User login
NCCN guidelines highlight ‘complicated’ treatment for pediatric lymphomas
The National Comprehensive Cancer Network (NCCN) has released its first set of guidelines for managing pediatric aggressive mature B-cell lymphomas.
The guidelines highlight the complexities of treating pediatric Burkitt lymphoma (BL) and diffuse large B-cell lymphoma (DLBCL), as recommendations include a range of multiagent regimens for different patient groups at various time points.
“The treatment of this disease is relatively complicated,” said Kimberly J. Davies, MD, a pediatric hematologist/oncologist at Dana-Farber Cancer Institute in Boston and chair of the guidelines panel. “The chemotherapy regimens have a lot of drugs, a lot of nuances to how they’re supposed to be given. These guidelines delineate that treatment and help the provider … make sure they are delivering the treatment a patient needs.”
The guidelines recommend different regimens according to a patient’s risk group, but the same treatment approach should be used for patients with BL and those with DLBCL.
“The biggest difference between pediatric and adult patients is that pediatric patients are more uniformly treated, regardless of what type of aggressive B-cell lymphoma they have,” said Matthew Barth, MD, a pediatric hematologist/oncologist at Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., and vice chair of the NCCN guidelines panel.
“Adults with diffuse large B-cell lymphoma and Burkitt lymphoma are generally treated with different chemotherapy regimens, but, in pediatrics, we use the same treatment regimens for both diffuse large B-cell lymphoma and Burkitt lymphoma,” he added.
As an example, the new guidelines recommend that pediatric patients with low-risk BL/DLBCL receive the POG9219 regimen (N Engl J Med. 1997 Oct 30;337[18]:1259-66) or FAB/LMB96 regimen A (Br J Haematol. 2008 Jun;141[6]:840-7) as induction, or they should be enrolled in a clinical trial.
On the other hand, induction for high-risk pediatric BL/DLBCL patients should consist of rituximab and a chemotherapy regimen used in the COG ANHL1131 trial. The recommendation to incorporate rituximab in high-risk pediatric patients is based on results from that trial (J Clin Oncol. 2016 May 20. doi: 10.1200/JCO.2016.34.15_suppl.10507).
“Until recent clinical trial data was available, we weren’t really sure how to incorporate rituximab into the treatment of pediatric patients with mature B-cell lymphomas,” Dr. Barth said. “We now have evidence that rituximab is clearly beneficial for patients who are in higher-risk groups.”
Dr. Barth and Dr. Davies both noted that pediatric BL and DLBCL have high cure rates. Long-term survival rates range from about 80% to more than 90%, according to the American Cancer Society. However, the patients who do relapse or progress can be difficult to treat.
“We have quite good cure rates at this point in time, which is a great success, but that means that a very small population of patients don’t respond to initial therapy, and … it’s hard to know what the best treatment for those patients is,” Dr. Davies said.
She noted that studies are underway to determine if immunotherapies, including chimeric antigen receptor T-cell therapy, might improve outcomes in patients with relapsed or refractory disease.
For now, the NCCN guidelines recommend clinical trial enrollment for relapsed/refractory patients. Alternatively, these patients can receive additional chemotherapy, and responders can proceed to transplant. Patients who don’t achieve at least a partial response may go on to a clinical trial or receive best supportive care.
Dr. Davies and Dr. Barth reported having no conflicts of interest.
The National Comprehensive Cancer Network (NCCN) has released its first set of guidelines for managing pediatric aggressive mature B-cell lymphomas.
The guidelines highlight the complexities of treating pediatric Burkitt lymphoma (BL) and diffuse large B-cell lymphoma (DLBCL), as recommendations include a range of multiagent regimens for different patient groups at various time points.
“The treatment of this disease is relatively complicated,” said Kimberly J. Davies, MD, a pediatric hematologist/oncologist at Dana-Farber Cancer Institute in Boston and chair of the guidelines panel. “The chemotherapy regimens have a lot of drugs, a lot of nuances to how they’re supposed to be given. These guidelines delineate that treatment and help the provider … make sure they are delivering the treatment a patient needs.”
The guidelines recommend different regimens according to a patient’s risk group, but the same treatment approach should be used for patients with BL and those with DLBCL.
“The biggest difference between pediatric and adult patients is that pediatric patients are more uniformly treated, regardless of what type of aggressive B-cell lymphoma they have,” said Matthew Barth, MD, a pediatric hematologist/oncologist at Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., and vice chair of the NCCN guidelines panel.
“Adults with diffuse large B-cell lymphoma and Burkitt lymphoma are generally treated with different chemotherapy regimens, but, in pediatrics, we use the same treatment regimens for both diffuse large B-cell lymphoma and Burkitt lymphoma,” he added.
As an example, the new guidelines recommend that pediatric patients with low-risk BL/DLBCL receive the POG9219 regimen (N Engl J Med. 1997 Oct 30;337[18]:1259-66) or FAB/LMB96 regimen A (Br J Haematol. 2008 Jun;141[6]:840-7) as induction, or they should be enrolled in a clinical trial.
On the other hand, induction for high-risk pediatric BL/DLBCL patients should consist of rituximab and a chemotherapy regimen used in the COG ANHL1131 trial. The recommendation to incorporate rituximab in high-risk pediatric patients is based on results from that trial (J Clin Oncol. 2016 May 20. doi: 10.1200/JCO.2016.34.15_suppl.10507).
“Until recent clinical trial data was available, we weren’t really sure how to incorporate rituximab into the treatment of pediatric patients with mature B-cell lymphomas,” Dr. Barth said. “We now have evidence that rituximab is clearly beneficial for patients who are in higher-risk groups.”
Dr. Barth and Dr. Davies both noted that pediatric BL and DLBCL have high cure rates. Long-term survival rates range from about 80% to more than 90%, according to the American Cancer Society. However, the patients who do relapse or progress can be difficult to treat.
“We have quite good cure rates at this point in time, which is a great success, but that means that a very small population of patients don’t respond to initial therapy, and … it’s hard to know what the best treatment for those patients is,” Dr. Davies said.
She noted that studies are underway to determine if immunotherapies, including chimeric antigen receptor T-cell therapy, might improve outcomes in patients with relapsed or refractory disease.
For now, the NCCN guidelines recommend clinical trial enrollment for relapsed/refractory patients. Alternatively, these patients can receive additional chemotherapy, and responders can proceed to transplant. Patients who don’t achieve at least a partial response may go on to a clinical trial or receive best supportive care.
Dr. Davies and Dr. Barth reported having no conflicts of interest.
The National Comprehensive Cancer Network (NCCN) has released its first set of guidelines for managing pediatric aggressive mature B-cell lymphomas.
The guidelines highlight the complexities of treating pediatric Burkitt lymphoma (BL) and diffuse large B-cell lymphoma (DLBCL), as recommendations include a range of multiagent regimens for different patient groups at various time points.
“The treatment of this disease is relatively complicated,” said Kimberly J. Davies, MD, a pediatric hematologist/oncologist at Dana-Farber Cancer Institute in Boston and chair of the guidelines panel. “The chemotherapy regimens have a lot of drugs, a lot of nuances to how they’re supposed to be given. These guidelines delineate that treatment and help the provider … make sure they are delivering the treatment a patient needs.”
The guidelines recommend different regimens according to a patient’s risk group, but the same treatment approach should be used for patients with BL and those with DLBCL.
“The biggest difference between pediatric and adult patients is that pediatric patients are more uniformly treated, regardless of what type of aggressive B-cell lymphoma they have,” said Matthew Barth, MD, a pediatric hematologist/oncologist at Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., and vice chair of the NCCN guidelines panel.
“Adults with diffuse large B-cell lymphoma and Burkitt lymphoma are generally treated with different chemotherapy regimens, but, in pediatrics, we use the same treatment regimens for both diffuse large B-cell lymphoma and Burkitt lymphoma,” he added.
As an example, the new guidelines recommend that pediatric patients with low-risk BL/DLBCL receive the POG9219 regimen (N Engl J Med. 1997 Oct 30;337[18]:1259-66) or FAB/LMB96 regimen A (Br J Haematol. 2008 Jun;141[6]:840-7) as induction, or they should be enrolled in a clinical trial.
On the other hand, induction for high-risk pediatric BL/DLBCL patients should consist of rituximab and a chemotherapy regimen used in the COG ANHL1131 trial. The recommendation to incorporate rituximab in high-risk pediatric patients is based on results from that trial (J Clin Oncol. 2016 May 20. doi: 10.1200/JCO.2016.34.15_suppl.10507).
“Until recent clinical trial data was available, we weren’t really sure how to incorporate rituximab into the treatment of pediatric patients with mature B-cell lymphomas,” Dr. Barth said. “We now have evidence that rituximab is clearly beneficial for patients who are in higher-risk groups.”
Dr. Barth and Dr. Davies both noted that pediatric BL and DLBCL have high cure rates. Long-term survival rates range from about 80% to more than 90%, according to the American Cancer Society. However, the patients who do relapse or progress can be difficult to treat.
“We have quite good cure rates at this point in time, which is a great success, but that means that a very small population of patients don’t respond to initial therapy, and … it’s hard to know what the best treatment for those patients is,” Dr. Davies said.
She noted that studies are underway to determine if immunotherapies, including chimeric antigen receptor T-cell therapy, might improve outcomes in patients with relapsed or refractory disease.
For now, the NCCN guidelines recommend clinical trial enrollment for relapsed/refractory patients. Alternatively, these patients can receive additional chemotherapy, and responders can proceed to transplant. Patients who don’t achieve at least a partial response may go on to a clinical trial or receive best supportive care.
Dr. Davies and Dr. Barth reported having no conflicts of interest.
Study halted; ‘hyperprogression’ seen with nivolumab for R/R PTCL
ORLANDO – There is an urgent need for new therapies to treat relapsed or refractory peripheral T-cell lymphoma, but results of a phase 2 study suggest that monotherapy with the immune checkpoint inhibitor nivolumab (Opdivo) is not the hoped-for salvage treatment.
An interim analysis of data on 12 patients with peripheral T-cell lymphoma (PTCL) treated with nivolumab monotherapy showed an overall response rate of 33%, consisting of 2 complete responses and 2 partial responses. But the responses were short lived, and one patient had hyperprogressive disease – dramatic progression within one cycle of treatment – while two more had progression within two cycles, leading to a trial halt, reported N. Nora Bennani, MD, from the Mayo Clinic in Rochester, Minn.
“These findings likely reflect the distinct biology of PTCL and should be considered when designing future studies using checkpoint inhibitors in these diseases,” she said at the annual meeting of the American Society of Hematology.
The rationale for using an immune checkpoint inhibitor directed against the programmed death–1 protein and its ligands (PD and PD-L1/2) is that malignant cells in PTCL induce a profoundly immunosuppressive tumor microenvironment. Checkpoint inhibitors have shown strong activity against relapsed Hodgkin lymphoma, and the Mayo Clinic researchers speculated that an anti-PD-1 agent could have a similar effect in PTCL.
They had originally planned to enroll 29 patients into a phase 2 trial with nivolumab delivered 240 mg every 2 weeks for eight cycles, followed by a dose of 480 mg given every 4 weeks until disease progression or intolerable toxicities.
Patients were eligible if they had biopsy-confirmed relapsed or refractory PTCL, measurable disease on cross-sectional imaging of at least 1.5 cm, and prior systemic chemoimmunotherapy and/or autologous stem cell transplantation.
The interim analysis included 12 patients who received at least one dose of nivolumab. Of the 12 patients, 6 had angioimmunoblastic T-cell lymphoma (AITL), 3 had PTCL not otherwise specified, and 1 each had ALK-negative anaplastic large cell lymphoma (ALK-ALCL), enteropathy-associated T-cell lymphoma (EATL), or hepatosplenic gamma/delta T-cell lymphoma.
All patients had Ann Arbor stage III/IV disease, and 11 had extranodal involvement.
As noted, there were 4 responses among the 12 patients, consisting of 1 complete response in the patient with ALK-ALCL and 1 in a patient with AITL, and 2 partial responses – 1 in a patient with PTCL-NOS, and 1 in the patient with EATL.
The median progression-free survival for all 12 patients was short at 2.7 months, and the median overall survival was estimated at 6.7 months.
“It was staggering to see this: The duration of response was significantly short, less than 2 months,” Dr. Bennani said.
Nonhematologic toxicities were seen in 5 of the 12 patients (42%), and hematologic adverse events occurred in 3 (25%). All patients are now off treatment, 10 because of disease progression, 1 because of acute pancreatitis, and the aforementioned patient with hyperprogressive disease.
The patient with hyperprogressive disease had significant progression in tonsillar and cervical lymphadenopathy within 7-10 days of nivolumab infusion, with biopsy-proven AITL in the involved nodes.
“I believe that, in this patient population, combination therapies will be key. I think checkpoint blockers alone are not going to be sufficient to see meaningful outcomes in these patients,” Dr. Bennani said in an interview.
“An overall response rate of 33% is significant, because most other agents that were FDA approved in this patient population have response rates around 30%,” she said, adding that it’s possible that the patients with rapid progression had disease too advanced to be effectively treated with a checkpoint inhibitor.
“Ideally however, if we want to move forward, it will need to be with combinations of checkpoint inhibitors with HDAC [histone deacetylase] inhibitors, hypomethylating agents, or even PI3 kinase inhibitors,” she said.
The study was supported by Bristol-Myers Squibb. Dr. Bennani reported research funding and advisory board activities for Bristol-Myers Squibb and others.
SOURCE: Bennani NN et al. ASH 2019, Abstract 467.
ORLANDO – There is an urgent need for new therapies to treat relapsed or refractory peripheral T-cell lymphoma, but results of a phase 2 study suggest that monotherapy with the immune checkpoint inhibitor nivolumab (Opdivo) is not the hoped-for salvage treatment.
An interim analysis of data on 12 patients with peripheral T-cell lymphoma (PTCL) treated with nivolumab monotherapy showed an overall response rate of 33%, consisting of 2 complete responses and 2 partial responses. But the responses were short lived, and one patient had hyperprogressive disease – dramatic progression within one cycle of treatment – while two more had progression within two cycles, leading to a trial halt, reported N. Nora Bennani, MD, from the Mayo Clinic in Rochester, Minn.
“These findings likely reflect the distinct biology of PTCL and should be considered when designing future studies using checkpoint inhibitors in these diseases,” she said at the annual meeting of the American Society of Hematology.
The rationale for using an immune checkpoint inhibitor directed against the programmed death–1 protein and its ligands (PD and PD-L1/2) is that malignant cells in PTCL induce a profoundly immunosuppressive tumor microenvironment. Checkpoint inhibitors have shown strong activity against relapsed Hodgkin lymphoma, and the Mayo Clinic researchers speculated that an anti-PD-1 agent could have a similar effect in PTCL.
They had originally planned to enroll 29 patients into a phase 2 trial with nivolumab delivered 240 mg every 2 weeks for eight cycles, followed by a dose of 480 mg given every 4 weeks until disease progression or intolerable toxicities.
