amplification of pain perception and associated pain suffering.1,2 With the rising recognition of the complexity of pain management in the 1960s, the treatment of pain became a recognized field of study, leading to the formation of interdisciplinary teams to treat pain. However, although efficacious, this model lacked adequate reimbursement structures and eventually subsided as opioids (which at the time were widely believed to be nonaddictive) become more prevalent.3 Not only is there a lack of empirical evidence for opioids in the management of chronic abdominal pain, there is a growing list of adverse consequences of prolonged opioid use for both the brain and gastrointestinal tract.4
Recently, there has been more clinical focus on behavioral interventions that can modulate gut pain signals and associated behaviors by reversing maladaptive emotional and cognitive brain processes.5 One such psychological process that has received little attention is the traumatizing nature of chronic abdominal pain. Chronic pain, particularly when it feels uncontrollable to patients, activates the brain’s fear circuitry and drives hyperarousal, emotional numbing, and consolidation of painful somatic memories, which become habitual and further amplify negative visceral signals.6,7 These processes are identical to the symptom manifestations of posttraumatic stress disorder (PTSD) such as intrusiveness, avoidance, negative mood and cognitions, and hyperarousal from life events. In fact, individuals with a history of other traumatizing exposures have an even higher risk of developing chronic pain disorders.8 This review has two objectives: to provide a theoretical framework for understanding chronic pain as a traumatizing experience with posttraumatic manifestations and to discuss behavioral interventions and adjunctive nonopioid pharmacotherapy embedded in multidisciplinary care models essential to reversing this negative brain-gut cycle and reducing pain-related suffering.
Trauma and chronic abdominal pain
Trauma is defined as an individual’s response to a threat to safety. Traumatized patients or those with PTSD are at higher risk for chronic abdominal pain.9 Given the strong neurobiological connection between the brain and gut that has been phylogenetically preserved, emotional (e.g., fear, terror) or physical (e.g., pain) signals represent danger, and with chronicity, there can be a kindling-related consolidation of these maladaptive neurobiological pathways leading to suffering (e.g., hopelessness, sense of failure) and disability (Figure 1).
