User login
Survival for older AML patients better with HSCT from unrelated donors
For adults aged 50 and older in first or second remission after induction therapy for acute myeloid leukemia, hematopoietic stem cell transplants (HSCT) from young matched unrelated donors was associated with better overall survival and lower risk for relapse than transplants from haploidentical donors, a retrospective study suggests,
Among 823 patients from the aged 50 to 75 with acute myeloid leukemia (AML) in a transplant registry, hazard ratios for both mortality and relapse were significantly higher for patients who received transplants from haploidentical siblings or offspring, compared with patients who received transplants from HLA-matched unrelated donors aged 40 or younger, reported Miguel-Angel Perales, MD, who is affiliated with Memorial Sloan Kettering Cancer Center in New York City, and colleagues.
“Our findings lend support to our hypothesis that a young [matched unrelated donor] should be the donor of choice when available. Furthermore, the data presented here suggest comparable times to transplantation in both treatment groups, confirming timely access to unrelated donors is no longer a barrier,” they wrote in Haematologica.Allogeneic transplants from matched unrelated donors have been performed for more than 30 years for treatment of patients with advanced myeloid and lymphoid malignancies. More recently, T-cell-replete bone marrow or peripheral blood transplants from haploidentical relatives, with post-transplant cyclophosphamide, tacrolimus, and mycophenolate mofetil to lower risk for graft-versus-host disease (GvHD) have become commonplace worldwide, and are established treatment options for patients with myeloid and lymphoid malignancies. There are conflicting studies suggesting that outcomes with haploidentical transplants are equivalent or superior to those seen with matched unrelated donors, the authors noted, but pointed to a 2018 study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplant and the Center for International Blood and Marrow Transplant Research (CIBMTR). Those study results found that, among transplant recipients aged 55 through 76, graft failure, nonrelapse mortality, and overall mortality were higher when the donors were haploidentical offspring rather than HLA-matched siblings.
To see whether patients aged 50 and older with AML might benefit more with transplants from hapolidentical relatives or matched unrelated donors, the investigators used CIBMTR data to review outcomes for 823 adults with AML who received a transplant in first or second remission at one of 90 U.S. centers from 2008 through 2015.
Of this cohort, 192 patients received grafts from haploidentical donors (25% from siblings and 75% from offspring), and 631 received grafts from matched unrelated donors ranging from 18 to 40 years of age.
Although the two groups were generally similar in demographic and disease characteristics, patients in the matched unrelated donor group had significantly higher frequency of poor-risk cytogenetics (P = .03) and were significantly more likely to have received a myeloablative condition regimen than a reduced-intensity regimen (P less than .001).
In the haploidentical group, 76% of patients were in first complete remission, and the remaining 24% were in second complete remission. In the HLA-matched group the respective proportions were 83% and 17%.
The median follow-up was 42 months in the haploidentical group and 47 months in the HLA-matched group. Five-year overall survival rates were 32% and 42%, respectively.
In multivariable models controlling for donor and recipient age, sex, performance score, hematopoietic cell transplant comorbidity score, cytomegalovirus serostatus, disease status, cytogenetic risk, transplant conditioning regimen intensity and transplant period, the hazard ratio (HR) for the primary endpoint of overall mortality was 1.27 for haploidentical vs. HLA-matched grafts (P = .04). The HR for relapse risk with haploidentical transplants was 1.32 (P =.04). No significant differences in risk of nonrelapse mortality were found between the two study arms.
Bone marrow grafts from matched unrelated donors were associated with significantly higher risk for chronic GvHD than haploidentical grafts (HR, 3.12; P less than .001), but there was no difference in chronic graft-versus-host disease (GvHD) incidence between peripheral blood grafts from matched unrelated donors and haploidentical grafts.
“These data support the view that matched unrelated donor transplant with donors younger than 40 years is to be preferred,” the investigators wrote.
But in an interview, coauthor
“Even though there appears to be that clinical benefit for this older AML patient population, that benefit is not huge, and when you’re also accounting for the process of finding a donor and just getting someone into transplant, a lot of us weren’t sure if this was really going to be practice changing as the field does move into haploidentical transplants being more common,” he said.
He noted that the better outcomes among patients who received transplants from matched unrelated donors may be at least in part explained by the higher proportion of patients with unrelated donors who received myeloablative conditioning regimens. In this study, 65% of patients with haploidentical donors underwent reduced-intensity conditioning with total body irradiation, cyclophosphamide, and fludarabine.“If we do a comparison of equal conditioning regimens, are we really going to see the same outcomes in this setting? This might actually argue that, if you’re going to do a haploidentical transplant, you might start thinking about those newer, more ablative conditioning regimens,” he said.Dr. Tomlinson added that the data are reassuring, because of the modest size of the benefit, and because “many, many of our studies are showing that haploidentical transplants do almost as well as the matched ones. The big question mark will be what are the long-term outcomes? What happens after 3 years from those transplants? And that is going to take a lot more high quality, mature data.”In an editorial accompanying the study, Richard E. Champlin, MD, of the University of Texas MD Anderson Cancer Center in Houston, noted that the more frequent use of reduced-intensity conditioning used for most patients in the haploidentical group has been associated in other studies with higher relapse rates, compared with other, more intense reduced-intensity regimens.
While he agreed that the study by Dr. Perales and colleagues “should give pause for thought, however, for those considering jumping to haploidentical transplants as a preferred approach in general,” he also noted that the study’s conclusion might not apply to cases where time-to-transplant is critical, or when other conditioning and GvHD prophylaxis regimens are used.
“The ideal study would compare optimized versions of both haploidentical and unrelated donor transplants, and use “intention-to-treat” analysis, including all patients for whom a transplant is intended from the time of initial HLA typing,” he wrote.
The study was funded by grants from the National Institutes of Health and the Office of Naval Research. Dr. Tomlinson reported no relevant disclosures. Dr. Champlin did not report disclosures.
SOURCE: Perales M-A et al. Haematologica. 2020 Jan 31;105(2):407-13.
For adults aged 50 and older in first or second remission after induction therapy for acute myeloid leukemia, hematopoietic stem cell transplants (HSCT) from young matched unrelated donors was associated with better overall survival and lower risk for relapse than transplants from haploidentical donors, a retrospective study suggests,
Among 823 patients from the aged 50 to 75 with acute myeloid leukemia (AML) in a transplant registry, hazard ratios for both mortality and relapse were significantly higher for patients who received transplants from haploidentical siblings or offspring, compared with patients who received transplants from HLA-matched unrelated donors aged 40 or younger, reported Miguel-Angel Perales, MD, who is affiliated with Memorial Sloan Kettering Cancer Center in New York City, and colleagues.
“Our findings lend support to our hypothesis that a young [matched unrelated donor] should be the donor of choice when available. Furthermore, the data presented here suggest comparable times to transplantation in both treatment groups, confirming timely access to unrelated donors is no longer a barrier,” they wrote in Haematologica.Allogeneic transplants from matched unrelated donors have been performed for more than 30 years for treatment of patients with advanced myeloid and lymphoid malignancies. More recently, T-cell-replete bone marrow or peripheral blood transplants from haploidentical relatives, with post-transplant cyclophosphamide, tacrolimus, and mycophenolate mofetil to lower risk for graft-versus-host disease (GvHD) have become commonplace worldwide, and are established treatment options for patients with myeloid and lymphoid malignancies. There are conflicting studies suggesting that outcomes with haploidentical transplants are equivalent or superior to those seen with matched unrelated donors, the authors noted, but pointed to a 2018 study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplant and the Center for International Blood and Marrow Transplant Research (CIBMTR). Those study results found that, among transplant recipients aged 55 through 76, graft failure, nonrelapse mortality, and overall mortality were higher when the donors were haploidentical offspring rather than HLA-matched siblings.
To see whether patients aged 50 and older with AML might benefit more with transplants from hapolidentical relatives or matched unrelated donors, the investigators used CIBMTR data to review outcomes for 823 adults with AML who received a transplant in first or second remission at one of 90 U.S. centers from 2008 through 2015.
Of this cohort, 192 patients received grafts from haploidentical donors (25% from siblings and 75% from offspring), and 631 received grafts from matched unrelated donors ranging from 18 to 40 years of age.
Although the two groups were generally similar in demographic and disease characteristics, patients in the matched unrelated donor group had significantly higher frequency of poor-risk cytogenetics (P = .03) and were significantly more likely to have received a myeloablative condition regimen than a reduced-intensity regimen (P less than .001).
In the haploidentical group, 76% of patients were in first complete remission, and the remaining 24% were in second complete remission. In the HLA-matched group the respective proportions were 83% and 17%.
The median follow-up was 42 months in the haploidentical group and 47 months in the HLA-matched group. Five-year overall survival rates were 32% and 42%, respectively.
In multivariable models controlling for donor and recipient age, sex, performance score, hematopoietic cell transplant comorbidity score, cytomegalovirus serostatus, disease status, cytogenetic risk, transplant conditioning regimen intensity and transplant period, the hazard ratio (HR) for the primary endpoint of overall mortality was 1.27 for haploidentical vs. HLA-matched grafts (P = .04). The HR for relapse risk with haploidentical transplants was 1.32 (P =.04). No significant differences in risk of nonrelapse mortality were found between the two study arms.
Bone marrow grafts from matched unrelated donors were associated with significantly higher risk for chronic GvHD than haploidentical grafts (HR, 3.12; P less than .001), but there was no difference in chronic graft-versus-host disease (GvHD) incidence between peripheral blood grafts from matched unrelated donors and haploidentical grafts.
“These data support the view that matched unrelated donor transplant with donors younger than 40 years is to be preferred,” the investigators wrote.
But in an interview, coauthor
“Even though there appears to be that clinical benefit for this older AML patient population, that benefit is not huge, and when you’re also accounting for the process of finding a donor and just getting someone into transplant, a lot of us weren’t sure if this was really going to be practice changing as the field does move into haploidentical transplants being more common,” he said.
He noted that the better outcomes among patients who received transplants from matched unrelated donors may be at least in part explained by the higher proportion of patients with unrelated donors who received myeloablative conditioning regimens. In this study, 65% of patients with haploidentical donors underwent reduced-intensity conditioning with total body irradiation, cyclophosphamide, and fludarabine.“If we do a comparison of equal conditioning regimens, are we really going to see the same outcomes in this setting? This might actually argue that, if you’re going to do a haploidentical transplant, you might start thinking about those newer, more ablative conditioning regimens,” he said.Dr. Tomlinson added that the data are reassuring, because of the modest size of the benefit, and because “many, many of our studies are showing that haploidentical transplants do almost as well as the matched ones. The big question mark will be what are the long-term outcomes? What happens after 3 years from those transplants? And that is going to take a lot more high quality, mature data.”In an editorial accompanying the study, Richard E. Champlin, MD, of the University of Texas MD Anderson Cancer Center in Houston, noted that the more frequent use of reduced-intensity conditioning used for most patients in the haploidentical group has been associated in other studies with higher relapse rates, compared with other, more intense reduced-intensity regimens.
While he agreed that the study by Dr. Perales and colleagues “should give pause for thought, however, for those considering jumping to haploidentical transplants as a preferred approach in general,” he also noted that the study’s conclusion might not apply to cases where time-to-transplant is critical, or when other conditioning and GvHD prophylaxis regimens are used.
“The ideal study would compare optimized versions of both haploidentical and unrelated donor transplants, and use “intention-to-treat” analysis, including all patients for whom a transplant is intended from the time of initial HLA typing,” he wrote.
The study was funded by grants from the National Institutes of Health and the Office of Naval Research. Dr. Tomlinson reported no relevant disclosures. Dr. Champlin did not report disclosures.
SOURCE: Perales M-A et al. Haematologica. 2020 Jan 31;105(2):407-13.
For adults aged 50 and older in first or second remission after induction therapy for acute myeloid leukemia, hematopoietic stem cell transplants (HSCT) from young matched unrelated donors was associated with better overall survival and lower risk for relapse than transplants from haploidentical donors, a retrospective study suggests,
Among 823 patients from the aged 50 to 75 with acute myeloid leukemia (AML) in a transplant registry, hazard ratios for both mortality and relapse were significantly higher for patients who received transplants from haploidentical siblings or offspring, compared with patients who received transplants from HLA-matched unrelated donors aged 40 or younger, reported Miguel-Angel Perales, MD, who is affiliated with Memorial Sloan Kettering Cancer Center in New York City, and colleagues.
“Our findings lend support to our hypothesis that a young [matched unrelated donor] should be the donor of choice when available. Furthermore, the data presented here suggest comparable times to transplantation in both treatment groups, confirming timely access to unrelated donors is no longer a barrier,” they wrote in Haematologica.Allogeneic transplants from matched unrelated donors have been performed for more than 30 years for treatment of patients with advanced myeloid and lymphoid malignancies. More recently, T-cell-replete bone marrow or peripheral blood transplants from haploidentical relatives, with post-transplant cyclophosphamide, tacrolimus, and mycophenolate mofetil to lower risk for graft-versus-host disease (GvHD) have become commonplace worldwide, and are established treatment options for patients with myeloid and lymphoid malignancies. There are conflicting studies suggesting that outcomes with haploidentical transplants are equivalent or superior to those seen with matched unrelated donors, the authors noted, but pointed to a 2018 study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplant and the Center for International Blood and Marrow Transplant Research (CIBMTR). Those study results found that, among transplant recipients aged 55 through 76, graft failure, nonrelapse mortality, and overall mortality were higher when the donors were haploidentical offspring rather than HLA-matched siblings.
To see whether patients aged 50 and older with AML might benefit more with transplants from hapolidentical relatives or matched unrelated donors, the investigators used CIBMTR data to review outcomes for 823 adults with AML who received a transplant in first or second remission at one of 90 U.S. centers from 2008 through 2015.
Of this cohort, 192 patients received grafts from haploidentical donors (25% from siblings and 75% from offspring), and 631 received grafts from matched unrelated donors ranging from 18 to 40 years of age.
Although the two groups were generally similar in demographic and disease characteristics, patients in the matched unrelated donor group had significantly higher frequency of poor-risk cytogenetics (P = .03) and were significantly more likely to have received a myeloablative condition regimen than a reduced-intensity regimen (P less than .001).
In the haploidentical group, 76% of patients were in first complete remission, and the remaining 24% were in second complete remission. In the HLA-matched group the respective proportions were 83% and 17%.
The median follow-up was 42 months in the haploidentical group and 47 months in the HLA-matched group. Five-year overall survival rates were 32% and 42%, respectively.
In multivariable models controlling for donor and recipient age, sex, performance score, hematopoietic cell transplant comorbidity score, cytomegalovirus serostatus, disease status, cytogenetic risk, transplant conditioning regimen intensity and transplant period, the hazard ratio (HR) for the primary endpoint of overall mortality was 1.27 for haploidentical vs. HLA-matched grafts (P = .04). The HR for relapse risk with haploidentical transplants was 1.32 (P =.04). No significant differences in risk of nonrelapse mortality were found between the two study arms.