Patients were eligible if they had biopsy-confirmed relapsed or refractory PTCL, measurable disease on cross-sectional imaging of at least 1.5 cm, and prior systemic chemoimmunotherapy and/or autologous stem cell transplantation.
The interim analysis included 12 patients who received at least one dose of nivolumab. Of the 12 patients, 6 had angioimmunoblastic T-cell lymphoma (AITL), 3 had PTCL not otherwise specified, and 1 each had ALK-negative anaplastic large cell lymphoma (ALK-ALCL), enteropathy-associated T-cell lymphoma (EATL), or hepatosplenic gamma/delta T-cell lymphoma.
All patients had Ann Arbor stage III/IV disease, and 11 had extranodal involvement.
As noted, there were 4 responses among the 12 patients, consisting of 1 complete response in the patient with ALK-ALCL and 1 in a patient with AITL, and 2 partial responses – 1 in a patient with PTCL-NOS, and 1 in the patient with EATL.
The median progression-free survival for all 12 patients was short at 2.7 months, and the median overall survival was estimated at 6.7 months.
“It was staggering to see this: The duration of response was significantly short, less than 2 months,” Dr. Bennani said.
Nonhematologic toxicities were seen in 5 of the 12 patients (42%), and hematologic adverse events occurred in 3 (25%). All patients are now off treatment, 10 because of disease progression, 1 because of acute pancreatitis, and the aforementioned patient with hyperprogressive disease.
The patient with hyperprogressive disease had significant progression in tonsillar and cervical lymphadenopathy within 7-10 days of nivolumab infusion, with biopsy-proven AITL in the involved nodes.
“I believe that, in this patient population, combination therapies will be key. I think checkpoint blockers alone are not going to be sufficient to see meaningful outcomes in these patients,” Dr. Bennani said in an interview.
“An overall response rate of 33% is significant, because most other agents that were FDA approved in this patient population have response rates around 30%,” she said, adding that it’s possible that the patients with rapid progression had disease too advanced to be effectively treated with a checkpoint inhibitor.
“Ideally however, if we want to move forward, it will need to be with combinations of checkpoint inhibitors with HDAC [histone deacetylase] inhibitors, hypomethylating agents, or even PI3 kinase inhibitors,” she said.
The study was supported by Bristol-Myers Squibb. Dr. Bennani reported research funding and advisory board activities for Bristol-Myers Squibb and others.
SOURCE: Bennani NN et al. ASH 2019, Abstract 467.
ORLANDO – There is an urgent need for new therapies to treat relapsed or refractory peripheral T-cell lymphoma, but results of a phase 2 study suggest that monotherapy with the immune checkpoint inhibitor nivolumab (Opdivo) is not the hoped-for salvage treatment.
An interim analysis of data on 12 patients with peripheral T-cell lymphoma (PTCL) treated with nivolumab monotherapy showed an overall response rate of 33%, consisting of 2 complete responses and 2 partial responses. But the responses were short lived, and one patient had hyperprogressive disease – dramatic progression within one cycle of treatment – while two more had progression within two cycles, leading to a trial halt, reported N. Nora Bennani, MD, from the Mayo Clinic in Rochester, Minn.
“These findings likely reflect the distinct biology of PTCL and should be considered when designing future studies using checkpoint inhibitors in these diseases,” she said at the annual meeting of the American Society of Hematology.
The rationale for using an immune checkpoint inhibitor directed against the programmed death–1 protein and its ligands (PD and PD-L1/2) is that malignant cells in PTCL induce a profoundly immunosuppressive tumor microenvironment. Checkpoint inhibitors have shown strong activity against relapsed Hodgkin lymphoma, and the Mayo Clinic researchers speculated that an anti-PD-1 agent could have a similar effect in PTCL.
They had originally planned to enroll 29 patients into a phase 2 trial with nivolumab delivered 240 mg every 2 weeks for eight cycles, followed by a dose of 480 mg given every 4 weeks until disease progression or intolerable toxicities.
Patients were eligible if they had biopsy-confirmed relapsed or refractory PTCL, measurable disease on cross-sectional imaging of at least 1.5 cm, and prior systemic chemoimmunotherapy and/or autologous stem cell transplantation.
The interim analysis included 12 patients who received at least one dose of nivolumab. Of the 12 patients, 6 had angioimmunoblastic T-cell lymphoma (AITL), 3 had PTCL not otherwise specified, and 1 each had ALK-negative anaplastic large cell lymphoma (ALK-ALCL), enteropathy-associated T-cell lymphoma (EATL), or hepatosplenic gamma/delta T-cell lymphoma.
All patients had Ann Arbor stage III/IV disease, and 11 had extranodal involvement.
As noted, there were 4 responses among the 12 patients, consisting of 1 complete response in the patient with ALK-ALCL and 1 in a patient with AITL, and 2 partial responses – 1 in a patient with PTCL-NOS, and 1 in the patient with EATL.
The median progression-free survival for all 12 patients was short at 2.7 months, and the median overall survival was estimated at 6.7 months.
“It was staggering to see this: The duration of response was significantly short, less than 2 months,” Dr. Bennani said.
Nonhematologic toxicities were seen in 5 of the 12 patients (42%), and hematologic adverse events occurred in 3 (25%). All patients are now off treatment, 10 because of disease progression, 1 because of acute pancreatitis, and the aforementioned patient with hyperprogressive disease.
The patient with hyperprogressive disease had significant progression in tonsillar and cervical lymphadenopathy within 7-10 days of nivolumab infusion, with biopsy-proven AITL in the involved nodes.
“I believe that, in this patient population, combination therapies will be key. I think checkpoint blockers alone are not going to be sufficient to see meaningful outcomes in these patients,” Dr. Bennani said in an interview.
“An overall response rate of 33% is significant, because most other agents that were FDA approved in this patient population have response rates around 30%,” she said, adding that it’s possible that the patients with rapid progression had disease too advanced to be effectively treated with a checkpoint inhibitor.
“Ideally however, if we want to move forward, it will need to be with combinations of checkpoint inhibitors with HDAC [histone deacetylase] inhibitors, hypomethylating agents, or even PI3 kinase inhibitors,” she said.
The study was supported by Bristol-Myers Squibb. Dr. Bennani reported research funding and advisory board activities for Bristol-Myers Squibb and others.
SOURCE: Bennani NN et al. ASH 2019, Abstract 467.
REPORTING FROM ASH 2019
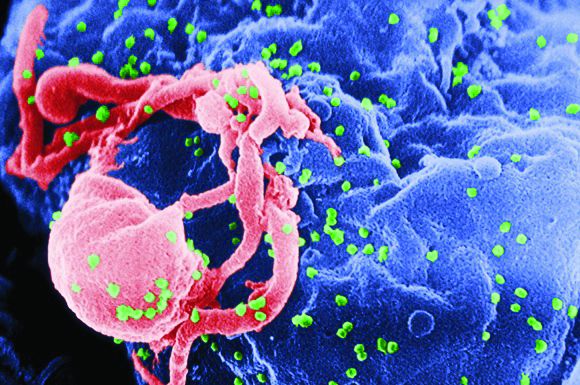
CAR T-cell therapy found safe, effective for HIV-associated lymphoma
HIV positivity does not preclude chimeric antigen receptor (CAR) T-cell therapy for patients with aggressive lymphoma, a report of two cases suggests. Both of the HIV-positive patients, one of whom had long-term psychiatric comorbidity, achieved durable remission on axicabtagene ciloleucel (Yescarta) without undue toxicity.
“To our knowledge, these are the first reported cases of CAR T-cell therapy administered to HIV-infected patients with lymphoma,” Jeremy S. Abramson, MD, of Massachusetts General Hospital, Boston and his colleagues wrote in Cancer. “Patients with HIV and AIDS, as well as those with preexisting mental illness, should not be considered disqualified from CAR T-cell therapy and deserve ongoing studies to optimize efficacy and safety in this population.”
The Food and Drug Administration has approved two CAR T-cell products that target the B-cell antigen CD19 for the treatment of refractory lymphoma. But their efficacy and safety in HIV-positive patients are unknown because this group has been excluded from pivotal clinical trials.
Dr. Abramson and coauthors detail the two cases of successful anti-CD19 CAR T-cell therapy with axicabtagene ciloleucel in patients with HIV-associated, refractory, high-grade B-cell lymphoma.
The first patient was an HIV-positive man with diffuse large B-cell lymphoma (DLBCL) of germinal center B-cell subtype who was intermittently adherent to antiretroviral therapy. His comorbidities included posttraumatic stress disorder and schizoaffective disorder.
Previous treatments for DLBCL included dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab (EPOCH-R), and rituximab, ifosfamide, carboplatin, and etoposide (RICE). A recurrence precluded high-dose chemotherapy with autologous stem cell support.
With close multidisciplinary management, including psychiatric consultation, the patient became a candidate for CAR T-cell therapy and received axicabtagene ciloleucel. He experienced grade 2 cytokine release syndrome and grade 3 neurologic toxicity, both of which resolved with treatment. Imaging showed complete remission at approximately 3 months that was sustained at 1 year. Additionally, he had an undetectable HIV viral load and was psychiatrically stable.
The second patient was a man with AIDS-associated, non–germinal center B-cell, Epstein-Barr virus–positive DLBCL who was adherent to antiretroviral therapy. His lymphoma had recurred rapidly after initially responding to dose-adjusted EPOCH-R and then was refractory to combination rituximab and lenalidomide. He previously had hepatitis B virus, cytomegalovirus, and Mycobacterium avium complex infections.
Because of prolonged cytopenias and infectious complications after the previous lymphoma treatments, the patient was considered a poor candidate for high-dose chemotherapy. He underwent CAR T-cell therapy with axicabtagene ciloleucel and had a complete remission on day 28. Additionally, his HIV infection remained well controlled.
“Although much remains to be learned regarding CAR T-cell therapy in patients with refractory hematologic malignancies, with or without HIV infection, the cases presented herein demonstrate that patients with chemotherapy-refractory, high-grade B-cell lymphoma can successfully undergo autologous CAR T-cell manufacturing, and subsequently can safely tolerate CAR T-cell therapy and achieve a durable complete remission,” the researchers wrote. “These cases have further demonstrated the proactive, multidisciplinary care required to navigate a patient with high-risk lymphoma through CAR T-cell therapy with attention to significant medical and psychiatric comorbidities.”
Dr. Abramson reported that he has acted as a paid member of the scientific advisory board and as a paid consultant for Kite Pharma, which markets Yescarta, and several other companies.
SOURCE: Abramson JS et al. Cancer. 2019 Sep 10. doi: 10.1002/cncr.32411.
HIV positivity does not preclude chimeric antigen receptor (CAR) T-cell therapy for patients with aggressive lymphoma, a report of two cases suggests. Both of the HIV-positive patients, one of whom had long-term psychiatric comorbidity, achieved durable remission on axicabtagene ciloleucel (Yescarta) without undue toxicity.
“To our knowledge, these are the first reported cases of CAR T-cell therapy administered to HIV-infected patients with lymphoma,” Jeremy S. Abramson, MD, of Massachusetts General Hospital, Boston and his colleagues wrote in Cancer. “Patients with HIV and AIDS, as well as those with preexisting mental illness, should not be considered disqualified from CAR T-cell therapy and deserve ongoing studies to optimize efficacy and safety in this population.”
The Food and Drug Administration has approved two CAR T-cell products that target the B-cell antigen CD19 for the treatment of refractory lymphoma. But their efficacy and safety in HIV-positive patients are unknown because this group has been excluded from pivotal clinical trials.
Dr. Abramson and coauthors detail the two cases of successful anti-CD19 CAR T-cell therapy with axicabtagene ciloleucel in patients with HIV-associated, refractory, high-grade B-cell lymphoma.
The first patient was an HIV-positive man with diffuse large B-cell lymphoma (DLBCL) of germinal center B-cell subtype who was intermittently adherent to antiretroviral therapy. His comorbidities included posttraumatic stress disorder and schizoaffective disorder.
Previous treatments for DLBCL included dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab (EPOCH-R), and rituximab, ifosfamide, carboplatin, and etoposide (RICE). A recurrence precluded high-dose chemotherapy with autologous stem cell support.
With close multidisciplinary management, including psychiatric consultation, the patient became a candidate for CAR T-cell therapy and received axicabtagene ciloleucel. He experienced grade 2 cytokine release syndrome and grade 3 neurologic toxicity, both of which resolved with treatment. Imaging showed complete remission at approximately 3 months that was sustained at 1 year. Additionally, he had an undetectable HIV viral load and was psychiatrically stable.
The second patient was a man with AIDS-associated, non–germinal center B-cell, Epstein-Barr virus–positive DLBCL who was adherent to antiretroviral therapy. His lymphoma had recurred rapidly after initially responding to dose-adjusted EPOCH-R and then was refractory to combination rituximab and lenalidomide. He previously had hepatitis B virus, cytomegalovirus, and Mycobacterium avium complex infections.
Because of prolonged cytopenias and infectious complications after the previous lymphoma treatments, the patient was considered a poor candidate for high-dose chemotherapy. He underwent CAR T-cell therapy with axicabtagene ciloleucel and had a complete remission on day 28. Additionally, his HIV infection remained well controlled.
“Although much remains to be learned regarding CAR T-cell therapy in patients with refractory hematologic malignancies, with or without HIV infection, the cases presented herein demonstrate that patients with chemotherapy-refractory, high-grade B-cell lymphoma can successfully undergo autologous CAR T-cell manufacturing, and subsequently can safely tolerate CAR T-cell therapy and achieve a durable complete remission,” the researchers wrote. “These cases have further demonstrated the proactive, multidisciplinary care required to navigate a patient with high-risk lymphoma through CAR T-cell therapy with attention to significant medical and psychiatric comorbidities.”
Dr. Abramson reported that he has acted as a paid member of the scientific advisory board and as a paid consultant for Kite Pharma, which markets Yescarta, and several other companies.
SOURCE: Abramson JS et al. Cancer. 2019 Sep 10. doi: 10.1002/cncr.32411.
HIV positivity does not preclude chimeric antigen receptor (CAR) T-cell therapy for patients with aggressive lymphoma, a report of two cases suggests. Both of the HIV-positive patients, one of whom had long-term psychiatric comorbidity, achieved durable remission on axicabtagene ciloleucel (Yescarta) without undue toxicity.
“To our knowledge, these are the first reported cases of CAR T-cell therapy administered to HIV-infected patients with lymphoma,” Jeremy S. Abramson, MD, of Massachusetts General Hospital, Boston and his colleagues wrote in Cancer. “Patients with HIV and AIDS, as well as those with preexisting mental illness, should not be considered disqualified from CAR T-cell therapy and deserve ongoing studies to optimize efficacy and safety in this population.”
The Food and Drug Administration has approved two CAR T-cell products that target the B-cell antigen CD19 for the treatment of refractory lymphoma. But their efficacy and safety in HIV-positive patients are unknown because this group has been excluded from pivotal clinical trials.
Dr. Abramson and coauthors detail the two cases of successful anti-CD19 CAR T-cell therapy with axicabtagene ciloleucel in patients with HIV-associated, refractory, high-grade B-cell lymphoma.
