User login
The September issue of Thoracic Surgery News is now available online
Be sure to visit our interactive digital or PDF version of the September issue of Thoracic Surgery News. This month we are featuring stories ranging from the risks of aspirin resistance in pediatric cardiac surgery patients to the recent Centers for Medicare and Medicaid Services decision to cover transcatheter mitral valve repair (TMVR) procedures. Also, in our News from the AATS section there is a call for abstracts for AATS Week (comprising the 95th AATS Annual Meeting and the AATS Mitral Conclave), as well as several exciting cardiothoracic surgery fellowship opportunities.
To view our September PDF and interactive digital edition, click here.
Be sure to visit our interactive digital or PDF version of the September issue of Thoracic Surgery News. This month we are featuring stories ranging from the risks of aspirin resistance in pediatric cardiac surgery patients to the recent Centers for Medicare and Medicaid Services decision to cover transcatheter mitral valve repair (TMVR) procedures. Also, in our News from the AATS section there is a call for abstracts for AATS Week (comprising the 95th AATS Annual Meeting and the AATS Mitral Conclave), as well as several exciting cardiothoracic surgery fellowship opportunities.
To view our September PDF and interactive digital edition, click here.
Be sure to visit our interactive digital or PDF version of the September issue of Thoracic Surgery News. This month we are featuring stories ranging from the risks of aspirin resistance in pediatric cardiac surgery patients to the recent Centers for Medicare and Medicaid Services decision to cover transcatheter mitral valve repair (TMVR) procedures. Also, in our News from the AATS section there is a call for abstracts for AATS Week (comprising the 95th AATS Annual Meeting and the AATS Mitral Conclave), as well as several exciting cardiothoracic surgery fellowship opportunities.
To view our September PDF and interactive digital edition, click here.
VIDEO: Consider local anesthesia for transfemoral TAVR
BARCELONA – An analysis of FRANCE 2 registry showed that local anesthesia during the transfemoral aortic valve replacement procedure is a safe and effective option, compared with general anesthesia.
The study was performed based on data from 2010 and 2011, and at the annual congress of the European Society of Cardiology, Dr. Romain Chopard of the University Hospital of Besançon, Paris, and his coinvestigators reported that the practice is rather common – even routine in some centers – today.
But, performing TAVR under local anesthesia is not common practice in the United States, said Dr. Deepak L. Bhatt, executive director of interventional cardiovascular programs at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, both in Boston.
In a video, Dr. Bhatt shares his thoughts on performing local anesthesia and why it hasn’t taken hold in the United States. He also shares his advice with physicians who perform the TAVR procedure.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
BARCELONA – An analysis of FRANCE 2 registry showed that local anesthesia during the transfemoral aortic valve replacement procedure is a safe and effective option, compared with general anesthesia.
The study was performed based on data from 2010 and 2011, and at the annual congress of the European Society of Cardiology, Dr. Romain Chopard of the University Hospital of Besançon, Paris, and his coinvestigators reported that the practice is rather common – even routine in some centers – today.
But, performing TAVR under local anesthesia is not common practice in the United States, said Dr. Deepak L. Bhatt, executive director of interventional cardiovascular programs at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, both in Boston.
In a video, Dr. Bhatt shares his thoughts on performing local anesthesia and why it hasn’t taken hold in the United States. He also shares his advice with physicians who perform the TAVR procedure.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
BARCELONA – An analysis of FRANCE 2 registry showed that local anesthesia during the transfemoral aortic valve replacement procedure is a safe and effective option, compared with general anesthesia.
The study was performed based on data from 2010 and 2011, and at the annual congress of the European Society of Cardiology, Dr. Romain Chopard of the University Hospital of Besançon, Paris, and his coinvestigators reported that the practice is rather common – even routine in some centers – today.
But, performing TAVR under local anesthesia is not common practice in the United States, said Dr. Deepak L. Bhatt, executive director of interventional cardiovascular programs at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, both in Boston.
In a video, Dr. Bhatt shares his thoughts on performing local anesthesia and why it hasn’t taken hold in the United States. He also shares his advice with physicians who perform the TAVR procedure.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
AT THE ESC CONGRESS 2014
VIDEO: Repositionable TAVR valve holds promise
BARCELONA – The transcatheter aortic valve replacement technology is changing rapidly, especially in Europe where the regulatory process is different and more types of valves are on the market.
One of the current focus areas in the development of TAVR devices is making retrievable and repositionable valves to improve the implantation process and patient outcomes. Late last year, Lotus Valve System reported favorable results for its valve in the REPRISE II study.
At the annual congress of the European Society of Cardiology, Dr. Stylianos A. Pyxaras presented another study showing that the repositionable Direct Flow Medical valve in elderly high-risk patients with severe aortic stenosis compared well in safety and efficacy with the results of the DISCOVER trial.
Dr. Deepak L. Bhatt, executive director of Interventional Cardiovascular Programs and professor of medicine at Harvard Medical School in Boston, shared his opinion about the findings and the future implications on practice. He was not involved in any of the mentioned studies.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Twitter: @naseemmiller
Lotus Valve System, REPRISE II, ESC
BARCELONA – The transcatheter aortic valve replacement technology is changing rapidly, especially in Europe where the regulatory process is different and more types of valves are on the market.
One of the current focus areas in the development of TAVR devices is making retrievable and repositionable valves to improve the implantation process and patient outcomes. Late last year, Lotus Valve System reported favorable results for its valve in the REPRISE II study.
At the annual congress of the European Society of Cardiology, Dr. Stylianos A. Pyxaras presented another study showing that the repositionable Direct Flow Medical valve in elderly high-risk patients with severe aortic stenosis compared well in safety and efficacy with the results of the DISCOVER trial.
Dr. Deepak L. Bhatt, executive director of Interventional Cardiovascular Programs and professor of medicine at Harvard Medical School in Boston, shared his opinion about the findings and the future implications on practice. He was not involved in any of the mentioned studies.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Twitter: @naseemmiller
BARCELONA – The transcatheter aortic valve replacement technology is changing rapidly, especially in Europe where the regulatory process is different and more types of valves are on the market.
One of the current focus areas in the development of TAVR devices is making retrievable and repositionable valves to improve the implantation process and patient outcomes. Late last year, Lotus Valve System reported favorable results for its valve in the REPRISE II study.
At the annual congress of the European Society of Cardiology, Dr. Stylianos A. Pyxaras presented another study showing that the repositionable Direct Flow Medical valve in elderly high-risk patients with severe aortic stenosis compared well in safety and efficacy with the results of the DISCOVER trial.
Dr. Deepak L. Bhatt, executive director of Interventional Cardiovascular Programs and professor of medicine at Harvard Medical School in Boston, shared his opinion about the findings and the future implications on practice. He was not involved in any of the mentioned studies.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Twitter: @naseemmiller
Lotus Valve System, REPRISE II, ESC
Lotus Valve System, REPRISE II, ESC
AT THE ESC CONGRESS 2014
Fractional flow reserve-guided PCI improves outcomes in stable heart disease
Fractional flow reserve-guided percutaneous coronary intervention plus best medical therapy improved outcomes when compared with medical therapy alone in patients with stable coronary artery disease in the Fractional Flow Reserve versus Angiography for Multivessel Evaluation 2 (FAME 2) trial.
A composite outcome of death from any cause, nonfatal myocardial infarction, or urgent revascularization within 2 years occurred in 8.1% of 447 patients who had at least one stenosis with a fractional flow reserve (FFR) of 0.80 and were randomized to undergo percutaneous coronary intervention (PCI) performed on the basis of the FFR, compared with 19.5% of 441 such patients who received medical therapy alone.
The difference was driven mainly by a 77% reduction in the need for urgent revascularization in interventional group as compared with the medical therapy group (4.0% vs. 16.3%, hazard ratio, 0.23). The overall rates of death and myocardial infarction did not differ significantly between the groups, Dr. Bernard D. Bruyne of the Cardiovascular Center Aalst, Belgium, and his colleagues reported at the annual congress of the European Society of Cardiology.
The findings of the open-label, randomized, multicenter trial were simultaneously published online Sept. 1 (N. Engl. J. Med. 2014 Sept. 1[doi:10.1056/NEJMoa1408758]).
The improved outcomes in the PCI group were the result of outcomes that occurred between 8 days and 2 years after randomization; in the first 7 days, more primary end-point events occurred in the PCI group than in the medical therapy group (2.2% vs. 0.9%, hazard ratio 2.49).
The rate of the primary endpoint was 9.0% among 332 additional patients who had an FFR of more than 0.80 in all stenoses, were enrolled into a registry, and received medical therapy alone, the researchers said.
The original FAME trial studied the procedure in patients who had already been selected for PCI. Compared with patients whose PCI was guided by angiography alone, those whose PCI was guided by FFR had significantly reduced rates of the composite end point of death, nonfatal myocardial infarction, and repeat revascularization at 1 year (N. Engl. J. Med. 2009;360:213-24).
FAME 2 evaluated use of FFR for improving the benefits of initial stenting as an alternative to noninvasive medical therapy. The trial was halted after a median of 7 months’ follow-up, when data safety and monitoring board found a highly statistically significant reduction in hospital readmission and urgent revascularization in the patients who received FFR-based stenting compared with those who received optimal medical therapy alone.
FAME 2 was supported by St. Jude Medical. Dr. De Bruyne reported that his institution receives grant support and consulting fees on his behalf from St. Jude Medical. Detailed disclosure information for several other authors is available with the full text of the article at www.NEJM.org.
The most impressive finding in the FAME 2 trial was a sustained reduced rate of urgent revascularization among patients undergoing early PCI.
Though the trigger in 60% of patients was based solely on clinical features and was potentially influenced by knowledge of the coronary anatomy, there was nonetheless a lower incidence of revascularization triggered by myocardial infarction or electrocardiographic changes in the PCI group than in the medical therapy group (3.4% versus 7.0%). This finding is consistent with recent evidence challenging the long-held view that acute coronary syndromes occur mainly at sites of noncritical stenoses.
It is plausible that stenting of vulnerable, hemodynamically significant lesions could prevent future coronary events.
The FAME 2 results show that early FFR-guided PCI in patients with stable coronary disease sustainably reduced the need for urgent revascularization. Given the continued improvement in the safety of stents and the procedures to implant them, PCI may eventually be shown to also have a favorable effect on other hard end points.
Dr. Jeffrey J. Rade is with the University of Massachusetts, Worcester. He made these comments in an accompanying editorial (N. Engl. J. Med. 2014 Sept. 1[doi:10.1056/NEJMe1410336]). He reported having no disclosures.
The most impressive finding in the FAME 2 trial was a sustained reduced rate of urgent revascularization among patients undergoing early PCI.
Though the trigger in 60% of patients was based solely on clinical features and was potentially influenced by knowledge of the coronary anatomy, there was nonetheless a lower incidence of revascularization triggered by myocardial infarction or electrocardiographic changes in the PCI group than in the medical therapy group (3.4% versus 7.0%). This finding is consistent with recent evidence challenging the long-held view that acute coronary syndromes occur mainly at sites of noncritical stenoses.
It is plausible that stenting of vulnerable, hemodynamically significant lesions could prevent future coronary events.
The FAME 2 results show that early FFR-guided PCI in patients with stable coronary disease sustainably reduced the need for urgent revascularization. Given the continued improvement in the safety of stents and the procedures to implant them, PCI may eventually be shown to also have a favorable effect on other hard end points.
Dr. Jeffrey J. Rade is with the University of Massachusetts, Worcester. He made these comments in an accompanying editorial (N. Engl. J. Med. 2014 Sept. 1[doi:10.1056/NEJMe1410336]). He reported having no disclosures.
The most impressive finding in the FAME 2 trial was a sustained reduced rate of urgent revascularization among patients undergoing early PCI.
Though the trigger in 60% of patients was based solely on clinical features and was potentially influenced by knowledge of the coronary anatomy, there was nonetheless a lower incidence of revascularization triggered by myocardial infarction or electrocardiographic changes in the PCI group than in the medical therapy group (3.4% versus 7.0%). This finding is consistent with recent evidence challenging the long-held view that acute coronary syndromes occur mainly at sites of noncritical stenoses.
It is plausible that stenting of vulnerable, hemodynamically significant lesions could prevent future coronary events.
The FAME 2 results show that early FFR-guided PCI in patients with stable coronary disease sustainably reduced the need for urgent revascularization. Given the continued improvement in the safety of stents and the procedures to implant them, PCI may eventually be shown to also have a favorable effect on other hard end points.
Dr. Jeffrey J. Rade is with the University of Massachusetts, Worcester. He made these comments in an accompanying editorial (N. Engl. J. Med. 2014 Sept. 1[doi:10.1056/NEJMe1410336]). He reported having no disclosures.
Fractional flow reserve-guided percutaneous coronary intervention plus best medical therapy improved outcomes when compared with medical therapy alone in patients with stable coronary artery disease in the Fractional Flow Reserve versus Angiography for Multivessel Evaluation 2 (FAME 2) trial.
A composite outcome of death from any cause, nonfatal myocardial infarction, or urgent revascularization within 2 years occurred in 8.1% of 447 patients who had at least one stenosis with a fractional flow reserve (FFR) of 0.80 and were randomized to undergo percutaneous coronary intervention (PCI) performed on the basis of the FFR, compared with 19.5% of 441 such patients who received medical therapy alone.
The difference was driven mainly by a 77% reduction in the need for urgent revascularization in interventional group as compared with the medical therapy group (4.0% vs. 16.3%, hazard ratio, 0.23). The overall rates of death and myocardial infarction did not differ significantly between the groups, Dr. Bernard D. Bruyne of the Cardiovascular Center Aalst, Belgium, and his colleagues reported at the annual congress of the European Society of Cardiology.
