User login
Global burden of hematologic malignancies
Research has shown an increase in the global incidence of leukemia and non-Hodgkin lymphoma (NHL) in recent years.
The Global Burden of Disease (GBD) study showed that, from 2006 to 2016, the incidence of NHL increased 45%, and the incidence of leukemia increased 26%.
These increases were largely due to population growth and aging.
Results from the GDB study were published in JAMA Oncology.
The study indicated that, in 2016, there were 17.2 million cases of cancer worldwide and 8.9 million cancer deaths.
One in 3 men were likely to get cancer during their lifetime, as were 1 in 5 women. Cancer was associated with 213.2 million disability-adjusted life years (DALYs).
The following table lists the 2016 global incidence and mortality figures for all cancers combined and for individual hematologic malignancies.
| Cancer type | Cases, thousands | Deaths, thousands |
| All cancers | 17,228 | 8927 |
| Leukemias | 467 | 310 |
| Acute lymphoid leukemia | 76 | 51 |
| Chronic lymphoid leukemia | 105 | 35 |
| Acute myeloid leukemia | 103 | 85 |
| Chronic myeloid leukemia | 32 | 22 |
| Other leukemias | 150 | 117 |
| Hodgkin lymphoma | 73 | 29 |
| NHL | 461 | 240 |
| Multiple myeloma | 139 | 98 |
Leukemia
In 2016, there were 467,000 new cases of leukemia and 310,000 leukemia deaths. Leukemia was responsible for 10.2 million DALYs. Leukemia developed in 1 in 118 men and 1 in 194 women worldwide.
Between 2006 and 2016, the global leukemia incidence increased by 26%—from 370,482 to 466,802 cases.
The researchers said the factors contributing to this increase were population growth (12%), population aging (10%), and an increase in age-specific incidence rates (3%).
NHL
In 2016, there were 461,000 new cases of NHL and 240,000 NHL deaths. NHL was responsible for 6.8 million DALYs. NHL developed in 1 in 110 men and 1 in 161 women worldwide.
Between 2006 and 2016, NHL increased by 45%, from 319,078 to 461,164 cases.
The factors contributing to this increase were increasing age-specific incidence rates (17%), changing population age structure (15%), and population growth (12%).
“A large proportion of the increase in cancer incidence can be explained by improving life expectancy and population growth—a development that can at least partially be attributed to a reduced burden from other common diseases,” the study authors wrote.
The authors also pointed out that prevention efforts are less effective for hematologic malignancies than for other cancers.
Research has shown an increase in the global incidence of leukemia and non-Hodgkin lymphoma (NHL) in recent years.
The Global Burden of Disease (GBD) study showed that, from 2006 to 2016, the incidence of NHL increased 45%, and the incidence of leukemia increased 26%.
These increases were largely due to population growth and aging.
Results from the GDB study were published in JAMA Oncology.
The study indicated that, in 2016, there were 17.2 million cases of cancer worldwide and 8.9 million cancer deaths.
One in 3 men were likely to get cancer during their lifetime, as were 1 in 5 women. Cancer was associated with 213.2 million disability-adjusted life years (DALYs).
The following table lists the 2016 global incidence and mortality figures for all cancers combined and for individual hematologic malignancies.
| Cancer type | Cases, thousands | Deaths, thousands |
| All cancers | 17,228 | 8927 |
| Leukemias | 467 | 310 |
| Acute lymphoid leukemia | 76 | 51 |
| Chronic lymphoid leukemia | 105 | 35 |
| Acute myeloid leukemia | 103 | 85 |
| Chronic myeloid leukemia | 32 | 22 |
| Other leukemias | 150 | 117 |
| Hodgkin lymphoma | 73 | 29 |
| NHL | 461 | 240 |
| Multiple myeloma | 139 | 98 |
Leukemia
In 2016, there were 467,000 new cases of leukemia and 310,000 leukemia deaths. Leukemia was responsible for 10.2 million DALYs. Leukemia developed in 1 in 118 men and 1 in 194 women worldwide.
Between 2006 and 2016, the global leukemia incidence increased by 26%—from 370,482 to 466,802 cases.
The researchers said the factors contributing to this increase were population growth (12%), population aging (10%), and an increase in age-specific incidence rates (3%).
NHL
In 2016, there were 461,000 new cases of NHL and 240,000 NHL deaths. NHL was responsible for 6.8 million DALYs. NHL developed in 1 in 110 men and 1 in 161 women worldwide.
Between 2006 and 2016, NHL increased by 45%, from 319,078 to 461,164 cases.
The factors contributing to this increase were increasing age-specific incidence rates (17%), changing population age structure (15%), and population growth (12%).
“A large proportion of the increase in cancer incidence can be explained by improving life expectancy and population growth—a development that can at least partially be attributed to a reduced burden from other common diseases,” the study authors wrote.
The authors also pointed out that prevention efforts are less effective for hematologic malignancies than for other cancers.
Research has shown an increase in the global incidence of leukemia and non-Hodgkin lymphoma (NHL) in recent years.
The Global Burden of Disease (GBD) study showed that, from 2006 to 2016, the incidence of NHL increased 45%, and the incidence of leukemia increased 26%.
These increases were largely due to population growth and aging.
Results from the GDB study were published in JAMA Oncology.
The study indicated that, in 2016, there were 17.2 million cases of cancer worldwide and 8.9 million cancer deaths.
One in 3 men were likely to get cancer during their lifetime, as were 1 in 5 women. Cancer was associated with 213.2 million disability-adjusted life years (DALYs).
The following table lists the 2016 global incidence and mortality figures for all cancers combined and for individual hematologic malignancies.
| Cancer type | Cases, thousands | Deaths, thousands |
| All cancers | 17,228 | 8927 |
| Leukemias | 467 | 310 |
| Acute lymphoid leukemia | 76 | 51 |
| Chronic lymphoid leukemia | 105 | 35 |
| Acute myeloid leukemia | 103 | 85 |
| Chronic myeloid leukemia | 32 | 22 |
| Other leukemias | 150 | 117 |
| Hodgkin lymphoma | 73 | 29 |
| NHL | 461 | 240 |
| Multiple myeloma | 139 | 98 |
Leukemia
In 2016, there were 467,000 new cases of leukemia and 310,000 leukemia deaths. Leukemia was responsible for 10.2 million DALYs. Leukemia developed in 1 in 118 men and 1 in 194 women worldwide.
Between 2006 and 2016, the global leukemia incidence increased by 26%—from 370,482 to 466,802 cases.
The researchers said the factors contributing to this increase were population growth (12%), population aging (10%), and an increase in age-specific incidence rates (3%).
NHL
In 2016, there were 461,000 new cases of NHL and 240,000 NHL deaths. NHL was responsible for 6.8 million DALYs. NHL developed in 1 in 110 men and 1 in 161 women worldwide.
Between 2006 and 2016, NHL increased by 45%, from 319,078 to 461,164 cases.
The factors contributing to this increase were increasing age-specific incidence rates (17%), changing population age structure (15%), and population growth (12%).
“A large proportion of the increase in cancer incidence can be explained by improving life expectancy and population growth—a development that can at least partially be attributed to a reduced burden from other common diseases,” the study authors wrote.
The authors also pointed out that prevention efforts are less effective for hematologic malignancies than for other cancers.
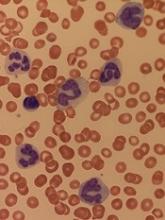
Study could change treatment of MLSM7
New findings could help improve treatment of an inherited bone marrow disorder known as myelodysplasia and leukemia syndrome with monosomy 7 (MLSM7), according to researchers.
While studying families affected by MLSM7, researchers identified germline mutations in SAMD9L or SAMD9 in patients who had hematologic abnormalities, myelodysplastic syndromes (MDS), or acute myeloid leukemia (AML).
However, these mutations were also present in apparently healthy family members, and the researchers found that bone marrow monosomy 7 sometimes resolved without treatment.
The team recounted these findings in JCI Insight.
The researchers analyzed blood samples from 16 siblings in 5 families affected by MLSM7 and found they all carried germline mutations in SAMD9 or SAMD9L. In 3 of the 5 families, there were apparently healthy parents who also carried the mutations.
“Surprisingly, the health consequences of these mutations varied tremendously for reasons that must still be determined, but the findings are already affecting how we may choose to manage these patients,” said study author Jeffery Klco, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Three of the 16 siblings developed AML and died of the disease or related complications. Two other siblings were diagnosed with MDS.