The first patient was an HIV-positive man with diffuse large B-cell lymphoma (DLBCL) of germinal center B-cell subtype who was intermittently adherent to antiretroviral therapy. His comorbidities included posttraumatic stress disorder and schizoaffective disorder.
Previous treatments for DLBCL included dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab (EPOCH-R), and rituximab, ifosfamide, carboplatin, and etoposide (RICE). A recurrence precluded high-dose chemotherapy with autologous stem cell support.
With close multidisciplinary management, including psychiatric consultation, the patient became a candidate for CAR T-cell therapy and received axicabtagene ciloleucel. He experienced grade 2 cytokine release syndrome and grade 3 neurologic toxicity, both of which resolved with treatment. Imaging showed complete remission at approximately 3 months that was sustained at 1 year. Additionally, he had an undetectable HIV viral load and was psychiatrically stable.
The second patient was a man with AIDS-associated, non–germinal center B-cell, Epstein-Barr virus–positive DLBCL who was adherent to antiretroviral therapy. His lymphoma had recurred rapidly after initially responding to dose-adjusted EPOCH-R and then was refractory to combination rituximab and lenalidomide. He previously had hepatitis B virus, cytomegalovirus, and Mycobacterium avium complex infections.
Because of prolonged cytopenias and infectious complications after the previous lymphoma treatments, the patient was considered a poor candidate for high-dose chemotherapy. He underwent CAR T-cell therapy with axicabtagene ciloleucel and had a complete remission on day 28. Additionally, his HIV infection remained well controlled.
“Although much remains to be learned regarding CAR T-cell therapy in patients with refractory hematologic malignancies, with or without HIV infection, the cases presented herein demonstrate that patients with chemotherapy-refractory, high-grade B-cell lymphoma can successfully undergo autologous CAR T-cell manufacturing, and subsequently can safely tolerate CAR T-cell therapy and achieve a durable complete remission,” the researchers wrote. “These cases have further demonstrated the proactive, multidisciplinary care required to navigate a patient with high-risk lymphoma through CAR T-cell therapy with attention to significant medical and psychiatric comorbidities.”
Dr. Abramson reported that he has acted as a paid member of the scientific advisory board and as a paid consultant for Kite Pharma, which markets Yescarta, and several other companies.
SOURCE: Abramson JS et al. Cancer. 2019 Sep 10. doi: 10.1002/cncr.32411.
FROM CANCER
Bispecific CAR T-cell therapy yields complete responses in relapsed/refractory non-Hodgkin lymphomas
CHICAGO – A bispecific anti-CD19, anti-CD20 chimeric antigen receptor (CAR) T cell approach is safe and produced complete responses in the majority of patients with relapsed or refractory non-Hodgkin lymphoma in a phase 1 study, an investigator reported.
Eleven of 17 assessable patients had a response to treatment with the bispecific lentiviral CAR T cell (LV20.19CAR) at day 28, and of those 11 patients, 9 had complete responses, all of which are ongoing, said Nirav Niranjan Shah, MD, of the Medical College of Wisconsin in Milwaukee.
“To date, there’s no dose-limiting toxicity, no ICU-level care, no deaths attributed to treatment, no grade 3 to 4 cytokine release syndrome, and only two patients had reversible grade 3 neurotoxicity,” Dr. Shah said at the annual meeting of the American Society of Clinical Oncology.
Patients who did relapse or progress on treatment maintained CD19 or CD20 positivity, with no observed downregulation of target receptors, he reported in an oral abstract session.
Of note, the CAR T cells were produced locally at the point of care, with a 100% success rate and a set 14-day manufacturing time, he added.
Bispecific targeting of CD19 and CD20 is a new approach being investigated at a time when there are already two CD19-specific CAR T cell therapies approved for aggressive B-cell non-Hodgkin lymphomas, Dr. Shah told attendees.
“Despite the great promise of CD19 CAR T cell therapies, very quickly after the development of these therapies, we discovered mechanisms of resistance—specifically, the development of a CD19 negative relapse,” he said.
The hypothesis that targeting more than one B-cell antigen could potentially mitigate that effect stemmed from preclinical studies showing that targeting both CD19 and CD20 decreased downregulation of CD19 but not other B-cell antigens, he added.
In the present phase 1 study of the first-in-human, bispecific tandem CAR T cell against CD19 and CD20, patients have been treated at several dose levels, some with a split infusion over 2 days to evaluate safety, and some with a single infusion, Dr. Shah said.
A total of 17 patients have been treated with a lymphodepletion regimen followed by LV20.19CAR: 8 patients with diffuse large B-cell lymphoma, 6 with mantle cell lymphoma, 2 with chronic lymphocytic leukemia, and 1 with follicular lymphoma, according to the investigator. The median age of patients is 59 years, and patients had received at least 3 and up to 11 prior lines of therapy.
There have been no dose-limiting toxicities to date with dosing up to the target of 2.5 x 106 cells/kg, Dr. Shah reported, adding that there has been no grade 3-4 cytokine release syndrome and no grade 4 neurotoxicity. Grade 1-2 cytokine release syndrome has been seen in 11 patients, while grade 3 neurotoxicity occurred in 2 patients.
Fourteen of 17 patients had a response, including 11 complete responses and 3 partial responses. Eleven patients were treated at the target dose of 2.5 x 106 cells/kg, and of those, 9 had a complete response and 1 had a partial response (overall response rate, Dr. Shah said.
To date, all patients in complete response have remained in a complete response, with durations of response of 1 to 18 months.
Next, investigators plan to conduct phase 2 studies in more specific cohorts, including patients with mantle cell lymphoma, and patients who have relapsed after CD19 CAR T cell therapy, Dr. Shah said.
Dr. Shah reported disclosures related to Cidara Therapeutics, Exelixis, Geron, Oncosec, Incyte, Jazz Pharmaceuticals, Juno Therapeutics, Kite Pharma, and Miltenyi Biotec.
SOURCE: Shah NN et al. ASCO 2019. Abstract 2510.
This article was updated on 7/8/2019
CHICAGO – A bispecific anti-CD19, anti-CD20 chimeric antigen receptor (CAR) T cell approach is safe and produced complete responses in the majority of patients with relapsed or refractory non-Hodgkin lymphoma in a phase 1 study, an investigator reported.
Eleven of 17 assessable patients had a response to treatment with the bispecific lentiviral CAR T cell (LV20.19CAR) at day 28, and of those 11 patients, 9 had complete responses, all of which are ongoing, said Nirav Niranjan Shah, MD, of the Medical College of Wisconsin in Milwaukee.
“To date, there’s no dose-limiting toxicity, no ICU-level care, no deaths attributed to treatment, no grade 3 to 4 cytokine release syndrome, and only two patients had reversible grade 3 neurotoxicity,” Dr. Shah said at the annual meeting of the American Society of Clinical Oncology.
Patients who did relapse or progress on treatment maintained CD19 or CD20 positivity, with no observed downregulation of target receptors, he reported in an oral abstract session.
Of note, the CAR T cells were produced locally at the point of care, with a 100% success rate and a set 14-day manufacturing time, he added.
Bispecific targeting of CD19 and CD20 is a new approach being investigated at a time when there are already two CD19-specific CAR T cell therapies approved for aggressive B-cell non-Hodgkin lymphomas, Dr. Shah told attendees.
“Despite the great promise of CD19 CAR T cell therapies, very quickly after the development of these therapies, we discovered mechanisms of resistance—specifically, the development of a CD19 negative relapse,” he said.
The hypothesis that targeting more than one B-cell antigen could potentially mitigate that effect stemmed from preclinical studies showing that targeting both CD19 and CD20 decreased downregulation of CD19 but not other B-cell antigens, he added.
In the present phase 1 study of the first-in-human, bispecific tandem CAR T cell against CD19 and CD20, patients have been treated at several dose levels, some with a split infusion over 2 days to evaluate safety, and some with a single infusion, Dr. Shah said.
A total of 17 patients have been treated with a lymphodepletion regimen followed by LV20.19CAR: 8 patients with diffuse large B-cell lymphoma, 6 with mantle cell lymphoma, 2 with chronic lymphocytic leukemia, and 1 with follicular lymphoma, according to the investigator. The median age of patients is 59 years, and patients had received at least 3 and up to 11 prior lines of therapy.
There have been no dose-limiting toxicities to date with dosing up to the target of 2.5 x 106 cells/kg, Dr. Shah reported, adding that there has been no grade 3-4 cytokine release syndrome and no grade 4 neurotoxicity. Grade 1-2 cytokine release syndrome has been seen in 11 patients, while grade 3 neurotoxicity occurred in 2 patients.
Fourteen of 17 patients had a response, including 11 complete responses and 3 partial responses. Eleven patients were treated at the target dose of 2.5 x 106 cells/kg, and of those, 9 had a complete response and 1 had a partial response (overall response rate, Dr. Shah said.
To date, all patients in complete response have remained in a complete response, with durations of response of 1 to 18 months.
Next, investigators plan to conduct phase 2 studies in more specific cohorts, including patients with mantle cell lymphoma, and patients who have relapsed after CD19 CAR T cell therapy, Dr. Shah said.
Dr. Shah reported disclosures related to Cidara Therapeutics, Exelixis, Geron, Oncosec, Incyte, Jazz Pharmaceuticals, Juno Therapeutics, Kite Pharma, and Miltenyi Biotec.
SOURCE: Shah NN et al. ASCO 2019. Abstract 2510.
This article was updated on 7/8/2019
CHICAGO – A bispecific anti-CD19, anti-CD20 chimeric antigen receptor (CAR) T cell approach is safe and produced complete responses in the majority of patients with relapsed or refractory non-Hodgkin lymphoma in a phase 1 study, an investigator reported.
Eleven of 17 assessable patients had a response to treatment with the bispecific lentiviral CAR T cell (LV20.19CAR) at day 28, and of those 11 patients, 9 had complete responses, all of which are ongoing, said Nirav Niranjan Shah, MD, of the Medical College of Wisconsin in Milwaukee.
“To date, there’s no dose-limiting toxicity, no ICU-level care, no deaths attributed to treatment, no grade 3 to 4 cytokine release syndrome, and only two patients had reversible grade 3 neurotoxicity,” Dr. Shah said at the annual meeting of the American Society of Clinical Oncology.
Patients who did relapse or progress on treatment maintained CD19 or CD20 positivity, with no observed downregulation of target receptors, he reported in an oral abstract session.
Of note, the CAR T cells were produced locally at the point of care, with a 100% success rate and a set 14-day manufacturing time, he added.
Bispecific targeting of CD19 and CD20 is a new approach being investigated at a time when there are already two CD19-specific CAR T cell therapies approved for aggressive B-cell non-Hodgkin lymphomas, Dr. Shah told attendees.
“Despite the great promise of CD19 CAR T cell therapies, very quickly after the development of these therapies, we discovered mechanisms of resistance—specifically, the development of a CD19 negative relapse,” he said.
The hypothesis that targeting more than one B-cell antigen could potentially mitigate that effect stemmed from preclinical studies showing that targeting both CD19 and CD20 decreased downregulation of CD19 but not other B-cell antigens, he added.
In the present phase 1 study of the first-in-human, bispecific tandem CAR T cell against CD19 and CD20, patients have been treated at several dose levels, some with a split infusion over 2 days to evaluate safety, and some with a single infusion, Dr. Shah said.
A total of 17 patients have been treated with a lymphodepletion regimen followed by LV20.19CAR: 8 patients with diffuse large B-cell lymphoma, 6 with mantle cell lymphoma, 2 with chronic lymphocytic leukemia, and 1 with follicular lymphoma, according to the investigator. The median age of patients is 59 years, and patients had received at least 3 and up to 11 prior lines of therapy.
There have been no dose-limiting toxicities to date with dosing up to the target of 2.5 x 106 cells/kg, Dr. Shah reported, adding that there has been no grade 3-4 cytokine release syndrome and no grade 4 neurotoxicity. Grade 1-2 cytokine release syndrome has been seen in 11 patients, while grade 3 neurotoxicity occurred in 2 patients.
Fourteen of 17 patients had a response, including 11 complete responses and 3 partial responses. Eleven patients were treated at the target dose of 2.5 x 106 cells/kg, and of those, 9 had a complete response and 1 had a partial response (overall response rate, Dr. Shah said.
To date, all patients in complete response have remained in a complete response, with durations of response of 1 to 18 months.
Next, investigators plan to conduct phase 2 studies in more specific cohorts, including patients with mantle cell lymphoma, and patients who have relapsed after CD19 CAR T cell therapy, Dr. Shah said.
Dr. Shah reported disclosures related to Cidara Therapeutics, Exelixis, Geron, Oncosec, Incyte, Jazz Pharmaceuticals, Juno Therapeutics, Kite Pharma, and Miltenyi Biotec.
SOURCE: Shah NN et al. ASCO 2019. Abstract 2510.
This article was updated on 7/8/2019
REPORTING FROM ASCO 2019
5F9 plus rituximab take a bite out of drug-resistant NHL
AMSTERDAM – The novel monoclonal antibody , thereby thwarting a mechanism that non-Hodgkin lymphomas (NHL) use to evade immune surveillance, investigators report.
Among 97 patients with relapsed or refractory aggressive or indolent lymphomas in a phase 1b/2 trial who were treated with Hu5F9 (5F9) plus rituximab, the objective response rate (ORR) was 45%, reported Mark Roschewski, MD, of the National Cancer Institute’s Center for Cancer Research in Bethesda, Md.
5F9 is an immune checkpoint inhibitor that targets CD47, the “don’t eat me” signal that inhibits macrophages from carrying out their crucial phagocytosis role.
“Rituximab, through its activity on the Fc receptor, places an extrinsic ‘eat me’ signal, so when you give these two things together you’re blocking the ‘don’t eat me’ signal and you’re placing the ‘eat me’ signal, and then the cell becomes susceptible to phagocytosis,” he said in a briefing prior to his presentation of the data at the annual congress of the European Hematology Association.
5F9 is the first agent in its class and the most advanced in clinical trials, but several similar agents are also in development. As previously reported, a similar molecule labeled TTI-621 has shown early activity in the treatment of T-cell lymphomas.
In an interview, Dr. Roschewski explained that the therapeutic approach shows promise for the treatment of NHL and nonmalignant diseases.
“This target isn’t even specific to cancer. There is rationale for using this to treat infections or other conditions. Basically, anything that your innate immune system should normally chew up, if that cell has always been evading it using that signal, this removes that [evasion] mechanism,” he said.
In preclinical studies, 5F9 showed the most activity against NHL and acute myeloid leukemia, he noted.
Results of the phase 1b portion of the study were reported in the New England Journal of Medicine (2018;379:1711-21). At the EHA Congress, Dr. Roschewski reported on extended follow-up of the phase 1b cohort and preliminary phase 2 data.
In phase 2, the investigators enrolled patients with diffuse large B-cell lymphoma (DLBCL) that was either primary refractory to standard therapy or relapsed/refractory after two or more prior lines of therapy and who were not eligible for chimeric antigen receptor T-cell therapy. They also enrolled a smaller cohort of patients with the indolent lymphoma histologies follicular lymphoma and marginal zone lymphoma (MZL) whose disease was relapsed or refractory to at least two prior lines.