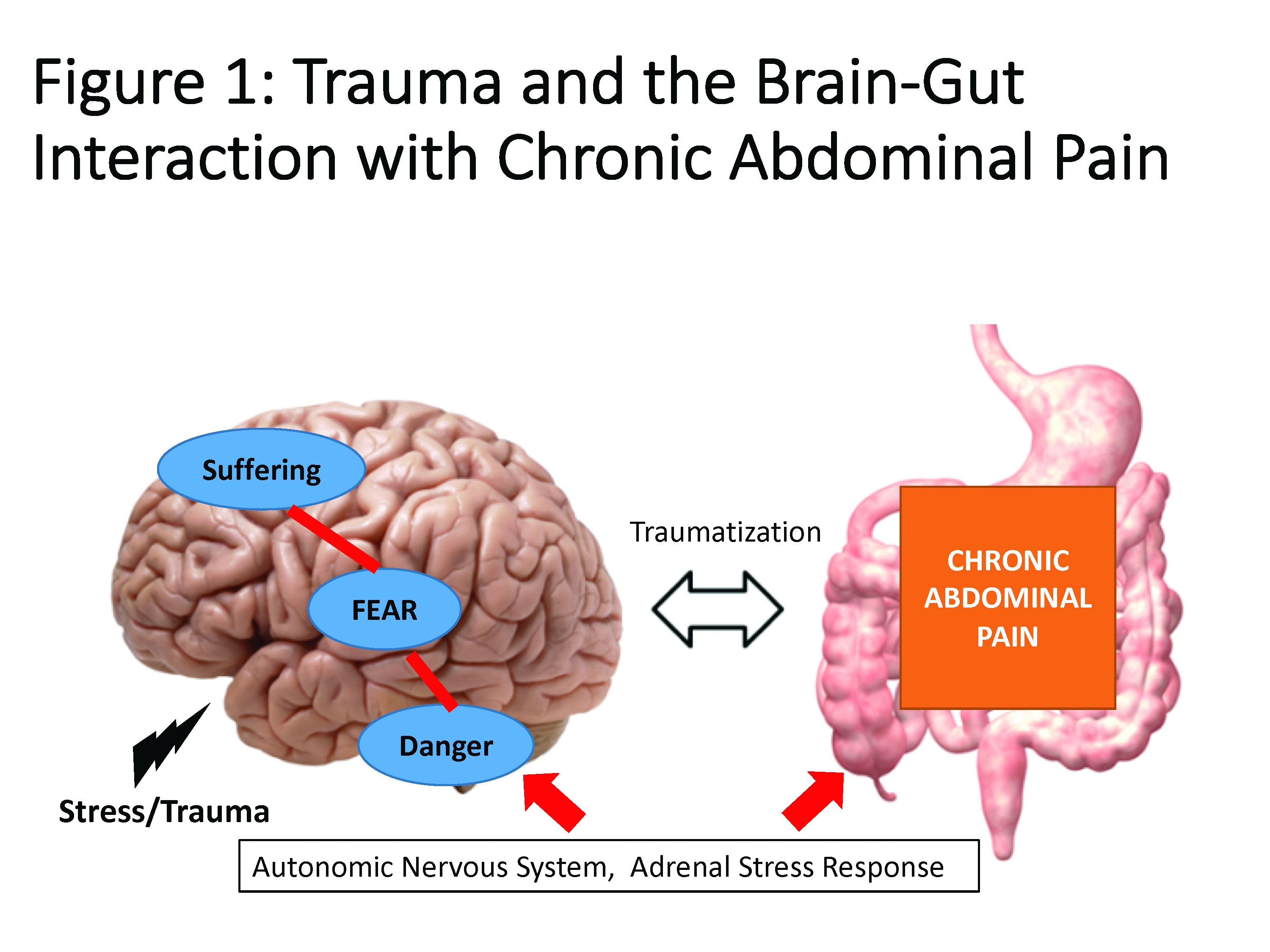
The interrelationship between chronic pain and trauma is multifaceted and is further complicated by the traumatizing nature of chronic pain itself, when pain is interpreted as a signal that the body is sick or even dangerously ill. Patients with chronic abdominal pain may seek multiple medical opinions and often undergo extensive, unnecessary, and sometimes harmful interventions to find the cause of their pain, with fear of disability and even death driving this search for answers.
The degree to which an individual with long-lasting pain interprets their discomfort as a risk to their well-being is related to the degree of trauma they experience because of their pain.10 Indeed, many of the negative symptoms associated with posttraumatic stress are also found in those with chronic abdominal pain. Trauma impacts the fear circuitry centers of the brain, leading to altered activation of the hypothalamic-pituitary-adrenal axis and the amygdala, as well as chronic activation of the sympathetic nervous system and stress-released hormones, all of which are potential pathways that dysregulate the brain-gut relationship.11-13 Worries for safety, which are reactivated by physiological cues (e.g., GI symptoms, pain), as well as avoidance of potential triggers of GI symptoms (e.g., food, exercise, medications, and situations such as travel or scheduled events, and fear of being trapped without bathroom access), are common. Traumatized individuals can experience a foreshortened sense of the future, which may lead to decreased investment in long-term determinants of health (e.g., balanced diet, exercise, social support) and have higher rates of functional impairment and higher health care utilization.14 Negative mood, including irritability, anxiety, depression, insomnia, and impaired concentration are common in those with trauma and chronic pain and can be accompanied by internalized blame (e.g., depression, substance abuse, suicidality) or externalized blame (e.g., negative relationships with health care providers, rejection from their support or faith system). These can be worsened by an impaired sense of trust, which impacts the patient-provider relationship and other sources of social support leading to lack of behavioral activation, anhedonia, and isolation.
