User login
LISTEN NOW: SHM President Robert Harrington Jr., MD, SFHM, discusses hospital medicine, value of diversity and teamwork
New SHM President Robert Harrington Jr., MD, SFHM, talks about his views on hospital medicine, the society and the value of diversity and teamwork.
New SHM President Robert Harrington Jr., MD, SFHM, talks about his views on hospital medicine, the society and the value of diversity and teamwork.
New SHM President Robert Harrington Jr., MD, SFHM, talks about his views on hospital medicine, the society and the value of diversity and teamwork.
VIDEO: Compliance plans, education can help physicians prevent Medicare fraud involvement
Medicare fraud and strategies to combat the crimes have become more intense as the program has grown in size and complexity, experts say.
As Medicare turns 50, Dr. Julie Taitsman, chief medical officer for the Department of Health & Human Services’ Office of Inspector General, discusses how doctors can avoid Medicare fraud. Dr. Taitsman shares common ways doctors and their billings come to the government’s attention and how doctors can fall prey to health fraud involvement.
In this exclusive video, Dr. Taitsman also discusses relevant health fraud laws that can impact physician practices and what doctors can expect of the OIG’s efforts to fight Medicare fraud in the future.
View the video interview on YouTube.
On Twitter @legal_med
Medicare fraud and strategies to combat the crimes have become more intense as the program has grown in size and complexity, experts say.
As Medicare turns 50, Dr. Julie Taitsman, chief medical officer for the Department of Health & Human Services’ Office of Inspector General, discusses how doctors can avoid Medicare fraud. Dr. Taitsman shares common ways doctors and their billings come to the government’s attention and how doctors can fall prey to health fraud involvement.
In this exclusive video, Dr. Taitsman also discusses relevant health fraud laws that can impact physician practices and what doctors can expect of the OIG’s efforts to fight Medicare fraud in the future.
View the video interview on YouTube.
On Twitter @legal_med
Medicare fraud and strategies to combat the crimes have become more intense as the program has grown in size and complexity, experts say.
As Medicare turns 50, Dr. Julie Taitsman, chief medical officer for the Department of Health & Human Services’ Office of Inspector General, discusses how doctors can avoid Medicare fraud. Dr. Taitsman shares common ways doctors and their billings come to the government’s attention and how doctors can fall prey to health fraud involvement.
In this exclusive video, Dr. Taitsman also discusses relevant health fraud laws that can impact physician practices and what doctors can expect of the OIG’s efforts to fight Medicare fraud in the future.
View the video interview on YouTube.
On Twitter @legal_med
Medicare at 50: Physicians struggle with antifraud regulations
For Dr. Carla L. Kakutani, it has become increasingly challenging to obtain durable medical equipment (DME) for her Medicare patients.
In addition to proving equipment is medically necessary, a 2013 rule requires physicians to document that a face-to-face encounter occurred between a patient and doctor or other health provider within 6 months of the DME order. (Enforcement of the rule has been delayed, but many physicians are currently complying with this policy.) Dr. Kakutani understands the added regulations are meant to prevent fraudulent billings, she said, but the heavy paperwork and additional red tape are burdensome.
“The problem is, [the process] turns into this back and forth between you, the equipment company, and Medicare,” said Dr. Kakutani, a family physician in Winters, Calif. “Meanwhile, the patient is waiting, and you’re being distracted from other things. The bad apples are making life rough for the rest of us.”
As Medicare turns 50 this year, Dr. Kakutani is not alone in her frustrations. In recent years, the U.S. Department of Health & Human Services has greatly expanded its efforts to combat Medicare fraud, and physicians across the country are feeling the effects.
The government’s primary antifraud tool is the Health Care Fraud Prevention and Enforcement Action Team (HEAT), created in 2009 to identify and investigate health fraud and abuse. CMS also works with an array of contractors to detect Medicare fraud, including comprehensive error rate testing (CERT) contractors, Medicare administrative contractors (MACs), Medicare drug integrity contractors (MEDICs), recovery audit program auditors (RACs), and zone program integrity contractors (ZPICs). In 2010, CMS launched the Fraud Prevention System (FPS), a predictive analytics technology that runs algorithms on all Medicare claims prior to payment. And in 2012, CMS created the Program Integrity Command Center that brings together investigators from Medicare, Medicaid, and the law enforcement community to develop predictive analytics that identify fraud and mobilize a rapid response.
Just how much Medicare fraud is happening at any given time is difficult to measure. In 2014, the federal government recouped $3 billion in Medicare- and Medicaid-related fraud settlements and judgments, according to an HHS analysis. In 2013 and 2012, the government recovered about $4 billion each year. And it’s nearly impossible to determine the volume of Medicare fraud committed by doctors, said Dr. Julie Taitsman, chief medical officer for the HHS Office of Inspector General.
“Getting at the actual amount of Medicare fraud in general, or Medicare fraud by physicians, is incredibly difficult,” Dr. Taitsman said in an interview. “We can tell you about the fraud we’ve identified, but we don’t know the total body of fraud.”
Dr. Taitsman stressed that all physicians play a major role in preventing health fraud and improving the quality of the Medicare system.
“Why it’s so important for physicians to practice with integrity – and we do believe that the vast majority of physicians practice with integrity – is because physicians control the bulk of care and services that [Medicare] patients receive,” Dr. Taitsman said. “That’s why it’s so important for physicians to be our partners in promoting high-quality care, promoting efficiency and compliance with the rules.”
But continually changing rules and guidelines make it difficult for many doctors to do just that, said Dr. James Szalados, an anesthesiologist and critical care physician based in Rochester, N.Y. Updates to payment rules, new OIG work plan targets, and growing documentation requirements can be overwhelming for practices.
“It’s not just the number of regulations, but it’s also the rate of change,” said Dr. Szalados, who is also an attorney. “For most doctors, it’s terrifying. They can’t keep up.”
Adhering to the latest regulations generally means hiring outside attorneys, consultants, and financial auditors who can help doctors self-police their practices, Dr. Szalados said.
Physicians also face Medicare fraud accusations from more directions than in the past, said Michael E. Clark, a Houston-based health law attorney and chair of the American Bar Association health law section. In addition to government claims, whistle-blower provisions under the False Claims Act allow individuals to file lawsuits alleging fraud and abuse on behalf of the government. If the government intervenes and the suit is successful, a whistle-blower can take home 15%-25% of money recovered. In 2014, the number of whistle-blower suits exceeded 700 for the second year in a row, according to the Department of Justice.
“A lot of people bringing these false claims actions are former or disgruntled employees or other doctors,” Mr. Clark said. “You might have a technical, regulatory type of theory, and yet it can be quickly changed into a fraud and abuse case.”
New laws have added to the challenge, Mr. Clark said. The Fraud Enforcement and Recovery Act (FERA), enacted in 2009, expands potential liability for false claims by applying the FCA to more entities and a larger range of transactions. The law also reduces the proof required to establish fault.
“FERA took away a lot of defenses that had been used successfully by defense counsel over the years on technical issues,” Mr. Clark said.
The antifraud climate has led many physicians to leave private practice or merge with hospitals or larger health systems, Dr. Szalados said. Other doctors have resorted to intentionally underbilling to avoid claim scrutiny, according to Dr. Robert A. Lee, who serves on the board of directors for the American Academy of Family Physicians . After a third-party compliance review, Dr. Lee’s private practice felt the best course of action was to bill more conservatively, he said.
“We kind of overdocument and undercode,” Dr. Lee said in an interview. “Of course that’s not fair to the physicians because they’re not billing for what they did do.”
On a more positive note, physicians are getting better at internal auditing and developing stronger compliance programs that address billing errors, said Alex T. Krouse, a health law attorney based in Mishawaka, Ind.
“I do think health care providers are getting more sophisticated and are really believing in the compliance-related function,” Mr. Krouse said in an interview. “That is helping and reducing the risk quite a bit.”
While antifraud enforcement will likely increase in the future, physicians that follow regulations and implement recommended protocols shouldn’t be too worried, Mr. Krouse added.
“If you’re a group, and you’re doing internal audits and you’ve got a compliance program in place, and you’re really working to have a compliant organization, the government’s aggressiveness and fraud detection is going to be minimal,” he said. “The aggressive tactics are really for those groups or organizations that have a blatant disregard for these processes.”
8 pro tips for avoiding fraud accusations
The possibility of coming under Medicare fraud scrutiny strikes fear in the heart of most physicians. Here’s what health law experts and federal officials recommend to stay in the clear:
• Designate a compliance officer. Assigning a specific employee to keep track of changing laws and regulations can help physicians remain compliant with antifraud regulations, said Mr. Krouse. The compliance officer should lead compliance efforts, inform staff of relevant rule changes, and take charge if billing practices come under government scrutiny.
• Retain a health law attorney. Seek the guidance of an experienced health law or Medicare fraud defense attorney should questions or billing problems arise, Mr. Clark recommended. Business or staff attorneys do not always have the needed expertise and can sometimes lead practices astray during critical times. Consider retaining a qualified, go-to health law attorney to answer questions and assist during crises.
• Develop a compliance program. Create strong compliance plans to address potential fraud, abuse, and billing issues, Dr. Taitsman advised. There is no one-size-fits all compliance plan, but the government offers suggested guidance about what plans should entail. No practice is too small to set up a compliance plan, she said.
• Perform internal audits. Internal audits should be a regular practice – annually or biennially – for all physicians, Mr. Krouse said. They can be completed by staff or a consultant.
• Send audit results to an attorney. If an internal audit is completed, the results should be conveyed first to an attorney, Mr. Clark said. Audit results shared directly with members of the medical practices are not privileged and could be communicated to the government. If an attorney shares audit results with physicians and practice leaders, the information is protected by the attorney-client privilege. The process limits the ability of staff members or disgruntled employees from sharing audit information or seeking whistle-blower claims.
• Build a strong disclosure protocol. The government is usually more lenient with health providers who are forthcoming about billing mistakes, Dr. Szalados said. Disclosing potential health fraud or billing errors can save the stress, time, and money associated with a government-initiated investigation. Under the Affordable Care Act, providers must return overpayments within 60 days of identifying them. Failing to report overpayments can lead to liability under the False Claims Act.
• Address billing errors immediately. If overbilling errors or systemic mistakes are found, doctors must do more than simply repay the government, Mr. Krouse said. Practices also must change their billing practices and develop an improvement plan. Have a process in place for how billing and coding issues will be addressed in the present and in the future, he recommended.
• Formulate a correction plan. Should a practice come under Medicare fraud suspicion, physicians should immediately analyze past billings. Conduct a thorough internal investigation that includes the extent of the problem and the scope of its threat to the practice, Mr. Krouse added. Create a corrective action plan and outline it to the government. A strong corrective plan goes a long way in negotiating settlements with the government, he said.
Various online resources are available to help physicians prevent Medicare fraud including a roadmap from CMS and guidance for new physicians by the OIG.
On Twitter @legal_med
For Dr. Carla L. Kakutani, it has become increasingly challenging to obtain durable medical equipment (DME) for her Medicare patients.