Dr. Roschewski reported on pooled data for 115 patients enrolled in phases 1b and 2: 70 with DLBCL, 41 with FL, and 4 with MZL.
The patients were heavily pretreated with a median of three prior lines of therapy. Of the patients with DLBCL, 59% had primary refractory disease, and 89% of the patients with DLBCL in phase 2 were not eligible for CAR T-cell therapy.
Among all patients in this analysis, 85% had disease that was refractory to a prior rituximab-containing regimen, and the majority had disease that was refractory to the last rituximab-containing regimen.
Among 97 patients evaluable for response (59 with DLBCL, 35 with FL, and 3 with MZL), the ORR was 45%, including 19% CR and 27% partial responses (PR). An additional 17% of patients had stable disease, and 38% experienced disease progression.
The ORR for DLBCL patients was 35%, consisting of 15% CR and 20% PR. An additional 12% of patients with DLBCL had stable disease, and 53% experienced progression.
Of the patients with indolent lymphomas, the ORR was 61%, including 24% CR and 37% PR. Of this group, 24% had stable disease, and 16% had disease progression.
For all patients, the median time to response was 1.8 months (range 1.6-7.3 months).
Efficacy among patients with DLBCL was similar across subtypes and for patients with primary refractory vs. acquired refractory disease. The responses also were similar irrespective of prior lines of therapy.
Patients tolerated the combination well, with no maximum tolerated dose at up to 45 mg/kg of 5F9, and no significant dose-related toxicities.
Most adverse events were grade 1 or 2. The most common adverse events included expected on-target anemia, caused by clearance of aging red blood cells, which are cleared by the CD47-blocking effects of 5F9. This anemia can be mitigated with an initial priming dose of 1 mg/kg 5FP that causes a transient mild decline in hemoglobin and a temporary reticulocytosis that soon resolves. Hemoglobin levels return to baseline even with continued 5F9 at doses much higher than the priming dose, Dr. Roschewski said.
Other adverse events were infusion reactions and related symptoms. There were no autoimmune adverse events, and just 8 of the 115 patients available for the safety analysis (7%) had to discontinue therapy.
Enrollment in the phase 2 trial is continuing, and a 30-mg/kg maintenance dose of 5F9 has been selected for a trial in patients with DLBCL who are either ineligible for CAR T-cell therapy or have disease that progressed on three or more prior lines of therapy.
The study is funded by Forty Seven and the Leukemia and Lymphoma Society. Dr. Roschewski reported having no financial disclosures.
SOURCE: Roschewski M et al. EHA Congress, Abstract S867.
AMSTERDAM – The novel monoclonal antibody , thereby thwarting a mechanism that non-Hodgkin lymphomas (NHL) use to evade immune surveillance, investigators report.
Among 97 patients with relapsed or refractory aggressive or indolent lymphomas in a phase 1b/2 trial who were treated with Hu5F9 (5F9) plus rituximab, the objective response rate (ORR) was 45%, reported Mark Roschewski, MD, of the National Cancer Institute’s Center for Cancer Research in Bethesda, Md.
5F9 is an immune checkpoint inhibitor that targets CD47, the “don’t eat me” signal that inhibits macrophages from carrying out their crucial phagocytosis role.
“Rituximab, through its activity on the Fc receptor, places an extrinsic ‘eat me’ signal, so when you give these two things together you’re blocking the ‘don’t eat me’ signal and you’re placing the ‘eat me’ signal, and then the cell becomes susceptible to phagocytosis,” he said in a briefing prior to his presentation of the data at the annual congress of the European Hematology Association.
5F9 is the first agent in its class and the most advanced in clinical trials, but several similar agents are also in development. As previously reported, a similar molecule labeled TTI-621 has shown early activity in the treatment of T-cell lymphomas.
In an interview, Dr. Roschewski explained that the therapeutic approach shows promise for the treatment of NHL and nonmalignant diseases.
“This target isn’t even specific to cancer. There is rationale for using this to treat infections or other conditions. Basically, anything that your innate immune system should normally chew up, if that cell has always been evading it using that signal, this removes that [evasion] mechanism,” he said.
In preclinical studies, 5F9 showed the most activity against NHL and acute myeloid leukemia, he noted.
Results of the phase 1b portion of the study were reported in the New England Journal of Medicine (2018;379:1711-21). At the EHA Congress, Dr. Roschewski reported on extended follow-up of the phase 1b cohort and preliminary phase 2 data.
In phase 2, the investigators enrolled patients with diffuse large B-cell lymphoma (DLBCL) that was either primary refractory to standard therapy or relapsed/refractory after two or more prior lines of therapy and who were not eligible for chimeric antigen receptor T-cell therapy. They also enrolled a smaller cohort of patients with the indolent lymphoma histologies follicular lymphoma and marginal zone lymphoma (MZL) whose disease was relapsed or refractory to at least two prior lines.
Dr. Roschewski reported on pooled data for 115 patients enrolled in phases 1b and 2: 70 with DLBCL, 41 with FL, and 4 with MZL.
The patients were heavily pretreated with a median of three prior lines of therapy. Of the patients with DLBCL, 59% had primary refractory disease, and 89% of the patients with DLBCL in phase 2 were not eligible for CAR T-cell therapy.
Among all patients in this analysis, 85% had disease that was refractory to a prior rituximab-containing regimen, and the majority had disease that was refractory to the last rituximab-containing regimen.
Among 97 patients evaluable for response (59 with DLBCL, 35 with FL, and 3 with MZL), the ORR was 45%, including 19% CR and 27% partial responses (PR). An additional 17% of patients had stable disease, and 38% experienced disease progression.
The ORR for DLBCL patients was 35%, consisting of 15% CR and 20% PR. An additional 12% of patients with DLBCL had stable disease, and 53% experienced progression.
Of the patients with indolent lymphomas, the ORR was 61%, including 24% CR and 37% PR. Of this group, 24% had stable disease, and 16% had disease progression.
For all patients, the median time to response was 1.8 months (range 1.6-7.3 months).
Efficacy among patients with DLBCL was similar across subtypes and for patients with primary refractory vs. acquired refractory disease. The responses also were similar irrespective of prior lines of therapy.
Patients tolerated the combination well, with no maximum tolerated dose at up to 45 mg/kg of 5F9, and no significant dose-related toxicities.
Most adverse events were grade 1 or 2. The most common adverse events included expected on-target anemia, caused by clearance of aging red blood cells, which are cleared by the CD47-blocking effects of 5F9. This anemia can be mitigated with an initial priming dose of 1 mg/kg 5FP that causes a transient mild decline in hemoglobin and a temporary reticulocytosis that soon resolves. Hemoglobin levels return to baseline even with continued 5F9 at doses much higher than the priming dose, Dr. Roschewski said.
Other adverse events were infusion reactions and related symptoms. There were no autoimmune adverse events, and just 8 of the 115 patients available for the safety analysis (7%) had to discontinue therapy.
Enrollment in the phase 2 trial is continuing, and a 30-mg/kg maintenance dose of 5F9 has been selected for a trial in patients with DLBCL who are either ineligible for CAR T-cell therapy or have disease that progressed on three or more prior lines of therapy.
The study is funded by Forty Seven and the Leukemia and Lymphoma Society. Dr. Roschewski reported having no financial disclosures.
SOURCE: Roschewski M et al. EHA Congress, Abstract S867.
AMSTERDAM – The novel monoclonal antibody , thereby thwarting a mechanism that non-Hodgkin lymphomas (NHL) use to evade immune surveillance, investigators report.
Among 97 patients with relapsed or refractory aggressive or indolent lymphomas in a phase 1b/2 trial who were treated with Hu5F9 (5F9) plus rituximab, the objective response rate (ORR) was 45%, reported Mark Roschewski, MD, of the National Cancer Institute’s Center for Cancer Research in Bethesda, Md.
5F9 is an immune checkpoint inhibitor that targets CD47, the “don’t eat me” signal that inhibits macrophages from carrying out their crucial phagocytosis role.
“Rituximab, through its activity on the Fc receptor, places an extrinsic ‘eat me’ signal, so when you give these two things together you’re blocking the ‘don’t eat me’ signal and you’re placing the ‘eat me’ signal, and then the cell becomes susceptible to phagocytosis,” he said in a briefing prior to his presentation of the data at the annual congress of the European Hematology Association.
5F9 is the first agent in its class and the most advanced in clinical trials, but several similar agents are also in development. As previously reported, a similar molecule labeled TTI-621 has shown early activity in the treatment of T-cell lymphomas.
In an interview, Dr. Roschewski explained that the therapeutic approach shows promise for the treatment of NHL and nonmalignant diseases.
“This target isn’t even specific to cancer. There is rationale for using this to treat infections or other conditions. Basically, anything that your innate immune system should normally chew up, if that cell has always been evading it using that signal, this removes that [evasion] mechanism,” he said.
In preclinical studies, 5F9 showed the most activity against NHL and acute myeloid leukemia, he noted.
Results of the phase 1b portion of the study were reported in the New England Journal of Medicine (2018;379:1711-21). At the EHA Congress, Dr. Roschewski reported on extended follow-up of the phase 1b cohort and preliminary phase 2 data.
In phase 2, the investigators enrolled patients with diffuse large B-cell lymphoma (DLBCL) that was either primary refractory to standard therapy or relapsed/refractory after two or more prior lines of therapy and who were not eligible for chimeric antigen receptor T-cell therapy. They also enrolled a smaller cohort of patients with the indolent lymphoma histologies follicular lymphoma and marginal zone lymphoma (MZL) whose disease was relapsed or refractory to at least two prior lines.
Dr. Roschewski reported on pooled data for 115 patients enrolled in phases 1b and 2: 70 with DLBCL, 41 with FL, and 4 with MZL.
The patients were heavily pretreated with a median of three prior lines of therapy. Of the patients with DLBCL, 59% had primary refractory disease, and 89% of the patients with DLBCL in phase 2 were not eligible for CAR T-cell therapy.
Among all patients in this analysis, 85% had disease that was refractory to a prior rituximab-containing regimen, and the majority had disease that was refractory to the last rituximab-containing regimen.
Among 97 patients evaluable for response (59 with DLBCL, 35 with FL, and 3 with MZL), the ORR was 45%, including 19% CR and 27% partial responses (PR). An additional 17% of patients had stable disease, and 38% experienced disease progression.
The ORR for DLBCL patients was 35%, consisting of 15% CR and 20% PR. An additional 12% of patients with DLBCL had stable disease, and 53% experienced progression.
Of the patients with indolent lymphomas, the ORR was 61%, including 24% CR and 37% PR. Of this group, 24% had stable disease, and 16% had disease progression.
For all patients, the median time to response was 1.8 months (range 1.6-7.3 months).
Efficacy among patients with DLBCL was similar across subtypes and for patients with primary refractory vs. acquired refractory disease. The responses also were similar irrespective of prior lines of therapy.
Patients tolerated the combination well, with no maximum tolerated dose at up to 45 mg/kg of 5F9, and no significant dose-related toxicities.
Most adverse events were grade 1 or 2. The most common adverse events included expected on-target anemia, caused by clearance of aging red blood cells, which are cleared by the CD47-blocking effects of 5F9. This anemia can be mitigated with an initial priming dose of 1 mg/kg 5FP that causes a transient mild decline in hemoglobin and a temporary reticulocytosis that soon resolves. Hemoglobin levels return to baseline even with continued 5F9 at doses much higher than the priming dose, Dr. Roschewski said.
Other adverse events were infusion reactions and related symptoms. There were no autoimmune adverse events, and just 8 of the 115 patients available for the safety analysis (7%) had to discontinue therapy.
Enrollment in the phase 2 trial is continuing, and a 30-mg/kg maintenance dose of 5F9 has been selected for a trial in patients with DLBCL who are either ineligible for CAR T-cell therapy or have disease that progressed on three or more prior lines of therapy.
The study is funded by Forty Seven and the Leukemia and Lymphoma Society. Dr. Roschewski reported having no financial disclosures.
SOURCE: Roschewski M et al. EHA Congress, Abstract S867.
REPORTING FROM EHA CONGRESS
Key clinical point: The combination of Hu5F9 and rituximab shows activity in heavily pretreated, relapsed/refractory lymphomas.
Major finding: Among all evaluable patients, the objective response rate was 45%. The objective response rate for patients with diffuse large B-cell lymphoma was 35%.
Study details: A pooled analysis of data from phase 1b/2 studies in patients with aggressive and indolent lymphomas. Among 97 patients evaluable for response, there were 59 patients with diffuse large B-cell lymphoma, 35 with follicular lymphoma, and 3 with marginal zone lymphoma.
Disclosures: The study is funded by Forty Seven and the Leukemia and Lymphoma Society. Dr. Roschewski reported having no financial disclosures.
Source: Roschewski M et al. EHA Congress, Abstract S867.
‘Encouraging’ responses seen with durvalumab plus R-CHOP in DLBCL
CHICAGO – A six-drug combination produced complete responses in previously untreated, high-risk diffuse large B-cell lymphoma (DLBCL) patients in a phase 2 trial.
Induction with durvalumab and R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) produced complete response rates of 54% in the entire cohort and 41% in patients with double- or triple-hit lymphoma. Immune-related adverse events (AEs) were common with this regimen, but no unexpected AEs occurred, according to researchers.
Grzegorz S. Nowakowski, MD, of the Mayo Clinic in Rochester, Minn., and colleagues presented these results in a poster at the annual meeting of the American Society of Clinical Oncology.
Treatment
The phase 2 trial (NCT03003520) was designed to assess durvalumab plus R-CHOP as well as durvalumab plus R-CHOP and lenalidomide (R2-CHOP) in patients with previously untreated, high-risk DLBCL. However, the R2-CHOP arm was closed early.
In cycle one, all patients received durvalumab plus R-CHOP. For subsequent cycles, patients with activated B-cell (ABC) DLBCL were assigned to durvalumab plus R2-CHOP, while patients with non-ABC DLBCL continued on durvalumab plus R-CHOP.
The R2-CHOP arm was closed early due to safety issues observed in trials combining checkpoint inhibitors with immunomodulatory agents. A partial clinical hold was placed on the R2-CHOP arm, but patients could continue on the regimen if they experienced a clinical benefit. Any patients with ABC DLBCL who were enrolled after the partial hold received treatment with durvalumab plus R-CHOP.
Induction was given for up to eight cycles and was followed by consolidation with durvalumab alone for up to 12 months from the start of induction.
Patient characteristics
The researchers presented data on 43 patients in the durvalumab plus R-CHOP arm. The patients’ median age was 62 years, and 61% were men.
“I think it’s worth noting that 46% of patients in the durvalumab plus R-CHOP group had very high-risk features, including double-hit or triple-hit genetic features,” said Justin Kline, MD, of the University of Chicago Medicine who reviewed this study in a poster discussion session.
Specifically, 30% of patients had double-hit lymphoma, and 16% had triple-hit lymphoma. Most patients had a high-intermediate-risk (49%) or high-risk (21%) International Prognostic Index score, and 79% of patients had Ann Arbor stage IV disease.
