User login
Severe hospital-acquired anemia linked to readmission, death
Severe hospital-acquired anemia (HAA) may increase a person’s risk of hospital readmission and death, a new study suggests.
Researchers studied more than 11,000 patients admitted to 6 Texas hospitals and found that a third of the patients developed HAA.
The team also found that severe HAA was associated with a higher risk of death or readmission, even after the researchers adjusted for other factors.
They reported these findings in the Journal of Hospital Medicine.
“This study shines a spotlight on a very common but underappreciated risk of hospitalization, hospital-acquired anemia, which has traditionally been viewed as an incidental change in the red blood count of no significance,” said study author Ethan Halm, MD, of the University of Texas Southwestern Medical Center in Dallas.
“However, our results showed that hospital-acquired anemia was associated with worse clinical outcomes after leaving the hospital, so it needs to be taken more seriously.”
Dr Halm and his colleagues looked at consecutive medicine discharges between November 1, 2009, and October 30, 2010, from 6 hospitals in Texas (safety-net, teaching, and nonteaching).
Of the 11,309 patients studied, 33.1% developed HAA. Most (21.6%) had mild HAA, followed by moderate HAA (10.1%), and severe HAA (1.4%).
The study’s primary outcome was a composite of 30-day mortality and nonelective readmission. This occurred in 9.7% of patients without HAA and 16.4% of those with severe HAA.
The researchers found that severe HAA was independently associated with a 39% increase in the odds of meeting the primary outcome (readmission or 30-day mortality).
The team noted that 85% of patients with severe HAA underwent a major procedure, had a discharge diagnosis of hemorrhage, and/or a discharge diagnosis of hemorrhagic disorder.
The researchers identified 2 potentially modifiable predictors of moderate or severe HAA. These were length of hospital stay (adjusted odds ratio=1.26 per day) and undergoing a major procedure (adjusted odds ratio=5.09).
“Our findings suggest that reducing blood loss during major surgeries and reducing unnecessary testing during hospital stays may lower a patient’s risk of developing severe hospital-acquired anemia, and potentially improve their recovery,” said Anil N. Makam, MD, of the University of Texas Southwestern Medical Center.
In the future, the researchers hope to examine other patient-centered outcomes that may be related to HAA, such as fatigue, functional impairment, and the trajectory of post-hospital recovery. ![]()
Severe hospital-acquired anemia (HAA) may increase a person’s risk of hospital readmission and death, a new study suggests.
Researchers studied more than 11,000 patients admitted to 6 Texas hospitals and found that a third of the patients developed HAA.
The team also found that severe HAA was associated with a higher risk of death or readmission, even after the researchers adjusted for other factors.
They reported these findings in the Journal of Hospital Medicine.
“This study shines a spotlight on a very common but underappreciated risk of hospitalization, hospital-acquired anemia, which has traditionally been viewed as an incidental change in the red blood count of no significance,” said study author Ethan Halm, MD, of the University of Texas Southwestern Medical Center in Dallas.
“However, our results showed that hospital-acquired anemia was associated with worse clinical outcomes after leaving the hospital, so it needs to be taken more seriously.”
Dr Halm and his colleagues looked at consecutive medicine discharges between November 1, 2009, and October 30, 2010, from 6 hospitals in Texas (safety-net, teaching, and nonteaching).
Of the 11,309 patients studied, 33.1% developed HAA. Most (21.6%) had mild HAA, followed by moderate HAA (10.1%), and severe HAA (1.4%).
The study’s primary outcome was a composite of 30-day mortality and nonelective readmission. This occurred in 9.7% of patients without HAA and 16.4% of those with severe HAA.
The researchers found that severe HAA was independently associated with a 39% increase in the odds of meeting the primary outcome (readmission or 30-day mortality).
The team noted that 85% of patients with severe HAA underwent a major procedure, had a discharge diagnosis of hemorrhage, and/or a discharge diagnosis of hemorrhagic disorder.
The researchers identified 2 potentially modifiable predictors of moderate or severe HAA. These were length of hospital stay (adjusted odds ratio=1.26 per day) and undergoing a major procedure (adjusted odds ratio=5.09).
“Our findings suggest that reducing blood loss during major surgeries and reducing unnecessary testing during hospital stays may lower a patient’s risk of developing severe hospital-acquired anemia, and potentially improve their recovery,” said Anil N. Makam, MD, of the University of Texas Southwestern Medical Center.
In the future, the researchers hope to examine other patient-centered outcomes that may be related to HAA, such as fatigue, functional impairment, and the trajectory of post-hospital recovery. ![]()
Severe hospital-acquired anemia (HAA) may increase a person’s risk of hospital readmission and death, a new study suggests.
Researchers studied more than 11,000 patients admitted to 6 Texas hospitals and found that a third of the patients developed HAA.
The team also found that severe HAA was associated with a higher risk of death or readmission, even after the researchers adjusted for other factors.
They reported these findings in the Journal of Hospital Medicine.
“This study shines a spotlight on a very common but underappreciated risk of hospitalization, hospital-acquired anemia, which has traditionally been viewed as an incidental change in the red blood count of no significance,” said study author Ethan Halm, MD, of the University of Texas Southwestern Medical Center in Dallas.
“However, our results showed that hospital-acquired anemia was associated with worse clinical outcomes after leaving the hospital, so it needs to be taken more seriously.”
Dr Halm and his colleagues looked at consecutive medicine discharges between November 1, 2009, and October 30, 2010, from 6 hospitals in Texas (safety-net, teaching, and nonteaching).
Of the 11,309 patients studied, 33.1% developed HAA. Most (21.6%) had mild HAA, followed by moderate HAA (10.1%), and severe HAA (1.4%).
The study’s primary outcome was a composite of 30-day mortality and nonelective readmission. This occurred in 9.7% of patients without HAA and 16.4% of those with severe HAA.
The researchers found that severe HAA was independently associated with a 39% increase in the odds of meeting the primary outcome (readmission or 30-day mortality).
The team noted that 85% of patients with severe HAA underwent a major procedure, had a discharge diagnosis of hemorrhage, and/or a discharge diagnosis of hemorrhagic disorder.
The researchers identified 2 potentially modifiable predictors of moderate or severe HAA. These were length of hospital stay (adjusted odds ratio=1.26 per day) and undergoing a major procedure (adjusted odds ratio=5.09).
“Our findings suggest that reducing blood loss during major surgeries and reducing unnecessary testing during hospital stays may lower a patient’s risk of developing severe hospital-acquired anemia, and potentially improve their recovery,” said Anil N. Makam, MD, of the University of Texas Southwestern Medical Center.
In the future, the researchers hope to examine other patient-centered outcomes that may be related to HAA, such as fatigue, functional impairment, and the trajectory of post-hospital recovery. ![]()
Drug receives rare pediatric disease designation for SCD
The US Food and Drug Administration (FDA) has granted rare pediatric disease designation to IMR-687, a product intended to treat sickle cell disease (SCD).
IMR-687 is the first SCD candidate to be designated as a drug for a rare pediatric disease, and this designation builds upon the FDA’s earlier granting of orphan designation for IMR-687.
IMR-687 is a selective inhibitor of phosphodiesterase-9 (PDE9i) in blood cells. It was specifically designed to address the underlying pathology of SCD.