Bone marrow grafts from matched unrelated donors were associated with significantly higher risk for chronic GvHD than haploidentical grafts (HR, 3.12; P less than .001), but there was no difference in chronic graft-versus-host disease (GvHD) incidence between peripheral blood grafts from matched unrelated donors and haploidentical grafts.
“These data support the view that matched unrelated donor transplant with donors younger than 40 years is to be preferred,” the investigators wrote.
But in an interview, coauthor
“Even though there appears to be that clinical benefit for this older AML patient population, that benefit is not huge, and when you’re also accounting for the process of finding a donor and just getting someone into transplant, a lot of us weren’t sure if this was really going to be practice changing as the field does move into haploidentical transplants being more common,” he said.
He noted that the better outcomes among patients who received transplants from matched unrelated donors may be at least in part explained by the higher proportion of patients with unrelated donors who received myeloablative conditioning regimens. In this study, 65% of patients with haploidentical donors underwent reduced-intensity conditioning with total body irradiation, cyclophosphamide, and fludarabine.“If we do a comparison of equal conditioning regimens, are we really going to see the same outcomes in this setting? This might actually argue that, if you’re going to do a haploidentical transplant, you might start thinking about those newer, more ablative conditioning regimens,” he said.Dr. Tomlinson added that the data are reassuring, because of the modest size of the benefit, and because “many, many of our studies are showing that haploidentical transplants do almost as well as the matched ones. The big question mark will be what are the long-term outcomes? What happens after 3 years from those transplants? And that is going to take a lot more high quality, mature data.”In an editorial accompanying the study, Richard E. Champlin, MD, of the University of Texas MD Anderson Cancer Center in Houston, noted that the more frequent use of reduced-intensity conditioning used for most patients in the haploidentical group has been associated in other studies with higher relapse rates, compared with other, more intense reduced-intensity regimens.
While he agreed that the study by Dr. Perales and colleagues “should give pause for thought, however, for those considering jumping to haploidentical transplants as a preferred approach in general,” he also noted that the study’s conclusion might not apply to cases where time-to-transplant is critical, or when other conditioning and GvHD prophylaxis regimens are used.
“The ideal study would compare optimized versions of both haploidentical and unrelated donor transplants, and use “intention-to-treat” analysis, including all patients for whom a transplant is intended from the time of initial HLA typing,” he wrote.
The study was funded by grants from the National Institutes of Health and the Office of Naval Research. Dr. Tomlinson reported no relevant disclosures. Dr. Champlin did not report disclosures.
SOURCE: Perales M-A et al. Haematologica. 2020 Jan 31;105(2):407-13.
FROM HAEMATOLOGICA
9/11 responders show increased risk of leukemia, other cancers
New data suggest an increased risk of leukemia among responders who worked at the World Trade Center site after the attacks on Sept. 11, 2001.
Previous studies have shown that 9/11 responders have a higher incidence of cancers than does the general population. The current study is the first to show a higher incidence of leukemia among responders. It also shows a higher incidence of thyroid and prostate cancers as well as all cancer types combined.
These findings were published in JNCI Cancer Spectrum.
“This study showed increased incidence of several cancer types compared to previously conducted studies with shorter follow-up periods,” study author Susan L, Teitelbaum, PhD, of the Icahn School of Medicine at Mount Sinai, New York, said in a press release.
“Because of the long latency period of many types of cancer, it is possible that increased rates of other cancers, as well as World Trade Center exposure health issues, may emerge after longer periods of study.”
Dr. Teitelbaum and colleagues evaluated responders enrolled in the World Trade Center Health Program General Responder Cohort from when it was established in July 2002 through the end of follow-up, which was Dec. 31, 2013, for New York residents and Dec. 31, 2012, for residents of other states.
To be eligible for the cohort, responders must have worked on the World Trade Center rescue and recovery effort a minimum of 4 hours in the first 4 days from Sept. 11, 2001, 24 hours in September 2001, or 80 hours from September through December 2001. Responders also had to complete at least one monitoring visit.
Responders’ data were linked to data from cancer registries in New York, New Jersey, Pennsylvania, and Connecticut (where most responders lived at the time of the attacks), as well as Florida and North Carolina (where responders were known to retire). The responders were linked to the registries using probabilistic matching algorithms, which made use of information such as patient name, address, social security number, sex, race, and birth date.
The researchers noted that patients who enrolled in the General Responder Cohort had their cancer certified for federally funded treatment, and this factor might result in “sicker members disproportionately self-selecting into the program.” To reduce this potential bias, the researchers conducted a restricted analysis in which counts of cancer cases and person-years of observation began 6 months after responder enrollment.
The researchers analyzed data on 28,729 responders who primarily worked in protective services (49.0%) and construction (20.8%). Responders spent a median of 52 days on the rescue and recovery effort, and 44.4% of them had some exposure to the dust cloud caused by the collapse of the towers.
In the restricted analysis, there were 1,072 cancers observed in 999 responders. Compared with the general population, responders had a significantly higher incidence of all cancers combined, with a standardized incidence ratio (SIR) of 1.09.
Responders had a significantly higher incidence of prostate cancer (SIR,1.25), thyroid cancer (SIR, 2.19), and leukemia (SIR, 1.41). The leukemia category included acute myeloid leukemia (SIR,1.58) and chronic lymphocytic leukemia (SIR, 1.08).
“Although other studies have revealed elevated SIRs for other hematologic malignancies, this is the first reported, statistically significant, elevated SIR for leukemia,” the researchers wrote. “Leukemia is known to occur after exposure to occupational carcinogens, including benzene (burning jet fuel and other sources at the [World Trade Center] site), possibly at low levels of exposure and with a latency of several years from exposure.”
A multivariate analysis showed no association between cancer incidence and the length of time responders spent on the rescue and recovery effort or the intensity of their exposure to the dust cloud or debris pile.
The analysis did show an elevated risk of all cancers combined with each 1-year increase in responder age (hazard ratio, 1.09), among male responders (HR, 1.21), and among responders who smoked at baseline (HR, 1.29).
This research was supported by the Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. The researchers disclosed no conflicts of interest.
SOURCE: Shapiro MZ et al. JNCI Cancer Spectr. 2020 Jan 14. doi: 10.1093/jncics/pkz090.
New data suggest an increased risk of leukemia among responders who worked at the World Trade Center site after the attacks on Sept. 11, 2001.
Previous studies have shown that 9/11 responders have a higher incidence of cancers than does the general population. The current study is the first to show a higher incidence of leukemia among responders. It also shows a higher incidence of thyroid and prostate cancers as well as all cancer types combined.
These findings were published in JNCI Cancer Spectrum.
“This study showed increased incidence of several cancer types compared to previously conducted studies with shorter follow-up periods,” study author Susan L, Teitelbaum, PhD, of the Icahn School of Medicine at Mount Sinai, New York, said in a press release.
“Because of the long latency period of many types of cancer, it is possible that increased rates of other cancers, as well as World Trade Center exposure health issues, may emerge after longer periods of study.”
Dr. Teitelbaum and colleagues evaluated responders enrolled in the World Trade Center Health Program General Responder Cohort from when it was established in July 2002 through the end of follow-up, which was Dec. 31, 2013, for New York residents and Dec. 31, 2012, for residents of other states.
To be eligible for the cohort, responders must have worked on the World Trade Center rescue and recovery effort a minimum of 4 hours in the first 4 days from Sept. 11, 2001, 24 hours in September 2001, or 80 hours from September through December 2001. Responders also had to complete at least one monitoring visit.
Responders’ data were linked to data from cancer registries in New York, New Jersey, Pennsylvania, and Connecticut (where most responders lived at the time of the attacks), as well as Florida and North Carolina (where responders were known to retire). The responders were linked to the registries using probabilistic matching algorithms, which made use of information such as patient name, address, social security number, sex, race, and birth date.
The researchers noted that patients who enrolled in the General Responder Cohort had their cancer certified for federally funded treatment, and this factor might result in “sicker members disproportionately self-selecting into the program.” To reduce this potential bias, the researchers conducted a restricted analysis in which counts of cancer cases and person-years of observation began 6 months after responder enrollment.
The researchers analyzed data on 28,729 responders who primarily worked in protective services (49.0%) and construction (20.8%). Responders spent a median of 52 days on the rescue and recovery effort, and 44.4% of them had some exposure to the dust cloud caused by the collapse of the towers.
In the restricted analysis, there were 1,072 cancers observed in 999 responders. Compared with the general population, responders had a significantly higher incidence of all cancers combined, with a standardized incidence ratio (SIR) of 1.09.
Responders had a significantly higher incidence of prostate cancer (SIR,1.25), thyroid cancer (SIR, 2.19), and leukemia (SIR, 1.41). The leukemia category included acute myeloid leukemia (SIR,1.58) and chronic lymphocytic leukemia (SIR, 1.08).
“Although other studies have revealed elevated SIRs for other hematologic malignancies, this is the first reported, statistically significant, elevated SIR for leukemia,” the researchers wrote. “Leukemia is known to occur after exposure to occupational carcinogens, including benzene (burning jet fuel and other sources at the [World Trade Center] site), possibly at low levels of exposure and with a latency of several years from exposure.”
A multivariate analysis showed no association between cancer incidence and the length of time responders spent on the rescue and recovery effort or the intensity of their exposure to the dust cloud or debris pile.
The analysis did show an elevated risk of all cancers combined with each 1-year increase in responder age (hazard ratio, 1.09), among male responders (HR, 1.21), and among responders who smoked at baseline (HR, 1.29).
This research was supported by the Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. The researchers disclosed no conflicts of interest.
SOURCE: Shapiro MZ et al. JNCI Cancer Spectr. 2020 Jan 14. doi: 10.1093/jncics/pkz090.
New data suggest an increased risk of leukemia among responders who worked at the World Trade Center site after the attacks on Sept. 11, 2001.
Previous studies have shown that 9/11 responders have a higher incidence of cancers than does the general population. The current study is the first to show a higher incidence of leukemia among responders. It also shows a higher incidence of thyroid and prostate cancers as well as all cancer types combined.
These findings were published in JNCI Cancer Spectrum.
“This study showed increased incidence of several cancer types compared to previously conducted studies with shorter follow-up periods,” study author Susan L, Teitelbaum, PhD, of the Icahn School of Medicine at Mount Sinai, New York, said in a press release.
“Because of the long latency period of many types of cancer, it is possible that increased rates of other cancers, as well as World Trade Center exposure health issues, may emerge after longer periods of study.”
Dr. Teitelbaum and colleagues evaluated responders enrolled in the World Trade Center Health Program General Responder Cohort from when it was established in July 2002 through the end of follow-up, which was Dec. 31, 2013, for New York residents and Dec. 31, 2012, for residents of other states.
To be eligible for the cohort, responders must have worked on the World Trade Center rescue and recovery effort a minimum of 4 hours in the first 4 days from Sept. 11, 2001, 24 hours in September 2001, or 80 hours from September through December 2001. Responders also had to complete at least one monitoring visit.
Responders’ data were linked to data from cancer registries in New York, New Jersey, Pennsylvania, and Connecticut (where most responders lived at the time of the attacks), as well as Florida and North Carolina (where responders were known to retire). The responders were linked to the registries using probabilistic matching algorithms, which made use of information such as patient name, address, social security number, sex, race, and birth date.
The researchers noted that patients who enrolled in the General Responder Cohort had their cancer certified for federally funded treatment, and this factor might result in “sicker members disproportionately self-selecting into the program.” To reduce this potential bias, the researchers conducted a restricted analysis in which counts of cancer cases and person-years of observation began 6 months after responder enrollment.
The researchers analyzed data on 28,729 responders who primarily worked in protective services (49.0%) and construction (20.8%). Responders spent a median of 52 days on the rescue and recovery effort, and 44.4% of them had some exposure to the dust cloud caused by the collapse of the towers.
In the restricted analysis, there were 1,072 cancers observed in 999 responders. Compared with the general population, responders had a significantly higher incidence of all cancers combined, with a standardized incidence ratio (SIR) of 1.09.
Responders had a significantly higher incidence of prostate cancer (SIR,1.25), thyroid cancer (SIR, 2.19), and leukemia (SIR, 1.41). The leukemia category included acute myeloid leukemia (SIR,1.58) and chronic lymphocytic leukemia (SIR, 1.08).
“Although other studies have revealed elevated SIRs for other hematologic malignancies, this is the first reported, statistically significant, elevated SIR for leukemia,” the researchers wrote. “Leukemia is known to occur after exposure to occupational carcinogens, including benzene (burning jet fuel and other sources at the [World Trade Center] site), possibly at low levels of exposure and with a latency of several years from exposure.”
A multivariate analysis showed no association between cancer incidence and the length of time responders spent on the rescue and recovery effort or the intensity of their exposure to the dust cloud or debris pile.
The analysis did show an elevated risk of all cancers combined with each 1-year increase in responder age (hazard ratio, 1.09), among male responders (HR, 1.21), and among responders who smoked at baseline (HR, 1.29).
This research was supported by the Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. The researchers disclosed no conflicts of interest.
SOURCE: Shapiro MZ et al. JNCI Cancer Spectr. 2020 Jan 14. doi: 10.1093/jncics/pkz090.
FROM JNCI CANCER SPECTRUM
Genomic profiling of AML and MDS yields prognostic clues
ORLANDO – A genome-wide study of blood and bone marrow samples from more than 1,300 adults with myeloid disorders has both confirmed the role of known or suspected driver mutations and uncovered new associations that could inform clinical care for patients with acute myeloid leukemia and myelodysplastic syndrome.
“Integration of mutational and expression data is important to refine subytpes and constellations of mutations with prognostic significance,” Ilaria Iacobucci, PhD, of St. Jude Children’s Research Hospital in Memphis said during a late-breaking abstract session at the annual meeting of the American Society of Hematology.
Her team conducted an analysis combining full genomic sequencing and gene-expression profiles in blood and bone marrow samples from 598 adults with acute myeloid leukemia (AML) and 706 with myelodysplastic syndrome (MDS).
The goals of the study were to provide “unbiased analysis of AML and MDS by integrated genomic and transcriptome data and clinico-pathologic features and clinical outcome” and to identify and define myeloid leukemia subtypes with diagnostic, prognostic, and therapeutic significance, she said.
The median age of the MDS cohort was 73.2 years (range 23.3-93.1). According to 2016 World Health Organization criteria, 37% had a diagnosis of MDS with excess blasts, 26.3% had MDS with ring sideroblasts, 20.9% had MDS with multilineage dysplasia, 14.6% had MDS with deletion 5q, and 1.1% had unclassifiable MDS.
The median age of the AML cohort was 68 years. Of this group, 31.7% had a diagnosis of AML not otherwise specified, 29.9% had known cytogenetic alterations, 27.3% had NPM1-mutated AML, and 9.7% had RUNX1-mutated disease.
Samples from all patients underwent tumor whole-genome sequencing and whole-transcriptome sequencing.
The combined sequencing confirmed a diagnosis of AML with recurrent genetic abnormalities in 11% of cases. These patients had disease with distinct gene-expression profiles and favorable prognosis. The sequencing identified combinations of mutations in genes linked with specific AML subtypes.