The remaining 11 siblings with the mutations were apparently healthy, although several had been treated for anemia and other conditions associated with low blood counts.
Some of these patients had a previous history of bone marrow monosomy 7 that spontaneously corrected over time. These patients, despite no therapy, appeared to have normal bone marrow function.
“This was an even greater surprise,” Dr Klco said. “The spontaneous recovery experienced by some children with the germline mutations suggests some patients with SAMD9 and SAMD9L mutations who were previously considered candidates for bone marrow transplantation may recover hematologic function on their own.”
Dr Klco and his colleagues have a theory that could explain the spontaneous correction. The team noted that SAMD9 and SAMD9L are activated in response to viral infections. While the normal function of both proteins is poorly understood, abnormally activated SAMD9 and SAMD9L are known to inhibit cell growth.
In this study, deep sequencing showed that selective pressure on developing blood cells favors cells without the SAMD9 or SAMD9L mutations. That may increase pressure for cells to selectively jettison chromosome 7 with the gene alteration or take other molecular measures to counteract the mutant protein.
Implications for treatment
This research also showed that, in patients who developed AML, loss of chromosome 7 was associated with the development of mutations in additional genes, including ETV6, KRAS, SETBP1, and RUNX1.
These same mutations are broadly associated with monosomy 7 in AML, which suggests that understanding how SAMD9 and SAMD9L mutations contribute to leukemia has implications beyond familial cases.
The presence of secondary mutations may also help clinicians identify which patients will benefit from immediate treatment, including chemotherapy or transplant to prevent or treat AML or myelodysplasia, Dr Klco said.
For patients without the mutations or significant symptoms due to low blood cell counts, watchful waiting with careful follow-up may sometimes be an option.
“Now that we know this disease can resolve without treatment in some patients, we need to focus on developing screening and treatment guidelines,” Dr Klco said. “We want to reserve hematopoietic bone marrow transplantation for those who truly need the procedure. These findings will help to point the way.”
“So little is known about SAMD9 and SAMD9L that we need to continue working in the lab to better understand how these mutations impact blood cell development and how they are activated in response to infections and other types of stress.”
New findings could help improve treatment of an inherited bone marrow disorder known as myelodysplasia and leukemia syndrome with monosomy 7 (MLSM7), according to researchers.
While studying families affected by MLSM7, researchers identified germline mutations in SAMD9L or SAMD9 in patients who had hematologic abnormalities, myelodysplastic syndromes (MDS), or acute myeloid leukemia (AML).
However, these mutations were also present in apparently healthy family members, and the researchers found that bone marrow monosomy 7 sometimes resolved without treatment.
The team recounted these findings in JCI Insight.
The researchers analyzed blood samples from 16 siblings in 5 families affected by MLSM7 and found they all carried germline mutations in SAMD9 or SAMD9L. In 3 of the 5 families, there were apparently healthy parents who also carried the mutations.
“Surprisingly, the health consequences of these mutations varied tremendously for reasons that must still be determined, but the findings are already affecting how we may choose to manage these patients,” said study author Jeffery Klco, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Three of the 16 siblings developed AML and died of the disease or related complications. Two other siblings were diagnosed with MDS.
The remaining 11 siblings with the mutations were apparently healthy, although several had been treated for anemia and other conditions associated with low blood counts.
Some of these patients had a previous history of bone marrow monosomy 7 that spontaneously corrected over time. These patients, despite no therapy, appeared to have normal bone marrow function.
“This was an even greater surprise,” Dr Klco said. “The spontaneous recovery experienced by some children with the germline mutations suggests some patients with SAMD9 and SAMD9L mutations who were previously considered candidates for bone marrow transplantation may recover hematologic function on their own.”
Dr Klco and his colleagues have a theory that could explain the spontaneous correction. The team noted that SAMD9 and SAMD9L are activated in response to viral infections. While the normal function of both proteins is poorly understood, abnormally activated SAMD9 and SAMD9L are known to inhibit cell growth.
In this study, deep sequencing showed that selective pressure on developing blood cells favors cells without the SAMD9 or SAMD9L mutations. That may increase pressure for cells to selectively jettison chromosome 7 with the gene alteration or take other molecular measures to counteract the mutant protein.
Implications for treatment
This research also showed that, in patients who developed AML, loss of chromosome 7 was associated with the development of mutations in additional genes, including ETV6, KRAS, SETBP1, and RUNX1.
These same mutations are broadly associated with monosomy 7 in AML, which suggests that understanding how SAMD9 and SAMD9L mutations contribute to leukemia has implications beyond familial cases.
The presence of secondary mutations may also help clinicians identify which patients will benefit from immediate treatment, including chemotherapy or transplant to prevent or treat AML or myelodysplasia, Dr Klco said.
For patients without the mutations or significant symptoms due to low blood cell counts, watchful waiting with careful follow-up may sometimes be an option.
“Now that we know this disease can resolve without treatment in some patients, we need to focus on developing screening and treatment guidelines,” Dr Klco said. “We want to reserve hematopoietic bone marrow transplantation for those who truly need the procedure. These findings will help to point the way.”
“So little is known about SAMD9 and SAMD9L that we need to continue working in the lab to better understand how these mutations impact blood cell development and how they are activated in response to infections and other types of stress.”
New findings could help improve treatment of an inherited bone marrow disorder known as myelodysplasia and leukemia syndrome with monosomy 7 (MLSM7), according to researchers.
While studying families affected by MLSM7, researchers identified germline mutations in SAMD9L or SAMD9 in patients who had hematologic abnormalities, myelodysplastic syndromes (MDS), or acute myeloid leukemia (AML).
However, these mutations were also present in apparently healthy family members, and the researchers found that bone marrow monosomy 7 sometimes resolved without treatment.
The team recounted these findings in JCI Insight.
The researchers analyzed blood samples from 16 siblings in 5 families affected by MLSM7 and found they all carried germline mutations in SAMD9 or SAMD9L. In 3 of the 5 families, there were apparently healthy parents who also carried the mutations.
“Surprisingly, the health consequences of these mutations varied tremendously for reasons that must still be determined, but the findings are already affecting how we may choose to manage these patients,” said study author Jeffery Klco, MD, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Three of the 16 siblings developed AML and died of the disease or related complications. Two other siblings were diagnosed with MDS.
The remaining 11 siblings with the mutations were apparently healthy, although several had been treated for anemia and other conditions associated with low blood counts.
Some of these patients had a previous history of bone marrow monosomy 7 that spontaneously corrected over time. These patients, despite no therapy, appeared to have normal bone marrow function.
“This was an even greater surprise,” Dr Klco said. “The spontaneous recovery experienced by some children with the germline mutations suggests some patients with SAMD9 and SAMD9L mutations who were previously considered candidates for bone marrow transplantation may recover hematologic function on their own.”
Dr Klco and his colleagues have a theory that could explain the spontaneous correction. The team noted that SAMD9 and SAMD9L are activated in response to viral infections. While the normal function of both proteins is poorly understood, abnormally activated SAMD9 and SAMD9L are known to inhibit cell growth.
In this study, deep sequencing showed that selective pressure on developing blood cells favors cells without the SAMD9 or SAMD9L mutations. That may increase pressure for cells to selectively jettison chromosome 7 with the gene alteration or take other molecular measures to counteract the mutant protein.
Implications for treatment
This research also showed that, in patients who developed AML, loss of chromosome 7 was associated with the development of mutations in additional genes, including ETV6, KRAS, SETBP1, and RUNX1.
These same mutations are broadly associated with monosomy 7 in AML, which suggests that understanding how SAMD9 and SAMD9L mutations contribute to leukemia has implications beyond familial cases.
The presence of secondary mutations may also help clinicians identify which patients will benefit from immediate treatment, including chemotherapy or transplant to prevent or treat AML or myelodysplasia, Dr Klco said.
For patients without the mutations or significant symptoms due to low blood cell counts, watchful waiting with careful follow-up may sometimes be an option.
“Now that we know this disease can resolve without treatment in some patients, we need to focus on developing screening and treatment guidelines,” Dr Klco said. “We want to reserve hematopoietic bone marrow transplantation for those who truly need the procedure. These findings will help to point the way.”
“So little is known about SAMD9 and SAMD9L that we need to continue working in the lab to better understand how these mutations impact blood cell development and how they are activated in response to infections and other types of stress.”