The findings of the open-label, randomized, multicenter trial were simultaneously published online Sept. 1 (N. Engl. J. Med. 2014 Sept. 1[doi:10.1056/NEJMoa1408758]).
The improved outcomes in the PCI group were the result of outcomes that occurred between 8 days and 2 years after randomization; in the first 7 days, more primary end-point events occurred in the PCI group than in the medical therapy group (2.2% vs. 0.9%, hazard ratio 2.49).
The rate of the primary endpoint was 9.0% among 332 additional patients who had an FFR of more than 0.80 in all stenoses, were enrolled into a registry, and received medical therapy alone, the researchers said.
The original FAME trial studied the procedure in patients who had already been selected for PCI. Compared with patients whose PCI was guided by angiography alone, those whose PCI was guided by FFR had significantly reduced rates of the composite end point of death, nonfatal myocardial infarction, and repeat revascularization at 1 year (N. Engl. J. Med. 2009;360:213-24).
FAME 2 evaluated use of FFR for improving the benefits of initial stenting as an alternative to noninvasive medical therapy. The trial was halted after a median of 7 months’ follow-up, when data safety and monitoring board found a highly statistically significant reduction in hospital readmission and urgent revascularization in the patients who received FFR-based stenting compared with those who received optimal medical therapy alone.
FAME 2 was supported by St. Jude Medical. Dr. De Bruyne reported that his institution receives grant support and consulting fees on his behalf from St. Jude Medical. Detailed disclosure information for several other authors is available with the full text of the article at www.NEJM.org.
Fractional flow reserve-guided percutaneous coronary intervention plus best medical therapy improved outcomes when compared with medical therapy alone in patients with stable coronary artery disease in the Fractional Flow Reserve versus Angiography for Multivessel Evaluation 2 (FAME 2) trial.
A composite outcome of death from any cause, nonfatal myocardial infarction, or urgent revascularization within 2 years occurred in 8.1% of 447 patients who had at least one stenosis with a fractional flow reserve (FFR) of 0.80 and were randomized to undergo percutaneous coronary intervention (PCI) performed on the basis of the FFR, compared with 19.5% of 441 such patients who received medical therapy alone.
The difference was driven mainly by a 77% reduction in the need for urgent revascularization in interventional group as compared with the medical therapy group (4.0% vs. 16.3%, hazard ratio, 0.23). The overall rates of death and myocardial infarction did not differ significantly between the groups, Dr. Bernard D. Bruyne of the Cardiovascular Center Aalst, Belgium, and his colleagues reported at the annual congress of the European Society of Cardiology.
The findings of the open-label, randomized, multicenter trial were simultaneously published online Sept. 1 (N. Engl. J. Med. 2014 Sept. 1[doi:10.1056/NEJMoa1408758]).
The improved outcomes in the PCI group were the result of outcomes that occurred between 8 days and 2 years after randomization; in the first 7 days, more primary end-point events occurred in the PCI group than in the medical therapy group (2.2% vs. 0.9%, hazard ratio 2.49).
The rate of the primary endpoint was 9.0% among 332 additional patients who had an FFR of more than 0.80 in all stenoses, were enrolled into a registry, and received medical therapy alone, the researchers said.
The original FAME trial studied the procedure in patients who had already been selected for PCI. Compared with patients whose PCI was guided by angiography alone, those whose PCI was guided by FFR had significantly reduced rates of the composite end point of death, nonfatal myocardial infarction, and repeat revascularization at 1 year (N. Engl. J. Med. 2009;360:213-24).
FAME 2 evaluated use of FFR for improving the benefits of initial stenting as an alternative to noninvasive medical therapy. The trial was halted after a median of 7 months’ follow-up, when data safety and monitoring board found a highly statistically significant reduction in hospital readmission and urgent revascularization in the patients who received FFR-based stenting compared with those who received optimal medical therapy alone.
FAME 2 was supported by St. Jude Medical. Dr. De Bruyne reported that his institution receives grant support and consulting fees on his behalf from St. Jude Medical. Detailed disclosure information for several other authors is available with the full text of the article at www.NEJM.org.
FROM THE ESC CONGRESS 2014
Key clinical point: Stenting cut the need for urgent revascularization in patients who had early PCI.
Major finding: The composite outcome occurred in 8.1% vs. 19.5% of intervention and medical therapy patients, respectively.
Data source: The open-label, randomized, multicenter FAME 2 study in 888 patients.
Disclosures: FAME 2 was supported by St. Jude Medical. Dr. De Bruyne reported that his institution receives grant support and consulting fees on his behalf from St. Jude Medical. Detailed disclosure information for several other authors is available with the full text of the article at www.NEJM.org.
Alirocumab sharply reduced major cardiovascular events
BARCELONA – When added to maximally tolerated statin therapy, the investigational PCSK9 inhibitor alirocumab resulted in a further 54% reduction in major cardiovascular events among high-cardiovascular-risk patients, based on a post-hoc analysis of a large randomized controlled Phase-3 trial.
The ODYSSEY LONG TERM trial is the largest and longest study of a PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor to report results to date, with roughly 1,900 patient-years of double-blind exposure to alirocumab. And although the ongoing trial is primarily a safety study, it is also now the first PCSK9 trial to provide what everyone watching the development of this novel drug class has been eagerly awaiting: clinical outcomes data, albeit in this case from a post-hoc secondary analysis.
“This is the first trial with any of the PCSK9 inhibitors to suggest that there will be a further significant reduction in cardiovascular events when added on to maximized statin therapy,” Dr. Jennifer G. Robinson said in presenting interim results of ODYSSEY LONG TERM at the annual congress of the European Society of Cardiology.
“We’re on the right track in terms of trying to achieve further reduction in cardiovascular events through additional lipid lowering. But this is not the definitive evidence. We need the prospective outcomes trials to validate this data and also to establish the long-term safety of these drugs when added to the statins,” cautioned Dr. Robinson, professor of epidemiology and of medicine and director of the prevention intervention center at the University of Iowa, Iowa City.
Nonetheless, on the basis of the dramatic LDL-lowering and reassuring evidence of safety shown in ODYSSEY LONG TERM and the other double-blind phase III trials presented at the congress, Sanofi and Regeneron announced plans to file for U.S. and European Union marketing approval of alirocumab before the end of the year. The proposed indication will be for LDL lowering, which regulatory agencies have accepted as a surrogate endpoint for prevention of clinical events.
Meanwhile, the definitive ODYSSEY OUTCOMES trial is underway in 18,000 patients with acute coronary syndromes, with prospective evaluation of CV outcomes as its primary endpoint. The composite endpoint employed in the big OUTCOMES trial is identical to that used in the ODYSSEY LONG TERM post hoc analysis.
ODYSSEY LONG TERM includes 2,341 patients at high CV risk and an LDL level greater than 70 mg/dL despite maximally tolerated statin therapy. The patients fall into two categories: those with heterozygous familial hypercholesterolemia and others at very high risk because of known coronary heart disease. Participants were randomized 2:1 to 150 mg of alirocumab by self-administered subcutaneous injection at home every 2 weeks or placebo in addition to their statin.
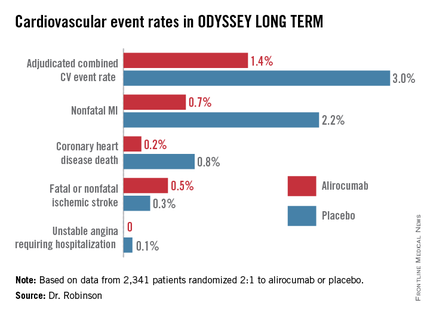
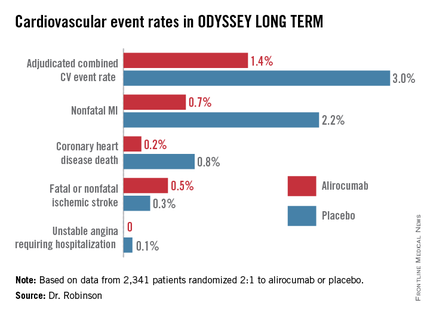
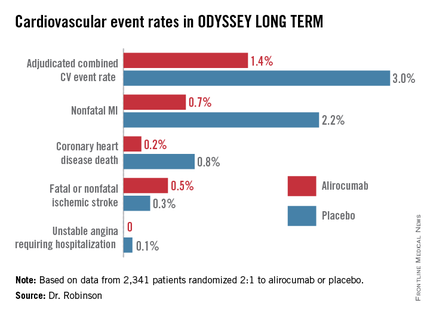
In the interim post-hoc efficacy analysis at 65 weeks, the combined rate of cardiac death, nonfatal MI, stroke, and unstable angina requiring hospitalization was 1.4% in the alirocumab arm compared to 3.0% in placebo-treated controls, for a highly significant 54% relative risk reduction (see graphic).
At 24 weeks, the alirocumab group showed a mean 62% reduction in LDL compared to placebo, a difference that remained constant at 52 weeks. The average LDL level at 52 weeks in the alirocumab group was 53 mg/dL, down from 123 mg/dL on active treatment at baseline; 79% of alirocumab-treated patients achieved an LDL below 70 mg/dL.
The incidence and types of adverse events in the alirocumab arm were essentially the same as with placebo, with no signal of problems in any domains, including neurocognitive function or allergic reactions.
ODYSSEY FH I and FH II
In a separate presentation, Dr. Michel Farnier reported on the alirocumab experience in 735 patients with heterozygous familial hypercholesterolemia in two phase III trials known as ODYSSEY FH I and FH II. At baseline, all were above their LDL goal despite maximally tolerated statin therapy, in two-thirds of cases with add-on ezetimibe. Participants were randomized 2:1 to add-on alirocumab at 75 mg every 2 weeks or to placebo.
The alirocumab-treated patients had 58% and 51% reductions in LDL, compared to actively treated controls at 24 weeks in the FH I and FH II trials. Of the alirocumab-treated patients, 72% and 81% achieved their prespecified LDL goal at 24 weeks, compared with 2% and 11% of controls.
“We have never before seen these kinds of percentages of patients with familial hypercholesterolemia reaching these LDL levels,” commented Dr. Farnier of Point Medical in Dijon, France.
ODYSSEY COMBO II
At the same hot-line clinical trials session, Dr. Christopher P. Cannon reported that alirocumab markedly outperformed ezetimibe as add-on therapy in the 720-patient, phase III, double-blind ODYSSEY COMBO II trial.
In this study, patients at very high CV risk who were unable to reach their desired goal of an LDL below 70 mg/dL despite maximum tolerated statin doses were randomized 2:1 to alirocumab at 75 mg once every 2 weeks or oral ezetimibe (Zetia) at its approved dose of 10 mg/day as an active comparator. Each participant also received placebo therapy.
By week 24, patients on alirocumab plus high-dose statin averaged a 51% reduction in LDL compared to baseline, versus a 21% reduction with ezetimibe plus statin. These effects were maintained at 1 year, with no evidence of tolerance.
Of patients on alirocumab, 77% achieved an LDL goal of less than 70 mg/dL at week 24, compared with 45% on ezetimibe. In addition, 60% of the alirocumab group had an LDL below 50 mg/dL, as did 15% on ezetimibe.
The study design called for patients in the alirocumab group who still had an LDL above 70 mg/dL at week 12 to be uptitrated from 75 mg to 150 mg every 2 weeks. But only 20% of patients needed to do so, according to Dr. Cannon, professor of medicine at Harvard University, Boston.
Will high-risk patient adhere long-term to treatment by self-injection? Dr. Cannon thinks so. He noted that 85% of patients in ODYSSEY COMBO II remained adherent to the biweekly self-injection protocol through 1 year.
“That has been a very pleasant surprise,” the cardiologist said. “The notion of injections for cholesterol management is foreign. It was a big surprise to us that patients really did it.”
‘Great news’ from alirocumab
The alirocumab results in the heterozygous familial hypercholesterolemia trials are “great news for patients with this disease,” discussant Dr. Robert M. Califf said. He noted that recent estimates put the prevalence of heterozygous familial hypercholesterolemia at roughly 1 in 250 persons in the general population, making the genetic disorder considerably more common than most physicians realize.
“These are people who have a terrible disease where a massive reduction in LDL, it seems to me, is clearly worthwhile,” commented Dr. Califf, professor of medicine and vice chancellor for clinical and translational research at Duke University in Durham, N.C.
As for Dr. Robinson’s ODYSSEY LONG TERM data showing a 54% reduction in major CV events, he said “It’s alluring. It looks great. It looks fantastic. And it sets up the large events trial. The only caution out of all of this from my perspective is that any study with less than 100 events is something that should be regarded with great interest but is not definitive.”
If approved, alirocumab could see widespread use, especially if the ODYSSEY OUTCOMES results prove positive. After all, heterozygous familial hypercholesterolemia is now recognized to be one of the most common of all inherited diseases. And Dr. Cannon said that in clinical trials in post-acute coronary syndrome patients placed on high-dose statins, it’s common for only about 40% to achieve an LDL level below 70 mg/dL. In clinical practice, the rate is probably even lower.*
“Down the line I think this level of LDL lowering is needed very badly. To get high-risk patients who have high cholesterol despite maximally dosed statins or statin-intolerance down to an LDL level of 50 mg/dL would be a pretty good thing. This will be applicable to millions of patients,” he predicted.*
Dr. Robinson said that at the American Heart Association meeting this November she and her ODYSSEY LONG TERM coinvestigators plan to present subgroup analyses looking at alirocumab efficacy and safety in patients with achieved LDL levels below 25 and even 15 mg/dL.
Dr. Robinson, Dr. Cannon, and Dr. Farnier reported receiving research grants and consultants’ fees from Sanofi and Regeneron as well as other pharmaceutical companies. Dr. Califf reported having no financial conflicts.
*CORRECTION: An earlier version of this story misattributed these statements.
