User login
TCT: Everolimus stents best paclitaxel for diabetes patients
SAN FRANCISCO – Everolimus-eluting stents were more effective than were paclitaxel-eluting stents in diabetes patients with coronary artery disease who underwent percutaneous coronary intervention (PCI) in the randomized, multicenter TUXEDO-India trial.
The everolimus-eluting stents were shown to be superior to paclitaxel-eluting stents on several endpoints, including target-vessel failure, myocardial infarction, and stent thrombosis at 1 year Dr. Upendra Kaul reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
Target vessel failure – the study’s primary endpoint, defined as a composite of cardiac death, target-vessel myocardial infarction, or ischemia-driven target-vessel revascularization – occurred in 5.6% of 914 patients randomized to the paclitaxel-eluting stent group, compared with 2.9% of 916 randomized to the everolimus-eluting stent group (relative risk, 1.89), Dr. Kaul of Fortis Escorts Heart Institute, New Delhi, reported at the meeting, which was sponsored by the Cardiovascular Research Foundation.
The rate of spontaneous MI was 3.2% vs. 1.2% in the groups, respectively, and the rate of stent thrombosis was 2.1% vs. 0.4%. Target-vessel revascularization and target-lesion revascularization rates in both groups were 3.4% vs. 1.2% with paclitaxel- and everolimus-eluting stents, respectively, he said, noting that the superiority of everolimus-eluting stents was maintained in insulin-requiring patients.
The findings, which were published online simultaneously (N Engl J Med. 2015 Oct. 14;doi: 10.1056/NEJMoa1510188), effectively end the debate regarding whether paclitaxel-eluting stents are the better choice in diabetes patients with coronary artery disease.
Paclitaxel-eluting stents are generally accepted to be inferior to limus-eluting stents in most patients, but data from numerous trials have been conflicting as to whether that is true in diabetes patients.
“In the absence of a dedicated adequately powered study, a definitive answer is not possible,” Dr. Kaul said.
The findings from TUXEDO, the largest trial to compare paclitaxel- and everolimus-eluting stents head to head in diabetes patients, support “the current worldwide practice of use of new-generation limus-eluting stents, even in patients with insulin-requiring diabetes,” he said.
The findings raise questions about the results of prior coronary artery bypass grafting vs. stenting trials that show superiority of CABG, because first-generation stents, which are inferior to everolimus-eluting stents, were used as comparators in those trials, he noted.
Indeed, current guidelines for bypass surgery and PCI are based upon the findings of those trials, and while the TUXEDO findings don’t invalidate those prior studies, they do raise questions about whether the differences in favor of bypass surgery are much smaller than believed in the setting of modern stent use, commented Dr. Bernard J. Gersh of the Mayo Clinic, Rochester, Minn.
The TUXEDO-India trial was supported by Boston Scientific.
SAN FRANCISCO – Everolimus-eluting stents were more effective than were paclitaxel-eluting stents in diabetes patients with coronary artery disease who underwent percutaneous coronary intervention (PCI) in the randomized, multicenter TUXEDO-India trial.
The everolimus-eluting stents were shown to be superior to paclitaxel-eluting stents on several endpoints, including target-vessel failure, myocardial infarction, and stent thrombosis at 1 year Dr. Upendra Kaul reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
Target vessel failure – the study’s primary endpoint, defined as a composite of cardiac death, target-vessel myocardial infarction, or ischemia-driven target-vessel revascularization – occurred in 5.6% of 914 patients randomized to the paclitaxel-eluting stent group, compared with 2.9% of 916 randomized to the everolimus-eluting stent group (relative risk, 1.89), Dr. Kaul of Fortis Escorts Heart Institute, New Delhi, reported at the meeting, which was sponsored by the Cardiovascular Research Foundation.
The rate of spontaneous MI was 3.2% vs. 1.2% in the groups, respectively, and the rate of stent thrombosis was 2.1% vs. 0.4%. Target-vessel revascularization and target-lesion revascularization rates in both groups were 3.4% vs. 1.2% with paclitaxel- and everolimus-eluting stents, respectively, he said, noting that the superiority of everolimus-eluting stents was maintained in insulin-requiring patients.
The findings, which were published online simultaneously (N Engl J Med. 2015 Oct. 14;doi: 10.1056/NEJMoa1510188), effectively end the debate regarding whether paclitaxel-eluting stents are the better choice in diabetes patients with coronary artery disease.
Paclitaxel-eluting stents are generally accepted to be inferior to limus-eluting stents in most patients, but data from numerous trials have been conflicting as to whether that is true in diabetes patients.
“In the absence of a dedicated adequately powered study, a definitive answer is not possible,” Dr. Kaul said.
The findings from TUXEDO, the largest trial to compare paclitaxel- and everolimus-eluting stents head to head in diabetes patients, support “the current worldwide practice of use of new-generation limus-eluting stents, even in patients with insulin-requiring diabetes,” he said.
The findings raise questions about the results of prior coronary artery bypass grafting vs. stenting trials that show superiority of CABG, because first-generation stents, which are inferior to everolimus-eluting stents, were used as comparators in those trials, he noted.
Indeed, current guidelines for bypass surgery and PCI are based upon the findings of those trials, and while the TUXEDO findings don’t invalidate those prior studies, they do raise questions about whether the differences in favor of bypass surgery are much smaller than believed in the setting of modern stent use, commented Dr. Bernard J. Gersh of the Mayo Clinic, Rochester, Minn.
The TUXEDO-India trial was supported by Boston Scientific.
SAN FRANCISCO – Everolimus-eluting stents were more effective than were paclitaxel-eluting stents in diabetes patients with coronary artery disease who underwent percutaneous coronary intervention (PCI) in the randomized, multicenter TUXEDO-India trial.
The everolimus-eluting stents were shown to be superior to paclitaxel-eluting stents on several endpoints, including target-vessel failure, myocardial infarction, and stent thrombosis at 1 year Dr. Upendra Kaul reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
Target vessel failure – the study’s primary endpoint, defined as a composite of cardiac death, target-vessel myocardial infarction, or ischemia-driven target-vessel revascularization – occurred in 5.6% of 914 patients randomized to the paclitaxel-eluting stent group, compared with 2.9% of 916 randomized to the everolimus-eluting stent group (relative risk, 1.89), Dr. Kaul of Fortis Escorts Heart Institute, New Delhi, reported at the meeting, which was sponsored by the Cardiovascular Research Foundation.
The rate of spontaneous MI was 3.2% vs. 1.2% in the groups, respectively, and the rate of stent thrombosis was 2.1% vs. 0.4%. Target-vessel revascularization and target-lesion revascularization rates in both groups were 3.4% vs. 1.2% with paclitaxel- and everolimus-eluting stents, respectively, he said, noting that the superiority of everolimus-eluting stents was maintained in insulin-requiring patients.
The findings, which were published online simultaneously (N Engl J Med. 2015 Oct. 14;doi: 10.1056/NEJMoa1510188), effectively end the debate regarding whether paclitaxel-eluting stents are the better choice in diabetes patients with coronary artery disease.
Paclitaxel-eluting stents are generally accepted to be inferior to limus-eluting stents in most patients, but data from numerous trials have been conflicting as to whether that is true in diabetes patients.
“In the absence of a dedicated adequately powered study, a definitive answer is not possible,” Dr. Kaul said.
The findings from TUXEDO, the largest trial to compare paclitaxel- and everolimus-eluting stents head to head in diabetes patients, support “the current worldwide practice of use of new-generation limus-eluting stents, even in patients with insulin-requiring diabetes,” he said.
The findings raise questions about the results of prior coronary artery bypass grafting vs. stenting trials that show superiority of CABG, because first-generation stents, which are inferior to everolimus-eluting stents, were used as comparators in those trials, he noted.
Indeed, current guidelines for bypass surgery and PCI are based upon the findings of those trials, and while the TUXEDO findings don’t invalidate those prior studies, they do raise questions about whether the differences in favor of bypass surgery are much smaller than believed in the setting of modern stent use, commented Dr. Bernard J. Gersh of the Mayo Clinic, Rochester, Minn.
The TUXEDO-India trial was supported by Boston Scientific.
AT TCT 2015
Key clinical point: Paclitaxel-eluting stents did not meet criterion for noninferiority to everolimus-eluting stents in diabetes mellitus patients with CAD who were undergoing PCI in the TUXEDO-India trial.
Major finding: Target vessel failure occurred in 5.6% vs. 2.9% of patients in the paclitaxel- vs. everolimus-eluting stent group (relative risk, 1.89).
Data source: The randomized, multicenter TUXEDO-India trial in 1,830 patients.
Disclosures: The TUXEDO-India trial was supported by Boston Scientific.
