User login
New SHM research on EMRs calls for ‘more caring, less clicking’
White paper offers concrete recommendations
One of the most significant shifts in hospital practice over recent decades has been the widespread adoption of electronic medical records as a replacement for conventional paper records.
While EMRs show a lot of promise – having the potential to centralize and simplify clinician notes, make information more accessible and reduce paper waste – there is strong evidence that they are not working as well as they could.
Some research suggests that these systems may decrease the working efficiency of clinicians. Now, major health care institutions are looking to understand why these systems are not working — as well as how they may be improved.
A recent white paper from the Society of Hospital Medicine’s Healthcare Information Technology Special Interest Group – titled “More Caring, Less Clicking” – reviews the current shortcomings of EMRs from a hospitalist perspective and provides recommendations for how these systems can be made more workable and efficient.
The current state of EMRs
“Numerous previous papers – including SHM’s 2017 white paper ‘Hospitalist Perspectives on Electronic Medical Records’ – have linked EMRs to decreased provider satisfaction and increased burnout related to multiple issues, including an increase in ‘screen time’ as opposed to patient ‘face-to-face’ time, and limitations in usability and interoperability,” said Rupesh Prasad, MD, SFHM, medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. “Studies have shown that most of a provider’s time spent is in areas like clinical documentation, entry of orders, and accessing patient information.”
The 2017 SHM white paper referenced by Dr. Prasad reported that 74% of hospitalists surveyed were dissatisfied with their EMR. A full one-quarter of surveyed physicians went so far as saying they would prefer switching to paper record keeping.
Other research has also found a possible link between EMRs and physician burnout and dissatisfaction. It is also not uncommon for hospitalists to spend up to 25% of their time at work using their EMR – time that should, ideally, be spent with patients.
The 2017 paper also showed that clinician notes in the United States are four times longer, on average, than notes in other countries. There are a few reasons for this – including technology design and billing requirements encouraging longer notes. Whatever the cause, however, longer notes linked to physician burnout may be partially responsible for the large amounts of time physicians spend looking at EMRs.
While EMRs may hold significant potential for hospitalists, as they are designed currently, they are simply not delivering the value many expected. The new white paper from the Healthcare Information Technology Special Interest Group outlines practical changes that could be made to EMRs to improve their use in hospitals.
The paper breaks down current issues with EMRs into five broad categories – documentation, clinical decision support, order entry, communication, and data review – to discuss how EMRs are currently failing in these areas as well as how they might be improved.
Improving EMR documentation
One of the most significant hurdles clinicians currently face lies in how EMRs currently store and display documentation. Combined with physician note-taking habits, this makes these systems much less usable than they could be. Longer notes, when displayed in current EMR UIs, mostly lead to clutter, making them harder to navigate and difficult to scan quickly for important information.
The authors identify a few different ways that future EMRs may be able to help with this problem.
EMR documentation tools will likely need to be redesigned to optimize documentation entry, standardize note formatting, and improve readability. Many electronic notes contain vestigial formatting and data left over from the design of paper notes. As a result, many of these electronic notes include information that is stored elsewhere and does not need to be explicitly included in every note. Cutting down on repetitive information storage will make important information more visible and help make patient notes easier to scan.
The paper also recommends a few other features that would make documentation more readable – like allowing clinicians to write documentation in SOAP format (subjective, objective, assessment, and plan), to facilitate critical thinking during the note-taking process, and having the EMR display that documentation in APSO format (assessment, plan, subjective, objective).
Doctors have long called for APSO or another note-taking format to replace SOAP in EMRs. Designing EMRs to rearrange SOAP notes to APSO could be a compromise that improves note readability while not requiring that clinicians learn new note-taking strategies.
The paper’s authors also recommended more extensive clinician training on writing notes. While clinicians are often taught how to write certain notes – like progress notes, histories, and physical and discharge summaries – more specific guidance is not always provided. Better training provided by institutions could help improve the quality and readability of clinician notes.
These changes, however, may not be as beneficial as possible without better institutional support for clinicians. Implementing some of the biggest changes recommended by the SHM will require some level of standardization across platforms and institution commitment to training clinicians on best use practices for EMRs. Improved responsiveness to clinician needs will require a coordinated effort with backing from both administrative and governance groups.
Expanding EMR usability
“Our white paper presents evidence-based recommendations that can be implemented at the ground level in collaboration with other stakeholders, including IT, informatics, and administration, to help improve on the current state,” Dr. Prasad said.
“We believe that hospitalists as key stakeholders in health care, have both the responsibility and are uniquely positioned to directly impact EMR functionality,” he noted. “For example, hospitalists can participate in designing appropriate, actionable alerts that would help with patient safety while also improving provider efficiency. Simple steps like limiting hard stops in order entry to would help speed up the process, and free up time for direct patient care. Availability of tools like secure text messaging would help with effective patient care team communication to improve safety and care delivery.”
EMRs often lack features like voice control and speech-to-text transcription, along with other basic accessibility features like compatibility with screen readers. Implementing these features could improve the efficiency of clinicians’ note-taking while also providing wider software usability.
EMRs are not typically designed to work with mobile devices, meaning clinicians cannot enter notes or order medications until they’ve returned to their desk or workstation.
This lack of functionality creates issues in several ways. When clinicians are unable to enter notes on the move, they will need to either keep mental notes or quickly jot down paper notes. This can effectively double the amount of note-taking that clinicians must do or introduce greater room for error. In cases where progress notes are taken throughout the day, this also means the EMR’s documentation timeline may not be accurate or usable.
Requiring clinicians to return to workstations before entering order information can also increase the risk of medication errors, which remains high despite hopes that EMRs could reduce error rates.
Adding support for cross-device and mobile EMR use could help improve the efficiency of note-taking and help cut down on error. Implementing mobile access could have a few different benefits for clinicians – like improving note-taking efficiency in hospitals, where doctors often see patients far away from their workstations.
EMRs also often lack support for certain hardware, like mobile stations and widescreen monitors, which can improve a clinician’s ability to document in real-time and are a better fit in certain work flows.
The SHM paper also recommends a few other tweaks to usability – like reducing the amount of password entry and reentry – that could make these systems easier to use and more efficient.
New features – like the use of natural language processing technology to analyze and organize information contained in clinicians’ notes – could provide further benefits and take full advantage of the advanced technologies that EMRs can integrate.
Dr. Prasad noted, however, that some of these upgrades – especially EMR compatibility with mobile devices – will require some institutional support. Bring-your-own-device policies or system-provided mobile devices will be necessary if institutions want their clinicians to be able to take advantage of mobile EMR access.
These policies will also likely require some kind of mobile device management solution to manage the security of sensitive patient data as it is accessed from personal devices. This may increase the level of necessary institutional buy-in for this support to work.
Designing EMRs with clinician needs in mind
Dr. Prasad said he and his coauthors recommend that EMR developers base more of their design on the needs of clinicians.
Currently, EMR interfaces can make important data unavailable, depending on what a clinician is trying to do. As a result, clinicians often need to rely on mental recall of important information as they navigate EMR systems.
These interfaces also typically do not support any level of user customization or process-specific interfaces, meaning every clinician is working with the same interface regardless of the tasks they need to perform or the information they need access to. Allowing for customization or implementing new process- or disease-specific interfaces could help avoid some of the problems caused by one-size-fits-all interfaces, which are not necessarily compatible with every clinician work flow.
EMR interfaces should also be designed, wherever possible, with familiar or standardized formats and the use of color coding and other techniques that can make interfaces easier to navigate quickly. Right now, many EMR systems utilize inconsistent layout design that can be cluttered with irrelevant information, slowing down interface navigation and sometimes requiring backtracking from clinicians.
Ideally, this will improve the speed of information gathering and data review, reducing the amount of time clinicians need to spend working with their EMR.
The white paper also recommends that EMR designers improve alert systems so that they are more actionable and interrupt clinicians less often – and that, when they do, they ensure that clinicians can respond to them. Designers should also reduce hard-stops or in-line alerts that halt clinicians’ work flows and require immediate responses where possible.
Increased EMR support for clinical decision support systems is one of the biggest health care trends expected to be seen throughout this decade. However, many clinicians are disappointed with the lack of flexibility and optimization of the current alerts that CDS provides. Updating and improving these knowledge-based systems will likely become essential for delivering better alerts and improving decision-making and efficiency.
Overall, EMR design should be informed by the needs of the people these products are designed to support, Dr. Prasad said. The people that work with EMRs – especially frontline staff like providers, nurses, and pharmacists that regularly interact with EMRs to provide care – should be involved early on in the EMR design process. Right now, their needs are not reflected in current EMR design. EMR companies, by working with these hospital staff members, could help improve ease of use and, ideally, prevent some of the errors associated with the current implementation of these systems.
“System designers should be able to avoid some of the most common problems of EMRs – and predict potential problems – by consistently soliciting and integrating clinician feedback during the design process and over the lifespan of a product,” Dr. Prasad said.
How EMRs can be improved
Over the past few years, EMRs have become quickly adopted by health care professionals and institutions. However, despite hopes that EMRs could significantly improve record keeping and note-taking, these systems continue to pose serious challenges for the clinicians who use them. Evidence from recent research suggests that these systems are inefficient and may contribute to physician burnout.
As a result, organizations like SHM are looking for ways that these systems can be improved.
“The growth of health IT has led to availability of large amounts of data and opportunities for applications in [artificial intelligence and machine learning,” Dr. Prasad noted. “While this has opened many avenues to help positively impact patient care and outcomes, it also poses multiple challenges like validation, customization, and governance. Hospitalists can partner with other health professions and IT leaders to work toward the common goal of improving the health of the population while also providing a positive experience to the end user.”
Another problem with current EMRs is their lack of flexibility. These systems are often not compatible with mobile devices and certain types of hardware and may be difficult or impossible to customize. They also frequently require unnecessary information during the note-taking process that results in cluttered and difficult-to-scan documentation. Improving EMR flexibility – and inviting clinicians to consult during the design process – could solve many of these problems.
New technological developments may also soon help developers improve their EMRs. In the future, as technology like natural language processing becomes more advanced and more commonly used, they may be able to make EMRs even more efficient and user friendly.
White paper offers concrete recommendations
White paper offers concrete recommendations
One of the most significant shifts in hospital practice over recent decades has been the widespread adoption of electronic medical records as a replacement for conventional paper records.
While EMRs show a lot of promise – having the potential to centralize and simplify clinician notes, make information more accessible and reduce paper waste – there is strong evidence that they are not working as well as they could.
Some research suggests that these systems may decrease the working efficiency of clinicians. Now, major health care institutions are looking to understand why these systems are not working — as well as how they may be improved.
A recent white paper from the Society of Hospital Medicine’s Healthcare Information Technology Special Interest Group – titled “More Caring, Less Clicking” – reviews the current shortcomings of EMRs from a hospitalist perspective and provides recommendations for how these systems can be made more workable and efficient.
The current state of EMRs
“Numerous previous papers – including SHM’s 2017 white paper ‘Hospitalist Perspectives on Electronic Medical Records’ – have linked EMRs to decreased provider satisfaction and increased burnout related to multiple issues, including an increase in ‘screen time’ as opposed to patient ‘face-to-face’ time, and limitations in usability and interoperability,” said Rupesh Prasad, MD, SFHM, medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. “Studies have shown that most of a provider’s time spent is in areas like clinical documentation, entry of orders, and accessing patient information.”
The 2017 SHM white paper referenced by Dr. Prasad reported that 74% of hospitalists surveyed were dissatisfied with their EMR. A full one-quarter of surveyed physicians went so far as saying they would prefer switching to paper record keeping.
Other research has also found a possible link between EMRs and physician burnout and dissatisfaction. It is also not uncommon for hospitalists to spend up to 25% of their time at work using their EMR – time that should, ideally, be spent with patients.
The 2017 paper also showed that clinician notes in the United States are four times longer, on average, than notes in other countries. There are a few reasons for this – including technology design and billing requirements encouraging longer notes. Whatever the cause, however, longer notes linked to physician burnout may be partially responsible for the large amounts of time physicians spend looking at EMRs.
While EMRs may hold significant potential for hospitalists, as they are designed currently, they are simply not delivering the value many expected. The new white paper from the Healthcare Information Technology Special Interest Group outlines practical changes that could be made to EMRs to improve their use in hospitals.
The paper breaks down current issues with EMRs into five broad categories – documentation, clinical decision support, order entry, communication, and data review – to discuss how EMRs are currently failing in these areas as well as how they might be improved.
Improving EMR documentation
One of the most significant hurdles clinicians currently face lies in how EMRs currently store and display documentation. Combined with physician note-taking habits, this makes these systems much less usable than they could be. Longer notes, when displayed in current EMR UIs, mostly lead to clutter, making them harder to navigate and difficult to scan quickly for important information.
The authors identify a few different ways that future EMRs may be able to help with this problem.
EMR documentation tools will likely need to be redesigned to optimize documentation entry, standardize note formatting, and improve readability. Many electronic notes contain vestigial formatting and data left over from the design of paper notes. As a result, many of these electronic notes include information that is stored elsewhere and does not need to be explicitly included in every note. Cutting down on repetitive information storage will make important information more visible and help make patient notes easier to scan.
The paper also recommends a few other features that would make documentation more readable – like allowing clinicians to write documentation in SOAP format (subjective, objective, assessment, and plan), to facilitate critical thinking during the note-taking process, and having the EMR display that documentation in APSO format (assessment, plan, subjective, objective).
Doctors have long called for APSO or another note-taking format to replace SOAP in EMRs. Designing EMRs to rearrange SOAP notes to APSO could be a compromise that improves note readability while not requiring that clinicians learn new note-taking strategies.
The paper’s authors also recommended more extensive clinician training on writing notes. While clinicians are often taught how to write certain notes – like progress notes, histories, and physical and discharge summaries – more specific guidance is not always provided. Better training provided by institutions could help improve the quality and readability of clinician notes.
These changes, however, may not be as beneficial as possible without better institutional support for clinicians. Implementing some of the biggest changes recommended by the SHM will require some level of standardization across platforms and institution commitment to training clinicians on best use practices for EMRs. Improved responsiveness to clinician needs will require a coordinated effort with backing from both administrative and governance groups.
Expanding EMR usability
“Our white paper presents evidence-based recommendations that can be implemented at the ground level in collaboration with other stakeholders, including IT, informatics, and administration, to help improve on the current state,” Dr. Prasad said.
“We believe that hospitalists as key stakeholders in health care, have both the responsibility and are uniquely positioned to directly impact EMR functionality,” he noted. “For example, hospitalists can participate in designing appropriate, actionable alerts that would help with patient safety while also improving provider efficiency. Simple steps like limiting hard stops in order entry to would help speed up the process, and free up time for direct patient care. Availability of tools like secure text messaging would help with effective patient care team communication to improve safety and care delivery.”
EMRs often lack features like voice control and speech-to-text transcription, along with other basic accessibility features like compatibility with screen readers. Implementing these features could improve the efficiency of clinicians’ note-taking while also providing wider software usability.
EMRs are not typically designed to work with mobile devices, meaning clinicians cannot enter notes or order medications until they’ve returned to their desk or workstation.
This lack of functionality creates issues in several ways. When clinicians are unable to enter notes on the move, they will need to either keep mental notes or quickly jot down paper notes. This can effectively double the amount of note-taking that clinicians must do or introduce greater room for error. In cases where progress notes are taken throughout the day, this also means the EMR’s documentation timeline may not be accurate or usable.
Requiring clinicians to return to workstations before entering order information can also increase the risk of medication errors, which remains high despite hopes that EMRs could reduce error rates.
Adding support for cross-device and mobile EMR use could help improve the efficiency of note-taking and help cut down on error. Implementing mobile access could have a few different benefits for clinicians – like improving note-taking efficiency in hospitals, where doctors often see patients far away from their workstations.
EMRs also often lack support for certain hardware, like mobile stations and widescreen monitors, which can improve a clinician’s ability to document in real-time and are a better fit in certain work flows.
The SHM paper also recommends a few other tweaks to usability – like reducing the amount of password entry and reentry – that could make these systems easier to use and more efficient.
New features – like the use of natural language processing technology to analyze and organize information contained in clinicians’ notes – could provide further benefits and take full advantage of the advanced technologies that EMRs can integrate.
Dr. Prasad noted, however, that some of these upgrades – especially EMR compatibility with mobile devices – will require some institutional support. Bring-your-own-device policies or system-provided mobile devices will be necessary if institutions want their clinicians to be able to take advantage of mobile EMR access.
These policies will also likely require some kind of mobile device management solution to manage the security of sensitive patient data as it is accessed from personal devices. This may increase the level of necessary institutional buy-in for this support to work.
Designing EMRs with clinician needs in mind
Dr. Prasad said he and his coauthors recommend that EMR developers base more of their design on the needs of clinicians.
Currently, EMR interfaces can make important data unavailable, depending on what a clinician is trying to do. As a result, clinicians often need to rely on mental recall of important information as they navigate EMR systems.
These interfaces also typically do not support any level of user customization or process-specific interfaces, meaning every clinician is working with the same interface regardless of the tasks they need to perform or the information they need access to. Allowing for customization or implementing new process- or disease-specific interfaces could help avoid some of the problems caused by one-size-fits-all interfaces, which are not necessarily compatible with every clinician work flow.
EMR interfaces should also be designed, wherever possible, with familiar or standardized formats and the use of color coding and other techniques that can make interfaces easier to navigate quickly. Right now, many EMR systems utilize inconsistent layout design that can be cluttered with irrelevant information, slowing down interface navigation and sometimes requiring backtracking from clinicians.
Ideally, this will improve the speed of information gathering and data review, reducing the amount of time clinicians need to spend working with their EMR.
The white paper also recommends that EMR designers improve alert systems so that they are more actionable and interrupt clinicians less often – and that, when they do, they ensure that clinicians can respond to them. Designers should also reduce hard-stops or in-line alerts that halt clinicians’ work flows and require immediate responses where possible.
Increased EMR support for clinical decision support systems is one of the biggest health care trends expected to be seen throughout this decade. However, many clinicians are disappointed with the lack of flexibility and optimization of the current alerts that CDS provides. Updating and improving these knowledge-based systems will likely become essential for delivering better alerts and improving decision-making and efficiency.
Overall, EMR design should be informed by the needs of the people these products are designed to support, Dr. Prasad said. The people that work with EMRs – especially frontline staff like providers, nurses, and pharmacists that regularly interact with EMRs to provide care – should be involved early on in the EMR design process. Right now, their needs are not reflected in current EMR design. EMR companies, by working with these hospital staff members, could help improve ease of use and, ideally, prevent some of the errors associated with the current implementation of these systems.
“System designers should be able to avoid some of the most common problems of EMRs – and predict potential problems – by consistently soliciting and integrating clinician feedback during the design process and over the lifespan of a product,” Dr. Prasad said.
How EMRs can be improved
Over the past few years, EMRs have become quickly adopted by health care professionals and institutions. However, despite hopes that EMRs could significantly improve record keeping and note-taking, these systems continue to pose serious challenges for the clinicians who use them. Evidence from recent research suggests that these systems are inefficient and may contribute to physician burnout.
As a result, organizations like SHM are looking for ways that these systems can be improved.
“The growth of health IT has led to availability of large amounts of data and opportunities for applications in [artificial intelligence and machine learning,” Dr. Prasad noted. “While this has opened many avenues to help positively impact patient care and outcomes, it also poses multiple challenges like validation, customization, and governance. Hospitalists can partner with other health professions and IT leaders to work toward the common goal of improving the health of the population while also providing a positive experience to the end user.”
Another problem with current EMRs is their lack of flexibility. These systems are often not compatible with mobile devices and certain types of hardware and may be difficult or impossible to customize. They also frequently require unnecessary information during the note-taking process that results in cluttered and difficult-to-scan documentation. Improving EMR flexibility – and inviting clinicians to consult during the design process – could solve many of these problems.
New technological developments may also soon help developers improve their EMRs. In the future, as technology like natural language processing becomes more advanced and more commonly used, they may be able to make EMRs even more efficient and user friendly.
One of the most significant shifts in hospital practice over recent decades has been the widespread adoption of electronic medical records as a replacement for conventional paper records.
While EMRs show a lot of promise – having the potential to centralize and simplify clinician notes, make information more accessible and reduce paper waste – there is strong evidence that they are not working as well as they could.
Some research suggests that these systems may decrease the working efficiency of clinicians. Now, major health care institutions are looking to understand why these systems are not working — as well as how they may be improved.
A recent white paper from the Society of Hospital Medicine’s Healthcare Information Technology Special Interest Group – titled “More Caring, Less Clicking” – reviews the current shortcomings of EMRs from a hospitalist perspective and provides recommendations for how these systems can be made more workable and efficient.
The current state of EMRs
“Numerous previous papers – including SHM’s 2017 white paper ‘Hospitalist Perspectives on Electronic Medical Records’ – have linked EMRs to decreased provider satisfaction and increased burnout related to multiple issues, including an increase in ‘screen time’ as opposed to patient ‘face-to-face’ time, and limitations in usability and interoperability,” said Rupesh Prasad, MD, SFHM, medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. “Studies have shown that most of a provider’s time spent is in areas like clinical documentation, entry of orders, and accessing patient information.”
The 2017 SHM white paper referenced by Dr. Prasad reported that 74% of hospitalists surveyed were dissatisfied with their EMR. A full one-quarter of surveyed physicians went so far as saying they would prefer switching to paper record keeping.
Other research has also found a possible link between EMRs and physician burnout and dissatisfaction. It is also not uncommon for hospitalists to spend up to 25% of their time at work using their EMR – time that should, ideally, be spent with patients.
The 2017 paper also showed that clinician notes in the United States are four times longer, on average, than notes in other countries. There are a few reasons for this – including technology design and billing requirements encouraging longer notes. Whatever the cause, however, longer notes linked to physician burnout may be partially responsible for the large amounts of time physicians spend looking at EMRs.
While EMRs may hold significant potential for hospitalists, as they are designed currently, they are simply not delivering the value many expected. The new white paper from the Healthcare Information Technology Special Interest Group outlines practical changes that could be made to EMRs to improve their use in hospitals.
The paper breaks down current issues with EMRs into five broad categories – documentation, clinical decision support, order entry, communication, and data review – to discuss how EMRs are currently failing in these areas as well as how they might be improved.
Improving EMR documentation
One of the most significant hurdles clinicians currently face lies in how EMRs currently store and display documentation. Combined with physician note-taking habits, this makes these systems much less usable than they could be. Longer notes, when displayed in current EMR UIs, mostly lead to clutter, making them harder to navigate and difficult to scan quickly for important information.
The authors identify a few different ways that future EMRs may be able to help with this problem.
EMR documentation tools will likely need to be redesigned to optimize documentation entry, standardize note formatting, and improve readability. Many electronic notes contain vestigial formatting and data left over from the design of paper notes. As a result, many of these electronic notes include information that is stored elsewhere and does not need to be explicitly included in every note. Cutting down on repetitive information storage will make important information more visible and help make patient notes easier to scan.
The paper also recommends a few other features that would make documentation more readable – like allowing clinicians to write documentation in SOAP format (subjective, objective, assessment, and plan), to facilitate critical thinking during the note-taking process, and having the EMR display that documentation in APSO format (assessment, plan, subjective, objective).