BARCELONA – When added to maximally tolerated statin therapy, the investigational PCSK9 inhibitor alirocumab resulted in a further 54% reduction in major cardiovascular events among high-cardiovascular-risk patients, based on a post-hoc analysis of a large randomized controlled Phase-3 trial.
The ODYSSEY LONG TERM trial is the largest and longest study of a PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor to report results to date, with roughly 1,900 patient-years of double-blind exposure to alirocumab. And although the ongoing trial is primarily a safety study, it is also now the first PCSK9 trial to provide what everyone watching the development of this novel drug class has been eagerly awaiting: clinical outcomes data, albeit in this case from a post-hoc secondary analysis.
“This is the first trial with any of the PCSK9 inhibitors to suggest that there will be a further significant reduction in cardiovascular events when added on to maximized statin therapy,” Dr. Jennifer G. Robinson said in presenting interim results of ODYSSEY LONG TERM at the annual congress of the European Society of Cardiology.
“We’re on the right track in terms of trying to achieve further reduction in cardiovascular events through additional lipid lowering. But this is not the definitive evidence. We need the prospective outcomes trials to validate this data and also to establish the long-term safety of these drugs when added to the statins,” cautioned Dr. Robinson, professor of epidemiology and of medicine and director of the prevention intervention center at the University of Iowa, Iowa City.
Nonetheless, on the basis of the dramatic LDL-lowering and reassuring evidence of safety shown in ODYSSEY LONG TERM and the other double-blind phase III trials presented at the congress, Sanofi and Regeneron announced plans to file for U.S. and European Union marketing approval of alirocumab before the end of the year. The proposed indication will be for LDL lowering, which regulatory agencies have accepted as a surrogate endpoint for prevention of clinical events.
Meanwhile, the definitive ODYSSEY OUTCOMES trial is underway in 18,000 patients with acute coronary syndromes, with prospective evaluation of CV outcomes as its primary endpoint. The composite endpoint employed in the big OUTCOMES trial is identical to that used in the ODYSSEY LONG TERM post hoc analysis.
ODYSSEY LONG TERM includes 2,341 patients at high CV risk and an LDL level greater than 70 mg/dL despite maximally tolerated statin therapy. The patients fall into two categories: those with heterozygous familial hypercholesterolemia and others at very high risk because of known coronary heart disease. Participants were randomized 2:1 to 150 mg of alirocumab by self-administered subcutaneous injection at home every 2 weeks or placebo in addition to their statin.
In the interim post-hoc efficacy analysis at 65 weeks, the combined rate of cardiac death, nonfatal MI, stroke, and unstable angina requiring hospitalization was 1.4% in the alirocumab arm compared to 3.0% in placebo-treated controls, for a highly significant 54% relative risk reduction (see graphic).
At 24 weeks, the alirocumab group showed a mean 62% reduction in LDL compared to placebo, a difference that remained constant at 52 weeks. The average LDL level at 52 weeks in the alirocumab group was 53 mg/dL, down from 123 mg/dL on active treatment at baseline; 79% of alirocumab-treated patients achieved an LDL below 70 mg/dL.
The incidence and types of adverse events in the alirocumab arm were essentially the same as with placebo, with no signal of problems in any domains, including neurocognitive function or allergic reactions.
ODYSSEY FH I and FH II
In a separate presentation, Dr. Michel Farnier reported on the alirocumab experience in 735 patients with heterozygous familial hypercholesterolemia in two phase III trials known as ODYSSEY FH I and FH II. At baseline, all were above their LDL goal despite maximally tolerated statin therapy, in two-thirds of cases with add-on ezetimibe. Participants were randomized 2:1 to add-on alirocumab at 75 mg every 2 weeks or to placebo.
The alirocumab-treated patients had 58% and 51% reductions in LDL, compared to actively treated controls at 24 weeks in the FH I and FH II trials. Of the alirocumab-treated patients, 72% and 81% achieved their prespecified LDL goal at 24 weeks, compared with 2% and 11% of controls.
“We have never before seen these kinds of percentages of patients with familial hypercholesterolemia reaching these LDL levels,” commented Dr. Farnier of Point Medical in Dijon, France.
ODYSSEY COMBO II
At the same hot-line clinical trials session, Dr. Christopher P. Cannon reported that alirocumab markedly outperformed ezetimibe as add-on therapy in the 720-patient, phase III, double-blind ODYSSEY COMBO II trial.
In this study, patients at very high CV risk who were unable to reach their desired goal of an LDL below 70 mg/dL despite maximum tolerated statin doses were randomized 2:1 to alirocumab at 75 mg once every 2 weeks or oral ezetimibe (Zetia) at its approved dose of 10 mg/day as an active comparator. Each participant also received placebo therapy.
By week 24, patients on alirocumab plus high-dose statin averaged a 51% reduction in LDL compared to baseline, versus a 21% reduction with ezetimibe plus statin. These effects were maintained at 1 year, with no evidence of tolerance.
Of patients on alirocumab, 77% achieved an LDL goal of less than 70 mg/dL at week 24, compared with 45% on ezetimibe. In addition, 60% of the alirocumab group had an LDL below 50 mg/dL, as did 15% on ezetimibe.
The study design called for patients in the alirocumab group who still had an LDL above 70 mg/dL at week 12 to be uptitrated from 75 mg to 150 mg every 2 weeks. But only 20% of patients needed to do so, according to Dr. Cannon, professor of medicine at Harvard University, Boston.
Will high-risk patient adhere long-term to treatment by self-injection? Dr. Cannon thinks so. He noted that 85% of patients in ODYSSEY COMBO II remained adherent to the biweekly self-injection protocol through 1 year.
“That has been a very pleasant surprise,” the cardiologist said. “The notion of injections for cholesterol management is foreign. It was a big surprise to us that patients really did it.”
‘Great news’ from alirocumab
The alirocumab results in the heterozygous familial hypercholesterolemia trials are “great news for patients with this disease,” discussant Dr. Robert M. Califf said. He noted that recent estimates put the prevalence of heterozygous familial hypercholesterolemia at roughly 1 in 250 persons in the general population, making the genetic disorder considerably more common than most physicians realize.
“These are people who have a terrible disease where a massive reduction in LDL, it seems to me, is clearly worthwhile,” commented Dr. Califf, professor of medicine and vice chancellor for clinical and translational research at Duke University in Durham, N.C.
As for Dr. Robinson’s ODYSSEY LONG TERM data showing a 54% reduction in major CV events, he said “It’s alluring. It looks great. It looks fantastic. And it sets up the large events trial. The only caution out of all of this from my perspective is that any study with less than 100 events is something that should be regarded with great interest but is not definitive.”
If approved, alirocumab could see widespread use, especially if the ODYSSEY OUTCOMES results prove positive. After all, heterozygous familial hypercholesterolemia is now recognized to be one of the most common of all inherited diseases. And Dr. Cannon said that in clinical trials in post-acute coronary syndrome patients placed on high-dose statins, it’s common for only about 40% to achieve an LDL level below 70 mg/dL. In clinical practice, the rate is probably even lower.*
“Down the line I think this level of LDL lowering is needed very badly. To get high-risk patients who have high cholesterol despite maximally dosed statins or statin-intolerance down to an LDL level of 50 mg/dL would be a pretty good thing. This will be applicable to millions of patients,” he predicted.*
Dr. Robinson said that at the American Heart Association meeting this November she and her ODYSSEY LONG TERM coinvestigators plan to present subgroup analyses looking at alirocumab efficacy and safety in patients with achieved LDL levels below 25 and even 15 mg/dL.
Dr. Robinson, Dr. Cannon, and Dr. Farnier reported receiving research grants and consultants’ fees from Sanofi and Regeneron as well as other pharmaceutical companies. Dr. Califf reported having no financial conflicts.
*CORRECTION: An earlier version of this story misattributed these statements.
BARCELONA – When added to maximally tolerated statin therapy, the investigational PCSK9 inhibitor alirocumab resulted in a further 54% reduction in major cardiovascular events among high-cardiovascular-risk patients, based on a post-hoc analysis of a large randomized controlled Phase-3 trial.
The ODYSSEY LONG TERM trial is the largest and longest study of a PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor to report results to date, with roughly 1,900 patient-years of double-blind exposure to alirocumab. And although the ongoing trial is primarily a safety study, it is also now the first PCSK9 trial to provide what everyone watching the development of this novel drug class has been eagerly awaiting: clinical outcomes data, albeit in this case from a post-hoc secondary analysis.
“This is the first trial with any of the PCSK9 inhibitors to suggest that there will be a further significant reduction in cardiovascular events when added on to maximized statin therapy,” Dr. Jennifer G. Robinson said in presenting interim results of ODYSSEY LONG TERM at the annual congress of the European Society of Cardiology.
“We’re on the right track in terms of trying to achieve further reduction in cardiovascular events through additional lipid lowering. But this is not the definitive evidence. We need the prospective outcomes trials to validate this data and also to establish the long-term safety of these drugs when added to the statins,” cautioned Dr. Robinson, professor of epidemiology and of medicine and director of the prevention intervention center at the University of Iowa, Iowa City.
Nonetheless, on the basis of the dramatic LDL-lowering and reassuring evidence of safety shown in ODYSSEY LONG TERM and the other double-blind phase III trials presented at the congress, Sanofi and Regeneron announced plans to file for U.S. and European Union marketing approval of alirocumab before the end of the year. The proposed indication will be for LDL lowering, which regulatory agencies have accepted as a surrogate endpoint for prevention of clinical events.
Meanwhile, the definitive ODYSSEY OUTCOMES trial is underway in 18,000 patients with acute coronary syndromes, with prospective evaluation of CV outcomes as its primary endpoint. The composite endpoint employed in the big OUTCOMES trial is identical to that used in the ODYSSEY LONG TERM post hoc analysis.
ODYSSEY LONG TERM includes 2,341 patients at high CV risk and an LDL level greater than 70 mg/dL despite maximally tolerated statin therapy. The patients fall into two categories: those with heterozygous familial hypercholesterolemia and others at very high risk because of known coronary heart disease. Participants were randomized 2:1 to 150 mg of alirocumab by self-administered subcutaneous injection at home every 2 weeks or placebo in addition to their statin.
In the interim post-hoc efficacy analysis at 65 weeks, the combined rate of cardiac death, nonfatal MI, stroke, and unstable angina requiring hospitalization was 1.4% in the alirocumab arm compared to 3.0% in placebo-treated controls, for a highly significant 54% relative risk reduction (see graphic).
At 24 weeks, the alirocumab group showed a mean 62% reduction in LDL compared to placebo, a difference that remained constant at 52 weeks. The average LDL level at 52 weeks in the alirocumab group was 53 mg/dL, down from 123 mg/dL on active treatment at baseline; 79% of alirocumab-treated patients achieved an LDL below 70 mg/dL.
The incidence and types of adverse events in the alirocumab arm were essentially the same as with placebo, with no signal of problems in any domains, including neurocognitive function or allergic reactions.
ODYSSEY FH I and FH II
In a separate presentation, Dr. Michel Farnier reported on the alirocumab experience in 735 patients with heterozygous familial hypercholesterolemia in two phase III trials known as ODYSSEY FH I and FH II. At baseline, all were above their LDL goal despite maximally tolerated statin therapy, in two-thirds of cases with add-on ezetimibe. Participants were randomized 2:1 to add-on alirocumab at 75 mg every 2 weeks or to placebo.
The alirocumab-treated patients had 58% and 51% reductions in LDL, compared to actively treated controls at 24 weeks in the FH I and FH II trials. Of the alirocumab-treated patients, 72% and 81% achieved their prespecified LDL goal at 24 weeks, compared with 2% and 11% of controls.
“We have never before seen these kinds of percentages of patients with familial hypercholesterolemia reaching these LDL levels,” commented Dr. Farnier of Point Medical in Dijon, France.
ODYSSEY COMBO II
At the same hot-line clinical trials session, Dr. Christopher P. Cannon reported that alirocumab markedly outperformed ezetimibe as add-on therapy in the 720-patient, phase III, double-blind ODYSSEY COMBO II trial.
In this study, patients at very high CV risk who were unable to reach their desired goal of an LDL below 70 mg/dL despite maximum tolerated statin doses were randomized 2:1 to alirocumab at 75 mg once every 2 weeks or oral ezetimibe (Zetia) at its approved dose of 10 mg/day as an active comparator. Each participant also received placebo therapy.
By week 24, patients on alirocumab plus high-dose statin averaged a 51% reduction in LDL compared to baseline, versus a 21% reduction with ezetimibe plus statin. These effects were maintained at 1 year, with no evidence of tolerance.
Of patients on alirocumab, 77% achieved an LDL goal of less than 70 mg/dL at week 24, compared with 45% on ezetimibe. In addition, 60% of the alirocumab group had an LDL below 50 mg/dL, as did 15% on ezetimibe.
The study design called for patients in the alirocumab group who still had an LDL above 70 mg/dL at week 12 to be uptitrated from 75 mg to 150 mg every 2 weeks. But only 20% of patients needed to do so, according to Dr. Cannon, professor of medicine at Harvard University, Boston.
Will high-risk patient adhere long-term to treatment by self-injection? Dr. Cannon thinks so. He noted that 85% of patients in ODYSSEY COMBO II remained adherent to the biweekly self-injection protocol through 1 year.
“That has been a very pleasant surprise,” the cardiologist said. “The notion of injections for cholesterol management is foreign. It was a big surprise to us that patients really did it.”
‘Great news’ from alirocumab
The alirocumab results in the heterozygous familial hypercholesterolemia trials are “great news for patients with this disease,” discussant Dr. Robert M. Califf said. He noted that recent estimates put the prevalence of heterozygous familial hypercholesterolemia at roughly 1 in 250 persons in the general population, making the genetic disorder considerably more common than most physicians realize.
