User login
Ten negotiation tenets to follow
Who’s going to negotiate your contract: you or a professional? Lawyer Scott Roman – at a recent AGA Regional Practice Skills Workshop – explained that answering this question early on can help ensure you maximize your contract benefits. His advice for any negotiation is keep to the following in mind:
- Prepare, prepare, prepare. Employers know when you’re winging it.
- Gain leverage. The more offers you have, the more leverage.
- Give yourself adequate time to negotiate.
- Establish your objectives and anticipate objectives of the employer.
- Determine the best case, worst case, and most likely scenario before you start negotiating.
- Try to define nonnegotiable issues.
- Try to get something each time you give something.
- Don’t negotiate against yourself.
- Keep cool and remember that these are people you may have to work with.
- Be flexible.
View the full presentation (login required), which also covers hot topics in negotiating your contract – more than 1-year base salary, bonuses, student loan repayment.
Visit www.gastro.org/education to see all on-demand education designed specifically for trainees and early career GIs.
Who’s going to negotiate your contract: you or a professional? Lawyer Scott Roman – at a recent AGA Regional Practice Skills Workshop – explained that answering this question early on can help ensure you maximize your contract benefits. His advice for any negotiation is keep to the following in mind:
- Prepare, prepare, prepare. Employers know when you’re winging it.
- Gain leverage. The more offers you have, the more leverage.
- Give yourself adequate time to negotiate.
- Establish your objectives and anticipate objectives of the employer.
- Determine the best case, worst case, and most likely scenario before you start negotiating.
- Try to define nonnegotiable issues.
- Try to get something each time you give something.
- Don’t negotiate against yourself.
- Keep cool and remember that these are people you may have to work with.
- Be flexible.
View the full presentation (login required), which also covers hot topics in negotiating your contract – more than 1-year base salary, bonuses, student loan repayment.
Visit www.gastro.org/education to see all on-demand education designed specifically for trainees and early career GIs.
Who’s going to negotiate your contract: you or a professional? Lawyer Scott Roman – at a recent AGA Regional Practice Skills Workshop – explained that answering this question early on can help ensure you maximize your contract benefits. His advice for any negotiation is keep to the following in mind:
- Prepare, prepare, prepare. Employers know when you’re winging it.
- Gain leverage. The more offers you have, the more leverage.
- Give yourself adequate time to negotiate.
- Establish your objectives and anticipate objectives of the employer.
- Determine the best case, worst case, and most likely scenario before you start negotiating.
- Try to define nonnegotiable issues.
- Try to get something each time you give something.
- Don’t negotiate against yourself.
- Keep cool and remember that these are people you may have to work with.
- Be flexible.
View the full presentation (login required), which also covers hot topics in negotiating your contract – more than 1-year base salary, bonuses, student loan repayment.
Visit www.gastro.org/education to see all on-demand education designed specifically for trainees and early career GIs.
What does burnout cost?
How are you feeling today? Simple words but a bit of introspection can go a long way. P It affects a physician’s well-being, effectiveness, productivity, and the ability to provide quality care. It also carries personal consequences for physicians including broken relationships, substance abuse, suicide, and depression.
Burnout may affect at least one-third of gastroenterologists. At greater risk are younger physicians, physicians performing high-risk procedures, and physicians experiencing work-life conflicts.
While the root cause of physician burnout varies from provider to provider, an overarching theme is work stress. Work stress may develop for a number of reasons, including issues at the level of the health care system (shifts in reimbursement or payment models, increasing clerical burden of the electronic medical record), organizational issues (e.g., dysfunctional administration, system-wide communication issues), and personal issues.
The key to preventing burnout is to first recognize that it can happen. Because initial symptoms build up internally, it can be easy to overlook. These seven steps can help you prevent burnout:
- Be self-aware and stay vigilant.
- Take care of yourself first.
- Stay connected to family, friends, and coworkers.
- Exercise.
- Ensure adequate sleep.
- Use your vacation time and ensure you disconnect yourself from work.
- Learn to say no.
A case study published in Clinical Gastroenterology and Hepatology delves deeper into how burnout develops, why it matters, and provides pathways to successfully combat it.
How are you feeling today? Simple words but a bit of introspection can go a long way. P It affects a physician’s well-being, effectiveness, productivity, and the ability to provide quality care. It also carries personal consequences for physicians including broken relationships, substance abuse, suicide, and depression.
Burnout may affect at least one-third of gastroenterologists. At greater risk are younger physicians, physicians performing high-risk procedures, and physicians experiencing work-life conflicts.
While the root cause of physician burnout varies from provider to provider, an overarching theme is work stress. Work stress may develop for a number of reasons, including issues at the level of the health care system (shifts in reimbursement or payment models, increasing clerical burden of the electronic medical record), organizational issues (e.g., dysfunctional administration, system-wide communication issues), and personal issues.
The key to preventing burnout is to first recognize that it can happen. Because initial symptoms build up internally, it can be easy to overlook. These seven steps can help you prevent burnout:
- Be self-aware and stay vigilant.
- Take care of yourself first.
- Stay connected to family, friends, and coworkers.
- Exercise.
- Ensure adequate sleep.
- Use your vacation time and ensure you disconnect yourself from work.
- Learn to say no.
A case study published in Clinical Gastroenterology and Hepatology delves deeper into how burnout develops, why it matters, and provides pathways to successfully combat it.
How are you feeling today? Simple words but a bit of introspection can go a long way. P It affects a physician’s well-being, effectiveness, productivity, and the ability to provide quality care. It also carries personal consequences for physicians including broken relationships, substance abuse, suicide, and depression.
Burnout may affect at least one-third of gastroenterologists. At greater risk are younger physicians, physicians performing high-risk procedures, and physicians experiencing work-life conflicts.
While the root cause of physician burnout varies from provider to provider, an overarching theme is work stress. Work stress may develop for a number of reasons, including issues at the level of the health care system (shifts in reimbursement or payment models, increasing clerical burden of the electronic medical record), organizational issues (e.g., dysfunctional administration, system-wide communication issues), and personal issues.
The key to preventing burnout is to first recognize that it can happen. Because initial symptoms build up internally, it can be easy to overlook. These seven steps can help you prevent burnout:
- Be self-aware and stay vigilant.
- Take care of yourself first.
- Stay connected to family, friends, and coworkers.
- Exercise.
- Ensure adequate sleep.
- Use your vacation time and ensure you disconnect yourself from work.
- Learn to say no.
A case study published in Clinical Gastroenterology and Hepatology delves deeper into how burnout develops, why it matters, and provides pathways to successfully combat it.
Sessions at DDW® 2018 designed for trainees and early career GIs
Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
With the exception of the AGA Postgraduate Course, all of the sessions are free, but you must register for DDW to attend. Registration is open and is complimentary for AGA member trainees, students, medical residents, and postdoctoral fellows until April 18. Visit the AGA website for additional details about these sessions.
Saturday, June 2, and Sunday, June 3
- Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
Sunday, June 3, 4-5:30 p.m.
- Advancing Clinical Practice: GI Fellow-Directed Quality Improvement Projects
Monday, June 4, 4-5:30 p.m.
- Board Review Course
Tuesday, June 5, 1:30-5:30 p.m.
Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
With the exception of the AGA Postgraduate Course, all of the sessions are free, but you must register for DDW to attend. Registration is open and is complimentary for AGA member trainees, students, medical residents, and postdoctoral fellows until April 18. Visit the AGA website for additional details about these sessions.
Saturday, June 2, and Sunday, June 3
- Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
Sunday, June 3, 4-5:30 p.m.
- Advancing Clinical Practice: GI Fellow-Directed Quality Improvement Projects
Monday, June 4, 4-5:30 p.m.
- Board Review Course
Tuesday, June 5, 1:30-5:30 p.m.
Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
With the exception of the AGA Postgraduate Course, all of the sessions are free, but you must register for DDW to attend. Registration is open and is complimentary for AGA member trainees, students, medical residents, and postdoctoral fellows until April 18. Visit the AGA website for additional details about these sessions.
Saturday, June 2, and Sunday, June 3
- Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
Sunday, June 3, 4-5:30 p.m.
- Advancing Clinical Practice: GI Fellow-Directed Quality Improvement Projects
Monday, June 4, 4-5:30 p.m.
- Board Review Course
Tuesday, June 5, 1:30-5:30 p.m.
Making the most of your DDW experience
It’s that time of the year again: Digestive Disease Week (DDW®)! This event evolved out of the AGA annual meetings and was first advertised as DDW in the January 1969 issue of Gastroenterology.1 Since that time, it has grown into a truly international event with over 14,000 attendees, 41% of whom attend from abroad.2
DDW is a collaborative event that is jointly sponsored by four professional GI/hepatology-related societies – the AGA, the American Association for the Study of Liver Diseases, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract. The conference topics cover the gamut of GI and hepatology conditions and participants represent all types of professional settings, including private practice (37%), hospitals (33%), and academic medical centers (28%).2 Whether you’re a first-time attendee or a seasoned participant, DDW offers something for everyone.
Plan ahead
Is there a new treatment or condition you’ve wanted to learn more about? Are you interested in testing the latest endoscopic devices or learning a new procedural technique? Experts from around the world come to DDW to showcase the latest developments in GI. However, with over 5,000 abstracts and lectures and almost 300 exhibition booths, it’s easy to feel overwhelmed by all the offerings. To make the most of your experience, plan ahead.
In the months prior to the conference, visit the DDW website to download the Preliminary Program. Pick out your can’t-miss lectures and events, and put them on your calendar right away. As DDW approaches, invitations from colleagues, societies, and industry grow, so preplanning is a necessity.
Approximately 1 month before DDW, the DDW Mobile App will become available for free download in the Apple and Google Play stores. You can highlight events of interest and place them on a personalized calendar. Allow for push notifications to get the latest updates and schedule changes throughout the event. In addition, the in-app maps of the venue are a fantastic way to locate where scheduled events will take place. Try to attend talks that are located close to one another. The conference center is expansive and you may miss your intended presentations by trying to catch overlapping sessions situated far from each other. If you prefer planning on a desktop or laptop, use the DDW Online Planner (available mid-April) to create your schedule. The information can then be synced to your mobile device through the app.
Upon arrival, be sure to pick up your attendee conference bag. Before recycling the contents, look for any product theaters, satellite symposia, exhibitor booths, or other advertised activities you may want to add to your schedule.
Practical tips
a) Register ahead of time and pick up your conference bag during off-hours to avoid long lines.
b) Book your hotel early. Most have generous cancellation policies. Registration is required before booking housing.
c) Pack comfortable shoes and dress in layers to accommodate both unpredictable weather and indoor climate control.
Make new connections and nurture old ones
Is your professional hero giving a talk? Are you looking to land your first job or make a move? Do you need some face time with a mentor outside your institution? DDW is a wonderful opportunity to connect with advisers and possible employers as well as potential and established collaborators. Schedules fill up quickly though, so try your best to email requests for meetings well ahead of time. The app also has a messaging feature you can use to communicate with other attendees.
At the meeting, be an active participant and ask questions. One of the greatest benefits of attending the conference is the opportunity to interact with others. For trainees and early career attendees, DDW is your debutante ball! Introduce yourself and your work to the broader GI community. Bring your business cards as well as a notebook to write down questions and comments about your study. Look engaging when standing by your poster and offer to walk visitors through your research. There will also be an opportunity to have free headshots taken in the Early Career area this year.
Also take advantage of DDW’s big draw to reconnect with old friends and colleagues from around the U.S. and the world. Schedule a time to catch up and swap stories. Learn from each other’s successes and mistakes. It’s good for the soul and your career.
Post-DDW
Attending DDW is only the start! The most important part of the conference is what happens afterward. Send an email to individuals you met to establish a line of communication and thank them for their advice or insight. Did someone offer to share a protocol, start a collaboration, or introduce you to a colleague? Take them up on the offer! Notes that were taken in the app can also be emailed. In addition, registration includes 2 years of access to DDW On Demand, an online library of sessions. If there were any nonticketed presentations that you missed, you can watch them upon your return. Similarly, access missed posters at the DDW ePosters archive, where you can read poster abstracts and view ePosters, if submitted. Abstracts will still be viewable through the app and online planner as well. Reach out to colleagues if you have questions about their work!
Also, don’t forget to take what you learned back to your community. Share your new knowledge with your colleagues and trainees, and consider if there are any new concepts or approaches that should be implemented in your practice.
Practical tip
Before it falls off your radar, submit for CME credits for the sessions you attended. To claim CME, you may flag sessions for CME using the DDW Mobile App, visit a CME kiosk on site or access the DDW CME Claim Site after the meeting. Visit the DDW website for more information on claiming CME.
Refine, refocus, and recharge
DDW is the most comprehensive GI event in the world. Take advantage of the learning opportunities to improve your own work. Note how the landscape of GI is evolving and use it to reevaluate your own career development strategy and how you want to contribute to the field. Most importantly, get inspired. After exploring the most up-to-date advances and connecting with colleagues and thought leaders at DDW, you will hopefully return to your home institution feeling reinvigorated, refreshed, and ready to apply your newfound insights to your patient care or to your research.
See you at DDW!
References
1. Notices. Gastroenterology. 1969;569(1):188-9. http://www.gastrojournal.org/article/S0016-5085(69)80085-5/pdf.
2. Exhibitor Prospectus | Digestive Disease Week® 2018. https://higherlogicdownload.s3.amazonaws.com/GASTRO/44b1f1fd-aaed-44c8-954f-b0eaea6b0462/UploadedFiles/B4KUryNTNS5lEaFk6jBQ_DDW%202018%20Exhibitor%20Prospectus_Staffchanges.pdf
Dr. Chen is assistant professor of medicine, New York University School of Medicine.
It’s that time of the year again: Digestive Disease Week (DDW®)! This event evolved out of the AGA annual meetings and was first advertised as DDW in the January 1969 issue of Gastroenterology.1 Since that time, it has grown into a truly international event with over 14,000 attendees, 41% of whom attend from abroad.2
DDW is a collaborative event that is jointly sponsored by four professional GI/hepatology-related societies – the AGA, the American Association for the Study of Liver Diseases, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract. The conference topics cover the gamut of GI and hepatology conditions and participants represent all types of professional settings, including private practice (37%), hospitals (33%), and academic medical centers (28%).2 Whether you’re a first-time attendee or a seasoned participant, DDW offers something for everyone.
Plan ahead
Is there a new treatment or condition you’ve wanted to learn more about? Are you interested in testing the latest endoscopic devices or learning a new procedural technique? Experts from around the world come to DDW to showcase the latest developments in GI. However, with over 5,000 abstracts and lectures and almost 300 exhibition booths, it’s easy to feel overwhelmed by all the offerings. To make the most of your experience, plan ahead.
In the months prior to the conference, visit the DDW website to download the Preliminary Program. Pick out your can’t-miss lectures and events, and put them on your calendar right away. As DDW approaches, invitations from colleagues, societies, and industry grow, so preplanning is a necessity.
Approximately 1 month before DDW, the DDW Mobile App will become available for free download in the Apple and Google Play stores. You can highlight events of interest and place them on a personalized calendar. Allow for push notifications to get the latest updates and schedule changes throughout the event. In addition, the in-app maps of the venue are a fantastic way to locate where scheduled events will take place. Try to attend talks that are located close to one another. The conference center is expansive and you may miss your intended presentations by trying to catch overlapping sessions situated far from each other. If you prefer planning on a desktop or laptop, use the DDW Online Planner (available mid-April) to create your schedule. The information can then be synced to your mobile device through the app.
Upon arrival, be sure to pick up your attendee conference bag. Before recycling the contents, look for any product theaters, satellite symposia, exhibitor booths, or other advertised activities you may want to add to your schedule.
Practical tips
a) Register ahead of time and pick up your conference bag during off-hours to avoid long lines.
b) Book your hotel early. Most have generous cancellation policies. Registration is required before booking housing.
c) Pack comfortable shoes and dress in layers to accommodate both unpredictable weather and indoor climate control.
Make new connections and nurture old ones
Is your professional hero giving a talk? Are you looking to land your first job or make a move? Do you need some face time with a mentor outside your institution? DDW is a wonderful opportunity to connect with advisers and possible employers as well as potential and established collaborators. Schedules fill up quickly though, so try your best to email requests for meetings well ahead of time. The app also has a messaging feature you can use to communicate with other attendees.
At the meeting, be an active participant and ask questions. One of the greatest benefits of attending the conference is the opportunity to interact with others. For trainees and early career attendees, DDW is your debutante ball! Introduce yourself and your work to the broader GI community. Bring your business cards as well as a notebook to write down questions and comments about your study. Look engaging when standing by your poster and offer to walk visitors through your research. There will also be an opportunity to have free headshots taken in the Early Career area this year.
Also take advantage of DDW’s big draw to reconnect with old friends and colleagues from around the U.S. and the world. Schedule a time to catch up and swap stories. Learn from each other’s successes and mistakes. It’s good for the soul and your career.
Post-DDW
Attending DDW is only the start! The most important part of the conference is what happens afterward. Send an email to individuals you met to establish a line of communication and thank them for their advice or insight. Did someone offer to share a protocol, start a collaboration, or introduce you to a colleague? Take them up on the offer! Notes that were taken in the app can also be emailed. In addition, registration includes 2 years of access to DDW On Demand, an online library of sessions. If there were any nonticketed presentations that you missed, you can watch them upon your return. Similarly, access missed posters at the DDW ePosters archive, where you can read poster abstracts and view ePosters, if submitted. Abstracts will still be viewable through the app and online planner as well. Reach out to colleagues if you have questions about their work!
Also, don’t forget to take what you learned back to your community. Share your new knowledge with your colleagues and trainees, and consider if there are any new concepts or approaches that should be implemented in your practice.
Practical tip
Before it falls off your radar, submit for CME credits for the sessions you attended. To claim CME, you may flag sessions for CME using the DDW Mobile App, visit a CME kiosk on site or access the DDW CME Claim Site after the meeting. Visit the DDW website for more information on claiming CME.
Refine, refocus, and recharge
DDW is the most comprehensive GI event in the world. Take advantage of the learning opportunities to improve your own work. Note how the landscape of GI is evolving and use it to reevaluate your own career development strategy and how you want to contribute to the field. Most importantly, get inspired. After exploring the most up-to-date advances and connecting with colleagues and thought leaders at DDW, you will hopefully return to your home institution feeling reinvigorated, refreshed, and ready to apply your newfound insights to your patient care or to your research.
See you at DDW!
References
1. Notices. Gastroenterology. 1969;569(1):188-9. http://www.gastrojournal.org/article/S0016-5085(69)80085-5/pdf.
2. Exhibitor Prospectus | Digestive Disease Week® 2018. https://higherlogicdownload.s3.amazonaws.com/GASTRO/44b1f1fd-aaed-44c8-954f-b0eaea6b0462/UploadedFiles/B4KUryNTNS5lEaFk6jBQ_DDW%202018%20Exhibitor%20Prospectus_Staffchanges.pdf
Dr. Chen is assistant professor of medicine, New York University School of Medicine.
It’s that time of the year again: Digestive Disease Week (DDW®)! This event evolved out of the AGA annual meetings and was first advertised as DDW in the January 1969 issue of Gastroenterology.1 Since that time, it has grown into a truly international event with over 14,000 attendees, 41% of whom attend from abroad.2
DDW is a collaborative event that is jointly sponsored by four professional GI/hepatology-related societies – the AGA, the American Association for the Study of Liver Diseases, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract. The conference topics cover the gamut of GI and hepatology conditions and participants represent all types of professional settings, including private practice (37%), hospitals (33%), and academic medical centers (28%).2 Whether you’re a first-time attendee or a seasoned participant, DDW offers something for everyone.
Plan ahead
Is there a new treatment or condition you’ve wanted to learn more about? Are you interested in testing the latest endoscopic devices or learning a new procedural technique? Experts from around the world come to DDW to showcase the latest developments in GI. However, with over 5,000 abstracts and lectures and almost 300 exhibition booths, it’s easy to feel overwhelmed by all the offerings. To make the most of your experience, plan ahead.
In the months prior to the conference, visit the DDW website to download the Preliminary Program. Pick out your can’t-miss lectures and events, and put them on your calendar right away. As DDW approaches, invitations from colleagues, societies, and industry grow, so preplanning is a necessity.
Approximately 1 month before DDW, the DDW Mobile App will become available for free download in the Apple and Google Play stores. You can highlight events of interest and place them on a personalized calendar. Allow for push notifications to get the latest updates and schedule changes throughout the event. In addition, the in-app maps of the venue are a fantastic way to locate where scheduled events will take place. Try to attend talks that are located close to one another. The conference center is expansive and you may miss your intended presentations by trying to catch overlapping sessions situated far from each other. If you prefer planning on a desktop or laptop, use the DDW Online Planner (available mid-April) to create your schedule. The information can then be synced to your mobile device through the app.
Upon arrival, be sure to pick up your attendee conference bag. Before recycling the contents, look for any product theaters, satellite symposia, exhibitor booths, or other advertised activities you may want to add to your schedule.
Practical tips
a) Register ahead of time and pick up your conference bag during off-hours to avoid long lines.
b) Book your hotel early. Most have generous cancellation policies. Registration is required before booking housing.
c) Pack comfortable shoes and dress in layers to accommodate both unpredictable weather and indoor climate control.
Make new connections and nurture old ones
Is your professional hero giving a talk? Are you looking to land your first job or make a move? Do you need some face time with a mentor outside your institution? DDW is a wonderful opportunity to connect with advisers and possible employers as well as potential and established collaborators. Schedules fill up quickly though, so try your best to email requests for meetings well ahead of time. The app also has a messaging feature you can use to communicate with other attendees.
At the meeting, be an active participant and ask questions. One of the greatest benefits of attending the conference is the opportunity to interact with others. For trainees and early career attendees, DDW is your debutante ball! Introduce yourself and your work to the broader GI community. Bring your business cards as well as a notebook to write down questions and comments about your study. Look engaging when standing by your poster and offer to walk visitors through your research. There will also be an opportunity to have free headshots taken in the Early Career area this year.
Also take advantage of DDW’s big draw to reconnect with old friends and colleagues from around the U.S. and the world. Schedule a time to catch up and swap stories. Learn from each other’s successes and mistakes. It’s good for the soul and your career.
Post-DDW
Attending DDW is only the start! The most important part of the conference is what happens afterward. Send an email to individuals you met to establish a line of communication and thank them for their advice or insight. Did someone offer to share a protocol, start a collaboration, or introduce you to a colleague? Take them up on the offer! Notes that were taken in the app can also be emailed. In addition, registration includes 2 years of access to DDW On Demand, an online library of sessions. If there were any nonticketed presentations that you missed, you can watch them upon your return. Similarly, access missed posters at the DDW ePosters archive, where you can read poster abstracts and view ePosters, if submitted. Abstracts will still be viewable through the app and online planner as well. Reach out to colleagues if you have questions about their work!
Also, don’t forget to take what you learned back to your community. Share your new knowledge with your colleagues and trainees, and consider if there are any new concepts or approaches that should be implemented in your practice.
Practical tip
Before it falls off your radar, submit for CME credits for the sessions you attended. To claim CME, you may flag sessions for CME using the DDW Mobile App, visit a CME kiosk on site or access the DDW CME Claim Site after the meeting. Visit the DDW website for more information on claiming CME.
Refine, refocus, and recharge
DDW is the most comprehensive GI event in the world. Take advantage of the learning opportunities to improve your own work. Note how the landscape of GI is evolving and use it to reevaluate your own career development strategy and how you want to contribute to the field. Most importantly, get inspired. After exploring the most up-to-date advances and connecting with colleagues and thought leaders at DDW, you will hopefully return to your home institution feeling reinvigorated, refreshed, and ready to apply your newfound insights to your patient care or to your research.
See you at DDW!
References
1. Notices. Gastroenterology. 1969;569(1):188-9. http://www.gastrojournal.org/article/S0016-5085(69)80085-5/pdf.
2. Exhibitor Prospectus | Digestive Disease Week® 2018. https://higherlogicdownload.s3.amazonaws.com/GASTRO/44b1f1fd-aaed-44c8-954f-b0eaea6b0462/UploadedFiles/B4KUryNTNS5lEaFk6jBQ_DDW%202018%20Exhibitor%20Prospectus_Staffchanges.pdf
Dr. Chen is assistant professor of medicine, New York University School of Medicine.