For example, combinations of mutations in KIT, ZBTB7A, ASXL2, RAD21, CSF3R, and DNM2 were associated with RUNX1-RUNXT1 leukemia, whereas mutations in FLT3, DDX54, WT1, and CALR in promyelocytic leukemia/retinoic acid receptor alpha were associated with promyelocytic leukemia, and KIT and BCORL1 mutations were associated with CBFB-rearranged leukemia.
In addition to rounding up the usual genomic suspects, the investigators also identified combinations that are associated with prognosis. Notably, NPM1 mutations were found in 27.4% of AML and 1% of MDS cases, and these mutations were characterized by four gene-expression signatures that were associated with different combinations of cooperating mutations in cohesin and signaling genes, and with outcome.
They found that patients with co-occurring NPM1 and FLT3 mutations had worse prognosis than those with mutations only in NPM1, whereas patients with NPM1 mutations co-occurring with cohesin gene mutations had better outcomes.
At a briefing prior to her presentation of the data, Dr. Iacobucci explained how her group’s findings might inform treatment, including the possibility of preventing development of AML in patients with MDS.
“What we are doing, in addition to the genomic part, is also establishing a repository of patient-derived xenografts, so in this way we can have the genome information, and we can have the biological material in vivo to test different therapies,” she said.
In an interview, Andrew H. Wei, MBBS, PhD, from the Alfred Hospital in Melbourne, who was not involved in the genomic study, commented on the role of sequencing in treatment of patients with myeloid malignancies.
“I think the future is that as the leukemia evolves, our therapy will evolve along with it. Furthermore, we now have the potential to measure many of these mutations with much higher sensitivity than just whole-genome sequencing, so we can imagine a future whereby we can track and measure these mutations as they rise in the patient’s bone marrow or blood before the patients becomes sick with florid leukemia, and it gives us the potential to predictably alter our management before they become sick,” he said.
The study was supported by St. Jude Children’s Research Hospital and the Leukemia and Lymphoma Society. Dr. Iacobucci and Dr. Wei reported having no relevant disclosures.
SOURCE: Iacobucci I et al. ASH 2019, Abstract LBA-4.
ORLANDO – A genome-wide study of blood and bone marrow samples from more than 1,300 adults with myeloid disorders has both confirmed the role of known or suspected driver mutations and uncovered new associations that could inform clinical care for patients with acute myeloid leukemia and myelodysplastic syndrome.
“Integration of mutational and expression data is important to refine subytpes and constellations of mutations with prognostic significance,” Ilaria Iacobucci, PhD, of St. Jude Children’s Research Hospital in Memphis said during a late-breaking abstract session at the annual meeting of the American Society of Hematology.
Her team conducted an analysis combining full genomic sequencing and gene-expression profiles in blood and bone marrow samples from 598 adults with acute myeloid leukemia (AML) and 706 with myelodysplastic syndrome (MDS).
The goals of the study were to provide “unbiased analysis of AML and MDS by integrated genomic and transcriptome data and clinico-pathologic features and clinical outcome” and to identify and define myeloid leukemia subtypes with diagnostic, prognostic, and therapeutic significance, she said.
The median age of the MDS cohort was 73.2 years (range 23.3-93.1). According to 2016 World Health Organization criteria, 37% had a diagnosis of MDS with excess blasts, 26.3% had MDS with ring sideroblasts, 20.9% had MDS with multilineage dysplasia, 14.6% had MDS with deletion 5q, and 1.1% had unclassifiable MDS.
The median age of the AML cohort was 68 years. Of this group, 31.7% had a diagnosis of AML not otherwise specified, 29.9% had known cytogenetic alterations, 27.3% had NPM1-mutated AML, and 9.7% had RUNX1-mutated disease.
Samples from all patients underwent tumor whole-genome sequencing and whole-transcriptome sequencing.
The combined sequencing confirmed a diagnosis of AML with recurrent genetic abnormalities in 11% of cases. These patients had disease with distinct gene-expression profiles and favorable prognosis. The sequencing identified combinations of mutations in genes linked with specific AML subtypes.
For example, combinations of mutations in KIT, ZBTB7A, ASXL2, RAD21, CSF3R, and DNM2 were associated with RUNX1-RUNXT1 leukemia, whereas mutations in FLT3, DDX54, WT1, and CALR in promyelocytic leukemia/retinoic acid receptor alpha were associated with promyelocytic leukemia, and KIT and BCORL1 mutations were associated with CBFB-rearranged leukemia.
In addition to rounding up the usual genomic suspects, the investigators also identified combinations that are associated with prognosis. Notably, NPM1 mutations were found in 27.4% of AML and 1% of MDS cases, and these mutations were characterized by four gene-expression signatures that were associated with different combinations of cooperating mutations in cohesin and signaling genes, and with outcome.
They found that patients with co-occurring NPM1 and FLT3 mutations had worse prognosis than those with mutations only in NPM1, whereas patients with NPM1 mutations co-occurring with cohesin gene mutations had better outcomes.
At a briefing prior to her presentation of the data, Dr. Iacobucci explained how her group’s findings might inform treatment, including the possibility of preventing development of AML in patients with MDS.
“What we are doing, in addition to the genomic part, is also establishing a repository of patient-derived xenografts, so in this way we can have the genome information, and we can have the biological material in vivo to test different therapies,” she said.
In an interview, Andrew H. Wei, MBBS, PhD, from the Alfred Hospital in Melbourne, who was not involved in the genomic study, commented on the role of sequencing in treatment of patients with myeloid malignancies.
“I think the future is that as the leukemia evolves, our therapy will evolve along with it. Furthermore, we now have the potential to measure many of these mutations with much higher sensitivity than just whole-genome sequencing, so we can imagine a future whereby we can track and measure these mutations as they rise in the patient’s bone marrow or blood before the patients becomes sick with florid leukemia, and it gives us the potential to predictably alter our management before they become sick,” he said.
The study was supported by St. Jude Children’s Research Hospital and the Leukemia and Lymphoma Society. Dr. Iacobucci and Dr. Wei reported having no relevant disclosures.
SOURCE: Iacobucci I et al. ASH 2019, Abstract LBA-4.
ORLANDO – A genome-wide study of blood and bone marrow samples from more than 1,300 adults with myeloid disorders has both confirmed the role of known or suspected driver mutations and uncovered new associations that could inform clinical care for patients with acute myeloid leukemia and myelodysplastic syndrome.
“Integration of mutational and expression data is important to refine subytpes and constellations of mutations with prognostic significance,” Ilaria Iacobucci, PhD, of St. Jude Children’s Research Hospital in Memphis said during a late-breaking abstract session at the annual meeting of the American Society of Hematology.
Her team conducted an analysis combining full genomic sequencing and gene-expression profiles in blood and bone marrow samples from 598 adults with acute myeloid leukemia (AML) and 706 with myelodysplastic syndrome (MDS).
The goals of the study were to provide “unbiased analysis of AML and MDS by integrated genomic and transcriptome data and clinico-pathologic features and clinical outcome” and to identify and define myeloid leukemia subtypes with diagnostic, prognostic, and therapeutic significance, she said.
The median age of the MDS cohort was 73.2 years (range 23.3-93.1). According to 2016 World Health Organization criteria, 37% had a diagnosis of MDS with excess blasts, 26.3% had MDS with ring sideroblasts, 20.9% had MDS with multilineage dysplasia, 14.6% had MDS with deletion 5q, and 1.1% had unclassifiable MDS.
The median age of the AML cohort was 68 years. Of this group, 31.7% had a diagnosis of AML not otherwise specified, 29.9% had known cytogenetic alterations, 27.3% had NPM1-mutated AML, and 9.7% had RUNX1-mutated disease.
Samples from all patients underwent tumor whole-genome sequencing and whole-transcriptome sequencing.
The combined sequencing confirmed a diagnosis of AML with recurrent genetic abnormalities in 11% of cases. These patients had disease with distinct gene-expression profiles and favorable prognosis. The sequencing identified combinations of mutations in genes linked with specific AML subtypes.
For example, combinations of mutations in KIT, ZBTB7A, ASXL2, RAD21, CSF3R, and DNM2 were associated with RUNX1-RUNXT1 leukemia, whereas mutations in FLT3, DDX54, WT1, and CALR in promyelocytic leukemia/retinoic acid receptor alpha were associated with promyelocytic leukemia, and KIT and BCORL1 mutations were associated with CBFB-rearranged leukemia.
In addition to rounding up the usual genomic suspects, the investigators also identified combinations that are associated with prognosis. Notably, NPM1 mutations were found in 27.4% of AML and 1% of MDS cases, and these mutations were characterized by four gene-expression signatures that were associated with different combinations of cooperating mutations in cohesin and signaling genes, and with outcome.
They found that patients with co-occurring NPM1 and FLT3 mutations had worse prognosis than those with mutations only in NPM1, whereas patients with NPM1 mutations co-occurring with cohesin gene mutations had better outcomes.
At a briefing prior to her presentation of the data, Dr. Iacobucci explained how her group’s findings might inform treatment, including the possibility of preventing development of AML in patients with MDS.
“What we are doing, in addition to the genomic part, is also establishing a repository of patient-derived xenografts, so in this way we can have the genome information, and we can have the biological material in vivo to test different therapies,” she said.
In an interview, Andrew H. Wei, MBBS, PhD, from the Alfred Hospital in Melbourne, who was not involved in the genomic study, commented on the role of sequencing in treatment of patients with myeloid malignancies.
“I think the future is that as the leukemia evolves, our therapy will evolve along with it. Furthermore, we now have the potential to measure many of these mutations with much higher sensitivity than just whole-genome sequencing, so we can imagine a future whereby we can track and measure these mutations as they rise in the patient’s bone marrow or blood before the patients becomes sick with florid leukemia, and it gives us the potential to predictably alter our management before they become sick,” he said.
The study was supported by St. Jude Children’s Research Hospital and the Leukemia and Lymphoma Society. Dr. Iacobucci and Dr. Wei reported having no relevant disclosures.
SOURCE: Iacobucci I et al. ASH 2019, Abstract LBA-4.
REPORTING FROM ASH 2019
Oral azacitidine: First maintenance therapy for AML
ORLANDO – For the first time, there is a maintenance therapy for patients with acute myeloid leukemia (AML) in remission that can improve overall survival – a new oral formulation of an old drug, azacitidine, known as CC-486 (Celgene).
“Oral azacitidine represents a new therapeutic standard for patients with AML in remission,” said lead author Andrew H. Wei, MBBS, PhD, from the Alfred Hospital in Melbourne.
“It’s not too hard to get these patients into remission,” commented another expert. “The problem comes in keeping them in remission.”
Dr. Wei noted that standard treatment with intensive induction chemotherapy for AML induces complete remission (CR) in 60%-80% of patients aged 60 years or younger and in 40%-60% of patients aged 60 years or older.
However, the majority of patients who attain complete remission (CR) will eventually relapse, and relapse is the primary obstacle to long-term survival, he said.
Despite various attempts, there has been no success over the past 30 years in defining maintenance treatment for these patients, Dr. Wei said.
The new results suggest that oral azacitidine could be an effective maintenance therapy.
Dr. Wei presented the results at the 2019 annual meeting of the American Society of Hematology. They come from the QUAZAR AML-001 study, conducted in 472 patients with poor-risk AML in first remission.
The results show that CC-486 significantly improved outcomes, compared with placebo plus best supportive care, in terms of median overall survival (24.7 vs. 14.8 months) and median relapse-free survival (10.2 vs. 4.8 months).
The trial was funded by Celgene, which said it will be submitting the data for regulatory approval for the new oral formulation of azacitidine, CC-486.
Experts predict new standard of care
Experts approached for comment agreed that maintenance oral azacitidine will become the new standard of care for patients with AML in first remission.
“Unlike therapy for acute lymphoblastic leukemia, maintenance therapy has not been part of the treatment algorithm for AML patients in first remission,” Harry P. Erba, MD, PhD, director of the leukemia program at the Duke Cancer Institute, Durham, N.C., told Medscape Medical News.
He explained that trials for maintenance after first remission in AML have failed. Recently, Dr. Erba noted, the HOVON97 trial with injectable azacitidine demonstrated improvement in relapse-free survival, compared with observation for older AML patients achieving remission after induction therapy. “However, there was no improvement in overall survival,” he said.
“Remission in AML is short lived,” Dr. Erba said. Oral azacitidine represents the first maintenance therapy in AML that has shown both significant and clinically meaningful improvements in overall and relapse-free survival and will represent a new standard of care for patients with AML in remission, Dr. Erba said. “Maintenance oral azacitidine will be practice changing,” he predicted.
HOVON97 was a small study of injectable azacitidine used as maintenance therapy for 12 months, but it was slow to accrue and did not meet its accrual target.
“In HOVON97, at 12 months, only one third of patients received less than the 12 cycles of therapy,” Dr. Wei said. He explained that, with injectable azacitidine, patients have to come into the hospital/clinic for 7 days a month, 84 days a year. Oral azacitidine is more convenient as patients do not have to come into the clinic, he said.
Dr. Wei pointed out that about 40 patients in the QUAZAR study, which started in 2013, are still on maintenance therapy, with one patient now having received 80 cycles of therapy (approximately 7 years). “Long-term maintenance therapy with azacitidine is possible,” he said.
Another expert was also impressed by the new results. “This is an important clinical trial that addresses an unmet need in AML care,” said John Mascarenhas, MD, director of the Adult Leukemia Program and leader of clinical investigation within the myeloproliferative disorders program at the Tisch Cancer Institute at the Icahn School of Medicine at Mount Sinai, New York.
“Older patients can often receive induction chemotherapy but frequently do not ultimately do well, as the disease relapses and survival is limited,” he explained.
“This large, randomized, double-blind, controlled study of intermediate- or poor-risk AML patients over the age of 55 years supports the use of maintenance oral azacitidine after initial remission to extend overall and relapse-free survival in older AML patients not eligible for transplant,” Dr. Mascarenhas said.
“This is still not a curative approach,” Dr. Wei said, but added that it prolongs relapse-free survival for older patients while maintaining a quality of life for as long as possible.
Study details
The QUAZAR phase 3 study enrolled patients with poor- or intermediate-risk cytogenetics who had an Eastern Cooperative Oncology Group performance status less than or equal to 3 and who had achieved CR or CR with incomplete count recovery (CRi) after induction therapy with or without consolidation therapy. In addition, patients were not candidates for stem cell transplants.
Patients had predominantly de novo AML (89%). Other baseline characteristics of note:
- 85% of patients had intermediate-risk and 15% had poor-risk cytogenetics
- 79% achieved CR and 21% achieved CRi after induction therapy
- 78% received at least one cycle of consolidation therapy
- 43% of patients had minimal residual disease (MRD)–positive disease
Patients were randomized to receive oral azacitidine 200 mg daily on days 1-14 of a repeat 28-day cycle (n = 278) or matching placebo (n = 274). Treatment was continued indefinitely until blast count was more than 15% or patients experienced unacceptable toxicity or went on to transplant.