Doctors have long called for APSO or another note-taking format to replace SOAP in EMRs. Designing EMRs to rearrange SOAP notes to APSO could be a compromise that improves note readability while not requiring that clinicians learn new note-taking strategies.
The paper’s authors also recommended more extensive clinician training on writing notes. While clinicians are often taught how to write certain notes – like progress notes, histories, and physical and discharge summaries – more specific guidance is not always provided. Better training provided by institutions could help improve the quality and readability of clinician notes.
These changes, however, may not be as beneficial as possible without better institutional support for clinicians. Implementing some of the biggest changes recommended by the SHM will require some level of standardization across platforms and institution commitment to training clinicians on best use practices for EMRs. Improved responsiveness to clinician needs will require a coordinated effort with backing from both administrative and governance groups.
Expanding EMR usability
“Our white paper presents evidence-based recommendations that can be implemented at the ground level in collaboration with other stakeholders, including IT, informatics, and administration, to help improve on the current state,” Dr. Prasad said.
“We believe that hospitalists as key stakeholders in health care, have both the responsibility and are uniquely positioned to directly impact EMR functionality,” he noted. “For example, hospitalists can participate in designing appropriate, actionable alerts that would help with patient safety while also improving provider efficiency. Simple steps like limiting hard stops in order entry to would help speed up the process, and free up time for direct patient care. Availability of tools like secure text messaging would help with effective patient care team communication to improve safety and care delivery.”
EMRs often lack features like voice control and speech-to-text transcription, along with other basic accessibility features like compatibility with screen readers. Implementing these features could improve the efficiency of clinicians’ note-taking while also providing wider software usability.
EMRs are not typically designed to work with mobile devices, meaning clinicians cannot enter notes or order medications until they’ve returned to their desk or workstation.
This lack of functionality creates issues in several ways. When clinicians are unable to enter notes on the move, they will need to either keep mental notes or quickly jot down paper notes. This can effectively double the amount of note-taking that clinicians must do or introduce greater room for error. In cases where progress notes are taken throughout the day, this also means the EMR’s documentation timeline may not be accurate or usable.
Requiring clinicians to return to workstations before entering order information can also increase the risk of medication errors, which remains high despite hopes that EMRs could reduce error rates.
Adding support for cross-device and mobile EMR use could help improve the efficiency of note-taking and help cut down on error. Implementing mobile access could have a few different benefits for clinicians – like improving note-taking efficiency in hospitals, where doctors often see patients far away from their workstations.
EMRs also often lack support for certain hardware, like mobile stations and widescreen monitors, which can improve a clinician’s ability to document in real-time and are a better fit in certain work flows.
The SHM paper also recommends a few other tweaks to usability – like reducing the amount of password entry and reentry – that could make these systems easier to use and more efficient.
New features – like the use of natural language processing technology to analyze and organize information contained in clinicians’ notes – could provide further benefits and take full advantage of the advanced technologies that EMRs can integrate.
Dr. Prasad noted, however, that some of these upgrades – especially EMR compatibility with mobile devices – will require some institutional support. Bring-your-own-device policies or system-provided mobile devices will be necessary if institutions want their clinicians to be able to take advantage of mobile EMR access.
These policies will also likely require some kind of mobile device management solution to manage the security of sensitive patient data as it is accessed from personal devices. This may increase the level of necessary institutional buy-in for this support to work.
Designing EMRs with clinician needs in mind
Dr. Prasad said he and his coauthors recommend that EMR developers base more of their design on the needs of clinicians.
Currently, EMR interfaces can make important data unavailable, depending on what a clinician is trying to do. As a result, clinicians often need to rely on mental recall of important information as they navigate EMR systems.
These interfaces also typically do not support any level of user customization or process-specific interfaces, meaning every clinician is working with the same interface regardless of the tasks they need to perform or the information they need access to. Allowing for customization or implementing new process- or disease-specific interfaces could help avoid some of the problems caused by one-size-fits-all interfaces, which are not necessarily compatible with every clinician work flow.
EMR interfaces should also be designed, wherever possible, with familiar or standardized formats and the use of color coding and other techniques that can make interfaces easier to navigate quickly. Right now, many EMR systems utilize inconsistent layout design that can be cluttered with irrelevant information, slowing down interface navigation and sometimes requiring backtracking from clinicians.
Ideally, this will improve the speed of information gathering and data review, reducing the amount of time clinicians need to spend working with their EMR.
The white paper also recommends that EMR designers improve alert systems so that they are more actionable and interrupt clinicians less often – and that, when they do, they ensure that clinicians can respond to them. Designers should also reduce hard-stops or in-line alerts that halt clinicians’ work flows and require immediate responses where possible.
Increased EMR support for clinical decision support systems is one of the biggest health care trends expected to be seen throughout this decade. However, many clinicians are disappointed with the lack of flexibility and optimization of the current alerts that CDS provides. Updating and improving these knowledge-based systems will likely become essential for delivering better alerts and improving decision-making and efficiency.
Overall, EMR design should be informed by the needs of the people these products are designed to support, Dr. Prasad said. The people that work with EMRs – especially frontline staff like providers, nurses, and pharmacists that regularly interact with EMRs to provide care – should be involved early on in the EMR design process. Right now, their needs are not reflected in current EMR design. EMR companies, by working with these hospital staff members, could help improve ease of use and, ideally, prevent some of the errors associated with the current implementation of these systems.
“System designers should be able to avoid some of the most common problems of EMRs – and predict potential problems – by consistently soliciting and integrating clinician feedback during the design process and over the lifespan of a product,” Dr. Prasad said.
How EMRs can be improved
Over the past few years, EMRs have become quickly adopted by health care professionals and institutions. However, despite hopes that EMRs could significantly improve record keeping and note-taking, these systems continue to pose serious challenges for the clinicians who use them. Evidence from recent research suggests that these systems are inefficient and may contribute to physician burnout.
As a result, organizations like SHM are looking for ways that these systems can be improved.
“The growth of health IT has led to availability of large amounts of data and opportunities for applications in [artificial intelligence and machine learning,” Dr. Prasad noted. “While this has opened many avenues to help positively impact patient care and outcomes, it also poses multiple challenges like validation, customization, and governance. Hospitalists can partner with other health professions and IT leaders to work toward the common goal of improving the health of the population while also providing a positive experience to the end user.”
Another problem with current EMRs is their lack of flexibility. These systems are often not compatible with mobile devices and certain types of hardware and may be difficult or impossible to customize. They also frequently require unnecessary information during the note-taking process that results in cluttered and difficult-to-scan documentation. Improving EMR flexibility – and inviting clinicians to consult during the design process – could solve many of these problems.
New technological developments may also soon help developers improve their EMRs. In the future, as technology like natural language processing becomes more advanced and more commonly used, they may be able to make EMRs even more efficient and user friendly.
Coming soon: The 2020 SoHM Report!
On behalf of SHM’s Practice Analysis Committee, I am excited to announce the scheduled September 2020 release of the 2020 State of Hospital Medicine Report (SoHM)!
For reasons all too familiar, this year’s SoHM survey process was unlike any in SHM’s history. We were still collecting survey responses from a few stragglers in early March when the entire world shut down almost overnight to flatten the curve of a deadly pandemic. Hospital medicine group (HMG) leaders were suddenly either up to their eyeballs trying to figure out how to safely care for huge influxes of COVID-19 patients that overwhelmed established systems of care or were trying to figure out how to staff in a low-volume environment with few COVID patients, a relative trickle of ED admissions, and virtually no surgical care. And everywhere, hospitals and their HMGs were quickly stressed in ways that would have been unimaginable just a couple of months earlier – financially, operationally, epidemiologically, and culturally.
SHM offices closed, with all staff working from home. And the talented people who would normally have been working diligently on the survey data were suddenly redirected to focus on COVID-related issues, including tracking government announcements that were changing daily and providing needed resources to SHM members. By the time they could raise their heads and begin thinking about survey data, we were months behind schedule.
I need to give a huge shout-out to our survey manager extraordinaire Josh Lapps, SHM’s Director of Policy and Practice Management, and his survey support team including Luke Heisinger and Kim Schonberger. Once they were able to turn their focus back to the SoHM, they worked like demons to catch up. And in addition to the work of preparing the SoHM for publication, they helped issue and analyze a follow-up survey to investigate how HMGs adjusted their staffing and operations in response to COVID! As I write this, we appear to be back on schedule for a September SoHM release date, with the COVID supplemental survey report to follow soon after. Thanks also to PAC committee members who, despite their own stresses, rose to the challenge of participating in calls and planning the supplemental survey.
Despite the pandemic, HMGs found survey participation valuable. When all was said and done, we had a respectable number of respondent groups: 502 this year vs. 569 in 2018. Although the number of respondent groups is down, the average group size has increased, so that an all-time high of 10,122 employed/contracted full-time equivalent (FTE) hospitalists (plus 484 locum tenens FTEs) are represented in the data set. The respondents continue to be very diverse, representing all practice models and every state – and even a couple of other countries. One notable change is a significant increase in pediatric HM group participation, thanks to a recruitment charge led by PAC member Sandra Gage, associate division chief of hospital medicine at Phoenix Children’s Hospital, and supported by the inclusion of several new pediatric HM-specific questions to better capture unique attributes of these hospital medicine practices.
We had more multisite respondents than ever, and the multisite respondents overwhelmingly used the new “retake” feature in the online version of the survey. I’m happy to report that we received consistent positive feedback about our new electronic survey platform, and thanks to its capabilities data analysis has been significantly automated, enhancing both efficiency and data reliability.
The survey content is more wide ranging than ever. In addition to the usual topics such as scope of services, staffing and scheduling, compensation models, evaluation and management code distribution, and HM group finances, the 2020 report will include the afore-referenced information about HM groups serving children, expanded information on nurse practitioner (NPs)/physician assistant (PA) roles, and data on diversity in HM physician leadership. The follow-up COVID survey will be published separately as a supplement, available only to purchasers of the SoHM report.
Multiple options for SoHM report purchase. All survey participants will receive access to the online version of the survey. Others may purchase the hard copy report, online access, or both. The report has a colorful, easy-to-read layout, and many of the tables have been streamlined to make them easier to read. I encourage you to sign up to preorder your copy of the SoHM Report today at www.hospitalmedicine.org/sohm; you’ll almost certainly discover a treasure trove of worthwhile information.
Use the report to assess how your practice compares to other practices, but always keep in mind that surveys don’t tell you what should be; they only tell you what currently is the case – or at least, what was during the survey period. New best practices not yet reflected in survey data are emerging all the time, and that is probably more true today in the new world affected by this pandemic than ever before. And while the ways others do things won’t always be right for your group’s unique situation and needs, it always helps to know how you compare with others. Whether you are partners or employees, you and your colleagues “own” the success of your hospital medicine practice and, armed with the best available data, are the best judges of what is right for you.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
On behalf of SHM’s Practice Analysis Committee, I am excited to announce the scheduled September 2020 release of the 2020 State of Hospital Medicine Report (SoHM)!
For reasons all too familiar, this year’s SoHM survey process was unlike any in SHM’s history. We were still collecting survey responses from a few stragglers in early March when the entire world shut down almost overnight to flatten the curve of a deadly pandemic. Hospital medicine group (HMG) leaders were suddenly either up to their eyeballs trying to figure out how to safely care for huge influxes of COVID-19 patients that overwhelmed established systems of care or were trying to figure out how to staff in a low-volume environment with few COVID patients, a relative trickle of ED admissions, and virtually no surgical care. And everywhere, hospitals and their HMGs were quickly stressed in ways that would have been unimaginable just a couple of months earlier – financially, operationally, epidemiologically, and culturally.
SHM offices closed, with all staff working from home. And the talented people who would normally have been working diligently on the survey data were suddenly redirected to focus on COVID-related issues, including tracking government announcements that were changing daily and providing needed resources to SHM members. By the time they could raise their heads and begin thinking about survey data, we were months behind schedule.
I need to give a huge shout-out to our survey manager extraordinaire Josh Lapps, SHM’s Director of Policy and Practice Management, and his survey support team including Luke Heisinger and Kim Schonberger. Once they were able to turn their focus back to the SoHM, they worked like demons to catch up. And in addition to the work of preparing the SoHM for publication, they helped issue and analyze a follow-up survey to investigate how HMGs adjusted their staffing and operations in response to COVID! As I write this, we appear to be back on schedule for a September SoHM release date, with the COVID supplemental survey report to follow soon after. Thanks also to PAC committee members who, despite their own stresses, rose to the challenge of participating in calls and planning the supplemental survey.
Despite the pandemic, HMGs found survey participation valuable. When all was said and done, we had a respectable number of respondent groups: 502 this year vs. 569 in 2018. Although the number of respondent groups is down, the average group size has increased, so that an all-time high of 10,122 employed/contracted full-time equivalent (FTE) hospitalists (plus 484 locum tenens FTEs) are represented in the data set. The respondents continue to be very diverse, representing all practice models and every state – and even a couple of other countries. One notable change is a significant increase in pediatric HM group participation, thanks to a recruitment charge led by PAC member Sandra Gage, associate division chief of hospital medicine at Phoenix Children’s Hospital, and supported by the inclusion of several new pediatric HM-specific questions to better capture unique attributes of these hospital medicine practices.
We had more multisite respondents than ever, and the multisite respondents overwhelmingly used the new “retake” feature in the online version of the survey. I’m happy to report that we received consistent positive feedback about our new electronic survey platform, and thanks to its capabilities data analysis has been significantly automated, enhancing both efficiency and data reliability.
The survey content is more wide ranging than ever. In addition to the usual topics such as scope of services, staffing and scheduling, compensation models, evaluation and management code distribution, and HM group finances, the 2020 report will include the afore-referenced information about HM groups serving children, expanded information on nurse practitioner (NPs)/physician assistant (PA) roles, and data on diversity in HM physician leadership. The follow-up COVID survey will be published separately as a supplement, available only to purchasers of the SoHM report.
Multiple options for SoHM report purchase. All survey participants will receive access to the online version of the survey. Others may purchase the hard copy report, online access, or both. The report has a colorful, easy-to-read layout, and many of the tables have been streamlined to make them easier to read. I encourage you to sign up to preorder your copy of the SoHM Report today at www.hospitalmedicine.org/sohm; you’ll almost certainly discover a treasure trove of worthwhile information.
Use the report to assess how your practice compares to other practices, but always keep in mind that surveys don’t tell you what should be; they only tell you what currently is the case – or at least, what was during the survey period. New best practices not yet reflected in survey data are emerging all the time, and that is probably more true today in the new world affected by this pandemic than ever before. And while the ways others do things won’t always be right for your group’s unique situation and needs, it always helps to know how you compare with others. Whether you are partners or employees, you and your colleagues “own” the success of your hospital medicine practice and, armed with the best available data, are the best judges of what is right for you.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
On behalf of SHM’s Practice Analysis Committee, I am excited to announce the scheduled September 2020 release of the 2020 State of Hospital Medicine Report (SoHM)!
For reasons all too familiar, this year’s SoHM survey process was unlike any in SHM’s history. We were still collecting survey responses from a few stragglers in early March when the entire world shut down almost overnight to flatten the curve of a deadly pandemic. Hospital medicine group (HMG) leaders were suddenly either up to their eyeballs trying to figure out how to safely care for huge influxes of COVID-19 patients that overwhelmed established systems of care or were trying to figure out how to staff in a low-volume environment with few COVID patients, a relative trickle of ED admissions, and virtually no surgical care. And everywhere, hospitals and their HMGs were quickly stressed in ways that would have been unimaginable just a couple of months earlier – financially, operationally, epidemiologically, and culturally.
SHM offices closed, with all staff working from home. And the talented people who would normally have been working diligently on the survey data were suddenly redirected to focus on COVID-related issues, including tracking government announcements that were changing daily and providing needed resources to SHM members. By the time they could raise their heads and begin thinking about survey data, we were months behind schedule.
I need to give a huge shout-out to our survey manager extraordinaire Josh Lapps, SHM’s Director of Policy and Practice Management, and his survey support team including Luke Heisinger and Kim Schonberger. Once they were able to turn their focus back to the SoHM, they worked like demons to catch up. And in addition to the work of preparing the SoHM for publication, they helped issue and analyze a follow-up survey to investigate how HMGs adjusted their staffing and operations in response to COVID! As I write this, we appear to be back on schedule for a September SoHM release date, with the COVID supplemental survey report to follow soon after. Thanks also to PAC committee members who, despite their own stresses, rose to the challenge of participating in calls and planning the supplemental survey.
Despite the pandemic, HMGs found survey participation valuable. When all was said and done, we had a respectable number of respondent groups: 502 this year vs. 569 in 2018. Although the number of respondent groups is down, the average group size has increased, so that an all-time high of 10,122 employed/contracted full-time equivalent (FTE) hospitalists (plus 484 locum tenens FTEs) are represented in the data set. The respondents continue to be very diverse, representing all practice models and every state – and even a couple of other countries. One notable change is a significant increase in pediatric HM group participation, thanks to a recruitment charge led by PAC member Sandra Gage, associate division chief of hospital medicine at Phoenix Children’s Hospital, and supported by the inclusion of several new pediatric HM-specific questions to better capture unique attributes of these hospital medicine practices.
We had more multisite respondents than ever, and the multisite respondents overwhelmingly used the new “retake” feature in the online version of the survey. I’m happy to report that we received consistent positive feedback about our new electronic survey platform, and thanks to its capabilities data analysis has been significantly automated, enhancing both efficiency and data reliability.
The survey content is more wide ranging than ever. In addition to the usual topics such as scope of services, staffing and scheduling, compensation models, evaluation and management code distribution, and HM group finances, the 2020 report will include the afore-referenced information about HM groups serving children, expanded information on nurse practitioner (NPs)/physician assistant (PA) roles, and data on diversity in HM physician leadership. The follow-up COVID survey will be published separately as a supplement, available only to purchasers of the SoHM report.
Multiple options for SoHM report purchase. All survey participants will receive access to the online version of the survey. Others may purchase the hard copy report, online access, or both. The report has a colorful, easy-to-read layout, and many of the tables have been streamlined to make them easier to read. I encourage you to sign up to preorder your copy of the SoHM Report today at www.hospitalmedicine.org/sohm; you’ll almost certainly discover a treasure trove of worthwhile information.
Use the report to assess how your practice compares to other practices, but always keep in mind that surveys don’t tell you what should be; they only tell you what currently is the case – or at least, what was during the survey period. New best practices not yet reflected in survey data are emerging all the time, and that is probably more true today in the new world affected by this pandemic than ever before. And while the ways others do things won’t always be right for your group’s unique situation and needs, it always helps to know how you compare with others. Whether you are partners or employees, you and your colleagues “own” the success of your hospital medicine practice and, armed with the best available data, are the best judges of what is right for you.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Dr. Eric E. Howell assumes new role as CEO of SHM
The Society of Hospital Medicine officially welcomed Eric E. Howell, MD, MHM, as chief executive officer on July 1, 2020. Dr. Howell reports to the Society of Hospital Medicine board of directors and is tasked with ensuring that SHM continues to serve the evolving needs and interests of its members while overseeing the organization’s strategic direction.
“The SHM board of directors is excited to work with Dr. Howell to navigate the future of SHM and of the hospital medicine specialty,” said Danielle Scheurer, MD, MSCR, SFHM, SHM president and chair of the CEO Search Committee. “With his extensive knowledge of the health care landscape and of SHM, Dr. Howell embodies the society’s dedication to empowering hospitalists to be positive change agents in their institutions and in the health care system as a whole.”
Prior to his current role, Dr. Howell served as chief operating officer of SHM for 2 years; in that role, he led senior management’s planning and defined organizational goals to drive growth. As the senior physician adviser to SHM’s Center for Quality Improvement for 5 years, he consulted for the society’s arm that conducts quality improvement programs for hospitalist teams. In addition to being a past president of SHM’s board of directors, he is the course director for the SHM Leadership Academies.
“Now more than ever, SHM has an opportunity to superserve hospitalists and the patients they serve, and I couldn’t be more excited to lead the society into its next chapter,” Dr. Howell said. “Supported by a dedicated member base and innovative staff, I am confident that SHM will continue on its successful path forward and will provide its members with the products, services, and tools that hospitalists need to improve patient care and adapt to the constantly evolving environment.”
In addition to serving in various capacities at SHM, Dr. Howell has served as a professor of medicine in the department of medicine at Johns Hopkins University, Baltimore. He has held multiple titles within the Johns Hopkins medical institutions, including chief of the division of hospital medicine at Johns Hopkins Bayview, section chief of hospital medicine for Johns Hopkins Community Physicians, deputy director of hospital operations for the department of medicine at Johns Hopkins Bayview Medical Center, and chief medical officer of operations at Johns Hopkins Bayview. Dr. Howell joined the Johns Hopkins Bayview hospitalist program in 2000, began the Howard County (Md.) General Hospital hospitalist program in 2010, and oversaw nearly 200 physicians and clinical staff providing patient care in three hospitals. Along with his role as SHM CEO, he will remain a member of the adjunct faculty at Johns Hopkins University.
More recently, Dr. Howell served as chief medical officer for the Baltimore Convention Center Field Hospital, a fully functional, 250-bed hospital created to care for patients in the Baltimore metropolitan area who were suffering from complications from COVID-19.
Dr. Howell received his electrical engineering degree from the University of Maryland, College Park, which has proven instrumental in his mastery of managing and implementing change in the hospital. His research has focused on the relationship between the emergency department and medicine floors, improving communication, throughput and patient outcomes.
The nationwide search process that led to Dr. Howell’s appointment was led by a CEO Search Committee, which included members of the SHM board of directors and was assisted by the executive search firm Spencer Stuart.
Dr. Howell succeeds Laurence Wellikson, MD, MHM, who helped in founding the Society of Hospital Medicine, its first and only CEO since 2000 prior to Dr. Howell’s appointment.
The Society of Hospital Medicine officially welcomed Eric E. Howell, MD, MHM, as chief executive officer on July 1, 2020. Dr. Howell reports to the Society of Hospital Medicine board of directors and is tasked with ensuring that SHM continues to serve the evolving needs and interests of its members while overseeing the organization’s strategic direction.
“The SHM board of directors is excited to work with Dr. Howell to navigate the future of SHM and of the hospital medicine specialty,” said Danielle Scheurer, MD, MSCR, SFHM, SHM president and chair of the CEO Search Committee. “With his extensive knowledge of the health care landscape and of SHM, Dr. Howell embodies the society’s dedication to empowering hospitalists to be positive change agents in their institutions and in the health care system as a whole.”
Prior to his current role, Dr. Howell served as chief operating officer of SHM for 2 years; in that role, he led senior management’s planning and defined organizational goals to drive growth. As the senior physician adviser to SHM’s Center for Quality Improvement for 5 years, he consulted for the society’s arm that conducts quality improvement programs for hospitalist teams. In addition to being a past president of SHM’s board of directors, he is the course director for the SHM Leadership Academies.
“Now more than ever, SHM has an opportunity to superserve hospitalists and the patients they serve, and I couldn’t be more excited to lead the society into its next chapter,” Dr. Howell said. “Supported by a dedicated member base and innovative staff, I am confident that SHM will continue on its successful path forward and will provide its members with the products, services, and tools that hospitalists need to improve patient care and adapt to the constantly evolving environment.”