Participate in Member Engagement Events at Clinical Congress 2015
When you register for Clinical Congress 2015, make plans to participate in these fun, engaging Member Engagement Events that will complement your educational experience:
ACS Taste of the City
Plan to join American College of Surgeons (ACS) leaders and staff for the free ACS Taste of the City, 5:00─7:00 pm Wednesday, October 7 at McCormick Place, Chicago, IL. This special event will showcase the diversity of Chicago restaurants and will feature music and other entertainment. To encourage a more relaxed environment after a full day of educational programming, participants are encouraged to dress casually and bring friends and family. The shuttle bus schedule will be extended to accommodate your participation in this event and allow family members to join you. Go to the ACS website to learn more about this and other Member Engagement activities at Clinical Congress.
Wake Up with ACS
The College will offer complimentary early morning Yoga and Zumba classes at the Hilton Hotel. Yoga classes will take place 6:00−7:00 am, Monday, October 5, and Zumba, 5:30−6:30 am, October 6. Advance registration is required due to space limitations. These classes are appropriate for all levels, and drinking water, yoga mats, and towels will be provided.
Visit the ACS website at https://www.facs.org/clincon2015/about/whats-new/member-engagement for updates in the coming weeks or contact [email protected] for more details.
When you register for Clinical Congress 2015, make plans to participate in these fun, engaging Member Engagement Events that will complement your educational experience:
ACS Taste of the City
Plan to join American College of Surgeons (ACS) leaders and staff for the free ACS Taste of the City, 5:00─7:00 pm Wednesday, October 7 at McCormick Place, Chicago, IL. This special event will showcase the diversity of Chicago restaurants and will feature music and other entertainment. To encourage a more relaxed environment after a full day of educational programming, participants are encouraged to dress casually and bring friends and family. The shuttle bus schedule will be extended to accommodate your participation in this event and allow family members to join you. Go to the ACS website to learn more about this and other Member Engagement activities at Clinical Congress.
Wake Up with ACS
The College will offer complimentary early morning Yoga and Zumba classes at the Hilton Hotel. Yoga classes will take place 6:00−7:00 am, Monday, October 5, and Zumba, 5:30−6:30 am, October 6. Advance registration is required due to space limitations. These classes are appropriate for all levels, and drinking water, yoga mats, and towels will be provided.
Visit the ACS website at https://www.facs.org/clincon2015/about/whats-new/member-engagement for updates in the coming weeks or contact [email protected] for more details.
When you register for Clinical Congress 2015, make plans to participate in these fun, engaging Member Engagement Events that will complement your educational experience:
ACS Taste of the City
Plan to join American College of Surgeons (ACS) leaders and staff for the free ACS Taste of the City, 5:00─7:00 pm Wednesday, October 7 at McCormick Place, Chicago, IL. This special event will showcase the diversity of Chicago restaurants and will feature music and other entertainment. To encourage a more relaxed environment after a full day of educational programming, participants are encouraged to dress casually and bring friends and family. The shuttle bus schedule will be extended to accommodate your participation in this event and allow family members to join you. Go to the ACS website to learn more about this and other Member Engagement activities at Clinical Congress.
Wake Up with ACS
The College will offer complimentary early morning Yoga and Zumba classes at the Hilton Hotel. Yoga classes will take place 6:00−7:00 am, Monday, October 5, and Zumba, 5:30−6:30 am, October 6. Advance registration is required due to space limitations. These classes are appropriate for all levels, and drinking water, yoga mats, and towels will be provided.
Visit the ACS website at https://www.facs.org/clincon2015/about/whats-new/member-engagement for updates in the coming weeks or contact [email protected] for more details.
Next Director of ACS Convention and Meetings selected
Robert J. Hope joined the American College of Surgeons (ACS) staff August 17 as the next Director of ACS Convention and Meetings. He will officially succeed Felix Niespodziewanski, who will retire in December after 25 years of service to the College. Mr. Hope, who has come on board now to ensure a smooth transition, most recently served as director of housing, registration, and travel services for the Radiological Society of North of America—a position he held for 17 years. Mr. Hope will be working closely with Mr. Niespodziewanski over the next few months to learn more about the ACS and the annual Clinical Congress. In addition, Jackie Mitchell has been promoted to Associate Director of ACS Convention and Meetings. Ms. Mitchell’s many years of experience with planning the Clinical Congress and other ACS events will further ease the change in leadership of ACS Convention and Meetings.
Robert J. Hope joined the American College of Surgeons (ACS) staff August 17 as the next Director of ACS Convention and Meetings. He will officially succeed Felix Niespodziewanski, who will retire in December after 25 years of service to the College. Mr. Hope, who has come on board now to ensure a smooth transition, most recently served as director of housing, registration, and travel services for the Radiological Society of North of America—a position he held for 17 years. Mr. Hope will be working closely with Mr. Niespodziewanski over the next few months to learn more about the ACS and the annual Clinical Congress. In addition, Jackie Mitchell has been promoted to Associate Director of ACS Convention and Meetings. Ms. Mitchell’s many years of experience with planning the Clinical Congress and other ACS events will further ease the change in leadership of ACS Convention and Meetings.
Robert J. Hope joined the American College of Surgeons (ACS) staff August 17 as the next Director of ACS Convention and Meetings. He will officially succeed Felix Niespodziewanski, who will retire in December after 25 years of service to the College. Mr. Hope, who has come on board now to ensure a smooth transition, most recently served as director of housing, registration, and travel services for the Radiological Society of North of America—a position he held for 17 years. Mr. Hope will be working closely with Mr. Niespodziewanski over the next few months to learn more about the ACS and the annual Clinical Congress. In addition, Jackie Mitchell has been promoted to Associate Director of ACS Convention and Meetings. Ms. Mitchell’s many years of experience with planning the Clinical Congress and other ACS events will further ease the change in leadership of ACS Convention and Meetings.
JACS receives highest impact factor to date
The Journal of the American College of Surgeons (JACS) recently learned of its 2014 Thompson-Reuters impact factor for 2014—5.122. This rating represents JACS’ highest impact factor to date and a 15 percent increase in impact from the previous year. JACS now ranks eighth of 198 surgery journals on the Thomson-Reuters list. Timothy J. Eberlein, MD, FACS, the Editor-in-Chief, credits the high impact factor to the dedication and hard work of the editors, staff, and hundreds of peer reviewers.
The impact factor of an academic journal is a measure reflecting the average number of citations to recent articles published in that journal, and is often used to gauge the relevance of a particular journal in its field. Thomson-Reuters ranks, evaluates, and compares journals within subject categories and publishes the results in Journal Citation Reports. The 2014 rating reflects the number of times articles published in a journal in 2012 and 2013 were cited. In other words, JACS papers published in 2012 and 2013 were cited an average of more than five times.
A strong impact factor can help to attract authors looking to publish their research in a journal that provides a maximum amount of exposure. JACS celebrates its position as one of the world’s top surgical journals and is dedicated to publishing high-quality scientific articles and provide surgeons with world-class content in timely and innovative ways.
The Journal of the American College of Surgeons (JACS) recently learned of its 2014 Thompson-Reuters impact factor for 2014—5.122. This rating represents JACS’ highest impact factor to date and a 15 percent increase in impact from the previous year. JACS now ranks eighth of 198 surgery journals on the Thomson-Reuters list. Timothy J. Eberlein, MD, FACS, the Editor-in-Chief, credits the high impact factor to the dedication and hard work of the editors, staff, and hundreds of peer reviewers.
The impact factor of an academic journal is a measure reflecting the average number of citations to recent articles published in that journal, and is often used to gauge the relevance of a particular journal in its field. Thomson-Reuters ranks, evaluates, and compares journals within subject categories and publishes the results in Journal Citation Reports. The 2014 rating reflects the number of times articles published in a journal in 2012 and 2013 were cited. In other words, JACS papers published in 2012 and 2013 were cited an average of more than five times.
A strong impact factor can help to attract authors looking to publish their research in a journal that provides a maximum amount of exposure. JACS celebrates its position as one of the world’s top surgical journals and is dedicated to publishing high-quality scientific articles and provide surgeons with world-class content in timely and innovative ways.
The Journal of the American College of Surgeons (JACS) recently learned of its 2014 Thompson-Reuters impact factor for 2014—5.122. This rating represents JACS’ highest impact factor to date and a 15 percent increase in impact from the previous year. JACS now ranks eighth of 198 surgery journals on the Thomson-Reuters list. Timothy J. Eberlein, MD, FACS, the Editor-in-Chief, credits the high impact factor to the dedication and hard work of the editors, staff, and hundreds of peer reviewers.
The impact factor of an academic journal is a measure reflecting the average number of citations to recent articles published in that journal, and is often used to gauge the relevance of a particular journal in its field. Thomson-Reuters ranks, evaluates, and compares journals within subject categories and publishes the results in Journal Citation Reports. The 2014 rating reflects the number of times articles published in a journal in 2012 and 2013 were cited. In other words, JACS papers published in 2012 and 2013 were cited an average of more than five times.
A strong impact factor can help to attract authors looking to publish their research in a journal that provides a maximum amount of exposure. JACS celebrates its position as one of the world’s top surgical journals and is dedicated to publishing high-quality scientific articles and provide surgeons with world-class content in timely and innovative ways.