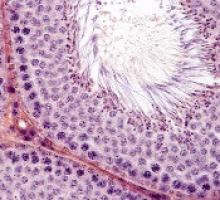
Treatments, disease affect spermatogonia in boys
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
FDA approves drug for IDH1-mutated AML
The US Food and Drug Administration (FDA) has granted full approval for the isocitrate dehydrogenase-1 (IDH1) inhibitor ivosidenib (Tibsovo®).
The drug is approved to treat adults with relapsed or refractory acute myeloid leukemia (AML) who have an IDH1 mutation, as detected by an FDA-approved test.
Ivosidenib was approved concurrently with the RealTime IDH1 Assay, a companion diagnostic that can detect IDH1 mutation.
The FDA granted approval of ivosidenib to Agios Pharmaceuticals, Inc., and approval of the RealTime IDH1 Assay to Abbott Laboratories.
The FDA’s approval of ivosidenib was based on data from a single-arm, phase 1 study. Agios received fast track, priority review, and orphan drug designations for ivosidenib.
Safety risks
Ivosidenib must be dispensed with a patient medication guide that describes important information about the drug’s uses and risks.
The prescribing information for ivosidenib includes a Boxed Warning noting that patients treated with ivosidenib have experienced symptoms of differentiation syndrome, which can be fatal if not treated.
Signs and symptoms of differentiation syndrome may include fever, dyspnea, acute respiratory distress, radiographic pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain, peripheral edema, or hepatic, renal, or multi-organ dysfunction.
At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor them closely until symptoms subside.
Ivosidenib also poses a risk of life-threatening QT prolongation and Guillain-Barré syndrome, so patients should be monitored for these adverse events (AEs) as well.
Phase 1 trial
Results from the phase 1 trial of ivosidenib were presented at the 2018 ASCO Annual Meeting and published simultaneously in NEJM. The following data were pulled from the drug’s prescribing information.
Efficacy results were available for 174 adults with relapsed/refractory AML and an IDH1 mutation identified or confirmed by the Abbott RealTime™ IDH1 assay. The patients received ivosidenib at a starting dose of 500 mg daily until disease progression, unacceptable toxicity, or hematopoietic stem cell transplant.
The patients had a median age of 67 (range, 18 to 87) and had received a median of 2 prior therapies (range, 1 to 6). Sixty-three percent were refractory to previous therapy, and 33% had secondary AML.
The study’s primary endpoint was the combined rate of complete remission (CR) rate and CR with partial hematologic improvement (CRh).
The CR+CRh rate was 32.8% (57/174), the CR rate was 24.7% (43/174), and the CRh rate was 8% (14/174).
The median duration of CR+CRh was 8.2 months (95% CI 5.6, 12). The median time to best response of CR or CRh was 2.0 months (range, 0.9 to 5.6 months).
Twelve percent of patients (21/174) went on to transplant.
The researchers evaluated the safety of ivosidenib in 179 patients treated with a dose of 500 mg daily. The median duration of exposure to ivosidenib was 3.9 months (range, 0.1 to 39.5 months).
Nineteen percent of patients (34/179) experienced differentiation syndrome. Seventy-nine percent of these patients (27/34) recovered after treatment or ivosidenib dose interruption.
The most frequent serious AEs (>5%) were differentiation syndrome (10%), leukocytosis (10%), and electrocardiogram QT prolongation (7%). There was one case of progressive multifocal leukoencephalopathy.
The most common AEs leading to dose interruption were QT prolongation (7%), differentiation syndrome (3%), leukocytosis (3%), and dyspnea (3%). AEs leading to a dose reduction included QT prolongation (1%), diarrhea (1%), nausea (1%), decreased hemoglobin (1%), and increased transaminases (1%).
AEs leading to permanent discontinuation of ivosidenib included Guillain-Barré syndrome (1%), rash (1%), stomatitis (1%), and creatinine increase (1%).
For additional data and more details on ivosidenib, see the full prescribing information or visit Tibsovo.com.
The US Food and Drug Administration (FDA) has granted full approval for the isocitrate dehydrogenase-1 (IDH1) inhibitor ivosidenib (Tibsovo®).
The drug is approved to treat adults with relapsed or refractory acute myeloid leukemia (AML) who have an IDH1 mutation, as detected by an FDA-approved test.
Ivosidenib was approved concurrently with the RealTime IDH1 Assay, a companion diagnostic that can detect IDH1 mutation.
The FDA granted approval of ivosidenib to Agios Pharmaceuticals, Inc., and approval of the RealTime IDH1 Assay to Abbott Laboratories.
The FDA’s approval of ivosidenib was based on data from a single-arm, phase 1 study. Agios received fast track, priority review, and orphan drug designations for ivosidenib.
Safety risks
Ivosidenib must be dispensed with a patient medication guide that describes important information about the drug’s uses and risks.
The prescribing information for ivosidenib includes a Boxed Warning noting that patients treated with ivosidenib have experienced symptoms of differentiation syndrome, which can be fatal if not treated.
Signs and symptoms of differentiation syndrome may include fever, dyspnea, acute respiratory distress, radiographic pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain, peripheral edema, or hepatic, renal, or multi-organ dysfunction.
At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor them closely until symptoms subside.
Ivosidenib also poses a risk of life-threatening QT prolongation and Guillain-Barré syndrome, so patients should be monitored for these adverse events (AEs) as well.
Phase 1 trial
Results from the phase 1 trial of ivosidenib were presented at the 2018 ASCO Annual Meeting and published simultaneously in NEJM. The following data were pulled from the drug’s prescribing information.
Efficacy results were available for 174 adults with relapsed/refractory AML and an IDH1 mutation identified or confirmed by the Abbott RealTime™ IDH1 assay. The patients received ivosidenib at a starting dose of 500 mg daily until disease progression, unacceptable toxicity, or hematopoietic stem cell transplant.
The patients had a median age of 67 (range, 18 to 87) and had received a median of 2 prior therapies (range, 1 to 6). Sixty-three percent were refractory to previous therapy, and 33% had secondary AML.
The study’s primary endpoint was the combined rate of complete remission (CR) rate and CR with partial hematologic improvement (CRh).
The CR+CRh rate was 32.8% (57/174), the CR rate was 24.7% (43/174), and the CRh rate was 8% (14/174).
The median duration of CR+CRh was 8.2 months (95% CI 5.6, 12). The median time to best response of CR or CRh was 2.0 months (range, 0.9 to 5.6 months).
Twelve percent of patients (21/174) went on to transplant.
The researchers evaluated the safety of ivosidenib in 179 patients treated with a dose of 500 mg daily. The median duration of exposure to ivosidenib was 3.9 months (range, 0.1 to 39.5 months).
Nineteen percent of patients (34/179) experienced differentiation syndrome. Seventy-nine percent of these patients (27/34) recovered after treatment or ivosidenib dose interruption.
The most frequent serious AEs (>5%) were differentiation syndrome (10%), leukocytosis (10%), and electrocardiogram QT prolongation (7%). There was one case of progressive multifocal leukoencephalopathy.
The most common AEs leading to dose interruption were QT prolongation (7%), differentiation syndrome (3%), leukocytosis (3%), and dyspnea (3%). AEs leading to a dose reduction included QT prolongation (1%), diarrhea (1%), nausea (1%), decreased hemoglobin (1%), and increased transaminases (1%).
AEs leading to permanent discontinuation of ivosidenib included Guillain-Barré syndrome (1%), rash (1%), stomatitis (1%), and creatinine increase (1%).
For additional data and more details on ivosidenib, see the full prescribing information or visit Tibsovo.com.
The US Food and Drug Administration (FDA) has granted full approval for the isocitrate dehydrogenase-1 (IDH1) inhibitor ivosidenib (Tibsovo®).
The drug is approved to treat adults with relapsed or refractory acute myeloid leukemia (AML) who have an IDH1 mutation, as detected by an FDA-approved test.
Ivosidenib was approved concurrently with the RealTime IDH1 Assay, a companion diagnostic that can detect IDH1 mutation.
The FDA granted approval of ivosidenib to Agios Pharmaceuticals, Inc., and approval of the RealTime IDH1 Assay to Abbott Laboratories.
The FDA’s approval of ivosidenib was based on data from a single-arm, phase 1 study. Agios received fast track, priority review, and orphan drug designations for ivosidenib.