In addition to proving equipment is medically necessary, a 2013 rule requires physicians to document that a face-to-face encounter occurred between a patient and doctor or other health provider within 6 months of the DME order. (Enforcement of the rule has been delayed, but many physicians are currently complying with this policy.) Dr. Kakutani understands the added regulations are meant to prevent fraudulent billings, she said, but the heavy paperwork and additional red tape are burdensome.
“The problem is, [the process] turns into this back and forth between you, the equipment company, and Medicare,” said Dr. Kakutani, a family physician in Winters, Calif. “Meanwhile, the patient is waiting, and you’re being distracted from other things. The bad apples are making life rough for the rest of us.”
As Medicare turns 50 this year, Dr. Kakutani is not alone in her frustrations. In recent years, the U.S. Department of Health & Human Services has greatly expanded its efforts to combat Medicare fraud, and physicians across the country are feeling the effects.
The government’s primary antifraud tool is the Health Care Fraud Prevention and Enforcement Action Team (HEAT), created in 2009 to identify and investigate health fraud and abuse. CMS also works with an array of contractors to detect Medicare fraud, including comprehensive error rate testing (CERT) contractors, Medicare administrative contractors (MACs), Medicare drug integrity contractors (MEDICs), recovery audit program auditors (RACs), and zone program integrity contractors (ZPICs). In 2010, CMS launched the Fraud Prevention System (FPS), a predictive analytics technology that runs algorithms on all Medicare claims prior to payment. And in 2012, CMS created the Program Integrity Command Center that brings together investigators from Medicare, Medicaid, and the law enforcement community to develop predictive analytics that identify fraud and mobilize a rapid response.
Just how much Medicare fraud is happening at any given time is difficult to measure. In 2014, the federal government recouped $3 billion in Medicare- and Medicaid-related fraud settlements and judgments, according to an HHS analysis. In 2013 and 2012, the government recovered about $4 billion each year. And it’s nearly impossible to determine the volume of Medicare fraud committed by doctors, said Dr. Julie Taitsman, chief medical officer for the HHS Office of Inspector General.
“Getting at the actual amount of Medicare fraud in general, or Medicare fraud by physicians, is incredibly difficult,” Dr. Taitsman said in an interview. “We can tell you about the fraud we’ve identified, but we don’t know the total body of fraud.”
Dr. Taitsman stressed that all physicians play a major role in preventing health fraud and improving the quality of the Medicare system.
“Why it’s so important for physicians to practice with integrity – and we do believe that the vast majority of physicians practice with integrity – is because physicians control the bulk of care and services that [Medicare] patients receive,” Dr. Taitsman said. “That’s why it’s so important for physicians to be our partners in promoting high-quality care, promoting efficiency and compliance with the rules.”
But continually changing rules and guidelines make it difficult for many doctors to do just that, said Dr. James Szalados, an anesthesiologist and critical care physician based in Rochester, N.Y. Updates to payment rules, new OIG work plan targets, and growing documentation requirements can be overwhelming for practices.
“It’s not just the number of regulations, but it’s also the rate of change,” said Dr. Szalados, who is also an attorney. “For most doctors, it’s terrifying. They can’t keep up.”
Adhering to the latest regulations generally means hiring outside attorneys, consultants, and financial auditors who can help doctors self-police their practices, Dr. Szalados said.
Physicians also face Medicare fraud accusations from more directions than in the past, said Michael E. Clark, a Houston-based health law attorney and chair of the American Bar Association health law section. In addition to government claims, whistle-blower provisions under the False Claims Act allow individuals to file lawsuits alleging fraud and abuse on behalf of the government. If the government intervenes and the suit is successful, a whistle-blower can take home 15%-25% of money recovered. In 2014, the number of whistle-blower suits exceeded 700 for the second year in a row, according to the Department of Justice.
“A lot of people bringing these false claims actions are former or disgruntled employees or other doctors,” Mr. Clark said. “You might have a technical, regulatory type of theory, and yet it can be quickly changed into a fraud and abuse case.”
New laws have added to the challenge, Mr. Clark said. The Fraud Enforcement and Recovery Act (FERA), enacted in 2009, expands potential liability for false claims by applying the FCA to more entities and a larger range of transactions. The law also reduces the proof required to establish fault.
“FERA took away a lot of defenses that had been used successfully by defense counsel over the years on technical issues,” Mr. Clark said.
The antifraud climate has led many physicians to leave private practice or merge with hospitals or larger health systems, Dr. Szalados said. Other doctors have resorted to intentionally underbilling to avoid claim scrutiny, according to Dr. Robert A. Lee, who serves on the board of directors for the American Academy of Family Physicians . After a third-party compliance review, Dr. Lee’s private practice felt the best course of action was to bill more conservatively, he said.
“We kind of overdocument and undercode,” Dr. Lee said in an interview. “Of course that’s not fair to the physicians because they’re not billing for what they did do.”
On a more positive note, physicians are getting better at internal auditing and developing stronger compliance programs that address billing errors, said Alex T. Krouse, a health law attorney based in Mishawaka, Ind.
“I do think health care providers are getting more sophisticated and are really believing in the compliance-related function,” Mr. Krouse said in an interview. “That is helping and reducing the risk quite a bit.”
While antifraud enforcement will likely increase in the future, physicians that follow regulations and implement recommended protocols shouldn’t be too worried, Mr. Krouse added.
“If you’re a group, and you’re doing internal audits and you’ve got a compliance program in place, and you’re really working to have a compliant organization, the government’s aggressiveness and fraud detection is going to be minimal,” he said. “The aggressive tactics are really for those groups or organizations that have a blatant disregard for these processes.”
8 pro tips for avoiding fraud accusations
The possibility of coming under Medicare fraud scrutiny strikes fear in the heart of most physicians. Here’s what health law experts and federal officials recommend to stay in the clear:
• Designate a compliance officer. Assigning a specific employee to keep track of changing laws and regulations can help physicians remain compliant with antifraud regulations, said Mr. Krouse. The compliance officer should lead compliance efforts, inform staff of relevant rule changes, and take charge if billing practices come under government scrutiny.
• Retain a health law attorney. Seek the guidance of an experienced health law or Medicare fraud defense attorney should questions or billing problems arise, Mr. Clark recommended. Business or staff attorneys do not always have the needed expertise and can sometimes lead practices astray during critical times. Consider retaining a qualified, go-to health law attorney to answer questions and assist during crises.
• Develop a compliance program. Create strong compliance plans to address potential fraud, abuse, and billing issues, Dr. Taitsman advised. There is no one-size-fits all compliance plan, but the government offers suggested guidance about what plans should entail. No practice is too small to set up a compliance plan, she said.
• Perform internal audits. Internal audits should be a regular practice – annually or biennially – for all physicians, Mr. Krouse said. They can be completed by staff or a consultant.
• Send audit results to an attorney. If an internal audit is completed, the results should be conveyed first to an attorney, Mr. Clark said. Audit results shared directly with members of the medical practices are not privileged and could be communicated to the government. If an attorney shares audit results with physicians and practice leaders, the information is protected by the attorney-client privilege. The process limits the ability of staff members or disgruntled employees from sharing audit information or seeking whistle-blower claims.
• Build a strong disclosure protocol. The government is usually more lenient with health providers who are forthcoming about billing mistakes, Dr. Szalados said. Disclosing potential health fraud or billing errors can save the stress, time, and money associated with a government-initiated investigation. Under the Affordable Care Act, providers must return overpayments within 60 days of identifying them. Failing to report overpayments can lead to liability under the False Claims Act.
• Address billing errors immediately. If overbilling errors or systemic mistakes are found, doctors must do more than simply repay the government, Mr. Krouse said. Practices also must change their billing practices and develop an improvement plan. Have a process in place for how billing and coding issues will be addressed in the present and in the future, he recommended.
• Formulate a correction plan. Should a practice come under Medicare fraud suspicion, physicians should immediately analyze past billings. Conduct a thorough internal investigation that includes the extent of the problem and the scope of its threat to the practice, Mr. Krouse added. Create a corrective action plan and outline it to the government. A strong corrective plan goes a long way in negotiating settlements with the government, he said.
Various online resources are available to help physicians prevent Medicare fraud including a roadmap from CMS and guidance for new physicians by the OIG.
On Twitter @legal_med
For Dr. Carla L. Kakutani, it has become increasingly challenging to obtain durable medical equipment (DME) for her Medicare patients.
In addition to proving equipment is medically necessary, a 2013 rule requires physicians to document that a face-to-face encounter occurred between a patient and doctor or other health provider within 6 months of the DME order. (Enforcement of the rule has been delayed, but many physicians are currently complying with this policy.) Dr. Kakutani understands the added regulations are meant to prevent fraudulent billings, she said, but the heavy paperwork and additional red tape are burdensome.
“The problem is, [the process] turns into this back and forth between you, the equipment company, and Medicare,” said Dr. Kakutani, a family physician in Winters, Calif. “Meanwhile, the patient is waiting, and you’re being distracted from other things. The bad apples are making life rough for the rest of us.”
As Medicare turns 50 this year, Dr. Kakutani is not alone in her frustrations. In recent years, the U.S. Department of Health & Human Services has greatly expanded its efforts to combat Medicare fraud, and physicians across the country are feeling the effects.
The government’s primary antifraud tool is the Health Care Fraud Prevention and Enforcement Action Team (HEAT), created in 2009 to identify and investigate health fraud and abuse. CMS also works with an array of contractors to detect Medicare fraud, including comprehensive error rate testing (CERT) contractors, Medicare administrative contractors (MACs), Medicare drug integrity contractors (MEDICs), recovery audit program auditors (RACs), and zone program integrity contractors (ZPICs). In 2010, CMS launched the Fraud Prevention System (FPS), a predictive analytics technology that runs algorithms on all Medicare claims prior to payment. And in 2012, CMS created the Program Integrity Command Center that brings together investigators from Medicare, Medicaid, and the law enforcement community to develop predictive analytics that identify fraud and mobilize a rapid response.
Just how much Medicare fraud is happening at any given time is difficult to measure. In 2014, the federal government recouped $3 billion in Medicare- and Medicaid-related fraud settlements and judgments, according to an HHS analysis. In 2013 and 2012, the government recovered about $4 billion each year. And it’s nearly impossible to determine the volume of Medicare fraud committed by doctors, said Dr. Julie Taitsman, chief medical officer for the HHS Office of Inspector General.
“Getting at the actual amount of Medicare fraud in general, or Medicare fraud by physicians, is incredibly difficult,” Dr. Taitsman said in an interview. “We can tell you about the fraud we’ve identified, but we don’t know the total body of fraud.”
Dr. Taitsman stressed that all physicians play a major role in preventing health fraud and improving the quality of the Medicare system.
“Why it’s so important for physicians to practice with integrity – and we do believe that the vast majority of physicians practice with integrity – is because physicians control the bulk of care and services that [Medicare] patients receive,” Dr. Taitsman said. “That’s why it’s so important for physicians to be our partners in promoting high-quality care, promoting efficiency and compliance with the rules.”
