User login
Dark lines in nails

The FP gave the patient a diagnosis of benign longitudinal melanonychia. LM may involve one or several digits, and the pigmented bands may vary in color (from light brown to black), vary in width (most range from 2–4 mm), and have sharp or blurred borders.
Extension of pigmentation to the skin adjacent to the nail plate involving the nail folds or the fingertip is called Hutchinson's sign, and is an important indicator for nail melanoma. A biopsy should be performed in an adult if the cause of longitudinal melanonychia is suspicious for melanoma.
The patient described here did not have Hutchinson’s sign. In fact, this case of LM was of an ethnic/genetic origin, as multiple pigmented bands of the nails are common in dark-skinned individuals.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of EJ Mayeaux, MD. This case was adapted from: Mayeaux EJ. Normal nail variants. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:819-821.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

The FP gave the patient a diagnosis of benign longitudinal melanonychia. LM may involve one or several digits, and the pigmented bands may vary in color (from light brown to black), vary in width (most range from 2–4 mm), and have sharp or blurred borders.
Extension of pigmentation to the skin adjacent to the nail plate involving the nail folds or the fingertip is called Hutchinson's sign, and is an important indicator for nail melanoma. A biopsy should be performed in an adult if the cause of longitudinal melanonychia is suspicious for melanoma.
The patient described here did not have Hutchinson’s sign. In fact, this case of LM was of an ethnic/genetic origin, as multiple pigmented bands of the nails are common in dark-skinned individuals.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of EJ Mayeaux, MD. This case was adapted from: Mayeaux EJ. Normal nail variants. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:819-821.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

The FP gave the patient a diagnosis of benign longitudinal melanonychia. LM may involve one or several digits, and the pigmented bands may vary in color (from light brown to black), vary in width (most range from 2–4 mm), and have sharp or blurred borders.
Extension of pigmentation to the skin adjacent to the nail plate involving the nail folds or the fingertip is called Hutchinson's sign, and is an important indicator for nail melanoma. A biopsy should be performed in an adult if the cause of longitudinal melanonychia is suspicious for melanoma.
The patient described here did not have Hutchinson’s sign. In fact, this case of LM was of an ethnic/genetic origin, as multiple pigmented bands of the nails are common in dark-skinned individuals.
Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. Photo courtesy of EJ Mayeaux, MD. This case was adapted from: Mayeaux EJ. Normal nail variants. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:819-821.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:
Fingernail streaks

The diagnosis
The patient was given a diagnosis of leukonychia, a benign condition involving white spots or lines in the nails. This young man had transverse striate leukonychia, but if the marks had been white spots, the diagnosis would have been leukonychia punctata.
Leukonychia is common in children and occurs less frequently as people age. Parents may fear that it represents a dietary deficiency (in particular, a lack of calcium), but this concern is unfounded. (The nail does not contain calcium.)
Leukonychia is usually the result of minor trauma to the nail cuticle or matrix. When the lesions are caused by a nervous habit, behavior modification can be helpful. Leukonychia can also be an indirect manifestation of autoimmunity, including alopecia areata or thyroid disease.
In this case, the patient was reassured that this was a nail finding that’s often associated with minor trauma, and not a nutritional deficiency.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ. Normal nail variants. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:819-821.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

The diagnosis
The patient was given a diagnosis of leukonychia, a benign condition involving white spots or lines in the nails. This young man had transverse striate leukonychia, but if the marks had been white spots, the diagnosis would have been leukonychia punctata.
Leukonychia is common in children and occurs less frequently as people age. Parents may fear that it represents a dietary deficiency (in particular, a lack of calcium), but this concern is unfounded. (The nail does not contain calcium.)
Leukonychia is usually the result of minor trauma to the nail cuticle or matrix. When the lesions are caused by a nervous habit, behavior modification can be helpful. Leukonychia can also be an indirect manifestation of autoimmunity, including alopecia areata or thyroid disease.
In this case, the patient was reassured that this was a nail finding that’s often associated with minor trauma, and not a nutritional deficiency.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ. Normal nail variants. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:819-821.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:

