User login
Don’t lose your access to essential resources
If you are a current AGA trainee, medical resident, or student member, please renew your membership today to ensure the continuation of your career-enhancing benefits for the upcoming membership year. Prepare for your next chapter with the latest news and breakthroughs in the field, as well as access to educational programs, events and much more.
While renewing, please update your member profile at My AGA for news and resources tailored to your professional interests. The deadline to renew is Aug. 31, 2018.
If you have any questions, please contact AGA Member Relations at [email protected] or 301-941-2651.
If you are a current AGA trainee, medical resident, or student member, please renew your membership today to ensure the continuation of your career-enhancing benefits for the upcoming membership year. Prepare for your next chapter with the latest news and breakthroughs in the field, as well as access to educational programs, events and much more.
While renewing, please update your member profile at My AGA for news and resources tailored to your professional interests. The deadline to renew is Aug. 31, 2018.
If you have any questions, please contact AGA Member Relations at [email protected] or 301-941-2651.
If you are a current AGA trainee, medical resident, or student member, please renew your membership today to ensure the continuation of your career-enhancing benefits for the upcoming membership year. Prepare for your next chapter with the latest news and breakthroughs in the field, as well as access to educational programs, events and much more.
While renewing, please update your member profile at My AGA for news and resources tailored to your professional interests. The deadline to renew is Aug. 31, 2018.
If you have any questions, please contact AGA Member Relations at [email protected] or 301-941-2651.
A successful career starts with taking charge
Successful careers don’t just happen. They are made by individuals who take charge and build their own success. The alternative is burnout.
“Part of burnout is feeling overburdened, overworked, and out of control,” said Barbara Jung, MD, AGAF, professor and chief of gastroenterology and hepatology at the University of Illinois at Chicago, during Strategies for a Successful Career: Wellness, Empowerment, Leadership and Resilience at Digestive Disease Week® (DDW) 2018. “If somebody is staying until 9 or 10 o’clock [at night] to finish notes, I have a discussion with them. It is good to be done at 5 p.m. and go home. It is all about setting your own priorities and not letting the job take over your life.”
Associations have a role to play, too. The ASGE Technology Committee reported in 2010 that up to 89% of GIs suffer musculoskeletal injuries from manipulating scopes. Colonoscopist’s thumb (left thumb tendonitis) and metacarpophalangeal joint strain were the most common injuries.
“Risk factors are part of our work,” said Mehnaz Shafi, MD, AGAF, professor of gastroenterology, hepatology and nutrition at the University of Texas MD Anderson Cancer Center, Houston. “Pinching, pushing, pulling, and awkward positions are part of what we do. This is an injury with consequences.”
Dr. Shafi chairs the AGA Task Force on Ergonomics. The group has recommended changes to endoscopic work stations that minimize injury. The most important changes include mounting monitors on flexible stands to accommodate GIs of all heights, adding straps to the control head to allow the fingers to relax, providing ergonomic training to all GIs and using patient beds that can be raised and lowered to accommodate both tall and short GIs.
“Shaping your career is one of the key principles in preventing burnout,” said Arthur DeCross, MD, AGAF, professor of medicine, gastroenterology and hepatology at the University of Rochester Medical Center, N.Y. “We know that more than half of gastroenterologists self-identify as being burned out. And one of the major contributors to burnout is lack of control over your work environment, your career, your colleagues. Taking control of your career can make a difference.”
Taking control can be particularly important for women. An AGA burnout survey in 2015 found that 51% of male GIs reported burnout versus 62% of female GIs.
One reason is women’s tendency to negotiate poorly on their own behalf, said Marie-Pier Tétreault, PhD, assistant professor of gastroenterology and hepatology at Northwestern University Feinberg School of Medicine, Chicago.
“It’s a matter of attitude,” she explained. “Men tend to believe they can and should make life happen. Women tend to believe that what you see is what you get. Even when women do negotiate, they tend to ask for 15%-30% less than their male colleagues. If you don’t ask, you won’t get.”
Simply taking the lead in negotiations can improve the outcome, she continued. Network with colleagues and mentors to find the appropriate ranges for salaries, benefits, and perks such as parking, spousal job opportunities, facilities and space, teaching expectations, administrative support, and more.
Successful careers don’t just happen. They are made by individuals who take charge and build their own success. The alternative is burnout.
“Part of burnout is feeling overburdened, overworked, and out of control,” said Barbara Jung, MD, AGAF, professor and chief of gastroenterology and hepatology at the University of Illinois at Chicago, during Strategies for a Successful Career: Wellness, Empowerment, Leadership and Resilience at Digestive Disease Week® (DDW) 2018. “If somebody is staying until 9 or 10 o’clock [at night] to finish notes, I have a discussion with them. It is good to be done at 5 p.m. and go home. It is all about setting your own priorities and not letting the job take over your life.”
Associations have a role to play, too. The ASGE Technology Committee reported in 2010 that up to 89% of GIs suffer musculoskeletal injuries from manipulating scopes. Colonoscopist’s thumb (left thumb tendonitis) and metacarpophalangeal joint strain were the most common injuries.
“Risk factors are part of our work,” said Mehnaz Shafi, MD, AGAF, professor of gastroenterology, hepatology and nutrition at the University of Texas MD Anderson Cancer Center, Houston. “Pinching, pushing, pulling, and awkward positions are part of what we do. This is an injury with consequences.”
Dr. Shafi chairs the AGA Task Force on Ergonomics. The group has recommended changes to endoscopic work stations that minimize injury. The most important changes include mounting monitors on flexible stands to accommodate GIs of all heights, adding straps to the control head to allow the fingers to relax, providing ergonomic training to all GIs and using patient beds that can be raised and lowered to accommodate both tall and short GIs.
“Shaping your career is one of the key principles in preventing burnout,” said Arthur DeCross, MD, AGAF, professor of medicine, gastroenterology and hepatology at the University of Rochester Medical Center, N.Y. “We know that more than half of gastroenterologists self-identify as being burned out. And one of the major contributors to burnout is lack of control over your work environment, your career, your colleagues. Taking control of your career can make a difference.”
Taking control can be particularly important for women. An AGA burnout survey in 2015 found that 51% of male GIs reported burnout versus 62% of female GIs.
One reason is women’s tendency to negotiate poorly on their own behalf, said Marie-Pier Tétreault, PhD, assistant professor of gastroenterology and hepatology at Northwestern University Feinberg School of Medicine, Chicago.
“It’s a matter of attitude,” she explained. “Men tend to believe they can and should make life happen. Women tend to believe that what you see is what you get. Even when women do negotiate, they tend to ask for 15%-30% less than their male colleagues. If you don’t ask, you won’t get.”
Simply taking the lead in negotiations can improve the outcome, she continued. Network with colleagues and mentors to find the appropriate ranges for salaries, benefits, and perks such as parking, spousal job opportunities, facilities and space, teaching expectations, administrative support, and more.
Successful careers don’t just happen. They are made by individuals who take charge and build their own success. The alternative is burnout.
“Part of burnout is feeling overburdened, overworked, and out of control,” said Barbara Jung, MD, AGAF, professor and chief of gastroenterology and hepatology at the University of Illinois at Chicago, during Strategies for a Successful Career: Wellness, Empowerment, Leadership and Resilience at Digestive Disease Week® (DDW) 2018. “If somebody is staying until 9 or 10 o’clock [at night] to finish notes, I have a discussion with them. It is good to be done at 5 p.m. and go home. It is all about setting your own priorities and not letting the job take over your life.”
Associations have a role to play, too. The ASGE Technology Committee reported in 2010 that up to 89% of GIs suffer musculoskeletal injuries from manipulating scopes. Colonoscopist’s thumb (left thumb tendonitis) and metacarpophalangeal joint strain were the most common injuries.
“Risk factors are part of our work,” said Mehnaz Shafi, MD, AGAF, professor of gastroenterology, hepatology and nutrition at the University of Texas MD Anderson Cancer Center, Houston. “Pinching, pushing, pulling, and awkward positions are part of what we do. This is an injury with consequences.”
Dr. Shafi chairs the AGA Task Force on Ergonomics. The group has recommended changes to endoscopic work stations that minimize injury. The most important changes include mounting monitors on flexible stands to accommodate GIs of all heights, adding straps to the control head to allow the fingers to relax, providing ergonomic training to all GIs and using patient beds that can be raised and lowered to accommodate both tall and short GIs.
“Shaping your career is one of the key principles in preventing burnout,” said Arthur DeCross, MD, AGAF, professor of medicine, gastroenterology and hepatology at the University of Rochester Medical Center, N.Y. “We know that more than half of gastroenterologists self-identify as being burned out. And one of the major contributors to burnout is lack of control over your work environment, your career, your colleagues. Taking control of your career can make a difference.”
Taking control can be particularly important for women. An AGA burnout survey in 2015 found that 51% of male GIs reported burnout versus 62% of female GIs.
One reason is women’s tendency to negotiate poorly on their own behalf, said Marie-Pier Tétreault, PhD, assistant professor of gastroenterology and hepatology at Northwestern University Feinberg School of Medicine, Chicago.
“It’s a matter of attitude,” she explained. “Men tend to believe they can and should make life happen. Women tend to believe that what you see is what you get. Even when women do negotiate, they tend to ask for 15%-30% less than their male colleagues. If you don’t ask, you won’t get.”
Simply taking the lead in negotiations can improve the outcome, she continued. Network with colleagues and mentors to find the appropriate ranges for salaries, benefits, and perks such as parking, spousal job opportunities, facilities and space, teaching expectations, administrative support, and more.
August 2018
Gastroenterology
How to maximize learning in a gastroenterology fellow clinic: Prepare to precept. Kumar NL; Perencevich ML. 2018 Jul;155(1):8-10. doi: 10.1053/j.gastro.2018.06.022.
Management of patients with functional heartburn. Lee YY; Wu JCY. 2018 Jun;154(8):2018-21. doi: 10.1053/j.gastro.2018.04.030.
Skills acquired during my 1-year AGA editorial fellowship. Shah ED. 2018 May;154(6):1563. doi: 10.1053/j.gastro.2018.03.043.
How to incorporate quality improvement and patient safety projects in your training. Siddique SM et al. 2018 May;154(6):1564-8. doi: 10.1053/j.gastro.2018.03.044.
Clin Gastro Hepatol.
Training the endo-thlete: An update in ergonomics in endoscopy. Singla M et al. 2018 Jul;16(7):1003-6. doi: 10.1016/j.cgh.2018.04.019.
Workup and management of bloating. Kamboj AK; Oxentenko AS. 2018 Jul;16(7):1030-3. doi: 10.1016/j.cgh.2017.12.046.
Hiatal and paraesophageal hernias. Callaway JP, Vaezi MF. 2018 Jun;16(6):810-3. doi: 10.1016/j.cgh.2017.12.045.
CMGH
A sabbatical: The gift that keeps on giving. Friedman SL. 2018;5(4):656-8. doi: 10.1016/j.jcmgh.2018.01.010.
Gastroenterology
How to maximize learning in a gastroenterology fellow clinic: Prepare to precept. Kumar NL; Perencevich ML. 2018 Jul;155(1):8-10. doi: 10.1053/j.gastro.2018.06.022.
Management of patients with functional heartburn. Lee YY; Wu JCY. 2018 Jun;154(8):2018-21. doi: 10.1053/j.gastro.2018.04.030.
Skills acquired during my 1-year AGA editorial fellowship. Shah ED. 2018 May;154(6):1563. doi: 10.1053/j.gastro.2018.03.043.
How to incorporate quality improvement and patient safety projects in your training. Siddique SM et al. 2018 May;154(6):1564-8. doi: 10.1053/j.gastro.2018.03.044.
Clin Gastro Hepatol.
Training the endo-thlete: An update in ergonomics in endoscopy. Singla M et al. 2018 Jul;16(7):1003-6. doi: 10.1016/j.cgh.2018.04.019.
Workup and management of bloating. Kamboj AK; Oxentenko AS. 2018 Jul;16(7):1030-3. doi: 10.1016/j.cgh.2017.12.046.
Hiatal and paraesophageal hernias. Callaway JP, Vaezi MF. 2018 Jun;16(6):810-3. doi: 10.1016/j.cgh.2017.12.045.
CMGH
A sabbatical: The gift that keeps on giving. Friedman SL. 2018;5(4):656-8. doi: 10.1016/j.jcmgh.2018.01.010.
Gastroenterology
How to maximize learning in a gastroenterology fellow clinic: Prepare to precept. Kumar NL; Perencevich ML. 2018 Jul;155(1):8-10. doi: 10.1053/j.gastro.2018.06.022.
Management of patients with functional heartburn. Lee YY; Wu JCY. 2018 Jun;154(8):2018-21. doi: 10.1053/j.gastro.2018.04.030.
Skills acquired during my 1-year AGA editorial fellowship. Shah ED. 2018 May;154(6):1563. doi: 10.1053/j.gastro.2018.03.043.
How to incorporate quality improvement and patient safety projects in your training. Siddique SM et al. 2018 May;154(6):1564-8. doi: 10.1053/j.gastro.2018.03.044.
Clin Gastro Hepatol.
Training the endo-thlete: An update in ergonomics in endoscopy. Singla M et al. 2018 Jul;16(7):1003-6. doi: 10.1016/j.cgh.2018.04.019.
Workup and management of bloating. Kamboj AK; Oxentenko AS. 2018 Jul;16(7):1030-3. doi: 10.1016/j.cgh.2017.12.046.
Hiatal and paraesophageal hernias. Callaway JP, Vaezi MF. 2018 Jun;16(6):810-3. doi: 10.1016/j.cgh.2017.12.045.
CMGH
A sabbatical: The gift that keeps on giving. Friedman SL. 2018;5(4):656-8. doi: 10.1016/j.jcmgh.2018.01.010.
Negotiating physician employment agreements
You have finally completed your residency or fellowship, and now you have a job offer. With some trepidation, you decide to read the employment agreement that has been emailed to you. You quickly realize that you do not understand much of it. All those legal terms! You lament the fact that medical school never taught you about the business of medicine. What are you going to do? The choices are actually quite simple: You can take the time to educate yourself or you can hire an expert. This article will review some of the basic principles of negotiating as well as some of the critical issues found in physician employment agreements today.
Whether you represent yourself or hire someone to do it for you, it is important to understand some of the basic principles of negotiating. These principles generally are applicable whether you are buying a house or negotiating your employment agreement.
Negotiations
The most important principle is preparation. For example, many physicians negotiate their salaries during the interview process. Consequently, it is imperative that, before you negotiate your compensation, you know the range of salaries in your area for your specialty. It is also important to know whether salaries are usually guaranteed in your market, or whether production-based salaries (which are based on the amount of your billings) are the norm. Never go into an interview unprepared!
Always try to gain leverage in your negotiations. The easiest way to accomplish this is by having multiple offers, and subtly letting your suitors know this. Allow adequate time to negotiate; the more time you have, the easier it is to negotiate. Establish your objectives and try to anticipate the objectives of the other party. Determine your best-case and worse-case scenarios, as well as the most likely outcome. Do not negotiate against yourself and try to get something every time you give something. Define the nonnegotiable issues, and do not waste time on them. Keep cool and be flexible.
The first question you must answer when you receive an employment agreement is who is going to negotiate it. Many new physicians hire attorneys to help them with their employment agreements and employers expect as much. It is best to engage an attorney before you begin your job search so you can get a better understanding of how the attorney can help you. Most attorneys do not charge a prospective client for such information. However, many physicians wait until they actually receive an offer before contacting an attorney. It is not uncommon for physicians to negotiate their salaries during job interviews even if they eventually hire an attorney to help them. This is usually attributable to a lack of negotiating experience and an eagerness to determine whether a job offer is viable. Keep in mind that an attorney often can negotiate a better starting salary than you, so try to resist the temptation to negotiate your salary during the interview process.
Compensation
With compensation in mind, what are some of the important issues? Today, many physician employers are converting to production-based compensation models. Consequently, it is important for new physicians to obtain guaranteed base salaries during their first few years of employment while they are building their practices.
On occasion, new physicians initially are offered production-based compensation models, which also allocate a share of practice overhead expenses to them. This is a very dangerous compensation model for a new physician. Under such a model, it is possible that a new physician could have a negative balance in his/her cost center at the end of the year, and actually owe his/her employer money.
Some physicians may be offered income guarantees by hospitals. There are several different types of income guarantees but they are frequently categorized together even though they differ significantly. The most common income guarantees offered to physicians are physician recruitment agreements (PRAs). Under a PRA, a hospital usually guarantees that a physician who relocates to the service area of the hospital collects a minimum amount of monthly revenue for 1-2 years, which is known as the guarantee period. The hospital also guarantees to pay certain monthly expenses of the physician during the guarantee period. This arrangement is actually structured as a loan by the hospital to the physician, and requires the physician to execute a promissory note with the hospital for the amounts advanced to the physician by the hospital. The promissory note is forgiven if the physician continues to practice in the service area for 2-3 years after the guarantee period. This type of guarantee provides an excellent opportunity for a new physician to establish a solo practice. A variation of this model involves a third party such as a medical group. Under this model, the hospital continues to guarantee the revenue of the new physician and pays the medical group the expenses it incurs as a result of hiring the new physician. These expenses are known as incremental practice expenses. The medical group also becomes a signatory to the promissory note. Other health care entities also have begun to offer PRAs to physicians. For example, an independent practice association in California recently entered into a PRA with a gastroenterologist.
Keep in mind that the promissory note executed by the physician may affect the credit of the physician, especially if he/she wants to obtain financing for a home purchase. Also, a hospital may seek security for the performance of the promissory note by collateralizing the personal assets of the physician instead of just his/her practice assets; this should be avoided.
The other type of income guarantee is provided to hospital-based physicians such as pathologists, radiologists, anesthesiologists, etc. Under this type of guarantee, a hospital ensures that the physicians receive a minimum threshold of collections. This type of guarantee may be necessary to attract hospital-based physicians to a hospital which has a low-income and/or Medicaid population. This is not a typical scenario for a gastroenterologist.
Some practices create incentives for physicians by offering a variety of bonuses. Most often these bonuses are production based but sometimes they are based on such quality issues as patient satisfaction. The most common types of production bonuses are based on attaining a level of collections above a dollar threshold or exceeding a minimum level of relative value units (RVUs).
To summarize, new physicians should always try to get at least a 2-year income guarantee. They should never allow an employer to allocate overhead to them during the first 2 years of employment. In addition, they should always try to negotiate realistic production-based bonuses.
Benefits
Fringe benefits are an integral part of a compensation package for a new physician. Most physician employers offer a generous package of health insurance, retirement, reimbursable expenses, and paid time off. These benefits should be clearly delineated in the employment agreement or employee handbook. A very common question about health benefits is when they become effective (the first day of employment, 30 days after employment, the first of the month after employment, etc.). This is significant because Consolidated Omnibus Budget Reconciliation Act (COBRA) is quite expensive. Another issue is whether health insurance also will cover the physician’s spouse and dependents. Most physician employers cover only the physician, not his/her spouse and dependents. If a new physician has a spouse who already provides family health benefits, it may behoove the physician to negotiate an allowance in lieu of health benefits.
Paid time off of 10-20 days are commonly given by physician employers to new physicians. Some employers also provide 5 or more additional days of paid time off for Continuing Medical Education (CME). Of course, once a physician goes onto production-based compensation, paid time off usually is not provided.
It is very important that a physician employer offer a retirement plan. Oftentimes, there is a matching contribution by the employer. However, it is not uncommon for there to be a year waiting period for eligibility in the retirement plan. Retirement plans vary significantly so it is advisable for a new physician to meet with the employer’s human resources department to get the details of the plan offered; the physician may want to confer with a financial advisor after obtaining this information.
Most physician employers reimburse licensing and DEA fees, medical staff dues, and board certification expenses. There is often a CME allowance as well. In competitive markets, some physician employers also offer innovative benefits such as student loan repayment programs, fellowship and residency stipends, and forgivable loans for housing. Sometimes these benefits are not included in the employment agreement; you may have to ask for them.
Indemnification/noncompetition
In addition to compensation and benefits, there are several other issues which are commonly found in employment agreements. Perhaps the most controversial is the issue of indemnification. The legal concept of indemnity allows a physician employer to recover damages and defense costs from a physician employee in certain circumstances. For example, if a physician employer has a $1,000,000/$3,000,000 malpractice policy covering itself and each of its physician employees, and if a physician commits malpractice and the award is $2,000,000, the employer may seek to recover the $1,000,000 deficit from the physician. In California, for example, the physician employer would be prohibited from seeking the deficit from the physician employee, but in most states, it is permitted. Because insurance policies usually do not cover physicians for damages, expenses, costs, etc as a result of an indemnification action, there is no practical way for a physician to protect himself/herself from the consequences. It is very important that physicians not sign any type of agreement with an indemnification clause in it without consulting an attorney first.
Another controversial issue is noncompete restrictions. In many states, a physician employer can restrict a physician employee from competing with it after an employment agreement is terminated. The noncompete prohibitions usually last for 1-2 years and extend over a geographic area, which often causes a terminated physician to relocate. Importantly, noncompete clauses are generally enforceable in most states.
