User login
Career Choices: Psychiatric oncology
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Saeed Ahmed, MD, Addiction Psychiatry Fellow at Boston University, talked with William Pirl, MD, MPH, FACLP, FAPOS. Dr. Pirl is Associate Professor, Psychiatry, Harvard Medical School. He joined Dana-Farber Cancer Institute in 2018 as Vice Chair for Psychosocial Oncology, Department of Psychosocial Oncology and Palliative Care. He is a past president of the American Psychosocial Oncology Society and North American Associate Editor for the journal Psycho-Oncology.
Dr. Ahmed: What made you choose the psychiatric oncology track, and how did your training lead you towards this path?
Dr. Pirl: I went to medical school thinking that I wanted to be a psychiatrist. However, I was really drawn to internal medicine, especially the process of sorting through medical differential diagnoses. I was deciding between applying for residency in medicine or psychiatry when I did an elective rotation in consultation-liaison (CL) psychiatry. Consultation-liaison psychiatry combined both medicine and psychiatry, which is exactly what I wanted to do. After residency, I wanted to do a CL fellowship outside of Boston, which is where I had done all of my medical education and training. One of my residency advisors suggested Memorial Sloan-Kettering Cancer Center, and I ended up going there. On the first day of fellowship, I realized that I’d only be working with cancer over that year, which I had not really thought about beforehand. Luckily, I loved it, and over the year I realized that the work had tremendous impact and meaning.
Dr. Ahmed: What are some of the pros and cons of working in psychiatric oncology?
Dr. Pirl: Things that I think are pros might be cons for some people. Consults in psychiatric oncology tend to be more relationship-based than they might be in other CL subspecialties. Oncology clinicians want to know who they are referring their patients to, and they are used to team-based care. If you like practicing as part of a multidisciplinary team, this is a pro.
Psychiatric oncology has more focus on existential issues, which interests me more than some other things in psychiatry. Bearing witness to so much tragedy can be a con at times, but psychiatrists who do this work learn ways to manage this within themselves. Psychiatric oncology also offers many experiences where you can see how much impact you make. It’s rewarding to see results and get positive feedback from patients and their families.
Continue to: Lastly, this is...
Lastly, this is a historic time in oncology. Over the last 15 years, things are happening that I never thought I would live to see. Some patients who 10 or 15 years ago would have had an expected survival of 6 to 9 months are now living years. We are now at a point where we might not actually know a patient’s prognosis, which introduces a whole other layer of uncertainty in cancer. Working as a psychiatrist during this time of rapidly evolving care is amazing. Cancer care will look very different over the next decade.
Dr. Ahmed: Based on your personal experience, what should one consider when choosing a psychiatric oncology program?
Dr. Pirl: I trained in a time before CL was a certified subspecialty of psychiatry. At that time, programs could focus solely on cancer, which cannot be done now. Trainees need to have broader training in certified fellowships. If someone knows that they are interested in psychiatric oncology, there are 2 programs that they should consider: the Dana-Farber Cancer Institute track of the Brigham and Women’s Hospital CL fellowship, and the Memorial Sloan-Kettering Cancer Center/New York Hospital CL fellowship. However, completing a CL fellowship will give someone the skills to do this work, even though they may not know all of the cancer content yet.
Dr. Ahmed: What are some of the career options and work settings in psychiatric oncology?
Dr. Pirl: There are many factors that make it difficult for psychiatrist to have a psychiatric oncology private practice. The amount of late cancellations and no-shows because of illness makes it hard to do this work without some institutional subsidy. Also, being able to communicate and work as a team with oncology providers is much easier if you are in the same place. Most psychiatrists who do psychiatric oncology work in a cancer center or hospital. Practice settings at those places include both inpatient and outpatient work. There is also a shortage of psychiatrists doing this work, which makes it easier to get a job and to advance into leadership roles.
Continue to: Dr. Ahmed...
Dr. Ahmed: What are some of the challenges in working in this field?
Dr. Pirl: One challenge is figuring out how to make sure you have income doing something that is not financially viable on its own. This is why most people work for cancer centers or hospitals and have some institutional subsidy for their work. Another challenge is access to care. There are not enough psychiatric resources for all the people with cancer who need them. Traditional referral-based models are getting harder and harder to manage. I think the emotional aspects of the work can also be challenging at times.
Dr. Ahmed: Where do you see the field going?
Dr. Pirl: Psychosocial care is now considered part of quality cancer care, and regulations require cancer centers to do certain aspects of it. This is leading to clinical growth and more integration into oncology. However, I am worried that we are not having enough psychiatry residents choose to do CL and/or psychiatric oncology. Some trainees are choosing to do a palliative care fellowship instead. When those trainees tell me why they want to do palliative care, I say that I do all of that and actually have much more time to do it because I am not managing constipation and vent settings. We need to do a better job of making trainees more aware of psychiatric oncology.
Dr. Ahmed: What advice do you have for those contemplating a career in psychiatric oncology?
Dr. Pirl: Please join the field. There is a shortage of psychiatrists who do this work, which is ironically one of the best and most meaningful jobs in psychiatry.
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Saeed Ahmed, MD, Addiction Psychiatry Fellow at Boston University, talked with William Pirl, MD, MPH, FACLP, FAPOS. Dr. Pirl is Associate Professor, Psychiatry, Harvard Medical School. He joined Dana-Farber Cancer Institute in 2018 as Vice Chair for Psychosocial Oncology, Department of Psychosocial Oncology and Palliative Care. He is a past president of the American Psychosocial Oncology Society and North American Associate Editor for the journal Psycho-Oncology.
Dr. Ahmed: What made you choose the psychiatric oncology track, and how did your training lead you towards this path?
Dr. Pirl: I went to medical school thinking that I wanted to be a psychiatrist. However, I was really drawn to internal medicine, especially the process of sorting through medical differential diagnoses. I was deciding between applying for residency in medicine or psychiatry when I did an elective rotation in consultation-liaison (CL) psychiatry. Consultation-liaison psychiatry combined both medicine and psychiatry, which is exactly what I wanted to do. After residency, I wanted to do a CL fellowship outside of Boston, which is where I had done all of my medical education and training. One of my residency advisors suggested Memorial Sloan-Kettering Cancer Center, and I ended up going there. On the first day of fellowship, I realized that I’d only be working with cancer over that year, which I had not really thought about beforehand. Luckily, I loved it, and over the year I realized that the work had tremendous impact and meaning.
Dr. Ahmed: What are some of the pros and cons of working in psychiatric oncology?
Dr. Pirl: Things that I think are pros might be cons for some people. Consults in psychiatric oncology tend to be more relationship-based than they might be in other CL subspecialties. Oncology clinicians want to know who they are referring their patients to, and they are used to team-based care. If you like practicing as part of a multidisciplinary team, this is a pro.
Psychiatric oncology has more focus on existential issues, which interests me more than some other things in psychiatry. Bearing witness to so much tragedy can be a con at times, but psychiatrists who do this work learn ways to manage this within themselves. Psychiatric oncology also offers many experiences where you can see how much impact you make. It’s rewarding to see results and get positive feedback from patients and their families.
Continue to: Lastly, this is...
Lastly, this is a historic time in oncology. Over the last 15 years, things are happening that I never thought I would live to see. Some patients who 10 or 15 years ago would have had an expected survival of 6 to 9 months are now living years. We are now at a point where we might not actually know a patient’s prognosis, which introduces a whole other layer of uncertainty in cancer. Working as a psychiatrist during this time of rapidly evolving care is amazing. Cancer care will look very different over the next decade.
Dr. Ahmed: Based on your personal experience, what should one consider when choosing a psychiatric oncology program?
Dr. Pirl: I trained in a time before CL was a certified subspecialty of psychiatry. At that time, programs could focus solely on cancer, which cannot be done now. Trainees need to have broader training in certified fellowships. If someone knows that they are interested in psychiatric oncology, there are 2 programs that they should consider: the Dana-Farber Cancer Institute track of the Brigham and Women’s Hospital CL fellowship, and the Memorial Sloan-Kettering Cancer Center/New York Hospital CL fellowship. However, completing a CL fellowship will give someone the skills to do this work, even though they may not know all of the cancer content yet.
Dr. Ahmed: What are some of the career options and work settings in psychiatric oncology?
Dr. Pirl: There are many factors that make it difficult for psychiatrist to have a psychiatric oncology private practice. The amount of late cancellations and no-shows because of illness makes it hard to do this work without some institutional subsidy. Also, being able to communicate and work as a team with oncology providers is much easier if you are in the same place. Most psychiatrists who do psychiatric oncology work in a cancer center or hospital. Practice settings at those places include both inpatient and outpatient work. There is also a shortage of psychiatrists doing this work, which makes it easier to get a job and to advance into leadership roles.
Continue to: Dr. Ahmed...
Dr. Ahmed: What are some of the challenges in working in this field?
Dr. Pirl: One challenge is figuring out how to make sure you have income doing something that is not financially viable on its own. This is why most people work for cancer centers or hospitals and have some institutional subsidy for their work. Another challenge is access to care. There are not enough psychiatric resources for all the people with cancer who need them. Traditional referral-based models are getting harder and harder to manage. I think the emotional aspects of the work can also be challenging at times.
Dr. Ahmed: Where do you see the field going?
Dr. Pirl: Psychosocial care is now considered part of quality cancer care, and regulations require cancer centers to do certain aspects of it. This is leading to clinical growth and more integration into oncology. However, I am worried that we are not having enough psychiatry residents choose to do CL and/or psychiatric oncology. Some trainees are choosing to do a palliative care fellowship instead. When those trainees tell me why they want to do palliative care, I say that I do all of that and actually have much more time to do it because I am not managing constipation and vent settings. We need to do a better job of making trainees more aware of psychiatric oncology.
Dr. Ahmed: What advice do you have for those contemplating a career in psychiatric oncology?
Dr. Pirl: Please join the field. There is a shortage of psychiatrists who do this work, which is ironically one of the best and most meaningful jobs in psychiatry.
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Saeed Ahmed, MD, Addiction Psychiatry Fellow at Boston University, talked with William Pirl, MD, MPH, FACLP, FAPOS. Dr. Pirl is Associate Professor, Psychiatry, Harvard Medical School. He joined Dana-Farber Cancer Institute in 2018 as Vice Chair for Psychosocial Oncology, Department of Psychosocial Oncology and Palliative Care. He is a past president of the American Psychosocial Oncology Society and North American Associate Editor for the journal Psycho-Oncology.
Dr. Ahmed: What made you choose the psychiatric oncology track, and how did your training lead you towards this path?
Dr. Pirl: I went to medical school thinking that I wanted to be a psychiatrist. However, I was really drawn to internal medicine, especially the process of sorting through medical differential diagnoses. I was deciding between applying for residency in medicine or psychiatry when I did an elective rotation in consultation-liaison (CL) psychiatry. Consultation-liaison psychiatry combined both medicine and psychiatry, which is exactly what I wanted to do. After residency, I wanted to do a CL fellowship outside of Boston, which is where I had done all of my medical education and training. One of my residency advisors suggested Memorial Sloan-Kettering Cancer Center, and I ended up going there. On the first day of fellowship, I realized that I’d only be working with cancer over that year, which I had not really thought about beforehand. Luckily, I loved it, and over the year I realized that the work had tremendous impact and meaning.
Dr. Ahmed: What are some of the pros and cons of working in psychiatric oncology?
Dr. Pirl: Things that I think are pros might be cons for some people. Consults in psychiatric oncology tend to be more relationship-based than they might be in other CL subspecialties. Oncology clinicians want to know who they are referring their patients to, and they are used to team-based care. If you like practicing as part of a multidisciplinary team, this is a pro.
Psychiatric oncology has more focus on existential issues, which interests me more than some other things in psychiatry. Bearing witness to so much tragedy can be a con at times, but psychiatrists who do this work learn ways to manage this within themselves. Psychiatric oncology also offers many experiences where you can see how much impact you make. It’s rewarding to see results and get positive feedback from patients and their families.
Continue to: Lastly, this is...
Lastly, this is a historic time in oncology. Over the last 15 years, things are happening that I never thought I would live to see. Some patients who 10 or 15 years ago would have had an expected survival of 6 to 9 months are now living years. We are now at a point where we might not actually know a patient’s prognosis, which introduces a whole other layer of uncertainty in cancer. Working as a psychiatrist during this time of rapidly evolving care is amazing. Cancer care will look very different over the next decade.
Dr. Ahmed: Based on your personal experience, what should one consider when choosing a psychiatric oncology program?
Dr. Pirl: I trained in a time before CL was a certified subspecialty of psychiatry. At that time, programs could focus solely on cancer, which cannot be done now. Trainees need to have broader training in certified fellowships. If someone knows that they are interested in psychiatric oncology, there are 2 programs that they should consider: the Dana-Farber Cancer Institute track of the Brigham and Women’s Hospital CL fellowship, and the Memorial Sloan-Kettering Cancer Center/New York Hospital CL fellowship. However, completing a CL fellowship will give someone the skills to do this work, even though they may not know all of the cancer content yet.
Dr. Ahmed: What are some of the career options and work settings in psychiatric oncology?
Dr. Pirl: There are many factors that make it difficult for psychiatrist to have a psychiatric oncology private practice. The amount of late cancellations and no-shows because of illness makes it hard to do this work without some institutional subsidy. Also, being able to communicate and work as a team with oncology providers is much easier if you are in the same place. Most psychiatrists who do psychiatric oncology work in a cancer center or hospital. Practice settings at those places include both inpatient and outpatient work. There is also a shortage of psychiatrists doing this work, which makes it easier to get a job and to advance into leadership roles.
Continue to: Dr. Ahmed...
Dr. Ahmed: What are some of the challenges in working in this field?
Dr. Pirl: One challenge is figuring out how to make sure you have income doing something that is not financially viable on its own. This is why most people work for cancer centers or hospitals and have some institutional subsidy for their work. Another challenge is access to care. There are not enough psychiatric resources for all the people with cancer who need them. Traditional referral-based models are getting harder and harder to manage. I think the emotional aspects of the work can also be challenging at times.
Dr. Ahmed: Where do you see the field going?
Dr. Pirl: Psychosocial care is now considered part of quality cancer care, and regulations require cancer centers to do certain aspects of it. This is leading to clinical growth and more integration into oncology. However, I am worried that we are not having enough psychiatry residents choose to do CL and/or psychiatric oncology. Some trainees are choosing to do a palliative care fellowship instead. When those trainees tell me why they want to do palliative care, I say that I do all of that and actually have much more time to do it because I am not managing constipation and vent settings. We need to do a better job of making trainees more aware of psychiatric oncology.
Dr. Ahmed: What advice do you have for those contemplating a career in psychiatric oncology?
Dr. Pirl: Please join the field. There is a shortage of psychiatrists who do this work, which is ironically one of the best and most meaningful jobs in psychiatry.
Feigning alcohol withdrawal symptoms can render the CIWA-Ar scale useless
The Clinical Institute Withdrawal Assessment for Alcohol–Revised (CIWA-Ar) scale is a well-established protocol that attempts to measure the degree of alcohol and benzodiazepine withdrawal. The CIWA-Ar scale measures 10 domains and indexes the severity of withdrawal on a scale from 0 to 67; scores >8 are generally considered to be indicative of at least mild-to-moderate withdrawal, and scores >20 represent significant withdrawal.1 Despite its common use in many medical settings, the CIWA-Ar scale has been impugned as a less-than-reliable index of true alcohol withdrawal2 and has the potential for misuse among ordering physicians.3 In this case report, I describe a malingering patient who intentionally and successfully feigned symptoms of alcohol withdrawal, which demonstrates that the purposeful reproduction of symptoms measured by the CIWA-Ar scale can render the protocol clinically useless.
CASE REPORT
Mr. G, a 63-year-old African-American man, was admitted to the general medical floor with a chief complaint of alcohol withdrawal. He had a history of alcohol use disorder, severe, and unspecified depression. He said he had been drinking a gallon of wine plus “a fifth” of vodka every day for the past 1.5 months. More than 1 year ago, he had been admitted for alcohol withdrawal with subsequent delirium tremens, but he denied having any other psychiatric history.