The diagnosis
The patient was given a diagnosis of leukonychia, a benign condition involving white spots or lines in the nails. This young man had transverse striate leukonychia, but if the marks had been white spots, the diagnosis would have been leukonychia punctata.
Leukonychia is common in children and occurs less frequently as people age. Parents may fear that it represents a dietary deficiency (in particular, a lack of calcium), but this concern is unfounded. (The nail does not contain calcium.)
Leukonychia is usually the result of minor trauma to the nail cuticle or matrix. When the lesions are caused by a nervous habit, behavior modification can be helpful. Leukonychia can also be an indirect manifestation of autoimmunity, including alopecia areata or thyroid disease.
In this case, the patient was reassured that this was a nail finding that’s often associated with minor trauma, and not a nutritional deficiency.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Mayeaux EJ. Normal nail variants. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:819-821.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
You can now get The Color Atlas of Family Medicine as an app for mobile devices including the iPhone and iPad by clicking this link:
Pruritic erythematous maculopapular rash
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 35-year-old man came into our clinic with a rash that had developed a week earlier after a trip to a North Carolina beach. The rash started on his upper inner arms (not including his axilla) and then developed in his groin, thighs, buttocks, and the tops of his feet. There was no rash on his back, head, or neck. The rash was a maculopapular eruption with some confluence, and it had a discrete distribution in his bathing suit area.
The patient said the rash was very itchy, although it had improved over the past couple of days. He did not have any systemic symptoms and hadn’t used any new soaps or detergents, nor had he recently worn any new clothes. He did note, however, that he’d experienced a similar rash in the past after trips to the beach, although the previous rashes were not as severe.
None of the other family members who’d accompanied him to the beach had developed the rash.
FIGURE
A discrete maculopapular eruption in the bathing suit area
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Seabather’s eruption
The patient was given a diagnosis of seabather’s eruption (SBE), also called seabather’s dermatitis or sea lice. SBE is an intensely itchy papular-erythematous dermatitis that can develop after an individual has been swimming in the ocean.1
Planula larvae of the scyphomedusae Linuche unguiculata—commonly known as the thimble jellyfish—are to blame for this form of dermatitis.2L unguiculata are most frequently found in the waters of the Caribbean, Gulf of Mexico, southern United States, and South America.1 Cases of SBE are most common in the spring and summer months, peaking in May.3 Those at highest risk include children, people with a history of SBE, and water sports enthusiasts (eg, surfers).4
L unguiculata larvae are small enough that they can make their way through the mesh of swimwear. As the bather gets out of the water, the suit acts as a sieve, with the water draining out and many of the larvae staying behind.1 Once the jellyfish are pressed against the skin, a defense mechanism is triggered and envenomation occurs.1,5
As a result, patients will develop rashes not only in areas beneath their swimsuits, but also in the skin folds, such as the axilla, and between the upper thighs. For surfers, the trouble spots are the chest and abdomen—places where the body rubs up against the surfboard.3,6
Onset does not occur immediately. Rather, it takes several hours for the lesions to develop, and new ones may continue to develop for days.5 Immediate stinging sensations are associated with prior cases of SBE and suggest a sensitization to the antigen.3
Not all reactions are the same. Some people will have a severe response, while others appear to be immune.2 More extreme systemic symptoms, such as fever, chills, nausea, malaise, sneezing, dyspnea, vomiting, headache, abdominal pain, and diarrhea have been seen in children and in cases of extensive envenomation.4,6
“Swimmer’s itch” is included in the differential
Other possible causes of pruritic rashes like the one our patient had (TABLE) include:
Cercarial dermatitis, also known as swimmer’s itch, is a maculopapular inflammation characterized by pain, prickling, and pruritus. It develops several hours after bathing in freshwater and is limited to exposed areas of the body. The cause of the dermatitis? The larval trematodes of Shistosoma and Trichobilharzia.5
Phytophotodermatitis is an erythematous pruritic inflammation of the skin with vesicles and bullae. The eruption, which is often hyperpigmented, occurs when an individual spends time in the sun after coming into contact with light-sensitive botanicals, such as limes.7
Infectious folliculitis is an infection of the hair follicle resulting in the formation of multiple pustules. Pseudomonas aeruginosa folliculitis, often called hot tub folliculitis, may be pruritic and tender.7
Grover’s disease is also known as transient acantholytic dermatosis and generally affects middle-aged men. It is a pruritic dermatosis of scaling papules that are distributed along the trunk and can show confluence. Although the cause is unknown, it has been linked with cases of high fever, intense exercise, and significant sun exposure.7
Table
The differential for a pruritic, erythematous maculopapular rash5,7
| Condition | Characteristics |
|---|---|
| Cercarial dermatitis | A maculopapular inflammation characterized by pain, prickling, and pruritus that develops several hours after bathing in freshwater and is limited to exposed areas of the body. |
| Phytophotodermatitis | An erythematous pruritic inflammation of the skin, with vesicles and bullae appearing with hyperpigmented streaks along the body. It occurs when an individual spends time in the sun after coming into contact with light-sensitive botanicals. |
| Infectious folliculitis | An infection of the hair follicle resulting in the formation of multiple pustules. Pseudomonas aeruginosa folliculitis is associated with hot tub use. |
| Seabather’s eruption | An erythematous pruritic papular dermatitis that develops several hours after exposure to ocean water. It is limited to areas of high friction and those covered by swimwear. |
| Grover’s disease | A pruritic dermatosis of scaling papules distributed along the trunk that mainly affects middle-aged men. Onset is associated with high fever, intense exercise, and significant sun exposure. |
Treatment usually isn’t needed
SBE usually resolves spontaneously within a week or 2.1 If treatment is necessary, start with topical corticosteroids and oral antihistamines. If this proves insufficient, move on to oral corticosteroids1 (strength of recommendation [SOR]: C). To minimize risk, swimmers should remove their bathing suits and shower as soon as possible after leaving the water4,6 (SOR: C).
Benadryl does the trick
We advised our patient to take diphenhydramine (Benadryl) and the itching went away. We also encouraged him to remove his bathing suit and shower as soon as possible after going in the ocean.
CORRESPONDENCE Blake Fagan, MD, MAHEC Family Medicine Residency Program, 118 W.T. Weaver Boulevard, Asheville, NC 28804; [email protected]
1. Rossetto AL, Dellatorre G, Silveira FL, et al. Seabather’s eruption: a clinical and epidemiological study of 38 cases in Santa Catarina State, Brazil. Rev Inst Med Trop Sao Paulo. 2009;51:169-175.
2. Black NA, Szmant AM, Tomchik RS. Planule of the scyphomedusa Linuche unguiculata as a possible cause of seabather’s eruption. Bulletin of Marine Science. 1994;54:955-960.
3. Tomchik RS, Russell MT, Szmant AM, et al. Clinical perspectives on seabather’s eruption, also known as ‘sea lice.’ JAMA. 1993;269:1669-1672.
4. Kumar S, Hlady WG, Malecki JM. Risk factors for seabather’s eruption: a prospective cohort study. Public Health Rep. 1997;112:59-62.
5. Haddad V, Lupi O, Lonza JP, et al. Tropical dermatology: marine and aquatic dermatology. J Am Acad Dermatol. 2009;61:733-750.
6. Wong DE, Meinking TL, Rosen LB, et al. Seabather’s eruption: clinical, histologic and immunologic features. J Am Acad Dermatol. 1994;30:399-406.
7. Wolff K, Johnson RA. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 6th ed. New York: McGraw-Hill; 2009. Available at: http://www.accessmedicine.com/resourceTOC.aspx?resourceID=45. Accessed August 6, 2010.
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 35-year-old man came into our clinic with a rash that had developed a week earlier after a trip to a North Carolina beach. The rash started on his upper inner arms (not including his axilla) and then developed in his groin, thighs, buttocks, and the tops of his feet. There was no rash on his back, head, or neck. The rash was a maculopapular eruption with some confluence, and it had a discrete distribution in his bathing suit area.
The patient said the rash was very itchy, although it had improved over the past couple of days. He did not have any systemic symptoms and hadn’t used any new soaps or detergents, nor had he recently worn any new clothes. He did note, however, that he’d experienced a similar rash in the past after trips to the beach, although the previous rashes were not as severe.
None of the other family members who’d accompanied him to the beach had developed the rash.
FIGURE
A discrete maculopapular eruption in the bathing suit area
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Seabather’s eruption
The patient was given a diagnosis of seabather’s eruption (SBE), also called seabather’s dermatitis or sea lice. SBE is an intensely itchy papular-erythematous dermatitis that can develop after an individual has been swimming in the ocean.1
Planula larvae of the scyphomedusae Linuche unguiculata—commonly known as the thimble jellyfish—are to blame for this form of dermatitis.2L unguiculata are most frequently found in the waters of the Caribbean, Gulf of Mexico, southern United States, and South America.1 Cases of SBE are most common in the spring and summer months, peaking in May.3 Those at highest risk include children, people with a history of SBE, and water sports enthusiasts (eg, surfers).4
L unguiculata larvae are small enough that they can make their way through the mesh of swimwear. As the bather gets out of the water, the suit acts as a sieve, with the water draining out and many of the larvae staying behind.1 Once the jellyfish are pressed against the skin, a defense mechanism is triggered and envenomation occurs.1,5
As a result, patients will develop rashes not only in areas beneath their swimsuits, but also in the skin folds, such as the axilla, and between the upper thighs. For surfers, the trouble spots are the chest and abdomen—places where the body rubs up against the surfboard.3,6
Onset does not occur immediately. Rather, it takes several hours for the lesions to develop, and new ones may continue to develop for days.5 Immediate stinging sensations are associated with prior cases of SBE and suggest a sensitization to the antigen.3
Not all reactions are the same. Some people will have a severe response, while others appear to be immune.2 More extreme systemic symptoms, such as fever, chills, nausea, malaise, sneezing, dyspnea, vomiting, headache, abdominal pain, and diarrhea have been seen in children and in cases of extensive envenomation.4,6
“Swimmer’s itch” is included in the differential
Other possible causes of pruritic rashes like the one our patient had (TABLE) include:
Cercarial dermatitis, also known as swimmer’s itch, is a maculopapular inflammation characterized by pain, prickling, and pruritus. It develops several hours after bathing in freshwater and is limited to exposed areas of the body. The cause of the dermatitis? The larval trematodes of Shistosoma and Trichobilharzia.5
Phytophotodermatitis is an erythematous pruritic inflammation of the skin with vesicles and bullae. The eruption, which is often hyperpigmented, occurs when an individual spends time in the sun after coming into contact with light-sensitive botanicals, such as limes.7
Infectious folliculitis is an infection of the hair follicle resulting in the formation of multiple pustules. Pseudomonas aeruginosa folliculitis, often called hot tub folliculitis, may be pruritic and tender.7
Grover’s disease is also known as transient acantholytic dermatosis and generally affects middle-aged men. It is a pruritic dermatosis of scaling papules that are distributed along the trunk and can show confluence. Although the cause is unknown, it has been linked with cases of high fever, intense exercise, and significant sun exposure.7
Table
The differential for a pruritic, erythematous maculopapular rash5,7
| Condition | Characteristics |
|---|---|
| Cercarial dermatitis | A maculopapular inflammation characterized by pain, prickling, and pruritus that develops several hours after bathing in freshwater and is limited to exposed areas of the body. |
| Phytophotodermatitis | An erythematous pruritic inflammation of the skin, with vesicles and bullae appearing with hyperpigmented streaks along the body. It occurs when an individual spends time in the sun after coming into contact with light-sensitive botanicals. |
| Infectious folliculitis | An infection of the hair follicle resulting in the formation of multiple pustules. Pseudomonas aeruginosa folliculitis is associated with hot tub use. |
| Seabather’s eruption | An erythematous pruritic papular dermatitis that develops several hours after exposure to ocean water. It is limited to areas of high friction and those covered by swimwear. |
| Grover’s disease | A pruritic dermatosis of scaling papules distributed along the trunk that mainly affects middle-aged men. Onset is associated with high fever, intense exercise, and significant sun exposure. |
Treatment usually isn’t needed
SBE usually resolves spontaneously within a week or 2.1 If treatment is necessary, start with topical corticosteroids and oral antihistamines. If this proves insufficient, move on to oral corticosteroids1 (strength of recommendation [SOR]: C). To minimize risk, swimmers should remove their bathing suits and shower as soon as possible after leaving the water4,6 (SOR: C).
Benadryl does the trick
We advised our patient to take diphenhydramine (Benadryl) and the itching went away. We also encouraged him to remove his bathing suit and shower as soon as possible after going in the ocean.
CORRESPONDENCE Blake Fagan, MD, MAHEC Family Medicine Residency Program, 118 W.T. Weaver Boulevard, Asheville, NC 28804; [email protected]
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 35-year-old man came into our clinic with a rash that had developed a week earlier after a trip to a North Carolina beach. The rash started on his upper inner arms (not including his axilla) and then developed in his groin, thighs, buttocks, and the tops of his feet. There was no rash on his back, head, or neck. The rash was a maculopapular eruption with some confluence, and it had a discrete distribution in his bathing suit area.
The patient said the rash was very itchy, although it had improved over the past couple of days. He did not have any systemic symptoms and hadn’t used any new soaps or detergents, nor had he recently worn any new clothes. He did note, however, that he’d experienced a similar rash in the past after trips to the beach, although the previous rashes were not as severe.
None of the other family members who’d accompanied him to the beach had developed the rash.
FIGURE
A discrete maculopapular eruption in the bathing suit area
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Seabather’s eruption
The patient was given a diagnosis of seabather’s eruption (SBE), also called seabather’s dermatitis or sea lice. SBE is an intensely itchy papular-erythematous dermatitis that can develop after an individual has been swimming in the ocean.1
Planula larvae of the scyphomedusae Linuche unguiculata—commonly known as the thimble jellyfish—are to blame for this form of dermatitis.2L unguiculata are most frequently found in the waters of the Caribbean, Gulf of Mexico, southern United States, and South America.1 Cases of SBE are most common in the spring and summer months, peaking in May.3 Those at highest risk include children, people with a history of SBE, and water sports enthusiasts (eg, surfers).4
L unguiculata larvae are small enough that they can make their way through the mesh of swimwear. As the bather gets out of the water, the suit acts as a sieve, with the water draining out and many of the larvae staying behind.1 Once the jellyfish are pressed against the skin, a defense mechanism is triggered and envenomation occurs.1,5
As a result, patients will develop rashes not only in areas beneath their swimsuits, but also in the skin folds, such as the axilla, and between the upper thighs. For surfers, the trouble spots are the chest and abdomen—places where the body rubs up against the surfboard.3,6
Onset does not occur immediately. Rather, it takes several hours for the lesions to develop, and new ones may continue to develop for days.5 Immediate stinging sensations are associated with prior cases of SBE and suggest a sensitization to the antigen.3
Not all reactions are the same. Some people will have a severe response, while others appear to be immune.2 More extreme systemic symptoms, such as fever, chills, nausea, malaise, sneezing, dyspnea, vomiting, headache, abdominal pain, and diarrhea have been seen in children and in cases of extensive envenomation.4,6
“Swimmer’s itch” is included in the differential
Other possible causes of pruritic rashes like the one our patient had (TABLE) include:
Cercarial dermatitis, also known as swimmer’s itch, is a maculopapular inflammation characterized by pain, prickling, and pruritus. It develops several hours after bathing in freshwater and is limited to exposed areas of the body. The cause of the dermatitis? The larval trematodes of Shistosoma and Trichobilharzia.5
Phytophotodermatitis is an erythematous pruritic inflammation of the skin with vesicles and bullae. The eruption, which is often hyperpigmented, occurs when an individual spends time in the sun after coming into contact with light-sensitive botanicals, such as limes.7
Infectious folliculitis is an infection of the hair follicle resulting in the formation of multiple pustules. Pseudomonas aeruginosa folliculitis, often called hot tub folliculitis, may be pruritic and tender.7
Grover’s disease is also known as transient acantholytic dermatosis and generally affects middle-aged men. It is a pruritic dermatosis of scaling papules that are distributed along the trunk and can show confluence. Although the cause is unknown, it has been linked with cases of high fever, intense exercise, and significant sun exposure.7
Table
The differential for a pruritic, erythematous maculopapular rash5,7
| Condition | Characteristics |
|---|---|
| Cercarial dermatitis | A maculopapular inflammation characterized by pain, prickling, and pruritus that develops several hours after bathing in freshwater and is limited to exposed areas of the body. |
| Phytophotodermatitis | An erythematous pruritic inflammation of the skin, with vesicles and bullae appearing with hyperpigmented streaks along the body. It occurs when an individual spends time in the sun after coming into contact with light-sensitive botanicals. |
| Infectious folliculitis | An infection of the hair follicle resulting in the formation of multiple pustules. Pseudomonas aeruginosa folliculitis is associated with hot tub use. |
| Seabather’s eruption | An erythematous pruritic papular dermatitis that develops several hours after exposure to ocean water. It is limited to areas of high friction and those covered by swimwear. |
| Grover’s disease | A pruritic dermatosis of scaling papules distributed along the trunk that mainly affects middle-aged men. Onset is associated with high fever, intense exercise, and significant sun exposure. |
Treatment usually isn’t needed
SBE usually resolves spontaneously within a week or 2.1 If treatment is necessary, start with topical corticosteroids and oral antihistamines. If this proves insufficient, move on to oral corticosteroids1 (strength of recommendation [SOR]: C). To minimize risk, swimmers should remove their bathing suits and shower as soon as possible after leaving the water4,6 (SOR: C).
Benadryl does the trick
We advised our patient to take diphenhydramine (Benadryl) and the itching went away. We also encouraged him to remove his bathing suit and shower as soon as possible after going in the ocean.
CORRESPONDENCE Blake Fagan, MD, MAHEC Family Medicine Residency Program, 118 W.T. Weaver Boulevard, Asheville, NC 28804; [email protected]
1. Rossetto AL, Dellatorre G, Silveira FL, et al. Seabather’s eruption: a clinical and epidemiological study of 38 cases in Santa Catarina State, Brazil. Rev Inst Med Trop Sao Paulo. 2009;51:169-175.
2. Black NA, Szmant AM, Tomchik RS. Planule of the scyphomedusa Linuche unguiculata as a possible cause of seabather’s eruption. Bulletin of Marine Science. 1994;54:955-960.
3. Tomchik RS, Russell MT, Szmant AM, et al. Clinical perspectives on seabather’s eruption, also known as ‘sea lice.’ JAMA. 1993;269:1669-1672.
4. Kumar S, Hlady WG, Malecki JM. Risk factors for seabather’s eruption: a prospective cohort study. Public Health Rep. 1997;112:59-62.
5. Haddad V, Lupi O, Lonza JP, et al. Tropical dermatology: marine and aquatic dermatology. J Am Acad Dermatol. 2009;61:733-750.
6. Wong DE, Meinking TL, Rosen LB, et al. Seabather’s eruption: clinical, histologic and immunologic features. J Am Acad Dermatol. 1994;30:399-406.
7. Wolff K, Johnson RA. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 6th ed. New York: McGraw-Hill; 2009. Available at: http://www.accessmedicine.com/resourceTOC.aspx?resourceID=45. Accessed August 6, 2010.
1. Rossetto AL, Dellatorre G, Silveira FL, et al. Seabather’s eruption: a clinical and epidemiological study of 38 cases in Santa Catarina State, Brazil. Rev Inst Med Trop Sao Paulo. 2009;51:169-175.
2. Black NA, Szmant AM, Tomchik RS. Planule of the scyphomedusa Linuche unguiculata as a possible cause of seabather’s eruption. Bulletin of Marine Science. 1994;54:955-960.
3. Tomchik RS, Russell MT, Szmant AM, et al. Clinical perspectives on seabather’s eruption, also known as ‘sea lice.’ JAMA. 1993;269:1669-1672.
4. Kumar S, Hlady WG, Malecki JM. Risk factors for seabather’s eruption: a prospective cohort study. Public Health Rep. 1997;112:59-62.
5. Haddad V, Lupi O, Lonza JP, et al. Tropical dermatology: marine and aquatic dermatology. J Am Acad Dermatol. 2009;61:733-750.
6. Wong DE, Meinking TL, Rosen LB, et al. Seabather’s eruption: clinical, histologic and immunologic features. J Am Acad Dermatol. 1994;30:399-406.
7. Wolff K, Johnson RA. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 6th ed. New York: McGraw-Hill; 2009. Available at: http://www.accessmedicine.com/resourceTOC.aspx?resourceID=45. Accessed August 6, 2010.
Papule on thigh