In addition to serving in various capacities at SHM, Dr. Howell has served as a professor of medicine in the department of medicine at Johns Hopkins University, Baltimore. He has held multiple titles within the Johns Hopkins medical institutions, including chief of the division of hospital medicine at Johns Hopkins Bayview, section chief of hospital medicine for Johns Hopkins Community Physicians, deputy director of hospital operations for the department of medicine at Johns Hopkins Bayview Medical Center, and chief medical officer of operations at Johns Hopkins Bayview. Dr. Howell joined the Johns Hopkins Bayview hospitalist program in 2000, began the Howard County (Md.) General Hospital hospitalist program in 2010, and oversaw nearly 200 physicians and clinical staff providing patient care in three hospitals. Along with his role as SHM CEO, he will remain a member of the adjunct faculty at Johns Hopkins University.
More recently, Dr. Howell served as chief medical officer for the Baltimore Convention Center Field Hospital, a fully functional, 250-bed hospital created to care for patients in the Baltimore metropolitan area who were suffering from complications from COVID-19.
Dr. Howell received his electrical engineering degree from the University of Maryland, College Park, which has proven instrumental in his mastery of managing and implementing change in the hospital. His research has focused on the relationship between the emergency department and medicine floors, improving communication, throughput and patient outcomes.
The nationwide search process that led to Dr. Howell’s appointment was led by a CEO Search Committee, which included members of the SHM board of directors and was assisted by the executive search firm Spencer Stuart.
Dr. Howell succeeds Laurence Wellikson, MD, MHM, who helped in founding the Society of Hospital Medicine, its first and only CEO since 2000 prior to Dr. Howell’s appointment.
The Society of Hospital Medicine officially welcomed Eric E. Howell, MD, MHM, as chief executive officer on July 1, 2020. Dr. Howell reports to the Society of Hospital Medicine board of directors and is tasked with ensuring that SHM continues to serve the evolving needs and interests of its members while overseeing the organization’s strategic direction.
“The SHM board of directors is excited to work with Dr. Howell to navigate the future of SHM and of the hospital medicine specialty,” said Danielle Scheurer, MD, MSCR, SFHM, SHM president and chair of the CEO Search Committee. “With his extensive knowledge of the health care landscape and of SHM, Dr. Howell embodies the society’s dedication to empowering hospitalists to be positive change agents in their institutions and in the health care system as a whole.”
Prior to his current role, Dr. Howell served as chief operating officer of SHM for 2 years; in that role, he led senior management’s planning and defined organizational goals to drive growth. As the senior physician adviser to SHM’s Center for Quality Improvement for 5 years, he consulted for the society’s arm that conducts quality improvement programs for hospitalist teams. In addition to being a past president of SHM’s board of directors, he is the course director for the SHM Leadership Academies.
“Now more than ever, SHM has an opportunity to superserve hospitalists and the patients they serve, and I couldn’t be more excited to lead the society into its next chapter,” Dr. Howell said. “Supported by a dedicated member base and innovative staff, I am confident that SHM will continue on its successful path forward and will provide its members with the products, services, and tools that hospitalists need to improve patient care and adapt to the constantly evolving environment.”
In addition to serving in various capacities at SHM, Dr. Howell has served as a professor of medicine in the department of medicine at Johns Hopkins University, Baltimore. He has held multiple titles within the Johns Hopkins medical institutions, including chief of the division of hospital medicine at Johns Hopkins Bayview, section chief of hospital medicine for Johns Hopkins Community Physicians, deputy director of hospital operations for the department of medicine at Johns Hopkins Bayview Medical Center, and chief medical officer of operations at Johns Hopkins Bayview. Dr. Howell joined the Johns Hopkins Bayview hospitalist program in 2000, began the Howard County (Md.) General Hospital hospitalist program in 2010, and oversaw nearly 200 physicians and clinical staff providing patient care in three hospitals. Along with his role as SHM CEO, he will remain a member of the adjunct faculty at Johns Hopkins University.
More recently, Dr. Howell served as chief medical officer for the Baltimore Convention Center Field Hospital, a fully functional, 250-bed hospital created to care for patients in the Baltimore metropolitan area who were suffering from complications from COVID-19.
Dr. Howell received his electrical engineering degree from the University of Maryland, College Park, which has proven instrumental in his mastery of managing and implementing change in the hospital. His research has focused on the relationship between the emergency department and medicine floors, improving communication, throughput and patient outcomes.
The nationwide search process that led to Dr. Howell’s appointment was led by a CEO Search Committee, which included members of the SHM board of directors and was assisted by the executive search firm Spencer Stuart.
Dr. Howell succeeds Laurence Wellikson, MD, MHM, who helped in founding the Society of Hospital Medicine, its first and only CEO since 2000 prior to Dr. Howell’s appointment.
The wave of the future
Longtime CEO bids farewell to SHM
Changing times
After more than 20 years, my leadership role as CEO at the Society of Hospital Medicine (SHM) has ended with the transition to Dr. Eric Howell as the new SHM CEO on July 1, 2020. Looking back, I think we can all be proud of how we have helped to shape the specialty of hospital medicine over these two decades and of how strong SHM has become to support our new specialty.
In 2000, few people knew what a hospitalist was (or more importantly what we could become) and the specialty of hospital medicine had not even been named yet. Today the reputation of SHM is firmly established and the specialty has been defined by a unique curriculum through the Core Competencies in Hospital Medicine for both adult and pediatric patients, and by several textbooks in hospital medicine. There are divisions or departments of hospital medicine at many hospitals and academic medical centers. We even managed to convince the American Board of Internal Medicine, the American Board of Family Medicine, and the American Board of Medical Specialties to create a credential of Focused Practice in Hospital Medicine as the first-ever certification not tied to specific fellowship training.
To recognize the contributions of our members, SHM has established Awards of Excellence and the Fellow and Senior Fellow in Hospital Medicine (FHM and SFHM) designations. We have gone from a small national association in Philadelphia to create 68 active chapters and more than 20 Special Interest Groups. In my time at SHM I have attended more than 75-chapter meetings and met with thousands of hospitalists in 46 states. We now have over 20,000 members at SHM, making us the fastest growing medical specialty ever.
When I started at the National Association of Inpatient Physicians (NAIP) our only meeting was an annual CME meeting for about 150-200 people. We now hold a national meeting every year for more than 4,000 attendees that is the “Center of the Universe for Hospital Medicine.” Understanding that we needed to educate the people who will lead change in our health care system, we developed from scratch a set of Leadership Academies that has already educated more than 2,500 hospitalist leaders. To train the educators in quality improvement in medical education we developed our Quality and Safety Educator Academy (QSEA) programs, and to promote career development of academic hospitalists we created our Academic Hospitalist Academy.
SHM is the leader in adult in-practice learning, specifically designed for hospitalists. SHM members have access to a state-of-the-art comprehensive hospitalist-based online education system as well as board review and maintenance of certification (MOC) review tools in our SPARK program, specifically for hospital medicine.
In the area of quality improvement, most medical societies convene a panel of experts, develop guidelines, publish them, and hope that change will occur. SHM has been much more proactive, creating the Center for Quality Improvement that has raised more than $10 million and developed Quality Improvement programs in more than 400 hospitals over the years, winning the prestigious Eisenberg Award along the way.
When I started at NAIP in 2000, our only communication tools were a 4-page newsletter and an email listserv. Along the way we have developed a broadly read newsmagazine (The Hospitalist), a well-recognized peer reviewed journal (Journal of Hospital Medicine), a robust website, and a significant social media presence.
From the very early days we knew that our specialty would not be totally successful by only facing inward. Change was coming to our health care system and hospitalists were going to be right in the middle. Despite our young age and limited resources, we have always hit above our weight class in advocacy. We actively participated in the development of the Affordable Care Act (Obamacare), making suggestions in payment reform, expanding the workforce with visa reform, and expanding the team of clinicians. Along the way SHM members rose to run the Centers for Medicare & Medicaid Services (CMS) and the Food and Drug Administration (FDA), and serve as U.S. Surgeon General.
Today in these troubled times, SHM continues to be a positive voice in promoting the use of PPE, the need for increased COVID-19 testing, and the recognition of our nation’s 60,000 hospitalists as essential frontline workers in the COVID-19 pandemic. With its longstanding role in promoting diversity and overcoming social injustice, SHM has had a positive national voice during the protests over police brutality.
We have proved to be a good partner with many other organizations and consistently were invited to partner in coalitions with the ED physicians (ACEP), the critical care docs (SCCM), the hospitals (AHA), the house of medicine (AMA), other internists (ACP), surgeons (ACS), and pediatricians (AAP), and so many other much more established societies, because we could be an active, flexible, and knowledgeable partner for more than 20 years.
Today, SHM and hospital medicine are clearly recognized as a force in the rapidly evolving health care system. With this comes not only influence but also responsibility, and I am certain the SHM Board, membership, and staff are ready for this challenge. The economic toll of our current pandemic will see colleges and other major companies and institutions go out of business and leave the landscape. SHM has a deep foundation and a well of strength to call on and will survive and thrive into the future.
SHM has been a good fit for me professionally and personally. Many of my skills and strengths have served SHM in our “early” years. I am very proud of what we have been able to accomplish TOGETHER. In the end it is the people I have been fortunate enough to meet and work with throughout these past 20 years that will stay with me, many of whom are lifelong friends. My mother, even today at 93, has always asked me to leave anything I do better off than when I came in the door. As I look back at my time helping to shape and lead SHM, I am sure I have answered my mother’s challenge and more.
I look forward to seeing many of you at a future SHM meeting and reveling in the way that hospitalists will actively play an important role in shaping our health care system in the future.
Dr. Wellikson is retiring as CEO of SHM.
Live long and prosper
Back in 2000, I was extremely fortunate to land my dream job as a hospitalist at Johns Hopkins Bayview in Baltimore. That dream exceeded my wildest aspirations. During my 20-year career as faculty in the Johns Hopkins School of Medicine I grew our tiny, 4 physician hospitalist group at Johns Hopkins Bayview into a multihospital program, complete with more than 150 physicians. That exceedingly rewarding work helped to shape the field of hospital medicine nationally and provided the foundation for my promotion to professor of medicine at Johns Hopkins in 2016.
Most professionals are lucky if they find one inspiring institution; I have found two. SHM has been my professional home since I became a hospitalist in 2000, and in that time I have dedicated as much creative energy to SHM as I have at Johns Hopkins.
Even at this time when the medical profession, and the entire world, has been rocked by the coronavirus, the fundamentals that have made SHM so successful will serve us well through the effects of this pandemic and beyond. It takes a skilled leader to nurture a professional society through the growth from only a few hundred members to thousands upon thousands, and at the same time crafting the profession into one of quality and high impact. These past 22 years Dr. Larry Wellikson, our retiring CEO, has skillfully accomplished just that by building lasting programs and people.
As you might imagine, my approach will work to add onto the legacy that Larry has left us. Yes, we will have to adapt SHM to the realities of the near future: virtual meetings, in-person events (yes, those will return one day) with appropriate social distancing until the coronavirus has faded, modified chapter meetings, and more. Someday the world will find a new normal, and SHM will evolve to meet the needs of our members and the patients we serve.
Through this pandemic and beyond, my vision – in partnership with the Board of Directors – will be to:
- Continue the work to enhance member engagement. We are primarily a membership organization, after all.
- Maintain our profession’s leadership role in the care continuum, particularly acute care.
- Be a deliberate sponsor of diversity and inclusion. I believe social justice is a moral imperative, and good business.
- Invest in teams: Chapters, special interest groups, and committees are key to success.
- Be financially prudent, so that this organization can serve its members through the best of times and those most challenging times.
Back in 2000 I joined my dream society, the Society of Hospital Medicine. That society exceeded my wildest aspirations. During my 20-year membership I started an SHM Chapter, was a leader in the Leadership Academies, joined the Board of Directors, participated in Annual Conferences, and helped lead the SHM Center for Quality Improvement. That exceedingly rewarding partnership helped shape the field of hospital medicine nationally and provided the foundation for my next role at SHM. I am excited and grateful to be the CEO of SHM.
I’ll end with something I use every day – “Eric Howell’s Core Values”:
- Make the world a better place.
- Invest in people.
- Be ethical and transparent.
- Do what you love.
- Try to use Star Trek references whenever possible. (Okay, this last one is not really a core value, but maybe a character trait?) At least the Vulcan greeting is appropriate for our times: Live long and prosper.
Dr. Howell is the new CEO for SHM as of July 1, 2020.
Longtime CEO bids farewell to SHM
Longtime CEO bids farewell to SHM
Changing times
After more than 20 years, my leadership role as CEO at the Society of Hospital Medicine (SHM) has ended with the transition to Dr. Eric Howell as the new SHM CEO on July 1, 2020. Looking back, I think we can all be proud of how we have helped to shape the specialty of hospital medicine over these two decades and of how strong SHM has become to support our new specialty.
In 2000, few people knew what a hospitalist was (or more importantly what we could become) and the specialty of hospital medicine had not even been named yet. Today the reputation of SHM is firmly established and the specialty has been defined by a unique curriculum through the Core Competencies in Hospital Medicine for both adult and pediatric patients, and by several textbooks in hospital medicine. There are divisions or departments of hospital medicine at many hospitals and academic medical centers. We even managed to convince the American Board of Internal Medicine, the American Board of Family Medicine, and the American Board of Medical Specialties to create a credential of Focused Practice in Hospital Medicine as the first-ever certification not tied to specific fellowship training.
To recognize the contributions of our members, SHM has established Awards of Excellence and the Fellow and Senior Fellow in Hospital Medicine (FHM and SFHM) designations. We have gone from a small national association in Philadelphia to create 68 active chapters and more than 20 Special Interest Groups. In my time at SHM I have attended more than 75-chapter meetings and met with thousands of hospitalists in 46 states. We now have over 20,000 members at SHM, making us the fastest growing medical specialty ever.
When I started at the National Association of Inpatient Physicians (NAIP) our only meeting was an annual CME meeting for about 150-200 people. We now hold a national meeting every year for more than 4,000 attendees that is the “Center of the Universe for Hospital Medicine.” Understanding that we needed to educate the people who will lead change in our health care system, we developed from scratch a set of Leadership Academies that has already educated more than 2,500 hospitalist leaders. To train the educators in quality improvement in medical education we developed our Quality and Safety Educator Academy (QSEA) programs, and to promote career development of academic hospitalists we created our Academic Hospitalist Academy.
SHM is the leader in adult in-practice learning, specifically designed for hospitalists. SHM members have access to a state-of-the-art comprehensive hospitalist-based online education system as well as board review and maintenance of certification (MOC) review tools in our SPARK program, specifically for hospital medicine.
In the area of quality improvement, most medical societies convene a panel of experts, develop guidelines, publish them, and hope that change will occur. SHM has been much more proactive, creating the Center for Quality Improvement that has raised more than $10 million and developed Quality Improvement programs in more than 400 hospitals over the years, winning the prestigious Eisenberg Award along the way.
When I started at NAIP in 2000, our only communication tools were a 4-page newsletter and an email listserv. Along the way we have developed a broadly read newsmagazine (The Hospitalist), a well-recognized peer reviewed journal (Journal of Hospital Medicine), a robust website, and a significant social media presence.
From the very early days we knew that our specialty would not be totally successful by only facing inward. Change was coming to our health care system and hospitalists were going to be right in the middle. Despite our young age and limited resources, we have always hit above our weight class in advocacy. We actively participated in the development of the Affordable Care Act (Obamacare), making suggestions in payment reform, expanding the workforce with visa reform, and expanding the team of clinicians. Along the way SHM members rose to run the Centers for Medicare & Medicaid Services (CMS) and the Food and Drug Administration (FDA), and serve as U.S. Surgeon General.
Today in these troubled times, SHM continues to be a positive voice in promoting the use of PPE, the need for increased COVID-19 testing, and the recognition of our nation’s 60,000 hospitalists as essential frontline workers in the COVID-19 pandemic. With its longstanding role in promoting diversity and overcoming social injustice, SHM has had a positive national voice during the protests over police brutality.
We have proved to be a good partner with many other organizations and consistently were invited to partner in coalitions with the ED physicians (ACEP), the critical care docs (SCCM), the hospitals (AHA), the house of medicine (AMA), other internists (ACP), surgeons (ACS), and pediatricians (AAP), and so many other much more established societies, because we could be an active, flexible, and knowledgeable partner for more than 20 years.
Today, SHM and hospital medicine are clearly recognized as a force in the rapidly evolving health care system. With this comes not only influence but also responsibility, and I am certain the SHM Board, membership, and staff are ready for this challenge. The economic toll of our current pandemic will see colleges and other major companies and institutions go out of business and leave the landscape. SHM has a deep foundation and a well of strength to call on and will survive and thrive into the future.
SHM has been a good fit for me professionally and personally. Many of my skills and strengths have served SHM in our “early” years. I am very proud of what we have been able to accomplish TOGETHER. In the end it is the people I have been fortunate enough to meet and work with throughout these past 20 years that will stay with me, many of whom are lifelong friends. My mother, even today at 93, has always asked me to leave anything I do better off than when I came in the door. As I look back at my time helping to shape and lead SHM, I am sure I have answered my mother’s challenge and more.
I look forward to seeing many of you at a future SHM meeting and reveling in the way that hospitalists will actively play an important role in shaping our health care system in the future.
Dr. Wellikson is retiring as CEO of SHM.
Live long and prosper
Back in 2000, I was extremely fortunate to land my dream job as a hospitalist at Johns Hopkins Bayview in Baltimore. That dream exceeded my wildest aspirations. During my 20-year career as faculty in the Johns Hopkins School of Medicine I grew our tiny, 4 physician hospitalist group at Johns Hopkins Bayview into a multihospital program, complete with more than 150 physicians. That exceedingly rewarding work helped to shape the field of hospital medicine nationally and provided the foundation for my promotion to professor of medicine at Johns Hopkins in 2016.
Most professionals are lucky if they find one inspiring institution; I have found two. SHM has been my professional home since I became a hospitalist in 2000, and in that time I have dedicated as much creative energy to SHM as I have at Johns Hopkins.
Even at this time when the medical profession, and the entire world, has been rocked by the coronavirus, the fundamentals that have made SHM so successful will serve us well through the effects of this pandemic and beyond. It takes a skilled leader to nurture a professional society through the growth from only a few hundred members to thousands upon thousands, and at the same time crafting the profession into one of quality and high impact. These past 22 years Dr. Larry Wellikson, our retiring CEO, has skillfully accomplished just that by building lasting programs and people.
As you might imagine, my approach will work to add onto the legacy that Larry has left us. Yes, we will have to adapt SHM to the realities of the near future: virtual meetings, in-person events (yes, those will return one day) with appropriate social distancing until the coronavirus has faded, modified chapter meetings, and more. Someday the world will find a new normal, and SHM will evolve to meet the needs of our members and the patients we serve.
Through this pandemic and beyond, my vision – in partnership with the Board of Directors – will be to:
- Continue the work to enhance member engagement. We are primarily a membership organization, after all.
- Maintain our profession’s leadership role in the care continuum, particularly acute care.
- Be a deliberate sponsor of diversity and inclusion. I believe social justice is a moral imperative, and good business.
- Invest in teams: Chapters, special interest groups, and committees are key to success.
- Be financially prudent, so that this organization can serve its members through the best of times and those most challenging times.
Back in 2000 I joined my dream society, the Society of Hospital Medicine. That society exceeded my wildest aspirations. During my 20-year membership I started an SHM Chapter, was a leader in the Leadership Academies, joined the Board of Directors, participated in Annual Conferences, and helped lead the SHM Center for Quality Improvement. That exceedingly rewarding partnership helped shape the field of hospital medicine nationally and provided the foundation for my next role at SHM. I am excited and grateful to be the CEO of SHM.
I’ll end with something I use every day – “Eric Howell’s Core Values”:
- Make the world a better place.
- Invest in people.
- Be ethical and transparent.
- Do what you love.
- Try to use Star Trek references whenever possible. (Okay, this last one is not really a core value, but maybe a character trait?) At least the Vulcan greeting is appropriate for our times: Live long and prosper.
Dr. Howell is the new CEO for SHM as of July 1, 2020.
Changing times
After more than 20 years, my leadership role as CEO at the Society of Hospital Medicine (SHM) has ended with the transition to Dr. Eric Howell as the new SHM CEO on July 1, 2020. Looking back, I think we can all be proud of how we have helped to shape the specialty of hospital medicine over these two decades and of how strong SHM has become to support our new specialty.
In 2000, few people knew what a hospitalist was (or more importantly what we could become) and the specialty of hospital medicine had not even been named yet. Today the reputation of SHM is firmly established and the specialty has been defined by a unique curriculum through the Core Competencies in Hospital Medicine for both adult and pediatric patients, and by several textbooks in hospital medicine. There are divisions or departments of hospital medicine at many hospitals and academic medical centers. We even managed to convince the American Board of Internal Medicine, the American Board of Family Medicine, and the American Board of Medical Specialties to create a credential of Focused Practice in Hospital Medicine as the first-ever certification not tied to specific fellowship training.
To recognize the contributions of our members, SHM has established Awards of Excellence and the Fellow and Senior Fellow in Hospital Medicine (FHM and SFHM) designations. We have gone from a small national association in Philadelphia to create 68 active chapters and more than 20 Special Interest Groups. In my time at SHM I have attended more than 75-chapter meetings and met with thousands of hospitalists in 46 states. We now have over 20,000 members at SHM, making us the fastest growing medical specialty ever.
When I started at the National Association of Inpatient Physicians (NAIP) our only meeting was an annual CME meeting for about 150-200 people. We now hold a national meeting every year for more than 4,000 attendees that is the “Center of the Universe for Hospital Medicine.” Understanding that we needed to educate the people who will lead change in our health care system, we developed from scratch a set of Leadership Academies that has already educated more than 2,500 hospitalist leaders. To train the educators in quality improvement in medical education we developed our Quality and Safety Educator Academy (QSEA) programs, and to promote career development of academic hospitalists we created our Academic Hospitalist Academy.
SHM is the leader in adult in-practice learning, specifically designed for hospitalists. SHM members have access to a state-of-the-art comprehensive hospitalist-based online education system as well as board review and maintenance of certification (MOC) review tools in our SPARK program, specifically for hospital medicine.
In the area of quality improvement, most medical societies convene a panel of experts, develop guidelines, publish them, and hope that change will occur. SHM has been much more proactive, creating the Center for Quality Improvement that has raised more than $10 million and developed Quality Improvement programs in more than 400 hospitals over the years, winning the prestigious Eisenberg Award along the way.
When I started at NAIP in 2000, our only communication tools were a 4-page newsletter and an email listserv. Along the way we have developed a broadly read newsmagazine (The Hospitalist), a well-recognized peer reviewed journal (Journal of Hospital Medicine), a robust website, and a significant social media presence.
From the very early days we knew that our specialty would not be totally successful by only facing inward. Change was coming to our health care system and hospitalists were going to be right in the middle. Despite our young age and limited resources, we have always hit above our weight class in advocacy. We actively participated in the development of the Affordable Care Act (Obamacare), making suggestions in payment reform, expanding the workforce with visa reform, and expanding the team of clinicians. Along the way SHM members rose to run the Centers for Medicare & Medicaid Services (CMS) and the Food and Drug Administration (FDA), and serve as U.S. Surgeon General.