In the emergency department, Mr. G was given IV lorazepam, 6 mg total, for alcohol withdrawal. He was reported to be “scoring” on the CIWA-Ar scale with apparently uncontrollable tremulousness, visual hallucinations, and confusion. His vitals were within normal limits, his mean corpuscular volume and lipase level were within normal limits, and the rest of his presentation was largely unremarkable.
Once admitted to the general medical floor, he continued to receive benzodiazepines for what was documented as severe alcohol withdrawal. When clinical staff were not in the room, the patient was observed to be resting comfortably without tremulousness. When the patient was seen by the psychiatry consultation service, he produced full body tremulousness with marked shoulder and hip thrusting. His account of how much he had been drinking contradicted the amount he reported to other teams in the hospital. When the consulting psychiatrist appeared unimpressed by his full body jerking, the patient abruptly pointed to the corner of the room and yelled “What is that?” when nothing was there. When the primary medical team suggested to the patient that his vitals were within normal limits and he did not appear to be in true alcohol withdrawal, the patient escalated the degree of his full body jerking.
Over the next few days, the patient routinely would tell clinical staff “I’m having DTs.” He also specifically requested lorazepam. After consultation, the medical and psychiatry teams determined the patient was feigning symptoms of alcohol withdrawal. The lorazepam was discontinued, and the patient was discharged home with outpatient psychiatric follow-up.
Limitations of the CIWA-Ar scale
The CIWA-Ar scale is intended to guide the need for medications, such as benzodiazepines, to help mitigate symptoms of alcohol withdrawal. Symptom-triggered benzodiazepine treatment has been shown to be superior to fixed-schedule dosing.4 However, symptom-triggered treatment is problematic in the setting of feigned symptoms.
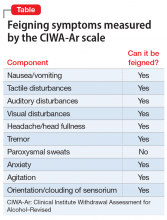
When psychiatrists and nurses calculate a CIWA-Ar score, they rely on both subjective accounts of a patient’s withdrawal severity as well as objective signs, such as vitals and a physical examination. Many of the elements included in the CIWA-Ar scale can be easily feigned (Table). Feigned alcohol withdrawal may fall into 2 categories: (1) the false reporting of subjective symptoms, and (2) the false portrayal of objective signs.
Continue to: The false reporting...
The false reporting of subjective symptoms can include the reported presence of nausea or vomiting, anxiety, tactile hallucinations, auditory hallucinations, headache or head fullness, and visual hallucinations. The false portrayal of objective signs can include the feigning of tremulousness, agitation, and confusion (eg, incorrectly answering orienting questions). In both categories, the simple presence of these signs or symptoms, whether falsely reported or falsely portrayed, would cause the patient to “score” on the CIWA-Ar scale.
Thus, the need to effectively rule out feigned symptoms is essential because inappropriate dosing of benzodiazepines can be dangerous, costly, and utilize limited hospital resources that could otherwise be diverted to a patient with a true medical or psychiatric illness. In these instances, it is crucial to pay close attention to vital signs because these are more reliable indices of withdrawal. A patient’s ability to purposefully feign symptoms of alcohol withdrawal highlights the limitations of the CIWA-Ar scale as a validated measure of alcohol withdrawal, and renders it effectively useless in the setting of either malingering or factitious disorder.
Resnick5 describes malingering as either pure malingering, partial malingering, or false imputation. Pure malingering refers to the feigning of a nonexistent disorder or illness. Partial malingering refers to the exaggeration of symptoms that are present, but to a lesser degree. False imputation refers to the attribution of symptoms from a separate disorder to one the patient knows is unrelated (eg, attributing chronic low back pain from a prior sports injury to a recent motor vehicle accident). In Mr. G’s case, he had multiple prior admissions for true, non-feigned alcohol withdrawal with subsequent delirium tremens. His knowledge of the signs and symptoms of alcohol withdrawal therefore helped him make calculated efforts to manipulate clinical staff in his quest to obtain benzodiazepines. Whether this was pure or partial malingering remained unclear because Mr. G’s true level of withdrawal could not be adequately assessed.
Potentially serious consequences
The CIWA-Ar scale is among the most widely used scales to determine the level of alcohol withdrawal and need for subsequent benzodiazepine treatment. However, its effective use is limited because it relies on subjective symptoms and objective signs that can be easily feigned or manipulated. In the setting of malingering or factitious disorder, when a patient is feigning symptoms of alcohol withdrawal, the CIWA-Ar scale may be rendered clinically useless. This can lead to dangerous iatrogenic adverse effects, lengthy and nontherapeutic hospital stays, and an increasing financial burden on health care systems.
1. Sullivan JT, Sykora K, Schneiderman J, et al. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict. 1989;84(11):1353-1357.
2. Knight E, Lappalainen L. Clinical Institute Withdrawal Assessment for Alcohol–Revised might be an unreliable tool in the management of alcohol withdrawal. Can Fam Physician. 2017;63(9):691-695.
3. Hecksel KA, Bostwick JM, Jaeger TM, et al. Inappropriate use of symptom-triggered therapy for alcohol withdrawal in the general hospital. Mayo Clin Proc. 2008;83(3):274-279.
4. Daeppen JB, Gache P, Landry U, et al. Symptom-triggered vs fixed-schedule doses of benzodiazepine for alcohol withdrawal: a randomized treatment trial. Arch Intern Med. 2002;162(10):1117-1121.
5. Resnick PJ. The detection of malingered mental illness. Behav Sci Law. 1984;2(1):20-38.
The Clinical Institute Withdrawal Assessment for Alcohol–Revised (CIWA-Ar) scale is a well-established protocol that attempts to measure the degree of alcohol and benzodiazepine withdrawal. The CIWA-Ar scale measures 10 domains and indexes the severity of withdrawal on a scale from 0 to 67; scores >8 are generally considered to be indicative of at least mild-to-moderate withdrawal, and scores >20 represent significant withdrawal.1 Despite its common use in many medical settings, the CIWA-Ar scale has been impugned as a less-than-reliable index of true alcohol withdrawal2 and has the potential for misuse among ordering physicians.3 In this case report, I describe a malingering patient who intentionally and successfully feigned symptoms of alcohol withdrawal, which demonstrates that the purposeful reproduction of symptoms measured by the CIWA-Ar scale can render the protocol clinically useless.
CASE REPORT
Mr. G, a 63-year-old African-American man, was admitted to the general medical floor with a chief complaint of alcohol withdrawal. He had a history of alcohol use disorder, severe, and unspecified depression. He said he had been drinking a gallon of wine plus “a fifth” of vodka every day for the past 1.5 months. More than 1 year ago, he had been admitted for alcohol withdrawal with subsequent delirium tremens, but he denied having any other psychiatric history.
In the emergency department, Mr. G was given IV lorazepam, 6 mg total, for alcohol withdrawal. He was reported to be “scoring” on the CIWA-Ar scale with apparently uncontrollable tremulousness, visual hallucinations, and confusion. His vitals were within normal limits, his mean corpuscular volume and lipase level were within normal limits, and the rest of his presentation was largely unremarkable.
Once admitted to the general medical floor, he continued to receive benzodiazepines for what was documented as severe alcohol withdrawal. When clinical staff were not in the room, the patient was observed to be resting comfortably without tremulousness. When the patient was seen by the psychiatry consultation service, he produced full body tremulousness with marked shoulder and hip thrusting. His account of how much he had been drinking contradicted the amount he reported to other teams in the hospital. When the consulting psychiatrist appeared unimpressed by his full body jerking, the patient abruptly pointed to the corner of the room and yelled “What is that?” when nothing was there. When the primary medical team suggested to the patient that his vitals were within normal limits and he did not appear to be in true alcohol withdrawal, the patient escalated the degree of his full body jerking.
Over the next few days, the patient routinely would tell clinical staff “I’m having DTs.” He also specifically requested lorazepam. After consultation, the medical and psychiatry teams determined the patient was feigning symptoms of alcohol withdrawal. The lorazepam was discontinued, and the patient was discharged home with outpatient psychiatric follow-up.
Limitations of the CIWA-Ar scale
The CIWA-Ar scale is intended to guide the need for medications, such as benzodiazepines, to help mitigate symptoms of alcohol withdrawal. Symptom-triggered benzodiazepine treatment has been shown to be superior to fixed-schedule dosing.4 However, symptom-triggered treatment is problematic in the setting of feigned symptoms.
When psychiatrists and nurses calculate a CIWA-Ar score, they rely on both subjective accounts of a patient’s withdrawal severity as well as objective signs, such as vitals and a physical examination. Many of the elements included in the CIWA-Ar scale can be easily feigned (Table). Feigned alcohol withdrawal may fall into 2 categories: (1) the false reporting of subjective symptoms, and (2) the false portrayal of objective signs.
Continue to: The false reporting...
The false reporting of subjective symptoms can include the reported presence of nausea or vomiting, anxiety, tactile hallucinations, auditory hallucinations, headache or head fullness, and visual hallucinations. The false portrayal of objective signs can include the feigning of tremulousness, agitation, and confusion (eg, incorrectly answering orienting questions). In both categories, the simple presence of these signs or symptoms, whether falsely reported or falsely portrayed, would cause the patient to “score” on the CIWA-Ar scale.
Thus, the need to effectively rule out feigned symptoms is essential because inappropriate dosing of benzodiazepines can be dangerous, costly, and utilize limited hospital resources that could otherwise be diverted to a patient with a true medical or psychiatric illness. In these instances, it is crucial to pay close attention to vital signs because these are more reliable indices of withdrawal. A patient’s ability to purposefully feign symptoms of alcohol withdrawal highlights the limitations of the CIWA-Ar scale as a validated measure of alcohol withdrawal, and renders it effectively useless in the setting of either malingering or factitious disorder.
Resnick5 describes malingering as either pure malingering, partial malingering, or false imputation. Pure malingering refers to the feigning of a nonexistent disorder or illness. Partial malingering refers to the exaggeration of symptoms that are present, but to a lesser degree. False imputation refers to the attribution of symptoms from a separate disorder to one the patient knows is unrelated (eg, attributing chronic low back pain from a prior sports injury to a recent motor vehicle accident). In Mr. G’s case, he had multiple prior admissions for true, non-feigned alcohol withdrawal with subsequent delirium tremens. His knowledge of the signs and symptoms of alcohol withdrawal therefore helped him make calculated efforts to manipulate clinical staff in his quest to obtain benzodiazepines. Whether this was pure or partial malingering remained unclear because Mr. G’s true level of withdrawal could not be adequately assessed.
Potentially serious consequences
The CIWA-Ar scale is among the most widely used scales to determine the level of alcohol withdrawal and need for subsequent benzodiazepine treatment. However, its effective use is limited because it relies on subjective symptoms and objective signs that can be easily feigned or manipulated. In the setting of malingering or factitious disorder, when a patient is feigning symptoms of alcohol withdrawal, the CIWA-Ar scale may be rendered clinically useless. This can lead to dangerous iatrogenic adverse effects, lengthy and nontherapeutic hospital stays, and an increasing financial burden on health care systems.
The Clinical Institute Withdrawal Assessment for Alcohol–Revised (CIWA-Ar) scale is a well-established protocol that attempts to measure the degree of alcohol and benzodiazepine withdrawal. The CIWA-Ar scale measures 10 domains and indexes the severity of withdrawal on a scale from 0 to 67; scores >8 are generally considered to be indicative of at least mild-to-moderate withdrawal, and scores >20 represent significant withdrawal.1 Despite its common use in many medical settings, the CIWA-Ar scale has been impugned as a less-than-reliable index of true alcohol withdrawal2 and has the potential for misuse among ordering physicians.3 In this case report, I describe a malingering patient who intentionally and successfully feigned symptoms of alcohol withdrawal, which demonstrates that the purposeful reproduction of symptoms measured by the CIWA-Ar scale can render the protocol clinically useless.
CASE REPORT
Mr. G, a 63-year-old African-American man, was admitted to the general medical floor with a chief complaint of alcohol withdrawal. He had a history of alcohol use disorder, severe, and unspecified depression. He said he had been drinking a gallon of wine plus “a fifth” of vodka every day for the past 1.5 months. More than 1 year ago, he had been admitted for alcohol withdrawal with subsequent delirium tremens, but he denied having any other psychiatric history.
In the emergency department, Mr. G was given IV lorazepam, 6 mg total, for alcohol withdrawal. He was reported to be “scoring” on the CIWA-Ar scale with apparently uncontrollable tremulousness, visual hallucinations, and confusion. His vitals were within normal limits, his mean corpuscular volume and lipase level were within normal limits, and the rest of his presentation was largely unremarkable.
Once admitted to the general medical floor, he continued to receive benzodiazepines for what was documented as severe alcohol withdrawal. When clinical staff were not in the room, the patient was observed to be resting comfortably without tremulousness. When the patient was seen by the psychiatry consultation service, he produced full body tremulousness with marked shoulder and hip thrusting. His account of how much he had been drinking contradicted the amount he reported to other teams in the hospital. When the consulting psychiatrist appeared unimpressed by his full body jerking, the patient abruptly pointed to the corner of the room and yelled “What is that?” when nothing was there. When the primary medical team suggested to the patient that his vitals were within normal limits and he did not appear to be in true alcohol withdrawal, the patient escalated the degree of his full body jerking.
Over the next few days, the patient routinely would tell clinical staff “I’m having DTs.” He also specifically requested lorazepam. After consultation, the medical and psychiatry teams determined the patient was feigning symptoms of alcohol withdrawal. The lorazepam was discontinued, and the patient was discharged home with outpatient psychiatric follow-up.
Limitations of the CIWA-Ar scale
The CIWA-Ar scale is intended to guide the need for medications, such as benzodiazepines, to help mitigate symptoms of alcohol withdrawal. Symptom-triggered benzodiazepine treatment has been shown to be superior to fixed-schedule dosing.4 However, symptom-triggered treatment is problematic in the setting of feigned symptoms.
When psychiatrists and nurses calculate a CIWA-Ar score, they rely on both subjective accounts of a patient’s withdrawal severity as well as objective signs, such as vitals and a physical examination. Many of the elements included in the CIWA-Ar scale can be easily feigned (Table). Feigned alcohol withdrawal may fall into 2 categories: (1) the false reporting of subjective symptoms, and (2) the false portrayal of objective signs.
Continue to: The false reporting...
The false reporting of subjective symptoms can include the reported presence of nausea or vomiting, anxiety, tactile hallucinations, auditory hallucinations, headache or head fullness, and visual hallucinations. The false portrayal of objective signs can include the feigning of tremulousness, agitation, and confusion (eg, incorrectly answering orienting questions). In both categories, the simple presence of these signs or symptoms, whether falsely reported or falsely portrayed, would cause the patient to “score” on the CIWA-Ar scale.
Thus, the need to effectively rule out feigned symptoms is essential because inappropriate dosing of benzodiazepines can be dangerous, costly, and utilize limited hospital resources that could otherwise be diverted to a patient with a true medical or psychiatric illness. In these instances, it is crucial to pay close attention to vital signs because these are more reliable indices of withdrawal. A patient’s ability to purposefully feign symptoms of alcohol withdrawal highlights the limitations of the CIWA-Ar scale as a validated measure of alcohol withdrawal, and renders it effectively useless in the setting of either malingering or factitious disorder.
Resnick5 describes malingering as either pure malingering, partial malingering, or false imputation. Pure malingering refers to the feigning of a nonexistent disorder or illness. Partial malingering refers to the exaggeration of symptoms that are present, but to a lesser degree. False imputation refers to the attribution of symptoms from a separate disorder to one the patient knows is unrelated (eg, attributing chronic low back pain from a prior sports injury to a recent motor vehicle accident). In Mr. G’s case, he had multiple prior admissions for true, non-feigned alcohol withdrawal with subsequent delirium tremens. His knowledge of the signs and symptoms of alcohol withdrawal therefore helped him make calculated efforts to manipulate clinical staff in his quest to obtain benzodiazepines. Whether this was pure or partial malingering remained unclear because Mr. G’s true level of withdrawal could not be adequately assessed.