Adopting new evidence into practice – a guide for the new gastroenterologist
The transition from gastroenterology fellowship to independent practice can be daunting. There may be concerns about procedural competency and increased levels of responsibility. Recent trainees have to manage their newly busy clinical schedules while trying to integrate evidence from a rapidly evolving landscape of medical literature into daily practice. Many recent graduates also are expected to participate in financial decisions or contribute to assessments about resource allocation regarding new technologies. These are challenges faced by those in both community and academic positions but may be more keenly felt in the first years of practice regardless of setting.
Without the benefit of experience, incorporating pertinent evidence from both within and outside of the field of gastroenterology as well as identifying disruptive technologies can be particularly difficult. There is scant guidance in this area, either during fellowship or from the existing literature1. Yet these are skills that, when properly developed, can be lifelong assets and, as a result, an evaluation of this process is warranted. Herein, we identify recent developments relevant to gastroenterologists to illustrate a conceptual framework for judging novel information.
A practical concern for the new gastroenterologist is learning to efficiently evaluate the merits of the latest research and then implement this knowledge in the clinic. Maintaining active society membership often includes access to scholarly journals. For example, AGA members receive Gastroenterology, Clinical Gastroenterology and Hepatology, and Cellular and Molecular Gastroenterology and Hepatology as part of their member benefits and have the opportunity to receive alerts when new content is published. Social media outlets such as Twitter and Facebook also simplify the process for readers to identify high-impact studies2 (see social media urls at the end of the story). In addition to reading, however, a critical review of these studies can prevent premature enthusiasm for modifying practice. The evolving evidence base for understanding proton pump inhibitor (PPI) risks is illustrative. Several studies attracted widespread media attention describing serious associated side effects, ranging from MI3 to dementia4 and stroke5. These studies were provocative but a decision to withhold PPIs from patients based on these concerns alone could lead to unintended consequences with poor outcomes. Ultimately, subsequent studies published only months later challenged these associations.6-8 Instead, thoughtful disclosure to patients of known risks and appropriate indications for PPI therapy based on resources such as the AGA Best Practice Advice9 is prudent. Reading more may be necessary but is insufficient; finding a forum to discuss novel research topics, such as in a monthly journal club10 or group practice meeting, can lead to stimulating discussion about how to apply pertinent research to change practice. The AGA Community is an excellent venue for this kind of interaction.
In many situations, keeping informed of updates about the risks and safety of medications prescribed by nongastroenterologists, particularly as they relate to GI conditions, can be even more difficult. A prime example of this is the rapidly expanding literature on indications and risks of direct oral anticoagulants. Rotating on the inpatient consultation service, with the chance to interact with multiple non-GI providers, affords an excellent opportunity to stay up to date. With the increased prevalence of atrial fibrillation as well as the potential expanded indications for direct oral anticoagulants based on recent randomized, controlled trials11,12, practicing gastroenterologists will be comanaging increasing numbers of patients hospitalized with gastrointestinal bleeding (GIB). Our understanding of the availability and indication for targeted reversal agents, such as idarucizumab, as well as nonspecific reversal agents, such as prothrombin complex concentrates, for those with life-threatening GIB is critical to optimal management of these patients. Multidisciplinary collaborations, such as with cardiogastroenterology clinics13, can be leveraged for optimal management of direct oral anticoagulants in the periendoscopy period.
Traditional outpatient consultative approaches are sometimes necessary but frequent reference to consensus societal guidelines on endoscopy in patients on antithrombotics14 should be made, particularly if they are printed and readily available in the ambulatory clinic and endoscopy suites. When information may be too new or sparse to utilize a national guideline, employing local data or experience to create a hospital-specific algorithm can ensure the delivery of high-quality, collaborative patient care.
Much like reviewing the literature, evaluating new technologies poses its own challenges. Changes in clinical practice may be slow, as in the adoption of noninvasive methods for Barrett’s esophagus screening.15 But in an age when news of advances and updates in management spreads at tremendous speed through the use of social media, the ability to pivot or assimilate new discoveries and techniques will become increasingly relevant and important. A professional society’s endorsement can provide a framework for a decision, but other principles at play include sensible, critical analyses of the outcomes and costs as well as a balance of organizational and societal perspectives.16 The use of impedance planimetry is one such example. This is a relatively new technology, but it has received increasing interest recently.17 The first questions when considering adopting this type of device likely will be about its supporting evidence and the risk for causing harm. The pace of publications regarding its use for measuring esophageal distensibility has accelerated18. But good data does not necessarily translate into extensive uptake. Other important factors also are practical, e.g., whether a technology committee’s approval is needed and what is the learning curve, available technical support, need for capital purchases, reimbursement, etc. Functional luminal imaging probe (FLIP®) technology was developed to assess compliance in primary esophageal disorders and now has been applied to several other areas including anorectal disease, bariatric surgery, and therapeutic endoscopy19,20. Although seemingly a niche market, there is potential widespread application and an opportunity for collaborations that might not have been evident at first blush. Ultimately, any evaluation of new technology is to a certain extent speculation. Is the technology mature or novel? If it is the latter, this may provide a marketing advantage and facilitate a relationship that could lead to academic partnerships.
Embracing new devices and modifications to existing practice paradigms happens on a spectrum21. We are reminded of the maxim, “never be the first or last to adopt change.” One must be on the lookout for revolutionary or game-changing advances but be cautious to avoid irresponsible enthusiasm. Whether it is incorporating evidence from a recent study into everyday practice or judging the potential of new equipment, a balance must be achieved between detailed evaluation of the literature and understanding the practical consequences and feasibility of implementing change. Although these may be competing interests, achieving this is a pivotal step in success for the new gastroenterologist.
AGA journals' social media accounts
http://twitter.com/aga_cgh
http://twitter.com/aga_cmgh
https://www.facebook.com/gastrojournal/
https://www.facebook.com/cghjournal/
https://www.facebook.com/cmghjournal/
References
1. Arora V et al. Closing the gap between internal medicine training and practice: Recommendations from recent graduates. Am J Med. 2005 Jun;118(6):685-7.
2. Gray DM et al. Making social media work for your practice. Clin Gastroenterol Hepatol. 2017 Nov;15:1651-4.
3. Shah NH et al. Proton pump inhibitor usage and the risk of myocardial infarction in the general population. PLoS One. 2015 Jun 10;10:e0124653.
4. Gomm W et al. Association of proton pump inhibitors with risk of dementia: A pharmacoepidemiological claims data analysis. JAMA Neurol. 2016 Apr;73(4):410-6.
5. Wang YF et al. Proton-pump inhibitor use and the risk of first-time ischemic stroke in the general population: A nationwide population-based study. Am J Gastroenterol. 2017 Jul;112:1084-93.
6. Nguyen LH et al. No significant association between proton pump inhibitor use and risk of stroke after adjustment for lifestyle factors and indication. Gastroenterology. 2018 Apr; 154(5):1290-7.
7. Lochhead P et al. Association between proton pump inhibitor use and cognitive function in women. Gastroenterology. 2017 Oct;153(4):971-9.
8. Landi SN et al. No increase in risk of acute myocardial infarction in privately insured adults prescribed proton pump inhibitors vs histamine-2 receptor antagonists (2002-2014). Gastroenterology 2018 Mar;154(4):861-73.
9. Freedberg DE et al. The risks and benefits of long-term use of proton pump inhibitors: Expert review and best practice advise from the American Gastroenterological Association. Gastroenterology. 2017 Mar;152:706-15.
10. Judd S et al. Approach to presenting a clinical journal club. Gastroenterology. 2014 Jun;146(7):1591-3.
11. Weitz JI et al. Rivaroxaban or aspirin for extended treatment of venous thromboembolism. N Engl J Med. 2017 Mar 30;376:1211-22.
12. Eikelboom JW et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017 Oct. 5;377:1319-30.
13. Abraham NS. Novel oral anticoagulants and gastrointestinal bleeding: a case for cardiogastroenterology. Clin Gastroenterol Hepatol. 2013;11(4):324-8.
14. Acosta RD et al. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016;83:3-16.
15. Sami SS et al. Screening for Barrett’s esophagus and esophageal adenocarcinoma: rationale, recent progress, challenges and future directions. Clin Gastroenterol Hepatol. 2015 Apr;13:623-34.
16. Laupacis A et al. How attractive does a new technology need to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ. 1992 Feb 15;146:473-81.
17. Hirano I et al. Functional lumen imaging probe for the management of esophageal disorders: Expert review from the clinical practice updates committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017 Mar;15:325-34.
18. Kwiatek MA et al. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc. 2010 Aug;72:272-82.
19. Leroi AM et al. The diagnostic value of the functional lumen imaging probe versus high-resolution anorectal manometry in patients with fecal incontinence. Neurogastroenterol Motil. 2018 Jan 18; doi: 10.1111/nmo.13291.
20. Reynolds JL et al. Intraoperative assessment of the effects of laparoscopic sleeve gastrectomy on the distensibility of the lower esophageal sphincter using impedance planimetry. Surg Endosc. 2016 Nov;30:4904-9.
21. Aisenberg J. Optical biopsy for colorectal polyps: moving along the S-shaped curve. Gastrointest Endosc. 2014 Mar;79:399-401.
Dr. Leiman, assistant professor of medicine, division of gastroenterology, Duke University, Durham, N.C.; Dr. Sengupta, assistant professor of medicine, section of gastroenterology, hepatology, and nutrition, University of Chicago Medical Center.
The transition from gastroenterology fellowship to independent practice can be daunting. There may be concerns about procedural competency and increased levels of responsibility. Recent trainees have to manage their newly busy clinical schedules while trying to integrate evidence from a rapidly evolving landscape of medical literature into daily practice. Many recent graduates also are expected to participate in financial decisions or contribute to assessments about resource allocation regarding new technologies. These are challenges faced by those in both community and academic positions but may be more keenly felt in the first years of practice regardless of setting.
Without the benefit of experience, incorporating pertinent evidence from both within and outside of the field of gastroenterology as well as identifying disruptive technologies can be particularly difficult. There is scant guidance in this area, either during fellowship or from the existing literature1. Yet these are skills that, when properly developed, can be lifelong assets and, as a result, an evaluation of this process is warranted. Herein, we identify recent developments relevant to gastroenterologists to illustrate a conceptual framework for judging novel information.
A practical concern for the new gastroenterologist is learning to efficiently evaluate the merits of the latest research and then implement this knowledge in the clinic. Maintaining active society membership often includes access to scholarly journals. For example, AGA members receive Gastroenterology, Clinical Gastroenterology and Hepatology, and Cellular and Molecular Gastroenterology and Hepatology as part of their member benefits and have the opportunity to receive alerts when new content is published. Social media outlets such as Twitter and Facebook also simplify the process for readers to identify high-impact studies2 (see social media urls at the end of the story). In addition to reading, however, a critical review of these studies can prevent premature enthusiasm for modifying practice. The evolving evidence base for understanding proton pump inhibitor (PPI) risks is illustrative. Several studies attracted widespread media attention describing serious associated side effects, ranging from MI3 to dementia4 and stroke5. These studies were provocative but a decision to withhold PPIs from patients based on these concerns alone could lead to unintended consequences with poor outcomes. Ultimately, subsequent studies published only months later challenged these associations.6-8 Instead, thoughtful disclosure to patients of known risks and appropriate indications for PPI therapy based on resources such as the AGA Best Practice Advice9 is prudent. Reading more may be necessary but is insufficient; finding a forum to discuss novel research topics, such as in a monthly journal club10 or group practice meeting, can lead to stimulating discussion about how to apply pertinent research to change practice. The AGA Community is an excellent venue for this kind of interaction.
In many situations, keeping informed of updates about the risks and safety of medications prescribed by nongastroenterologists, particularly as they relate to GI conditions, can be even more difficult. A prime example of this is the rapidly expanding literature on indications and risks of direct oral anticoagulants. Rotating on the inpatient consultation service, with the chance to interact with multiple non-GI providers, affords an excellent opportunity to stay up to date. With the increased prevalence of atrial fibrillation as well as the potential expanded indications for direct oral anticoagulants based on recent randomized, controlled trials11,12, practicing gastroenterologists will be comanaging increasing numbers of patients hospitalized with gastrointestinal bleeding (GIB). Our understanding of the availability and indication for targeted reversal agents, such as idarucizumab, as well as nonspecific reversal agents, such as prothrombin complex concentrates, for those with life-threatening GIB is critical to optimal management of these patients. Multidisciplinary collaborations, such as with cardiogastroenterology clinics13, can be leveraged for optimal management of direct oral anticoagulants in the periendoscopy period.
Traditional outpatient consultative approaches are sometimes necessary but frequent reference to consensus societal guidelines on endoscopy in patients on antithrombotics14 should be made, particularly if they are printed and readily available in the ambulatory clinic and endoscopy suites. When information may be too new or sparse to utilize a national guideline, employing local data or experience to create a hospital-specific algorithm can ensure the delivery of high-quality, collaborative patient care.
Much like reviewing the literature, evaluating new technologies poses its own challenges. Changes in clinical practice may be slow, as in the adoption of noninvasive methods for Barrett’s esophagus screening.15 But in an age when news of advances and updates in management spreads at tremendous speed through the use of social media, the ability to pivot or assimilate new discoveries and techniques will become increasingly relevant and important. A professional society’s endorsement can provide a framework for a decision, but other principles at play include sensible, critical analyses of the outcomes and costs as well as a balance of organizational and societal perspectives.16 The use of impedance planimetry is one such example. This is a relatively new technology, but it has received increasing interest recently.17 The first questions when considering adopting this type of device likely will be about its supporting evidence and the risk for causing harm. The pace of publications regarding its use for measuring esophageal distensibility has accelerated18. But good data does not necessarily translate into extensive uptake. Other important factors also are practical, e.g., whether a technology committee’s approval is needed and what is the learning curve, available technical support, need for capital purchases, reimbursement, etc. Functional luminal imaging probe (FLIP®) technology was developed to assess compliance in primary esophageal disorders and now has been applied to several other areas including anorectal disease, bariatric surgery, and therapeutic endoscopy19,20. Although seemingly a niche market, there is potential widespread application and an opportunity for collaborations that might not have been evident at first blush. Ultimately, any evaluation of new technology is to a certain extent speculation. Is the technology mature or novel? If it is the latter, this may provide a marketing advantage and facilitate a relationship that could lead to academic partnerships.
Embracing new devices and modifications to existing practice paradigms happens on a spectrum21. We are reminded of the maxim, “never be the first or last to adopt change.” One must be on the lookout for revolutionary or game-changing advances but be cautious to avoid irresponsible enthusiasm. Whether it is incorporating evidence from a recent study into everyday practice or judging the potential of new equipment, a balance must be achieved between detailed evaluation of the literature and understanding the practical consequences and feasibility of implementing change. Although these may be competing interests, achieving this is a pivotal step in success for the new gastroenterologist.
AGA journals' social media accounts
http://twitter.com/aga_cgh
http://twitter.com/aga_cmgh
https://www.facebook.com/gastrojournal/
https://www.facebook.com/cghjournal/
https://www.facebook.com/cmghjournal/
References
1. Arora V et al. Closing the gap between internal medicine training and practice: Recommendations from recent graduates. Am J Med. 2005 Jun;118(6):685-7.
2. Gray DM et al. Making social media work for your practice. Clin Gastroenterol Hepatol. 2017 Nov;15:1651-4.
3. Shah NH et al. Proton pump inhibitor usage and the risk of myocardial infarction in the general population. PLoS One. 2015 Jun 10;10:e0124653.
4. Gomm W et al. Association of proton pump inhibitors with risk of dementia: A pharmacoepidemiological claims data analysis. JAMA Neurol. 2016 Apr;73(4):410-6.
5. Wang YF et al. Proton-pump inhibitor use and the risk of first-time ischemic stroke in the general population: A nationwide population-based study. Am J Gastroenterol. 2017 Jul;112:1084-93.
6. Nguyen LH et al. No significant association between proton pump inhibitor use and risk of stroke after adjustment for lifestyle factors and indication. Gastroenterology. 2018 Apr; 154(5):1290-7.
7. Lochhead P et al. Association between proton pump inhibitor use and cognitive function in women. Gastroenterology. 2017 Oct;153(4):971-9.
8. Landi SN et al. No increase in risk of acute myocardial infarction in privately insured adults prescribed proton pump inhibitors vs histamine-2 receptor antagonists (2002-2014). Gastroenterology 2018 Mar;154(4):861-73.
9. Freedberg DE et al. The risks and benefits of long-term use of proton pump inhibitors: Expert review and best practice advise from the American Gastroenterological Association. Gastroenterology. 2017 Mar;152:706-15.
10. Judd S et al. Approach to presenting a clinical journal club. Gastroenterology. 2014 Jun;146(7):1591-3.
11. Weitz JI et al. Rivaroxaban or aspirin for extended treatment of venous thromboembolism. N Engl J Med. 2017 Mar 30;376:1211-22.
12. Eikelboom JW et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017 Oct. 5;377:1319-30.
13. Abraham NS. Novel oral anticoagulants and gastrointestinal bleeding: a case for cardiogastroenterology. Clin Gastroenterol Hepatol. 2013;11(4):324-8.
14. Acosta RD et al. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016;83:3-16.
15. Sami SS et al. Screening for Barrett’s esophagus and esophageal adenocarcinoma: rationale, recent progress, challenges and future directions. Clin Gastroenterol Hepatol. 2015 Apr;13:623-34.
16. Laupacis A et al. How attractive does a new technology need to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ. 1992 Feb 15;146:473-81.
17. Hirano I et al. Functional lumen imaging probe for the management of esophageal disorders: Expert review from the clinical practice updates committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017 Mar;15:325-34.
18. Kwiatek MA et al. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc. 2010 Aug;72:272-82.
19. Leroi AM et al. The diagnostic value of the functional lumen imaging probe versus high-resolution anorectal manometry in patients with fecal incontinence. Neurogastroenterol Motil. 2018 Jan 18; doi: 10.1111/nmo.13291.
20. Reynolds JL et al. Intraoperative assessment of the effects of laparoscopic sleeve gastrectomy on the distensibility of the lower esophageal sphincter using impedance planimetry. Surg Endosc. 2016 Nov;30:4904-9.
21. Aisenberg J. Optical biopsy for colorectal polyps: moving along the S-shaped curve. Gastrointest Endosc. 2014 Mar;79:399-401.
Dr. Leiman, assistant professor of medicine, division of gastroenterology, Duke University, Durham, N.C.; Dr. Sengupta, assistant professor of medicine, section of gastroenterology, hepatology, and nutrition, University of Chicago Medical Center.
The transition from gastroenterology fellowship to independent practice can be daunting. There may be concerns about procedural competency and increased levels of responsibility. Recent trainees have to manage their newly busy clinical schedules while trying to integrate evidence from a rapidly evolving landscape of medical literature into daily practice. Many recent graduates also are expected to participate in financial decisions or contribute to assessments about resource allocation regarding new technologies. These are challenges faced by those in both community and academic positions but may be more keenly felt in the first years of practice regardless of setting.
Without the benefit of experience, incorporating pertinent evidence from both within and outside of the field of gastroenterology as well as identifying disruptive technologies can be particularly difficult. There is scant guidance in this area, either during fellowship or from the existing literature1. Yet these are skills that, when properly developed, can be lifelong assets and, as a result, an evaluation of this process is warranted. Herein, we identify recent developments relevant to gastroenterologists to illustrate a conceptual framework for judging novel information.
A practical concern for the new gastroenterologist is learning to efficiently evaluate the merits of the latest research and then implement this knowledge in the clinic. Maintaining active society membership often includes access to scholarly journals. For example, AGA members receive Gastroenterology, Clinical Gastroenterology and Hepatology, and Cellular and Molecular Gastroenterology and Hepatology as part of their member benefits and have the opportunity to receive alerts when new content is published. Social media outlets such as Twitter and Facebook also simplify the process for readers to identify high-impact studies2 (see social media urls at the end of the story). In addition to reading, however, a critical review of these studies can prevent premature enthusiasm for modifying practice. The evolving evidence base for understanding proton pump inhibitor (PPI) risks is illustrative. Several studies attracted widespread media attention describing serious associated side effects, ranging from MI3 to dementia4 and stroke5. These studies were provocative but a decision to withhold PPIs from patients based on these concerns alone could lead to unintended consequences with poor outcomes. Ultimately, subsequent studies published only months later challenged these associations.6-8 Instead, thoughtful disclosure to patients of known risks and appropriate indications for PPI therapy based on resources such as the AGA Best Practice Advice9 is prudent. Reading more may be necessary but is insufficient; finding a forum to discuss novel research topics, such as in a monthly journal club10 or group practice meeting, can lead to stimulating discussion about how to apply pertinent research to change practice. The AGA Community is an excellent venue for this kind of interaction.
In many situations, keeping informed of updates about the risks and safety of medications prescribed by nongastroenterologists, particularly as they relate to GI conditions, can be even more difficult. A prime example of this is the rapidly expanding literature on indications and risks of direct oral anticoagulants. Rotating on the inpatient consultation service, with the chance to interact with multiple non-GI providers, affords an excellent opportunity to stay up to date. With the increased prevalence of atrial fibrillation as well as the potential expanded indications for direct oral anticoagulants based on recent randomized, controlled trials11,12, practicing gastroenterologists will be comanaging increasing numbers of patients hospitalized with gastrointestinal bleeding (GIB). Our understanding of the availability and indication for targeted reversal agents, such as idarucizumab, as well as nonspecific reversal agents, such as prothrombin complex concentrates, for those with life-threatening GIB is critical to optimal management of these patients. Multidisciplinary collaborations, such as with cardiogastroenterology clinics13, can be leveraged for optimal management of direct oral anticoagulants in the periendoscopy period.
Traditional outpatient consultative approaches are sometimes necessary but frequent reference to consensus societal guidelines on endoscopy in patients on antithrombotics14 should be made, particularly if they are printed and readily available in the ambulatory clinic and endoscopy suites. When information may be too new or sparse to utilize a national guideline, employing local data or experience to create a hospital-specific algorithm can ensure the delivery of high-quality, collaborative patient care.
Much like reviewing the literature, evaluating new technologies poses its own challenges. Changes in clinical practice may be slow, as in the adoption of noninvasive methods for Barrett’s esophagus screening.15 But in an age when news of advances and updates in management spreads at tremendous speed through the use of social media, the ability to pivot or assimilate new discoveries and techniques will become increasingly relevant and important. A professional society’s endorsement can provide a framework for a decision, but other principles at play include sensible, critical analyses of the outcomes and costs as well as a balance of organizational and societal perspectives.16 The use of impedance planimetry is one such example. This is a relatively new technology, but it has received increasing interest recently.17 The first questions when considering adopting this type of device likely will be about its supporting evidence and the risk for causing harm. The pace of publications regarding its use for measuring esophageal distensibility has accelerated18. But good data does not necessarily translate into extensive uptake. Other important factors also are practical, e.g., whether a technology committee’s approval is needed and what is the learning curve, available technical support, need for capital purchases, reimbursement, etc. Functional luminal imaging probe (FLIP®) technology was developed to assess compliance in primary esophageal disorders and now has been applied to several other areas including anorectal disease, bariatric surgery, and therapeutic endoscopy19,20. Although seemingly a niche market, there is potential widespread application and an opportunity for collaborations that might not have been evident at first blush. Ultimately, any evaluation of new technology is to a certain extent speculation. Is the technology mature or novel? If it is the latter, this may provide a marketing advantage and facilitate a relationship that could lead to academic partnerships.
Embracing new devices and modifications to existing practice paradigms happens on a spectrum21. We are reminded of the maxim, “never be the first or last to adopt change.” One must be on the lookout for revolutionary or game-changing advances but be cautious to avoid irresponsible enthusiasm. Whether it is incorporating evidence from a recent study into everyday practice or judging the potential of new equipment, a balance must be achieved between detailed evaluation of the literature and understanding the practical consequences and feasibility of implementing change. Although these may be competing interests, achieving this is a pivotal step in success for the new gastroenterologist.
AGA journals' social media accounts
http://twitter.com/aga_cgh
http://twitter.com/aga_cmgh
https://www.facebook.com/gastrojournal/
https://www.facebook.com/cghjournal/
https://www.facebook.com/cmghjournal/
References
1. Arora V et al. Closing the gap between internal medicine training and practice: Recommendations from recent graduates. Am J Med. 2005 Jun;118(6):685-7.
2. Gray DM et al. Making social media work for your practice. Clin Gastroenterol Hepatol. 2017 Nov;15:1651-4.
3. Shah NH et al. Proton pump inhibitor usage and the risk of myocardial infarction in the general population. PLoS One. 2015 Jun 10;10:e0124653.
4. Gomm W et al. Association of proton pump inhibitors with risk of dementia: A pharmacoepidemiological claims data analysis. JAMA Neurol. 2016 Apr;73(4):410-6.
