User login
Single-agent acalabrutinib ‘impressive’ in patients with WM
CHICAGO—Acalabrutinib monotherapy was highly effective in Waldenström’s macroglobulinemia (WM) in a phase 2 study, investigator Roger Owen, MD, reported at the 2018 ASCO Annual Meeting.
The BTK inhibitor was effective in both treatment-naïve and relapsed/refractory patients, with overall response rates for both groups in excess of 90%, and “amazing” major response rates—partial response or better—of approximately 80%, Dr Owen said.
Dr Owen, of the St James's Institute of Oncology, Leeds Teaching Hospitals NHS Trust in Leeds, UK, reported the findings as abstract 7501.*
Durations of response were excellent, according to Dr Owen, who also reported 2-year progression-free survival of 90% in treatment-naïve patients and 82% in relapsed/refractory patients.
The safety profile was favorable, with most adverse events of low grade, and a very limited number of dropouts due to adverse events, according to the investigator.
“I think this study clearly demonstrates the highly effective nature of acalabrutinib in Waldenström’s macroglobulinemia,” Dr Owen stated.
Acalabrutinib is a selective BTK inhibitor with minimal off-target activity, he said. The BTK inhibitor ibrutinib also has demonstrated activity in Waldenström’s, but has been associated with toxicities such as atrial fibrillation and bleeding, he noted.
In this phase 2 acalabrutinib study (NCT02180724), which included 14 treatment-naïve and 92 relapsed/refractory patients, atrial fibrillation occurred in 5 patients. However, 4 of those cases were grade 1-2, and only one was grade 3, according to Dr Owen.
Investigators observed grade 3 hypertension in 3 relapsed/refractory patients.
Bleeding events occurred in more than half of patients, though only 3 of those events were grade 3, and no patient discontinued treatment due to a bleeding episode.
These efficacy results are “impressive,” and the fact that very few cardiac events were seen is important, said Bruce D. Cheson, MD, of Georgetown University Medical Center in Washington, DC.
Dr Cheson commented on the acalabrutinib results in his presentation during ASCO on non-chemotherapy treatments for lymphoid malignancies.
“One can construct a non-chemo algorithm now for Waldenström’s, for patients who are MYD88 mutated, which is more than 90% of patients,” he said. “Right now ibrutinib, and perhaps in the future acalabrutinib, can be the initial therapy with or without rituximab based on the results of ongoing trials.”
However, single non-chemotherapy agents will not be sufficient to achieve cure of lymphoid malignancies, Dr Cheson added.
“We need to carefully develop rational combinations, identifying biomarkers for response, for resistance, for toxicity,” he said.
The study was sponsored by Acerta Pharma BV.
*Data presented at the meeting differ from the abstract.
CHICAGO—Acalabrutinib monotherapy was highly effective in Waldenström’s macroglobulinemia (WM) in a phase 2 study, investigator Roger Owen, MD, reported at the 2018 ASCO Annual Meeting.
The BTK inhibitor was effective in both treatment-naïve and relapsed/refractory patients, with overall response rates for both groups in excess of 90%, and “amazing” major response rates—partial response or better—of approximately 80%, Dr Owen said.
Dr Owen, of the St James's Institute of Oncology, Leeds Teaching Hospitals NHS Trust in Leeds, UK, reported the findings as abstract 7501.*
Durations of response were excellent, according to Dr Owen, who also reported 2-year progression-free survival of 90% in treatment-naïve patients and 82% in relapsed/refractory patients.
The safety profile was favorable, with most adverse events of low grade, and a very limited number of dropouts due to adverse events, according to the investigator.
“I think this study clearly demonstrates the highly effective nature of acalabrutinib in Waldenström’s macroglobulinemia,” Dr Owen stated.
Acalabrutinib is a selective BTK inhibitor with minimal off-target activity, he said. The BTK inhibitor ibrutinib also has demonstrated activity in Waldenström’s, but has been associated with toxicities such as atrial fibrillation and bleeding, he noted.
In this phase 2 acalabrutinib study (NCT02180724), which included 14 treatment-naïve and 92 relapsed/refractory patients, atrial fibrillation occurred in 5 patients. However, 4 of those cases were grade 1-2, and only one was grade 3, according to Dr Owen.
Investigators observed grade 3 hypertension in 3 relapsed/refractory patients.
Bleeding events occurred in more than half of patients, though only 3 of those events were grade 3, and no patient discontinued treatment due to a bleeding episode.
These efficacy results are “impressive,” and the fact that very few cardiac events were seen is important, said Bruce D. Cheson, MD, of Georgetown University Medical Center in Washington, DC.
Dr Cheson commented on the acalabrutinib results in his presentation during ASCO on non-chemotherapy treatments for lymphoid malignancies.
“One can construct a non-chemo algorithm now for Waldenström’s, for patients who are MYD88 mutated, which is more than 90% of patients,” he said. “Right now ibrutinib, and perhaps in the future acalabrutinib, can be the initial therapy with or without rituximab based on the results of ongoing trials.”
However, single non-chemotherapy agents will not be sufficient to achieve cure of lymphoid malignancies, Dr Cheson added.
“We need to carefully develop rational combinations, identifying biomarkers for response, for resistance, for toxicity,” he said.
The study was sponsored by Acerta Pharma BV.
*Data presented at the meeting differ from the abstract.
CHICAGO—Acalabrutinib monotherapy was highly effective in Waldenström’s macroglobulinemia (WM) in a phase 2 study, investigator Roger Owen, MD, reported at the 2018 ASCO Annual Meeting.
The BTK inhibitor was effective in both treatment-naïve and relapsed/refractory patients, with overall response rates for both groups in excess of 90%, and “amazing” major response rates—partial response or better—of approximately 80%, Dr Owen said.
Dr Owen, of the St James's Institute of Oncology, Leeds Teaching Hospitals NHS Trust in Leeds, UK, reported the findings as abstract 7501.*
Durations of response were excellent, according to Dr Owen, who also reported 2-year progression-free survival of 90% in treatment-naïve patients and 82% in relapsed/refractory patients.
The safety profile was favorable, with most adverse events of low grade, and a very limited number of dropouts due to adverse events, according to the investigator.
“I think this study clearly demonstrates the highly effective nature of acalabrutinib in Waldenström’s macroglobulinemia,” Dr Owen stated.
Acalabrutinib is a selective BTK inhibitor with minimal off-target activity, he said. The BTK inhibitor ibrutinib also has demonstrated activity in Waldenström’s, but has been associated with toxicities such as atrial fibrillation and bleeding, he noted.
In this phase 2 acalabrutinib study (NCT02180724), which included 14 treatment-naïve and 92 relapsed/refractory patients, atrial fibrillation occurred in 5 patients. However, 4 of those cases were grade 1-2, and only one was grade 3, according to Dr Owen.
Investigators observed grade 3 hypertension in 3 relapsed/refractory patients.
Bleeding events occurred in more than half of patients, though only 3 of those events were grade 3, and no patient discontinued treatment due to a bleeding episode.
These efficacy results are “impressive,” and the fact that very few cardiac events were seen is important, said Bruce D. Cheson, MD, of Georgetown University Medical Center in Washington, DC.
Dr Cheson commented on the acalabrutinib results in his presentation during ASCO on non-chemotherapy treatments for lymphoid malignancies.
“One can construct a non-chemo algorithm now for Waldenström’s, for patients who are MYD88 mutated, which is more than 90% of patients,” he said. “Right now ibrutinib, and perhaps in the future acalabrutinib, can be the initial therapy with or without rituximab based on the results of ongoing trials.”
However, single non-chemotherapy agents will not be sufficient to achieve cure of lymphoid malignancies, Dr Cheson added.
“We need to carefully develop rational combinations, identifying biomarkers for response, for resistance, for toxicity,” he said.
The study was sponsored by Acerta Pharma BV.
*Data presented at the meeting differ from the abstract.
Overcoming TP53 mutation proves difficult in MCL
, new findings suggest.
“TP53 mutated MCL remains a major challenge, and our results underline the importance of molecular profiling, including TP53 status, in future trials exploring novel agents,” wrote Christian Winther Eskelund, MD, of Rigshospitalet in Copenhagen, and his colleagues. The findings were published in Haematologica.
The researchers noted that the results will need validation in a larger cohort of patients.
They performed an analysis of 50 MCL patients who enrolled in the Nordic MCL4 trial between 2009 and 2013. Patients were either over age 65 years or were younger but unfit for autologous stem cell transplantation. Despite the addition of lenalidomide to the chemoimmunotherapy regimen, patients with TP53 mutations had worse overall and progression-free survival and were significantly quicker to experience relapse.
After a median follow up of 47 months, median overall survival was 25 months for patients with TP53 mutations, compared with 69 months for those without (P less than .0001). Similarly, median progression-free survival was 10 months in patients with the mutation, compared with 42 months in patients without it (P = .001). Time to relapse was a median of 10 months in these mutated patients, compared with 58 months for unmutated MCL patients (P less than .0001).
TP53 mutations were identified in six patients (14%), one of whom withdrew consent at day 28 of the study. Of the remaining patients with mutations, all of them either progressed or relapsed during the study and none were alive at the most recent follow-up. During the study, patients received an induction phase of six cycles of lenalidomide plus bendamustine-rituximab (weeks 1-24), followed by a maintenance phase of lenalidomide (weeks 25-56).
SOURCE: Eskelund CW et al. Haematologica. 2018 May 24. doi: 10.3324/haematol.2018.194399.
, new findings suggest.
“TP53 mutated MCL remains a major challenge, and our results underline the importance of molecular profiling, including TP53 status, in future trials exploring novel agents,” wrote Christian Winther Eskelund, MD, of Rigshospitalet in Copenhagen, and his colleagues. The findings were published in Haematologica.
The researchers noted that the results will need validation in a larger cohort of patients.
They performed an analysis of 50 MCL patients who enrolled in the Nordic MCL4 trial between 2009 and 2013. Patients were either over age 65 years or were younger but unfit for autologous stem cell transplantation. Despite the addition of lenalidomide to the chemoimmunotherapy regimen, patients with TP53 mutations had worse overall and progression-free survival and were significantly quicker to experience relapse.