Tail coverage
Malpractice tail coverage often can be an issue as well. For many years, physician employers routinely paid the cost of tail coverage for a physician employee after termination of employment. Tail coverage is necessary because most malpractice policies are claims-made insurance instead of occurrence insurance. This means that the insurance is applicable when a claim is filed versus when a malpractice act or omission occurred. Because of the significant cost of tail coverage, many physician employers attempt to transfer this financial responsibility to physician employees. Depending on a physician’s specialty, tail coverage can be quite costly. Consequently, it behooves physicians to carefully negotiate this issue. If a physician employer is unwilling to provide tail coverage, a compromise may be proposed whereby the physician employee is responsible only for the cost of tail coverage if he/she terminates the employment agreement without cause or if the physician employer terminates the employment agreement for cause. Conversely, the physician employer would be responsible for the cost if the physician employer terminates the employment agreement without cause or the physician employee terminates the employment agreement for cause.
Equity accrual
Finally, new physicians always should ask whether there is an opportunity to obtain equity in the organizations that hire them. Many for-profit physician employers provide such an opportunity to new physicians after 2-3 years. However, timing is just one factor. Importantly, the cost of the buy-in is critical especially to new physicians with student loans. Recognizing this problem, the trend today is for physician employers to have nominal buy-ins. Notwithstanding this trend, some physician employers also own ambulatory surgery centers and the buy-ins for these entities must be at fair market value and cannot be financed by the center or its owners under the law. Consequently, the buy-in for ambulatory surgery centers is usually substantial and requires a physician to obtain outside financing.
In conclusion, when evaluating the viability of a physician employment opportunity, salary should be only one factor considered. Fringe benefits, the opportunity for equity, and the fairness of the employment agreement also should be weighed heavily by a physician. It is important for a physician to be comfortable with his/her peers and work environment. Selecting the right job opportunity can be challenging. However, the process will be much easier if you remember the basic principles of negotiating.
You have finally completed your residency or fellowship, and now you have a job offer. With some trepidation, you decide to read the employment agreement that has been emailed to you. You quickly realize that you do not understand much of it. All those legal terms! You lament the fact that medical school never taught you about the business of medicine. What are you going to do? The choices are actually quite simple: You can take the time to educate yourself or you can hire an expert. This article will review some of the basic principles of negotiating as well as some of the critical issues found in physician employment agreements today.
Whether you represent yourself or hire someone to do it for you, it is important to understand some of the basic principles of negotiating. These principles generally are applicable whether you are buying a house or negotiating your employment agreement.
Negotiations
The most important principle is preparation. For example, many physicians negotiate their salaries during the interview process. Consequently, it is imperative that, before you negotiate your compensation, you know the range of salaries in your area for your specialty. It is also important to know whether salaries are usually guaranteed in your market, or whether production-based salaries (which are based on the amount of your billings) are the norm. Never go into an interview unprepared!
Always try to gain leverage in your negotiations. The easiest way to accomplish this is by having multiple offers, and subtly letting your suitors know this. Allow adequate time to negotiate; the more time you have, the easier it is to negotiate. Establish your objectives and try to anticipate the objectives of the other party. Determine your best-case and worse-case scenarios, as well as the most likely outcome. Do not negotiate against yourself and try to get something every time you give something. Define the nonnegotiable issues, and do not waste time on them. Keep cool and be flexible.
The first question you must answer when you receive an employment agreement is who is going to negotiate it. Many new physicians hire attorneys to help them with their employment agreements and employers expect as much. It is best to engage an attorney before you begin your job search so you can get a better understanding of how the attorney can help you. Most attorneys do not charge a prospective client for such information. However, many physicians wait until they actually receive an offer before contacting an attorney. It is not uncommon for physicians to negotiate their salaries during job interviews even if they eventually hire an attorney to help them. This is usually attributable to a lack of negotiating experience and an eagerness to determine whether a job offer is viable. Keep in mind that an attorney often can negotiate a better starting salary than you, so try to resist the temptation to negotiate your salary during the interview process.
Compensation
With compensation in mind, what are some of the important issues? Today, many physician employers are converting to production-based compensation models. Consequently, it is important for new physicians to obtain guaranteed base salaries during their first few years of employment while they are building their practices.
On occasion, new physicians initially are offered production-based compensation models, which also allocate a share of practice overhead expenses to them. This is a very dangerous compensation model for a new physician. Under such a model, it is possible that a new physician could have a negative balance in his/her cost center at the end of the year, and actually owe his/her employer money.
Some physicians may be offered income guarantees by hospitals. There are several different types of income guarantees but they are frequently categorized together even though they differ significantly. The most common income guarantees offered to physicians are physician recruitment agreements (PRAs). Under a PRA, a hospital usually guarantees that a physician who relocates to the service area of the hospital collects a minimum amount of monthly revenue for 1-2 years, which is known as the guarantee period. The hospital also guarantees to pay certain monthly expenses of the physician during the guarantee period. This arrangement is actually structured as a loan by the hospital to the physician, and requires the physician to execute a promissory note with the hospital for the amounts advanced to the physician by the hospital. The promissory note is forgiven if the physician continues to practice in the service area for 2-3 years after the guarantee period. This type of guarantee provides an excellent opportunity for a new physician to establish a solo practice. A variation of this model involves a third party such as a medical group. Under this model, the hospital continues to guarantee the revenue of the new physician and pays the medical group the expenses it incurs as a result of hiring the new physician. These expenses are known as incremental practice expenses. The medical group also becomes a signatory to the promissory note. Other health care entities also have begun to offer PRAs to physicians. For example, an independent practice association in California recently entered into a PRA with a gastroenterologist.
Keep in mind that the promissory note executed by the physician may affect the credit of the physician, especially if he/she wants to obtain financing for a home purchase. Also, a hospital may seek security for the performance of the promissory note by collateralizing the personal assets of the physician instead of just his/her practice assets; this should be avoided.
The other type of income guarantee is provided to hospital-based physicians such as pathologists, radiologists, anesthesiologists, etc. Under this type of guarantee, a hospital ensures that the physicians receive a minimum threshold of collections. This type of guarantee may be necessary to attract hospital-based physicians to a hospital which has a low-income and/or Medicaid population. This is not a typical scenario for a gastroenterologist.
Some practices create incentives for physicians by offering a variety of bonuses. Most often these bonuses are production based but sometimes they are based on such quality issues as patient satisfaction. The most common types of production bonuses are based on attaining a level of collections above a dollar threshold or exceeding a minimum level of relative value units (RVUs).
To summarize, new physicians should always try to get at least a 2-year income guarantee. They should never allow an employer to allocate overhead to them during the first 2 years of employment. In addition, they should always try to negotiate realistic production-based bonuses.
Benefits
Fringe benefits are an integral part of a compensation package for a new physician. Most physician employers offer a generous package of health insurance, retirement, reimbursable expenses, and paid time off. These benefits should be clearly delineated in the employment agreement or employee handbook. A very common question about health benefits is when they become effective (the first day of employment, 30 days after employment, the first of the month after employment, etc.). This is significant because Consolidated Omnibus Budget Reconciliation Act (COBRA) is quite expensive. Another issue is whether health insurance also will cover the physician’s spouse and dependents. Most physician employers cover only the physician, not his/her spouse and dependents. If a new physician has a spouse who already provides family health benefits, it may behoove the physician to negotiate an allowance in lieu of health benefits.
Paid time off of 10-20 days are commonly given by physician employers to new physicians. Some employers also provide 5 or more additional days of paid time off for Continuing Medical Education (CME). Of course, once a physician goes onto production-based compensation, paid time off usually is not provided.
It is very important that a physician employer offer a retirement plan. Oftentimes, there is a matching contribution by the employer. However, it is not uncommon for there to be a year waiting period for eligibility in the retirement plan. Retirement plans vary significantly so it is advisable for a new physician to meet with the employer’s human resources department to get the details of the plan offered; the physician may want to confer with a financial advisor after obtaining this information.
Most physician employers reimburse licensing and DEA fees, medical staff dues, and board certification expenses. There is often a CME allowance as well. In competitive markets, some physician employers also offer innovative benefits such as student loan repayment programs, fellowship and residency stipends, and forgivable loans for housing. Sometimes these benefits are not included in the employment agreement; you may have to ask for them.
Indemnification/noncompetition
In addition to compensation and benefits, there are several other issues which are commonly found in employment agreements. Perhaps the most controversial is the issue of indemnification. The legal concept of indemnity allows a physician employer to recover damages and defense costs from a physician employee in certain circumstances. For example, if a physician employer has a $1,000,000/$3,000,000 malpractice policy covering itself and each of its physician employees, and if a physician commits malpractice and the award is $2,000,000, the employer may seek to recover the $1,000,000 deficit from the physician. In California, for example, the physician employer would be prohibited from seeking the deficit from the physician employee, but in most states, it is permitted. Because insurance policies usually do not cover physicians for damages, expenses, costs, etc as a result of an indemnification action, there is no practical way for a physician to protect himself/herself from the consequences. It is very important that physicians not sign any type of agreement with an indemnification clause in it without consulting an attorney first.
Another controversial issue is noncompete restrictions. In many states, a physician employer can restrict a physician employee from competing with it after an employment agreement is terminated. The noncompete prohibitions usually last for 1-2 years and extend over a geographic area, which often causes a terminated physician to relocate. Importantly, noncompete clauses are generally enforceable in most states.
Tail coverage
Malpractice tail coverage often can be an issue as well. For many years, physician employers routinely paid the cost of tail coverage for a physician employee after termination of employment. Tail coverage is necessary because most malpractice policies are claims-made insurance instead of occurrence insurance. This means that the insurance is applicable when a claim is filed versus when a malpractice act or omission occurred. Because of the significant cost of tail coverage, many physician employers attempt to transfer this financial responsibility to physician employees. Depending on a physician’s specialty, tail coverage can be quite costly. Consequently, it behooves physicians to carefully negotiate this issue. If a physician employer is unwilling to provide tail coverage, a compromise may be proposed whereby the physician employee is responsible only for the cost of tail coverage if he/she terminates the employment agreement without cause or if the physician employer terminates the employment agreement for cause. Conversely, the physician employer would be responsible for the cost if the physician employer terminates the employment agreement without cause or the physician employee terminates the employment agreement for cause.
Equity accrual
Finally, new physicians always should ask whether there is an opportunity to obtain equity in the organizations that hire them. Many for-profit physician employers provide such an opportunity to new physicians after 2-3 years. However, timing is just one factor. Importantly, the cost of the buy-in is critical especially to new physicians with student loans. Recognizing this problem, the trend today is for physician employers to have nominal buy-ins. Notwithstanding this trend, some physician employers also own ambulatory surgery centers and the buy-ins for these entities must be at fair market value and cannot be financed by the center or its owners under the law. Consequently, the buy-in for ambulatory surgery centers is usually substantial and requires a physician to obtain outside financing.
In conclusion, when evaluating the viability of a physician employment opportunity, salary should be only one factor considered. Fringe benefits, the opportunity for equity, and the fairness of the employment agreement also should be weighed heavily by a physician. It is important for a physician to be comfortable with his/her peers and work environment. Selecting the right job opportunity can be challenging. However, the process will be much easier if you remember the basic principles of negotiating.
You have finally completed your residency or fellowship, and now you have a job offer. With some trepidation, you decide to read the employment agreement that has been emailed to you. You quickly realize that you do not understand much of it. All those legal terms! You lament the fact that medical school never taught you about the business of medicine. What are you going to do? The choices are actually quite simple: You can take the time to educate yourself or you can hire an expert. This article will review some of the basic principles of negotiating as well as some of the critical issues found in physician employment agreements today.
Whether you represent yourself or hire someone to do it for you, it is important to understand some of the basic principles of negotiating. These principles generally are applicable whether you are buying a house or negotiating your employment agreement.
Negotiations
The most important principle is preparation. For example, many physicians negotiate their salaries during the interview process. Consequently, it is imperative that, before you negotiate your compensation, you know the range of salaries in your area for your specialty. It is also important to know whether salaries are usually guaranteed in your market, or whether production-based salaries (which are based on the amount of your billings) are the norm. Never go into an interview unprepared!
Always try to gain leverage in your negotiations. The easiest way to accomplish this is by having multiple offers, and subtly letting your suitors know this. Allow adequate time to negotiate; the more time you have, the easier it is to negotiate. Establish your objectives and try to anticipate the objectives of the other party. Determine your best-case and worse-case scenarios, as well as the most likely outcome. Do not negotiate against yourself and try to get something every time you give something. Define the nonnegotiable issues, and do not waste time on them. Keep cool and be flexible.
The first question you must answer when you receive an employment agreement is who is going to negotiate it. Many new physicians hire attorneys to help them with their employment agreements and employers expect as much. It is best to engage an attorney before you begin your job search so you can get a better understanding of how the attorney can help you. Most attorneys do not charge a prospective client for such information. However, many physicians wait until they actually receive an offer before contacting an attorney. It is not uncommon for physicians to negotiate their salaries during job interviews even if they eventually hire an attorney to help them. This is usually attributable to a lack of negotiating experience and an eagerness to determine whether a job offer is viable. Keep in mind that an attorney often can negotiate a better starting salary than you, so try to resist the temptation to negotiate your salary during the interview process.
Compensation
With compensation in mind, what are some of the important issues? Today, many physician employers are converting to production-based compensation models. Consequently, it is important for new physicians to obtain guaranteed base salaries during their first few years of employment while they are building their practices.
On occasion, new physicians initially are offered production-based compensation models, which also allocate a share of practice overhead expenses to them. This is a very dangerous compensation model for a new physician. Under such a model, it is possible that a new physician could have a negative balance in his/her cost center at the end of the year, and actually owe his/her employer money.
Some physicians may be offered income guarantees by hospitals. There are several different types of income guarantees but they are frequently categorized together even though they differ significantly. The most common income guarantees offered to physicians are physician recruitment agreements (PRAs). Under a PRA, a hospital usually guarantees that a physician who relocates to the service area of the hospital collects a minimum amount of monthly revenue for 1-2 years, which is known as the guarantee period. The hospital also guarantees to pay certain monthly expenses of the physician during the guarantee period. This arrangement is actually structured as a loan by the hospital to the physician, and requires the physician to execute a promissory note with the hospital for the amounts advanced to the physician by the hospital. The promissory note is forgiven if the physician continues to practice in the service area for 2-3 years after the guarantee period. This type of guarantee provides an excellent opportunity for a new physician to establish a solo practice. A variation of this model involves a third party such as a medical group. Under this model, the hospital continues to guarantee the revenue of the new physician and pays the medical group the expenses it incurs as a result of hiring the new physician. These expenses are known as incremental practice expenses. The medical group also becomes a signatory to the promissory note. Other health care entities also have begun to offer PRAs to physicians. For example, an independent practice association in California recently entered into a PRA with a gastroenterologist.
Keep in mind that the promissory note executed by the physician may affect the credit of the physician, especially if he/she wants to obtain financing for a home purchase. Also, a hospital may seek security for the performance of the promissory note by collateralizing the personal assets of the physician instead of just his/her practice assets; this should be avoided.
The other type of income guarantee is provided to hospital-based physicians such as pathologists, radiologists, anesthesiologists, etc. Under this type of guarantee, a hospital ensures that the physicians receive a minimum threshold of collections. This type of guarantee may be necessary to attract hospital-based physicians to a hospital which has a low-income and/or Medicaid population. This is not a typical scenario for a gastroenterologist.
Some practices create incentives for physicians by offering a variety of bonuses. Most often these bonuses are production based but sometimes they are based on such quality issues as patient satisfaction. The most common types of production bonuses are based on attaining a level of collections above a dollar threshold or exceeding a minimum level of relative value units (RVUs).
To summarize, new physicians should always try to get at least a 2-year income guarantee. They should never allow an employer to allocate overhead to them during the first 2 years of employment. In addition, they should always try to negotiate realistic production-based bonuses.
Benefits
Fringe benefits are an integral part of a compensation package for a new physician. Most physician employers offer a generous package of health insurance, retirement, reimbursable expenses, and paid time off. These benefits should be clearly delineated in the employment agreement or employee handbook. A very common question about health benefits is when they become effective (the first day of employment, 30 days after employment, the first of the month after employment, etc.). This is significant because Consolidated Omnibus Budget Reconciliation Act (COBRA) is quite expensive. Another issue is whether health insurance also will cover the physician’s spouse and dependents. Most physician employers cover only the physician, not his/her spouse and dependents. If a new physician has a spouse who already provides family health benefits, it may behoove the physician to negotiate an allowance in lieu of health benefits.
Paid time off of 10-20 days are commonly given by physician employers to new physicians. Some employers also provide 5 or more additional days of paid time off for Continuing Medical Education (CME). Of course, once a physician goes onto production-based compensation, paid time off usually is not provided.
It is very important that a physician employer offer a retirement plan. Oftentimes, there is a matching contribution by the employer. However, it is not uncommon for there to be a year waiting period for eligibility in the retirement plan. Retirement plans vary significantly so it is advisable for a new physician to meet with the employer’s human resources department to get the details of the plan offered; the physician may want to confer with a financial advisor after obtaining this information.
Most physician employers reimburse licensing and DEA fees, medical staff dues, and board certification expenses. There is often a CME allowance as well. In competitive markets, some physician employers also offer innovative benefits such as student loan repayment programs, fellowship and residency stipends, and forgivable loans for housing. Sometimes these benefits are not included in the employment agreement; you may have to ask for them.
Indemnification/noncompetition
In addition to compensation and benefits, there are several other issues which are commonly found in employment agreements. Perhaps the most controversial is the issue of indemnification. The legal concept of indemnity allows a physician employer to recover damages and defense costs from a physician employee in certain circumstances. For example, if a physician employer has a $1,000,000/$3,000,000 malpractice policy covering itself and each of its physician employees, and if a physician commits malpractice and the award is $2,000,000, the employer may seek to recover the $1,000,000 deficit from the physician. In California, for example, the physician employer would be prohibited from seeking the deficit from the physician employee, but in most states, it is permitted. Because insurance policies usually do not cover physicians for damages, expenses, costs, etc as a result of an indemnification action, there is no practical way for a physician to protect himself/herself from the consequences. It is very important that physicians not sign any type of agreement with an indemnification clause in it without consulting an attorney first.
Another controversial issue is noncompete restrictions. In many states, a physician employer can restrict a physician employee from competing with it after an employment agreement is terminated. The noncompete prohibitions usually last for 1-2 years and extend over a geographic area, which often causes a terminated physician to relocate. Importantly, noncompete clauses are generally enforceable in most states.
Tail coverage
Malpractice tail coverage often can be an issue as well. For many years, physician employers routinely paid the cost of tail coverage for a physician employee after termination of employment. Tail coverage is necessary because most malpractice policies are claims-made insurance instead of occurrence insurance. This means that the insurance is applicable when a claim is filed versus when a malpractice act or omission occurred. Because of the significant cost of tail coverage, many physician employers attempt to transfer this financial responsibility to physician employees. Depending on a physician’s specialty, tail coverage can be quite costly. Consequently, it behooves physicians to carefully negotiate this issue. If a physician employer is unwilling to provide tail coverage, a compromise may be proposed whereby the physician employee is responsible only for the cost of tail coverage if he/she terminates the employment agreement without cause or if the physician employer terminates the employment agreement for cause. Conversely, the physician employer would be responsible for the cost if the physician employer terminates the employment agreement without cause or the physician employee terminates the employment agreement for cause.
Equity accrual
Finally, new physicians always should ask whether there is an opportunity to obtain equity in the organizations that hire them. Many for-profit physician employers provide such an opportunity to new physicians after 2-3 years. However, timing is just one factor. Importantly, the cost of the buy-in is critical especially to new physicians with student loans. Recognizing this problem, the trend today is for physician employers to have nominal buy-ins. Notwithstanding this trend, some physician employers also own ambulatory surgery centers and the buy-ins for these entities must be at fair market value and cannot be financed by the center or its owners under the law. Consequently, the buy-in for ambulatory surgery centers is usually substantial and requires a physician to obtain outside financing.
In conclusion, when evaluating the viability of a physician employment opportunity, salary should be only one factor considered. Fringe benefits, the opportunity for equity, and the fairness of the employment agreement also should be weighed heavily by a physician. It is important for a physician to be comfortable with his/her peers and work environment. Selecting the right job opportunity can be challenging. However, the process will be much easier if you remember the basic principles of negotiating.
My experience with the 2017 Gastroenterology Editorial Fellowship
When I entered the Gastroenterology Editorial Fellowship last year, many of my cofellows asked, “What exactly is an editorial fellowship?” After completing the program, I can now reflect on what was truly a fantastic year-long experience that complemented my final year of fellowship training.
Manuscripts certainly don’t review and accept themselves into journals, and fellowship training usually gives little insight into how manuscripts move through the submission, peer review, and production processes. What happens while authors wait for an editorial decision?
Since its first publication in 1943, Gastroenterology has importantly affected clinical care and the direction of research in our field. The quality of the American Gastroenterological Association’s flagship journal is derived from the sweat and muscle put in daily by gastroenterology-oriented and hepatology-oriented professionals who strive to transform the steady stream of cutting-edge manuscript submissions into an influential monthly publication read by a broad audience of clinicians, trainees, academic researchers, and policy makers. Without a doubt, this fellowship provided me with a sincere appreciation for the dedication that the board of editors puts into the peer review process and into maintaining the quality of monthly publications.