Another commonality is hypervigilance, as those with chronic abdominal pain are often hyperaware of physical symptoms and always “on alert” for a signal indicative of a pain flare. Anxiety and depression frequently co-occur in populations with trauma and chronic pain; these diagnoses are associated with higher rates of catastrophizing and learned helplessness, which may be exacerbated by lack of a “cure” for functional gastrointestinal disorders (FGIDs) and chronic pain.15 These factors could potentially lead to lack of engagement with treatment or, alternatively, risky or destructive attempts to cure pain including dangerous complementary alternative treatments or substance abuse to numb sensations. Another feature of trauma in chronic pain is the sense of dissociation from and lack of control over the body, sometimes induced by negative medical experiences (e.g., unwanted physical examinations, medication side effects, traumatic procedures, or hospitalizations).16,17
The importance of treating trauma in the management of chronic pain
Behavioral treatment is increasingly being recognized as an essential component in the management of any chronic pain syndrome.18 The most studied psychosocial interventions for chronic abdominal pain are cognitive-behavioral therapy (CBT) and gut-focused hypnosis. CBT is usually a problem-focused, short-term intervention that can be delivered individually in the office, via group therapy, or through virtual platforms. CBT is most effective when cognitive distortions and ineffective behaviors create emotional distress, and the therapy targets patient’s stress reactivity, visceral anxiety, catastrophizing, and inflexible coping styles.5 Gut-focused hypnosis is the second most–studied behavioral treatment for chronic abdominal pain and utilizes the trance state to make positive suggestions leading to broad and lasting physiological and psychological improvement.19 In addition to pain management, both CBT and hypnosis are efficacious treatments for PTSD.20,21
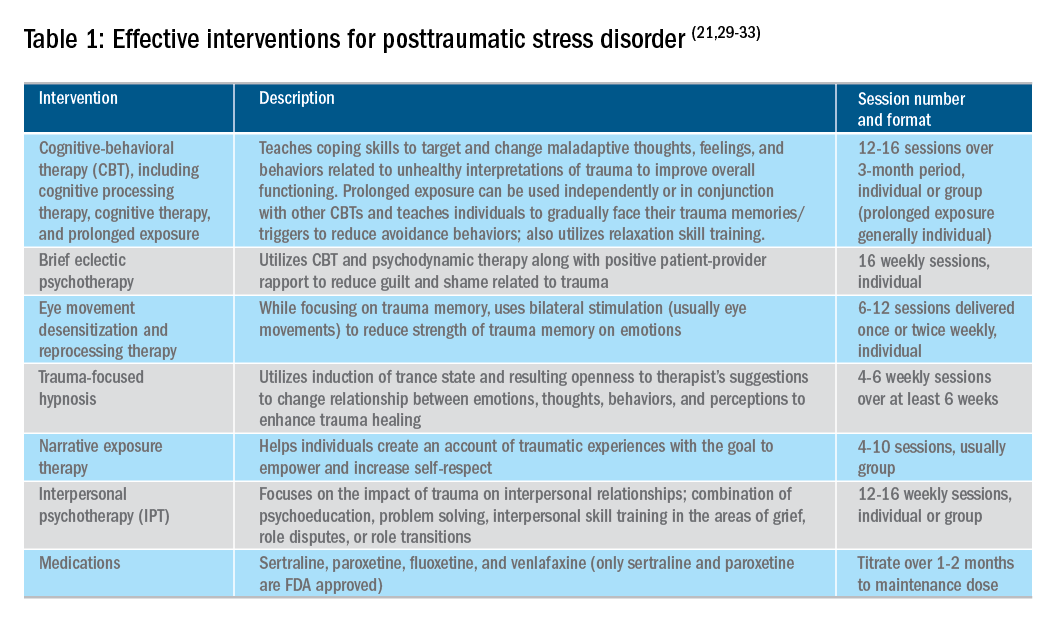
Utilizing a multidisciplinary medical team including integrated behavioral experts, such as in a patient-centered medical home, is considered the standard of care for treatment of chronic pain. The patient-provider relationship is essential, as is consistent follow-up to ensure effective symptom management and improvements in quality of life. Additionally, patient education, including a positive (i.e., clear) diagnosis and information on the brain-gut relationship, is associated with symptom improvement. In our subspecialty medical home for inflammatory bowel disease (IBD), we found that, in our patients who were on opioids for their chronic pain, engagement with our embedded behavioral and pain specialists resulted in significant reduction in opioid use and depression as well as improved self-reported quality of life.22 Gastroenterologists and advanced-practice providers operating without embedded behavioral therapists can consider referring patients to behavioral treatment (e.g., licensed clinical social workers, licensed professional counselors, marriage and family therapists, psychologists, and psychiatrists; the latter often specialize in medication management and may not offer behavioral therapy) for trauma if patients have undergone a traumatic event (e.g., exposure to any potentially life-threatening event, serious injury, or violence) at any point in their lifetime and are experiencing intrusive symptoms (e.g., memories, dreams, or flashbacks to trauma), avoidance of trauma reminders, and negative mood or hyperarousal related to traumatic events (Table 1).23