Efficacy
As of Aug. 2, 2018, 70% of patients had completed induction, 2% had completed consolidation, 44% remained on treatment, and 54% had discontinued therapy. The most common reasons for stopping treatment were progression (16%), AEs (14%), and consent withdrawal (12%).
“The combination of durvalumab plus R-CHOP demonstrated encouraging response rates … in subjects with high-risk DLBCL, including double- and triple-hit lymphomas,” Dr. Kline said.
The complete response rate was 54% (20/37) at the end of induction and 68% (n = 25) at the end of consolidation. The partial response rate at the end of consolidation was 30% (n = 11).
In patients with double- or triple-hit lymphoma, the complete response rate at the end of induction was 41% (7/17). The overall response rate in this group was 88% (n = 15).
Safety
“The safety profile was as expected for the components of the combination, and no new safety signals were observed,” Dr. Kline said.
He noted that AEs of special interest, or immune-related AEs, occurred in 61% of patients, but most of these events were grade 1 or 2.
AEs of special interest included diarrhea (28%), rash (23%), infusion-related reactions (16%), dermatitis (12%), hypothyroidism (5%), myocarditis (5%), adrenal insufficiency (2%), and hepatitis (2%).
Grade 3 or 4 AEs of special interest included infusion-related reactions (5%), rash (2%), diarrhea (2%), and hepatitis (2%).
The safety and efficacy results support further evaluation of durvalumab plus R-CHOP, although it will be important to identify DLBCL patients who are more likely to derive a clinical benefit from PD-1 or PD-L1 blockade, Dr. Kline said.
“This early study showed that the combination is feasible,” Dr. Nowakowski added. “I think, down the road, we’ll need to identify patients who can actually benefit from this combination. We definitely have clinical evidence of exceptional responses to PD-1 blockade.”
The trial was sponsored by Celgene. Dr. Nowakowski reported relationships with Celgene, Genentech, MorphoSys, and NanoString Technologies. Dr. Kline reported relationships with Cardinal Health, Merck, Seattle Genetics, Kite/Gilead, ITeos Therapeutics, and Bristol-Myers Squibb.
SOURCE: Nowakowski GS et al. ASCO 2019, Abstract 7520.
CHICAGO – A six-drug combination produced complete responses in previously untreated, high-risk diffuse large B-cell lymphoma (DLBCL) patients in a phase 2 trial.
Induction with durvalumab and R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) produced complete response rates of 54% in the entire cohort and 41% in patients with double- or triple-hit lymphoma. Immune-related adverse events (AEs) were common with this regimen, but no unexpected AEs occurred, according to researchers.
Grzegorz S. Nowakowski, MD, of the Mayo Clinic in Rochester, Minn., and colleagues presented these results in a poster at the annual meeting of the American Society of Clinical Oncology.
Treatment
The phase 2 trial (NCT03003520) was designed to assess durvalumab plus R-CHOP as well as durvalumab plus R-CHOP and lenalidomide (R2-CHOP) in patients with previously untreated, high-risk DLBCL. However, the R2-CHOP arm was closed early.
In cycle one, all patients received durvalumab plus R-CHOP. For subsequent cycles, patients with activated B-cell (ABC) DLBCL were assigned to durvalumab plus R2-CHOP, while patients with non-ABC DLBCL continued on durvalumab plus R-CHOP.
The R2-CHOP arm was closed early due to safety issues observed in trials combining checkpoint inhibitors with immunomodulatory agents. A partial clinical hold was placed on the R2-CHOP arm, but patients could continue on the regimen if they experienced a clinical benefit. Any patients with ABC DLBCL who were enrolled after the partial hold received treatment with durvalumab plus R-CHOP.
Induction was given for up to eight cycles and was followed by consolidation with durvalumab alone for up to 12 months from the start of induction.
Patient characteristics
The researchers presented data on 43 patients in the durvalumab plus R-CHOP arm. The patients’ median age was 62 years, and 61% were men.
“I think it’s worth noting that 46% of patients in the durvalumab plus R-CHOP group had very high-risk features, including double-hit or triple-hit genetic features,” said Justin Kline, MD, of the University of Chicago Medicine who reviewed this study in a poster discussion session.
Specifically, 30% of patients had double-hit lymphoma, and 16% had triple-hit lymphoma. Most patients had a high-intermediate-risk (49%) or high-risk (21%) International Prognostic Index score, and 79% of patients had Ann Arbor stage IV disease.
Efficacy
As of Aug. 2, 2018, 70% of patients had completed induction, 2% had completed consolidation, 44% remained on treatment, and 54% had discontinued therapy. The most common reasons for stopping treatment were progression (16%), AEs (14%), and consent withdrawal (12%).
“The combination of durvalumab plus R-CHOP demonstrated encouraging response rates … in subjects with high-risk DLBCL, including double- and triple-hit lymphomas,” Dr. Kline said.
The complete response rate was 54% (20/37) at the end of induction and 68% (n = 25) at the end of consolidation. The partial response rate at the end of consolidation was 30% (n = 11).
In patients with double- or triple-hit lymphoma, the complete response rate at the end of induction was 41% (7/17). The overall response rate in this group was 88% (n = 15).
Safety
“The safety profile was as expected for the components of the combination, and no new safety signals were observed,” Dr. Kline said.
He noted that AEs of special interest, or immune-related AEs, occurred in 61% of patients, but most of these events were grade 1 or 2.
AEs of special interest included diarrhea (28%), rash (23%), infusion-related reactions (16%), dermatitis (12%), hypothyroidism (5%), myocarditis (5%), adrenal insufficiency (2%), and hepatitis (2%).
Grade 3 or 4 AEs of special interest included infusion-related reactions (5%), rash (2%), diarrhea (2%), and hepatitis (2%).
The safety and efficacy results support further evaluation of durvalumab plus R-CHOP, although it will be important to identify DLBCL patients who are more likely to derive a clinical benefit from PD-1 or PD-L1 blockade, Dr. Kline said.
“This early study showed that the combination is feasible,” Dr. Nowakowski added. “I think, down the road, we’ll need to identify patients who can actually benefit from this combination. We definitely have clinical evidence of exceptional responses to PD-1 blockade.”
The trial was sponsored by Celgene. Dr. Nowakowski reported relationships with Celgene, Genentech, MorphoSys, and NanoString Technologies. Dr. Kline reported relationships with Cardinal Health, Merck, Seattle Genetics, Kite/Gilead, ITeos Therapeutics, and Bristol-Myers Squibb.
SOURCE: Nowakowski GS et al. ASCO 2019, Abstract 7520.
CHICAGO – A six-drug combination produced complete responses in previously untreated, high-risk diffuse large B-cell lymphoma (DLBCL) patients in a phase 2 trial.
Induction with durvalumab and R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) produced complete response rates of 54% in the entire cohort and 41% in patients with double- or triple-hit lymphoma. Immune-related adverse events (AEs) were common with this regimen, but no unexpected AEs occurred, according to researchers.
Grzegorz S. Nowakowski, MD, of the Mayo Clinic in Rochester, Minn., and colleagues presented these results in a poster at the annual meeting of the American Society of Clinical Oncology.
Treatment
The phase 2 trial (NCT03003520) was designed to assess durvalumab plus R-CHOP as well as durvalumab plus R-CHOP and lenalidomide (R2-CHOP) in patients with previously untreated, high-risk DLBCL. However, the R2-CHOP arm was closed early.
In cycle one, all patients received durvalumab plus R-CHOP. For subsequent cycles, patients with activated B-cell (ABC) DLBCL were assigned to durvalumab plus R2-CHOP, while patients with non-ABC DLBCL continued on durvalumab plus R-CHOP.
The R2-CHOP arm was closed early due to safety issues observed in trials combining checkpoint inhibitors with immunomodulatory agents. A partial clinical hold was placed on the R2-CHOP arm, but patients could continue on the regimen if they experienced a clinical benefit. Any patients with ABC DLBCL who were enrolled after the partial hold received treatment with durvalumab plus R-CHOP.
Induction was given for up to eight cycles and was followed by consolidation with durvalumab alone for up to 12 months from the start of induction.
Patient characteristics
The researchers presented data on 43 patients in the durvalumab plus R-CHOP arm. The patients’ median age was 62 years, and 61% were men.
“I think it’s worth noting that 46% of patients in the durvalumab plus R-CHOP group had very high-risk features, including double-hit or triple-hit genetic features,” said Justin Kline, MD, of the University of Chicago Medicine who reviewed this study in a poster discussion session.
Specifically, 30% of patients had double-hit lymphoma, and 16% had triple-hit lymphoma. Most patients had a high-intermediate-risk (49%) or high-risk (21%) International Prognostic Index score, and 79% of patients had Ann Arbor stage IV disease.
Efficacy
As of Aug. 2, 2018, 70% of patients had completed induction, 2% had completed consolidation, 44% remained on treatment, and 54% had discontinued therapy. The most common reasons for stopping treatment were progression (16%), AEs (14%), and consent withdrawal (12%).
“The combination of durvalumab plus R-CHOP demonstrated encouraging response rates … in subjects with high-risk DLBCL, including double- and triple-hit lymphomas,” Dr. Kline said.
The complete response rate was 54% (20/37) at the end of induction and 68% (n = 25) at the end of consolidation. The partial response rate at the end of consolidation was 30% (n = 11).
In patients with double- or triple-hit lymphoma, the complete response rate at the end of induction was 41% (7/17). The overall response rate in this group was 88% (n = 15).
Safety
“The safety profile was as expected for the components of the combination, and no new safety signals were observed,” Dr. Kline said.
He noted that AEs of special interest, or immune-related AEs, occurred in 61% of patients, but most of these events were grade 1 or 2.
AEs of special interest included diarrhea (28%), rash (23%), infusion-related reactions (16%), dermatitis (12%), hypothyroidism (5%), myocarditis (5%), adrenal insufficiency (2%), and hepatitis (2%).
Grade 3 or 4 AEs of special interest included infusion-related reactions (5%), rash (2%), diarrhea (2%), and hepatitis (2%).
The safety and efficacy results support further evaluation of durvalumab plus R-CHOP, although it will be important to identify DLBCL patients who are more likely to derive a clinical benefit from PD-1 or PD-L1 blockade, Dr. Kline said.
“This early study showed that the combination is feasible,” Dr. Nowakowski added. “I think, down the road, we’ll need to identify patients who can actually benefit from this combination. We definitely have clinical evidence of exceptional responses to PD-1 blockade.”
The trial was sponsored by Celgene. Dr. Nowakowski reported relationships with Celgene, Genentech, MorphoSys, and NanoString Technologies. Dr. Kline reported relationships with Cardinal Health, Merck, Seattle Genetics, Kite/Gilead, ITeos Therapeutics, and Bristol-Myers Squibb.
SOURCE: Nowakowski GS et al. ASCO 2019, Abstract 7520.
REPORTING FROM ASCO 2019
Chemo-free Smart Start regimen looks promising in poor-prognosis DLBCL
CHICAGO – A chemotherapy-free regimen has produced promising early response and survival outcomes in patients with a particularly poor-prognosis subtype of diffuse large B-cell lymphoma, an investigator reported at the annual meeting of the American Society of Clinical Oncology.
The overall response rate was 86% after two cycles of combined rituximab, lenalidomide, and ibrutinib – or RLI – in patients with newly diagnosed diffuse large B-cell lymphoma (DLBCL) of the non–germinal center (non-GCB) subtype, said Jason Westin, MD, of the department of lymphoma/myeloma at the University of Texas MD Anderson Cancer Center in Houston.
The response rate increased to 96% after subsequent cycles of RLI plus standard chemotherapy, said Dr.Westin, who added that the rates of progression-free and overall survival at 1 year were also 96% in the investigator initiated, single-arm, open-label, phase 2 study, called Smart Start.
That looks quite favorable, compared with what’s been achieved in previous studies in this poor-prognosis group of patients, Dr. Westin said during a podium presentation of Smart Start data, though he cautioned against direct comparison to historical studies and added that further follow-up is needed.
“Our survival outcomes appear excellent with about a year’s worth of follow-up,” he said during his presentation. “I’d say the novel/novel combinations, with and without chemotherapy, are feasible for large cell, and next step studies are warranted.”
Jasmine M. Zain, MD, of City of Hope Comprehensive Cancer Center, said these results so far raise the possibility of an effective chemotherapy-free treatment regimen for aggressive lymphomas.
“This regimen, particularly for non-GCB subtypes, is extremely promising,” Dr. Zain said during a podium discussion of the study. “I think we were all oohing and aahing over the results, and it could possibly even be practice changing.”
Moving to a nonchemotherapy regimen could raise new questions for treatment of non-GCB and possibly also GCB subtypes of DLBCL, such as when the treatments could be stopped, or whether a maintenance approach would be useful, she added.
The Smart Start study enrolled a total of 60 patients with non-GCB DLBCL. The patients received RLI for two 21-day cycles, followed by another six cycles of RLI plus chemotherapy, which was either EPOCH or CHOP, at the investigators’ discretion.
“With a median follow-up of 362 days, we’ve had three progression events,” Dr. Westin said in his discussion of the preliminary efficacy results.
Adverse events were similar to what would be expected for standard chemotherapy, according to Dr. Westin, except for rash, which was seen mainly in cycles one and two.
There were two deaths on study protocol, including one fatal fungal infection that investigators attributed to high dose corticosteroids and RLI. There were no subsequent fungal infections after a protocol amendment prohibiting corticosteroids during the RLI-only cycles, according to the investigators’ report.
The high response rates following the initial lead-in phase made investigators wonder what would happen without subsequent chemotherapy, Dr. Westin told attendees during his oral presentation. In one case, a 74-year-old man did complete the two lead-in cycles of RLI and declined further therapy.
“He’s now nearly 2 years out, without any additional therapy, and has not relapsed to date,” Dr. Westin said. “This is, again, with 6 weeks worth of RLI therapy.”
Final results and minimal residual disease data from the Smart Start study will be presented at a conference later in 2019, Dr. Westin said.
The study received research support and funding from the ASCO Conquer Cancer Foundation. The trial drug and support were provided by Celgene and Janssen. Dr. Westin reported disclosures related to Celgene, Genentech/Abbvie, Kite Pharma, Kite/Gilead, Novartis, ProNAi, Spectrum Pharmaceuticals, Bristol-Myers Squibb, Janssen, and Karyopharm Therapeutics.
SOURCE: Westin J et al. ASCO 2019, Abstract 7508.
CHICAGO – A chemotherapy-free regimen has produced promising early response and survival outcomes in patients with a particularly poor-prognosis subtype of diffuse large B-cell lymphoma, an investigator reported at the annual meeting of the American Society of Clinical Oncology.
The overall response rate was 86% after two cycles of combined rituximab, lenalidomide, and ibrutinib – or RLI – in patients with newly diagnosed diffuse large B-cell lymphoma (DLBCL) of the non–germinal center (non-GCB) subtype, said Jason Westin, MD, of the department of lymphoma/myeloma at the University of Texas MD Anderson Cancer Center in Houston.