“These are people who have a terrible disease where a massive reduction in LDL, it seems to me, is clearly worthwhile,” commented Dr. Califf, professor of medicine and vice chancellor for clinical and translational research at Duke University in Durham, N.C.
As for Dr. Robinson’s ODYSSEY LONG TERM data showing a 54% reduction in major CV events, he said “It’s alluring. It looks great. It looks fantastic. And it sets up the large events trial. The only caution out of all of this from my perspective is that any study with less than 100 events is something that should be regarded with great interest but is not definitive.”
If approved, alirocumab could see widespread use, especially if the ODYSSEY OUTCOMES results prove positive. After all, heterozygous familial hypercholesterolemia is now recognized to be one of the most common of all inherited diseases. And Dr. Cannon said that in clinical trials in post-acute coronary syndrome patients placed on high-dose statins, it’s common for only about 40% to achieve an LDL level below 70 mg/dL. In clinical practice, the rate is probably even lower.*
“Down the line I think this level of LDL lowering is needed very badly. To get high-risk patients who have high cholesterol despite maximally dosed statins or statin-intolerance down to an LDL level of 50 mg/dL would be a pretty good thing. This will be applicable to millions of patients,” he predicted.*
Dr. Robinson said that at the American Heart Association meeting this November she and her ODYSSEY LONG TERM coinvestigators plan to present subgroup analyses looking at alirocumab efficacy and safety in patients with achieved LDL levels below 25 and even 15 mg/dL.
Dr. Robinson, Dr. Cannon, and Dr. Farnier reported receiving research grants and consultants’ fees from Sanofi and Regeneron as well as other pharmaceutical companies. Dr. Califf reported having no financial conflicts.
*CORRECTION: An earlier version of this story misattributed these statements.
AT THE ESC CONGRESS 2014
Key clinical point: The lower-is-better approach to LDL reduction gets a big boost from a study that showed adding alirocumab to maximally tolerated statin therapy was associated with 54% fewer major adverse cardiovascular events compared to statin plus placebo in high-cardiovascular-risk patients.
Major finding: The incidence of the composite cardiovascular event endpoint at 65 weeks was 1.4% in those on alirocumab plus maximally tolerated statin therapy and 3.0% in those on placebo plus statin.
Data source: This was an interim post hoc analysis from the Phase-3, double-blind, randomized, prospective ODYSSEY LONG TERM trial of more than 2,300 randomized patients.
Disclosures: The ODYSSEY clinical trials program is sponsored by Sanofi and Regeneron. The study presenters reported receiving research grants and consultants’ fees from those and other companies.
COPPS-2 curtails colchicine enthusiasm in cardiac surgery
Patients undergoing cardiac surgery who took colchicine had significantly less postpericardiotomy syndrome than did those on placebo, but this protective effect did not extend to postoperative atrial fibrillation and pericardial or pleural effusions in the double-blind COPPS-2 trial.
The failure of colchicine to prevent postoperative atrial fibrillation (AF) was probably due to more frequent adverse events (36 vs. 21 with placebo), especially gastrointestinal intolerance (26 vs. 12), and drug discontinuation (39 vs. 32), since a prespecified on-treatment analysis showed a significant reduction in AF in patients tolerating the drug, Dr. Massimo Imazio reported at the annual congress of the European Society of Cardiology.
"The high rate of adverse effects is a reason for concern and suggests that colchicine should be considered only in well-selected patients," Dr. Imazio and his associates wrote in an article on COPPS-2 simultaneously published online (JAMA 2014 [doi:10.1001/jama.2014.11026]).
Colchicine has been a promising strategy for postpericardiotomy syndrome prevention, besting methylprednisolone and aspirin in a large meta-analysis (Am. J. Cardiol. 2011;108:575-9).
In the largest trial, COPPS (Colchicine for the Prevention of the Postpericardiotomy Syndrome), Dr. Imazio reported that colchicine significantly reduced the incidence of postpericardiotomy syndrome (8.9% vs. 21.1%), postoperative pericardial effusions (relative risk reduction, 43.9%), and pleural effusions (RRR, 52.3%) at 12 months, compared with placebo (Am. Heart J. 2011;162:527-32 and Eur. Heart J. 2010;31:2749-54). Colchicine was given for 1 month, beginning on the third postoperative day with a 1-mg twice-daily loading dose.
In COPPS-2, the 360 consecutive candidates for cardiac surgery also were given colchicine or placebo for 1 month, but treatment was started 48-72 hours before surgery to pretreat patients and improve colchicine’s ability to prevent postoperative systemic inflammation and its complications.
Colchicine also was administered using weight-based dosing (0.5 mg twice daily in patients weighing at least 70 kg or 0.5 mg once daily in those under 70 kg), and they avoided the loading dose in an effort to improve adherence.
"However, we observed a 2-fold increase of adverse effects and study drug discontinuations compared with those reported in the COPPS trial, likely due to significant vulnerability of patients in the perioperative phase, when the use of antibiotics and proton pump inhibitors is common and also increases the risk of gastrointestinal effects (e.g., diarrhea)," explained Dr. Imazio of Maria Vittoria Hospital and the University of Torino (Italy).
Still, colchicine provided significant protection in the COPPS-2 primary outcome of postpericardiotomy syndrome, compared with placebo (19.4% vs. 29.4%; 95% confidence interval, 1.1%-18.7%). The number needed to treat was 10.
The outcome did not differ significantly among predetermined subgroups based on age, sex, and presence or absence of pericardial effusion, although colchicine was especially efficacious in the setting of systemic inflammation with elevated C-reactive protein, the authors noted.
The intention-to-treat analysis revealed no significant differences between the colchicine and placebo groups for postoperative AF (33.9% vs. 41.7%; 95% CI, –2.2%-17.6%) or postoperative pericardial/pleural effusion (57.2% vs. 58.9%; 95% CI, –8.5%-11.7%).
The prespecified on-treatment analysis, however, showed a 14.2% absolute difference in postoperative AF, favoring colchicine over placebo (27% vs. 41.2%; 95% CI, 3.3%-24.7%).
"While the efficacy of colchicine for postpericardiotomy syndrome prevention is confirmed, the extent of efficacy for postoperative AF needs to be further investigated in future trials," Dr. Imazio stated.
Ongoing studies also will better clarify the potential of colchicine using lower doses that may be better tolerated.
The 360 patients were evenly randomized from 11 centers in Italy between March 2012 and March 2014. Their mean age was 67.5 years, 69% were men, and 36% had planned valvular surgery. Key exclusion criteria were absence of sinus rhythm at enrollment, urgent cardiac surgery, cardiac transplantation, and contraindications to colchicine.
COPPS-2 was supported by the Italian National Health Service and FARGIM. Acarpia provided the study drug. Dr. Imazio reported no conflicts of interest. A coauthor reported consultancy for Servier, serving on an advisory board for Boehringer Ingelheim, and lecturer fees from Abbott, AstraZeneca, Merck, Serono, Richter Gedeon, and Teva.
Patients undergoing cardiac surgery who took colchicine had significantly less postpericardiotomy syndrome than did those on placebo, but this protective effect did not extend to postoperative atrial fibrillation and pericardial or pleural effusions in the double-blind COPPS-2 trial.
The failure of colchicine to prevent postoperative atrial fibrillation (AF) was probably due to more frequent adverse events (36 vs. 21 with placebo), especially gastrointestinal intolerance (26 vs. 12), and drug discontinuation (39 vs. 32), since a prespecified on-treatment analysis showed a significant reduction in AF in patients tolerating the drug, Dr. Massimo Imazio reported at the annual congress of the European Society of Cardiology.
"The high rate of adverse effects is a reason for concern and suggests that colchicine should be considered only in well-selected patients," Dr. Imazio and his associates wrote in an article on COPPS-2 simultaneously published online (JAMA 2014 [doi:10.1001/jama.2014.11026]).
Colchicine has been a promising strategy for postpericardiotomy syndrome prevention, besting methylprednisolone and aspirin in a large meta-analysis (Am. J. Cardiol. 2011;108:575-9).
In the largest trial, COPPS (Colchicine for the Prevention of the Postpericardiotomy Syndrome), Dr. Imazio reported that colchicine significantly reduced the incidence of postpericardiotomy syndrome (8.9% vs. 21.1%), postoperative pericardial effusions (relative risk reduction, 43.9%), and pleural effusions (RRR, 52.3%) at 12 months, compared with placebo (Am. Heart J. 2011;162:527-32 and Eur. Heart J. 2010;31:2749-54). Colchicine was given for 1 month, beginning on the third postoperative day with a 1-mg twice-daily loading dose.
In COPPS-2, the 360 consecutive candidates for cardiac surgery also were given colchicine or placebo for 1 month, but treatment was started 48-72 hours before surgery to pretreat patients and improve colchicine’s ability to prevent postoperative systemic inflammation and its complications.
Colchicine also was administered using weight-based dosing (0.5 mg twice daily in patients weighing at least 70 kg or 0.5 mg once daily in those under 70 kg), and they avoided the loading dose in an effort to improve adherence.
"However, we observed a 2-fold increase of adverse effects and study drug discontinuations compared with those reported in the COPPS trial, likely due to significant vulnerability of patients in the perioperative phase, when the use of antibiotics and proton pump inhibitors is common and also increases the risk of gastrointestinal effects (e.g., diarrhea)," explained Dr. Imazio of Maria Vittoria Hospital and the University of Torino (Italy).
Still, colchicine provided significant protection in the COPPS-2 primary outcome of postpericardiotomy syndrome, compared with placebo (19.4% vs. 29.4%; 95% confidence interval, 1.1%-18.7%). The number needed to treat was 10.
The outcome did not differ significantly among predetermined subgroups based on age, sex, and presence or absence of pericardial effusion, although colchicine was especially efficacious in the setting of systemic inflammation with elevated C-reactive protein, the authors noted.
The intention-to-treat analysis revealed no significant differences between the colchicine and placebo groups for postoperative AF (33.9% vs. 41.7%; 95% CI, –2.2%-17.6%) or postoperative pericardial/pleural effusion (57.2% vs. 58.9%; 95% CI, –8.5%-11.7%).
The prespecified on-treatment analysis, however, showed a 14.2% absolute difference in postoperative AF, favoring colchicine over placebo (27% vs. 41.2%; 95% CI, 3.3%-24.7%).
"While the efficacy of colchicine for postpericardiotomy syndrome prevention is confirmed, the extent of efficacy for postoperative AF needs to be further investigated in future trials," Dr. Imazio stated.
Ongoing studies also will better clarify the potential of colchicine using lower doses that may be better tolerated.
The 360 patients were evenly randomized from 11 centers in Italy between March 2012 and March 2014. Their mean age was 67.5 years, 69% were men, and 36% had planned valvular surgery. Key exclusion criteria were absence of sinus rhythm at enrollment, urgent cardiac surgery, cardiac transplantation, and contraindications to colchicine.
COPPS-2 was supported by the Italian National Health Service and FARGIM. Acarpia provided the study drug. Dr. Imazio reported no conflicts of interest. A coauthor reported consultancy for Servier, serving on an advisory board for Boehringer Ingelheim, and lecturer fees from Abbott, AstraZeneca, Merck, Serono, Richter Gedeon, and Teva.
Patients undergoing cardiac surgery who took colchicine had significantly less postpericardiotomy syndrome than did those on placebo, but this protective effect did not extend to postoperative atrial fibrillation and pericardial or pleural effusions in the double-blind COPPS-2 trial.
The failure of colchicine to prevent postoperative atrial fibrillation (AF) was probably due to more frequent adverse events (36 vs. 21 with placebo), especially gastrointestinal intolerance (26 vs. 12), and drug discontinuation (39 vs. 32), since a prespecified on-treatment analysis showed a significant reduction in AF in patients tolerating the drug, Dr. Massimo Imazio reported at the annual congress of the European Society of Cardiology.
"The high rate of adverse effects is a reason for concern and suggests that colchicine should be considered only in well-selected patients," Dr. Imazio and his associates wrote in an article on COPPS-2 simultaneously published online (JAMA 2014 [doi:10.1001/jama.2014.11026]).
Colchicine has been a promising strategy for postpericardiotomy syndrome prevention, besting methylprednisolone and aspirin in a large meta-analysis (Am. J. Cardiol. 2011;108:575-9).
In the largest trial, COPPS (Colchicine for the Prevention of the Postpericardiotomy Syndrome), Dr. Imazio reported that colchicine significantly reduced the incidence of postpericardiotomy syndrome (8.9% vs. 21.1%), postoperative pericardial effusions (relative risk reduction, 43.9%), and pleural effusions (RRR, 52.3%) at 12 months, compared with placebo (Am. Heart J. 2011;162:527-32 and Eur. Heart J. 2010;31:2749-54). Colchicine was given for 1 month, beginning on the third postoperative day with a 1-mg twice-daily loading dose.
In COPPS-2, the 360 consecutive candidates for cardiac surgery also were given colchicine or placebo for 1 month, but treatment was started 48-72 hours before surgery to pretreat patients and improve colchicine’s ability to prevent postoperative systemic inflammation and its complications.
Colchicine also was administered using weight-based dosing (0.5 mg twice daily in patients weighing at least 70 kg or 0.5 mg once daily in those under 70 kg), and they avoided the loading dose in an effort to improve adherence.
"However, we observed a 2-fold increase of adverse effects and study drug discontinuations compared with those reported in the COPPS trial, likely due to significant vulnerability of patients in the perioperative phase, when the use of antibiotics and proton pump inhibitors is common and also increases the risk of gastrointestinal effects (e.g., diarrhea)," explained Dr. Imazio of Maria Vittoria Hospital and the University of Torino (Italy).
Still, colchicine provided significant protection in the COPPS-2 primary outcome of postpericardiotomy syndrome, compared with placebo (19.4% vs. 29.4%; 95% confidence interval, 1.1%-18.7%). The number needed to treat was 10.