At a median follow-up of over 41.2 months (3 years, 5 months), median overall survival was significantly longer for patients receiving oral azacitidine at 24.7 months versus 14.8 months for placebo (P less than .0009; hazard ratio, 0.69).
Relapse-free survival was also significantly prolonged, to 10.2 months for patients on oral azacitidine versus 4.8 months for placebo (HR, 0.65; P less than .0001).
Patients on oral azacitidine reported more grade 1-2 gastrointestinal adverse events, such as nausea (65% vs. 24% on placebo), vomiting (60% vs. 10%), and diarrhea (50% vs 22%), as well as more cytopenia. The most common grade 3-4 adverse events were neutropenia (41% with oral azacitidine vs. 24% on placebo), thrombocytopenia (23% vs. 22%), and anemia (14% vs. 13%).
Although Dr. Erba supported the use of oral azacitidine as maintenance therapy, he pointed out that it was hard to convince patients, especially older ones, to continue on maintenance therapy indefinitely. “The toxicities of continuing on a drug indefinitely are real issues,” he said, explaining that most elderly patients cannot cope with even grade 1-2 nausea, diarrhea, and vomiting over the long term.
But he noted that, regardless of the higher incidence of some adverse events with oral azacitidine, the health-related quality of life of patients on oral azacitidine was similar to those on placebo.
Awaiting longer follow-up
Both experts said that longer-term follow-up is needed.
“We need a longer follow-up to see how the curves plateau,” Dr. Erba said. He would also like to see a comparative analysis of the data in patients who are MRD negative versus those who are MRD positive.
“The final results of this study, including the impact of measurable residual disease on outcome in this setting, will potentially have practice-changing implications,” said Dr. Mascarenhas.
At the press conference, Dr. Wei pointed out that, based on the data from QUAZAR, oral azacitidine is likely to be evaluated in the frontline setting of AML. “The elderly make up about two-thirds of all AML patients, and oral azacitidine will be a better option than 7 days per month for chemotherapy treatment in the clinic,” he said. “Oral azacitidine in the future may also be the backbone for other combinations.”
The study was funded by Celgene.
Dr. Wei receives honoraria from AbbVie, Macrogenics, Pfizer, Astellas, Janssen, Servier, Celgene, Amgen, AstraZeneca, Novartis, and Genentech; is on the board of directors or serves on the advisory committees for AbbVie, Macrogenics, Pfizer, Astellas, Servier, Celgene, Amgen, Novartis, and Genentech; and receives research funding from AbbVie, Servier, Celgene, Amgen, AstraZeneca, and Novartis. As a former employee of the Walter and Eliza Hall Institute, Dr. Wei receives a fraction of its royalty stream related to venetoclax.
A partial list of Dr. Erba’s conflict of interest includes consulting with Agios, Novartis, Daiichi Sankyo, MacroGenics, Jazz Pharmaceuticals, Seattle Genetics, GlycoMimetics, Amgen, Pfizer, Celgene, AbbVie, Covance, Immunogen, Astellas Pharma, Incyte; being on the speakers bureau or receiving lecture fees from Agios, Novartis, MacroGenics, Jazz Pharmaceuticals, Celgene; receiving research funding from Novartis, Daiichi Sankyo, MacroGenics, GlycoMimetics, Celgene; being on the data and safety monitoring board of GlycoMimetics; and chairing independent review boards for several trials across several companies.
A version of this story originally appeared on Medscape.com.
ORLANDO – For the first time, there is a maintenance therapy for patients with acute myeloid leukemia (AML) in remission that can improve overall survival – a new oral formulation of an old drug, azacitidine, known as CC-486 (Celgene).
“Oral azacitidine represents a new therapeutic standard for patients with AML in remission,” said lead author Andrew H. Wei, MBBS, PhD, from the Alfred Hospital in Melbourne.
“It’s not too hard to get these patients into remission,” commented another expert. “The problem comes in keeping them in remission.”
Dr. Wei noted that standard treatment with intensive induction chemotherapy for AML induces complete remission (CR) in 60%-80% of patients aged 60 years or younger and in 40%-60% of patients aged 60 years or older.
However, the majority of patients who attain complete remission (CR) will eventually relapse, and relapse is the primary obstacle to long-term survival, he said.
Despite various attempts, there has been no success over the past 30 years in defining maintenance treatment for these patients, Dr. Wei said.
The new results suggest that oral azacitidine could be an effective maintenance therapy.
Dr. Wei presented the results at the 2019 annual meeting of the American Society of Hematology. They come from the QUAZAR AML-001 study, conducted in 472 patients with poor-risk AML in first remission.
The results show that CC-486 significantly improved outcomes, compared with placebo plus best supportive care, in terms of median overall survival (24.7 vs. 14.8 months) and median relapse-free survival (10.2 vs. 4.8 months).
The trial was funded by Celgene, which said it will be submitting the data for regulatory approval for the new oral formulation of azacitidine, CC-486.
Experts predict new standard of care
Experts approached for comment agreed that maintenance oral azacitidine will become the new standard of care for patients with AML in first remission.
“Unlike therapy for acute lymphoblastic leukemia, maintenance therapy has not been part of the treatment algorithm for AML patients in first remission,” Harry P. Erba, MD, PhD, director of the leukemia program at the Duke Cancer Institute, Durham, N.C., told Medscape Medical News.
He explained that trials for maintenance after first remission in AML have failed. Recently, Dr. Erba noted, the HOVON97 trial with injectable azacitidine demonstrated improvement in relapse-free survival, compared with observation for older AML patients achieving remission after induction therapy. “However, there was no improvement in overall survival,” he said.
“Remission in AML is short lived,” Dr. Erba said. Oral azacitidine represents the first maintenance therapy in AML that has shown both significant and clinically meaningful improvements in overall and relapse-free survival and will represent a new standard of care for patients with AML in remission, Dr. Erba said. “Maintenance oral azacitidine will be practice changing,” he predicted.
HOVON97 was a small study of injectable azacitidine used as maintenance therapy for 12 months, but it was slow to accrue and did not meet its accrual target.
“In HOVON97, at 12 months, only one third of patients received less than the 12 cycles of therapy,” Dr. Wei said. He explained that, with injectable azacitidine, patients have to come into the hospital/clinic for 7 days a month, 84 days a year. Oral azacitidine is more convenient as patients do not have to come into the clinic, he said.
Dr. Wei pointed out that about 40 patients in the QUAZAR study, which started in 2013, are still on maintenance therapy, with one patient now having received 80 cycles of therapy (approximately 7 years). “Long-term maintenance therapy with azacitidine is possible,” he said.
Another expert was also impressed by the new results. “This is an important clinical trial that addresses an unmet need in AML care,” said John Mascarenhas, MD, director of the Adult Leukemia Program and leader of clinical investigation within the myeloproliferative disorders program at the Tisch Cancer Institute at the Icahn School of Medicine at Mount Sinai, New York.
“Older patients can often receive induction chemotherapy but frequently do not ultimately do well, as the disease relapses and survival is limited,” he explained.
“This large, randomized, double-blind, controlled study of intermediate- or poor-risk AML patients over the age of 55 years supports the use of maintenance oral azacitidine after initial remission to extend overall and relapse-free survival in older AML patients not eligible for transplant,” Dr. Mascarenhas said.
“This is still not a curative approach,” Dr. Wei said, but added that it prolongs relapse-free survival for older patients while maintaining a quality of life for as long as possible.
Study details
The QUAZAR phase 3 study enrolled patients with poor- or intermediate-risk cytogenetics who had an Eastern Cooperative Oncology Group performance status less than or equal to 3 and who had achieved CR or CR with incomplete count recovery (CRi) after induction therapy with or without consolidation therapy. In addition, patients were not candidates for stem cell transplants.
Patients had predominantly de novo AML (89%). Other baseline characteristics of note:
- 85% of patients had intermediate-risk and 15% had poor-risk cytogenetics
- 79% achieved CR and 21% achieved CRi after induction therapy
- 78% received at least one cycle of consolidation therapy
- 43% of patients had minimal residual disease (MRD)–positive disease
Patients were randomized to receive oral azacitidine 200 mg daily on days 1-14 of a repeat 28-day cycle (n = 278) or matching placebo (n = 274). Treatment was continued indefinitely until blast count was more than 15% or patients experienced unacceptable toxicity or went on to transplant.
At a median follow-up of over 41.2 months (3 years, 5 months), median overall survival was significantly longer for patients receiving oral azacitidine at 24.7 months versus 14.8 months for placebo (P less than .0009; hazard ratio, 0.69).
Relapse-free survival was also significantly prolonged, to 10.2 months for patients on oral azacitidine versus 4.8 months for placebo (HR, 0.65; P less than .0001).
Patients on oral azacitidine reported more grade 1-2 gastrointestinal adverse events, such as nausea (65% vs. 24% on placebo), vomiting (60% vs. 10%), and diarrhea (50% vs 22%), as well as more cytopenia. The most common grade 3-4 adverse events were neutropenia (41% with oral azacitidine vs. 24% on placebo), thrombocytopenia (23% vs. 22%), and anemia (14% vs. 13%).
Although Dr. Erba supported the use of oral azacitidine as maintenance therapy, he pointed out that it was hard to convince patients, especially older ones, to continue on maintenance therapy indefinitely. “The toxicities of continuing on a drug indefinitely are real issues,” he said, explaining that most elderly patients cannot cope with even grade 1-2 nausea, diarrhea, and vomiting over the long term.
But he noted that, regardless of the higher incidence of some adverse events with oral azacitidine, the health-related quality of life of patients on oral azacitidine was similar to those on placebo.
Awaiting longer follow-up
Both experts said that longer-term follow-up is needed.
“We need a longer follow-up to see how the curves plateau,” Dr. Erba said. He would also like to see a comparative analysis of the data in patients who are MRD negative versus those who are MRD positive.
“The final results of this study, including the impact of measurable residual disease on outcome in this setting, will potentially have practice-changing implications,” said Dr. Mascarenhas.
At the press conference, Dr. Wei pointed out that, based on the data from QUAZAR, oral azacitidine is likely to be evaluated in the frontline setting of AML. “The elderly make up about two-thirds of all AML patients, and oral azacitidine will be a better option than 7 days per month for chemotherapy treatment in the clinic,” he said. “Oral azacitidine in the future may also be the backbone for other combinations.”
The study was funded by Celgene.
Dr. Wei receives honoraria from AbbVie, Macrogenics, Pfizer, Astellas, Janssen, Servier, Celgene, Amgen, AstraZeneca, Novartis, and Genentech; is on the board of directors or serves on the advisory committees for AbbVie, Macrogenics, Pfizer, Astellas, Servier, Celgene, Amgen, Novartis, and Genentech; and receives research funding from AbbVie, Servier, Celgene, Amgen, AstraZeneca, and Novartis. As a former employee of the Walter and Eliza Hall Institute, Dr. Wei receives a fraction of its royalty stream related to venetoclax.
A partial list of Dr. Erba’s conflict of interest includes consulting with Agios, Novartis, Daiichi Sankyo, MacroGenics, Jazz Pharmaceuticals, Seattle Genetics, GlycoMimetics, Amgen, Pfizer, Celgene, AbbVie, Covance, Immunogen, Astellas Pharma, Incyte; being on the speakers bureau or receiving lecture fees from Agios, Novartis, MacroGenics, Jazz Pharmaceuticals, Celgene; receiving research funding from Novartis, Daiichi Sankyo, MacroGenics, GlycoMimetics, Celgene; being on the data and safety monitoring board of GlycoMimetics; and chairing independent review boards for several trials across several companies.
A version of this story originally appeared on Medscape.com.
ORLANDO – For the first time, there is a maintenance therapy for patients with acute myeloid leukemia (AML) in remission that can improve overall survival – a new oral formulation of an old drug, azacitidine, known as CC-486 (Celgene).
“Oral azacitidine represents a new therapeutic standard for patients with AML in remission,” said lead author Andrew H. Wei, MBBS, PhD, from the Alfred Hospital in Melbourne.
“It’s not too hard to get these patients into remission,” commented another expert. “The problem comes in keeping them in remission.”
Dr. Wei noted that standard treatment with intensive induction chemotherapy for AML induces complete remission (CR) in 60%-80% of patients aged 60 years or younger and in 40%-60% of patients aged 60 years or older.
However, the majority of patients who attain complete remission (CR) will eventually relapse, and relapse is the primary obstacle to long-term survival, he said.
Despite various attempts, there has been no success over the past 30 years in defining maintenance treatment for these patients, Dr. Wei said.
The new results suggest that oral azacitidine could be an effective maintenance therapy.
Dr. Wei presented the results at the 2019 annual meeting of the American Society of Hematology. They come from the QUAZAR AML-001 study, conducted in 472 patients with poor-risk AML in first remission.
The results show that CC-486 significantly improved outcomes, compared with placebo plus best supportive care, in terms of median overall survival (24.7 vs. 14.8 months) and median relapse-free survival (10.2 vs. 4.8 months).
The trial was funded by Celgene, which said it will be submitting the data for regulatory approval for the new oral formulation of azacitidine, CC-486.
Experts predict new standard of care
Experts approached for comment agreed that maintenance oral azacitidine will become the new standard of care for patients with AML in first remission.
“Unlike therapy for acute lymphoblastic leukemia, maintenance therapy has not been part of the treatment algorithm for AML patients in first remission,” Harry P. Erba, MD, PhD, director of the leukemia program at the Duke Cancer Institute, Durham, N.C., told Medscape Medical News.
He explained that trials for maintenance after first remission in AML have failed. Recently, Dr. Erba noted, the HOVON97 trial with injectable azacitidine demonstrated improvement in relapse-free survival, compared with observation for older AML patients achieving remission after induction therapy. “However, there was no improvement in overall survival,” he said.
“Remission in AML is short lived,” Dr. Erba said. Oral azacitidine represents the first maintenance therapy in AML that has shown both significant and clinically meaningful improvements in overall and relapse-free survival and will represent a new standard of care for patients with AML in remission, Dr. Erba said. “Maintenance oral azacitidine will be practice changing,” he predicted.
HOVON97 was a small study of injectable azacitidine used as maintenance therapy for 12 months, but it was slow to accrue and did not meet its accrual target.
“In HOVON97, at 12 months, only one third of patients received less than the 12 cycles of therapy,” Dr. Wei said. He explained that, with injectable azacitidine, patients have to come into the hospital/clinic for 7 days a month, 84 days a year. Oral azacitidine is more convenient as patients do not have to come into the clinic, he said.
Dr. Wei pointed out that about 40 patients in the QUAZAR study, which started in 2013, are still on maintenance therapy, with one patient now having received 80 cycles of therapy (approximately 7 years). “Long-term maintenance therapy with azacitidine is possible,” he said.
Another expert was also impressed by the new results. “This is an important clinical trial that addresses an unmet need in AML care,” said John Mascarenhas, MD, director of the Adult Leukemia Program and leader of clinical investigation within the myeloproliferative disorders program at the Tisch Cancer Institute at the Icahn School of Medicine at Mount Sinai, New York.