Apply by December 1 for 2016 Nizar N. Oweida, MD, FACS, Scholarship
Surgeons who serve small communities are eligible to apply for the 2016 Nizar N. Oweida, MD, FACS, Scholarship of the American College of Surgeons (ACS). Completed applications are due December 15, 2015. The $5,000 Oweida Scholarship subsidizes the attendance of a Fellow or Associate Fellow to the annual ACS Clinical Congress.
This scholarship will help to defray travel expenses for the Clinical Congress, including Postgraduate Course fees, hotel costs, and per diem expenses. The scholar, who will receive preferential housing close to the Clinical Congress site, will be expected to make his or her own travel arrangements.
Basic Requirements
Oweida Scholarship applicants must meet the following requirements:
• Serves a small town or rural community in the U.S. or Canada
• Is a Fellow or Associate Fellow in good standing
• Is younger than 55 years of age on the date the application is filed
Activities
The Oweida Scholar will attend the ACS Clinical Congress 2016 in Washington, DC, October 16–20. At the annual meeting of the Scholarships Committee and the Rural Surgeons Forum, the scholar will meet with colleagues and receive the scholarship check.
The Executive Committee of the Board of Governors will select the scholar. Oweida Scholarship applicants should submit a single PDF consisting of the following items in this order:
• A one-page essay, discussing the following specific items:
• Why the applicant wants to receive the Oweida Scholarship
• Why the applicant believes he or she is qualified to receive the scholarship
• Why the applicant characterizes his or her practice as serving a small community
• One copy of the applicant’s current curriculum vitae
A scholar and an alternate will be selected, and all applicants will be notified of the outcome of the selection process by February 1, 2016.
The Oweida Scholar must attend the full week of the Clinical Congress in the year for which the award is designated; use of scholarship may not be postponed. The Oweida Scholar will provide a brief report on his or her experiences at the Clinical Congress for possible future publication in the Bulletin of the American College of Surgeons. The scholar also must submit a simple accounting for the award. These items will be due December 1, 2016.
Send applications for this scholarship to Kate Early, Scholarships Administrator, at [email protected], or mail to: Scholarships Sections, ACS, 633 N. Saint Clair St., Chicago, IL 60611-3211.
For more information, contact Ms. Early at 312-202-5281.
Surgeons who serve small communities are eligible to apply for the 2016 Nizar N. Oweida, MD, FACS, Scholarship of the American College of Surgeons (ACS). Completed applications are due December 15, 2015. The $5,000 Oweida Scholarship subsidizes the attendance of a Fellow or Associate Fellow to the annual ACS Clinical Congress.
This scholarship will help to defray travel expenses for the Clinical Congress, including Postgraduate Course fees, hotel costs, and per diem expenses. The scholar, who will receive preferential housing close to the Clinical Congress site, will be expected to make his or her own travel arrangements.
Basic Requirements
Oweida Scholarship applicants must meet the following requirements:
• Serves a small town or rural community in the U.S. or Canada
• Is a Fellow or Associate Fellow in good standing
• Is younger than 55 years of age on the date the application is filed
Activities
The Oweida Scholar will attend the ACS Clinical Congress 2016 in Washington, DC, October 16–20. At the annual meeting of the Scholarships Committee and the Rural Surgeons Forum, the scholar will meet with colleagues and receive the scholarship check.
The Executive Committee of the Board of Governors will select the scholar. Oweida Scholarship applicants should submit a single PDF consisting of the following items in this order:
• A one-page essay, discussing the following specific items:
• Why the applicant wants to receive the Oweida Scholarship
• Why the applicant believes he or she is qualified to receive the scholarship
• Why the applicant characterizes his or her practice as serving a small community
• One copy of the applicant’s current curriculum vitae
A scholar and an alternate will be selected, and all applicants will be notified of the outcome of the selection process by February 1, 2016.
The Oweida Scholar must attend the full week of the Clinical Congress in the year for which the award is designated; use of scholarship may not be postponed. The Oweida Scholar will provide a brief report on his or her experiences at the Clinical Congress for possible future publication in the Bulletin of the American College of Surgeons. The scholar also must submit a simple accounting for the award. These items will be due December 1, 2016.
Send applications for this scholarship to Kate Early, Scholarships Administrator, at [email protected], or mail to: Scholarships Sections, ACS, 633 N. Saint Clair St., Chicago, IL 60611-3211.
For more information, contact Ms. Early at 312-202-5281.
Surgeons who serve small communities are eligible to apply for the 2016 Nizar N. Oweida, MD, FACS, Scholarship of the American College of Surgeons (ACS). Completed applications are due December 15, 2015. The $5,000 Oweida Scholarship subsidizes the attendance of a Fellow or Associate Fellow to the annual ACS Clinical Congress.
This scholarship will help to defray travel expenses for the Clinical Congress, including Postgraduate Course fees, hotel costs, and per diem expenses. The scholar, who will receive preferential housing close to the Clinical Congress site, will be expected to make his or her own travel arrangements.
Basic Requirements
Oweida Scholarship applicants must meet the following requirements:
• Serves a small town or rural community in the U.S. or Canada
• Is a Fellow or Associate Fellow in good standing
• Is younger than 55 years of age on the date the application is filed
Activities
The Oweida Scholar will attend the ACS Clinical Congress 2016 in Washington, DC, October 16–20. At the annual meeting of the Scholarships Committee and the Rural Surgeons Forum, the scholar will meet with colleagues and receive the scholarship check.
The Executive Committee of the Board of Governors will select the scholar. Oweida Scholarship applicants should submit a single PDF consisting of the following items in this order:
• A one-page essay, discussing the following specific items:
• Why the applicant wants to receive the Oweida Scholarship
• Why the applicant believes he or she is qualified to receive the scholarship
• Why the applicant characterizes his or her practice as serving a small community
• One copy of the applicant’s current curriculum vitae
A scholar and an alternate will be selected, and all applicants will be notified of the outcome of the selection process by February 1, 2016.
The Oweida Scholar must attend the full week of the Clinical Congress in the year for which the award is designated; use of scholarship may not be postponed. The Oweida Scholar will provide a brief report on his or her experiences at the Clinical Congress for possible future publication in the Bulletin of the American College of Surgeons. The scholar also must submit a simple accounting for the award. These items will be due December 1, 2016.
Send applications for this scholarship to Kate Early, Scholarships Administrator, at [email protected], or mail to: Scholarships Sections, ACS, 633 N. Saint Clair St., Chicago, IL 60611-3211.
For more information, contact Ms. Early at 312-202-5281.
Register by November 2 for annual ACS-AEI Postgraduate Course
The 8th Annual American College of Surgeons-Accredited Education Institute (ACS-AEI) Postgraduate Course, November 13–14 at the department of surgery, Stanford School of Medicine, Palo Alto, CA, will focus on Surgical Education: Expanding Definitions of Simulation. Learn more about the course at https://www.facs.org/education/accreditation/aei/pgcourse.
On the first day, course attendees will learn how to better assess technical skills and how to conduct in situ simulation (simulation that takes place in the actual work environment). They also will learn how simulation is incorporated into credentialing and certification. They then will review issues of faculty and resident wellness, covering such concerns as physician burnout and life balance. The second day of the course will feature interactive games and a hands-on workshop on simulation-based inter-professional education. The session will conclude with a “scavenger hunt” of Stanford’s simulation centers and skills laboratories, giving participants a unique behind-the-scenes view of a pioneer in simulation-based learning.
In addition, participants will have ample opportunities to network with other AEI representatives as well as ACS-AEI program staff. The ACS-AEIs educate and train practicing surgeons, surgical residents, medical students, and members of the surgical team using simulation-based education.
For more information and to reserve your course attendance, visit the ACS website at https://www.facs.org/education/accreditation/aei/pgcourse. For additional information, contact Cathy Wojcik at [email protected].
The 8th Annual American College of Surgeons-Accredited Education Institute (ACS-AEI) Postgraduate Course, November 13–14 at the department of surgery, Stanford School of Medicine, Palo Alto, CA, will focus on Surgical Education: Expanding Definitions of Simulation. Learn more about the course at https://www.facs.org/education/accreditation/aei/pgcourse.
On the first day, course attendees will learn how to better assess technical skills and how to conduct in situ simulation (simulation that takes place in the actual work environment). They also will learn how simulation is incorporated into credentialing and certification. They then will review issues of faculty and resident wellness, covering such concerns as physician burnout and life balance. The second day of the course will feature interactive games and a hands-on workshop on simulation-based inter-professional education. The session will conclude with a “scavenger hunt” of Stanford’s simulation centers and skills laboratories, giving participants a unique behind-the-scenes view of a pioneer in simulation-based learning.
In addition, participants will have ample opportunities to network with other AEI representatives as well as ACS-AEI program staff. The ACS-AEIs educate and train practicing surgeons, surgical residents, medical students, and members of the surgical team using simulation-based education.
For more information and to reserve your course attendance, visit the ACS website at https://www.facs.org/education/accreditation/aei/pgcourse. For additional information, contact Cathy Wojcik at [email protected].