Near the beginning of my editorial fellowship, I spent a week at Vanderbilt University with the on-site editors. This was an irreplaceable opportunity for a trainee like myself to meet with both clinical- and research-oriented academic gastroenterologists who integrate demanding editorial roles into busy and fulfilling professional careers. Throughout my week there, I met with editors and staff who held various roles within the journal. Overall, this experience taught me about what metrics the journal uses to ensure quality, how manuscripts move from submission to publication, and how the direction and content of the journal is directed toward both AGA members and a broader readership.
At its core, the fellowship was focused on teaching the fundamental process of peer review. High-quality reviews for Gastroenterology provide consultative content and methodological expertise to editors who can then provide direction and make editorial recommendations to the authors. During my fellowship, I learned how to write a structured and nuanced review on the basis of novelty, clinical relevance and effects, and methodological rigor. I was paired with one of the associate editors on the basis of my primary content area of interest and regularly provided reviews for original article submissions. As the year progressed, I become more comfortable with reviewing beyond my immediate knowledge base. I also became more adept at providing detailed comments that would be insightful and accessible to both authors and editors.
Each week, I participated in a phone call with the board of editors, which was composed of thought leaders with content expertise in both gastroenterology and hepatology. During the call, we would thoughtfully critique some of the most cutting-edge research in our field; each manuscript often represented the culmination of years of meticulous work by research groups and multinational collaborations. From a fellow’s perspective, these calls gave me access to what may be the most insightful discussions taking place in our field, discussions which could have potential implications on future disease management principles and clinical practice guidelines. Through our meetings, it became apparent how much work goes into finding quality reviewers and how much time goes into assimilating the resulting recommendations into a cohesive discussion. This was an opportunity to learn how associate editors walk the entire board through a manuscript: from a basis of current knowledge and practice, through the conduct and findings of a particular study, and ultimately, to how study findings might affect the field.
What I came away with the most from the Gastroenterology Editorial Fellowship was an appreciation for the importance of the editorial and peer review process in maintaining the integrity and detail needed in high-quality research. Ultimately, this fellowship gave me a meaningful and immediate way to give back to the field that I can continue over the course of my professional career. I am certain that this unique program will continue to give future editorial fellows the skills and motivation they need to become actively involved in the editorial and peer review processes when they are beginning their independent careers.
Dr. Shah, MD, MBA, is an assistant professor; he is also the director of the Center for Gastrointestinal Motility in the division of gastroenterology in the department of internal medicine at Dartmouth-Hitchcock Medical Center, Lebanon, N.H.
When I entered the Gastroenterology Editorial Fellowship last year, many of my cofellows asked, “What exactly is an editorial fellowship?” After completing the program, I can now reflect on what was truly a fantastic year-long experience that complemented my final year of fellowship training.
Manuscripts certainly don’t review and accept themselves into journals, and fellowship training usually gives little insight into how manuscripts move through the submission, peer review, and production processes. What happens while authors wait for an editorial decision?
Since its first publication in 1943, Gastroenterology has importantly affected clinical care and the direction of research in our field. The quality of the American Gastroenterological Association’s flagship journal is derived from the sweat and muscle put in daily by gastroenterology-oriented and hepatology-oriented professionals who strive to transform the steady stream of cutting-edge manuscript submissions into an influential monthly publication read by a broad audience of clinicians, trainees, academic researchers, and policy makers. Without a doubt, this fellowship provided me with a sincere appreciation for the dedication that the board of editors puts into the peer review process and into maintaining the quality of monthly publications.
Near the beginning of my editorial fellowship, I spent a week at Vanderbilt University with the on-site editors. This was an irreplaceable opportunity for a trainee like myself to meet with both clinical- and research-oriented academic gastroenterologists who integrate demanding editorial roles into busy and fulfilling professional careers. Throughout my week there, I met with editors and staff who held various roles within the journal. Overall, this experience taught me about what metrics the journal uses to ensure quality, how manuscripts move from submission to publication, and how the direction and content of the journal is directed toward both AGA members and a broader readership.
At its core, the fellowship was focused on teaching the fundamental process of peer review. High-quality reviews for Gastroenterology provide consultative content and methodological expertise to editors who can then provide direction and make editorial recommendations to the authors. During my fellowship, I learned how to write a structured and nuanced review on the basis of novelty, clinical relevance and effects, and methodological rigor. I was paired with one of the associate editors on the basis of my primary content area of interest and regularly provided reviews for original article submissions. As the year progressed, I become more comfortable with reviewing beyond my immediate knowledge base. I also became more adept at providing detailed comments that would be insightful and accessible to both authors and editors.
Each week, I participated in a phone call with the board of editors, which was composed of thought leaders with content expertise in both gastroenterology and hepatology. During the call, we would thoughtfully critique some of the most cutting-edge research in our field; each manuscript often represented the culmination of years of meticulous work by research groups and multinational collaborations. From a fellow’s perspective, these calls gave me access to what may be the most insightful discussions taking place in our field, discussions which could have potential implications on future disease management principles and clinical practice guidelines. Through our meetings, it became apparent how much work goes into finding quality reviewers and how much time goes into assimilating the resulting recommendations into a cohesive discussion. This was an opportunity to learn how associate editors walk the entire board through a manuscript: from a basis of current knowledge and practice, through the conduct and findings of a particular study, and ultimately, to how study findings might affect the field.
What I came away with the most from the Gastroenterology Editorial Fellowship was an appreciation for the importance of the editorial and peer review process in maintaining the integrity and detail needed in high-quality research. Ultimately, this fellowship gave me a meaningful and immediate way to give back to the field that I can continue over the course of my professional career. I am certain that this unique program will continue to give future editorial fellows the skills and motivation they need to become actively involved in the editorial and peer review processes when they are beginning their independent careers.
Dr. Shah, MD, MBA, is an assistant professor; he is also the director of the Center for Gastrointestinal Motility in the division of gastroenterology in the department of internal medicine at Dartmouth-Hitchcock Medical Center, Lebanon, N.H.
When I entered the Gastroenterology Editorial Fellowship last year, many of my cofellows asked, “What exactly is an editorial fellowship?” After completing the program, I can now reflect on what was truly a fantastic year-long experience that complemented my final year of fellowship training.
Manuscripts certainly don’t review and accept themselves into journals, and fellowship training usually gives little insight into how manuscripts move through the submission, peer review, and production processes. What happens while authors wait for an editorial decision?
Since its first publication in 1943, Gastroenterology has importantly affected clinical care and the direction of research in our field. The quality of the American Gastroenterological Association’s flagship journal is derived from the sweat and muscle put in daily by gastroenterology-oriented and hepatology-oriented professionals who strive to transform the steady stream of cutting-edge manuscript submissions into an influential monthly publication read by a broad audience of clinicians, trainees, academic researchers, and policy makers. Without a doubt, this fellowship provided me with a sincere appreciation for the dedication that the board of editors puts into the peer review process and into maintaining the quality of monthly publications.
Near the beginning of my editorial fellowship, I spent a week at Vanderbilt University with the on-site editors. This was an irreplaceable opportunity for a trainee like myself to meet with both clinical- and research-oriented academic gastroenterologists who integrate demanding editorial roles into busy and fulfilling professional careers. Throughout my week there, I met with editors and staff who held various roles within the journal. Overall, this experience taught me about what metrics the journal uses to ensure quality, how manuscripts move from submission to publication, and how the direction and content of the journal is directed toward both AGA members and a broader readership.
At its core, the fellowship was focused on teaching the fundamental process of peer review. High-quality reviews for Gastroenterology provide consultative content and methodological expertise to editors who can then provide direction and make editorial recommendations to the authors. During my fellowship, I learned how to write a structured and nuanced review on the basis of novelty, clinical relevance and effects, and methodological rigor. I was paired with one of the associate editors on the basis of my primary content area of interest and regularly provided reviews for original article submissions. As the year progressed, I become more comfortable with reviewing beyond my immediate knowledge base. I also became more adept at providing detailed comments that would be insightful and accessible to both authors and editors.
Each week, I participated in a phone call with the board of editors, which was composed of thought leaders with content expertise in both gastroenterology and hepatology. During the call, we would thoughtfully critique some of the most cutting-edge research in our field; each manuscript often represented the culmination of years of meticulous work by research groups and multinational collaborations. From a fellow’s perspective, these calls gave me access to what may be the most insightful discussions taking place in our field, discussions which could have potential implications on future disease management principles and clinical practice guidelines. Through our meetings, it became apparent how much work goes into finding quality reviewers and how much time goes into assimilating the resulting recommendations into a cohesive discussion. This was an opportunity to learn how associate editors walk the entire board through a manuscript: from a basis of current knowledge and practice, through the conduct and findings of a particular study, and ultimately, to how study findings might affect the field.
What I came away with the most from the Gastroenterology Editorial Fellowship was an appreciation for the importance of the editorial and peer review process in maintaining the integrity and detail needed in high-quality research. Ultimately, this fellowship gave me a meaningful and immediate way to give back to the field that I can continue over the course of my professional career. I am certain that this unique program will continue to give future editorial fellows the skills and motivation they need to become actively involved in the editorial and peer review processes when they are beginning their independent careers.
Dr. Shah, MD, MBA, is an assistant professor; he is also the director of the Center for Gastrointestinal Motility in the division of gastroenterology in the department of internal medicine at Dartmouth-Hitchcock Medical Center, Lebanon, N.H.
May 2018
Gastroenterology
How to perform a high-quality examination in patients with Barrett’s esophagus. Everson M et al. 2018 April;154(5):1222-6. doi.org/10.1053/j.gastro.2018.03.001
How to become a physician executive: From fellowship to leadership. Shah ED and Allen JI. 2018 March;154(4):784-7. doi.org/10.1053/j.gastro.2018.02.009
How to obtain training in nutrition during the gastroenterology fellowship. Micic D et al.2018 Feb;154(3):467-70. doi.org/10.1053/j.gastro.2018.01.006
Clin Gastroenterol Hepatol.
Physician burnout: The hidden health care crisis. Lacy BE and Chan JL.2018 March;16(3):311-7. doi.org/10.1016/j.cgh.2017.06.043
AGA Perspectives
Vol. 14 No. 1 | December/January 2018
Everything you need to know about MOC. AGA staff writers.
Vol. 13 No. 5 | October/November 2017
Gastroenterologists as patient advocates in public policy. Siddique SM and Mehta S.
Gastroenterology
How to perform a high-quality examination in patients with Barrett’s esophagus. Everson M et al. 2018 April;154(5):1222-6. doi.org/10.1053/j.gastro.2018.03.001
How to become a physician executive: From fellowship to leadership. Shah ED and Allen JI. 2018 March;154(4):784-7. doi.org/10.1053/j.gastro.2018.02.009
How to obtain training in nutrition during the gastroenterology fellowship. Micic D et al.2018 Feb;154(3):467-70. doi.org/10.1053/j.gastro.2018.01.006
Clin Gastroenterol Hepatol.
Physician burnout: The hidden health care crisis. Lacy BE and Chan JL.2018 March;16(3):311-7. doi.org/10.1016/j.cgh.2017.06.043
AGA Perspectives
Vol. 14 No. 1 | December/January 2018
Everything you need to know about MOC. AGA staff writers.
Vol. 13 No. 5 | October/November 2017
Gastroenterologists as patient advocates in public policy. Siddique SM and Mehta S.
Gastroenterology
How to perform a high-quality examination in patients with Barrett’s esophagus. Everson M et al. 2018 April;154(5):1222-6. doi.org/10.1053/j.gastro.2018.03.001
How to become a physician executive: From fellowship to leadership. Shah ED and Allen JI. 2018 March;154(4):784-7. doi.org/10.1053/j.gastro.2018.02.009
How to obtain training in nutrition during the gastroenterology fellowship. Micic D et al.2018 Feb;154(3):467-70. doi.org/10.1053/j.gastro.2018.01.006
Clin Gastroenterol Hepatol.
Physician burnout: The hidden health care crisis. Lacy BE and Chan JL.2018 March;16(3):311-7. doi.org/10.1016/j.cgh.2017.06.043
AGA Perspectives
Vol. 14 No. 1 | December/January 2018
Everything you need to know about MOC. AGA staff writers.
Vol. 13 No. 5 | October/November 2017
Gastroenterologists as patient advocates in public policy. Siddique SM and Mehta S.
Underserved populations and colorectal cancer screening: Patient perceptions of barriers to care and effective interventions
Editor's Note:
Importantly, these barriers often vary between specific population subsets. In this month’s In Focus article, brought to you by The New Gastroenterologist, the members of the AGA Institute Diversity Committee provide an enlightening overview of the barriers affecting underserved populations as well as strategies that can be employed to overcome these impediments. Better understanding of patient-specific barriers will, I hope, allow us to more effectively redress them and ultimately increase colorectal cancer screening rates in all populations.
Bryson W. Katona, MD, PhD
Editor in Chief, The New Gastroenterologist
Despite the positive public health effects of colorectal cancer (CRC) screening, there remains differential uptake of CRC screening in the United States. Minority populations born in the United States and immigrant populations are among those with the lowest rates of CRC screening, and both socioeconomic status and ethnicity are strongly associated with stage of CRC at diagnosis.1,2 Thus, recognizing the economic, social, and cultural factors that result in low rates of CRC screening in underserved populations is important in order to devise targeted interventions to increase CRC uptake and reduce morbidity and mortality in these populations.

What are the facts and figures?
The overall rate of screening colonoscopies has increased in all ethnic groups in the past 10 years but still falls below the goal of 71% established by the Healthy People project (www.healthypeople.gov) for the year 2020.3 According to the Centers for Disease Control and Prevention ethnicity-specific data for U.S.-born populations, 60% of whites, 55% of African Americans (AA), 50% of American Indian/Alaskan natives (AI/AN), 46% of Latino Americans, and 47% of Asians undergo CRC screening (Figure 1A).4 While CRC incidence in non-Hispanic whites age 50 years and older has dropped by 32% since 2000 because of screening, this trend has not been observed in AAs.5,6
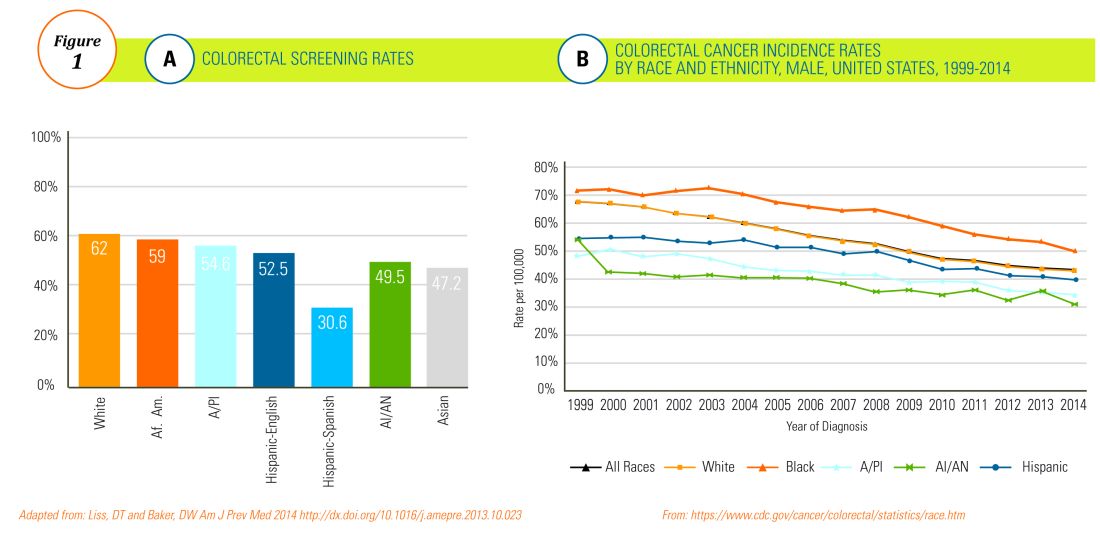
The incidence of CRC in AAs is estimated at 49/10,000, one of the highest amongst U.S. populations and is the second and third most common cancer in AA women and men, respectively (Figure 1B).
Similar to AAs, AI/AN patients present with more advanced CRC disease and at younger ages and have lower survival rates, compared with other racial groups, a trend that has not changed in the last decade.7 CRC screening data in this population vary according to sex, geographic location, and health care utilization, with as few as 4.0% of asymptomatic, average-risk AI/ANs who receive medical care in the Indian Health Services being screened for CRC.8
The low rate of CRC screening among Latinos also poses a significant obstacle to the Healthy People project since it is expected that by 2060 Latinos will constitute 30% of the U.S. population. Therefore, strategies to improve CRC screening in this population are needed to continue the gains made in overall CRC mortality rates.
The percentage of immigrants in the U.S. population increased from 4.7% in 1970 to 13.5% in 2015. Immigrants, regardless of their ethnicity, represent a very vulnerable population, and CRC screening data in this population are not as robust as for U.S.-born groups. In general, immigrants have substantially lower CRC screening rates, compared with U.S.-born populations (21% vs. 60%),9 and it is suspected that additional, significant barriers to CRC screening and care exist for undocumented immigrants.
Another often overlooked group, are individuals with physical or cognitive disabilities. In this group, screening rates range from 49% to 65%.10
Finally, while information is available for many health care conditions and disparities faced by various ethnic groups, there are few CRC screening data for the LGBTQ community. Perhaps amplifying this problem is the existence of conflicting data in this population, with some studies suggesting there is no difference in CRC risk across groups in the LGBTQ community and others suggesting an increased risk.11,12 Notably, sexual orientation has been identified as a positive predictor of CRC screening in gay and bisexual men – CRC screening rates are higher in these groups, compared with heterosexual men.13 In contrast, no such difference has been found between homosexual and heterosexual women.14
What are the barriers?
Several common themes contribute to disparities in CRC screening among minority groups, including psychosocial/cultural, socioeconomic, provider-specific, and insurance-related factors. Some patient-related barriers include issues of illiteracy, having poor health literacy or English proficiency, having only grade school education,15,16 cultural misconceptions, transportation issues, difficulties affording copayments or deductibles, and a lack of follow-up for scheduled appointments and exams.17-20 Poor health literacy has a profound effect on exam perceptions, fear of test results, and compliance with scheduling tests and bowel preparation instructions21-25; it also affects one’s understanding of the importance of CRC screening, the recommended screening age, and the available choice of screening tests.
Even when some apparent barriers are mitigated, disparities in CRC screening remain. For example, even among the insured and among Medicare beneficiaries, screening rates and adequate follow-up rates after abnormal findings remain lower among AAs and those of low socioeconomic status than they are among whites.26-28 At least part of this paradox results from the presence of unmeasured cultural/belief systems that affect CRC screening uptake. Some of these factors include fear and/or denial of CRC diagnoses, mistrust of the health care system, and reluctance to undergo medical treatment and surgery.16,29 AAs are also less likely to be aware of a family history of CRC and to discuss personal and/or family history of CRC or polyps, which can thereby hinder the identification of high-risk individuals who would benefit from early screening.15,30
The deeply rooted sense of fatalism also plays a crucial role and has been cited for many minority and immigrant populations. Fatalism leads patients to view a diagnosis of cancer as a matter of “fate” or “God’s will,” and therefore, it is to be endured.23,31 Similarly, in a qualitative study of 44 Somali men living in St. Paul and Minneapolis, believing cancer was more common in whites, believing they were protected from cancer by God, fearing a cancer diagnosis, and fearing ostracism from their community were reported as barriers to cancer screening.32
Perceptions about CRC screening methods in Latino populations also have a tremendous influence and can include fear, stigma of sexual prejudice, embarrassment of being exposed during the exam, worries about humiliation in a male sense of masculinity, a lack of trust in the medical professionals, a sense of being a “guinea pig” for physicians, concerns about health care racism, and expectations of pain.33-37 Studies have reported that immigrants are afraid to seek health care because of the increasingly hostile environment associated with immigration enforcement.38 In addition, the impending dissolution of the Deferred Action for Childhood Arrivals act is likely to augment the barriers to care for Latino groups.39
In addition, provider-specific barriers to care also exist. Racial and ethnic minorities are less likely than whites to receive recommendations for screening by their physician. In fact, this factor alone has been demonstrated to be the main reason for lack of screening among AAs in a Californian cohort.40 In addition, patients from rural areas or those from AI/AN communities are at especially increased risk for lack of access to care because of a scarcity of providers along with patient perceptions regarding their primary care provider’s ability to connect them to subspecialists.41-43 Other cited examples include misconceptions about and poor treatment of the LGBTQ population by health care providers/systems.44
How can we intervene successfully?
Characterization of barriers is important because it promotes the development of targeted interventions. Intervention models include community engagement programs, incorporation of fecal occult testing, and patient navigator programs.45-47 In response to the alarming disparity in CRC screening rates in Latino communities, several interventions have been set in motion in different clinical scenarios, which include patient navigation and a focus on patient education.