But continually changing rules and guidelines make it difficult for many doctors to do just that, said Dr. James Szalados, an anesthesiologist and critical care physician based in Rochester, N.Y. Updates to payment rules, new OIG work plan targets, and growing documentation requirements can be overwhelming for practices.
“It’s not just the number of regulations, but it’s also the rate of change,” said Dr. Szalados, who is also an attorney. “For most doctors, it’s terrifying. They can’t keep up.”
Adhering to the latest regulations generally means hiring outside attorneys, consultants, and financial auditors who can help doctors self-police their practices, Dr. Szalados said.
Physicians also face Medicare fraud accusations from more directions than in the past, said Michael E. Clark, a Houston-based health law attorney and chair of the American Bar Association health law section. In addition to government claims, whistle-blower provisions under the False Claims Act allow individuals to file lawsuits alleging fraud and abuse on behalf of the government. If the government intervenes and the suit is successful, a whistle-blower can take home 15%-25% of money recovered. In 2014, the number of whistle-blower suits exceeded 700 for the second year in a row, according to the Department of Justice.
“A lot of people bringing these false claims actions are former or disgruntled employees or other doctors,” Mr. Clark said. “You might have a technical, regulatory type of theory, and yet it can be quickly changed into a fraud and abuse case.”
New laws have added to the challenge, Mr. Clark said. The Fraud Enforcement and Recovery Act (FERA), enacted in 2009, expands potential liability for false claims by applying the FCA to more entities and a larger range of transactions. The law also reduces the proof required to establish fault.
“FERA took away a lot of defenses that had been used successfully by defense counsel over the years on technical issues,” Mr. Clark said.
The antifraud climate has led many physicians to leave private practice or merge with hospitals or larger health systems, Dr. Szalados said. Other doctors have resorted to intentionally underbilling to avoid claim scrutiny, according to Dr. Robert A. Lee, who serves on the board of directors for the American Academy of Family Physicians . After a third-party compliance review, Dr. Lee’s private practice felt the best course of action was to bill more conservatively, he said.
“We kind of overdocument and undercode,” Dr. Lee said in an interview. “Of course that’s not fair to the physicians because they’re not billing for what they did do.”
On a more positive note, physicians are getting better at internal auditing and developing stronger compliance programs that address billing errors, said Alex T. Krouse, a health law attorney based in Mishawaka, Ind.
“I do think health care providers are getting more sophisticated and are really believing in the compliance-related function,” Mr. Krouse said in an interview. “That is helping and reducing the risk quite a bit.”
While antifraud enforcement will likely increase in the future, physicians that follow regulations and implement recommended protocols shouldn’t be too worried, Mr. Krouse added.
“If you’re a group, and you’re doing internal audits and you’ve got a compliance program in place, and you’re really working to have a compliant organization, the government’s aggressiveness and fraud detection is going to be minimal,” he said. “The aggressive tactics are really for those groups or organizations that have a blatant disregard for these processes.”
8 pro tips for avoiding fraud accusations
The possibility of coming under Medicare fraud scrutiny strikes fear in the heart of most physicians. Here’s what health law experts and federal officials recommend to stay in the clear:
• Designate a compliance officer. Assigning a specific employee to keep track of changing laws and regulations can help physicians remain compliant with antifraud regulations, said Mr. Krouse. The compliance officer should lead compliance efforts, inform staff of relevant rule changes, and take charge if billing practices come under government scrutiny.
• Retain a health law attorney. Seek the guidance of an experienced health law or Medicare fraud defense attorney should questions or billing problems arise, Mr. Clark recommended. Business or staff attorneys do not always have the needed expertise and can sometimes lead practices astray during critical times. Consider retaining a qualified, go-to health law attorney to answer questions and assist during crises.
• Develop a compliance program. Create strong compliance plans to address potential fraud, abuse, and billing issues, Dr. Taitsman advised. There is no one-size-fits all compliance plan, but the government offers suggested guidance about what plans should entail. No practice is too small to set up a compliance plan, she said.
• Perform internal audits. Internal audits should be a regular practice – annually or biennially – for all physicians, Mr. Krouse said. They can be completed by staff or a consultant.
• Send audit results to an attorney. If an internal audit is completed, the results should be conveyed first to an attorney, Mr. Clark said. Audit results shared directly with members of the medical practices are not privileged and could be communicated to the government. If an attorney shares audit results with physicians and practice leaders, the information is protected by the attorney-client privilege. The process limits the ability of staff members or disgruntled employees from sharing audit information or seeking whistle-blower claims.
• Build a strong disclosure protocol. The government is usually more lenient with health providers who are forthcoming about billing mistakes, Dr. Szalados said. Disclosing potential health fraud or billing errors can save the stress, time, and money associated with a government-initiated investigation. Under the Affordable Care Act, providers must return overpayments within 60 days of identifying them. Failing to report overpayments can lead to liability under the False Claims Act.
• Address billing errors immediately. If overbilling errors or systemic mistakes are found, doctors must do more than simply repay the government, Mr. Krouse said. Practices also must change their billing practices and develop an improvement plan. Have a process in place for how billing and coding issues will be addressed in the present and in the future, he recommended.
• Formulate a correction plan. Should a practice come under Medicare fraud suspicion, physicians should immediately analyze past billings. Conduct a thorough internal investigation that includes the extent of the problem and the scope of its threat to the practice, Mr. Krouse added. Create a corrective action plan and outline it to the government. A strong corrective plan goes a long way in negotiating settlements with the government, he said.
Various online resources are available to help physicians prevent Medicare fraud including a roadmap from CMS and guidance for new physicians by the OIG.
On Twitter @legal_med
New state litigation challenges physicians’ authority to regulate nonphysicians
The conflict between physicians and nonphysicians over how scope of practice should be regulated is heating up as a new antitrust challenge pits a medical board against a pain clinic.
The owners of Axcess Medical Clinic Inc. are suing the Mississippi State Board of Medical Licensure over a rule that requires pain clinics be owned by a hospital or licensed physician. The clinic claims the rule is anticompetitive and forced it to close, according to a lawsuit filed April 24 in U.S. District Court for the Southern District of Mississippi.
The lawsuit follows a February decision by the U.S. Supreme Court against a local dental board that attempted to stop nonprofessionals from providing teeth-whitening services. The Justices ruled the dental board had violated federal antitrust regulations because the board was not adequately supervised by the state. At the time, physician leaders worried the high court ruling could generate further lawsuits and alter state medical boards’ ability to regulate scope of practice.
The Mississippi case stems from a 2011 board rule that requires pain management clinics to be owned or operated by a hospital or licensed physician. The rule also requires that pain management clinics register with the board before doing business. Then-owner of Axcess Medical Clinic, Kenneth Charles Knight, requested that the clinic be grandfathered against complying with the rule because it opened in 2010, according to court records. The lawsuit claims the board failed to address the request, and Mr. Knight was forced to sell his ownership to a physician to salvage his investment. The physician later rescinded the purchase and the shares reverted back to Mr. Knight.
In 2012, Mr. Knight divested his majority ownership to family physician Dr. Fitzhugh L. Neal Jr., according to court documents. The board approved the clinic’s registration, but later requested more information about the physician’s proof of ownership. According to the lawsuit, the board found the physician was practicing pain management without proper qualifications and did not renew its registration. The clinic temporarily closed, but reopened a month later with a new registration, court documents state. In 2013, the licensure board issued new education and certification requirements for physicians to practice pain management. The requirements forced Axcess Medical Clinic to permanently close, the lawsuit states.
Plaintiffs Mr. Knight and Dr. Neal claim the board violated state and federal antitrust regulations by engaging in anticompetitive activities that deprived patients of choice. The suit also alleges that the board is made up of market participants who are not adequately supervised by the state.
An attorney for Axcess Medical Clinic said he could not provide timely comment on the case.
Dr. H. Vann Craig, executive director for the Mississippi State Board of Medical Licensure declined to comment on details of the litigation, but defended the board’s general practices. He noted that he is not aware of any Federal Trade Commission interest in the case.
“Our process is we try to deal with physicians and make sure they’re qualified to be doing what they are doing,” he said in an interview.
The board, which will be represented by the Mississippi Attorney General’s office, has not yet issued a formal response to the lawsuit.
The vagueness of the Supreme Court’s decision opened the door for further legal challenges, according to Joshua Prober, senior vice president and general counsel for the American Osteopathic Association (AOA). The high court’s decision found North Carolina’s model for state licensing board regulation did not provide for sufficient state oversight of a board made up of market competitors, but the ruling does not provide clear guidance on what’s expected from state governments in structuring state licensing boards, he said.
“Instead, it said its inquiry would be ‘flexible and context dependent,’ which appears to invite challenges to structures used in other states,” he said. “Because antitrust litigation provides that a successful plaintiff can recover treble damages, there can be a generous payoff for a successful challenge.”
On Twitter @legal_med
The conflict between physicians and nonphysicians over how scope of practice should be regulated is heating up as a new antitrust challenge pits a medical board against a pain clinic.
The owners of Axcess Medical Clinic Inc. are suing the Mississippi State Board of Medical Licensure over a rule that requires pain clinics be owned by a hospital or licensed physician. The clinic claims the rule is anticompetitive and forced it to close, according to a lawsuit filed April 24 in U.S. District Court for the Southern District of Mississippi.
The lawsuit follows a February decision by the U.S. Supreme Court against a local dental board that attempted to stop nonprofessionals from providing teeth-whitening services. The Justices ruled the dental board had violated federal antitrust regulations because the board was not adequately supervised by the state. At the time, physician leaders worried the high court ruling could generate further lawsuits and alter state medical boards’ ability to regulate scope of practice.
The Mississippi case stems from a 2011 board rule that requires pain management clinics to be owned or operated by a hospital or licensed physician. The rule also requires that pain management clinics register with the board before doing business. Then-owner of Axcess Medical Clinic, Kenneth Charles Knight, requested that the clinic be grandfathered against complying with the rule because it opened in 2010, according to court records. The lawsuit claims the board failed to address the request, and Mr. Knight was forced to sell his ownership to a physician to salvage his investment. The physician later rescinded the purchase and the shares reverted back to Mr. Knight.
In 2012, Mr. Knight divested his majority ownership to family physician Dr. Fitzhugh L. Neal Jr., according to court documents. The board approved the clinic’s registration, but later requested more information about the physician’s proof of ownership. According to the lawsuit, the board found the physician was practicing pain management without proper qualifications and did not renew its registration. The clinic temporarily closed, but reopened a month later with a new registration, court documents state. In 2013, the licensure board issued new education and certification requirements for physicians to practice pain management. The requirements forced Axcess Medical Clinic to permanently close, the lawsuit states.
Plaintiffs Mr. Knight and Dr. Neal claim the board violated state and federal antitrust regulations by engaging in anticompetitive activities that deprived patients of choice. The suit also alleges that the board is made up of market participants who are not adequately supervised by the state.
An attorney for Axcess Medical Clinic said he could not provide timely comment on the case.