In preclinical studies, IMR-687 demonstrated the ability to increase fetal globin. This prevented the polymerization of sickled hemoglobin and reduced red blood cell sickling, leukocytosis, and the occlusion of blood vessels.
Researchers presented these results at the 2016 ASH Annual Meeting.
Imara Inc., the company developing IMR-687, is conducting a phase 1a trial of the product in healthy volunteers.
If the trial has a positive outcome (results are expected this summer), Imara will initiate a phase 2a study in adults with SCD later this year. The company expects to initiate a phase 2 study in pediatric patients in 2018.
About rare pediatric disease designation
Rare pediatric disease designation is granted to drugs that show promise to treat orphan diseases affecting fewer than 200,000 patients in the US, primarily patients age 18 or younger.
The designation provides incentives to advance the development of drugs for rare disease, including access to the FDA’s expedited review and approval programs.
Under the FDA’s Rare Pediatric Disease Priority Review Voucher Program, a sponsor with rare pediatric disease designation who receives an approval of a new drug application is eligible for a voucher that can be redeemed to obtain priority review for any subsequent marketing application.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted rare pediatric disease designation to IMR-687, a product intended to treat sickle cell disease (SCD).
IMR-687 is the first SCD candidate to be designated as a drug for a rare pediatric disease, and this designation builds upon the FDA’s earlier granting of orphan designation for IMR-687.
IMR-687 is a selective inhibitor of phosphodiesterase-9 (PDE9i) in blood cells. It was specifically designed to address the underlying pathology of SCD.
In preclinical studies, IMR-687 demonstrated the ability to increase fetal globin. This prevented the polymerization of sickled hemoglobin and reduced red blood cell sickling, leukocytosis, and the occlusion of blood vessels.
Researchers presented these results at the 2016 ASH Annual Meeting.
Imara Inc., the company developing IMR-687, is conducting a phase 1a trial of the product in healthy volunteers.
If the trial has a positive outcome (results are expected this summer), Imara will initiate a phase 2a study in adults with SCD later this year. The company expects to initiate a phase 2 study in pediatric patients in 2018.
About rare pediatric disease designation
Rare pediatric disease designation is granted to drugs that show promise to treat orphan diseases affecting fewer than 200,000 patients in the US, primarily patients age 18 or younger.
The designation provides incentives to advance the development of drugs for rare disease, including access to the FDA’s expedited review and approval programs.
Under the FDA’s Rare Pediatric Disease Priority Review Voucher Program, a sponsor with rare pediatric disease designation who receives an approval of a new drug application is eligible for a voucher that can be redeemed to obtain priority review for any subsequent marketing application.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted rare pediatric disease designation to IMR-687, a product intended to treat sickle cell disease (SCD).
IMR-687 is the first SCD candidate to be designated as a drug for a rare pediatric disease, and this designation builds upon the FDA’s earlier granting of orphan designation for IMR-687.
IMR-687 is a selective inhibitor of phosphodiesterase-9 (PDE9i) in blood cells. It was specifically designed to address the underlying pathology of SCD.
In preclinical studies, IMR-687 demonstrated the ability to increase fetal globin. This prevented the polymerization of sickled hemoglobin and reduced red blood cell sickling, leukocytosis, and the occlusion of blood vessels.
Researchers presented these results at the 2016 ASH Annual Meeting.
Imara Inc., the company developing IMR-687, is conducting a phase 1a trial of the product in healthy volunteers.
If the trial has a positive outcome (results are expected this summer), Imara will initiate a phase 2a study in adults with SCD later this year. The company expects to initiate a phase 2 study in pediatric patients in 2018.
About rare pediatric disease designation
Rare pediatric disease designation is granted to drugs that show promise to treat orphan diseases affecting fewer than 200,000 patients in the US, primarily patients age 18 or younger.
The designation provides incentives to advance the development of drugs for rare disease, including access to the FDA’s expedited review and approval programs.
Under the FDA’s Rare Pediatric Disease Priority Review Voucher Program, a sponsor with rare pediatric disease designation who receives an approval of a new drug application is eligible for a voucher that can be redeemed to obtain priority review for any subsequent marketing application.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
Oral iron of no benefit in heart failure with iron deficiency
High-dose oral iron therapy doesn’t improve exercise capacity in the estimated 50% of patients with symptomatic heart failure who also have iron deficiency, according to a report published online May 16 in JAMA.
Iron deficiency in patients with HF, regardless of their hemoglobin status, is associated with reduced functional capacity, poorer quality of life, and increased mortality. Iron plays a crucial role in the delivery and utilization of oxygen, and “cells with high-energy demands, including skeletal and cardiac myocytes, are particularly sensitive to depleted iron stores,” said Gregory D. Lewis, MD, of the pulmonary critical care unit of Massachusetts General Hospital, Boston, and his associates.
The IRONOUT study was conducted at 23 U.S. medical centers, where outcomes after 16 weeks of oral iron therapy (150 mg twice daily) were compared against matching placebo in 225 patients. The median patient age was 63 years, and the median duration of HF was 5.7 years. Ischemic heart disease was the primary cause of HF in 78% of the study participants.
These patients had low LVEF and poor exercise capacity, despite having high rates of guideline-directed treatment with medications.
The primary endpoint was a change in peak oxygen uptake (peak VO2) at the conclusion of treatment, a measure that “reflects the multiple mechanisms by which iron repletion is expected to improve systemic oxygen delivery and utilization.” Change in peak VO2 was not significantly different between the 111 participants who took oral iron supplements (+23 mL/min) and the 114 who took placebo (–2 mL/min), the investigators wrote (JAMA Pediatr. 2017 May 16. doi: 10.1001/jama.2017.5427).
In subgroup analyses, oral iron also failed to improve peak VO2 in any subgroup of patients: neither men nor women; neither those with decreased hemoglobin nor those with normal hemoglobin levels; nor patients with or without venous congestion at baseline. Oral iron also failed to improve secondary endpoints including 6-minute walk distance, quality of life scores, NT-proBNP levels, and ventilatory efficiency.
In contrast to previous studies of IV iron repletion, oral iron supplementation “produced minimal improvement in iron stores, implicating the route of administration rather than the strategy of iron repletion in the lack of clinical benefit,” Dr. Lewis and his associates said.
This study was funded by the National Heart, Lung, and Blood Institute, which also conceived, designed, and conducted the trial. Dr. Lewis reported ties to Abbott, Novartis, Shape Systems, Stealth Bio Therapeutics, Ironwood, Cheetah Medical, Luitpold, and SoniVie. His associates reported ties to numerous industry sources.
High-dose oral iron therapy doesn’t improve exercise capacity in the estimated 50% of patients with symptomatic heart failure who also have iron deficiency, according to a report published online May 16 in JAMA.
Iron deficiency in patients with HF, regardless of their hemoglobin status, is associated with reduced functional capacity, poorer quality of life, and increased mortality. Iron plays a crucial role in the delivery and utilization of oxygen, and “cells with high-energy demands, including skeletal and cardiac myocytes, are particularly sensitive to depleted iron stores,” said Gregory D. Lewis, MD, of the pulmonary critical care unit of Massachusetts General Hospital, Boston, and his associates.