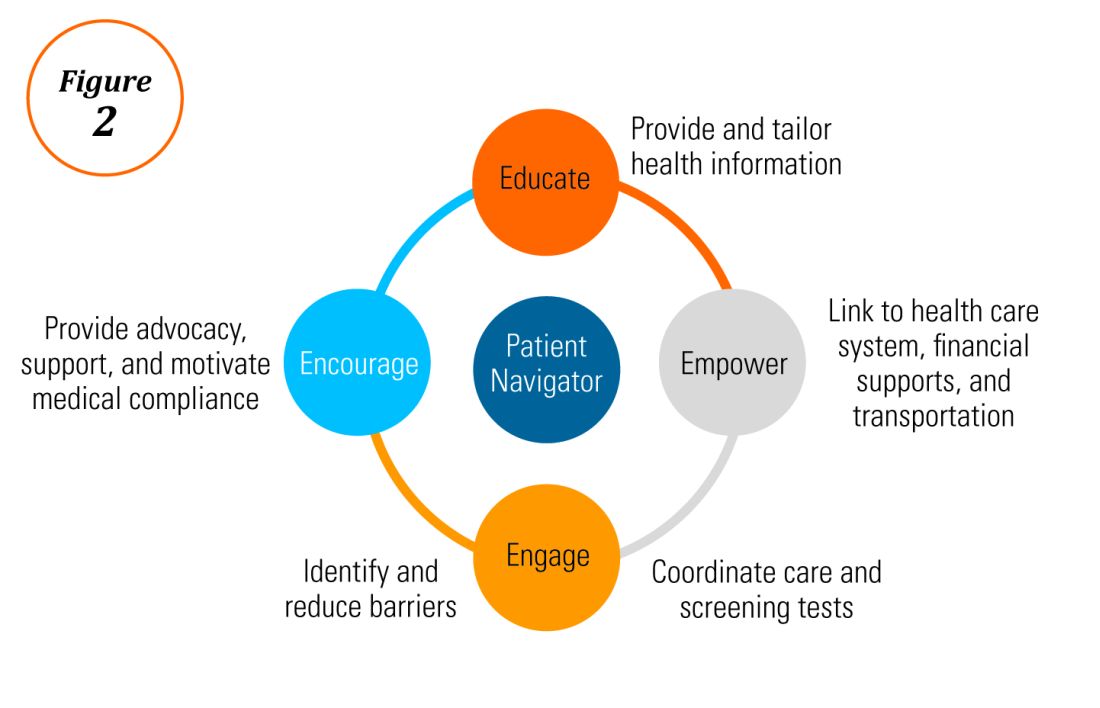
Randomized trials have shown that outreach efforts and patient navigation increase CRC screening rates in AAs.48,54,55 Studies evaluating the effects of print-based educational materials on improving screening showed improvement in screening rates, decreases in cancer-related fatalistic attitudes, and patients had a better understanding of the benefits of screening as compared with the cost associated with screening and the cost of advanced disease.56 Similarly, the use of touch-screen computers that tailor informational messages to decisional stage and screening barriers increased participation in CRC screening.57 Including patient navigators along with printed education material was even more effective at increasing the proportion of patients getting colonoscopy screening than providing printed material alone, with more-intensive navigation needed for individuals with low literacy.58 Grubbs et al.reported the success of their patient navigation program, which included wider comprehensive screening and coverage for colonoscopy screening.59 In AAs, they estimated an annual reduction of CRC incidence and mortality of 4,200 and 2,700 patients, respectively.
Among immigrants, there is an increased likelihood of CRC screening in those immigrants with a higher number of primary care visits.60 The intersection of culture, race, socioeconomic status, housing enclaves, limited English proficiency, low health literacy, and immigration policy all play a role in immigrant health and access to health care.61
Therefore, different strategies may be needed for each immigrant group to improve CRC screening. For this group of patients, efforts aimed at mitigating the adverse effects of national immigration policies on immigrant populations may have the additional consequence of improving health care access and CRC screening for these patients.
Data gaps still exist in our understanding of patient perceptions, perspectives, and barriers that present opportunities for further study to develop long-lasting interventions that will improve health care of underserved populations. By raising awareness of the barriers, physicians can enhance their own self-awareness to keenly be attuned to these challenges as patients cross their clinic threshold for medical care.
Additional resources link: www.cdc.gov/cancer/colorectal/
References
1. Klabunde CN et al. Trends in colorectal cancer test use among vulnerable populations in the United States. Cancer Epidemiol Biomarkers Prev. 2011 Aug;20(8):1611-21.
2. Parikh-Patel A et al. Colorectal cancer stage at diagnosis by socioeconomic and urban/rural status in California, 1988-2000. Cancer. 2006 Sep;107(5 Suppl):1189-95.
3. Promotion OoDPaH. Healthy People 2020. Cancer. Volume 2017.
4. Centers for Disease Control and Prevention. Cancer screening – United States, 2010. MMWR Morb Mortal Wkly Rep. 2012 Jan 27;61(3):41-5.
5. Doubeni CA et al. Racial and ethnic trends of colorectal cancer screening among Medicare enrollees. Am J Prev Med. 2010 Feb;38(2):184-91.
6. Kupfer SS et al. Reducing colorectal cancer risk among African Americans. Gastroenterology. 2015 Nov;149(6):1302-4.
7. Espey DK et al. Annual report to the nation on the status of cancer, 1975-2004, featuring cancer in American Indians and Alaska Natives. Cancer. 2007 Nov;110(10):2119-52.
8. Day LW et al. Screening prevalence and incidence of colorectal cancer among American Indian/Alaskan natives in the Indian Health Service. Dig Dis Sci. 2011 Jul;56(7):2104-13.
9. Gupta S et al. Challenges and possible solutions to colorectal cancer screening for the underserved. J Natl Cancer Inst. 2014 Apr;106(4):dju032.
10. Steele CB et al. Colorectal cancer incidence and screening – United States, 2008 and 2010. MMWR Suppl. 2013 Nov 22;62(3):53-60.
11. Boehmer U et al. Cancer survivorship and sexual orientation. Cancer 2011 Aug 15;117(16):3796-804.
12. Austin SB, Pazaris MJ, Wei EK, et al. Application of the Rosner-Wei risk-prediction model to estimate sexual orientation patterns in colon cancer risk in a prospective cohort of US women. Cancer Causes Control. 2014 Aug;25(8):999-1006.
13. Heslin KC et al. Sexual orientation and testing for prostate and colorectal cancers among men in California. Med Care. 2008 Dec;46(12):1240-8.
14. McElroy JA et al. Advancing Health Care for Lesbian, Gay, Bisexual, and Transgender Patients in Missouri. Mo Med. 2015 Jul-Aug;112(4):262-5.
15. Greiner KA et al. Knowledge and perceptions of colorectal cancer screening among urban African Americans. J Gen Intern Med. 2005 Nov;20(11):977-83.
16. Green PM, Kelly BA. Colorectal cancer knowledge, perceptions, and behaviors in African Americans. Cancer Nurs. 2004 May-Jun;27(3):206-15; quiz 216-7.
17. Berkowitz Z et al. Beliefs, risk perceptions, and gaps in knowledge as barriers to colorectal cancer screening in older adults. J Am Geriatr Soc. 2008 Feb;56(2):307-14.
18. Dolan NC et al. Colorectal cancer screening knowledge, attitudes, and beliefs among veterans: Does literacy make a difference? J Clin Oncol. 2004 Jul;22(13):2617-22.
19. Peterson NB et al. The influence of health literacy on colorectal cancer screening knowledge, beliefs and behavior. J Natl Med Assoc. 2007 Oct;99(10):1105-12.
20. Haddock MG et al. Intraoperative irradiation for locally recurrent colorectal cancer in previously irradiated patients. Int J Radiat Oncol Biol Phys. 2001 Apr 1;49(5):1267-74.
21. Jones RM et al. Patient-reported barriers to colorectal cancer screening: a mixed-methods analysis. Am J Prev Med. 2010 May;38(5):508-16.
22. Basch CH et al. Screening colonoscopy bowel preparation: experience in an urban minority population. Therap Adv Gastroenterol. 2013 Nov;6(6):442-6.
23. Davis JL et al. Sociodemographic differences in fears and mistrust contributing to unwillingness to participate in cancer screenings. J Health Care Poor Underserved. 2012 Nov;23(4 Suppl):67-76.
24. Robinson CM et al. Barriers to colorectal cancer screening among publicly insured urban women: no knowledge of tests and no clinician recommendation. J Natl Med Assoc. 2011 Aug;103(8):746-53.
25. Goldman RE et al. Perspectives of colorectal cancer risk and screening among Dominicans and Puerto Ricans: Stigma and misperceptions. Qual Health Res. 2009 Nov;19(11):1559-68.
26. Laiyemo AO et al. Race and colorectal cancer disparities: Health-care utilization vs different cancer susceptibilities. J Natl Cancer Inst. 2010 Apr 21;102(8):538-46.
27. White A et al. Racial disparities and treatment trends in a large cohort of elderly African Americans and Caucasians with colorectal cancer, 1991 to 2002. Cancer. 2008 Dec 15;113(12):3400-9.
28. Doubeni CA et al. Neighborhood socioeconomic status and use of colonoscopy in an insured population – A retrospective cohort study. PLoS One. 2012;7(5):e36392.
29. Tammana VS, Laiyemo AO. Colorectal cancer disparities: Issues, controversies and solutions. World J Gastroenterol. 2014 Jan 28;20(4):869-76.
30. Carethers JM. Screening for colorectal cancer in African Americans: determinants and rationale for an earlier age to commence screening. Dig Dis Sci. 2015 Mar;60(3):711-21.
31. Miranda-Diaz C et al. Barriers for Compliance to Breast, Colorectal, and Cervical Screening Cancer Tests among Hispanic Patients. Int J Environ Res Public Health. 2015 Dec 22;13(1):ijerph13010021.
32. Sewali B et al. Understanding cancer screening service utilization by Somali men in Minnesota. J Immigr Minor Health. 2015 Jun;17(3):773-80.
33. Walsh JM et al. Barriers to colorectal cancer screening in Latino and Vietnamese Americans. Compared with non-Latino white Americans. J Gen Intern Med. 2004 Feb;19(2):156-66.
34. Perez-Stable EJ et al. Self-reported use of cancer screening tests among Latinos and Anglos in a prepaid health plan. Arch Intern Med. 1994 May 23;154(10):1073-81.
35. Shariff-Marco S et al. Racial/ethnic differences in self-reported racism and its association with cancer-related health behaviors. Am J Public Health. 2010 Feb;100(2):364-74.
36. Powe BD et al. Comparing knowledge of colorectal and prostate cancer among African American and Hispanic men. Cancer Nurs. 2009 Sep-Oct;32(5):412-7.
37. Jun J, Oh KM. Asian and Hispanic Americans’ cancer fatalism and colon cancer screening. Am J Health Behav. 2013 Mar;37(2):145-54.
38. Hacker K et al. The impact of Immigration and Customs Enforcement on immigrant health: Perceptions of immigrants in Everett, Massachusetts, USA. Soc Sci Med. 2011 Aug;73(4):586-94.
39. Firger J. Rescinding DACA could spur a public health crisis, from lost services to higher rates of depression, substance abuse. Newsweek.
40. May FP et al. Racial minorities are more likely than whites to report lack of provider recommendation for colon cancer screening. Am J Gastroenterol. 2015 Oct;110(10):1388-94.
41. Levy BT et al. Why hasn’t this patient been screened for colon cancer? An Iowa Research Network study. J Am Board Fam Med. 2007 Sep-Oct;20(5):458-68.
42. Rosenblatt RA. A view from the periphery – health care in rural America. N Engl J Med. 2004 Sep 9;351(11):1049-51.
43. Young WF et al. Predictors of colorectal screening in rural Colorado: testing to prevent colon cancer in the high plains research network. J Rural Health. 2007 Summer;23(3):238-45.
44. Kates J et al. Health and Access to Care and Coverage for Lesbian, Gay, Bisexual, and Transgender (LGBT) Individuals in the U.S. In: Foundation KF, ed. Disparities Policy Issue Brief. Volume 2017; Aug 30, 2017.
45. Katz ML et al. Improving colorectal cancer screening by using community volunteers: results of the Carolinas cancer education and screening (CARES) project. Cancer. 2007 Oct 1;110(7):1602-10.
46. Jean-Jacques M et al. Program to improve colorectal cancer screening in a low-income, racially diverse population: A randomized controlled trial. Ann Fam Med. 2012 Sep-Oct;10(5):412-7.
47. Reuland DS et al. Effect of combined patient decision aid and patient navigation vs usual care for colorectal cancer screening in a vulnerable patient population: A randomized clinical trial. JAMA Intern Med. 2017 Jul 1;177(7):967-74.
48. Percac-Lima S et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med. 2009 Feb;24(2):211-7.
49. Nash D et al. Evaluation of an intervention to increase screening colonoscopy in an urban public hospital setting. J Urban Health. 2006 Mar;83(2):231-43.
50. Lebwohl B et al. Effect of a patient navigator program on the volume and quality of colonoscopy. J Clin Gastroenterol. 2011 May-Jun;45(5):e47-53.
51. Khankari K et al. Improving colorectal cancer screening among the medically underserved: A pilot study within a federally qualified health center. J Gen Intern Med. 2007 Oct;22(10):1410-4.
52. Wang JH et al. Recruiting Chinese Americans into cancer screening intervention trials: Strategies and outcomes. Clin Trials. 2014 Apr;11(2):167-77.
53. Katz ML et al. Patient activation increases colorectal cancer screening rates: a randomized trial among low-income minority patients. Cancer Epidemiol Biomarkers Prev. 2012 Jan;21(1):45-52.
54. Ford ME et al. Enhancing adherence among older African American men enrolled in a longitudinal cancer screening trial. Gerontologist. 2006 Aug;46(4):545-50.
55. Christie J et al. A randomized controlled trial using patient navigation to increase colonoscopy screening among low-income minorities. J Natl Med Assoc. 2008 Mar;100(3):278-84.
56. Philip EJ et al. Evaluating the impact of an educational intervention to increase CRC screening rates in the African American community: A preliminary study. Cancer Causes Control. 2010 Oct;21(10):1685-91.
57. Greiner KA et al. Implementation intentions and colorectal screening: A randomized trial in safety-net clinics. Am J Prev Med. 2014 Dec;47(6):703-14.
58. Horne HN et al. Effect of patient navigation on colorectal cancer screening in a community-based randomized controlled trial of urban African American adults. Cancer Causes Control. 2015 Feb;26(2):239-46.
59. Grubbs SS et al. Eliminating racial disparities in colorectal cancer in the real world: It took a village. J Clin Oncol. 2013 Jun 1;31(16):1928-30.
60. Jung MY et al. The Chinese and Korean American immigrant experience: a mixed-methods examination of facilitators and barriers of colorectal cancer screening. Ethn Health. 2017 Feb 25:1-20.
61. Viruell-Fuentes EA et al. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012 Dec;75(12):2099-106.
Dr. Oduyebo is a third-year fellow at the Mayo Clinic, Rochester, Minn.; Dr. Malespin is an assistant professor in the department of medicine and the medical director of hepatology at the University of Florida Health, Jacksonville; Dr. Mendoza Ladd is an assistant professor of medicine at Texas Tech University, El Paso; Dr. Day is an associate professor of medicine at the University of California, San Francisco; Dr. Charabaty is an associate professor of medicine and the director of the IBD Center in the division of gastroenterology at Medstar-Georgetown University Center, Washington; Dr. Chen is an associate professor of medicine, the director of patient safety and quality, and the director of the small-bowel endoscopy program in division of gastroenterology at Washington University, St. Louis; Dr. Carr is an assistant professor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia; Dr. Quezada is an assistant dean for admissions, an assistant dean for academic and multicultural affairs, and an assistant professor of medicine in the division of gastroenterology and hepatology at the University of Maryland, Baltimore; and Dr. Lamousé-Smith is a director of translational medicine, immunology, and early development at Janssen Pharmaceuticals Research and Development, Spring House, Penn.
Editor's Note:
Importantly, these barriers often vary between specific population subsets. In this month’s In Focus article, brought to you by The New Gastroenterologist, the members of the AGA Institute Diversity Committee provide an enlightening overview of the barriers affecting underserved populations as well as strategies that can be employed to overcome these impediments. Better understanding of patient-specific barriers will, I hope, allow us to more effectively redress them and ultimately increase colorectal cancer screening rates in all populations.
Bryson W. Katona, MD, PhD
Editor in Chief, The New Gastroenterologist
Despite the positive public health effects of colorectal cancer (CRC) screening, there remains differential uptake of CRC screening in the United States. Minority populations born in the United States and immigrant populations are among those with the lowest rates of CRC screening, and both socioeconomic status and ethnicity are strongly associated with stage of CRC at diagnosis.1,2 Thus, recognizing the economic, social, and cultural factors that result in low rates of CRC screening in underserved populations is important in order to devise targeted interventions to increase CRC uptake and reduce morbidity and mortality in these populations.

What are the facts and figures?
The overall rate of screening colonoscopies has increased in all ethnic groups in the past 10 years but still falls below the goal of 71% established by the Healthy People project (www.healthypeople.gov) for the year 2020.3 According to the Centers for Disease Control and Prevention ethnicity-specific data for U.S.-born populations, 60% of whites, 55% of African Americans (AA), 50% of American Indian/Alaskan natives (AI/AN), 46% of Latino Americans, and 47% of Asians undergo CRC screening (Figure 1A).4 While CRC incidence in non-Hispanic whites age 50 years and older has dropped by 32% since 2000 because of screening, this trend has not been observed in AAs.5,6
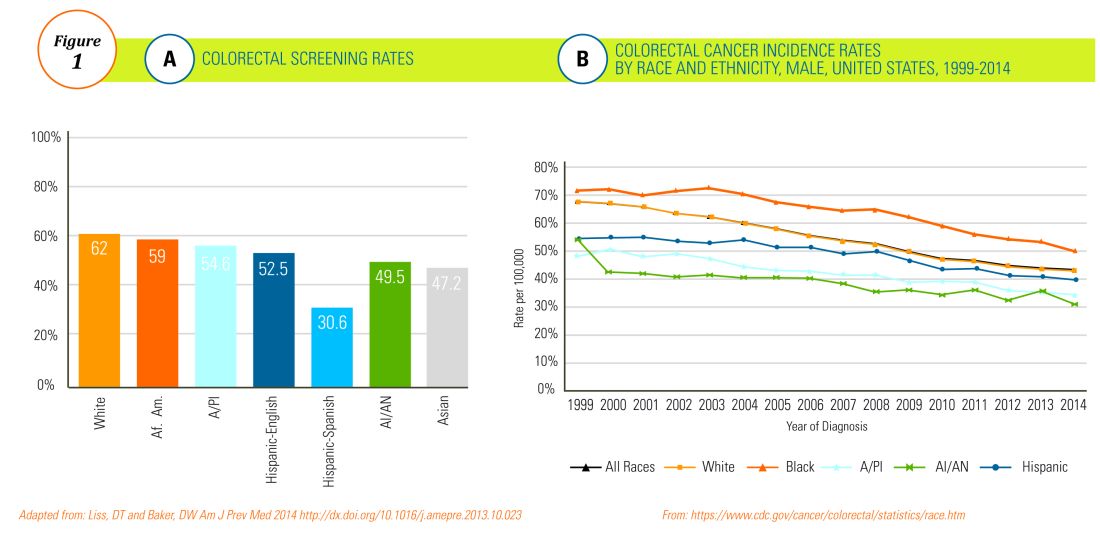
The incidence of CRC in AAs is estimated at 49/10,000, one of the highest amongst U.S. populations and is the second and third most common cancer in AA women and men, respectively (Figure 1B).
Similar to AAs, AI/AN patients present with more advanced CRC disease and at younger ages and have lower survival rates, compared with other racial groups, a trend that has not changed in the last decade.7 CRC screening data in this population vary according to sex, geographic location, and health care utilization, with as few as 4.0% of asymptomatic, average-risk AI/ANs who receive medical care in the Indian Health Services being screened for CRC.8
The low rate of CRC screening among Latinos also poses a significant obstacle to the Healthy People project since it is expected that by 2060 Latinos will constitute 30% of the U.S. population. Therefore, strategies to improve CRC screening in this population are needed to continue the gains made in overall CRC mortality rates.
The percentage of immigrants in the U.S. population increased from 4.7% in 1970 to 13.5% in 2015. Immigrants, regardless of their ethnicity, represent a very vulnerable population, and CRC screening data in this population are not as robust as for U.S.-born groups. In general, immigrants have substantially lower CRC screening rates, compared with U.S.-born populations (21% vs. 60%),9 and it is suspected that additional, significant barriers to CRC screening and care exist for undocumented immigrants.
Another often overlooked group, are individuals with physical or cognitive disabilities. In this group, screening rates range from 49% to 65%.10
Finally, while information is available for many health care conditions and disparities faced by various ethnic groups, there are few CRC screening data for the LGBTQ community. Perhaps amplifying this problem is the existence of conflicting data in this population, with some studies suggesting there is no difference in CRC risk across groups in the LGBTQ community and others suggesting an increased risk.11,12 Notably, sexual orientation has been identified as a positive predictor of CRC screening in gay and bisexual men – CRC screening rates are higher in these groups, compared with heterosexual men.13 In contrast, no such difference has been found between homosexual and heterosexual women.14
What are the barriers?