5. Wang YF et al. Proton-pump inhibitor use and the risk of first-time ischemic stroke in the general population: A nationwide population-based study. Am J Gastroenterol. 2017 Jul;112:1084-93.
6. Nguyen LH et al. No significant association between proton pump inhibitor use and risk of stroke after adjustment for lifestyle factors and indication. Gastroenterology. 2018 Apr; 154(5):1290-7.
7. Lochhead P et al. Association between proton pump inhibitor use and cognitive function in women. Gastroenterology. 2017 Oct;153(4):971-9.
8. Landi SN et al. No increase in risk of acute myocardial infarction in privately insured adults prescribed proton pump inhibitors vs histamine-2 receptor antagonists (2002-2014). Gastroenterology 2018 Mar;154(4):861-73.
9. Freedberg DE et al. The risks and benefits of long-term use of proton pump inhibitors: Expert review and best practice advise from the American Gastroenterological Association. Gastroenterology. 2017 Mar;152:706-15.
10. Judd S et al. Approach to presenting a clinical journal club. Gastroenterology. 2014 Jun;146(7):1591-3.
11. Weitz JI et al. Rivaroxaban or aspirin for extended treatment of venous thromboembolism. N Engl J Med. 2017 Mar 30;376:1211-22.
12. Eikelboom JW et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017 Oct. 5;377:1319-30.
13. Abraham NS. Novel oral anticoagulants and gastrointestinal bleeding: a case for cardiogastroenterology. Clin Gastroenterol Hepatol. 2013;11(4):324-8.
14. Acosta RD et al. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016;83:3-16.
15. Sami SS et al. Screening for Barrett’s esophagus and esophageal adenocarcinoma: rationale, recent progress, challenges and future directions. Clin Gastroenterol Hepatol. 2015 Apr;13:623-34.
16. Laupacis A et al. How attractive does a new technology need to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ. 1992 Feb 15;146:473-81.
17. Hirano I et al. Functional lumen imaging probe for the management of esophageal disorders: Expert review from the clinical practice updates committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017 Mar;15:325-34.
18. Kwiatek MA et al. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc. 2010 Aug;72:272-82.
19. Leroi AM et al. The diagnostic value of the functional lumen imaging probe versus high-resolution anorectal manometry in patients with fecal incontinence. Neurogastroenterol Motil. 2018 Jan 18; doi: 10.1111/nmo.13291.
20. Reynolds JL et al. Intraoperative assessment of the effects of laparoscopic sleeve gastrectomy on the distensibility of the lower esophageal sphincter using impedance planimetry. Surg Endosc. 2016 Nov;30:4904-9.
21. Aisenberg J. Optical biopsy for colorectal polyps: moving along the S-shaped curve. Gastrointest Endosc. 2014 Mar;79:399-401.
Dr. Leiman, assistant professor of medicine, division of gastroenterology, Duke University, Durham, N.C.; Dr. Sengupta, assistant professor of medicine, section of gastroenterology, hepatology, and nutrition, University of Chicago Medical Center.
Advanced training in hepatology
Unlike previous hepatologists, who were trained through gastroenterology programs, most new practitioners seek advanced training in a fellowship year focused exclusively on hepatology.
Like practitioners in many medical subspecialties, transplant hepatologists have varied career goals and responsibilities. Hepatologists who continue to specifically practice transplant hepatology are affiliated with a liver transplant center, which is generally a hospital-based practice. However, most hepatologists also treat nontransplant hepatology patients and some who have completed advanced hepatology training focus exclusively on these patients or provide community-based care for transplant recipients from other centers. Caring for patients with end-stage liver disease and liver transplant recipients can be clinically demanding but also very rewarding. There are also many opportunities for academic pursuits within a hepatology career including areas in urgent need of clinical and basic investigation, clinical trials for novel agents to treat common diseases, education (including leadership in advanced hepatology training), and involvement in professional societies such as the American Gastroenterological Association (AGA) and American Association for the Study of Liver Disease (AASLD).
What are the opportunities for advanced hepatology training?
In 1999, the AASLD determined that the practice of transplant hepatology required its own specialized knowledge and that most practicing gastroenterologists did not consider themselves adequately prepared to care for patients with advanced liver disease.1,2 The following year, the AASLD applied to the American Board of Internal Medicine (ABIM) to develop formalized liver transplant training. After several years of debate and development, the first ABIM certification exam in transplant hepatology was held in 2006 and is now offered every 2 years.2
There are currently three pathways to achieve advanced training in hepatology. The traditional pathway is a 1-year Accreditation Council for Graduate Medical Education (ACGME) transplant fellowship that is separate from, and must follow completion of, a gastroenterology fellowship. There are currently 51 ACGME-accredited 1-year transplant hepatology fellowships in the United States. These fellowships are only at institutions with ACGME-accredited training in internal medicine and gastroenterology as well. The full and updated list of programs can be found on the ACGME website.3 The second pathway is the relatively new ABIM “pilot” program during which the transplant hepatology fellowship year is combined with the third year of gastroenterology fellowship (discussed in detail below). Finally, there remain many 1-year training programs that are not ACGME-accredited, may not be associated with a gastroenterology fellowship program, and do have not regulated requirements for entry. Trainees who complete non-ACGME programs are not candidates for ABIM board certification.
How does one apply for transplant hepatology fellowship?
Transplant hepatology fellowships do not participate in a match system. Therefore, the interviews and offers for training spots may occur at different times depending on the program and the region of the country. In general, fellows apply by the fall of their second year of gastroenterology fellowship in order to begin training after graduating from the third year of fellowship. Each program has its individual approach to the application process and most have this information available on a website as to how to apply. A complete list of ACGME-accredited programs along with the program directors and contact information is available on the ABIM website.3
What is the gastroenterology/transplant hepatology pilot training program?
The AASLD and ABIM have developed a combined gastroenterology and transplant hepatology pilot fellowship training program that allows eligible gastroenterology fellows to spend their third year training in transplant hepatology. This approach has the potential to shorten the total training from 4 years to 3. In addition, if all gastroenterology and transplant hepatology competencies are achieved by the end of the third year, fellows approved to be in this program are eligible to take both gastroenterology and transplant hepatology ABIM certification exams.
Any ACGME-accredited gastroenterology fellowship program that has an accredited hepatology counterpart is eligible to participate in this pilot. Eligible programs and fellows must apply to AASLD during the fellow’s second year. The fellow applicant must complete all clinical gastroenterology requirements before the end of the second year of fellowship and be on a trajectory to meet competency milestones, as the majority of the third year will focus on hepatology.
Since 2012, 59 fellows from 31 programs have participated in this pilot program.4 If you are interested in participating in this pilot program at your institution, it is important to confer with program directors as early as possible to meet all training requirements. In addition, applications are submitted to the Pilot Steering Taskforce during the fellow’s second year for review. This is not meant to be a competitive process and all fellows who meet the criteria are approved.
This track may not be ideal for all fellows interested in advanced and transplant hepatology. In particular, there may be a trade-off between achieving clinical competency in a shortened training period and pursuing scholarly activity. This pilot program is designed to be an intensive clinical track, so fellows who wish to focus on research should discuss with their program directors whether this is the best approach.
What has been your career path after advanced training in hepatology?
I first became interested in hepatology during my inpatient rotations as a medical student. This interest led me to become involved in research in this area very early in my career. The current structure of the fellowship as well as the board certification exam were both developed while I was in training and I adjusted my plans to complete 3 years of gastroenterology fellowship followed by an ACGME-accredited liver transplant fellowship year. Since completing training, I have worked as an attending at an academic medical center in a large liver transplant program and continue to care for patients with all forms of liver disease. In addition, I continued to pursue research as a large component of my job and now have NIH funding and direct the Transplant Clinical Research Center at Columbia University. Finally, I have always been devoted to education and am the program director for the transplant hepatology fellowship at our institution.
What is the future of advanced hepatology training?
The current transplant hepatology training system has evolved significantly since its inception, including development of curricula, ongoing modification of training requirements, and the development of the innovative pilot program. However, there are issues that continue to be debated by the community. For example, it is not certain when or if the combined gastroenterology and transplant hepatology pilot program will become a permanent pathway for training or how best to select fellows for this approach.
Hepatology continues to be a very dynamic area of medicine. With diseases such as nonalcoholic fatty liver disease and hepatocellular carcinoma on the rise, the urgent need for training in HCV treatment to combat the global epidemic of viral hepatitis, and the growing number of patients on the liver transplant waiting list, there has never been a more exciting time to choose hepatology as a career.
References
1. Luxon BA. So you want to be a hepatologist? Gastroenterology. 2013;145(6):1182-5.
2. Bacon BR, Grosso LJ, Freedman N, Althouse LA. Subspecialty certification in transplant hepatology. Liver Transpl. 2007;13(11):1479-81.
3. https://apps.acgme.org/ads/public/reports/report/1.
4. https://www.aasld.org/events-professional-development/educational-learning-faq.
Dr. Verna is assistant professor of medicine, program director, transplant hepatology fellowship, director of clinical research, Transplant Clinical Research Center, Columbia University Medical Center, New York.
Unlike previous hepatologists, who were trained through gastroenterology programs, most new practitioners seek advanced training in a fellowship year focused exclusively on hepatology.
Like practitioners in many medical subspecialties, transplant hepatologists have varied career goals and responsibilities. Hepatologists who continue to specifically practice transplant hepatology are affiliated with a liver transplant center, which is generally a hospital-based practice. However, most hepatologists also treat nontransplant hepatology patients and some who have completed advanced hepatology training focus exclusively on these patients or provide community-based care for transplant recipients from other centers. Caring for patients with end-stage liver disease and liver transplant recipients can be clinically demanding but also very rewarding. There are also many opportunities for academic pursuits within a hepatology career including areas in urgent need of clinical and basic investigation, clinical trials for novel agents to treat common diseases, education (including leadership in advanced hepatology training), and involvement in professional societies such as the American Gastroenterological Association (AGA) and American Association for the Study of Liver Disease (AASLD).
What are the opportunities for advanced hepatology training?
In 1999, the AASLD determined that the practice of transplant hepatology required its own specialized knowledge and that most practicing gastroenterologists did not consider themselves adequately prepared to care for patients with advanced liver disease.1,2 The following year, the AASLD applied to the American Board of Internal Medicine (ABIM) to develop formalized liver transplant training. After several years of debate and development, the first ABIM certification exam in transplant hepatology was held in 2006 and is now offered every 2 years.2
There are currently three pathways to achieve advanced training in hepatology. The traditional pathway is a 1-year Accreditation Council for Graduate Medical Education (ACGME) transplant fellowship that is separate from, and must follow completion of, a gastroenterology fellowship. There are currently 51 ACGME-accredited 1-year transplant hepatology fellowships in the United States. These fellowships are only at institutions with ACGME-accredited training in internal medicine and gastroenterology as well. The full and updated list of programs can be found on the ACGME website.3 The second pathway is the relatively new ABIM “pilot” program during which the transplant hepatology fellowship year is combined with the third year of gastroenterology fellowship (discussed in detail below). Finally, there remain many 1-year training programs that are not ACGME-accredited, may not be associated with a gastroenterology fellowship program, and do have not regulated requirements for entry. Trainees who complete non-ACGME programs are not candidates for ABIM board certification.
How does one apply for transplant hepatology fellowship?
Transplant hepatology fellowships do not participate in a match system. Therefore, the interviews and offers for training spots may occur at different times depending on the program and the region of the country. In general, fellows apply by the fall of their second year of gastroenterology fellowship in order to begin training after graduating from the third year of fellowship. Each program has its individual approach to the application process and most have this information available on a website as to how to apply. A complete list of ACGME-accredited programs along with the program directors and contact information is available on the ABIM website.3
What is the gastroenterology/transplant hepatology pilot training program?
The AASLD and ABIM have developed a combined gastroenterology and transplant hepatology pilot fellowship training program that allows eligible gastroenterology fellows to spend their third year training in transplant hepatology. This approach has the potential to shorten the total training from 4 years to 3. In addition, if all gastroenterology and transplant hepatology competencies are achieved by the end of the third year, fellows approved to be in this program are eligible to take both gastroenterology and transplant hepatology ABIM certification exams.
Any ACGME-accredited gastroenterology fellowship program that has an accredited hepatology counterpart is eligible to participate in this pilot. Eligible programs and fellows must apply to AASLD during the fellow’s second year. The fellow applicant must complete all clinical gastroenterology requirements before the end of the second year of fellowship and be on a trajectory to meet competency milestones, as the majority of the third year will focus on hepatology.
Since 2012, 59 fellows from 31 programs have participated in this pilot program.4 If you are interested in participating in this pilot program at your institution, it is important to confer with program directors as early as possible to meet all training requirements. In addition, applications are submitted to the Pilot Steering Taskforce during the fellow’s second year for review. This is not meant to be a competitive process and all fellows who meet the criteria are approved.
This track may not be ideal for all fellows interested in advanced and transplant hepatology. In particular, there may be a trade-off between achieving clinical competency in a shortened training period and pursuing scholarly activity. This pilot program is designed to be an intensive clinical track, so fellows who wish to focus on research should discuss with their program directors whether this is the best approach.
What has been your career path after advanced training in hepatology?
I first became interested in hepatology during my inpatient rotations as a medical student. This interest led me to become involved in research in this area very early in my career. The current structure of the fellowship as well as the board certification exam were both developed while I was in training and I adjusted my plans to complete 3 years of gastroenterology fellowship followed by an ACGME-accredited liver transplant fellowship year. Since completing training, I have worked as an attending at an academic medical center in a large liver transplant program and continue to care for patients with all forms of liver disease. In addition, I continued to pursue research as a large component of my job and now have NIH funding and direct the Transplant Clinical Research Center at Columbia University. Finally, I have always been devoted to education and am the program director for the transplant hepatology fellowship at our institution.
What is the future of advanced hepatology training?
The current transplant hepatology training system has evolved significantly since its inception, including development of curricula, ongoing modification of training requirements, and the development of the innovative pilot program. However, there are issues that continue to be debated by the community. For example, it is not certain when or if the combined gastroenterology and transplant hepatology pilot program will become a permanent pathway for training or how best to select fellows for this approach.
Hepatology continues to be a very dynamic area of medicine. With diseases such as nonalcoholic fatty liver disease and hepatocellular carcinoma on the rise, the urgent need for training in HCV treatment to combat the global epidemic of viral hepatitis, and the growing number of patients on the liver transplant waiting list, there has never been a more exciting time to choose hepatology as a career.
References
1. Luxon BA. So you want to be a hepatologist? Gastroenterology. 2013;145(6):1182-5.
2. Bacon BR, Grosso LJ, Freedman N, Althouse LA. Subspecialty certification in transplant hepatology. Liver Transpl. 2007;13(11):1479-81.
3. https://apps.acgme.org/ads/public/reports/report/1.
4. https://www.aasld.org/events-professional-development/educational-learning-faq.
Dr. Verna is assistant professor of medicine, program director, transplant hepatology fellowship, director of clinical research, Transplant Clinical Research Center, Columbia University Medical Center, New York.
Unlike previous hepatologists, who were trained through gastroenterology programs, most new practitioners seek advanced training in a fellowship year focused exclusively on hepatology.
Like practitioners in many medical subspecialties, transplant hepatologists have varied career goals and responsibilities. Hepatologists who continue to specifically practice transplant hepatology are affiliated with a liver transplant center, which is generally a hospital-based practice. However, most hepatologists also treat nontransplant hepatology patients and some who have completed advanced hepatology training focus exclusively on these patients or provide community-based care for transplant recipients from other centers. Caring for patients with end-stage liver disease and liver transplant recipients can be clinically demanding but also very rewarding. There are also many opportunities for academic pursuits within a hepatology career including areas in urgent need of clinical and basic investigation, clinical trials for novel agents to treat common diseases, education (including leadership in advanced hepatology training), and involvement in professional societies such as the American Gastroenterological Association (AGA) and American Association for the Study of Liver Disease (AASLD).
What are the opportunities for advanced hepatology training?
In 1999, the AASLD determined that the practice of transplant hepatology required its own specialized knowledge and that most practicing gastroenterologists did not consider themselves adequately prepared to care for patients with advanced liver disease.1,2 The following year, the AASLD applied to the American Board of Internal Medicine (ABIM) to develop formalized liver transplant training. After several years of debate and development, the first ABIM certification exam in transplant hepatology was held in 2006 and is now offered every 2 years.2
There are currently three pathways to achieve advanced training in hepatology. The traditional pathway is a 1-year Accreditation Council for Graduate Medical Education (ACGME) transplant fellowship that is separate from, and must follow completion of, a gastroenterology fellowship. There are currently 51 ACGME-accredited 1-year transplant hepatology fellowships in the United States. These fellowships are only at institutions with ACGME-accredited training in internal medicine and gastroenterology as well. The full and updated list of programs can be found on the ACGME website.3 The second pathway is the relatively new ABIM “pilot” program during which the transplant hepatology fellowship year is combined with the third year of gastroenterology fellowship (discussed in detail below). Finally, there remain many 1-year training programs that are not ACGME-accredited, may not be associated with a gastroenterology fellowship program, and do have not regulated requirements for entry. Trainees who complete non-ACGME programs are not candidates for ABIM board certification.
How does one apply for transplant hepatology fellowship?
Transplant hepatology fellowships do not participate in a match system. Therefore, the interviews and offers for training spots may occur at different times depending on the program and the region of the country. In general, fellows apply by the fall of their second year of gastroenterology fellowship in order to begin training after graduating from the third year of fellowship. Each program has its individual approach to the application process and most have this information available on a website as to how to apply. A complete list of ACGME-accredited programs along with the program directors and contact information is available on the ABIM website.3
What is the gastroenterology/transplant hepatology pilot training program?
The AASLD and ABIM have developed a combined gastroenterology and transplant hepatology pilot fellowship training program that allows eligible gastroenterology fellows to spend their third year training in transplant hepatology. This approach has the potential to shorten the total training from 4 years to 3. In addition, if all gastroenterology and transplant hepatology competencies are achieved by the end of the third year, fellows approved to be in this program are eligible to take both gastroenterology and transplant hepatology ABIM certification exams.
Any ACGME-accredited gastroenterology fellowship program that has an accredited hepatology counterpart is eligible to participate in this pilot. Eligible programs and fellows must apply to AASLD during the fellow’s second year. The fellow applicant must complete all clinical gastroenterology requirements before the end of the second year of fellowship and be on a trajectory to meet competency milestones, as the majority of the third year will focus on hepatology.
Since 2012, 59 fellows from 31 programs have participated in this pilot program.4 If you are interested in participating in this pilot program at your institution, it is important to confer with program directors as early as possible to meet all training requirements. In addition, applications are submitted to the Pilot Steering Taskforce during the fellow’s second year for review. This is not meant to be a competitive process and all fellows who meet the criteria are approved.
This track may not be ideal for all fellows interested in advanced and transplant hepatology. In particular, there may be a trade-off between achieving clinical competency in a shortened training period and pursuing scholarly activity. This pilot program is designed to be an intensive clinical track, so fellows who wish to focus on research should discuss with their program directors whether this is the best approach.
What has been your career path after advanced training in hepatology?
I first became interested in hepatology during my inpatient rotations as a medical student. This interest led me to become involved in research in this area very early in my career. The current structure of the fellowship as well as the board certification exam were both developed while I was in training and I adjusted my plans to complete 3 years of gastroenterology fellowship followed by an ACGME-accredited liver transplant fellowship year. Since completing training, I have worked as an attending at an academic medical center in a large liver transplant program and continue to care for patients with all forms of liver disease. In addition, I continued to pursue research as a large component of my job and now have NIH funding and direct the Transplant Clinical Research Center at Columbia University. Finally, I have always been devoted to education and am the program director for the transplant hepatology fellowship at our institution.
What is the future of advanced hepatology training?
The current transplant hepatology training system has evolved significantly since its inception, including development of curricula, ongoing modification of training requirements, and the development of the innovative pilot program. However, there are issues that continue to be debated by the community. For example, it is not certain when or if the combined gastroenterology and transplant hepatology pilot program will become a permanent pathway for training or how best to select fellows for this approach.
Hepatology continues to be a very dynamic area of medicine. With diseases such as nonalcoholic fatty liver disease and hepatocellular carcinoma on the rise, the urgent need for training in HCV treatment to combat the global epidemic of viral hepatitis, and the growing number of patients on the liver transplant waiting list, there has never been a more exciting time to choose hepatology as a career.
References
1. Luxon BA. So you want to be a hepatologist? Gastroenterology. 2013;145(6):1182-5.
2. Bacon BR, Grosso LJ, Freedman N, Althouse LA. Subspecialty certification in transplant hepatology. Liver Transpl. 2007;13(11):1479-81.
3. https://apps.acgme.org/ads/public/reports/report/1.
4. https://www.aasld.org/events-professional-development/educational-learning-faq.
Dr. Verna is assistant professor of medicine, program director, transplant hepatology fellowship, director of clinical research, Transplant Clinical Research Center, Columbia University Medical Center, New York.
Welcome to The New Gastroenterologist online!
Dear Colleagues,
It is with great excitement that I introduce the first e-newsletter version of The New Gastroenterologist! As more content in medicine, and life in general, is moving toward digital platforms, we at the AGA believe this transition will improve both content dissemination and accessibility to all our readers. In this new format, we will continue to provide articles on topics of importance to the early-career community, expand our offerings by including the new “In Focus” articles (concise overviews of GI topics) both digitally and in GI & Hepatology News print issues, as well as increase the use of multimedia resources, such as videos, to further enhance our content.
In this issue of The New Gastroenterologist, our In Focus article provides a practical overview of the management of chronic constipation. This article, written by Nitin Ahuja and James Reynolds from the Neurogastroenterology and Motility Program at the University of Pennsylvania, Philadelphia, addresses a common topic in our field, and can also be found in the February print issue of GI & Hepatology News. To complement this article, there is a corresponding video abstract that can be viewed.
Also in this issue, Richard Peek (Vanderbilt University, Nashville, Tenn.) – one of the Coeditors in Chief of Gastroenterology – provides a summary of the newly created 1-year editorial fellowship for the AGA’s flagship journal. This is a fantastic new opportunity and you can learn firsthand about the experience of the inaugural editorial fellow, Eric Shah (University of Michigan, Ann Arbor), in an accompanying video. Additionally, as helping patients make a successful transition from a pediatric GI practice to an adult GI practice can be very challenging, in this issue Manreet Kaur and Allyson Wyatt (Baylor College of Medicine, Houston) provide a primer on how to successfully aid in this transition.
Are you considering a career in hospital administration? If so, you will enjoy reading about pursuing a career in hospital administration from Brijen Shah, who is the chief medical officer of Mount Sinai Queens (Icahn School of Medicine at Mount Sinai, New York). Have you been to one of the AGA’s Regional Practice Skills Workshops? These workshops are sponsored by the AGA Trainee and Early Career Committee and held in a growing number of cities across the country. In this issue, Munish Ashat (University of Iowa, Iowa City) provides a recap of the workshop he attended, complete with many useful career pearls.
I hope that you also enjoy the other features in the new e-newsletter format of The New Gastroenterologist. I especially want to point out one of our new sections entitled “In Case You Missed It.” As we all undoubtedly experience information overload with so many new articles released each month, this section collects relevant articles from the numerous AGA publications and consolidates them to ensure you don’t miss any of this great content.
If you are interested in contributing to future issues of The New Gastroenterologist or if there are topics that would interest you, please let us know. You can contact me ([email protected]) or the managing editor of The New Gastroenterologist, Ryan Farrell ([email protected]).
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an instructor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
Dear Colleagues,
It is with great excitement that I introduce the first e-newsletter version of The New Gastroenterologist! As more content in medicine, and life in general, is moving toward digital platforms, we at the AGA believe this transition will improve both content dissemination and accessibility to all our readers. In this new format, we will continue to provide articles on topics of importance to the early-career community, expand our offerings by including the new “In Focus” articles (concise overviews of GI topics) both digitally and in GI & Hepatology News print issues, as well as increase the use of multimedia resources, such as videos, to further enhance our content.
In this issue of The New Gastroenterologist, our In Focus article provides a practical overview of the management of chronic constipation. This article, written by Nitin Ahuja and James Reynolds from the Neurogastroenterology and Motility Program at the University of Pennsylvania, Philadelphia, addresses a common topic in our field, and can also be found in the February print issue of GI & Hepatology News. To complement this article, there is a corresponding video abstract that can be viewed.