Dr. H. Vann Craig, executive director for the Mississippi State Board of Medical Licensure declined to comment on details of the litigation, but defended the board’s general practices. He noted that he is not aware of any Federal Trade Commission interest in the case.
“Our process is we try to deal with physicians and make sure they’re qualified to be doing what they are doing,” he said in an interview.
The board, which will be represented by the Mississippi Attorney General’s office, has not yet issued a formal response to the lawsuit.
The vagueness of the Supreme Court’s decision opened the door for further legal challenges, according to Joshua Prober, senior vice president and general counsel for the American Osteopathic Association (AOA). The high court’s decision found North Carolina’s model for state licensing board regulation did not provide for sufficient state oversight of a board made up of market competitors, but the ruling does not provide clear guidance on what’s expected from state governments in structuring state licensing boards, he said.
“Instead, it said its inquiry would be ‘flexible and context dependent,’ which appears to invite challenges to structures used in other states,” he said. “Because antitrust litigation provides that a successful plaintiff can recover treble damages, there can be a generous payoff for a successful challenge.”
On Twitter @legal_med
The conflict between physicians and nonphysicians over how scope of practice should be regulated is heating up as a new antitrust challenge pits a medical board against a pain clinic.
The owners of Axcess Medical Clinic Inc. are suing the Mississippi State Board of Medical Licensure over a rule that requires pain clinics be owned by a hospital or licensed physician. The clinic claims the rule is anticompetitive and forced it to close, according to a lawsuit filed April 24 in U.S. District Court for the Southern District of Mississippi.
The lawsuit follows a February decision by the U.S. Supreme Court against a local dental board that attempted to stop nonprofessionals from providing teeth-whitening services. The Justices ruled the dental board had violated federal antitrust regulations because the board was not adequately supervised by the state. At the time, physician leaders worried the high court ruling could generate further lawsuits and alter state medical boards’ ability to regulate scope of practice.
The Mississippi case stems from a 2011 board rule that requires pain management clinics to be owned or operated by a hospital or licensed physician. The rule also requires that pain management clinics register with the board before doing business. Then-owner of Axcess Medical Clinic, Kenneth Charles Knight, requested that the clinic be grandfathered against complying with the rule because it opened in 2010, according to court records. The lawsuit claims the board failed to address the request, and Mr. Knight was forced to sell his ownership to a physician to salvage his investment. The physician later rescinded the purchase and the shares reverted back to Mr. Knight.
In 2012, Mr. Knight divested his majority ownership to family physician Dr. Fitzhugh L. Neal Jr., according to court documents. The board approved the clinic’s registration, but later requested more information about the physician’s proof of ownership. According to the lawsuit, the board found the physician was practicing pain management without proper qualifications and did not renew its registration. The clinic temporarily closed, but reopened a month later with a new registration, court documents state. In 2013, the licensure board issued new education and certification requirements for physicians to practice pain management. The requirements forced Axcess Medical Clinic to permanently close, the lawsuit states.
Plaintiffs Mr. Knight and Dr. Neal claim the board violated state and federal antitrust regulations by engaging in anticompetitive activities that deprived patients of choice. The suit also alleges that the board is made up of market participants who are not adequately supervised by the state.
An attorney for Axcess Medical Clinic said he could not provide timely comment on the case.
Dr. H. Vann Craig, executive director for the Mississippi State Board of Medical Licensure declined to comment on details of the litigation, but defended the board’s general practices. He noted that he is not aware of any Federal Trade Commission interest in the case.
“Our process is we try to deal with physicians and make sure they’re qualified to be doing what they are doing,” he said in an interview.
The board, which will be represented by the Mississippi Attorney General’s office, has not yet issued a formal response to the lawsuit.
The vagueness of the Supreme Court’s decision opened the door for further legal challenges, according to Joshua Prober, senior vice president and general counsel for the American Osteopathic Association (AOA). The high court’s decision found North Carolina’s model for state licensing board regulation did not provide for sufficient state oversight of a board made up of market competitors, but the ruling does not provide clear guidance on what’s expected from state governments in structuring state licensing boards, he said.
“Instead, it said its inquiry would be ‘flexible and context dependent,’ which appears to invite challenges to structures used in other states,” he said. “Because antitrust litigation provides that a successful plaintiff can recover treble damages, there can be a generous payoff for a successful challenge.”
On Twitter @legal_med
HIMSS15: Doctors can develop patient engagement platforms through strong partnerships
CHICAGO – For Margaret Mary Health in Batesville, Ind., partnerships were central to the formation of its community-wide patient portal.
In 2012, the hospital launched a portal that combines the records and information of multiple health providers in southeast Indiana and surrounding areas into a single system that patients can access. The approach departs from a standard portal model in which each physician practice has its own portal and patients must assess their health information from multiple sources, according to Dr. Jeffrey Hatcher, a Batesville ob.gyn and medical staff liaison for Margaret Mary Health.
“The whole goal of electronic records was to consolidate and centralize and streamline health care records,” Dr. Hatcher said in an interview. “In a lot of ways, what we’re doing is just building on that process. We’ve eliminated the need for all of those individual portals and connected the patients and their physicians to the health information exchange (HIE). Those practices feed the information through the HIE into the patient’s chart.”
Margaret Mary began efforts to design its portal in early 2011. The hospital partnered with NoMoreClipboard, a company that offers patient engagement tools to health providers, and HealthBridge, a nonprofit corporation that supports health information technology adoption and health information exchange (HIE). The timing was perfect, Dr. Hatcher said, because NoMoreClipboard and Indiana Health Information Technology Inc. (IHIT) had just received a joint $1.5 million grant from the Office of the National Coordinator for Health Information Technology (ONC) to develop, deploy, and pilot test solutions that enable patients to access electronic health information exchange data.
Despite a knowledgeable design team, the road to Margaret Mary’s united provider portal was strewn with bumps and obstacles, Dr. Hatcher said at the annual meeting of the Healthcare Information and Management Systems Society (HIMSS). Developers encountered skepticism from some health providers and received push back from electronic health record (EHR) vendors.
The vendors’ “excitement to participate and help us develop this was not as great because it basically took the place of their product,” Dr. Hatcher said in an interview. “It’s a really slow process to get them to cooperate. They’re just not willing to move things along at a pace that’s rapid enough.”
Dr. Hatcher’s team worked to gain the trust of each participant. One key was ensuring that each provider was comfortable with what medical information would be released and when, and what type of sensitive information should be withheld and for how long, he said. Portal developers also had to create policies for the system and take into account the various data access rules of patients’ home states – including Indiana, Ohio, and Kentucky.
There were privacy issues as well. While the hospital serves a regional population of 70,000, it is situated in the rural community of Batesville, a town of 7,000. Residents in the small community historically have passed down identical first and last names for several generations leading to four or five people in the community with the same name, according to a case study on the project by NoMoreClipboard.
To address the situation, development experts created standards-based policies to securely match consumers with their data, and once authenticated, transport those data into patients’ personal health record.
Since the portal launched in 2012, 18,000 patients have accepted their access codes and about 5,000 patient have used the portal, Dr. Hatcher said. Because the portal links to HealthBridge, patients are able to get data from across the continuum of care, whether or not they receive the care at Margaret Mary. HealthBridge serves southwest Ohio, southeast Indiana and northern Kentucky. Additionally, several Cincinnati hospitals have authorized sharing their HIE data with Margaret Mary patients who use the portal.
No hard numbers on the portal’s impact yet exist, but providers have noted an increase in productivity and a rise in patient satisfaction, Dr. Hatcher said.
“When you look at the care perspective, it’s changed the dynamics of the conversations we’re having,” he said. “When patients get data, we can point them to trusted websites and they can come in prepared. The follow-up appointment becomes more of a discussion and not a lab review. Now you’re spending [more] time planning care.”
Dr. Hatcher encourages other physicians and health systems to participate in such patient engagement efforts, especially as Stage 3 of meaningful use approaches. The Centers for Medicare & Medicaid Services has proposed that all physicians and hospitals meet Stage 3 meaningful use requirements beginning in 2018. The proposed rule also calls for 25% of patients to access their data, although it allows for third-party providers to access a patient’s account as a means of satisfying the requirement.
“As we begin this heath care–sharing process, it’s really important to have patients in a position where they’re more educated about the process that’s going on with them,” Dr. Hatcher said in an interview. “The more you educate your patients, the more it helps them embrace what you’re trying to do. It’ll be hard to meet the upcoming meaningful use measures if you don’t have patients engaged in their health care plan.”
Health providers interested in creating a similar patient portal should review what other health systems have done in the past and build on their ideas, Dr. Hatcher added.
“You’ve got to have the enthusiasm of your medical staff,” he said. “You’ve got to have the support of your organization, and you have to have a vision. Know what you want before you start. If you do that, then you’re well on your way.”
On Twitter @legal_med
CHICAGO – For Margaret Mary Health in Batesville, Ind., partnerships were central to the formation of its community-wide patient portal.
In 2012, the hospital launched a portal that combines the records and information of multiple health providers in southeast Indiana and surrounding areas into a single system that patients can access. The approach departs from a standard portal model in which each physician practice has its own portal and patients must assess their health information from multiple sources, according to Dr. Jeffrey Hatcher, a Batesville ob.gyn and medical staff liaison for Margaret Mary Health.
“The whole goal of electronic records was to consolidate and centralize and streamline health care records,” Dr. Hatcher said in an interview. “In a lot of ways, what we’re doing is just building on that process. We’ve eliminated the need for all of those individual portals and connected the patients and their physicians to the health information exchange (HIE). Those practices feed the information through the HIE into the patient’s chart.”
Margaret Mary began efforts to design its portal in early 2011. The hospital partnered with NoMoreClipboard, a company that offers patient engagement tools to health providers, and HealthBridge, a nonprofit corporation that supports health information technology adoption and health information exchange (HIE). The timing was perfect, Dr. Hatcher said, because NoMoreClipboard and Indiana Health Information Technology Inc. (IHIT) had just received a joint $1.5 million grant from the Office of the National Coordinator for Health Information Technology (ONC) to develop, deploy, and pilot test solutions that enable patients to access electronic health information exchange data.
Despite a knowledgeable design team, the road to Margaret Mary’s united provider portal was strewn with bumps and obstacles, Dr. Hatcher said at the annual meeting of the Healthcare Information and Management Systems Society (HIMSS). Developers encountered skepticism from some health providers and received push back from electronic health record (EHR) vendors.
The vendors’ “excitement to participate and help us develop this was not as great because it basically took the place of their product,” Dr. Hatcher said in an interview. “It’s a really slow process to get them to cooperate. They’re just not willing to move things along at a pace that’s rapid enough.”
Dr. Hatcher’s team worked to gain the trust of each participant. One key was ensuring that each provider was comfortable with what medical information would be released and when, and what type of sensitive information should be withheld and for how long, he said. Portal developers also had to create policies for the system and take into account the various data access rules of patients’ home states – including Indiana, Ohio, and Kentucky.