The response rate increased to 96% after subsequent cycles of RLI plus standard chemotherapy, said Dr.Westin, who added that the rates of progression-free and overall survival at 1 year were also 96% in the investigator initiated, single-arm, open-label, phase 2 study, called Smart Start.
That looks quite favorable, compared with what’s been achieved in previous studies in this poor-prognosis group of patients, Dr. Westin said during a podium presentation of Smart Start data, though he cautioned against direct comparison to historical studies and added that further follow-up is needed.
“Our survival outcomes appear excellent with about a year’s worth of follow-up,” he said during his presentation. “I’d say the novel/novel combinations, with and without chemotherapy, are feasible for large cell, and next step studies are warranted.”
Jasmine M. Zain, MD, of City of Hope Comprehensive Cancer Center, said these results so far raise the possibility of an effective chemotherapy-free treatment regimen for aggressive lymphomas.
“This regimen, particularly for non-GCB subtypes, is extremely promising,” Dr. Zain said during a podium discussion of the study. “I think we were all oohing and aahing over the results, and it could possibly even be practice changing.”
Moving to a nonchemotherapy regimen could raise new questions for treatment of non-GCB and possibly also GCB subtypes of DLBCL, such as when the treatments could be stopped, or whether a maintenance approach would be useful, she added.
The Smart Start study enrolled a total of 60 patients with non-GCB DLBCL. The patients received RLI for two 21-day cycles, followed by another six cycles of RLI plus chemotherapy, which was either EPOCH or CHOP, at the investigators’ discretion.
“With a median follow-up of 362 days, we’ve had three progression events,” Dr. Westin said in his discussion of the preliminary efficacy results.
Adverse events were similar to what would be expected for standard chemotherapy, according to Dr. Westin, except for rash, which was seen mainly in cycles one and two.
There were two deaths on study protocol, including one fatal fungal infection that investigators attributed to high dose corticosteroids and RLI. There were no subsequent fungal infections after a protocol amendment prohibiting corticosteroids during the RLI-only cycles, according to the investigators’ report.
The high response rates following the initial lead-in phase made investigators wonder what would happen without subsequent chemotherapy, Dr. Westin told attendees during his oral presentation. In one case, a 74-year-old man did complete the two lead-in cycles of RLI and declined further therapy.
“He’s now nearly 2 years out, without any additional therapy, and has not relapsed to date,” Dr. Westin said. “This is, again, with 6 weeks worth of RLI therapy.”
Final results and minimal residual disease data from the Smart Start study will be presented at a conference later in 2019, Dr. Westin said.
The study received research support and funding from the ASCO Conquer Cancer Foundation. The trial drug and support were provided by Celgene and Janssen. Dr. Westin reported disclosures related to Celgene, Genentech/Abbvie, Kite Pharma, Kite/Gilead, Novartis, ProNAi, Spectrum Pharmaceuticals, Bristol-Myers Squibb, Janssen, and Karyopharm Therapeutics.
SOURCE: Westin J et al. ASCO 2019, Abstract 7508.
CHICAGO – A chemotherapy-free regimen has produced promising early response and survival outcomes in patients with a particularly poor-prognosis subtype of diffuse large B-cell lymphoma, an investigator reported at the annual meeting of the American Society of Clinical Oncology.
The overall response rate was 86% after two cycles of combined rituximab, lenalidomide, and ibrutinib – or RLI – in patients with newly diagnosed diffuse large B-cell lymphoma (DLBCL) of the non–germinal center (non-GCB) subtype, said Jason Westin, MD, of the department of lymphoma/myeloma at the University of Texas MD Anderson Cancer Center in Houston.
The response rate increased to 96% after subsequent cycles of RLI plus standard chemotherapy, said Dr.Westin, who added that the rates of progression-free and overall survival at 1 year were also 96% in the investigator initiated, single-arm, open-label, phase 2 study, called Smart Start.
That looks quite favorable, compared with what’s been achieved in previous studies in this poor-prognosis group of patients, Dr. Westin said during a podium presentation of Smart Start data, though he cautioned against direct comparison to historical studies and added that further follow-up is needed.
“Our survival outcomes appear excellent with about a year’s worth of follow-up,” he said during his presentation. “I’d say the novel/novel combinations, with and without chemotherapy, are feasible for large cell, and next step studies are warranted.”
Jasmine M. Zain, MD, of City of Hope Comprehensive Cancer Center, said these results so far raise the possibility of an effective chemotherapy-free treatment regimen for aggressive lymphomas.
“This regimen, particularly for non-GCB subtypes, is extremely promising,” Dr. Zain said during a podium discussion of the study. “I think we were all oohing and aahing over the results, and it could possibly even be practice changing.”
Moving to a nonchemotherapy regimen could raise new questions for treatment of non-GCB and possibly also GCB subtypes of DLBCL, such as when the treatments could be stopped, or whether a maintenance approach would be useful, she added.
The Smart Start study enrolled a total of 60 patients with non-GCB DLBCL. The patients received RLI for two 21-day cycles, followed by another six cycles of RLI plus chemotherapy, which was either EPOCH or CHOP, at the investigators’ discretion.
“With a median follow-up of 362 days, we’ve had three progression events,” Dr. Westin said in his discussion of the preliminary efficacy results.
Adverse events were similar to what would be expected for standard chemotherapy, according to Dr. Westin, except for rash, which was seen mainly in cycles one and two.
There were two deaths on study protocol, including one fatal fungal infection that investigators attributed to high dose corticosteroids and RLI. There were no subsequent fungal infections after a protocol amendment prohibiting corticosteroids during the RLI-only cycles, according to the investigators’ report.
The high response rates following the initial lead-in phase made investigators wonder what would happen without subsequent chemotherapy, Dr. Westin told attendees during his oral presentation. In one case, a 74-year-old man did complete the two lead-in cycles of RLI and declined further therapy.
“He’s now nearly 2 years out, without any additional therapy, and has not relapsed to date,” Dr. Westin said. “This is, again, with 6 weeks worth of RLI therapy.”
Final results and minimal residual disease data from the Smart Start study will be presented at a conference later in 2019, Dr. Westin said.
The study received research support and funding from the ASCO Conquer Cancer Foundation. The trial drug and support were provided by Celgene and Janssen. Dr. Westin reported disclosures related to Celgene, Genentech/Abbvie, Kite Pharma, Kite/Gilead, Novartis, ProNAi, Spectrum Pharmaceuticals, Bristol-Myers Squibb, Janssen, and Karyopharm Therapeutics.
SOURCE: Westin J et al. ASCO 2019, Abstract 7508.
REPORTING FROM ASCO 2019
SC-PEG comparable to pegaspargase in young ALL/LL patients
CHICAGO – Calaspargase pegol (SC-PEG) produces similar outcomes as standard pegaspargase in pediatric and young adult patients with newly diagnosed acute lymphoblastic leukemia (ALL) or lymphoblastic lymphoma (LL), according to a phase 2 trial.
Patients who received SC-PEG every 3 weeks had similar serum asparaginase activity (SAA), toxicities, and survival rates as patients who received standard pegaspargase every 2 weeks.
Lynda M. Vrooman, MD, of Dana-Farber Cancer Institute in Boston, presented these results at the annual meeting of the American Society of Clinical Oncology.
The trial (NCT01574274) enrolled 239 patients, 230 with ALL and 9 with LL. Most patients had B-cell (n = 207) disease. The patients’ median age was 5.2 years (range, 1.0-20.9 years).
“There were no differences in presenting features by randomization,” Dr. Vrooman noted.
The patients were randomized to receive pegaspargase (n = 120) or SC-PEG (n = 119), a pegylated asparaginase formulation with longer half-life. SC-PEG was given at 2,500 IU/m2 every 3 weeks, and pegaspargase was given at 2,500 IU/m2 every 2 weeks.
Either asparaginase product was given as part of a 4-week induction regimen (vincristine, prednisone, doxorubicin, and methotrexate), a 3-week intensification regimen (intrathecal chemotherapy with or without radiotherapy) for central nervous system disease, and a 27-week second consolidation regimen (mercaptopurine, methotrexate, and, in high-risk patients, doxorubicin).
SAA
The researchers observed significantly longer SAA with SC-PEG during induction but not after.
During induction, at 25 days after the first asparaginase dose, 88% of patients on SC-PEG and 17% of those on pegaspargase had SAA of at least 0.10 IU/mL (P less than .001). Post-induction, at week 25, 100% of patients in each group had a nadir SAA of at least 0.10 IU/mL.
“The high nadir serum asparaginase activity levels observed for both preparations suggest dosing strategies could be further optimized,” Dr. Vrooman noted.
Safety
There were no significant differences in adverse events between the SC-PEG and pegaspargase arms during or after induction.
Adverse events during induction (in the SC-PEG and pegaspargase arms, respectively) included grade 2 or higher asparaginase allergy (0% and 1%), grade 2 or higher pancreatitis (3% in both), grade 2 or higher thrombosis (3% and 9%), grade 4 hyperbilirubinemia (3% and 1%), grade 3 or higher bacterial infection (12% and 9%), and grade 3 or higher fungal infection (4% and 5%).
Adverse events after induction (in the SC-PEG and pegaspargase arms, respectively) included grade 2 or higher asparaginase allergy (17% and 14%), grade 2 or higher pancreatitis (15% in both), grade 2 or higher thrombosis (18% and 13%), grade 4 hyperbilirubinemia (4% and 3%), grade 3 or higher bacterial infection (12% and 15%), grade 3 or higher fungal infection (2% and 1%), grade 2 or higher bone fracture (3% and 8%), and grade 2 or higher osteonecrosis (3% and 4%).
Response and survival
The complete response rate was 95% (109/115) in the SC-PEG arm and 99% (114/115) in the pegaspargase arm. Rates of induction failure were 3% (n = 4) and 1% (n = 1), respectively, and rates of relapse were 3% (n = 5) and 8% (n = 10), respectively.
There were two induction deaths and two remission deaths in the SC-PEG arm but no induction or remission deaths in the pegaspargase arm.
The median follow-up was 4 years. The 4-year event-free survival rate was 87.7% with SC-PEG and 90.2% with pegaspargase (P = .78). The 4-year overall survival rate was 94.8% and 95.6%, respectively (P = .74).
In closing, Dr. Vrooman said these data suggest SC-PEG provides similar results as standard pegaspargase. She noted that these data informed the U.S. approval of SC-PEG for pediatric and young adult ALL.
This trial was sponsored by the Dana-Farber Cancer Institute in collaboration with Shire and the National Cancer Institute. Dr. Vrooman said she had no relationships to disclose.
SOURCE: Vrooman LM et al. ASCO 2019. Abstract 10006.
CHICAGO – Calaspargase pegol (SC-PEG) produces similar outcomes as standard pegaspargase in pediatric and young adult patients with newly diagnosed acute lymphoblastic leukemia (ALL) or lymphoblastic lymphoma (LL), according to a phase 2 trial.
Patients who received SC-PEG every 3 weeks had similar serum asparaginase activity (SAA), toxicities, and survival rates as patients who received standard pegaspargase every 2 weeks.
Lynda M. Vrooman, MD, of Dana-Farber Cancer Institute in Boston, presented these results at the annual meeting of the American Society of Clinical Oncology.
The trial (NCT01574274) enrolled 239 patients, 230 with ALL and 9 with LL. Most patients had B-cell (n = 207) disease. The patients’ median age was 5.2 years (range, 1.0-20.9 years).
“There were no differences in presenting features by randomization,” Dr. Vrooman noted.
The patients were randomized to receive pegaspargase (n = 120) or SC-PEG (n = 119), a pegylated asparaginase formulation with longer half-life. SC-PEG was given at 2,500 IU/m2 every 3 weeks, and pegaspargase was given at 2,500 IU/m2 every 2 weeks.
Either asparaginase product was given as part of a 4-week induction regimen (vincristine, prednisone, doxorubicin, and methotrexate), a 3-week intensification regimen (intrathecal chemotherapy with or without radiotherapy) for central nervous system disease, and a 27-week second consolidation regimen (mercaptopurine, methotrexate, and, in high-risk patients, doxorubicin).
SAA
The researchers observed significantly longer SAA with SC-PEG during induction but not after.
During induction, at 25 days after the first asparaginase dose, 88% of patients on SC-PEG and 17% of those on pegaspargase had SAA of at least 0.10 IU/mL (P less than .001). Post-induction, at week 25, 100% of patients in each group had a nadir SAA of at least 0.10 IU/mL.
“The high nadir serum asparaginase activity levels observed for both preparations suggest dosing strategies could be further optimized,” Dr. Vrooman noted.
Safety
There were no significant differences in adverse events between the SC-PEG and pegaspargase arms during or after induction.
Adverse events during induction (in the SC-PEG and pegaspargase arms, respectively) included grade 2 or higher asparaginase allergy (0% and 1%), grade 2 or higher pancreatitis (3% in both), grade 2 or higher thrombosis (3% and 9%), grade 4 hyperbilirubinemia (3% and 1%), grade 3 or higher bacterial infection (12% and 9%), and grade 3 or higher fungal infection (4% and 5%).
Adverse events after induction (in the SC-PEG and pegaspargase arms, respectively) included grade 2 or higher asparaginase allergy (17% and 14%), grade 2 or higher pancreatitis (15% in both), grade 2 or higher thrombosis (18% and 13%), grade 4 hyperbilirubinemia (4% and 3%), grade 3 or higher bacterial infection (12% and 15%), grade 3 or higher fungal infection (2% and 1%), grade 2 or higher bone fracture (3% and 8%), and grade 2 or higher osteonecrosis (3% and 4%).
Response and survival
The complete response rate was 95% (109/115) in the SC-PEG arm and 99% (114/115) in the pegaspargase arm. Rates of induction failure were 3% (n = 4) and 1% (n = 1), respectively, and rates of relapse were 3% (n = 5) and 8% (n = 10), respectively.
There were two induction deaths and two remission deaths in the SC-PEG arm but no induction or remission deaths in the pegaspargase arm.
The median follow-up was 4 years. The 4-year event-free survival rate was 87.7% with SC-PEG and 90.2% with pegaspargase (P = .78). The 4-year overall survival rate was 94.8% and 95.6%, respectively (P = .74).
In closing, Dr. Vrooman said these data suggest SC-PEG provides similar results as standard pegaspargase. She noted that these data informed the U.S. approval of SC-PEG for pediatric and young adult ALL.
This trial was sponsored by the Dana-Farber Cancer Institute in collaboration with Shire and the National Cancer Institute. Dr. Vrooman said she had no relationships to disclose.
SOURCE: Vrooman LM et al. ASCO 2019. Abstract 10006.
CHICAGO – Calaspargase pegol (SC-PEG) produces similar outcomes as standard pegaspargase in pediatric and young adult patients with newly diagnosed acute lymphoblastic leukemia (ALL) or lymphoblastic lymphoma (LL), according to a phase 2 trial.
Patients who received SC-PEG every 3 weeks had similar serum asparaginase activity (SAA), toxicities, and survival rates as patients who received standard pegaspargase every 2 weeks.