Also in this issue, Richard Peek (Vanderbilt University, Nashville, Tenn.) – one of the Coeditors in Chief of Gastroenterology – provides a summary of the newly created 1-year editorial fellowship for the AGA’s flagship journal. This is a fantastic new opportunity and you can learn firsthand about the experience of the inaugural editorial fellow, Eric Shah (University of Michigan, Ann Arbor), in an accompanying video. Additionally, as helping patients make a successful transition from a pediatric GI practice to an adult GI practice can be very challenging, in this issue Manreet Kaur and Allyson Wyatt (Baylor College of Medicine, Houston) provide a primer on how to successfully aid in this transition.
Are you considering a career in hospital administration? If so, you will enjoy reading about pursuing a career in hospital administration from Brijen Shah, who is the chief medical officer of Mount Sinai Queens (Icahn School of Medicine at Mount Sinai, New York). Have you been to one of the AGA’s Regional Practice Skills Workshops? These workshops are sponsored by the AGA Trainee and Early Career Committee and held in a growing number of cities across the country. In this issue, Munish Ashat (University of Iowa, Iowa City) provides a recap of the workshop he attended, complete with many useful career pearls.
I hope that you also enjoy the other features in the new e-newsletter format of The New Gastroenterologist. I especially want to point out one of our new sections entitled “In Case You Missed It.” As we all undoubtedly experience information overload with so many new articles released each month, this section collects relevant articles from the numerous AGA publications and consolidates them to ensure you don’t miss any of this great content.
If you are interested in contributing to future issues of The New Gastroenterologist or if there are topics that would interest you, please let us know. You can contact me ([email protected]) or the managing editor of The New Gastroenterologist, Ryan Farrell ([email protected]).
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an instructor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
Dear Colleagues,
It is with great excitement that I introduce the first e-newsletter version of The New Gastroenterologist! As more content in medicine, and life in general, is moving toward digital platforms, we at the AGA believe this transition will improve both content dissemination and accessibility to all our readers. In this new format, we will continue to provide articles on topics of importance to the early-career community, expand our offerings by including the new “In Focus” articles (concise overviews of GI topics) both digitally and in GI & Hepatology News print issues, as well as increase the use of multimedia resources, such as videos, to further enhance our content.
In this issue of The New Gastroenterologist, our In Focus article provides a practical overview of the management of chronic constipation. This article, written by Nitin Ahuja and James Reynolds from the Neurogastroenterology and Motility Program at the University of Pennsylvania, Philadelphia, addresses a common topic in our field, and can also be found in the February print issue of GI & Hepatology News. To complement this article, there is a corresponding video abstract that can be viewed.
Also in this issue, Richard Peek (Vanderbilt University, Nashville, Tenn.) – one of the Coeditors in Chief of Gastroenterology – provides a summary of the newly created 1-year editorial fellowship for the AGA’s flagship journal. This is a fantastic new opportunity and you can learn firsthand about the experience of the inaugural editorial fellow, Eric Shah (University of Michigan, Ann Arbor), in an accompanying video. Additionally, as helping patients make a successful transition from a pediatric GI practice to an adult GI practice can be very challenging, in this issue Manreet Kaur and Allyson Wyatt (Baylor College of Medicine, Houston) provide a primer on how to successfully aid in this transition.
Are you considering a career in hospital administration? If so, you will enjoy reading about pursuing a career in hospital administration from Brijen Shah, who is the chief medical officer of Mount Sinai Queens (Icahn School of Medicine at Mount Sinai, New York). Have you been to one of the AGA’s Regional Practice Skills Workshops? These workshops are sponsored by the AGA Trainee and Early Career Committee and held in a growing number of cities across the country. In this issue, Munish Ashat (University of Iowa, Iowa City) provides a recap of the workshop he attended, complete with many useful career pearls.
I hope that you also enjoy the other features in the new e-newsletter format of The New Gastroenterologist. I especially want to point out one of our new sections entitled “In Case You Missed It.” As we all undoubtedly experience information overload with so many new articles released each month, this section collects relevant articles from the numerous AGA publications and consolidates them to ensure you don’t miss any of this great content.
If you are interested in contributing to future issues of The New Gastroenterologist or if there are topics that would interest you, please let us know. You can contact me ([email protected]) or the managing editor of The New Gastroenterologist, Ryan Farrell ([email protected]).
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an instructor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
AGA Regional Practice Skills Workshops: New perspectives for young GI physicians
Medicine is an evolving field, and in this era of ever-changing medicine, physicians-in-training often lag behind in understanding the nuances of “real-world” medicine. From negotiating job contracts to understanding medical billing, coding systems, and performance metrics, physicians who are fresh out of training often feel ill prepared to deal with these issues that are rarely discussed during fellowship.
The American Gastroenterological Association’s Regional Practice Skills Workshops are designed to fill this void and provide the tools necessary to navigate the challenging transition from training into practice. Since the first pilot workshops were held in 2014, AGA’s Trainee and Early Career Committee has been diligently working to expand the number of workshop sites so that more trainees can benefit from them. This year, workshops will be held in Columbus, Ohio (Feb. 24), and in Philadelphia (April 11). An exciting development in 2017 was the opportunity to live stream the event held at the University of California, Los Angeles, to Stanford (Calif.) University and the University of Iowa, Iowa City.
This aforementioned workshop at UCLA was divided into two sessions. The first was focused on “Practice Options,” with talks geared toward highlighting the different practice models available in the GI market, including positions in academia, private practice, and mixed environments.
William Chey, MD, a professor of medicine at the University of Michigan, Ann Arbor, shared his experience as an academic gastroenterologist as well as his experience in managing a GI consulting firm. His advice to young gastroenterologists was to diversify. He suggested options such as working for pharmaceutical companies, being involved in drug trials, working in the innovation industry, and proactively seeking leadership positions in different organizations. V. Raman Muthusamy MD, AGAF, a clinical professor of medicine at UCLA, led the discussion with the million-dollar question: What is my net worth? He suggested doing some homework before negotiating one’s salary by visiting the Medical Group Management Association’s website. Having this information can provide a trainee with a head start in the negotiation process. Dr. Muthusamy recommended recalculating one’s net worth every 5 years and renegotiating your contract based on this information. In addition to possibly leading to a salary boost, such knowledge will render internal validation and boost self-confidence about one’s skill set. Keep in mind however, that checking this too often can be adversely distracting. Lynn S. Connolly, MD, also of UCLA brought to light the important fact that female gastroenterologists are often paid lower salaries than their male counterparts, even after adjusting for vacation time, practice type, and work hours. She urged female gastroenterologists not to undervalue themselves and avoid falling into this pitfall. Lin Chang, MD, a professor of medicine at UCLA, reinforced the need for young GI fellows to be passionate about the path they choose and to not make random choices or decisions based on convenience alone.
Gareth Dulai, MD, a gastroenterologist with Kaiser Permanente in Downey, CA, discussed the advantages of working in a big company, including salaries that are transparent and match the national average. One also does not have to worry about hiring staff and managing overhead costs. Martha Hierro, MD, who has been in private practice since fellowship, felt that a private group practice enables a higher salary potential and better flexibility with one’s schedule. Her group also has a pathology lab, research lab, and imaging center, which further augments the group’s earnings. The downsides to private practice, compared with bigger academic settings, include cumbersome negotiations with insurance companies and financial constraints when purchasing new technology. She advised young GI physicians to go through the partnership clause very carefully before joining any private practice. She recommended being prepared and fully informed before negotiating a contract, including speaking to other practicing gastroenterologists in the area about the earning potential in the practice. In the end, both speakers agreed that all types of practices have pros and cons and one can always move from one setting to another.
For young GI fellows who want to work as administrators, the common consensus among the panel members was that fellows should attend leadership courses at national meetings early in training and participate in the committees of national organizations like the AGA. Reaching out to educators and mentors is of key importance. Dr. Chey recommended that, when fellows are provided with an opportunity to work with a potential mentor, they should think it through before accepting the opportunity and, if they do accept it, make sure they finish the task in a timely manner.
The second session of the workshop was geared toward the interview process. James H. Tabibian, MD, PhD, of the University of California, Davis, shared some useful tips for job hunting. It is never too early to start the process of job hunting, and timing depends on the type of position one is seeking. For a competitive position, it may be best to start the process early. When looking for jobs, contact methods could include in-person encounters at national meetings, such as Digestive Disease Week, or through a mutual colleague or mentor. Emails to potential future employers should be succinct with an updated resume attached. Most importantly, make sure to follow up in a professional manner.
Dr. Connolly, who also spoke about interviewing, pointed out that one should always ask questions about the program and never offer any negative information about oneself. Discussing salary potential during an interview may not be perceived as a positive sign. One might ask the interviewer about what things the interviewer enjoys the most at work, what defines success in this position at the institution, what constitutes an ideal candidate for the program, and what is the growth plan for the program over the next 5-10 years. For subspecialty interviews, some questions that are good to ask include the volume of procedures done at the institute, what might a typical day for a fellow look like, where do fellows typically work after finishing, and how is the call schedule set up. In the end, look confident, be humble, and believe in yourself. You control how you are perceived.
Once you are offered a job, the next big task is contract negotiation. Negotiating a contract can be very time consuming and stressful. Some key concepts to keep in mind are: a) prepare ahead of time and know the institution well; b) the more offers you have, the more leverage you can get; c) take adequate time to evaluate the contract before signing; d) establish which clauses are nonnegotiable for you; e) try to get something back for everything you give up during negotiations; f) do not negotiate with yourself; g) keep calm and be flexible; and h) know what you want out of your job. Always keep in mind base salary and bonuses, student loan repayment, relocation expenses, medical and disability insurance, and malpractice insurance coverage. Always consider the possibility of buying into the practice. Be wary of indemnification and unreasonable noncompete clauses.
Overall, my colleagues and I found the workshop to be extremely informative. The live stream format was very well received, and as an audience, we felt engaged and encouraged to participate. We certainly appreciated the opportunity to ask questions in real time. This format allowed all our fellows to participate without needing to travel and to gain access to invaluable content that will surely help us in making important career decisions.
Dr. Ashat is a first-year gastroenterology fellow at The University of Iowa, Iowa City.
Medicine is an evolving field, and in this era of ever-changing medicine, physicians-in-training often lag behind in understanding the nuances of “real-world” medicine. From negotiating job contracts to understanding medical billing, coding systems, and performance metrics, physicians who are fresh out of training often feel ill prepared to deal with these issues that are rarely discussed during fellowship.
The American Gastroenterological Association’s Regional Practice Skills Workshops are designed to fill this void and provide the tools necessary to navigate the challenging transition from training into practice. Since the first pilot workshops were held in 2014, AGA’s Trainee and Early Career Committee has been diligently working to expand the number of workshop sites so that more trainees can benefit from them. This year, workshops will be held in Columbus, Ohio (Feb. 24), and in Philadelphia (April 11). An exciting development in 2017 was the opportunity to live stream the event held at the University of California, Los Angeles, to Stanford (Calif.) University and the University of Iowa, Iowa City.
This aforementioned workshop at UCLA was divided into two sessions. The first was focused on “Practice Options,” with talks geared toward highlighting the different practice models available in the GI market, including positions in academia, private practice, and mixed environments.
William Chey, MD, a professor of medicine at the University of Michigan, Ann Arbor, shared his experience as an academic gastroenterologist as well as his experience in managing a GI consulting firm. His advice to young gastroenterologists was to diversify. He suggested options such as working for pharmaceutical companies, being involved in drug trials, working in the innovation industry, and proactively seeking leadership positions in different organizations. V. Raman Muthusamy MD, AGAF, a clinical professor of medicine at UCLA, led the discussion with the million-dollar question: What is my net worth? He suggested doing some homework before negotiating one’s salary by visiting the Medical Group Management Association’s website. Having this information can provide a trainee with a head start in the negotiation process. Dr. Muthusamy recommended recalculating one’s net worth every 5 years and renegotiating your contract based on this information. In addition to possibly leading to a salary boost, such knowledge will render internal validation and boost self-confidence about one’s skill set. Keep in mind however, that checking this too often can be adversely distracting. Lynn S. Connolly, MD, also of UCLA brought to light the important fact that female gastroenterologists are often paid lower salaries than their male counterparts, even after adjusting for vacation time, practice type, and work hours. She urged female gastroenterologists not to undervalue themselves and avoid falling into this pitfall. Lin Chang, MD, a professor of medicine at UCLA, reinforced the need for young GI fellows to be passionate about the path they choose and to not make random choices or decisions based on convenience alone.
Gareth Dulai, MD, a gastroenterologist with Kaiser Permanente in Downey, CA, discussed the advantages of working in a big company, including salaries that are transparent and match the national average. One also does not have to worry about hiring staff and managing overhead costs. Martha Hierro, MD, who has been in private practice since fellowship, felt that a private group practice enables a higher salary potential and better flexibility with one’s schedule. Her group also has a pathology lab, research lab, and imaging center, which further augments the group’s earnings. The downsides to private practice, compared with bigger academic settings, include cumbersome negotiations with insurance companies and financial constraints when purchasing new technology. She advised young GI physicians to go through the partnership clause very carefully before joining any private practice. She recommended being prepared and fully informed before negotiating a contract, including speaking to other practicing gastroenterologists in the area about the earning potential in the practice. In the end, both speakers agreed that all types of practices have pros and cons and one can always move from one setting to another.
For young GI fellows who want to work as administrators, the common consensus among the panel members was that fellows should attend leadership courses at national meetings early in training and participate in the committees of national organizations like the AGA. Reaching out to educators and mentors is of key importance. Dr. Chey recommended that, when fellows are provided with an opportunity to work with a potential mentor, they should think it through before accepting the opportunity and, if they do accept it, make sure they finish the task in a timely manner.
The second session of the workshop was geared toward the interview process. James H. Tabibian, MD, PhD, of the University of California, Davis, shared some useful tips for job hunting. It is never too early to start the process of job hunting, and timing depends on the type of position one is seeking. For a competitive position, it may be best to start the process early. When looking for jobs, contact methods could include in-person encounters at national meetings, such as Digestive Disease Week, or through a mutual colleague or mentor. Emails to potential future employers should be succinct with an updated resume attached. Most importantly, make sure to follow up in a professional manner.
Dr. Connolly, who also spoke about interviewing, pointed out that one should always ask questions about the program and never offer any negative information about oneself. Discussing salary potential during an interview may not be perceived as a positive sign. One might ask the interviewer about what things the interviewer enjoys the most at work, what defines success in this position at the institution, what constitutes an ideal candidate for the program, and what is the growth plan for the program over the next 5-10 years. For subspecialty interviews, some questions that are good to ask include the volume of procedures done at the institute, what might a typical day for a fellow look like, where do fellows typically work after finishing, and how is the call schedule set up. In the end, look confident, be humble, and believe in yourself. You control how you are perceived.
Once you are offered a job, the next big task is contract negotiation. Negotiating a contract can be very time consuming and stressful. Some key concepts to keep in mind are: a) prepare ahead of time and know the institution well; b) the more offers you have, the more leverage you can get; c) take adequate time to evaluate the contract before signing; d) establish which clauses are nonnegotiable for you; e) try to get something back for everything you give up during negotiations; f) do not negotiate with yourself; g) keep calm and be flexible; and h) know what you want out of your job. Always keep in mind base salary and bonuses, student loan repayment, relocation expenses, medical and disability insurance, and malpractice insurance coverage. Always consider the possibility of buying into the practice. Be wary of indemnification and unreasonable noncompete clauses.
Overall, my colleagues and I found the workshop to be extremely informative. The live stream format was very well received, and as an audience, we felt engaged and encouraged to participate. We certainly appreciated the opportunity to ask questions in real time. This format allowed all our fellows to participate without needing to travel and to gain access to invaluable content that will surely help us in making important career decisions.
Dr. Ashat is a first-year gastroenterology fellow at The University of Iowa, Iowa City.
Medicine is an evolving field, and in this era of ever-changing medicine, physicians-in-training often lag behind in understanding the nuances of “real-world” medicine. From negotiating job contracts to understanding medical billing, coding systems, and performance metrics, physicians who are fresh out of training often feel ill prepared to deal with these issues that are rarely discussed during fellowship.
The American Gastroenterological Association’s Regional Practice Skills Workshops are designed to fill this void and provide the tools necessary to navigate the challenging transition from training into practice. Since the first pilot workshops were held in 2014, AGA’s Trainee and Early Career Committee has been diligently working to expand the number of workshop sites so that more trainees can benefit from them. This year, workshops will be held in Columbus, Ohio (Feb. 24), and in Philadelphia (April 11). An exciting development in 2017 was the opportunity to live stream the event held at the University of California, Los Angeles, to Stanford (Calif.) University and the University of Iowa, Iowa City.
This aforementioned workshop at UCLA was divided into two sessions. The first was focused on “Practice Options,” with talks geared toward highlighting the different practice models available in the GI market, including positions in academia, private practice, and mixed environments.
William Chey, MD, a professor of medicine at the University of Michigan, Ann Arbor, shared his experience as an academic gastroenterologist as well as his experience in managing a GI consulting firm. His advice to young gastroenterologists was to diversify. He suggested options such as working for pharmaceutical companies, being involved in drug trials, working in the innovation industry, and proactively seeking leadership positions in different organizations. V. Raman Muthusamy MD, AGAF, a clinical professor of medicine at UCLA, led the discussion with the million-dollar question: What is my net worth? He suggested doing some homework before negotiating one’s salary by visiting the Medical Group Management Association’s website. Having this information can provide a trainee with a head start in the negotiation process. Dr. Muthusamy recommended recalculating one’s net worth every 5 years and renegotiating your contract based on this information. In addition to possibly leading to a salary boost, such knowledge will render internal validation and boost self-confidence about one’s skill set. Keep in mind however, that checking this too often can be adversely distracting. Lynn S. Connolly, MD, also of UCLA brought to light the important fact that female gastroenterologists are often paid lower salaries than their male counterparts, even after adjusting for vacation time, practice type, and work hours. She urged female gastroenterologists not to undervalue themselves and avoid falling into this pitfall. Lin Chang, MD, a professor of medicine at UCLA, reinforced the need for young GI fellows to be passionate about the path they choose and to not make random choices or decisions based on convenience alone.
Gareth Dulai, MD, a gastroenterologist with Kaiser Permanente in Downey, CA, discussed the advantages of working in a big company, including salaries that are transparent and match the national average. One also does not have to worry about hiring staff and managing overhead costs. Martha Hierro, MD, who has been in private practice since fellowship, felt that a private group practice enables a higher salary potential and better flexibility with one’s schedule. Her group also has a pathology lab, research lab, and imaging center, which further augments the group’s earnings. The downsides to private practice, compared with bigger academic settings, include cumbersome negotiations with insurance companies and financial constraints when purchasing new technology. She advised young GI physicians to go through the partnership clause very carefully before joining any private practice. She recommended being prepared and fully informed before negotiating a contract, including speaking to other practicing gastroenterologists in the area about the earning potential in the practice. In the end, both speakers agreed that all types of practices have pros and cons and one can always move from one setting to another.
For young GI fellows who want to work as administrators, the common consensus among the panel members was that fellows should attend leadership courses at national meetings early in training and participate in the committees of national organizations like the AGA. Reaching out to educators and mentors is of key importance. Dr. Chey recommended that, when fellows are provided with an opportunity to work with a potential mentor, they should think it through before accepting the opportunity and, if they do accept it, make sure they finish the task in a timely manner.
The second session of the workshop was geared toward the interview process. James H. Tabibian, MD, PhD, of the University of California, Davis, shared some useful tips for job hunting. It is never too early to start the process of job hunting, and timing depends on the type of position one is seeking. For a competitive position, it may be best to start the process early. When looking for jobs, contact methods could include in-person encounters at national meetings, such as Digestive Disease Week, or through a mutual colleague or mentor. Emails to potential future employers should be succinct with an updated resume attached. Most importantly, make sure to follow up in a professional manner.
Dr. Connolly, who also spoke about interviewing, pointed out that one should always ask questions about the program and never offer any negative information about oneself. Discussing salary potential during an interview may not be perceived as a positive sign. One might ask the interviewer about what things the interviewer enjoys the most at work, what defines success in this position at the institution, what constitutes an ideal candidate for the program, and what is the growth plan for the program over the next 5-10 years. For subspecialty interviews, some questions that are good to ask include the volume of procedures done at the institute, what might a typical day for a fellow look like, where do fellows typically work after finishing, and how is the call schedule set up. In the end, look confident, be humble, and believe in yourself. You control how you are perceived.
Once you are offered a job, the next big task is contract negotiation. Negotiating a contract can be very time consuming and stressful. Some key concepts to keep in mind are: a) prepare ahead of time and know the institution well; b) the more offers you have, the more leverage you can get; c) take adequate time to evaluate the contract before signing; d) establish which clauses are nonnegotiable for you; e) try to get something back for everything you give up during negotiations; f) do not negotiate with yourself; g) keep calm and be flexible; and h) know what you want out of your job. Always keep in mind base salary and bonuses, student loan repayment, relocation expenses, medical and disability insurance, and malpractice insurance coverage. Always consider the possibility of buying into the practice. Be wary of indemnification and unreasonable noncompete clauses.
Overall, my colleagues and I found the workshop to be extremely informative. The live stream format was very well received, and as an audience, we felt engaged and encouraged to participate. We certainly appreciated the opportunity to ask questions in real time. This format allowed all our fellows to participate without needing to travel and to gain access to invaluable content that will surely help us in making important career decisions.
Dr. Ashat is a first-year gastroenterology fellow at The University of Iowa, Iowa City.
Chronic constipation: Practical approaches and novel therapies
While constipation is one of the most common symptoms managed by practicing gastroenterologists, it can also be among the most challenging. As a presenting complaint, constipation manifests with widely varying degrees of severity and may be seen in all age groups, ethnicities, and socioeconomic backgrounds. Its implications can include chronic and serious functional impairment as well as protracted and often excessive health care utilization. A growing number of pharmacologic and nonpharmacologic interventions have become available and proven to be effective when appropriately deployed. As such, health care providers and particularly gastroenterologists should strive to develop logical and efficient strategies for addressing this common disorder.
Clinical importance
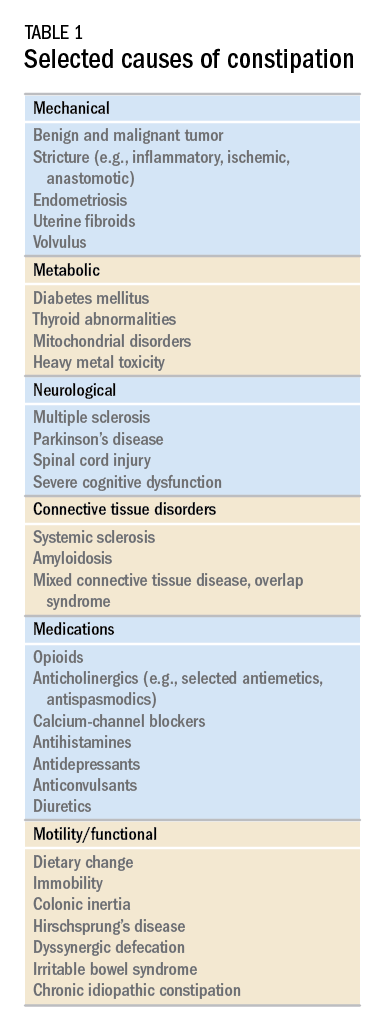
While there are a variety of etiologies for constipation (Table 1), a large proportion of chronic cases fall within the framework of functional gastrointestinal disorders, a category with a substantial burden of disease across the population. Prevalence estimates vary, but constipation likely affects between 12% and 20% of the North American population.1 Research has demonstrated significant health care expenditures associated with chronic constipation management; U.S. estimates suggest direct costs on the order of hundreds of millions of dollars per year, roughly half of which are attributable to inpatient care.2 The financial burden of constipation also includes indirect costs associated with absenteeism as well as the risks of hospitalization and invasive procedures.3
Physical and emotional complications can be likewise significant and affect all age groups, from newborns to patients in the last days of life. Hirschsprung’s disease, for example, can lead to life-threatening sequelae in infancy, such as spontaneous perforation or enterocolitis, or more prolonged functional impairments when it remains undiagnosed. Severe constipation in childhood can lead to encopresis, translating in turn into ostracism and impaired social functioning. Fecal incontinence associated with overflow diarrhea is common and debilitating, particularly in the elderly population.