The physician performed a 2-mm punch biopsy, which revealed that the lesion was an angiokeratoma. An angiokeratoma is a benign pink-red to blue-black variably sized papule or plaque that is typically 2 to 10 mm in diameter. Angiokeratomas are composed of a series of subepidermal dilated capillaries that have a characteristic hyperkeratotic surface and bleed easily. These lesions are rare, with a prevalence estimated to be 0.16% in the general population.
The pathogenesis of angiokeratoma formation in unclear; however, there are multiple theories. The development of these lesions may be related to repeated trauma or friction at a particular site. Alternatively, increased venous blood pressure or primary degeneration of vascular elastic tissue could explain their development. While their cause is unclear, the initial event in the development of an angiokeratoma is believed to be the development of a vascular ectasia within the papillary dermis. The epidermal reaction appears to be a secondary phenomenon due to increased proliferative capacity on the surface of the vessels.
If the diagnosis is straightforward and biopsy is not needed, no treatment is needed because simple angiokeratomas are benign entities. However, treatment may be considered for cosmetic purposes, or to prevent bothersome bleeding.
In the case of this patient, the lesion was removed by shave biopsy with clear margins.
Adapted from:
Clark SM, Beachkofsky TM, Wisco OJ, et al. Photo Rounds: Verrucous papule on thigh. J Fam Pract. 2010;59:645-648.

The physician performed a 2-mm punch biopsy, which revealed that the lesion was an angiokeratoma. An angiokeratoma is a benign pink-red to blue-black variably sized papule or plaque that is typically 2 to 10 mm in diameter. Angiokeratomas are composed of a series of subepidermal dilated capillaries that have a characteristic hyperkeratotic surface and bleed easily. These lesions are rare, with a prevalence estimated to be 0.16% in the general population.
The pathogenesis of angiokeratoma formation in unclear; however, there are multiple theories. The development of these lesions may be related to repeated trauma or friction at a particular site. Alternatively, increased venous blood pressure or primary degeneration of vascular elastic tissue could explain their development. While their cause is unclear, the initial event in the development of an angiokeratoma is believed to be the development of a vascular ectasia within the papillary dermis. The epidermal reaction appears to be a secondary phenomenon due to increased proliferative capacity on the surface of the vessels.
If the diagnosis is straightforward and biopsy is not needed, no treatment is needed because simple angiokeratomas are benign entities. However, treatment may be considered for cosmetic purposes, or to prevent bothersome bleeding.
In the case of this patient, the lesion was removed by shave biopsy with clear margins.
Adapted from:
Clark SM, Beachkofsky TM, Wisco OJ, et al. Photo Rounds: Verrucous papule on thigh. J Fam Pract. 2010;59:645-648.

The physician performed a 2-mm punch biopsy, which revealed that the lesion was an angiokeratoma. An angiokeratoma is a benign pink-red to blue-black variably sized papule or plaque that is typically 2 to 10 mm in diameter. Angiokeratomas are composed of a series of subepidermal dilated capillaries that have a characteristic hyperkeratotic surface and bleed easily. These lesions are rare, with a prevalence estimated to be 0.16% in the general population.
The pathogenesis of angiokeratoma formation in unclear; however, there are multiple theories. The development of these lesions may be related to repeated trauma or friction at a particular site. Alternatively, increased venous blood pressure or primary degeneration of vascular elastic tissue could explain their development. While their cause is unclear, the initial event in the development of an angiokeratoma is believed to be the development of a vascular ectasia within the papillary dermis. The epidermal reaction appears to be a secondary phenomenon due to increased proliferative capacity on the surface of the vessels.
If the diagnosis is straightforward and biopsy is not needed, no treatment is needed because simple angiokeratomas are benign entities. However, treatment may be considered for cosmetic purposes, or to prevent bothersome bleeding.
In the case of this patient, the lesion was removed by shave biopsy with clear margins.
Adapted from:
Clark SM, Beachkofsky TM, Wisco OJ, et al. Photo Rounds: Verrucous papule on thigh. J Fam Pract. 2010;59:645-648.
Small area of hair loss

The FP diagnosed tufted folliculitis in this patient. This is a clinical diagnosis made when numerous hairs grow from a single follicle. When this pattern occurs in larger areas of the scalp, it is usually a case of lichen planopilaris. A small area of involvement of tufted folliculitis has a better prognosis than full-blown lichen planopilaris.
The FP prescribed a high-potency topical corticosteroid and injected 10 mg/mL triamcinolone acetonide into the active area of hair loss. A follow-up appointment was set for one month.
In a case like this, the best outcome would be to prevent the spread of the alopecia and to stop the itching. As is true with all cicatricial alopecias, there is no real chance of hair regrowth and the tufts do not go away.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Scarring alopecia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:815-818.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See