With the traumatization component of chronic abdominal pain, which can further drive maladaptive coping cycles, incorporation of trauma-informed treatment into gastroenterology clinics is an avenue toward more effective treatment. The core principles of trauma-informed care include safety, choice, collaboration, trustworthiness, and empowerment,24 and are easily aligned with patient-centered models of care such as the interdisciplinary medical home model. Incorporation of screening techniques, interdisciplinary training of clinicians, and use of behavioral providers with experience in evidenced-based treatments of trauma enhance a clinic’s ability to effectively identify and treat individuals who have trauma because of their abdominal pain.25 Additionally, the most common behavioral interventions for functional gastrointestinal disorders (FGIDs) are also efficacious in the treatment of trauma. CBT is a well-validated treatment for PTSD that utilizes exposure therapy to help individuals restructure negative beliefs shaped by their negative experience and develop relaxation skills. Hypnosis is also validated in the treatment of trauma, with the possible mechanism of action being the replacement of the negative or dissociated traumatic trance with a healthy, adaptive trance facilitated by the hypnotherapist.21
Adjunctive nonopioid medications for chronic abdominal pain
While there are few randomized controlled trials establishing efficacy of pharmacotherapy for sustained improvement of abdominal pain or related suffering, several small trials and consensus clinical expert opinion suggest partial improvement in these domains.26,27 Central neuromodulators that can attenuate chronic visceral pain include antidepressants, antipsychotics, and other central nervous system–targeted medications.26 Tricyclic antidepressants (e.g., amitriptyline, nortriptyline, imipramine, desipramine) are often first-line treatment for FGIDs.28 Serotonin noradrenergic reuptake inhibitors (e.g., duloxetine, venlafaxine, desvenlafaxine, milnacipran) are also effective in pain management. Selective serotonin reuptake inhibitors (e.g., paroxetine, fluoxetine, sertraline, citalopram, escitalopram) can be used, especially when comorbid depression, anxiety, and phobic disorders are present. Tetracyclic antidepressants (e.g., mirtazapine, mianserin, trazodone) are effective treatments for early satiety, nausea/vomiting, insomnia, and low weight. Augmenting agents are utilized when single agents do not provide maximum benefit, including quetiapine (disturbed sleep), bupropion (fatigue), aripiprazole, buspirone, and tandospirone (dyspeptic features and anxiety). Delta ligands including gabapentin and pregabalin are helpful for abdominal wall pain or fibromyalgia. Ketamine is a newer but promising pathway for treatment of pain and depression and is increasingly being utilized in outpatient settings. Additionally, partial opioid-receptor agonists including methadone and suboxone have been reported to decrease pain in addition to their efficacy in addiction recovery. Medical marijuana is another area of growing interest, and while research has yet to show a clear effect in pain management, it does appear helpful in nausea and appetite stimulation. Obtaining a therapeutic response is the first treatment goal, after which a patient should be monitored in at least 6-month intervals to ensure sustained benefits and tolerability, and if these are not met, enhancement of treatment or a slow taper is indicated. As in all treatments, a positive patient-provider relationship predicts improved treatment adherence and outcomes.26 However, while these pharmacological interventions can reduce symptom severity, there is little evidence that they reduce traumatization without adjunctive psychotherapy.29
Summary
Both behavioral and pharmacological treatment options are available for chronic abdominal pain and most useful if traumatic manifestations are assessed and included as treatment targets. A multidisciplinary approach to the treatment of chronic abdominal pain with increased screening and treatment of trauma is a promising pathway to improved care and management for patients with chronic pain. If trauma is left untreated, the benefits of otherwise effective treatments are likely to be significantly limited.