The IRONOUT study was conducted at 23 U.S. medical centers, where outcomes after 16 weeks of oral iron therapy (150 mg twice daily) were compared against matching placebo in 225 patients. The median patient age was 63 years, and the median duration of HF was 5.7 years. Ischemic heart disease was the primary cause of HF in 78% of the study participants.
These patients had low LVEF and poor exercise capacity, despite having high rates of guideline-directed treatment with medications.
The primary endpoint was a change in peak oxygen uptake (peak VO2) at the conclusion of treatment, a measure that “reflects the multiple mechanisms by which iron repletion is expected to improve systemic oxygen delivery and utilization.” Change in peak VO2 was not significantly different between the 111 participants who took oral iron supplements (+23 mL/min) and the 114 who took placebo (–2 mL/min), the investigators wrote (JAMA Pediatr. 2017 May 16. doi: 10.1001/jama.2017.5427).
In subgroup analyses, oral iron also failed to improve peak VO2 in any subgroup of patients: neither men nor women; neither those with decreased hemoglobin nor those with normal hemoglobin levels; nor patients with or without venous congestion at baseline. Oral iron also failed to improve secondary endpoints including 6-minute walk distance, quality of life scores, NT-proBNP levels, and ventilatory efficiency.
In contrast to previous studies of IV iron repletion, oral iron supplementation “produced minimal improvement in iron stores, implicating the route of administration rather than the strategy of iron repletion in the lack of clinical benefit,” Dr. Lewis and his associates said.
This study was funded by the National Heart, Lung, and Blood Institute, which also conceived, designed, and conducted the trial. Dr. Lewis reported ties to Abbott, Novartis, Shape Systems, Stealth Bio Therapeutics, Ironwood, Cheetah Medical, Luitpold, and SoniVie. His associates reported ties to numerous industry sources.
High-dose oral iron therapy doesn’t improve exercise capacity in the estimated 50% of patients with symptomatic heart failure who also have iron deficiency, according to a report published online May 16 in JAMA.
Iron deficiency in patients with HF, regardless of their hemoglobin status, is associated with reduced functional capacity, poorer quality of life, and increased mortality. Iron plays a crucial role in the delivery and utilization of oxygen, and “cells with high-energy demands, including skeletal and cardiac myocytes, are particularly sensitive to depleted iron stores,” said Gregory D. Lewis, MD, of the pulmonary critical care unit of Massachusetts General Hospital, Boston, and his associates.
The IRONOUT study was conducted at 23 U.S. medical centers, where outcomes after 16 weeks of oral iron therapy (150 mg twice daily) were compared against matching placebo in 225 patients. The median patient age was 63 years, and the median duration of HF was 5.7 years. Ischemic heart disease was the primary cause of HF in 78% of the study participants.
These patients had low LVEF and poor exercise capacity, despite having high rates of guideline-directed treatment with medications.
The primary endpoint was a change in peak oxygen uptake (peak VO2) at the conclusion of treatment, a measure that “reflects the multiple mechanisms by which iron repletion is expected to improve systemic oxygen delivery and utilization.” Change in peak VO2 was not significantly different between the 111 participants who took oral iron supplements (+23 mL/min) and the 114 who took placebo (–2 mL/min), the investigators wrote (JAMA Pediatr. 2017 May 16. doi: 10.1001/jama.2017.5427).
In subgroup analyses, oral iron also failed to improve peak VO2 in any subgroup of patients: neither men nor women; neither those with decreased hemoglobin nor those with normal hemoglobin levels; nor patients with or without venous congestion at baseline. Oral iron also failed to improve secondary endpoints including 6-minute walk distance, quality of life scores, NT-proBNP levels, and ventilatory efficiency.
In contrast to previous studies of IV iron repletion, oral iron supplementation “produced minimal improvement in iron stores, implicating the route of administration rather than the strategy of iron repletion in the lack of clinical benefit,” Dr. Lewis and his associates said.
This study was funded by the National Heart, Lung, and Blood Institute, which also conceived, designed, and conducted the trial. Dr. Lewis reported ties to Abbott, Novartis, Shape Systems, Stealth Bio Therapeutics, Ironwood, Cheetah Medical, Luitpold, and SoniVie. His associates reported ties to numerous industry sources.
Key clinical point: High-dose oral iron therapy doesn’t improve exercise capacity in the estimated 50% of patients with symptomatic heart failure and iron deficiency.
Major finding: Change in peak VO2 was not significantly different between the 111 participants who took oral iron supplements (+23 mL/min) and the 114 who took placebo (–2 mL/min).
Data source: A multicenter, randomized, double-blind, placebo-controlled phase II trial involving 225 patients treated for 16 weeks.
Disclosures: This study was funded by the National Heart, Lung, and Blood Institute (NCT02188784), which also conceived, designed, and conducted the trial. Dr. Lewis reported ties to Abbott, Novartis, Shape Systems, Stealth Bio Therapeutics, Ironwood, Cheetah Medical, Luitpold, and SoniVie. His associates reported ties to numerous industry sources.
Iron-transporting molecule could treat anemia, iron overload
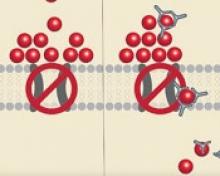
Researchers say they have identified a small molecule that can transport iron when typical transport routes are mutated or absent.
The molecule, hinokitiol, was able to move iron into or out of cells by wrapping around iron atoms and shuttling them across the membrane layer.
Hinokitiol promoted gut iron absorption in rats and mice deficient in iron transport complexes, and it promoted hemoglobin production in zebrafish that otherwise couldn’t transport iron effectively.
The researchers believe these findings, published in Science, may lead to new treatments for disorders associated with iron metabolism, such as anemias and hemochromatosis.
“The long-term therapeutic implications of our work with hinokitiol points to potentially using this chemical to correct anemias caused by genetic deficiencies of iron transporters required for normal red cell formation,” said study author Barry Paw, MD, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“At the same time, hinokitiol has the potential to correct iron-overload syndromes, such as hemochromatosis. More extensive clinical trials are necessary to work out the full potential of hinokitiol and to identify potential toxicities that we have not identified using preclinical models.”
Dr Paw and his colleagues discovered the potential of hinokitiol when screening for a molecule that could restore growth to yeast lacking an iron transporter complex. Hinokitiol is a natural product originally isolated from the Taiwanese hinoki tree.
The researchers found that hinokitiol could transport iron across the yeast cellular membrane in mutant yeasts lacking their major iron uptake transporters. Three hinokitiol molecules can wrap around an iron atom and transport it directly across the membrane where the missing protein should be.
The team also tested hinokitiol in mice, rats, and zebrafish that were missing iron-transport proteins.
Orally administered hinokitiol restored iron uptake in the guts of ferroportin-deficient mice and DMT1-deficient rats, and adding hinokitiol to a tank housing DMT1- and mitoferrin-deficient zebrafish prompted hemoglobin production in the fish.
The researchers also found that hinokitiol restored iron transport in human cells taken from the lining of the gut.
“We found that hinokitiol can restore iron transport within cells, out of cells, or both,” Dr Paw said. “It can also promote iron gut absorption and the creation of hemoglobin in some of our models. These findings suggest that small molecules like hinokitiol that can mimic the biological function of a missing protein may have potential for treating human diseases.” ![]()
Researchers say they have identified a small molecule that can transport iron when typical transport routes are mutated or absent.