Safety risks
Ivosidenib must be dispensed with a patient medication guide that describes important information about the drug’s uses and risks.
The prescribing information for ivosidenib includes a Boxed Warning noting that patients treated with ivosidenib have experienced symptoms of differentiation syndrome, which can be fatal if not treated.
Signs and symptoms of differentiation syndrome may include fever, dyspnea, acute respiratory distress, radiographic pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain, peripheral edema, or hepatic, renal, or multi-organ dysfunction.
At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor them closely until symptoms subside.
Ivosidenib also poses a risk of life-threatening QT prolongation and Guillain-Barré syndrome, so patients should be monitored for these adverse events (AEs) as well.
Phase 1 trial
Results from the phase 1 trial of ivosidenib were presented at the 2018 ASCO Annual Meeting and published simultaneously in NEJM. The following data were pulled from the drug’s prescribing information.
Efficacy results were available for 174 adults with relapsed/refractory AML and an IDH1 mutation identified or confirmed by the Abbott RealTime™ IDH1 assay. The patients received ivosidenib at a starting dose of 500 mg daily until disease progression, unacceptable toxicity, or hematopoietic stem cell transplant.
The patients had a median age of 67 (range, 18 to 87) and had received a median of 2 prior therapies (range, 1 to 6). Sixty-three percent were refractory to previous therapy, and 33% had secondary AML.
The study’s primary endpoint was the combined rate of complete remission (CR) rate and CR with partial hematologic improvement (CRh).
The CR+CRh rate was 32.8% (57/174), the CR rate was 24.7% (43/174), and the CRh rate was 8% (14/174).
The median duration of CR+CRh was 8.2 months (95% CI 5.6, 12). The median time to best response of CR or CRh was 2.0 months (range, 0.9 to 5.6 months).
Twelve percent of patients (21/174) went on to transplant.
The researchers evaluated the safety of ivosidenib in 179 patients treated with a dose of 500 mg daily. The median duration of exposure to ivosidenib was 3.9 months (range, 0.1 to 39.5 months).
Nineteen percent of patients (34/179) experienced differentiation syndrome. Seventy-nine percent of these patients (27/34) recovered after treatment or ivosidenib dose interruption.
The most frequent serious AEs (>5%) were differentiation syndrome (10%), leukocytosis (10%), and electrocardiogram QT prolongation (7%). There was one case of progressive multifocal leukoencephalopathy.
The most common AEs leading to dose interruption were QT prolongation (7%), differentiation syndrome (3%), leukocytosis (3%), and dyspnea (3%). AEs leading to a dose reduction included QT prolongation (1%), diarrhea (1%), nausea (1%), decreased hemoglobin (1%), and increased transaminases (1%).
AEs leading to permanent discontinuation of ivosidenib included Guillain-Barré syndrome (1%), rash (1%), stomatitis (1%), and creatinine increase (1%).
For additional data and more details on ivosidenib, see the full prescribing information or visit Tibsovo.com.
FDA approves biosimilar filgrastim
The US Food and Drug Administration (FDA) has approved the leukocyte growth factor Nivestym™ (filgrastim-aafi), a biosimilar to Neupogen (filgrastim).
Nivestym is approved to treat patients with nonmyeloid malignancies who are receiving myelosuppressive chemotherapy or undergoing bone marrow transplant, acute myeloid leukemia patients receiving induction or consolidation chemotherapy, patients undergoing autologous peripheral blood progenitor cell collection, and patients with severe chronic neutropenia.
The FDA’s approval of Nivestym was based on a review of evidence suggesting the drug is highly similar to Neupogen, according to Pfizer, the company developing Nivestym.
The full approved indication for Nivestym is as follows:
- To decrease the incidence of infection, as manifested by febrile neutropenia, in patients with nonmyeloid malignancies receiving myelosuppressive anticancer drugs associated with a significant incidence of severe neutropenia with fever
- To reduce the time to neutrophil recovery and the duration of fever following induction or consolidation chemotherapy in patients with acute myeloid leukemia
- To reduce the duration of neutropenia and neutropenia-related clinical sequelae (eg, febrile neutropenia) in patients with nonmyeloid malignancies undergoing myeloablative chemotherapy followed by bone marrow transplant
- For the mobilization of autologous hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis
- For chronic administration to reduce the incidence and duration of sequelae of severe neutropenia (eg, fever, infections, oropharyngeal ulcers) in symptomatic patients with congenital neutropenia, cyclic neutropenia, or idiopathic neutropenia.
For more details on Nivestym, see the full prescribing information.
The US Food and Drug Administration (FDA) has approved the leukocyte growth factor Nivestym™ (filgrastim-aafi), a biosimilar to Neupogen (filgrastim).
Nivestym is approved to treat patients with nonmyeloid malignancies who are receiving myelosuppressive chemotherapy or undergoing bone marrow transplant, acute myeloid leukemia patients receiving induction or consolidation chemotherapy, patients undergoing autologous peripheral blood progenitor cell collection, and patients with severe chronic neutropenia.
The FDA’s approval of Nivestym was based on a review of evidence suggesting the drug is highly similar to Neupogen, according to Pfizer, the company developing Nivestym.
The full approved indication for Nivestym is as follows:
- To decrease the incidence of infection, as manifested by febrile neutropenia, in patients with nonmyeloid malignancies receiving myelosuppressive anticancer drugs associated with a significant incidence of severe neutropenia with fever
- To reduce the time to neutrophil recovery and the duration of fever following induction or consolidation chemotherapy in patients with acute myeloid leukemia
- To reduce the duration of neutropenia and neutropenia-related clinical sequelae (eg, febrile neutropenia) in patients with nonmyeloid malignancies undergoing myeloablative chemotherapy followed by bone marrow transplant
- For the mobilization of autologous hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis
- For chronic administration to reduce the incidence and duration of sequelae of severe neutropenia (eg, fever, infections, oropharyngeal ulcers) in symptomatic patients with congenital neutropenia, cyclic neutropenia, or idiopathic neutropenia.
For more details on Nivestym, see the full prescribing information.
The US Food and Drug Administration (FDA) has approved the leukocyte growth factor Nivestym™ (filgrastim-aafi), a biosimilar to Neupogen (filgrastim).
Nivestym is approved to treat patients with nonmyeloid malignancies who are receiving myelosuppressive chemotherapy or undergoing bone marrow transplant, acute myeloid leukemia patients receiving induction or consolidation chemotherapy, patients undergoing autologous peripheral blood progenitor cell collection, and patients with severe chronic neutropenia.
The FDA’s approval of Nivestym was based on a review of evidence suggesting the drug is highly similar to Neupogen, according to Pfizer, the company developing Nivestym.
The full approved indication for Nivestym is as follows:
- To decrease the incidence of infection, as manifested by febrile neutropenia, in patients with nonmyeloid malignancies receiving myelosuppressive anticancer drugs associated with a significant incidence of severe neutropenia with fever
- To reduce the time to neutrophil recovery and the duration of fever following induction or consolidation chemotherapy in patients with acute myeloid leukemia
- To reduce the duration of neutropenia and neutropenia-related clinical sequelae (eg, febrile neutropenia) in patients with nonmyeloid malignancies undergoing myeloablative chemotherapy followed by bone marrow transplant
- For the mobilization of autologous hematopoietic progenitor cells into the peripheral blood for collection by leukapheresis
- For chronic administration to reduce the incidence and duration of sequelae of severe neutropenia (eg, fever, infections, oropharyngeal ulcers) in symptomatic patients with congenital neutropenia, cyclic neutropenia, or idiopathic neutropenia.
For more details on Nivestym, see the full prescribing information.
FDA approves Nivestym, second biosimilar to Neupogen
Nivestym (filgrastim-aafi), a biosimilar to Neupogen (filgrastim) was approved July 20 by the Food and Drug Administration, according to a statement provided by the agency. Nivestym is the second biosimilar to Neupogen to be approved in the United States.
- Patients with cancer receiving myelosuppressive chemotherapy.
- Patients with acute myeloid leukemia receiving induction or consolidation chemotherapy.
- Patients with cancer undergoing bone marrow transplantation.
- Patients undergoing autologous peripheral blood progenitor cell collection and therapy.
- Patients with severe chronic neutropenia.
According to a press release from Pfizer, the manufacturer of the biosimilar, Nivestym is expected to be available in the United States at a significant discount to the current wholesale acquisition cost of Neupogen, which is not inclusive of discounts to payers, providers, distributors, and other purchasing organizations.