References
1. Apkarian AV et al. Prog Neurobiol. 2009 Feb;87(2):81-97.
2. Gallagher RM et al. Pain Med. 2011 Jan;12(1):1-2.
3. Collier R et al. CMAJ. 2018 Jan 8;190(1):E26-7. doi: 10.1503/cmaj.109-5523.
4. Szigethy E et al. Nature Reviews Gastroenterology & Hepatology, 2018;15:168-80.
5. Ballou S et al. Clin Transl Gastroenterol. 2017 Jan;8(1):e214.
6. Egloff N et al. J Pain Res. 2013 Nov 5;6:765-70.
7. Fashler S et al. J Pain Res. 2016 Aug 10;9:551-61.
8. McKernan LC et al. Clin J Pain. 2019 May;35(5):385-93.
9. Ju T et al. J Clin Gastroenterol. 2018 Dec 19. doi: 10.1097/MCG.0000000000001153.
10. Fishbain DA et al. Pain Med. 2017 Apr 1;18(4):711-35.
11. Martin CR et al. Cell Mol Gastroenterol Hepatol. 2018;6(2):133-48.
12. Osadchiy V et al. Clin Gastroenterol Hepatol. 2019 Jan;17(2):322-32.
13. Brzozowski B et al. Curr Neuropharmacol. 2016 Nov;14(8):892-900.
14. Outclat SD et al. Pain Med. 2014;15(11):1872-9.
15. Asmundson GJ et al. Can J Psychiatry. 2002;Dec;47(10):930-7.
16. Taft TH et al. Inflamm Bowel Dis. 2019 Mar 7. doi: 10.1093/ibd/izz032.
17. Duckworth MP et al. International Journal of Rehabilitation and Health, 2000 Apr;5(2):129-39.
18. Scascighini L et al. Rheumatology (Oxford). 2008 May;47(5):670-8.
19. Palsson O et al. European Gastroenterology & Hepatology Review. 2010;6(1):42-6.
20. Watkins LE et al. Frontiers in Behavioral Neuroscience. 2018;12:1-9.
21. O’Toole SK et al. J Trauma Stress. 2016 Feb;29(1):97-100.
22. Goldblum Y et al. Digestive Disease Week. San Diego. 2019. Abstract in press.
23. American Psychiatric Association. Diagnostic and Statistical Manual (of Mental Disorders), Fifth Edition. Arlington, Va: American Psychiatric Publishing, 2013.
24. United States Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. 2018. Trauma-informed approach and trauma-specific interventions. Retrieved from samhsa.gov/nctic/trauma-interventions.
25. Click BH et al. Inflamm Bowel Dis. 2017;23(5):681-94.
26. Drossman DA et al. Gastroenterology. 2018 Mar;154(4):1140-71.
27. Thorkelson G et al. Inflamm Bowel Dis. 2016 Jun 1;22(6):1509-22.
28. Törnblom H et al. Current Gastroenterology Reports. 2018;20(12):58.
29. Watkins LE et al. Front Behav Neurosci. 2018;12:258.
30. American Psychiatric Association. Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults. 2017.
31. Bisson JI et al. Cochrane Database Syst Rev. 2013 Dec 13;(12):CD003388.
32. Department of Veterans Affairs and Department of Defense. VA/DOD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. 2017.
33. Karatzias T et al. Psychol Med. 2019 Mar 12:1-15. doi: 10.1017/S0033291719000436. Advance online publication.
Emily Weaver, LCSW, is a UPMC Total Care–IBD program senior social worker, Eva Szigethy, MD, PhD, is professor of psychiatry and medicine, codirector, IBD Total Care Medical Home, University of Pittsburgh Medical Center, departments of medicine and psychiatry.