The molecule, hinokitiol, was able to move iron into or out of cells by wrapping around iron atoms and shuttling them across the membrane layer.
Hinokitiol promoted gut iron absorption in rats and mice deficient in iron transport complexes, and it promoted hemoglobin production in zebrafish that otherwise couldn’t transport iron effectively.
The researchers believe these findings, published in Science, may lead to new treatments for disorders associated with iron metabolism, such as anemias and hemochromatosis.
“The long-term therapeutic implications of our work with hinokitiol points to potentially using this chemical to correct anemias caused by genetic deficiencies of iron transporters required for normal red cell formation,” said study author Barry Paw, MD, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“At the same time, hinokitiol has the potential to correct iron-overload syndromes, such as hemochromatosis. More extensive clinical trials are necessary to work out the full potential of hinokitiol and to identify potential toxicities that we have not identified using preclinical models.”
Dr Paw and his colleagues discovered the potential of hinokitiol when screening for a molecule that could restore growth to yeast lacking an iron transporter complex. Hinokitiol is a natural product originally isolated from the Taiwanese hinoki tree.
The researchers found that hinokitiol could transport iron across the yeast cellular membrane in mutant yeasts lacking their major iron uptake transporters. Three hinokitiol molecules can wrap around an iron atom and transport it directly across the membrane where the missing protein should be.
The team also tested hinokitiol in mice, rats, and zebrafish that were missing iron-transport proteins.
Orally administered hinokitiol restored iron uptake in the guts of ferroportin-deficient mice and DMT1-deficient rats, and adding hinokitiol to a tank housing DMT1- and mitoferrin-deficient zebrafish prompted hemoglobin production in the fish.
The researchers also found that hinokitiol restored iron transport in human cells taken from the lining of the gut.
“We found that hinokitiol can restore iron transport within cells, out of cells, or both,” Dr Paw said. “It can also promote iron gut absorption and the creation of hemoglobin in some of our models. These findings suggest that small molecules like hinokitiol that can mimic the biological function of a missing protein may have potential for treating human diseases.” ![]()
Researchers say they have identified a small molecule that can transport iron when typical transport routes are mutated or absent.
The molecule, hinokitiol, was able to move iron into or out of cells by wrapping around iron atoms and shuttling them across the membrane layer.
Hinokitiol promoted gut iron absorption in rats and mice deficient in iron transport complexes, and it promoted hemoglobin production in zebrafish that otherwise couldn’t transport iron effectively.
The researchers believe these findings, published in Science, may lead to new treatments for disorders associated with iron metabolism, such as anemias and hemochromatosis.
“The long-term therapeutic implications of our work with hinokitiol points to potentially using this chemical to correct anemias caused by genetic deficiencies of iron transporters required for normal red cell formation,” said study author Barry Paw, MD, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“At the same time, hinokitiol has the potential to correct iron-overload syndromes, such as hemochromatosis. More extensive clinical trials are necessary to work out the full potential of hinokitiol and to identify potential toxicities that we have not identified using preclinical models.”
Dr Paw and his colleagues discovered the potential of hinokitiol when screening for a molecule that could restore growth to yeast lacking an iron transporter complex. Hinokitiol is a natural product originally isolated from the Taiwanese hinoki tree.
The researchers found that hinokitiol could transport iron across the yeast cellular membrane in mutant yeasts lacking their major iron uptake transporters. Three hinokitiol molecules can wrap around an iron atom and transport it directly across the membrane where the missing protein should be.
The team also tested hinokitiol in mice, rats, and zebrafish that were missing iron-transport proteins.
Orally administered hinokitiol restored iron uptake in the guts of ferroportin-deficient mice and DMT1-deficient rats, and adding hinokitiol to a tank housing DMT1- and mitoferrin-deficient zebrafish prompted hemoglobin production in the fish.
The researchers also found that hinokitiol restored iron transport in human cells taken from the lining of the gut.
“We found that hinokitiol can restore iron transport within cells, out of cells, or both,” Dr Paw said. “It can also promote iron gut absorption and the creation of hemoglobin in some of our models. These findings suggest that small molecules like hinokitiol that can mimic the biological function of a missing protein may have potential for treating human diseases.” ![]()
EMA recommends drug receive orphan designation for PNH
The European Medicines Agency (EMA) has recommended orphan drug designation for the complement C3 inhibitor APL-2 as a treatment for paroxysmal nocturnal hemoglobinuria (PNH).
APL-2 is a synthetic cyclic peptide conjugated to a polyethylene glycol polymer that binds specifically to C3 and C3b, blocking all 3 pathways of complement activation (classical, lectin, and alternative).
This comprehensive inhibition of complement-mediated pathology may have the potential to control symptoms and modify underlying disease in patients with PNH, according to Apellis Pharmaceuticals, Inc., the company developing APL-2.
APL-2 has been evaluated in a pair of phase 1 studies of healthy volunteers. Results from these studies were presented at the 2016 ASH Annual Meeting (abstract 1251).
Now, Apellis is evaluating APL-2 in PNH patients in a pair of phase 1b trials.
In PADDOCK (NCT02588833), researchers are assessing the safety, tolerability, pharmacokinetics, pharmacodynamics, and preliminary efficacy of multiple doses of APL-2 administered by daily subcutaneous injection in patients with PNH who have not received the standard of care in the past.
In PHAROAH (NCT02264639), researchers are assessing the safety, tolerability, pharmacokinetics, and pharmacodynamics of single and multiple doses of APL-2 administered by subcutaneous injection as an add-on to the standard of care in patients with PNH.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval. The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The European Commission typically makes a decision within 30 days. ![]()
The European Medicines Agency (EMA) has recommended orphan drug designation for the complement C3 inhibitor APL-2 as a treatment for paroxysmal nocturnal hemoglobinuria (PNH).
APL-2 is a synthetic cyclic peptide conjugated to a polyethylene glycol polymer that binds specifically to C3 and C3b, blocking all 3 pathways of complement activation (classical, lectin, and alternative).
This comprehensive inhibition of complement-mediated pathology may have the potential to control symptoms and modify underlying disease in patients with PNH, according to Apellis Pharmaceuticals, Inc., the company developing APL-2.
APL-2 has been evaluated in a pair of phase 1 studies of healthy volunteers. Results from these studies were presented at the 2016 ASH Annual Meeting (abstract 1251).
Now, Apellis is evaluating APL-2 in PNH patients in a pair of phase 1b trials.
In PADDOCK (NCT02588833), researchers are assessing the safety, tolerability, pharmacokinetics, pharmacodynamics, and preliminary efficacy of multiple doses of APL-2 administered by daily subcutaneous injection in patients with PNH who have not received the standard of care in the past.
In PHAROAH (NCT02264639), researchers are assessing the safety, tolerability, pharmacokinetics, and pharmacodynamics of single and multiple doses of APL-2 administered by subcutaneous injection as an add-on to the standard of care in patients with PNH.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval. The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The European Commission typically makes a decision within 30 days. ![]()
The European Medicines Agency (EMA) has recommended orphan drug designation for the complement C3 inhibitor APL-2 as a treatment for paroxysmal nocturnal hemoglobinuria (PNH).