Today in these troubled times, SHM continues to be a positive voice in promoting the use of PPE, the need for increased COVID-19 testing, and the recognition of our nation’s 60,000 hospitalists as essential frontline workers in the COVID-19 pandemic. With its longstanding role in promoting diversity and overcoming social injustice, SHM has had a positive national voice during the protests over police brutality.
We have proved to be a good partner with many other organizations and consistently were invited to partner in coalitions with the ED physicians (ACEP), the critical care docs (SCCM), the hospitals (AHA), the house of medicine (AMA), other internists (ACP), surgeons (ACS), and pediatricians (AAP), and so many other much more established societies, because we could be an active, flexible, and knowledgeable partner for more than 20 years.
Today, SHM and hospital medicine are clearly recognized as a force in the rapidly evolving health care system. With this comes not only influence but also responsibility, and I am certain the SHM Board, membership, and staff are ready for this challenge. The economic toll of our current pandemic will see colleges and other major companies and institutions go out of business and leave the landscape. SHM has a deep foundation and a well of strength to call on and will survive and thrive into the future.
SHM has been a good fit for me professionally and personally. Many of my skills and strengths have served SHM in our “early” years. I am very proud of what we have been able to accomplish TOGETHER. In the end it is the people I have been fortunate enough to meet and work with throughout these past 20 years that will stay with me, many of whom are lifelong friends. My mother, even today at 93, has always asked me to leave anything I do better off than when I came in the door. As I look back at my time helping to shape and lead SHM, I am sure I have answered my mother’s challenge and more.
I look forward to seeing many of you at a future SHM meeting and reveling in the way that hospitalists will actively play an important role in shaping our health care system in the future.
Dr. Wellikson is retiring as CEO of SHM.
Live long and prosper
Back in 2000, I was extremely fortunate to land my dream job as a hospitalist at Johns Hopkins Bayview in Baltimore. That dream exceeded my wildest aspirations. During my 20-year career as faculty in the Johns Hopkins School of Medicine I grew our tiny, 4 physician hospitalist group at Johns Hopkins Bayview into a multihospital program, complete with more than 150 physicians. That exceedingly rewarding work helped to shape the field of hospital medicine nationally and provided the foundation for my promotion to professor of medicine at Johns Hopkins in 2016.
Most professionals are lucky if they find one inspiring institution; I have found two. SHM has been my professional home since I became a hospitalist in 2000, and in that time I have dedicated as much creative energy to SHM as I have at Johns Hopkins.
Even at this time when the medical profession, and the entire world, has been rocked by the coronavirus, the fundamentals that have made SHM so successful will serve us well through the effects of this pandemic and beyond. It takes a skilled leader to nurture a professional society through the growth from only a few hundred members to thousands upon thousands, and at the same time crafting the profession into one of quality and high impact. These past 22 years Dr. Larry Wellikson, our retiring CEO, has skillfully accomplished just that by building lasting programs and people.
As you might imagine, my approach will work to add onto the legacy that Larry has left us. Yes, we will have to adapt SHM to the realities of the near future: virtual meetings, in-person events (yes, those will return one day) with appropriate social distancing until the coronavirus has faded, modified chapter meetings, and more. Someday the world will find a new normal, and SHM will evolve to meet the needs of our members and the patients we serve.
Through this pandemic and beyond, my vision – in partnership with the Board of Directors – will be to:
- Continue the work to enhance member engagement. We are primarily a membership organization, after all.
- Maintain our profession’s leadership role in the care continuum, particularly acute care.
- Be a deliberate sponsor of diversity and inclusion. I believe social justice is a moral imperative, and good business.
- Invest in teams: Chapters, special interest groups, and committees are key to success.
- Be financially prudent, so that this organization can serve its members through the best of times and those most challenging times.
Back in 2000 I joined my dream society, the Society of Hospital Medicine. That society exceeded my wildest aspirations. During my 20-year membership I started an SHM Chapter, was a leader in the Leadership Academies, joined the Board of Directors, participated in Annual Conferences, and helped lead the SHM Center for Quality Improvement. That exceedingly rewarding partnership helped shape the field of hospital medicine nationally and provided the foundation for my next role at SHM. I am excited and grateful to be the CEO of SHM.
I’ll end with something I use every day – “Eric Howell’s Core Values”:
- Make the world a better place.
- Invest in people.
- Be ethical and transparent.
- Do what you love.
- Try to use Star Trek references whenever possible. (Okay, this last one is not really a core value, but maybe a character trait?) At least the Vulcan greeting is appropriate for our times: Live long and prosper.
Dr. Howell is the new CEO for SHM as of July 1, 2020.
SHM responds to racism in the United States
The Society of Hospital Medicine deplores the negative impact of racism in our nation and will always strive to remedy racial inequities in our health care system. Racism in our society cannot be ignored. Nor will SHM ignore racism’s impact on public health. SHM enthusiastically supports its members working to promote equity and reduce the adverse impact of racism. We are committed to using our platform to improve the health of patients everywhere.
SHM would like to reaffirm its long-valued dedication to diversity and inclusion. We remain committed to promoting healthy discussions and action throughout our publications, resources and member communities, as outlined by our diversity and inclusion statement.
SHM Diversity and Inclusion Statement
Hospitalists are charged with treating individuals at their most vulnerable moments, when being respected as a whole person is crucial to advance patients’ healing and wellness. Within our workforce, diversity is a strength in all its forms, which helps us learn about the human experience, grow as leaders, and ultimately create a respectful environment for all regardless of age, race, religion, national origin, gender identity, sexual orientation, socioeconomic status, appearance, or ability.
To this end, the Society of Hospital Medicine will work to eliminate health disparities for our patients and foster inclusive and equitable cultures across our care teams and institutions with the goal of moving medicine and humanity forward.
The Society of Hospital Medicine deplores the negative impact of racism in our nation and will always strive to remedy racial inequities in our health care system. Racism in our society cannot be ignored. Nor will SHM ignore racism’s impact on public health. SHM enthusiastically supports its members working to promote equity and reduce the adverse impact of racism. We are committed to using our platform to improve the health of patients everywhere.
SHM would like to reaffirm its long-valued dedication to diversity and inclusion. We remain committed to promoting healthy discussions and action throughout our publications, resources and member communities, as outlined by our diversity and inclusion statement.
SHM Diversity and Inclusion Statement
Hospitalists are charged with treating individuals at their most vulnerable moments, when being respected as a whole person is crucial to advance patients’ healing and wellness. Within our workforce, diversity is a strength in all its forms, which helps us learn about the human experience, grow as leaders, and ultimately create a respectful environment for all regardless of age, race, religion, national origin, gender identity, sexual orientation, socioeconomic status, appearance, or ability.
To this end, the Society of Hospital Medicine will work to eliminate health disparities for our patients and foster inclusive and equitable cultures across our care teams and institutions with the goal of moving medicine and humanity forward.
The Society of Hospital Medicine deplores the negative impact of racism in our nation and will always strive to remedy racial inequities in our health care system. Racism in our society cannot be ignored. Nor will SHM ignore racism’s impact on public health. SHM enthusiastically supports its members working to promote equity and reduce the adverse impact of racism. We are committed to using our platform to improve the health of patients everywhere.
SHM would like to reaffirm its long-valued dedication to diversity and inclusion. We remain committed to promoting healthy discussions and action throughout our publications, resources and member communities, as outlined by our diversity and inclusion statement.
SHM Diversity and Inclusion Statement
Hospitalists are charged with treating individuals at their most vulnerable moments, when being respected as a whole person is crucial to advance patients’ healing and wellness. Within our workforce, diversity is a strength in all its forms, which helps us learn about the human experience, grow as leaders, and ultimately create a respectful environment for all regardless of age, race, religion, national origin, gender identity, sexual orientation, socioeconomic status, appearance, or ability.
To this end, the Society of Hospital Medicine will work to eliminate health disparities for our patients and foster inclusive and equitable cultures across our care teams and institutions with the goal of moving medicine and humanity forward.
Farewell to Larry Wellikson, MD, MHM
SHM cofounders praise the Society’s outgoing CEO
Setting the table for over 2 decades
I first met Larry in the spring of 1998 after I had made a presentation to the American College of Physicians’ Board of Regents on the Society for Hospital Medicine’s (then the National Association of Inpatient Physicians) new position statement that referral to hospitalists by primary care physicians should be voluntary. At the time, a number of managed care companies around the United States were compelling primary care physicians to use hospitalists to care for their hospitalized patients apparently because they felt hospitalists could do it more efficiently. SHM became the first professional society to voice the position which in turn was broadly endorsed by physician organizations, including the American Medical Association and the ACP.
Larry sought me out, engaged with me, and handed me his business card. He seemed keen on becoming a part of the rapidly accelerating hospitalist movement and, in retrospect, putting his signature on it. He had recently built and exited from a very large and successful independent physician association during the heyday of California managed care and was eager for a new challenge.
Unlike me, who was just a few years out of residency, Larry was at the height of his professional powers, with the right blend of experience on the one hand and energy on the other to take on a project like SHM.
Larry’s first contribution came in the form of facilitating a 2-day strategic planning meeting with the SHM board in the fall of 1998. John Nelson, MD, had moved to Philadelphia for 3 months to establish the operational foundation of SHM and guide SHM’s first staff member, Angela Musial. One of the most notable achievements during that time was a strategic planning board meeting, which largely set the course for SHM’s early years. Larry was a taskmaster, forcing us to make tough choices about what we wanted to accomplish and to establish concrete goals with timelines and milestones. The adult supervision Larry brought was a new and vital thing for us.
There was a lot at stake in ’97, ‘98, and ‘99. The demand for hospitalists across the nation was skyrocketing and there was a strong need for leadership and bold direction. Academics, community-based hospitalists, pediatricians, entrepreneurs, nonphysician hospital team members, heads of organized medicine, and government and industry leaders were just some of the key stakeholders looking for a seat at the HM table. That table would go on to be set for some 2 decades by Larry Wellikson.
From the beginning, many observers remarked that SHM had established an aggressive agenda. There was an unrelenting need to erect a big tent as a home for diverse stakeholders. John and I and the SHM board were doing all we could to continue to build momentum while also leading our local hospitalist groups and trying to maintain a semblance of balance with our young families back home.
It was against this backdrop, in late 1999, while on yet another flight crisscrossing the country to promote HM and SHM, that John; Bob Wachter, MD (who had by that time replaced John and I as SHM president); and I decided we needed a full-time CEO. By that time, each of us had participated in conversations with Larry. We rapidly decided, with buy-in from the board, that we would offer Larry the position. He accepted and became CEO in January 2000.
To list here all of Larry’s accomplishments since taking the helm at SHM would be impossible. Indeed, all that SHM has achieved is closely tied to Larry. Instead, I would like to call out character traits Larry brought to SHM that are now part of SHM’s DNA and a large part of the reason SHM has been so successful over the past 20 years.
Solution oriented. SHM’s culture has always been to take conditions as they are and work to make things better. There is no place for excessively airing grievances and complaining about “what is being done to us.”
Eschewing the status quo. We can do better. There is too much that needs to be done to wait.
Appropriately irreverent of the norms of the medical establishment. Physicians are by nature careful, plodding, considered, cautious, and methodical. The velocity of change in HM called for a different approach in order to be relevant, one better characterized as the move-fast-and-break-things ethos of a Silicon Valley startup.
Bringing diverse stakeholders to the table. A signature move has been to assemble influential people to lay out the issues before setting a course of action.
Strong bias to action. There is a time to analyze and discuss, but all of this ultimately is in service of taking action to achieve a tangible result.
Working to achieve consensus to a point, then moving forward. Considerable resources have been put into bringing stakeholders together, studying problems, and gaining a common understanding of issues. But this has never been at the expense of taking bold action, even if controversial at times.
Involving industry in creative ways to the benefit of patients. SHM pioneered an approach to use resources gained through industry partnerships to perform national scale improvement activities with groups of hospitalist mentor-experts working with local teams to make care more reliable for patients.
Tirelessly connecting to frontline hospitalists. The lifeblood of SHM is frontline hospitalists. Larry has taken the time to develop relationships with as many as possible, often through personally visiting their communities.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of SHM.
Dynamism
By John Nelson, MD, MHM
You probably know a few people with a magnetic personality. Larry Wellikson is the neodymium variety. Boundless energy, confidence that he has the answer or knows exactly where to find it, and ability to instantly recall every conversation he’s had with you, are traits that have energized his years leading SHM and have led countless people to regard him as friend and mentor.
Watch him at the SHM annual conference. There he goes, fast walking to his next commitment while facing backward to complete from a growing distance the conversation with a person he just bumped into along the way. It is like this for Larry from 6 a.m. until midnight. Like Alexander Hamilton, “the man is nonstop.”
Bill Campbell was the “Trillion Dollar Coach” who had his own success as a business leader, but is best known for mentoring Steve Jobs, the Google founders, and many others who went on to become titans of tech. Larry is hospital medicine’s “Coach,” and has inspired and guided the careers of so many clinicians, administrators, and entrepreneurs in hospital medicine and health care more broadly.
The biggest difference between these two highly effective leaders and mentors might be money; SHM has paid him pretty well, but alas, no stock options.
Larry is a great storyteller, and it doesn’t take long for a conversation with him to arrive at the point where he cites the example of how issues faced by someone else have parallels to your situation, the advice he gave that person, and how things turned out. Mostly this advice is about navigating professional life, but he is also happy to share wisdom about parenting, marriage, money, and sports. And most any other topic.
Larry was very accomplished even prior to connecting with SHM. He had a thriving clinical career, and though he left practice long ago he has maintained a close connection with many people he first met when they were his patients. I was surprised years ago when he drove up a new top-of-the-line Lexus – the two-seater with the solid convertible roof that folded into the trunk with the push of a button. I expressed surprise that he’d buy such a swanky car and he explained that a former patient, now long-time friend, was a Lexus distributor and arranged for Larry to drive it away for something like the cost of a Camry.
He also had terrific success forming and leading a large California independent physician association prior to connecting with SHM. Just ask him to show you the magazine with him on the cover and a glowing article detailing his accomplishments. Seriously, ask him, there’s a good chance he’ll have a copy with him.
When Dr. Win Whitcomb and I were trying to figure out how to start a new medical society and position our field to mature into a real specialty we were lucky enough to connect with many health care leaders who we thought could help. Most tended to pat us on the shoulder and say something along the lines of “good luck with your little hobby, now I have to get back to my important work.” But here was Larry with his impressive resume, having served as one of the leaders who crafted the merger of two giant medical societies (ACP and the American Society of Internal Medicine), keenly interested in our tiny new organization, and excited to serve as facilitator for our first strategic planning session.
SHM got a turbocharger when Larry signed on. For me it has felt like speeding down a highway, top down, radio blasting great music, and happy anticipation of what is around the next corner. I have never been disappointed, and certainly don’t plan to get out of Larry’s car just because he’s retiring as CEO.
Dr. Nelson is cofounder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants in La Quinta, Calif.
SHM cofounders praise the Society’s outgoing CEO
SHM cofounders praise the Society’s outgoing CEO
Setting the table for over 2 decades
I first met Larry in the spring of 1998 after I had made a presentation to the American College of Physicians’ Board of Regents on the Society for Hospital Medicine’s (then the National Association of Inpatient Physicians) new position statement that referral to hospitalists by primary care physicians should be voluntary. At the time, a number of managed care companies around the United States were compelling primary care physicians to use hospitalists to care for their hospitalized patients apparently because they felt hospitalists could do it more efficiently. SHM became the first professional society to voice the position which in turn was broadly endorsed by physician organizations, including the American Medical Association and the ACP.
Larry sought me out, engaged with me, and handed me his business card. He seemed keen on becoming a part of the rapidly accelerating hospitalist movement and, in retrospect, putting his signature on it. He had recently built and exited from a very large and successful independent physician association during the heyday of California managed care and was eager for a new challenge.
Unlike me, who was just a few years out of residency, Larry was at the height of his professional powers, with the right blend of experience on the one hand and energy on the other to take on a project like SHM.
Larry’s first contribution came in the form of facilitating a 2-day strategic planning meeting with the SHM board in the fall of 1998. John Nelson, MD, had moved to Philadelphia for 3 months to establish the operational foundation of SHM and guide SHM’s first staff member, Angela Musial. One of the most notable achievements during that time was a strategic planning board meeting, which largely set the course for SHM’s early years. Larry was a taskmaster, forcing us to make tough choices about what we wanted to accomplish and to establish concrete goals with timelines and milestones. The adult supervision Larry brought was a new and vital thing for us.
There was a lot at stake in ’97, ‘98, and ‘99. The demand for hospitalists across the nation was skyrocketing and there was a strong need for leadership and bold direction. Academics, community-based hospitalists, pediatricians, entrepreneurs, nonphysician hospital team members, heads of organized medicine, and government and industry leaders were just some of the key stakeholders looking for a seat at the HM table. That table would go on to be set for some 2 decades by Larry Wellikson.
From the beginning, many observers remarked that SHM had established an aggressive agenda. There was an unrelenting need to erect a big tent as a home for diverse stakeholders. John and I and the SHM board were doing all we could to continue to build momentum while also leading our local hospitalist groups and trying to maintain a semblance of balance with our young families back home.
It was against this backdrop, in late 1999, while on yet another flight crisscrossing the country to promote HM and SHM, that John; Bob Wachter, MD (who had by that time replaced John and I as SHM president); and I decided we needed a full-time CEO. By that time, each of us had participated in conversations with Larry. We rapidly decided, with buy-in from the board, that we would offer Larry the position. He accepted and became CEO in January 2000.
To list here all of Larry’s accomplishments since taking the helm at SHM would be impossible. Indeed, all that SHM has achieved is closely tied to Larry. Instead, I would like to call out character traits Larry brought to SHM that are now part of SHM’s DNA and a large part of the reason SHM has been so successful over the past 20 years.
Solution oriented. SHM’s culture has always been to take conditions as they are and work to make things better. There is no place for excessively airing grievances and complaining about “what is being done to us.”
Eschewing the status quo. We can do better. There is too much that needs to be done to wait.
Appropriately irreverent of the norms of the medical establishment. Physicians are by nature careful, plodding, considered, cautious, and methodical. The velocity of change in HM called for a different approach in order to be relevant, one better characterized as the move-fast-and-break-things ethos of a Silicon Valley startup.
Bringing diverse stakeholders to the table. A signature move has been to assemble influential people to lay out the issues before setting a course of action.
Strong bias to action. There is a time to analyze and discuss, but all of this ultimately is in service of taking action to achieve a tangible result.
Working to achieve consensus to a point, then moving forward. Considerable resources have been put into bringing stakeholders together, studying problems, and gaining a common understanding of issues. But this has never been at the expense of taking bold action, even if controversial at times.
Involving industry in creative ways to the benefit of patients. SHM pioneered an approach to use resources gained through industry partnerships to perform national scale improvement activities with groups of hospitalist mentor-experts working with local teams to make care more reliable for patients.
Tirelessly connecting to frontline hospitalists. The lifeblood of SHM is frontline hospitalists. Larry has taken the time to develop relationships with as many as possible, often through personally visiting their communities.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of SHM.
Dynamism
By John Nelson, MD, MHM
You probably know a few people with a magnetic personality. Larry Wellikson is the neodymium variety. Boundless energy, confidence that he has the answer or knows exactly where to find it, and ability to instantly recall every conversation he’s had with you, are traits that have energized his years leading SHM and have led countless people to regard him as friend and mentor.
Watch him at the SHM annual conference. There he goes, fast walking to his next commitment while facing backward to complete from a growing distance the conversation with a person he just bumped into along the way. It is like this for Larry from 6 a.m. until midnight. Like Alexander Hamilton, “the man is nonstop.”
Bill Campbell was the “Trillion Dollar Coach” who had his own success as a business leader, but is best known for mentoring Steve Jobs, the Google founders, and many others who went on to become titans of tech. Larry is hospital medicine’s “Coach,” and has inspired and guided the careers of so many clinicians, administrators, and entrepreneurs in hospital medicine and health care more broadly.
The biggest difference between these two highly effective leaders and mentors might be money; SHM has paid him pretty well, but alas, no stock options.
Larry is a great storyteller, and it doesn’t take long for a conversation with him to arrive at the point where he cites the example of how issues faced by someone else have parallels to your situation, the advice he gave that person, and how things turned out. Mostly this advice is about navigating professional life, but he is also happy to share wisdom about parenting, marriage, money, and sports. And most any other topic.
Larry was very accomplished even prior to connecting with SHM. He had a thriving clinical career, and though he left practice long ago he has maintained a close connection with many people he first met when they were his patients. I was surprised years ago when he drove up a new top-of-the-line Lexus – the two-seater with the solid convertible roof that folded into the trunk with the push of a button. I expressed surprise that he’d buy such a swanky car and he explained that a former patient, now long-time friend, was a Lexus distributor and arranged for Larry to drive it away for something like the cost of a Camry.
He also had terrific success forming and leading a large California independent physician association prior to connecting with SHM. Just ask him to show you the magazine with him on the cover and a glowing article detailing his accomplishments. Seriously, ask him, there’s a good chance he’ll have a copy with him.
When Dr. Win Whitcomb and I were trying to figure out how to start a new medical society and position our field to mature into a real specialty we were lucky enough to connect with many health care leaders who we thought could help. Most tended to pat us on the shoulder and say something along the lines of “good luck with your little hobby, now I have to get back to my important work.” But here was Larry with his impressive resume, having served as one of the leaders who crafted the merger of two giant medical societies (ACP and the American Society of Internal Medicine), keenly interested in our tiny new organization, and excited to serve as facilitator for our first strategic planning session.
SHM got a turbocharger when Larry signed on. For me it has felt like speeding down a highway, top down, radio blasting great music, and happy anticipation of what is around the next corner. I have never been disappointed, and certainly don’t plan to get out of Larry’s car just because he’s retiring as CEO.
Dr. Nelson is cofounder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants in La Quinta, Calif.
Setting the table for over 2 decades
I first met Larry in the spring of 1998 after I had made a presentation to the American College of Physicians’ Board of Regents on the Society for Hospital Medicine’s (then the National Association of Inpatient Physicians) new position statement that referral to hospitalists by primary care physicians should be voluntary. At the time, a number of managed care companies around the United States were compelling primary care physicians to use hospitalists to care for their hospitalized patients apparently because they felt hospitalists could do it more efficiently. SHM became the first professional society to voice the position which in turn was broadly endorsed by physician organizations, including the American Medical Association and the ACP.
Larry sought me out, engaged with me, and handed me his business card. He seemed keen on becoming a part of the rapidly accelerating hospitalist movement and, in retrospect, putting his signature on it. He had recently built and exited from a very large and successful independent physician association during the heyday of California managed care and was eager for a new challenge.
Unlike me, who was just a few years out of residency, Larry was at the height of his professional powers, with the right blend of experience on the one hand and energy on the other to take on a project like SHM.