After a median follow up of 47 months, median overall survival was 25 months for patients with TP53 mutations, compared with 69 months for those without (P less than .0001). Similarly, median progression-free survival was 10 months in patients with the mutation, compared with 42 months in patients without it (P = .001). Time to relapse was a median of 10 months in these mutated patients, compared with 58 months for unmutated MCL patients (P less than .0001).
TP53 mutations were identified in six patients (14%), one of whom withdrew consent at day 28 of the study. Of the remaining patients with mutations, all of them either progressed or relapsed during the study and none were alive at the most recent follow-up. During the study, patients received an induction phase of six cycles of lenalidomide plus bendamustine-rituximab (weeks 1-24), followed by a maintenance phase of lenalidomide (weeks 25-56).
SOURCE: Eskelund CW et al. Haematologica. 2018 May 24. doi: 10.3324/haematol.2018.194399.
, new findings suggest.
“TP53 mutated MCL remains a major challenge, and our results underline the importance of molecular profiling, including TP53 status, in future trials exploring novel agents,” wrote Christian Winther Eskelund, MD, of Rigshospitalet in Copenhagen, and his colleagues. The findings were published in Haematologica.
The researchers noted that the results will need validation in a larger cohort of patients.
They performed an analysis of 50 MCL patients who enrolled in the Nordic MCL4 trial between 2009 and 2013. Patients were either over age 65 years or were younger but unfit for autologous stem cell transplantation. Despite the addition of lenalidomide to the chemoimmunotherapy regimen, patients with TP53 mutations had worse overall and progression-free survival and were significantly quicker to experience relapse.
After a median follow up of 47 months, median overall survival was 25 months for patients with TP53 mutations, compared with 69 months for those without (P less than .0001). Similarly, median progression-free survival was 10 months in patients with the mutation, compared with 42 months in patients without it (P = .001). Time to relapse was a median of 10 months in these mutated patients, compared with 58 months for unmutated MCL patients (P less than .0001).
TP53 mutations were identified in six patients (14%), one of whom withdrew consent at day 28 of the study. Of the remaining patients with mutations, all of them either progressed or relapsed during the study and none were alive at the most recent follow-up. During the study, patients received an induction phase of six cycles of lenalidomide plus bendamustine-rituximab (weeks 1-24), followed by a maintenance phase of lenalidomide (weeks 25-56).
SOURCE: Eskelund CW et al. Haematologica. 2018 May 24. doi: 10.3324/haematol.2018.194399.
FROM HAEMATOLOGICA
Older, cheaper drug formulation to remain available
The 140 mg capsules of Imbruvica® (ibrutinib) will remain on the market, according to Pharmacyclics LLC.
Pharmacyclics (an AbbVie company) and Janssen had planned to discontinue the capsules after introducing a single-tablet formulation of Imbruvica earlier this year.
However, the companies received negative feedback about the discontinuation and decided to keep the 140 mg capsules on the market.
In February, the US Food and Drug Administration (FDA) approved a single-tablet formulation of Imbruvica that is available in 4 doses—140 mg, 280 mg, 420 mg, and 560 mg.
Pharmacyclics and Janssen introduced this formulation to enable a once-a-day dosing regimen. The companies said the goal with the new formulation was to improve adherence because some patients had to take 3 or 4 pills every day to get the recommended dose of Imbruvica.
After introducing the new formulation, Pharmacyclics and Janssen planned to discontinue the 140 mg capsules.
Critics spoke out against this change in an article published in The Cancer Letter. They noted that discontinuing the old formulation would mean price increases for some patients. That’s because the single-tablet formulation of Imbruvica has the same price regardless of dose—$400 per tablet.
Patients on lower doses of Imbruvica would experience an increase in cost if they switched from the capsules to the tablet formulation. In fact, costs could triple for patients on the 140 mg dose.
Pharmacyclics argued that most patients on Imbruvica—those taking the 420 mg and 560 mg doses—would see no increase in out-of-pocket costs when transitioning to the single-tablet formulation. And patients on the 560 mg dose would likely see a decrease in their out-of-pocket costs.
However, critics pointed to results of a recent pilot study, which indicated that the recommended dose of Imbruvica for patients with chronic lymphocytic leukemia (CLL)—420 mg—may be too high. The results suggested that CLL patients could receive lower doses of Imbruvica without a reduction in efficacy.
Therefore, keeping the 140 mg capsules on the market could mean lower costs for some CLL patients.
In addition to voicing concerns about costs, the critics pointed out that discontinuing the 140 mg capsules of Imbruvica would make it more difficult to adjust patients’ doses when needed.
Pharmacyclics said its YOU&i™ Dose Exchange Program can aid healthcare professionals in adjusting doses before patients have finished their current pack of Imbruvica. Patients would receive a “rapid shipment” of their new dose at no additional cost.
But the critics said this program “creates a barrier to optimal prescribing for some patients” and urged the FDA to review the safety of the program.
Roughly a month after the critics made this recommendation in The Cancer Letter article, Pharmacyclics announced that the 140 mg capsules of Imbruvica would remain on the market.
The 140 mg capsules of Imbruvica® (ibrutinib) will remain on the market, according to Pharmacyclics LLC.
Pharmacyclics (an AbbVie company) and Janssen had planned to discontinue the capsules after introducing a single-tablet formulation of Imbruvica earlier this year.
However, the companies received negative feedback about the discontinuation and decided to keep the 140 mg capsules on the market.
In February, the US Food and Drug Administration (FDA) approved a single-tablet formulation of Imbruvica that is available in 4 doses—140 mg, 280 mg, 420 mg, and 560 mg.
Pharmacyclics and Janssen introduced this formulation to enable a once-a-day dosing regimen. The companies said the goal with the new formulation was to improve adherence because some patients had to take 3 or 4 pills every day to get the recommended dose of Imbruvica.
After introducing the new formulation, Pharmacyclics and Janssen planned to discontinue the 140 mg capsules.
Critics spoke out against this change in an article published in The Cancer Letter. They noted that discontinuing the old formulation would mean price increases for some patients. That’s because the single-tablet formulation of Imbruvica has the same price regardless of dose—$400 per tablet.
Patients on lower doses of Imbruvica would experience an increase in cost if they switched from the capsules to the tablet formulation. In fact, costs could triple for patients on the 140 mg dose.
Pharmacyclics argued that most patients on Imbruvica—those taking the 420 mg and 560 mg doses—would see no increase in out-of-pocket costs when transitioning to the single-tablet formulation. And patients on the 560 mg dose would likely see a decrease in their out-of-pocket costs.
However, critics pointed to results of a recent pilot study, which indicated that the recommended dose of Imbruvica for patients with chronic lymphocytic leukemia (CLL)—420 mg—may be too high. The results suggested that CLL patients could receive lower doses of Imbruvica without a reduction in efficacy.
Therefore, keeping the 140 mg capsules on the market could mean lower costs for some CLL patients.
In addition to voicing concerns about costs, the critics pointed out that discontinuing the 140 mg capsules of Imbruvica would make it more difficult to adjust patients’ doses when needed.
Pharmacyclics said its YOU&i™ Dose Exchange Program can aid healthcare professionals in adjusting doses before patients have finished their current pack of Imbruvica. Patients would receive a “rapid shipment” of their new dose at no additional cost.
But the critics said this program “creates a barrier to optimal prescribing for some patients” and urged the FDA to review the safety of the program.
Roughly a month after the critics made this recommendation in The Cancer Letter article, Pharmacyclics announced that the 140 mg capsules of Imbruvica would remain on the market.
The 140 mg capsules of Imbruvica® (ibrutinib) will remain on the market, according to Pharmacyclics LLC.
Pharmacyclics (an AbbVie company) and Janssen had planned to discontinue the capsules after introducing a single-tablet formulation of Imbruvica earlier this year.
However, the companies received negative feedback about the discontinuation and decided to keep the 140 mg capsules on the market.
In February, the US Food and Drug Administration (FDA) approved a single-tablet formulation of Imbruvica that is available in 4 doses—140 mg, 280 mg, 420 mg, and 560 mg.
Pharmacyclics and Janssen introduced this formulation to enable a once-a-day dosing regimen. The companies said the goal with the new formulation was to improve adherence because some patients had to take 3 or 4 pills every day to get the recommended dose of Imbruvica.
After introducing the new formulation, Pharmacyclics and Janssen planned to discontinue the 140 mg capsules.
Critics spoke out against this change in an article published in The Cancer Letter. They noted that discontinuing the old formulation would mean price increases for some patients. That’s because the single-tablet formulation of Imbruvica has the same price regardless of dose—$400 per tablet.
Patients on lower doses of Imbruvica would experience an increase in cost if they switched from the capsules to the tablet formulation. In fact, costs could triple for patients on the 140 mg dose.
Pharmacyclics argued that most patients on Imbruvica—those taking the 420 mg and 560 mg doses—would see no increase in out-of-pocket costs when transitioning to the single-tablet formulation. And patients on the 560 mg dose would likely see a decrease in their out-of-pocket costs.
However, critics pointed to results of a recent pilot study, which indicated that the recommended dose of Imbruvica for patients with chronic lymphocytic leukemia (CLL)—420 mg—may be too high. The results suggested that CLL patients could receive lower doses of Imbruvica without a reduction in efficacy.
Therefore, keeping the 140 mg capsules on the market could mean lower costs for some CLL patients.
In addition to voicing concerns about costs, the critics pointed out that discontinuing the 140 mg capsules of Imbruvica would make it more difficult to adjust patients’ doses when needed.
Pharmacyclics said its YOU&i™ Dose Exchange Program can aid healthcare professionals in adjusting doses before patients have finished their current pack of Imbruvica. Patients would receive a “rapid shipment” of their new dose at no additional cost.
But the critics said this program “creates a barrier to optimal prescribing for some patients” and urged the FDA to review the safety of the program.
Roughly a month after the critics made this recommendation in The Cancer Letter article, Pharmacyclics announced that the 140 mg capsules of Imbruvica would remain on the market.
Pediatric cancers are on the rise
PITTSBURGH – The incidence of many pediatric cancers are on the rise, and the increase is occurring in nearly all demographic groups studied, according to the latest data from the U.S. Centers for Disease Control and Prevention.