APL-2 is a synthetic cyclic peptide conjugated to a polyethylene glycol polymer that binds specifically to C3 and C3b, blocking all 3 pathways of complement activation (classical, lectin, and alternative).
This comprehensive inhibition of complement-mediated pathology may have the potential to control symptoms and modify underlying disease in patients with PNH, according to Apellis Pharmaceuticals, Inc., the company developing APL-2.
APL-2 has been evaluated in a pair of phase 1 studies of healthy volunteers. Results from these studies were presented at the 2016 ASH Annual Meeting (abstract 1251).
Now, Apellis is evaluating APL-2 in PNH patients in a pair of phase 1b trials.
In PADDOCK (NCT02588833), researchers are assessing the safety, tolerability, pharmacokinetics, pharmacodynamics, and preliminary efficacy of multiple doses of APL-2 administered by daily subcutaneous injection in patients with PNH who have not received the standard of care in the past.
In PHAROAH (NCT02264639), researchers are assessing the safety, tolerability, pharmacokinetics, and pharmacodynamics of single and multiple doses of APL-2 administered by subcutaneous injection as an add-on to the standard of care in patients with PNH.
About orphan designation
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if the drug receives regulatory approval. The designation also provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure.
The EMA adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. The European Commission typically makes a decision within 30 days. ![]()
PPIs triple heart failure hospitalization risk in atrial fib patients
PARIS – Unwarranted prescriptions for proton pump inhibitors tripled the rate at which patients with atrial fibrillation needed hospitalization for a first episode of acute heart failure, in a retrospective study of 172 patients at a single center in Portugal.
About a third of the atrial fibrillation patients received a proton pump inhibitor (PPI) without a clear indication, and the PPI recipients developed heart failure at 2.9 times the rate as patients not on a PPI, a statistically significant difference, João B. Augusto, MD, reported at a meeting held by the Heart Failure Association of the European Society of Cardiology. Dr. Augusto believes that these patients largely had no need for PPI treatment, and the drug may have cut iron and vitamin B12 absorption by lowering gastric acid, resulting in deficiencies that produced anemia, and following that, heart failure, he suggested.
The study focused on 423 patients admitted to Fernando da Fonseca Hospital during January 2014–June 2015 with a primary or secondary diagnosis of atrial fibrillation. He excluded 101 patients with a history of heart failure, 109 patients on antiplatelet therapy, and 33 patients with a clear need for PPI treatment because of a gastrointestinal condition. Another 11 patients were lost to follow-up, leaving 172 patients followed for 1 year.
At the time of their initial hospitalization, 53 patients (31%) received a prescription for a PPI despite having no gastrointestinal diagnosis, likely a prophylactic step for patients receiving an oral anticoagulant, Dr. Augusto said. The patients averaged 69 years old, and nearly two-thirds were men.
During 1-year follow-up, the incidence of hospitalization for acute heart failure was 8% in the patients not on a PPI and 23% among those on a PPI, a statistically significant difference. In a regression analysis that controlled for age and chronic kidney disease, the incidence of acute heart failure was 2.9 times more common among patients on a PPI, Dr. Augusto said. He and his associates used these findings to educate their hospital’s staff to not needlessly prescribe a PPI to atrial fibrillation patients.
Dr. Augusto had no disclosures.
[email protected]
On Twitter @mitchelzoler
PARIS – Unwarranted prescriptions for proton pump inhibitors tripled the rate at which patients with atrial fibrillation needed hospitalization for a first episode of acute heart failure, in a retrospective study of 172 patients at a single center in Portugal.
About a third of the atrial fibrillation patients received a proton pump inhibitor (PPI) without a clear indication, and the PPI recipients developed heart failure at 2.9 times the rate as patients not on a PPI, a statistically significant difference, João B. Augusto, MD, reported at a meeting held by the Heart Failure Association of the European Society of Cardiology. Dr. Augusto believes that these patients largely had no need for PPI treatment, and the drug may have cut iron and vitamin B12 absorption by lowering gastric acid, resulting in deficiencies that produced anemia, and following that, heart failure, he suggested.
The study focused on 423 patients admitted to Fernando da Fonseca Hospital during January 2014–June 2015 with a primary or secondary diagnosis of atrial fibrillation. He excluded 101 patients with a history of heart failure, 109 patients on antiplatelet therapy, and 33 patients with a clear need for PPI treatment because of a gastrointestinal condition. Another 11 patients were lost to follow-up, leaving 172 patients followed for 1 year.
At the time of their initial hospitalization, 53 patients (31%) received a prescription for a PPI despite having no gastrointestinal diagnosis, likely a prophylactic step for patients receiving an oral anticoagulant, Dr. Augusto said. The patients averaged 69 years old, and nearly two-thirds were men.
During 1-year follow-up, the incidence of hospitalization for acute heart failure was 8% in the patients not on a PPI and 23% among those on a PPI, a statistically significant difference. In a regression analysis that controlled for age and chronic kidney disease, the incidence of acute heart failure was 2.9 times more common among patients on a PPI, Dr. Augusto said. He and his associates used these findings to educate their hospital’s staff to not needlessly prescribe a PPI to atrial fibrillation patients.
Dr. Augusto had no disclosures.
[email protected]
On Twitter @mitchelzoler
PARIS – Unwarranted prescriptions for proton pump inhibitors tripled the rate at which patients with atrial fibrillation needed hospitalization for a first episode of acute heart failure, in a retrospective study of 172 patients at a single center in Portugal.
About a third of the atrial fibrillation patients received a proton pump inhibitor (PPI) without a clear indication, and the PPI recipients developed heart failure at 2.9 times the rate as patients not on a PPI, a statistically significant difference, João B. Augusto, MD, reported at a meeting held by the Heart Failure Association of the European Society of Cardiology. Dr. Augusto believes that these patients largely had no need for PPI treatment, and the drug may have cut iron and vitamin B12 absorption by lowering gastric acid, resulting in deficiencies that produced anemia, and following that, heart failure, he suggested.
The study focused on 423 patients admitted to Fernando da Fonseca Hospital during January 2014–June 2015 with a primary or secondary diagnosis of atrial fibrillation. He excluded 101 patients with a history of heart failure, 109 patients on antiplatelet therapy, and 33 patients with a clear need for PPI treatment because of a gastrointestinal condition. Another 11 patients were lost to follow-up, leaving 172 patients followed for 1 year.
At the time of their initial hospitalization, 53 patients (31%) received a prescription for a PPI despite having no gastrointestinal diagnosis, likely a prophylactic step for patients receiving an oral anticoagulant, Dr. Augusto said. The patients averaged 69 years old, and nearly two-thirds were men.
During 1-year follow-up, the incidence of hospitalization for acute heart failure was 8% in the patients not on a PPI and 23% among those on a PPI, a statistically significant difference. In a regression analysis that controlled for age and chronic kidney disease, the incidence of acute heart failure was 2.9 times more common among patients on a PPI, Dr. Augusto said. He and his associates used these findings to educate their hospital’s staff to not needlessly prescribe a PPI to atrial fibrillation patients.
Dr. Augusto had no disclosures.
[email protected]
On Twitter @mitchelzoler
AT HEART FAILURE 2017
Key clinical point:
Major finding: Atrial fibrillation patients had a 2.9 times higher acute heart failure rate on a proton pump inhibitor, compared with no PPI.