Larry’s first contribution came in the form of facilitating a 2-day strategic planning meeting with the SHM board in the fall of 1998. John Nelson, MD, had moved to Philadelphia for 3 months to establish the operational foundation of SHM and guide SHM’s first staff member, Angela Musial. One of the most notable achievements during that time was a strategic planning board meeting, which largely set the course for SHM’s early years. Larry was a taskmaster, forcing us to make tough choices about what we wanted to accomplish and to establish concrete goals with timelines and milestones. The adult supervision Larry brought was a new and vital thing for us.
There was a lot at stake in ’97, ‘98, and ‘99. The demand for hospitalists across the nation was skyrocketing and there was a strong need for leadership and bold direction. Academics, community-based hospitalists, pediatricians, entrepreneurs, nonphysician hospital team members, heads of organized medicine, and government and industry leaders were just some of the key stakeholders looking for a seat at the HM table. That table would go on to be set for some 2 decades by Larry Wellikson.
From the beginning, many observers remarked that SHM had established an aggressive agenda. There was an unrelenting need to erect a big tent as a home for diverse stakeholders. John and I and the SHM board were doing all we could to continue to build momentum while also leading our local hospitalist groups and trying to maintain a semblance of balance with our young families back home.
It was against this backdrop, in late 1999, while on yet another flight crisscrossing the country to promote HM and SHM, that John; Bob Wachter, MD (who had by that time replaced John and I as SHM president); and I decided we needed a full-time CEO. By that time, each of us had participated in conversations with Larry. We rapidly decided, with buy-in from the board, that we would offer Larry the position. He accepted and became CEO in January 2000.
To list here all of Larry’s accomplishments since taking the helm at SHM would be impossible. Indeed, all that SHM has achieved is closely tied to Larry. Instead, I would like to call out character traits Larry brought to SHM that are now part of SHM’s DNA and a large part of the reason SHM has been so successful over the past 20 years.
Solution oriented. SHM’s culture has always been to take conditions as they are and work to make things better. There is no place for excessively airing grievances and complaining about “what is being done to us.”
Eschewing the status quo. We can do better. There is too much that needs to be done to wait.
Appropriately irreverent of the norms of the medical establishment. Physicians are by nature careful, plodding, considered, cautious, and methodical. The velocity of change in HM called for a different approach in order to be relevant, one better characterized as the move-fast-and-break-things ethos of a Silicon Valley startup.
Bringing diverse stakeholders to the table. A signature move has been to assemble influential people to lay out the issues before setting a course of action.
Strong bias to action. There is a time to analyze and discuss, but all of this ultimately is in service of taking action to achieve a tangible result.
Working to achieve consensus to a point, then moving forward. Considerable resources have been put into bringing stakeholders together, studying problems, and gaining a common understanding of issues. But this has never been at the expense of taking bold action, even if controversial at times.
Involving industry in creative ways to the benefit of patients. SHM pioneered an approach to use resources gained through industry partnerships to perform national scale improvement activities with groups of hospitalist mentor-experts working with local teams to make care more reliable for patients.
Tirelessly connecting to frontline hospitalists. The lifeblood of SHM is frontline hospitalists. Larry has taken the time to develop relationships with as many as possible, often through personally visiting their communities.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn., and cofounder and past president of SHM.
Dynamism
By John Nelson, MD, MHM
You probably know a few people with a magnetic personality. Larry Wellikson is the neodymium variety. Boundless energy, confidence that he has the answer or knows exactly where to find it, and ability to instantly recall every conversation he’s had with you, are traits that have energized his years leading SHM and have led countless people to regard him as friend and mentor.
Watch him at the SHM annual conference. There he goes, fast walking to his next commitment while facing backward to complete from a growing distance the conversation with a person he just bumped into along the way. It is like this for Larry from 6 a.m. until midnight. Like Alexander Hamilton, “the man is nonstop.”
Bill Campbell was the “Trillion Dollar Coach” who had his own success as a business leader, but is best known for mentoring Steve Jobs, the Google founders, and many others who went on to become titans of tech. Larry is hospital medicine’s “Coach,” and has inspired and guided the careers of so many clinicians, administrators, and entrepreneurs in hospital medicine and health care more broadly.
The biggest difference between these two highly effective leaders and mentors might be money; SHM has paid him pretty well, but alas, no stock options.
Larry is a great storyteller, and it doesn’t take long for a conversation with him to arrive at the point where he cites the example of how issues faced by someone else have parallels to your situation, the advice he gave that person, and how things turned out. Mostly this advice is about navigating professional life, but he is also happy to share wisdom about parenting, marriage, money, and sports. And most any other topic.
Larry was very accomplished even prior to connecting with SHM. He had a thriving clinical career, and though he left practice long ago he has maintained a close connection with many people he first met when they were his patients. I was surprised years ago when he drove up a new top-of-the-line Lexus – the two-seater with the solid convertible roof that folded into the trunk with the push of a button. I expressed surprise that he’d buy such a swanky car and he explained that a former patient, now long-time friend, was a Lexus distributor and arranged for Larry to drive it away for something like the cost of a Camry.
He also had terrific success forming and leading a large California independent physician association prior to connecting with SHM. Just ask him to show you the magazine with him on the cover and a glowing article detailing his accomplishments. Seriously, ask him, there’s a good chance he’ll have a copy with him.
When Dr. Win Whitcomb and I were trying to figure out how to start a new medical society and position our field to mature into a real specialty we were lucky enough to connect with many health care leaders who we thought could help. Most tended to pat us on the shoulder and say something along the lines of “good luck with your little hobby, now I have to get back to my important work.” But here was Larry with his impressive resume, having served as one of the leaders who crafted the merger of two giant medical societies (ACP and the American Society of Internal Medicine), keenly interested in our tiny new organization, and excited to serve as facilitator for our first strategic planning session.
SHM got a turbocharger when Larry signed on. For me it has felt like speeding down a highway, top down, radio blasting great music, and happy anticipation of what is around the next corner. I have never been disappointed, and certainly don’t plan to get out of Larry’s car just because he’s retiring as CEO.
Dr. Nelson is cofounder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants in La Quinta, Calif.
The SHM 2019 Chapter Excellence Awards
The Society of Hospital Medicine is proud to recognize its chapters for their hard work and dedication in 2019 through Chapter Excellence Awards. Each year, chapters strive to demonstrate growth, sustenance, and innovation within their chapter activities, which are then applauded for their successes throughout the subsequent year. In 2019, a new Bronze category was established, for a total of four Status Awards that chapters can earn.
Please join SHM in congratulating the following chapters on their year of success in 2019!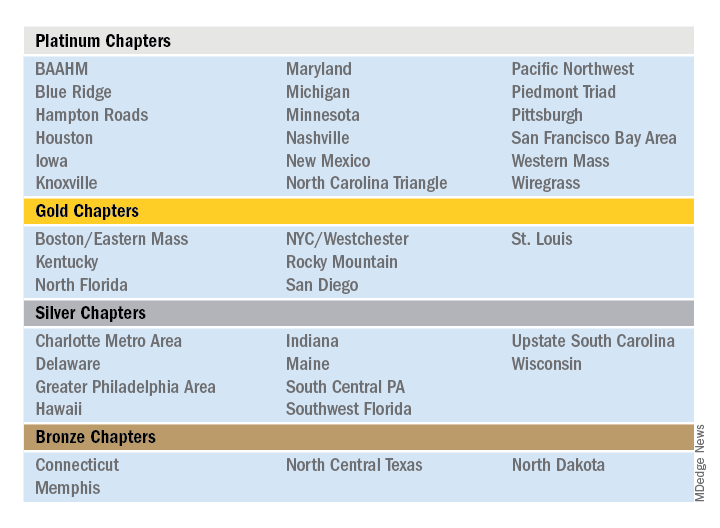
Outstanding Chapter of the Year
The Outstanding Chapter of the Year Award goes to one chapter who exemplifies high performance, going above and beyond the basic chapter requirements. The recipient of the Outstanding Chapter of the Year Award for 2019 is the Wiregrass Chapter of SHM. The chapter has a strong and engaged leadership which includes representation at all levels of the hospital medicine team, including physician hospitalists, advanced care provider hospitalists, practice administrators, nurses, residents, and medical students.
In the last year, the Wiregrass leadership team has organized programs and events to cater to and engage all the chapter’s members. This includes a variety of innovative ideas that catered toward medical education, health care provider well-being, engagement, mentorship, and community involvement.
The SHM Wiregrass Chapter’s biggest accomplishment in 2019 was the creation of an exchange program for physician and advanced practice provider hospitalists between the SHM New Mexico Chapter and the SHM Wiregrass Chapter. This idea first arose at HM19, where the chapter leaders had met during a networking event and debated the role of clinician wellbeing, quality of medical education, and faculty development to individual hospital medicine group (HMG) practice styles.
Clinician well-being is the prerequisite to the triple aim of improving the health of populations, enhancing the patient experience, and reducing the cost of care. Each HMG faces similar challenges but approaches to solving them vary. Professional challenges can affect the well-being of the individual clinicians. Having interinstitutional exchange programs provides a platform to exchange ideas and establish mentors. Also, the quality of medical education is directly linked to the quality of faculty development. Improving the quality of medical education requires a multifaceted approach by highly developed faculty. The complex factors affecting medical education and faculty development are further complicated by geographic location, patient characteristics, and professional growth opportunities. Overcoming these obstacles requires an innovative and collaborative approach. Although faculty exchanges are common in academic medicine, they are not commonly attempted with HMGs.
Hospitalists are responsible for a significant part of inpatient training for residents, medical students, and nurse practitioners/physician assistants (NPs/PAs), but their faculty training can vary based on location. Being a young specialty, only 2 decades old, hospital medicine is still evolving and incorporating NP/PA and physician hospitalists in varied practice models. Each HMG addresses common obstacles differently based on their culture and practice styles. The chapter leaders determined an exchange program would afford the opportunity for visiting faculty members to experience these differences. This emphasized the role and importance of exchanging ideas and contemplated a solution to benefit more practicing hospitalists.
The chapter leaders researched the characteristics of individual academic HMGs and structured a tailored faculty exchange involving physicians and NPs/PAs. During the exchange program planning, the visiting faculty itinerary was tailored to a well-planned agenda for 1 week, with separate tracks for physicians and NPs/PAs giving increased access to their individual peer practice styles. Additionally, the visiting faculty had meetings and discussions with HMG and hospital leadership, to specifically address each visiting faculty institution’s challenges. The overall goal of this exchange program was to promote cross-institutional collaboration, increase engagement, improve medical education through faculty development, and improve the quality of care. The focus of the exchange program was to share ideas and innovation and learn the approaches to unique challenges at each institution. Out of this also came collaboration and mentoring opportunities.
The evaluation process of the exchange involved interviews, a survey, and the establishment of shared QI projects in mutual areas of challenge. The survey provided feedback, lessons learned from the exchange, and areas to be improved. Collaborative QI projects currently underway as a result of the exchange include paging etiquette, quality of sleep for hospitalized patients, and onboarding of NPs/PAs in HMGs.
This innovation addressed faculty development and medical education via clinician well-being. The physician and NP/PA Faculty Exchange was an essential and meaningful innovation that resulted in increased SHM member engagement, cross-institutional collaboration, networking, and mentorship.
Additional projects that the SHM Wiregrass Chapter successfully implemented in 2019 include a “Women in Medicine” event that recognized women physician and advanced practice provider hospitalist leaders, a poster competition that expanded its research, clinical vignettes, and quality categories to include a fourth category of innovation, featuring 75 posters. Additionally, the chapter held a policy meeting with six Alabama state legislators, creating new channels of collaboration between the legislators and the chapter. Lastly, the chapter held a successful community event and launched a mentor program targeting medical students and residents.
Rising Star Chapter
The Rising Star Chapter Award goes to one chapter who has been active for 2 years or less, who in the past 12 months have made improvements to their leadership, stability and growth, and membership. The recipient of the Rising Star Chapter Award for 2019 is the Blue Ridge Chapter of SHM, which has made significant strides to develop since its launch in the fall of 2018. The chapter represents counties in northwest Tennessee, southwest Virginia, and western North Carolina.
The chapter held three meetings in 2019 which were well attended by hospitalists, residents/fellows, administrators, advanced practice providers, and nurses. On average, attendees from five to six different hospitalist groups are represented. The chapter hosted both Dr. Chris Frost, immediate past president of the SHM board of directors, and Dr. Ron Greeno, a past president of the SHM board of directors.
The SHM Blue Ridge Chapter has collaborated with both the ACP Tennessee Chapter and the Healthcare MBA program at Haslam College of Business at the University of Tennessee.
The chapter leadership regularly attends local medical residency programs at noon conferences to attract and recruit young physicians into chapter activities. Overall, the chapter has seen a growth in membership in 2019. The Blue Ridge Chapter is an active, enthusiastic chapter that is rapidly growing and thriving.
Outstanding Membership Recruitment and Retention
The Outstanding Membership Recruitment and Retention Award is a new exemplary award for 2019 that goes to one chapter who has gone above and beyond to implement initiatives to recruit and retain SHM members in their chapter. The recipient of the Outstanding Membership Recruitment and Retention Award for 2019 is the Western Massachusetts Chapter of SHM, which has done outstanding work to recruit and retain the membership. In 2019, the SHM membership in the chapter grew by 24%. The chapter utilized Chapter Development Funds to launch new initiatives to conduct outreach to nonmember hospitalists in the community and invite them to meetings to obtain the SHM experience. Additionally, the chapter encouraged residents to join and get involved by hosting a poster competition.
The Western Massachusetts Chapter focused on being innovative, inclusive, and creative to retain their existing meetings. For example, the chapter hosted a new “Jeopardy Session” event that featured a nontraditional jeopardy game that attracted a large attendance including local residents. Additionally, the chapter insured that all clinical and nonclinical members of the hospital medicine team were included and encouraged to participate in all chapter meetings. Lastly, the chapter launched a local awards program to recognize senior hospitalist and early career hospitalist who contributed to chapter development.
Most Engaged Chapter Leader
The Most Engaged Chapter Leader Award is a new exemplary award for 2019 that goes to one chapter leader or district chair who is either nominated or self-nominated and has demonstrated how they or their nominee has gone above and beyond in the past year to grow and sustain their chapter and/or district and continues to carry out the SHM mission. The recipient of the Most Engaged Chapter Leader Award for 2019 goes to Thérèse Franco, MD, SFHM, president of the Pacific Northwest Chapter.
Dr. Franco has served as the chapter’s president for 2 years and has served on the SHM Chapter Support Committee for 3 years. She has previously participated as a mentor in the glycemic control mentored implementation program, and as chair and cochair of the RIV contest. She continues to review abstracts, volunteer as a judge and offer local education on glycemic control through the Washington State Hospital Association, promoting SHM’s work there. One of Dr. Franco’s core strengths has been effective collaboration with past leaders (such as Rachel Thompson, MD, and Kimberly Bell, MD), future leaders, and other organizations (such as the Washington State Medical Association and the King County Medical Association). Dr. Franco has recruited an outstanding leadership team and new advisory committee for the Pacific Northwest Chapter, resulting a fantastic year of growth, innovation, and development.
The Society of Hospital Medicine is proud to recognize its chapters for their hard work and dedication in 2019 through Chapter Excellence Awards. Each year, chapters strive to demonstrate growth, sustenance, and innovation within their chapter activities, which are then applauded for their successes throughout the subsequent year. In 2019, a new Bronze category was established, for a total of four Status Awards that chapters can earn.
Please join SHM in congratulating the following chapters on their year of success in 2019!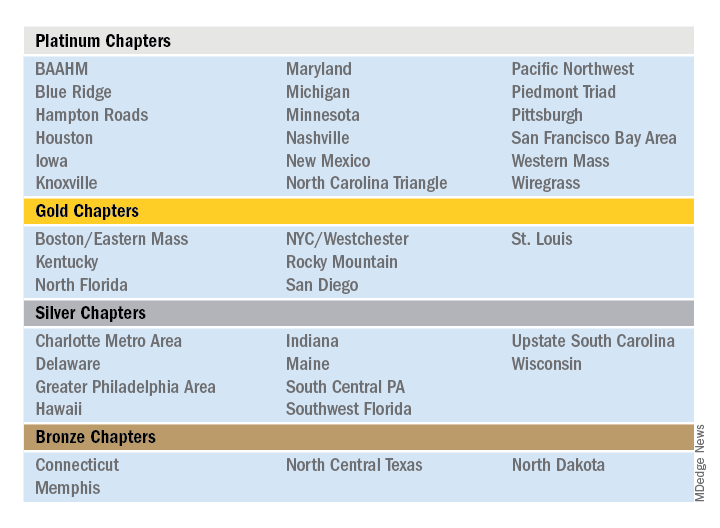
Outstanding Chapter of the Year
The Outstanding Chapter of the Year Award goes to one chapter who exemplifies high performance, going above and beyond the basic chapter requirements. The recipient of the Outstanding Chapter of the Year Award for 2019 is the Wiregrass Chapter of SHM. The chapter has a strong and engaged leadership which includes representation at all levels of the hospital medicine team, including physician hospitalists, advanced care provider hospitalists, practice administrators, nurses, residents, and medical students.
In the last year, the Wiregrass leadership team has organized programs and events to cater to and engage all the chapter’s members. This includes a variety of innovative ideas that catered toward medical education, health care provider well-being, engagement, mentorship, and community involvement.
The SHM Wiregrass Chapter’s biggest accomplishment in 2019 was the creation of an exchange program for physician and advanced practice provider hospitalists between the SHM New Mexico Chapter and the SHM Wiregrass Chapter. This idea first arose at HM19, where the chapter leaders had met during a networking event and debated the role of clinician wellbeing, quality of medical education, and faculty development to individual hospital medicine group (HMG) practice styles.
Clinician well-being is the prerequisite to the triple aim of improving the health of populations, enhancing the patient experience, and reducing the cost of care. Each HMG faces similar challenges but approaches to solving them vary. Professional challenges can affect the well-being of the individual clinicians. Having interinstitutional exchange programs provides a platform to exchange ideas and establish mentors. Also, the quality of medical education is directly linked to the quality of faculty development. Improving the quality of medical education requires a multifaceted approach by highly developed faculty. The complex factors affecting medical education and faculty development are further complicated by geographic location, patient characteristics, and professional growth opportunities. Overcoming these obstacles requires an innovative and collaborative approach. Although faculty exchanges are common in academic medicine, they are not commonly attempted with HMGs.
Hospitalists are responsible for a significant part of inpatient training for residents, medical students, and nurse practitioners/physician assistants (NPs/PAs), but their faculty training can vary based on location. Being a young specialty, only 2 decades old, hospital medicine is still evolving and incorporating NP/PA and physician hospitalists in varied practice models. Each HMG addresses common obstacles differently based on their culture and practice styles. The chapter leaders determined an exchange program would afford the opportunity for visiting faculty members to experience these differences. This emphasized the role and importance of exchanging ideas and contemplated a solution to benefit more practicing hospitalists.
The chapter leaders researched the characteristics of individual academic HMGs and structured a tailored faculty exchange involving physicians and NPs/PAs. During the exchange program planning, the visiting faculty itinerary was tailored to a well-planned agenda for 1 week, with separate tracks for physicians and NPs/PAs giving increased access to their individual peer practice styles. Additionally, the visiting faculty had meetings and discussions with HMG and hospital leadership, to specifically address each visiting faculty institution’s challenges. The overall goal of this exchange program was to promote cross-institutional collaboration, increase engagement, improve medical education through faculty development, and improve the quality of care. The focus of the exchange program was to share ideas and innovation and learn the approaches to unique challenges at each institution. Out of this also came collaboration and mentoring opportunities.
The evaluation process of the exchange involved interviews, a survey, and the establishment of shared QI projects in mutual areas of challenge. The survey provided feedback, lessons learned from the exchange, and areas to be improved. Collaborative QI projects currently underway as a result of the exchange include paging etiquette, quality of sleep for hospitalized patients, and onboarding of NPs/PAs in HMGs.
This innovation addressed faculty development and medical education via clinician well-being. The physician and NP/PA Faculty Exchange was an essential and meaningful innovation that resulted in increased SHM member engagement, cross-institutional collaboration, networking, and mentorship.
Additional projects that the SHM Wiregrass Chapter successfully implemented in 2019 include a “Women in Medicine” event that recognized women physician and advanced practice provider hospitalist leaders, a poster competition that expanded its research, clinical vignettes, and quality categories to include a fourth category of innovation, featuring 75 posters. Additionally, the chapter held a policy meeting with six Alabama state legislators, creating new channels of collaboration between the legislators and the chapter. Lastly, the chapter held a successful community event and launched a mentor program targeting medical students and residents.
Rising Star Chapter
The Rising Star Chapter Award goes to one chapter who has been active for 2 years or less, who in the past 12 months have made improvements to their leadership, stability and growth, and membership. The recipient of the Rising Star Chapter Award for 2019 is the Blue Ridge Chapter of SHM, which has made significant strides to develop since its launch in the fall of 2018. The chapter represents counties in northwest Tennessee, southwest Virginia, and western North Carolina.
The chapter held three meetings in 2019 which were well attended by hospitalists, residents/fellows, administrators, advanced practice providers, and nurses. On average, attendees from five to six different hospitalist groups are represented. The chapter hosted both Dr. Chris Frost, immediate past president of the SHM board of directors, and Dr. Ron Greeno, a past president of the SHM board of directors.
The SHM Blue Ridge Chapter has collaborated with both the ACP Tennessee Chapter and the Healthcare MBA program at Haslam College of Business at the University of Tennessee.
The chapter leadership regularly attends local medical residency programs at noon conferences to attract and recruit young physicians into chapter activities. Overall, the chapter has seen a growth in membership in 2019. The Blue Ridge Chapter is an active, enthusiastic chapter that is rapidly growing and thriving.
Outstanding Membership Recruitment and Retention
The Outstanding Membership Recruitment and Retention Award is a new exemplary award for 2019 that goes to one chapter who has gone above and beyond to implement initiatives to recruit and retain SHM members in their chapter. The recipient of the Outstanding Membership Recruitment and Retention Award for 2019 is the Western Massachusetts Chapter of SHM, which has done outstanding work to recruit and retain the membership. In 2019, the SHM membership in the chapter grew by 24%. The chapter utilized Chapter Development Funds to launch new initiatives to conduct outreach to nonmember hospitalists in the community and invite them to meetings to obtain the SHM experience. Additionally, the chapter encouraged residents to join and get involved by hosting a poster competition.
The Western Massachusetts Chapter focused on being innovative, inclusive, and creative to retain their existing meetings. For example, the chapter hosted a new “Jeopardy Session” event that featured a nontraditional jeopardy game that attracted a large attendance including local residents. Additionally, the chapter insured that all clinical and nonclinical members of the hospital medicine team were included and encouraged to participate in all chapter meetings. Lastly, the chapter launched a local awards program to recognize senior hospitalist and early career hospitalist who contributed to chapter development.
Most Engaged Chapter Leader
The Most Engaged Chapter Leader Award is a new exemplary award for 2019 that goes to one chapter leader or district chair who is either nominated or self-nominated and has demonstrated how they or their nominee has gone above and beyond in the past year to grow and sustain their chapter and/or district and continues to carry out the SHM mission. The recipient of the Most Engaged Chapter Leader Award for 2019 goes to Thérèse Franco, MD, SFHM, president of the Pacific Northwest Chapter.