The 8th Annual American College of Surgeons-Accredited Education Institute (ACS-AEI) Postgraduate Course, November 13–14 at the department of surgery, Stanford School of Medicine, Palo Alto, CA, will focus on Surgical Education: Expanding Definitions of Simulation. Learn more about the course at https://www.facs.org/education/accreditation/aei/pgcourse.
On the first day, course attendees will learn how to better assess technical skills and how to conduct in situ simulation (simulation that takes place in the actual work environment). They also will learn how simulation is incorporated into credentialing and certification. They then will review issues of faculty and resident wellness, covering such concerns as physician burnout and life balance. The second day of the course will feature interactive games and a hands-on workshop on simulation-based inter-professional education. The session will conclude with a “scavenger hunt” of Stanford’s simulation centers and skills laboratories, giving participants a unique behind-the-scenes view of a pioneer in simulation-based learning.
In addition, participants will have ample opportunities to network with other AEI representatives as well as ACS-AEI program staff. The ACS-AEIs educate and train practicing surgeons, surgical residents, medical students, and members of the surgical team using simulation-based education.
For more information and to reserve your course attendance, visit the ACS website at https://www.facs.org/education/accreditation/aei/pgcourse. For additional information, contact Cathy Wojcik at [email protected].
Applications now being accepted for 2016-2018 Faculty Research Fellowships honoring ACS leaders
The American College of Surgeons (ACS) is offering two-year faculty research fellowships for surgeons entering academic careers in surgery or a surgical specialty. These 2016−2018 fellowships are supported through the generosity of Fellows, Chapters, and friends of the College. The closing date for receipt of completed applications and all supporting documents is November 2, 2015.
All of the fellowships are intended to assist a surgeon in the establishment of a new and independent research program. Applicants should have demonstrated their potential to work as independent investigators. The fellowship award is $40,000 per year for each of two years, to support the research.
There are five ACS Faculty Research Fellowships now available, and three of them have been established to honor an ACS leader:
• The Franklin H. Martin, MD, FACS, Faculty Research Fellowship of the American College of Surgeons, which honors the founder of the ACS
• The C. James Carrico, MD, FACS, Faculty Research Fellowship for the Study of Trauma and Critical Care
• The Thomas R. Russell, MD, FACS, Faculty Research Fellowship, which is designated to support research aimed at improving surgical outcomes
General guidelines
General policies covering the granting of the ACS Faculty Research Fellowships include the following:
• The fellowships are open to Fellows or Associate Fellows of the College who have: (1) completed the chief residency year or accredited fellowship training within the preceding five years; and (2) received a full-time faculty appointment in a department of surgery or a surgical specialty at a medical school accredited by the Liaison Committee on Medical Education in the U.S. or by the Committee for Accreditation of Canadian Medical Schools in Canada. Applicants who directly enter academic surgery following residency or fellowship will receive preference.
• Recipients may use the award to support their research or academic enrichment in any way deemed maximally supportive of their investigations. Each fellowship grant must support the research of the recipient and is not intended to diminish or replace the usual, expected compensation or benefits. Indirect costs are not paid to a recipient or to a recipient’s institution.
• Applications for these fellowships may be submitted even if comparable applications have been made to organizations such as the National Institutes of Health (NIH) or industry sources. If a recipient is offered a scholarship, fellowship, or research career development award from such an agency or organization, that individual is responsible for contacting the College’s Scholarships Administrator to request approval of the additional award.
• The Scholarship Committee reserves the right to review potentially overlapping awards and adjust its award accordingly.
• The College encourages each applicant to leverage the funds provided through one of these fellowships with time and monies provided by the applicant’s department. Formal statements of matching funds and time from the applicant’s department will promote favorable review by the College.
• Supporting letters from the head of the department of surgery (or the surgical specialty) and from the mentor supervising an applicant’s research effort must be submitted. This approval would involve a commitment to continuation of the academic position and the provision of research facilities. Only in exceptional circumstances will more than one fellowship be granted in a single year to applicants from the same institution.
• Each applicant must submit a research plan and budget for the two-year period of the respective fellowship, even though renewed approval by the Scholarships Committee of the College is required for the second year.
• A minimum of 50 percent of a Fellow’s time must be spent conducting the research proposed in the application. This percentage may run concurrently with the time requirements of NIH or other accepted funding.
• Faculty Research Fellows are expected to attend the ACS Clinical Congress in 2018 to present a report at the Surgical Forum and to receive a certificate at the annual meeting of the Scholarships Committee.
Application forms may be obtained from the College’s website: www.facs.org, or upon request from the Scholarships Administrator, at [email protected].
The American College of Surgeons (ACS) is offering two-year faculty research fellowships for surgeons entering academic careers in surgery or a surgical specialty. These 2016−2018 fellowships are supported through the generosity of Fellows, Chapters, and friends of the College. The closing date for receipt of completed applications and all supporting documents is November 2, 2015.
All of the fellowships are intended to assist a surgeon in the establishment of a new and independent research program. Applicants should have demonstrated their potential to work as independent investigators. The fellowship award is $40,000 per year for each of two years, to support the research.
There are five ACS Faculty Research Fellowships now available, and three of them have been established to honor an ACS leader:
• The Franklin H. Martin, MD, FACS, Faculty Research Fellowship of the American College of Surgeons, which honors the founder of the ACS
• The C. James Carrico, MD, FACS, Faculty Research Fellowship for the Study of Trauma and Critical Care
• The Thomas R. Russell, MD, FACS, Faculty Research Fellowship, which is designated to support research aimed at improving surgical outcomes
General guidelines
General policies covering the granting of the ACS Faculty Research Fellowships include the following:
• The fellowships are open to Fellows or Associate Fellows of the College who have: (1) completed the chief residency year or accredited fellowship training within the preceding five years; and (2) received a full-time faculty appointment in a department of surgery or a surgical specialty at a medical school accredited by the Liaison Committee on Medical Education in the U.S. or by the Committee for Accreditation of Canadian Medical Schools in Canada. Applicants who directly enter academic surgery following residency or fellowship will receive preference.
• Recipients may use the award to support their research or academic enrichment in any way deemed maximally supportive of their investigations. Each fellowship grant must support the research of the recipient and is not intended to diminish or replace the usual, expected compensation or benefits. Indirect costs are not paid to a recipient or to a recipient’s institution.
• Applications for these fellowships may be submitted even if comparable applications have been made to organizations such as the National Institutes of Health (NIH) or industry sources. If a recipient is offered a scholarship, fellowship, or research career development award from such an agency or organization, that individual is responsible for contacting the College’s Scholarships Administrator to request approval of the additional award.
• The Scholarship Committee reserves the right to review potentially overlapping awards and adjust its award accordingly.
• The College encourages each applicant to leverage the funds provided through one of these fellowships with time and monies provided by the applicant’s department. Formal statements of matching funds and time from the applicant’s department will promote favorable review by the College.
• Supporting letters from the head of the department of surgery (or the surgical specialty) and from the mentor supervising an applicant’s research effort must be submitted. This approval would involve a commitment to continuation of the academic position and the provision of research facilities. Only in exceptional circumstances will more than one fellowship be granted in a single year to applicants from the same institution.
• Each applicant must submit a research plan and budget for the two-year period of the respective fellowship, even though renewed approval by the Scholarships Committee of the College is required for the second year.
• A minimum of 50 percent of a Fellow’s time must be spent conducting the research proposed in the application. This percentage may run concurrently with the time requirements of NIH or other accepted funding.
• Faculty Research Fellows are expected to attend the ACS Clinical Congress in 2018 to present a report at the Surgical Forum and to receive a certificate at the annual meeting of the Scholarships Committee.
Application forms may be obtained from the College’s website: www.facs.org, or upon request from the Scholarships Administrator, at [email protected].
The American College of Surgeons (ACS) is offering two-year faculty research fellowships for surgeons entering academic careers in surgery or a surgical specialty. These 2016−2018 fellowships are supported through the generosity of Fellows, Chapters, and friends of the College. The closing date for receipt of completed applications and all supporting documents is November 2, 2015.
All of the fellowships are intended to assist a surgeon in the establishment of a new and independent research program. Applicants should have demonstrated their potential to work as independent investigators. The fellowship award is $40,000 per year for each of two years, to support the research.
There are five ACS Faculty Research Fellowships now available, and three of them have been established to honor an ACS leader:
• The Franklin H. Martin, MD, FACS, Faculty Research Fellowship of the American College of Surgeons, which honors the founder of the ACS
• The C. James Carrico, MD, FACS, Faculty Research Fellowship for the Study of Trauma and Critical Care
• The Thomas R. Russell, MD, FACS, Faculty Research Fellowship, which is designated to support research aimed at improving surgical outcomes
General guidelines
General policies covering the granting of the ACS Faculty Research Fellowships include the following:
• The fellowships are open to Fellows or Associate Fellows of the College who have: (1) completed the chief residency year or accredited fellowship training within the preceding five years; and (2) received a full-time faculty appointment in a department of surgery or a surgical specialty at a medical school accredited by the Liaison Committee on Medical Education in the U.S. or by the Committee for Accreditation of Canadian Medical Schools in Canada. Applicants who directly enter academic surgery following residency or fellowship will receive preference.