The outcome did not differ significantly among predetermined subgroups based on age, sex, and presence or absence of pericardial effusion, although colchicine was especially efficacious in the setting of systemic inflammation with elevated C-reactive protein, the authors noted.
The intention-to-treat analysis revealed no significant differences between the colchicine and placebo groups for postoperative AF (33.9% vs. 41.7%; 95% CI, –2.2%-17.6%) or postoperative pericardial/pleural effusion (57.2% vs. 58.9%; 95% CI, –8.5%-11.7%).
The prespecified on-treatment analysis, however, showed a 14.2% absolute difference in postoperative AF, favoring colchicine over placebo (27% vs. 41.2%; 95% CI, 3.3%-24.7%).
"While the efficacy of colchicine for postpericardiotomy syndrome prevention is confirmed, the extent of efficacy for postoperative AF needs to be further investigated in future trials," Dr. Imazio stated.
Ongoing studies also will better clarify the potential of colchicine using lower doses that may be better tolerated.
The 360 patients were evenly randomized from 11 centers in Italy between March 2012 and March 2014. Their mean age was 67.5 years, 69% were men, and 36% had planned valvular surgery. Key exclusion criteria were absence of sinus rhythm at enrollment, urgent cardiac surgery, cardiac transplantation, and contraindications to colchicine.
COPPS-2 was supported by the Italian National Health Service and FARGIM. Acarpia provided the study drug. Dr. Imazio reported no conflicts of interest. A coauthor reported consultancy for Servier, serving on an advisory board for Boehringer Ingelheim, and lecturer fees from Abbott, AstraZeneca, Merck, Serono, Richter Gedeon, and Teva.
FROM THE ESC CONGRESS 2014
Key clinical point: Perioperative use of colchicine should be considered only in well-selected patients.
Major finding: Perioperative colchicine use cut the incidence of postpericardiotomy syndrome, but not postoperative atrial fibrillation or pericardial/pleural effusion.
Data source: Double-blind, randomized clinical trial in 360 consecutive candidates for heart surgery.
Disclosures: COPPS-2 was supported by the Italian National Health Service and FARGIM. Acarpia provided the study drug. Dr. Imazio reported no conflicts of interest. A coauthor reported consultancy for Servier, serving on an advisory board for Boehringer Ingelheim, and lecturer fees from Abbott, AstraZeneca, Merck, Serono, Richter Gedeon, and Teva.
Arch replacement with FET not worse when acute
TORONTO – Operative mortality with total aortic arch replacement using a four-branched graft and frozen elephant trunk implantation (Sun’s procedure) was 6.5%, including those whose type A aortic dissection was defined as acute.
Operative mortality was higher in acute versus chronic type A aortic dissection (TAAD) patients undergoing the procedure (8.1% vs. 4.3%; P = .031), as was the incidence of stroke (2.2% vs. 0.6%; P = .046), and respiratory complications (20.8% vs. 8.6%; P less than .001).
However, although the risk of operative mortality in acute patients was 1.95 times higher than for chronic patients, in multivariate analysis, acuteness was not identified as a significant risk factor for operative mortality (odds ratio, 1.67; P = .152).
The factors identified as increasing risk of operative mortality were coexisting cerebrovascular disease; malperfusion of the brain, kidneys, spinal cord, and viscera; concomitant extra-anatomic bypass; and cardiopulmonary bypass time exceeding 180 minutes.
"This study proves the safety of frozen elephant trunk with total arch replacement," said Dr. Wei-Guo Ma of Yale University, New Haven, Conn.
"Operative mortality was not affected by either the acute or chronic phase. Instead it was affected by seven other factors, such as prior CVD [cerebrovascular disease], malperfusion, and longer CPB [cardiopulmonary bypass] time.
"If a patient comes without those risk factors, surgeons can go ahead and perform this emergent frozen elephant trunk for him without fear of imposing greater risk of mortality," he said.
Standard TAAD remains a highly lethal condition, with the greatest surgical risk seen during the acute phase. Although some progress has been made, surgeons continue to debate the optimal surgical approach to TAAD, in particular the extent of distal aortic repair. Some advocate a more limited approach of hemiarch repair only, while others propose that total arch repair offers better outcomes.
Sun’s procedure is performed with right axillary artery cannulation for cardiopulmonary bypass and selective antegrade cerebral perfusion, under moderate hypothermic circulatory arrest at 25° C.
The frozen elephant trunk (Cronus, MicroPort Medical, Shanghai, China) is implanted into the descending aorta, followed by total arch replacement using a four-branched vascular graft, with a special sequence for aortic reconstruction (i.e., proximal descending aorta to left carotid artery to ascending aorta to left subclavian artery to innominate artery). Associated operations, including coronary artery bypass grafting, are performed during the cooling phase, if needed.
In this case series, presented by Dr. Ma at the annual meeting of the American Association for Thoracic Surgery, acuteness was defined as an interval between onset of symptoms and surgery of 14 days or less.
TAAD was diagnosed preoperatively by transthoracic echocardiography or computed tomographic angiography, with the location of the intimal tear confirmed during surgery.
The surgeons retrospectively compared early outcomes between acute and chronic TAAD patients after Sun’s procedure, seeking to identify risk factors for operative mortality in both groups and seeking to determine whether acuteness significantly affects operative mortality after this extensive surgical approach.
Between April 2003 and September 2012, Sun’s procedure was performed on 803 patients with acute or chronic TAAD. Mean age was 46 years and 80% of the cohort was male. A total of 456 were classified as acute TAAD patients, with a mean of 5.5 days lapsing between onset of symptoms to surgery (median, 4.1 days), and 347 were chronic, with 197 days lapsing between onset of symptoms and surgery (median, 38 days).
Clinically apparent malperfusion was common, seen in 12.6% of cases, 12.3% of the acute arm and 9.2% of the chronic arm. Patients with malperfusion had an overall mortality of 19.3% (25% in the acute arm and 9.4% in the chronic arm; P less than .001).
"Visceral malperfusion tended to be the most lethal, with five of seven patients dying," reported Dr. Ma. He also noted the young age of their cohort as compared to other regions of the world: 88.8% of patients were under 60 years of age.
Acute, minus natural selection
The invited discussant on the abstract, Dr. Malakh L. Shrestha took issue with the study’s conclusion that acuteness did not affect operative mortality. Dr. Shrestha is the division manager of valvular and coronary artery surgery at the Hannover (Germany) Medical School.
"As a high volume center, what we’ve learned is that acute and chronic aortic dissection patients are two totally different subsets of patients in terms of clinical presentation and mortality. The greatest danger in the acute patient is in the first few hours after the dissection, with the majority of patients dying without surgical intervention."
At Dr. Shrestha’s center in Germany, a high-volume aortic center, they often see patients within the first few hours of their dissection and they’ve found a significantly higher mortality in these patients, compared with chronic TAAD whether an ascending aortic replacement or a frozen elephant trunk procedure is done.
With a median of 4.1 days lapsing between onset of symptoms and surgery in the Ma et al. study, Dr. Shrestha argued that "although on the basis of classification, you can still say they’re acute, there has been some sort of natural selection. So, I think that means, at least for your conclusions, that you need to clarify the statement that there is no difference between acute and chronic, because these are obviously not the same subset of patients that we see in the Western world."
Dr. Ma agreed that natural selection was indeed at play in their series, in that about 80% of their patients were referrals that were transferred in some cases from hundreds of miles away, with many dying en route or before surgery. He also concurred that had their mean and median number of days in their acute cohort been less, indeed, mortality might have been higher.
Dr. Ma reported having no conflicts of interest. Dr. Shrestha is a consultant for Edwards Lifesciences.
TORONTO – Operative mortality with total aortic arch replacement using a four-branched graft and frozen elephant trunk implantation (Sun’s procedure) was 6.5%, including those whose type A aortic dissection was defined as acute.
Operative mortality was higher in acute versus chronic type A aortic dissection (TAAD) patients undergoing the procedure (8.1% vs. 4.3%; P = .031), as was the incidence of stroke (2.2% vs. 0.6%; P = .046), and respiratory complications (20.8% vs. 8.6%; P less than .001).
However, although the risk of operative mortality in acute patients was 1.95 times higher than for chronic patients, in multivariate analysis, acuteness was not identified as a significant risk factor for operative mortality (odds ratio, 1.67; P = .152).
The factors identified as increasing risk of operative mortality were coexisting cerebrovascular disease; malperfusion of the brain, kidneys, spinal cord, and viscera; concomitant extra-anatomic bypass; and cardiopulmonary bypass time exceeding 180 minutes.
"This study proves the safety of frozen elephant trunk with total arch replacement," said Dr. Wei-Guo Ma of Yale University, New Haven, Conn.
"Operative mortality was not affected by either the acute or chronic phase. Instead it was affected by seven other factors, such as prior CVD [cerebrovascular disease], malperfusion, and longer CPB [cardiopulmonary bypass] time.
"If a patient comes without those risk factors, surgeons can go ahead and perform this emergent frozen elephant trunk for him without fear of imposing greater risk of mortality," he said.
Standard TAAD remains a highly lethal condition, with the greatest surgical risk seen during the acute phase. Although some progress has been made, surgeons continue to debate the optimal surgical approach to TAAD, in particular the extent of distal aortic repair. Some advocate a more limited approach of hemiarch repair only, while others propose that total arch repair offers better outcomes.
Sun’s procedure is performed with right axillary artery cannulation for cardiopulmonary bypass and selective antegrade cerebral perfusion, under moderate hypothermic circulatory arrest at 25° C.
The frozen elephant trunk (Cronus, MicroPort Medical, Shanghai, China) is implanted into the descending aorta, followed by total arch replacement using a four-branched vascular graft, with a special sequence for aortic reconstruction (i.e., proximal descending aorta to left carotid artery to ascending aorta to left subclavian artery to innominate artery). Associated operations, including coronary artery bypass grafting, are performed during the cooling phase, if needed.
In this case series, presented by Dr. Ma at the annual meeting of the American Association for Thoracic Surgery, acuteness was defined as an interval between onset of symptoms and surgery of 14 days or less.
TAAD was diagnosed preoperatively by transthoracic echocardiography or computed tomographic angiography, with the location of the intimal tear confirmed during surgery.
The surgeons retrospectively compared early outcomes between acute and chronic TAAD patients after Sun’s procedure, seeking to identify risk factors for operative mortality in both groups and seeking to determine whether acuteness significantly affects operative mortality after this extensive surgical approach.
Between April 2003 and September 2012, Sun’s procedure was performed on 803 patients with acute or chronic TAAD. Mean age was 46 years and 80% of the cohort was male. A total of 456 were classified as acute TAAD patients, with a mean of 5.5 days lapsing between onset of symptoms to surgery (median, 4.1 days), and 347 were chronic, with 197 days lapsing between onset of symptoms and surgery (median, 38 days).
Clinically apparent malperfusion was common, seen in 12.6% of cases, 12.3% of the acute arm and 9.2% of the chronic arm. Patients with malperfusion had an overall mortality of 19.3% (25% in the acute arm and 9.4% in the chronic arm; P less than .001).
"Visceral malperfusion tended to be the most lethal, with five of seven patients dying," reported Dr. Ma. He also noted the young age of their cohort as compared to other regions of the world: 88.8% of patients were under 60 years of age.
Acute, minus natural selection
The invited discussant on the abstract, Dr. Malakh L. Shrestha took issue with the study’s conclusion that acuteness did not affect operative mortality. Dr. Shrestha is the division manager of valvular and coronary artery surgery at the Hannover (Germany) Medical School.
"As a high volume center, what we’ve learned is that acute and chronic aortic dissection patients are two totally different subsets of patients in terms of clinical presentation and mortality. The greatest danger in the acute patient is in the first few hours after the dissection, with the majority of patients dying without surgical intervention."
At Dr. Shrestha’s center in Germany, a high-volume aortic center, they often see patients within the first few hours of their dissection and they’ve found a significantly higher mortality in these patients, compared with chronic TAAD whether an ascending aortic replacement or a frozen elephant trunk procedure is done.
With a median of 4.1 days lapsing between onset of symptoms and surgery in the Ma et al. study, Dr. Shrestha argued that "although on the basis of classification, you can still say they’re acute, there has been some sort of natural selection. So, I think that means, at least for your conclusions, that you need to clarify the statement that there is no difference between acute and chronic, because these are obviously not the same subset of patients that we see in the Western world."
Dr. Ma agreed that natural selection was indeed at play in their series, in that about 80% of their patients were referrals that were transferred in some cases from hundreds of miles away, with many dying en route or before surgery. He also concurred that had their mean and median number of days in their acute cohort been less, indeed, mortality might have been higher.
Dr. Ma reported having no conflicts of interest. Dr. Shrestha is a consultant for Edwards Lifesciences.
TORONTO – Operative mortality with total aortic arch replacement using a four-branched graft and frozen elephant trunk implantation (Sun’s procedure) was 6.5%, including those whose type A aortic dissection was defined as acute.
Operative mortality was higher in acute versus chronic type A aortic dissection (TAAD) patients undergoing the procedure (8.1% vs. 4.3%; P = .031), as was the incidence of stroke (2.2% vs. 0.6%; P = .046), and respiratory complications (20.8% vs. 8.6%; P less than .001).
However, although the risk of operative mortality in acute patients was 1.95 times higher than for chronic patients, in multivariate analysis, acuteness was not identified as a significant risk factor for operative mortality (odds ratio, 1.67; P = .152).
The factors identified as increasing risk of operative mortality were coexisting cerebrovascular disease; malperfusion of the brain, kidneys, spinal cord, and viscera; concomitant extra-anatomic bypass; and cardiopulmonary bypass time exceeding 180 minutes.