Data source: Retrospective review of 172 atrial fibrillation patients seen during 2014-2015 at a single center in Portugal.
Disclosures: Dr. Augusto had no disclosures.
Drug elicits responses in MDS patients
VALENCIA, SPAIN—Phase 2 results suggest luspatercept can produce erythroid responses and enable transfusion independence in patients with myelodysplastic syndromes (MDS).
Erythroid response rates were similar whether or not patients had received prior treatment with erythropoiesis-stimulating agents (ESAs).
However, patients without prior ESA exposure were more likely to achieve transfusion independence.
Most adverse events (AEs) considered possibly or probably related to luspatercept were grade 1 or 2.
Uwe Platzbecker, MD, of Universitätsklinikum Carl Gustav Carus in Dresden, Germany, presented these results at the 14th International Symposium on MDS.
The research was sponsored by Acceleron Pharma Inc., the company developing luspatercept in collaboration with Celgene Corporation.
Dr Platzbecker explained that luspatercept, formerly ACE-536, is a modified activin receptor type IIB fusion protein that acts as a ligand trap for GDF11 and other TGF-βfamily ligands to suppress Smad2/3 signaling.
He presented data from a phase 2 base study and an extension study of luspatercept. The base study included 89 patients who received luspatercept for 3 months. The long-term extension study included 52 patients who may receive luspatercept for an additional 5 years.
The patients received luspatercept at doses ranging from 0.125 mg/kg to 1.75 mg/kg in the base study and 1.0 mg/kg to 1.75 mg/kg in the extension study. They received the drug subcutaneously every 3 weeks.
There were 82 patients evaluable for efficacy. They were a median of 2.3 years from diagnosis (range, 0-14). Their median age was 72 (range, 29-90), 63% were male, and 52% had prior treatment with ESAs.
The outcome measures used in these studies were clinically meaningful erythroid hematologic improvement per the International Working Group’s criteria (IWG HI-E) and red blood cell transfusion independence (RBC-TI).
IWG HI-E was defined as hemoglobin increase ≥ 1.5 g/dL sustained for ≥ 8 weeks in patients with a transfusion burden at baseline of less than 4 RBC units every 8 weeks and baseline hemoglobin levels below 10 g/dL. For patients with a greater transfusion burden at baseline, erythroid response was defined as a reduction of ≥ 4 RBC units sustained for ≥ 8 weeks.
RBC-TI was defined as no RBC transfusions for ≥ 8 weeks in patients with a baseline transfusion burden of at least 2 RBC units every 8 weeks.
Response data
In ESA-naïve patients, 48% (11/23) achieved RBC-TI with luspatercept, and 51% (20/39) achieved an IWG HI-E response.
Among patients with prior ESA treatment, 33% (11/33) achieved RBC-TI with luspatercept, and 51% (22/43) achieved an IWG HI-E response.
In patients with baseline erythropoietin (EPO) levels ≤ 500 international units per liter (IU/L), RBC-TI and IWG HI-E response rates were positive in both ring sideroblast-positive (RS+) and RS-negative (RS-) patients, according to the researchers.
| Baseline
EPO (IU/L) |
RS status | IWG HI-E, n=82
n (%) |
RBC-TI, n=56
n (%) |
| ≤ 500 | RS+ | 30/46 (65%) | 16/29 (55%) |
| RS- | 6/14 (43%) | 4/7 (57%) | |
| > 500 | RS+ | 5/9 (56%) | 2/9 (22%) |
| RS- | 1/11 (9%) | 0/9 (0%) | |
| Unknown | 0/2 (0%) | 0/2 (0%) |
*Table includes ESA-refractory and ESA-naïve patients. Patients treated at dose levels ≥ 0.75 mg/kg.
Safety data
All 89 patients were evaluable for safety. Common AEs (occurring in at least 3 patients) that were considered possibly or probably related to study drug were fatigue (6.7%), headache (6.7%), hypertension (5.6%), diarrhea (4.5%), arthralgia (3.4%), bone pain (3.4%), injection site erythema (3.4%), myalgia (3.4%), and peripheral edema (3.4%).
Grade 3 AEs possibly or probably related to study drug were ascites, blast cell count increase, blood bilirubin increase, hypertension, platelet count increase, and pleural effusion.
Grade 3 serious AEs possibly or probably related to study drug were general physical health deterioration and myalgia. ![]()
VALENCIA, SPAIN—Phase 2 results suggest luspatercept can produce erythroid responses and enable transfusion independence in patients with myelodysplastic syndromes (MDS).
Erythroid response rates were similar whether or not patients had received prior treatment with erythropoiesis-stimulating agents (ESAs).
However, patients without prior ESA exposure were more likely to achieve transfusion independence.
Most adverse events (AEs) considered possibly or probably related to luspatercept were grade 1 or 2.
Uwe Platzbecker, MD, of Universitätsklinikum Carl Gustav Carus in Dresden, Germany, presented these results at the 14th International Symposium on MDS.
The research was sponsored by Acceleron Pharma Inc., the company developing luspatercept in collaboration with Celgene Corporation.
Dr Platzbecker explained that luspatercept, formerly ACE-536, is a modified activin receptor type IIB fusion protein that acts as a ligand trap for GDF11 and other TGF-βfamily ligands to suppress Smad2/3 signaling.
He presented data from a phase 2 base study and an extension study of luspatercept. The base study included 89 patients who received luspatercept for 3 months. The long-term extension study included 52 patients who may receive luspatercept for an additional 5 years.
The patients received luspatercept at doses ranging from 0.125 mg/kg to 1.75 mg/kg in the base study and 1.0 mg/kg to 1.75 mg/kg in the extension study. They received the drug subcutaneously every 3 weeks.
There were 82 patients evaluable for efficacy. They were a median of 2.3 years from diagnosis (range, 0-14). Their median age was 72 (range, 29-90), 63% were male, and 52% had prior treatment with ESAs.
The outcome measures used in these studies were clinically meaningful erythroid hematologic improvement per the International Working Group’s criteria (IWG HI-E) and red blood cell transfusion independence (RBC-TI).
IWG HI-E was defined as hemoglobin increase ≥ 1.5 g/dL sustained for ≥ 8 weeks in patients with a transfusion burden at baseline of less than 4 RBC units every 8 weeks and baseline hemoglobin levels below 10 g/dL. For patients with a greater transfusion burden at baseline, erythroid response was defined as a reduction of ≥ 4 RBC units sustained for ≥ 8 weeks.
RBC-TI was defined as no RBC transfusions for ≥ 8 weeks in patients with a baseline transfusion burden of at least 2 RBC units every 8 weeks.
Response data
In ESA-naïve patients, 48% (11/23) achieved RBC-TI with luspatercept, and 51% (20/39) achieved an IWG HI-E response.
Among patients with prior ESA treatment, 33% (11/33) achieved RBC-TI with luspatercept, and 51% (22/43) achieved an IWG HI-E response.