Potentially serious consequences
The CIWA-Ar scale is among the most widely used scales to determine the level of alcohol withdrawal and need for subsequent benzodiazepine treatment. However, its effective use is limited because it relies on subjective symptoms and objective signs that can be easily feigned or manipulated. In the setting of malingering or factitious disorder, when a patient is feigning symptoms of alcohol withdrawal, the CIWA-Ar scale may be rendered clinically useless. This can lead to dangerous iatrogenic adverse effects, lengthy and nontherapeutic hospital stays, and an increasing financial burden on health care systems.
1. Sullivan JT, Sykora K, Schneiderman J, et al. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict. 1989;84(11):1353-1357.
2. Knight E, Lappalainen L. Clinical Institute Withdrawal Assessment for Alcohol–Revised might be an unreliable tool in the management of alcohol withdrawal. Can Fam Physician. 2017;63(9):691-695.
3. Hecksel KA, Bostwick JM, Jaeger TM, et al. Inappropriate use of symptom-triggered therapy for alcohol withdrawal in the general hospital. Mayo Clin Proc. 2008;83(3):274-279.
4. Daeppen JB, Gache P, Landry U, et al. Symptom-triggered vs fixed-schedule doses of benzodiazepine for alcohol withdrawal: a randomized treatment trial. Arch Intern Med. 2002;162(10):1117-1121.
5. Resnick PJ. The detection of malingered mental illness. Behav Sci Law. 1984;2(1):20-38.
1. Sullivan JT, Sykora K, Schneiderman J, et al. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict. 1989;84(11):1353-1357.
2. Knight E, Lappalainen L. Clinical Institute Withdrawal Assessment for Alcohol–Revised might be an unreliable tool in the management of alcohol withdrawal. Can Fam Physician. 2017;63(9):691-695.
3. Hecksel KA, Bostwick JM, Jaeger TM, et al. Inappropriate use of symptom-triggered therapy for alcohol withdrawal in the general hospital. Mayo Clin Proc. 2008;83(3):274-279.
4. Daeppen JB, Gache P, Landry U, et al. Symptom-triggered vs fixed-schedule doses of benzodiazepine for alcohol withdrawal: a randomized treatment trial. Arch Intern Med. 2002;162(10):1117-1121.
5. Resnick PJ. The detection of malingered mental illness. Behav Sci Law. 1984;2(1):20-38.
A reflection on Ghana’s mental health system
In recent years, the delivery of mental health services in Ghana has expanded substantially, especially since the passing of the Mental Health Act in 2012. In this article, I reflect on my experience as a visiting psychiatry resident in August 2018 at 2 Ghanaian hospitals located in Accra and Navrongo. Evident strengths of the mental health system were family support for patients and the scope of psychiatrists, while the most prominent weakness was the inadequate funding. As treatment of mental illness expands, more funding, psychiatrists, and mental health workers will be critical for the continued success of Ghana’s mental health system.
Psychiatric treatment in Ghana
Ghana has a population of approximately 28 million people, yet the country has an estimated 18 to 25 psychiatrists, up from 11 psychiatrists in 2011.1-3 Compared with the United States, which has 10.54 psychiatrists per 100,000 people (approximately 1 psychiatrist per 9,500 people), Ghana has .058 psychiatrists per 100,000 people (approximately 1 psychiatrist per 1.7 million people).4 In Ghana, most psychiatric care is delivered by mental health nurses, community mental health officers (CMHOs), and clinical psychiatric officers; supervision by psychiatrists is limited.3 Due to low public awareness, a scarcity of clinicians, and limited access to diagnostic services and medications, individuals with psychiatric illness in Ghana are often stigmatized, undertreated, and mistreated. To address this, in March 2012, Ghana passed Mental Health Act 846, which established a mental health commission and outlined protections for individuals with mental health needs.5 Since then, the number of people seeking treatment and the number of clinicians have expanded, but there are still significant challenges, such as a lack of funding for medications and facilities, and limited clinicians.6
During my last year of psychiatry residency at Mount Sinai Hospital in New York, I spent several weeks in Ghana at 2 institutions, observing and supervising the provision of psychiatric services. This was my first experience with the country’s health care system; therefore, my objectives were to:
- assess the current state of psychiatric services through observation and interviews with clinical staff
- provide instruction to clinicians in areas of need.
Two-thirds of my time was spent at the Accra Psychiatric Hospital, 1 of only 3 psychiatric hospitals in Ghana, all of which are located in the southern region of the country. The remainder of my time was spent at the Navrongo War Memorial Hospital in Ghana’s Northern Region.
The Accra Psychiatric Hospital is a sprawling complex near the center of the capital city. Every morning I walked through a large outdoor waiting area to the examination room, which was filled with at least 30 patients by 9
Navrongo War Memorial Hospital. There are no practicing psychiatrists in the northern region of the country; therefore, all mental health care is delivered by mental health nurses and CMHOs. CMHOs have 1 year of training plus a minimum of 2 years of service. They focus on identifying psychiatric cases in the community and coordinating treatment. Nurses have prescribing rights. A psychiatrist should be scheduled to visit the various districts in the region every 6 months to provide supervision, but this is not always feasible.
When I visited, I was the only psychiatrist who had been to this hospital in more than 1 year. During my time there, I reviewed the treatment protocols and gave lectures on the management of psychiatric emergencies and motivational interviewing, because addiction to alcohol and tramadol are 2 of the most pressing mental health problems in the country.7 I also saw patients with nurses, and supervised them on their assessment and treatment.
Continue to: In Ghana...
In Ghana, psychiatric services are often delivered using the community mental health model, in which many patients are visited in their homes. One morning, we went to a prayer camp to see if there were any individuals who would benefit from psychiatric services. There were no cases that day, but during the visit I sat under a tree where a few years before it was not uncommon to find a person who was psychotic or agitated chained to the tree. Several years of outreach by the local nurses has resulted in the camp leaders better recognizing mental illness early and contacting the nurses, as opposed to locking a person in chains for an extended period.
On one occasion, we answered a crisis call where a person experiencing a psychotic episode had locked himself in his house. The team talked with the individual through a locked screen door for 30 minutes, after which he eventually came out of the home to speak with us. A few days later, the patient accepted fluphenazine decanoate injection at his home. Two weeks later, he came to the outpatient clinic to continue treatment. Four months later, the patient was still in treatment and had started an apprenticeship for repairing cars.
As I was walking out of the hospital on my last day, I was called back to see a woman with a seizure who had been brought to the hospital. Unfortunately, there was no more diazepam in stock with which to treat her. This event highlighted the lack of resources available in this setting.
3 Take-home messages
My experience at both hospitals led me to reflect on 3 important factors impacting the mental health system in Ghana:
Family support. For at least 80% of appointments, patients were accompanied by family members or friends. The family hierarchy is still dominant in the Ghanaian culture, and clinicians often need the buy-in of the family, especially when financial support is required. More often than not, families enhanced patients’ treatment, but in some instances, they were a barrier.
Continue to: The types of cases
The types of cases. Most of the patients coming to both hospitals had diagnoses of bipolar disorder, schizophrenia, substance use disorder, or epilepsy. My impression was that patients or family members sought treatment for disorders that were conspicuous. I saw <5 cases of depression or anxiety. I wonder if this was because:
- patients with these disorders were referred to psychologists
- patients sought out faith-based treatment
- there was a lower incidence of these disorders, or these disorders were detected less frequently.
Inadequate funding. Despite the clinicians’ astute observations and diagnoses, they faced challenges, including a lack of access to medications because pharmacies were out of stock, or the patient or hospital could not afford the medication. At times, these challenges resulted in patients admitted to the hospital not receiving medications. When Mental Health Act 846 was implemented, it was widely purported that mental health care would be available to everyone, but the funding mechanism was not firmly established.8,9 Currently, laboratory workup, mental health treatment, and medications are not covered by health insurance, and government funding for mental health is insufficient. Therefore, in most areas, the entire cost burden of psychiatric care falls on patients and their families, or on hospitals.
Making progress despite barriers
In her inaugural address, former American Psychiatric Association President Altha J. Stewart, MD, named expanding the organization’s work in global mental health as one of her 3 primary goals.10 There are several means by which American psychiatrists can support the work of psychiatrists in Ghana and elsewhere. One way is by helping the mental health commission and other entities within the country petition the government and health insurance companies to expand coverage for mental health services. Teleconferencing, in which psychiatrists in Ghana or other parts of the world provide supervision to mid-level clinicians, has been piloted in other countries such as Liberia and could be implemented to address the critical shortages of psychiatrists in certain regions.11
In the past 7 years, Ghana has made significant strides in destigmatizing mental illness, and as a result more individuals are seeking treatment and more clinicians at all levels are being trained. Despite significant barriers, physicians, nurses, and other mental health workers deliver empathic and evidence-based treatment in a manner that defies the mental health system’s current limitations.
1. Ofori-Atta A, Attafuah J, Jack H, et al. Joining psychiatric care and faith healing in a prayer camp in Ghana: randomised trial. Br J Psychiatry. 2018;212(1):34-41.
2. Ghana has only 18 psychiatrists; experts beg government for more funds. GhanaWeb. https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Ghana-has-only-18-psychiatrists-experts-beg-government-for-more-funds-591732. Published October 17, 2017. Accessed July 24, 2019.
3. Agyapong VIO, Farren C, McAuliffe E. Improving Ghana’s mental healthcare through task-shifting-psychiatrists and health policy directors perceptions about government’s commitment and the role of community mental health workers. Global Health. 2016;12:57.
4. World Health Organization. Global Health Observatory data repository. http://apps.who.int/gho/data/node.main.MHHR?lang=en. Published April 25, 2019. Accessed July 24, 2019.
5. Walker GH, Osei A. Mental health law in Ghana. BJPsych Int. 2017;14(2):38-39.
6. Doku VC, Wusu-Takyi A, Awakame J. Implementing the Mental Health Act in Ghana: any challenges ahead? Ghana Med J. 2012;46(4):241-250.
7. Kissiedu E. High dose Tramadol floods market. Business Day. http://businessdayghana.com/high-dose-tramadol-floods-market/. Published September 25, 2017. Accessed July 24, 2019.
8. Badu E, O’Brien AP, Mitchell R. An integrative review of potential enablers and barriers to accessing mental health services in Ghana. Health Res Policy Syst. 2018;16(1):110.
9. Ghana mental health care delivery risks collapse for lack of funds. News Ghana. https://www.newsghana.com.gh/ghana-mental-health-care-delivery-risks-collapse-for-lack-of-funds/. Published May 29, 2018. Accessed July 24, 2019.
10. Stewart AJ. Response to the Presidential Address. Am J Psychiatry. 2018;175(8):726-727.
11. Katz, CL, Washington FB, Sacco M, et al. A resident-based telepsychiatry supervision pilot program in Liberia. Psychiatr Serv. 2018;70(3):243-246.
In recent years, the delivery of mental health services in Ghana has expanded substantially, especially since the passing of the Mental Health Act in 2012. In this article, I reflect on my experience as a visiting psychiatry resident in August 2018 at 2 Ghanaian hospitals located in Accra and Navrongo. Evident strengths of the mental health system were family support for patients and the scope of psychiatrists, while the most prominent weakness was the inadequate funding. As treatment of mental illness expands, more funding, psychiatrists, and mental health workers will be critical for the continued success of Ghana’s mental health system.
Psychiatric treatment in Ghana
Ghana has a population of approximately 28 million people, yet the country has an estimated 18 to 25 psychiatrists, up from 11 psychiatrists in 2011.1-3 Compared with the United States, which has 10.54 psychiatrists per 100,000 people (approximately 1 psychiatrist per 9,500 people), Ghana has .058 psychiatrists per 100,000 people (approximately 1 psychiatrist per 1.7 million people).4 In Ghana, most psychiatric care is delivered by mental health nurses, community mental health officers (CMHOs), and clinical psychiatric officers; supervision by psychiatrists is limited.3 Due to low public awareness, a scarcity of clinicians, and limited access to diagnostic services and medications, individuals with psychiatric illness in Ghana are often stigmatized, undertreated, and mistreated. To address this, in March 2012, Ghana passed Mental Health Act 846, which established a mental health commission and outlined protections for individuals with mental health needs.5 Since then, the number of people seeking treatment and the number of clinicians have expanded, but there are still significant challenges, such as a lack of funding for medications and facilities, and limited clinicians.6
During my last year of psychiatry residency at Mount Sinai Hospital in New York, I spent several weeks in Ghana at 2 institutions, observing and supervising the provision of psychiatric services. This was my first experience with the country’s health care system; therefore, my objectives were to:
- assess the current state of psychiatric services through observation and interviews with clinical staff
- provide instruction to clinicians in areas of need.
Two-thirds of my time was spent at the Accra Psychiatric Hospital, 1 of only 3 psychiatric hospitals in Ghana, all of which are located in the southern region of the country. The remainder of my time was spent at the Navrongo War Memorial Hospital in Ghana’s Northern Region.
The Accra Psychiatric Hospital is a sprawling complex near the center of the capital city. Every morning I walked through a large outdoor waiting area to the examination room, which was filled with at least 30 patients by 9
Navrongo War Memorial Hospital. There are no practicing psychiatrists in the northern region of the country; therefore, all mental health care is delivered by mental health nurses and CMHOs. CMHOs have 1 year of training plus a minimum of 2 years of service. They focus on identifying psychiatric cases in the community and coordinating treatment. Nurses have prescribing rights. A psychiatrist should be scheduled to visit the various districts in the region every 6 months to provide supervision, but this is not always feasible.
When I visited, I was the only psychiatrist who had been to this hospital in more than 1 year. During my time there, I reviewed the treatment protocols and gave lectures on the management of psychiatric emergencies and motivational interviewing, because addiction to alcohol and tramadol are 2 of the most pressing mental health problems in the country.7 I also saw patients with nurses, and supervised them on their assessment and treatment.
Continue to: In Ghana...
In Ghana, psychiatric services are often delivered using the community mental health model, in which many patients are visited in their homes. One morning, we went to a prayer camp to see if there were any individuals who would benefit from psychiatric services. There were no cases that day, but during the visit I sat under a tree where a few years before it was not uncommon to find a person who was psychotic or agitated chained to the tree. Several years of outreach by the local nurses has resulted in the camp leaders better recognizing mental illness early and contacting the nurses, as opposed to locking a person in chains for an extended period.
On one occasion, we answered a crisis call where a person experiencing a psychotic episode had locked himself in his house. The team talked with the individual through a locked screen door for 30 minutes, after which he eventually came out of the home to speak with us. A few days later, the patient accepted fluphenazine decanoate injection at his home. Two weeks later, he came to the outpatient clinic to continue treatment. Four months later, the patient was still in treatment and had started an apprenticeship for repairing cars.
As I was walking out of the hospital on my last day, I was called back to see a woman with a seizure who had been brought to the hospital. Unfortunately, there was no more diazepam in stock with which to treat her. This event highlighted the lack of resources available in this setting.
3 Take-home messages
My experience at both hospitals led me to reflect on 3 important factors impacting the mental health system in Ghana:
Family support. For at least 80% of appointments, patients were accompanied by family members or friends. The family hierarchy is still dominant in the Ghanaian culture, and clinicians often need the buy-in of the family, especially when financial support is required. More often than not, families enhanced patients’ treatment, but in some instances, they were a barrier.
Continue to: The types of cases
The types of cases. Most of the patients coming to both hospitals had diagnoses of bipolar disorder, schizophrenia, substance use disorder, or epilepsy. My impression was that patients or family members sought treatment for disorders that were conspicuous. I saw <5 cases of depression or anxiety. I wonder if this was because:
- patients with these disorders were referred to psychologists
- patients sought out faith-based treatment
- there was a lower incidence of these disorders, or these disorders were detected less frequently.