"This study proves the safety of frozen elephant trunk with total arch replacement," said Dr. Wei-Guo Ma of Yale University, New Haven, Conn.
"Operative mortality was not affected by either the acute or chronic phase. Instead it was affected by seven other factors, such as prior CVD [cerebrovascular disease], malperfusion, and longer CPB [cardiopulmonary bypass] time.
"If a patient comes without those risk factors, surgeons can go ahead and perform this emergent frozen elephant trunk for him without fear of imposing greater risk of mortality," he said.
Standard TAAD remains a highly lethal condition, with the greatest surgical risk seen during the acute phase. Although some progress has been made, surgeons continue to debate the optimal surgical approach to TAAD, in particular the extent of distal aortic repair. Some advocate a more limited approach of hemiarch repair only, while others propose that total arch repair offers better outcomes.
Sun’s procedure is performed with right axillary artery cannulation for cardiopulmonary bypass and selective antegrade cerebral perfusion, under moderate hypothermic circulatory arrest at 25° C.
The frozen elephant trunk (Cronus, MicroPort Medical, Shanghai, China) is implanted into the descending aorta, followed by total arch replacement using a four-branched vascular graft, with a special sequence for aortic reconstruction (i.e., proximal descending aorta to left carotid artery to ascending aorta to left subclavian artery to innominate artery). Associated operations, including coronary artery bypass grafting, are performed during the cooling phase, if needed.
In this case series, presented by Dr. Ma at the annual meeting of the American Association for Thoracic Surgery, acuteness was defined as an interval between onset of symptoms and surgery of 14 days or less.
TAAD was diagnosed preoperatively by transthoracic echocardiography or computed tomographic angiography, with the location of the intimal tear confirmed during surgery.
The surgeons retrospectively compared early outcomes between acute and chronic TAAD patients after Sun’s procedure, seeking to identify risk factors for operative mortality in both groups and seeking to determine whether acuteness significantly affects operative mortality after this extensive surgical approach.
Between April 2003 and September 2012, Sun’s procedure was performed on 803 patients with acute or chronic TAAD. Mean age was 46 years and 80% of the cohort was male. A total of 456 were classified as acute TAAD patients, with a mean of 5.5 days lapsing between onset of symptoms to surgery (median, 4.1 days), and 347 were chronic, with 197 days lapsing between onset of symptoms and surgery (median, 38 days).
Clinically apparent malperfusion was common, seen in 12.6% of cases, 12.3% of the acute arm and 9.2% of the chronic arm. Patients with malperfusion had an overall mortality of 19.3% (25% in the acute arm and 9.4% in the chronic arm; P less than .001).
"Visceral malperfusion tended to be the most lethal, with five of seven patients dying," reported Dr. Ma. He also noted the young age of their cohort as compared to other regions of the world: 88.8% of patients were under 60 years of age.
Acute, minus natural selection
The invited discussant on the abstract, Dr. Malakh L. Shrestha took issue with the study’s conclusion that acuteness did not affect operative mortality. Dr. Shrestha is the division manager of valvular and coronary artery surgery at the Hannover (Germany) Medical School.
"As a high volume center, what we’ve learned is that acute and chronic aortic dissection patients are two totally different subsets of patients in terms of clinical presentation and mortality. The greatest danger in the acute patient is in the first few hours after the dissection, with the majority of patients dying without surgical intervention."
At Dr. Shrestha’s center in Germany, a high-volume aortic center, they often see patients within the first few hours of their dissection and they’ve found a significantly higher mortality in these patients, compared with chronic TAAD whether an ascending aortic replacement or a frozen elephant trunk procedure is done.
With a median of 4.1 days lapsing between onset of symptoms and surgery in the Ma et al. study, Dr. Shrestha argued that "although on the basis of classification, you can still say they’re acute, there has been some sort of natural selection. So, I think that means, at least for your conclusions, that you need to clarify the statement that there is no difference between acute and chronic, because these are obviously not the same subset of patients that we see in the Western world."
Dr. Ma agreed that natural selection was indeed at play in their series, in that about 80% of their patients were referrals that were transferred in some cases from hundreds of miles away, with many dying en route or before surgery. He also concurred that had their mean and median number of days in their acute cohort been less, indeed, mortality might have been higher.
Dr. Ma reported having no conflicts of interest. Dr. Shrestha is a consultant for Edwards Lifesciences.
Key clinical point: Operative mortality risk factors included CVD; malperfusion of the brain, kidneys, spinal cord, and viscera; and CPB time exceeding 180 minutes.
Major finding: After multivariate adjustment, acute and chronic TAAD patients had similar operative mortality after total arch replacement and frozen elephant trunk implantation.
Data source: Case series with 803 TAAD patients, 456 defined as acute (less than 14 days from symptom onset) and 347 chronic (more than 14 days from symptom onset).
Disclosures: Dr. Ma reported having no conflicts of interest. Dr. Shrestha is a consultant for Edwards Lifesciences.
Left ventricular dysfunction common after mitral valve repair
TORONTO – Early postoperative left ventricular dysfunction occurs in about 18% of patients who undergo "early" mitral valve repair for severe degenerative disease and have normal preoperative ejection fractions exceeding 60%.
In two-thirds of these patients, the left ventricular dysfunction is persistent and associated with increased mortality, reported Dr. Rakesh Suri of the Mayo Clinic in Rochester, Minn.
"These results may help redefine what we have held true for the last few decades," Dr. David H. Adams said after hearing the data presented at the annual meeting of the American Association for Thoracic Surgery.
Dr. Adams is program director of the Mitral Valve Repair Center, Mount Sinai Medical Center, New York.
Guidelines from the American College of Cardiology/American Heart Association recommend that, for patients with severe degenerative mitral regurgitation due to leaflet prolapse, mitral valve repair needs to be done before the onset of left ventricular dysfunction.
However, despite this preemptive approach, a proportion of patients experience a profound decrease in left ventricular ejection fraction (LVEF), to less than 50% in the immediate postoperative period.
Dr. Suri and his colleagues studied the incidence, predictors, and short- and long-term consequences of this phenomenon in 1,705 patients with severe degenerative mitral regurgitation but LVEF greater than 60% who underwent mitral valve repair at the Mayo Clinic from Jan. 1, 1993, to June 30, 2012.
Patients were excluded from the study if they were under age 18, had a history of significant coronary artery disease, or were undergoing concomitant cardiac procedures other than Maze, tricuspid valve repair, or closure of a patent foramen ovale, the researchers noted.
After mitral valve repair, 82% of the cohort had normal LVEF (50% or more), and 18% developed early LV dysfunction (less than 50%).
Mean preoperative LVEF was 65.8% in the group that maintained normal ejection fraction post repair and 66.3% in the group that developed LV dysfunction (P less than .001).
In the group of patients in whom an early decline in LV function was noted, the mean fall in LVEF was 36%, compared with a postrepair drop of 11% in patients whose function remained in the normal range (P less than .001).
When the researchers looked at whether or not patients went to surgery with guideline-based class I or IIa triggers for mitral valve repair, those being symptoms of LV dysfunction, atrial fibrillation, or pulmonary hypertension, they found that 37% of patients who did not develop LV dysfunction and 22% of those who did had no class I or IIa triggers.
"In other words, the guidelines were incapable of defining this population prior to the performance of mitral valve repair," Dr. Suri explained.
On multivariate analysis, predictors of early LV dysfunction were higher right ventricular systolic pressure and LV end-systolic dimension (both P less than .001).
Patients with early LV dysfunction continued to have significantly diminished LVEF at less than 5, 5-10, and less than 10 years.
"Examined in terms of the ability to recover a normal ejection fraction with time, we saw that amongst those with no LV dysfunction following mitral valve repair, two-thirds went on to complete recovery," explained Dr. Suri.
"In contrast, among those with early LV dysfunction, only one-third were capable of recovering normal LV function with time. In other words, two-thirds had persistent LV dysfunction despite undergoing ‘early’ mitral valve repair," Dr. Suri said.
Early LVEF of less than 40% was seen to increased late mortality risk by 70%.
According to these data, a "normal" preoperative ejection fraction should not provide false reassurance of the capacity for restoration of LV function late following mitral valve repair, suggesting that surgical intervention prior to the onset of excessive LV dilation or pulmonary hypertension is warranted, Dr. Suri said.
"So much of the evidence base that serves as a foundation for the ACC/AHA guidelines comes from the Mayo experience, and your new data is provocative and will have implications for future guidelines," said Dr. Adams, the invited discussant for the abstract.
Dr. Suri reported having no disclosures related to this presentation.
TORONTO – Early postoperative left ventricular dysfunction occurs in about 18% of patients who undergo "early" mitral valve repair for severe degenerative disease and have normal preoperative ejection fractions exceeding 60%.
In two-thirds of these patients, the left ventricular dysfunction is persistent and associated with increased mortality, reported Dr. Rakesh Suri of the Mayo Clinic in Rochester, Minn.
"These results may help redefine what we have held true for the last few decades," Dr. David H. Adams said after hearing the data presented at the annual meeting of the American Association for Thoracic Surgery.
Dr. Adams is program director of the Mitral Valve Repair Center, Mount Sinai Medical Center, New York.
Guidelines from the American College of Cardiology/American Heart Association recommend that, for patients with severe degenerative mitral regurgitation due to leaflet prolapse, mitral valve repair needs to be done before the onset of left ventricular dysfunction.
However, despite this preemptive approach, a proportion of patients experience a profound decrease in left ventricular ejection fraction (LVEF), to less than 50% in the immediate postoperative period.
Dr. Suri and his colleagues studied the incidence, predictors, and short- and long-term consequences of this phenomenon in 1,705 patients with severe degenerative mitral regurgitation but LVEF greater than 60% who underwent mitral valve repair at the Mayo Clinic from Jan. 1, 1993, to June 30, 2012.
Patients were excluded from the study if they were under age 18, had a history of significant coronary artery disease, or were undergoing concomitant cardiac procedures other than Maze, tricuspid valve repair, or closure of a patent foramen ovale, the researchers noted.
After mitral valve repair, 82% of the cohort had normal LVEF (50% or more), and 18% developed early LV dysfunction (less than 50%).
Mean preoperative LVEF was 65.8% in the group that maintained normal ejection fraction post repair and 66.3% in the group that developed LV dysfunction (P less than .001).
In the group of patients in whom an early decline in LV function was noted, the mean fall in LVEF was 36%, compared with a postrepair drop of 11% in patients whose function remained in the normal range (P less than .001).
When the researchers looked at whether or not patients went to surgery with guideline-based class I or IIa triggers for mitral valve repair, those being symptoms of LV dysfunction, atrial fibrillation, or pulmonary hypertension, they found that 37% of patients who did not develop LV dysfunction and 22% of those who did had no class I or IIa triggers.
"In other words, the guidelines were incapable of defining this population prior to the performance of mitral valve repair," Dr. Suri explained.
On multivariate analysis, predictors of early LV dysfunction were higher right ventricular systolic pressure and LV end-systolic dimension (both P less than .001).
Patients with early LV dysfunction continued to have significantly diminished LVEF at less than 5, 5-10, and less than 10 years.
"Examined in terms of the ability to recover a normal ejection fraction with time, we saw that amongst those with no LV dysfunction following mitral valve repair, two-thirds went on to complete recovery," explained Dr. Suri.
"In contrast, among those with early LV dysfunction, only one-third were capable of recovering normal LV function with time. In other words, two-thirds had persistent LV dysfunction despite undergoing ‘early’ mitral valve repair," Dr. Suri said.
Early LVEF of less than 40% was seen to increased late mortality risk by 70%.
According to these data, a "normal" preoperative ejection fraction should not provide false reassurance of the capacity for restoration of LV function late following mitral valve repair, suggesting that surgical intervention prior to the onset of excessive LV dilation or pulmonary hypertension is warranted, Dr. Suri said.
"So much of the evidence base that serves as a foundation for the ACC/AHA guidelines comes from the Mayo experience, and your new data is provocative and will have implications for future guidelines," said Dr. Adams, the invited discussant for the abstract.
Dr. Suri reported having no disclosures related to this presentation.
TORONTO – Early postoperative left ventricular dysfunction occurs in about 18% of patients who undergo "early" mitral valve repair for severe degenerative disease and have normal preoperative ejection fractions exceeding 60%.
In two-thirds of these patients, the left ventricular dysfunction is persistent and associated with increased mortality, reported Dr. Rakesh Suri of the Mayo Clinic in Rochester, Minn.
"These results may help redefine what we have held true for the last few decades," Dr. David H. Adams said after hearing the data presented at the annual meeting of the American Association for Thoracic Surgery.
Dr. Adams is program director of the Mitral Valve Repair Center, Mount Sinai Medical Center, New York.
Guidelines from the American College of Cardiology/American Heart Association recommend that, for patients with severe degenerative mitral regurgitation due to leaflet prolapse, mitral valve repair needs to be done before the onset of left ventricular dysfunction.
However, despite this preemptive approach, a proportion of patients experience a profound decrease in left ventricular ejection fraction (LVEF), to less than 50% in the immediate postoperative period.
Dr. Suri and his colleagues studied the incidence, predictors, and short- and long-term consequences of this phenomenon in 1,705 patients with severe degenerative mitral regurgitation but LVEF greater than 60% who underwent mitral valve repair at the Mayo Clinic from Jan. 1, 1993, to June 30, 2012.
Patients were excluded from the study if they were under age 18, had a history of significant coronary artery disease, or were undergoing concomitant cardiac procedures other than Maze, tricuspid valve repair, or closure of a patent foramen ovale, the researchers noted.
After mitral valve repair, 82% of the cohort had normal LVEF (50% or more), and 18% developed early LV dysfunction (less than 50%).