In patients with baseline erythropoietin (EPO) levels ≤ 500 international units per liter (IU/L), RBC-TI and IWG HI-E response rates were positive in both ring sideroblast-positive (RS+) and RS-negative (RS-) patients, according to the researchers.
| Baseline
EPO (IU/L) |
RS status | IWG HI-E, n=82
n (%) |
RBC-TI, n=56
n (%) |
| ≤ 500 | RS+ | 30/46 (65%) | 16/29 (55%) |
| RS- | 6/14 (43%) | 4/7 (57%) | |
| > 500 | RS+ | 5/9 (56%) | 2/9 (22%) |
| RS- | 1/11 (9%) | 0/9 (0%) | |
| Unknown | 0/2 (0%) | 0/2 (0%) |
*Table includes ESA-refractory and ESA-naïve patients. Patients treated at dose levels ≥ 0.75 mg/kg.
Safety data
All 89 patients were evaluable for safety. Common AEs (occurring in at least 3 patients) that were considered possibly or probably related to study drug were fatigue (6.7%), headache (6.7%), hypertension (5.6%), diarrhea (4.5%), arthralgia (3.4%), bone pain (3.4%), injection site erythema (3.4%), myalgia (3.4%), and peripheral edema (3.4%).
Grade 3 AEs possibly or probably related to study drug were ascites, blast cell count increase, blood bilirubin increase, hypertension, platelet count increase, and pleural effusion.
Grade 3 serious AEs possibly or probably related to study drug were general physical health deterioration and myalgia. ![]()
VALENCIA, SPAIN—Phase 2 results suggest luspatercept can produce erythroid responses and enable transfusion independence in patients with myelodysplastic syndromes (MDS).
Erythroid response rates were similar whether or not patients had received prior treatment with erythropoiesis-stimulating agents (ESAs).
However, patients without prior ESA exposure were more likely to achieve transfusion independence.
Most adverse events (AEs) considered possibly or probably related to luspatercept were grade 1 or 2.
Uwe Platzbecker, MD, of Universitätsklinikum Carl Gustav Carus in Dresden, Germany, presented these results at the 14th International Symposium on MDS.
The research was sponsored by Acceleron Pharma Inc., the company developing luspatercept in collaboration with Celgene Corporation.
Dr Platzbecker explained that luspatercept, formerly ACE-536, is a modified activin receptor type IIB fusion protein that acts as a ligand trap for GDF11 and other TGF-βfamily ligands to suppress Smad2/3 signaling.
He presented data from a phase 2 base study and an extension study of luspatercept. The base study included 89 patients who received luspatercept for 3 months. The long-term extension study included 52 patients who may receive luspatercept for an additional 5 years.
The patients received luspatercept at doses ranging from 0.125 mg/kg to 1.75 mg/kg in the base study and 1.0 mg/kg to 1.75 mg/kg in the extension study. They received the drug subcutaneously every 3 weeks.
There were 82 patients evaluable for efficacy. They were a median of 2.3 years from diagnosis (range, 0-14). Their median age was 72 (range, 29-90), 63% were male, and 52% had prior treatment with ESAs.
The outcome measures used in these studies were clinically meaningful erythroid hematologic improvement per the International Working Group’s criteria (IWG HI-E) and red blood cell transfusion independence (RBC-TI).
IWG HI-E was defined as hemoglobin increase ≥ 1.5 g/dL sustained for ≥ 8 weeks in patients with a transfusion burden at baseline of less than 4 RBC units every 8 weeks and baseline hemoglobin levels below 10 g/dL. For patients with a greater transfusion burden at baseline, erythroid response was defined as a reduction of ≥ 4 RBC units sustained for ≥ 8 weeks.
RBC-TI was defined as no RBC transfusions for ≥ 8 weeks in patients with a baseline transfusion burden of at least 2 RBC units every 8 weeks.
Response data
In ESA-naïve patients, 48% (11/23) achieved RBC-TI with luspatercept, and 51% (20/39) achieved an IWG HI-E response.
Among patients with prior ESA treatment, 33% (11/33) achieved RBC-TI with luspatercept, and 51% (22/43) achieved an IWG HI-E response.
In patients with baseline erythropoietin (EPO) levels ≤ 500 international units per liter (IU/L), RBC-TI and IWG HI-E response rates were positive in both ring sideroblast-positive (RS+) and RS-negative (RS-) patients, according to the researchers.
| Baseline
EPO (IU/L) |
RS status | IWG HI-E, n=82
n (%) |
RBC-TI, n=56
n (%) |
| ≤ 500 | RS+ | 30/46 (65%) | 16/29 (55%) |
| RS- | 6/14 (43%) | 4/7 (57%) | |
| > 500 | RS+ | 5/9 (56%) | 2/9 (22%) |
| RS- | 1/11 (9%) | 0/9 (0%) | |
| Unknown | 0/2 (0%) | 0/2 (0%) |
*Table includes ESA-refractory and ESA-naïve patients. Patients treated at dose levels ≥ 0.75 mg/kg.
Safety data
All 89 patients were evaluable for safety. Common AEs (occurring in at least 3 patients) that were considered possibly or probably related to study drug were fatigue (6.7%), headache (6.7%), hypertension (5.6%), diarrhea (4.5%), arthralgia (3.4%), bone pain (3.4%), injection site erythema (3.4%), myalgia (3.4%), and peripheral edema (3.4%).
Grade 3 AEs possibly or probably related to study drug were ascites, blast cell count increase, blood bilirubin increase, hypertension, platelet count increase, and pleural effusion.
Grade 3 serious AEs possibly or probably related to study drug were general physical health deterioration and myalgia. ![]()
Novel inhibitor proves ‘potent’ in hematologic malignancies
BOSTON—A pair of preclinical studies suggest the FLT3/BTK inhibitor CG’806 is active in a range of hematologic malignancies.
In one of the studies, CG’806 proved particularly effective against acute myeloid leukemia (AML) cells harboring mutant forms of FLT3, and the compound was able to eradicate AML in mice.
In another study, researchers found CG’806 exhibited “broad potency” against leukemias, lymphomas, myelodysplastic syndromes (MDS), and myeloproliferative neoplasms (MPNs).
Both studies were presented as posters at Hematologic Malignancies: Translating Discoveries to Novel Therapies (poster 25 and poster 44).
Both studies involved researchers from Aptose Biosciences, the company developing CG’806.
Poster 25
Weiguo Zhang, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston, and his colleagues presented poster 25, “CG’806, a first-in-class FLT3/BTK inhibitor, exerts superior potency against AML cells harboring ITD, TKD and gatekeeper mutated FLT3 or wild-type FLT3.”
The researchers tested CG’806 and other FLT3 inhibitors in human or murine leukemia cell lines with wild-type (WT) FLT3, FLT3-ITD mutations, FLT3 TKD domain mutations, or ITD plus TKD mutations.
Compared to second-generation FLT3 inhibitors (quizartinib, gilteritinib, or crenolanib), CG’806 showed more pronounced anti-proliferative effects in leukemia cells with ITD mutations, D835 mutations, ITD plus F691I/Y842D/D835 mutations, or in FLT3 WT cells.
With CG’086, the IC50s in human AML cell lines were 0.17 nM for MV4-11 (FLT3-ITD) and 0.82 nM for MOLM13 (FLT3-ITD).
The IC50s in the murine leukemia cell lines were 9.49 nM for Ba/F3 (FLT3-WT), 0.30 nM for Ba/F3 (FLT3-ITD), 8.26 nM for Ba/F3 (FLT3-D835Y), 9.72 nM for Ba/F3 (FLT3-ITD+D835Y), and 0.43 nM for Ba/F3 (FLT3-ITD+F691L).