Pediatric cancers that increased significantly in incidence from 2001 through 2014, compared with previous time periods, include thyroid carcinoma, hepatic tumors, lymphomas, renal tumors, and brain tumors. Other cancer types remained unchanged, except malignant melanoma, which saw a significant decline in incidence over the same period, reported David A. Siegel, MD, of the Epidemic Intelligence Service at the CDC in Atlanta.
Recent studies of trends in pediatric cancer have either used data from before 2010 or covered less than a third of the U.S. population, the investigators noted.
To get a more accurate estimate of current trends, the investigators relied on the United States Cancer Statistics, which combines data from the Surveillance, Epidemiology, and End Results (SEER) program and the National Program of Cancer Registries. Together, the combined databases cover 100% of the U.S. population.
Dr. Siegel and his colleagues looked at cancer incidence rates and trends among individuals younger than 20 years of age from across 48 states from 2001 to 2014 – Mississippi, Nevada, and the District of Columbia were not included.
They used a joinpoint regression method to calculate average annual percent change (AAPC) in rates, then stratified rates and trends by sex, age, and race/ethnicity; location; economic status; and cancer type.
During the 14-year period of the study, there were a total of 196,200 incident cases of pediatric cancer, for an overall cancer incidence rate of 173 per million. The pediatric cancer with the highest incident rate was leukemia of any type (45.6 per million), brain tumors (30.8), and lymphomas (26.0).
Incidence rates were highest among males, patients from infancy through age 4, non-Hispanic whites, children who live in the Northeast region, those who live in the wealthiest counties, and those who live in urban/metropolitan counties. The overall pediatric cancer incidence rate increased, with an AAPC of 0.7 (95% confidence interval, 0.5-0.8).
“Rates increased in each stratum of sex, age, and race/ethnicity (except non-Hispanic American Indian/Alaska Native), region, economic status, and rural/urban classification,” the investigators wrote.
Cancers with significantly increased AAPC included thyroid carcinomas (AAPC, 4.8), hepatic tumors (2.5), lymphomas (1.7), renal tumors (0.6), and brain tumors (all types, 0.4).
There were no significant changes in the incidence of either germ cell cancer, retinoblastoma, leukemia, neuroblastoma, soft-tissue sarcomas, or bone tumors.
The only significant decrease over the study period was in the incidence of melanoma in children (–2.6).
“Possible causes of increasing rates might include changes in diagnostic, coding, and reporting standards, increased detection, population-based changes (such as increasing obesity), and environmental exposures,” they wrote.
Public health campaigns about the dangers of UV exposure and promoting the use of sunscreens may account for the decline in the incidence of malignant melanoma, they suggested.
The study was supported by the CDC. Dr. Siegel and coauthors are CDC employees. They reported having no conflicts of interest.
SOURCE: Siegel DA et al. ASPHO 2018, Abstract 605.
PITTSBURGH – The incidence of many pediatric cancers are on the rise, and the increase is occurring in nearly all demographic groups studied, according to the latest data from the U.S. Centers for Disease Control and Prevention.
Pediatric cancers that increased significantly in incidence from 2001 through 2014, compared with previous time periods, include thyroid carcinoma, hepatic tumors, lymphomas, renal tumors, and brain tumors. Other cancer types remained unchanged, except malignant melanoma, which saw a significant decline in incidence over the same period, reported David A. Siegel, MD, of the Epidemic Intelligence Service at the CDC in Atlanta.
Recent studies of trends in pediatric cancer have either used data from before 2010 or covered less than a third of the U.S. population, the investigators noted.
To get a more accurate estimate of current trends, the investigators relied on the United States Cancer Statistics, which combines data from the Surveillance, Epidemiology, and End Results (SEER) program and the National Program of Cancer Registries. Together, the combined databases cover 100% of the U.S. population.
Dr. Siegel and his colleagues looked at cancer incidence rates and trends among individuals younger than 20 years of age from across 48 states from 2001 to 2014 – Mississippi, Nevada, and the District of Columbia were not included.
They used a joinpoint regression method to calculate average annual percent change (AAPC) in rates, then stratified rates and trends by sex, age, and race/ethnicity; location; economic status; and cancer type.
During the 14-year period of the study, there were a total of 196,200 incident cases of pediatric cancer, for an overall cancer incidence rate of 173 per million. The pediatric cancer with the highest incident rate was leukemia of any type (45.6 per million), brain tumors (30.8), and lymphomas (26.0).
Incidence rates were highest among males, patients from infancy through age 4, non-Hispanic whites, children who live in the Northeast region, those who live in the wealthiest counties, and those who live in urban/metropolitan counties. The overall pediatric cancer incidence rate increased, with an AAPC of 0.7 (95% confidence interval, 0.5-0.8).
“Rates increased in each stratum of sex, age, and race/ethnicity (except non-Hispanic American Indian/Alaska Native), region, economic status, and rural/urban classification,” the investigators wrote.
Cancers with significantly increased AAPC included thyroid carcinomas (AAPC, 4.8), hepatic tumors (2.5), lymphomas (1.7), renal tumors (0.6), and brain tumors (all types, 0.4).
There were no significant changes in the incidence of either germ cell cancer, retinoblastoma, leukemia, neuroblastoma, soft-tissue sarcomas, or bone tumors.
The only significant decrease over the study period was in the incidence of melanoma in children (–2.6).
“Possible causes of increasing rates might include changes in diagnostic, coding, and reporting standards, increased detection, population-based changes (such as increasing obesity), and environmental exposures,” they wrote.
Public health campaigns about the dangers of UV exposure and promoting the use of sunscreens may account for the decline in the incidence of malignant melanoma, they suggested.
The study was supported by the CDC. Dr. Siegel and coauthors are CDC employees. They reported having no conflicts of interest.
SOURCE: Siegel DA et al. ASPHO 2018, Abstract 605.
PITTSBURGH – The incidence of many pediatric cancers are on the rise, and the increase is occurring in nearly all demographic groups studied, according to the latest data from the U.S. Centers for Disease Control and Prevention.
Pediatric cancers that increased significantly in incidence from 2001 through 2014, compared with previous time periods, include thyroid carcinoma, hepatic tumors, lymphomas, renal tumors, and brain tumors. Other cancer types remained unchanged, except malignant melanoma, which saw a significant decline in incidence over the same period, reported David A. Siegel, MD, of the Epidemic Intelligence Service at the CDC in Atlanta.
Recent studies of trends in pediatric cancer have either used data from before 2010 or covered less than a third of the U.S. population, the investigators noted.
To get a more accurate estimate of current trends, the investigators relied on the United States Cancer Statistics, which combines data from the Surveillance, Epidemiology, and End Results (SEER) program and the National Program of Cancer Registries. Together, the combined databases cover 100% of the U.S. population.
Dr. Siegel and his colleagues looked at cancer incidence rates and trends among individuals younger than 20 years of age from across 48 states from 2001 to 2014 – Mississippi, Nevada, and the District of Columbia were not included.
They used a joinpoint regression method to calculate average annual percent change (AAPC) in rates, then stratified rates and trends by sex, age, and race/ethnicity; location; economic status; and cancer type.
During the 14-year period of the study, there were a total of 196,200 incident cases of pediatric cancer, for an overall cancer incidence rate of 173 per million. The pediatric cancer with the highest incident rate was leukemia of any type (45.6 per million), brain tumors (30.8), and lymphomas (26.0).
Incidence rates were highest among males, patients from infancy through age 4, non-Hispanic whites, children who live in the Northeast region, those who live in the wealthiest counties, and those who live in urban/metropolitan counties. The overall pediatric cancer incidence rate increased, with an AAPC of 0.7 (95% confidence interval, 0.5-0.8).
“Rates increased in each stratum of sex, age, and race/ethnicity (except non-Hispanic American Indian/Alaska Native), region, economic status, and rural/urban classification,” the investigators wrote.
Cancers with significantly increased AAPC included thyroid carcinomas (AAPC, 4.8), hepatic tumors (2.5), lymphomas (1.7), renal tumors (0.6), and brain tumors (all types, 0.4).
There were no significant changes in the incidence of either germ cell cancer, retinoblastoma, leukemia, neuroblastoma, soft-tissue sarcomas, or bone tumors.
The only significant decrease over the study period was in the incidence of melanoma in children (–2.6).
“Possible causes of increasing rates might include changes in diagnostic, coding, and reporting standards, increased detection, population-based changes (such as increasing obesity), and environmental exposures,” they wrote.
Public health campaigns about the dangers of UV exposure and promoting the use of sunscreens may account for the decline in the incidence of malignant melanoma, they suggested.
The study was supported by the CDC. Dr. Siegel and coauthors are CDC employees. They reported having no conflicts of interest.
SOURCE: Siegel DA et al. ASPHO 2018, Abstract 605.
REPORTING FROM ASPHO 2018
Key clinical point: Major finding: From 2001 to 2014, there were 196,200 incident cases of pediatric cancer for an overall cancer incidence rate of 173 per 1 million.
Study details: A review of data from the United States Cancer Statistics for children under age 20.
Disclosures: The CDC supported the study. Dr. Siegel and his coauthors are CDC employees. They reported having no conflicts of interest.
Source: Siegel DA et al. ASPHO 2018, Abstract 605.
Adding bortezomib does not improve MCL outcomes
Bortezomib added to an alternating chemoimmunotherapy regimen did not improve time to treatment failure in patients with newly diagnosed mantle cell lymphoma (MCL), results of a phase 2 study have suggested.
Response rates and time to treatment failure were similar to what has been seen historically without the addition of bortezomib, according to study investigator Jorge E. Romaguera, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The phase 2 study included 95 patients with newly diagnosed MCL treated with alternating cycles of bortezomib added to rituximab plus hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (BzR-hyperCVAD) and bortezomib added to rituximab plus high-dose methotrexate and high-dose cytarabine (BzR-MA).
Of 87 patients evaluable for response, alternating BzR-hyperCVAD/BzR-MA resulted in an overall response rate of 100% and a complete response rate of 82%, Dr. Romaguera and his colleagues reported in the journal Cancer. At a median follow-up of 44 months, median time to treatment failure was 55 months, and median overall survival had not yet been reached, according to the report.