Several common themes contribute to disparities in CRC screening among minority groups, including psychosocial/cultural, socioeconomic, provider-specific, and insurance-related factors. Some patient-related barriers include issues of illiteracy, having poor health literacy or English proficiency, having only grade school education,15,16 cultural misconceptions, transportation issues, difficulties affording copayments or deductibles, and a lack of follow-up for scheduled appointments and exams.17-20 Poor health literacy has a profound effect on exam perceptions, fear of test results, and compliance with scheduling tests and bowel preparation instructions21-25; it also affects one’s understanding of the importance of CRC screening, the recommended screening age, and the available choice of screening tests.
Even when some apparent barriers are mitigated, disparities in CRC screening remain. For example, even among the insured and among Medicare beneficiaries, screening rates and adequate follow-up rates after abnormal findings remain lower among AAs and those of low socioeconomic status than they are among whites.26-28 At least part of this paradox results from the presence of unmeasured cultural/belief systems that affect CRC screening uptake. Some of these factors include fear and/or denial of CRC diagnoses, mistrust of the health care system, and reluctance to undergo medical treatment and surgery.16,29 AAs are also less likely to be aware of a family history of CRC and to discuss personal and/or family history of CRC or polyps, which can thereby hinder the identification of high-risk individuals who would benefit from early screening.15,30
The deeply rooted sense of fatalism also plays a crucial role and has been cited for many minority and immigrant populations. Fatalism leads patients to view a diagnosis of cancer as a matter of “fate” or “God’s will,” and therefore, it is to be endured.23,31 Similarly, in a qualitative study of 44 Somali men living in St. Paul and Minneapolis, believing cancer was more common in whites, believing they were protected from cancer by God, fearing a cancer diagnosis, and fearing ostracism from their community were reported as barriers to cancer screening.32
Perceptions about CRC screening methods in Latino populations also have a tremendous influence and can include fear, stigma of sexual prejudice, embarrassment of being exposed during the exam, worries about humiliation in a male sense of masculinity, a lack of trust in the medical professionals, a sense of being a “guinea pig” for physicians, concerns about health care racism, and expectations of pain.33-37 Studies have reported that immigrants are afraid to seek health care because of the increasingly hostile environment associated with immigration enforcement.38 In addition, the impending dissolution of the Deferred Action for Childhood Arrivals act is likely to augment the barriers to care for Latino groups.39
In addition, provider-specific barriers to care also exist. Racial and ethnic minorities are less likely than whites to receive recommendations for screening by their physician. In fact, this factor alone has been demonstrated to be the main reason for lack of screening among AAs in a Californian cohort.40 In addition, patients from rural areas or those from AI/AN communities are at especially increased risk for lack of access to care because of a scarcity of providers along with patient perceptions regarding their primary care provider’s ability to connect them to subspecialists.41-43 Other cited examples include misconceptions about and poor treatment of the LGBTQ population by health care providers/systems.44
How can we intervene successfully?
Characterization of barriers is important because it promotes the development of targeted interventions. Intervention models include community engagement programs, incorporation of fecal occult testing, and patient navigator programs.45-47 In response to the alarming disparity in CRC screening rates in Latino communities, several interventions have been set in motion in different clinical scenarios, which include patient navigation and a focus on patient education.
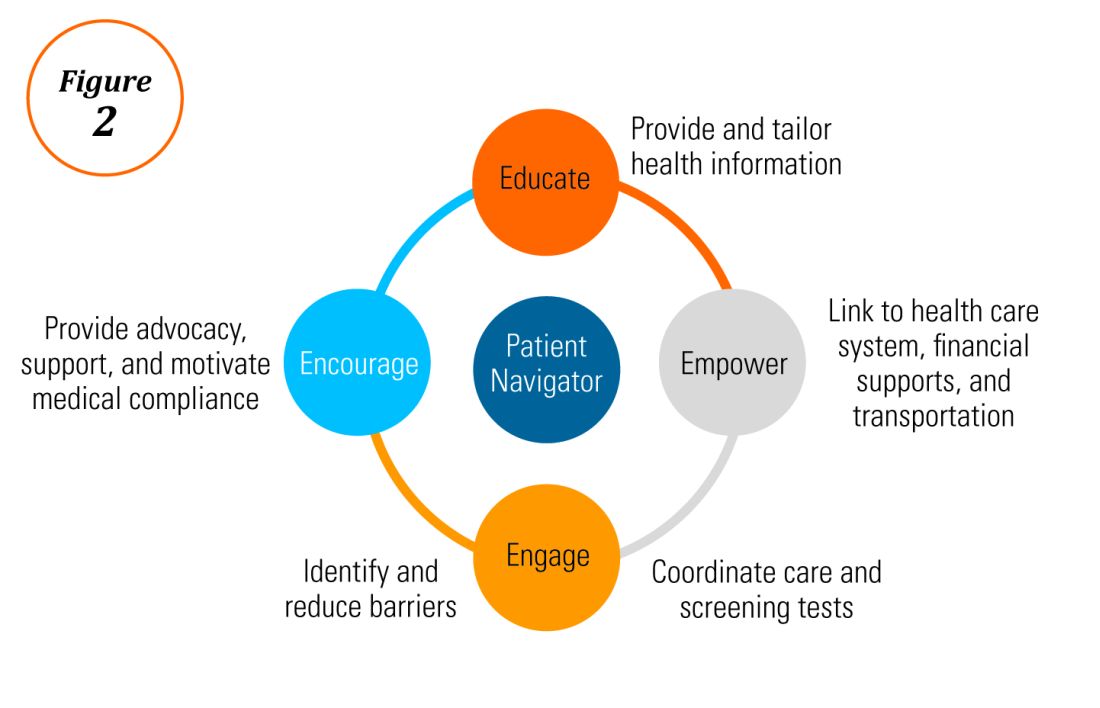
Randomized trials have shown that outreach efforts and patient navigation increase CRC screening rates in AAs.48,54,55 Studies evaluating the effects of print-based educational materials on improving screening showed improvement in screening rates, decreases in cancer-related fatalistic attitudes, and patients had a better understanding of the benefits of screening as compared with the cost associated with screening and the cost of advanced disease.56 Similarly, the use of touch-screen computers that tailor informational messages to decisional stage and screening barriers increased participation in CRC screening.57 Including patient navigators along with printed education material was even more effective at increasing the proportion of patients getting colonoscopy screening than providing printed material alone, with more-intensive navigation needed for individuals with low literacy.58 Grubbs et al.reported the success of their patient navigation program, which included wider comprehensive screening and coverage for colonoscopy screening.59 In AAs, they estimated an annual reduction of CRC incidence and mortality of 4,200 and 2,700 patients, respectively.
Among immigrants, there is an increased likelihood of CRC screening in those immigrants with a higher number of primary care visits.60 The intersection of culture, race, socioeconomic status, housing enclaves, limited English proficiency, low health literacy, and immigration policy all play a role in immigrant health and access to health care.61
Therefore, different strategies may be needed for each immigrant group to improve CRC screening. For this group of patients, efforts aimed at mitigating the adverse effects of national immigration policies on immigrant populations may have the additional consequence of improving health care access and CRC screening for these patients.
Data gaps still exist in our understanding of patient perceptions, perspectives, and barriers that present opportunities for further study to develop long-lasting interventions that will improve health care of underserved populations. By raising awareness of the barriers, physicians can enhance their own self-awareness to keenly be attuned to these challenges as patients cross their clinic threshold for medical care.
Additional resources link: www.cdc.gov/cancer/colorectal/
References
1. Klabunde CN et al. Trends in colorectal cancer test use among vulnerable populations in the United States. Cancer Epidemiol Biomarkers Prev. 2011 Aug;20(8):1611-21.
2. Parikh-Patel A et al. Colorectal cancer stage at diagnosis by socioeconomic and urban/rural status in California, 1988-2000. Cancer. 2006 Sep;107(5 Suppl):1189-95.
3. Promotion OoDPaH. Healthy People 2020. Cancer. Volume 2017.
4. Centers for Disease Control and Prevention. Cancer screening – United States, 2010. MMWR Morb Mortal Wkly Rep. 2012 Jan 27;61(3):41-5.
5. Doubeni CA et al. Racial and ethnic trends of colorectal cancer screening among Medicare enrollees. Am J Prev Med. 2010 Feb;38(2):184-91.
6. Kupfer SS et al. Reducing colorectal cancer risk among African Americans. Gastroenterology. 2015 Nov;149(6):1302-4.
7. Espey DK et al. Annual report to the nation on the status of cancer, 1975-2004, featuring cancer in American Indians and Alaska Natives. Cancer. 2007 Nov;110(10):2119-52.
8. Day LW et al. Screening prevalence and incidence of colorectal cancer among American Indian/Alaskan natives in the Indian Health Service. Dig Dis Sci. 2011 Jul;56(7):2104-13.
9. Gupta S et al. Challenges and possible solutions to colorectal cancer screening for the underserved. J Natl Cancer Inst. 2014 Apr;106(4):dju032.
10. Steele CB et al. Colorectal cancer incidence and screening – United States, 2008 and 2010. MMWR Suppl. 2013 Nov 22;62(3):53-60.
11. Boehmer U et al. Cancer survivorship and sexual orientation. Cancer 2011 Aug 15;117(16):3796-804.
12. Austin SB, Pazaris MJ, Wei EK, et al. Application of the Rosner-Wei risk-prediction model to estimate sexual orientation patterns in colon cancer risk in a prospective cohort of US women. Cancer Causes Control. 2014 Aug;25(8):999-1006.
13. Heslin KC et al. Sexual orientation and testing for prostate and colorectal cancers among men in California. Med Care. 2008 Dec;46(12):1240-8.
14. McElroy JA et al. Advancing Health Care for Lesbian, Gay, Bisexual, and Transgender Patients in Missouri. Mo Med. 2015 Jul-Aug;112(4):262-5.
15. Greiner KA et al. Knowledge and perceptions of colorectal cancer screening among urban African Americans. J Gen Intern Med. 2005 Nov;20(11):977-83.
16. Green PM, Kelly BA. Colorectal cancer knowledge, perceptions, and behaviors in African Americans. Cancer Nurs. 2004 May-Jun;27(3):206-15; quiz 216-7.
17. Berkowitz Z et al. Beliefs, risk perceptions, and gaps in knowledge as barriers to colorectal cancer screening in older adults. J Am Geriatr Soc. 2008 Feb;56(2):307-14.
18. Dolan NC et al. Colorectal cancer screening knowledge, attitudes, and beliefs among veterans: Does literacy make a difference? J Clin Oncol. 2004 Jul;22(13):2617-22.
19. Peterson NB et al. The influence of health literacy on colorectal cancer screening knowledge, beliefs and behavior. J Natl Med Assoc. 2007 Oct;99(10):1105-12.
20. Haddock MG et al. Intraoperative irradiation for locally recurrent colorectal cancer in previously irradiated patients. Int J Radiat Oncol Biol Phys. 2001 Apr 1;49(5):1267-74.
21. Jones RM et al. Patient-reported barriers to colorectal cancer screening: a mixed-methods analysis. Am J Prev Med. 2010 May;38(5):508-16.
22. Basch CH et al. Screening colonoscopy bowel preparation: experience in an urban minority population. Therap Adv Gastroenterol. 2013 Nov;6(6):442-6.
23. Davis JL et al. Sociodemographic differences in fears and mistrust contributing to unwillingness to participate in cancer screenings. J Health Care Poor Underserved. 2012 Nov;23(4 Suppl):67-76.
24. Robinson CM et al. Barriers to colorectal cancer screening among publicly insured urban women: no knowledge of tests and no clinician recommendation. J Natl Med Assoc. 2011 Aug;103(8):746-53.
25. Goldman RE et al. Perspectives of colorectal cancer risk and screening among Dominicans and Puerto Ricans: Stigma and misperceptions. Qual Health Res. 2009 Nov;19(11):1559-68.
26. Laiyemo AO et al. Race and colorectal cancer disparities: Health-care utilization vs different cancer susceptibilities. J Natl Cancer Inst. 2010 Apr 21;102(8):538-46.
27. White A et al. Racial disparities and treatment trends in a large cohort of elderly African Americans and Caucasians with colorectal cancer, 1991 to 2002. Cancer. 2008 Dec 15;113(12):3400-9.
28. Doubeni CA et al. Neighborhood socioeconomic status and use of colonoscopy in an insured population – A retrospective cohort study. PLoS One. 2012;7(5):e36392.
29. Tammana VS, Laiyemo AO. Colorectal cancer disparities: Issues, controversies and solutions. World J Gastroenterol. 2014 Jan 28;20(4):869-76.
30. Carethers JM. Screening for colorectal cancer in African Americans: determinants and rationale for an earlier age to commence screening. Dig Dis Sci. 2015 Mar;60(3):711-21.
31. Miranda-Diaz C et al. Barriers for Compliance to Breast, Colorectal, and Cervical Screening Cancer Tests among Hispanic Patients. Int J Environ Res Public Health. 2015 Dec 22;13(1):ijerph13010021.
32. Sewali B et al. Understanding cancer screening service utilization by Somali men in Minnesota. J Immigr Minor Health. 2015 Jun;17(3):773-80.
33. Walsh JM et al. Barriers to colorectal cancer screening in Latino and Vietnamese Americans. Compared with non-Latino white Americans. J Gen Intern Med. 2004 Feb;19(2):156-66.
34. Perez-Stable EJ et al. Self-reported use of cancer screening tests among Latinos and Anglos in a prepaid health plan. Arch Intern Med. 1994 May 23;154(10):1073-81.
35. Shariff-Marco S et al. Racial/ethnic differences in self-reported racism and its association with cancer-related health behaviors. Am J Public Health. 2010 Feb;100(2):364-74.
36. Powe BD et al. Comparing knowledge of colorectal and prostate cancer among African American and Hispanic men. Cancer Nurs. 2009 Sep-Oct;32(5):412-7.
37. Jun J, Oh KM. Asian and Hispanic Americans’ cancer fatalism and colon cancer screening. Am J Health Behav. 2013 Mar;37(2):145-54.
38. Hacker K et al. The impact of Immigration and Customs Enforcement on immigrant health: Perceptions of immigrants in Everett, Massachusetts, USA. Soc Sci Med. 2011 Aug;73(4):586-94.
39. Firger J. Rescinding DACA could spur a public health crisis, from lost services to higher rates of depression, substance abuse. Newsweek.
40. May FP et al. Racial minorities are more likely than whites to report lack of provider recommendation for colon cancer screening. Am J Gastroenterol. 2015 Oct;110(10):1388-94.
41. Levy BT et al. Why hasn’t this patient been screened for colon cancer? An Iowa Research Network study. J Am Board Fam Med. 2007 Sep-Oct;20(5):458-68.
42. Rosenblatt RA. A view from the periphery – health care in rural America. N Engl J Med. 2004 Sep 9;351(11):1049-51.
43. Young WF et al. Predictors of colorectal screening in rural Colorado: testing to prevent colon cancer in the high plains research network. J Rural Health. 2007 Summer;23(3):238-45.
44. Kates J et al. Health and Access to Care and Coverage for Lesbian, Gay, Bisexual, and Transgender (LGBT) Individuals in the U.S. In: Foundation KF, ed. Disparities Policy Issue Brief. Volume 2017; Aug 30, 2017.
45. Katz ML et al. Improving colorectal cancer screening by using community volunteers: results of the Carolinas cancer education and screening (CARES) project. Cancer. 2007 Oct 1;110(7):1602-10.
46. Jean-Jacques M et al. Program to improve colorectal cancer screening in a low-income, racially diverse population: A randomized controlled trial. Ann Fam Med. 2012 Sep-Oct;10(5):412-7.
47. Reuland DS et al. Effect of combined patient decision aid and patient navigation vs usual care for colorectal cancer screening in a vulnerable patient population: A randomized clinical trial. JAMA Intern Med. 2017 Jul 1;177(7):967-74.
48. Percac-Lima S et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med. 2009 Feb;24(2):211-7.
49. Nash D et al. Evaluation of an intervention to increase screening colonoscopy in an urban public hospital setting. J Urban Health. 2006 Mar;83(2):231-43.
50. Lebwohl B et al. Effect of a patient navigator program on the volume and quality of colonoscopy. J Clin Gastroenterol. 2011 May-Jun;45(5):e47-53.
51. Khankari K et al. Improving colorectal cancer screening among the medically underserved: A pilot study within a federally qualified health center. J Gen Intern Med. 2007 Oct;22(10):1410-4.
52. Wang JH et al. Recruiting Chinese Americans into cancer screening intervention trials: Strategies and outcomes. Clin Trials. 2014 Apr;11(2):167-77.
53. Katz ML et al. Patient activation increases colorectal cancer screening rates: a randomized trial among low-income minority patients. Cancer Epidemiol Biomarkers Prev. 2012 Jan;21(1):45-52.
54. Ford ME et al. Enhancing adherence among older African American men enrolled in a longitudinal cancer screening trial. Gerontologist. 2006 Aug;46(4):545-50.
55. Christie J et al. A randomized controlled trial using patient navigation to increase colonoscopy screening among low-income minorities. J Natl Med Assoc. 2008 Mar;100(3):278-84.
56. Philip EJ et al. Evaluating the impact of an educational intervention to increase CRC screening rates in the African American community: A preliminary study. Cancer Causes Control. 2010 Oct;21(10):1685-91.
57. Greiner KA et al. Implementation intentions and colorectal screening: A randomized trial in safety-net clinics. Am J Prev Med. 2014 Dec;47(6):703-14.
58. Horne HN et al. Effect of patient navigation on colorectal cancer screening in a community-based randomized controlled trial of urban African American adults. Cancer Causes Control. 2015 Feb;26(2):239-46.
59. Grubbs SS et al. Eliminating racial disparities in colorectal cancer in the real world: It took a village. J Clin Oncol. 2013 Jun 1;31(16):1928-30.
60. Jung MY et al. The Chinese and Korean American immigrant experience: a mixed-methods examination of facilitators and barriers of colorectal cancer screening. Ethn Health. 2017 Feb 25:1-20.
61. Viruell-Fuentes EA et al. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012 Dec;75(12):2099-106.
Dr. Oduyebo is a third-year fellow at the Mayo Clinic, Rochester, Minn.; Dr. Malespin is an assistant professor in the department of medicine and the medical director of hepatology at the University of Florida Health, Jacksonville; Dr. Mendoza Ladd is an assistant professor of medicine at Texas Tech University, El Paso; Dr. Day is an associate professor of medicine at the University of California, San Francisco; Dr. Charabaty is an associate professor of medicine and the director of the IBD Center in the division of gastroenterology at Medstar-Georgetown University Center, Washington; Dr. Chen is an associate professor of medicine, the director of patient safety and quality, and the director of the small-bowel endoscopy program in division of gastroenterology at Washington University, St. Louis; Dr. Carr is an assistant professor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia; Dr. Quezada is an assistant dean for admissions, an assistant dean for academic and multicultural affairs, and an assistant professor of medicine in the division of gastroenterology and hepatology at the University of Maryland, Baltimore; and Dr. Lamousé-Smith is a director of translational medicine, immunology, and early development at Janssen Pharmaceuticals Research and Development, Spring House, Penn.
Editor's Note:
Importantly, these barriers often vary between specific population subsets. In this month’s In Focus article, brought to you by The New Gastroenterologist, the members of the AGA Institute Diversity Committee provide an enlightening overview of the barriers affecting underserved populations as well as strategies that can be employed to overcome these impediments. Better understanding of patient-specific barriers will, I hope, allow us to more effectively redress them and ultimately increase colorectal cancer screening rates in all populations.
Bryson W. Katona, MD, PhD
Editor in Chief, The New Gastroenterologist
Despite the positive public health effects of colorectal cancer (CRC) screening, there remains differential uptake of CRC screening in the United States. Minority populations born in the United States and immigrant populations are among those with the lowest rates of CRC screening, and both socioeconomic status and ethnicity are strongly associated with stage of CRC at diagnosis.1,2 Thus, recognizing the economic, social, and cultural factors that result in low rates of CRC screening in underserved populations is important in order to devise targeted interventions to increase CRC uptake and reduce morbidity and mortality in these populations.

What are the facts and figures?