Lynda M. Vrooman, MD, of Dana-Farber Cancer Institute in Boston, presented these results at the annual meeting of the American Society of Clinical Oncology.
The trial (NCT01574274) enrolled 239 patients, 230 with ALL and 9 with LL. Most patients had B-cell (n = 207) disease. The patients’ median age was 5.2 years (range, 1.0-20.9 years).
“There were no differences in presenting features by randomization,” Dr. Vrooman noted.
The patients were randomized to receive pegaspargase (n = 120) or SC-PEG (n = 119), a pegylated asparaginase formulation with longer half-life. SC-PEG was given at 2,500 IU/m2 every 3 weeks, and pegaspargase was given at 2,500 IU/m2 every 2 weeks.
Either asparaginase product was given as part of a 4-week induction regimen (vincristine, prednisone, doxorubicin, and methotrexate), a 3-week intensification regimen (intrathecal chemotherapy with or without radiotherapy) for central nervous system disease, and a 27-week second consolidation regimen (mercaptopurine, methotrexate, and, in high-risk patients, doxorubicin).
SAA
The researchers observed significantly longer SAA with SC-PEG during induction but not after.
During induction, at 25 days after the first asparaginase dose, 88% of patients on SC-PEG and 17% of those on pegaspargase had SAA of at least 0.10 IU/mL (P less than .001). Post-induction, at week 25, 100% of patients in each group had a nadir SAA of at least 0.10 IU/mL.
“The high nadir serum asparaginase activity levels observed for both preparations suggest dosing strategies could be further optimized,” Dr. Vrooman noted.
Safety
There were no significant differences in adverse events between the SC-PEG and pegaspargase arms during or after induction.
Adverse events during induction (in the SC-PEG and pegaspargase arms, respectively) included grade 2 or higher asparaginase allergy (0% and 1%), grade 2 or higher pancreatitis (3% in both), grade 2 or higher thrombosis (3% and 9%), grade 4 hyperbilirubinemia (3% and 1%), grade 3 or higher bacterial infection (12% and 9%), and grade 3 or higher fungal infection (4% and 5%).
Adverse events after induction (in the SC-PEG and pegaspargase arms, respectively) included grade 2 or higher asparaginase allergy (17% and 14%), grade 2 or higher pancreatitis (15% in both), grade 2 or higher thrombosis (18% and 13%), grade 4 hyperbilirubinemia (4% and 3%), grade 3 or higher bacterial infection (12% and 15%), grade 3 or higher fungal infection (2% and 1%), grade 2 or higher bone fracture (3% and 8%), and grade 2 or higher osteonecrosis (3% and 4%).
Response and survival
The complete response rate was 95% (109/115) in the SC-PEG arm and 99% (114/115) in the pegaspargase arm. Rates of induction failure were 3% (n = 4) and 1% (n = 1), respectively, and rates of relapse were 3% (n = 5) and 8% (n = 10), respectively.
There were two induction deaths and two remission deaths in the SC-PEG arm but no induction or remission deaths in the pegaspargase arm.
The median follow-up was 4 years. The 4-year event-free survival rate was 87.7% with SC-PEG and 90.2% with pegaspargase (P = .78). The 4-year overall survival rate was 94.8% and 95.6%, respectively (P = .74).
In closing, Dr. Vrooman said these data suggest SC-PEG provides similar results as standard pegaspargase. She noted that these data informed the U.S. approval of SC-PEG for pediatric and young adult ALL.
This trial was sponsored by the Dana-Farber Cancer Institute in collaboration with Shire and the National Cancer Institute. Dr. Vrooman said she had no relationships to disclose.
SOURCE: Vrooman LM et al. ASCO 2019. Abstract 10006.
REPORTING FROM ASCO 2019
FDA opts not to ban textured breast implants
The Food and Drug Administration decided to continue to allow U.S. sales of textured breast implants, which have been identified as the cause of a rare but significant cancer, breast implant–associated anaplastic large cell lymphoma.

A statement the agency released on May 2 said “The FDA does not believe that, on the basis of available data and information, the device [textured implants] meets the banning standard set forth in the Federal Food and Drug Cosmetic Act.” roughly half of them in the United States.
In coming to this decision, following 2 days of public testimony and discussions by an advisory committee in late March, the FDA is bucking the path taken by regulatory bodies of the European Union as well as several other counties. The EU acted in December 2018 to produce the equivalent of a ban on sales of textured breast implants marketed by Allergan. Then in April 2019, the French drug and device regulatory agency expanded this ban to textured breast implants sold by five other companies.
During the FDA advisory committee meeting in March, one of the world’s experts on BIA-ALCL, Mark W. Clemens, MD, a plastic surgeon at MD Anderson Cancer Center in Houston, said that of about 500 case reports received by the FDA, not one had involved a confirmed and “pure” episode of BIA-ALCL linked with a smooth breast implant. A team of experts recently reached the same conclusion when reviewing the reported worldwide incidence of BIA-ALCL in a published review (Plast Reconstr Surg. 2019 March;143[3S]:30S-40S).
Despite these reports, the FDA said in its new statement that “While the majority of women who develop BIA-ALCL have had textured implants, there are known cases in women with smooth-surface breast implants, and many reports do not include the surface texture of the implant at the time of diagnosis.” The agency added that it is “focused on strengthening the evidence generated to help inform future regulatory action.” During the March advisory committee meeting, some members of the panel spoke against a marketing ban on textured implants for reasons such as the modest number of reported cases and because of the importance of having a textured implant option available.
The FDA took several other notable steps in its May 2 statement:
The agency formally acknowledged that many breast implant recipients have reported experiencing adverse effects that include chronic fatigue, cognitive issues, and joint and muscle pain. “While the FDA doesn’t have definitive evidence demonstrating breast implants cause these symptoms, the current evidence supports that some women experience systemic symptoms that may resolve when their breast implants are removed.” The agency also cited the term that patients have coined for these symptoms: Breast Implant Illness.
The FDA made a commitment to “take steps to improve the information available to women and health care professionals about the risks of breast implants,” including the risk for BIA-ALCL, the increased risk for this cancer with textured implants, and the risk for systemic symptoms. The agency said it would work with stakeholders on possible changes to breast implant labeling, including a possible boxed warning, and a patient-decision checklist.
The FDA announced a change in how manufacturers will file medical device reports for breast implants. The agency will no longer allow these filings to be “summary” reports and will instead require manufacturers to file full individual medical device reports for each case that will be publicly available, with the intent to make reporting more transparent and complete.
Finally, the FDA announced that it would partner with two U.S. breast implant registries, the PROFILE registry of BIA-ALCL cases, and the National Breast Implant Registry, both run by the Plastic Surgery Foundation.
The FDA did not address in its statement other issues that came up during the March advisory committee hearings, including a panel recommendation to change follow-up imaging from MRI to ultrasound for monitoring women with implants for rupture, and the extensive, off-label use of surgical mesh during breast implant surgery.
The Food and Drug Administration decided to continue to allow U.S. sales of textured breast implants, which have been identified as the cause of a rare but significant cancer, breast implant–associated anaplastic large cell lymphoma.

A statement the agency released on May 2 said “The FDA does not believe that, on the basis of available data and information, the device [textured implants] meets the banning standard set forth in the Federal Food and Drug Cosmetic Act.” roughly half of them in the United States.
In coming to this decision, following 2 days of public testimony and discussions by an advisory committee in late March, the FDA is bucking the path taken by regulatory bodies of the European Union as well as several other counties. The EU acted in December 2018 to produce the equivalent of a ban on sales of textured breast implants marketed by Allergan. Then in April 2019, the French drug and device regulatory agency expanded this ban to textured breast implants sold by five other companies.
During the FDA advisory committee meeting in March, one of the world’s experts on BIA-ALCL, Mark W. Clemens, MD, a plastic surgeon at MD Anderson Cancer Center in Houston, said that of about 500 case reports received by the FDA, not one had involved a confirmed and “pure” episode of BIA-ALCL linked with a smooth breast implant. A team of experts recently reached the same conclusion when reviewing the reported worldwide incidence of BIA-ALCL in a published review (Plast Reconstr Surg. 2019 March;143[3S]:30S-40S).
Despite these reports, the FDA said in its new statement that “While the majority of women who develop BIA-ALCL have had textured implants, there are known cases in women with smooth-surface breast implants, and many reports do not include the surface texture of the implant at the time of diagnosis.” The agency added that it is “focused on strengthening the evidence generated to help inform future regulatory action.” During the March advisory committee meeting, some members of the panel spoke against a marketing ban on textured implants for reasons such as the modest number of reported cases and because of the importance of having a textured implant option available.
The FDA took several other notable steps in its May 2 statement:
The agency formally acknowledged that many breast implant recipients have reported experiencing adverse effects that include chronic fatigue, cognitive issues, and joint and muscle pain. “While the FDA doesn’t have definitive evidence demonstrating breast implants cause these symptoms, the current evidence supports that some women experience systemic symptoms that may resolve when their breast implants are removed.” The agency also cited the term that patients have coined for these symptoms: Breast Implant Illness.
The FDA made a commitment to “take steps to improve the information available to women and health care professionals about the risks of breast implants,” including the risk for BIA-ALCL, the increased risk for this cancer with textured implants, and the risk for systemic symptoms. The agency said it would work with stakeholders on possible changes to breast implant labeling, including a possible boxed warning, and a patient-decision checklist.
The FDA announced a change in how manufacturers will file medical device reports for breast implants. The agency will no longer allow these filings to be “summary” reports and will instead require manufacturers to file full individual medical device reports for each case that will be publicly available, with the intent to make reporting more transparent and complete.
Finally, the FDA announced that it would partner with two U.S. breast implant registries, the PROFILE registry of BIA-ALCL cases, and the National Breast Implant Registry, both run by the Plastic Surgery Foundation.
The FDA did not address in its statement other issues that came up during the March advisory committee hearings, including a panel recommendation to change follow-up imaging from MRI to ultrasound for monitoring women with implants for rupture, and the extensive, off-label use of surgical mesh during breast implant surgery.
The Food and Drug Administration decided to continue to allow U.S. sales of textured breast implants, which have been identified as the cause of a rare but significant cancer, breast implant–associated anaplastic large cell lymphoma.

A statement the agency released on May 2 said “The FDA does not believe that, on the basis of available data and information, the device [textured implants] meets the banning standard set forth in the Federal Food and Drug Cosmetic Act.” roughly half of them in the United States.
In coming to this decision, following 2 days of public testimony and discussions by an advisory committee in late March, the FDA is bucking the path taken by regulatory bodies of the European Union as well as several other counties. The EU acted in December 2018 to produce the equivalent of a ban on sales of textured breast implants marketed by Allergan. Then in April 2019, the French drug and device regulatory agency expanded this ban to textured breast implants sold by five other companies.
During the FDA advisory committee meeting in March, one of the world’s experts on BIA-ALCL, Mark W. Clemens, MD, a plastic surgeon at MD Anderson Cancer Center in Houston, said that of about 500 case reports received by the FDA, not one had involved a confirmed and “pure” episode of BIA-ALCL linked with a smooth breast implant. A team of experts recently reached the same conclusion when reviewing the reported worldwide incidence of BIA-ALCL in a published review (Plast Reconstr Surg. 2019 March;143[3S]:30S-40S).
Despite these reports, the FDA said in its new statement that “While the majority of women who develop BIA-ALCL have had textured implants, there are known cases in women with smooth-surface breast implants, and many reports do not include the surface texture of the implant at the time of diagnosis.” The agency added that it is “focused on strengthening the evidence generated to help inform future regulatory action.” During the March advisory committee meeting, some members of the panel spoke against a marketing ban on textured implants for reasons such as the modest number of reported cases and because of the importance of having a textured implant option available.
The FDA took several other notable steps in its May 2 statement:
The agency formally acknowledged that many breast implant recipients have reported experiencing adverse effects that include chronic fatigue, cognitive issues, and joint and muscle pain. “While the FDA doesn’t have definitive evidence demonstrating breast implants cause these symptoms, the current evidence supports that some women experience systemic symptoms that may resolve when their breast implants are removed.” The agency also cited the term that patients have coined for these symptoms: Breast Implant Illness.
The FDA made a commitment to “take steps to improve the information available to women and health care professionals about the risks of breast implants,” including the risk for BIA-ALCL, the increased risk for this cancer with textured implants, and the risk for systemic symptoms. The agency said it would work with stakeholders on possible changes to breast implant labeling, including a possible boxed warning, and a patient-decision checklist.
The FDA announced a change in how manufacturers will file medical device reports for breast implants. The agency will no longer allow these filings to be “summary” reports and will instead require manufacturers to file full individual medical device reports for each case that will be publicly available, with the intent to make reporting more transparent and complete.
Finally, the FDA announced that it would partner with two U.S. breast implant registries, the PROFILE registry of BIA-ALCL cases, and the National Breast Implant Registry, both run by the Plastic Surgery Foundation.
The FDA did not address in its statement other issues that came up during the March advisory committee hearings, including a panel recommendation to change follow-up imaging from MRI to ultrasound for monitoring women with implants for rupture, and the extensive, off-label use of surgical mesh during breast implant surgery.
Monitoring, early intervention key to CAR T safety
GLASGOW – Constant patient monitoring and early intervention with tocilizumab and steroids are essential to the safe delivery of chimeric antigen receptor (CAR) T-cell therapy in patients with non-Hodgkin lymphoma (NHL), according to a leading expert.
As a clinical researcher at MD Anderson Cancer Center in Houston, Loretta Nastoupil, MD has played an active role in the evolution of CAR T-cell therapy, from early trials to ongoing development of treatment protocols. During a presentation at the annual meeting of the British Society for Haematology, Dr. Nastoupil discussed leading topics in CAR T-cell therapy, with an emphasis on safe delivery.
“[Toxicity] is something we don’t talk about as much as we should, partly because this therapy works and it’s really exciting,” Dr. Nastoupil said. “But the toxicity is not something that I minimize, and it’s very challenging. It’s led us to restructure our inpatient services. It’s led to a lot of sleepless nights. These patients can do very, very well, or they can do very, very poorly in terms of toxicity and I think the most important strategy is recognition and early intervention.”
Monitoring
Early recognition depends on close monitoring, Dr. Nastoupil said, which is carried out by highly trained nursing staff who follow therapy-specific decision algorithms.
“We have nurses that are on the front line,” Dr. Nastoupil said. “They’re the most important group. We have staff that round on [patients] daily, but the nurses are there 24 hours a day. We have a flow sheet where they grade cytokine release syndrome and neurotoxicity every 8 hours, or if there is an acute change in symptoms or toxicity, they’ll do it in real time.”
Dr. Nastoupil said that if these toxicities are detected, intervention is occurring sooner than it did with some of the first patients to receive CAR-T cell therapy.
“Initially there was a lot of fear surrounding anything that would abort the CAR-T cell therapy,” Dr. Nastoupil said. “There was concern that if you were trying to mitigate some of the toxicity you might have a negative impact on efficacy ... [W]ith the first iteration of studies, generally we were waiting until grade 3 or higher cytokine release syndrome before initiating either tocilizumab and/or steroids. As the studies evolved, it started to move into grade 2 toxicity that we started using therapy, mostly because we started to see that those patients were still responding.”