The FP diagnosed tufted folliculitis in this patient. This is a clinical diagnosis made when numerous hairs grow from a single follicle. When this pattern occurs in larger areas of the scalp, it is usually a case of lichen planopilaris. A small area of involvement of tufted folliculitis has a better prognosis than full-blown lichen planopilaris.
The FP prescribed a high-potency topical corticosteroid and injected 10 mg/mL triamcinolone acetonide into the active area of hair loss. A follow-up appointment was set for one month.
In a case like this, the best outcome would be to prevent the spread of the alopecia and to stop the itching. As is true with all cicatricial alopecias, there is no real chance of hair regrowth and the tufts do not go away.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Scarring alopecia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:815-818.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See

The FP diagnosed tufted folliculitis in this patient. This is a clinical diagnosis made when numerous hairs grow from a single follicle. When this pattern occurs in larger areas of the scalp, it is usually a case of lichen planopilaris. A small area of involvement of tufted folliculitis has a better prognosis than full-blown lichen planopilaris.
The FP prescribed a high-potency topical corticosteroid and injected 10 mg/mL triamcinolone acetonide into the active area of hair loss. A follow-up appointment was set for one month.
In a case like this, the best outcome would be to prevent the spread of the alopecia and to stop the itching. As is true with all cicatricial alopecias, there is no real chance of hair regrowth and the tufts do not go away.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Scarring alopecia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:815-818.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See
Hair loss, lesions

|

|
The family physician (FP) had experience with cicatricial alopecias and was able to make the diagnosis of dissecting cellulitis (also known as dissecting folliculitis) on appearance only (FIGURE 1). Dissecting cellulitis of the scalp causes painful purulent nodules and sinus tracks (FIGURE 2) leading to scarring alopecia.
Dissecting cellulitis presents with deep inflammatory nodules, primarily over the occiput, that progress to coalescing regions of boggy scalp. Sinus tracks may form and Staphylococcus aureus is frequently cultured from the inflamed lesions. When dissecting cellulitis occurs with acne conglobata and hidradenitis suppurativa, the syndrome is referred to as the follicular occlusion triad. (In this case, the patient had 2 of the 3 elements of the triad; he did not have acne conglobata.)
Dissecting cellulitis may have a mixed neutrophilic and lymphocytic infiltrate on biopsy. The FP opened one purulent scalp lesion and sent a culture. The culture grew out S aureus that was not methicillin-resistant and was sensitive to doxycycline. The physician prescribed doxycycline 100 mg BID. (One option after maximizing any benefits from antibiotics would involve prescribing oral isotretinoin.)
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Scarring alopecia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:815-818.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See

|

|
The family physician (FP) had experience with cicatricial alopecias and was able to make the diagnosis of dissecting cellulitis (also known as dissecting folliculitis) on appearance only (FIGURE 1). Dissecting cellulitis of the scalp causes painful purulent nodules and sinus tracks (FIGURE 2) leading to scarring alopecia.
Dissecting cellulitis presents with deep inflammatory nodules, primarily over the occiput, that progress to coalescing regions of boggy scalp. Sinus tracks may form and Staphylococcus aureus is frequently cultured from the inflamed lesions. When dissecting cellulitis occurs with acne conglobata and hidradenitis suppurativa, the syndrome is referred to as the follicular occlusion triad. (In this case, the patient had 2 of the 3 elements of the triad; he did not have acne conglobata.)
Dissecting cellulitis may have a mixed neutrophilic and lymphocytic infiltrate on biopsy. The FP opened one purulent scalp lesion and sent a culture. The culture grew out S aureus that was not methicillin-resistant and was sensitive to doxycycline. The physician prescribed doxycycline 100 mg BID. (One option after maximizing any benefits from antibiotics would involve prescribing oral isotretinoin.)
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Scarring alopecia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:815-818.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See

|

|
The family physician (FP) had experience with cicatricial alopecias and was able to make the diagnosis of dissecting cellulitis (also known as dissecting folliculitis) on appearance only (FIGURE 1). Dissecting cellulitis of the scalp causes painful purulent nodules and sinus tracks (FIGURE 2) leading to scarring alopecia.
Dissecting cellulitis presents with deep inflammatory nodules, primarily over the occiput, that progress to coalescing regions of boggy scalp. Sinus tracks may form and Staphylococcus aureus is frequently cultured from the inflamed lesions. When dissecting cellulitis occurs with acne conglobata and hidradenitis suppurativa, the syndrome is referred to as the follicular occlusion triad. (In this case, the patient had 2 of the 3 elements of the triad; he did not have acne conglobata.)
Dissecting cellulitis may have a mixed neutrophilic and lymphocytic infiltrate on biopsy. The FP opened one purulent scalp lesion and sent a culture. The culture grew out S aureus that was not methicillin-resistant and was sensitive to doxycycline. The physician prescribed doxycycline 100 mg BID. (One option after maximizing any benefits from antibiotics would involve prescribing oral isotretinoin.)
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Scarring alopecia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:815-818.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See
Alopecia

A 4-mm punch biopsy that included hair follicles at the active edge revealed that this was a case of lichen planopilaris. LPP most commonly affects middle-aged women. It mostly occurs on the frontal and parietal scalp and causes follicular hyperkeratosis, pruritus, perifollicular erythema, a violaceous scalp, and scalp pain.
Oral, topical, or injectable agents can decrease symptoms of itching and inflammation and stop the progression of the disease. Unfortunately these agents cannot reverse the disease.
Since a lymphocytic infiltrate predominates in LPP, experts recommend starting with an oral anti-inflammatory agent such as doxycycline or hydroxychloroquine. Topical agents include high-potency corticosteroids or topical tacrolimus to the involved areas. Intralesional injections of triamcinolone acetonide 10 mg/mL may be helpful.
If severe symptoms and signs of activity persist after 3 to 6 months of doxycycline or hydroxychloroquine, then mycophenolate mofetil should be considered, as well as a referral to a dermatologist.
In this case, once the patient understood that there was no treatment that would bring back the hair on her bald areas, she decided to forego treatment.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Scarring alopecia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:815-818.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See

A 4-mm punch biopsy that included hair follicles at the active edge revealed that this was a case of lichen planopilaris. LPP most commonly affects middle-aged women. It mostly occurs on the frontal and parietal scalp and causes follicular hyperkeratosis, pruritus, perifollicular erythema, a violaceous scalp, and scalp pain.
Oral, topical, or injectable agents can decrease symptoms of itching and inflammation and stop the progression of the disease. Unfortunately these agents cannot reverse the disease.
Since a lymphocytic infiltrate predominates in LPP, experts recommend starting with an oral anti-inflammatory agent such as doxycycline or hydroxychloroquine. Topical agents include high-potency corticosteroids or topical tacrolimus to the involved areas. Intralesional injections of triamcinolone acetonide 10 mg/mL may be helpful.
If severe symptoms and signs of activity persist after 3 to 6 months of doxycycline or hydroxychloroquine, then mycophenolate mofetil should be considered, as well as a referral to a dermatologist.
In this case, once the patient understood that there was no treatment that would bring back the hair on her bald areas, she decided to forego treatment.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Scarring alopecia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:815-818.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See

A 4-mm punch biopsy that included hair follicles at the active edge revealed that this was a case of lichen planopilaris. LPP most commonly affects middle-aged women. It mostly occurs on the frontal and parietal scalp and causes follicular hyperkeratosis, pruritus, perifollicular erythema, a violaceous scalp, and scalp pain.
Oral, topical, or injectable agents can decrease symptoms of itching and inflammation and stop the progression of the disease. Unfortunately these agents cannot reverse the disease.
Since a lymphocytic infiltrate predominates in LPP, experts recommend starting with an oral anti-inflammatory agent such as doxycycline or hydroxychloroquine. Topical agents include high-potency corticosteroids or topical tacrolimus to the involved areas. Intralesional injections of triamcinolone acetonide 10 mg/mL may be helpful.
If severe symptoms and signs of activity persist after 3 to 6 months of doxycycline or hydroxychloroquine, then mycophenolate mofetil should be considered, as well as a referral to a dermatologist.
In this case, once the patient understood that there was no treatment that would bring back the hair on her bald areas, she decided to forego treatment.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Scarring alopecia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:815-818.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See
Hair loss, eruptions

|

|
The FP cultured the pus and it grew methicillin-resistant Staphylococcus aureus; a punch biopsy around an inflamed follicle revealed that this was a case of folliculitis decalvans.
Folliculitis decalvans is a chronic painful neutrophilic bacterial folliculitis characterized by bogginess or induration of the scalp with pustules, erosions, crusts, and scale. It has been suggested that this results from an abnormal host response to S aureus, which is often cultured from the lesions. (In one case series, the disease ran a protracted course with temporary improvement while the patient was on antibiotics, but a flare-up of the disease occurred when the antibiotics were stopped.)
One or 2 punch biopsies are needed to diagnose most forms of scarring alopecia. If 2 punch biopsies are performed, ask the pathologist to cut one vertically and the other horizontally to get the most information about the disease process.
Purulent scalp lesions should be cultured and treatment directed to the predominant pathogen (most commonly S aureus). Oral rifampin 600 mg daily is given for 10 days along with 10 weeks of another antibiotic. This may include oral clindamycin 300 mg twice daily, cephalexin 500 mg 4 times daily, or doxycycline 100 mg twice daily.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Scarring alopecia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:815-818.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See