There were privacy issues as well. While the hospital serves a regional population of 70,000, it is situated in the rural community of Batesville, a town of 7,000. Residents in the small community historically have passed down identical first and last names for several generations leading to four or five people in the community with the same name, according to a case study on the project by NoMoreClipboard.
To address the situation, development experts created standards-based policies to securely match consumers with their data, and once authenticated, transport those data into patients’ personal health record.
Since the portal launched in 2012, 18,000 patients have accepted their access codes and about 5,000 patient have used the portal, Dr. Hatcher said. Because the portal links to HealthBridge, patients are able to get data from across the continuum of care, whether or not they receive the care at Margaret Mary. HealthBridge serves southwest Ohio, southeast Indiana and northern Kentucky. Additionally, several Cincinnati hospitals have authorized sharing their HIE data with Margaret Mary patients who use the portal.
No hard numbers on the portal’s impact yet exist, but providers have noted an increase in productivity and a rise in patient satisfaction, Dr. Hatcher said.
“When you look at the care perspective, it’s changed the dynamics of the conversations we’re having,” he said. “When patients get data, we can point them to trusted websites and they can come in prepared. The follow-up appointment becomes more of a discussion and not a lab review. Now you’re spending [more] time planning care.”
Dr. Hatcher encourages other physicians and health systems to participate in such patient engagement efforts, especially as Stage 3 of meaningful use approaches. The Centers for Medicare & Medicaid Services has proposed that all physicians and hospitals meet Stage 3 meaningful use requirements beginning in 2018. The proposed rule also calls for 25% of patients to access their data, although it allows for third-party providers to access a patient’s account as a means of satisfying the requirement.
“As we begin this heath care–sharing process, it’s really important to have patients in a position where they’re more educated about the process that’s going on with them,” Dr. Hatcher said in an interview. “The more you educate your patients, the more it helps them embrace what you’re trying to do. It’ll be hard to meet the upcoming meaningful use measures if you don’t have patients engaged in their health care plan.”
Health providers interested in creating a similar patient portal should review what other health systems have done in the past and build on their ideas, Dr. Hatcher added.
“You’ve got to have the enthusiasm of your medical staff,” he said. “You’ve got to have the support of your organization, and you have to have a vision. Know what you want before you start. If you do that, then you’re well on your way.”
On Twitter @legal_med
CHICAGO – For Margaret Mary Health in Batesville, Ind., partnerships were central to the formation of its community-wide patient portal.
In 2012, the hospital launched a portal that combines the records and information of multiple health providers in southeast Indiana and surrounding areas into a single system that patients can access. The approach departs from a standard portal model in which each physician practice has its own portal and patients must assess their health information from multiple sources, according to Dr. Jeffrey Hatcher, a Batesville ob.gyn and medical staff liaison for Margaret Mary Health.
“The whole goal of electronic records was to consolidate and centralize and streamline health care records,” Dr. Hatcher said in an interview. “In a lot of ways, what we’re doing is just building on that process. We’ve eliminated the need for all of those individual portals and connected the patients and their physicians to the health information exchange (HIE). Those practices feed the information through the HIE into the patient’s chart.”
Margaret Mary began efforts to design its portal in early 2011. The hospital partnered with NoMoreClipboard, a company that offers patient engagement tools to health providers, and HealthBridge, a nonprofit corporation that supports health information technology adoption and health information exchange (HIE). The timing was perfect, Dr. Hatcher said, because NoMoreClipboard and Indiana Health Information Technology Inc. (IHIT) had just received a joint $1.5 million grant from the Office of the National Coordinator for Health Information Technology (ONC) to develop, deploy, and pilot test solutions that enable patients to access electronic health information exchange data.
Despite a knowledgeable design team, the road to Margaret Mary’s united provider portal was strewn with bumps and obstacles, Dr. Hatcher said at the annual meeting of the Healthcare Information and Management Systems Society (HIMSS). Developers encountered skepticism from some health providers and received push back from electronic health record (EHR) vendors.
The vendors’ “excitement to participate and help us develop this was not as great because it basically took the place of their product,” Dr. Hatcher said in an interview. “It’s a really slow process to get them to cooperate. They’re just not willing to move things along at a pace that’s rapid enough.”
Dr. Hatcher’s team worked to gain the trust of each participant. One key was ensuring that each provider was comfortable with what medical information would be released and when, and what type of sensitive information should be withheld and for how long, he said. Portal developers also had to create policies for the system and take into account the various data access rules of patients’ home states – including Indiana, Ohio, and Kentucky.
There were privacy issues as well. While the hospital serves a regional population of 70,000, it is situated in the rural community of Batesville, a town of 7,000. Residents in the small community historically have passed down identical first and last names for several generations leading to four or five people in the community with the same name, according to a case study on the project by NoMoreClipboard.
To address the situation, development experts created standards-based policies to securely match consumers with their data, and once authenticated, transport those data into patients’ personal health record.
Since the portal launched in 2012, 18,000 patients have accepted their access codes and about 5,000 patient have used the portal, Dr. Hatcher said. Because the portal links to HealthBridge, patients are able to get data from across the continuum of care, whether or not they receive the care at Margaret Mary. HealthBridge serves southwest Ohio, southeast Indiana and northern Kentucky. Additionally, several Cincinnati hospitals have authorized sharing their HIE data with Margaret Mary patients who use the portal.
No hard numbers on the portal’s impact yet exist, but providers have noted an increase in productivity and a rise in patient satisfaction, Dr. Hatcher said.
“When you look at the care perspective, it’s changed the dynamics of the conversations we’re having,” he said. “When patients get data, we can point them to trusted websites and they can come in prepared. The follow-up appointment becomes more of a discussion and not a lab review. Now you’re spending [more] time planning care.”
Dr. Hatcher encourages other physicians and health systems to participate in such patient engagement efforts, especially as Stage 3 of meaningful use approaches. The Centers for Medicare & Medicaid Services has proposed that all physicians and hospitals meet Stage 3 meaningful use requirements beginning in 2018. The proposed rule also calls for 25% of patients to access their data, although it allows for third-party providers to access a patient’s account as a means of satisfying the requirement.
“As we begin this heath care–sharing process, it’s really important to have patients in a position where they’re more educated about the process that’s going on with them,” Dr. Hatcher said in an interview. “The more you educate your patients, the more it helps them embrace what you’re trying to do. It’ll be hard to meet the upcoming meaningful use measures if you don’t have patients engaged in their health care plan.”
Health providers interested in creating a similar patient portal should review what other health systems have done in the past and build on their ideas, Dr. Hatcher added.
“You’ve got to have the enthusiasm of your medical staff,” he said. “You’ve got to have the support of your organization, and you have to have a vision. Know what you want before you start. If you do that, then you’re well on your way.”
On Twitter @legal_med
AT HIMSS15
More physicians support Democratic candidates
Most U.S. physicians who made political contributions during the 2013-2014 congressional election cycle donated to Democrats, continuing the trend away from Republicans that was first noted among medical professionals between 1991 and 2012, according to a report published April 27 in JAMA Internal Medicine.
In an analysis of physicians’ federal political contributions, 55% of contributors donated to Democrats and 45% to Republicans during the most recent congressional election cycle. In contrast, general public support resulted in the “Republican surge” in which conservatives gained nine Senate seats and increased their majority in the House, said Adam Bonica, Ph.D., of the department of political science, Stanford (Calif.) University, and his associates.
The current report shows that the shift away from predominantly Republican and toward predominantly Democratic support, which began in the 1990s, still persists for physicians.
“Given the increasing numbers of women physicians and salaried physicians, who typically ally with the Democrats, in contrast to surgeons, who typically ally with the Republicans, our findings suggest that the medical profession will be challenged to achieve consensus on health policy issues. The profession is unlikely to speak with one voice on questions such as the provision of health insurance or controlling the costs of medical care,” the investigators wrote (JAMA Intern. Med. 2015 April 27 [doi:10.1001/jamainternmed.2015.1332]).
However, this polarization among physicians “may spur both political parties to work harder to maintain and increase physicians’ support. Thus, the political divisions among physicians may have the unintended effect of enhancing the political standing of the medical profession,” they added.
Most U.S. physicians who made political contributions during the 2013-2014 congressional election cycle donated to Democrats, continuing the trend away from Republicans that was first noted among medical professionals between 1991 and 2012, according to a report published April 27 in JAMA Internal Medicine.
In an analysis of physicians’ federal political contributions, 55% of contributors donated to Democrats and 45% to Republicans during the most recent congressional election cycle. In contrast, general public support resulted in the “Republican surge” in which conservatives gained nine Senate seats and increased their majority in the House, said Adam Bonica, Ph.D., of the department of political science, Stanford (Calif.) University, and his associates.
The current report shows that the shift away from predominantly Republican and toward predominantly Democratic support, which began in the 1990s, still persists for physicians.
“Given the increasing numbers of women physicians and salaried physicians, who typically ally with the Democrats, in contrast to surgeons, who typically ally with the Republicans, our findings suggest that the medical profession will be challenged to achieve consensus on health policy issues. The profession is unlikely to speak with one voice on questions such as the provision of health insurance or controlling the costs of medical care,” the investigators wrote (JAMA Intern. Med. 2015 April 27 [doi:10.1001/jamainternmed.2015.1332]).
However, this polarization among physicians “may spur both political parties to work harder to maintain and increase physicians’ support. Thus, the political divisions among physicians may have the unintended effect of enhancing the political standing of the medical profession,” they added.
Most U.S. physicians who made political contributions during the 2013-2014 congressional election cycle donated to Democrats, continuing the trend away from Republicans that was first noted among medical professionals between 1991 and 2012, according to a report published April 27 in JAMA Internal Medicine.
In an analysis of physicians’ federal political contributions, 55% of contributors donated to Democrats and 45% to Republicans during the most recent congressional election cycle. In contrast, general public support resulted in the “Republican surge” in which conservatives gained nine Senate seats and increased their majority in the House, said Adam Bonica, Ph.D., of the department of political science, Stanford (Calif.) University, and his associates.
The current report shows that the shift away from predominantly Republican and toward predominantly Democratic support, which began in the 1990s, still persists for physicians.
“Given the increasing numbers of women physicians and salaried physicians, who typically ally with the Democrats, in contrast to surgeons, who typically ally with the Republicans, our findings suggest that the medical profession will be challenged to achieve consensus on health policy issues. The profession is unlikely to speak with one voice on questions such as the provision of health insurance or controlling the costs of medical care,” the investigators wrote (JAMA Intern. Med. 2015 April 27 [doi:10.1001/jamainternmed.2015.1332]).
However, this polarization among physicians “may spur both political parties to work harder to maintain and increase physicians’ support. Thus, the political divisions among physicians may have the unintended effect of enhancing the political standing of the medical profession,” they added.
Key clinical point: More physicians contributed to Democratic candidates in the 2013-2014 congressional election cycle, despite the “Republican surge.”
Major finding: Fifty-five percent of physicians who contributed to federal congressional campaigns during the most recent election cycle donated to Democrats, while 45% donated to Republicans.
Data source: An analysis of 2013 and 2014 federal campaign contributions from physicians.