“Older patients can often receive induction chemotherapy but frequently do not ultimately do well, as the disease relapses and survival is limited,” he explained.
“This large, randomized, double-blind, controlled study of intermediate- or poor-risk AML patients over the age of 55 years supports the use of maintenance oral azacitidine after initial remission to extend overall and relapse-free survival in older AML patients not eligible for transplant,” Dr. Mascarenhas said.
“This is still not a curative approach,” Dr. Wei said, but added that it prolongs relapse-free survival for older patients while maintaining a quality of life for as long as possible.
Study details
The QUAZAR phase 3 study enrolled patients with poor- or intermediate-risk cytogenetics who had an Eastern Cooperative Oncology Group performance status less than or equal to 3 and who had achieved CR or CR with incomplete count recovery (CRi) after induction therapy with or without consolidation therapy. In addition, patients were not candidates for stem cell transplants.
Patients had predominantly de novo AML (89%). Other baseline characteristics of note:
- 85% of patients had intermediate-risk and 15% had poor-risk cytogenetics
- 79% achieved CR and 21% achieved CRi after induction therapy
- 78% received at least one cycle of consolidation therapy
- 43% of patients had minimal residual disease (MRD)–positive disease
Patients were randomized to receive oral azacitidine 200 mg daily on days 1-14 of a repeat 28-day cycle (n = 278) or matching placebo (n = 274). Treatment was continued indefinitely until blast count was more than 15% or patients experienced unacceptable toxicity or went on to transplant.
At a median follow-up of over 41.2 months (3 years, 5 months), median overall survival was significantly longer for patients receiving oral azacitidine at 24.7 months versus 14.8 months for placebo (P less than .0009; hazard ratio, 0.69).
Relapse-free survival was also significantly prolonged, to 10.2 months for patients on oral azacitidine versus 4.8 months for placebo (HR, 0.65; P less than .0001).
Patients on oral azacitidine reported more grade 1-2 gastrointestinal adverse events, such as nausea (65% vs. 24% on placebo), vomiting (60% vs. 10%), and diarrhea (50% vs 22%), as well as more cytopenia. The most common grade 3-4 adverse events were neutropenia (41% with oral azacitidine vs. 24% on placebo), thrombocytopenia (23% vs. 22%), and anemia (14% vs. 13%).
Although Dr. Erba supported the use of oral azacitidine as maintenance therapy, he pointed out that it was hard to convince patients, especially older ones, to continue on maintenance therapy indefinitely. “The toxicities of continuing on a drug indefinitely are real issues,” he said, explaining that most elderly patients cannot cope with even grade 1-2 nausea, diarrhea, and vomiting over the long term.
But he noted that, regardless of the higher incidence of some adverse events with oral azacitidine, the health-related quality of life of patients on oral azacitidine was similar to those on placebo.
Awaiting longer follow-up
Both experts said that longer-term follow-up is needed.
“We need a longer follow-up to see how the curves plateau,” Dr. Erba said. He would also like to see a comparative analysis of the data in patients who are MRD negative versus those who are MRD positive.
“The final results of this study, including the impact of measurable residual disease on outcome in this setting, will potentially have practice-changing implications,” said Dr. Mascarenhas.
At the press conference, Dr. Wei pointed out that, based on the data from QUAZAR, oral azacitidine is likely to be evaluated in the frontline setting of AML. “The elderly make up about two-thirds of all AML patients, and oral azacitidine will be a better option than 7 days per month for chemotherapy treatment in the clinic,” he said. “Oral azacitidine in the future may also be the backbone for other combinations.”
The study was funded by Celgene.
Dr. Wei receives honoraria from AbbVie, Macrogenics, Pfizer, Astellas, Janssen, Servier, Celgene, Amgen, AstraZeneca, Novartis, and Genentech; is on the board of directors or serves on the advisory committees for AbbVie, Macrogenics, Pfizer, Astellas, Servier, Celgene, Amgen, Novartis, and Genentech; and receives research funding from AbbVie, Servier, Celgene, Amgen, AstraZeneca, and Novartis. As a former employee of the Walter and Eliza Hall Institute, Dr. Wei receives a fraction of its royalty stream related to venetoclax.
A partial list of Dr. Erba’s conflict of interest includes consulting with Agios, Novartis, Daiichi Sankyo, MacroGenics, Jazz Pharmaceuticals, Seattle Genetics, GlycoMimetics, Amgen, Pfizer, Celgene, AbbVie, Covance, Immunogen, Astellas Pharma, Incyte; being on the speakers bureau or receiving lecture fees from Agios, Novartis, MacroGenics, Jazz Pharmaceuticals, Celgene; receiving research funding from Novartis, Daiichi Sankyo, MacroGenics, GlycoMimetics, Celgene; being on the data and safety monitoring board of GlycoMimetics; and chairing independent review boards for several trials across several companies.
A version of this story originally appeared on Medscape.com.
Kidney function in African American AML patients not linked to reduced survival compared with whites
ORLANDO – While African Americans with acute myeloid leukemia were more likely to have evidence of abnormal kidney function, the excess of this comorbidity didn’t affect overall survival, compared with whites, according to a study of more than 1,000 patients.
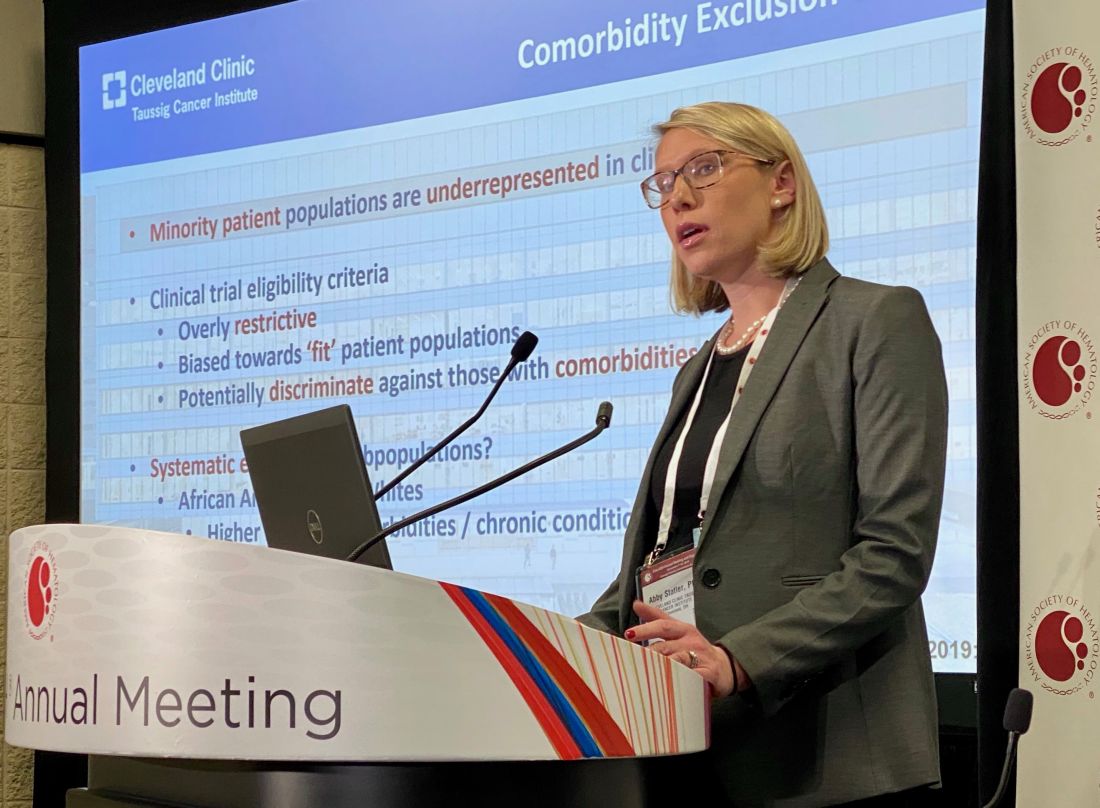
A total of 63% of African Americans with acute myeloid leukemia (AML) presented with a renal function abnormality that could have excluded them from a clinical trial, compared with 56% in the overall cohort; however, analysis of outcomes data suggested that renal function abnormalities were not associated with decreased survival in African Americans versus whites, said Abby Statler, PhD, MPH, of the Cleveland Clinic.
The findings may have implications for the design of clinical trials that might exclude patients on the basis of comorbidities that don’t actually affect survival, according to Dr. Statler.
“If we’re able to liberalize renal function eligibility criteria ... this may reduce racial disparities in clinical trial enrollment, which might be a major step in improving the diversity of cancer patient populations,” Dr. Statler said in a press conference at the annual meeting of the American Society of Hematology.
Overly restrictive criteria could be a significant barrier to clinical trial enrollment among minority patient populations, according to Dr. Statler.
Eligibility criteria are generally biased toward “fit” patient populations, which means they may discriminate against less-fit groups, such as African Americans who, compared with whites, have higher rates of comorbidities and report poorer overall health, according to Dr. Statler.
Laura Michaelis, MD, who chaired the press conference, said these findings suggest current clinical trial designs may be “too restrictive.”
“Once it’s published and validated, [these] data should definitely make us think twice about when you limit a patient’s enrollment in a trial,” Dr. Michaelis said in an interview.
Restrictive eligibility criteria may not only limit access to minority populations, but also may slow clinical trial accrual and completion, and make it harder to generalize clinical trial findings to the overall population, said Dr. Michaelis, associate professor of medicine in the division of hematology and oncology, Medical College of Wisconsin, Milwaukee.
The study by Dr. Statler and colleagues included 1,040 AML patients who received chemotherapy at Cleveland Clinic between 2003 and 2019. About 10% of the patients in the analysis were African American and 90% were white.
Median overall survival was not significantly different by race, at 13.7 months for African Americans and 14.9 months for whites (P = 0.89), according to results published in the study abstract.
Mild creatinine elevation did not appear to affect survival in this study, according to the investigator. Survival was not significantly different between patients with normal creatinine and those with creatinine up to 1.5 times the upper limit of normal. However, higher levels of creatinine were significantly associated with worse survival, Dr. Statler said.
Further analyses showed that these survival findings by creatinine level held up specifically in the African American subgroup as well, Dr. Statler said in the press conference.
Dr. Statler provided no disclosures related to the presentation. Study coauthors described disclosures related to Amgen, SimulStat, Bristol-Myers Squibb, Takeda, Pfizer, Novartis, Celgene Corporation, Abbvie, and Incyte, among others.
SOURCE: Statler A et al. ASH 2019, Abstract 381.
ORLANDO – While African Americans with acute myeloid leukemia were more likely to have evidence of abnormal kidney function, the excess of this comorbidity didn’t affect overall survival, compared with whites, according to a study of more than 1,000 patients.
A total of 63% of African Americans with acute myeloid leukemia (AML) presented with a renal function abnormality that could have excluded them from a clinical trial, compared with 56% in the overall cohort; however, analysis of outcomes data suggested that renal function abnormalities were not associated with decreased survival in African Americans versus whites, said Abby Statler, PhD, MPH, of the Cleveland Clinic.
The findings may have implications for the design of clinical trials that might exclude patients on the basis of comorbidities that don’t actually affect survival, according to Dr. Statler.
“If we’re able to liberalize renal function eligibility criteria ... this may reduce racial disparities in clinical trial enrollment, which might be a major step in improving the diversity of cancer patient populations,” Dr. Statler said in a press conference at the annual meeting of the American Society of Hematology.
Overly restrictive criteria could be a significant barrier to clinical trial enrollment among minority patient populations, according to Dr. Statler.
Eligibility criteria are generally biased toward “fit” patient populations, which means they may discriminate against less-fit groups, such as African Americans who, compared with whites, have higher rates of comorbidities and report poorer overall health, according to Dr. Statler.
Laura Michaelis, MD, who chaired the press conference, said these findings suggest current clinical trial designs may be “too restrictive.”
“Once it’s published and validated, [these] data should definitely make us think twice about when you limit a patient’s enrollment in a trial,” Dr. Michaelis said in an interview.
Restrictive eligibility criteria may not only limit access to minority populations, but also may slow clinical trial accrual and completion, and make it harder to generalize clinical trial findings to the overall population, said Dr. Michaelis, associate professor of medicine in the division of hematology and oncology, Medical College of Wisconsin, Milwaukee.
The study by Dr. Statler and colleagues included 1,040 AML patients who received chemotherapy at Cleveland Clinic between 2003 and 2019. About 10% of the patients in the analysis were African American and 90% were white.
Median overall survival was not significantly different by race, at 13.7 months for African Americans and 14.9 months for whites (P = 0.89), according to results published in the study abstract.
Mild creatinine elevation did not appear to affect survival in this study, according to the investigator. Survival was not significantly different between patients with normal creatinine and those with creatinine up to 1.5 times the upper limit of normal. However, higher levels of creatinine were significantly associated with worse survival, Dr. Statler said.
Further analyses showed that these survival findings by creatinine level held up specifically in the African American subgroup as well, Dr. Statler said in the press conference.
Dr. Statler provided no disclosures related to the presentation. Study coauthors described disclosures related to Amgen, SimulStat, Bristol-Myers Squibb, Takeda, Pfizer, Novartis, Celgene Corporation, Abbvie, and Incyte, among others.
SOURCE: Statler A et al. ASH 2019, Abstract 381.
ORLANDO – While African Americans with acute myeloid leukemia were more likely to have evidence of abnormal kidney function, the excess of this comorbidity didn’t affect overall survival, compared with whites, according to a study of more than 1,000 patients.
A total of 63% of African Americans with acute myeloid leukemia (AML) presented with a renal function abnormality that could have excluded them from a clinical trial, compared with 56% in the overall cohort; however, analysis of outcomes data suggested that renal function abnormalities were not associated with decreased survival in African Americans versus whites, said Abby Statler, PhD, MPH, of the Cleveland Clinic.
The findings may have implications for the design of clinical trials that might exclude patients on the basis of comorbidities that don’t actually affect survival, according to Dr. Statler.
“If we’re able to liberalize renal function eligibility criteria ... this may reduce racial disparities in clinical trial enrollment, which might be a major step in improving the diversity of cancer patient populations,” Dr. Statler said in a press conference at the annual meeting of the American Society of Hematology.
Overly restrictive criteria could be a significant barrier to clinical trial enrollment among minority patient populations, according to Dr. Statler.
Eligibility criteria are generally biased toward “fit” patient populations, which means they may discriminate against less-fit groups, such as African Americans who, compared with whites, have higher rates of comorbidities and report poorer overall health, according to Dr. Statler.
Laura Michaelis, MD, who chaired the press conference, said these findings suggest current clinical trial designs may be “too restrictive.”
“Once it’s published and validated, [these] data should definitely make us think twice about when you limit a patient’s enrollment in a trial,” Dr. Michaelis said in an interview.
Restrictive eligibility criteria may not only limit access to minority populations, but also may slow clinical trial accrual and completion, and make it harder to generalize clinical trial findings to the overall population, said Dr. Michaelis, associate professor of medicine in the division of hematology and oncology, Medical College of Wisconsin, Milwaukee.