The FDA statement notes that a biosimilar is approved based on a showing that it is highly similar to an already approved biologic product, known as a reference product. The biosimilar also must be shown to have no clinically meaningful differences in terms of safety and effectiveness from the reference product. Only minor differences in clinically inactive components are allowable in biosimilar products.
Prescribing information is available here.
Nivestym (filgrastim-aafi), a biosimilar to Neupogen (filgrastim) was approved July 20 by the Food and Drug Administration, according to a statement provided by the agency. Nivestym is the second biosimilar to Neupogen to be approved in the United States.
- Patients with cancer receiving myelosuppressive chemotherapy.
- Patients with acute myeloid leukemia receiving induction or consolidation chemotherapy.
- Patients with cancer undergoing bone marrow transplantation.
- Patients undergoing autologous peripheral blood progenitor cell collection and therapy.
- Patients with severe chronic neutropenia.
According to a press release from Pfizer, the manufacturer of the biosimilar, Nivestym is expected to be available in the United States at a significant discount to the current wholesale acquisition cost of Neupogen, which is not inclusive of discounts to payers, providers, distributors, and other purchasing organizations.
The FDA statement notes that a biosimilar is approved based on a showing that it is highly similar to an already approved biologic product, known as a reference product. The biosimilar also must be shown to have no clinically meaningful differences in terms of safety and effectiveness from the reference product. Only minor differences in clinically inactive components are allowable in biosimilar products.
Prescribing information is available here.
Nivestym (filgrastim-aafi), a biosimilar to Neupogen (filgrastim) was approved July 20 by the Food and Drug Administration, according to a statement provided by the agency. Nivestym is the second biosimilar to Neupogen to be approved in the United States.
- Patients with cancer receiving myelosuppressive chemotherapy.
- Patients with acute myeloid leukemia receiving induction or consolidation chemotherapy.
- Patients with cancer undergoing bone marrow transplantation.
- Patients undergoing autologous peripheral blood progenitor cell collection and therapy.
- Patients with severe chronic neutropenia.
According to a press release from Pfizer, the manufacturer of the biosimilar, Nivestym is expected to be available in the United States at a significant discount to the current wholesale acquisition cost of Neupogen, which is not inclusive of discounts to payers, providers, distributors, and other purchasing organizations.
The FDA statement notes that a biosimilar is approved based on a showing that it is highly similar to an already approved biologic product, known as a reference product. The biosimilar also must be shown to have no clinically meaningful differences in terms of safety and effectiveness from the reference product. Only minor differences in clinically inactive components are allowable in biosimilar products.
Prescribing information is available here.
FDA approves IDH1 inhibitor for relapsed/refractory AML
The Food and Drug Administration has approved ivosidenib (Tibsovo) as the first treatment of adult patients with relapsed/refractory acute myeloid leukemia (AML) and an isocitrate dehydrogenase-1 (IDH1) mutation.
More specifically, the oral treatment has been approved for patients whose mutations have been identified by the Abbott RealTime IDH1 assay, a companion diagnostic test.
The approval was based on results from a phase 1, open-label, single-arm, multicenter, dose-escalation and expansion trial of adult patients in this AML population. The primary end point was combined complete remission and complete remission with partial hematologic improvement; this combined rate was 32.8%, and the median duration of this remission was 8.2 months.
The most serious adverse events included differentiation syndrome, QTc prolongation, and Guillain-Barré syndrome. Other adverse reactions included fatigue, leukocytosis, arthralgia, diarrhea, dyspnea, edema, and constipation.
Ivosidenib is marketed as Tibsovo by Agios Pharmaceuticals. The RealTime IDH1 Assay is marketed by Abbott Laboratories.
The Food and Drug Administration has approved ivosidenib (Tibsovo) as the first treatment of adult patients with relapsed/refractory acute myeloid leukemia (AML) and an isocitrate dehydrogenase-1 (IDH1) mutation.
More specifically, the oral treatment has been approved for patients whose mutations have been identified by the Abbott RealTime IDH1 assay, a companion diagnostic test.
The approval was based on results from a phase 1, open-label, single-arm, multicenter, dose-escalation and expansion trial of adult patients in this AML population. The primary end point was combined complete remission and complete remission with partial hematologic improvement; this combined rate was 32.8%, and the median duration of this remission was 8.2 months.
The most serious adverse events included differentiation syndrome, QTc prolongation, and Guillain-Barré syndrome. Other adverse reactions included fatigue, leukocytosis, arthralgia, diarrhea, dyspnea, edema, and constipation.
Ivosidenib is marketed as Tibsovo by Agios Pharmaceuticals. The RealTime IDH1 Assay is marketed by Abbott Laboratories.
The Food and Drug Administration has approved ivosidenib (Tibsovo) as the first treatment of adult patients with relapsed/refractory acute myeloid leukemia (AML) and an isocitrate dehydrogenase-1 (IDH1) mutation.
More specifically, the oral treatment has been approved for patients whose mutations have been identified by the Abbott RealTime IDH1 assay, a companion diagnostic test.
The approval was based on results from a phase 1, open-label, single-arm, multicenter, dose-escalation and expansion trial of adult patients in this AML population. The primary end point was combined complete remission and complete remission with partial hematologic improvement; this combined rate was 32.8%, and the median duration of this remission was 8.2 months.
The most serious adverse events included differentiation syndrome, QTc prolongation, and Guillain-Barré syndrome. Other adverse reactions included fatigue, leukocytosis, arthralgia, diarrhea, dyspnea, edema, and constipation.
Ivosidenib is marketed as Tibsovo by Agios Pharmaceuticals. The RealTime IDH1 Assay is marketed by Abbott Laboratories.
Diabetics have higher risk of hematologic, other cancers
A review of data from more than 19 million people indicates that diabetes significantly raises a person’s risk of developing cancer.
When researchers compared patients with diabetes and without, both male and female diabetics had an increased risk of leukemias and lymphomas as well as certain solid tumors.
Researchers also found that diabetes conferred a higher cancer risk for women than men, both for all cancers combined and for some specific cancers, including leukemia.
“The link between diabetes and the risk of developing cancer is now firmly established,” said Toshiaki Ohkuma, PhD, of The George Institute for Global Health at the University of New South Wales in Australia.
“We have also demonstrated, for the first time, that women with diabetes are more likely to develop any form of cancer and have a significantly higher chance of developing kidney, oral, and stomach cancers and leukemia.”
Dr Ohkuma and his colleagues reported these findings in Diabetologia.
The researchers conducted a systematic search in PubMed MEDLINE to identify reports on the links between diabetes and cancer. Additional reports were identified from the reference lists of the relevant studies.
Only those cohort studies providing relative risks (RRs) for the association between diabetes and cancer for both women and men were included. In total, 107 relevant articles were identified, along with 36 cohorts of individual participant data.
RRs for cancer were obtained for patients with diabetes (types 1 and 2 combined) versus those without diabetes, for both men and women. The women-to-men ratios of these relative risk ratios (RRRs) were then calculated to determine the excess risk in women if present.
Data on all-site cancer was available from 47 studies, involving 121 cohorts and 19,239,302 individuals.
Diabetics vs non-diabetics
Women with diabetes had a 27% higher risk of all-site cancer compared to women without diabetes (RR=1.27; 95% CI 1.21, 1.32; P<0.001).
For men, the risk of all-site cancer was 19% higher among those with diabetes than those without (RR=1.19; 95% CI 1.13, 1.25; P<0.001).
There were several hematologic malignancies for which diabetics had an increased risk, as shown in the following table.
| Cancer type | RR for women (99% CI) | RR for men (99% CI) |
| Lymphatic and hematopoietic tissue | 1.24 (1.05, 1.46)* | 1.21 (0.98, 1.48) |
| Leukemia | 1.53 (1.00, 2.33) | 1.22 (0.80, 1.85) |
| Myeloid leukemia | 0.83 (0.39, 1.76) | 1.12 (0.77, 1.62) |
| Acute myeloid leukemia | 1.33 (1.12, 1.57)* | 1.14 (0.56, 2.33) |
| Chronic myeloid leukemia | 1.67 (1.27, 2.20)* | 1.62 (1.32, 1.98)* |
| Lymphoid leukemia | 1.74 (0.31, 9.79) | 1.20 (0.86, 1.68) |
| Lymphoma | 2.31 (0.57, 9.30) | 1.80 (0.68, 4.75) |
| Non-Hodgkin lymphoma | 1.16 (1.02, 1.32)* | 1.20 (1.08, 1.34)* |
| Hodgkin lymphoma | 1.20 (0.61, 2.38) | 1.36 (1.05, 1.77)* |
| Multiple myeloma | 1.19 (0.97, 1.47) | 1.12 (0.90, 1.41) |
| *denotes statistical significance with a P value < 0.01 | ||
Sex comparison
Calculation of the women-to-men ratio revealed that women with diabetes had a 6% greater excess risk of all-site cancer compared to men with diabetes (RRR=1.06; 95% CI 1.03, 1.09; P<0.001).