Disclosures: The authors reported no relevant conflicts of interest.
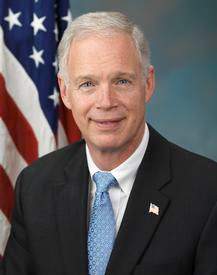
Senators prep for Supreme Court strike down of federal subsidies
WASHINGTON – As the Supreme Court prepares to rule this summer on King v. Burwell, Republican Senators are offering plans should the court strike down subsidies to those who have bought health insurance via the federal exchange.
“I suspect that President Obama will create some kind of executive order to allow states to turn [federally run exchanges] into state exchanges, but the law says you can’t establish a state exchange past a certain date. That throws it back to Congress,” Sen. Ron Johnson (R-Wisc.) said at a press conference.
If there isn’t a way forward already in sight, Sen. Johnson said that he thinks the House Republican leadership will do nothing and tell President Obama, “This is a problem of your own making.”
To avoid that kind of posturing – as well as to convince the Supreme Court that a pro-King ruling would not be harmful to patients – Sen. Johnson said, “We need to have a plan in place.”
His bill, S. 1016, the Preserving Freedom and Choice in Health Care Act, at press time had 31 cosponsors, more than the handful of similar bill introduced in the Senate.
“I’m trying to keep this as simple as possible so it has the greatest chance of success,” Sen. Johnson said. “Let’s maintain the status quo, let’s not throw this whole health insurance market into chaos.”
Should the Supreme Court strike down King v. Burwell, S. 1016 would continue through August 2017 subsidies for patients who currently have insurance bought through a federal exchange – temporarily codifying the status quo and the Obama administration’s interpretation of the Affordable Care Act.
The bill also would repeal both the ACA’s individual mandate to have health insurance and its employer mandate to provide health insurance, as well as the essential health benefits package, which Rep. Johnson said is the reason why the ACA makes health insurance expensive.
“A 60-year-old guy like me has to buy an insurance plan that has maternity coverage. When the government mandates that, it establishes a base price, and it’s going to be higher than if you have an insurance marketplace that doesn’t have all that mandated coverage,” he said. “The way this has all been implemented, if you don’t get the subsidies, you’re paying a lot, and you don’t particularly like Obamacare.”
Time is ticking down for a contingency plan: The Supreme Court is expected to rule the first week of June.
“This may not be the final product,” Sen. Johnson said of his bill, which has yet to be scored by the Congressional Budget Office. “There may be some tweaks and some additions to it over the next week or so, and then whatever comes out of that process is what I think leadership will get behind.”
On Twitter @whitneymcknight
WASHINGTON – As the Supreme Court prepares to rule this summer on King v. Burwell, Republican Senators are offering plans should the court strike down subsidies to those who have bought health insurance via the federal exchange.
“I suspect that President Obama will create some kind of executive order to allow states to turn [federally run exchanges] into state exchanges, but the law says you can’t establish a state exchange past a certain date. That throws it back to Congress,” Sen. Ron Johnson (R-Wisc.) said at a press conference.
If there isn’t a way forward already in sight, Sen. Johnson said that he thinks the House Republican leadership will do nothing and tell President Obama, “This is a problem of your own making.”
To avoid that kind of posturing – as well as to convince the Supreme Court that a pro-King ruling would not be harmful to patients – Sen. Johnson said, “We need to have a plan in place.”
His bill, S. 1016, the Preserving Freedom and Choice in Health Care Act, at press time had 31 cosponsors, more than the handful of similar bill introduced in the Senate.
“I’m trying to keep this as simple as possible so it has the greatest chance of success,” Sen. Johnson said. “Let’s maintain the status quo, let’s not throw this whole health insurance market into chaos.”
Should the Supreme Court strike down King v. Burwell, S. 1016 would continue through August 2017 subsidies for patients who currently have insurance bought through a federal exchange – temporarily codifying the status quo and the Obama administration’s interpretation of the Affordable Care Act.
The bill also would repeal both the ACA’s individual mandate to have health insurance and its employer mandate to provide health insurance, as well as the essential health benefits package, which Rep. Johnson said is the reason why the ACA makes health insurance expensive.
“A 60-year-old guy like me has to buy an insurance plan that has maternity coverage. When the government mandates that, it establishes a base price, and it’s going to be higher than if you have an insurance marketplace that doesn’t have all that mandated coverage,” he said. “The way this has all been implemented, if you don’t get the subsidies, you’re paying a lot, and you don’t particularly like Obamacare.”
Time is ticking down for a contingency plan: The Supreme Court is expected to rule the first week of June.
“This may not be the final product,” Sen. Johnson said of his bill, which has yet to be scored by the Congressional Budget Office. “There may be some tweaks and some additions to it over the next week or so, and then whatever comes out of that process is what I think leadership will get behind.”
On Twitter @whitneymcknight
WASHINGTON – As the Supreme Court prepares to rule this summer on King v. Burwell, Republican Senators are offering plans should the court strike down subsidies to those who have bought health insurance via the federal exchange.
“I suspect that President Obama will create some kind of executive order to allow states to turn [federally run exchanges] into state exchanges, but the law says you can’t establish a state exchange past a certain date. That throws it back to Congress,” Sen. Ron Johnson (R-Wisc.) said at a press conference.
If there isn’t a way forward already in sight, Sen. Johnson said that he thinks the House Republican leadership will do nothing and tell President Obama, “This is a problem of your own making.”
To avoid that kind of posturing – as well as to convince the Supreme Court that a pro-King ruling would not be harmful to patients – Sen. Johnson said, “We need to have a plan in place.”
His bill, S. 1016, the Preserving Freedom and Choice in Health Care Act, at press time had 31 cosponsors, more than the handful of similar bill introduced in the Senate.
“I’m trying to keep this as simple as possible so it has the greatest chance of success,” Sen. Johnson said. “Let’s maintain the status quo, let’s not throw this whole health insurance market into chaos.”
Should the Supreme Court strike down King v. Burwell, S. 1016 would continue through August 2017 subsidies for patients who currently have insurance bought through a federal exchange – temporarily codifying the status quo and the Obama administration’s interpretation of the Affordable Care Act.
The bill also would repeal both the ACA’s individual mandate to have health insurance and its employer mandate to provide health insurance, as well as the essential health benefits package, which Rep. Johnson said is the reason why the ACA makes health insurance expensive.
“A 60-year-old guy like me has to buy an insurance plan that has maternity coverage. When the government mandates that, it establishes a base price, and it’s going to be higher than if you have an insurance marketplace that doesn’t have all that mandated coverage,” he said. “The way this has all been implemented, if you don’t get the subsidies, you’re paying a lot, and you don’t particularly like Obamacare.”
Time is ticking down for a contingency plan: The Supreme Court is expected to rule the first week of June.
“This may not be the final product,” Sen. Johnson said of his bill, which has yet to be scored by the Congressional Budget Office. “There may be some tweaks and some additions to it over the next week or so, and then whatever comes out of that process is what I think leadership will get behind.”
On Twitter @whitneymcknight
Tennessee, Kansas also warned: Expand Medicaid or risk hospital funds
Add Tennessee and Kansas to the list of states that have been warned by the Obama administration that failing to expand Medicaid under the Affordable Care Act could jeopardize special funding to pay hospitals and doctors for treating the poor.
The Centers for Medicare & Medicaid Services confirmed on April 21 that it gave officials in those states the same message delivered to Texas and Florida about the risk to funding for so-called “uncompensated care pools” – Medicaid money that helps pay the cost of care for the uninsured.
The April 14 letter to Florida officials drew the ire of Republican Gov. Rick Scott, who said the federal government should not link the $1.3 billion in uncompensated care funding with the state’s decision not to expand Medicaid. He has threatened a lawsuit against the Obama administration if it cuts off the funding, which is set to expire June 30.
The Texas funding is scheduled to end in September of 2016. Officials there have also expressed indignation at what they perceive to be coercive pressure, and talked about joining Gov. Scott’s lawsuit.
Kansas Medicaid officials said they received about $45 million this year in federal funding for their state’s uncompensated care program, which began in 2013 and is slated to continue through 2017.
Tennessee Medicaid spokeswoman Kelly Gunderson said her state gets over $750 million in federal funding to cover uncompensated care.
The first message was delivered in the April 14 letter from Vikki Wachino, acting director of the Center for Medicaid & CHIP Services, to Florida Medicaid officials. She said that expanding Medicaid coverage is a better way to help patients and providers get access to health care than an “over-reliance on supplemental payments” to providers through a program called the Low Income Pool (LIP).
“Medicaid expansion would reduce uncompensated care in the state, and therefore have an impact on the LIP, which is why the state’s expansion status is an important consideration in our approach regarding extending the LIP beyond June,” she wrote.
CMS spokesman Aaron Albright said on April 21 that the Obama administration wants to apply similar principles to all the states that receive such funding, whether or not they expanded Medicaid.
“We’ve been in contact with those states that have uncompensated care pools and reiterated that we look forward to an ongoing dialogue to develop a solution that works for patients, hospitals and the taxpayer,” he said. “We told states that our letter to Florida articulates key principles CMS will use in considering proposals regarding uncompensated care pool programs in their states, but that discussions with each state will also take into account state-specific circumstances.”
CMS officials confirmed they also have reached out to states that expanded Medicaid about the future criteria for the funding. These states include California, Massachusetts, Arizona, Hawaii, and New Mexico.
Each state has negotiated its own program with the federal government to pay providers for treating the uninsured. But the programs differ in scope, funding, and length of time remaining.
Judy Solomon of the left-leaning Center on Budget and Policy Priorities said the special federal funding that some states negotiated for uncompensated care was never supposed to last indefinitely. The need for the funding changed as millions of people gained health coverage under the health law, she said.
“These demonstration programs are at the discretion of the Secretary of HHS and there is no entitlement to any state or providers to continue these funding arrangements when they expire,” Ms. Solomon said, adding, “The need for uncompensated care funding is changing dramatically.”
Arizona Medicaid spokeswoman Monica Higuera Coury said her state, which did expand Medicaid, was also told that the special funding would begin to be phased out this year. Arizona receives a maximum $137 million a year to offset uncompensated care costs at Phoenix Children’s Hospital. “We are looking forward to working with … CMS to put a transition plan together that moves us away from total reliance on the [funding] while still protecting this very important safety net for our children,” she said.
Some experts were surprised the Obama administration linked Medicaid expansion to the special funding because of the potential legal issues.
“No one would be shocked to hear that states don’t need the money because uncompensated care has dropped … but saying you are taking away this money because you are not expanding is trickier,” said Charlene Frizzera, a senior adviser at consulting firm Leavitt Partners. “People are shocked that CMS has done that.”
But Joan Alker, executive director of Georgetown University’s Center for Children and Families, said the administration was simply acting as a steward of taxpayer money.“I wouldn’t call it hardball, but rather responsible policy and fiscal oversight to ensure that federal tax dollars are spent in the most effective way,” she said. “When coverage is available to reduce the number of uninsured people … and states refuse those funds, why should the federal government provide them with unauthorized funding to put a Band-Aid on it?”