The study by Dr. Statler and colleagues included 1,040 AML patients who received chemotherapy at Cleveland Clinic between 2003 and 2019. About 10% of the patients in the analysis were African American and 90% were white.
Median overall survival was not significantly different by race, at 13.7 months for African Americans and 14.9 months for whites (P = 0.89), according to results published in the study abstract.
Mild creatinine elevation did not appear to affect survival in this study, according to the investigator. Survival was not significantly different between patients with normal creatinine and those with creatinine up to 1.5 times the upper limit of normal. However, higher levels of creatinine were significantly associated with worse survival, Dr. Statler said.
Further analyses showed that these survival findings by creatinine level held up specifically in the African American subgroup as well, Dr. Statler said in the press conference.
Dr. Statler provided no disclosures related to the presentation. Study coauthors described disclosures related to Amgen, SimulStat, Bristol-Myers Squibb, Takeda, Pfizer, Novartis, Celgene Corporation, Abbvie, and Incyte, among others.
SOURCE: Statler A et al. ASH 2019, Abstract 381.
REPORTING FROM ASH 2019
Will TP53-mutated AML respond to immunotherapy?
NATIONAL HARBOR, MD. – New research has shown increased immune infiltration in patients with TP53-mutated acute myeloid leukemia (AML).
Patients with TP53-mutated AML had higher levels of T-cell infiltration, immune checkpoint molecules, and interferon (IFN)–gamma signaling than patients with wild-type TP53.
These findings may indicate that patients with TP53-mutated AML will respond to T-cell targeting immunotherapies, but more investigation is needed, according to Sergio Rutella, MD, PhD, of Nottingham (England) Trent University.
Dr. Rutella described the findings at the annual meeting of the Society for Immunotherapy of Cancer.
He and his colleagues recently identified subgroups of AML, called “immune infiltrated” and “immune depleted,” that can predict chemotherapy resistance and response to flotetuzumab (ASH 2019, Abstract 460). However, the team has not determined the genetic drivers of immune infiltration in AML.*
With the current study, Dr. Rutella and his colleagues wanted to determine if TP53 mutations are associated with the AML immune milieu and see if TP53-mutated patients might benefit from immunotherapy.
Discovery cohort
The researchers first analyzed 147 patients with non-promyelocytic AML from the Cancer Genome Atlas. In total, 9% of these patients (n = 13) had TP53-mutated AML. The researchers assessed how 45 immune gene and biological activity signatures correlated with prognostic molecular lesions (TP53 mutations, FLT3-ITD, etc.) and clinical outcomes in this cohort.
The data showed that immune subtypes were associated with overall survival (OS). The median OS was 11.8 months in patients with immune-infiltrated AML, 16.4 months in patients with intermediate AML, and 25.8 months in patients with immune-depleted AML.
The inflammatory chemokine score (P = .011), IDO1 score (P = .027), IFN-gamma score (P = .036), and B7H3 score (P = .045) were all significantly associated with OS. In fact, these factors were all better predictors of OS than cytogenetic risk score (P = .049).
The IFN-gamma score, inflammatory chemokine score, and lymphoid score were all significantly higher in TP53-mutated patients than in patients with RUNX1 mutations, NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .05).
Likewise, the tumor inflammation signature score was significantly higher among TP53-mutated patients than among patients with NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .01).
Validation cohort and bone marrow samples
The researchers also looked at data from a validation cohort, which consisted of 140 patients with non-promyelocytic AML in the Beat AML Master Trial. Twelve percent of these patients (n = 17) had TP53 mutations.
Data in this cohort showed that CD3G messenger RNA (mRNA) was significantly higher in TP53-mutated AML than in TP53-wild-type AML (P = .04). The same was true for CD8A mRNA (P = .0002) and GZMB mRNA (P = .0005).
Likewise, IFN-gamma mRNA (P = .0052), IFIT2 mRNA (P = .0064), and IFIT3 mRNA (P = .003) were all significantly higher in patients with TP53-mutated AML.
Lastly, the researchers analyzed gene expression profiles of bone marrow samples from patients with AML, 36 with mutated TP53 and 24 with wild-type TP53.
The team found that IFN-gamma–induced genes (IFNG and IRF1), markers of T-cell infiltration (CD8A and CD3G) and senescence (EOMES, KLRD1, and HRAS), immune checkpoint molecules (IDO1, LAG3, PDL1, and VISTA), effector function molecules (GZMB, GZMK, and GZMM), and proinflammatory cytokines (IL17A and TNF) were all significantly overexpressed in TP53-mutated AML.
Among the top overexpressed genes in TP53-mutated AML were genes associated with IFN signaling and inflammation pathways – IL-33, IL-6, IFN-gamma, OASL, RIPK2, TNFAIP3, CSF1, and PTGER4. The IL-17 and TNF signaling pathways were the most enriched pathways in TP53-mutated AML.
“Our analysis of primary bone marrow samples showed that TP53-mutated samples are enriched in IL-17, TNF, and IFN signaling molecules, and show higher levels of T-cell infiltrations and immune checkpoints relative to their wild-type counterparts,” Dr. Rutella said.
“The in silico analysis indicated that TP53-mutated cases will show higher levels of T-cell infiltration, immune checkpoints, and IFN-gamma signaling, compared with AML subgroups without risk-defining molecular lesions,” he added. “This is speculative. Whether TP53-mutated AML can be amenable to respond to T-cell targeting immunotherapies is still to be determined.”
Dr. Rutella reported research support from NanoString Technologies, MacroGenics, and Kura Oncology.
SOURCE: Rutella S et al. SITC 2019. Abstract O3.
*This article was updated on 11/19/2019.
NATIONAL HARBOR, MD. – New research has shown increased immune infiltration in patients with TP53-mutated acute myeloid leukemia (AML).
Patients with TP53-mutated AML had higher levels of T-cell infiltration, immune checkpoint molecules, and interferon (IFN)–gamma signaling than patients with wild-type TP53.
These findings may indicate that patients with TP53-mutated AML will respond to T-cell targeting immunotherapies, but more investigation is needed, according to Sergio Rutella, MD, PhD, of Nottingham (England) Trent University.
Dr. Rutella described the findings at the annual meeting of the Society for Immunotherapy of Cancer.
He and his colleagues recently identified subgroups of AML, called “immune infiltrated” and “immune depleted,” that can predict chemotherapy resistance and response to flotetuzumab (ASH 2019, Abstract 460). However, the team has not determined the genetic drivers of immune infiltration in AML.*
With the current study, Dr. Rutella and his colleagues wanted to determine if TP53 mutations are associated with the AML immune milieu and see if TP53-mutated patients might benefit from immunotherapy.
Discovery cohort
The researchers first analyzed 147 patients with non-promyelocytic AML from the Cancer Genome Atlas. In total, 9% of these patients (n = 13) had TP53-mutated AML. The researchers assessed how 45 immune gene and biological activity signatures correlated with prognostic molecular lesions (TP53 mutations, FLT3-ITD, etc.) and clinical outcomes in this cohort.
The data showed that immune subtypes were associated with overall survival (OS). The median OS was 11.8 months in patients with immune-infiltrated AML, 16.4 months in patients with intermediate AML, and 25.8 months in patients with immune-depleted AML.
The inflammatory chemokine score (P = .011), IDO1 score (P = .027), IFN-gamma score (P = .036), and B7H3 score (P = .045) were all significantly associated with OS. In fact, these factors were all better predictors of OS than cytogenetic risk score (P = .049).
The IFN-gamma score, inflammatory chemokine score, and lymphoid score were all significantly higher in TP53-mutated patients than in patients with RUNX1 mutations, NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .05).
Likewise, the tumor inflammation signature score was significantly higher among TP53-mutated patients than among patients with NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .01).
Validation cohort and bone marrow samples
The researchers also looked at data from a validation cohort, which consisted of 140 patients with non-promyelocytic AML in the Beat AML Master Trial. Twelve percent of these patients (n = 17) had TP53 mutations.
Data in this cohort showed that CD3G messenger RNA (mRNA) was significantly higher in TP53-mutated AML than in TP53-wild-type AML (P = .04). The same was true for CD8A mRNA (P = .0002) and GZMB mRNA (P = .0005).
Likewise, IFN-gamma mRNA (P = .0052), IFIT2 mRNA (P = .0064), and IFIT3 mRNA (P = .003) were all significantly higher in patients with TP53-mutated AML.
Lastly, the researchers analyzed gene expression profiles of bone marrow samples from patients with AML, 36 with mutated TP53 and 24 with wild-type TP53.
The team found that IFN-gamma–induced genes (IFNG and IRF1), markers of T-cell infiltration (CD8A and CD3G) and senescence (EOMES, KLRD1, and HRAS), immune checkpoint molecules (IDO1, LAG3, PDL1, and VISTA), effector function molecules (GZMB, GZMK, and GZMM), and proinflammatory cytokines (IL17A and TNF) were all significantly overexpressed in TP53-mutated AML.
Among the top overexpressed genes in TP53-mutated AML were genes associated with IFN signaling and inflammation pathways – IL-33, IL-6, IFN-gamma, OASL, RIPK2, TNFAIP3, CSF1, and PTGER4. The IL-17 and TNF signaling pathways were the most enriched pathways in TP53-mutated AML.
“Our analysis of primary bone marrow samples showed that TP53-mutated samples are enriched in IL-17, TNF, and IFN signaling molecules, and show higher levels of T-cell infiltrations and immune checkpoints relative to their wild-type counterparts,” Dr. Rutella said.
“The in silico analysis indicated that TP53-mutated cases will show higher levels of T-cell infiltration, immune checkpoints, and IFN-gamma signaling, compared with AML subgroups without risk-defining molecular lesions,” he added. “This is speculative. Whether TP53-mutated AML can be amenable to respond to T-cell targeting immunotherapies is still to be determined.”
Dr. Rutella reported research support from NanoString Technologies, MacroGenics, and Kura Oncology.
SOURCE: Rutella S et al. SITC 2019. Abstract O3.
*This article was updated on 11/19/2019.
NATIONAL HARBOR, MD. – New research has shown increased immune infiltration in patients with TP53-mutated acute myeloid leukemia (AML).
Patients with TP53-mutated AML had higher levels of T-cell infiltration, immune checkpoint molecules, and interferon (IFN)–gamma signaling than patients with wild-type TP53.
These findings may indicate that patients with TP53-mutated AML will respond to T-cell targeting immunotherapies, but more investigation is needed, according to Sergio Rutella, MD, PhD, of Nottingham (England) Trent University.
Dr. Rutella described the findings at the annual meeting of the Society for Immunotherapy of Cancer.
He and his colleagues recently identified subgroups of AML, called “immune infiltrated” and “immune depleted,” that can predict chemotherapy resistance and response to flotetuzumab (ASH 2019, Abstract 460). However, the team has not determined the genetic drivers of immune infiltration in AML.*
With the current study, Dr. Rutella and his colleagues wanted to determine if TP53 mutations are associated with the AML immune milieu and see if TP53-mutated patients might benefit from immunotherapy.
Discovery cohort
The researchers first analyzed 147 patients with non-promyelocytic AML from the Cancer Genome Atlas. In total, 9% of these patients (n = 13) had TP53-mutated AML. The researchers assessed how 45 immune gene and biological activity signatures correlated with prognostic molecular lesions (TP53 mutations, FLT3-ITD, etc.) and clinical outcomes in this cohort.
The data showed that immune subtypes were associated with overall survival (OS). The median OS was 11.8 months in patients with immune-infiltrated AML, 16.4 months in patients with intermediate AML, and 25.8 months in patients with immune-depleted AML.
The inflammatory chemokine score (P = .011), IDO1 score (P = .027), IFN-gamma score (P = .036), and B7H3 score (P = .045) were all significantly associated with OS. In fact, these factors were all better predictors of OS than cytogenetic risk score (P = .049).
The IFN-gamma score, inflammatory chemokine score, and lymphoid score were all significantly higher in TP53-mutated patients than in patients with RUNX1 mutations, NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .05).
Likewise, the tumor inflammation signature score was significantly higher among TP53-mutated patients than among patients with NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .01).
Validation cohort and bone marrow samples
The researchers also looked at data from a validation cohort, which consisted of 140 patients with non-promyelocytic AML in the Beat AML Master Trial. Twelve percent of these patients (n = 17) had TP53 mutations.
Data in this cohort showed that CD3G messenger RNA (mRNA) was significantly higher in TP53-mutated AML than in TP53-wild-type AML (P = .04). The same was true for CD8A mRNA (P = .0002) and GZMB mRNA (P = .0005).
Likewise, IFN-gamma mRNA (P = .0052), IFIT2 mRNA (P = .0064), and IFIT3 mRNA (P = .003) were all significantly higher in patients with TP53-mutated AML.
Lastly, the researchers analyzed gene expression profiles of bone marrow samples from patients with AML, 36 with mutated TP53 and 24 with wild-type TP53.
The team found that IFN-gamma–induced genes (IFNG and IRF1), markers of T-cell infiltration (CD8A and CD3G) and senescence (EOMES, KLRD1, and HRAS), immune checkpoint molecules (IDO1, LAG3, PDL1, and VISTA), effector function molecules (GZMB, GZMK, and GZMM), and proinflammatory cytokines (IL17A and TNF) were all significantly overexpressed in TP53-mutated AML.
Among the top overexpressed genes in TP53-mutated AML were genes associated with IFN signaling and inflammation pathways – IL-33, IL-6, IFN-gamma, OASL, RIPK2, TNFAIP3, CSF1, and PTGER4. The IL-17 and TNF signaling pathways were the most enriched pathways in TP53-mutated AML.
“Our analysis of primary bone marrow samples showed that TP53-mutated samples are enriched in IL-17, TNF, and IFN signaling molecules, and show higher levels of T-cell infiltrations and immune checkpoints relative to their wild-type counterparts,” Dr. Rutella said.
“The in silico analysis indicated that TP53-mutated cases will show higher levels of T-cell infiltration, immune checkpoints, and IFN-gamma signaling, compared with AML subgroups without risk-defining molecular lesions,” he added. “This is speculative. Whether TP53-mutated AML can be amenable to respond to T-cell targeting immunotherapies is still to be determined.”
Dr. Rutella reported research support from NanoString Technologies, MacroGenics, and Kura Oncology.
SOURCE: Rutella S et al. SITC 2019. Abstract O3.
*This article was updated on 11/19/2019.
REPORTING FROM SITC 2019
Caspofungin bests fluconazole for antifungal prophylaxis in young AML patients
Antifungal prophylaxis with caspofungin led to a lower incidence of invasive fungal disease, compared with fluconazole, in children and young adults with acute myeloid leukemia (AML), according to new study findings.
The results suggest caspofungin may be an appropriate prophylactic strategy to prevent invasive fungal disease in younger patients with newly diagnosed AML, reported Brian T. Fisher, DO, of the University of Pennsylvania, Philadelphia, and colleagues. The study was published in JAMA.