The women-to-men ratios also showed significantly higher risks for female diabetics for:
- Kidney cancer—RRR=1.11 (99% CI 1.04, 1.18; P<0.001)
- Oral cancer—RRR=1.13 (99% CI 1.00, 1.28; P=0.009)
- Stomach cancer—RRR=1.14 (99% CI 1.07, 1.22; P<0.001)
- Leukemia—RRR=1.15 (99% CI 1.02, 1.28; P=0.002).
However, women had a significantly lower risk of liver cancer (RRR=0.88; 99% CI 0.79, 0.99; P=0.005).
There are several possible reasons for the excess cancer risk observed in women, according to study author Sanne Peters, PhD, of The George Institute for Global Health at the University of Oxford in the UK.
For example, on average, women are in the pre-diabetic state of impaired glucose tolerance 2 years longer than men.
“Historically, we know that women are often under-treated when they first present with symptoms of diabetes, are less likely to receive intensive care, and are not taking the same levels of medications as men,” Dr Peters said. “All of these could go some way into explaining why women are at greater risk of developing cancer, but, without more research, we can’t be certain.”
A review of data from more than 19 million people indicates that diabetes significantly raises a person’s risk of developing cancer.
When researchers compared patients with diabetes and without, both male and female diabetics had an increased risk of leukemias and lymphomas as well as certain solid tumors.
Researchers also found that diabetes conferred a higher cancer risk for women than men, both for all cancers combined and for some specific cancers, including leukemia.
“The link between diabetes and the risk of developing cancer is now firmly established,” said Toshiaki Ohkuma, PhD, of The George Institute for Global Health at the University of New South Wales in Australia.
“We have also demonstrated, for the first time, that women with diabetes are more likely to develop any form of cancer and have a significantly higher chance of developing kidney, oral, and stomach cancers and leukemia.”
Dr Ohkuma and his colleagues reported these findings in Diabetologia.
The researchers conducted a systematic search in PubMed MEDLINE to identify reports on the links between diabetes and cancer. Additional reports were identified from the reference lists of the relevant studies.
Only those cohort studies providing relative risks (RRs) for the association between diabetes and cancer for both women and men were included. In total, 107 relevant articles were identified, along with 36 cohorts of individual participant data.
RRs for cancer were obtained for patients with diabetes (types 1 and 2 combined) versus those without diabetes, for both men and women. The women-to-men ratios of these relative risk ratios (RRRs) were then calculated to determine the excess risk in women if present.
Data on all-site cancer was available from 47 studies, involving 121 cohorts and 19,239,302 individuals.
Diabetics vs non-diabetics
Women with diabetes had a 27% higher risk of all-site cancer compared to women without diabetes (RR=1.27; 95% CI 1.21, 1.32; P<0.001).
For men, the risk of all-site cancer was 19% higher among those with diabetes than those without (RR=1.19; 95% CI 1.13, 1.25; P<0.001).
There were several hematologic malignancies for which diabetics had an increased risk, as shown in the following table.
| Cancer type | RR for women (99% CI) | RR for men (99% CI) |
| Lymphatic and hematopoietic tissue | 1.24 (1.05, 1.46)* | 1.21 (0.98, 1.48) |
| Leukemia | 1.53 (1.00, 2.33) | 1.22 (0.80, 1.85) |
| Myeloid leukemia | 0.83 (0.39, 1.76) | 1.12 (0.77, 1.62) |
| Acute myeloid leukemia | 1.33 (1.12, 1.57)* | 1.14 (0.56, 2.33) |
| Chronic myeloid leukemia | 1.67 (1.27, 2.20)* | 1.62 (1.32, 1.98)* |
| Lymphoid leukemia | 1.74 (0.31, 9.79) | 1.20 (0.86, 1.68) |
| Lymphoma | 2.31 (0.57, 9.30) | 1.80 (0.68, 4.75) |
| Non-Hodgkin lymphoma | 1.16 (1.02, 1.32)* | 1.20 (1.08, 1.34)* |
| Hodgkin lymphoma | 1.20 (0.61, 2.38) | 1.36 (1.05, 1.77)* |
| Multiple myeloma | 1.19 (0.97, 1.47) | 1.12 (0.90, 1.41) |
| *denotes statistical significance with a P value < 0.01 | ||
Sex comparison
Calculation of the women-to-men ratio revealed that women with diabetes had a 6% greater excess risk of all-site cancer compared to men with diabetes (RRR=1.06; 95% CI 1.03, 1.09; P<0.001).
The women-to-men ratios also showed significantly higher risks for female diabetics for:
- Kidney cancer—RRR=1.11 (99% CI 1.04, 1.18; P<0.001)
- Oral cancer—RRR=1.13 (99% CI 1.00, 1.28; P=0.009)
- Stomach cancer—RRR=1.14 (99% CI 1.07, 1.22; P<0.001)
- Leukemia—RRR=1.15 (99% CI 1.02, 1.28; P=0.002).
However, women had a significantly lower risk of liver cancer (RRR=0.88; 99% CI 0.79, 0.99; P=0.005).
There are several possible reasons for the excess cancer risk observed in women, according to study author Sanne Peters, PhD, of The George Institute for Global Health at the University of Oxford in the UK.
For example, on average, women are in the pre-diabetic state of impaired glucose tolerance 2 years longer than men.
“Historically, we know that women are often under-treated when they first present with symptoms of diabetes, are less likely to receive intensive care, and are not taking the same levels of medications as men,” Dr Peters said. “All of these could go some way into explaining why women are at greater risk of developing cancer, but, without more research, we can’t be certain.”
A review of data from more than 19 million people indicates that diabetes significantly raises a person’s risk of developing cancer.
When researchers compared patients with diabetes and without, both male and female diabetics had an increased risk of leukemias and lymphomas as well as certain solid tumors.
Researchers also found that diabetes conferred a higher cancer risk for women than men, both for all cancers combined and for some specific cancers, including leukemia.
“The link between diabetes and the risk of developing cancer is now firmly established,” said Toshiaki Ohkuma, PhD, of The George Institute for Global Health at the University of New South Wales in Australia.
“We have also demonstrated, for the first time, that women with diabetes are more likely to develop any form of cancer and have a significantly higher chance of developing kidney, oral, and stomach cancers and leukemia.”
Dr Ohkuma and his colleagues reported these findings in Diabetologia.
The researchers conducted a systematic search in PubMed MEDLINE to identify reports on the links between diabetes and cancer. Additional reports were identified from the reference lists of the relevant studies.
Only those cohort studies providing relative risks (RRs) for the association between diabetes and cancer for both women and men were included. In total, 107 relevant articles were identified, along with 36 cohorts of individual participant data.
RRs for cancer were obtained for patients with diabetes (types 1 and 2 combined) versus those without diabetes, for both men and women. The women-to-men ratios of these relative risk ratios (RRRs) were then calculated to determine the excess risk in women if present.
Data on all-site cancer was available from 47 studies, involving 121 cohorts and 19,239,302 individuals.
Diabetics vs non-diabetics
Women with diabetes had a 27% higher risk of all-site cancer compared to women without diabetes (RR=1.27; 95% CI 1.21, 1.32; P<0.001).
For men, the risk of all-site cancer was 19% higher among those with diabetes than those without (RR=1.19; 95% CI 1.13, 1.25; P<0.001).