|

|
The FP cultured the pus and it grew methicillin-resistant Staphylococcus aureus; a punch biopsy around an inflamed follicle revealed that this was a case of folliculitis decalvans.
Folliculitis decalvans is a chronic painful neutrophilic bacterial folliculitis characterized by bogginess or induration of the scalp with pustules, erosions, crusts, and scale. It has been suggested that this results from an abnormal host response to S aureus, which is often cultured from the lesions. (In one case series, the disease ran a protracted course with temporary improvement while the patient was on antibiotics, but a flare-up of the disease occurred when the antibiotics were stopped.)
One or 2 punch biopsies are needed to diagnose most forms of scarring alopecia. If 2 punch biopsies are performed, ask the pathologist to cut one vertically and the other horizontally to get the most information about the disease process.
Purulent scalp lesions should be cultured and treatment directed to the predominant pathogen (most commonly S aureus). Oral rifampin 600 mg daily is given for 10 days along with 10 weeks of another antibiotic. This may include oral clindamycin 300 mg twice daily, cephalexin 500 mg 4 times daily, or doxycycline 100 mg twice daily.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Scarring alopecia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:815-818.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See

|

|
The FP cultured the pus and it grew methicillin-resistant Staphylococcus aureus; a punch biopsy around an inflamed follicle revealed that this was a case of folliculitis decalvans.
Folliculitis decalvans is a chronic painful neutrophilic bacterial folliculitis characterized by bogginess or induration of the scalp with pustules, erosions, crusts, and scale. It has been suggested that this results from an abnormal host response to S aureus, which is often cultured from the lesions. (In one case series, the disease ran a protracted course with temporary improvement while the patient was on antibiotics, but a flare-up of the disease occurred when the antibiotics were stopped.)
One or 2 punch biopsies are needed to diagnose most forms of scarring alopecia. If 2 punch biopsies are performed, ask the pathologist to cut one vertically and the other horizontally to get the most information about the disease process.
Purulent scalp lesions should be cultured and treatment directed to the predominant pathogen (most commonly S aureus). Oral rifampin 600 mg daily is given for 10 days along with 10 weeks of another antibiotic. This may include oral clindamycin 300 mg twice daily, cephalexin 500 mg 4 times daily, or doxycycline 100 mg twice daily.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Usatine R. Scarring alopecia. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:815-818.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See
Pruritic rash on trunk
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 48-YEAR-OLD HISPANIC MAN came into our dermatology clinic with a 2-month history of a pruritic rash that was confined mainly to the trunk. Prior to this visit, he had tried topical corticosteroids and antifungals, but they had not helped.
His trunk showed erythematous macules and reticulate patches with interspersed thin urticarial plaques without scale (FIGURE). Given that the patient had no vesicles or lichenification (which one would expect with eczematous dermatitis) and that the topical steroids did not provide any relief, we performed a biopsy.
FIGURE
Erythematous macules and reticulate patches without scale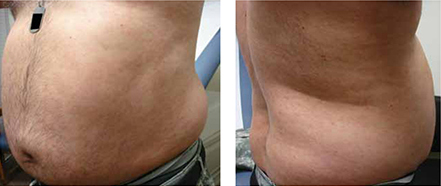
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Secondary syphilis
Our patient’s punch biopsy showed an unremarkable epidermis but a superficial perivascular infiltrate. On higher magnification, the infiltrate proved to be predominately plasma cells. After further investigation and interview, the patient revealed a history of unprotected sex with multiple women; his rapid plasma reagin (RPR) was elevated with a titer of 1:256. Specific treponemal antibody tests confirmed the diagnosis of syphilis. The patient’s human immunodeficiency virus (HIV) test was negative.
Syphilis, a systemic disease with varied dermatological findings, has been described as “the great imitator.” Although it is on the list of differential diagnoses for multiple conditions, it is rarely the culprit—especially given how uncommon it has become in 20th century medicine. With the worldwide HIV epidemic, safe sex programs effectively dropped the incidence of primary and secondary syphilis in the United States to the lowest in recorded history in the year 2001 at 2.17/100,000.1
More recently, however, this infection appears to be making a comeback. Beginning in 2002, its incidence started to rise, reaching 4.6/100,000 in 2009.1
Secondary syphilis usually appears 6 to 8 weeks after the appearance of the primary chancre. As the pathogen spreads into the bloodstream, a host of systemic symptoms may occur, including an influenza-like illness of body aches, fever, fatigue, and headache. While the exanthem of secondary syphilis is traditionally described as a nonpruritic, papular eruption involving the trunk, extremities, face, palms, and soles, a number of cutaneous manifestations are possible, including localized alopecia and syphilids.2 In addition, a number of atypical cases are described in the literature, although none has described an urticarial variant, as seen in our case.
The differential included urticaria and lupus erythematosus
The differential diagnosis for our patient included urticaria, telangiectasia macularis eruptiva perstans, subacute cutaneous lupus erythematosus, and mycosis fungoides. All of these conditions can be distinguished from secondary syphilis by serology and/or biopsy.
Urticaria is a common dermatologic problem with numerous etiologies. It presents as pruritic raised edematous erythematous wheels that blanch with pressure. Although it affects 15% to 25% of the general population at least once in their lives,3 it may progress to life-threatening anaphylaxis. Isolated acute urticaria usually responds to oral antihistamines.
Telangiectasia macularis eruptiva perstans is a form of cutaneous mastocytosis that appears as persistent macules that are red to brown and may exhibit telangiectasia.4 Systemic disease may be evaluated using serum tryptase levels. Patients without systemic disease are managed with oral antihistamines.
Subacute cutaneous lupus erythematosus (SCLE) often presents precipitously as erythematous maculopapular lesions that may coalesce into annular or papulosquamous plaques.5 It has a predilection for sun-exposed areas and is more common in women.5 Multiple drugs have been associated with SCLE, including phenytoin, calcium channel blockers, and thiazide diuretics.6 Treatment consists of discontinuing the offending drug (if one is identified), avoiding (or protecting against) sun exposure, and using topical corticosteroids, oral corticosteroids, and/or antimalarials.
Mycosis fungoides is a form of primary cutaneous T-cell lymphoma that more commonly affects males.7 It begins as erythematous pruritic patches that typically involve the sun-spared areas of the lower abdomen and proximal extremities; it progresses slowly.7 As lesions develop into plaques, they may appear psoriasiform. Treatment depends on the stage of the disease and ranges from topical corticosteroids to systemic radiation and chemotherapy.8
Serology greatly aids diagnosis
If syphilis is not treated during the primary stage, it may progress directly into latency or into the second stage of infection. Preventing progression into late findings hinges upon proper diagnostics. While the initial suspicion should begin with history and physical examination, serology is most frequently used to confirm the presence of Treponema pallidum.
It may take as long as 3 weeks after the appearance of the primary chancre for serology to become positive.9 During this interval, directly visualizing the pathogen via dark-field microscopy may be useful. Following this interval, nontreponemal serology such as the RPR and venereal disease research laboratory (VDRL) are frequently used as the initial serology. These rapid tests detect the antibody to cardiolipin and are relatively inexpensive.
Infection is confirmed with specific treponemal tests, including the fluorescent treponemal antibody absorption (FTA-abs), treponemal enzyme immunoassay, and treponemal particle agglutination tests. These tests are specific for T pallidum and confirm a positive RPR or VDRL. However, specific treponemal tests will not differentiate syphilis from nonvenereal treponematoses such as Bejel, Yaws, and Pinta.10
The common belief is that nontreponemal tests may become negative after successful treatment, and treponemal tests will remain positive indefinitely after successful treatment. However, a study found that 28% of patients treated during primary syphilis and 44% of patients treated during secondary syphilis had positive nontreponemal tests 3 years after treatment.11 In the same study, nearly a quarter of patients treated during primary syphilis no longer had positive FTA-abs 3 years after treatment.11
Penicillin remains the first-line treatment
Once the presence of T pallidum is confirmed, treatment depends on the stage of infection (TABLE). In nonallergic patients, benzathine penicillin G is the standard of care. It should be administered as a single intramuscular (IM) dose of 2.4 million units during primary, secondary, and early latent syphilis12 (strength of recommendation [SOR]: C). Late latent and tertiary syphilis require 3 to 4 weeks of penicillin therapy that is usually achieved with 3 weekly IM injections of 2.4 million units benzathine penicillin G12 (SOR: C). Owing largely to the selective permeability of the blood-brain barrier, neurosyphilis requires a larger dose of 3 million to 4 million units intravenous aqueous crystalline benzathine penicillin every 4 hours for 10 to 14 days12 (SOR: C).
Penicillin desensitization should be considered in penicillin-allergic patients, particularly in those who are pregnant or have HIV infection.12
Treatment success can be determined by a 4-fold decline in RPR/VDRL titer over a period of 3 to 6 months after treatment. During the first 24 hours after initial treatment, patients may develop an acute febrile illness known as the Jarisch-Herxheimer reaction. This is largely the result of massive lysis of the pathogen, spilling large quantities of inflammatory cytokines into the bloodstream.13
Table
Syphilis treatment by stage of infection12
| Stage | Time since exposure | Treatment |
|---|---|---|
| Primary | 10-90 days | Adults Children |
| Secondary | 4-10 weeks | Adults Children |
| Early latent | After primary or secondary stages, <1 year | Adults Children |
| Late latent | >1 year of no symptoms | Adults Children |
| Tertiary | Months to years | Adults See above |
| Neurosyphilis (at any stage) | Any time after infection | Aqueous crystalline penicillin G 18-24 million units/d, administered as 3-4 million units IV every 4 hours or continuous infusion, for 10-14 days Alternative |
| IM, intramuscular; IV, intravenous. | ||
Our patient’s symptoms resolved with penicillin
Given the nebulous history of exposure, we treated the patient as having late latent syphilis (rather than secondary syphilis) and administered 2.4 million units benzathine penicillin G IM weekly for 3 weeks. After this treatment course, the pruritic lesions resolved and the patient’s RPR titer dropped to 1:8 in 3 months.
Our case demonstrates a unique atypical presentation of secondary syphilis. To our knowledge, there is no mention of secondary syphilis mimicking urticaria in the literature. The pruritus that accompanied the lesions was also atypical; however, one study noted 42% of patients experience this symptom in secondary syphilis.14 Fortunately, serological studies confirmed the diagnosis and the patient’s symptoms resolved with standard therapy.
CORRESPONDENCE
Peter L. Mattei, MD, 641 Bainbridge Drive, Mullica Hill, NJ 08062; [email protected]
1. Centers for Disease Control and Prevention. Summary of notifiable diseases: United States, 2009. MMWR Morb Mortal Wkly Rep. 2011;58:1-100.
2. Bolognia JL, Jorizzo JL, Rapini RP. eds. Dermatology (e-dition). 2nd ed. Mosby Elsevier; 2008. Available at: http://www.expertconsultbook.com/expertconsult/op/book.do?method=display&type=bookPage&decorator=none&eid=4-u1.0-B978-1-4160-2999-1..50002-3&isbn=978-1-4160-2999-1. Accessed March 29, 2010.
3. Fonacier LS, Dreskin SC, Leung DY. Allergic skin diseases. J Allergy Clin Immunol. 2010;125(2 suppl 2):S138-S149.
4. Nguyen NQ. Telangiectasia macularis eruptiva perstans. Dermatol Online J. 2004;10:1.-
5. Wechsler HL. Cutaneous disease in systemic lupus erythematosus. Clin Dermatol. 1985;3:79-87.
6. Rothfield N, Sontheimer RD, Bernstein M. Lupus erythematosus: systemic and cutaneous manifestations. Clin Dermatol. 2006;24:348-362.
7. Galper SL, Smith BD, Wilson LD. Diagnosis and management of mycosis fungoides. Oncology (Williston Park). 2010;24:491-501.
8. Lansigan F, Foss FM. Current and emerging treatment strategies for cutaneous T-cell lymphoma. Drugs. 2010;70:273-286.
9. Eccleston K, Collins L, Higgins SP. Primary syphilis. Int J STD AIDS. 2008;19:145-151.
10. Koff AB, Rosen T. Nonvenereal treponematoses: yaws, endemic syphilis, and pinta. J Am Acad Dermatol. 1993;29:519-535.
11. Romanowski B, Sutherland R, Fick GH, et al. Serologic response to treatment of infectious syphilis. Ann Intern Med. 1991;114:1005-1009.
12. Workowski KA, Berman SM. Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59(RR-12):1-110.
13. Mandell GL, Bennet JE, Dolin R. Principles and Practice of Infectious Diseases. 6th ed. New York, NY: Elsevier Health Sciences; 2005:2768–2784.
14. Chapel TA. The signs and symptoms of secondary syphilis. Sex Transm Dis. 1980;7:161-164.
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 48-YEAR-OLD HISPANIC MAN came into our dermatology clinic with a 2-month history of a pruritic rash that was confined mainly to the trunk. Prior to this visit, he had tried topical corticosteroids and antifungals, but they had not helped.
His trunk showed erythematous macules and reticulate patches with interspersed thin urticarial plaques without scale (FIGURE). Given that the patient had no vesicles or lichenification (which one would expect with eczematous dermatitis) and that the topical steroids did not provide any relief, we performed a biopsy.
FIGURE
Erythematous macules and reticulate patches without scale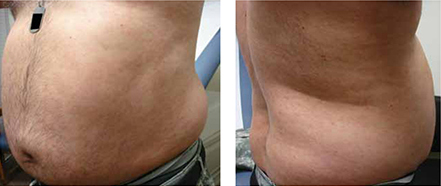
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Secondary syphilis
Our patient’s punch biopsy showed an unremarkable epidermis but a superficial perivascular infiltrate. On higher magnification, the infiltrate proved to be predominately plasma cells. After further investigation and interview, the patient revealed a history of unprotected sex with multiple women; his rapid plasma reagin (RPR) was elevated with a titer of 1:256. Specific treponemal antibody tests confirmed the diagnosis of syphilis. The patient’s human immunodeficiency virus (HIV) test was negative.
Syphilis, a systemic disease with varied dermatological findings, has been described as “the great imitator.” Although it is on the list of differential diagnoses for multiple conditions, it is rarely the culprit—especially given how uncommon it has become in 20th century medicine. With the worldwide HIV epidemic, safe sex programs effectively dropped the incidence of primary and secondary syphilis in the United States to the lowest in recorded history in the year 2001 at 2.17/100,000.1
More recently, however, this infection appears to be making a comeback. Beginning in 2002, its incidence started to rise, reaching 4.6/100,000 in 2009.1
Secondary syphilis usually appears 6 to 8 weeks after the appearance of the primary chancre. As the pathogen spreads into the bloodstream, a host of systemic symptoms may occur, including an influenza-like illness of body aches, fever, fatigue, and headache. While the exanthem of secondary syphilis is traditionally described as a nonpruritic, papular eruption involving the trunk, extremities, face, palms, and soles, a number of cutaneous manifestations are possible, including localized alopecia and syphilids.2 In addition, a number of atypical cases are described in the literature, although none has described an urticarial variant, as seen in our case.
The differential included urticaria and lupus erythematosus
The differential diagnosis for our patient included urticaria, telangiectasia macularis eruptiva perstans, subacute cutaneous lupus erythematosus, and mycosis fungoides. All of these conditions can be distinguished from secondary syphilis by serology and/or biopsy.
Urticaria is a common dermatologic problem with numerous etiologies. It presents as pruritic raised edematous erythematous wheels that blanch with pressure. Although it affects 15% to 25% of the general population at least once in their lives,3 it may progress to life-threatening anaphylaxis. Isolated acute urticaria usually responds to oral antihistamines.
Telangiectasia macularis eruptiva perstans is a form of cutaneous mastocytosis that appears as persistent macules that are red to brown and may exhibit telangiectasia.4 Systemic disease may be evaluated using serum tryptase levels. Patients without systemic disease are managed with oral antihistamines.
Subacute cutaneous lupus erythematosus (SCLE) often presents precipitously as erythematous maculopapular lesions that may coalesce into annular or papulosquamous plaques.5 It has a predilection for sun-exposed areas and is more common in women.5 Multiple drugs have been associated with SCLE, including phenytoin, calcium channel blockers, and thiazide diuretics.6 Treatment consists of discontinuing the offending drug (if one is identified), avoiding (or protecting against) sun exposure, and using topical corticosteroids, oral corticosteroids, and/or antimalarials.