The potential mechanical complications of constipation lead to its overlap with a variety of other gastrointestinal complaints. For example, the difficulties of passing inspissated stool can provoke lower gastrointestinal bleeding from irritated hemorrhoids, anal fissures, stercoral ulcers, or prolapsed rectal tissue. Retained stool can also lead to upper gastrointestinal symptoms such as postprandial bloating or early satiety.4 Delayed fecal discharge can promote an increase in fermentative microbiota, associated in turn with the production of short-chain fatty acids, methane, and other gaseous byproducts.
The initial assessment
History
Taking an appropriate history is an essential step toward achieving a successful outcome. Presenting concerns related to constipation can range from hard, infrequent, or small-volume stools; abdominal or rectal pain associated with the process of elimination; and bloating, nausea, or early satiety. A sound diagnosis requires a keen understanding of what patients mean when they indicate that they are constipated, an accurate assessment of its impact on quality of life, and a careful inventory of potentially associated complications.
It is critical to define the duration of the problem. Not infrequently, patients will focus on recent events while failing to reveal that altered bowel habits or other functional symptoms have been problematic for years. Reminding the patients to “begin at the beginning” can aid enormously in contextualizing their complaints. Individuals with longstanding symptoms and previously negative evaluations are much less likely to present with a new organic disease than are those in whom symptoms have truly arisen de novo.
Defining constipation by frequency of bowel eliminations alone has proved inaccurate at predicting actual severity. This is in part because the bowel movement frequency varies widely in healthy individuals (anywhere from thrice daily to once every 3 days) and in part because the primary indicator of effective evacuation is not frequency but volume – a much more difficult quantity for patients to gauge.5 The Bristol Stool Scale is a simple, standardized tool that more accurately evaluates the presence or absence of colonic dysfunction. For example, patients passing Type 1-2 (hard or lumpy) stools often have an element of constipation that needs to be addressed.6 However, the interpretation of stool consistency assessments is still aided by awareness of both frequency and volume. A patient passing multiple small-volume Type 6-7 (loose or watery) stools may be the most constipated, presenting with overflow or paradoxical diarrhea attributable to fecal impaction.
Physical examination
An expert physical exam is another essential aspect of the initial assessment. Alarm features can be elicited in this context as well via signs of pallor, weight loss, blood in the stool, physical abuse, or advanced psychological distress. Attention should also be paid to signs of a systemic disorder that might be associated with gastrointestinal dysmotility including previously unrecognized signs of Raynaud’s syndrome, sclerodactyly, amyloidosis, surgical scars, and joint hypermobility.7,8 Abdominal bloating, a frequently vague symptomatic complaint, can be correlated with the presence or absence of distention as perceived by the patient and/or the examiner.9
Any initial evaluation of constipation should also include a detailed digital rectal exam. A complete examination should include a careful visual assessment of the perianal region for external lesions and of the degree and directional appropriateness of pelvic floor excursion (perineal elevation and descent) during squeeze and simulated defecation maneuvers, respectively. Digital examination should include palpation for the presence or absence of pain as well as stool, blood, or masses in the rectal vault, as well as an assessment of sphincter tone at baseline, with squeeze, and with simulated defecation. Rectal pressure generation with the latter maneuver can also be qualitatively assessed. Research has suggested moderate agreement between the digital rectal examination and formal manometric evaluation in diagnosing dyssynergic defecation, underscoring the former’s utility in guiding initial management decisions.10
Testing
It is reasonable to exclude metabolic, inflammatory, or other secondary etiologies of constipation in patients in whom history or examination raises suspicion. Likewise, colonoscopy should be considered in patients with alarm features or who are due for age-appropriate screening. That said, in the absence of risk factors or ancillary signs and symptoms, a detailed diagnostic work-up is often unnecessary. The AGA’s Medical Position Statement on Constipation recommends a complete blood count as the only test to be ordered on a standard basis in the work-up of constipation.11
In patients new to one’s practice, the diligent retrieval of prior records is one of the most efficient ways to avoid wasting health care resources. Locating an old abdominal radiograph that demonstrates extensive retained stool can not only secure the diagnosis for vague symptomatic complaints but also obviate the need for more extensive testing. One should instead consider how symptom duration and the associated changes in objectives measures such as weight and laboratory parameters can be used to justify or refute the need for repeating costly or invasive studies.
It is important to consider the potential contribution of defecatory dyssynergy to chronic constipation early in a patient’s presentation, and to return to this possibility in the future if initial therapeutic interventions are unsuccessful. An abnormal qualitative assessment on digital rectal examination should trigger a more formal characterization of the patient’s defecatory mechanics via anorectal manometry (ARM) and balloon expulsion testing (BET). Likewise, a lack of response to initial pharmacotherapy should prompt suspicion for outlet dysfunction, which can be queried with functional testing even if a rectal examination is qualitatively unrevealing.
Initial approach to the chronically constipated patient
The aforementioned AGA Medical Position Statement provides a helpful algorithm regarding the diagnostic approach to constipation (Figure 1). In the absence of concern for secondary etiologies of constipation, an initial therapeutic trial of dietary, lifestyle, and medication-based intervention is reasonable for mild symptoms. Patients should be encouraged to strive for 25-30 grams of dietary fiber intake per day. For patients unable to reach this goal via high-fiber foods alone, psyllium husk is a popular supplement, but it should be initiated at modest doses to mitigate the risk of bloating. Fiber may be supplemented with the use of osmotic laxatives (e.g., polyethylene glycol) with instructions that the initial dose may be modified as needed to optimal effectiveness. Selective response to rectal therapies (e.g., bisacodyl or glycerin suppositories) over osmotic laxatives may also suggest utility in early queries of outlet dysfunction.
An abdominal radiograph can be helpful not only to diagnose constipation but also to assess the stool burden present at the time of beginning treatment. For patients presenting with a significant degree of fecal loading, an initial bowel cleanse with four liters of osmotically balanced polyethylene glycol can be a useful means of eliminating background fecal impactions that might have mitigated the effectiveness of initial therapies in the past or that might reduce the effectiveness of daily laxative therapy moving forward.
Patients with a diagnosis of defecatory dyssynergy made via ARM/BET should be referred to pelvic floor physical therapy with biofeedback. Recognizing that courses of therapy are highly individualized in practice, randomized controlled trials suggest symptom improvement in 70%-80% of patients, with the majority also demonstrating maintenance of response.12 Biofeedback appears to be an essential component of this modality based on meta-analysis data and should be requested specifically by the referring provider.13
Pharmacologic agents

For those patients with more severe initial presentations or whose symptoms persist despite initial medical management, there are several pharmacologic agents that may be considered on a prescription basis (Table 2). Linaclotide, a minimally absorbed guanylate cyclase agonist, is approved by the Food and Drug Administration for patients with irritable bowel syndrome with constipation (IBS-C) and chronic idiopathic constipation (CIC). Improvements in constipation tend to occur over a slightly shorter timeline than in abdominal pain, though both have been demonstrated in comparison to placebo.14,15 Plecanatide, a newer agent with a similar mechanism of action, has demonstrated improvements in bowel movement frequency and was recently approved for CIC.16 Lubiprostone, a chloride channel agonist, has demonstrated benefit for IBS-C and CIC as well, though its side effect profile is more varied, including dose-related nausea in up to 30% of patients.17
For patients with opioid-induced constipation who cannot wean from the opioid medications, the peripheral acting mu-opioid receptor antagonists may be quite helpful. These include injectable as well as oral formulations (e.g., methylnaltrexone and naloxegol, respectively) with additional agents under active investigation in particular clinical subsets (e.g., naldemedine for patients with cancer-related pain).18,19 Prucalopride, a selective serotonin receptor agonist, has also demonstrated benefit for constipation; it is available abroad but not yet approved for use in the United States.20 Prucalopride shares its primary mechanism of action (selective agonism of the 5HT4 serotonin receptor) with cisapride, a previously quite popular gastrointestinal motility agent that was subsequently withdrawn from the U.S. market because of arrhythmia risk.21 This risk is likely attributable to cisapride’s dual binding affinity for potassium channels, a feature that prucalopride does not share; as such, cardiotoxicity is not an active concern with the latter agent.22
Still other pharmacologic agents with novel mechanisms of action are currently under investigation. Tenapanor, an inhibitor of a particular sodium/potassium exchanger in the gut lumen, mitigates intestinal sodium absorption, which increases fluid volume and transit. A recent phase 2 study demonstrated significantly increased stool frequency relative to placebo in patients with IBS-C.23 Elobixibat, an ileal bile acid transport inhibitor, promotes colonic retention of bile acids and, in placebo-controlled studies, has led to accelerated colonic transit and an increased number of spontaneous bowel movements in patients with CIC.24
Persistent constipation
In cases of refractory constipation (in practical terms, symptoms that persist despite trials of escalating medical therapy over at least 6 weeks), it is worth revisiting the question of etiology. Querying defecatory dyssynergy via ARM/BET, if not pursued prior to trials of newer pharmacologic agents, should certainly be explored in the event that such trials fail. Inconclusive results of ARM and BET testing, or BET abnormalities that persist despite a course of physical therapy with biofeedback, may raise suspicion for pelvic organ prolapse, which may be formally evaluated with defecography. Additional testing for metabolic or structural predispositions toward constipation may also be reasonable at this juncture.
Formal colonic transit testing via radio-opaque markers, scintigraphy, or the wireless motility capsule is often inaccurate in the setting of dyssynergic defecation and should be pursued only after this entity has been excluded or successfully treated.25 While there are not many practical distinctions at present in the therapeutic management of slow-transit versus normal-transit constipation, the use of novel medications with an explicitly prokinetic mechanism of action may be reasonable to consider in the setting of a document delay in colonic transit. Such delays can also help justify further specialized diagnostic testing (e.g., colonic manometry), and, in rare refractory cases, surgical intervention.
Consideration of colectomy should be reserved for highly selected patients with delayed colonic transit, normal defecatory mechanics, and the absence of potentially explanatory background conditions (e.g., connective tissue disease). Clear evidence of an underlying colonic myopathy or neuropathy may militate in favor of a more targeted surgical intervention (e.g., subtotal colectomy) or guide one’s clinical evaluation toward alternative systemic diagnoses. A diverting loop ileostomy with interval assessment of symptoms may be useful to clarify the potential benefits of colectomy while preserving the option of operative reversal. Proximal transit delays should be definitively excluded before pursuing colonic resections given evidence that multisegment transit delays portend significantly worse postoperative outcomes.26
Conclusion
Constipation is a common, sometimes confusing presenting complaint and the variety of established and emergent options for diagnosis and therapy can lend themselves to haphazard application. Patients and providers both are well served by a clinical approach, rooted in a comprehensive history and examination, that begins to organize these options in thoughtful sequence.
Dr. Ahuja is assistant professor of clinical medicine, division of gastroenterology; Dr. Reynolds is professor of clinical medicine, and director of the program in neurogastroenterology and motility, division of gastroenterology, Perelman School of Medicine, University of Pennsylvania, Philadelphia.
References
1. Higgins P.D., Johanson J.F. Epidemiology of constipation in North America: a systematic review. Am J Gastroenterol. 2004 Apr;99(4):750-9. PubMed PMID: 15089911.
2. Martin B.C., Barghout V., Cerulli A. Direct medical costs of constipation in the United States. Manage Care Interface. 2006 Dec;19(12):43-9. PubMed PMID: 17274481.
3. Sun S.X., Dibonaventura M., Purayidathil F.W., et al. Impact of chronic constipation on health-related quality of life, work productivity, and healthcare resource use: an analysis of the National Health and Wellness Survey. Dig Dis Sc. 2011 Sep;56(9):2688-95. PubMed PMID: 21380761.
4. Heidelbaugh J.J., Stelwagon M., Miller S.A., et al. The spectrum of constipation-predominant irritable bowel syndrome and chronic idiopathic constipation: US survey assessing symptoms, care seeking, and disease burden. Am J Gastroenterol. 2015 Apr;110(4):580-7.
5. Mitsuhashi S., Ballou S., Jiang Z.G., et al. Characterizing normal bowel frequency and consistency in a representative sample of adults in the United States (NHANES). Am J Gastroenterol. 2017 Aug 01. PubMed PMID: 28762379.
6. Saad R.J., Rao S.S., Koch K.L., et al. Do stool form and frequency correlate with whole-gut and colonic transit? Results from a multicenter study in constipated individuals and healthy controls. Am J Gastroenterol. 2010 Feb;105(2):403-11. PubMed PMID: 19888202.
7. Castori M., Morlino S., Pascolini G., et al. Gastrointestinal and nutritional issues in joint hypermobility syndrome/Ehlers-Danlos syndrome, hypermobility type. American Journal of Medical Genetics Part C, Semin Med Genet. 2015 Mar;169C(1):54-75. PubMed PMID: 25821092.
8. Nagaraja V., McMahan Z.H., Getzug T., Khanna D. Management of gastrointestinal involvement in scleroderma. Curr Treatm Opt Rheumatol. 2015 Mar 01;1(1):82-105. PubMed PMID: 26005632. Pubmed Central PMCID: 4437639.
9. Malagelada J.R., Accarino A., Azpiroz F. Bloating and abdominal distension: Old misconceptions and current knowledge. Am J Gastroenterol. 2017 Aug;112(8):1221-31. PubMed PMID: 28508867.
10. Soh J.S., Lee H.J., Jung K.W., et al. The diagnostic value of a digital rectal examination compared with high-resolution anorectal manometry in patients with chronic constipation and fecal incontinence. Am J Gastroenterol. 2015 Aug;110(8):1197-204. PubMed PMID: 26032152.
11. American Gastroenterological Association, Bharucha A.E., Dorn S.D., Lembo A., Pressman A. American Gastroenterological Association medical position statement on constipation. Gastroenterology. 2013 Jan;144(1):211-7. PubMed PMID: 23261064.
12. Skardoon G.R., Khera A.J., Emmanuel A.V., Burgell R.E. Review article: dyssynergic defaecation and biofeedback therapy in the pathophysiology and management of functional constipation. Aliment Pharmacol Therapeut. 2017 Aug;46(4):410-23. PubMed PMID: 28660663.
13. Koh C.E., Young C.J., Young J.M., Solomon M.J. Systematic review of randomized controlled trials of the effectiveness of biofeedback for pelvic floor dysfunction. Br J Surg. 2008 Sep;95(9):1079-87. PubMed PMID: 18655219.
14. Rao S., Lembo A.J., Shiff S.J., et al. A 12-week, randomized, controlled trial with a 4-week randomized withdrawal period to evaluate the efficacy and safety of linaclotide in irritable bowel syndrome with constipation. Am J Gastroenterol. 2012 Nov;107(11):1714-24; quiz p 25. PubMed PMID: 22986440. Pubmed Central PMCID: 3504311.
15. Lacy B.E., Schey R., Shiff S.J., et al. Linaclotide in chronic idiopathic constipation patients with moderate to severe abdominal bloating: A randomized, controlled trial. PloS One. 2015;10(7):e0134349. PubMed PMID: 26222318. Pubmed Central PMCID: 4519259.
16. Miner P.B., Jr., Koltun W.D., Wiener G.J., et al. A randomized phase III clinical trial of plecanatide, a uroguanylin analog, in patients with chronic idiopathic constipation. Am J Gastroenterol. 2017 Apr;112(4):613-21. PubMed PMID: 28169285. Pubmed Central PMCID: 5415706.
17. Johanson J.F., Drossman D.A., Panas R., Wahle A., Ueno R. Clinical trial: phase 2 study of lubiprostone for irritable bowel syndrome with constipation. Aliment Pharmacol Therapeut. 2008 Apr;27(8):685-96. PubMed PMID: 18248656.
18. Chey W.D., Webster L., Sostek M., Lappalainen J., Barker P.N., Tack J. Naloxegol for opioid-induced constipation in patients with noncancer pain. N Engl J Med. 2014 Jun 19;370(25):2387-96. PubMed PMID: 24896818.
19. Katakami N., Oda K., Tauchi K., et al. Phase IIb, randomized, double-blind, placebo-controlled study of naldemedine for the treatment of opioid-induced constipation in patients with cancer. J Clin Oncol. 2017 Jun 10;35(17):1921-8. PubMed PMID: 28445097.
20. Sajid M.S., Hebbar M., Baig M.K., Li A., Philipose Z. Use of prucalopride for chronic constipation: A systematic review and meta-analysis of published randomized, controlled trials. J Neurogastroenterol Motil. 2016 Jul 30;22(3):412-22. PubMed PMID: 27127190. Pubmed Central PMCID: 4930296.
21. Quigley E.M. Cisapride: What can we learn from the rise and fall of a prokinetic? J Dig Dis. 2011 Jun;12(3):147-56. PubMed PMID: 21615867.
22. Conlon K., De Maeyer J.H., Bruce C., et al. Nonclinical cardiovascular studies of prucalopride, a highly selective 5-hydroxytryptamine 4 receptor agonist. J Pharmacol Exp Therapeut. 2017 Nov; doi: 10.1124/jpet.117.244079 [epub ahead of print].
23. Chey W.D., Lembo A.J., Rosenbaum D.P. Tenapanor treatment of patients with constipation-predominant irritable bowel syndrome: a phase 2, randomized, placebo-controlled efficacy and safety trial. Am J Gastroenterol. 2017;112:763-74.
24. Simren M., Bajor A., Gillberg P-G, Rudling M., Abrahamsson H. Randomised clinical trial: the ileal bile acid transporter inhibitor A3309 vs. placebo in patients with chronic idiopathic constipation – a double-blind study. Aliment Pharmacol Ther. 2011 Jul;34(1):41-50.
25. Zarate N., Knowles C.H., Newell M., et al. In patients with slow transit constipation, the pattern of colonic transit delay does not differentiate between those with and without impaired rectal evacuation. Am J Gastroenterol. 2008 Feb;103(2):427-34. PubMed PMID: 18070233.
26. Redmond J.M., Smith G.W., Barofsky I., et al. Physiological tests to predict long-term outcome of total abdominal colectomy for intractable constipation. Am J Gastroenterol. 1995 May;90(5):748-53. PubMed PMID: 7733081.
While constipation is one of the most common symptoms managed by practicing gastroenterologists, it can also be among the most challenging. As a presenting complaint, constipation manifests with widely varying degrees of severity and may be seen in all age groups, ethnicities, and socioeconomic backgrounds. Its implications can include chronic and serious functional impairment as well as protracted and often excessive health care utilization. A growing number of pharmacologic and nonpharmacologic interventions have become available and proven to be effective when appropriately deployed. As such, health care providers and particularly gastroenterologists should strive to develop logical and efficient strategies for addressing this common disorder.
Clinical importance
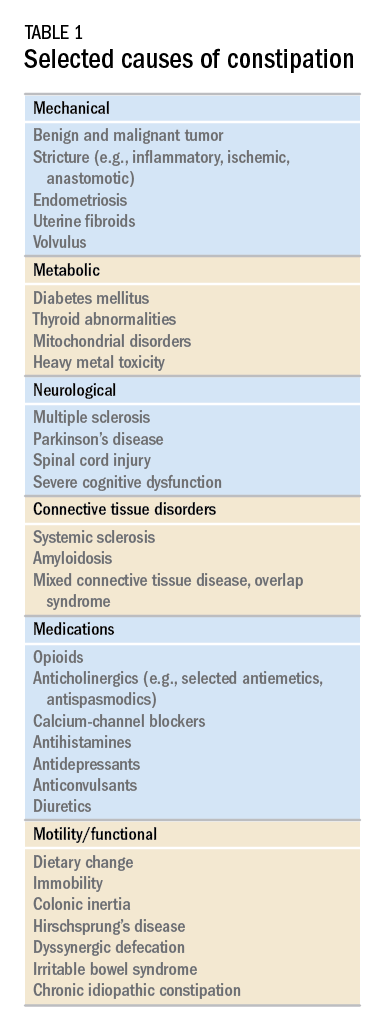
While there are a variety of etiologies for constipation (Table 1), a large proportion of chronic cases fall within the framework of functional gastrointestinal disorders, a category with a substantial burden of disease across the population. Prevalence estimates vary, but constipation likely affects between 12% and 20% of the North American population.1 Research has demonstrated significant health care expenditures associated with chronic constipation management; U.S. estimates suggest direct costs on the order of hundreds of millions of dollars per year, roughly half of which are attributable to inpatient care.2 The financial burden of constipation also includes indirect costs associated with absenteeism as well as the risks of hospitalization and invasive procedures.3
Physical and emotional complications can be likewise significant and affect all age groups, from newborns to patients in the last days of life. Hirschsprung’s disease, for example, can lead to life-threatening sequelae in infancy, such as spontaneous perforation or enterocolitis, or more prolonged functional impairments when it remains undiagnosed. Severe constipation in childhood can lead to encopresis, translating in turn into ostracism and impaired social functioning. Fecal incontinence associated with overflow diarrhea is common and debilitating, particularly in the elderly population.
The potential mechanical complications of constipation lead to its overlap with a variety of other gastrointestinal complaints. For example, the difficulties of passing inspissated stool can provoke lower gastrointestinal bleeding from irritated hemorrhoids, anal fissures, stercoral ulcers, or prolapsed rectal tissue. Retained stool can also lead to upper gastrointestinal symptoms such as postprandial bloating or early satiety.4 Delayed fecal discharge can promote an increase in fermentative microbiota, associated in turn with the production of short-chain fatty acids, methane, and other gaseous byproducts.
The initial assessment
History
Taking an appropriate history is an essential step toward achieving a successful outcome. Presenting concerns related to constipation can range from hard, infrequent, or small-volume stools; abdominal or rectal pain associated with the process of elimination; and bloating, nausea, or early satiety. A sound diagnosis requires a keen understanding of what patients mean when they indicate that they are constipated, an accurate assessment of its impact on quality of life, and a careful inventory of potentially associated complications.
It is critical to define the duration of the problem. Not infrequently, patients will focus on recent events while failing to reveal that altered bowel habits or other functional symptoms have been problematic for years. Reminding the patients to “begin at the beginning” can aid enormously in contextualizing their complaints. Individuals with longstanding symptoms and previously negative evaluations are much less likely to present with a new organic disease than are those in whom symptoms have truly arisen de novo.
Defining constipation by frequency of bowel eliminations alone has proved inaccurate at predicting actual severity. This is in part because the bowel movement frequency varies widely in healthy individuals (anywhere from thrice daily to once every 3 days) and in part because the primary indicator of effective evacuation is not frequency but volume – a much more difficult quantity for patients to gauge.5 The Bristol Stool Scale is a simple, standardized tool that more accurately evaluates the presence or absence of colonic dysfunction. For example, patients passing Type 1-2 (hard or lumpy) stools often have an element of constipation that needs to be addressed.6 However, the interpretation of stool consistency assessments is still aided by awareness of both frequency and volume. A patient passing multiple small-volume Type 6-7 (loose or watery) stools may be the most constipated, presenting with overflow or paradoxical diarrhea attributable to fecal impaction.
Physical examination
An expert physical exam is another essential aspect of the initial assessment. Alarm features can be elicited in this context as well via signs of pallor, weight loss, blood in the stool, physical abuse, or advanced psychological distress. Attention should also be paid to signs of a systemic disorder that might be associated with gastrointestinal dysmotility including previously unrecognized signs of Raynaud’s syndrome, sclerodactyly, amyloidosis, surgical scars, and joint hypermobility.7,8 Abdominal bloating, a frequently vague symptomatic complaint, can be correlated with the presence or absence of distention as perceived by the patient and/or the examiner.9
Any initial evaluation of constipation should also include a detailed digital rectal exam. A complete examination should include a careful visual assessment of the perianal region for external lesions and of the degree and directional appropriateness of pelvic floor excursion (perineal elevation and descent) during squeeze and simulated defecation maneuvers, respectively. Digital examination should include palpation for the presence or absence of pain as well as stool, blood, or masses in the rectal vault, as well as an assessment of sphincter tone at baseline, with squeeze, and with simulated defecation. Rectal pressure generation with the latter maneuver can also be qualitatively assessed. Research has suggested moderate agreement between the digital rectal examination and formal manometric evaluation in diagnosing dyssynergic defecation, underscoring the former’s utility in guiding initial management decisions.10
Testing
It is reasonable to exclude metabolic, inflammatory, or other secondary etiologies of constipation in patients in whom history or examination raises suspicion. Likewise, colonoscopy should be considered in patients with alarm features or who are due for age-appropriate screening. That said, in the absence of risk factors or ancillary signs and symptoms, a detailed diagnostic work-up is often unnecessary. The AGA’s Medical Position Statement on Constipation recommends a complete blood count as the only test to be ordered on a standard basis in the work-up of constipation.11
In patients new to one’s practice, the diligent retrieval of prior records is one of the most efficient ways to avoid wasting health care resources. Locating an old abdominal radiograph that demonstrates extensive retained stool can not only secure the diagnosis for vague symptomatic complaints but also obviate the need for more extensive testing. One should instead consider how symptom duration and the associated changes in objectives measures such as weight and laboratory parameters can be used to justify or refute the need for repeating costly or invasive studies.