Mean preoperative LVEF was 65.8% in the group that maintained normal ejection fraction post repair and 66.3% in the group that developed LV dysfunction (P less than .001).
In the group of patients in whom an early decline in LV function was noted, the mean fall in LVEF was 36%, compared with a postrepair drop of 11% in patients whose function remained in the normal range (P less than .001).
When the researchers looked at whether or not patients went to surgery with guideline-based class I or IIa triggers for mitral valve repair, those being symptoms of LV dysfunction, atrial fibrillation, or pulmonary hypertension, they found that 37% of patients who did not develop LV dysfunction and 22% of those who did had no class I or IIa triggers.
"In other words, the guidelines were incapable of defining this population prior to the performance of mitral valve repair," Dr. Suri explained.
On multivariate analysis, predictors of early LV dysfunction were higher right ventricular systolic pressure and LV end-systolic dimension (both P less than .001).
Patients with early LV dysfunction continued to have significantly diminished LVEF at less than 5, 5-10, and less than 10 years.
"Examined in terms of the ability to recover a normal ejection fraction with time, we saw that amongst those with no LV dysfunction following mitral valve repair, two-thirds went on to complete recovery," explained Dr. Suri.
"In contrast, among those with early LV dysfunction, only one-third were capable of recovering normal LV function with time. In other words, two-thirds had persistent LV dysfunction despite undergoing ‘early’ mitral valve repair," Dr. Suri said.
Early LVEF of less than 40% was seen to increased late mortality risk by 70%.
According to these data, a "normal" preoperative ejection fraction should not provide false reassurance of the capacity for restoration of LV function late following mitral valve repair, suggesting that surgical intervention prior to the onset of excessive LV dilation or pulmonary hypertension is warranted, Dr. Suri said.
"So much of the evidence base that serves as a foundation for the ACC/AHA guidelines comes from the Mayo experience, and your new data is provocative and will have implications for future guidelines," said Dr. Adams, the invited discussant for the abstract.
Dr. Suri reported having no disclosures related to this presentation.
Key clinical point: Guidelines were incapable of defining the at-risk population prior to mitral valve repair.
Major finding: A total of 18% of patients with severe degenerative mitral disease but normal preoperative LVEF who underwent mitral valve repair had early postoperative decreases in LV function (to less than 50%). Two-thirds of these patients had persistent LV dysfunction.
Data source: Retrospective analysis of 1,705 patients with severe degenerative mitral regurgitation who underwent mitral valve repair.
Disclosures: Dr. Suri reported having no disclosures related to this presentation.
Most U.S. surgeons, centers do little off-pump CABG
TORONTO – In the United States, fewer than one in five coronary artery bypass graft surgeries are done without cardiopulmonary bypass, according to a large Society of Thoracic Surgeons database study conducted by Dr. Faisal G. Bakaeen of Baylor College of Medicine, the Michael E. DeBakey VA Medical Center, and the Texas Heart Institute, Houston, and colleagues.
As of 2012, 84% of the centers in the United States were doing either 0 or fewer than 50 off-pump cases per year. Among U.S. surgeons, 86% did either no off-pump coronary artery bypass grafts (CABG) or 20 or fewer cases per year.
"We speculate that this decline is because off-pump is technically a more demanding operation than on-pump," said Dr. Bakaeen during his presentation at the annual meeting of the American Association of Thoracic Surgery.
"There are [also] concerns about graft patency and the completeness of revascularization and randomized, controlled trials have shown no mortality or major – and I emphasize major – morbidity benefit."
The invited discussant for the abstract, Dr. Harold L. Lazar, the director of cardiothoracic surgery research at Boston Medical Center, suggested that off-pump CABG numbers "will continue to decline" as overall CABG volume continues to decline, and as higher-volume centers and surgeons opt to do fewer off-pump cases.
"Cardiac surgeons have always been motivated to adopt new techniques that will result in improved outcomes for their patients," said Dr. Lazar. "The continuing decline in the use of OP-CABG [off-pump CABG ] by U.S. surgeons is an indication that OP-CABG is not this type of technique."
Introduced in the early 1990s, off-pump CABG was initially touted as a means of avoiding several of the adverse effects of cardiopulmonary bypass and aortic manipulation. However, the relative benefits of off-pump as compared to on-pump CABG continue to be hotly debated.
Dr. Bakaeen and colleagues used the Society of Thoracic Surgeons Adult Cardiac Surgery Database to examine national trends in the use of off- versus on-pump CABG, looking specifically at volume-specific trends among centers and surgeons.
"This is a megadatabase with a huge number of patients, over 2.1 million patients and over 1,200 centers," said Dr. Bakaeen.
The off-pump and on-pump CABG percentages were calculated in aggregate, by center, and by surgeon for a total of 2,137,841 isolated primary CABG procedures performed between Jan. 1, 1997 and Sept. 30, 2012.
Based on 2007/2008 yearly off-pump volume, the analysis subgroups were "high" [center number greater than 200 cases, surgeon number greater than 100 cases], "intermediate" [center number equals 50-200, surgeon number equals 20-100], and "low" [center number less than 50, surgeon number less than 20].
The utilization of off-pump peaked in 2002 at about 23% but then decreased to 17% in 2012. Most of this decrease was found to be driven by higher-volume centers and higher-volume surgeons doing fewer off-pump cases.
Indeed, for the most recent years studied (2011-2012), 12% of U.S. centers (1,056) and 34% of U.S. surgeons (2,626) did not do any off-pump CABG cases.
Another 72% of centers and 52% of surgeons were low-volume operators (less than 50 cases/year and less than 20 cases/year, respectively.
Only 1% of centers (150) and 1% of surgeons (38) were classified as high-volume off-pump operators.
Of note, while the overall conversion rate – cases that were started as on- or off-pump and switched midprocedure – has remained fairly steady at 6%, the rate of unplanned conversions has risen from a low of about 1% in 2004 to about 3.2% in 2012.
"What was interesting was that there was a direct correlation between off-pump volume and the experience of the surgeon and the conversion rate," reported Dr. Bakaeen.
"So, if you are a higher-volume, experienced off-pump surgeon, you are three times less likely to convert than a low-volume surgeon [P less than .01]."
Dr. Bakaeen concluded that, "off-pump CABG utilization will likely continue to be concentrated in specialized centers and performed by dedicated off-pump surgeons."
Dr. Lazar added: "No operation that can only be performed by a select group of experienced, talented surgeons has ever achieved the test of time. CABG surgery must be performed expertly under all circumstances in all patients and at all hospitals, regardless of cardiac volume. These goals appear to be best achieved with on-pump CABG, which remains the gold standard."
Dr. Bakaeen reported having no financial disclosures.
Dr. Lazar reported that he receives grants and research support from Eli Lilly.
TORONTO – In the United States, fewer than one in five coronary artery bypass graft surgeries are done without cardiopulmonary bypass, according to a large Society of Thoracic Surgeons database study conducted by Dr. Faisal G. Bakaeen of Baylor College of Medicine, the Michael E. DeBakey VA Medical Center, and the Texas Heart Institute, Houston, and colleagues.
As of 2012, 84% of the centers in the United States were doing either 0 or fewer than 50 off-pump cases per year. Among U.S. surgeons, 86% did either no off-pump coronary artery bypass grafts (CABG) or 20 or fewer cases per year.
"We speculate that this decline is because off-pump is technically a more demanding operation than on-pump," said Dr. Bakaeen during his presentation at the annual meeting of the American Association of Thoracic Surgery.
"There are [also] concerns about graft patency and the completeness of revascularization and randomized, controlled trials have shown no mortality or major – and I emphasize major – morbidity benefit."
The invited discussant for the abstract, Dr. Harold L. Lazar, the director of cardiothoracic surgery research at Boston Medical Center, suggested that off-pump CABG numbers "will continue to decline" as overall CABG volume continues to decline, and as higher-volume centers and surgeons opt to do fewer off-pump cases.
"Cardiac surgeons have always been motivated to adopt new techniques that will result in improved outcomes for their patients," said Dr. Lazar. "The continuing decline in the use of OP-CABG [off-pump CABG ] by U.S. surgeons is an indication that OP-CABG is not this type of technique."
Introduced in the early 1990s, off-pump CABG was initially touted as a means of avoiding several of the adverse effects of cardiopulmonary bypass and aortic manipulation. However, the relative benefits of off-pump as compared to on-pump CABG continue to be hotly debated.
Dr. Bakaeen and colleagues used the Society of Thoracic Surgeons Adult Cardiac Surgery Database to examine national trends in the use of off- versus on-pump CABG, looking specifically at volume-specific trends among centers and surgeons.
"This is a megadatabase with a huge number of patients, over 2.1 million patients and over 1,200 centers," said Dr. Bakaeen.
The off-pump and on-pump CABG percentages were calculated in aggregate, by center, and by surgeon for a total of 2,137,841 isolated primary CABG procedures performed between Jan. 1, 1997 and Sept. 30, 2012.
Based on 2007/2008 yearly off-pump volume, the analysis subgroups were "high" [center number greater than 200 cases, surgeon number greater than 100 cases], "intermediate" [center number equals 50-200, surgeon number equals 20-100], and "low" [center number less than 50, surgeon number less than 20].
The utilization of off-pump peaked in 2002 at about 23% but then decreased to 17% in 2012. Most of this decrease was found to be driven by higher-volume centers and higher-volume surgeons doing fewer off-pump cases.
Indeed, for the most recent years studied (2011-2012), 12% of U.S. centers (1,056) and 34% of U.S. surgeons (2,626) did not do any off-pump CABG cases.
Another 72% of centers and 52% of surgeons were low-volume operators (less than 50 cases/year and less than 20 cases/year, respectively.
Only 1% of centers (150) and 1% of surgeons (38) were classified as high-volume off-pump operators.
Of note, while the overall conversion rate – cases that were started as on- or off-pump and switched midprocedure – has remained fairly steady at 6%, the rate of unplanned conversions has risen from a low of about 1% in 2004 to about 3.2% in 2012.
"What was interesting was that there was a direct correlation between off-pump volume and the experience of the surgeon and the conversion rate," reported Dr. Bakaeen.
"So, if you are a higher-volume, experienced off-pump surgeon, you are three times less likely to convert than a low-volume surgeon [P less than .01]."
Dr. Bakaeen concluded that, "off-pump CABG utilization will likely continue to be concentrated in specialized centers and performed by dedicated off-pump surgeons."
Dr. Lazar added: "No operation that can only be performed by a select group of experienced, talented surgeons has ever achieved the test of time. CABG surgery must be performed expertly under all circumstances in all patients and at all hospitals, regardless of cardiac volume. These goals appear to be best achieved with on-pump CABG, which remains the gold standard."
Dr. Bakaeen reported having no financial disclosures.
Dr. Lazar reported that he receives grants and research support from Eli Lilly.
TORONTO – In the United States, fewer than one in five coronary artery bypass graft surgeries are done without cardiopulmonary bypass, according to a large Society of Thoracic Surgeons database study conducted by Dr. Faisal G. Bakaeen of Baylor College of Medicine, the Michael E. DeBakey VA Medical Center, and the Texas Heart Institute, Houston, and colleagues.
As of 2012, 84% of the centers in the United States were doing either 0 or fewer than 50 off-pump cases per year. Among U.S. surgeons, 86% did either no off-pump coronary artery bypass grafts (CABG) or 20 or fewer cases per year.
"We speculate that this decline is because off-pump is technically a more demanding operation than on-pump," said Dr. Bakaeen during his presentation at the annual meeting of the American Association of Thoracic Surgery.
"There are [also] concerns about graft patency and the completeness of revascularization and randomized, controlled trials have shown no mortality or major – and I emphasize major – morbidity benefit."
The invited discussant for the abstract, Dr. Harold L. Lazar, the director of cardiothoracic surgery research at Boston Medical Center, suggested that off-pump CABG numbers "will continue to decline" as overall CABG volume continues to decline, and as higher-volume centers and surgeons opt to do fewer off-pump cases.
"Cardiac surgeons have always been motivated to adopt new techniques that will result in improved outcomes for their patients," said Dr. Lazar. "The continuing decline in the use of OP-CABG [off-pump CABG ] by U.S. surgeons is an indication that OP-CABG is not this type of technique."
Introduced in the early 1990s, off-pump CABG was initially touted as a means of avoiding several of the adverse effects of cardiopulmonary bypass and aortic manipulation. However, the relative benefits of off-pump as compared to on-pump CABG continue to be hotly debated.
Dr. Bakaeen and colleagues used the Society of Thoracic Surgeons Adult Cardiac Surgery Database to examine national trends in the use of off- versus on-pump CABG, looking specifically at volume-specific trends among centers and surgeons.
"This is a megadatabase with a huge number of patients, over 2.1 million patients and over 1,200 centers," said Dr. Bakaeen.
The off-pump and on-pump CABG percentages were calculated in aggregate, by center, and by surgeon for a total of 2,137,841 isolated primary CABG procedures performed between Jan. 1, 1997 and Sept. 30, 2012.
Based on 2007/2008 yearly off-pump volume, the analysis subgroups were "high" [center number greater than 200 cases, surgeon number greater than 100 cases], "intermediate" [center number equals 50-200, surgeon number equals 20-100], and "low" [center number less than 50, surgeon number less than 20].
The utilization of off-pump peaked in 2002 at about 23% but then decreased to 17% in 2012. Most of this decrease was found to be driven by higher-volume centers and higher-volume surgeons doing fewer off-pump cases.
Indeed, for the most recent years studied (2011-2012), 12% of U.S. centers (1,056) and 34% of U.S. surgeons (2,626) did not do any off-pump CABG cases.
Another 72% of centers and 52% of surgeons were low-volume operators (less than 50 cases/year and less than 20 cases/year, respectively.
Only 1% of centers (150) and 1% of surgeons (38) were classified as high-volume off-pump operators.