At MD Anderson, these earlier interventions have decreased severity of adverse events.
“It’s rare nowadays to have grade 3 or 4 cytokine release syndrome because we are generally introducing abortive therapy at grade 2,” Dr. Nastoupil said, citing increased use of steroids and tocilizumab.
Currently, no consensus exists for managing these events, partly because clinicians are still learning about best management practices.
“There will be a consensus on management,” Dr. Nastoupil said. “I think that’s needed. The problem is, it will probably evolve as we get more experience with managing these patients. I think there’s been a little hesitation to put something out on paper knowing that a year from now that might change.”
Grading toxicity
In contrast, Dr. Nastoupil said that a consensus has been reached for grading acute toxicity. Of note, fever is now considered an essential element of cytokine release syndrome.
“The first thing we see [with cytokine release syndrome] is fever, generally speaking,” Dr. Nastoupil said. “That will prompt a workup for infection because these patients are going to be neutropenic. And we initiate broad spectrum antimicrobials.”
She said that some patients treated with CAR T-cell therapy have had disseminated fungal infections, so clinicians need to be on the lookout for septic shock.
To assess neurotoxicity, the team at MD Anderson uses an objective scoring system, called “CARTOX.” This helps maintain consistency when facing broadly different neurological presentations.
“There’s such a wide ranging spectrum of patients that are undergoing neurotoxicity you can’t expect someone, even myself, to be consistent when you are trying to tease out how serious it is,” Dr. Nastoupil said.
With CARTOX, nurses can easily score patients and call clinicians with results. Still, this doesn’t eliminate difficulties inherent to managing neurotoxicity, particularly when it is severe.
“I’d say one of the areas that is still very challenging is when [patients with neurotoxicity] are no longer responding,” Dr. Nastoupil said. “You have to be very mindful of seizure activity. We’ve had a couple of patients with status [epilepticus]. You don’t see seizure activity physically, but when you do an EEG, you pick it up.”
Dr. Nastoupil added that most centers are now giving patients prophylactic levetiracetam (Keppra) to lower seizure risk.
Choosing therapy
When selecting between the two therapies currently approved by the Food and Drug Administration – tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta) – based on safety, Dr. Nastoupil said that rates of cytokine release syndrome appear similar, but neurotoxicity rates may differ.
“Cytokine release syndrome in my opinion is probably more similar than different in terms of grade 3 or higher because tocilizumab and steroids work quite well in aborting those toxicities,” Dr. Nastoupil said. “But neurotoxicity still sticks out in my mind as the most striking difference, where with axicabtagene you see more grade 3 or higher neurotoxicity, though very, very few deaths as a result of this. But it’s very challenging in terms of management.”
According to Dr. Nastoupil, comparisons between CAR T-cell therapies have been complicated by differences in clinical trial methodologies. However, she offered a general conclusion regarding efficacy.
“[W]hat I’ll tell you, at the end of the day, is [that existing CAR T-cell therapies] all seem to sort of settle out around 30%-40% in terms of durable responses,” Dr. Nastoupil said.
Dr. Nastoupil concluded her presentation with an overview and look to the future.
“I do think [CAR T-cell therapy] is transformative, particularly for our chemo refractory patients,” she said. “There is nothing else like it. The problem right now is that it is only durable in 40% of patients. So can we be better at selecting out patients that are more likely to respond? Does introducing this in earlier lines of therapy increase that fraction of patients that are potentially cured?”
Considering these questions, she said: “We need more patients. We need more data. We need longer follow-up to understand the nuances of this therapy.”
Dr. Nastoupil previously reported financial relationships with Celgene, Genentech, Gilead, Merck, Novartis, Spectrum, and TG Therapeutics.
GLASGOW – Constant patient monitoring and early intervention with tocilizumab and steroids are essential to the safe delivery of chimeric antigen receptor (CAR) T-cell therapy in patients with non-Hodgkin lymphoma (NHL), according to a leading expert.
As a clinical researcher at MD Anderson Cancer Center in Houston, Loretta Nastoupil, MD has played an active role in the evolution of CAR T-cell therapy, from early trials to ongoing development of treatment protocols. During a presentation at the annual meeting of the British Society for Haematology, Dr. Nastoupil discussed leading topics in CAR T-cell therapy, with an emphasis on safe delivery.
“[Toxicity] is something we don’t talk about as much as we should, partly because this therapy works and it’s really exciting,” Dr. Nastoupil said. “But the toxicity is not something that I minimize, and it’s very challenging. It’s led us to restructure our inpatient services. It’s led to a lot of sleepless nights. These patients can do very, very well, or they can do very, very poorly in terms of toxicity and I think the most important strategy is recognition and early intervention.”
Monitoring
Early recognition depends on close monitoring, Dr. Nastoupil said, which is carried out by highly trained nursing staff who follow therapy-specific decision algorithms.
“We have nurses that are on the front line,” Dr. Nastoupil said. “They’re the most important group. We have staff that round on [patients] daily, but the nurses are there 24 hours a day. We have a flow sheet where they grade cytokine release syndrome and neurotoxicity every 8 hours, or if there is an acute change in symptoms or toxicity, they’ll do it in real time.”
Dr. Nastoupil said that if these toxicities are detected, intervention is occurring sooner than it did with some of the first patients to receive CAR-T cell therapy.
“Initially there was a lot of fear surrounding anything that would abort the CAR-T cell therapy,” Dr. Nastoupil said. “There was concern that if you were trying to mitigate some of the toxicity you might have a negative impact on efficacy ... [W]ith the first iteration of studies, generally we were waiting until grade 3 or higher cytokine release syndrome before initiating either tocilizumab and/or steroids. As the studies evolved, it started to move into grade 2 toxicity that we started using therapy, mostly because we started to see that those patients were still responding.”
At MD Anderson, these earlier interventions have decreased severity of adverse events.
“It’s rare nowadays to have grade 3 or 4 cytokine release syndrome because we are generally introducing abortive therapy at grade 2,” Dr. Nastoupil said, citing increased use of steroids and tocilizumab.
Currently, no consensus exists for managing these events, partly because clinicians are still learning about best management practices.
“There will be a consensus on management,” Dr. Nastoupil said. “I think that’s needed. The problem is, it will probably evolve as we get more experience with managing these patients. I think there’s been a little hesitation to put something out on paper knowing that a year from now that might change.”
Grading toxicity
In contrast, Dr. Nastoupil said that a consensus has been reached for grading acute toxicity. Of note, fever is now considered an essential element of cytokine release syndrome.
“The first thing we see [with cytokine release syndrome] is fever, generally speaking,” Dr. Nastoupil said. “That will prompt a workup for infection because these patients are going to be neutropenic. And we initiate broad spectrum antimicrobials.”
She said that some patients treated with CAR T-cell therapy have had disseminated fungal infections, so clinicians need to be on the lookout for septic shock.
To assess neurotoxicity, the team at MD Anderson uses an objective scoring system, called “CARTOX.” This helps maintain consistency when facing broadly different neurological presentations.
“There’s such a wide ranging spectrum of patients that are undergoing neurotoxicity you can’t expect someone, even myself, to be consistent when you are trying to tease out how serious it is,” Dr. Nastoupil said.
With CARTOX, nurses can easily score patients and call clinicians with results. Still, this doesn’t eliminate difficulties inherent to managing neurotoxicity, particularly when it is severe.
“I’d say one of the areas that is still very challenging is when [patients with neurotoxicity] are no longer responding,” Dr. Nastoupil said. “You have to be very mindful of seizure activity. We’ve had a couple of patients with status [epilepticus]. You don’t see seizure activity physically, but when you do an EEG, you pick it up.”
Dr. Nastoupil added that most centers are now giving patients prophylactic levetiracetam (Keppra) to lower seizure risk.
Choosing therapy
When selecting between the two therapies currently approved by the Food and Drug Administration – tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta) – based on safety, Dr. Nastoupil said that rates of cytokine release syndrome appear similar, but neurotoxicity rates may differ.
“Cytokine release syndrome in my opinion is probably more similar than different in terms of grade 3 or higher because tocilizumab and steroids work quite well in aborting those toxicities,” Dr. Nastoupil said. “But neurotoxicity still sticks out in my mind as the most striking difference, where with axicabtagene you see more grade 3 or higher neurotoxicity, though very, very few deaths as a result of this. But it’s very challenging in terms of management.”
According to Dr. Nastoupil, comparisons between CAR T-cell therapies have been complicated by differences in clinical trial methodologies. However, she offered a general conclusion regarding efficacy.
“[W]hat I’ll tell you, at the end of the day, is [that existing CAR T-cell therapies] all seem to sort of settle out around 30%-40% in terms of durable responses,” Dr. Nastoupil said.
Dr. Nastoupil concluded her presentation with an overview and look to the future.
“I do think [CAR T-cell therapy] is transformative, particularly for our chemo refractory patients,” she said. “There is nothing else like it. The problem right now is that it is only durable in 40% of patients. So can we be better at selecting out patients that are more likely to respond? Does introducing this in earlier lines of therapy increase that fraction of patients that are potentially cured?”
Considering these questions, she said: “We need more patients. We need more data. We need longer follow-up to understand the nuances of this therapy.”
Dr. Nastoupil previously reported financial relationships with Celgene, Genentech, Gilead, Merck, Novartis, Spectrum, and TG Therapeutics.
GLASGOW – Constant patient monitoring and early intervention with tocilizumab and steroids are essential to the safe delivery of chimeric antigen receptor (CAR) T-cell therapy in patients with non-Hodgkin lymphoma (NHL), according to a leading expert.
As a clinical researcher at MD Anderson Cancer Center in Houston, Loretta Nastoupil, MD has played an active role in the evolution of CAR T-cell therapy, from early trials to ongoing development of treatment protocols. During a presentation at the annual meeting of the British Society for Haematology, Dr. Nastoupil discussed leading topics in CAR T-cell therapy, with an emphasis on safe delivery.
“[Toxicity] is something we don’t talk about as much as we should, partly because this therapy works and it’s really exciting,” Dr. Nastoupil said. “But the toxicity is not something that I minimize, and it’s very challenging. It’s led us to restructure our inpatient services. It’s led to a lot of sleepless nights. These patients can do very, very well, or they can do very, very poorly in terms of toxicity and I think the most important strategy is recognition and early intervention.”
Monitoring
Early recognition depends on close monitoring, Dr. Nastoupil said, which is carried out by highly trained nursing staff who follow therapy-specific decision algorithms.
“We have nurses that are on the front line,” Dr. Nastoupil said. “They’re the most important group. We have staff that round on [patients] daily, but the nurses are there 24 hours a day. We have a flow sheet where they grade cytokine release syndrome and neurotoxicity every 8 hours, or if there is an acute change in symptoms or toxicity, they’ll do it in real time.”
Dr. Nastoupil said that if these toxicities are detected, intervention is occurring sooner than it did with some of the first patients to receive CAR-T cell therapy.
“Initially there was a lot of fear surrounding anything that would abort the CAR-T cell therapy,” Dr. Nastoupil said. “There was concern that if you were trying to mitigate some of the toxicity you might have a negative impact on efficacy ... [W]ith the first iteration of studies, generally we were waiting until grade 3 or higher cytokine release syndrome before initiating either tocilizumab and/or steroids. As the studies evolved, it started to move into grade 2 toxicity that we started using therapy, mostly because we started to see that those patients were still responding.”
At MD Anderson, these earlier interventions have decreased severity of adverse events.
“It’s rare nowadays to have grade 3 or 4 cytokine release syndrome because we are generally introducing abortive therapy at grade 2,” Dr. Nastoupil said, citing increased use of steroids and tocilizumab.
Currently, no consensus exists for managing these events, partly because clinicians are still learning about best management practices.
“There will be a consensus on management,” Dr. Nastoupil said. “I think that’s needed. The problem is, it will probably evolve as we get more experience with managing these patients. I think there’s been a little hesitation to put something out on paper knowing that a year from now that might change.”
Grading toxicity
In contrast, Dr. Nastoupil said that a consensus has been reached for grading acute toxicity. Of note, fever is now considered an essential element of cytokine release syndrome.
“The first thing we see [with cytokine release syndrome] is fever, generally speaking,” Dr. Nastoupil said. “That will prompt a workup for infection because these patients are going to be neutropenic. And we initiate broad spectrum antimicrobials.”
She said that some patients treated with CAR T-cell therapy have had disseminated fungal infections, so clinicians need to be on the lookout for septic shock.
To assess neurotoxicity, the team at MD Anderson uses an objective scoring system, called “CARTOX.” This helps maintain consistency when facing broadly different neurological presentations.
“There’s such a wide ranging spectrum of patients that are undergoing neurotoxicity you can’t expect someone, even myself, to be consistent when you are trying to tease out how serious it is,” Dr. Nastoupil said.
With CARTOX, nurses can easily score patients and call clinicians with results. Still, this doesn’t eliminate difficulties inherent to managing neurotoxicity, particularly when it is severe.
“I’d say one of the areas that is still very challenging is when [patients with neurotoxicity] are no longer responding,” Dr. Nastoupil said. “You have to be very mindful of seizure activity. We’ve had a couple of patients with status [epilepticus]. You don’t see seizure activity physically, but when you do an EEG, you pick it up.”
Dr. Nastoupil added that most centers are now giving patients prophylactic levetiracetam (Keppra) to lower seizure risk.
Choosing therapy
When selecting between the two therapies currently approved by the Food and Drug Administration – tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta) – based on safety, Dr. Nastoupil said that rates of cytokine release syndrome appear similar, but neurotoxicity rates may differ.
“Cytokine release syndrome in my opinion is probably more similar than different in terms of grade 3 or higher because tocilizumab and steroids work quite well in aborting those toxicities,” Dr. Nastoupil said. “But neurotoxicity still sticks out in my mind as the most striking difference, where with axicabtagene you see more grade 3 or higher neurotoxicity, though very, very few deaths as a result of this. But it’s very challenging in terms of management.”
According to Dr. Nastoupil, comparisons between CAR T-cell therapies have been complicated by differences in clinical trial methodologies. However, she offered a general conclusion regarding efficacy.
“[W]hat I’ll tell you, at the end of the day, is [that existing CAR T-cell therapies] all seem to sort of settle out around 30%-40% in terms of durable responses,” Dr. Nastoupil said.
Dr. Nastoupil concluded her presentation with an overview and look to the future.
“I do think [CAR T-cell therapy] is transformative, particularly for our chemo refractory patients,” she said. “There is nothing else like it. The problem right now is that it is only durable in 40% of patients. So can we be better at selecting out patients that are more likely to respond? Does introducing this in earlier lines of therapy increase that fraction of patients that are potentially cured?”
Considering these questions, she said: “We need more patients. We need more data. We need longer follow-up to understand the nuances of this therapy.”
Dr. Nastoupil previously reported financial relationships with Celgene, Genentech, Gilead, Merck, Novartis, Spectrum, and TG Therapeutics.
EXPERT ANALYSIS FROM BSH 2019