Kaiser Health News (KHN) is a nonprofit national health policy news service.
*This article was updated April 23, 2015
Add Tennessee and Kansas to the list of states that have been warned by the Obama administration that failing to expand Medicaid under the Affordable Care Act could jeopardize special funding to pay hospitals and doctors for treating the poor.
The Centers for Medicare & Medicaid Services confirmed on April 21 that it gave officials in those states the same message delivered to Texas and Florida about the risk to funding for so-called “uncompensated care pools” – Medicaid money that helps pay the cost of care for the uninsured.
The April 14 letter to Florida officials drew the ire of Republican Gov. Rick Scott, who said the federal government should not link the $1.3 billion in uncompensated care funding with the state’s decision not to expand Medicaid. He has threatened a lawsuit against the Obama administration if it cuts off the funding, which is set to expire June 30.
The Texas funding is scheduled to end in September of 2016. Officials there have also expressed indignation at what they perceive to be coercive pressure, and talked about joining Gov. Scott’s lawsuit.
Kansas Medicaid officials said they received about $45 million this year in federal funding for their state’s uncompensated care program, which began in 2013 and is slated to continue through 2017.
Tennessee Medicaid spokeswoman Kelly Gunderson said her state gets over $750 million in federal funding to cover uncompensated care.
The first message was delivered in the April 14 letter from Vikki Wachino, acting director of the Center for Medicaid & CHIP Services, to Florida Medicaid officials. She said that expanding Medicaid coverage is a better way to help patients and providers get access to health care than an “over-reliance on supplemental payments” to providers through a program called the Low Income Pool (LIP).
“Medicaid expansion would reduce uncompensated care in the state, and therefore have an impact on the LIP, which is why the state’s expansion status is an important consideration in our approach regarding extending the LIP beyond June,” she wrote.
CMS spokesman Aaron Albright said on April 21 that the Obama administration wants to apply similar principles to all the states that receive such funding, whether or not they expanded Medicaid.
“We’ve been in contact with those states that have uncompensated care pools and reiterated that we look forward to an ongoing dialogue to develop a solution that works for patients, hospitals and the taxpayer,” he said. “We told states that our letter to Florida articulates key principles CMS will use in considering proposals regarding uncompensated care pool programs in their states, but that discussions with each state will also take into account state-specific circumstances.”
CMS officials confirmed they also have reached out to states that expanded Medicaid about the future criteria for the funding. These states include California, Massachusetts, Arizona, Hawaii, and New Mexico.
Each state has negotiated its own program with the federal government to pay providers for treating the uninsured. But the programs differ in scope, funding, and length of time remaining.
Judy Solomon of the left-leaning Center on Budget and Policy Priorities said the special federal funding that some states negotiated for uncompensated care was never supposed to last indefinitely. The need for the funding changed as millions of people gained health coverage under the health law, she said.
“These demonstration programs are at the discretion of the Secretary of HHS and there is no entitlement to any state or providers to continue these funding arrangements when they expire,” Ms. Solomon said, adding, “The need for uncompensated care funding is changing dramatically.”
Arizona Medicaid spokeswoman Monica Higuera Coury said her state, which did expand Medicaid, was also told that the special funding would begin to be phased out this year. Arizona receives a maximum $137 million a year to offset uncompensated care costs at Phoenix Children’s Hospital. “We are looking forward to working with … CMS to put a transition plan together that moves us away from total reliance on the [funding] while still protecting this very important safety net for our children,” she said.
Some experts were surprised the Obama administration linked Medicaid expansion to the special funding because of the potential legal issues.
“No one would be shocked to hear that states don’t need the money because uncompensated care has dropped … but saying you are taking away this money because you are not expanding is trickier,” said Charlene Frizzera, a senior adviser at consulting firm Leavitt Partners. “People are shocked that CMS has done that.”
But Joan Alker, executive director of Georgetown University’s Center for Children and Families, said the administration was simply acting as a steward of taxpayer money.“I wouldn’t call it hardball, but rather responsible policy and fiscal oversight to ensure that federal tax dollars are spent in the most effective way,” she said. “When coverage is available to reduce the number of uninsured people … and states refuse those funds, why should the federal government provide them with unauthorized funding to put a Band-Aid on it?”
Kaiser Health News (KHN) is a nonprofit national health policy news service.
*This article was updated April 23, 2015
Add Tennessee and Kansas to the list of states that have been warned by the Obama administration that failing to expand Medicaid under the Affordable Care Act could jeopardize special funding to pay hospitals and doctors for treating the poor.
The Centers for Medicare & Medicaid Services confirmed on April 21 that it gave officials in those states the same message delivered to Texas and Florida about the risk to funding for so-called “uncompensated care pools” – Medicaid money that helps pay the cost of care for the uninsured.
The April 14 letter to Florida officials drew the ire of Republican Gov. Rick Scott, who said the federal government should not link the $1.3 billion in uncompensated care funding with the state’s decision not to expand Medicaid. He has threatened a lawsuit against the Obama administration if it cuts off the funding, which is set to expire June 30.
The Texas funding is scheduled to end in September of 2016. Officials there have also expressed indignation at what they perceive to be coercive pressure, and talked about joining Gov. Scott’s lawsuit.
Kansas Medicaid officials said they received about $45 million this year in federal funding for their state’s uncompensated care program, which began in 2013 and is slated to continue through 2017.
Tennessee Medicaid spokeswoman Kelly Gunderson said her state gets over $750 million in federal funding to cover uncompensated care.
The first message was delivered in the April 14 letter from Vikki Wachino, acting director of the Center for Medicaid & CHIP Services, to Florida Medicaid officials. She said that expanding Medicaid coverage is a better way to help patients and providers get access to health care than an “over-reliance on supplemental payments” to providers through a program called the Low Income Pool (LIP).
“Medicaid expansion would reduce uncompensated care in the state, and therefore have an impact on the LIP, which is why the state’s expansion status is an important consideration in our approach regarding extending the LIP beyond June,” she wrote.
CMS spokesman Aaron Albright said on April 21 that the Obama administration wants to apply similar principles to all the states that receive such funding, whether or not they expanded Medicaid.
“We’ve been in contact with those states that have uncompensated care pools and reiterated that we look forward to an ongoing dialogue to develop a solution that works for patients, hospitals and the taxpayer,” he said. “We told states that our letter to Florida articulates key principles CMS will use in considering proposals regarding uncompensated care pool programs in their states, but that discussions with each state will also take into account state-specific circumstances.”
CMS officials confirmed they also have reached out to states that expanded Medicaid about the future criteria for the funding. These states include California, Massachusetts, Arizona, Hawaii, and New Mexico.
Each state has negotiated its own program with the federal government to pay providers for treating the uninsured. But the programs differ in scope, funding, and length of time remaining.
Judy Solomon of the left-leaning Center on Budget and Policy Priorities said the special federal funding that some states negotiated for uncompensated care was never supposed to last indefinitely. The need for the funding changed as millions of people gained health coverage under the health law, she said.
“These demonstration programs are at the discretion of the Secretary of HHS and there is no entitlement to any state or providers to continue these funding arrangements when they expire,” Ms. Solomon said, adding, “The need for uncompensated care funding is changing dramatically.”
Arizona Medicaid spokeswoman Monica Higuera Coury said her state, which did expand Medicaid, was also told that the special funding would begin to be phased out this year. Arizona receives a maximum $137 million a year to offset uncompensated care costs at Phoenix Children’s Hospital. “We are looking forward to working with … CMS to put a transition plan together that moves us away from total reliance on the [funding] while still protecting this very important safety net for our children,” she said.
Some experts were surprised the Obama administration linked Medicaid expansion to the special funding because of the potential legal issues.
“No one would be shocked to hear that states don’t need the money because uncompensated care has dropped … but saying you are taking away this money because you are not expanding is trickier,” said Charlene Frizzera, a senior adviser at consulting firm Leavitt Partners. “People are shocked that CMS has done that.”
But Joan Alker, executive director of Georgetown University’s Center for Children and Families, said the administration was simply acting as a steward of taxpayer money.“I wouldn’t call it hardball, but rather responsible policy and fiscal oversight to ensure that federal tax dollars are spent in the most effective way,” she said. “When coverage is available to reduce the number of uninsured people … and states refuse those funds, why should the federal government provide them with unauthorized funding to put a Band-Aid on it?”
Kaiser Health News (KHN) is a nonprofit national health policy news service.
*This article was updated April 23, 2015
ICD-10 prep: Reduce claim backlogs, develop contingency plan
CHICAGO – Between now and the Oct. 1 ICD-10 transition, physicians should examine their past claims, reduce backlogs, and develop contingency plans to address unforeseen challenges, Betty Gomez said at the annual meeting of the Healthcare Information and Management Systems Society.
Physicians “think about Oct 1, 2015, and we think, ‘OK, all of my [preparations] are done. Great,’ ” said Ms. Gomez, a regulatory strategy consultant based in Louisville, Ky. But “Oct. 1 really marks the beginning of you ‘operationalizing’ your work and living in an ICD-10 world. It doesn’t stop there. It’s just the first milestone.”
Over the next 6 months, physicians should assess their coding systems and ensure they are fully prepared to work efficiently when ICD-10 goes live, Ms. Gomez said. A first step is getting a handle on the number of pending and denied claims. If an excess of pending claims exist, work immediately to lessen that excess.
“With the transition, there are going to be unforeseen obstacles and challenges,” she said. “You don’t want to have a pile and then be piling on top of that.”
Ms. Gomez recommended creating ways to monitor performance and develop thresholds for success. Benchmarks can help determine what success looks like and what issues should trigger concern. As Oct. 1 approaches, have a checklist in place to ensure all necessary tasks are completed. Questions might include: Do I have a response team or designated staff member in place to address potential problems that arise on or after Oct. 1.? Are staff members educated on when to use ICD-9 and when to use ICD-10 codes after the transition?
“You need to make sure you can continue to use both ICD-9 and ICD-10 codes, based on date of service or date of discharge,” Ms. Gomez said. “Verification is so important. You can never go wrong with making sure everything is in order.”
In terms of financial preparation, discuss with the practice’s top payers what kind of contingency plans are needed to ensure their revenue remains sufficient after Oct. 1, said F. Phil Cartagena Jr., ICD-10 program manager for Partners Healthcare System in Boston. The general recommendation is that practices have a minimum of 3 months of cash flow on hand, Mr. Cartagena said in an interview. However, it’s beneficial for practices to work out agreements in which payers match or partially match physicians’ current monthly run rate during the transition. Such arrangements can help mitigate claim denials that take time to be adjudicated, thus delaying cash flow.
“Your business isn’t going to change,” Mr. Cartagena said. “The patients that you’re seeing and the things that you are doing aren’t going to radically change, but if the ability to properly account for them and get paid for them changes, you don’t want it to have a major impact to your bottom line.”
Mr. Cartagena also suggested that physicians start more extensive patient documentation now, rather than waiting until ICD-10. As most physicians know, the nearly fivefold increase in the number of codes also requires more specific documentation than did ICD-9.