Mycosis fungoides is a form of primary cutaneous T-cell lymphoma that more commonly affects males.7 It begins as erythematous pruritic patches that typically involve the sun-spared areas of the lower abdomen and proximal extremities; it progresses slowly.7 As lesions develop into plaques, they may appear psoriasiform. Treatment depends on the stage of the disease and ranges from topical corticosteroids to systemic radiation and chemotherapy.8
Serology greatly aids diagnosis
If syphilis is not treated during the primary stage, it may progress directly into latency or into the second stage of infection. Preventing progression into late findings hinges upon proper diagnostics. While the initial suspicion should begin with history and physical examination, serology is most frequently used to confirm the presence of Treponema pallidum.
It may take as long as 3 weeks after the appearance of the primary chancre for serology to become positive.9 During this interval, directly visualizing the pathogen via dark-field microscopy may be useful. Following this interval, nontreponemal serology such as the RPR and venereal disease research laboratory (VDRL) are frequently used as the initial serology. These rapid tests detect the antibody to cardiolipin and are relatively inexpensive.
Infection is confirmed with specific treponemal tests, including the fluorescent treponemal antibody absorption (FTA-abs), treponemal enzyme immunoassay, and treponemal particle agglutination tests. These tests are specific for T pallidum and confirm a positive RPR or VDRL. However, specific treponemal tests will not differentiate syphilis from nonvenereal treponematoses such as Bejel, Yaws, and Pinta.10
The common belief is that nontreponemal tests may become negative after successful treatment, and treponemal tests will remain positive indefinitely after successful treatment. However, a study found that 28% of patients treated during primary syphilis and 44% of patients treated during secondary syphilis had positive nontreponemal tests 3 years after treatment.11 In the same study, nearly a quarter of patients treated during primary syphilis no longer had positive FTA-abs 3 years after treatment.11
Penicillin remains the first-line treatment
Once the presence of T pallidum is confirmed, treatment depends on the stage of infection (TABLE). In nonallergic patients, benzathine penicillin G is the standard of care. It should be administered as a single intramuscular (IM) dose of 2.4 million units during primary, secondary, and early latent syphilis12 (strength of recommendation [SOR]: C). Late latent and tertiary syphilis require 3 to 4 weeks of penicillin therapy that is usually achieved with 3 weekly IM injections of 2.4 million units benzathine penicillin G12 (SOR: C). Owing largely to the selective permeability of the blood-brain barrier, neurosyphilis requires a larger dose of 3 million to 4 million units intravenous aqueous crystalline benzathine penicillin every 4 hours for 10 to 14 days12 (SOR: C).
Penicillin desensitization should be considered in penicillin-allergic patients, particularly in those who are pregnant or have HIV infection.12
Treatment success can be determined by a 4-fold decline in RPR/VDRL titer over a period of 3 to 6 months after treatment. During the first 24 hours after initial treatment, patients may develop an acute febrile illness known as the Jarisch-Herxheimer reaction. This is largely the result of massive lysis of the pathogen, spilling large quantities of inflammatory cytokines into the bloodstream.13
Table
Syphilis treatment by stage of infection12
| Stage | Time since exposure | Treatment |
|---|---|---|
| Primary | 10-90 days | Adults Children |
| Secondary | 4-10 weeks | Adults Children |
| Early latent | After primary or secondary stages, <1 year | Adults Children |
| Late latent | >1 year of no symptoms | Adults Children |
| Tertiary | Months to years | Adults See above |
| Neurosyphilis (at any stage) | Any time after infection | Aqueous crystalline penicillin G 18-24 million units/d, administered as 3-4 million units IV every 4 hours or continuous infusion, for 10-14 days Alternative |
| IM, intramuscular; IV, intravenous. | ||
Our patient’s symptoms resolved with penicillin
Given the nebulous history of exposure, we treated the patient as having late latent syphilis (rather than secondary syphilis) and administered 2.4 million units benzathine penicillin G IM weekly for 3 weeks. After this treatment course, the pruritic lesions resolved and the patient’s RPR titer dropped to 1:8 in 3 months.
Our case demonstrates a unique atypical presentation of secondary syphilis. To our knowledge, there is no mention of secondary syphilis mimicking urticaria in the literature. The pruritus that accompanied the lesions was also atypical; however, one study noted 42% of patients experience this symptom in secondary syphilis.14 Fortunately, serological studies confirmed the diagnosis and the patient’s symptoms resolved with standard therapy.
CORRESPONDENCE
Peter L. Mattei, MD, 641 Bainbridge Drive, Mullica Hill, NJ 08062; [email protected]
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A 48-YEAR-OLD HISPANIC MAN came into our dermatology clinic with a 2-month history of a pruritic rash that was confined mainly to the trunk. Prior to this visit, he had tried topical corticosteroids and antifungals, but they had not helped.
His trunk showed erythematous macules and reticulate patches with interspersed thin urticarial plaques without scale (FIGURE). Given that the patient had no vesicles or lichenification (which one would expect with eczematous dermatitis) and that the topical steroids did not provide any relief, we performed a biopsy.
FIGURE
Erythematous macules and reticulate patches without scale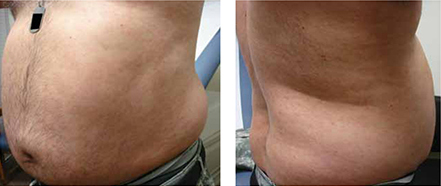
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Secondary syphilis
Our patient’s punch biopsy showed an unremarkable epidermis but a superficial perivascular infiltrate. On higher magnification, the infiltrate proved to be predominately plasma cells. After further investigation and interview, the patient revealed a history of unprotected sex with multiple women; his rapid plasma reagin (RPR) was elevated with a titer of 1:256. Specific treponemal antibody tests confirmed the diagnosis of syphilis. The patient’s human immunodeficiency virus (HIV) test was negative.
Syphilis, a systemic disease with varied dermatological findings, has been described as “the great imitator.” Although it is on the list of differential diagnoses for multiple conditions, it is rarely the culprit—especially given how uncommon it has become in 20th century medicine. With the worldwide HIV epidemic, safe sex programs effectively dropped the incidence of primary and secondary syphilis in the United States to the lowest in recorded history in the year 2001 at 2.17/100,000.1
More recently, however, this infection appears to be making a comeback. Beginning in 2002, its incidence started to rise, reaching 4.6/100,000 in 2009.1
Secondary syphilis usually appears 6 to 8 weeks after the appearance of the primary chancre. As the pathogen spreads into the bloodstream, a host of systemic symptoms may occur, including an influenza-like illness of body aches, fever, fatigue, and headache. While the exanthem of secondary syphilis is traditionally described as a nonpruritic, papular eruption involving the trunk, extremities, face, palms, and soles, a number of cutaneous manifestations are possible, including localized alopecia and syphilids.2 In addition, a number of atypical cases are described in the literature, although none has described an urticarial variant, as seen in our case.
The differential included urticaria and lupus erythematosus
The differential diagnosis for our patient included urticaria, telangiectasia macularis eruptiva perstans, subacute cutaneous lupus erythematosus, and mycosis fungoides. All of these conditions can be distinguished from secondary syphilis by serology and/or biopsy.
Urticaria is a common dermatologic problem with numerous etiologies. It presents as pruritic raised edematous erythematous wheels that blanch with pressure. Although it affects 15% to 25% of the general population at least once in their lives,3 it may progress to life-threatening anaphylaxis. Isolated acute urticaria usually responds to oral antihistamines.
Telangiectasia macularis eruptiva perstans is a form of cutaneous mastocytosis that appears as persistent macules that are red to brown and may exhibit telangiectasia.4 Systemic disease may be evaluated using serum tryptase levels. Patients without systemic disease are managed with oral antihistamines.
Subacute cutaneous lupus erythematosus (SCLE) often presents precipitously as erythematous maculopapular lesions that may coalesce into annular or papulosquamous plaques.5 It has a predilection for sun-exposed areas and is more common in women.5 Multiple drugs have been associated with SCLE, including phenytoin, calcium channel blockers, and thiazide diuretics.6 Treatment consists of discontinuing the offending drug (if one is identified), avoiding (or protecting against) sun exposure, and using topical corticosteroids, oral corticosteroids, and/or antimalarials.
Mycosis fungoides is a form of primary cutaneous T-cell lymphoma that more commonly affects males.7 It begins as erythematous pruritic patches that typically involve the sun-spared areas of the lower abdomen and proximal extremities; it progresses slowly.7 As lesions develop into plaques, they may appear psoriasiform. Treatment depends on the stage of the disease and ranges from topical corticosteroids to systemic radiation and chemotherapy.8
Serology greatly aids diagnosis
If syphilis is not treated during the primary stage, it may progress directly into latency or into the second stage of infection. Preventing progression into late findings hinges upon proper diagnostics. While the initial suspicion should begin with history and physical examination, serology is most frequently used to confirm the presence of Treponema pallidum.
It may take as long as 3 weeks after the appearance of the primary chancre for serology to become positive.9 During this interval, directly visualizing the pathogen via dark-field microscopy may be useful. Following this interval, nontreponemal serology such as the RPR and venereal disease research laboratory (VDRL) are frequently used as the initial serology. These rapid tests detect the antibody to cardiolipin and are relatively inexpensive.
Infection is confirmed with specific treponemal tests, including the fluorescent treponemal antibody absorption (FTA-abs), treponemal enzyme immunoassay, and treponemal particle agglutination tests. These tests are specific for T pallidum and confirm a positive RPR or VDRL. However, specific treponemal tests will not differentiate syphilis from nonvenereal treponematoses such as Bejel, Yaws, and Pinta.10
The common belief is that nontreponemal tests may become negative after successful treatment, and treponemal tests will remain positive indefinitely after successful treatment. However, a study found that 28% of patients treated during primary syphilis and 44% of patients treated during secondary syphilis had positive nontreponemal tests 3 years after treatment.11 In the same study, nearly a quarter of patients treated during primary syphilis no longer had positive FTA-abs 3 years after treatment.11
Penicillin remains the first-line treatment
Once the presence of T pallidum is confirmed, treatment depends on the stage of infection (TABLE). In nonallergic patients, benzathine penicillin G is the standard of care. It should be administered as a single intramuscular (IM) dose of 2.4 million units during primary, secondary, and early latent syphilis12 (strength of recommendation [SOR]: C). Late latent and tertiary syphilis require 3 to 4 weeks of penicillin therapy that is usually achieved with 3 weekly IM injections of 2.4 million units benzathine penicillin G12 (SOR: C). Owing largely to the selective permeability of the blood-brain barrier, neurosyphilis requires a larger dose of 3 million to 4 million units intravenous aqueous crystalline benzathine penicillin every 4 hours for 10 to 14 days12 (SOR: C).
Penicillin desensitization should be considered in penicillin-allergic patients, particularly in those who are pregnant or have HIV infection.12
Treatment success can be determined by a 4-fold decline in RPR/VDRL titer over a period of 3 to 6 months after treatment. During the first 24 hours after initial treatment, patients may develop an acute febrile illness known as the Jarisch-Herxheimer reaction. This is largely the result of massive lysis of the pathogen, spilling large quantities of inflammatory cytokines into the bloodstream.13
Table
Syphilis treatment by stage of infection12
| Stage | Time since exposure | Treatment |
|---|---|---|
| Primary | 10-90 days | Adults Children |
| Secondary | 4-10 weeks | Adults Children |
| Early latent | After primary or secondary stages, <1 year | Adults Children |
| Late latent | >1 year of no symptoms | Adults Children |
| Tertiary | Months to years | Adults See above |
| Neurosyphilis (at any stage) | Any time after infection | Aqueous crystalline penicillin G 18-24 million units/d, administered as 3-4 million units IV every 4 hours or continuous infusion, for 10-14 days Alternative |
| IM, intramuscular; IV, intravenous. | ||
Our patient’s symptoms resolved with penicillin
Given the nebulous history of exposure, we treated the patient as having late latent syphilis (rather than secondary syphilis) and administered 2.4 million units benzathine penicillin G IM weekly for 3 weeks. After this treatment course, the pruritic lesions resolved and the patient’s RPR titer dropped to 1:8 in 3 months.
Our case demonstrates a unique atypical presentation of secondary syphilis. To our knowledge, there is no mention of secondary syphilis mimicking urticaria in the literature. The pruritus that accompanied the lesions was also atypical; however, one study noted 42% of patients experience this symptom in secondary syphilis.14 Fortunately, serological studies confirmed the diagnosis and the patient’s symptoms resolved with standard therapy.
CORRESPONDENCE
Peter L. Mattei, MD, 641 Bainbridge Drive, Mullica Hill, NJ 08062; [email protected]
1. Centers for Disease Control and Prevention. Summary of notifiable diseases: United States, 2009. MMWR Morb Mortal Wkly Rep. 2011;58:1-100.
2. Bolognia JL, Jorizzo JL, Rapini RP. eds. Dermatology (e-dition). 2nd ed. Mosby Elsevier; 2008. Available at: http://www.expertconsultbook.com/expertconsult/op/book.do?method=display&type=bookPage&decorator=none&eid=4-u1.0-B978-1-4160-2999-1..50002-3&isbn=978-1-4160-2999-1. Accessed March 29, 2010.
3. Fonacier LS, Dreskin SC, Leung DY. Allergic skin diseases. J Allergy Clin Immunol. 2010;125(2 suppl 2):S138-S149.
4. Nguyen NQ. Telangiectasia macularis eruptiva perstans. Dermatol Online J. 2004;10:1.-
5. Wechsler HL. Cutaneous disease in systemic lupus erythematosus. Clin Dermatol. 1985;3:79-87.
6. Rothfield N, Sontheimer RD, Bernstein M. Lupus erythematosus: systemic and cutaneous manifestations. Clin Dermatol. 2006;24:348-362.
7. Galper SL, Smith BD, Wilson LD. Diagnosis and management of mycosis fungoides. Oncology (Williston Park). 2010;24:491-501.
8. Lansigan F, Foss FM. Current and emerging treatment strategies for cutaneous T-cell lymphoma. Drugs. 2010;70:273-286.
9. Eccleston K, Collins L, Higgins SP. Primary syphilis. Int J STD AIDS. 2008;19:145-151.
10. Koff AB, Rosen T. Nonvenereal treponematoses: yaws, endemic syphilis, and pinta. J Am Acad Dermatol. 1993;29:519-535.
11. Romanowski B, Sutherland R, Fick GH, et al. Serologic response to treatment of infectious syphilis. Ann Intern Med. 1991;114:1005-1009.
12. Workowski KA, Berman SM. Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59(RR-12):1-110.
13. Mandell GL, Bennet JE, Dolin R. Principles and Practice of Infectious Diseases. 6th ed. New York, NY: Elsevier Health Sciences; 2005:2768–2784.
14. Chapel TA. The signs and symptoms of secondary syphilis. Sex Transm Dis. 1980;7:161-164.
1. Centers for Disease Control and Prevention. Summary of notifiable diseases: United States, 2009. MMWR Morb Mortal Wkly Rep. 2011;58:1-100.
2. Bolognia JL, Jorizzo JL, Rapini RP. eds. Dermatology (e-dition). 2nd ed. Mosby Elsevier; 2008. Available at: http://www.expertconsultbook.com/expertconsult/op/book.do?method=display&type=bookPage&decorator=none&eid=4-u1.0-B978-1-4160-2999-1..50002-3&isbn=978-1-4160-2999-1. Accessed March 29, 2010.
3. Fonacier LS, Dreskin SC, Leung DY. Allergic skin diseases. J Allergy Clin Immunol. 2010;125(2 suppl 2):S138-S149.
4. Nguyen NQ. Telangiectasia macularis eruptiva perstans. Dermatol Online J. 2004;10:1.-
5. Wechsler HL. Cutaneous disease in systemic lupus erythematosus. Clin Dermatol. 1985;3:79-87.
6. Rothfield N, Sontheimer RD, Bernstein M. Lupus erythematosus: systemic and cutaneous manifestations. Clin Dermatol. 2006;24:348-362.
7. Galper SL, Smith BD, Wilson LD. Diagnosis and management of mycosis fungoides. Oncology (Williston Park). 2010;24:491-501.
8. Lansigan F, Foss FM. Current and emerging treatment strategies for cutaneous T-cell lymphoma. Drugs. 2010;70:273-286.
9. Eccleston K, Collins L, Higgins SP. Primary syphilis. Int J STD AIDS. 2008;19:145-151.
10. Koff AB, Rosen T. Nonvenereal treponematoses: yaws, endemic syphilis, and pinta. J Am Acad Dermatol. 1993;29:519-535.
11. Romanowski B, Sutherland R, Fick GH, et al. Serologic response to treatment of infectious syphilis. Ann Intern Med. 1991;114:1005-1009.
12. Workowski KA, Berman SM. Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59(RR-12):1-110.
13. Mandell GL, Bennet JE, Dolin R. Principles and Practice of Infectious Diseases. 6th ed. New York, NY: Elsevier Health Sciences; 2005:2768–2784.
14. Chapel TA. The signs and symptoms of secondary syphilis. Sex Transm Dis. 1980;7:161-164.
Bald spots on scalp