Dr. Romaguera and his coauthors compared these results with those from a previous study of alternating R-hyperCVAD/R-MA, in which the median time to treatment failure was 56.4 months. “This suggests that the addition of bortezomib does not improve the outcome,” they wrote in the current report.
Although more follow-up is needed, the landscape of MCL treatment is changing quickly, they added. In particular, lenalidomide and ibrutinib, already approved for relapsed/refractory MCL, are now being evaluated as part of first-line MCL regimens. “These drugs will offer strategies of either consolidation or maintenance after induction and will hopefully help continue to improve the duration of the initial response and the overall outcome,” the researchers wrote.
In the current phase 2 study, the fact that 100% of patients achieved complete response suggested that relapses come from minimal residual disease, which “has clearly become a clinical factor for the outcomes of patients with MCL and will likely become the next endpoint,” they wrote.
The researchers reported having no financial disclosures related to the study, which was supported by Takeda Oncology.
SOURCE: Romaguera JE et al. Cancer. 2018 May 3. doi: 10.1002/cncr.31361.
Bortezomib added to an alternating chemoimmunotherapy regimen did not improve time to treatment failure in patients with newly diagnosed mantle cell lymphoma (MCL), results of a phase 2 study have suggested.
Response rates and time to treatment failure were similar to what has been seen historically without the addition of bortezomib, according to study investigator Jorge E. Romaguera, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The phase 2 study included 95 patients with newly diagnosed MCL treated with alternating cycles of bortezomib added to rituximab plus hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (BzR-hyperCVAD) and bortezomib added to rituximab plus high-dose methotrexate and high-dose cytarabine (BzR-MA).
Of 87 patients evaluable for response, alternating BzR-hyperCVAD/BzR-MA resulted in an overall response rate of 100% and a complete response rate of 82%, Dr. Romaguera and his colleagues reported in the journal Cancer. At a median follow-up of 44 months, median time to treatment failure was 55 months, and median overall survival had not yet been reached, according to the report.
Dr. Romaguera and his coauthors compared these results with those from a previous study of alternating R-hyperCVAD/R-MA, in which the median time to treatment failure was 56.4 months. “This suggests that the addition of bortezomib does not improve the outcome,” they wrote in the current report.
Although more follow-up is needed, the landscape of MCL treatment is changing quickly, they added. In particular, lenalidomide and ibrutinib, already approved for relapsed/refractory MCL, are now being evaluated as part of first-line MCL regimens. “These drugs will offer strategies of either consolidation or maintenance after induction and will hopefully help continue to improve the duration of the initial response and the overall outcome,” the researchers wrote.
In the current phase 2 study, the fact that 100% of patients achieved complete response suggested that relapses come from minimal residual disease, which “has clearly become a clinical factor for the outcomes of patients with MCL and will likely become the next endpoint,” they wrote.
The researchers reported having no financial disclosures related to the study, which was supported by Takeda Oncology.
SOURCE: Romaguera JE et al. Cancer. 2018 May 3. doi: 10.1002/cncr.31361.
Bortezomib added to an alternating chemoimmunotherapy regimen did not improve time to treatment failure in patients with newly diagnosed mantle cell lymphoma (MCL), results of a phase 2 study have suggested.
Response rates and time to treatment failure were similar to what has been seen historically without the addition of bortezomib, according to study investigator Jorge E. Romaguera, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The phase 2 study included 95 patients with newly diagnosed MCL treated with alternating cycles of bortezomib added to rituximab plus hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (BzR-hyperCVAD) and bortezomib added to rituximab plus high-dose methotrexate and high-dose cytarabine (BzR-MA).
Of 87 patients evaluable for response, alternating BzR-hyperCVAD/BzR-MA resulted in an overall response rate of 100% and a complete response rate of 82%, Dr. Romaguera and his colleagues reported in the journal Cancer. At a median follow-up of 44 months, median time to treatment failure was 55 months, and median overall survival had not yet been reached, according to the report.
Dr. Romaguera and his coauthors compared these results with those from a previous study of alternating R-hyperCVAD/R-MA, in which the median time to treatment failure was 56.4 months. “This suggests that the addition of bortezomib does not improve the outcome,” they wrote in the current report.
Although more follow-up is needed, the landscape of MCL treatment is changing quickly, they added. In particular, lenalidomide and ibrutinib, already approved for relapsed/refractory MCL, are now being evaluated as part of first-line MCL regimens. “These drugs will offer strategies of either consolidation or maintenance after induction and will hopefully help continue to improve the duration of the initial response and the overall outcome,” the researchers wrote.
In the current phase 2 study, the fact that 100% of patients achieved complete response suggested that relapses come from minimal residual disease, which “has clearly become a clinical factor for the outcomes of patients with MCL and will likely become the next endpoint,” they wrote.
The researchers reported having no financial disclosures related to the study, which was supported by Takeda Oncology.
SOURCE: Romaguera JE et al. Cancer. 2018 May 3. doi: 10.1002/cncr.31361.
FROM CANCER
Key clinical point:
Major finding: Rates of overall and complete response were 100% and 82%, respectively, while time to treatment failure was 55 months.
Study details: A phase 2 trial that included 95 patients treated with alternating cycles of bortezomib added to rituximab plus hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (BzR-hyperCVAD) and bortezomib added to rituximab plus high-dose methotrexate and high-dose cytarabine (BzR-MA).
Disclosures: The study was supported by Takeda Oncology. The researchers reported having no financial disclosures related to the study.
Source: Romaguera JE et al. Cancer. 2018 May 3. doi: 10.1002/cncr.31361
Umbralisib has ‘distinct’ safety profile
Phase 1 trial results suggest umbralisib, a PI3Kδ/CK1ε inhibitor, can be safe and active in patients with relapsed or refractory B-cell malignancies.
Researchers said the safety profile of umbralisib “was distinct from that of other PI3Kδ inhibitors,” as it produced few immune-mediated adverse events (AEs).
Umbralisib also produced an objective response rate of 37% in the entire study cohort, 80% in patients with chronic lymphocytic leukemia (CLL), 53% in patients with follicular lymphoma (FL), and 31% in patients with diffuse large B-cell lymphoma (DLBCL).
These results were published in The Lancet Oncology. The study was sponsored by TG Therapeutics, Inc.
The trial enrolled 90 patients between January 17, 2013, and January 14, 2016.
There were 24 patients with CLL, 22 with FL, 16 with DLBCL, 11 with Hodgkin lymphoma, 6 with mantle cell lymphoma, 5 with marginal zone lymphoma, 3 with Waldenstrom’s macroglobulinemia, 2 with T-cell lymphoma, and 1 with hairy cell leukemia.
The median number of prior therapies was 3 (range, 2-5), and 49% of patients were refractory to previous therapy.
Treatment
Patients took umbralisib once daily in 28-day cycles until disease progression, unacceptable toxicity, or withdrawal of consent.
Initially, patients took the drug in a fasting state at doses of 50 mg, 100 mg, 200 mg, 400 mg, 800 mg, 1200 mg, or 1800 mg.
In April 2014, the researchers did a second dose-escalation with a micronized formulation of umbralisib, taken with food, at doses of 200 mg, 400 mg, 800 mg, 1200 mg, or 1800 mg.
In August, 2014, all patients who were still on the study transitioned to the 800 mg dose of the micronized formulation. This was the recommended phase 2 dose.
At the data cutoff in November 2016, 44 patients (49%) had received umbralisib for more than 6 cycles, and 23 (26%) had received the drug for more than 12 cycles. Thirteen patients (14%) were still taking umbralisib at the end of the study.
Most patients who stopped treatment did so because of disease progression (n=50, 56%) or AEs (n=9, 10%).
“We are pleased to have treated the first patient ever with umbralisib over 5 years ago and believe it has an important place in the treatment landscape for patients with hematologic malignancies,” said study author Howard A. Burris, MD, of the Sarah Cannon Research Institute in Nashville, Tennessee.
“Several patients from this phase 1 study are still on study today, approaching 5 years of continuous daily therapy, speaking to both the safety and efficacy profile of this unique agent.”
Safety
Dose-limiting toxicities (DLTs) occurred in 4 patients. One DLT was grade 3 maculopapular rash in a patient receiving the 800 mg dose of the initial formulation.
Another DLT was grade 3 hypokalemia in a patient receiving 1800 mg of the initial formulation. A third DLT was grade 3 fatigue, which occurred in 2 patients receiving 1800 mg of the micronized formulation.
Because of these toxicities, the maximum tolerated dose was 1200 mg of the micronized formulation.
The most common treatment-emergent AEs were diarrhea (43%), nausea (42%), and fatigue (31%). The most common grade 3/4 AEs were neutropenia (13%), anemia (9%), and thrombocytopenia (7%).
Serious AEs considered at least possibly related to umbralisib were pneumonia (3%), lung infection (1%), febrile neutropenia (1%), and colitis (2%).
Treatment discontinuation due to AEs considered at least possibly related to umbralisib occurred in 6 patients (7%). Two patients had grade 3 colitis, 2 had increased ALT/AST (grade 1 and grade 4), 1 had grade 2 diarrhea, and 1 had grade 3 fatigue.
There were no treatment-related deaths.
The researchers said the safety profile of umbralisib was distinct from that of other PI3Kδ inhibitors, as patients in this trial had fewer occurrences of autoimmune-like toxicities, such as colitis.
“Preclinically, umbralisib has a very unique profile, selectively inhibiting both PI3Kδ and CK1ε,” said study author Owen O’Connor, MD, PhD, of Columbia Presbyterian Medical Center in New York, New York.
“The clinical results in this paper support our thesis that the differentiated preclinical profile explains the differences seen in the clinic between umbralisib and the other PI3Kδ inhibitors.”
Response
The objective response rate was 37%, with 33 patients achieving a response and 3 patients having a complete response (CR).
Sixteen CLL patients responded (80%), all with partial responses (PRs). Four DLBCL patients responded (31%), all with PRs. And 9 FL patients responded (53%), 2 with CRs.