The randomized, open-label study included 517 children, adolescents, and young adults with de novo, relapsed, or secondary AML. Study patients received treatment in 115 centers throughout United States and Canada. The median age of patients in the study was 9 years (range, 0-26 years); 56% were male and approximately 69% were white.
Study subjects were randomly assigned to receive antifungal prophylaxis with 70 mg/m2 (maximum dose 70 mg/day) of intravenous caspofungin on day 1, followed by 50 mg/m2 per day (maximum dose 50 mg/day) thereafter, or age-dosed intravenous or oral fluconazole.
Prophylactic therapy was initiated 24-72 hours after the completion of each chemotherapy cycle, and was maintained until the end of the neutropenic period following each cycle.
At 5-month follow-up, the cumulative incidence rate of probable or proven invasive fungal disease was 3.1% (95% confidence interval, 1.3%-7.0%) in the caspofungin arm, compared with 7.2% (95% CI, 4.4%-11.8%) in the fluconazole arm (overall P = .03).
In addition, the 5-month cumulative incidence rate of probable or proven invasive aspergillosis infection was 0.5% (95%CI, 0.1%-3.5%) in patients who received caspofungin, compared with 3.1% (95% CI, 1.4%-6.9%) in patients who received fluconazole (overall P = .046).
“No statistically significant differences in empirical antifungal therapy or 2-year overall survival were observed,” they reported.
With respect to safety, the most frequently reported adverse events were hypokalemia (22 events in the caspofungin arm vs. 13 in the fluconazole arm), respiratory failure (6 events in the caspofungin arm vs. 9 in the fluconazole arm), and elevated alanine transaminase (4 events in the caspofungin arm vs. 8 in the fluconazole arm).
The researchers acknowledged a key limitation of the study was the short duration of follow-up. As a result, the precision of some comparative measures may have been reduced.
The National Cancer Institute funded the study. The authors reported financial affiliations with Astellas, Celgene, Leadiant Biosciences, Merck, Nabriva Therapeutics, Novartis, Pfizer, Shire, and T2 Biosystems.
SOURCE: Fisher BT et al. JAMA. 2019;322(17):1673-81.
Antifungal prophylaxis with caspofungin led to a lower incidence of invasive fungal disease, compared with fluconazole, in children and young adults with acute myeloid leukemia (AML), according to new study findings.
The results suggest caspofungin may be an appropriate prophylactic strategy to prevent invasive fungal disease in younger patients with newly diagnosed AML, reported Brian T. Fisher, DO, of the University of Pennsylvania, Philadelphia, and colleagues. The study was published in JAMA.
The randomized, open-label study included 517 children, adolescents, and young adults with de novo, relapsed, or secondary AML. Study patients received treatment in 115 centers throughout United States and Canada. The median age of patients in the study was 9 years (range, 0-26 years); 56% were male and approximately 69% were white.
Study subjects were randomly assigned to receive antifungal prophylaxis with 70 mg/m2 (maximum dose 70 mg/day) of intravenous caspofungin on day 1, followed by 50 mg/m2 per day (maximum dose 50 mg/day) thereafter, or age-dosed intravenous or oral fluconazole.
Prophylactic therapy was initiated 24-72 hours after the completion of each chemotherapy cycle, and was maintained until the end of the neutropenic period following each cycle.
At 5-month follow-up, the cumulative incidence rate of probable or proven invasive fungal disease was 3.1% (95% confidence interval, 1.3%-7.0%) in the caspofungin arm, compared with 7.2% (95% CI, 4.4%-11.8%) in the fluconazole arm (overall P = .03).
In addition, the 5-month cumulative incidence rate of probable or proven invasive aspergillosis infection was 0.5% (95%CI, 0.1%-3.5%) in patients who received caspofungin, compared with 3.1% (95% CI, 1.4%-6.9%) in patients who received fluconazole (overall P = .046).
“No statistically significant differences in empirical antifungal therapy or 2-year overall survival were observed,” they reported.
With respect to safety, the most frequently reported adverse events were hypokalemia (22 events in the caspofungin arm vs. 13 in the fluconazole arm), respiratory failure (6 events in the caspofungin arm vs. 9 in the fluconazole arm), and elevated alanine transaminase (4 events in the caspofungin arm vs. 8 in the fluconazole arm).
The researchers acknowledged a key limitation of the study was the short duration of follow-up. As a result, the precision of some comparative measures may have been reduced.
The National Cancer Institute funded the study. The authors reported financial affiliations with Astellas, Celgene, Leadiant Biosciences, Merck, Nabriva Therapeutics, Novartis, Pfizer, Shire, and T2 Biosystems.
SOURCE: Fisher BT et al. JAMA. 2019;322(17):1673-81.
Antifungal prophylaxis with caspofungin led to a lower incidence of invasive fungal disease, compared with fluconazole, in children and young adults with acute myeloid leukemia (AML), according to new study findings.
The results suggest caspofungin may be an appropriate prophylactic strategy to prevent invasive fungal disease in younger patients with newly diagnosed AML, reported Brian T. Fisher, DO, of the University of Pennsylvania, Philadelphia, and colleagues. The study was published in JAMA.
The randomized, open-label study included 517 children, adolescents, and young adults with de novo, relapsed, or secondary AML. Study patients received treatment in 115 centers throughout United States and Canada. The median age of patients in the study was 9 years (range, 0-26 years); 56% were male and approximately 69% were white.
Study subjects were randomly assigned to receive antifungal prophylaxis with 70 mg/m2 (maximum dose 70 mg/day) of intravenous caspofungin on day 1, followed by 50 mg/m2 per day (maximum dose 50 mg/day) thereafter, or age-dosed intravenous or oral fluconazole.
Prophylactic therapy was initiated 24-72 hours after the completion of each chemotherapy cycle, and was maintained until the end of the neutropenic period following each cycle.
At 5-month follow-up, the cumulative incidence rate of probable or proven invasive fungal disease was 3.1% (95% confidence interval, 1.3%-7.0%) in the caspofungin arm, compared with 7.2% (95% CI, 4.4%-11.8%) in the fluconazole arm (overall P = .03).
In addition, the 5-month cumulative incidence rate of probable or proven invasive aspergillosis infection was 0.5% (95%CI, 0.1%-3.5%) in patients who received caspofungin, compared with 3.1% (95% CI, 1.4%-6.9%) in patients who received fluconazole (overall P = .046).
“No statistically significant differences in empirical antifungal therapy or 2-year overall survival were observed,” they reported.
With respect to safety, the most frequently reported adverse events were hypokalemia (22 events in the caspofungin arm vs. 13 in the fluconazole arm), respiratory failure (6 events in the caspofungin arm vs. 9 in the fluconazole arm), and elevated alanine transaminase (4 events in the caspofungin arm vs. 8 in the fluconazole arm).
The researchers acknowledged a key limitation of the study was the short duration of follow-up. As a result, the precision of some comparative measures may have been reduced.
The National Cancer Institute funded the study. The authors reported financial affiliations with Astellas, Celgene, Leadiant Biosciences, Merck, Nabriva Therapeutics, Novartis, Pfizer, Shire, and T2 Biosystems.
SOURCE: Fisher BT et al. JAMA. 2019;322(17):1673-81.
FROM JAMA
Hematopoietic cell transplant offers realistic cure in secondary AML
yielding significantly better survival outcomes, according to findings from an observational study.
Although secondary AML has been identified as an independent predictor of poor prognosis, it is not included in current risk classifications that provide the basis of deciding when to perform HCT.
Christer Nilsson, MD, of Karolinska Institute, Stockholm, and colleagues, used two nationwide Swedish registries – the Swedish AML Registry and the Swedish Cancer Registry – to characterize how often HCT is performed in these patients and to evaluate its impact in a real-world setting. The registries include all patients with AML diagnosed between 1997 and 2013.
Their findings are in Biology of Blood and Marrow Transplantation.
The analysis included 3,337 adult patients with AML who were intensively treated and did not have acute promyelocytic leukemia. More than three-quarters of the patients had de novo AML and the remainder had secondary AML that was either therapy related or developed after an antecedent myeloid disease. In total, 100 patients with secondary AML underwent HCT while in first complete remission.
In terms of crude survival at 5 years after diagnosis, patients with secondary AML who did not undergo HCT did very poorly. The survival rate was 0% in those with AML preceded by myeloproliferative neoplasm (MPN-AML), 2% in patients with AML preceded by myelodysplastic syndrome (MDS-AML), and 4% in patients with therapy-related AML (t-AML). In contrast, the 5-year overall survival in patients who underwent HCT at any time point or disease stage was 32% for patients with MPN-AML, 18% for patients with MDS-AML, and 25% for patients t-AML.
These crude survival figures suggest that “HCT is the sole realistic curable treatment option for [secondary] AML,” the researchers wrote.
The researchers also performed a propensity score matching analysis of HCT versus chemotherapy consolidation in patients with secondary AML who had been in first complete remission for more than 90 days. The model matched 45 patients who underwent HCT with 66 patients treated with chemotherapy consolidation. The projected 5-year overall survival was 48% in the HCT group, compared with 20% in the consolidation group (P = .01). Similarly, 5-year relapse-free survival was also higher in the HCT group, compared with the consolidation group (43% vs. 21%, P = .02).
“Ideally, the role of transplantation in [secondary] AML should be evaluated in a prospective randomized trial, minimizing the risk of any bias,” the researchers wrote. “However, such a trial is lacking and most likely will never be performed.”
The researchers concluded that HCT should be considered for all patients with secondary AML who are eligible and fit for transplantation.
The study was supported by the Swedish Cancer Foundation, Swedish Research Council, Stockholm County Council, Gothenberg Medical Society, and Assar Gabrielsson Foundation. The researchers reported having no conflicts of interest.
SOURCE: Nilson C et al. Biol Blood Marrow Tranplant. 2019;25:1770-8.
yielding significantly better survival outcomes, according to findings from an observational study.
Although secondary AML has been identified as an independent predictor of poor prognosis, it is not included in current risk classifications that provide the basis of deciding when to perform HCT.
Christer Nilsson, MD, of Karolinska Institute, Stockholm, and colleagues, used two nationwide Swedish registries – the Swedish AML Registry and the Swedish Cancer Registry – to characterize how often HCT is performed in these patients and to evaluate its impact in a real-world setting. The registries include all patients with AML diagnosed between 1997 and 2013.
Their findings are in Biology of Blood and Marrow Transplantation.
The analysis included 3,337 adult patients with AML who were intensively treated and did not have acute promyelocytic leukemia. More than three-quarters of the patients had de novo AML and the remainder had secondary AML that was either therapy related or developed after an antecedent myeloid disease. In total, 100 patients with secondary AML underwent HCT while in first complete remission.
In terms of crude survival at 5 years after diagnosis, patients with secondary AML who did not undergo HCT did very poorly. The survival rate was 0% in those with AML preceded by myeloproliferative neoplasm (MPN-AML), 2% in patients with AML preceded by myelodysplastic syndrome (MDS-AML), and 4% in patients with therapy-related AML (t-AML). In contrast, the 5-year overall survival in patients who underwent HCT at any time point or disease stage was 32% for patients with MPN-AML, 18% for patients with MDS-AML, and 25% for patients t-AML.
These crude survival figures suggest that “HCT is the sole realistic curable treatment option for [secondary] AML,” the researchers wrote.
The researchers also performed a propensity score matching analysis of HCT versus chemotherapy consolidation in patients with secondary AML who had been in first complete remission for more than 90 days. The model matched 45 patients who underwent HCT with 66 patients treated with chemotherapy consolidation. The projected 5-year overall survival was 48% in the HCT group, compared with 20% in the consolidation group (P = .01). Similarly, 5-year relapse-free survival was also higher in the HCT group, compared with the consolidation group (43% vs. 21%, P = .02).
“Ideally, the role of transplantation in [secondary] AML should be evaluated in a prospective randomized trial, minimizing the risk of any bias,” the researchers wrote. “However, such a trial is lacking and most likely will never be performed.”
The researchers concluded that HCT should be considered for all patients with secondary AML who are eligible and fit for transplantation.
The study was supported by the Swedish Cancer Foundation, Swedish Research Council, Stockholm County Council, Gothenberg Medical Society, and Assar Gabrielsson Foundation. The researchers reported having no conflicts of interest.
SOURCE: Nilson C et al. Biol Blood Marrow Tranplant. 2019;25:1770-8.
yielding significantly better survival outcomes, according to findings from an observational study.
Although secondary AML has been identified as an independent predictor of poor prognosis, it is not included in current risk classifications that provide the basis of deciding when to perform HCT.
Christer Nilsson, MD, of Karolinska Institute, Stockholm, and colleagues, used two nationwide Swedish registries – the Swedish AML Registry and the Swedish Cancer Registry – to characterize how often HCT is performed in these patients and to evaluate its impact in a real-world setting. The registries include all patients with AML diagnosed between 1997 and 2013.
Their findings are in Biology of Blood and Marrow Transplantation.
The analysis included 3,337 adult patients with AML who were intensively treated and did not have acute promyelocytic leukemia. More than three-quarters of the patients had de novo AML and the remainder had secondary AML that was either therapy related or developed after an antecedent myeloid disease. In total, 100 patients with secondary AML underwent HCT while in first complete remission.
In terms of crude survival at 5 years after diagnosis, patients with secondary AML who did not undergo HCT did very poorly. The survival rate was 0% in those with AML preceded by myeloproliferative neoplasm (MPN-AML), 2% in patients with AML preceded by myelodysplastic syndrome (MDS-AML), and 4% in patients with therapy-related AML (t-AML). In contrast, the 5-year overall survival in patients who underwent HCT at any time point or disease stage was 32% for patients with MPN-AML, 18% for patients with MDS-AML, and 25% for patients t-AML.
These crude survival figures suggest that “HCT is the sole realistic curable treatment option for [secondary] AML,” the researchers wrote.
The researchers also performed a propensity score matching analysis of HCT versus chemotherapy consolidation in patients with secondary AML who had been in first complete remission for more than 90 days. The model matched 45 patients who underwent HCT with 66 patients treated with chemotherapy consolidation. The projected 5-year overall survival was 48% in the HCT group, compared with 20% in the consolidation group (P = .01). Similarly, 5-year relapse-free survival was also higher in the HCT group, compared with the consolidation group (43% vs. 21%, P = .02).
“Ideally, the role of transplantation in [secondary] AML should be evaluated in a prospective randomized trial, minimizing the risk of any bias,” the researchers wrote. “However, such a trial is lacking and most likely will never be performed.”
The researchers concluded that HCT should be considered for all patients with secondary AML who are eligible and fit for transplantation.
The study was supported by the Swedish Cancer Foundation, Swedish Research Council, Stockholm County Council, Gothenberg Medical Society, and Assar Gabrielsson Foundation. The researchers reported having no conflicts of interest.
SOURCE: Nilson C et al. Biol Blood Marrow Tranplant. 2019;25:1770-8.
FROM BIOLOGY OF BLOOD AND MARROW TRANSPLANTATION
Adverse cytogenetics trump molecular risk in NPM1-mutated AML
A pooled analysis suggests adverse cytogenetics are a key factor negatively impacting outcomes in patients with NPM1mut/FLT3-ITDneg/low acute myeloid leukemia (AML).