Of note, while the overall conversion rate – cases that were started as on- or off-pump and switched midprocedure – has remained fairly steady at 6%, the rate of unplanned conversions has risen from a low of about 1% in 2004 to about 3.2% in 2012.
"What was interesting was that there was a direct correlation between off-pump volume and the experience of the surgeon and the conversion rate," reported Dr. Bakaeen.
"So, if you are a higher-volume, experienced off-pump surgeon, you are three times less likely to convert than a low-volume surgeon [P less than .01]."
Dr. Bakaeen concluded that, "off-pump CABG utilization will likely continue to be concentrated in specialized centers and performed by dedicated off-pump surgeons."
Dr. Lazar added: "No operation that can only be performed by a select group of experienced, talented surgeons has ever achieved the test of time. CABG surgery must be performed expertly under all circumstances in all patients and at all hospitals, regardless of cardiac volume. These goals appear to be best achieved with on-pump CABG, which remains the gold standard."
Dr. Bakaeen reported having no financial disclosures.
Dr. Lazar reported that he receives grants and research support from Eli Lilly.
Major finding: Currently, fewer than one in five CABGs done in the US are off-pump. Most surgeons and centers are doing either no off-pump CABG or are low-volume operators.
Data source: STS Adult Cardiac Surgery Database, 2,137,841 CABG procedures conducted between 1997 and 2012 at 1,263 U.S. centers with 2,626 surgeons.
Disclosures: Dr. Bakaeen reported having no financial disclosures. Dr. Lazar reported that he receives grants and research support from Eli Lilly.
Procedure volume predicts repair vs. mitral replacement
TORONTO – Mitral valve repair rates continue to show great variability, ranging from 0% to 90% for patients with moderate to severe mitral regurgitation, according to data presented by Dr. Damien J. LaPar, a thoracic surgeon at the University of Virginia, Charlottesville.
Surgeons performing more than 20 mitral cases per year were about three times more likely to perform a repair over a replacement compared with surgeons performing fewer than 20 mitral surgeries per year.
"Average annual surgeon volume appears more significantly associated with an increased likelihood for mitral repair than institutional volume," Dr. LaPar reported at the annual meeting of the American Association for Thoracic Surgery. A video of his live presentation is available at the AATS website.
Mitral valve repair appears to be underused despite accumulated data favoring repair over replacement in the treatment of patients with moderate to severe mitral regurgitation. Dr. LaPar and colleagues evaluated the relationship between procedure volume and propensity for mitral repair (over replacement) in a multi-institution cohort of patients.
The Virginia Cardiac Surgery Quality Initiative is a voluntary consortium of 17 collaborating cardiac surgery centers in Virginia that captures about 99% of all the operations performed in the state, with each center contributing their data to the Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database.
Records for 4,178 patients were evaluated for 2001-2012; 2,516 of these patients underwent isolated mitral valve replacement and 1,662 underwent isolated mitral valve repair. To examine confounding, a propensity-matched cohort was developed with 1,661 patients in each group.
Median annual mitral procedure volume was 54 cases per year for hospitals, ranging from 5 to 128, and 13 cases per year for individual surgeons, ranging from 0 to 58 cases. Mitral valve repair rates also ranged significantly, from 35% to 70% of all mitral valve procedures for hospitals and from 0% to 90% for surgeons.
Mitral valve replacement patients presented with higher STS PROM (5.6% vs. 1.7%, P less than .001), higher age, and a greater number of comorbidities. When the researchers adjusted for STS PROM, both average annual hospital (P = .04) and surgeon (P less than .0001) mitral procedure volumes were associated with probability of mitral repair, with surgeon volume showing more influence in the decision to repair rather than replace the mitral valve.
When the propensity to perform mitral valve repair was plotted against surgeon volume, there was a clear "inflection point" of increased probability for repair over replacement when the average annual surgeon mitral volume (a surrogate for surgeon experience) exceeded 20 operations yearly. This finding was validated in the propensity-matched cohort.
"We did a post hoc analysis and demonstrated that when you categorize volume by our visible threshold of 20 cases per year, for both hospital and surgeon volume in the overall cohort, hospitals and surgeons performing more than 20 cases per year, more strongly performed mitral valve repair," said Dr. LaPar.
Indeed, among surgeons and hospitals performing more than 20 mitral operations annually, repairs were done in 62% of cases, compared to 37% for lower-volume centers. Among surgeons performing more than 20 mitral cases per year, repair rates were 73% compared to 26% for lower-volume mitral operators (both P less than .001).
Similarly significant differences were seen in the propensity-matched cohort, although the effect was more muted (53% vs. 47% for high- and low-volume hospitals and 67% vs. 39% for high- and low-volume surgeons; P less than .001 for both).
"In the upcoming era of percutaneous mitral valve repair technology, we believe that surgeon volume and expertise should act as a gatekeeper and should dictate not only access to this technology but the role of surgeons and cardiologists in this," concluded Dr. LaPar.
"This will be an excellent contribution to the literature further defining the relationship between surgeon volume and hospital center volume in mitral valve surgical outcomes and choice of operation," said the invited discussant, Dr. David A Fullerton of the University of Colorado at Denver, Aurora.
Dr. Daniel Drake, head of the Michigan Society of Thoracic and Cardiovascular Surgeons Mitral Initiative, added that in his state they have started to see a greater number of referrals – based on an assessment of case complexity – from less experienced surgeons to more experienced surgeons. Dr. LaPar noted that he hadn’t yet seen this widely in Virginia.
Dr. LaPar and Dr. Fullerton reported no disclosures.
TORONTO – Mitral valve repair rates continue to show great variability, ranging from 0% to 90% for patients with moderate to severe mitral regurgitation, according to data presented by Dr. Damien J. LaPar, a thoracic surgeon at the University of Virginia, Charlottesville.
Surgeons performing more than 20 mitral cases per year were about three times more likely to perform a repair over a replacement compared with surgeons performing fewer than 20 mitral surgeries per year.
"Average annual surgeon volume appears more significantly associated with an increased likelihood for mitral repair than institutional volume," Dr. LaPar reported at the annual meeting of the American Association for Thoracic Surgery. A video of his live presentation is available at the AATS website.
Mitral valve repair appears to be underused despite accumulated data favoring repair over replacement in the treatment of patients with moderate to severe mitral regurgitation. Dr. LaPar and colleagues evaluated the relationship between procedure volume and propensity for mitral repair (over replacement) in a multi-institution cohort of patients.
The Virginia Cardiac Surgery Quality Initiative is a voluntary consortium of 17 collaborating cardiac surgery centers in Virginia that captures about 99% of all the operations performed in the state, with each center contributing their data to the Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database.
Records for 4,178 patients were evaluated for 2001-2012; 2,516 of these patients underwent isolated mitral valve replacement and 1,662 underwent isolated mitral valve repair. To examine confounding, a propensity-matched cohort was developed with 1,661 patients in each group.
Median annual mitral procedure volume was 54 cases per year for hospitals, ranging from 5 to 128, and 13 cases per year for individual surgeons, ranging from 0 to 58 cases. Mitral valve repair rates also ranged significantly, from 35% to 70% of all mitral valve procedures for hospitals and from 0% to 90% for surgeons.
Mitral valve replacement patients presented with higher STS PROM (5.6% vs. 1.7%, P less than .001), higher age, and a greater number of comorbidities. When the researchers adjusted for STS PROM, both average annual hospital (P = .04) and surgeon (P less than .0001) mitral procedure volumes were associated with probability of mitral repair, with surgeon volume showing more influence in the decision to repair rather than replace the mitral valve.
When the propensity to perform mitral valve repair was plotted against surgeon volume, there was a clear "inflection point" of increased probability for repair over replacement when the average annual surgeon mitral volume (a surrogate for surgeon experience) exceeded 20 operations yearly. This finding was validated in the propensity-matched cohort.
"We did a post hoc analysis and demonstrated that when you categorize volume by our visible threshold of 20 cases per year, for both hospital and surgeon volume in the overall cohort, hospitals and surgeons performing more than 20 cases per year, more strongly performed mitral valve repair," said Dr. LaPar.
Indeed, among surgeons and hospitals performing more than 20 mitral operations annually, repairs were done in 62% of cases, compared to 37% for lower-volume centers. Among surgeons performing more than 20 mitral cases per year, repair rates were 73% compared to 26% for lower-volume mitral operators (both P less than .001).
Similarly significant differences were seen in the propensity-matched cohort, although the effect was more muted (53% vs. 47% for high- and low-volume hospitals and 67% vs. 39% for high- and low-volume surgeons; P less than .001 for both).
"In the upcoming era of percutaneous mitral valve repair technology, we believe that surgeon volume and expertise should act as a gatekeeper and should dictate not only access to this technology but the role of surgeons and cardiologists in this," concluded Dr. LaPar.
"This will be an excellent contribution to the literature further defining the relationship between surgeon volume and hospital center volume in mitral valve surgical outcomes and choice of operation," said the invited discussant, Dr. David A Fullerton of the University of Colorado at Denver, Aurora.
Dr. Daniel Drake, head of the Michigan Society of Thoracic and Cardiovascular Surgeons Mitral Initiative, added that in his state they have started to see a greater number of referrals – based on an assessment of case complexity – from less experienced surgeons to more experienced surgeons. Dr. LaPar noted that he hadn’t yet seen this widely in Virginia.
Dr. LaPar and Dr. Fullerton reported no disclosures.
TORONTO – Mitral valve repair rates continue to show great variability, ranging from 0% to 90% for patients with moderate to severe mitral regurgitation, according to data presented by Dr. Damien J. LaPar, a thoracic surgeon at the University of Virginia, Charlottesville.
Surgeons performing more than 20 mitral cases per year were about three times more likely to perform a repair over a replacement compared with surgeons performing fewer than 20 mitral surgeries per year.
"Average annual surgeon volume appears more significantly associated with an increased likelihood for mitral repair than institutional volume," Dr. LaPar reported at the annual meeting of the American Association for Thoracic Surgery. A video of his live presentation is available at the AATS website.
Mitral valve repair appears to be underused despite accumulated data favoring repair over replacement in the treatment of patients with moderate to severe mitral regurgitation. Dr. LaPar and colleagues evaluated the relationship between procedure volume and propensity for mitral repair (over replacement) in a multi-institution cohort of patients.
The Virginia Cardiac Surgery Quality Initiative is a voluntary consortium of 17 collaborating cardiac surgery centers in Virginia that captures about 99% of all the operations performed in the state, with each center contributing their data to the Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database.
Records for 4,178 patients were evaluated for 2001-2012; 2,516 of these patients underwent isolated mitral valve replacement and 1,662 underwent isolated mitral valve repair. To examine confounding, a propensity-matched cohort was developed with 1,661 patients in each group.
Median annual mitral procedure volume was 54 cases per year for hospitals, ranging from 5 to 128, and 13 cases per year for individual surgeons, ranging from 0 to 58 cases. Mitral valve repair rates also ranged significantly, from 35% to 70% of all mitral valve procedures for hospitals and from 0% to 90% for surgeons.
Mitral valve replacement patients presented with higher STS PROM (5.6% vs. 1.7%, P less than .001), higher age, and a greater number of comorbidities. When the researchers adjusted for STS PROM, both average annual hospital (P = .04) and surgeon (P less than .0001) mitral procedure volumes were associated with probability of mitral repair, with surgeon volume showing more influence in the decision to repair rather than replace the mitral valve.
When the propensity to perform mitral valve repair was plotted against surgeon volume, there was a clear "inflection point" of increased probability for repair over replacement when the average annual surgeon mitral volume (a surrogate for surgeon experience) exceeded 20 operations yearly. This finding was validated in the propensity-matched cohort.
"We did a post hoc analysis and demonstrated that when you categorize volume by our visible threshold of 20 cases per year, for both hospital and surgeon volume in the overall cohort, hospitals and surgeons performing more than 20 cases per year, more strongly performed mitral valve repair," said Dr. LaPar.
Indeed, among surgeons and hospitals performing more than 20 mitral operations annually, repairs were done in 62% of cases, compared to 37% for lower-volume centers. Among surgeons performing more than 20 mitral cases per year, repair rates were 73% compared to 26% for lower-volume mitral operators (both P less than .001).
Similarly significant differences were seen in the propensity-matched cohort, although the effect was more muted (53% vs. 47% for high- and low-volume hospitals and 67% vs. 39% for high- and low-volume surgeons; P less than .001 for both).
"In the upcoming era of percutaneous mitral valve repair technology, we believe that surgeon volume and expertise should act as a gatekeeper and should dictate not only access to this technology but the role of surgeons and cardiologists in this," concluded Dr. LaPar.
"This will be an excellent contribution to the literature further defining the relationship between surgeon volume and hospital center volume in mitral valve surgical outcomes and choice of operation," said the invited discussant, Dr. David A Fullerton of the University of Colorado at Denver, Aurora.
Dr. Daniel Drake, head of the Michigan Society of Thoracic and Cardiovascular Surgeons Mitral Initiative, added that in his state they have started to see a greater number of referrals – based on an assessment of case complexity – from less experienced surgeons to more experienced surgeons. Dr. LaPar noted that he hadn’t yet seen this widely in Virginia.
Dr. LaPar and Dr. Fullerton reported no disclosures.
Key clinical point: Surgeon volume appears more significantly associated with an increased likelihood for mitral repair than institutional volume.
Major finding: MV repair rates among surgeons ranged from 0 to 90% for patients with moderate to severe mitral regurgitation. Surgeons with lower annual mitral valve procedure volumes were about three times less likely to perform the procedure than were surgeons with higher volumes.
Data source: STS certified patients records from 17 surgical centers in Virginia, representing 100 surgeons and 99% of cardiac operations performed in the state.
Disclosures: Dr. LaPar and Dr. Fullerton reported having no financial disclosures.