The remaining CR occurred in a Hodgkin lymphoma patient, and this was the only response in this patient group.
One patient with marginal zone lymphoma had a PR, as did 1 patient with mantle cell lymphoma. All other patients had stable disease or progressed.
The mean duration of response was 13.4 months in the CLL patients, 6.4 months in the DLBCL patients, and 9.3 months in the FL patients.
Phase 1 trial results suggest umbralisib, a PI3Kδ/CK1ε inhibitor, can be safe and active in patients with relapsed or refractory B-cell malignancies.
Researchers said the safety profile of umbralisib “was distinct from that of other PI3Kδ inhibitors,” as it produced few immune-mediated adverse events (AEs).
Umbralisib also produced an objective response rate of 37% in the entire study cohort, 80% in patients with chronic lymphocytic leukemia (CLL), 53% in patients with follicular lymphoma (FL), and 31% in patients with diffuse large B-cell lymphoma (DLBCL).
These results were published in The Lancet Oncology. The study was sponsored by TG Therapeutics, Inc.
The trial enrolled 90 patients between January 17, 2013, and January 14, 2016.
There were 24 patients with CLL, 22 with FL, 16 with DLBCL, 11 with Hodgkin lymphoma, 6 with mantle cell lymphoma, 5 with marginal zone lymphoma, 3 with Waldenstrom’s macroglobulinemia, 2 with T-cell lymphoma, and 1 with hairy cell leukemia.
The median number of prior therapies was 3 (range, 2-5), and 49% of patients were refractory to previous therapy.
Treatment
Patients took umbralisib once daily in 28-day cycles until disease progression, unacceptable toxicity, or withdrawal of consent.
Initially, patients took the drug in a fasting state at doses of 50 mg, 100 mg, 200 mg, 400 mg, 800 mg, 1200 mg, or 1800 mg.
In April 2014, the researchers did a second dose-escalation with a micronized formulation of umbralisib, taken with food, at doses of 200 mg, 400 mg, 800 mg, 1200 mg, or 1800 mg.
In August, 2014, all patients who were still on the study transitioned to the 800 mg dose of the micronized formulation. This was the recommended phase 2 dose.
At the data cutoff in November 2016, 44 patients (49%) had received umbralisib for more than 6 cycles, and 23 (26%) had received the drug for more than 12 cycles. Thirteen patients (14%) were still taking umbralisib at the end of the study.
Most patients who stopped treatment did so because of disease progression (n=50, 56%) or AEs (n=9, 10%).
“We are pleased to have treated the first patient ever with umbralisib over 5 years ago and believe it has an important place in the treatment landscape for patients with hematologic malignancies,” said study author Howard A. Burris, MD, of the Sarah Cannon Research Institute in Nashville, Tennessee.
“Several patients from this phase 1 study are still on study today, approaching 5 years of continuous daily therapy, speaking to both the safety and efficacy profile of this unique agent.”
Safety
Dose-limiting toxicities (DLTs) occurred in 4 patients. One DLT was grade 3 maculopapular rash in a patient receiving the 800 mg dose of the initial formulation.
Another DLT was grade 3 hypokalemia in a patient receiving 1800 mg of the initial formulation. A third DLT was grade 3 fatigue, which occurred in 2 patients receiving 1800 mg of the micronized formulation.
Because of these toxicities, the maximum tolerated dose was 1200 mg of the micronized formulation.
The most common treatment-emergent AEs were diarrhea (43%), nausea (42%), and fatigue (31%). The most common grade 3/4 AEs were neutropenia (13%), anemia (9%), and thrombocytopenia (7%).
Serious AEs considered at least possibly related to umbralisib were pneumonia (3%), lung infection (1%), febrile neutropenia (1%), and colitis (2%).
Treatment discontinuation due to AEs considered at least possibly related to umbralisib occurred in 6 patients (7%). Two patients had grade 3 colitis, 2 had increased ALT/AST (grade 1 and grade 4), 1 had grade 2 diarrhea, and 1 had grade 3 fatigue.
There were no treatment-related deaths.
The researchers said the safety profile of umbralisib was distinct from that of other PI3Kδ inhibitors, as patients in this trial had fewer occurrences of autoimmune-like toxicities, such as colitis.
“Preclinically, umbralisib has a very unique profile, selectively inhibiting both PI3Kδ and CK1ε,” said study author Owen O’Connor, MD, PhD, of Columbia Presbyterian Medical Center in New York, New York.
“The clinical results in this paper support our thesis that the differentiated preclinical profile explains the differences seen in the clinic between umbralisib and the other PI3Kδ inhibitors.”
Response
The objective response rate was 37%, with 33 patients achieving a response and 3 patients having a complete response (CR).
Sixteen CLL patients responded (80%), all with partial responses (PRs). Four DLBCL patients responded (31%), all with PRs. And 9 FL patients responded (53%), 2 with CRs.
The remaining CR occurred in a Hodgkin lymphoma patient, and this was the only response in this patient group.
One patient with marginal zone lymphoma had a PR, as did 1 patient with mantle cell lymphoma. All other patients had stable disease or progressed.
The mean duration of response was 13.4 months in the CLL patients, 6.4 months in the DLBCL patients, and 9.3 months in the FL patients.
Phase 1 trial results suggest umbralisib, a PI3Kδ/CK1ε inhibitor, can be safe and active in patients with relapsed or refractory B-cell malignancies.
Researchers said the safety profile of umbralisib “was distinct from that of other PI3Kδ inhibitors,” as it produced few immune-mediated adverse events (AEs).
Umbralisib also produced an objective response rate of 37% in the entire study cohort, 80% in patients with chronic lymphocytic leukemia (CLL), 53% in patients with follicular lymphoma (FL), and 31% in patients with diffuse large B-cell lymphoma (DLBCL).
These results were published in The Lancet Oncology. The study was sponsored by TG Therapeutics, Inc.
The trial enrolled 90 patients between January 17, 2013, and January 14, 2016.
There were 24 patients with CLL, 22 with FL, 16 with DLBCL, 11 with Hodgkin lymphoma, 6 with mantle cell lymphoma, 5 with marginal zone lymphoma, 3 with Waldenstrom’s macroglobulinemia, 2 with T-cell lymphoma, and 1 with hairy cell leukemia.
The median number of prior therapies was 3 (range, 2-5), and 49% of patients were refractory to previous therapy.
Treatment
Patients took umbralisib once daily in 28-day cycles until disease progression, unacceptable toxicity, or withdrawal of consent.
Initially, patients took the drug in a fasting state at doses of 50 mg, 100 mg, 200 mg, 400 mg, 800 mg, 1200 mg, or 1800 mg.
In April 2014, the researchers did a second dose-escalation with a micronized formulation of umbralisib, taken with food, at doses of 200 mg, 400 mg, 800 mg, 1200 mg, or 1800 mg.
In August, 2014, all patients who were still on the study transitioned to the 800 mg dose of the micronized formulation. This was the recommended phase 2 dose.
At the data cutoff in November 2016, 44 patients (49%) had received umbralisib for more than 6 cycles, and 23 (26%) had received the drug for more than 12 cycles. Thirteen patients (14%) were still taking umbralisib at the end of the study.
Most patients who stopped treatment did so because of disease progression (n=50, 56%) or AEs (n=9, 10%).
“We are pleased to have treated the first patient ever with umbralisib over 5 years ago and believe it has an important place in the treatment landscape for patients with hematologic malignancies,” said study author Howard A. Burris, MD, of the Sarah Cannon Research Institute in Nashville, Tennessee.
“Several patients from this phase 1 study are still on study today, approaching 5 years of continuous daily therapy, speaking to both the safety and efficacy profile of this unique agent.”
Safety
Dose-limiting toxicities (DLTs) occurred in 4 patients. One DLT was grade 3 maculopapular rash in a patient receiving the 800 mg dose of the initial formulation.
Another DLT was grade 3 hypokalemia in a patient receiving 1800 mg of the initial formulation. A third DLT was grade 3 fatigue, which occurred in 2 patients receiving 1800 mg of the micronized formulation.
Because of these toxicities, the maximum tolerated dose was 1200 mg of the micronized formulation.
The most common treatment-emergent AEs were diarrhea (43%), nausea (42%), and fatigue (31%). The most common grade 3/4 AEs were neutropenia (13%), anemia (9%), and thrombocytopenia (7%).
Serious AEs considered at least possibly related to umbralisib were pneumonia (3%), lung infection (1%), febrile neutropenia (1%), and colitis (2%).
Treatment discontinuation due to AEs considered at least possibly related to umbralisib occurred in 6 patients (7%). Two patients had grade 3 colitis, 2 had increased ALT/AST (grade 1 and grade 4), 1 had grade 2 diarrhea, and 1 had grade 3 fatigue.
There were no treatment-related deaths.
The researchers said the safety profile of umbralisib was distinct from that of other PI3Kδ inhibitors, as patients in this trial had fewer occurrences of autoimmune-like toxicities, such as colitis.
“Preclinically, umbralisib has a very unique profile, selectively inhibiting both PI3Kδ and CK1ε,” said study author Owen O’Connor, MD, PhD, of Columbia Presbyterian Medical Center in New York, New York.
“The clinical results in this paper support our thesis that the differentiated preclinical profile explains the differences seen in the clinic between umbralisib and the other PI3Kδ inhibitors.”
Response
The objective response rate was 37%, with 33 patients achieving a response and 3 patients having a complete response (CR).
Sixteen CLL patients responded (80%), all with partial responses (PRs). Four DLBCL patients responded (31%), all with PRs. And 9 FL patients responded (53%), 2 with CRs.
The remaining CR occurred in a Hodgkin lymphoma patient, and this was the only response in this patient group.
One patient with marginal zone lymphoma had a PR, as did 1 patient with mantle cell lymphoma. All other patients had stable disease or progressed.
The mean duration of response was 13.4 months in the CLL patients, 6.4 months in the DLBCL patients, and 9.3 months in the FL patients.