Inadequate funding. Despite the clinicians’ astute observations and diagnoses, they faced challenges, including a lack of access to medications because pharmacies were out of stock, or the patient or hospital could not afford the medication. At times, these challenges resulted in patients admitted to the hospital not receiving medications. When Mental Health Act 846 was implemented, it was widely purported that mental health care would be available to everyone, but the funding mechanism was not firmly established.8,9 Currently, laboratory workup, mental health treatment, and medications are not covered by health insurance, and government funding for mental health is insufficient. Therefore, in most areas, the entire cost burden of psychiatric care falls on patients and their families, or on hospitals.
Making progress despite barriers
In her inaugural address, former American Psychiatric Association President Altha J. Stewart, MD, named expanding the organization’s work in global mental health as one of her 3 primary goals.10 There are several means by which American psychiatrists can support the work of psychiatrists in Ghana and elsewhere. One way is by helping the mental health commission and other entities within the country petition the government and health insurance companies to expand coverage for mental health services. Teleconferencing, in which psychiatrists in Ghana or other parts of the world provide supervision to mid-level clinicians, has been piloted in other countries such as Liberia and could be implemented to address the critical shortages of psychiatrists in certain regions.11
In the past 7 years, Ghana has made significant strides in destigmatizing mental illness, and as a result more individuals are seeking treatment and more clinicians at all levels are being trained. Despite significant barriers, physicians, nurses, and other mental health workers deliver empathic and evidence-based treatment in a manner that defies the mental health system’s current limitations.
In recent years, the delivery of mental health services in Ghana has expanded substantially, especially since the passing of the Mental Health Act in 2012. In this article, I reflect on my experience as a visiting psychiatry resident in August 2018 at 2 Ghanaian hospitals located in Accra and Navrongo. Evident strengths of the mental health system were family support for patients and the scope of psychiatrists, while the most prominent weakness was the inadequate funding. As treatment of mental illness expands, more funding, psychiatrists, and mental health workers will be critical for the continued success of Ghana’s mental health system.
Psychiatric treatment in Ghana
Ghana has a population of approximately 28 million people, yet the country has an estimated 18 to 25 psychiatrists, up from 11 psychiatrists in 2011.1-3 Compared with the United States, which has 10.54 psychiatrists per 100,000 people (approximately 1 psychiatrist per 9,500 people), Ghana has .058 psychiatrists per 100,000 people (approximately 1 psychiatrist per 1.7 million people).4 In Ghana, most psychiatric care is delivered by mental health nurses, community mental health officers (CMHOs), and clinical psychiatric officers; supervision by psychiatrists is limited.3 Due to low public awareness, a scarcity of clinicians, and limited access to diagnostic services and medications, individuals with psychiatric illness in Ghana are often stigmatized, undertreated, and mistreated. To address this, in March 2012, Ghana passed Mental Health Act 846, which established a mental health commission and outlined protections for individuals with mental health needs.5 Since then, the number of people seeking treatment and the number of clinicians have expanded, but there are still significant challenges, such as a lack of funding for medications and facilities, and limited clinicians.6
During my last year of psychiatry residency at Mount Sinai Hospital in New York, I spent several weeks in Ghana at 2 institutions, observing and supervising the provision of psychiatric services. This was my first experience with the country’s health care system; therefore, my objectives were to:
- assess the current state of psychiatric services through observation and interviews with clinical staff
- provide instruction to clinicians in areas of need.
Two-thirds of my time was spent at the Accra Psychiatric Hospital, 1 of only 3 psychiatric hospitals in Ghana, all of which are located in the southern region of the country. The remainder of my time was spent at the Navrongo War Memorial Hospital in Ghana’s Northern Region.
The Accra Psychiatric Hospital is a sprawling complex near the center of the capital city. Every morning I walked through a large outdoor waiting area to the examination room, which was filled with at least 30 patients by 9
Navrongo War Memorial Hospital. There are no practicing psychiatrists in the northern region of the country; therefore, all mental health care is delivered by mental health nurses and CMHOs. CMHOs have 1 year of training plus a minimum of 2 years of service. They focus on identifying psychiatric cases in the community and coordinating treatment. Nurses have prescribing rights. A psychiatrist should be scheduled to visit the various districts in the region every 6 months to provide supervision, but this is not always feasible.
When I visited, I was the only psychiatrist who had been to this hospital in more than 1 year. During my time there, I reviewed the treatment protocols and gave lectures on the management of psychiatric emergencies and motivational interviewing, because addiction to alcohol and tramadol are 2 of the most pressing mental health problems in the country.7 I also saw patients with nurses, and supervised them on their assessment and treatment.
Continue to: In Ghana...
In Ghana, psychiatric services are often delivered using the community mental health model, in which many patients are visited in their homes. One morning, we went to a prayer camp to see if there were any individuals who would benefit from psychiatric services. There were no cases that day, but during the visit I sat under a tree where a few years before it was not uncommon to find a person who was psychotic or agitated chained to the tree. Several years of outreach by the local nurses has resulted in the camp leaders better recognizing mental illness early and contacting the nurses, as opposed to locking a person in chains for an extended period.
On one occasion, we answered a crisis call where a person experiencing a psychotic episode had locked himself in his house. The team talked with the individual through a locked screen door for 30 minutes, after which he eventually came out of the home to speak with us. A few days later, the patient accepted fluphenazine decanoate injection at his home. Two weeks later, he came to the outpatient clinic to continue treatment. Four months later, the patient was still in treatment and had started an apprenticeship for repairing cars.
As I was walking out of the hospital on my last day, I was called back to see a woman with a seizure who had been brought to the hospital. Unfortunately, there was no more diazepam in stock with which to treat her. This event highlighted the lack of resources available in this setting.
3 Take-home messages
My experience at both hospitals led me to reflect on 3 important factors impacting the mental health system in Ghana:
Family support. For at least 80% of appointments, patients were accompanied by family members or friends. The family hierarchy is still dominant in the Ghanaian culture, and clinicians often need the buy-in of the family, especially when financial support is required. More often than not, families enhanced patients’ treatment, but in some instances, they were a barrier.
Continue to: The types of cases
The types of cases. Most of the patients coming to both hospitals had diagnoses of bipolar disorder, schizophrenia, substance use disorder, or epilepsy. My impression was that patients or family members sought treatment for disorders that were conspicuous. I saw <5 cases of depression or anxiety. I wonder if this was because:
- patients with these disorders were referred to psychologists
- patients sought out faith-based treatment
- there was a lower incidence of these disorders, or these disorders were detected less frequently.
Inadequate funding. Despite the clinicians’ astute observations and diagnoses, they faced challenges, including a lack of access to medications because pharmacies were out of stock, or the patient or hospital could not afford the medication. At times, these challenges resulted in patients admitted to the hospital not receiving medications. When Mental Health Act 846 was implemented, it was widely purported that mental health care would be available to everyone, but the funding mechanism was not firmly established.8,9 Currently, laboratory workup, mental health treatment, and medications are not covered by health insurance, and government funding for mental health is insufficient. Therefore, in most areas, the entire cost burden of psychiatric care falls on patients and their families, or on hospitals.
Making progress despite barriers
In her inaugural address, former American Psychiatric Association President Altha J. Stewart, MD, named expanding the organization’s work in global mental health as one of her 3 primary goals.10 There are several means by which American psychiatrists can support the work of psychiatrists in Ghana and elsewhere. One way is by helping the mental health commission and other entities within the country petition the government and health insurance companies to expand coverage for mental health services. Teleconferencing, in which psychiatrists in Ghana or other parts of the world provide supervision to mid-level clinicians, has been piloted in other countries such as Liberia and could be implemented to address the critical shortages of psychiatrists in certain regions.11
In the past 7 years, Ghana has made significant strides in destigmatizing mental illness, and as a result more individuals are seeking treatment and more clinicians at all levels are being trained. Despite significant barriers, physicians, nurses, and other mental health workers deliver empathic and evidence-based treatment in a manner that defies the mental health system’s current limitations.
1. Ofori-Atta A, Attafuah J, Jack H, et al. Joining psychiatric care and faith healing in a prayer camp in Ghana: randomised trial. Br J Psychiatry. 2018;212(1):34-41.
2. Ghana has only 18 psychiatrists; experts beg government for more funds. GhanaWeb. https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Ghana-has-only-18-psychiatrists-experts-beg-government-for-more-funds-591732. Published October 17, 2017. Accessed July 24, 2019.
3. Agyapong VIO, Farren C, McAuliffe E. Improving Ghana’s mental healthcare through task-shifting-psychiatrists and health policy directors perceptions about government’s commitment and the role of community mental health workers. Global Health. 2016;12:57.
4. World Health Organization. Global Health Observatory data repository. http://apps.who.int/gho/data/node.main.MHHR?lang=en. Published April 25, 2019. Accessed July 24, 2019.
5. Walker GH, Osei A. Mental health law in Ghana. BJPsych Int. 2017;14(2):38-39.
6. Doku VC, Wusu-Takyi A, Awakame J. Implementing the Mental Health Act in Ghana: any challenges ahead? Ghana Med J. 2012;46(4):241-250.
7. Kissiedu E. High dose Tramadol floods market. Business Day. http://businessdayghana.com/high-dose-tramadol-floods-market/. Published September 25, 2017. Accessed July 24, 2019.
8. Badu E, O’Brien AP, Mitchell R. An integrative review of potential enablers and barriers to accessing mental health services in Ghana. Health Res Policy Syst. 2018;16(1):110.
9. Ghana mental health care delivery risks collapse for lack of funds. News Ghana. https://www.newsghana.com.gh/ghana-mental-health-care-delivery-risks-collapse-for-lack-of-funds/. Published May 29, 2018. Accessed July 24, 2019.
10. Stewart AJ. Response to the Presidential Address. Am J Psychiatry. 2018;175(8):726-727.
11. Katz, CL, Washington FB, Sacco M, et al. A resident-based telepsychiatry supervision pilot program in Liberia. Psychiatr Serv. 2018;70(3):243-246.
1. Ofori-Atta A, Attafuah J, Jack H, et al. Joining psychiatric care and faith healing in a prayer camp in Ghana: randomised trial. Br J Psychiatry. 2018;212(1):34-41.
2. Ghana has only 18 psychiatrists; experts beg government for more funds. GhanaWeb. https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Ghana-has-only-18-psychiatrists-experts-beg-government-for-more-funds-591732. Published October 17, 2017. Accessed July 24, 2019.
3. Agyapong VIO, Farren C, McAuliffe E. Improving Ghana’s mental healthcare through task-shifting-psychiatrists and health policy directors perceptions about government’s commitment and the role of community mental health workers. Global Health. 2016;12:57.
4. World Health Organization. Global Health Observatory data repository. http://apps.who.int/gho/data/node.main.MHHR?lang=en. Published April 25, 2019. Accessed July 24, 2019.
5. Walker GH, Osei A. Mental health law in Ghana. BJPsych Int. 2017;14(2):38-39.
6. Doku VC, Wusu-Takyi A, Awakame J. Implementing the Mental Health Act in Ghana: any challenges ahead? Ghana Med J. 2012;46(4):241-250.
7. Kissiedu E. High dose Tramadol floods market. Business Day. http://businessdayghana.com/high-dose-tramadol-floods-market/. Published September 25, 2017. Accessed July 24, 2019.
8. Badu E, O’Brien AP, Mitchell R. An integrative review of potential enablers and barriers to accessing mental health services in Ghana. Health Res Policy Syst. 2018;16(1):110.
9. Ghana mental health care delivery risks collapse for lack of funds. News Ghana. https://www.newsghana.com.gh/ghana-mental-health-care-delivery-risks-collapse-for-lack-of-funds/. Published May 29, 2018. Accessed July 24, 2019.
10. Stewart AJ. Response to the Presidential Address. Am J Psychiatry. 2018;175(8):726-727.
11. Katz, CL, Washington FB, Sacco M, et al. A resident-based telepsychiatry supervision pilot program in Liberia. Psychiatr Serv. 2018;70(3):243-246.
The challenges of caring for a physician with a mental illness
A physician’s mental health is important for the delivery of quality health care to his/her patients. Early identification and treatment of physicians with mental illnesses is challenging because physicians may neglect their own mental health due to the associated stigma, time constraints, or uncertainty regarding where to seek help. Physicians often worry about whom to confide in and harbor a fear that others will doubt his/her competence after recovery.1 Physicians have higher rates of suicide than the general population.2 According to data from the National Violent Death Reporting System, a diagnosed mental illness or a job problem significantly contribute to suicide among physicians.3 Additionally, physicians also have high rates of substance use and affective disorders.1,4
Here, we present the case of a physician we treated on an inpatient psychiatry unit who stirred profound emotions in us as trainees, and discuss how we managed this complicated scenario.
CASE REPORT
Dr. P, a 35-year-old male endocrinologist, was admitted to our inpatient psychiatry unit with a diagnosis of bipolar disorder, manic, severe, with psychotic features. Earlier that day, Dr. P had walked out of his private outpatient practice where he still had several appointments. After he had been missing for several hours, he was picked up by the police. Dr. P had 2 prior psychiatric admissions; the last one had occurred >10 years ago. A few weeks before this admission, he stopped taking lithium, while continuing escitalopram. He had not been keeping his appointments with his outpatient psychiatrist.
At admission, Dr. P had pressured speech, grandiose delusions, an expansive affect, and aggressive behavior. He was responding to internal stimuli with no insight into his illness. He was evasive when asked about hallucinations. Dr. P believed he was superior in intelligence and physical prowess to everyone in the emergency department (ED), and for that reason, the ED staff was persecuting him. His urine toxicology was negative.
On the inpatient unit, because Dr. P exhibited posturing, mutism, and negativism, catatonia associated with bipolar disorder was added to his diagnosis. For the first 2 days, his catatonia was managed with oral lorazepam, 2 mg twice daily. Dr. P was also observed giving medical advice to other patients on the unit, and was told to stop. Throughout his hospitalization, he dictated his own treatment and would frequently debate with his treatment team on the pharmacologic basis for treatment decisions, asserting his expertise as a physician and claiming to have a general clinical knowledge of the acute management of bipolar disorder.
Dr. P was eventually stabilized on oral lithium, 450 mg twice daily, and aripiprazole, 10 mg/d. He also received oral clonazepam, as needed for acute agitation, which was eventually tapered and discontinued. He gradually responded to treatment, and demonstrated improved insight. The treatment team met with Dr. P’s parents, who also were physicians, to discuss treatment goals, management considerations, and an aftercare plan. After spending 8 days in the hospital, Dr. P was discharged home to the care of his immediate family, and instructed to follow up with his outpatient psychiatrist. We do not know if he resumed clinical duties.
Managing an extremely knowledgeable patient
During his hospitalization, Dr. P frequently challenged our clinical knowledge; he would repeatedly remind us that he was a physician and that we were still trainees, which caused us to second-guess ourselves. Eventually, the attending physician on our team was able to impress upon Dr. P the clearly established roles of the treatment team and the patient. It was also important to maintain open communication channels with Dr. P and his family, and to address his anxiety by discussing the treatment plan in detail.5
Continue to: Although his queries on medication...
Although his queries on medication pharmacodynamics and pharmacokinetics were daunting, we empathized with him, recognizing that his knowledge invariably contributed to his anxiety. We engaged with Dr. P and his parents and elaborated on the rationale behind treatment decisions. This earned his trust and tremendously facilitated his recovery.
We were also cautious about using benzodiazepines to treat Dr. P’s catatonia because we were concerned that his knowledge could aid him in feigning symptoms to obtain these medications. Physicians have a high rate of prescription medication abuse, mainly opiates and benzodiazepines.2 The abuse of prescription medications by physicians is related to several psychological and psychiatric factors, including anxiety, depression, stress at work, personality problems, loss of loved ones, and pain. While treating physician patients, treatment decisions that include the use of opiates and benzodiazepines should be carefully considered.
A complicated scenario
Managing a physician patient can be a rewarding experience; however, there are several factors that can impact the experience, including:
- The treating physicians’ anxiety and countertransference/transference dynamics. We repeatedly imagined ourselves in Dr. P’s position and thought long and hard about how this scenario could happen to anyone in the medical profession; these thoughts induced significant anxiety in each of us. Further, interacting with Dr. P was reminiscent of our training under senior residents and attendings. Dr. P viewed us—his treatment team—as his trainees and challenged our clinical knowledge and actions.