Alopecia areata (AA) is a common, chronic skin disorder manifested as a sudden loss of hair without accompanying inflammation or scarring. AA may extend to involve the whole scalp (alopecia totalis) or the whole body (alopecia universalis). The average age of onset is 25 to 27 years.
AA is secondary to an autoimmune phenomenon involving antibodies, T-cells, and cytokines. Microscopic evaluation of the hair from the periphery of the involved skin reveals "exclamation point" hairs, which are characterized by proximal thinning while the distal portion remains of normal caliber. Thyroid abnormalities, vitiligo, and pernicious anemia may accompany AA and hence screening laboratory tests (eg, thyroid stimulating hormone, hemoglobin) may be helpful to exclude thyroid disorders and anemia. Biopsy is usually not needed unless the diagnosis is uncertain.
The treatment of choice in patients older than 10 years of age with <50% scalp involvement is intralesional steroids. Triamcinolone acetonide 5 to 10 mg/mL is injected into multiple areas not to exceed 40 mg/mL per visit. For patients who are younger than 10 years of age, mid-potency topical steroids can be used. One randomized controlled trial showed aromatherapy with topical essential oils to be a safe and effective treatment for alopecia areata. Although spontaneous recovery usually occurs, the course of AA is unpredictable and often characterized by recurrent periods of hair loss and regrowth.
In this case, the mother and child were reassured that alopecia areata is a condition in which the hair is likely to re-grow without treatment. Neither of them wanted intralesional injections or topical therapies. One year later during a well-child exam, the physician noted that the girl’s hair had fully regrown.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Haynes, J. Alopecia areata. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:807-810.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See