It is important to consider the potential contribution of defecatory dyssynergy to chronic constipation early in a patient’s presentation, and to return to this possibility in the future if initial therapeutic interventions are unsuccessful. An abnormal qualitative assessment on digital rectal examination should trigger a more formal characterization of the patient’s defecatory mechanics via anorectal manometry (ARM) and balloon expulsion testing (BET). Likewise, a lack of response to initial pharmacotherapy should prompt suspicion for outlet dysfunction, which can be queried with functional testing even if a rectal examination is qualitatively unrevealing.
Initial approach to the chronically constipated patient
The aforementioned AGA Medical Position Statement provides a helpful algorithm regarding the diagnostic approach to constipation (Figure 1). In the absence of concern for secondary etiologies of constipation, an initial therapeutic trial of dietary, lifestyle, and medication-based intervention is reasonable for mild symptoms. Patients should be encouraged to strive for 25-30 grams of dietary fiber intake per day. For patients unable to reach this goal via high-fiber foods alone, psyllium husk is a popular supplement, but it should be initiated at modest doses to mitigate the risk of bloating. Fiber may be supplemented with the use of osmotic laxatives (e.g., polyethylene glycol) with instructions that the initial dose may be modified as needed to optimal effectiveness. Selective response to rectal therapies (e.g., bisacodyl or glycerin suppositories) over osmotic laxatives may also suggest utility in early queries of outlet dysfunction.
An abdominal radiograph can be helpful not only to diagnose constipation but also to assess the stool burden present at the time of beginning treatment. For patients presenting with a significant degree of fecal loading, an initial bowel cleanse with four liters of osmotically balanced polyethylene glycol can be a useful means of eliminating background fecal impactions that might have mitigated the effectiveness of initial therapies in the past or that might reduce the effectiveness of daily laxative therapy moving forward.
Patients with a diagnosis of defecatory dyssynergy made via ARM/BET should be referred to pelvic floor physical therapy with biofeedback. Recognizing that courses of therapy are highly individualized in practice, randomized controlled trials suggest symptom improvement in 70%-80% of patients, with the majority also demonstrating maintenance of response.12 Biofeedback appears to be an essential component of this modality based on meta-analysis data and should be requested specifically by the referring provider.13
Pharmacologic agents

For those patients with more severe initial presentations or whose symptoms persist despite initial medical management, there are several pharmacologic agents that may be considered on a prescription basis (Table 2). Linaclotide, a minimally absorbed guanylate cyclase agonist, is approved by the Food and Drug Administration for patients with irritable bowel syndrome with constipation (IBS-C) and chronic idiopathic constipation (CIC). Improvements in constipation tend to occur over a slightly shorter timeline than in abdominal pain, though both have been demonstrated in comparison to placebo.14,15 Plecanatide, a newer agent with a similar mechanism of action, has demonstrated improvements in bowel movement frequency and was recently approved for CIC.16 Lubiprostone, a chloride channel agonist, has demonstrated benefit for IBS-C and CIC as well, though its side effect profile is more varied, including dose-related nausea in up to 30% of patients.17
For patients with opioid-induced constipation who cannot wean from the opioid medications, the peripheral acting mu-opioid receptor antagonists may be quite helpful. These include injectable as well as oral formulations (e.g., methylnaltrexone and naloxegol, respectively) with additional agents under active investigation in particular clinical subsets (e.g., naldemedine for patients with cancer-related pain).18,19 Prucalopride, a selective serotonin receptor agonist, has also demonstrated benefit for constipation; it is available abroad but not yet approved for use in the United States.20 Prucalopride shares its primary mechanism of action (selective agonism of the 5HT4 serotonin receptor) with cisapride, a previously quite popular gastrointestinal motility agent that was subsequently withdrawn from the U.S. market because of arrhythmia risk.21 This risk is likely attributable to cisapride’s dual binding affinity for potassium channels, a feature that prucalopride does not share; as such, cardiotoxicity is not an active concern with the latter agent.22
Still other pharmacologic agents with novel mechanisms of action are currently under investigation. Tenapanor, an inhibitor of a particular sodium/potassium exchanger in the gut lumen, mitigates intestinal sodium absorption, which increases fluid volume and transit. A recent phase 2 study demonstrated significantly increased stool frequency relative to placebo in patients with IBS-C.23 Elobixibat, an ileal bile acid transport inhibitor, promotes colonic retention of bile acids and, in placebo-controlled studies, has led to accelerated colonic transit and an increased number of spontaneous bowel movements in patients with CIC.24
Persistent constipation
In cases of refractory constipation (in practical terms, symptoms that persist despite trials of escalating medical therapy over at least 6 weeks), it is worth revisiting the question of etiology. Querying defecatory dyssynergy via ARM/BET, if not pursued prior to trials of newer pharmacologic agents, should certainly be explored in the event that such trials fail. Inconclusive results of ARM and BET testing, or BET abnormalities that persist despite a course of physical therapy with biofeedback, may raise suspicion for pelvic organ prolapse, which may be formally evaluated with defecography. Additional testing for metabolic or structural predispositions toward constipation may also be reasonable at this juncture.
Formal colonic transit testing via radio-opaque markers, scintigraphy, or the wireless motility capsule is often inaccurate in the setting of dyssynergic defecation and should be pursued only after this entity has been excluded or successfully treated.25 While there are not many practical distinctions at present in the therapeutic management of slow-transit versus normal-transit constipation, the use of novel medications with an explicitly prokinetic mechanism of action may be reasonable to consider in the setting of a document delay in colonic transit. Such delays can also help justify further specialized diagnostic testing (e.g., colonic manometry), and, in rare refractory cases, surgical intervention.
Consideration of colectomy should be reserved for highly selected patients with delayed colonic transit, normal defecatory mechanics, and the absence of potentially explanatory background conditions (e.g., connective tissue disease). Clear evidence of an underlying colonic myopathy or neuropathy may militate in favor of a more targeted surgical intervention (e.g., subtotal colectomy) or guide one’s clinical evaluation toward alternative systemic diagnoses. A diverting loop ileostomy with interval assessment of symptoms may be useful to clarify the potential benefits of colectomy while preserving the option of operative reversal. Proximal transit delays should be definitively excluded before pursuing colonic resections given evidence that multisegment transit delays portend significantly worse postoperative outcomes.26
Conclusion
Constipation is a common, sometimes confusing presenting complaint and the variety of established and emergent options for diagnosis and therapy can lend themselves to haphazard application. Patients and providers both are well served by a clinical approach, rooted in a comprehensive history and examination, that begins to organize these options in thoughtful sequence.
Dr. Ahuja is assistant professor of clinical medicine, division of gastroenterology; Dr. Reynolds is professor of clinical medicine, and director of the program in neurogastroenterology and motility, division of gastroenterology, Perelman School of Medicine, University of Pennsylvania, Philadelphia.
References
1. Higgins P.D., Johanson J.F. Epidemiology of constipation in North America: a systematic review. Am J Gastroenterol. 2004 Apr;99(4):750-9. PubMed PMID: 15089911.
2. Martin B.C., Barghout V., Cerulli A. Direct medical costs of constipation in the United States. Manage Care Interface. 2006 Dec;19(12):43-9. PubMed PMID: 17274481.
3. Sun S.X., Dibonaventura M., Purayidathil F.W., et al. Impact of chronic constipation on health-related quality of life, work productivity, and healthcare resource use: an analysis of the National Health and Wellness Survey. Dig Dis Sc. 2011 Sep;56(9):2688-95. PubMed PMID: 21380761.
4. Heidelbaugh J.J., Stelwagon M., Miller S.A., et al. The spectrum of constipation-predominant irritable bowel syndrome and chronic idiopathic constipation: US survey assessing symptoms, care seeking, and disease burden. Am J Gastroenterol. 2015 Apr;110(4):580-7.
5. Mitsuhashi S., Ballou S., Jiang Z.G., et al. Characterizing normal bowel frequency and consistency in a representative sample of adults in the United States (NHANES). Am J Gastroenterol. 2017 Aug 01. PubMed PMID: 28762379.
6. Saad R.J., Rao S.S., Koch K.L., et al. Do stool form and frequency correlate with whole-gut and colonic transit? Results from a multicenter study in constipated individuals and healthy controls. Am J Gastroenterol. 2010 Feb;105(2):403-11. PubMed PMID: 19888202.
7. Castori M., Morlino S., Pascolini G., et al. Gastrointestinal and nutritional issues in joint hypermobility syndrome/Ehlers-Danlos syndrome, hypermobility type. American Journal of Medical Genetics Part C, Semin Med Genet. 2015 Mar;169C(1):54-75. PubMed PMID: 25821092.
8. Nagaraja V., McMahan Z.H., Getzug T., Khanna D. Management of gastrointestinal involvement in scleroderma. Curr Treatm Opt Rheumatol. 2015 Mar 01;1(1):82-105. PubMed PMID: 26005632. Pubmed Central PMCID: 4437639.
9. Malagelada J.R., Accarino A., Azpiroz F. Bloating and abdominal distension: Old misconceptions and current knowledge. Am J Gastroenterol. 2017 Aug;112(8):1221-31. PubMed PMID: 28508867.
10. Soh J.S., Lee H.J., Jung K.W., et al. The diagnostic value of a digital rectal examination compared with high-resolution anorectal manometry in patients with chronic constipation and fecal incontinence. Am J Gastroenterol. 2015 Aug;110(8):1197-204. PubMed PMID: 26032152.
11. American Gastroenterological Association, Bharucha A.E., Dorn S.D., Lembo A., Pressman A. American Gastroenterological Association medical position statement on constipation. Gastroenterology. 2013 Jan;144(1):211-7. PubMed PMID: 23261064.
12. Skardoon G.R., Khera A.J., Emmanuel A.V., Burgell R.E. Review article: dyssynergic defaecation and biofeedback therapy in the pathophysiology and management of functional constipation. Aliment Pharmacol Therapeut. 2017 Aug;46(4):410-23. PubMed PMID: 28660663.
13. Koh C.E., Young C.J., Young J.M., Solomon M.J. Systematic review of randomized controlled trials of the effectiveness of biofeedback for pelvic floor dysfunction. Br J Surg. 2008 Sep;95(9):1079-87. PubMed PMID: 18655219.
14. Rao S., Lembo A.J., Shiff S.J., et al. A 12-week, randomized, controlled trial with a 4-week randomized withdrawal period to evaluate the efficacy and safety of linaclotide in irritable bowel syndrome with constipation. Am J Gastroenterol. 2012 Nov;107(11):1714-24; quiz p 25. PubMed PMID: 22986440. Pubmed Central PMCID: 3504311.
15. Lacy B.E., Schey R., Shiff S.J., et al. Linaclotide in chronic idiopathic constipation patients with moderate to severe abdominal bloating: A randomized, controlled trial. PloS One. 2015;10(7):e0134349. PubMed PMID: 26222318. Pubmed Central PMCID: 4519259.
16. Miner P.B., Jr., Koltun W.D., Wiener G.J., et al. A randomized phase III clinical trial of plecanatide, a uroguanylin analog, in patients with chronic idiopathic constipation. Am J Gastroenterol. 2017 Apr;112(4):613-21. PubMed PMID: 28169285. Pubmed Central PMCID: 5415706.
17. Johanson J.F., Drossman D.A., Panas R., Wahle A., Ueno R. Clinical trial: phase 2 study of lubiprostone for irritable bowel syndrome with constipation. Aliment Pharmacol Therapeut. 2008 Apr;27(8):685-96. PubMed PMID: 18248656.
18. Chey W.D., Webster L., Sostek M., Lappalainen J., Barker P.N., Tack J. Naloxegol for opioid-induced constipation in patients with noncancer pain. N Engl J Med. 2014 Jun 19;370(25):2387-96. PubMed PMID: 24896818.
19. Katakami N., Oda K., Tauchi K., et al. Phase IIb, randomized, double-blind, placebo-controlled study of naldemedine for the treatment of opioid-induced constipation in patients with cancer. J Clin Oncol. 2017 Jun 10;35(17):1921-8. PubMed PMID: 28445097.
20. Sajid M.S., Hebbar M., Baig M.K., Li A., Philipose Z. Use of prucalopride for chronic constipation: A systematic review and meta-analysis of published randomized, controlled trials. J Neurogastroenterol Motil. 2016 Jul 30;22(3):412-22. PubMed PMID: 27127190. Pubmed Central PMCID: 4930296.
21. Quigley E.M. Cisapride: What can we learn from the rise and fall of a prokinetic? J Dig Dis. 2011 Jun;12(3):147-56. PubMed PMID: 21615867.
22. Conlon K., De Maeyer J.H., Bruce C., et al. Nonclinical cardiovascular studies of prucalopride, a highly selective 5-hydroxytryptamine 4 receptor agonist. J Pharmacol Exp Therapeut. 2017 Nov; doi: 10.1124/jpet.117.244079 [epub ahead of print].
23. Chey W.D., Lembo A.J., Rosenbaum D.P. Tenapanor treatment of patients with constipation-predominant irritable bowel syndrome: a phase 2, randomized, placebo-controlled efficacy and safety trial. Am J Gastroenterol. 2017;112:763-74.
24. Simren M., Bajor A., Gillberg P-G, Rudling M., Abrahamsson H. Randomised clinical trial: the ileal bile acid transporter inhibitor A3309 vs. placebo in patients with chronic idiopathic constipation – a double-blind study. Aliment Pharmacol Ther. 2011 Jul;34(1):41-50.
25. Zarate N., Knowles C.H., Newell M., et al. In patients with slow transit constipation, the pattern of colonic transit delay does not differentiate between those with and without impaired rectal evacuation. Am J Gastroenterol. 2008 Feb;103(2):427-34. PubMed PMID: 18070233.
26. Redmond J.M., Smith G.W., Barofsky I., et al. Physiological tests to predict long-term outcome of total abdominal colectomy for intractable constipation. Am J Gastroenterol. 1995 May;90(5):748-53. PubMed PMID: 7733081.
While constipation is one of the most common symptoms managed by practicing gastroenterologists, it can also be among the most challenging. As a presenting complaint, constipation manifests with widely varying degrees of severity and may be seen in all age groups, ethnicities, and socioeconomic backgrounds. Its implications can include chronic and serious functional impairment as well as protracted and often excessive health care utilization. A growing number of pharmacologic and nonpharmacologic interventions have become available and proven to be effective when appropriately deployed. As such, health care providers and particularly gastroenterologists should strive to develop logical and efficient strategies for addressing this common disorder.
Clinical importance
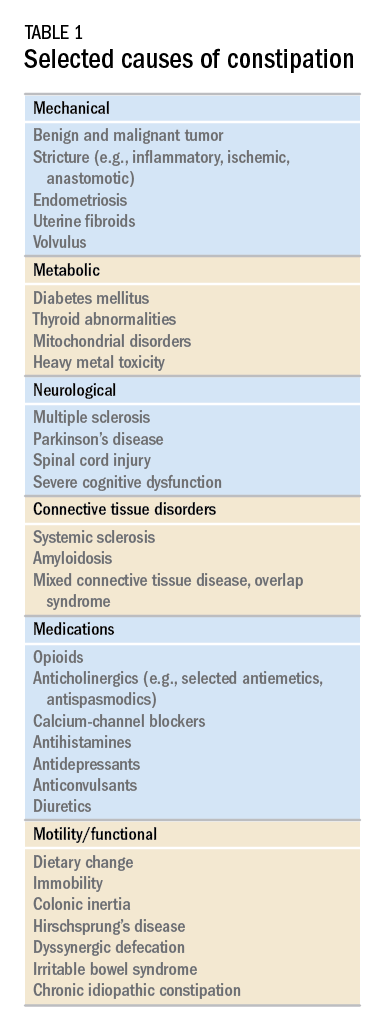
While there are a variety of etiologies for constipation (Table 1), a large proportion of chronic cases fall within the framework of functional gastrointestinal disorders, a category with a substantial burden of disease across the population. Prevalence estimates vary, but constipation likely affects between 12% and 20% of the North American population.1 Research has demonstrated significant health care expenditures associated with chronic constipation management; U.S. estimates suggest direct costs on the order of hundreds of millions of dollars per year, roughly half of which are attributable to inpatient care.2 The financial burden of constipation also includes indirect costs associated with absenteeism as well as the risks of hospitalization and invasive procedures.3
Physical and emotional complications can be likewise significant and affect all age groups, from newborns to patients in the last days of life. Hirschsprung’s disease, for example, can lead to life-threatening sequelae in infancy, such as spontaneous perforation or enterocolitis, or more prolonged functional impairments when it remains undiagnosed. Severe constipation in childhood can lead to encopresis, translating in turn into ostracism and impaired social functioning. Fecal incontinence associated with overflow diarrhea is common and debilitating, particularly in the elderly population.
The potential mechanical complications of constipation lead to its overlap with a variety of other gastrointestinal complaints. For example, the difficulties of passing inspissated stool can provoke lower gastrointestinal bleeding from irritated hemorrhoids, anal fissures, stercoral ulcers, or prolapsed rectal tissue. Retained stool can also lead to upper gastrointestinal symptoms such as postprandial bloating or early satiety.4 Delayed fecal discharge can promote an increase in fermentative microbiota, associated in turn with the production of short-chain fatty acids, methane, and other gaseous byproducts.
The initial assessment
History
Taking an appropriate history is an essential step toward achieving a successful outcome. Presenting concerns related to constipation can range from hard, infrequent, or small-volume stools; abdominal or rectal pain associated with the process of elimination; and bloating, nausea, or early satiety. A sound diagnosis requires a keen understanding of what patients mean when they indicate that they are constipated, an accurate assessment of its impact on quality of life, and a careful inventory of potentially associated complications.
It is critical to define the duration of the problem. Not infrequently, patients will focus on recent events while failing to reveal that altered bowel habits or other functional symptoms have been problematic for years. Reminding the patients to “begin at the beginning” can aid enormously in contextualizing their complaints. Individuals with longstanding symptoms and previously negative evaluations are much less likely to present with a new organic disease than are those in whom symptoms have truly arisen de novo.
Defining constipation by frequency of bowel eliminations alone has proved inaccurate at predicting actual severity. This is in part because the bowel movement frequency varies widely in healthy individuals (anywhere from thrice daily to once every 3 days) and in part because the primary indicator of effective evacuation is not frequency but volume – a much more difficult quantity for patients to gauge.5 The Bristol Stool Scale is a simple, standardized tool that more accurately evaluates the presence or absence of colonic dysfunction. For example, patients passing Type 1-2 (hard or lumpy) stools often have an element of constipation that needs to be addressed.6 However, the interpretation of stool consistency assessments is still aided by awareness of both frequency and volume. A patient passing multiple small-volume Type 6-7 (loose or watery) stools may be the most constipated, presenting with overflow or paradoxical diarrhea attributable to fecal impaction.
Physical examination
An expert physical exam is another essential aspect of the initial assessment. Alarm features can be elicited in this context as well via signs of pallor, weight loss, blood in the stool, physical abuse, or advanced psychological distress. Attention should also be paid to signs of a systemic disorder that might be associated with gastrointestinal dysmotility including previously unrecognized signs of Raynaud’s syndrome, sclerodactyly, amyloidosis, surgical scars, and joint hypermobility.7,8 Abdominal bloating, a frequently vague symptomatic complaint, can be correlated with the presence or absence of distention as perceived by the patient and/or the examiner.9
Any initial evaluation of constipation should also include a detailed digital rectal exam. A complete examination should include a careful visual assessment of the perianal region for external lesions and of the degree and directional appropriateness of pelvic floor excursion (perineal elevation and descent) during squeeze and simulated defecation maneuvers, respectively. Digital examination should include palpation for the presence or absence of pain as well as stool, blood, or masses in the rectal vault, as well as an assessment of sphincter tone at baseline, with squeeze, and with simulated defecation. Rectal pressure generation with the latter maneuver can also be qualitatively assessed. Research has suggested moderate agreement between the digital rectal examination and formal manometric evaluation in diagnosing dyssynergic defecation, underscoring the former’s utility in guiding initial management decisions.10
Testing
It is reasonable to exclude metabolic, inflammatory, or other secondary etiologies of constipation in patients in whom history or examination raises suspicion. Likewise, colonoscopy should be considered in patients with alarm features or who are due for age-appropriate screening. That said, in the absence of risk factors or ancillary signs and symptoms, a detailed diagnostic work-up is often unnecessary. The AGA’s Medical Position Statement on Constipation recommends a complete blood count as the only test to be ordered on a standard basis in the work-up of constipation.11
In patients new to one’s practice, the diligent retrieval of prior records is one of the most efficient ways to avoid wasting health care resources. Locating an old abdominal radiograph that demonstrates extensive retained stool can not only secure the diagnosis for vague symptomatic complaints but also obviate the need for more extensive testing. One should instead consider how symptom duration and the associated changes in objectives measures such as weight and laboratory parameters can be used to justify or refute the need for repeating costly or invasive studies.
It is important to consider the potential contribution of defecatory dyssynergy to chronic constipation early in a patient’s presentation, and to return to this possibility in the future if initial therapeutic interventions are unsuccessful. An abnormal qualitative assessment on digital rectal examination should trigger a more formal characterization of the patient’s defecatory mechanics via anorectal manometry (ARM) and balloon expulsion testing (BET). Likewise, a lack of response to initial pharmacotherapy should prompt suspicion for outlet dysfunction, which can be queried with functional testing even if a rectal examination is qualitatively unrevealing.
Initial approach to the chronically constipated patient
The aforementioned AGA Medical Position Statement provides a helpful algorithm regarding the diagnostic approach to constipation (Figure 1). In the absence of concern for secondary etiologies of constipation, an initial therapeutic trial of dietary, lifestyle, and medication-based intervention is reasonable for mild symptoms. Patients should be encouraged to strive for 25-30 grams of dietary fiber intake per day. For patients unable to reach this goal via high-fiber foods alone, psyllium husk is a popular supplement, but it should be initiated at modest doses to mitigate the risk of bloating. Fiber may be supplemented with the use of osmotic laxatives (e.g., polyethylene glycol) with instructions that the initial dose may be modified as needed to optimal effectiveness. Selective response to rectal therapies (e.g., bisacodyl or glycerin suppositories) over osmotic laxatives may also suggest utility in early queries of outlet dysfunction.
An abdominal radiograph can be helpful not only to diagnose constipation but also to assess the stool burden present at the time of beginning treatment. For patients presenting with a significant degree of fecal loading, an initial bowel cleanse with four liters of osmotically balanced polyethylene glycol can be a useful means of eliminating background fecal impactions that might have mitigated the effectiveness of initial therapies in the past or that might reduce the effectiveness of daily laxative therapy moving forward.