In patients with adverse chromosomal abnormalities, NPM1 mutational status was found not to confer a favorable outcome. The findings suggest cytogenetic risk outweighs molecular risk in patients with NPM1 mutations and the FLT3-ITDneg/low genotype.
“Patients carrying adverse-risk cytogenetics shared a virtually identical unfavorable outcome, regardless of whether the otherwise beneficial NPM1mut/FLT3-ITDneg/low status was present. The type of the adverse chromosomal abnormality did not seem to influence this effect, although low numbers might obscure detection of heterogeneity among individual aberrations,” Linus Angenendt, MD, of University Hospital Munster (Germany) and colleagues, wrote in the Journal of Clinical Oncology.
The researchers retrospectively analyzed 2,426 patients with NPM1mut/FLT3-ITDneg/low AML. Of these, 17.6% had an abnormal karyotype, and 3.4% had adverse-risk chromosomal aberrations.
Prior to analysis, individual patient data were pooled from nine international AML study group registries or treatment centers.
After analysis, the researchers found that adverse cytogenetics were associated with inferior complete remission rates (66.3%), compared with in patients with normal karyotype or intermediate-risk cytogenetic abnormalities (87.7% and 86.0%, respectively; P less than .001). The complete remission rates for the NPM1mut/FLT3-ITDneg/low AML adverse cytogenetics group was similar to patients with NPM1wt/FLT3-ITDneg/low and adverse cytogenetic abnormalities (66.3% vs. 57.5%).
Five-year event-free survival rates and overall survival rates were also lower in patients with NPM1mut/FLT3-ITDneg/low AML and adverse cytogenetics, compared with patients with normal karyotype or intermediate-risk cytogenetic abnormalities (P less than .001).
“Even though the combination of an NPM1 mutation with these abnormalities is rare, the prognostic effect of adverse cytogenetics in NPM1mut AML has important implications for postremission treatment decisions, in particular, the current recommendation that patients who are NPM1mut/FLT3-ITDneg/low not receive allogeneic hematopoietic stem cell transplantation (HSCT), given their presumed low risk of relapse might be altered if the adverse karyotype increased the risk,” they wrote.
The type of chromosomal aberration did not appear to impact this effect, but the small sample size may have hindered the ability to detect a difference between different abnormalities, the researchers noted.
One key limitation of the study was the retrospective design. As a result, in patients with an abnormal karyotype, some genetic analyses could have been underutilized.
“These results demand additional validation within prospective trials,” the researchers concluded.
The study was funded by the University of Munster Medical School, the German Research Foundation, the French government, the Ministry of Health of the Czech Republic, and others. The authors reported financial affiliations with numerous pharmaceutical companies.
SOURCE: Angenendt L et al. J Clin Oncol. 2019 Oct 10;37(29):2632-42.
A pooled analysis suggests adverse cytogenetics are a key factor negatively impacting outcomes in patients with NPM1mut/FLT3-ITDneg/low acute myeloid leukemia (AML).
In patients with adverse chromosomal abnormalities, NPM1 mutational status was found not to confer a favorable outcome. The findings suggest cytogenetic risk outweighs molecular risk in patients with NPM1 mutations and the FLT3-ITDneg/low genotype.
“Patients carrying adverse-risk cytogenetics shared a virtually identical unfavorable outcome, regardless of whether the otherwise beneficial NPM1mut/FLT3-ITDneg/low status was present. The type of the adverse chromosomal abnormality did not seem to influence this effect, although low numbers might obscure detection of heterogeneity among individual aberrations,” Linus Angenendt, MD, of University Hospital Munster (Germany) and colleagues, wrote in the Journal of Clinical Oncology.
The researchers retrospectively analyzed 2,426 patients with NPM1mut/FLT3-ITDneg/low AML. Of these, 17.6% had an abnormal karyotype, and 3.4% had adverse-risk chromosomal aberrations.
Prior to analysis, individual patient data were pooled from nine international AML study group registries or treatment centers.
After analysis, the researchers found that adverse cytogenetics were associated with inferior complete remission rates (66.3%), compared with in patients with normal karyotype or intermediate-risk cytogenetic abnormalities (87.7% and 86.0%, respectively; P less than .001). The complete remission rates for the NPM1mut/FLT3-ITDneg/low AML adverse cytogenetics group was similar to patients with NPM1wt/FLT3-ITDneg/low and adverse cytogenetic abnormalities (66.3% vs. 57.5%).
Five-year event-free survival rates and overall survival rates were also lower in patients with NPM1mut/FLT3-ITDneg/low AML and adverse cytogenetics, compared with patients with normal karyotype or intermediate-risk cytogenetic abnormalities (P less than .001).
“Even though the combination of an NPM1 mutation with these abnormalities is rare, the prognostic effect of adverse cytogenetics in NPM1mut AML has important implications for postremission treatment decisions, in particular, the current recommendation that patients who are NPM1mut/FLT3-ITDneg/low not receive allogeneic hematopoietic stem cell transplantation (HSCT), given their presumed low risk of relapse might be altered if the adverse karyotype increased the risk,” they wrote.
The type of chromosomal aberration did not appear to impact this effect, but the small sample size may have hindered the ability to detect a difference between different abnormalities, the researchers noted.
One key limitation of the study was the retrospective design. As a result, in patients with an abnormal karyotype, some genetic analyses could have been underutilized.
“These results demand additional validation within prospective trials,” the researchers concluded.
The study was funded by the University of Munster Medical School, the German Research Foundation, the French government, the Ministry of Health of the Czech Republic, and others. The authors reported financial affiliations with numerous pharmaceutical companies.
SOURCE: Angenendt L et al. J Clin Oncol. 2019 Oct 10;37(29):2632-42.
A pooled analysis suggests adverse cytogenetics are a key factor negatively impacting outcomes in patients with NPM1mut/FLT3-ITDneg/low acute myeloid leukemia (AML).
In patients with adverse chromosomal abnormalities, NPM1 mutational status was found not to confer a favorable outcome. The findings suggest cytogenetic risk outweighs molecular risk in patients with NPM1 mutations and the FLT3-ITDneg/low genotype.
“Patients carrying adverse-risk cytogenetics shared a virtually identical unfavorable outcome, regardless of whether the otherwise beneficial NPM1mut/FLT3-ITDneg/low status was present. The type of the adverse chromosomal abnormality did not seem to influence this effect, although low numbers might obscure detection of heterogeneity among individual aberrations,” Linus Angenendt, MD, of University Hospital Munster (Germany) and colleagues, wrote in the Journal of Clinical Oncology.
The researchers retrospectively analyzed 2,426 patients with NPM1mut/FLT3-ITDneg/low AML. Of these, 17.6% had an abnormal karyotype, and 3.4% had adverse-risk chromosomal aberrations.
Prior to analysis, individual patient data were pooled from nine international AML study group registries or treatment centers.
After analysis, the researchers found that adverse cytogenetics were associated with inferior complete remission rates (66.3%), compared with in patients with normal karyotype or intermediate-risk cytogenetic abnormalities (87.7% and 86.0%, respectively; P less than .001). The complete remission rates for the NPM1mut/FLT3-ITDneg/low AML adverse cytogenetics group was similar to patients with NPM1wt/FLT3-ITDneg/low and adverse cytogenetic abnormalities (66.3% vs. 57.5%).
Five-year event-free survival rates and overall survival rates were also lower in patients with NPM1mut/FLT3-ITDneg/low AML and adverse cytogenetics, compared with patients with normal karyotype or intermediate-risk cytogenetic abnormalities (P less than .001).
“Even though the combination of an NPM1 mutation with these abnormalities is rare, the prognostic effect of adverse cytogenetics in NPM1mut AML has important implications for postremission treatment decisions, in particular, the current recommendation that patients who are NPM1mut/FLT3-ITDneg/low not receive allogeneic hematopoietic stem cell transplantation (HSCT), given their presumed low risk of relapse might be altered if the adverse karyotype increased the risk,” they wrote.
The type of chromosomal aberration did not appear to impact this effect, but the small sample size may have hindered the ability to detect a difference between different abnormalities, the researchers noted.
One key limitation of the study was the retrospective design. As a result, in patients with an abnormal karyotype, some genetic analyses could have been underutilized.
“These results demand additional validation within prospective trials,” the researchers concluded.
The study was funded by the University of Munster Medical School, the German Research Foundation, the French government, the Ministry of Health of the Czech Republic, and others. The authors reported financial affiliations with numerous pharmaceutical companies.
SOURCE: Angenendt L et al. J Clin Oncol. 2019 Oct 10;37(29):2632-42.
REPORTING FROM THE JOURNAL OF CLINICAL ONCOLOGY
Genetic analysis highlights value of germline variants in MDS, AML
Germline DDX41 mutations were found to be relatively prevalent and showed favorable outcomes in a cohort of patients with myelodysplastic syndromes or acute myeloid leukemia, according to a genetic analysis.
The results demonstrate that systematic genetic testing for DDX41 mutations may aid in clinical decision making for adults with myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML).
“We screened a large, unselected cohort of adult patients diagnosed with MDS/AML to analyze the biological and clinical features of DDX41-related myeloid malignancies,” wrote Marie Sébert, MD, PhD, of Hôpital Saint Louis in Paris and colleagues. The results were published in Blood.
The researchers used next-generation sequencing to analyze blood and bone marrow samples from 1,385 patients with MDS or AML to detect DDX41 mutations. A variant allele frequency of greater than 0.4 was regarded as indicative of a germline origin, and only specific variants (minor allele frequency of less than 0.01) were included.
The team analyzed various parameters relevant to DDX41-related myeloid disorders, including patient demographics, karyotyping, and treatment response rates, in addition to the prevalence of DDX41-related malignancies.
A total of 28 distinct germline DDX41 variants were detected among 43 unrelated patients. The researchers classified 21 of the variants as causal, with the rest being of unknown significance.
“We focused on the 33 patients having causal variants, representing 2.4% of our cohort,” they wrote.
The majority of patients with DDX41-related MDS/AML were male, with a median age of 69 years. Few patients (27%) had a family history of blood malignancies, while the majority of patients (85%) had a normal karyotype.
With respect to treatment, most high-risk patients received either azacitidine or intensive chemotherapy, with overall response rates of 73% and 100%, respectively. The median overall survival was 5.2 years.
There are currently no consensus recommendations on genetic counseling and follow-up of asymptomatic carriers and more studies are needed to refine clinical management and genetic counseling, the researchers wrote. “However, in our experience, DDX41-mutated patients frequently presented mild cytopenias years before overt hematological myeloid malignancy, suggesting that watchful surveillance would allow the detection of disease evolution.”
No funding sources were reported, and the authors reported having no conflicts of interest.
SOURCE: Sébert M et al. Blood. 2019 Sep 4. doi: 10.1182/blood.2019000909.
Germline DDX41 mutations were found to be relatively prevalent and showed favorable outcomes in a cohort of patients with myelodysplastic syndromes or acute myeloid leukemia, according to a genetic analysis.
The results demonstrate that systematic genetic testing for DDX41 mutations may aid in clinical decision making for adults with myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML).
“We screened a large, unselected cohort of adult patients diagnosed with MDS/AML to analyze the biological and clinical features of DDX41-related myeloid malignancies,” wrote Marie Sébert, MD, PhD, of Hôpital Saint Louis in Paris and colleagues. The results were published in Blood.
The researchers used next-generation sequencing to analyze blood and bone marrow samples from 1,385 patients with MDS or AML to detect DDX41 mutations. A variant allele frequency of greater than 0.4 was regarded as indicative of a germline origin, and only specific variants (minor allele frequency of less than 0.01) were included.
The team analyzed various parameters relevant to DDX41-related myeloid disorders, including patient demographics, karyotyping, and treatment response rates, in addition to the prevalence of DDX41-related malignancies.
A total of 28 distinct germline DDX41 variants were detected among 43 unrelated patients. The researchers classified 21 of the variants as causal, with the rest being of unknown significance.
“We focused on the 33 patients having causal variants, representing 2.4% of our cohort,” they wrote.
The majority of patients with DDX41-related MDS/AML were male, with a median age of 69 years. Few patients (27%) had a family history of blood malignancies, while the majority of patients (85%) had a normal karyotype.
With respect to treatment, most high-risk patients received either azacitidine or intensive chemotherapy, with overall response rates of 73% and 100%, respectively. The median overall survival was 5.2 years.
There are currently no consensus recommendations on genetic counseling and follow-up of asymptomatic carriers and more studies are needed to refine clinical management and genetic counseling, the researchers wrote. “However, in our experience, DDX41-mutated patients frequently presented mild cytopenias years before overt hematological myeloid malignancy, suggesting that watchful surveillance would allow the detection of disease evolution.”
No funding sources were reported, and the authors reported having no conflicts of interest.
SOURCE: Sébert M et al. Blood. 2019 Sep 4. doi: 10.1182/blood.2019000909.
Germline DDX41 mutations were found to be relatively prevalent and showed favorable outcomes in a cohort of patients with myelodysplastic syndromes or acute myeloid leukemia, according to a genetic analysis.
The results demonstrate that systematic genetic testing for DDX41 mutations may aid in clinical decision making for adults with myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML).
“We screened a large, unselected cohort of adult patients diagnosed with MDS/AML to analyze the biological and clinical features of DDX41-related myeloid malignancies,” wrote Marie Sébert, MD, PhD, of Hôpital Saint Louis in Paris and colleagues. The results were published in Blood.
The researchers used next-generation sequencing to analyze blood and bone marrow samples from 1,385 patients with MDS or AML to detect DDX41 mutations. A variant allele frequency of greater than 0.4 was regarded as indicative of a germline origin, and only specific variants (minor allele frequency of less than 0.01) were included.
The team analyzed various parameters relevant to DDX41-related myeloid disorders, including patient demographics, karyotyping, and treatment response rates, in addition to the prevalence of DDX41-related malignancies.
A total of 28 distinct germline DDX41 variants were detected among 43 unrelated patients. The researchers classified 21 of the variants as causal, with the rest being of unknown significance.
“We focused on the 33 patients having causal variants, representing 2.4% of our cohort,” they wrote.
The majority of patients with DDX41-related MDS/AML were male, with a median age of 69 years. Few patients (27%) had a family history of blood malignancies, while the majority of patients (85%) had a normal karyotype.
With respect to treatment, most high-risk patients received either azacitidine or intensive chemotherapy, with overall response rates of 73% and 100%, respectively. The median overall survival was 5.2 years.
There are currently no consensus recommendations on genetic counseling and follow-up of asymptomatic carriers and more studies are needed to refine clinical management and genetic counseling, the researchers wrote. “However, in our experience, DDX41-mutated patients frequently presented mild cytopenias years before overt hematological myeloid malignancy, suggesting that watchful surveillance would allow the detection of disease evolution.”
No funding sources were reported, and the authors reported having no conflicts of interest.
SOURCE: Sébert M et al. Blood. 2019 Sep 4. doi: 10.1182/blood.2019000909.
FROM BLOOD