- The physician-patient’s emotional responses, which may include anxiety, despair, denial, and an inability to accept role reversal.
Our medical culture needs a paradigm shift. We need a model designed to encourage early self-disclosure and treatment-seeking among physicians with mental illness. This will reduce the stigma towards mental illness in our profession.
1. Bianchi EF, Bhattacharyya MR, Meakin R. Exploring senior doctors’ beliefs and attitudes regarding mental illness within the medical profession: a qualitative study. BMJ Open. 2016;6(9):e012598. doi: 10.1136/bmjopen-2016 012598.
2. Schernhammer ES, Colditz GA. Suicide rates among physicians: a quantitative and gender assessment (meta-analysis). Am J Psychiatry. 2004;161(12):2295-2302.
3. Gold KJ, Sen A, Schwenk TL. Details on suicide among US physicians: data from the National Violent Death Reporting System. Gen Hosp Psychiatry. 2013;35(1):45-49.
4. Schneck SA. “Doctoring” doctors and their families. JAMA. 1998;280(23):2039-2042.
5. Marshall EJ. Doctors’ health and fitness to practise: treating addicted doctors. Occup Med (Lond). 2008;58(5):334-340.
A physician’s mental health is important for the delivery of quality health care to his/her patients. Early identification and treatment of physicians with mental illnesses is challenging because physicians may neglect their own mental health due to the associated stigma, time constraints, or uncertainty regarding where to seek help. Physicians often worry about whom to confide in and harbor a fear that others will doubt his/her competence after recovery.1 Physicians have higher rates of suicide than the general population.2 According to data from the National Violent Death Reporting System, a diagnosed mental illness or a job problem significantly contribute to suicide among physicians.3 Additionally, physicians also have high rates of substance use and affective disorders.1,4
Here, we present the case of a physician we treated on an inpatient psychiatry unit who stirred profound emotions in us as trainees, and discuss how we managed this complicated scenario.
CASE REPORT
Dr. P, a 35-year-old male endocrinologist, was admitted to our inpatient psychiatry unit with a diagnosis of bipolar disorder, manic, severe, with psychotic features. Earlier that day, Dr. P had walked out of his private outpatient practice where he still had several appointments. After he had been missing for several hours, he was picked up by the police. Dr. P had 2 prior psychiatric admissions; the last one had occurred >10 years ago. A few weeks before this admission, he stopped taking lithium, while continuing escitalopram. He had not been keeping his appointments with his outpatient psychiatrist.
At admission, Dr. P had pressured speech, grandiose delusions, an expansive affect, and aggressive behavior. He was responding to internal stimuli with no insight into his illness. He was evasive when asked about hallucinations. Dr. P believed he was superior in intelligence and physical prowess to everyone in the emergency department (ED), and for that reason, the ED staff was persecuting him. His urine toxicology was negative.
On the inpatient unit, because Dr. P exhibited posturing, mutism, and negativism, catatonia associated with bipolar disorder was added to his diagnosis. For the first 2 days, his catatonia was managed with oral lorazepam, 2 mg twice daily. Dr. P was also observed giving medical advice to other patients on the unit, and was told to stop. Throughout his hospitalization, he dictated his own treatment and would frequently debate with his treatment team on the pharmacologic basis for treatment decisions, asserting his expertise as a physician and claiming to have a general clinical knowledge of the acute management of bipolar disorder.
Dr. P was eventually stabilized on oral lithium, 450 mg twice daily, and aripiprazole, 10 mg/d. He also received oral clonazepam, as needed for acute agitation, which was eventually tapered and discontinued. He gradually responded to treatment, and demonstrated improved insight. The treatment team met with Dr. P’s parents, who also were physicians, to discuss treatment goals, management considerations, and an aftercare plan. After spending 8 days in the hospital, Dr. P was discharged home to the care of his immediate family, and instructed to follow up with his outpatient psychiatrist. We do not know if he resumed clinical duties.
Managing an extremely knowledgeable patient
During his hospitalization, Dr. P frequently challenged our clinical knowledge; he would repeatedly remind us that he was a physician and that we were still trainees, which caused us to second-guess ourselves. Eventually, the attending physician on our team was able to impress upon Dr. P the clearly established roles of the treatment team and the patient. It was also important to maintain open communication channels with Dr. P and his family, and to address his anxiety by discussing the treatment plan in detail.5
Continue to: Although his queries on medication...
Although his queries on medication pharmacodynamics and pharmacokinetics were daunting, we empathized with him, recognizing that his knowledge invariably contributed to his anxiety. We engaged with Dr. P and his parents and elaborated on the rationale behind treatment decisions. This earned his trust and tremendously facilitated his recovery.
We were also cautious about using benzodiazepines to treat Dr. P’s catatonia because we were concerned that his knowledge could aid him in feigning symptoms to obtain these medications. Physicians have a high rate of prescription medication abuse, mainly opiates and benzodiazepines.2 The abuse of prescription medications by physicians is related to several psychological and psychiatric factors, including anxiety, depression, stress at work, personality problems, loss of loved ones, and pain. While treating physician patients, treatment decisions that include the use of opiates and benzodiazepines should be carefully considered.
A complicated scenario
Managing a physician patient can be a rewarding experience; however, there are several factors that can impact the experience, including:
- The treating physicians’ anxiety and countertransference/transference dynamics. We repeatedly imagined ourselves in Dr. P’s position and thought long and hard about how this scenario could happen to anyone in the medical profession; these thoughts induced significant anxiety in each of us. Further, interacting with Dr. P was reminiscent of our training under senior residents and attendings. Dr. P viewed us—his treatment team—as his trainees and challenged our clinical knowledge and actions.
- The physician-patient’s emotional responses, which may include anxiety, despair, denial, and an inability to accept role reversal.
Our medical culture needs a paradigm shift. We need a model designed to encourage early self-disclosure and treatment-seeking among physicians with mental illness. This will reduce the stigma towards mental illness in our profession.
A physician’s mental health is important for the delivery of quality health care to his/her patients. Early identification and treatment of physicians with mental illnesses is challenging because physicians may neglect their own mental health due to the associated stigma, time constraints, or uncertainty regarding where to seek help. Physicians often worry about whom to confide in and harbor a fear that others will doubt his/her competence after recovery.1 Physicians have higher rates of suicide than the general population.2 According to data from the National Violent Death Reporting System, a diagnosed mental illness or a job problem significantly contribute to suicide among physicians.3 Additionally, physicians also have high rates of substance use and affective disorders.1,4
Here, we present the case of a physician we treated on an inpatient psychiatry unit who stirred profound emotions in us as trainees, and discuss how we managed this complicated scenario.
CASE REPORT
Dr. P, a 35-year-old male endocrinologist, was admitted to our inpatient psychiatry unit with a diagnosis of bipolar disorder, manic, severe, with psychotic features. Earlier that day, Dr. P had walked out of his private outpatient practice where he still had several appointments. After he had been missing for several hours, he was picked up by the police. Dr. P had 2 prior psychiatric admissions; the last one had occurred >10 years ago. A few weeks before this admission, he stopped taking lithium, while continuing escitalopram. He had not been keeping his appointments with his outpatient psychiatrist.
At admission, Dr. P had pressured speech, grandiose delusions, an expansive affect, and aggressive behavior. He was responding to internal stimuli with no insight into his illness. He was evasive when asked about hallucinations. Dr. P believed he was superior in intelligence and physical prowess to everyone in the emergency department (ED), and for that reason, the ED staff was persecuting him. His urine toxicology was negative.
On the inpatient unit, because Dr. P exhibited posturing, mutism, and negativism, catatonia associated with bipolar disorder was added to his diagnosis. For the first 2 days, his catatonia was managed with oral lorazepam, 2 mg twice daily. Dr. P was also observed giving medical advice to other patients on the unit, and was told to stop. Throughout his hospitalization, he dictated his own treatment and would frequently debate with his treatment team on the pharmacologic basis for treatment decisions, asserting his expertise as a physician and claiming to have a general clinical knowledge of the acute management of bipolar disorder.
Dr. P was eventually stabilized on oral lithium, 450 mg twice daily, and aripiprazole, 10 mg/d. He also received oral clonazepam, as needed for acute agitation, which was eventually tapered and discontinued. He gradually responded to treatment, and demonstrated improved insight. The treatment team met with Dr. P’s parents, who also were physicians, to discuss treatment goals, management considerations, and an aftercare plan. After spending 8 days in the hospital, Dr. P was discharged home to the care of his immediate family, and instructed to follow up with his outpatient psychiatrist. We do not know if he resumed clinical duties.
Managing an extremely knowledgeable patient
During his hospitalization, Dr. P frequently challenged our clinical knowledge; he would repeatedly remind us that he was a physician and that we were still trainees, which caused us to second-guess ourselves. Eventually, the attending physician on our team was able to impress upon Dr. P the clearly established roles of the treatment team and the patient. It was also important to maintain open communication channels with Dr. P and his family, and to address his anxiety by discussing the treatment plan in detail.5
Continue to: Although his queries on medication...
Although his queries on medication pharmacodynamics and pharmacokinetics were daunting, we empathized with him, recognizing that his knowledge invariably contributed to his anxiety. We engaged with Dr. P and his parents and elaborated on the rationale behind treatment decisions. This earned his trust and tremendously facilitated his recovery.
We were also cautious about using benzodiazepines to treat Dr. P’s catatonia because we were concerned that his knowledge could aid him in feigning symptoms to obtain these medications. Physicians have a high rate of prescription medication abuse, mainly opiates and benzodiazepines.2 The abuse of prescription medications by physicians is related to several psychological and psychiatric factors, including anxiety, depression, stress at work, personality problems, loss of loved ones, and pain. While treating physician patients, treatment decisions that include the use of opiates and benzodiazepines should be carefully considered.
A complicated scenario
Managing a physician patient can be a rewarding experience; however, there are several factors that can impact the experience, including:
- The treating physicians’ anxiety and countertransference/transference dynamics. We repeatedly imagined ourselves in Dr. P’s position and thought long and hard about how this scenario could happen to anyone in the medical profession; these thoughts induced significant anxiety in each of us. Further, interacting with Dr. P was reminiscent of our training under senior residents and attendings. Dr. P viewed us—his treatment team—as his trainees and challenged our clinical knowledge and actions.
- The physician-patient’s emotional responses, which may include anxiety, despair, denial, and an inability to accept role reversal.
Our medical culture needs a paradigm shift. We need a model designed to encourage early self-disclosure and treatment-seeking among physicians with mental illness. This will reduce the stigma towards mental illness in our profession.
1. Bianchi EF, Bhattacharyya MR, Meakin R. Exploring senior doctors’ beliefs and attitudes regarding mental illness within the medical profession: a qualitative study. BMJ Open. 2016;6(9):e012598. doi: 10.1136/bmjopen-2016 012598.
2. Schernhammer ES, Colditz GA. Suicide rates among physicians: a quantitative and gender assessment (meta-analysis). Am J Psychiatry. 2004;161(12):2295-2302.
3. Gold KJ, Sen A, Schwenk TL. Details on suicide among US physicians: data from the National Violent Death Reporting System. Gen Hosp Psychiatry. 2013;35(1):45-49.
4. Schneck SA. “Doctoring” doctors and their families. JAMA. 1998;280(23):2039-2042.
5. Marshall EJ. Doctors’ health and fitness to practise: treating addicted doctors. Occup Med (Lond). 2008;58(5):334-340.
1. Bianchi EF, Bhattacharyya MR, Meakin R. Exploring senior doctors’ beliefs and attitudes regarding mental illness within the medical profession: a qualitative study. BMJ Open. 2016;6(9):e012598. doi: 10.1136/bmjopen-2016 012598.
2. Schernhammer ES, Colditz GA. Suicide rates among physicians: a quantitative and gender assessment (meta-analysis). Am J Psychiatry. 2004;161(12):2295-2302.
3. Gold KJ, Sen A, Schwenk TL. Details on suicide among US physicians: data from the National Violent Death Reporting System. Gen Hosp Psychiatry. 2013;35(1):45-49.
4. Schneck SA. “Doctoring” doctors and their families. JAMA. 1998;280(23):2039-2042.
5. Marshall EJ. Doctors’ health and fitness to practise: treating addicted doctors. Occup Med (Lond). 2008;58(5):334-340.
Autism, pain, and the NMDA receptor
Ms. G, a 36-year-old woman, presented to the emergency department (ED) requesting a neurologic evaluation. She told clinicians she had “NMDA receptor encephalitis.”
Ms. G reported successful self-treatment of “life-long” body pain that was precipitated by multiple external stimuli (food, social encounters, interpersonal conflict, etc.). Through her own research, she had learned that both ketamine and magnesium could alter nociception in rats through N-methyl-
In the ED, Ms. G had a labile affect, pressured speech, and flight of ideas. She denied any history of psychiatric treatment, suicide attempts, or substance abuse. Ms. G’s family reported she had been unusually social, talkative, and impulsive. She was admitted to the inpatient psychiatric unit with a diagnosis of mania.
On psychiatric evaluation, Ms. G was grandiose, irritable, and perseverative about her aberrant symptoms. She felt she did not experience the world as other people did, but found relief from her chronic pain after taking Delsym. She was not taking other medications. Ms. G did not report a family history of bipolar disorder or psychosis. Her laboratory results, including a comprehensive metabolic panel, complete blood count, lipid panel, thyroid studies, urine drug screening, and urinalysis, were unremarkable. Her blood pressure was mildly elevated (141/82 mm Hg).
Ms. G’s eventual diagnosis was substance-induced mania (DXM). The DXM-containing cough syrup and magnesium were discontinued in the hospital. She was stabilized on lithium extended-release, 900 mg/d (blood level 0.8 mmol/L), and olanzapine, 10 mg/d at bedtime. However, after discharge, Ms. G resumed using Delsym, which resulted in 3 subsequent psychiatric hospitalizations for mania during the next year.
I first treated Ms. G as an outpatient after her second hospitalization. At that point, she was stable. Her mental status was calm and cooperative, and she had a linear thought process. At her baseline, in the absence of mania, she had a blunted affect. She understood that DXM caused her to have manic symptoms, but she continued to believe that Delsym and magnesium cured her physical suffering and social inhibition. I noticed Ms. G would use figurative language inappropriately. I later learned she had sensitivities to food textures and a specialized interest in electronics. Because of this, I suspected Ms. G was on the autism spectrum; she met several DSM-5 criteria for autism spectrum disorder (ASD), particularly deficits in social-emotional reciprocity, highly restricted interests, and hyperreactivity to sensory input.
Upon routine lab screening, Ms. G was found to have hypothyroidism, with a thyroid-stimulating hormone level of 6.67 mcIU/mL. This resolved after discontinuing lithium. Olanzapine caused adverse metabolic effects and also was discontinued. Ms. G remained euthymic without any mood-stabilizing medication, except during periods when she abused DXM, when she would again become manic. Eventually, her motivation to avoid hospitalization would promote her abstinence.
Continue to: Implications of NMDA receptor antagonism
Implications of NMDA receptor antagonism
The use of ketamine as an NMDA receptor antagonist for treating depression and other psychiatric illnesses has gained momentum. Esketamine, the S-enantiomer of racemic ketamine, is now available as an FDA-approved intranasal formulation for treatment-resistant depression. Ketamine stops afferent nociception to the brain and is used as an analgesic (at low concentrations) and anesthetic (at high concentrations).1
Dextromethorphan is abused as a recreational drug because at high doses it works similarly to both ketamine and phencyclidine. Individuals who abuse DXM can develop psychosis, motor/cognitive impairment, agitation, fevers, hypertension, tachycardia, and death.2 In patients with ASD, researchers have identified genetic variations of NMDA receptors that are linked to dysfunction of these receptors.3 In animal models, as well as in humans, researchers have found that suppression or excitation of the NMDA receptor can ameliorate ASD symptoms, including social withdrawal and repetitive behaviors.3
Many individuals with ASD suffer from sensory abnormalities, including a reduced sensitivity to pain or a crippling sensitivity to various stimuli. Patients with ASD may have difficulty describing these abnormalities, and as a result, they may be misdiagnosed. One case report described a 15-year-old girl diagnosed with social anxiety and chronic generalized pain when in social situations.4 Pediatric rheumatologists had diagnosed her with “amplified pain syndrome.” When she presented to a mental health clinic for a neurodevelopmental evaluation, she explained to clinicians how she simply “did not ‘get’ people; they are just empty shells” and subsequently was given a diagnosis of ASD.4
In psychiatric patients who have comorbid substance use disorders, it is vital for clinicians to not only detect the presence of substance misuse, but also to understand what drives the patient toward abuse. Ms. G’s case, with its combination of substance abuse and ASD, illustrates the importance of listening to our patients for more precise diagnostic formulations, which then shape our treatment recommendations.