Patients with a diagnosis of defecatory dyssynergy made via ARM/BET should be referred to pelvic floor physical therapy with biofeedback. Recognizing that courses of therapy are highly individualized in practice, randomized controlled trials suggest symptom improvement in 70%-80% of patients, with the majority also demonstrating maintenance of response.12 Biofeedback appears to be an essential component of this modality based on meta-analysis data and should be requested specifically by the referring provider.13
Pharmacologic agents

For those patients with more severe initial presentations or whose symptoms persist despite initial medical management, there are several pharmacologic agents that may be considered on a prescription basis (Table 2). Linaclotide, a minimally absorbed guanylate cyclase agonist, is approved by the Food and Drug Administration for patients with irritable bowel syndrome with constipation (IBS-C) and chronic idiopathic constipation (CIC). Improvements in constipation tend to occur over a slightly shorter timeline than in abdominal pain, though both have been demonstrated in comparison to placebo.14,15 Plecanatide, a newer agent with a similar mechanism of action, has demonstrated improvements in bowel movement frequency and was recently approved for CIC.16 Lubiprostone, a chloride channel agonist, has demonstrated benefit for IBS-C and CIC as well, though its side effect profile is more varied, including dose-related nausea in up to 30% of patients.17
For patients with opioid-induced constipation who cannot wean from the opioid medications, the peripheral acting mu-opioid receptor antagonists may be quite helpful. These include injectable as well as oral formulations (e.g., methylnaltrexone and naloxegol, respectively) with additional agents under active investigation in particular clinical subsets (e.g., naldemedine for patients with cancer-related pain).18,19 Prucalopride, a selective serotonin receptor agonist, has also demonstrated benefit for constipation; it is available abroad but not yet approved for use in the United States.20 Prucalopride shares its primary mechanism of action (selective agonism of the 5HT4 serotonin receptor) with cisapride, a previously quite popular gastrointestinal motility agent that was subsequently withdrawn from the U.S. market because of arrhythmia risk.21 This risk is likely attributable to cisapride’s dual binding affinity for potassium channels, a feature that prucalopride does not share; as such, cardiotoxicity is not an active concern with the latter agent.22
Still other pharmacologic agents with novel mechanisms of action are currently under investigation. Tenapanor, an inhibitor of a particular sodium/potassium exchanger in the gut lumen, mitigates intestinal sodium absorption, which increases fluid volume and transit. A recent phase 2 study demonstrated significantly increased stool frequency relative to placebo in patients with IBS-C.23 Elobixibat, an ileal bile acid transport inhibitor, promotes colonic retention of bile acids and, in placebo-controlled studies, has led to accelerated colonic transit and an increased number of spontaneous bowel movements in patients with CIC.24
Persistent constipation
In cases of refractory constipation (in practical terms, symptoms that persist despite trials of escalating medical therapy over at least 6 weeks), it is worth revisiting the question of etiology. Querying defecatory dyssynergy via ARM/BET, if not pursued prior to trials of newer pharmacologic agents, should certainly be explored in the event that such trials fail. Inconclusive results of ARM and BET testing, or BET abnormalities that persist despite a course of physical therapy with biofeedback, may raise suspicion for pelvic organ prolapse, which may be formally evaluated with defecography. Additional testing for metabolic or structural predispositions toward constipation may also be reasonable at this juncture.
Formal colonic transit testing via radio-opaque markers, scintigraphy, or the wireless motility capsule is often inaccurate in the setting of dyssynergic defecation and should be pursued only after this entity has been excluded or successfully treated.25 While there are not many practical distinctions at present in the therapeutic management of slow-transit versus normal-transit constipation, the use of novel medications with an explicitly prokinetic mechanism of action may be reasonable to consider in the setting of a document delay in colonic transit. Such delays can also help justify further specialized diagnostic testing (e.g., colonic manometry), and, in rare refractory cases, surgical intervention.
Consideration of colectomy should be reserved for highly selected patients with delayed colonic transit, normal defecatory mechanics, and the absence of potentially explanatory background conditions (e.g., connective tissue disease). Clear evidence of an underlying colonic myopathy or neuropathy may militate in favor of a more targeted surgical intervention (e.g., subtotal colectomy) or guide one’s clinical evaluation toward alternative systemic diagnoses. A diverting loop ileostomy with interval assessment of symptoms may be useful to clarify the potential benefits of colectomy while preserving the option of operative reversal. Proximal transit delays should be definitively excluded before pursuing colonic resections given evidence that multisegment transit delays portend significantly worse postoperative outcomes.26
Conclusion
Constipation is a common, sometimes confusing presenting complaint and the variety of established and emergent options for diagnosis and therapy can lend themselves to haphazard application. Patients and providers both are well served by a clinical approach, rooted in a comprehensive history and examination, that begins to organize these options in thoughtful sequence.
Dr. Ahuja is assistant professor of clinical medicine, division of gastroenterology; Dr. Reynolds is professor of clinical medicine, and director of the program in neurogastroenterology and motility, division of gastroenterology, Perelman School of Medicine, University of Pennsylvania, Philadelphia.
References
1. Higgins P.D., Johanson J.F. Epidemiology of constipation in North America: a systematic review. Am J Gastroenterol. 2004 Apr;99(4):750-9. PubMed PMID: 15089911.
2. Martin B.C., Barghout V., Cerulli A. Direct medical costs of constipation in the United States. Manage Care Interface. 2006 Dec;19(12):43-9. PubMed PMID: 17274481.
3. Sun S.X., Dibonaventura M., Purayidathil F.W., et al. Impact of chronic constipation on health-related quality of life, work productivity, and healthcare resource use: an analysis of the National Health and Wellness Survey. Dig Dis Sc. 2011 Sep;56(9):2688-95. PubMed PMID: 21380761.
4. Heidelbaugh J.J., Stelwagon M., Miller S.A., et al. The spectrum of constipation-predominant irritable bowel syndrome and chronic idiopathic constipation: US survey assessing symptoms, care seeking, and disease burden. Am J Gastroenterol. 2015 Apr;110(4):580-7.
5. Mitsuhashi S., Ballou S., Jiang Z.G., et al. Characterizing normal bowel frequency and consistency in a representative sample of adults in the United States (NHANES). Am J Gastroenterol. 2017 Aug 01. PubMed PMID: 28762379.
6. Saad R.J., Rao S.S., Koch K.L., et al. Do stool form and frequency correlate with whole-gut and colonic transit? Results from a multicenter study in constipated individuals and healthy controls. Am J Gastroenterol. 2010 Feb;105(2):403-11. PubMed PMID: 19888202.
7. Castori M., Morlino S., Pascolini G., et al. Gastrointestinal and nutritional issues in joint hypermobility syndrome/Ehlers-Danlos syndrome, hypermobility type. American Journal of Medical Genetics Part C, Semin Med Genet. 2015 Mar;169C(1):54-75. PubMed PMID: 25821092.
8. Nagaraja V., McMahan Z.H., Getzug T., Khanna D. Management of gastrointestinal involvement in scleroderma. Curr Treatm Opt Rheumatol. 2015 Mar 01;1(1):82-105. PubMed PMID: 26005632. Pubmed Central PMCID: 4437639.
9. Malagelada J.R., Accarino A., Azpiroz F. Bloating and abdominal distension: Old misconceptions and current knowledge. Am J Gastroenterol. 2017 Aug;112(8):1221-31. PubMed PMID: 28508867.
10. Soh J.S., Lee H.J., Jung K.W., et al. The diagnostic value of a digital rectal examination compared with high-resolution anorectal manometry in patients with chronic constipation and fecal incontinence. Am J Gastroenterol. 2015 Aug;110(8):1197-204. PubMed PMID: 26032152.
11. American Gastroenterological Association, Bharucha A.E., Dorn S.D., Lembo A., Pressman A. American Gastroenterological Association medical position statement on constipation. Gastroenterology. 2013 Jan;144(1):211-7. PubMed PMID: 23261064.
12. Skardoon G.R., Khera A.J., Emmanuel A.V., Burgell R.E. Review article: dyssynergic defaecation and biofeedback therapy in the pathophysiology and management of functional constipation. Aliment Pharmacol Therapeut. 2017 Aug;46(4):410-23. PubMed PMID: 28660663.
13. Koh C.E., Young C.J., Young J.M., Solomon M.J. Systematic review of randomized controlled trials of the effectiveness of biofeedback for pelvic floor dysfunction. Br J Surg. 2008 Sep;95(9):1079-87. PubMed PMID: 18655219.
14. Rao S., Lembo A.J., Shiff S.J., et al. A 12-week, randomized, controlled trial with a 4-week randomized withdrawal period to evaluate the efficacy and safety of linaclotide in irritable bowel syndrome with constipation. Am J Gastroenterol. 2012 Nov;107(11):1714-24; quiz p 25. PubMed PMID: 22986440. Pubmed Central PMCID: 3504311.
15. Lacy B.E., Schey R., Shiff S.J., et al. Linaclotide in chronic idiopathic constipation patients with moderate to severe abdominal bloating: A randomized, controlled trial. PloS One. 2015;10(7):e0134349. PubMed PMID: 26222318. Pubmed Central PMCID: 4519259.
16. Miner P.B., Jr., Koltun W.D., Wiener G.J., et al. A randomized phase III clinical trial of plecanatide, a uroguanylin analog, in patients with chronic idiopathic constipation. Am J Gastroenterol. 2017 Apr;112(4):613-21. PubMed PMID: 28169285. Pubmed Central PMCID: 5415706.
17. Johanson J.F., Drossman D.A., Panas R., Wahle A., Ueno R. Clinical trial: phase 2 study of lubiprostone for irritable bowel syndrome with constipation. Aliment Pharmacol Therapeut. 2008 Apr;27(8):685-96. PubMed PMID: 18248656.
18. Chey W.D., Webster L., Sostek M., Lappalainen J., Barker P.N., Tack J. Naloxegol for opioid-induced constipation in patients with noncancer pain. N Engl J Med. 2014 Jun 19;370(25):2387-96. PubMed PMID: 24896818.
19. Katakami N., Oda K., Tauchi K., et al. Phase IIb, randomized, double-blind, placebo-controlled study of naldemedine for the treatment of opioid-induced constipation in patients with cancer. J Clin Oncol. 2017 Jun 10;35(17):1921-8. PubMed PMID: 28445097.
20. Sajid M.S., Hebbar M., Baig M.K., Li A., Philipose Z. Use of prucalopride for chronic constipation: A systematic review and meta-analysis of published randomized, controlled trials. J Neurogastroenterol Motil. 2016 Jul 30;22(3):412-22. PubMed PMID: 27127190. Pubmed Central PMCID: 4930296.
21. Quigley E.M. Cisapride: What can we learn from the rise and fall of a prokinetic? J Dig Dis. 2011 Jun;12(3):147-56. PubMed PMID: 21615867.
22. Conlon K., De Maeyer J.H., Bruce C., et al. Nonclinical cardiovascular studies of prucalopride, a highly selective 5-hydroxytryptamine 4 receptor agonist. J Pharmacol Exp Therapeut. 2017 Nov; doi: 10.1124/jpet.117.244079 [epub ahead of print].
23. Chey W.D., Lembo A.J., Rosenbaum D.P. Tenapanor treatment of patients with constipation-predominant irritable bowel syndrome: a phase 2, randomized, placebo-controlled efficacy and safety trial. Am J Gastroenterol. 2017;112:763-74.
24. Simren M., Bajor A., Gillberg P-G, Rudling M., Abrahamsson H. Randomised clinical trial: the ileal bile acid transporter inhibitor A3309 vs. placebo in patients with chronic idiopathic constipation – a double-blind study. Aliment Pharmacol Ther. 2011 Jul;34(1):41-50.
25. Zarate N., Knowles C.H., Newell M., et al. In patients with slow transit constipation, the pattern of colonic transit delay does not differentiate between those with and without impaired rectal evacuation. Am J Gastroenterol. 2008 Feb;103(2):427-34. PubMed PMID: 18070233.
26. Redmond J.M., Smith G.W., Barofsky I., et al. Physiological tests to predict long-term outcome of total abdominal colectomy for intractable constipation. Am J Gastroenterol. 1995 May;90(5):748-53. PubMed PMID: 7733081.
Transitioning GI patients from pediatric to adult care
As pediatric patients with chronic gastrointestinal (GI) disorders mature into adulthood, they require a seamless transition of care into an adult practice. Health care transition is more than a simple transfer of care to an adult provider; it is a purposeful, planned movement of young adults with chronic medical conditions from a child-centered health care system to adult-oriented one.1 Many adolescents with chronic GI disorders are at increased risk of developmental and psychosocial delays and depressive disorders.2-6 A successful transition program can mitigate some of the psychosocial impacts of chronic disorders by improving self-efficacy and autonomy.7
Timing of transition
Unlike other nations where legislation often mandates the age of transition to adult care, the United States leaves decisions about the appropriate time to transition to the discretion of individual patients and pediatricians. While the actual transfer of care may not happen until later, it is prudent to start planning when the patient is in early adolescence. The pediatric gastroenterologist should initiate the discussion with patients and caregivers when the child is 13-15 years of age.12,13 Since health care transition is a complex and lengthy process, it should be approached within a framework that is appropriate for the developmental stage of the patient and at a time when their disease is in remission.14
During the initial discussions, the idea of transition should be introduced to the patient and his or her family by emphasizing the benefits of improved self-management skills, adherence to therapy, and normalization of development. The pediatrician should encourage a greater sense of independence and self-reliance by seeing the patient alone for at least a portion of the clinic visit and encourage future independent visits.
Developing a transition plan
Once the concept of transition of care has been introduced, it is prudent to devise a transition plan tailored to the specific needs and goals of the patient and family.24 Each plan should include who the adult provider will be, the tasks the adolescent must master before entering adult care, and how the care will be financed (because insurance coverage and options may change).25 A well-planned transition should enhance self-efficacy and self-management skills, increase knowledge of medical states, ensure adherence to therapy, and encourage independent decision making.12
Assessing transition readiness
Once the process of transitioning has been initiated, it is helpful to assess transition readiness at regular intervals. This will identify gaps in knowledge and inform appropriate interventions for individual patients. There are several questionnaires that can be administered at regular intervals and be made an integral part of routine clinic visits for adolescent patients. These assessments are now billable under CPT Code 99420 (administration and interpretation of health risk assessment). A standardized instrument should be used and the results recorded in the clinical encounter to ensure billing compliance.
The Transition Readiness Assessment Questionnaire (available online at www.GotTransition.org) is a validated tool that assesses an individual’s awareness of his or her medical needs, treatment plan, and ability to communicate effectively with his or her health care provider.26-28 While not specific to GI disorders, it has been validated in IBD patients and shown to correlate well with the IBD Self-Efficacy Scale for Adolescents.29,30 The University of North Carolina’s TRxANSITION Index, as well as the Social-Ecological Model of Adolescent and Young Adult Readiness for Transition, can be used for patients with various chronic diseases.31,32 Instruments specifically developed to assess transition readiness among patients with IBD include the “IBD-Yourself” questionnaire and MyHealth Passport for IBD.33,34 Additionally, Hait et al. provide a checklist of age-appropriate tasks for patients and their providers.14 The North American Society for Pediatric Gastroenterology, Hepatology and Nutrition has created the “Healthcare Provider Transition Checklist,” which is applicable to all chronic GI disorders.35
Transfer of care
The actual transfer of care is the culmination of the transition process. While the onus of initiating and monitoring a patient’s progress is driven by his or her pediatric provider, a responsive adult provider is integral, so it is vital to identify an adult gastroenterologist ahead of time. This can be especially difficult because most adult gastroenterologists feel uncomfortable about addressing adolescent developmental and mental health issues.36
Local chapters of societies such as the Crohn’s and Colitis Foundation, the American Liver Foundation, and statewide GI societies affiliated with the American College of Gastroenterology, as well as local or regional teaching institutions, are all good resources to identify adult providers interested in a coordinated transition of young adults into their practices. Depending on the availability of a local adult gastroenterologist, one approach to minimize the “growing pains” of transition can be to establish joint clinic visits with pediatric and adult providers; this strategy can help foster trust in the new physician and is generally well-received by patients.37,38 Other institutions may offer alternating visits with adult and pediatric providers during the first year of transition.
Regardless of the manner of the actual transfer of care, it is imperative the adult gastroenterologist be well versed with the natural history and disease complications of the pediatric onset of the specific GI disorder and also appreciate nutrition and concerns regarding growth and radiation. Moreover, they must recognize the convergence and divergence of traditional pediatric and adult care models, as well as the move from a family-centered to an individual-focused environment.39
At the time of the patient’s initial visit, the adult gastroenterologist needs a detailed history of the patient’s disease, a list of past and present medications, the details of any disease- or treatment-related complications or surgeries, and so on. The transfer of relevant medical records is an often overlooked, yet easily remediable, aspect of transfer of care.36 The overall process is best completed by eliciting posttransfer feedback from patients and families after they have established care with the adult provider.
Developing a transition model
In the absence of standard, disease-specific models of transition, most institutions adapt available resources to develop their own protocols. In 2011, a joint task force of the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians published a clinical report on transition. Based on recommendations put forth by the Center for Health Care Transition Improvement – a joint endeavor of the Maternal and Child Health Bureau and the National Alliance to Advance Adolescent Health – the aforementioned task force developed a “Got Transition” model that incorporates six core elements of health care transition (Table 1).
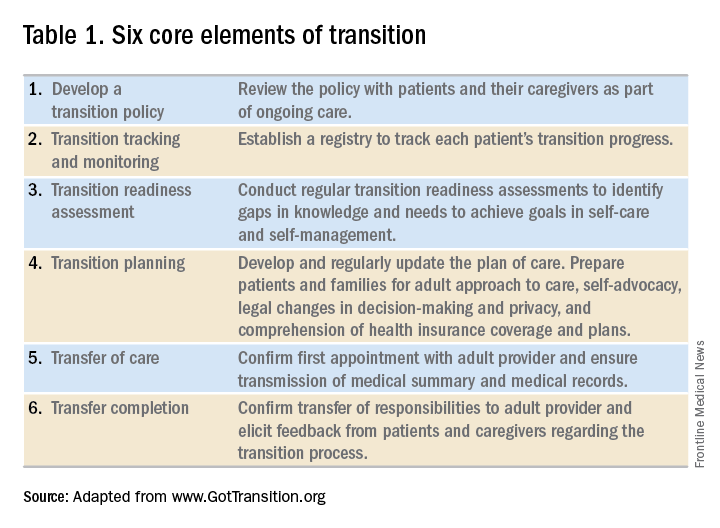
Within the realm of chronic GI disorders, IBD has the most reported data on various models of transition. These include joint adult and pediatric visits, coordinator-initiated transitions, and patient preparation using the assessment tools detailed above. There are no data comparing the efficacy and success of these models and, in the absence of a universally established model for transition in IBD, each institution needs to adopt an approach that best suits the needs of patients and utilizes available resources.
As is the case for patients with IBD, patients with celiac disease need to assume exclusive responsibility for their care as young adults. An important aspect of transition planning for patients with celiac disease is the need to incorporate dietician-led didactic sessions during the transition process. Since patients with celiac disease do not require medications to manage their disease, they are often lost to follow-up as young adults.40 In addition to dietary compliance, it is important to educate young adults about the long-term complications related to celiac disease and the need for regular clinical assessment and monitoring.
Transition of care for patients with EoE is relatively understudied. As EoE was first described only in the 1990s, the diagnosis is still relatively new, and transition programs are limited.41 The natural history and progression of EoE had led to disparate management strategies in adults and children. While the latter are managed with dietary modifications and steroids, adults with EoE often require frequent esophageal dilations because of the increased incidence of fibrosis. In a study of pediatric patients with EoE, most scored lower on transition readiness assessments than did patients with other chronic health conditions.42 Since a majority of patients with EoE require lifelong treatment, they need to be better prepared for transition to adult care.43
In summary, regardless of disease state, transition of care requires planning on the part of the pediatric provider and also close collaboration with patient coordinators, nurses, social workers, and adult providers. While transition is often a complex and lengthy process, it fosters self-reliance and independence among patients while improving their quality of life. Effective communication between pediatric and adult providers as well as patients and families is key to successful transition of care.
Dr. Kaur is the medical director at the Inflammatory Bowel Disease Center and an assistant professor in the section of gastroenterology and hepatology in the department of medicine at Baylor College of Medicine, Houston; Dr. Wyatt is an assistant professor in the section of gastroenterology, hepatology, and nutrition in the department of pediatrics at Baylor.
References
1. Blum RW et al. J Adolesc Health. 1993 Nov;14(7):570-6.
2. Greenley RN et al. J Pediatr Psychol. 2010 Sep;35(8):857-69.
3. Simsek S et al. J Pediatr Gastroenterol Nutr. 2015 Sep;61(3):303-6.
4. Kanof ME et al. Gastroenterology. 1988 Dec;95(6):1523-7.
5. Mackner LM et al. Inflamm Bowel Dis. 2006 Mar;12(3):239-44.
6. Hummel TZ et al. J Pediatr Gastroenterol Nutr. 2013 Aug;57(2):219-24.
7. Rosen DS et al. J Adolesc Health. 2003 Oct;33(4):309-11.
8. Bollegala N et al. J Crohns Colitis. 2013 Mar;7(2):e55-60.
9. Reed-Knight B et al. J Pediatr Psychol. 2011 Apr;36(3):308-17.
10. Holmes-Walker DJ et al. Diabet Med. 2007 Jul;24(7):764-9.
11. Dabadie A et al. Gastroenterol Clin Biol. 2008 May;32(5 Pt 1):451-9.
12. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002 Dec;110(6 Pt 2):1304-6.
13. Baldassano R et al. J Pediatr Gastroenterol Nutr. 2002 Mar;34(3):245-8.
14. Hait E et al. Inflamm Bowel Dis. 2006 Jan;12(1):70-3.
15. Gray WN et al. Inflamm Bowel Dis. 2015 May;21(5):1125-31.
16. Whitfield EP et al. J Pediatr Gastroenterol Nutr. 2015 Jan;60(1):36-41.
17. Rosen D et al. Inflamm Bowel Dis. 2016 Mar;22(3):702-8.
18. Fishman LN et al. J Pediatr Gastroenterol Nutr. 2014 Aug;59(2):221-4.
19. Huang JS et al. Clin Gastroenterol Hepatol. 2012 Jun;10(6):626-32.
20. Habibi H et al. Clin Nurse Spec. 2017 Nov;31(6):329-34.
21. Yerushalmy-Feler A et al. Eur J Gastroenterol Hepatol. 2017 Jul;29(7):831-7.
22. Shanske S et al. Soc Work Health Care. 2012;51(4):279-95.
23. Fredericks EM et al. J Clin Psychol Med Settings. 2015 Sep;22(2-3):150-9.
24. Hardin AP et al. Pediatrics. 2017. doi: 10.1542/peds.2017-2151.
25. Leung Y et al. Inflamm Bowel Dis. 2011 Oct;17(10):2169-73.
26. Wood DL et al. Acad Pediatr. 2014 Jul-Aug;14(4):415-22.
27. Sample Transition Readiness Assessment for Youth. Got Transition/Center for Health Care Transition Improvement, Jan 2014. Accessed Jan 4, 2017, at http://www.gottransition.org/resourceGet.cfm?id=224.
28. Sawicki GS et al. J Pediatr Psychol. 2011 Mar;36(2):160-71.
29. Izaguirre MR et al. J Pediatr Gastroenterol Nutr. 2017 Nov;65(5):546-50.
30. Carlsen K et al. Inflamm Bowel Dis. 2017 Mar;23(3):341-6.
31. Ferris ME et al. Ren Fail. 2012;34(6):744-53.
32. Schwartz LA et al. Child Care Health Dev. 2011 Nov;37(6):883-95.
33. Zijlstra M et al. J Crohns Colitis. 2013 Oct;7(9):e375-85.
34. Benchimol EI et al. Inflamm Bowel Dis. 2011 May;17(5):1131-7.
35. Heath Care Provider Transitioning Checklist. NASPGHAN. Accessed Jan 4, 2018, at https://www.naspghan.org/files/documents/pdfs/medical-resources/ibd/Checklist_PatientandHealthcareProdiver_TransitionfromPedtoAdult.pdf.
36. Hait EJ et al. J Pediatr Gastroenterol Nutr. 2009 Jan;48(1):61-5.
37. Escher JC. Dig Dis. 2009;27(3):382-6.
38. Crowley R et al. Arch Dis Child. 2011 Jun;96(6):548-53.
39. Trivedi I et al. Gastroenterol Res Pract. 2015;2015:260807.
40. O’Leary C et al. Am J Gastroenterol. 2004 Dec;99(12):2437-41.
41. de Silva PSA et al. Pediatr Clin North Am. 2017 Jun;64(3):707-20.
42. Eluri S et al. J Pediatr Gastroenterol Nutr. 2017 Jul;65(1):53-7.
43. Dellon ES et al. Dis Esophagus. 2013 Jan;26(1):7-13.
As pediatric patients with chronic gastrointestinal (GI) disorders mature into adulthood, they require a seamless transition of care into an adult practice. Health care transition is more than a simple transfer of care to an adult provider; it is a purposeful, planned movement of young adults with chronic medical conditions from a child-centered health care system to adult-oriented one.1 Many adolescents with chronic GI disorders are at increased risk of developmental and psychosocial delays and depressive disorders.2-6 A successful transition program can mitigate some of the psychosocial impacts of chronic disorders by improving self-efficacy and autonomy.7
Timing of transition
Unlike other nations where legislation often mandates the age of transition to adult care, the United States leaves decisions about the appropriate time to transition to the discretion of individual patients and pediatricians. While the actual transfer of care may not happen until later, it is prudent to start planning when the patient is in early adolescence. The pediatric gastroenterologist should initiate the discussion with patients and caregivers when the child is 13-15 years of age.12,13 Since health care transition is a complex and lengthy process, it should be approached within a framework that is appropriate for the developmental stage of the patient and at a time when their disease is in remission.14
During the initial discussions, the idea of transition should be introduced to the patient and his or her family by emphasizing the benefits of improved self-management skills, adherence to therapy, and normalization of development. The pediatrician should encourage a greater sense of independence and self-reliance by seeing the patient alone for at least a portion of the clinic visit and encourage future independent visits.