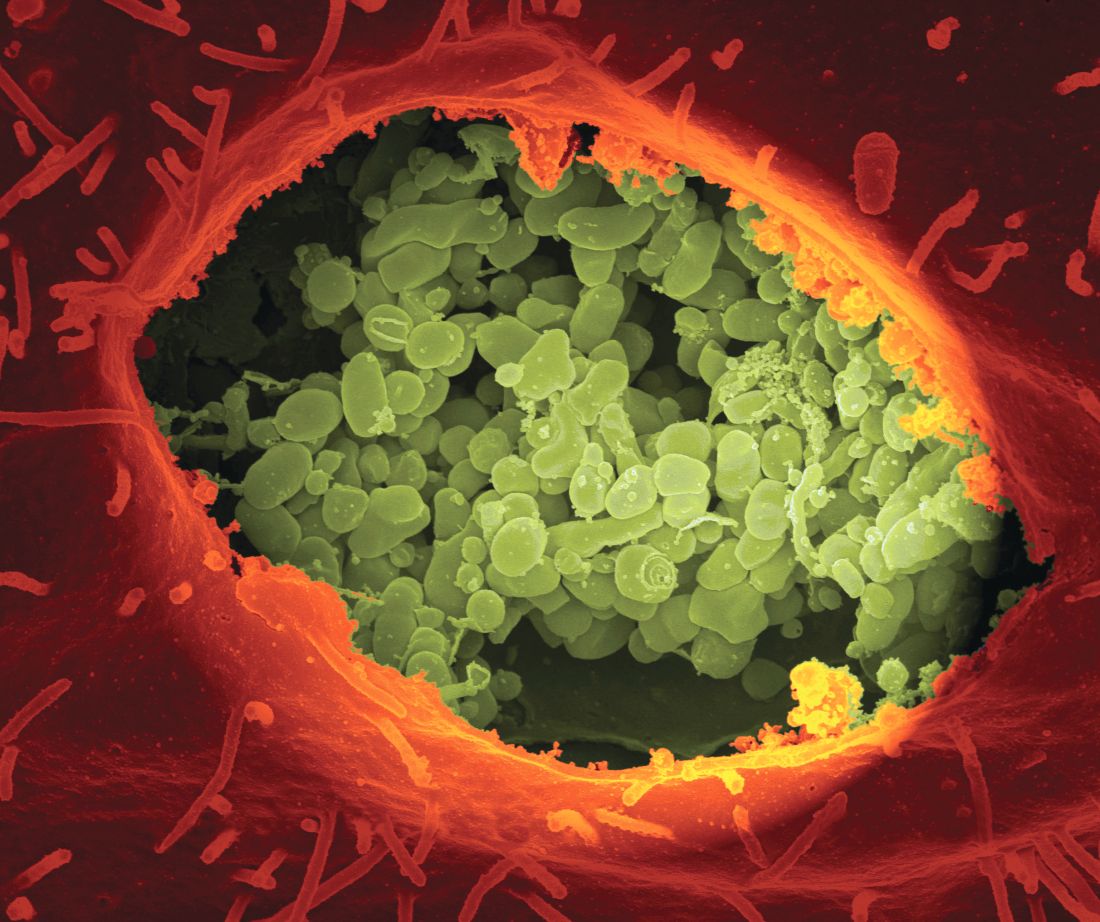
Study: No link between non-Hodgkin lymphoma and Q fever
Sonja E. van Roeden, MD, and colleagues from Utrecht University, the Netherlands, performed a retrospective, population-based analysis of the entire general population of the Netherlands from 2002 to 2013, encompassing the 3-year period of a large Q fever epidemic in the country.
In total, there were 48,760 cases of NHL diagnosed between Jan. 1, 2002 and Dec. 31, 2013, with the annual incidence ranging from 21.4 cases per 100,000 population in 2002 to 26.7 in 2010. While researchers found a significant association between NHL incidence and areas of high endemicity of Q fever in 2009 (relative risk 1.16; P = .029), there were no other associations.
Among the 439 people with chronic Q fever, 5 went on to develop NHL, resulting in a relative risk of 4.99 (P = .0003), compared with the general population of the Netherlands.
“The absence of an exposure-response relation between the intensity of exposure and risk of non-Hodgkin lymphoma, based on reported incidence of acute Q fever, does not imply a causal relation,” the researchers wrote. “However, one could consider exposure to C. burnetii in people with chronic Q fever as more intense than in acute Q fever because of the ongoing character and duration of exposure, and assume an exposure-response relation on the basis of the higher risk for non-Hodgkin lymphoma in patients with chronic Q fever.”
The researchers reported having no financial disclosures.
SOURCE: van Roeden SE et al. Lancet Haematol. 2018 May;5:e211-9.
Sonja E. van Roeden, MD, and colleagues from Utrecht University, the Netherlands, performed a retrospective, population-based analysis of the entire general population of the Netherlands from 2002 to 2013, encompassing the 3-year period of a large Q fever epidemic in the country.
In total, there were 48,760 cases of NHL diagnosed between Jan. 1, 2002 and Dec. 31, 2013, with the annual incidence ranging from 21.4 cases per 100,000 population in 2002 to 26.7 in 2010. While researchers found a significant association between NHL incidence and areas of high endemicity of Q fever in 2009 (relative risk 1.16; P = .029), there were no other associations.
Among the 439 people with chronic Q fever, 5 went on to develop NHL, resulting in a relative risk of 4.99 (P = .0003), compared with the general population of the Netherlands.
“The absence of an exposure-response relation between the intensity of exposure and risk of non-Hodgkin lymphoma, based on reported incidence of acute Q fever, does not imply a causal relation,” the researchers wrote. “However, one could consider exposure to C. burnetii in people with chronic Q fever as more intense than in acute Q fever because of the ongoing character and duration of exposure, and assume an exposure-response relation on the basis of the higher risk for non-Hodgkin lymphoma in patients with chronic Q fever.”
The researchers reported having no financial disclosures.
SOURCE: van Roeden SE et al. Lancet Haematol. 2018 May;5:e211-9.
Sonja E. van Roeden, MD, and colleagues from Utrecht University, the Netherlands, performed a retrospective, population-based analysis of the entire general population of the Netherlands from 2002 to 2013, encompassing the 3-year period of a large Q fever epidemic in the country.
In total, there were 48,760 cases of NHL diagnosed between Jan. 1, 2002 and Dec. 31, 2013, with the annual incidence ranging from 21.4 cases per 100,000 population in 2002 to 26.7 in 2010. While researchers found a significant association between NHL incidence and areas of high endemicity of Q fever in 2009 (relative risk 1.16; P = .029), there were no other associations.
Among the 439 people with chronic Q fever, 5 went on to develop NHL, resulting in a relative risk of 4.99 (P = .0003), compared with the general population of the Netherlands.
“The absence of an exposure-response relation between the intensity of exposure and risk of non-Hodgkin lymphoma, based on reported incidence of acute Q fever, does not imply a causal relation,” the researchers wrote. “However, one could consider exposure to C. burnetii in people with chronic Q fever as more intense than in acute Q fever because of the ongoing character and duration of exposure, and assume an exposure-response relation on the basis of the higher risk for non-Hodgkin lymphoma in patients with chronic Q fever.”
The researchers reported having no financial disclosures.
SOURCE: van Roeden SE et al. Lancet Haematol. 2018 May;5:e211-9.
FROM LANCET HAEMATOLOGY
‘Long-term benefits’ with nivolumab in cHL
Nivolumab can provide “long-term benefits” in patients with relapsed or refractory classical Hodgkin lymphoma (cHL), according to researchers.
Extended follow-up of the CheckMate-205 study showed that nearly 70% of patients responded to nivolumab.
The median duration of response was 17 months, and the median progression-free survival (PFS) was 15 months.
The most common drug-related AEs were fatigue, diarrhea, infusion-related reactions, rash, nausea, and pruritus.
Philippe Armand, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts, and his colleagues reported these results in the Journal of Clinical Oncology.
The study was sponsored by Bristol-Myers Squibb Company.
Patients
This phase 2 trial enrolled 243 adults with relapsed or refractory cHL who had undergone autologous hematopoietic stem cell transplant (auto-HSCT).
Their median age was 34 (range, 26-46), and 58% were male. Fifty-seven percent had stage IV disease, 20% had stage III, 21% had stage II, and 2% had stage I.
Patients had received a median of 4 prior therapies (range, 3-5). The median time from diagnosis to first nivolumab dose was 4.5 years (range, 2.4-7.6), and the median time from most recent auto-HSCT to first nivolumab dose was 2.0 years (range, 0.9-4.9).
The researchers divided patients into 3 cohorts according to exposure to brentuximab vedotin (BV):
- Cohort A was BV-naïve (n=63)
- Cohort B received BV only after auto-HSCT (n=80)
- Cohort C received BV before and/or after auto-HSCT (n=100).
Baseline characteristics were generally similar across the cohorts. However, cohort A had fewer prior treatments (median of 2 vs 4 in cohorts B and C).
Cohort B had the longest interval between diagnosis and first nivolumab dose (6.2 years vs 3.1 in cohort A and 3.5 in C) and between most recent auto-HSCT and first nivolumab dose (3.4 years vs 1 in cohort A and 1.7 in C).
Treatment
All patients received nivolumab at 3 mg/kg once every 2 weeks until disease progression or unacceptable toxicity.
In cohort C, patients who were in complete response (CR) for 1 year had to discontinue nivolumab, but they could resume treatment if they relapsed within 2 years.
A protocol amendment allowed patients to continue treatment despite progression if they had stable performance status and were deriving “perceived clinical benefit.”
At a median follow-up of 18 months, 40% percent of all patients were still on treatment, including 48% of patients in cohort A, 40% in cohort B, and 35% in cohort C.
Safety
The most common drug-related AEs were fatigue (23%), diarrhea (15%), infusion-related reactions (14%), rash (12%), nausea (10%), and pruritus (10%).
The most common grade 3/4 drug-related AEs were lipase increase (5%), neutropenia (3%), ALT increase (2%), AST increase (2%), and amylase increase (2%).
The most common serious drug-related AEs were infusion-related reactions (2%), pneumonitis (1%), pneumonia (1%), pleural effusion (1%), and pyrexia (1%).
Seven percent of patients discontinued treatment due to AEs. The most common of these were pneumonitis (2%) and autoimmune hepatitis (1%).