1. Vadivelu N, Schermer E, Kodumudi V, et al. Role of ketamine for analgesia in adults and children. J Anaesthesiol Clin Pharmacol. 2016;32(3):298-306.
2. Martinak B, Bolis R, Black J, et al. Dextromethorphan in cough syrup: the poor man’s psychosis. Psychopharmacol Bull. 2017;47(4):59-63.
3. Lee E, Choi S, Kim E. NMDA receptor dysfunction in autism spectrum disorders. Curr Opin Pharmacol. 2015;20:8-13.
4. Clarke C. Autism spectrum disorder and amplified pain. Case Rep Psychiatry. 2015;2015:930874. doi: 10.1155/2015/930874.
Ms. G, a 36-year-old woman, presented to the emergency department (ED) requesting a neurologic evaluation. She told clinicians she had “NMDA receptor encephalitis.”
Ms. G reported successful self-treatment of “life-long” body pain that was precipitated by multiple external stimuli (food, social encounters, interpersonal conflict, etc.). Through her own research, she had learned that both ketamine and magnesium could alter nociception in rats through N-methyl-
In the ED, Ms. G had a labile affect, pressured speech, and flight of ideas. She denied any history of psychiatric treatment, suicide attempts, or substance abuse. Ms. G’s family reported she had been unusually social, talkative, and impulsive. She was admitted to the inpatient psychiatric unit with a diagnosis of mania.
On psychiatric evaluation, Ms. G was grandiose, irritable, and perseverative about her aberrant symptoms. She felt she did not experience the world as other people did, but found relief from her chronic pain after taking Delsym. She was not taking other medications. Ms. G did not report a family history of bipolar disorder or psychosis. Her laboratory results, including a comprehensive metabolic panel, complete blood count, lipid panel, thyroid studies, urine drug screening, and urinalysis, were unremarkable. Her blood pressure was mildly elevated (141/82 mm Hg).
Ms. G’s eventual diagnosis was substance-induced mania (DXM). The DXM-containing cough syrup and magnesium were discontinued in the hospital. She was stabilized on lithium extended-release, 900 mg/d (blood level 0.8 mmol/L), and olanzapine, 10 mg/d at bedtime. However, after discharge, Ms. G resumed using Delsym, which resulted in 3 subsequent psychiatric hospitalizations for mania during the next year.
I first treated Ms. G as an outpatient after her second hospitalization. At that point, she was stable. Her mental status was calm and cooperative, and she had a linear thought process. At her baseline, in the absence of mania, she had a blunted affect. She understood that DXM caused her to have manic symptoms, but she continued to believe that Delsym and magnesium cured her physical suffering and social inhibition. I noticed Ms. G would use figurative language inappropriately. I later learned she had sensitivities to food textures and a specialized interest in electronics. Because of this, I suspected Ms. G was on the autism spectrum; she met several DSM-5 criteria for autism spectrum disorder (ASD), particularly deficits in social-emotional reciprocity, highly restricted interests, and hyperreactivity to sensory input.
Upon routine lab screening, Ms. G was found to have hypothyroidism, with a thyroid-stimulating hormone level of 6.67 mcIU/mL. This resolved after discontinuing lithium. Olanzapine caused adverse metabolic effects and also was discontinued. Ms. G remained euthymic without any mood-stabilizing medication, except during periods when she abused DXM, when she would again become manic. Eventually, her motivation to avoid hospitalization would promote her abstinence.
Continue to: Implications of NMDA receptor antagonism
Implications of NMDA receptor antagonism
The use of ketamine as an NMDA receptor antagonist for treating depression and other psychiatric illnesses has gained momentum. Esketamine, the S-enantiomer of racemic ketamine, is now available as an FDA-approved intranasal formulation for treatment-resistant depression. Ketamine stops afferent nociception to the brain and is used as an analgesic (at low concentrations) and anesthetic (at high concentrations).1
Dextromethorphan is abused as a recreational drug because at high doses it works similarly to both ketamine and phencyclidine. Individuals who abuse DXM can develop psychosis, motor/cognitive impairment, agitation, fevers, hypertension, tachycardia, and death.2 In patients with ASD, researchers have identified genetic variations of NMDA receptors that are linked to dysfunction of these receptors.3 In animal models, as well as in humans, researchers have found that suppression or excitation of the NMDA receptor can ameliorate ASD symptoms, including social withdrawal and repetitive behaviors.3
Many individuals with ASD suffer from sensory abnormalities, including a reduced sensitivity to pain or a crippling sensitivity to various stimuli. Patients with ASD may have difficulty describing these abnormalities, and as a result, they may be misdiagnosed. One case report described a 15-year-old girl diagnosed with social anxiety and chronic generalized pain when in social situations.4 Pediatric rheumatologists had diagnosed her with “amplified pain syndrome.” When she presented to a mental health clinic for a neurodevelopmental evaluation, she explained to clinicians how she simply “did not ‘get’ people; they are just empty shells” and subsequently was given a diagnosis of ASD.4
In psychiatric patients who have comorbid substance use disorders, it is vital for clinicians to not only detect the presence of substance misuse, but also to understand what drives the patient toward abuse. Ms. G’s case, with its combination of substance abuse and ASD, illustrates the importance of listening to our patients for more precise diagnostic formulations, which then shape our treatment recommendations.
Ms. G, a 36-year-old woman, presented to the emergency department (ED) requesting a neurologic evaluation. She told clinicians she had “NMDA receptor encephalitis.”
Ms. G reported successful self-treatment of “life-long” body pain that was precipitated by multiple external stimuli (food, social encounters, interpersonal conflict, etc.). Through her own research, she had learned that both ketamine and magnesium could alter nociception in rats through N-methyl-
In the ED, Ms. G had a labile affect, pressured speech, and flight of ideas. She denied any history of psychiatric treatment, suicide attempts, or substance abuse. Ms. G’s family reported she had been unusually social, talkative, and impulsive. She was admitted to the inpatient psychiatric unit with a diagnosis of mania.
On psychiatric evaluation, Ms. G was grandiose, irritable, and perseverative about her aberrant symptoms. She felt she did not experience the world as other people did, but found relief from her chronic pain after taking Delsym. She was not taking other medications. Ms. G did not report a family history of bipolar disorder or psychosis. Her laboratory results, including a comprehensive metabolic panel, complete blood count, lipid panel, thyroid studies, urine drug screening, and urinalysis, were unremarkable. Her blood pressure was mildly elevated (141/82 mm Hg).
Ms. G’s eventual diagnosis was substance-induced mania (DXM). The DXM-containing cough syrup and magnesium were discontinued in the hospital. She was stabilized on lithium extended-release, 900 mg/d (blood level 0.8 mmol/L), and olanzapine, 10 mg/d at bedtime. However, after discharge, Ms. G resumed using Delsym, which resulted in 3 subsequent psychiatric hospitalizations for mania during the next year.
I first treated Ms. G as an outpatient after her second hospitalization. At that point, she was stable. Her mental status was calm and cooperative, and she had a linear thought process. At her baseline, in the absence of mania, she had a blunted affect. She understood that DXM caused her to have manic symptoms, but she continued to believe that Delsym and magnesium cured her physical suffering and social inhibition. I noticed Ms. G would use figurative language inappropriately. I later learned she had sensitivities to food textures and a specialized interest in electronics. Because of this, I suspected Ms. G was on the autism spectrum; she met several DSM-5 criteria for autism spectrum disorder (ASD), particularly deficits in social-emotional reciprocity, highly restricted interests, and hyperreactivity to sensory input.
Upon routine lab screening, Ms. G was found to have hypothyroidism, with a thyroid-stimulating hormone level of 6.67 mcIU/mL. This resolved after discontinuing lithium. Olanzapine caused adverse metabolic effects and also was discontinued. Ms. G remained euthymic without any mood-stabilizing medication, except during periods when she abused DXM, when she would again become manic. Eventually, her motivation to avoid hospitalization would promote her abstinence.
Continue to: Implications of NMDA receptor antagonism
Implications of NMDA receptor antagonism
The use of ketamine as an NMDA receptor antagonist for treating depression and other psychiatric illnesses has gained momentum. Esketamine, the S-enantiomer of racemic ketamine, is now available as an FDA-approved intranasal formulation for treatment-resistant depression. Ketamine stops afferent nociception to the brain and is used as an analgesic (at low concentrations) and anesthetic (at high concentrations).1
Dextromethorphan is abused as a recreational drug because at high doses it works similarly to both ketamine and phencyclidine. Individuals who abuse DXM can develop psychosis, motor/cognitive impairment, agitation, fevers, hypertension, tachycardia, and death.2 In patients with ASD, researchers have identified genetic variations of NMDA receptors that are linked to dysfunction of these receptors.3 In animal models, as well as in humans, researchers have found that suppression or excitation of the NMDA receptor can ameliorate ASD symptoms, including social withdrawal and repetitive behaviors.3
Many individuals with ASD suffer from sensory abnormalities, including a reduced sensitivity to pain or a crippling sensitivity to various stimuli. Patients with ASD may have difficulty describing these abnormalities, and as a result, they may be misdiagnosed. One case report described a 15-year-old girl diagnosed with social anxiety and chronic generalized pain when in social situations.4 Pediatric rheumatologists had diagnosed her with “amplified pain syndrome.” When she presented to a mental health clinic for a neurodevelopmental evaluation, she explained to clinicians how she simply “did not ‘get’ people; they are just empty shells” and subsequently was given a diagnosis of ASD.4
In psychiatric patients who have comorbid substance use disorders, it is vital for clinicians to not only detect the presence of substance misuse, but also to understand what drives the patient toward abuse. Ms. G’s case, with its combination of substance abuse and ASD, illustrates the importance of listening to our patients for more precise diagnostic formulations, which then shape our treatment recommendations.
1. Vadivelu N, Schermer E, Kodumudi V, et al. Role of ketamine for analgesia in adults and children. J Anaesthesiol Clin Pharmacol. 2016;32(3):298-306.
2. Martinak B, Bolis R, Black J, et al. Dextromethorphan in cough syrup: the poor man’s psychosis. Psychopharmacol Bull. 2017;47(4):59-63.
3. Lee E, Choi S, Kim E. NMDA receptor dysfunction in autism spectrum disorders. Curr Opin Pharmacol. 2015;20:8-13.
4. Clarke C. Autism spectrum disorder and amplified pain. Case Rep Psychiatry. 2015;2015:930874. doi: 10.1155/2015/930874.
1. Vadivelu N, Schermer E, Kodumudi V, et al. Role of ketamine for analgesia in adults and children. J Anaesthesiol Clin Pharmacol. 2016;32(3):298-306.
2. Martinak B, Bolis R, Black J, et al. Dextromethorphan in cough syrup: the poor man’s psychosis. Psychopharmacol Bull. 2017;47(4):59-63.
3. Lee E, Choi S, Kim E. NMDA receptor dysfunction in autism spectrum disorders. Curr Opin Pharmacol. 2015;20:8-13.
4. Clarke C. Autism spectrum disorder and amplified pain. Case Rep Psychiatry. 2015;2015:930874. doi: 10.1155/2015/930874.
Career Choices: Forensic psychiatry
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Saeed Ahmed, MD, Addiction Psychiatry Fellow at Boston University Medical Center/Boston University School of Medicine, talked with Paul S. Appelbaum, MD, Elizabeth K. Dollard Professor of Psychiatry, Medicine, and Law, and Director, Center for Law, Ethics, and Psychiatry, Department of Psychiatry, Columbia University Vagelos College of Physicians and Surgeons. Dr. Appelbaum is currently Chair of the DSM Steering Committee for the American Psychiatric Association, and Co-chair of the Standing Committee on Ethics of the World Psychiatric Association. He performs forensic evaluations in civil and criminal cases, and treats patients with a broad variety of illnesses, including depression, anxiety, and adjustment problems.
Dr. Ahmed: What made you pick the forensic psychiatry track, and how did your training lead you towards this path?
Dr. Appelbaum: I was a debater in high school and college, and a fair number of our topics dealt with legal issues, which I’d always found intriguing. However, on entering medical school, I had assumed that I would need to leave those interests behind me. During the first week of medical school, though, we were all asked to select a behavioral science elective for the semester, and on the list was “Law and Psychiatry.” I didn’t know what it involved, but it sounded interesting, so I signed up. The class was taught by Dr. Alan Stone, a professor at Harvard Law School and the most important figure in the academic study of legal issues in psychiatry. By the end of the first class—on the Friday afternoon of my first week in medical school—I was so excited by the things we were discussing that I pretty much decided this was what I wanted to focus on in my career.
Later in medical school, I joined a research project looking at violence on the inpatient psychiatric units, as a way of broadening my knowledge of the field. During residency—we’re talking about the late 1970s, which was a time of great legal ferment about regulation of psychiatric practice—I persuaded my attending psychiatrist to join me in studying patients who were exercising their newly granted right to refuse treatment. That’s how Dr. Tom Gutheil and I started working together, a collaboration that continues today, with the publication of the 5th edition of our text, Clinical Handbook of Psychiatry and Law. I was also able to get foundation funding to do a study of patients’ decision-making capacities, a topic that has remained a focus of my research to the present day. During my final year of residency, I was able to create a chief residency in legal psychiatry, which allowed me to take law school courses, pursue my research, and supervise the more junior residents in their forensic evaluations.
Today, most people headed toward careers in forensic psychiatry take a fellowship after residency, but [such fellowships] were few and far between in 1980. So I went to Alan Stone for advice, and he said, “Go work with Loren Roth in Pittsburgh for 5 years, and you’ll be able to do anything you want after that.” I tracked down Loren Roth, then the leading empirical researcher on issues related to law and psychiatry, explained that Alan Stone had said I should go work with him, and somehow it all worked out. My first faculty job was with his Law and Psychiatry Program at the University of Pittsburgh.
Dr. Ahmed: What are some of the pros and cons of working in forensic psychiatry?
Continue to: Dr. Appelbaum...
Dr. Appelbaum: It may sound at first as though forensic psychiatry is a narrow subspecialty of psychiatry. But the field is actually immense, and the diversity of experiences that it provides is one of the big pros of a career in forensic psychiatry. On the academic side of the field, topics of research interest include prediction and management of violence, involuntary commitment and treatment, informed consent and decisional capacity, privacy and confidentiality of psychiatric treatment, criminal responsibility, and correctional treatment. Clinically, forensic psychiatrists perform a variety of evaluations, ranging from competence to consent to treatment, testamentary capacity, emotional harms in tort cases, psychiatric malpractice, sexual harassment and work-related disability, to competence to stand trial, voluntariness of confessions, insanity defense, and pre-sentencing assessments. Indeed, after nearly 40 years in the field, I still occasionally get asked to do evaluations of a type that I’ve never done before. Increasingly, forensic psychiatrists are involved in treating offenders, both in correctional facilities and in outpatient settings. Most people trained in forensic psychiatry mix their forensic work with general clinical work, whether inpatient or outpatient. So the flexibility that the field offers to craft a career is one of its great advantages.