Dr. Franco has served as the chapter’s president for 2 years and has served on the SHM Chapter Support Committee for 3 years. She has previously participated as a mentor in the glycemic control mentored implementation program, and as chair and cochair of the RIV contest. She continues to review abstracts, volunteer as a judge and offer local education on glycemic control through the Washington State Hospital Association, promoting SHM’s work there. One of Dr. Franco’s core strengths has been effective collaboration with past leaders (such as Rachel Thompson, MD, and Kimberly Bell, MD), future leaders, and other organizations (such as the Washington State Medical Association and the King County Medical Association). Dr. Franco has recruited an outstanding leadership team and new advisory committee for the Pacific Northwest Chapter, resulting a fantastic year of growth, innovation, and development.
The Society of Hospital Medicine is proud to recognize its chapters for their hard work and dedication in 2019 through Chapter Excellence Awards. Each year, chapters strive to demonstrate growth, sustenance, and innovation within their chapter activities, which are then applauded for their successes throughout the subsequent year. In 2019, a new Bronze category was established, for a total of four Status Awards that chapters can earn.
Please join SHM in congratulating the following chapters on their year of success in 2019!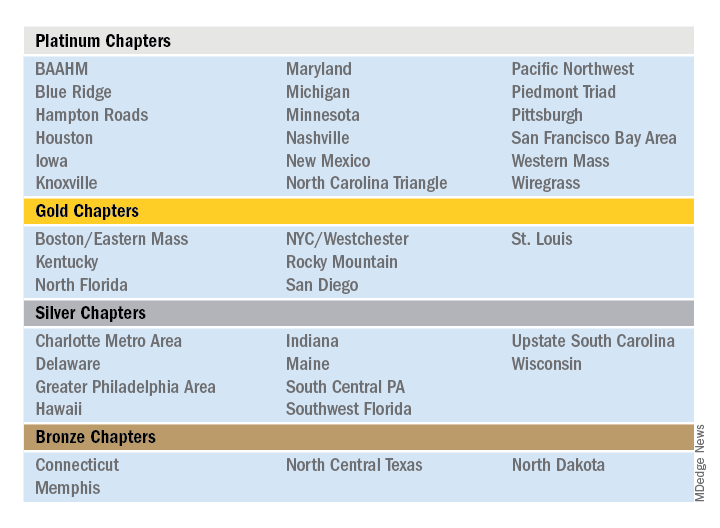
Outstanding Chapter of the Year
The Outstanding Chapter of the Year Award goes to one chapter who exemplifies high performance, going above and beyond the basic chapter requirements. The recipient of the Outstanding Chapter of the Year Award for 2019 is the Wiregrass Chapter of SHM. The chapter has a strong and engaged leadership which includes representation at all levels of the hospital medicine team, including physician hospitalists, advanced care provider hospitalists, practice administrators, nurses, residents, and medical students.
In the last year, the Wiregrass leadership team has organized programs and events to cater to and engage all the chapter’s members. This includes a variety of innovative ideas that catered toward medical education, health care provider well-being, engagement, mentorship, and community involvement.
The SHM Wiregrass Chapter’s biggest accomplishment in 2019 was the creation of an exchange program for physician and advanced practice provider hospitalists between the SHM New Mexico Chapter and the SHM Wiregrass Chapter. This idea first arose at HM19, where the chapter leaders had met during a networking event and debated the role of clinician wellbeing, quality of medical education, and faculty development to individual hospital medicine group (HMG) practice styles.
Clinician well-being is the prerequisite to the triple aim of improving the health of populations, enhancing the patient experience, and reducing the cost of care. Each HMG faces similar challenges but approaches to solving them vary. Professional challenges can affect the well-being of the individual clinicians. Having interinstitutional exchange programs provides a platform to exchange ideas and establish mentors. Also, the quality of medical education is directly linked to the quality of faculty development. Improving the quality of medical education requires a multifaceted approach by highly developed faculty. The complex factors affecting medical education and faculty development are further complicated by geographic location, patient characteristics, and professional growth opportunities. Overcoming these obstacles requires an innovative and collaborative approach. Although faculty exchanges are common in academic medicine, they are not commonly attempted with HMGs.
Hospitalists are responsible for a significant part of inpatient training for residents, medical students, and nurse practitioners/physician assistants (NPs/PAs), but their faculty training can vary based on location. Being a young specialty, only 2 decades old, hospital medicine is still evolving and incorporating NP/PA and physician hospitalists in varied practice models. Each HMG addresses common obstacles differently based on their culture and practice styles. The chapter leaders determined an exchange program would afford the opportunity for visiting faculty members to experience these differences. This emphasized the role and importance of exchanging ideas and contemplated a solution to benefit more practicing hospitalists.
The chapter leaders researched the characteristics of individual academic HMGs and structured a tailored faculty exchange involving physicians and NPs/PAs. During the exchange program planning, the visiting faculty itinerary was tailored to a well-planned agenda for 1 week, with separate tracks for physicians and NPs/PAs giving increased access to their individual peer practice styles. Additionally, the visiting faculty had meetings and discussions with HMG and hospital leadership, to specifically address each visiting faculty institution’s challenges. The overall goal of this exchange program was to promote cross-institutional collaboration, increase engagement, improve medical education through faculty development, and improve the quality of care. The focus of the exchange program was to share ideas and innovation and learn the approaches to unique challenges at each institution. Out of this also came collaboration and mentoring opportunities.
The evaluation process of the exchange involved interviews, a survey, and the establishment of shared QI projects in mutual areas of challenge. The survey provided feedback, lessons learned from the exchange, and areas to be improved. Collaborative QI projects currently underway as a result of the exchange include paging etiquette, quality of sleep for hospitalized patients, and onboarding of NPs/PAs in HMGs.
This innovation addressed faculty development and medical education via clinician well-being. The physician and NP/PA Faculty Exchange was an essential and meaningful innovation that resulted in increased SHM member engagement, cross-institutional collaboration, networking, and mentorship.
Additional projects that the SHM Wiregrass Chapter successfully implemented in 2019 include a “Women in Medicine” event that recognized women physician and advanced practice provider hospitalist leaders, a poster competition that expanded its research, clinical vignettes, and quality categories to include a fourth category of innovation, featuring 75 posters. Additionally, the chapter held a policy meeting with six Alabama state legislators, creating new channels of collaboration between the legislators and the chapter. Lastly, the chapter held a successful community event and launched a mentor program targeting medical students and residents.
Rising Star Chapter
The Rising Star Chapter Award goes to one chapter who has been active for 2 years or less, who in the past 12 months have made improvements to their leadership, stability and growth, and membership. The recipient of the Rising Star Chapter Award for 2019 is the Blue Ridge Chapter of SHM, which has made significant strides to develop since its launch in the fall of 2018. The chapter represents counties in northwest Tennessee, southwest Virginia, and western North Carolina.
The chapter held three meetings in 2019 which were well attended by hospitalists, residents/fellows, administrators, advanced practice providers, and nurses. On average, attendees from five to six different hospitalist groups are represented. The chapter hosted both Dr. Chris Frost, immediate past president of the SHM board of directors, and Dr. Ron Greeno, a past president of the SHM board of directors.
The SHM Blue Ridge Chapter has collaborated with both the ACP Tennessee Chapter and the Healthcare MBA program at Haslam College of Business at the University of Tennessee.
The chapter leadership regularly attends local medical residency programs at noon conferences to attract and recruit young physicians into chapter activities. Overall, the chapter has seen a growth in membership in 2019. The Blue Ridge Chapter is an active, enthusiastic chapter that is rapidly growing and thriving.
Outstanding Membership Recruitment and Retention
The Outstanding Membership Recruitment and Retention Award is a new exemplary award for 2019 that goes to one chapter who has gone above and beyond to implement initiatives to recruit and retain SHM members in their chapter. The recipient of the Outstanding Membership Recruitment and Retention Award for 2019 is the Western Massachusetts Chapter of SHM, which has done outstanding work to recruit and retain the membership. In 2019, the SHM membership in the chapter grew by 24%. The chapter utilized Chapter Development Funds to launch new initiatives to conduct outreach to nonmember hospitalists in the community and invite them to meetings to obtain the SHM experience. Additionally, the chapter encouraged residents to join and get involved by hosting a poster competition.
The Western Massachusetts Chapter focused on being innovative, inclusive, and creative to retain their existing meetings. For example, the chapter hosted a new “Jeopardy Session” event that featured a nontraditional jeopardy game that attracted a large attendance including local residents. Additionally, the chapter insured that all clinical and nonclinical members of the hospital medicine team were included and encouraged to participate in all chapter meetings. Lastly, the chapter launched a local awards program to recognize senior hospitalist and early career hospitalist who contributed to chapter development.
Most Engaged Chapter Leader
The Most Engaged Chapter Leader Award is a new exemplary award for 2019 that goes to one chapter leader or district chair who is either nominated or self-nominated and has demonstrated how they or their nominee has gone above and beyond in the past year to grow and sustain their chapter and/or district and continues to carry out the SHM mission. The recipient of the Most Engaged Chapter Leader Award for 2019 goes to Thérèse Franco, MD, SFHM, president of the Pacific Northwest Chapter.
Dr. Franco has served as the chapter’s president for 2 years and has served on the SHM Chapter Support Committee for 3 years. She has previously participated as a mentor in the glycemic control mentored implementation program, and as chair and cochair of the RIV contest. She continues to review abstracts, volunteer as a judge and offer local education on glycemic control through the Washington State Hospital Association, promoting SHM’s work there. One of Dr. Franco’s core strengths has been effective collaboration with past leaders (such as Rachel Thompson, MD, and Kimberly Bell, MD), future leaders, and other organizations (such as the Washington State Medical Association and the King County Medical Association). Dr. Franco has recruited an outstanding leadership team and new advisory committee for the Pacific Northwest Chapter, resulting a fantastic year of growth, innovation, and development.
Presenting the 2020 SHM Award of Excellence winners
Outstanding Service in Hospital Medicine
Efren Manjarrez, MD, SFHM, FACP, is an associate professor of clinical medicine at the University of Miami Miller School of Medicine, where he also serves as a hospitalist in the division of hospital medicine. His high-impact work at his home institution and through SHM has been extensive.
He founded the division of hospital medicine at the University of Miami in 2000 and later served as the division chief and patient safety officer. Dr. Manjarrez served in the prestigious role of course director for HM15 and as co-course director for the Adult Hospital Medicine Boot Camp.
One of his most enduring contributions is as an author of the white paper on hospitalist handoffs, published in the Journal of Hospital Medicine in 2009, which continues to be cited and validated. He was an assistant editor for the Journal of Hospital Medicine and continues to review articles for JHM. Dr. Manjarrez is also a senior fellow in hospital medicine.
Excellence in Research
Shoshana J. Herzig, MD, MPH, is the director of hospital medicine research at Beth Israel Deaconess Medical Center in Boston, where she also serves as a hospitalist. She is also an associate professor of medicine at Harvard Medical School, also in Boston.
She has published nearly 50 original peer-reviewed manuscripts in some of medicine’s top journals. Her impressive research, which primarily focuses on patterns of medication utilization and associated outcomes in hospitalized adults, has been cited more than 1,500 times in the medical literature.
In addition to her work on medication safety, she is also a site PI for the Hospital Medicine Research Network (HOMERuN), a nationwide collaborative of hospital medicine researchers.
Dr. Herzig has been a member of SHM since 2008 and has attended the annual conference every year since. She has served as an RIV abstract judge, was instrumental in developing SHM’s consensus statement on safe opioid prescribing, and has served as an editor for the Journal of Hospital Medicine since 2012 and has been a senior deputy editor since 2015.
Clinical Leadership for Physicians
Karen Smith, MD, MEd, SFHM, is the chief of the division of hospitalist medicine and past president of the medical staff at Children’s National Medical Center in Washington. She also serves as associate professor of pediatrics at the George Washington University School of Medicine. She has consistently worked to create a supportive environment in which to promote wellness among her staff and colleagues.
She was one of three founding faculty members of the division of hospital medicine at Children’s National, and under her leadership, the division has seen substantial growth. It has evolved from a single site to a comprehensive model of services, spanning six community hospitals and a specialty hospital for rehabilitation and subacute care.
To increase morale, Dr. Smith spearheaded the development of a virtual physician lounge. She reserved a conference room once a month and provided free lunch to medical staff members of different specialties. Its success led to the construction of a full-time lounge – all because of Dr. Smith’s perseverance and forward thinking.
She is a past member of SHM’s Pediatrics Committee and Hospital Quality and Patient Safety Committee and is a senior fellow in hospital medicine.
Excellence in Teaching
Kathleen M. Finn, MD, M.Phil, SFHM, is the senior associate program director for resident and faculty development in the Massachusetts General Hospital internal medicine residency program at Harvard Medical School, both in Boston, where she also is an assistant professor of medicine. She has excelled at teaching at all levels and in all kinds of settings, from clinical teaching on inpatient rounds, educating faculty through workshops to serving as course director for Hospital Medicine 2018 in Orlando. She constantly strives to think creatively and to teach in new ways and considers her career to be a synergy of all three domains in medical education: clinical teaching, leadership, and research.
Her interest in improving the art of inpatient teaching has also taken Dr. Finn into the medical education research space, where she has conducted and published several significant studies.
She was the codirector of the Boston chapter of SHM for 18 years and is well known for her dedication to SHM’s annual conference. She gained a reputation on the Annual Conference Committee for coming up with creative topics, including the Great Debate series.
Dr. Finn has previously served on the editorial board for the Journal of Hospital Medicine, where she continues to be a reviewer. She is a senior fellow in hospital medicine.
Excellence in Teaching
Juan Nicolás Lessing, MD, is an assistant professor of medicine within the division of hospital medicine at the Medical School at the University of Colorado at Denver, Aurora. He has dedicated himself to the teaching and study of clinical reasoning processes and has cocreated a resident clinical reasoning curriculum, which has been expended to all residency classes.
Dr. Lessing’s dedication to mentorship has been extraordinary. In fewer than 5 years, he has mentored more than 50 learners, resulting in 54 competitive abstracts, posters, and presentations. He has led more than 24 workshops and consistently sponsors junior colleagues to join him. In summary, he teaches learners how to learn rather than what to learn. Additionally, Dr. Lessing created and facilitated several impactful department-wide sessions on how we can learn from our mistakes to openly discuss missed diagnoses. He served as a co-PI on the LOOP study, a multicenter endeavor to provide real-time feedback to admitting residents on a patient’s clinical course, which was published in the Journal of Hospital Medicine.
Dr. Lessing has been actively involved with SHM since medical school, is a graduate of SHM’s Academic Hospitalist Academy, and serves on the executive board for the Rocky Mountain chapter of SHM.
Clinical Leadership for NPs/PAs
Ilaria Gadalla, DMSc, PA-C, is a hospitalist at Treasure Coast Hospitalists in Port St. Lucia, Fla., and also serves as the physician assistant department chair/program director at South University, where she supervises more than 40 PAs, medical directors, and administrative staff.
She continuously drives innovative projects for NPs and PAs to demonstrate excellence in collaboration by working closely with C-suite administration to expand QI (quality improvement) and education efforts. A prime example is the optimal communication system that she developed within her first week as a hospitalist in the Port St. Lucie area. Nursing, ED, and pharmacy staff had difficulty contacting hospitalists since the EMR would not reflect the assigned hospitalist, so she developed a simple contact sheet that included the hospitalist team each day. This method is still in use today.
Ms. Gadalla is the chair of SHM’s NP/PA special interest group who was integral in drafting the recent white paper on NP/PA integration and optimization.
Excellence in Humanitarian Services
Khaalisha Ajala, MD, MBA, is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She cares for patients of diverse backgrounds directly and also has a deep-seeded passion for public health and patient education, always demonstrating how to bring this passion to trainee education.
Using her knowledge as an MBA, Dr. Ajala has designed, developed, and now maintains her own nonprofit agency, Heart Beats & Hip-Hop. Through this organization, she has hosted public health fairs to conduct health screenings in less-traditional local settings, where community members who may not have access to care can gain exposure to a health care provider.
More broadly, in the last year, she has made two journeys – one to Thailand and another to Ethiopia – to work with Emory trainees in educational and clinical efforts to help them engage the global community in health improvement. In Thailand, she taught students how to care for patients at risk for trafficking and sexual exploitation. While in Ethiopia, she served as an educator and clinical preceptor to Emory residents in the global health pathway, teaching them to care for high-risk patients at a local hospital.
With her active and unrelenting humanitarian efforts in mind, she was also chosen as a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
Diversity Leadership
Kimberly D. Manning, MD, FACP, FAAP, is a professor of medicine and the associate vice chair of diversity, equity and inclusion at the Emory University School of Medicine in Atlanta, where she also is a hospitalist at Grady Memorial Hospital. She demonstrates a strong passion for building and strengthening diverse clinical learning environments. This inspired her to promote cultural competency via lectures, curriculum development, and more.
Dr. Manning has designed a new educational modality – Bite-Sized Teaching (abbreviated “BST” and read as “BEAST”-Mode Teaching). This engages trainees as the teachers of their peers. As part of those sessions, Dr. Manning intentionally encourages and engages trainees from all backgrounds, including women, minorities, and trainees with varied ethnic and cultural perspectives.
Her leadership on the Emory Task Force on Diversity, Equity and Inclusion led her to be named the department of medicine’s first associate vice chair of diversity, equity and inclusion. Due in large part to her engagement, the medical school just admitted its largest class of underrepresented minorities, nearly doubling numbers from prior years.
She has received the 2018 AGCME Parker J. Palmer Courage to Teach Award and the 2019 Lifetime Achievement Award by the Association of Black Women Physicians.
Leadership for Practice Manager
Douglas G. Philpot, MHA, MBA, MHR, FACHE, currently the hospitalist program director at Intermountain Healthcare in Salt Lake City, epitomizes excellence in practice management.
In mid-2018, Intermountain Healthcare transitioned to a new organizational structure that brought all medical and surgical operations under one leadership team. Prior to this reorganization, hospitalist groups were largely divided by the geographies they served, each operating independently.
After the reorganization, it was apparent that staffing structures among groups varied greatly. Dr. Philpot pored over the workload and billing data and determined the most efficient use of how to staff hospitalist providers. He recently created a program that allows all stakeholders to meet and discuss in an unbiased manner how and when to add resources to a given group. As a result, the team is better able to make smart decisions that translate into improved quality, better patient experience, a more engaged hospitalist group and improved financial decisions. This is a model that Intermountain is now looking to apply to other specialties.
Team Award in Quality Improvement
The Michigan Hospital Medicine Safety Consortium has been in place for a decade and has worked together to improve quality and safety for patients across Michigan and the nation. It has been led since its inception by Scott Flanders, MD, a hospitalist at the University of Michigan, Ann Arbor.
At each participating hospital, teams include hospitalists, infectious disease clinicians, interventional radiologists, nephrologists, nurses, pharmacists, administrators, and more. This integration ensures that the team’s work is highly relevant and generalizable for hospitals around the country.
Their initiatives have informed regulatory and guideline writing authorities in the United States and beyond. For example, findings from their venous thromboembolism project demonstrated that the majority of hospitalized patients do not benefit from VTE prophylaxis, but rather, targeted strategies to define those at high risk. In 2016, their work helped to prevent 852 VTEs in Michigan alone. This led to changes in national guidelines that now emphasize deimplementing pharmacologic VTE prophylaxis and focused risk-assessment in U.S. hospitals.
Their antimicrobial use initiative has led to a robust partnership between hospitalists, hospitals, and national partners, such as the Centers for Disease Control and Prevention. Early work has informed a key gap in stewardship – discharge antibiotic prescribing – which has been a focus for SHM, the CDC, and many others. Efforts have already led to a reduction in thousands of unnecessary antibiotic prescriptions in Michigan.
Junior Investigator Award
SHM’s Research Committee presents the Junior Investigator Award to recognize early-career hospitalist researchers who are leading the way in their field. We are pleased to present the HM20 Junior Investigator Award to Valerie Vaughn, MD, MSc.
Dr. Vaughn is an assistant professor and research scientist in the division of hospital medicine at the University of Michigan and Veterans Affairs Ann Arbor Healthcare System.
Her research is focused on engaging hospitalists in antibiotic prescribing, especially at discharge. She is the hospitalist lead for an initiative to improve antibiotic prescribing in 46 hospitals across Michigan. She has already made a national contribution to the field – two manuscripts that have received high praise and have been cited by the Joint Commission and the CDC in their updated recommendations for antibiotic stewardship. She has a grant from the Gordon and Betty Moore Foundation to study the role of diagnostic error in antibiotic overuse and just received a K08 career development award from the Agency for Healthcare Research and Quality to study methods to improve antibiotic prescribing at hospital discharge.
One of Dr. Vaughn’s career goals is to advance hospital medicine through mentoring the next generation of hospitalists. In 2017, she authored a manuscript titled “Mentee Missteps” in JAMA, which has been viewed nearly 40,000 times since publication. She continues to give talks on this topic and mentors clinical hospitalists on research projects to improve quality and safety.
Dr. Vaughn has worked closely with SHM and represents the society at the CDC’s Healthcare Infection Control Practices Advisory Committee quarterly meetings.
Certificate of Leadership in Hospital Medicine
The Certificate of Leadership in Hospital Medicine (CLHM) cultivates leadership skills in the context of specific hospital medicine challenges. This designation informs employers – or potential employers – with confidence that a candidate is equipped and ready to lead teams and grow an organization.
Charmaine Lewis, MD, MPH, FHM, CLHM, is the quality director for New Hanover Hospitalists in Wilmington, N.C., a role she has held for 7 years. She is also clinical assistant professor, department of medicine, University of North Carolina School of Medicine, Chapel Hill, serving as a mentor for internal medicine, surgery, and obstetrics residents completing projects in quality improvement.
While sitting on the CHF and readmissions committees at her institution, Dr. Lewis was asked why patients with heart failure came back to the hospital. This question launched an in-depth search for real-time and accurate data on heart failure patients in her institution. She worked with the Heart Failure Steering Committee to develop a process to close care gaps and document compliance to the ACC/AHA Get with the Guidelines: Heart Failure recommendations. She facilitated order set revisions, smart-phrase documentation in EPIC, and scripted bedside interdisciplinary rounding to facilitate compliance prior to patient discharge. She also created an end-user friendly dashboard to report compliance with medical leaders, and eventually this project was selected by the department of medicine as their annual quality goal. The project has led to the improvement of CHF GWTG Composite Bundle compliance from 76% to 93%, and compliance with use of aldosterone antagonists from 22% to 85%.
Outstanding Service in Hospital Medicine
Efren Manjarrez, MD, SFHM, FACP, is an associate professor of clinical medicine at the University of Miami Miller School of Medicine, where he also serves as a hospitalist in the division of hospital medicine. His high-impact work at his home institution and through SHM has been extensive.
He founded the division of hospital medicine at the University of Miami in 2000 and later served as the division chief and patient safety officer. Dr. Manjarrez served in the prestigious role of course director for HM15 and as co-course director for the Adult Hospital Medicine Boot Camp.