• Recipients may use the award to support their research or academic enrichment in any way deemed maximally supportive of their investigations. Each fellowship grant must support the research of the recipient and is not intended to diminish or replace the usual, expected compensation or benefits. Indirect costs are not paid to a recipient or to a recipient’s institution.
• Applications for these fellowships may be submitted even if comparable applications have been made to organizations such as the National Institutes of Health (NIH) or industry sources. If a recipient is offered a scholarship, fellowship, or research career development award from such an agency or organization, that individual is responsible for contacting the College’s Scholarships Administrator to request approval of the additional award.
• The Scholarship Committee reserves the right to review potentially overlapping awards and adjust its award accordingly.
• The College encourages each applicant to leverage the funds provided through one of these fellowships with time and monies provided by the applicant’s department. Formal statements of matching funds and time from the applicant’s department will promote favorable review by the College.
• Supporting letters from the head of the department of surgery (or the surgical specialty) and from the mentor supervising an applicant’s research effort must be submitted. This approval would involve a commitment to continuation of the academic position and the provision of research facilities. Only in exceptional circumstances will more than one fellowship be granted in a single year to applicants from the same institution.
• Each applicant must submit a research plan and budget for the two-year period of the respective fellowship, even though renewed approval by the Scholarships Committee of the College is required for the second year.
• A minimum of 50 percent of a Fellow’s time must be spent conducting the research proposed in the application. This percentage may run concurrently with the time requirements of NIH or other accepted funding.
• Faculty Research Fellows are expected to attend the ACS Clinical Congress in 2018 to present a report at the Surgical Forum and to receive a certificate at the annual meeting of the Scholarships Committee.
Application forms may be obtained from the College’s website: www.facs.org, or upon request from the Scholarships Administrator, at [email protected].
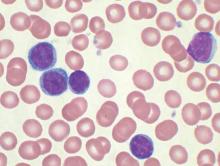
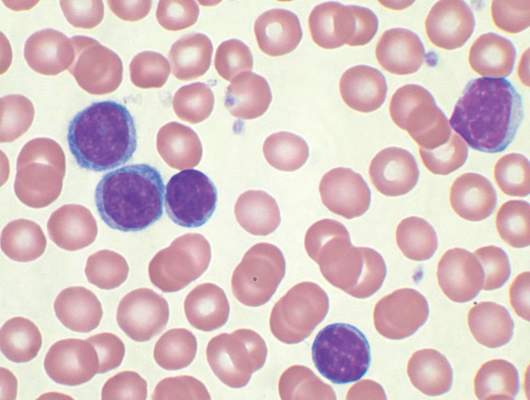
No evidence for CLL transmission via blood transfusion
Analysis of data from blood transfusions that took place in Sweden and Denmark over a 30-year period showed no indication that chronic lymphocytic leukemia (CLL) risk is higher among recipients of blood from donors who subsequently developed CLL, according to researchers.
The study compared 7,413 recipients of blood from 796 donors who subsequently developed CLL (exposed group), with 80,431 recipients from 7,477 donors free of CLL (unexposed group). In total, 12 recipients in the exposed group and 107 in the unexposed group were later diagnosed with CLL, for an incidence rate ratio of 0.94 (95% confidence interval, 0.52-1.71). When defining “exposed” as receiving blood less than 10 years before donor CLL diagnosis, the incidence rate ratio was 0.46 (95% CI, 0.12-1.85).
“The analyses provided little evidence that donor MBL [monoclonal B-cell lymphocytosis]/CLL transmission in blood products influences recipient CLL risk,” wrote Dr. Henrik Hjalgrim of the department of epidemiology research at Statens Serum Institut, Copenhagen, and his colleagues (Blood 2015 doi: 10.1182/blood-2015-03-632844).
MBL is fairly common in healthy individuals (estimated at 7.1% in a study of American blood donors aged 45-91 years) and may progress to CLL at various rates depending on the MBL cell count. Results from previous studies investigating the association between transfusion and risk of CLL or small lymphocytic lymphoma have been mixed, they noted.
Using a retrospective approach, Dr. Hjalgrim and his associates first identified donors subsequently diagnosed with CLL, then identified control donors free from CLL who were matched for age, sex, county, number of donations, and blood type.
In case MBL may have progressed in the recipient but not the donor, investigators also examined whether CLL clustered among recipients from an individual donor, regardless of donor CLL status, but found no such clusters.
Limiting the analysis was the lack of donor MBL status, for which postdonation CLL diagnosis substituted. Some recipients in the exposed group may have received blood drawn before the donor developed MBL.
Dr. Hjalgrim and his coauthors reported having no disclosures.
Analysis of data from blood transfusions that took place in Sweden and Denmark over a 30-year period showed no indication that chronic lymphocytic leukemia (CLL) risk is higher among recipients of blood from donors who subsequently developed CLL, according to researchers.
The study compared 7,413 recipients of blood from 796 donors who subsequently developed CLL (exposed group), with 80,431 recipients from 7,477 donors free of CLL (unexposed group). In total, 12 recipients in the exposed group and 107 in the unexposed group were later diagnosed with CLL, for an incidence rate ratio of 0.94 (95% confidence interval, 0.52-1.71). When defining “exposed” as receiving blood less than 10 years before donor CLL diagnosis, the incidence rate ratio was 0.46 (95% CI, 0.12-1.85).
“The analyses provided little evidence that donor MBL [monoclonal B-cell lymphocytosis]/CLL transmission in blood products influences recipient CLL risk,” wrote Dr. Henrik Hjalgrim of the department of epidemiology research at Statens Serum Institut, Copenhagen, and his colleagues (Blood 2015 doi: 10.1182/blood-2015-03-632844).
MBL is fairly common in healthy individuals (estimated at 7.1% in a study of American blood donors aged 45-91 years) and may progress to CLL at various rates depending on the MBL cell count. Results from previous studies investigating the association between transfusion and risk of CLL or small lymphocytic lymphoma have been mixed, they noted.
Using a retrospective approach, Dr. Hjalgrim and his associates first identified donors subsequently diagnosed with CLL, then identified control donors free from CLL who were matched for age, sex, county, number of donations, and blood type.
In case MBL may have progressed in the recipient but not the donor, investigators also examined whether CLL clustered among recipients from an individual donor, regardless of donor CLL status, but found no such clusters.
Limiting the analysis was the lack of donor MBL status, for which postdonation CLL diagnosis substituted. Some recipients in the exposed group may have received blood drawn before the donor developed MBL.
Dr. Hjalgrim and his coauthors reported having no disclosures.
Analysis of data from blood transfusions that took place in Sweden and Denmark over a 30-year period showed no indication that chronic lymphocytic leukemia (CLL) risk is higher among recipients of blood from donors who subsequently developed CLL, according to researchers.
The study compared 7,413 recipients of blood from 796 donors who subsequently developed CLL (exposed group), with 80,431 recipients from 7,477 donors free of CLL (unexposed group). In total, 12 recipients in the exposed group and 107 in the unexposed group were later diagnosed with CLL, for an incidence rate ratio of 0.94 (95% confidence interval, 0.52-1.71). When defining “exposed” as receiving blood less than 10 years before donor CLL diagnosis, the incidence rate ratio was 0.46 (95% CI, 0.12-1.85).
“The analyses provided little evidence that donor MBL [monoclonal B-cell lymphocytosis]/CLL transmission in blood products influences recipient CLL risk,” wrote Dr. Henrik Hjalgrim of the department of epidemiology research at Statens Serum Institut, Copenhagen, and his colleagues (Blood 2015 doi: 10.1182/blood-2015-03-632844).
MBL is fairly common in healthy individuals (estimated at 7.1% in a study of American blood donors aged 45-91 years) and may progress to CLL at various rates depending on the MBL cell count. Results from previous studies investigating the association between transfusion and risk of CLL or small lymphocytic lymphoma have been mixed, they noted.
Using a retrospective approach, Dr. Hjalgrim and his associates first identified donors subsequently diagnosed with CLL, then identified control donors free from CLL who were matched for age, sex, county, number of donations, and blood type.
In case MBL may have progressed in the recipient but not the donor, investigators also examined whether CLL clustered among recipients from an individual donor, regardless of donor CLL status, but found no such clusters.
Limiting the analysis was the lack of donor MBL status, for which postdonation CLL diagnosis substituted. Some recipients in the exposed group may have received blood drawn before the donor developed MBL.
Dr. Hjalgrim and his coauthors reported having no disclosures.
FROM BLOOD
Key clinical point: There is no evidence for higher risk of chronic lymphocytic leukemia (CLL) among recipients of blood products from donors who subsequently were diagnosed with CLL.
Major finding: Among exposed recipients (7,413 who received blood from 796 donors who subsequently developed CLL), 12 were diagnosed with CLL. Among unexposed recipients (80,431 who received blood from 7,477 donors free of CLL), 107 were diagnosed with CLL, for an incidence rate ratio of 0.94 (95% CI, 0.52-1.71).