“The more specific that you can be, the better it is, whether it matters for actually coding the record correctly, or if it’s for stratifying your patient mix or having a better understanding clinically of how the diagnoses of your patient population break down,” he said. “It all comes back to the more information you have on the patients, the better they can be coded, and the better information you get at the end of all of it to understand your mix.”
On Twitter @legal_med
CHICAGO – Between now and the Oct. 1 ICD-10 transition, physicians should examine their past claims, reduce backlogs, and develop contingency plans to address unforeseen challenges, Betty Gomez said at the annual meeting of the Healthcare Information and Management Systems Society.
Physicians “think about Oct 1, 2015, and we think, ‘OK, all of my [preparations] are done. Great,’ ” said Ms. Gomez, a regulatory strategy consultant based in Louisville, Ky. But “Oct. 1 really marks the beginning of you ‘operationalizing’ your work and living in an ICD-10 world. It doesn’t stop there. It’s just the first milestone.”
Over the next 6 months, physicians should assess their coding systems and ensure they are fully prepared to work efficiently when ICD-10 goes live, Ms. Gomez said. A first step is getting a handle on the number of pending and denied claims. If an excess of pending claims exist, work immediately to lessen that excess.
“With the transition, there are going to be unforeseen obstacles and challenges,” she said. “You don’t want to have a pile and then be piling on top of that.”
Ms. Gomez recommended creating ways to monitor performance and develop thresholds for success. Benchmarks can help determine what success looks like and what issues should trigger concern. As Oct. 1 approaches, have a checklist in place to ensure all necessary tasks are completed. Questions might include: Do I have a response team or designated staff member in place to address potential problems that arise on or after Oct. 1.? Are staff members educated on when to use ICD-9 and when to use ICD-10 codes after the transition?
“You need to make sure you can continue to use both ICD-9 and ICD-10 codes, based on date of service or date of discharge,” Ms. Gomez said. “Verification is so important. You can never go wrong with making sure everything is in order.”
In terms of financial preparation, discuss with the practice’s top payers what kind of contingency plans are needed to ensure their revenue remains sufficient after Oct. 1, said F. Phil Cartagena Jr., ICD-10 program manager for Partners Healthcare System in Boston. The general recommendation is that practices have a minimum of 3 months of cash flow on hand, Mr. Cartagena said in an interview. However, it’s beneficial for practices to work out agreements in which payers match or partially match physicians’ current monthly run rate during the transition. Such arrangements can help mitigate claim denials that take time to be adjudicated, thus delaying cash flow.
“Your business isn’t going to change,” Mr. Cartagena said. “The patients that you’re seeing and the things that you are doing aren’t going to radically change, but if the ability to properly account for them and get paid for them changes, you don’t want it to have a major impact to your bottom line.”
Mr. Cartagena also suggested that physicians start more extensive patient documentation now, rather than waiting until ICD-10. As most physicians know, the nearly fivefold increase in the number of codes also requires more specific documentation than did ICD-9.
“The more specific that you can be, the better it is, whether it matters for actually coding the record correctly, or if it’s for stratifying your patient mix or having a better understanding clinically of how the diagnoses of your patient population break down,” he said. “It all comes back to the more information you have on the patients, the better they can be coded, and the better information you get at the end of all of it to understand your mix.”
On Twitter @legal_med
CHICAGO – Between now and the Oct. 1 ICD-10 transition, physicians should examine their past claims, reduce backlogs, and develop contingency plans to address unforeseen challenges, Betty Gomez said at the annual meeting of the Healthcare Information and Management Systems Society.
Physicians “think about Oct 1, 2015, and we think, ‘OK, all of my [preparations] are done. Great,’ ” said Ms. Gomez, a regulatory strategy consultant based in Louisville, Ky. But “Oct. 1 really marks the beginning of you ‘operationalizing’ your work and living in an ICD-10 world. It doesn’t stop there. It’s just the first milestone.”
Over the next 6 months, physicians should assess their coding systems and ensure they are fully prepared to work efficiently when ICD-10 goes live, Ms. Gomez said. A first step is getting a handle on the number of pending and denied claims. If an excess of pending claims exist, work immediately to lessen that excess.
“With the transition, there are going to be unforeseen obstacles and challenges,” she said. “You don’t want to have a pile and then be piling on top of that.”
Ms. Gomez recommended creating ways to monitor performance and develop thresholds for success. Benchmarks can help determine what success looks like and what issues should trigger concern. As Oct. 1 approaches, have a checklist in place to ensure all necessary tasks are completed. Questions might include: Do I have a response team or designated staff member in place to address potential problems that arise on or after Oct. 1.? Are staff members educated on when to use ICD-9 and when to use ICD-10 codes after the transition?
“You need to make sure you can continue to use both ICD-9 and ICD-10 codes, based on date of service or date of discharge,” Ms. Gomez said. “Verification is so important. You can never go wrong with making sure everything is in order.”
In terms of financial preparation, discuss with the practice’s top payers what kind of contingency plans are needed to ensure their revenue remains sufficient after Oct. 1, said F. Phil Cartagena Jr., ICD-10 program manager for Partners Healthcare System in Boston. The general recommendation is that practices have a minimum of 3 months of cash flow on hand, Mr. Cartagena said in an interview. However, it’s beneficial for practices to work out agreements in which payers match or partially match physicians’ current monthly run rate during the transition. Such arrangements can help mitigate claim denials that take time to be adjudicated, thus delaying cash flow.
“Your business isn’t going to change,” Mr. Cartagena said. “The patients that you’re seeing and the things that you are doing aren’t going to radically change, but if the ability to properly account for them and get paid for them changes, you don’t want it to have a major impact to your bottom line.”
Mr. Cartagena also suggested that physicians start more extensive patient documentation now, rather than waiting until ICD-10. As most physicians know, the nearly fivefold increase in the number of codes also requires more specific documentation than did ICD-9.
“The more specific that you can be, the better it is, whether it matters for actually coding the record correctly, or if it’s for stratifying your patient mix or having a better understanding clinically of how the diagnoses of your patient population break down,” he said. “It all comes back to the more information you have on the patients, the better they can be coded, and the better information you get at the end of all of it to understand your mix.”
On Twitter @legal_med
EXPERT ANALYSIS FROM HIMSS15
Coalition decries legislative interference in medicine
A coalition of physician, consumer, and other advocacy groups is asking politicians to stop trying to regulate the physician-patient relationship.
The Coalition to Protect the Patient-Provider Relationship – which includes the American College of Obstetricians and Gynecologists, the American Academy of Family Physicians, the American College of Physicians, and 13 other organizations – issued a statement expressing “serious concern” about the increasing number of government actions that “inappropriately interfere” in the relationship between patients and their health care providers by asking providers to violate their medical training and their ethical obligations to patients.
The statement points to laws recently enacted in Arizona and Arkansas that require abortion providers to inform patients that medication abortion may be reversible, a claim that is not supported by science, the coalition wrote.
“The mandate is emblematic of a larger trend of lawmakers abusing their responsibilities by imposing ideological views on licensed and highly trained health care professionals,” the coalition said in its statement.
The coalition urged lawmakers to follow four principles to protect the patient-provider relationship:
The coalition’s statement comes as physician organizations are increasingly pushing back against lawmakers for attempts to legislate their interactions with patients, including a Florida law that bars physicians from asking families about the presence of guns in the home and requirements in other states that women have ultrasonography before an abortion.
In 2012, the ACP, AAFP, ACOG, American Academy of Pediatrics, and American College of Surgeons wrote a joint editorial in the New England Journal of Medicine condemning these laws (2012;367:1557-9).
“Physicians must have the ability and freedom to speak to their patients freely and confidentially, to provide patients with factual information relevant to their health, to fully answer their patients’ questions, and to advise them on the course of best care without the fear of penalty,” the groups wrote in the editorial.
On Twitter @maryellenny
A coalition of physician, consumer, and other advocacy groups is asking politicians to stop trying to regulate the physician-patient relationship.
The Coalition to Protect the Patient-Provider Relationship – which includes the American College of Obstetricians and Gynecologists, the American Academy of Family Physicians, the American College of Physicians, and 13 other organizations – issued a statement expressing “serious concern” about the increasing number of government actions that “inappropriately interfere” in the relationship between patients and their health care providers by asking providers to violate their medical training and their ethical obligations to patients.
The statement points to laws recently enacted in Arizona and Arkansas that require abortion providers to inform patients that medication abortion may be reversible, a claim that is not supported by science, the coalition wrote.
“The mandate is emblematic of a larger trend of lawmakers abusing their responsibilities by imposing ideological views on licensed and highly trained health care professionals,” the coalition said in its statement.
The coalition urged lawmakers to follow four principles to protect the patient-provider relationship:
The coalition’s statement comes as physician organizations are increasingly pushing back against lawmakers for attempts to legislate their interactions with patients, including a Florida law that bars physicians from asking families about the presence of guns in the home and requirements in other states that women have ultrasonography before an abortion.
In 2012, the ACP, AAFP, ACOG, American Academy of Pediatrics, and American College of Surgeons wrote a joint editorial in the New England Journal of Medicine condemning these laws (2012;367:1557-9).
“Physicians must have the ability and freedom to speak to their patients freely and confidentially, to provide patients with factual information relevant to their health, to fully answer their patients’ questions, and to advise them on the course of best care without the fear of penalty,” the groups wrote in the editorial.
On Twitter @maryellenny
A coalition of physician, consumer, and other advocacy groups is asking politicians to stop trying to regulate the physician-patient relationship.
The Coalition to Protect the Patient-Provider Relationship – which includes the American College of Obstetricians and Gynecologists, the American Academy of Family Physicians, the American College of Physicians, and 13 other organizations – issued a statement expressing “serious concern” about the increasing number of government actions that “inappropriately interfere” in the relationship between patients and their health care providers by asking providers to violate their medical training and their ethical obligations to patients.
The statement points to laws recently enacted in Arizona and Arkansas that require abortion providers to inform patients that medication abortion may be reversible, a claim that is not supported by science, the coalition wrote.
“The mandate is emblematic of a larger trend of lawmakers abusing their responsibilities by imposing ideological views on licensed and highly trained health care professionals,” the coalition said in its statement.
The coalition urged lawmakers to follow four principles to protect the patient-provider relationship:
The coalition’s statement comes as physician organizations are increasingly pushing back against lawmakers for attempts to legislate their interactions with patients, including a Florida law that bars physicians from asking families about the presence of guns in the home and requirements in other states that women have ultrasonography before an abortion.
In 2012, the ACP, AAFP, ACOG, American Academy of Pediatrics, and American College of Surgeons wrote a joint editorial in the New England Journal of Medicine condemning these laws (2012;367:1557-9).
“Physicians must have the ability and freedom to speak to their patients freely and confidentially, to provide patients with factual information relevant to their health, to fully answer their patients’ questions, and to advise them on the course of best care without the fear of penalty,” the groups wrote in the editorial.
On Twitter @maryellenny