One of his most enduring contributions is as an author of the white paper on hospitalist handoffs, published in the Journal of Hospital Medicine in 2009, which continues to be cited and validated. He was an assistant editor for the Journal of Hospital Medicine and continues to review articles for JHM. Dr. Manjarrez is also a senior fellow in hospital medicine.
Excellence in Research
Shoshana J. Herzig, MD, MPH, is the director of hospital medicine research at Beth Israel Deaconess Medical Center in Boston, where she also serves as a hospitalist. She is also an associate professor of medicine at Harvard Medical School, also in Boston.
She has published nearly 50 original peer-reviewed manuscripts in some of medicine’s top journals. Her impressive research, which primarily focuses on patterns of medication utilization and associated outcomes in hospitalized adults, has been cited more than 1,500 times in the medical literature.
In addition to her work on medication safety, she is also a site PI for the Hospital Medicine Research Network (HOMERuN), a nationwide collaborative of hospital medicine researchers.
Dr. Herzig has been a member of SHM since 2008 and has attended the annual conference every year since. She has served as an RIV abstract judge, was instrumental in developing SHM’s consensus statement on safe opioid prescribing, and has served as an editor for the Journal of Hospital Medicine since 2012 and has been a senior deputy editor since 2015.
Clinical Leadership for Physicians
Karen Smith, MD, MEd, SFHM, is the chief of the division of hospitalist medicine and past president of the medical staff at Children’s National Medical Center in Washington. She also serves as associate professor of pediatrics at the George Washington University School of Medicine. She has consistently worked to create a supportive environment in which to promote wellness among her staff and colleagues.
She was one of three founding faculty members of the division of hospital medicine at Children’s National, and under her leadership, the division has seen substantial growth. It has evolved from a single site to a comprehensive model of services, spanning six community hospitals and a specialty hospital for rehabilitation and subacute care.
To increase morale, Dr. Smith spearheaded the development of a virtual physician lounge. She reserved a conference room once a month and provided free lunch to medical staff members of different specialties. Its success led to the construction of a full-time lounge – all because of Dr. Smith’s perseverance and forward thinking.
She is a past member of SHM’s Pediatrics Committee and Hospital Quality and Patient Safety Committee and is a senior fellow in hospital medicine.
Excellence in Teaching
Kathleen M. Finn, MD, M.Phil, SFHM, is the senior associate program director for resident and faculty development in the Massachusetts General Hospital internal medicine residency program at Harvard Medical School, both in Boston, where she also is an assistant professor of medicine. She has excelled at teaching at all levels and in all kinds of settings, from clinical teaching on inpatient rounds, educating faculty through workshops to serving as course director for Hospital Medicine 2018 in Orlando. She constantly strives to think creatively and to teach in new ways and considers her career to be a synergy of all three domains in medical education: clinical teaching, leadership, and research.
Her interest in improving the art of inpatient teaching has also taken Dr. Finn into the medical education research space, where she has conducted and published several significant studies.
She was the codirector of the Boston chapter of SHM for 18 years and is well known for her dedication to SHM’s annual conference. She gained a reputation on the Annual Conference Committee for coming up with creative topics, including the Great Debate series.
Dr. Finn has previously served on the editorial board for the Journal of Hospital Medicine, where she continues to be a reviewer. She is a senior fellow in hospital medicine.
Excellence in Teaching
Juan Nicolás Lessing, MD, is an assistant professor of medicine within the division of hospital medicine at the Medical School at the University of Colorado at Denver, Aurora. He has dedicated himself to the teaching and study of clinical reasoning processes and has cocreated a resident clinical reasoning curriculum, which has been expended to all residency classes.
Dr. Lessing’s dedication to mentorship has been extraordinary. In fewer than 5 years, he has mentored more than 50 learners, resulting in 54 competitive abstracts, posters, and presentations. He has led more than 24 workshops and consistently sponsors junior colleagues to join him. In summary, he teaches learners how to learn rather than what to learn. Additionally, Dr. Lessing created and facilitated several impactful department-wide sessions on how we can learn from our mistakes to openly discuss missed diagnoses. He served as a co-PI on the LOOP study, a multicenter endeavor to provide real-time feedback to admitting residents on a patient’s clinical course, which was published in the Journal of Hospital Medicine.
Dr. Lessing has been actively involved with SHM since medical school, is a graduate of SHM’s Academic Hospitalist Academy, and serves on the executive board for the Rocky Mountain chapter of SHM.
Clinical Leadership for NPs/PAs
Ilaria Gadalla, DMSc, PA-C, is a hospitalist at Treasure Coast Hospitalists in Port St. Lucia, Fla., and also serves as the physician assistant department chair/program director at South University, where she supervises more than 40 PAs, medical directors, and administrative staff.
She continuously drives innovative projects for NPs and PAs to demonstrate excellence in collaboration by working closely with C-suite administration to expand QI (quality improvement) and education efforts. A prime example is the optimal communication system that she developed within her first week as a hospitalist in the Port St. Lucie area. Nursing, ED, and pharmacy staff had difficulty contacting hospitalists since the EMR would not reflect the assigned hospitalist, so she developed a simple contact sheet that included the hospitalist team each day. This method is still in use today.
Ms. Gadalla is the chair of SHM’s NP/PA special interest group who was integral in drafting the recent white paper on NP/PA integration and optimization.
Excellence in Humanitarian Services
Khaalisha Ajala, MD, MBA, is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She cares for patients of diverse backgrounds directly and also has a deep-seeded passion for public health and patient education, always demonstrating how to bring this passion to trainee education.
Using her knowledge as an MBA, Dr. Ajala has designed, developed, and now maintains her own nonprofit agency, Heart Beats & Hip-Hop. Through this organization, she has hosted public health fairs to conduct health screenings in less-traditional local settings, where community members who may not have access to care can gain exposure to a health care provider.
More broadly, in the last year, she has made two journeys – one to Thailand and another to Ethiopia – to work with Emory trainees in educational and clinical efforts to help them engage the global community in health improvement. In Thailand, she taught students how to care for patients at risk for trafficking and sexual exploitation. While in Ethiopia, she served as an educator and clinical preceptor to Emory residents in the global health pathway, teaching them to care for high-risk patients at a local hospital.
With her active and unrelenting humanitarian efforts in mind, she was also chosen as a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
Diversity Leadership
Kimberly D. Manning, MD, FACP, FAAP, is a professor of medicine and the associate vice chair of diversity, equity and inclusion at the Emory University School of Medicine in Atlanta, where she also is a hospitalist at Grady Memorial Hospital. She demonstrates a strong passion for building and strengthening diverse clinical learning environments. This inspired her to promote cultural competency via lectures, curriculum development, and more.
Dr. Manning has designed a new educational modality – Bite-Sized Teaching (abbreviated “BST” and read as “BEAST”-Mode Teaching). This engages trainees as the teachers of their peers. As part of those sessions, Dr. Manning intentionally encourages and engages trainees from all backgrounds, including women, minorities, and trainees with varied ethnic and cultural perspectives.
Her leadership on the Emory Task Force on Diversity, Equity and Inclusion led her to be named the department of medicine’s first associate vice chair of diversity, equity and inclusion. Due in large part to her engagement, the medical school just admitted its largest class of underrepresented minorities, nearly doubling numbers from prior years.
She has received the 2018 AGCME Parker J. Palmer Courage to Teach Award and the 2019 Lifetime Achievement Award by the Association of Black Women Physicians.
Leadership for Practice Manager
Douglas G. Philpot, MHA, MBA, MHR, FACHE, currently the hospitalist program director at Intermountain Healthcare in Salt Lake City, epitomizes excellence in practice management.
In mid-2018, Intermountain Healthcare transitioned to a new organizational structure that brought all medical and surgical operations under one leadership team. Prior to this reorganization, hospitalist groups were largely divided by the geographies they served, each operating independently.
After the reorganization, it was apparent that staffing structures among groups varied greatly. Dr. Philpot pored over the workload and billing data and determined the most efficient use of how to staff hospitalist providers. He recently created a program that allows all stakeholders to meet and discuss in an unbiased manner how and when to add resources to a given group. As a result, the team is better able to make smart decisions that translate into improved quality, better patient experience, a more engaged hospitalist group and improved financial decisions. This is a model that Intermountain is now looking to apply to other specialties.
Team Award in Quality Improvement
The Michigan Hospital Medicine Safety Consortium has been in place for a decade and has worked together to improve quality and safety for patients across Michigan and the nation. It has been led since its inception by Scott Flanders, MD, a hospitalist at the University of Michigan, Ann Arbor.
At each participating hospital, teams include hospitalists, infectious disease clinicians, interventional radiologists, nephrologists, nurses, pharmacists, administrators, and more. This integration ensures that the team’s work is highly relevant and generalizable for hospitals around the country.
Their initiatives have informed regulatory and guideline writing authorities in the United States and beyond. For example, findings from their venous thromboembolism project demonstrated that the majority of hospitalized patients do not benefit from VTE prophylaxis, but rather, targeted strategies to define those at high risk. In 2016, their work helped to prevent 852 VTEs in Michigan alone. This led to changes in national guidelines that now emphasize deimplementing pharmacologic VTE prophylaxis and focused risk-assessment in U.S. hospitals.
Their antimicrobial use initiative has led to a robust partnership between hospitalists, hospitals, and national partners, such as the Centers for Disease Control and Prevention. Early work has informed a key gap in stewardship – discharge antibiotic prescribing – which has been a focus for SHM, the CDC, and many others. Efforts have already led to a reduction in thousands of unnecessary antibiotic prescriptions in Michigan.
Junior Investigator Award
SHM’s Research Committee presents the Junior Investigator Award to recognize early-career hospitalist researchers who are leading the way in their field. We are pleased to present the HM20 Junior Investigator Award to Valerie Vaughn, MD, MSc.
Dr. Vaughn is an assistant professor and research scientist in the division of hospital medicine at the University of Michigan and Veterans Affairs Ann Arbor Healthcare System.
Her research is focused on engaging hospitalists in antibiotic prescribing, especially at discharge. She is the hospitalist lead for an initiative to improve antibiotic prescribing in 46 hospitals across Michigan. She has already made a national contribution to the field – two manuscripts that have received high praise and have been cited by the Joint Commission and the CDC in their updated recommendations for antibiotic stewardship. She has a grant from the Gordon and Betty Moore Foundation to study the role of diagnostic error in antibiotic overuse and just received a K08 career development award from the Agency for Healthcare Research and Quality to study methods to improve antibiotic prescribing at hospital discharge.
One of Dr. Vaughn’s career goals is to advance hospital medicine through mentoring the next generation of hospitalists. In 2017, she authored a manuscript titled “Mentee Missteps” in JAMA, which has been viewed nearly 40,000 times since publication. She continues to give talks on this topic and mentors clinical hospitalists on research projects to improve quality and safety.
Dr. Vaughn has worked closely with SHM and represents the society at the CDC’s Healthcare Infection Control Practices Advisory Committee quarterly meetings.
Certificate of Leadership in Hospital Medicine
The Certificate of Leadership in Hospital Medicine (CLHM) cultivates leadership skills in the context of specific hospital medicine challenges. This designation informs employers – or potential employers – with confidence that a candidate is equipped and ready to lead teams and grow an organization.
Charmaine Lewis, MD, MPH, FHM, CLHM, is the quality director for New Hanover Hospitalists in Wilmington, N.C., a role she has held for 7 years. She is also clinical assistant professor, department of medicine, University of North Carolina School of Medicine, Chapel Hill, serving as a mentor for internal medicine, surgery, and obstetrics residents completing projects in quality improvement.
While sitting on the CHF and readmissions committees at her institution, Dr. Lewis was asked why patients with heart failure came back to the hospital. This question launched an in-depth search for real-time and accurate data on heart failure patients in her institution. She worked with the Heart Failure Steering Committee to develop a process to close care gaps and document compliance to the ACC/AHA Get with the Guidelines: Heart Failure recommendations. She facilitated order set revisions, smart-phrase documentation in EPIC, and scripted bedside interdisciplinary rounding to facilitate compliance prior to patient discharge. She also created an end-user friendly dashboard to report compliance with medical leaders, and eventually this project was selected by the department of medicine as their annual quality goal. The project has led to the improvement of CHF GWTG Composite Bundle compliance from 76% to 93%, and compliance with use of aldosterone antagonists from 22% to 85%.
Outstanding Service in Hospital Medicine
Efren Manjarrez, MD, SFHM, FACP, is an associate professor of clinical medicine at the University of Miami Miller School of Medicine, where he also serves as a hospitalist in the division of hospital medicine. His high-impact work at his home institution and through SHM has been extensive.
He founded the division of hospital medicine at the University of Miami in 2000 and later served as the division chief and patient safety officer. Dr. Manjarrez served in the prestigious role of course director for HM15 and as co-course director for the Adult Hospital Medicine Boot Camp.
One of his most enduring contributions is as an author of the white paper on hospitalist handoffs, published in the Journal of Hospital Medicine in 2009, which continues to be cited and validated. He was an assistant editor for the Journal of Hospital Medicine and continues to review articles for JHM. Dr. Manjarrez is also a senior fellow in hospital medicine.
Excellence in Research
Shoshana J. Herzig, MD, MPH, is the director of hospital medicine research at Beth Israel Deaconess Medical Center in Boston, where she also serves as a hospitalist. She is also an associate professor of medicine at Harvard Medical School, also in Boston.
She has published nearly 50 original peer-reviewed manuscripts in some of medicine’s top journals. Her impressive research, which primarily focuses on patterns of medication utilization and associated outcomes in hospitalized adults, has been cited more than 1,500 times in the medical literature.
In addition to her work on medication safety, she is also a site PI for the Hospital Medicine Research Network (HOMERuN), a nationwide collaborative of hospital medicine researchers.
Dr. Herzig has been a member of SHM since 2008 and has attended the annual conference every year since. She has served as an RIV abstract judge, was instrumental in developing SHM’s consensus statement on safe opioid prescribing, and has served as an editor for the Journal of Hospital Medicine since 2012 and has been a senior deputy editor since 2015.
Clinical Leadership for Physicians
Karen Smith, MD, MEd, SFHM, is the chief of the division of hospitalist medicine and past president of the medical staff at Children’s National Medical Center in Washington. She also serves as associate professor of pediatrics at the George Washington University School of Medicine. She has consistently worked to create a supportive environment in which to promote wellness among her staff and colleagues.
She was one of three founding faculty members of the division of hospital medicine at Children’s National, and under her leadership, the division has seen substantial growth. It has evolved from a single site to a comprehensive model of services, spanning six community hospitals and a specialty hospital for rehabilitation and subacute care.
To increase morale, Dr. Smith spearheaded the development of a virtual physician lounge. She reserved a conference room once a month and provided free lunch to medical staff members of different specialties. Its success led to the construction of a full-time lounge – all because of Dr. Smith’s perseverance and forward thinking.
She is a past member of SHM’s Pediatrics Committee and Hospital Quality and Patient Safety Committee and is a senior fellow in hospital medicine.
Excellence in Teaching
Kathleen M. Finn, MD, M.Phil, SFHM, is the senior associate program director for resident and faculty development in the Massachusetts General Hospital internal medicine residency program at Harvard Medical School, both in Boston, where she also is an assistant professor of medicine. She has excelled at teaching at all levels and in all kinds of settings, from clinical teaching on inpatient rounds, educating faculty through workshops to serving as course director for Hospital Medicine 2018 in Orlando. She constantly strives to think creatively and to teach in new ways and considers her career to be a synergy of all three domains in medical education: clinical teaching, leadership, and research.
Her interest in improving the art of inpatient teaching has also taken Dr. Finn into the medical education research space, where she has conducted and published several significant studies.
She was the codirector of the Boston chapter of SHM for 18 years and is well known for her dedication to SHM’s annual conference. She gained a reputation on the Annual Conference Committee for coming up with creative topics, including the Great Debate series.
Dr. Finn has previously served on the editorial board for the Journal of Hospital Medicine, where she continues to be a reviewer. She is a senior fellow in hospital medicine.
Excellence in Teaching
Juan Nicolás Lessing, MD, is an assistant professor of medicine within the division of hospital medicine at the Medical School at the University of Colorado at Denver, Aurora. He has dedicated himself to the teaching and study of clinical reasoning processes and has cocreated a resident clinical reasoning curriculum, which has been expended to all residency classes.
Dr. Lessing’s dedication to mentorship has been extraordinary. In fewer than 5 years, he has mentored more than 50 learners, resulting in 54 competitive abstracts, posters, and presentations. He has led more than 24 workshops and consistently sponsors junior colleagues to join him. In summary, he teaches learners how to learn rather than what to learn. Additionally, Dr. Lessing created and facilitated several impactful department-wide sessions on how we can learn from our mistakes to openly discuss missed diagnoses. He served as a co-PI on the LOOP study, a multicenter endeavor to provide real-time feedback to admitting residents on a patient’s clinical course, which was published in the Journal of Hospital Medicine.
Dr. Lessing has been actively involved with SHM since medical school, is a graduate of SHM’s Academic Hospitalist Academy, and serves on the executive board for the Rocky Mountain chapter of SHM.
Clinical Leadership for NPs/PAs
Ilaria Gadalla, DMSc, PA-C, is a hospitalist at Treasure Coast Hospitalists in Port St. Lucia, Fla., and also serves as the physician assistant department chair/program director at South University, where she supervises more than 40 PAs, medical directors, and administrative staff.
She continuously drives innovative projects for NPs and PAs to demonstrate excellence in collaboration by working closely with C-suite administration to expand QI (quality improvement) and education efforts. A prime example is the optimal communication system that she developed within her first week as a hospitalist in the Port St. Lucie area. Nursing, ED, and pharmacy staff had difficulty contacting hospitalists since the EMR would not reflect the assigned hospitalist, so she developed a simple contact sheet that included the hospitalist team each day. This method is still in use today.
Ms. Gadalla is the chair of SHM’s NP/PA special interest group who was integral in drafting the recent white paper on NP/PA integration and optimization.
Excellence in Humanitarian Services
Khaalisha Ajala, MD, MBA, is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She cares for patients of diverse backgrounds directly and also has a deep-seeded passion for public health and patient education, always demonstrating how to bring this passion to trainee education.
Using her knowledge as an MBA, Dr. Ajala has designed, developed, and now maintains her own nonprofit agency, Heart Beats & Hip-Hop. Through this organization, she has hosted public health fairs to conduct health screenings in less-traditional local settings, where community members who may not have access to care can gain exposure to a health care provider.
More broadly, in the last year, she has made two journeys – one to Thailand and another to Ethiopia – to work with Emory trainees in educational and clinical efforts to help them engage the global community in health improvement. In Thailand, she taught students how to care for patients at risk for trafficking and sexual exploitation. While in Ethiopia, she served as an educator and clinical preceptor to Emory residents in the global health pathway, teaching them to care for high-risk patients at a local hospital.
With her active and unrelenting humanitarian efforts in mind, she was also chosen as a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
Diversity Leadership
Kimberly D. Manning, MD, FACP, FAAP, is a professor of medicine and the associate vice chair of diversity, equity and inclusion at the Emory University School of Medicine in Atlanta, where she also is a hospitalist at Grady Memorial Hospital. She demonstrates a strong passion for building and strengthening diverse clinical learning environments. This inspired her to promote cultural competency via lectures, curriculum development, and more.
Dr. Manning has designed a new educational modality – Bite-Sized Teaching (abbreviated “BST” and read as “BEAST”-Mode Teaching). This engages trainees as the teachers of their peers. As part of those sessions, Dr. Manning intentionally encourages and engages trainees from all backgrounds, including women, minorities, and trainees with varied ethnic and cultural perspectives.
Her leadership on the Emory Task Force on Diversity, Equity and Inclusion led her to be named the department of medicine’s first associate vice chair of diversity, equity and inclusion. Due in large part to her engagement, the medical school just admitted its largest class of underrepresented minorities, nearly doubling numbers from prior years.
She has received the 2018 AGCME Parker J. Palmer Courage to Teach Award and the 2019 Lifetime Achievement Award by the Association of Black Women Physicians.
Leadership for Practice Manager
Douglas G. Philpot, MHA, MBA, MHR, FACHE, currently the hospitalist program director at Intermountain Healthcare in Salt Lake City, epitomizes excellence in practice management.
In mid-2018, Intermountain Healthcare transitioned to a new organizational structure that brought all medical and surgical operations under one leadership team. Prior to this reorganization, hospitalist groups were largely divided by the geographies they served, each operating independently.
After the reorganization, it was apparent that staffing structures among groups varied greatly. Dr. Philpot pored over the workload and billing data and determined the most efficient use of how to staff hospitalist providers. He recently created a program that allows all stakeholders to meet and discuss in an unbiased manner how and when to add resources to a given group. As a result, the team is better able to make smart decisions that translate into improved quality, better patient experience, a more engaged hospitalist group and improved financial decisions. This is a model that Intermountain is now looking to apply to other specialties.
Team Award in Quality Improvement
The Michigan Hospital Medicine Safety Consortium has been in place for a decade and has worked together to improve quality and safety for patients across Michigan and the nation. It has been led since its inception by Scott Flanders, MD, a hospitalist at the University of Michigan, Ann Arbor.
At each participating hospital, teams include hospitalists, infectious disease clinicians, interventional radiologists, nephrologists, nurses, pharmacists, administrators, and more. This integration ensures that the team’s work is highly relevant and generalizable for hospitals around the country.
Their initiatives have informed regulatory and guideline writing authorities in the United States and beyond. For example, findings from their venous thromboembolism project demonstrated that the majority of hospitalized patients do not benefit from VTE prophylaxis, but rather, targeted strategies to define those at high risk. In 2016, their work helped to prevent 852 VTEs in Michigan alone. This led to changes in national guidelines that now emphasize deimplementing pharmacologic VTE prophylaxis and focused risk-assessment in U.S. hospitals.
Their antimicrobial use initiative has led to a robust partnership between hospitalists, hospitals, and national partners, such as the Centers for Disease Control and Prevention. Early work has informed a key gap in stewardship – discharge antibiotic prescribing – which has been a focus for SHM, the CDC, and many others. Efforts have already led to a reduction in thousands of unnecessary antibiotic prescriptions in Michigan.
Junior Investigator Award
SHM’s Research Committee presents the Junior Investigator Award to recognize early-career hospitalist researchers who are leading the way in their field. We are pleased to present the HM20 Junior Investigator Award to Valerie Vaughn, MD, MSc.
Dr. Vaughn is an assistant professor and research scientist in the division of hospital medicine at the University of Michigan and Veterans Affairs Ann Arbor Healthcare System.
Her research is focused on engaging hospitalists in antibiotic prescribing, especially at discharge. She is the hospitalist lead for an initiative to improve antibiotic prescribing in 46 hospitals across Michigan. She has already made a national contribution to the field – two manuscripts that have received high praise and have been cited by the Joint Commission and the CDC in their updated recommendations for antibiotic stewardship. She has a grant from the Gordon and Betty Moore Foundation to study the role of diagnostic error in antibiotic overuse and just received a K08 career development award from the Agency for Healthcare Research and Quality to study methods to improve antibiotic prescribing at hospital discharge.
One of Dr. Vaughn’s career goals is to advance hospital medicine through mentoring the next generation of hospitalists. In 2017, she authored a manuscript titled “Mentee Missteps” in JAMA, which has been viewed nearly 40,000 times since publication. She continues to give talks on this topic and mentors clinical hospitalists on research projects to improve quality and safety.