Data source: The Scandinavian Donations and Transfusions (SCANDAT2) database comprises information, including donor and recipient health outcomes, for more than 20 million blood products handled by blood banks from 1968 to 2010.
Disclosures: Dr. Hjalgrim and his coauthors reported having no disclosures.
Joseph P. Vacanti, MD, FACS, receives 2015 Jacobson Innovation Award
Joseph P. Vacanti, MD, FACS, received the 2015 Jacobson Innovation Award of the American College of Surgeons (ACS) at a dinner on June 5 at the John B. Murphy Memorial Auditorium in Chicago, IL. Dr. Vacanti is the John Homans Professor of Surgery at Harvard Medical School and is the director of the Laboratory for Tissue Engineering and Organ Fabrication, co-director of the Center for Regenerative Medicine, and chief of pediatric transplantation at Massachusetts General Hospital, Boston.
The prestigious Jacobson Innovation Award honors living surgeons who have been innovators of a new development or technique in any field of surgery and is made possible through a gift from Julius H. Jacobson II, MD, FACS, and his wife, Joan. Dr. Jacobson is a general vascular surgeon known for his pioneering work in microsurgery.
Honored for tissue engineering
This year’s Jacobson Innovation Award honors Dr. Vacanti for his work in the field of tissue engineering, which began in the early 1980s and stemmed from a long-held interest in addressing organ shortages. Working with Robert Langer, ScD, the David H. Koch Institute Professor at the Massachusetts Institute of Technology, Cambridge, Dr. Vacanti developed an approach using tissue-specific cells placed in scaffolds made of biodegradable polymers. The cells, derived from both living tissue or stem cells, are then bathed in growth factors and proceed to multiply, filling the scaffold. The cells then grow into three-dimensional tissue that, once implanted in the body, recreates its proper tissue function. Blood vessels grow into the new tissue, the scaffold degrades, and the lab-grown tissue becomes indistinguishable from its surroundings.
Dr. Vacanti also has been an innovator in pediatric surgery. In 1984, while at Children’s Hospital Boston, Dr. Vacanti instituted New England’s first successful pediatric extracorporeal membrane oxygenation program. In addition, he started the nation’s first liver transplantation program specifically for the pediatric population.
Dr. Vacanti was a founding co-president of the Tissue Engineering Society, now the Tissue Engineering Regenerative Medicine International Society (TERMIS) and which boasts 5,000 active members from 80 countries worldwide. He was also the founding senior editor of the journal Tissue Engineering, which serves the members of TERMIS. The journal can be found in 1,700 libraries in 20 countries and is provided free online to 106 developing countries.
Dr. Vacanti has authored more than 320 original reports, 69 book chapters, 54 reviews, and 473 abstracts. He has 81 patents or patents pending in the U.S., Canada, Europe, and Japan.
“As I stand here tonight, I ask myself: ‘How did a Sicilian-American kid from Omaha, Nebraska, end up on this podium?’” Dr. Vacanti said to the approximately 100 guests at the dinner. “My answer is my family, my friends, and my heroes. Just like everyone in this room, we are descendants of immigrants. In my case, my grandparents emigrated from Sicily because of poverty and lack of opportunity. My grandfather could barely speak English but fought in the trenches in France in World War I and gained his American citizenship. He then worked in the boiler shops of the Union Pacific Railroad and taught me the value of hard work, but also the value of using my mind to obtain an education. My father was a professor of oral surgery and endodontics at Creighton University’s dental school, and my mother was a premedical student before marrying my father after World War II. It was that influence that led me to want to become a surgeon at the young age of four.”
Dr. Vacanti also paid tribute to the mentors who encouraged his growth as a surgeon as well as those individuals who have inspired and supported him throughout his career. “My surgical heroes and mentors are Dr. William Hardy Hendren III [MD, FACS, FRCSI(Hon), FRCSEng(Hon), FRCSGlas(Hon)] and Dr. Judah Folkman [MD, FACS], both previous Jacobson Award recipients. Both taught me about surgical innovation and how to think about a problem and its definitive solution,” he said. “Dr. Folkman advised me that if I was going to devote my life to something that I should pick something important. My closest friend, Mr. Walter Smith, has been very important in advising me through the years on many matters both personal and professional, and Dr. Robert Langer [MD, FACS] has been a partner and friend in all of this work through many years.”
Recipient of numerous awards
Dr. Vacanti has received numerous honors and awards. In 2001, he was elected to the Institute of Medicine of the National Academy of Sciences. In 2007, the Board of Directors of City Trusts, acting for the city of Philadelphia, presented him the John Scott Award, which is given to the most deserving men and women whose inventions have contributed significantly to the comfort, welfare, and happiness of human beings. The award has been given in memory of Benjamin Franklin since 1822, and previous recipients include Madame Marie Curie, Orville and Wilbur Wright, Thomas Edison, and Jonas Salk, MD.
Dr. Vacanti became a 2011 Thomson Reuters Citation Laureate in the field of physiology or medicine. Thomson Reuters Citation Laureates are an elite group of highly cited, high-impact researchers, who are likely contenders for other awards in the future, including the Nobel Prize.
Dr. Vacanti also received the William E. Ladd Medal in 2013, which is the highest honor awarded by the surgical section of the American Academy of Pediatrics and considered by many to be the most prestigious award in the field of pediatric surgery.
Joseph P. Vacanti, MD, FACS, received the 2015 Jacobson Innovation Award of the American College of Surgeons (ACS) at a dinner on June 5 at the John B. Murphy Memorial Auditorium in Chicago, IL. Dr. Vacanti is the John Homans Professor of Surgery at Harvard Medical School and is the director of the Laboratory for Tissue Engineering and Organ Fabrication, co-director of the Center for Regenerative Medicine, and chief of pediatric transplantation at Massachusetts General Hospital, Boston.
The prestigious Jacobson Innovation Award honors living surgeons who have been innovators of a new development or technique in any field of surgery and is made possible through a gift from Julius H. Jacobson II, MD, FACS, and his wife, Joan. Dr. Jacobson is a general vascular surgeon known for his pioneering work in microsurgery.
Honored for tissue engineering
This year’s Jacobson Innovation Award honors Dr. Vacanti for his work in the field of tissue engineering, which began in the early 1980s and stemmed from a long-held interest in addressing organ shortages. Working with Robert Langer, ScD, the David H. Koch Institute Professor at the Massachusetts Institute of Technology, Cambridge, Dr. Vacanti developed an approach using tissue-specific cells placed in scaffolds made of biodegradable polymers. The cells, derived from both living tissue or stem cells, are then bathed in growth factors and proceed to multiply, filling the scaffold. The cells then grow into three-dimensional tissue that, once implanted in the body, recreates its proper tissue function. Blood vessels grow into the new tissue, the scaffold degrades, and the lab-grown tissue becomes indistinguishable from its surroundings.
Dr. Vacanti also has been an innovator in pediatric surgery. In 1984, while at Children’s Hospital Boston, Dr. Vacanti instituted New England’s first successful pediatric extracorporeal membrane oxygenation program. In addition, he started the nation’s first liver transplantation program specifically for the pediatric population.
Dr. Vacanti was a founding co-president of the Tissue Engineering Society, now the Tissue Engineering Regenerative Medicine International Society (TERMIS) and which boasts 5,000 active members from 80 countries worldwide. He was also the founding senior editor of the journal Tissue Engineering, which serves the members of TERMIS. The journal can be found in 1,700 libraries in 20 countries and is provided free online to 106 developing countries.
Dr. Vacanti has authored more than 320 original reports, 69 book chapters, 54 reviews, and 473 abstracts. He has 81 patents or patents pending in the U.S., Canada, Europe, and Japan.
“As I stand here tonight, I ask myself: ‘How did a Sicilian-American kid from Omaha, Nebraska, end up on this podium?’” Dr. Vacanti said to the approximately 100 guests at the dinner. “My answer is my family, my friends, and my heroes. Just like everyone in this room, we are descendants of immigrants. In my case, my grandparents emigrated from Sicily because of poverty and lack of opportunity. My grandfather could barely speak English but fought in the trenches in France in World War I and gained his American citizenship. He then worked in the boiler shops of the Union Pacific Railroad and taught me the value of hard work, but also the value of using my mind to obtain an education. My father was a professor of oral surgery and endodontics at Creighton University’s dental school, and my mother was a premedical student before marrying my father after World War II. It was that influence that led me to want to become a surgeon at the young age of four.”
Dr. Vacanti also paid tribute to the mentors who encouraged his growth as a surgeon as well as those individuals who have inspired and supported him throughout his career. “My surgical heroes and mentors are Dr. William Hardy Hendren III [MD, FACS, FRCSI(Hon), FRCSEng(Hon), FRCSGlas(Hon)] and Dr. Judah Folkman [MD, FACS], both previous Jacobson Award recipients. Both taught me about surgical innovation and how to think about a problem and its definitive solution,” he said. “Dr. Folkman advised me that if I was going to devote my life to something that I should pick something important. My closest friend, Mr. Walter Smith, has been very important in advising me through the years on many matters both personal and professional, and Dr. Robert Langer [MD, FACS] has been a partner and friend in all of this work through many years.”