Developing a transition plan
Once the concept of transition of care has been introduced, it is prudent to devise a transition plan tailored to the specific needs and goals of the patient and family.24 Each plan should include who the adult provider will be, the tasks the adolescent must master before entering adult care, and how the care will be financed (because insurance coverage and options may change).25 A well-planned transition should enhance self-efficacy and self-management skills, increase knowledge of medical states, ensure adherence to therapy, and encourage independent decision making.12
Assessing transition readiness
Once the process of transitioning has been initiated, it is helpful to assess transition readiness at regular intervals. This will identify gaps in knowledge and inform appropriate interventions for individual patients. There are several questionnaires that can be administered at regular intervals and be made an integral part of routine clinic visits for adolescent patients. These assessments are now billable under CPT Code 99420 (administration and interpretation of health risk assessment). A standardized instrument should be used and the results recorded in the clinical encounter to ensure billing compliance.
The Transition Readiness Assessment Questionnaire (available online at www.GotTransition.org) is a validated tool that assesses an individual’s awareness of his or her medical needs, treatment plan, and ability to communicate effectively with his or her health care provider.26-28 While not specific to GI disorders, it has been validated in IBD patients and shown to correlate well with the IBD Self-Efficacy Scale for Adolescents.29,30 The University of North Carolina’s TRxANSITION Index, as well as the Social-Ecological Model of Adolescent and Young Adult Readiness for Transition, can be used for patients with various chronic diseases.31,32 Instruments specifically developed to assess transition readiness among patients with IBD include the “IBD-Yourself” questionnaire and MyHealth Passport for IBD.33,34 Additionally, Hait et al. provide a checklist of age-appropriate tasks for patients and their providers.14 The North American Society for Pediatric Gastroenterology, Hepatology and Nutrition has created the “Healthcare Provider Transition Checklist,” which is applicable to all chronic GI disorders.35
Transfer of care
The actual transfer of care is the culmination of the transition process. While the onus of initiating and monitoring a patient’s progress is driven by his or her pediatric provider, a responsive adult provider is integral, so it is vital to identify an adult gastroenterologist ahead of time. This can be especially difficult because most adult gastroenterologists feel uncomfortable about addressing adolescent developmental and mental health issues.36
Local chapters of societies such as the Crohn’s and Colitis Foundation, the American Liver Foundation, and statewide GI societies affiliated with the American College of Gastroenterology, as well as local or regional teaching institutions, are all good resources to identify adult providers interested in a coordinated transition of young adults into their practices. Depending on the availability of a local adult gastroenterologist, one approach to minimize the “growing pains” of transition can be to establish joint clinic visits with pediatric and adult providers; this strategy can help foster trust in the new physician and is generally well-received by patients.37,38 Other institutions may offer alternating visits with adult and pediatric providers during the first year of transition.
Regardless of the manner of the actual transfer of care, it is imperative the adult gastroenterologist be well versed with the natural history and disease complications of the pediatric onset of the specific GI disorder and also appreciate nutrition and concerns regarding growth and radiation. Moreover, they must recognize the convergence and divergence of traditional pediatric and adult care models, as well as the move from a family-centered to an individual-focused environment.39
At the time of the patient’s initial visit, the adult gastroenterologist needs a detailed history of the patient’s disease, a list of past and present medications, the details of any disease- or treatment-related complications or surgeries, and so on. The transfer of relevant medical records is an often overlooked, yet easily remediable, aspect of transfer of care.36 The overall process is best completed by eliciting posttransfer feedback from patients and families after they have established care with the adult provider.
Developing a transition model
In the absence of standard, disease-specific models of transition, most institutions adapt available resources to develop their own protocols. In 2011, a joint task force of the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians published a clinical report on transition. Based on recommendations put forth by the Center for Health Care Transition Improvement – a joint endeavor of the Maternal and Child Health Bureau and the National Alliance to Advance Adolescent Health – the aforementioned task force developed a “Got Transition” model that incorporates six core elements of health care transition (Table 1).
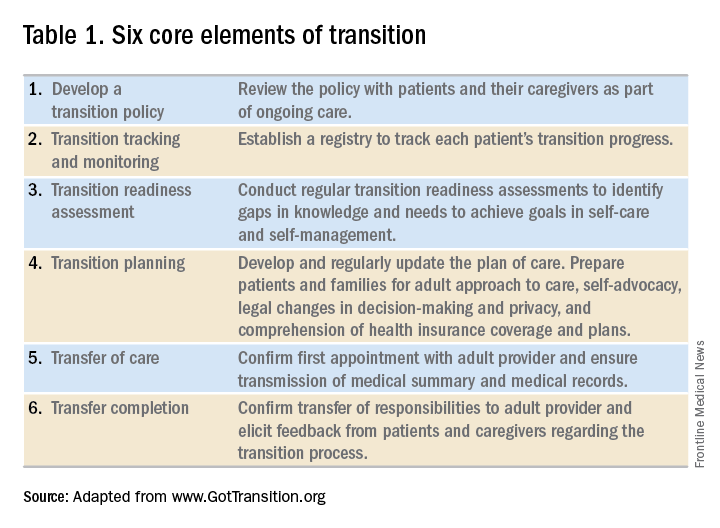
Within the realm of chronic GI disorders, IBD has the most reported data on various models of transition. These include joint adult and pediatric visits, coordinator-initiated transitions, and patient preparation using the assessment tools detailed above. There are no data comparing the efficacy and success of these models and, in the absence of a universally established model for transition in IBD, each institution needs to adopt an approach that best suits the needs of patients and utilizes available resources.
As is the case for patients with IBD, patients with celiac disease need to assume exclusive responsibility for their care as young adults. An important aspect of transition planning for patients with celiac disease is the need to incorporate dietician-led didactic sessions during the transition process. Since patients with celiac disease do not require medications to manage their disease, they are often lost to follow-up as young adults.40 In addition to dietary compliance, it is important to educate young adults about the long-term complications related to celiac disease and the need for regular clinical assessment and monitoring.
Transition of care for patients with EoE is relatively understudied. As EoE was first described only in the 1990s, the diagnosis is still relatively new, and transition programs are limited.41 The natural history and progression of EoE had led to disparate management strategies in adults and children. While the latter are managed with dietary modifications and steroids, adults with EoE often require frequent esophageal dilations because of the increased incidence of fibrosis. In a study of pediatric patients with EoE, most scored lower on transition readiness assessments than did patients with other chronic health conditions.42 Since a majority of patients with EoE require lifelong treatment, they need to be better prepared for transition to adult care.43
In summary, regardless of disease state, transition of care requires planning on the part of the pediatric provider and also close collaboration with patient coordinators, nurses, social workers, and adult providers. While transition is often a complex and lengthy process, it fosters self-reliance and independence among patients while improving their quality of life. Effective communication between pediatric and adult providers as well as patients and families is key to successful transition of care.
Dr. Kaur is the medical director at the Inflammatory Bowel Disease Center and an assistant professor in the section of gastroenterology and hepatology in the department of medicine at Baylor College of Medicine, Houston; Dr. Wyatt is an assistant professor in the section of gastroenterology, hepatology, and nutrition in the department of pediatrics at Baylor.
References
1. Blum RW et al. J Adolesc Health. 1993 Nov;14(7):570-6.
2. Greenley RN et al. J Pediatr Psychol. 2010 Sep;35(8):857-69.
3. Simsek S et al. J Pediatr Gastroenterol Nutr. 2015 Sep;61(3):303-6.
4. Kanof ME et al. Gastroenterology. 1988 Dec;95(6):1523-7.
5. Mackner LM et al. Inflamm Bowel Dis. 2006 Mar;12(3):239-44.
6. Hummel TZ et al. J Pediatr Gastroenterol Nutr. 2013 Aug;57(2):219-24.
7. Rosen DS et al. J Adolesc Health. 2003 Oct;33(4):309-11.
8. Bollegala N et al. J Crohns Colitis. 2013 Mar;7(2):e55-60.
9. Reed-Knight B et al. J Pediatr Psychol. 2011 Apr;36(3):308-17.
10. Holmes-Walker DJ et al. Diabet Med. 2007 Jul;24(7):764-9.
11. Dabadie A et al. Gastroenterol Clin Biol. 2008 May;32(5 Pt 1):451-9.
12. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002 Dec;110(6 Pt 2):1304-6.
13. Baldassano R et al. J Pediatr Gastroenterol Nutr. 2002 Mar;34(3):245-8.
14. Hait E et al. Inflamm Bowel Dis. 2006 Jan;12(1):70-3.
15. Gray WN et al. Inflamm Bowel Dis. 2015 May;21(5):1125-31.
16. Whitfield EP et al. J Pediatr Gastroenterol Nutr. 2015 Jan;60(1):36-41.
17. Rosen D et al. Inflamm Bowel Dis. 2016 Mar;22(3):702-8.
18. Fishman LN et al. J Pediatr Gastroenterol Nutr. 2014 Aug;59(2):221-4.
19. Huang JS et al. Clin Gastroenterol Hepatol. 2012 Jun;10(6):626-32.
20. Habibi H et al. Clin Nurse Spec. 2017 Nov;31(6):329-34.
21. Yerushalmy-Feler A et al. Eur J Gastroenterol Hepatol. 2017 Jul;29(7):831-7.
22. Shanske S et al. Soc Work Health Care. 2012;51(4):279-95.
23. Fredericks EM et al. J Clin Psychol Med Settings. 2015 Sep;22(2-3):150-9.
24. Hardin AP et al. Pediatrics. 2017. doi: 10.1542/peds.2017-2151.
25. Leung Y et al. Inflamm Bowel Dis. 2011 Oct;17(10):2169-73.
26. Wood DL et al. Acad Pediatr. 2014 Jul-Aug;14(4):415-22.
27. Sample Transition Readiness Assessment for Youth. Got Transition/Center for Health Care Transition Improvement, Jan 2014. Accessed Jan 4, 2017, at http://www.gottransition.org/resourceGet.cfm?id=224.
28. Sawicki GS et al. J Pediatr Psychol. 2011 Mar;36(2):160-71.
29. Izaguirre MR et al. J Pediatr Gastroenterol Nutr. 2017 Nov;65(5):546-50.
30. Carlsen K et al. Inflamm Bowel Dis. 2017 Mar;23(3):341-6.
31. Ferris ME et al. Ren Fail. 2012;34(6):744-53.
32. Schwartz LA et al. Child Care Health Dev. 2011 Nov;37(6):883-95.
33. Zijlstra M et al. J Crohns Colitis. 2013 Oct;7(9):e375-85.
34. Benchimol EI et al. Inflamm Bowel Dis. 2011 May;17(5):1131-7.
35. Heath Care Provider Transitioning Checklist. NASPGHAN. Accessed Jan 4, 2018, at https://www.naspghan.org/files/documents/pdfs/medical-resources/ibd/Checklist_PatientandHealthcareProdiver_TransitionfromPedtoAdult.pdf.
36. Hait EJ et al. J Pediatr Gastroenterol Nutr. 2009 Jan;48(1):61-5.
37. Escher JC. Dig Dis. 2009;27(3):382-6.
38. Crowley R et al. Arch Dis Child. 2011 Jun;96(6):548-53.
39. Trivedi I et al. Gastroenterol Res Pract. 2015;2015:260807.
40. O’Leary C et al. Am J Gastroenterol. 2004 Dec;99(12):2437-41.
41. de Silva PSA et al. Pediatr Clin North Am. 2017 Jun;64(3):707-20.
42. Eluri S et al. J Pediatr Gastroenterol Nutr. 2017 Jul;65(1):53-7.
43. Dellon ES et al. Dis Esophagus. 2013 Jan;26(1):7-13.
As pediatric patients with chronic gastrointestinal (GI) disorders mature into adulthood, they require a seamless transition of care into an adult practice. Health care transition is more than a simple transfer of care to an adult provider; it is a purposeful, planned movement of young adults with chronic medical conditions from a child-centered health care system to adult-oriented one.1 Many adolescents with chronic GI disorders are at increased risk of developmental and psychosocial delays and depressive disorders.2-6 A successful transition program can mitigate some of the psychosocial impacts of chronic disorders by improving self-efficacy and autonomy.7
Timing of transition
Unlike other nations where legislation often mandates the age of transition to adult care, the United States leaves decisions about the appropriate time to transition to the discretion of individual patients and pediatricians. While the actual transfer of care may not happen until later, it is prudent to start planning when the patient is in early adolescence. The pediatric gastroenterologist should initiate the discussion with patients and caregivers when the child is 13-15 years of age.12,13 Since health care transition is a complex and lengthy process, it should be approached within a framework that is appropriate for the developmental stage of the patient and at a time when their disease is in remission.14
During the initial discussions, the idea of transition should be introduced to the patient and his or her family by emphasizing the benefits of improved self-management skills, adherence to therapy, and normalization of development. The pediatrician should encourage a greater sense of independence and self-reliance by seeing the patient alone for at least a portion of the clinic visit and encourage future independent visits.
Developing a transition plan
Once the concept of transition of care has been introduced, it is prudent to devise a transition plan tailored to the specific needs and goals of the patient and family.24 Each plan should include who the adult provider will be, the tasks the adolescent must master before entering adult care, and how the care will be financed (because insurance coverage and options may change).25 A well-planned transition should enhance self-efficacy and self-management skills, increase knowledge of medical states, ensure adherence to therapy, and encourage independent decision making.12
Assessing transition readiness
Once the process of transitioning has been initiated, it is helpful to assess transition readiness at regular intervals. This will identify gaps in knowledge and inform appropriate interventions for individual patients. There are several questionnaires that can be administered at regular intervals and be made an integral part of routine clinic visits for adolescent patients. These assessments are now billable under CPT Code 99420 (administration and interpretation of health risk assessment). A standardized instrument should be used and the results recorded in the clinical encounter to ensure billing compliance.
The Transition Readiness Assessment Questionnaire (available online at www.GotTransition.org) is a validated tool that assesses an individual’s awareness of his or her medical needs, treatment plan, and ability to communicate effectively with his or her health care provider.26-28 While not specific to GI disorders, it has been validated in IBD patients and shown to correlate well with the IBD Self-Efficacy Scale for Adolescents.29,30 The University of North Carolina’s TRxANSITION Index, as well as the Social-Ecological Model of Adolescent and Young Adult Readiness for Transition, can be used for patients with various chronic diseases.31,32 Instruments specifically developed to assess transition readiness among patients with IBD include the “IBD-Yourself” questionnaire and MyHealth Passport for IBD.33,34 Additionally, Hait et al. provide a checklist of age-appropriate tasks for patients and their providers.14 The North American Society for Pediatric Gastroenterology, Hepatology and Nutrition has created the “Healthcare Provider Transition Checklist,” which is applicable to all chronic GI disorders.35
Transfer of care
The actual transfer of care is the culmination of the transition process. While the onus of initiating and monitoring a patient’s progress is driven by his or her pediatric provider, a responsive adult provider is integral, so it is vital to identify an adult gastroenterologist ahead of time. This can be especially difficult because most adult gastroenterologists feel uncomfortable about addressing adolescent developmental and mental health issues.36
Local chapters of societies such as the Crohn’s and Colitis Foundation, the American Liver Foundation, and statewide GI societies affiliated with the American College of Gastroenterology, as well as local or regional teaching institutions, are all good resources to identify adult providers interested in a coordinated transition of young adults into their practices. Depending on the availability of a local adult gastroenterologist, one approach to minimize the “growing pains” of transition can be to establish joint clinic visits with pediatric and adult providers; this strategy can help foster trust in the new physician and is generally well-received by patients.37,38 Other institutions may offer alternating visits with adult and pediatric providers during the first year of transition.
Regardless of the manner of the actual transfer of care, it is imperative the adult gastroenterologist be well versed with the natural history and disease complications of the pediatric onset of the specific GI disorder and also appreciate nutrition and concerns regarding growth and radiation. Moreover, they must recognize the convergence and divergence of traditional pediatric and adult care models, as well as the move from a family-centered to an individual-focused environment.39
At the time of the patient’s initial visit, the adult gastroenterologist needs a detailed history of the patient’s disease, a list of past and present medications, the details of any disease- or treatment-related complications or surgeries, and so on. The transfer of relevant medical records is an often overlooked, yet easily remediable, aspect of transfer of care.36 The overall process is best completed by eliciting posttransfer feedback from patients and families after they have established care with the adult provider.
Developing a transition model
In the absence of standard, disease-specific models of transition, most institutions adapt available resources to develop their own protocols. In 2011, a joint task force of the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians published a clinical report on transition. Based on recommendations put forth by the Center for Health Care Transition Improvement – a joint endeavor of the Maternal and Child Health Bureau and the National Alliance to Advance Adolescent Health – the aforementioned task force developed a “Got Transition” model that incorporates six core elements of health care transition (Table 1).
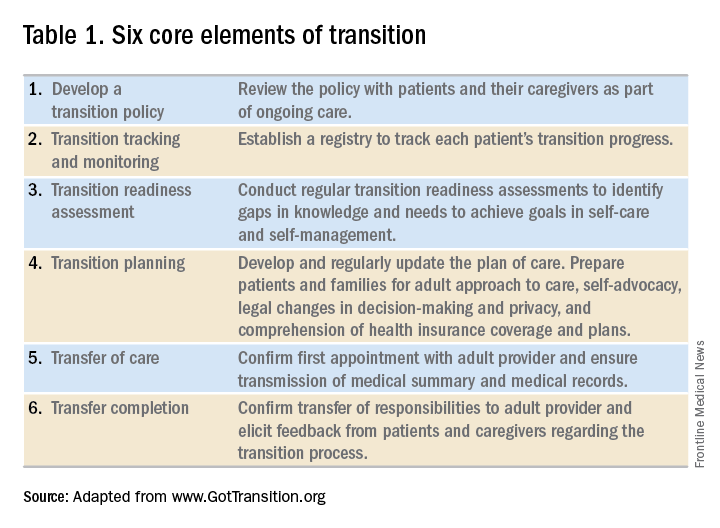
Within the realm of chronic GI disorders, IBD has the most reported data on various models of transition. These include joint adult and pediatric visits, coordinator-initiated transitions, and patient preparation using the assessment tools detailed above. There are no data comparing the efficacy and success of these models and, in the absence of a universally established model for transition in IBD, each institution needs to adopt an approach that best suits the needs of patients and utilizes available resources.
As is the case for patients with IBD, patients with celiac disease need to assume exclusive responsibility for their care as young adults. An important aspect of transition planning for patients with celiac disease is the need to incorporate dietician-led didactic sessions during the transition process. Since patients with celiac disease do not require medications to manage their disease, they are often lost to follow-up as young adults.40 In addition to dietary compliance, it is important to educate young adults about the long-term complications related to celiac disease and the need for regular clinical assessment and monitoring.
Transition of care for patients with EoE is relatively understudied. As EoE was first described only in the 1990s, the diagnosis is still relatively new, and transition programs are limited.41 The natural history and progression of EoE had led to disparate management strategies in adults and children. While the latter are managed with dietary modifications and steroids, adults with EoE often require frequent esophageal dilations because of the increased incidence of fibrosis. In a study of pediatric patients with EoE, most scored lower on transition readiness assessments than did patients with other chronic health conditions.42 Since a majority of patients with EoE require lifelong treatment, they need to be better prepared for transition to adult care.43
In summary, regardless of disease state, transition of care requires planning on the part of the pediatric provider and also close collaboration with patient coordinators, nurses, social workers, and adult providers. While transition is often a complex and lengthy process, it fosters self-reliance and independence among patients while improving their quality of life. Effective communication between pediatric and adult providers as well as patients and families is key to successful transition of care.
Dr. Kaur is the medical director at the Inflammatory Bowel Disease Center and an assistant professor in the section of gastroenterology and hepatology in the department of medicine at Baylor College of Medicine, Houston; Dr. Wyatt is an assistant professor in the section of gastroenterology, hepatology, and nutrition in the department of pediatrics at Baylor.
References
1. Blum RW et al. J Adolesc Health. 1993 Nov;14(7):570-6.
2. Greenley RN et al. J Pediatr Psychol. 2010 Sep;35(8):857-69.
3. Simsek S et al. J Pediatr Gastroenterol Nutr. 2015 Sep;61(3):303-6.
4. Kanof ME et al. Gastroenterology. 1988 Dec;95(6):1523-7.
5. Mackner LM et al. Inflamm Bowel Dis. 2006 Mar;12(3):239-44.
6. Hummel TZ et al. J Pediatr Gastroenterol Nutr. 2013 Aug;57(2):219-24.
7. Rosen DS et al. J Adolesc Health. 2003 Oct;33(4):309-11.
8. Bollegala N et al. J Crohns Colitis. 2013 Mar;7(2):e55-60.
9. Reed-Knight B et al. J Pediatr Psychol. 2011 Apr;36(3):308-17.
10. Holmes-Walker DJ et al. Diabet Med. 2007 Jul;24(7):764-9.
11. Dabadie A et al. Gastroenterol Clin Biol. 2008 May;32(5 Pt 1):451-9.
12. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002 Dec;110(6 Pt 2):1304-6.
13. Baldassano R et al. J Pediatr Gastroenterol Nutr. 2002 Mar;34(3):245-8.
14. Hait E et al. Inflamm Bowel Dis. 2006 Jan;12(1):70-3.
15. Gray WN et al. Inflamm Bowel Dis. 2015 May;21(5):1125-31.
16. Whitfield EP et al. J Pediatr Gastroenterol Nutr. 2015 Jan;60(1):36-41.
17. Rosen D et al. Inflamm Bowel Dis. 2016 Mar;22(3):702-8.
18. Fishman LN et al. J Pediatr Gastroenterol Nutr. 2014 Aug;59(2):221-4.
19. Huang JS et al. Clin Gastroenterol Hepatol. 2012 Jun;10(6):626-32.
20. Habibi H et al. Clin Nurse Spec. 2017 Nov;31(6):329-34.
21. Yerushalmy-Feler A et al. Eur J Gastroenterol Hepatol. 2017 Jul;29(7):831-7.
22. Shanske S et al. Soc Work Health Care. 2012;51(4):279-95.
23. Fredericks EM et al. J Clin Psychol Med Settings. 2015 Sep;22(2-3):150-9.
24. Hardin AP et al. Pediatrics. 2017. doi: 10.1542/peds.2017-2151.
25. Leung Y et al. Inflamm Bowel Dis. 2011 Oct;17(10):2169-73.
26. Wood DL et al. Acad Pediatr. 2014 Jul-Aug;14(4):415-22.
27. Sample Transition Readiness Assessment for Youth. Got Transition/Center for Health Care Transition Improvement, Jan 2014. Accessed Jan 4, 2017, at http://www.gottransition.org/resourceGet.cfm?id=224.
28. Sawicki GS et al. J Pediatr Psychol. 2011 Mar;36(2):160-71.
29. Izaguirre MR et al. J Pediatr Gastroenterol Nutr. 2017 Nov;65(5):546-50.
30. Carlsen K et al. Inflamm Bowel Dis. 2017 Mar;23(3):341-6.
31. Ferris ME et al. Ren Fail. 2012;34(6):744-53.
32. Schwartz LA et al. Child Care Health Dev. 2011 Nov;37(6):883-95.
33. Zijlstra M et al. J Crohns Colitis. 2013 Oct;7(9):e375-85.
34. Benchimol EI et al. Inflamm Bowel Dis. 2011 May;17(5):1131-7.
35. Heath Care Provider Transitioning Checklist. NASPGHAN. Accessed Jan 4, 2018, at https://www.naspghan.org/files/documents/pdfs/medical-resources/ibd/Checklist_PatientandHealthcareProdiver_TransitionfromPedtoAdult.pdf.
36. Hait EJ et al. J Pediatr Gastroenterol Nutr. 2009 Jan;48(1):61-5.
37. Escher JC. Dig Dis. 2009;27(3):382-6.
38. Crowley R et al. Arch Dis Child. 2011 Jun;96(6):548-53.
39. Trivedi I et al. Gastroenterol Res Pract. 2015;2015:260807.
40. O’Leary C et al. Am J Gastroenterol. 2004 Dec;99(12):2437-41.
41. de Silva PSA et al. Pediatr Clin North Am. 2017 Jun;64(3):707-20.
42. Eluri S et al. J Pediatr Gastroenterol Nutr. 2017 Jul;65(1):53-7.
43. Dellon ES et al. Dis Esophagus. 2013 Jan;26(1):7-13.