The overall rate of screening colonoscopies has increased in all ethnic groups in the past 10 years but still falls below the goal of 71% established by the Healthy People project (www.healthypeople.gov) for the year 2020.3 According to the Centers for Disease Control and Prevention ethnicity-specific data for U.S.-born populations, 60% of whites, 55% of African Americans (AA), 50% of American Indian/Alaskan natives (AI/AN), 46% of Latino Americans, and 47% of Asians undergo CRC screening (Figure 1A).4 While CRC incidence in non-Hispanic whites age 50 years and older has dropped by 32% since 2000 because of screening, this trend has not been observed in AAs.5,6
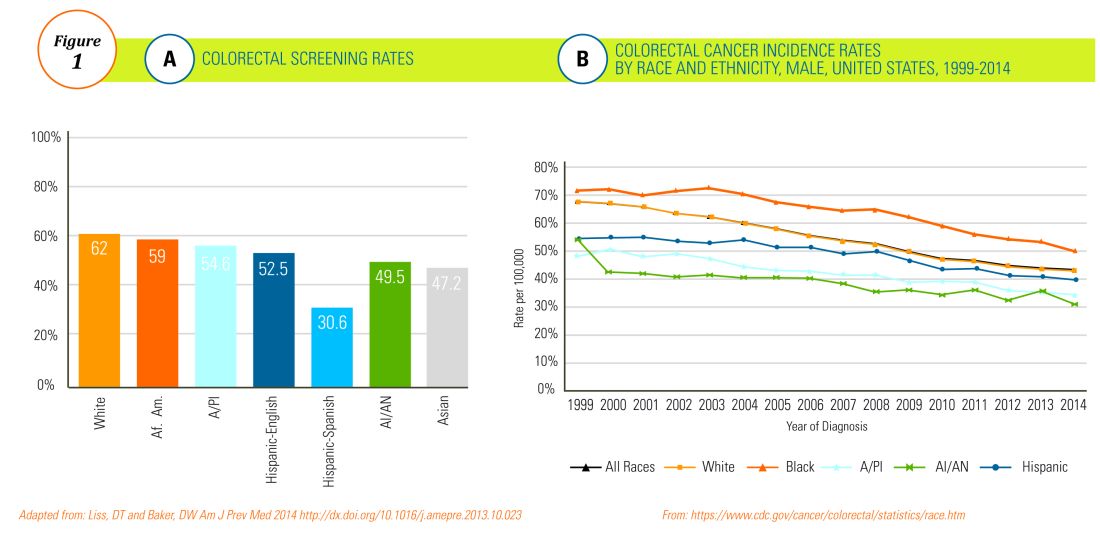
The incidence of CRC in AAs is estimated at 49/10,000, one of the highest amongst U.S. populations and is the second and third most common cancer in AA women and men, respectively (Figure 1B).
Similar to AAs, AI/AN patients present with more advanced CRC disease and at younger ages and have lower survival rates, compared with other racial groups, a trend that has not changed in the last decade.7 CRC screening data in this population vary according to sex, geographic location, and health care utilization, with as few as 4.0% of asymptomatic, average-risk AI/ANs who receive medical care in the Indian Health Services being screened for CRC.8
The low rate of CRC screening among Latinos also poses a significant obstacle to the Healthy People project since it is expected that by 2060 Latinos will constitute 30% of the U.S. population. Therefore, strategies to improve CRC screening in this population are needed to continue the gains made in overall CRC mortality rates.
The percentage of immigrants in the U.S. population increased from 4.7% in 1970 to 13.5% in 2015. Immigrants, regardless of their ethnicity, represent a very vulnerable population, and CRC screening data in this population are not as robust as for U.S.-born groups. In general, immigrants have substantially lower CRC screening rates, compared with U.S.-born populations (21% vs. 60%),9 and it is suspected that additional, significant barriers to CRC screening and care exist for undocumented immigrants.
Another often overlooked group, are individuals with physical or cognitive disabilities. In this group, screening rates range from 49% to 65%.10
Finally, while information is available for many health care conditions and disparities faced by various ethnic groups, there are few CRC screening data for the LGBTQ community. Perhaps amplifying this problem is the existence of conflicting data in this population, with some studies suggesting there is no difference in CRC risk across groups in the LGBTQ community and others suggesting an increased risk.11,12 Notably, sexual orientation has been identified as a positive predictor of CRC screening in gay and bisexual men – CRC screening rates are higher in these groups, compared with heterosexual men.13 In contrast, no such difference has been found between homosexual and heterosexual women.14
What are the barriers?
Several common themes contribute to disparities in CRC screening among minority groups, including psychosocial/cultural, socioeconomic, provider-specific, and insurance-related factors. Some patient-related barriers include issues of illiteracy, having poor health literacy or English proficiency, having only grade school education,15,16 cultural misconceptions, transportation issues, difficulties affording copayments or deductibles, and a lack of follow-up for scheduled appointments and exams.17-20 Poor health literacy has a profound effect on exam perceptions, fear of test results, and compliance with scheduling tests and bowel preparation instructions21-25; it also affects one’s understanding of the importance of CRC screening, the recommended screening age, and the available choice of screening tests.
Even when some apparent barriers are mitigated, disparities in CRC screening remain. For example, even among the insured and among Medicare beneficiaries, screening rates and adequate follow-up rates after abnormal findings remain lower among AAs and those of low socioeconomic status than they are among whites.26-28 At least part of this paradox results from the presence of unmeasured cultural/belief systems that affect CRC screening uptake. Some of these factors include fear and/or denial of CRC diagnoses, mistrust of the health care system, and reluctance to undergo medical treatment and surgery.16,29 AAs are also less likely to be aware of a family history of CRC and to discuss personal and/or family history of CRC or polyps, which can thereby hinder the identification of high-risk individuals who would benefit from early screening.15,30
The deeply rooted sense of fatalism also plays a crucial role and has been cited for many minority and immigrant populations. Fatalism leads patients to view a diagnosis of cancer as a matter of “fate” or “God’s will,” and therefore, it is to be endured.23,31 Similarly, in a qualitative study of 44 Somali men living in St. Paul and Minneapolis, believing cancer was more common in whites, believing they were protected from cancer by God, fearing a cancer diagnosis, and fearing ostracism from their community were reported as barriers to cancer screening.32
Perceptions about CRC screening methods in Latino populations also have a tremendous influence and can include fear, stigma of sexual prejudice, embarrassment of being exposed during the exam, worries about humiliation in a male sense of masculinity, a lack of trust in the medical professionals, a sense of being a “guinea pig” for physicians, concerns about health care racism, and expectations of pain.33-37 Studies have reported that immigrants are afraid to seek health care because of the increasingly hostile environment associated with immigration enforcement.38 In addition, the impending dissolution of the Deferred Action for Childhood Arrivals act is likely to augment the barriers to care for Latino groups.39
In addition, provider-specific barriers to care also exist. Racial and ethnic minorities are less likely than whites to receive recommendations for screening by their physician. In fact, this factor alone has been demonstrated to be the main reason for lack of screening among AAs in a Californian cohort.40 In addition, patients from rural areas or those from AI/AN communities are at especially increased risk for lack of access to care because of a scarcity of providers along with patient perceptions regarding their primary care provider’s ability to connect them to subspecialists.41-43 Other cited examples include misconceptions about and poor treatment of the LGBTQ population by health care providers/systems.44
How can we intervene successfully?
Characterization of barriers is important because it promotes the development of targeted interventions. Intervention models include community engagement programs, incorporation of fecal occult testing, and patient navigator programs.45-47 In response to the alarming disparity in CRC screening rates in Latino communities, several interventions have been set in motion in different clinical scenarios, which include patient navigation and a focus on patient education.
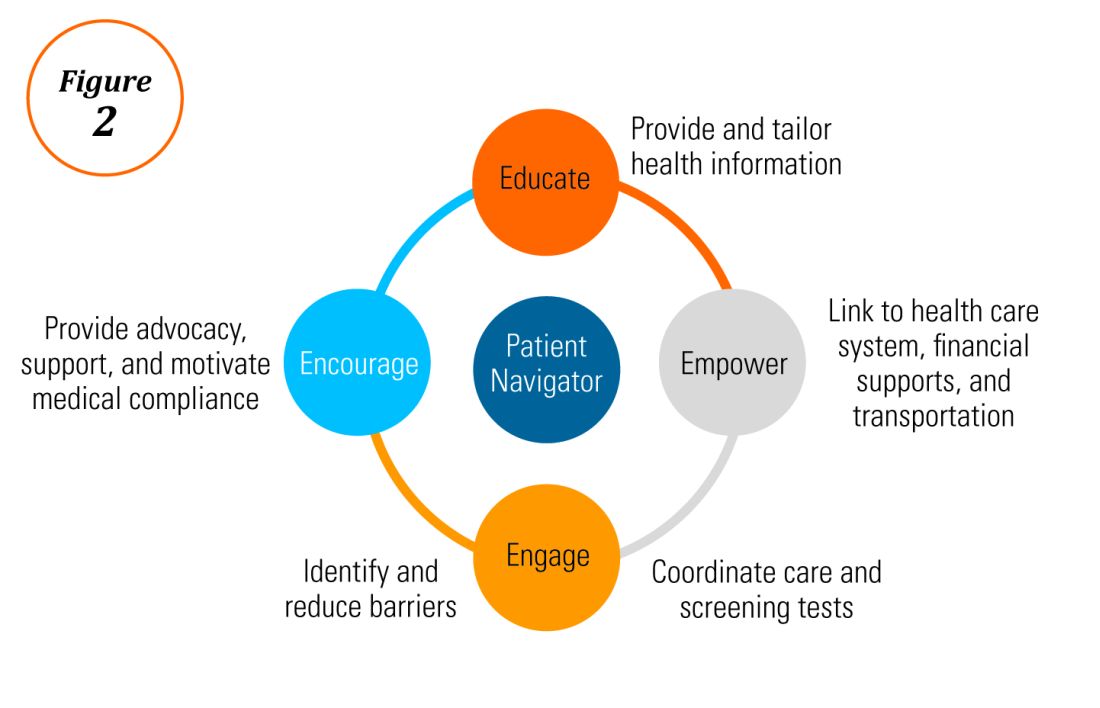
Randomized trials have shown that outreach efforts and patient navigation increase CRC screening rates in AAs.48,54,55 Studies evaluating the effects of print-based educational materials on improving screening showed improvement in screening rates, decreases in cancer-related fatalistic attitudes, and patients had a better understanding of the benefits of screening as compared with the cost associated with screening and the cost of advanced disease.56 Similarly, the use of touch-screen computers that tailor informational messages to decisional stage and screening barriers increased participation in CRC screening.57 Including patient navigators along with printed education material was even more effective at increasing the proportion of patients getting colonoscopy screening than providing printed material alone, with more-intensive navigation needed for individuals with low literacy.58 Grubbs et al.reported the success of their patient navigation program, which included wider comprehensive screening and coverage for colonoscopy screening.59 In AAs, they estimated an annual reduction of CRC incidence and mortality of 4,200 and 2,700 patients, respectively.
Among immigrants, there is an increased likelihood of CRC screening in those immigrants with a higher number of primary care visits.60 The intersection of culture, race, socioeconomic status, housing enclaves, limited English proficiency, low health literacy, and immigration policy all play a role in immigrant health and access to health care.61
Therefore, different strategies may be needed for each immigrant group to improve CRC screening. For this group of patients, efforts aimed at mitigating the adverse effects of national immigration policies on immigrant populations may have the additional consequence of improving health care access and CRC screening for these patients.
Data gaps still exist in our understanding of patient perceptions, perspectives, and barriers that present opportunities for further study to develop long-lasting interventions that will improve health care of underserved populations. By raising awareness of the barriers, physicians can enhance their own self-awareness to keenly be attuned to these challenges as patients cross their clinic threshold for medical care.
Additional resources link: www.cdc.gov/cancer/colorectal/
References
1. Klabunde CN et al. Trends in colorectal cancer test use among vulnerable populations in the United States. Cancer Epidemiol Biomarkers Prev. 2011 Aug;20(8):1611-21.
2. Parikh-Patel A et al. Colorectal cancer stage at diagnosis by socioeconomic and urban/rural status in California, 1988-2000. Cancer. 2006 Sep;107(5 Suppl):1189-95.
3. Promotion OoDPaH. Healthy People 2020. Cancer. Volume 2017.
4. Centers for Disease Control and Prevention. Cancer screening – United States, 2010. MMWR Morb Mortal Wkly Rep. 2012 Jan 27;61(3):41-5.
5. Doubeni CA et al. Racial and ethnic trends of colorectal cancer screening among Medicare enrollees. Am J Prev Med. 2010 Feb;38(2):184-91.
6. Kupfer SS et al. Reducing colorectal cancer risk among African Americans. Gastroenterology. 2015 Nov;149(6):1302-4.
7. Espey DK et al. Annual report to the nation on the status of cancer, 1975-2004, featuring cancer in American Indians and Alaska Natives. Cancer. 2007 Nov;110(10):2119-52.
8. Day LW et al. Screening prevalence and incidence of colorectal cancer among American Indian/Alaskan natives in the Indian Health Service. Dig Dis Sci. 2011 Jul;56(7):2104-13.
9. Gupta S et al. Challenges and possible solutions to colorectal cancer screening for the underserved. J Natl Cancer Inst. 2014 Apr;106(4):dju032.
10. Steele CB et al. Colorectal cancer incidence and screening – United States, 2008 and 2010. MMWR Suppl. 2013 Nov 22;62(3):53-60.
11. Boehmer U et al. Cancer survivorship and sexual orientation. Cancer 2011 Aug 15;117(16):3796-804.
12. Austin SB, Pazaris MJ, Wei EK, et al. Application of the Rosner-Wei risk-prediction model to estimate sexual orientation patterns in colon cancer risk in a prospective cohort of US women. Cancer Causes Control. 2014 Aug;25(8):999-1006.
13. Heslin KC et al. Sexual orientation and testing for prostate and colorectal cancers among men in California. Med Care. 2008 Dec;46(12):1240-8.
14. McElroy JA et al. Advancing Health Care for Lesbian, Gay, Bisexual, and Transgender Patients in Missouri. Mo Med. 2015 Jul-Aug;112(4):262-5.
15. Greiner KA et al. Knowledge and perceptions of colorectal cancer screening among urban African Americans. J Gen Intern Med. 2005 Nov;20(11):977-83.
16. Green PM, Kelly BA. Colorectal cancer knowledge, perceptions, and behaviors in African Americans. Cancer Nurs. 2004 May-Jun;27(3):206-15; quiz 216-7.
17. Berkowitz Z et al. Beliefs, risk perceptions, and gaps in knowledge as barriers to colorectal cancer screening in older adults. J Am Geriatr Soc. 2008 Feb;56(2):307-14.
18. Dolan NC et al. Colorectal cancer screening knowledge, attitudes, and beliefs among veterans: Does literacy make a difference? J Clin Oncol. 2004 Jul;22(13):2617-22.
19. Peterson NB et al. The influence of health literacy on colorectal cancer screening knowledge, beliefs and behavior. J Natl Med Assoc. 2007 Oct;99(10):1105-12.
20. Haddock MG et al. Intraoperative irradiation for locally recurrent colorectal cancer in previously irradiated patients. Int J Radiat Oncol Biol Phys. 2001 Apr 1;49(5):1267-74.
21. Jones RM et al. Patient-reported barriers to colorectal cancer screening: a mixed-methods analysis. Am J Prev Med. 2010 May;38(5):508-16.
22. Basch CH et al. Screening colonoscopy bowel preparation: experience in an urban minority population. Therap Adv Gastroenterol. 2013 Nov;6(6):442-6.
23. Davis JL et al. Sociodemographic differences in fears and mistrust contributing to unwillingness to participate in cancer screenings. J Health Care Poor Underserved. 2012 Nov;23(4 Suppl):67-76.
24. Robinson CM et al. Barriers to colorectal cancer screening among publicly insured urban women: no knowledge of tests and no clinician recommendation. J Natl Med Assoc. 2011 Aug;103(8):746-53.
25. Goldman RE et al. Perspectives of colorectal cancer risk and screening among Dominicans and Puerto Ricans: Stigma and misperceptions. Qual Health Res. 2009 Nov;19(11):1559-68.
26. Laiyemo AO et al. Race and colorectal cancer disparities: Health-care utilization vs different cancer susceptibilities. J Natl Cancer Inst. 2010 Apr 21;102(8):538-46.
27. White A et al. Racial disparities and treatment trends in a large cohort of elderly African Americans and Caucasians with colorectal cancer, 1991 to 2002. Cancer. 2008 Dec 15;113(12):3400-9.
28. Doubeni CA et al. Neighborhood socioeconomic status and use of colonoscopy in an insured population – A retrospective cohort study. PLoS One. 2012;7(5):e36392.
29. Tammana VS, Laiyemo AO. Colorectal cancer disparities: Issues, controversies and solutions. World J Gastroenterol. 2014 Jan 28;20(4):869-76.
30. Carethers JM. Screening for colorectal cancer in African Americans: determinants and rationale for an earlier age to commence screening. Dig Dis Sci. 2015 Mar;60(3):711-21.
31. Miranda-Diaz C et al. Barriers for Compliance to Breast, Colorectal, and Cervical Screening Cancer Tests among Hispanic Patients. Int J Environ Res Public Health. 2015 Dec 22;13(1):ijerph13010021.
32. Sewali B et al. Understanding cancer screening service utilization by Somali men in Minnesota. J Immigr Minor Health. 2015 Jun;17(3):773-80.
33. Walsh JM et al. Barriers to colorectal cancer screening in Latino and Vietnamese Americans. Compared with non-Latino white Americans. J Gen Intern Med. 2004 Feb;19(2):156-66.
34. Perez-Stable EJ et al. Self-reported use of cancer screening tests among Latinos and Anglos in a prepaid health plan. Arch Intern Med. 1994 May 23;154(10):1073-81.
35. Shariff-Marco S et al. Racial/ethnic differences in self-reported racism and its association with cancer-related health behaviors. Am J Public Health. 2010 Feb;100(2):364-74.
36. Powe BD et al. Comparing knowledge of colorectal and prostate cancer among African American and Hispanic men. Cancer Nurs. 2009 Sep-Oct;32(5):412-7.
37. Jun J, Oh KM. Asian and Hispanic Americans’ cancer fatalism and colon cancer screening. Am J Health Behav. 2013 Mar;37(2):145-54.
38. Hacker K et al. The impact of Immigration and Customs Enforcement on immigrant health: Perceptions of immigrants in Everett, Massachusetts, USA. Soc Sci Med. 2011 Aug;73(4):586-94.
39. Firger J. Rescinding DACA could spur a public health crisis, from lost services to higher rates of depression, substance abuse. Newsweek.
40. May FP et al. Racial minorities are more likely than whites to report lack of provider recommendation for colon cancer screening. Am J Gastroenterol. 2015 Oct;110(10):1388-94.
41. Levy BT et al. Why hasn’t this patient been screened for colon cancer? An Iowa Research Network study. J Am Board Fam Med. 2007 Sep-Oct;20(5):458-68.
42. Rosenblatt RA. A view from the periphery – health care in rural America. N Engl J Med. 2004 Sep 9;351(11):1049-51.
43. Young WF et al. Predictors of colorectal screening in rural Colorado: testing to prevent colon cancer in the high plains research network. J Rural Health. 2007 Summer;23(3):238-45.
44. Kates J et al. Health and Access to Care and Coverage for Lesbian, Gay, Bisexual, and Transgender (LGBT) Individuals in the U.S. In: Foundation KF, ed. Disparities Policy Issue Brief. Volume 2017; Aug 30, 2017.
45. Katz ML et al. Improving colorectal cancer screening by using community volunteers: results of the Carolinas cancer education and screening (CARES) project. Cancer. 2007 Oct 1;110(7):1602-10.
46. Jean-Jacques M et al. Program to improve colorectal cancer screening in a low-income, racially diverse population: A randomized controlled trial. Ann Fam Med. 2012 Sep-Oct;10(5):412-7.
47. Reuland DS et al. Effect of combined patient decision aid and patient navigation vs usual care for colorectal cancer screening in a vulnerable patient population: A randomized clinical trial. JAMA Intern Med. 2017 Jul 1;177(7):967-74.
48. Percac-Lima S et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med. 2009 Feb;24(2):211-7.
49. Nash D et al. Evaluation of an intervention to increase screening colonoscopy in an urban public hospital setting. J Urban Health. 2006 Mar;83(2):231-43.
50. Lebwohl B et al. Effect of a patient navigator program on the volume and quality of colonoscopy. J Clin Gastroenterol. 2011 May-Jun;45(5):e47-53.
51. Khankari K et al. Improving colorectal cancer screening among the medically underserved: A pilot study within a federally qualified health center. J Gen Intern Med. 2007 Oct;22(10):1410-4.
52. Wang JH et al. Recruiting Chinese Americans into cancer screening intervention trials: Strategies and outcomes. Clin Trials. 2014 Apr;11(2):167-77.
53. Katz ML et al. Patient activation increases colorectal cancer screening rates: a randomized trial among low-income minority patients. Cancer Epidemiol Biomarkers Prev. 2012 Jan;21(1):45-52.
54. Ford ME et al. Enhancing adherence among older African American men enrolled in a longitudinal cancer screening trial. Gerontologist. 2006 Aug;46(4):545-50.
55. Christie J et al. A randomized controlled trial using patient navigation to increase colonoscopy screening among low-income minorities. J Natl Med Assoc. 2008 Mar;100(3):278-84.
56. Philip EJ et al. Evaluating the impact of an educational intervention to increase CRC screening rates in the African American community: A preliminary study. Cancer Causes Control. 2010 Oct;21(10):1685-91.
57. Greiner KA et al. Implementation intentions and colorectal screening: A randomized trial in safety-net clinics. Am J Prev Med. 2014 Dec;47(6):703-14.
58. Horne HN et al. Effect of patient navigation on colorectal cancer screening in a community-based randomized controlled trial of urban African American adults. Cancer Causes Control. 2015 Feb;26(2):239-46.
59. Grubbs SS et al. Eliminating racial disparities in colorectal cancer in the real world: It took a village. J Clin Oncol. 2013 Jun 1;31(16):1928-30.