On the cons side, a career in forensic psychiatry can mean a life of what Alan Stone called “moral peril.” By that he meant that forensic psychiatrists face constant ethical challenges as they perform evaluations and provide testimony. One challenge is to stay grounded in the evidence base of psychiatry and resist the temptation to draw conclusions that may seem “right” but that go beyond what psychiatric knowledge can actually support. Making that challenge even more difficult in private forensic practice is knowing that the party for whom one is working has specific interests that they are hoping you will support, and very definite ideas about what they want your conclusions to be. It may be in your financial interest to accommodate them, but in the long run, your reputation is your most valuable asset. Staying honest both to one’s beliefs and to the broader evidence base in psychiatry is an ongoing challenge, but a critical necessity.
Dr. Ahmed: Based on your personal experience, what should one consider when choosing a forensic psychiatry program?
Dr. Appelbaum: Having supervised forensic psychiatry fellowships for roughly 30 years, I think one of the most important aspects of a training program is its breadth. Given the diversity of the field, a program with a limited number of training sites that focuses on a restricted set of evaluations (usually related to criminal law) will not offer a fellow an optimal training experience. Diverse placements with a variety of evaluations to be performed under the supervision of experienced forensic psychiatrists, and without excessive service demands, are key aspects of a top-notch program. In addition, not everything can be learned hands-on; didactic training is indispensable. Fellows should be offered sufficient background on legal issues and the research base in forensic psychiatry to ground their subsequent work. Finally, for many fellows their time in fellowship is the last opportunity they may have to engage in research or other scholarly projects under supervision, another valuable component of a training program. A good question to ask of any program: What are your former fellows doing now? If the answers don’t reflect the career path you hope to pursue, that’s not the program for you.
Dr. Ahmed: What are some of the career options and work settings for forensic psychiatrists?
Continue to: Dr. Appelbaum...
Dr. Appelbaum: One of the advantages of forensic psychiatry is the plethora of work settings available. People headed to private practice can often combine clinical practice with forensic work, a necessity when starting one’s career and waiting to establish steady referral pipelines. Psychiatrists with forensic training are in demand in correctional facilities (which often pay higher salaries than comparable jobs in psychiatric facilities), forensic hospitals, and court clinics. Opportunities for academic involvement include directing fellowship programs, teaching residents, and conducting research. With regard to research, although funding is harder to come by than, for example, for studies of the biology of major psychiatric syndromes, determined psychiatrists can often find ways of framing questions related to forensic issues so that they appeal to funders’ priorities. As one gains experience, opportunities for consultation for law enforcement agencies, intelligence agencies, and federal and state mental health agencies may be available. It is rare for a forensic psychiatrist to do just one of these things; most forensic psychiatrists engage in a mix of types of work, including general clinical work. The possibilities are manifold.
Dr. Ahmed: What are some of the challenges in working in this field?
Dr. Appelbaum: I talked already about some of the ethical challenges in forensic psychiatry. In addition, as a subspecialty that applies psychiatric knowledge to legal questions, forensic psychiatry requires its practitioners to stay up-to-date with both advances in psychiatry and changes in the law, not to mention variations across jurisdictions. This is not an area of specialization in which one can pay attention during fellowship and then coast through a career. In my view, it’s also critical for a good forensic psychiatrist to be an excellent clinician; forensic cases frequently offer diagnostic challenges that require the highest level of clinical skills to address. Finally, for people early in their careers, it can take a few years before they are well-enough known to get a steady flow of private forensic cases. So having a plan B during that career phase will be essential.
Dr. Ahmed: Where do you see forensic psychiatry going?
Dr. Appelbaum: Forensic evaluations will need to incorporate new assessment techniques and new knowledge—although not before they have been demonstrated to be valid and reliable. I can foresee increased use of specialized neuroimaging assessments, genomic and other “omic” testing, and measurement of other neurophysiologic parameters. As we know more about the etiology of psychiatric disorders, that will impact everything from evaluations of causation in emotional harms cases to conclusions about which divorcing parent may be better able to handle primary custody of a child. I think there will be exciting opportunities in the coming decades to integrate growing scientific knowledge about psychiatric illnesses into forensic psychiatry.
Continue to: Dr. Ahmed...
Dr. Ahmed: What advice do you have for those contemplating a career in forensic psychiatry?
Dr. Appelbaum: Residents thinking about undertaking training in forensic psychiatry should come to one of the annual meetings of the American Academy of Psychiatry and the Law, the major professional organization of forensic psychiatrists, which takes place every October
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Saeed Ahmed, MD, Addiction Psychiatry Fellow at Boston University Medical Center/Boston University School of Medicine, talked with Paul S. Appelbaum, MD, Elizabeth K. Dollard Professor of Psychiatry, Medicine, and Law, and Director, Center for Law, Ethics, and Psychiatry, Department of Psychiatry, Columbia University Vagelos College of Physicians and Surgeons. Dr. Appelbaum is currently Chair of the DSM Steering Committee for the American Psychiatric Association, and Co-chair of the Standing Committee on Ethics of the World Psychiatric Association. He performs forensic evaluations in civil and criminal cases, and treats patients with a broad variety of illnesses, including depression, anxiety, and adjustment problems.
Dr. Ahmed: What made you pick the forensic psychiatry track, and how did your training lead you towards this path?
Dr. Appelbaum: I was a debater in high school and college, and a fair number of our topics dealt with legal issues, which I’d always found intriguing. However, on entering medical school, I had assumed that I would need to leave those interests behind me. During the first week of medical school, though, we were all asked to select a behavioral science elective for the semester, and on the list was “Law and Psychiatry.” I didn’t know what it involved, but it sounded interesting, so I signed up. The class was taught by Dr. Alan Stone, a professor at Harvard Law School and the most important figure in the academic study of legal issues in psychiatry. By the end of the first class—on the Friday afternoon of my first week in medical school—I was so excited by the things we were discussing that I pretty much decided this was what I wanted to focus on in my career.
Later in medical school, I joined a research project looking at violence on the inpatient psychiatric units, as a way of broadening my knowledge of the field. During residency—we’re talking about the late 1970s, which was a time of great legal ferment about regulation of psychiatric practice—I persuaded my attending psychiatrist to join me in studying patients who were exercising their newly granted right to refuse treatment. That’s how Dr. Tom Gutheil and I started working together, a collaboration that continues today, with the publication of the 5th edition of our text, Clinical Handbook of Psychiatry and Law. I was also able to get foundation funding to do a study of patients’ decision-making capacities, a topic that has remained a focus of my research to the present day. During my final year of residency, I was able to create a chief residency in legal psychiatry, which allowed me to take law school courses, pursue my research, and supervise the more junior residents in their forensic evaluations.
Today, most people headed toward careers in forensic psychiatry take a fellowship after residency, but [such fellowships] were few and far between in 1980. So I went to Alan Stone for advice, and he said, “Go work with Loren Roth in Pittsburgh for 5 years, and you’ll be able to do anything you want after that.” I tracked down Loren Roth, then the leading empirical researcher on issues related to law and psychiatry, explained that Alan Stone had said I should go work with him, and somehow it all worked out. My first faculty job was with his Law and Psychiatry Program at the University of Pittsburgh.
Dr. Ahmed: What are some of the pros and cons of working in forensic psychiatry?
Continue to: Dr. Appelbaum...
Dr. Appelbaum: It may sound at first as though forensic psychiatry is a narrow subspecialty of psychiatry. But the field is actually immense, and the diversity of experiences that it provides is one of the big pros of a career in forensic psychiatry. On the academic side of the field, topics of research interest include prediction and management of violence, involuntary commitment and treatment, informed consent and decisional capacity, privacy and confidentiality of psychiatric treatment, criminal responsibility, and correctional treatment. Clinically, forensic psychiatrists perform a variety of evaluations, ranging from competence to consent to treatment, testamentary capacity, emotional harms in tort cases, psychiatric malpractice, sexual harassment and work-related disability, to competence to stand trial, voluntariness of confessions, insanity defense, and pre-sentencing assessments. Indeed, after nearly 40 years in the field, I still occasionally get asked to do evaluations of a type that I’ve never done before. Increasingly, forensic psychiatrists are involved in treating offenders, both in correctional facilities and in outpatient settings. Most people trained in forensic psychiatry mix their forensic work with general clinical work, whether inpatient or outpatient. So the flexibility that the field offers to craft a career is one of its great advantages.
On the cons side, a career in forensic psychiatry can mean a life of what Alan Stone called “moral peril.” By that he meant that forensic psychiatrists face constant ethical challenges as they perform evaluations and provide testimony. One challenge is to stay grounded in the evidence base of psychiatry and resist the temptation to draw conclusions that may seem “right” but that go beyond what psychiatric knowledge can actually support. Making that challenge even more difficult in private forensic practice is knowing that the party for whom one is working has specific interests that they are hoping you will support, and very definite ideas about what they want your conclusions to be. It may be in your financial interest to accommodate them, but in the long run, your reputation is your most valuable asset. Staying honest both to one’s beliefs and to the broader evidence base in psychiatry is an ongoing challenge, but a critical necessity.
Dr. Ahmed: Based on your personal experience, what should one consider when choosing a forensic psychiatry program?
Dr. Appelbaum: Having supervised forensic psychiatry fellowships for roughly 30 years, I think one of the most important aspects of a training program is its breadth. Given the diversity of the field, a program with a limited number of training sites that focuses on a restricted set of evaluations (usually related to criminal law) will not offer a fellow an optimal training experience. Diverse placements with a variety of evaluations to be performed under the supervision of experienced forensic psychiatrists, and without excessive service demands, are key aspects of a top-notch program. In addition, not everything can be learned hands-on; didactic training is indispensable. Fellows should be offered sufficient background on legal issues and the research base in forensic psychiatry to ground their subsequent work. Finally, for many fellows their time in fellowship is the last opportunity they may have to engage in research or other scholarly projects under supervision, another valuable component of a training program. A good question to ask of any program: What are your former fellows doing now? If the answers don’t reflect the career path you hope to pursue, that’s not the program for you.
Dr. Ahmed: What are some of the career options and work settings for forensic psychiatrists?
Continue to: Dr. Appelbaum...
Dr. Appelbaum: One of the advantages of forensic psychiatry is the plethora of work settings available. People headed to private practice can often combine clinical practice with forensic work, a necessity when starting one’s career and waiting to establish steady referral pipelines. Psychiatrists with forensic training are in demand in correctional facilities (which often pay higher salaries than comparable jobs in psychiatric facilities), forensic hospitals, and court clinics. Opportunities for academic involvement include directing fellowship programs, teaching residents, and conducting research. With regard to research, although funding is harder to come by than, for example, for studies of the biology of major psychiatric syndromes, determined psychiatrists can often find ways of framing questions related to forensic issues so that they appeal to funders’ priorities. As one gains experience, opportunities for consultation for law enforcement agencies, intelligence agencies, and federal and state mental health agencies may be available. It is rare for a forensic psychiatrist to do just one of these things; most forensic psychiatrists engage in a mix of types of work, including general clinical work. The possibilities are manifold.
Dr. Ahmed: What are some of the challenges in working in this field?
Dr. Appelbaum: I talked already about some of the ethical challenges in forensic psychiatry. In addition, as a subspecialty that applies psychiatric knowledge to legal questions, forensic psychiatry requires its practitioners to stay up-to-date with both advances in psychiatry and changes in the law, not to mention variations across jurisdictions. This is not an area of specialization in which one can pay attention during fellowship and then coast through a career. In my view, it’s also critical for a good forensic psychiatrist to be an excellent clinician; forensic cases frequently offer diagnostic challenges that require the highest level of clinical skills to address. Finally, for people early in their careers, it can take a few years before they are well-enough known to get a steady flow of private forensic cases. So having a plan B during that career phase will be essential.
Dr. Ahmed: Where do you see forensic psychiatry going?
Dr. Appelbaum: Forensic evaluations will need to incorporate new assessment techniques and new knowledge—although not before they have been demonstrated to be valid and reliable. I can foresee increased use of specialized neuroimaging assessments, genomic and other “omic” testing, and measurement of other neurophysiologic parameters. As we know more about the etiology of psychiatric disorders, that will impact everything from evaluations of causation in emotional harms cases to conclusions about which divorcing parent may be better able to handle primary custody of a child. I think there will be exciting opportunities in the coming decades to integrate growing scientific knowledge about psychiatric illnesses into forensic psychiatry.
Continue to: Dr. Ahmed...
Dr. Ahmed: What advice do you have for those contemplating a career in forensic psychiatry?
Dr. Appelbaum: Residents thinking about undertaking training in forensic psychiatry should come to one of the annual meetings of the American Academy of Psychiatry and the Law, the major professional organization of forensic psychiatrists, which takes place every October
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Saeed Ahmed, MD, Addiction Psychiatry Fellow at Boston University Medical Center/Boston University School of Medicine, talked with Paul S. Appelbaum, MD, Elizabeth K. Dollard Professor of Psychiatry, Medicine, and Law, and Director, Center for Law, Ethics, and Psychiatry, Department of Psychiatry, Columbia University Vagelos College of Physicians and Surgeons. Dr. Appelbaum is currently Chair of the DSM Steering Committee for the American Psychiatric Association, and Co-chair of the Standing Committee on Ethics of the World Psychiatric Association. He performs forensic evaluations in civil and criminal cases, and treats patients with a broad variety of illnesses, including depression, anxiety, and adjustment problems.
Dr. Ahmed: What made you pick the forensic psychiatry track, and how did your training lead you towards this path?
Dr. Appelbaum: I was a debater in high school and college, and a fair number of our topics dealt with legal issues, which I’d always found intriguing. However, on entering medical school, I had assumed that I would need to leave those interests behind me. During the first week of medical school, though, we were all asked to select a behavioral science elective for the semester, and on the list was “Law and Psychiatry.” I didn’t know what it involved, but it sounded interesting, so I signed up. The class was taught by Dr. Alan Stone, a professor at Harvard Law School and the most important figure in the academic study of legal issues in psychiatry. By the end of the first class—on the Friday afternoon of my first week in medical school—I was so excited by the things we were discussing that I pretty much decided this was what I wanted to focus on in my career.
Later in medical school, I joined a research project looking at violence on the inpatient psychiatric units, as a way of broadening my knowledge of the field. During residency—we’re talking about the late 1970s, which was a time of great legal ferment about regulation of psychiatric practice—I persuaded my attending psychiatrist to join me in studying patients who were exercising their newly granted right to refuse treatment. That’s how Dr. Tom Gutheil and I started working together, a collaboration that continues today, with the publication of the 5th edition of our text, Clinical Handbook of Psychiatry and Law. I was also able to get foundation funding to do a study of patients’ decision-making capacities, a topic that has remained a focus of my research to the present day. During my final year of residency, I was able to create a chief residency in legal psychiatry, which allowed me to take law school courses, pursue my research, and supervise the more junior residents in their forensic evaluations.
Today, most people headed toward careers in forensic psychiatry take a fellowship after residency, but [such fellowships] were few and far between in 1980. So I went to Alan Stone for advice, and he said, “Go work with Loren Roth in Pittsburgh for 5 years, and you’ll be able to do anything you want after that.” I tracked down Loren Roth, then the leading empirical researcher on issues related to law and psychiatry, explained that Alan Stone had said I should go work with him, and somehow it all worked out. My first faculty job was with his Law and Psychiatry Program at the University of Pittsburgh.
Dr. Ahmed: What are some of the pros and cons of working in forensic psychiatry?
Continue to: Dr. Appelbaum...
Dr. Appelbaum: It may sound at first as though forensic psychiatry is a narrow subspecialty of psychiatry. But the field is actually immense, and the diversity of experiences that it provides is one of the big pros of a career in forensic psychiatry. On the academic side of the field, topics of research interest include prediction and management of violence, involuntary commitment and treatment, informed consent and decisional capacity, privacy and confidentiality of psychiatric treatment, criminal responsibility, and correctional treatment. Clinically, forensic psychiatrists perform a variety of evaluations, ranging from competence to consent to treatment, testamentary capacity, emotional harms in tort cases, psychiatric malpractice, sexual harassment and work-related disability, to competence to stand trial, voluntariness of confessions, insanity defense, and pre-sentencing assessments. Indeed, after nearly 40 years in the field, I still occasionally get asked to do evaluations of a type that I’ve never done before. Increasingly, forensic psychiatrists are involved in treating offenders, both in correctional facilities and in outpatient settings. Most people trained in forensic psychiatry mix their forensic work with general clinical work, whether inpatient or outpatient. So the flexibility that the field offers to craft a career is one of its great advantages.