Recipient of numerous awards
Dr. Vacanti has received numerous honors and awards. In 2001, he was elected to the Institute of Medicine of the National Academy of Sciences. In 2007, the Board of Directors of City Trusts, acting for the city of Philadelphia, presented him the John Scott Award, which is given to the most deserving men and women whose inventions have contributed significantly to the comfort, welfare, and happiness of human beings. The award has been given in memory of Benjamin Franklin since 1822, and previous recipients include Madame Marie Curie, Orville and Wilbur Wright, Thomas Edison, and Jonas Salk, MD.
Dr. Vacanti became a 2011 Thomson Reuters Citation Laureate in the field of physiology or medicine. Thomson Reuters Citation Laureates are an elite group of highly cited, high-impact researchers, who are likely contenders for other awards in the future, including the Nobel Prize.
Dr. Vacanti also received the William E. Ladd Medal in 2013, which is the highest honor awarded by the surgical section of the American Academy of Pediatrics and considered by many to be the most prestigious award in the field of pediatric surgery.
Joseph P. Vacanti, MD, FACS, received the 2015 Jacobson Innovation Award of the American College of Surgeons (ACS) at a dinner on June 5 at the John B. Murphy Memorial Auditorium in Chicago, IL. Dr. Vacanti is the John Homans Professor of Surgery at Harvard Medical School and is the director of the Laboratory for Tissue Engineering and Organ Fabrication, co-director of the Center for Regenerative Medicine, and chief of pediatric transplantation at Massachusetts General Hospital, Boston.
The prestigious Jacobson Innovation Award honors living surgeons who have been innovators of a new development or technique in any field of surgery and is made possible through a gift from Julius H. Jacobson II, MD, FACS, and his wife, Joan. Dr. Jacobson is a general vascular surgeon known for his pioneering work in microsurgery.
Honored for tissue engineering
This year’s Jacobson Innovation Award honors Dr. Vacanti for his work in the field of tissue engineering, which began in the early 1980s and stemmed from a long-held interest in addressing organ shortages. Working with Robert Langer, ScD, the David H. Koch Institute Professor at the Massachusetts Institute of Technology, Cambridge, Dr. Vacanti developed an approach using tissue-specific cells placed in scaffolds made of biodegradable polymers. The cells, derived from both living tissue or stem cells, are then bathed in growth factors and proceed to multiply, filling the scaffold. The cells then grow into three-dimensional tissue that, once implanted in the body, recreates its proper tissue function. Blood vessels grow into the new tissue, the scaffold degrades, and the lab-grown tissue becomes indistinguishable from its surroundings.
Dr. Vacanti also has been an innovator in pediatric surgery. In 1984, while at Children’s Hospital Boston, Dr. Vacanti instituted New England’s first successful pediatric extracorporeal membrane oxygenation program. In addition, he started the nation’s first liver transplantation program specifically for the pediatric population.
Dr. Vacanti was a founding co-president of the Tissue Engineering Society, now the Tissue Engineering Regenerative Medicine International Society (TERMIS) and which boasts 5,000 active members from 80 countries worldwide. He was also the founding senior editor of the journal Tissue Engineering, which serves the members of TERMIS. The journal can be found in 1,700 libraries in 20 countries and is provided free online to 106 developing countries.
Dr. Vacanti has authored more than 320 original reports, 69 book chapters, 54 reviews, and 473 abstracts. He has 81 patents or patents pending in the U.S., Canada, Europe, and Japan.
“As I stand here tonight, I ask myself: ‘How did a Sicilian-American kid from Omaha, Nebraska, end up on this podium?’” Dr. Vacanti said to the approximately 100 guests at the dinner. “My answer is my family, my friends, and my heroes. Just like everyone in this room, we are descendants of immigrants. In my case, my grandparents emigrated from Sicily because of poverty and lack of opportunity. My grandfather could barely speak English but fought in the trenches in France in World War I and gained his American citizenship. He then worked in the boiler shops of the Union Pacific Railroad and taught me the value of hard work, but also the value of using my mind to obtain an education. My father was a professor of oral surgery and endodontics at Creighton University’s dental school, and my mother was a premedical student before marrying my father after World War II. It was that influence that led me to want to become a surgeon at the young age of four.”
Dr. Vacanti also paid tribute to the mentors who encouraged his growth as a surgeon as well as those individuals who have inspired and supported him throughout his career. “My surgical heroes and mentors are Dr. William Hardy Hendren III [MD, FACS, FRCSI(Hon), FRCSEng(Hon), FRCSGlas(Hon)] and Dr. Judah Folkman [MD, FACS], both previous Jacobson Award recipients. Both taught me about surgical innovation and how to think about a problem and its definitive solution,” he said. “Dr. Folkman advised me that if I was going to devote my life to something that I should pick something important. My closest friend, Mr. Walter Smith, has been very important in advising me through the years on many matters both personal and professional, and Dr. Robert Langer [MD, FACS] has been a partner and friend in all of this work through many years.”
Recipient of numerous awards
Dr. Vacanti has received numerous honors and awards. In 2001, he was elected to the Institute of Medicine of the National Academy of Sciences. In 2007, the Board of Directors of City Trusts, acting for the city of Philadelphia, presented him the John Scott Award, which is given to the most deserving men and women whose inventions have contributed significantly to the comfort, welfare, and happiness of human beings. The award has been given in memory of Benjamin Franklin since 1822, and previous recipients include Madame Marie Curie, Orville and Wilbur Wright, Thomas Edison, and Jonas Salk, MD.
Dr. Vacanti became a 2011 Thomson Reuters Citation Laureate in the field of physiology or medicine. Thomson Reuters Citation Laureates are an elite group of highly cited, high-impact researchers, who are likely contenders for other awards in the future, including the Nobel Prize.
Dr. Vacanti also received the William E. Ladd Medal in 2013, which is the highest honor awarded by the surgical section of the American Academy of Pediatrics and considered by many to be the most prestigious award in the field of pediatric surgery.
ACS, Hartford Foundation launch geriatric care initiative
The American College of Surgeons (ACS), in partnership with the John A. Hartford Foundation, announced a four-year initiative aimed at improving health care for older surgical patients through a standards and verification program for hospitals. The initiative, issued June 11, features leaders who are pioneers in the field of geriatric surgery and long-time Hartford grantees, Clifford Y. Ko, MD, MS, MSHS, FACS, Director of the ACS Division of Research and Optimal Patient Care, and Ronnie Rosenthal, MD, FACS, Chair of the ACS Geriatric Surgery Task Force and chief of surgery at the Veterans Affairs Connecticut Healthcare System. The Hartford Foundation awarded a $2.9 million grant for the program.
Growing need for geriatric care
The U.S. geriatric population continues to grow. The Census Bureau reports that more people were 65 years and older in 2010 than in any previous census. Moreover, the largest percentage point increase for the “oldest-old population” (defined as age 85 and older) over the previous two decades was concentrated in the 90- to 94-year-old age group, which increased from 25 percent of the oldest-old group in 1990 to 26.2 percent in 2000, and 26.4 percent in 2010.*
“More than ever, 80, 90, and even 100-year-olds are undergoing surgery, and that trend will only grow. This important partnership between the John A. Hartford Foundation and the ACS to develop standards and then verify that hospitals can deliver optimal geriatric surgical care will save lives, improve outcomes, and reduce harm for older adults across the country,” said Terry Fulmer, PhD, RN, FAAN, president of the Hartford Foundation.
Longstanding commitment
The ACS has long been committed to quality geriatric surgical care. In 2012, the ACS, in partnership with the American Geriatrics Society, published joint guidelines in the Journal of the American College of Surgeons for the perioperative care of the nation’s elderly patients.† These standards apply to every surgical patient ages 65 and older as defined by Medicare regulations.
“We have worked with the John A. Hartford Foundation for many years to develop meaningful tools for improving geriatric surgical care. The current project aims to develop and integrate geriatric surgery standards that will help facilities with infrastructure, standards, processes and protocols, and the integration of data—all to improve the care of the geriatric surgical patient,” Dr. Ko said.
Setting the standards
The Geriatric Surgery Verification and Quality Improvement Program will produce a framework for all hospitals, regardless of size, location, or population served, to improve the quality of care they provide to older adults undergoing surgery. The project will convene experts and engage a broad set of stakeholders representing patients, families, caregivers, multidisciplinary health providers, and industry payors, with the following objectives:
Set standards for hospitals related to the needed infrastructure for optimal care (for example, staffing, resources, and care processes).
Select and develop measures that matter for older patients against which hospitals can be assessed and target areas for improvement. (This objective will include new patient-reported outcomes.)
Develop educational resources for patients and providers.
Build a peer-review verification program that promotes public assurance and a culture of improvement, similar to the ACS’ successful cancer, trauma, and bariatric quality programs, which have been shown to improve care and save lives.