There were no deaths due to drug-related AEs.
Efficacy
The objective response rate was 69% overall, 65% in cohort A, 68% in cohort B, and 73% in cohort C.
CR was the best response for 16% of all patients, 29% of cohort A, 13% of cohort B, and 12% of cohort C.
The median duration of response was 17 months overall, 20 months for cohort A, 16 months for cohort B, 15 months for cohort C, and 20 months for patients who achieved a CR.
The researchers said responses were similar irrespective of BV treatment sequence.
The median PFS was 15 months for all patients, 18 months for cohort A, 15 months for cohort B, 12 months for cohort C, and 22 months for patients who achieved a CR.
The median overall survival was not reached in any of the cohorts.
The 12-month overall survival was 92% overall, 93% in cohort A, 95% in cohort B, 90% in cohort C, and 100% in patients who achieved a CR.
Subsequent HSCT
Forty-four patients proceeded to allogeneic HSCT after nivolumab, and the median post-HSCT follow-up was 5.5 months (range, 2.9-11.8).
At 6 months, the rate of transplant-related mortality was 13%, and the rate of disease progression was 7%.
The rate of grade 2-4 acute graft-vs-host disease (GVHD) was 30%, the rate of grade 3-4 acute GVHD was 20%, and the rate of chronic GVHD was 15%.
Nivolumab can provide “long-term benefits” in patients with relapsed or refractory classical Hodgkin lymphoma (cHL), according to researchers.
Extended follow-up of the CheckMate-205 study showed that nearly 70% of patients responded to nivolumab.
The median duration of response was 17 months, and the median progression-free survival (PFS) was 15 months.
The most common drug-related AEs were fatigue, diarrhea, infusion-related reactions, rash, nausea, and pruritus.
Philippe Armand, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts, and his colleagues reported these results in the Journal of Clinical Oncology.
The study was sponsored by Bristol-Myers Squibb Company.
Patients
This phase 2 trial enrolled 243 adults with relapsed or refractory cHL who had undergone autologous hematopoietic stem cell transplant (auto-HSCT).
Their median age was 34 (range, 26-46), and 58% were male. Fifty-seven percent had stage IV disease, 20% had stage III, 21% had stage II, and 2% had stage I.
Patients had received a median of 4 prior therapies (range, 3-5). The median time from diagnosis to first nivolumab dose was 4.5 years (range, 2.4-7.6), and the median time from most recent auto-HSCT to first nivolumab dose was 2.0 years (range, 0.9-4.9).
The researchers divided patients into 3 cohorts according to exposure to brentuximab vedotin (BV):
- Cohort A was BV-naïve (n=63)
- Cohort B received BV only after auto-HSCT (n=80)
- Cohort C received BV before and/or after auto-HSCT (n=100).
Baseline characteristics were generally similar across the cohorts. However, cohort A had fewer prior treatments (median of 2 vs 4 in cohorts B and C).
Cohort B had the longest interval between diagnosis and first nivolumab dose (6.2 years vs 3.1 in cohort A and 3.5 in C) and between most recent auto-HSCT and first nivolumab dose (3.4 years vs 1 in cohort A and 1.7 in C).
Treatment
All patients received nivolumab at 3 mg/kg once every 2 weeks until disease progression or unacceptable toxicity.
In cohort C, patients who were in complete response (CR) for 1 year had to discontinue nivolumab, but they could resume treatment if they relapsed within 2 years.
A protocol amendment allowed patients to continue treatment despite progression if they had stable performance status and were deriving “perceived clinical benefit.”
At a median follow-up of 18 months, 40% percent of all patients were still on treatment, including 48% of patients in cohort A, 40% in cohort B, and 35% in cohort C.
Safety
The most common drug-related AEs were fatigue (23%), diarrhea (15%), infusion-related reactions (14%), rash (12%), nausea (10%), and pruritus (10%).
The most common grade 3/4 drug-related AEs were lipase increase (5%), neutropenia (3%), ALT increase (2%), AST increase (2%), and amylase increase (2%).
The most common serious drug-related AEs were infusion-related reactions (2%), pneumonitis (1%), pneumonia (1%), pleural effusion (1%), and pyrexia (1%).
Seven percent of patients discontinued treatment due to AEs. The most common of these were pneumonitis (2%) and autoimmune hepatitis (1%).
There were no deaths due to drug-related AEs.
Efficacy
The objective response rate was 69% overall, 65% in cohort A, 68% in cohort B, and 73% in cohort C.
CR was the best response for 16% of all patients, 29% of cohort A, 13% of cohort B, and 12% of cohort C.
The median duration of response was 17 months overall, 20 months for cohort A, 16 months for cohort B, 15 months for cohort C, and 20 months for patients who achieved a CR.
The researchers said responses were similar irrespective of BV treatment sequence.
The median PFS was 15 months for all patients, 18 months for cohort A, 15 months for cohort B, 12 months for cohort C, and 22 months for patients who achieved a CR.
The median overall survival was not reached in any of the cohorts.
The 12-month overall survival was 92% overall, 93% in cohort A, 95% in cohort B, 90% in cohort C, and 100% in patients who achieved a CR.
Subsequent HSCT
Forty-four patients proceeded to allogeneic HSCT after nivolumab, and the median post-HSCT follow-up was 5.5 months (range, 2.9-11.8).
At 6 months, the rate of transplant-related mortality was 13%, and the rate of disease progression was 7%.
The rate of grade 2-4 acute graft-vs-host disease (GVHD) was 30%, the rate of grade 3-4 acute GVHD was 20%, and the rate of chronic GVHD was 15%.
Nivolumab can provide “long-term benefits” in patients with relapsed or refractory classical Hodgkin lymphoma (cHL), according to researchers.
Extended follow-up of the CheckMate-205 study showed that nearly 70% of patients responded to nivolumab.
The median duration of response was 17 months, and the median progression-free survival (PFS) was 15 months.
The most common drug-related AEs were fatigue, diarrhea, infusion-related reactions, rash, nausea, and pruritus.
Philippe Armand, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts, and his colleagues reported these results in the Journal of Clinical Oncology.
The study was sponsored by Bristol-Myers Squibb Company.
Patients
This phase 2 trial enrolled 243 adults with relapsed or refractory cHL who had undergone autologous hematopoietic stem cell transplant (auto-HSCT).
Their median age was 34 (range, 26-46), and 58% were male. Fifty-seven percent had stage IV disease, 20% had stage III, 21% had stage II, and 2% had stage I.
Patients had received a median of 4 prior therapies (range, 3-5). The median time from diagnosis to first nivolumab dose was 4.5 years (range, 2.4-7.6), and the median time from most recent auto-HSCT to first nivolumab dose was 2.0 years (range, 0.9-4.9).
The researchers divided patients into 3 cohorts according to exposure to brentuximab vedotin (BV):
- Cohort A was BV-naïve (n=63)
- Cohort B received BV only after auto-HSCT (n=80)
- Cohort C received BV before and/or after auto-HSCT (n=100).
Baseline characteristics were generally similar across the cohorts. However, cohort A had fewer prior treatments (median of 2 vs 4 in cohorts B and C).
Cohort B had the longest interval between diagnosis and first nivolumab dose (6.2 years vs 3.1 in cohort A and 3.5 in C) and between most recent auto-HSCT and first nivolumab dose (3.4 years vs 1 in cohort A and 1.7 in C).
Treatment
All patients received nivolumab at 3 mg/kg once every 2 weeks until disease progression or unacceptable toxicity.
In cohort C, patients who were in complete response (CR) for 1 year had to discontinue nivolumab, but they could resume treatment if they relapsed within 2 years.
A protocol amendment allowed patients to continue treatment despite progression if they had stable performance status and were deriving “perceived clinical benefit.”
At a median follow-up of 18 months, 40% percent of all patients were still on treatment, including 48% of patients in cohort A, 40% in cohort B, and 35% in cohort C.
Safety
The most common drug-related AEs were fatigue (23%), diarrhea (15%), infusion-related reactions (14%), rash (12%), nausea (10%), and pruritus (10%).
The most common grade 3/4 drug-related AEs were lipase increase (5%), neutropenia (3%), ALT increase (2%), AST increase (2%), and amylase increase (2%).
The most common serious drug-related AEs were infusion-related reactions (2%), pneumonitis (1%), pneumonia (1%), pleural effusion (1%), and pyrexia (1%).
Seven percent of patients discontinued treatment due to AEs. The most common of these were pneumonitis (2%) and autoimmune hepatitis (1%).
There were no deaths due to drug-related AEs.
Efficacy
The objective response rate was 69% overall, 65% in cohort A, 68% in cohort B, and 73% in cohort C.
CR was the best response for 16% of all patients, 29% of cohort A, 13% of cohort B, and 12% of cohort C.
The median duration of response was 17 months overall, 20 months for cohort A, 16 months for cohort B, 15 months for cohort C, and 20 months for patients who achieved a CR.
The researchers said responses were similar irrespective of BV treatment sequence.
The median PFS was 15 months for all patients, 18 months for cohort A, 15 months for cohort B, 12 months for cohort C, and 22 months for patients who achieved a CR.
The median overall survival was not reached in any of the cohorts.
The 12-month overall survival was 92% overall, 93% in cohort A, 95% in cohort B, 90% in cohort C, and 100% in patients who achieved a CR.
Subsequent HSCT
Forty-four patients proceeded to allogeneic HSCT after nivolumab, and the median post-HSCT follow-up was 5.5 months (range, 2.9-11.8).
At 6 months, the rate of transplant-related mortality was 13%, and the rate of disease progression was 7%.
The rate of grade 2-4 acute graft-vs-host disease (GVHD) was 30%, the rate of grade 3-4 acute GVHD was 20%, and the rate of chronic GVHD was 15%.
Drug granted fast track designations for FL, DLBCL
The US Food and Drug Administration (FDA) has granted 2 fast track designations to 5F9, an anti-CD47 antibody.
The designations are for 5F9 as a treatment for relapsed or refractory diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL).
Data supporting the fast track designations were derived from a phase 1b/2 trial of 5F9 in combination with rituximab in patients with relapsed or refractory B-cell non-Hodgkin lymphoma, including DLBCL and FL.