There were several hematologic malignancies for which diabetics had an increased risk, as shown in the following table.
| Cancer type | RR for women (99% CI) | RR for men (99% CI) |
| Lymphatic and hematopoietic tissue | 1.24 (1.05, 1.46)* | 1.21 (0.98, 1.48) |
| Leukemia | 1.53 (1.00, 2.33) | 1.22 (0.80, 1.85) |
| Myeloid leukemia | 0.83 (0.39, 1.76) | 1.12 (0.77, 1.62) |
| Acute myeloid leukemia | 1.33 (1.12, 1.57)* | 1.14 (0.56, 2.33) |
| Chronic myeloid leukemia | 1.67 (1.27, 2.20)* | 1.62 (1.32, 1.98)* |
| Lymphoid leukemia | 1.74 (0.31, 9.79) | 1.20 (0.86, 1.68) |
| Lymphoma | 2.31 (0.57, 9.30) | 1.80 (0.68, 4.75) |
| Non-Hodgkin lymphoma | 1.16 (1.02, 1.32)* | 1.20 (1.08, 1.34)* |
| Hodgkin lymphoma | 1.20 (0.61, 2.38) | 1.36 (1.05, 1.77)* |
| Multiple myeloma | 1.19 (0.97, 1.47) | 1.12 (0.90, 1.41) |
| *denotes statistical significance with a P value < 0.01 | ||
Sex comparison
Calculation of the women-to-men ratio revealed that women with diabetes had a 6% greater excess risk of all-site cancer compared to men with diabetes (RRR=1.06; 95% CI 1.03, 1.09; P<0.001).
The women-to-men ratios also showed significantly higher risks for female diabetics for:
- Kidney cancer—RRR=1.11 (99% CI 1.04, 1.18; P<0.001)
- Oral cancer—RRR=1.13 (99% CI 1.00, 1.28; P=0.009)
- Stomach cancer—RRR=1.14 (99% CI 1.07, 1.22; P<0.001)
- Leukemia—RRR=1.15 (99% CI 1.02, 1.28; P=0.002).
However, women had a significantly lower risk of liver cancer (RRR=0.88; 99% CI 0.79, 0.99; P=0.005).
There are several possible reasons for the excess cancer risk observed in women, according to study author Sanne Peters, PhD, of The George Institute for Global Health at the University of Oxford in the UK.
For example, on average, women are in the pre-diabetic state of impaired glucose tolerance 2 years longer than men.
“Historically, we know that women are often under-treated when they first present with symptoms of diabetes, are less likely to receive intensive care, and are not taking the same levels of medications as men,” Dr Peters said. “All of these could go some way into explaining why women are at greater risk of developing cancer, but, without more research, we can’t be certain.”
Study suggests dasatinib could treat AML, JMML
New research suggests dasatinib could treat certain patients with juvenile myelomonocytic leukemia (JMML) or acute myeloid leukemia (AML).
The study showed that TNK2 inhibition has a negative effect on PTPN11-mutant leukemias.
PTPN11-mutant JMML and AML cells were sensitive to treatment with dasatinib, which inhibits TNK2.
Dasatinib also induced hematologic remission in a patient with PTPN11-mutant JMML.
Investigators reported these results in Science Signaling.
Past research showed that mutations in PTPN11 result in excessive cell proliferation and drive tumor growth in some cases of JMML and AML.
In the current study, investigators analyzed PTPN11-mutated leukemia cells and found that PTPN11 is activated by TNK2.
The investigators said TNK2 phosphorylates PTPN11, which then dephosphorylates TNK2 in a negative feedback loop. They also found that coexpression of TNK2 and mutant PTPN11 results in “robust” MAPK pathway activation.
Inhibiting TNK2 with dasatinib blocked MAPK signaling and colony formation in vitro.
Additional experiments showed that PTPN11-mutant AML samples were significantly more sensitive to dasatinib than wild-type AML samples.
Investigators also tested dasatinib in a sample from a JMML patient carrying a PTPN11 G60R mutation.
This patient’s cells were 10 times more sensitive to dasatinib than the average sample from a cohort of 151 patients who had AML, acute lymphoblastic leukemia, myeloproliferative neoplasms, or chronic lymphocytic leukemia.
Because the JMML patient’s cells were so responsive to dasatinib, the investigators decided to administer the drug to the patient.
The patient achieved sustained hematologic remission with dasatinib, and this allowed him to receive a stem cell transplant using an unrelated cord blood donor. The patient had previously failed 2 transplants (with myeloablative conditioning) from a matched sibling donor.
The third transplant prolonged the patient’s life by a year, but he eventually died of relapsed disease.
The investigators said this case study and the in vitro results support further investigation into the efficacy of dasatinib and other TNK2 inhibitors in PTPN11-mutant leukemias.
New research suggests dasatinib could treat certain patients with juvenile myelomonocytic leukemia (JMML) or acute myeloid leukemia (AML).
The study showed that TNK2 inhibition has a negative effect on PTPN11-mutant leukemias.
PTPN11-mutant JMML and AML cells were sensitive to treatment with dasatinib, which inhibits TNK2.
Dasatinib also induced hematologic remission in a patient with PTPN11-mutant JMML.
Investigators reported these results in Science Signaling.
Past research showed that mutations in PTPN11 result in excessive cell proliferation and drive tumor growth in some cases of JMML and AML.
In the current study, investigators analyzed PTPN11-mutated leukemia cells and found that PTPN11 is activated by TNK2.
The investigators said TNK2 phosphorylates PTPN11, which then dephosphorylates TNK2 in a negative feedback loop. They also found that coexpression of TNK2 and mutant PTPN11 results in “robust” MAPK pathway activation.
Inhibiting TNK2 with dasatinib blocked MAPK signaling and colony formation in vitro.
Additional experiments showed that PTPN11-mutant AML samples were significantly more sensitive to dasatinib than wild-type AML samples.
Investigators also tested dasatinib in a sample from a JMML patient carrying a PTPN11 G60R mutation.
This patient’s cells were 10 times more sensitive to dasatinib than the average sample from a cohort of 151 patients who had AML, acute lymphoblastic leukemia, myeloproliferative neoplasms, or chronic lymphocytic leukemia.
Because the JMML patient’s cells were so responsive to dasatinib, the investigators decided to administer the drug to the patient.
The patient achieved sustained hematologic remission with dasatinib, and this allowed him to receive a stem cell transplant using an unrelated cord blood donor. The patient had previously failed 2 transplants (with myeloablative conditioning) from a matched sibling donor.
The third transplant prolonged the patient’s life by a year, but he eventually died of relapsed disease.
The investigators said this case study and the in vitro results support further investigation into the efficacy of dasatinib and other TNK2 inhibitors in PTPN11-mutant leukemias.
New research suggests dasatinib could treat certain patients with juvenile myelomonocytic leukemia (JMML) or acute myeloid leukemia (AML).
The study showed that TNK2 inhibition has a negative effect on PTPN11-mutant leukemias.
PTPN11-mutant JMML and AML cells were sensitive to treatment with dasatinib, which inhibits TNK2.
Dasatinib also induced hematologic remission in a patient with PTPN11-mutant JMML.
Investigators reported these results in Science Signaling.
Past research showed that mutations in PTPN11 result in excessive cell proliferation and drive tumor growth in some cases of JMML and AML.
In the current study, investigators analyzed PTPN11-mutated leukemia cells and found that PTPN11 is activated by TNK2.
The investigators said TNK2 phosphorylates PTPN11, which then dephosphorylates TNK2 in a negative feedback loop. They also found that coexpression of TNK2 and mutant PTPN11 results in “robust” MAPK pathway activation.
Inhibiting TNK2 with dasatinib blocked MAPK signaling and colony formation in vitro.
Additional experiments showed that PTPN11-mutant AML samples were significantly more sensitive to dasatinib than wild-type AML samples.
Investigators also tested dasatinib in a sample from a JMML patient carrying a PTPN11 G60R mutation.
This patient’s cells were 10 times more sensitive to dasatinib than the average sample from a cohort of 151 patients who had AML, acute lymphoblastic leukemia, myeloproliferative neoplasms, or chronic lymphocytic leukemia.
Because the JMML patient’s cells were so responsive to dasatinib, the investigators decided to administer the drug to the patient.
The patient achieved sustained hematologic remission with dasatinib, and this allowed him to receive a stem cell transplant using an unrelated cord blood donor. The patient had previously failed 2 transplants (with myeloablative conditioning) from a matched sibling donor.
The third transplant prolonged the patient’s life by a year, but he eventually died of relapsed disease.
The investigators said this case study and the in vitro results support further investigation into the efficacy of dasatinib and other TNK2 inhibitors in PTPN11-mutant leukemias.