Alopecia areata (AA) is a common, chronic skin disorder manifested as a sudden loss of hair without accompanying inflammation or scarring. AA may extend to involve the whole scalp (alopecia totalis) or the whole body (alopecia universalis). The average age of onset is 25 to 27 years.
AA is secondary to an autoimmune phenomenon involving antibodies, T-cells, and cytokines. Microscopic evaluation of the hair from the periphery of the involved skin reveals "exclamation point" hairs, which are characterized by proximal thinning while the distal portion remains of normal caliber. Thyroid abnormalities, vitiligo, and pernicious anemia may accompany AA and hence screening laboratory tests (eg, thyroid stimulating hormone, hemoglobin) may be helpful to exclude thyroid disorders and anemia. Biopsy is usually not needed unless the diagnosis is uncertain.
The treatment of choice in patients older than 10 years of age with <50% scalp involvement is intralesional steroids. Triamcinolone acetonide 5 to 10 mg/mL is injected into multiple areas not to exceed 40 mg/mL per visit. For patients who are younger than 10 years of age, mid-potency topical steroids can be used. One randomized controlled trial showed aromatherapy with topical essential oils to be a safe and effective treatment for alopecia areata. Although spontaneous recovery usually occurs, the course of AA is unpredictable and often characterized by recurrent periods of hair loss and regrowth.
In this case, the mother and child were reassured that alopecia areata is a condition in which the hair is likely to re-grow without treatment. Neither of them wanted intralesional injections or topical therapies. One year later during a well-child exam, the physician noted that the girl’s hair had fully regrown.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Haynes, J. Alopecia areata. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:807-810.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See

Alopecia areata (AA) is a common, chronic skin disorder manifested as a sudden loss of hair without accompanying inflammation or scarring. AA may extend to involve the whole scalp (alopecia totalis) or the whole body (alopecia universalis). The average age of onset is 25 to 27 years.
AA is secondary to an autoimmune phenomenon involving antibodies, T-cells, and cytokines. Microscopic evaluation of the hair from the periphery of the involved skin reveals "exclamation point" hairs, which are characterized by proximal thinning while the distal portion remains of normal caliber. Thyroid abnormalities, vitiligo, and pernicious anemia may accompany AA and hence screening laboratory tests (eg, thyroid stimulating hormone, hemoglobin) may be helpful to exclude thyroid disorders and anemia. Biopsy is usually not needed unless the diagnosis is uncertain.
The treatment of choice in patients older than 10 years of age with <50% scalp involvement is intralesional steroids. Triamcinolone acetonide 5 to 10 mg/mL is injected into multiple areas not to exceed 40 mg/mL per visit. For patients who are younger than 10 years of age, mid-potency topical steroids can be used. One randomized controlled trial showed aromatherapy with topical essential oils to be a safe and effective treatment for alopecia areata. Although spontaneous recovery usually occurs, the course of AA is unpredictable and often characterized by recurrent periods of hair loss and regrowth.
In this case, the mother and child were reassured that alopecia areata is a condition in which the hair is likely to re-grow without treatment. Neither of them wanted intralesional injections or topical therapies. One year later during a well-child exam, the physician noted that the girl’s hair had fully regrown.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Haynes, J. Alopecia areata. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. The Color Atlas of Family Medicine. New York, NY: McGraw-Hill; 2009:807-810.
To learn more about The Color Atlas of Family Medicine, see:
• http://www.amazon.com/Color-Atlas-Family-Medicine/dp/0071474641
The Color Atlas of Family Medicine is also available as an app for mobile devices. See