60. Jung MY et al. The Chinese and Korean American immigrant experience: a mixed-methods examination of facilitators and barriers of colorectal cancer screening. Ethn Health. 2017 Feb 25:1-20.
61. Viruell-Fuentes EA et al. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012 Dec;75(12):2099-106.
Dr. Oduyebo is a third-year fellow at the Mayo Clinic, Rochester, Minn.; Dr. Malespin is an assistant professor in the department of medicine and the medical director of hepatology at the University of Florida Health, Jacksonville; Dr. Mendoza Ladd is an assistant professor of medicine at Texas Tech University, El Paso; Dr. Day is an associate professor of medicine at the University of California, San Francisco; Dr. Charabaty is an associate professor of medicine and the director of the IBD Center in the division of gastroenterology at Medstar-Georgetown University Center, Washington; Dr. Chen is an associate professor of medicine, the director of patient safety and quality, and the director of the small-bowel endoscopy program in division of gastroenterology at Washington University, St. Louis; Dr. Carr is an assistant professor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia; Dr. Quezada is an assistant dean for admissions, an assistant dean for academic and multicultural affairs, and an assistant professor of medicine in the division of gastroenterology and hepatology at the University of Maryland, Baltimore; and Dr. Lamousé-Smith is a director of translational medicine, immunology, and early development at Janssen Pharmaceuticals Research and Development, Spring House, Penn.
Barriers to screening, navigating DDW®, hepatology training, retirement, and more in this issue
Dear Colleagues,
Welcome to the second edition of The New Gastroenterologist in its e-newsletter format! As more content in medicine, and life in general, is moving toward digital platforms, we at the AGA believe this transition will improve both content dissemination and accessibility to all our readers. In this new format, we will to continue to provide articles on topics of importance to the early-career community, expand our offerings by including the new “In Focus” articles (concise overviews of GI topics) both digitally and in GI & Hepatology News print issues, as well as increase the use of multimedia resources, such as videos, to further enhance our content.
The “In Focus” article this month is authored by the members of the AGA’s Diversity Committee and focuses on the extremely important topic of barriers preventing colorectal cancer screening in underserved populations. This comprehensive overview will undoubtedly help us in our mission to ensure valuable colorectal cancer screening is more frequently, and widely, applied. And be sure to look for it in the May print issue of GI & Hepatology News as well.
Digestive Disease Week (DDW®), which many of us will be attending, features cutting-edge research and provides an invaluable opportunity for networking. With DDW right around the corner, Lea Ann Chen (NYU) gives some very helpful pointers to ensure that you get the most out of your experience. Additionally, David Leiman (Duke) and Neil Sengupta (University of Chicago) provide an overview of how best to incorporate new evidence into your daily practice. This is such a critical topic nowadays given the ever-growing number of journal articles published as well as the speed at which information is disseminated both throughout our field and in the popular press.
In our postfellowship pathways section, Elizabeth Verna (Columbia) provides an overview of the advanced training options available in hepatology including the new ABIM pilot program that combines a transplant hepatology fellowship year with the third year of fellowship. Finally, there is an overview on strategies for retirement savings by A.J. Bellamah (BNB Wealth Management), which is an area where so many of us get a late start due to extended training and student loan burden.
Please also check out the “In Case You Missed It” section to see selected articles published in the AGA journals, which are particularly relevant to those of us in our early careers. If you have any ideas for future articles, or are interested in contributing to The New Gastroenterologist, please contact me at [email protected] or the managing editor, Ryan Farrell, at [email protected].
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an instructor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
Dear Colleagues,
Welcome to the second edition of The New Gastroenterologist in its e-newsletter format! As more content in medicine, and life in general, is moving toward digital platforms, we at the AGA believe this transition will improve both content dissemination and accessibility to all our readers. In this new format, we will to continue to provide articles on topics of importance to the early-career community, expand our offerings by including the new “In Focus” articles (concise overviews of GI topics) both digitally and in GI & Hepatology News print issues, as well as increase the use of multimedia resources, such as videos, to further enhance our content.
The “In Focus” article this month is authored by the members of the AGA’s Diversity Committee and focuses on the extremely important topic of barriers preventing colorectal cancer screening in underserved populations. This comprehensive overview will undoubtedly help us in our mission to ensure valuable colorectal cancer screening is more frequently, and widely, applied. And be sure to look for it in the May print issue of GI & Hepatology News as well.
Digestive Disease Week (DDW®), which many of us will be attending, features cutting-edge research and provides an invaluable opportunity for networking. With DDW right around the corner, Lea Ann Chen (NYU) gives some very helpful pointers to ensure that you get the most out of your experience. Additionally, David Leiman (Duke) and Neil Sengupta (University of Chicago) provide an overview of how best to incorporate new evidence into your daily practice. This is such a critical topic nowadays given the ever-growing number of journal articles published as well as the speed at which information is disseminated both throughout our field and in the popular press.
In our postfellowship pathways section, Elizabeth Verna (Columbia) provides an overview of the advanced training options available in hepatology including the new ABIM pilot program that combines a transplant hepatology fellowship year with the third year of fellowship. Finally, there is an overview on strategies for retirement savings by A.J. Bellamah (BNB Wealth Management), which is an area where so many of us get a late start due to extended training and student loan burden.
Please also check out the “In Case You Missed It” section to see selected articles published in the AGA journals, which are particularly relevant to those of us in our early careers. If you have any ideas for future articles, or are interested in contributing to The New Gastroenterologist, please contact me at [email protected] or the managing editor, Ryan Farrell, at [email protected].
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an instructor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
Dear Colleagues,
Welcome to the second edition of The New Gastroenterologist in its e-newsletter format! As more content in medicine, and life in general, is moving toward digital platforms, we at the AGA believe this transition will improve both content dissemination and accessibility to all our readers. In this new format, we will to continue to provide articles on topics of importance to the early-career community, expand our offerings by including the new “In Focus” articles (concise overviews of GI topics) both digitally and in GI & Hepatology News print issues, as well as increase the use of multimedia resources, such as videos, to further enhance our content.
The “In Focus” article this month is authored by the members of the AGA’s Diversity Committee and focuses on the extremely important topic of barriers preventing colorectal cancer screening in underserved populations. This comprehensive overview will undoubtedly help us in our mission to ensure valuable colorectal cancer screening is more frequently, and widely, applied. And be sure to look for it in the May print issue of GI & Hepatology News as well.
Digestive Disease Week (DDW®), which many of us will be attending, features cutting-edge research and provides an invaluable opportunity for networking. With DDW right around the corner, Lea Ann Chen (NYU) gives some very helpful pointers to ensure that you get the most out of your experience. Additionally, David Leiman (Duke) and Neil Sengupta (University of Chicago) provide an overview of how best to incorporate new evidence into your daily practice. This is such a critical topic nowadays given the ever-growing number of journal articles published as well as the speed at which information is disseminated both throughout our field and in the popular press.
In our postfellowship pathways section, Elizabeth Verna (Columbia) provides an overview of the advanced training options available in hepatology including the new ABIM pilot program that combines a transplant hepatology fellowship year with the third year of fellowship. Finally, there is an overview on strategies for retirement savings by A.J. Bellamah (BNB Wealth Management), which is an area where so many of us get a late start due to extended training and student loan burden.
Please also check out the “In Case You Missed It” section to see selected articles published in the AGA journals, which are particularly relevant to those of us in our early careers. If you have any ideas for future articles, or are interested in contributing to The New Gastroenterologist, please contact me at [email protected] or the managing editor, Ryan Farrell, at [email protected].
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an instructor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
Foundations for financial security: Get out of student debt and on the fast track to financial prosperity
Approaching the concept of retirement savings is particularly unique for medical professionals: Balancing a tremendously demanding career with family life and personal time allows few to have the luxury of extra time to address financial planning. Many in the field have higher priorities than saving for retirement on their minds, which compounds the issue.
According to the Association of American Medical Colleges, 76% of medical students will have student debt by the time they graduate. Among those students, the average debt is a staggering $190,000. The average American couple has only about $163,000 in savings by the time they are about 60 years old, so coming out of school, the average doctor will have more in debt than most have saved in their lifetimes. This means that many doctors can’t really start saving significantly until the latter half of their careers. With that in mind, consider these tips to help you on your journey to financial security.
Pay off debt or start saving for retirement?
When it comes to the decision of investing toward retirement or paying off debt more aggressively, there is really only one question that needs to be answered: “Can I make more investing than the loan is costing me?” Given the fact that Direct Graduate Plus Loans are now sitting at about 7% interest rates, an investment would have to make more than 7% per year to make sense. While we can look back at the historical performance of the stock market over time, it is pretty safe to say that in this scenario paying off the student loans as aggressively as possible is the best choice. The reason being is that the loans have a guaranteed cost of 7% per year in accrued interest, whereas an investment is never fully guaranteed to grow.
Make no mistake: High-interest debt is a financial dead weight; the longer it sits, the more it will attempt to sink you financially. A general rule of thumb is that the higher the interest rate on the loan, the more aggressively it should be paid off. Once the high interest loans are taken care of, saving for retirement can reenter the equation.
The company match
That being said, there is one caveat to this rule that you should strongly consider if the opportunity exists: the 401(k) or 403(b) company match. If you work in a position that offers a match on retirement plan contributions, taking advantage of this could substantially benefit you. In a typical safe harbor retirement plan, you will see something like a 3.5% company match for a 6% salary contribution. While there is no one formula that applies to every situation, an opportunity such as this shouldn’t be passed up.
Saving for retirement can be difficult enough. Why not take advantage of a situation in which you are getting free money? You should think about contributing enough to get the maximum match and putting the rest toward student debt. If you are unsure about your particular course of action, I’d suggest speaking to your financial professional to assist in coming up with a suitable game plan.
Roth deferral option
While many folks understand the general ins and outs of how retirement plans work, they fail to realize that there are actually two different types of contributions that can be made in most 401(k)s and 403(b)s: traditional deferrals and Roth deferrals. A traditional deferral is the standard pretax contribution option that lets you skip paying taxes now. Instead, you get taxed at your normal income tax bracket when the money is withdrawn in retirement. This is the option that most people use.
Roth deferrals are posttax contributions. Every dollar contributed gets taxed as ordinary income. Why would one do this, you ask? While there are a variety of different benefits, the primary advantage is that you never have to pay taxes on this money again. To reiterate, you pay taxes on this money now and never have to pay any taxes on it again. This can be extraordinarily helpful in retirement because it gives you the flexibility to choose between taxable and tax-free income.
While you can contribute to personal Roth IRAs to the tune of $5,500 a year if you are under 50 years old and $6,500 if you are 50 years and older, high income earners can be hampered by income limits. For instance, if you make over $135,000 a year as a single person or over $199,000 as a married couple, you are ineligible to make Roth IRA contributions. However, a benefit to Roth contributions in your company 401(k) or 403(b) plan is that these income limits don’t apply. Regardless of your level of income, you can make Roth deferrals in company sponsored retirement plans that allow them.
This strategy is best fit for, but not limited to, those who are earlier on in their careers and can reasonably expect to make much more in the future than they do now. Younger investors have the benefit of time: The more time an investment has to grow, the more it should be worth later on. Also, younger professionals are probably going to be paying the least amount of taxes early in their careers. While not all retirement plans allow for Roth deferrals, if the option is available, why not get taxes out of the way while it’s still relatively cheaper to do so?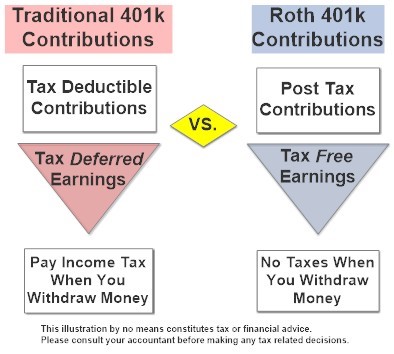
More aggressive strategies for those who need to “catch up” on retirement savings
Because many in the medical field have burdensome student loans, saving for retirement is often something that is pushed off by necessity. That being said, there are different ways to start saving more aggressively the closer you get toward retirement.
Catch up contributions. 401(k)s, 403(b)s, and IRAs all have built in “catch up” contributions that allow those aged 50 or older to save more. For instance, up to age 49 years, the maximum annual contribution in a 401(k) or 403(b) is $18,500 for 2018. At age 50 years, you are allowed to add an additional $6000 “catch up” contribution for a total of $24,500 per year. Likewise, IRAs allow for an additional $1000 per year contribution at age 50 years for a $6500 total yearly contribution.
Spousal IRAs. If you have a nonworking spouse, you may be able to contribute to an IRA on his or her behalf. To be eligible for a spousal IRA contribution, you must be married, file a joint income tax return, and have an earned income of at least what is being contributed to the IRAs. This would allow an additional $5,500 to $6,500 in retirement savings per year depending on your spouse’s age.
Simplified Employee Pension IRAs. For those who are self-employed, it could be worthwhile to look into opening up a Simplified Employee Pension (SEP) IRA. These types of retirement plans are similar to traditional IRAs except that they can only be opened up by an employer. The benefit of a SEP IRA is that it allows for a maximum pretax contribution of up to $54,000 or 25% of your total income, whichever is less.
Cash balance plans. For very-high-earning business owners or sole proprietors, saving $24,500 a year pretax in a 401(k) isn’t necessarily going to move the needle all that much. However, there is a plan available that may help tremendously. The cash balance plan is a little known hybrid retirement plan that allows high-earning practices and business owners to put away a serious amount of money in a short amount of time. For instance, an optimally set up cash balance plan would allow a 59 year old to save up to $278,000 in qualified pretax dollars in a single year. Undoubtedly, such plans are one of the most effective and efficient ways to save money for retirement for those who qualify.
Check out the maximum contributions limits of some retirement strategies below based on your age group.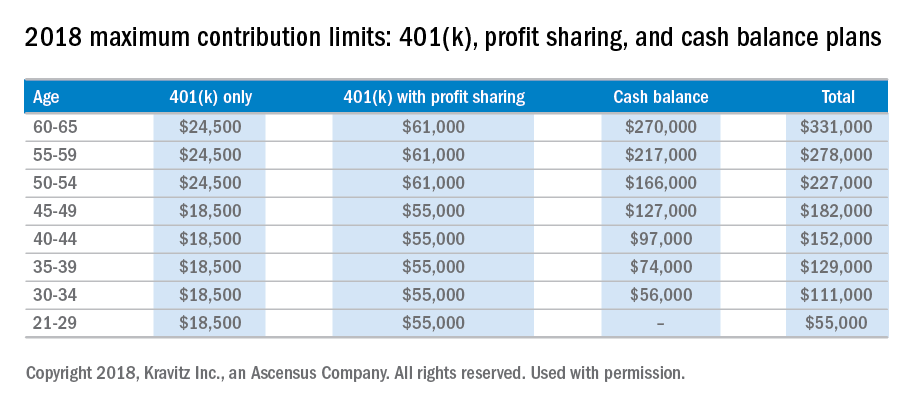
It’s important to realize that it is time that makes money, not timing. Establishing a smart investment plan early in your career will pay huge dividends and save mountains of heartache in your future. If you are unsure about which retirement plan works best for you, I’d recommend speaking to a qualified financial professional to assist you in the process. When it comes to planning for retirement, sooner is always better than later. The financial sacrifices of starting early are never as great as most young professionals fear.
Disclaimer:
This material has been prepared for educational purposes only and is not intended to provide, and should not be relied on for tax, legal, accounting advice, or financial advice. You should consult your own tax, legal, accounting, and financial advisors before engaging in any transaction. Securities offered through Capitol Securities Management Member FINRA, SIPC
Mr. Bellamah is a registered investment advisor with BNB Wealth Management http://www.bnbinc.com/.
Approaching the concept of retirement savings is particularly unique for medical professionals: Balancing a tremendously demanding career with family life and personal time allows few to have the luxury of extra time to address financial planning. Many in the field have higher priorities than saving for retirement on their minds, which compounds the issue.
According to the Association of American Medical Colleges, 76% of medical students will have student debt by the time they graduate. Among those students, the average debt is a staggering $190,000. The average American couple has only about $163,000 in savings by the time they are about 60 years old, so coming out of school, the average doctor will have more in debt than most have saved in their lifetimes. This means that many doctors can’t really start saving significantly until the latter half of their careers. With that in mind, consider these tips to help you on your journey to financial security.
Pay off debt or start saving for retirement?
When it comes to the decision of investing toward retirement or paying off debt more aggressively, there is really only one question that needs to be answered: “Can I make more investing than the loan is costing me?” Given the fact that Direct Graduate Plus Loans are now sitting at about 7% interest rates, an investment would have to make more than 7% per year to make sense. While we can look back at the historical performance of the stock market over time, it is pretty safe to say that in this scenario paying off the student loans as aggressively as possible is the best choice. The reason being is that the loans have a guaranteed cost of 7% per year in accrued interest, whereas an investment is never fully guaranteed to grow.
Make no mistake: High-interest debt is a financial dead weight; the longer it sits, the more it will attempt to sink you financially. A general rule of thumb is that the higher the interest rate on the loan, the more aggressively it should be paid off. Once the high interest loans are taken care of, saving for retirement can reenter the equation.
The company match
That being said, there is one caveat to this rule that you should strongly consider if the opportunity exists: the 401(k) or 403(b) company match. If you work in a position that offers a match on retirement plan contributions, taking advantage of this could substantially benefit you. In a typical safe harbor retirement plan, you will see something like a 3.5% company match for a 6% salary contribution. While there is no one formula that applies to every situation, an opportunity such as this shouldn’t be passed up.
Saving for retirement can be difficult enough. Why not take advantage of a situation in which you are getting free money? You should think about contributing enough to get the maximum match and putting the rest toward student debt. If you are unsure about your particular course of action, I’d suggest speaking to your financial professional to assist in coming up with a suitable game plan.
Roth deferral option
While many folks understand the general ins and outs of how retirement plans work, they fail to realize that there are actually two different types of contributions that can be made in most 401(k)s and 403(b)s: traditional deferrals and Roth deferrals. A traditional deferral is the standard pretax contribution option that lets you skip paying taxes now. Instead, you get taxed at your normal income tax bracket when the money is withdrawn in retirement. This is the option that most people use.
Roth deferrals are posttax contributions. Every dollar contributed gets taxed as ordinary income. Why would one do this, you ask? While there are a variety of different benefits, the primary advantage is that you never have to pay taxes on this money again. To reiterate, you pay taxes on this money now and never have to pay any taxes on it again. This can be extraordinarily helpful in retirement because it gives you the flexibility to choose between taxable and tax-free income.
While you can contribute to personal Roth IRAs to the tune of $5,500 a year if you are under 50 years old and $6,500 if you are 50 years and older, high income earners can be hampered by income limits. For instance, if you make over $135,000 a year as a single person or over $199,000 as a married couple, you are ineligible to make Roth IRA contributions. However, a benefit to Roth contributions in your company 401(k) or 403(b) plan is that these income limits don’t apply. Regardless of your level of income, you can make Roth deferrals in company sponsored retirement plans that allow them.
This strategy is best fit for, but not limited to, those who are earlier on in their careers and can reasonably expect to make much more in the future than they do now. Younger investors have the benefit of time: The more time an investment has to grow, the more it should be worth later on. Also, younger professionals are probably going to be paying the least amount of taxes early in their careers. While not all retirement plans allow for Roth deferrals, if the option is available, why not get taxes out of the way while it’s still relatively cheaper to do so?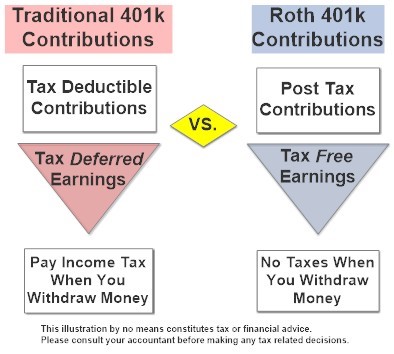
More aggressive strategies for those who need to “catch up” on retirement savings
Because many in the medical field have burdensome student loans, saving for retirement is often something that is pushed off by necessity. That being said, there are different ways to start saving more aggressively the closer you get toward retirement.
Catch up contributions. 401(k)s, 403(b)s, and IRAs all have built in “catch up” contributions that allow those aged 50 or older to save more. For instance, up to age 49 years, the maximum annual contribution in a 401(k) or 403(b) is $18,500 for 2018. At age 50 years, you are allowed to add an additional $6000 “catch up” contribution for a total of $24,500 per year. Likewise, IRAs allow for an additional $1000 per year contribution at age 50 years for a $6500 total yearly contribution.
Spousal IRAs. If you have a nonworking spouse, you may be able to contribute to an IRA on his or her behalf. To be eligible for a spousal IRA contribution, you must be married, file a joint income tax return, and have an earned income of at least what is being contributed to the IRAs. This would allow an additional $5,500 to $6,500 in retirement savings per year depending on your spouse’s age.
Simplified Employee Pension IRAs. For those who are self-employed, it could be worthwhile to look into opening up a Simplified Employee Pension (SEP) IRA. These types of retirement plans are similar to traditional IRAs except that they can only be opened up by an employer. The benefit of a SEP IRA is that it allows for a maximum pretax contribution of up to $54,000 or 25% of your total income, whichever is less.