On the cons side, a career in forensic psychiatry can mean a life of what Alan Stone called “moral peril.” By that he meant that forensic psychiatrists face constant ethical challenges as they perform evaluations and provide testimony. One challenge is to stay grounded in the evidence base of psychiatry and resist the temptation to draw conclusions that may seem “right” but that go beyond what psychiatric knowledge can actually support. Making that challenge even more difficult in private forensic practice is knowing that the party for whom one is working has specific interests that they are hoping you will support, and very definite ideas about what they want your conclusions to be. It may be in your financial interest to accommodate them, but in the long run, your reputation is your most valuable asset. Staying honest both to one’s beliefs and to the broader evidence base in psychiatry is an ongoing challenge, but a critical necessity.
Dr. Ahmed: Based on your personal experience, what should one consider when choosing a forensic psychiatry program?
Dr. Appelbaum: Having supervised forensic psychiatry fellowships for roughly 30 years, I think one of the most important aspects of a training program is its breadth. Given the diversity of the field, a program with a limited number of training sites that focuses on a restricted set of evaluations (usually related to criminal law) will not offer a fellow an optimal training experience. Diverse placements with a variety of evaluations to be performed under the supervision of experienced forensic psychiatrists, and without excessive service demands, are key aspects of a top-notch program. In addition, not everything can be learned hands-on; didactic training is indispensable. Fellows should be offered sufficient background on legal issues and the research base in forensic psychiatry to ground their subsequent work. Finally, for many fellows their time in fellowship is the last opportunity they may have to engage in research or other scholarly projects under supervision, another valuable component of a training program. A good question to ask of any program: What are your former fellows doing now? If the answers don’t reflect the career path you hope to pursue, that’s not the program for you.
Dr. Ahmed: What are some of the career options and work settings for forensic psychiatrists?
Continue to: Dr. Appelbaum...
Dr. Appelbaum: One of the advantages of forensic psychiatry is the plethora of work settings available. People headed to private practice can often combine clinical practice with forensic work, a necessity when starting one’s career and waiting to establish steady referral pipelines. Psychiatrists with forensic training are in demand in correctional facilities (which often pay higher salaries than comparable jobs in psychiatric facilities), forensic hospitals, and court clinics. Opportunities for academic involvement include directing fellowship programs, teaching residents, and conducting research. With regard to research, although funding is harder to come by than, for example, for studies of the biology of major psychiatric syndromes, determined psychiatrists can often find ways of framing questions related to forensic issues so that they appeal to funders’ priorities. As one gains experience, opportunities for consultation for law enforcement agencies, intelligence agencies, and federal and state mental health agencies may be available. It is rare for a forensic psychiatrist to do just one of these things; most forensic psychiatrists engage in a mix of types of work, including general clinical work. The possibilities are manifold.
Dr. Ahmed: What are some of the challenges in working in this field?
Dr. Appelbaum: I talked already about some of the ethical challenges in forensic psychiatry. In addition, as a subspecialty that applies psychiatric knowledge to legal questions, forensic psychiatry requires its practitioners to stay up-to-date with both advances in psychiatry and changes in the law, not to mention variations across jurisdictions. This is not an area of specialization in which one can pay attention during fellowship and then coast through a career. In my view, it’s also critical for a good forensic psychiatrist to be an excellent clinician; forensic cases frequently offer diagnostic challenges that require the highest level of clinical skills to address. Finally, for people early in their careers, it can take a few years before they are well-enough known to get a steady flow of private forensic cases. So having a plan B during that career phase will be essential.
Dr. Ahmed: Where do you see forensic psychiatry going?
Dr. Appelbaum: Forensic evaluations will need to incorporate new assessment techniques and new knowledge—although not before they have been demonstrated to be valid and reliable. I can foresee increased use of specialized neuroimaging assessments, genomic and other “omic” testing, and measurement of other neurophysiologic parameters. As we know more about the etiology of psychiatric disorders, that will impact everything from evaluations of causation in emotional harms cases to conclusions about which divorcing parent may be better able to handle primary custody of a child. I think there will be exciting opportunities in the coming decades to integrate growing scientific knowledge about psychiatric illnesses into forensic psychiatry.
Continue to: Dr. Ahmed...
Dr. Ahmed: What advice do you have for those contemplating a career in forensic psychiatry?
Dr. Appelbaum: Residents thinking about undertaking training in forensic psychiatry should come to one of the annual meetings of the American Academy of Psychiatry and the Law, the major professional organization of forensic psychiatrists, which takes place every October
Prenatal exposure to illegal substances: Exploring alternatives to fetal assault bills
Near completion of my rounds at a residential substance abuse treatment center, my last patient was a 32-year-old mother. She reported she was there because her newborn had tested positive for cocaine. She stated, “I want to do better. I thought this pregnancy would change things, but it was so hard to stop.” Her admission made me reflect on a proposed bill in my state of Tennessee called the Fetal Assault Bill, which if put into law would affect women such as my patient and her newborn child.
The Tennessee Fetal Assault Bill was originally enacted in 2014, expired in 2016, and failed to pass in 2017. The bill was reintroduced for consideration in February 2019. If enacted, it would subject a woman to prosecution if her illegal use of a substance while pregnant causes her child to be born addicted to or harmed by that drug. However, the mother is protected from prosecution if she “enrolled in an addiction recovery program before the child is born, remained in the program after delivery, and successfully completed the program, regardless of whether the child was born addicted to or harmed by the narcotic drug.”1 This bill is based on the premise that the unborn fetus has the same rights as a born child, and that the threat of incarceration will deter pregnant women from using illegal substances while pregnant.
Pregnant women may enroll in a drug treatment program prior to delivery to avoid prosecution; however, there is a paucity of addiction treatment centers available to pregnant women. Moreover, there is limited access in areas where babies are more likely to be born affected by the use of illegal substances. Few provisions have been made to address the additional barriers to treatment these women face, such as a lack of insurance or underinsurance for rehabilitation treatment, lack of transportation, and limited finances. Additional barriers include limited social supports, the need for childcare arrangements for existing children, and social stigma.
A 2017 report by Amnesty International regarding the original enactment of the Tennessee Fetal Assault Bill in 2014 noted some mothers who used illegal substances were afraid of prosecution.2 This fear caused some to delay prenatal care or evade social services in order to prevent being reported. According to Amnesty International, laws such as the one proposed in Tennessee often show disparities in how they are implemented. Research shows that women of lower socioeconomic status and minorities tend to receive more frequent drug testing and harsher punishments.3
There are benefits to dedicating more resources to addiction treatment and other social services for pregnant women who use illegal substances. Reports show that mothers are motivated to stay abstinent in treatment centers where they are housed with their children. This model of treatment is more cost-effective than incarceration, which includes legal costs, prison costs, and foster care bills. Moreover, a possible felony charge may hinder a woman’s job opportunities and further compound her problems and those of her infant.
In the light of these benefits, instead of re-enacting the 2014 law, which did not yield any conclusive benefits for newborns or mothers who used illegal substances, alternatives should be attempted. Early identification of and interventions for women who are at risk for substance use while pregnant should be implemented. Practical, accessible support services will encourage sobriety, prevent fetal exposure to illegal substances, and improve child health outcomes. Research shows that substance abuse treatment during pregnancy reduces the risk of harm before birth and improves the quality of parental care after birth.4 Legislators and clinicians should emphasize improving access to treatment, expanding integrative addiction treatment centers, and encouraging self-reporting early in pregnancy. This goal cannot be achieved with an emphasis on incarcerating mothers.
1. House Bill 1168. 111th Tennessee General Assembly (Tenn 2019). http://www.capitol.tn.gov/Bills/111/Bill/HB1168.pdf. Accessed August 8, 2019.
2. Amnesty International. Criminalizing pregnancy: policing pregnant women who use drugs in the USA. https://www.amnesty.org/download/Documents/AMR5162032017ENGLISH.pdf. Published May 23, 2017. Accessed August 8, 2019.
3. Paltrow LM, Flavin J. Arrests of and forced interventions on pregnant women in the United States, 1973-2005: implications for women’s legal status and public health. J Health Polit Policy Law. 2013;38(2):299-343.
4. Ashley OS, Marsden ME, Brady TM. Effectiveness of substance abuse treatment programming for women: a review. Am J Drug Alcohol Abuse. 2003;29(1):19-53.
Near completion of my rounds at a residential substance abuse treatment center, my last patient was a 32-year-old mother. She reported she was there because her newborn had tested positive for cocaine. She stated, “I want to do better. I thought this pregnancy would change things, but it was so hard to stop.” Her admission made me reflect on a proposed bill in my state of Tennessee called the Fetal Assault Bill, which if put into law would affect women such as my patient and her newborn child.
The Tennessee Fetal Assault Bill was originally enacted in 2014, expired in 2016, and failed to pass in 2017. The bill was reintroduced for consideration in February 2019. If enacted, it would subject a woman to prosecution if her illegal use of a substance while pregnant causes her child to be born addicted to or harmed by that drug. However, the mother is protected from prosecution if she “enrolled in an addiction recovery program before the child is born, remained in the program after delivery, and successfully completed the program, regardless of whether the child was born addicted to or harmed by the narcotic drug.”1 This bill is based on the premise that the unborn fetus has the same rights as a born child, and that the threat of incarceration will deter pregnant women from using illegal substances while pregnant.
Pregnant women may enroll in a drug treatment program prior to delivery to avoid prosecution; however, there is a paucity of addiction treatment centers available to pregnant women. Moreover, there is limited access in areas where babies are more likely to be born affected by the use of illegal substances. Few provisions have been made to address the additional barriers to treatment these women face, such as a lack of insurance or underinsurance for rehabilitation treatment, lack of transportation, and limited finances. Additional barriers include limited social supports, the need for childcare arrangements for existing children, and social stigma.
A 2017 report by Amnesty International regarding the original enactment of the Tennessee Fetal Assault Bill in 2014 noted some mothers who used illegal substances were afraid of prosecution.2 This fear caused some to delay prenatal care or evade social services in order to prevent being reported. According to Amnesty International, laws such as the one proposed in Tennessee often show disparities in how they are implemented. Research shows that women of lower socioeconomic status and minorities tend to receive more frequent drug testing and harsher punishments.3
There are benefits to dedicating more resources to addiction treatment and other social services for pregnant women who use illegal substances. Reports show that mothers are motivated to stay abstinent in treatment centers where they are housed with their children. This model of treatment is more cost-effective than incarceration, which includes legal costs, prison costs, and foster care bills. Moreover, a possible felony charge may hinder a woman’s job opportunities and further compound her problems and those of her infant.
In the light of these benefits, instead of re-enacting the 2014 law, which did not yield any conclusive benefits for newborns or mothers who used illegal substances, alternatives should be attempted. Early identification of and interventions for women who are at risk for substance use while pregnant should be implemented. Practical, accessible support services will encourage sobriety, prevent fetal exposure to illegal substances, and improve child health outcomes. Research shows that substance abuse treatment during pregnancy reduces the risk of harm before birth and improves the quality of parental care after birth.4 Legislators and clinicians should emphasize improving access to treatment, expanding integrative addiction treatment centers, and encouraging self-reporting early in pregnancy. This goal cannot be achieved with an emphasis on incarcerating mothers.
Near completion of my rounds at a residential substance abuse treatment center, my last patient was a 32-year-old mother. She reported she was there because her newborn had tested positive for cocaine. She stated, “I want to do better. I thought this pregnancy would change things, but it was so hard to stop.” Her admission made me reflect on a proposed bill in my state of Tennessee called the Fetal Assault Bill, which if put into law would affect women such as my patient and her newborn child.
The Tennessee Fetal Assault Bill was originally enacted in 2014, expired in 2016, and failed to pass in 2017. The bill was reintroduced for consideration in February 2019. If enacted, it would subject a woman to prosecution if her illegal use of a substance while pregnant causes her child to be born addicted to or harmed by that drug. However, the mother is protected from prosecution if she “enrolled in an addiction recovery program before the child is born, remained in the program after delivery, and successfully completed the program, regardless of whether the child was born addicted to or harmed by the narcotic drug.”1 This bill is based on the premise that the unborn fetus has the same rights as a born child, and that the threat of incarceration will deter pregnant women from using illegal substances while pregnant.
Pregnant women may enroll in a drug treatment program prior to delivery to avoid prosecution; however, there is a paucity of addiction treatment centers available to pregnant women. Moreover, there is limited access in areas where babies are more likely to be born affected by the use of illegal substances. Few provisions have been made to address the additional barriers to treatment these women face, such as a lack of insurance or underinsurance for rehabilitation treatment, lack of transportation, and limited finances. Additional barriers include limited social supports, the need for childcare arrangements for existing children, and social stigma.
A 2017 report by Amnesty International regarding the original enactment of the Tennessee Fetal Assault Bill in 2014 noted some mothers who used illegal substances were afraid of prosecution.2 This fear caused some to delay prenatal care or evade social services in order to prevent being reported. According to Amnesty International, laws such as the one proposed in Tennessee often show disparities in how they are implemented. Research shows that women of lower socioeconomic status and minorities tend to receive more frequent drug testing and harsher punishments.3
There are benefits to dedicating more resources to addiction treatment and other social services for pregnant women who use illegal substances. Reports show that mothers are motivated to stay abstinent in treatment centers where they are housed with their children. This model of treatment is more cost-effective than incarceration, which includes legal costs, prison costs, and foster care bills. Moreover, a possible felony charge may hinder a woman’s job opportunities and further compound her problems and those of her infant.
In the light of these benefits, instead of re-enacting the 2014 law, which did not yield any conclusive benefits for newborns or mothers who used illegal substances, alternatives should be attempted. Early identification of and interventions for women who are at risk for substance use while pregnant should be implemented. Practical, accessible support services will encourage sobriety, prevent fetal exposure to illegal substances, and improve child health outcomes. Research shows that substance abuse treatment during pregnancy reduces the risk of harm before birth and improves the quality of parental care after birth.4 Legislators and clinicians should emphasize improving access to treatment, expanding integrative addiction treatment centers, and encouraging self-reporting early in pregnancy. This goal cannot be achieved with an emphasis on incarcerating mothers.
1. House Bill 1168. 111th Tennessee General Assembly (Tenn 2019). http://www.capitol.tn.gov/Bills/111/Bill/HB1168.pdf. Accessed August 8, 2019.
2. Amnesty International. Criminalizing pregnancy: policing pregnant women who use drugs in the USA. https://www.amnesty.org/download/Documents/AMR5162032017ENGLISH.pdf. Published May 23, 2017. Accessed August 8, 2019.
3. Paltrow LM, Flavin J. Arrests of and forced interventions on pregnant women in the United States, 1973-2005: implications for women’s legal status and public health. J Health Polit Policy Law. 2013;38(2):299-343.
4. Ashley OS, Marsden ME, Brady TM. Effectiveness of substance abuse treatment programming for women: a review. Am J Drug Alcohol Abuse. 2003;29(1):19-53.
1. House Bill 1168. 111th Tennessee General Assembly (Tenn 2019). http://www.capitol.tn.gov/Bills/111/Bill/HB1168.pdf. Accessed August 8, 2019.
2. Amnesty International. Criminalizing pregnancy: policing pregnant women who use drugs in the USA. https://www.amnesty.org/download/Documents/AMR5162032017ENGLISH.pdf. Published May 23, 2017. Accessed August 8, 2019.
3. Paltrow LM, Flavin J. Arrests of and forced interventions on pregnant women in the United States, 1973-2005: implications for women’s legal status and public health. J Health Polit Policy Law. 2013;38(2):299-343.
4. Ashley OS, Marsden ME, Brady TM. Effectiveness of substance abuse treatment programming for women: a review. Am J Drug Alcohol Abuse. 2003;29(1):19-53.