Explaining enasidenib resistance in AML
New research helps explain enasidenib resistance among patients with IDH2-mutant acute myeloid leukemia (AML).
Researchers found that leukemic cells stop responding to enasidenib when IDH2 clones develop additional mutations.
This may mean that enasidenib will have to be combined with other drugs to prevent AML relapse, the researchers said.
They reported their findings in Nature Medicine.
Previous research indicated that enasidenib prompts differentiation to induce responses in AML. In a phase 1/2 trial, enasidenib produced responses in about 40% of patients with relapsed/refractory, IDH2-mutated AML. However, most patients eventually relapsed.
“[T]he initial studies did not show which AML cells responded to enasidenib and started to differentiate again,” said Stéphane de Botton, MD, PhD, of Institut Gustave Roussy in Villejuif, France.
“It was also unclear how the cells become resistant to therapy. We wanted to answer these questions.”
To do so, Dr de Botton and his colleagues analyzed sequential samples from 37 AML patients treated with enasidenib on the phase 1/2 trial. Thirty of these patients had initially responded to the drug.
“We used techniques to study genetic mutations on a cell-by-cell basis and reconstructed the ‘family tree’ of a patient’s AML,” said Lynn Quek, MD, of the University of Oxford in the UK.
“We then tracked changes in the family of AML cells as they responded to enasidenib and as patients lost response to the drug. This is the first time that anyone has done such a detailed study at a single-cell level.”
The researchers said they observed variable differentiation arrest in IDH2-mutant clones before enasidenib treatment.
Overall, treatment promoted hematopoietic differentiation from either terminal or ancestral mutant clones. However, enasidenib also promoted differentiation of nonmutant cells in a minority of patients.
When the researchers compared samples taken at diagnosis and relapse, they did not find second-site mutations in IDH2 at relapse.
The team said relapse was the result of clonal evolution or selection of terminal or ancestral clones, which suggests there are multiple pathways that could potentially be targeted to restore differentiation arrest.
“We have provided genetic proof that enasidenib was able to differentiate cancer cells so that some of their normal functions were restored, even though they still contained the IDH2 mutation,” said Virginie Penard-Lacronique, of Gustave Roussy.
“This is important because, unless we can track these clones, we don’t know whether the mature cells in a patient are coming from normal cells after all the cancer cells have been killed or from leukemic cells that are now able to mature. In this paper, we show that, in 4 out of 5 cases, the mature cells are coming from leukemic bone marrow cells that can be induced to differentiate by this new drug.”
The researchers said these results suggest enasidenib must be combined with other drugs to prevent AML relapse.
“Now that we have shown that [enasidenib] needs to be combined with other drugs to stop the cancer returning, we think that it’s important that the combination therapy should be given to AML patients early on in their disease,” Dr de Botton said. “International trials are now taking place comparing combinations of enasidenib and other drugs with the normal standard of care.”
New research helps explain enasidenib resistance among patients with IDH2-mutant acute myeloid leukemia (AML).
Researchers found that leukemic cells stop responding to enasidenib when IDH2 clones develop additional mutations.
This may mean that enasidenib will have to be combined with other drugs to prevent AML relapse, the researchers said.
They reported their findings in Nature Medicine.
Previous research indicated that enasidenib prompts differentiation to induce responses in AML. In a phase 1/2 trial, enasidenib produced responses in about 40% of patients with relapsed/refractory, IDH2-mutated AML. However, most patients eventually relapsed.
“[T]he initial studies did not show which AML cells responded to enasidenib and started to differentiate again,” said Stéphane de Botton, MD, PhD, of Institut Gustave Roussy in Villejuif, France.
“It was also unclear how the cells become resistant to therapy. We wanted to answer these questions.”
To do so, Dr de Botton and his colleagues analyzed sequential samples from 37 AML patients treated with enasidenib on the phase 1/2 trial. Thirty of these patients had initially responded to the drug.
“We used techniques to study genetic mutations on a cell-by-cell basis and reconstructed the ‘family tree’ of a patient’s AML,” said Lynn Quek, MD, of the University of Oxford in the UK.
“We then tracked changes in the family of AML cells as they responded to enasidenib and as patients lost response to the drug. This is the first time that anyone has done such a detailed study at a single-cell level.”
The researchers said they observed variable differentiation arrest in IDH2-mutant clones before enasidenib treatment.
Overall, treatment promoted hematopoietic differentiation from either terminal or ancestral mutant clones. However, enasidenib also promoted differentiation of nonmutant cells in a minority of patients.
When the researchers compared samples taken at diagnosis and relapse, they did not find second-site mutations in IDH2 at relapse.
The team said relapse was the result of clonal evolution or selection of terminal or ancestral clones, which suggests there are multiple pathways that could potentially be targeted to restore differentiation arrest.
“We have provided genetic proof that enasidenib was able to differentiate cancer cells so that some of their normal functions were restored, even though they still contained the IDH2 mutation,” said Virginie Penard-Lacronique, of Gustave Roussy.
“This is important because, unless we can track these clones, we don’t know whether the mature cells in a patient are coming from normal cells after all the cancer cells have been killed or from leukemic cells that are now able to mature. In this paper, we show that, in 4 out of 5 cases, the mature cells are coming from leukemic bone marrow cells that can be induced to differentiate by this new drug.”
The researchers said these results suggest enasidenib must be combined with other drugs to prevent AML relapse.
“Now that we have shown that [enasidenib] needs to be combined with other drugs to stop the cancer returning, we think that it’s important that the combination therapy should be given to AML patients early on in their disease,” Dr de Botton said. “International trials are now taking place comparing combinations of enasidenib and other drugs with the normal standard of care.”
New research helps explain enasidenib resistance among patients with IDH2-mutant acute myeloid leukemia (AML).
Researchers found that leukemic cells stop responding to enasidenib when IDH2 clones develop additional mutations.
This may mean that enasidenib will have to be combined with other drugs to prevent AML relapse, the researchers said.
They reported their findings in Nature Medicine.
Previous research indicated that enasidenib prompts differentiation to induce responses in AML. In a phase 1/2 trial, enasidenib produced responses in about 40% of patients with relapsed/refractory, IDH2-mutated AML. However, most patients eventually relapsed.
“[T]he initial studies did not show which AML cells responded to enasidenib and started to differentiate again,” said Stéphane de Botton, MD, PhD, of Institut Gustave Roussy in Villejuif, France.
“It was also unclear how the cells become resistant to therapy. We wanted to answer these questions.”
To do so, Dr de Botton and his colleagues analyzed sequential samples from 37 AML patients treated with enasidenib on the phase 1/2 trial. Thirty of these patients had initially responded to the drug.
“We used techniques to study genetic mutations on a cell-by-cell basis and reconstructed the ‘family tree’ of a patient’s AML,” said Lynn Quek, MD, of the University of Oxford in the UK.
“We then tracked changes in the family of AML cells as they responded to enasidenib and as patients lost response to the drug. This is the first time that anyone has done such a detailed study at a single-cell level.”
The researchers said they observed variable differentiation arrest in IDH2-mutant clones before enasidenib treatment.
Overall, treatment promoted hematopoietic differentiation from either terminal or ancestral mutant clones. However, enasidenib also promoted differentiation of nonmutant cells in a minority of patients.
When the researchers compared samples taken at diagnosis and relapse, they did not find second-site mutations in IDH2 at relapse.
The team said relapse was the result of clonal evolution or selection of terminal or ancestral clones, which suggests there are multiple pathways that could potentially be targeted to restore differentiation arrest.
“We have provided genetic proof that enasidenib was able to differentiate cancer cells so that some of their normal functions were restored, even though they still contained the IDH2 mutation,” said Virginie Penard-Lacronique, of Gustave Roussy.
“This is important because, unless we can track these clones, we don’t know whether the mature cells in a patient are coming from normal cells after all the cancer cells have been killed or from leukemic cells that are now able to mature. In this paper, we show that, in 4 out of 5 cases, the mature cells are coming from leukemic bone marrow cells that can be induced to differentiate by this new drug.”
The researchers said these results suggest enasidenib must be combined with other drugs to prevent AML relapse.
“Now that we have shown that [enasidenib] needs to be combined with other drugs to stop the cancer returning, we think that it’s important that the combination therapy should be given to AML patients early on in their disease,” Dr de Botton said. “International trials are now taking place comparing combinations of enasidenib and other drugs with the normal standard of care.”