Forty Seven, Inc., the company developing 5F9, expects to announce initial safety and efficacy data from the phase 1b portion of the trial in the second quarter of 2018.
About fast track designation
The FDA’s fast track drug development program is designed to expedite clinical development and submission of applications for drugs with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the drug’s development plan and written communications about issues such as trial design and use of biomarkers.
Drugs that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met.
Fast track drugs may also be eligible for rolling review, which allows a developer to submit individual sections of a drug’s application for review as they are ready, rather than waiting until all sections are complete.
The US Food and Drug Administration (FDA) has granted 2 fast track designations to 5F9, an anti-CD47 antibody.
The designations are for 5F9 as a treatment for relapsed or refractory diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL).
Data supporting the fast track designations were derived from a phase 1b/2 trial of 5F9 in combination with rituximab in patients with relapsed or refractory B-cell non-Hodgkin lymphoma, including DLBCL and FL.
Forty Seven, Inc., the company developing 5F9, expects to announce initial safety and efficacy data from the phase 1b portion of the trial in the second quarter of 2018.
About fast track designation
The FDA’s fast track drug development program is designed to expedite clinical development and submission of applications for drugs with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the drug’s development plan and written communications about issues such as trial design and use of biomarkers.
Drugs that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met.
Fast track drugs may also be eligible for rolling review, which allows a developer to submit individual sections of a drug’s application for review as they are ready, rather than waiting until all sections are complete.
The US Food and Drug Administration (FDA) has granted 2 fast track designations to 5F9, an anti-CD47 antibody.
The designations are for 5F9 as a treatment for relapsed or refractory diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL).
Data supporting the fast track designations were derived from a phase 1b/2 trial of 5F9 in combination with rituximab in patients with relapsed or refractory B-cell non-Hodgkin lymphoma, including DLBCL and FL.
Forty Seven, Inc., the company developing 5F9, expects to announce initial safety and efficacy data from the phase 1b portion of the trial in the second quarter of 2018.
About fast track designation
The FDA’s fast track drug development program is designed to expedite clinical development and submission of applications for drugs with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the drug’s development plan and written communications about issues such as trial design and use of biomarkers.
Drugs that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met.
Fast track drugs may also be eligible for rolling review, which allows a developer to submit individual sections of a drug’s application for review as they are ready, rather than waiting until all sections are complete.
Novartis CAR T-cell therapy adds a lymphoma indication
Novartis’s after failure of two or more lines of systemic therapy.
The Food and Drug Administration approved the expanded indication on May 1. The chimeric antigen receptor (CAR) T-cell therapy was initially approved in Aug. 2017 for refractory or relapsed B-cell precursor acute lymphoblastic leukemia (ALL) in patients up to 25 years old. The new approval brings tisagenlecleucel into direct competition with Gilead Science’s CAR T-cell therapy axicabtagene ciloleucel (Yescarta), which was approved in Oct. 2017 for B-cell lymphoma.
Besides matching the competition, she said the lower price is because tisagenlecleucel takes longer to work for lymphoma, and the response isn’t as potent as for childhood ALL. Novartis is looking into chronic lymphocytic leukemia, multiple myeloma, and solid tumor indications for tisagenlecleucel and other CAR T-cell agents, she added.
The Centers for Medicare & Medicaid Services recently committed to covering outpatient administration of both agents for their initial indications; Novartis is working with CMS for coverage of the new lymphoma indication.
With both products, T cells are collected then shipped off to a company facility where a CAR gene is spliced into their DNA, essentially programming the T cells to attack the targeted cancer. The cells are then infused back into the patient.
In the phase 2 JULIET trial, tisagenlecleucel showed an overall response rate of 50% among 68 B-cell lymphoma patients, with 32% achieving complete response (CR) and 18% achieving partial response (PR). The median duration of response was not reached.
Axicabtagene ciloleucel’s label reports an objective response rate of 72% among 101 patients, with CR in 51% and PR in 21%. Median duration of response was 9.2 months but was also not reached among complete responders.
“Different trials. Different CARTs. Different levels of disease. Our drug is cryopreserved and theirs is not. No way to compare them,” the Novartis spokeswoman said when asked about the response differences.
T-cell reprogramming isn’t clean at this point in medical history; both agents carry black box warnings of potentially fatal cytokine release syndrome and neurologic toxicity, and both are subject to Risk Evaluation and Mitigation Strategy programs.
The B-cell lymphoma indication for both therapies includes diffuse large B-cell lymphoma (DLBCL), high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. The Gilead product carries an additional indication for primary mediastinal large B-cell lymphoma. Neither agent is indicated for primary central nervous system lymphoma. Both labels say that patients should not donate blood, organs, or tissues after treatment. Tisagenlecleucel labeling also notes that some commercial HIV nucleic acid tests may yield false positives after treatment.
Novartis said in a press release that T cells are treated at the company’s Morris Plains, N.J., facility with a turnaround time of about 22 days. Cryopreservation of the harvested cells gives providers some flexibility in treatment timing.
Novartis’s after failure of two or more lines of systemic therapy.
The Food and Drug Administration approved the expanded indication on May 1. The chimeric antigen receptor (CAR) T-cell therapy was initially approved in Aug. 2017 for refractory or relapsed B-cell precursor acute lymphoblastic leukemia (ALL) in patients up to 25 years old. The new approval brings tisagenlecleucel into direct competition with Gilead Science’s CAR T-cell therapy axicabtagene ciloleucel (Yescarta), which was approved in Oct. 2017 for B-cell lymphoma.
Besides matching the competition, she said the lower price is because tisagenlecleucel takes longer to work for lymphoma, and the response isn’t as potent as for childhood ALL. Novartis is looking into chronic lymphocytic leukemia, multiple myeloma, and solid tumor indications for tisagenlecleucel and other CAR T-cell agents, she added.
The Centers for Medicare & Medicaid Services recently committed to covering outpatient administration of both agents for their initial indications; Novartis is working with CMS for coverage of the new lymphoma indication.
With both products, T cells are collected then shipped off to a company facility where a CAR gene is spliced into their DNA, essentially programming the T cells to attack the targeted cancer. The cells are then infused back into the patient.
In the phase 2 JULIET trial, tisagenlecleucel showed an overall response rate of 50% among 68 B-cell lymphoma patients, with 32% achieving complete response (CR) and 18% achieving partial response (PR). The median duration of response was not reached.
Axicabtagene ciloleucel’s label reports an objective response rate of 72% among 101 patients, with CR in 51% and PR in 21%. Median duration of response was 9.2 months but was also not reached among complete responders.
“Different trials. Different CARTs. Different levels of disease. Our drug is cryopreserved and theirs is not. No way to compare them,” the Novartis spokeswoman said when asked about the response differences.
T-cell reprogramming isn’t clean at this point in medical history; both agents carry black box warnings of potentially fatal cytokine release syndrome and neurologic toxicity, and both are subject to Risk Evaluation and Mitigation Strategy programs.
The B-cell lymphoma indication for both therapies includes diffuse large B-cell lymphoma (DLBCL), high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. The Gilead product carries an additional indication for primary mediastinal large B-cell lymphoma. Neither agent is indicated for primary central nervous system lymphoma. Both labels say that patients should not donate blood, organs, or tissues after treatment. Tisagenlecleucel labeling also notes that some commercial HIV nucleic acid tests may yield false positives after treatment.
Novartis said in a press release that T cells are treated at the company’s Morris Plains, N.J., facility with a turnaround time of about 22 days. Cryopreservation of the harvested cells gives providers some flexibility in treatment timing.
Novartis’s after failure of two or more lines of systemic therapy.
The Food and Drug Administration approved the expanded indication on May 1. The chimeric antigen receptor (CAR) T-cell therapy was initially approved in Aug. 2017 for refractory or relapsed B-cell precursor acute lymphoblastic leukemia (ALL) in patients up to 25 years old. The new approval brings tisagenlecleucel into direct competition with Gilead Science’s CAR T-cell therapy axicabtagene ciloleucel (Yescarta), which was approved in Oct. 2017 for B-cell lymphoma.
Besides matching the competition, she said the lower price is because tisagenlecleucel takes longer to work for lymphoma, and the response isn’t as potent as for childhood ALL. Novartis is looking into chronic lymphocytic leukemia, multiple myeloma, and solid tumor indications for tisagenlecleucel and other CAR T-cell agents, she added.
The Centers for Medicare & Medicaid Services recently committed to covering outpatient administration of both agents for their initial indications; Novartis is working with CMS for coverage of the new lymphoma indication.
With both products, T cells are collected then shipped off to a company facility where a CAR gene is spliced into their DNA, essentially programming the T cells to attack the targeted cancer. The cells are then infused back into the patient.
In the phase 2 JULIET trial, tisagenlecleucel showed an overall response rate of 50% among 68 B-cell lymphoma patients, with 32% achieving complete response (CR) and 18% achieving partial response (PR). The median duration of response was not reached.
Axicabtagene ciloleucel’s label reports an objective response rate of 72% among 101 patients, with CR in 51% and PR in 21%. Median duration of response was 9.2 months but was also not reached among complete responders.
“Different trials. Different CARTs. Different levels of disease. Our drug is cryopreserved and theirs is not. No way to compare them,” the Novartis spokeswoman said when asked about the response differences.
T-cell reprogramming isn’t clean at this point in medical history; both agents carry black box warnings of potentially fatal cytokine release syndrome and neurologic toxicity, and both are subject to Risk Evaluation and Mitigation Strategy programs.
The B-cell lymphoma indication for both therapies includes diffuse large B-cell lymphoma (DLBCL), high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. The Gilead product carries an additional indication for primary mediastinal large B-cell lymphoma. Neither agent is indicated for primary central nervous system lymphoma. Both labels say that patients should not donate blood, organs, or tissues after treatment. Tisagenlecleucel labeling also notes that some commercial HIV nucleic acid tests may yield false positives after treatment.
Novartis said in a press release that T cells are treated at the company’s Morris Plains, N.J., facility with a turnaround time of about 22 days. Cryopreservation of the harvested cells gives providers some flexibility in treatment timing.