Cash balance plans. For very-high-earning business owners or sole proprietors, saving $24,500 a year pretax in a 401(k) isn’t necessarily going to move the needle all that much. However, there is a plan available that may help tremendously. The cash balance plan is a little known hybrid retirement plan that allows high-earning practices and business owners to put away a serious amount of money in a short amount of time. For instance, an optimally set up cash balance plan would allow a 59 year old to save up to $278,000 in qualified pretax dollars in a single year. Undoubtedly, such plans are one of the most effective and efficient ways to save money for retirement for those who qualify.
Check out the maximum contributions limits of some retirement strategies below based on your age group.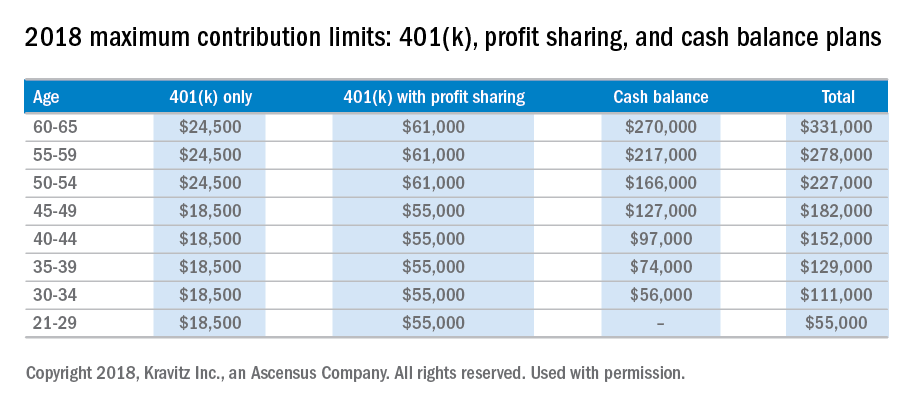
It’s important to realize that it is time that makes money, not timing. Establishing a smart investment plan early in your career will pay huge dividends and save mountains of heartache in your future. If you are unsure about which retirement plan works best for you, I’d recommend speaking to a qualified financial professional to assist you in the process. When it comes to planning for retirement, sooner is always better than later. The financial sacrifices of starting early are never as great as most young professionals fear.
Disclaimer:
This material has been prepared for educational purposes only and is not intended to provide, and should not be relied on for tax, legal, accounting advice, or financial advice. You should consult your own tax, legal, accounting, and financial advisors before engaging in any transaction. Securities offered through Capitol Securities Management Member FINRA, SIPC
Mr. Bellamah is a registered investment advisor with BNB Wealth Management http://www.bnbinc.com/.
Approaching the concept of retirement savings is particularly unique for medical professionals: Balancing a tremendously demanding career with family life and personal time allows few to have the luxury of extra time to address financial planning. Many in the field have higher priorities than saving for retirement on their minds, which compounds the issue.
According to the Association of American Medical Colleges, 76% of medical students will have student debt by the time they graduate. Among those students, the average debt is a staggering $190,000. The average American couple has only about $163,000 in savings by the time they are about 60 years old, so coming out of school, the average doctor will have more in debt than most have saved in their lifetimes. This means that many doctors can’t really start saving significantly until the latter half of their careers. With that in mind, consider these tips to help you on your journey to financial security.
Pay off debt or start saving for retirement?
When it comes to the decision of investing toward retirement or paying off debt more aggressively, there is really only one question that needs to be answered: “Can I make more investing than the loan is costing me?” Given the fact that Direct Graduate Plus Loans are now sitting at about 7% interest rates, an investment would have to make more than 7% per year to make sense. While we can look back at the historical performance of the stock market over time, it is pretty safe to say that in this scenario paying off the student loans as aggressively as possible is the best choice. The reason being is that the loans have a guaranteed cost of 7% per year in accrued interest, whereas an investment is never fully guaranteed to grow.
Make no mistake: High-interest debt is a financial dead weight; the longer it sits, the more it will attempt to sink you financially. A general rule of thumb is that the higher the interest rate on the loan, the more aggressively it should be paid off. Once the high interest loans are taken care of, saving for retirement can reenter the equation.
The company match
That being said, there is one caveat to this rule that you should strongly consider if the opportunity exists: the 401(k) or 403(b) company match. If you work in a position that offers a match on retirement plan contributions, taking advantage of this could substantially benefit you. In a typical safe harbor retirement plan, you will see something like a 3.5% company match for a 6% salary contribution. While there is no one formula that applies to every situation, an opportunity such as this shouldn’t be passed up.
Saving for retirement can be difficult enough. Why not take advantage of a situation in which you are getting free money? You should think about contributing enough to get the maximum match and putting the rest toward student debt. If you are unsure about your particular course of action, I’d suggest speaking to your financial professional to assist in coming up with a suitable game plan.
Roth deferral option
While many folks understand the general ins and outs of how retirement plans work, they fail to realize that there are actually two different types of contributions that can be made in most 401(k)s and 403(b)s: traditional deferrals and Roth deferrals. A traditional deferral is the standard pretax contribution option that lets you skip paying taxes now. Instead, you get taxed at your normal income tax bracket when the money is withdrawn in retirement. This is the option that most people use.
Roth deferrals are posttax contributions. Every dollar contributed gets taxed as ordinary income. Why would one do this, you ask? While there are a variety of different benefits, the primary advantage is that you never have to pay taxes on this money again. To reiterate, you pay taxes on this money now and never have to pay any taxes on it again. This can be extraordinarily helpful in retirement because it gives you the flexibility to choose between taxable and tax-free income.
While you can contribute to personal Roth IRAs to the tune of $5,500 a year if you are under 50 years old and $6,500 if you are 50 years and older, high income earners can be hampered by income limits. For instance, if you make over $135,000 a year as a single person or over $199,000 as a married couple, you are ineligible to make Roth IRA contributions. However, a benefit to Roth contributions in your company 401(k) or 403(b) plan is that these income limits don’t apply. Regardless of your level of income, you can make Roth deferrals in company sponsored retirement plans that allow them.
This strategy is best fit for, but not limited to, those who are earlier on in their careers and can reasonably expect to make much more in the future than they do now. Younger investors have the benefit of time: The more time an investment has to grow, the more it should be worth later on. Also, younger professionals are probably going to be paying the least amount of taxes early in their careers. While not all retirement plans allow for Roth deferrals, if the option is available, why not get taxes out of the way while it’s still relatively cheaper to do so?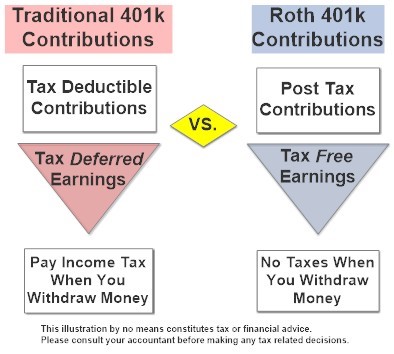
More aggressive strategies for those who need to “catch up” on retirement savings
Because many in the medical field have burdensome student loans, saving for retirement is often something that is pushed off by necessity. That being said, there are different ways to start saving more aggressively the closer you get toward retirement.
Catch up contributions. 401(k)s, 403(b)s, and IRAs all have built in “catch up” contributions that allow those aged 50 or older to save more. For instance, up to age 49 years, the maximum annual contribution in a 401(k) or 403(b) is $18,500 for 2018. At age 50 years, you are allowed to add an additional $6000 “catch up” contribution for a total of $24,500 per year. Likewise, IRAs allow for an additional $1000 per year contribution at age 50 years for a $6500 total yearly contribution.
Spousal IRAs. If you have a nonworking spouse, you may be able to contribute to an IRA on his or her behalf. To be eligible for a spousal IRA contribution, you must be married, file a joint income tax return, and have an earned income of at least what is being contributed to the IRAs. This would allow an additional $5,500 to $6,500 in retirement savings per year depending on your spouse’s age.
Simplified Employee Pension IRAs. For those who are self-employed, it could be worthwhile to look into opening up a Simplified Employee Pension (SEP) IRA. These types of retirement plans are similar to traditional IRAs except that they can only be opened up by an employer. The benefit of a SEP IRA is that it allows for a maximum pretax contribution of up to $54,000 or 25% of your total income, whichever is less.
Cash balance plans. For very-high-earning business owners or sole proprietors, saving $24,500 a year pretax in a 401(k) isn’t necessarily going to move the needle all that much. However, there is a plan available that may help tremendously. The cash balance plan is a little known hybrid retirement plan that allows high-earning practices and business owners to put away a serious amount of money in a short amount of time. For instance, an optimally set up cash balance plan would allow a 59 year old to save up to $278,000 in qualified pretax dollars in a single year. Undoubtedly, such plans are one of the most effective and efficient ways to save money for retirement for those who qualify.
Check out the maximum contributions limits of some retirement strategies below based on your age group.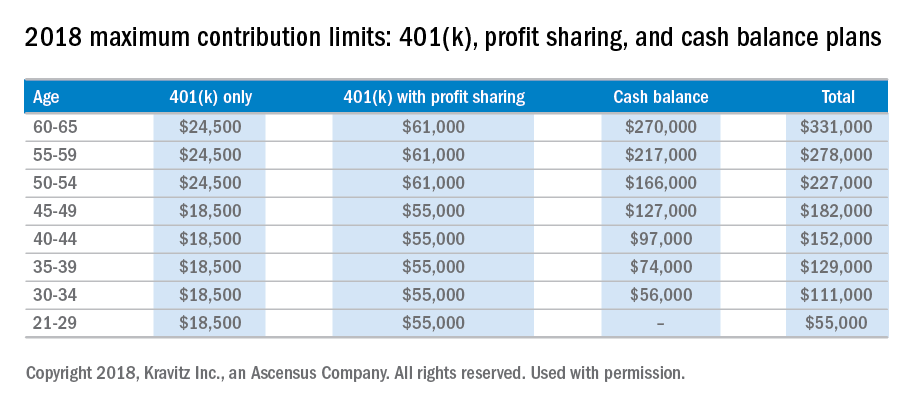
It’s important to realize that it is time that makes money, not timing. Establishing a smart investment plan early in your career will pay huge dividends and save mountains of heartache in your future. If you are unsure about which retirement plan works best for you, I’d recommend speaking to a qualified financial professional to assist you in the process. When it comes to planning for retirement, sooner is always better than later. The financial sacrifices of starting early are never as great as most young professionals fear.
Disclaimer:
This material has been prepared for educational purposes only and is not intended to provide, and should not be relied on for tax, legal, accounting advice, or financial advice. You should consult your own tax, legal, accounting, and financial advisors before engaging in any transaction. Securities offered through Capitol Securities Management Member FINRA, SIPC
Mr. Bellamah is a registered investment advisor with BNB Wealth Management http://www.bnbinc.com/.
Calendar
For more information about upcoming events and award deadlines, please visit http://www.gastro.org/education and http://www.gastro.org/research-funding.
June 2-5, 2018
DIGESTIVE DISEASE WEEK® (DDW) 2018 – WASHINGTON, DC
DDW® is the premier meeting for the GI professional. Every year, it attracts approximately 15,000 physicians, researchers, and academics from around the world who desire to stay up to date in the field.
AGA Trainee and Early-Career GI Sessions
Join your colleagues at special sessions to meet the unique needs of physicians who are new to the field. Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
- June 2, 8:15 a.m.–5:30 p.m.; June 3, 8:30 a.m.–12:35 p.m.
AGA Postgraduate Course: From Abstract to Reality
Attend this multi-topic course to get practical, useful information to push your practice to the next level. The 2018 course will provide a comprehensive look at the latest medical, surgical, and technological advances over the past 12 months that aim to keep you up to date in a field that is rapidly changing. Each presenter will turn abstract ideas into concrete action items that you can immediately implement in your practice. AGA member trainees and early-career GIs receive discounted pricing for this course. - June 3, 4–5:30 p.m.
Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
During this session, attendees will obtain effective negotiation techniques and learn how to navigate difficult situations in clinical and research environments. - June 3, 6-7 p.m.
AGA Early Career Networking Hour
This event is open to all DDW trainee and early career GI attendees and provides a casual atmosphere to bond with your peers. Complimentary food and drinks will be available. - June 4, 4–5:30 p.m.
Advancing Clinical Practice: Gastroenterology Fellow–Directed Quality-Improvement Projects
This trainee-focused session will showcase selected abstracts from GI fellows based on quality improvement with a state-of-the-art lecture. Attendees will be provided with information that defines practical approaches to quality improvement from start to finish. A limited supply of coffee and tea will be provided during the session. - June 5, 1:30–5:30 p.m.
Board Review Course
This session, designed using content from DDSEP® 8, serves as a primer for third-year fellows preparing for the board exam as well as a review course for others wanting to test their knowledge. Session attendees will receive a $50 coupon to use at the AGA Store at DDW to purchase DDSEP 8.
UPCOMING EVENTS
June 4-8, 2018
Exosomes/Microvesicles: Heterogeneity, Biogenesis, Function, and Therapeutic Developments (E2)
Deepen your understanding of the structural and functional complexity of extracellular vesicles, their biogenesis and function in health and disease, cargo enrichment, potential as ideal biomarkers, and breakthroughs in their use as therapeutic targets/agents.
Breckenridge, CO
June 13-14; Aug. 15-16; Sept. 19-20; Oct. 10-11, 2018
Two-Day, In-Depth Coding and Billing Seminar
Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Nashville, TN (6/13-6/14); Baltimore, MD (8/15-8/16); Atlanta, GA (9/19-9/20); Las Vegas, NV (10/10-10/11)
Aug. 10–12, 2018
Principles of GI for the NP and PA
Hear from the experts as they provide you with critical updates on treating and managing patients with a variety of GI disorders.
Chicago, IL
Aug. 18-19, 2018
James W. Freston Conference: Obesity and Metabolic Disease – Integrating New Paradigms in Pathophysiology to Advance Treatment
Collaborate with researchers and clinicians to help advance obesity treatment and enhance the continuum of obesity care.
Arlington, VA
Feb. 7-9, 2019
Crohn’s & Colitis Congress™ (A Partnership of the Crohn’s & Colitis Foundation and American Gastroenterological Association)
Expand your knowledge, network with IBD leaders, spark innovative research and get inspired to improve patient care.
Las Vegas, NV
For more information about upcoming events and award deadlines, please visit http://www.gastro.org/education and http://www.gastro.org/research-funding.
June 2-5, 2018
DIGESTIVE DISEASE WEEK® (DDW) 2018 – WASHINGTON, DC
DDW® is the premier meeting for the GI professional. Every year, it attracts approximately 15,000 physicians, researchers, and academics from around the world who desire to stay up to date in the field.
AGA Trainee and Early-Career GI Sessions
Join your colleagues at special sessions to meet the unique needs of physicians who are new to the field. Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
- June 2, 8:15 a.m.–5:30 p.m.; June 3, 8:30 a.m.–12:35 p.m.
AGA Postgraduate Course: From Abstract to Reality
Attend this multi-topic course to get practical, useful information to push your practice to the next level. The 2018 course will provide a comprehensive look at the latest medical, surgical, and technological advances over the past 12 months that aim to keep you up to date in a field that is rapidly changing. Each presenter will turn abstract ideas into concrete action items that you can immediately implement in your practice. AGA member trainees and early-career GIs receive discounted pricing for this course. - June 3, 4–5:30 p.m.
Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
During this session, attendees will obtain effective negotiation techniques and learn how to navigate difficult situations in clinical and research environments. - June 3, 6-7 p.m.
AGA Early Career Networking Hour
This event is open to all DDW trainee and early career GI attendees and provides a casual atmosphere to bond with your peers. Complimentary food and drinks will be available. - June 4, 4–5:30 p.m.
Advancing Clinical Practice: Gastroenterology Fellow–Directed Quality-Improvement Projects
This trainee-focused session will showcase selected abstracts from GI fellows based on quality improvement with a state-of-the-art lecture. Attendees will be provided with information that defines practical approaches to quality improvement from start to finish. A limited supply of coffee and tea will be provided during the session. - June 5, 1:30–5:30 p.m.
Board Review Course
This session, designed using content from DDSEP® 8, serves as a primer for third-year fellows preparing for the board exam as well as a review course for others wanting to test their knowledge. Session attendees will receive a $50 coupon to use at the AGA Store at DDW to purchase DDSEP 8.
UPCOMING EVENTS
June 4-8, 2018
Exosomes/Microvesicles: Heterogeneity, Biogenesis, Function, and Therapeutic Developments (E2)
Deepen your understanding of the structural and functional complexity of extracellular vesicles, their biogenesis and function in health and disease, cargo enrichment, potential as ideal biomarkers, and breakthroughs in their use as therapeutic targets/agents.
Breckenridge, CO
June 13-14; Aug. 15-16; Sept. 19-20; Oct. 10-11, 2018
Two-Day, In-Depth Coding and Billing Seminar
Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Nashville, TN (6/13-6/14); Baltimore, MD (8/15-8/16); Atlanta, GA (9/19-9/20); Las Vegas, NV (10/10-10/11)
Aug. 10–12, 2018
Principles of GI for the NP and PA
Hear from the experts as they provide you with critical updates on treating and managing patients with a variety of GI disorders.
Chicago, IL
Aug. 18-19, 2018
James W. Freston Conference: Obesity and Metabolic Disease – Integrating New Paradigms in Pathophysiology to Advance Treatment
Collaborate with researchers and clinicians to help advance obesity treatment and enhance the continuum of obesity care.
Arlington, VA
Feb. 7-9, 2019
Crohn’s & Colitis Congress™ (A Partnership of the Crohn’s & Colitis Foundation and American Gastroenterological Association)
Expand your knowledge, network with IBD leaders, spark innovative research and get inspired to improve patient care.
Las Vegas, NV
For more information about upcoming events and award deadlines, please visit http://www.gastro.org/education and http://www.gastro.org/research-funding.
June 2-5, 2018
DIGESTIVE DISEASE WEEK® (DDW) 2018 – WASHINGTON, DC
DDW® is the premier meeting for the GI professional. Every year, it attracts approximately 15,000 physicians, researchers, and academics from around the world who desire to stay up to date in the field.
AGA Trainee and Early-Career GI Sessions
Join your colleagues at special sessions to meet the unique needs of physicians who are new to the field. Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
- June 2, 8:15 a.m.–5:30 p.m.; June 3, 8:30 a.m.–12:35 p.m.
AGA Postgraduate Course: From Abstract to Reality
Attend this multi-topic course to get practical, useful information to push your practice to the next level. The 2018 course will provide a comprehensive look at the latest medical, surgical, and technological advances over the past 12 months that aim to keep you up to date in a field that is rapidly changing. Each presenter will turn abstract ideas into concrete action items that you can immediately implement in your practice. AGA member trainees and early-career GIs receive discounted pricing for this course. - June 3, 4–5:30 p.m.
Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
During this session, attendees will obtain effective negotiation techniques and learn how to navigate difficult situations in clinical and research environments. - June 3, 6-7 p.m.
AGA Early Career Networking Hour
This event is open to all DDW trainee and early career GI attendees and provides a casual atmosphere to bond with your peers. Complimentary food and drinks will be available. - June 4, 4–5:30 p.m.
Advancing Clinical Practice: Gastroenterology Fellow–Directed Quality-Improvement Projects
This trainee-focused session will showcase selected abstracts from GI fellows based on quality improvement with a state-of-the-art lecture. Attendees will be provided with information that defines practical approaches to quality improvement from start to finish. A limited supply of coffee and tea will be provided during the session. - June 5, 1:30–5:30 p.m.
Board Review Course
This session, designed using content from DDSEP® 8, serves as a primer for third-year fellows preparing for the board exam as well as a review course for others wanting to test their knowledge. Session attendees will receive a $50 coupon to use at the AGA Store at DDW to purchase DDSEP 8.
UPCOMING EVENTS
June 4-8, 2018
Exosomes/Microvesicles: Heterogeneity, Biogenesis, Function, and Therapeutic Developments (E2)
Deepen your understanding of the structural and functional complexity of extracellular vesicles, their biogenesis and function in health and disease, cargo enrichment, potential as ideal biomarkers, and breakthroughs in their use as therapeutic targets/agents.
Breckenridge, CO
June 13-14; Aug. 15-16; Sept. 19-20; Oct. 10-11, 2018
Two-Day, In-Depth Coding and Billing Seminar
Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Nashville, TN (6/13-6/14); Baltimore, MD (8/15-8/16); Atlanta, GA (9/19-9/20); Las Vegas, NV (10/10-10/11)
Aug. 10–12, 2018
Principles of GI for the NP and PA
Hear from the experts as they provide you with critical updates on treating and managing patients with a variety of GI disorders.
Chicago, IL
Aug. 18-19, 2018
James W. Freston Conference: Obesity and Metabolic Disease – Integrating New Paradigms in Pathophysiology to Advance Treatment
Collaborate with researchers and clinicians to help advance obesity treatment and enhance the continuum of obesity care.
Arlington, VA
Feb. 7-9, 2019
Crohn’s & Colitis Congress™ (A Partnership of the Crohn’s & Colitis Foundation and American Gastroenterological Association)
Expand your knowledge, network with IBD leaders, spark innovative research and get inspired to improve patient care.
Las Vegas, NV