“This is a great opportunity to improve the care and outcomes of geriatric surgery patients—and is relevant to nearly all fields in surgery. This program will involve several disciplines and be a total team effort,” Dr. Ko said.
This work builds on the ACS’ robust data collection and quality improvement infrastructure. It will draw upon the network of experts and growing evidence base in geriatric surgery that has been developed with support from the foundation over the last 20 years.
“The ACS has a long and successful track record of helping hospitals build an infrastructure for surgical quality improvement,” said Christopher A. Langston, PhD, Hartford Foundation program director. “This new verification program will make it easier for hospitals and health systems to focus on doing their best for the large and vulnerable patient population of older adults—and receive public credit for providing them with the right kind of care.”
*U.S. Census Bureau Statistical Brief. The Older Population: 2010. Available at: www.census.gov/prod/cen2010/briefs/c2010br-09.pdf. Accessed June 9, 2015.
†Chow WB, Rosenthal RA, Merkow RP, Ko CY, Esnaola NF. Optimal preoperative assessment of the geriatric surgical patient: A best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. J Am Coll Surg. 2012;215(4):453-466.
The American College of Surgeons (ACS), in partnership with the John A. Hartford Foundation, announced a four-year initiative aimed at improving health care for older surgical patients through a standards and verification program for hospitals. The initiative, issued June 11, features leaders who are pioneers in the field of geriatric surgery and long-time Hartford grantees, Clifford Y. Ko, MD, MS, MSHS, FACS, Director of the ACS Division of Research and Optimal Patient Care, and Ronnie Rosenthal, MD, FACS, Chair of the ACS Geriatric Surgery Task Force and chief of surgery at the Veterans Affairs Connecticut Healthcare System. The Hartford Foundation awarded a $2.9 million grant for the program.
Growing need for geriatric care
The U.S. geriatric population continues to grow. The Census Bureau reports that more people were 65 years and older in 2010 than in any previous census. Moreover, the largest percentage point increase for the “oldest-old population” (defined as age 85 and older) over the previous two decades was concentrated in the 90- to 94-year-old age group, which increased from 25 percent of the oldest-old group in 1990 to 26.2 percent in 2000, and 26.4 percent in 2010.*
“More than ever, 80, 90, and even 100-year-olds are undergoing surgery, and that trend will only grow. This important partnership between the John A. Hartford Foundation and the ACS to develop standards and then verify that hospitals can deliver optimal geriatric surgical care will save lives, improve outcomes, and reduce harm for older adults across the country,” said Terry Fulmer, PhD, RN, FAAN, president of the Hartford Foundation.
Longstanding commitment
The ACS has long been committed to quality geriatric surgical care. In 2012, the ACS, in partnership with the American Geriatrics Society, published joint guidelines in the Journal of the American College of Surgeons for the perioperative care of the nation’s elderly patients.† These standards apply to every surgical patient ages 65 and older as defined by Medicare regulations.
“We have worked with the John A. Hartford Foundation for many years to develop meaningful tools for improving geriatric surgical care. The current project aims to develop and integrate geriatric surgery standards that will help facilities with infrastructure, standards, processes and protocols, and the integration of data—all to improve the care of the geriatric surgical patient,” Dr. Ko said.
Setting the standards
The Geriatric Surgery Verification and Quality Improvement Program will produce a framework for all hospitals, regardless of size, location, or population served, to improve the quality of care they provide to older adults undergoing surgery. The project will convene experts and engage a broad set of stakeholders representing patients, families, caregivers, multidisciplinary health providers, and industry payors, with the following objectives:
Set standards for hospitals related to the needed infrastructure for optimal care (for example, staffing, resources, and care processes).
Select and develop measures that matter for older patients against which hospitals can be assessed and target areas for improvement. (This objective will include new patient-reported outcomes.)
Develop educational resources for patients and providers.
Build a peer-review verification program that promotes public assurance and a culture of improvement, similar to the ACS’ successful cancer, trauma, and bariatric quality programs, which have been shown to improve care and save lives.
“This is a great opportunity to improve the care and outcomes of geriatric surgery patients—and is relevant to nearly all fields in surgery. This program will involve several disciplines and be a total team effort,” Dr. Ko said.
This work builds on the ACS’ robust data collection and quality improvement infrastructure. It will draw upon the network of experts and growing evidence base in geriatric surgery that has been developed with support from the foundation over the last 20 years.
“The ACS has a long and successful track record of helping hospitals build an infrastructure for surgical quality improvement,” said Christopher A. Langston, PhD, Hartford Foundation program director. “This new verification program will make it easier for hospitals and health systems to focus on doing their best for the large and vulnerable patient population of older adults—and receive public credit for providing them with the right kind of care.”
*U.S. Census Bureau Statistical Brief. The Older Population: 2010. Available at: www.census.gov/prod/cen2010/briefs/c2010br-09.pdf. Accessed June 9, 2015.
†Chow WB, Rosenthal RA, Merkow RP, Ko CY, Esnaola NF. Optimal preoperative assessment of the geriatric surgical patient: A best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. J Am Coll Surg. 2012;215(4):453-466.
The American College of Surgeons (ACS), in partnership with the John A. Hartford Foundation, announced a four-year initiative aimed at improving health care for older surgical patients through a standards and verification program for hospitals. The initiative, issued June 11, features leaders who are pioneers in the field of geriatric surgery and long-time Hartford grantees, Clifford Y. Ko, MD, MS, MSHS, FACS, Director of the ACS Division of Research and Optimal Patient Care, and Ronnie Rosenthal, MD, FACS, Chair of the ACS Geriatric Surgery Task Force and chief of surgery at the Veterans Affairs Connecticut Healthcare System. The Hartford Foundation awarded a $2.9 million grant for the program.
Growing need for geriatric care
The U.S. geriatric population continues to grow. The Census Bureau reports that more people were 65 years and older in 2010 than in any previous census. Moreover, the largest percentage point increase for the “oldest-old population” (defined as age 85 and older) over the previous two decades was concentrated in the 90- to 94-year-old age group, which increased from 25 percent of the oldest-old group in 1990 to 26.2 percent in 2000, and 26.4 percent in 2010.*
“More than ever, 80, 90, and even 100-year-olds are undergoing surgery, and that trend will only grow. This important partnership between the John A. Hartford Foundation and the ACS to develop standards and then verify that hospitals can deliver optimal geriatric surgical care will save lives, improve outcomes, and reduce harm for older adults across the country,” said Terry Fulmer, PhD, RN, FAAN, president of the Hartford Foundation.
Longstanding commitment
The ACS has long been committed to quality geriatric surgical care. In 2012, the ACS, in partnership with the American Geriatrics Society, published joint guidelines in the Journal of the American College of Surgeons for the perioperative care of the nation’s elderly patients.† These standards apply to every surgical patient ages 65 and older as defined by Medicare regulations.
“We have worked with the John A. Hartford Foundation for many years to develop meaningful tools for improving geriatric surgical care. The current project aims to develop and integrate geriatric surgery standards that will help facilities with infrastructure, standards, processes and protocols, and the integration of data—all to improve the care of the geriatric surgical patient,” Dr. Ko said.
Setting the standards
The Geriatric Surgery Verification and Quality Improvement Program will produce a framework for all hospitals, regardless of size, location, or population served, to improve the quality of care they provide to older adults undergoing surgery. The project will convene experts and engage a broad set of stakeholders representing patients, families, caregivers, multidisciplinary health providers, and industry payors, with the following objectives:
Set standards for hospitals related to the needed infrastructure for optimal care (for example, staffing, resources, and care processes).
Select and develop measures that matter for older patients against which hospitals can be assessed and target areas for improvement. (This objective will include new patient-reported outcomes.)
Develop educational resources for patients and providers.
Build a peer-review verification program that promotes public assurance and a culture of improvement, similar to the ACS’ successful cancer, trauma, and bariatric quality programs, which have been shown to improve care and save lives.
“This is a great opportunity to improve the care and outcomes of geriatric surgery patients—and is relevant to nearly all fields in surgery. This program will involve several disciplines and be a total team effort,” Dr. Ko said.
This work builds on the ACS’ robust data collection and quality improvement infrastructure. It will draw upon the network of experts and growing evidence base in geriatric surgery that has been developed with support from the foundation over the last 20 years.
“The ACS has a long and successful track record of helping hospitals build an infrastructure for surgical quality improvement,” said Christopher A. Langston, PhD, Hartford Foundation program director. “This new verification program will make it easier for hospitals and health systems to focus on doing their best for the large and vulnerable patient population of older adults—and receive public credit for providing them with the right kind of care.”
*U.S. Census Bureau Statistical Brief. The Older Population: 2010. Available at: www.census.gov/prod/cen2010/briefs/c2010br-09.pdf. Accessed June 9, 2015.
†Chow WB, Rosenthal RA, Merkow RP, Ko CY, Esnaola NF. Optimal preoperative assessment of the geriatric surgical patient: A best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. J Am Coll Surg. 2012;215(4):453-466.