Dr. Vaughn has worked closely with SHM and represents the society at the CDC’s Healthcare Infection Control Practices Advisory Committee quarterly meetings.
Certificate of Leadership in Hospital Medicine
The Certificate of Leadership in Hospital Medicine (CLHM) cultivates leadership skills in the context of specific hospital medicine challenges. This designation informs employers – or potential employers – with confidence that a candidate is equipped and ready to lead teams and grow an organization.
Charmaine Lewis, MD, MPH, FHM, CLHM, is the quality director for New Hanover Hospitalists in Wilmington, N.C., a role she has held for 7 years. She is also clinical assistant professor, department of medicine, University of North Carolina School of Medicine, Chapel Hill, serving as a mentor for internal medicine, surgery, and obstetrics residents completing projects in quality improvement.
While sitting on the CHF and readmissions committees at her institution, Dr. Lewis was asked why patients with heart failure came back to the hospital. This question launched an in-depth search for real-time and accurate data on heart failure patients in her institution. She worked with the Heart Failure Steering Committee to develop a process to close care gaps and document compliance to the ACC/AHA Get with the Guidelines: Heart Failure recommendations. She facilitated order set revisions, smart-phrase documentation in EPIC, and scripted bedside interdisciplinary rounding to facilitate compliance prior to patient discharge. She also created an end-user friendly dashboard to report compliance with medical leaders, and eventually this project was selected by the department of medicine as their annual quality goal. The project has led to the improvement of CHF GWTG Composite Bundle compliance from 76% to 93%, and compliance with use of aldosterone antagonists from 22% to 85%.
Transitions: From editor to president
As I transition out of the role of medical editor for The Hospitalist, and into the role of president of the Society of Hospital Medicine, it is a bittersweet but exciting transition.
In the relatively short time I have served as editor, so much has changed in our hospitalist community! In the last 4 years alone, we have increased:
• Membership from 14,000 to 20,000
• Chapters from 46 to 68
• Special Interest Groups from 8 to 22
• Subscribers to The Hospitalist from 15,000 to 30,000.
This is all a testimony to the engagement of our membership. SHM is clearly no ordinary specialty society; it is full of incredibly intelligent, invested, and talented members, who actively participate in the society for the betterment of their local teams and patients. It is such a privilege to lead this amazing team.
As for The Hospitalist, I would like to warmly welcome Weijen Chang, MD, FACP, SFHM, as the incoming editor. Weijen served as the pediatrics editor for many years and has been extensively involved on The Hospitalist’s editorial advisory board for even longer. He also has a broad track record of experience as a hospitalist in many settings; that combined with an inquisitive mind and curious spirit makes him the ideal editor for The Hospitalist. He brings energy and enthusiasm and will serve us very well.
While I will miss being intimately involved with The Hospitalist, I am very much looking forward to serving in the role of SHM president starting in April. During this pivotal year, SHM will transition from our one-and-only CEO, Larry Wellikson, MD, MHM, to our newly minted CEO Eric Howell, MD, MHM, who will officially transition in July 2020.
This is a very exciting time in the history of SHM, as we refocus on our mission, vision, values, and core activities. As a membership organization, our primary focus has been, and will always be, serving our member’s needs! As a “Big Tent” organization, we have always supported a broad and diverse set of members, ranging far beyond physician hospitalists, to trainees, medical students, nurse practitioners, physician assistants, practice administrators, and other hospital-based specialists. Being in such a dynamic industry, our diverse members needs are constantly and rapidly changing along with the dramatic transformations in the landscape, including profound shifts in care and reimbursement models that could change the very definition of a hospitalist.
While we continuously scour the landscape and anticipate our members’ needs, we will never lose sight of our core mission, which is to promote exceptional care for hospitalized patients. We will continue to do this by supporting all of our members with tools and materials to help them be the very best they can, for all of our patients. As a humble and servant leader, I am prepared to meet the demands and challenges of the year ahead, with energy and focus, and fulfill the needs of our members, so that together, we can make health care better for those we serve.
Thank you in advance for allowing me the great pleasure of serving this amazing and innovative organization!
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is the outgoing medical editor of The Hospitalist, and president-elect of SHM.
As I transition out of the role of medical editor for The Hospitalist, and into the role of president of the Society of Hospital Medicine, it is a bittersweet but exciting transition.
In the relatively short time I have served as editor, so much has changed in our hospitalist community! In the last 4 years alone, we have increased:
• Membership from 14,000 to 20,000
• Chapters from 46 to 68
• Special Interest Groups from 8 to 22
• Subscribers to The Hospitalist from 15,000 to 30,000.
This is all a testimony to the engagement of our membership. SHM is clearly no ordinary specialty society; it is full of incredibly intelligent, invested, and talented members, who actively participate in the society for the betterment of their local teams and patients. It is such a privilege to lead this amazing team.
As for The Hospitalist, I would like to warmly welcome Weijen Chang, MD, FACP, SFHM, as the incoming editor. Weijen served as the pediatrics editor for many years and has been extensively involved on The Hospitalist’s editorial advisory board for even longer. He also has a broad track record of experience as a hospitalist in many settings; that combined with an inquisitive mind and curious spirit makes him the ideal editor for The Hospitalist. He brings energy and enthusiasm and will serve us very well.
While I will miss being intimately involved with The Hospitalist, I am very much looking forward to serving in the role of SHM president starting in April. During this pivotal year, SHM will transition from our one-and-only CEO, Larry Wellikson, MD, MHM, to our newly minted CEO Eric Howell, MD, MHM, who will officially transition in July 2020.
This is a very exciting time in the history of SHM, as we refocus on our mission, vision, values, and core activities. As a membership organization, our primary focus has been, and will always be, serving our member’s needs! As a “Big Tent” organization, we have always supported a broad and diverse set of members, ranging far beyond physician hospitalists, to trainees, medical students, nurse practitioners, physician assistants, practice administrators, and other hospital-based specialists. Being in such a dynamic industry, our diverse members needs are constantly and rapidly changing along with the dramatic transformations in the landscape, including profound shifts in care and reimbursement models that could change the very definition of a hospitalist.
While we continuously scour the landscape and anticipate our members’ needs, we will never lose sight of our core mission, which is to promote exceptional care for hospitalized patients. We will continue to do this by supporting all of our members with tools and materials to help them be the very best they can, for all of our patients. As a humble and servant leader, I am prepared to meet the demands and challenges of the year ahead, with energy and focus, and fulfill the needs of our members, so that together, we can make health care better for those we serve.
Thank you in advance for allowing me the great pleasure of serving this amazing and innovative organization!
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is the outgoing medical editor of The Hospitalist, and president-elect of SHM.
As I transition out of the role of medical editor for The Hospitalist, and into the role of president of the Society of Hospital Medicine, it is a bittersweet but exciting transition.
In the relatively short time I have served as editor, so much has changed in our hospitalist community! In the last 4 years alone, we have increased:
• Membership from 14,000 to 20,000
• Chapters from 46 to 68
• Special Interest Groups from 8 to 22
• Subscribers to The Hospitalist from 15,000 to 30,000.
This is all a testimony to the engagement of our membership. SHM is clearly no ordinary specialty society; it is full of incredibly intelligent, invested, and talented members, who actively participate in the society for the betterment of their local teams and patients. It is such a privilege to lead this amazing team.
As for The Hospitalist, I would like to warmly welcome Weijen Chang, MD, FACP, SFHM, as the incoming editor. Weijen served as the pediatrics editor for many years and has been extensively involved on The Hospitalist’s editorial advisory board for even longer. He also has a broad track record of experience as a hospitalist in many settings; that combined with an inquisitive mind and curious spirit makes him the ideal editor for The Hospitalist. He brings energy and enthusiasm and will serve us very well.
While I will miss being intimately involved with The Hospitalist, I am very much looking forward to serving in the role of SHM president starting in April. During this pivotal year, SHM will transition from our one-and-only CEO, Larry Wellikson, MD, MHM, to our newly minted CEO Eric Howell, MD, MHM, who will officially transition in July 2020.
This is a very exciting time in the history of SHM, as we refocus on our mission, vision, values, and core activities. As a membership organization, our primary focus has been, and will always be, serving our member’s needs! As a “Big Tent” organization, we have always supported a broad and diverse set of members, ranging far beyond physician hospitalists, to trainees, medical students, nurse practitioners, physician assistants, practice administrators, and other hospital-based specialists. Being in such a dynamic industry, our diverse members needs are constantly and rapidly changing along with the dramatic transformations in the landscape, including profound shifts in care and reimbursement models that could change the very definition of a hospitalist.
While we continuously scour the landscape and anticipate our members’ needs, we will never lose sight of our core mission, which is to promote exceptional care for hospitalized patients. We will continue to do this by supporting all of our members with tools and materials to help them be the very best they can, for all of our patients. As a humble and servant leader, I am prepared to meet the demands and challenges of the year ahead, with energy and focus, and fulfill the needs of our members, so that together, we can make health care better for those we serve.
Thank you in advance for allowing me the great pleasure of serving this amazing and innovative organization!
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is the outgoing medical editor of The Hospitalist, and president-elect of SHM.
The future of hospital medicine
Assured? Or a definite maybe?
When I started at SHM in 2000, there were fewer than 1,000 hospitalists in the US, and now there are more than 60,000. SHM (back then, we were the National Association of Inpatient Physicians) had about 300 members; now, we have more than 20,000.
Today, hospitalists are part of the medical staff at virtually every hospital in the country, and hospital medicine is recognized as a unique medical specialty with our own knowledge base, textbooks, competencies, meetings, and medical professional society. In a health care environment swirling with change, we are one of the few specialties forged with the ability to adapt and, at times, lead this change. Yet there is so much disruption and instability that there are still many twists and turns in the road that will affect hospitalists’ ability to carve out an even brighter future.
Consolidation has come to health care on a large scale. Hospitals are merging. Health insurers are combining, and even large hospital medicine companies like TeamHealth, Sound, Envision, and others are merging, growing, and acquiring.
At the same time, outside forces from industries not usually associated with health care or inpatient care are swarming into our world: CVS acquires Aetna and aims to reshape primary care; Amazon dominates health care supply chains and moves into pharmacy benefits, and even gets into health care delivery via their partnership with Berkshire Hathaway and JP Morgan; Walmart merges with Humana to create one of the biggest players in Medicare; and Apple expands their inroads into wearables and chronic disease management.
Employment of clinicians has grown logarithmically, especially with inpatient physicians, reshaping the medical staff compensation and accountability. At the same time, payers, both government and private, are evolving into population health with an emphasis not so much on transactions (visits and procedures), but more aligned with outcomes, effectiveness, and efficiency.
All of this leads to a new paradigm of what is important and a new set of values that seems at times more like corporate America where the loyalty of employees can be torn between their employer and the patient. This is especially troublesome in a field traditionally based on the primacy of the doctor-patient relationship. This can put the hospitalist right in the middle at the time when the patient can be most vulnerable.
This has led to new ways to deliver the care that hospitalists provide. First as a pilot and now moving more mainstream, patients with several diagnoses (e.g., heart failure, dehydration, or pneumonia) are now managed not in bricks and mortar hospitals, but in “hospitals at home.” The last few days of a typical hospitalization now take place outside the hospital in a skilled nursing facility (SNF). Fear of uncompensated and unnecessary readmissions leads hospitals to engage hospitalists to handle the first few post-discharge outpatient visits.
This is just a small part of the expanding scope for hospitalists. In addition to managing SNFs and the discharge clinic, hospitalists are now the major providers of perioperative care and play a growing role in palliative care, especially for inpatients. As other specialties that abut hospital medicine have increasing demands and yet fewer new specialists, hospitalists are taking on more critical care and geriatrics, providing procedures, and occupy an evolving role in the emergency room.
There is a lot of work coming towards hospital medicine, and to expand our workforce, hospital medicine groups have incorporated advanced practice providers, including nurse practitioners and physician assistants. But building a true team of health professionals is not seamless or easy with each constituency having a unique scope of practice, limits on their licensure, their own culture, and a distinct training background.
But wait. There will be more new players on the hospital medicine team going forward – some we cannot even anticipate at the present time. In the future, the hospitalist may not even touch the electronic health record (EHR). Clinicians have never excelled at data entry or analysis, and it is time to use a combination of artificial intelligence (AI), voice-activated gathering of history into the record, and staff trained to manage the EHR on both the input and the output sides.
While there may be cheering for this new approach to the EHR – especially because it is a major factor in hospitalist burnout – this will refocus the role and work of the hospitalist to be more of a reviewer and integrator of data, and a strategist and decision-maker overseeing 30 or more patients. As Amazon, CVS, and Walmart move into health care, they will look for the best way to utilize the $300-400/hour hospitalist to the top of our skill level.
In the end, this all comes back to how hospitalists add value, how we can create a career that is rewarding, and how we can help hospitalists be resilient and avoid burnout.
The good news is that hospitalists will not be replaced by AI, nor should we expect to have our incomes cut as less well-trained alternatives replace highly compensated physicians in other specialties. This is a real prospect for many other specialties like dermatology, radiology, pathology, anesthesiology, and even cardiology. But hospitalists will need to adapt to changes in what is valued (i.e., how you can be the most effective and efficient) and to a new job description (i.e., overseeing more patients and managing a team that does more of the H&P, data collecting, and bedside work).
After 20 years of coming out of nowhere to being in the middle of everything in health care, I am confident that hospitalists, with the help of SHM, can continue to forge a path where we can be key difference makers and where we can create a rewarding and sustainable career. It won’t “just happen.” It is not inevitable. But if the past 20 years is any example, we are well-positioned to make the adaptation to succeed in the next 20 years. It is up to all of us to make it happen.
Dr. Wellikson is the CEO of SHM and is retiring from his role in 2020. This article is the second in a series celebrating Dr. Wellikson’s tenure as CEO.
Assured? Or a definite maybe?
Assured? Or a definite maybe?
When I started at SHM in 2000, there were fewer than 1,000 hospitalists in the US, and now there are more than 60,000. SHM (back then, we were the National Association of Inpatient Physicians) had about 300 members; now, we have more than 20,000.
Today, hospitalists are part of the medical staff at virtually every hospital in the country, and hospital medicine is recognized as a unique medical specialty with our own knowledge base, textbooks, competencies, meetings, and medical professional society. In a health care environment swirling with change, we are one of the few specialties forged with the ability to adapt and, at times, lead this change. Yet there is so much disruption and instability that there are still many twists and turns in the road that will affect hospitalists’ ability to carve out an even brighter future.
Consolidation has come to health care on a large scale. Hospitals are merging. Health insurers are combining, and even large hospital medicine companies like TeamHealth, Sound, Envision, and others are merging, growing, and acquiring.
At the same time, outside forces from industries not usually associated with health care or inpatient care are swarming into our world: CVS acquires Aetna and aims to reshape primary care; Amazon dominates health care supply chains and moves into pharmacy benefits, and even gets into health care delivery via their partnership with Berkshire Hathaway and JP Morgan; Walmart merges with Humana to create one of the biggest players in Medicare; and Apple expands their inroads into wearables and chronic disease management.
Employment of clinicians has grown logarithmically, especially with inpatient physicians, reshaping the medical staff compensation and accountability. At the same time, payers, both government and private, are evolving into population health with an emphasis not so much on transactions (visits and procedures), but more aligned with outcomes, effectiveness, and efficiency.
All of this leads to a new paradigm of what is important and a new set of values that seems at times more like corporate America where the loyalty of employees can be torn between their employer and the patient. This is especially troublesome in a field traditionally based on the primacy of the doctor-patient relationship. This can put the hospitalist right in the middle at the time when the patient can be most vulnerable.
This has led to new ways to deliver the care that hospitalists provide. First as a pilot and now moving more mainstream, patients with several diagnoses (e.g., heart failure, dehydration, or pneumonia) are now managed not in bricks and mortar hospitals, but in “hospitals at home.” The last few days of a typical hospitalization now take place outside the hospital in a skilled nursing facility (SNF). Fear of uncompensated and unnecessary readmissions leads hospitals to engage hospitalists to handle the first few post-discharge outpatient visits.
This is just a small part of the expanding scope for hospitalists. In addition to managing SNFs and the discharge clinic, hospitalists are now the major providers of perioperative care and play a growing role in palliative care, especially for inpatients. As other specialties that abut hospital medicine have increasing demands and yet fewer new specialists, hospitalists are taking on more critical care and geriatrics, providing procedures, and occupy an evolving role in the emergency room.
There is a lot of work coming towards hospital medicine, and to expand our workforce, hospital medicine groups have incorporated advanced practice providers, including nurse practitioners and physician assistants. But building a true team of health professionals is not seamless or easy with each constituency having a unique scope of practice, limits on their licensure, their own culture, and a distinct training background.
But wait. There will be more new players on the hospital medicine team going forward – some we cannot even anticipate at the present time. In the future, the hospitalist may not even touch the electronic health record (EHR). Clinicians have never excelled at data entry or analysis, and it is time to use a combination of artificial intelligence (AI), voice-activated gathering of history into the record, and staff trained to manage the EHR on both the input and the output sides.
While there may be cheering for this new approach to the EHR – especially because it is a major factor in hospitalist burnout – this will refocus the role and work of the hospitalist to be more of a reviewer and integrator of data, and a strategist and decision-maker overseeing 30 or more patients. As Amazon, CVS, and Walmart move into health care, they will look for the best way to utilize the $300-400/hour hospitalist to the top of our skill level.
In the end, this all comes back to how hospitalists add value, how we can create a career that is rewarding, and how we can help hospitalists be resilient and avoid burnout.
The good news is that hospitalists will not be replaced by AI, nor should we expect to have our incomes cut as less well-trained alternatives replace highly compensated physicians in other specialties. This is a real prospect for many other specialties like dermatology, radiology, pathology, anesthesiology, and even cardiology. But hospitalists will need to adapt to changes in what is valued (i.e., how you can be the most effective and efficient) and to a new job description (i.e., overseeing more patients and managing a team that does more of the H&P, data collecting, and bedside work).
After 20 years of coming out of nowhere to being in the middle of everything in health care, I am confident that hospitalists, with the help of SHM, can continue to forge a path where we can be key difference makers and where we can create a rewarding and sustainable career. It won’t “just happen.” It is not inevitable. But if the past 20 years is any example, we are well-positioned to make the adaptation to succeed in the next 20 years. It is up to all of us to make it happen.
Dr. Wellikson is the CEO of SHM and is retiring from his role in 2020. This article is the second in a series celebrating Dr. Wellikson’s tenure as CEO.
When I started at SHM in 2000, there were fewer than 1,000 hospitalists in the US, and now there are more than 60,000. SHM (back then, we were the National Association of Inpatient Physicians) had about 300 members; now, we have more than 20,000.
Today, hospitalists are part of the medical staff at virtually every hospital in the country, and hospital medicine is recognized as a unique medical specialty with our own knowledge base, textbooks, competencies, meetings, and medical professional society. In a health care environment swirling with change, we are one of the few specialties forged with the ability to adapt and, at times, lead this change. Yet there is so much disruption and instability that there are still many twists and turns in the road that will affect hospitalists’ ability to carve out an even brighter future.
Consolidation has come to health care on a large scale. Hospitals are merging. Health insurers are combining, and even large hospital medicine companies like TeamHealth, Sound, Envision, and others are merging, growing, and acquiring.
At the same time, outside forces from industries not usually associated with health care or inpatient care are swarming into our world: CVS acquires Aetna and aims to reshape primary care; Amazon dominates health care supply chains and moves into pharmacy benefits, and even gets into health care delivery via their partnership with Berkshire Hathaway and JP Morgan; Walmart merges with Humana to create one of the biggest players in Medicare; and Apple expands their inroads into wearables and chronic disease management.
Employment of clinicians has grown logarithmically, especially with inpatient physicians, reshaping the medical staff compensation and accountability. At the same time, payers, both government and private, are evolving into population health with an emphasis not so much on transactions (visits and procedures), but more aligned with outcomes, effectiveness, and efficiency.
All of this leads to a new paradigm of what is important and a new set of values that seems at times more like corporate America where the loyalty of employees can be torn between their employer and the patient. This is especially troublesome in a field traditionally based on the primacy of the doctor-patient relationship. This can put the hospitalist right in the middle at the time when the patient can be most vulnerable.
This has led to new ways to deliver the care that hospitalists provide. First as a pilot and now moving more mainstream, patients with several diagnoses (e.g., heart failure, dehydration, or pneumonia) are now managed not in bricks and mortar hospitals, but in “hospitals at home.” The last few days of a typical hospitalization now take place outside the hospital in a skilled nursing facility (SNF). Fear of uncompensated and unnecessary readmissions leads hospitals to engage hospitalists to handle the first few post-discharge outpatient visits.
This is just a small part of the expanding scope for hospitalists. In addition to managing SNFs and the discharge clinic, hospitalists are now the major providers of perioperative care and play a growing role in palliative care, especially for inpatients. As other specialties that abut hospital medicine have increasing demands and yet fewer new specialists, hospitalists are taking on more critical care and geriatrics, providing procedures, and occupy an evolving role in the emergency room.
There is a lot of work coming towards hospital medicine, and to expand our workforce, hospital medicine groups have incorporated advanced practice providers, including nurse practitioners and physician assistants. But building a true team of health professionals is not seamless or easy with each constituency having a unique scope of practice, limits on their licensure, their own culture, and a distinct training background.
But wait. There will be more new players on the hospital medicine team going forward – some we cannot even anticipate at the present time. In the future, the hospitalist may not even touch the electronic health record (EHR). Clinicians have never excelled at data entry or analysis, and it is time to use a combination of artificial intelligence (AI), voice-activated gathering of history into the record, and staff trained to manage the EHR on both the input and the output sides.
While there may be cheering for this new approach to the EHR – especially because it is a major factor in hospitalist burnout – this will refocus the role and work of the hospitalist to be more of a reviewer and integrator of data, and a strategist and decision-maker overseeing 30 or more patients. As Amazon, CVS, and Walmart move into health care, they will look for the best way to utilize the $300-400/hour hospitalist to the top of our skill level.
In the end, this all comes back to how hospitalists add value, how we can create a career that is rewarding, and how we can help hospitalists be resilient and avoid burnout.
The good news is that hospitalists will not be replaced by AI, nor should we expect to have our incomes cut as less well-trained alternatives replace highly compensated physicians in other specialties. This is a real prospect for many other specialties like dermatology, radiology, pathology, anesthesiology, and even cardiology. But hospitalists will need to adapt to changes in what is valued (i.e., how you can be the most effective and efficient) and to a new job description (i.e., overseeing more patients and managing a team that does more of the H&P, data collecting, and bedside work).
After 20 years of coming out of nowhere to being in the middle of everything in health care, I am confident that hospitalists, with the help of SHM, can continue to forge a path where we can be key difference makers and where we can create a rewarding and sustainable career. It won’t “just happen.” It is not inevitable. But if the past 20 years is any example, we are well-positioned to make the adaptation to succeed in the next 20 years. It is up to all of us to make it happen.
Dr. Wellikson is the CEO of SHM and is retiring from his role in 2020. This article is the second in a series celebrating Dr. Wellikson’s tenure as CEO.