The researchers also found that CG’806 “triggers marked apoptosis” in FLT3-ITD-mutated primary AML samples but minimal apoptosis in normal bone marrow cells.
Another finding was that once-daily oral dosing of CG’806 in a murine model of AML (MV4-11) resulted in sustained micromolar plasma concentration over a 24-hour period.
This was accompanied by complete elimination of AML FLT3-ITD tumors without toxicity, the researchers said.
Poster 44
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented poster 44, “CG’806, a First-in-Class FLT3/BTK Inhibitor, Exhibits Potent Activity against AML Patient Samples with Mutant or Wild-Type FLT3, as well as Other Hematologic Malignancy Subtypes.”
The researchers tested CG’806 in samples from patients with AML (n=82), MDS/MPNs (n=15), acute lymphoblastic leukemia (ALL, n=17), chronic lymphocytic leukemia (CLL, n=58), and chronic myeloid leukemia (CML, n=4).
The team observed “broad sensitivity” to CG’806, with 59% (48/82) of AML, 53% (8/15) of MDS/MPN, 40% (23/58) of CLL, 29% (5/17) of ALL, and 25% (1/4) of CML cases exhibiting an IC50 of less than 100 nM.
Among the 38 tested AML samples with known FLT3 mutational status, the FLT3-ITD+ AML samples tended to have enhanced sensitivity to CG’806 (median IC50 = 20 nM, n=8) relative to the FLT3-WT samples (median IC50 = 120 nM, n=30).
The researchers also found that CG’806 exerted potent anti-proliferative activity against human AML, B-ALL, mantle cell lymphoma, Burkitt lymphoma, and diffuse large B-cell lymphoma cell lines.
“The analyses of CG’806 against primary hematologic malignancy patient samples and cultured cell lines show evidence of potent and broad drug activity in AML and other disease subtypes and support further development of this agent for hematologic malignancies,” Dr Kurtz said. ![]()
BOSTON—A pair of preclinical studies suggest the FLT3/BTK inhibitor CG’806 is active in a range of hematologic malignancies.
In one of the studies, CG’806 proved particularly effective against acute myeloid leukemia (AML) cells harboring mutant forms of FLT3, and the compound was able to eradicate AML in mice.
In another study, researchers found CG’806 exhibited “broad potency” against leukemias, lymphomas, myelodysplastic syndromes (MDS), and myeloproliferative neoplasms (MPNs).
Both studies were presented as posters at Hematologic Malignancies: Translating Discoveries to Novel Therapies (poster 25 and poster 44).
Both studies involved researchers from Aptose Biosciences, the company developing CG’806.
Poster 25
Weiguo Zhang, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston, and his colleagues presented poster 25, “CG’806, a first-in-class FLT3/BTK inhibitor, exerts superior potency against AML cells harboring ITD, TKD and gatekeeper mutated FLT3 or wild-type FLT3.”
The researchers tested CG’806 and other FLT3 inhibitors in human or murine leukemia cell lines with wild-type (WT) FLT3, FLT3-ITD mutations, FLT3 TKD domain mutations, or ITD plus TKD mutations.
Compared to second-generation FLT3 inhibitors (quizartinib, gilteritinib, or crenolanib), CG’806 showed more pronounced anti-proliferative effects in leukemia cells with ITD mutations, D835 mutations, ITD plus F691I/Y842D/D835 mutations, or in FLT3 WT cells.
With CG’086, the IC50s in human AML cell lines were 0.17 nM for MV4-11 (FLT3-ITD) and 0.82 nM for MOLM13 (FLT3-ITD).
The IC50s in the murine leukemia cell lines were 9.49 nM for Ba/F3 (FLT3-WT), 0.30 nM for Ba/F3 (FLT3-ITD), 8.26 nM for Ba/F3 (FLT3-D835Y), 9.72 nM for Ba/F3 (FLT3-ITD+D835Y), and 0.43 nM for Ba/F3 (FLT3-ITD+F691L).
The researchers also found that CG’806 “triggers marked apoptosis” in FLT3-ITD-mutated primary AML samples but minimal apoptosis in normal bone marrow cells.
Another finding was that once-daily oral dosing of CG’806 in a murine model of AML (MV4-11) resulted in sustained micromolar plasma concentration over a 24-hour period.
This was accompanied by complete elimination of AML FLT3-ITD tumors without toxicity, the researchers said.
Poster 44
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented poster 44, “CG’806, a First-in-Class FLT3/BTK Inhibitor, Exhibits Potent Activity against AML Patient Samples with Mutant or Wild-Type FLT3, as well as Other Hematologic Malignancy Subtypes.”
The researchers tested CG’806 in samples from patients with AML (n=82), MDS/MPNs (n=15), acute lymphoblastic leukemia (ALL, n=17), chronic lymphocytic leukemia (CLL, n=58), and chronic myeloid leukemia (CML, n=4).
The team observed “broad sensitivity” to CG’806, with 59% (48/82) of AML, 53% (8/15) of MDS/MPN, 40% (23/58) of CLL, 29% (5/17) of ALL, and 25% (1/4) of CML cases exhibiting an IC50 of less than 100 nM.
Among the 38 tested AML samples with known FLT3 mutational status, the FLT3-ITD+ AML samples tended to have enhanced sensitivity to CG’806 (median IC50 = 20 nM, n=8) relative to the FLT3-WT samples (median IC50 = 120 nM, n=30).
The researchers also found that CG’806 exerted potent anti-proliferative activity against human AML, B-ALL, mantle cell lymphoma, Burkitt lymphoma, and diffuse large B-cell lymphoma cell lines.
“The analyses of CG’806 against primary hematologic malignancy patient samples and cultured cell lines show evidence of potent and broad drug activity in AML and other disease subtypes and support further development of this agent for hematologic malignancies,” Dr Kurtz said. ![]()
BOSTON—A pair of preclinical studies suggest the FLT3/BTK inhibitor CG’806 is active in a range of hematologic malignancies.
In one of the studies, CG’806 proved particularly effective against acute myeloid leukemia (AML) cells harboring mutant forms of FLT3, and the compound was able to eradicate AML in mice.
In another study, researchers found CG’806 exhibited “broad potency” against leukemias, lymphomas, myelodysplastic syndromes (MDS), and myeloproliferative neoplasms (MPNs).
Both studies were presented as posters at Hematologic Malignancies: Translating Discoveries to Novel Therapies (poster 25 and poster 44).
Both studies involved researchers from Aptose Biosciences, the company developing CG’806.
Poster 25
Weiguo Zhang, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston, and his colleagues presented poster 25, “CG’806, a first-in-class FLT3/BTK inhibitor, exerts superior potency against AML cells harboring ITD, TKD and gatekeeper mutated FLT3 or wild-type FLT3.”
The researchers tested CG’806 and other FLT3 inhibitors in human or murine leukemia cell lines with wild-type (WT) FLT3, FLT3-ITD mutations, FLT3 TKD domain mutations, or ITD plus TKD mutations.
Compared to second-generation FLT3 inhibitors (quizartinib, gilteritinib, or crenolanib), CG’806 showed more pronounced anti-proliferative effects in leukemia cells with ITD mutations, D835 mutations, ITD plus F691I/Y842D/D835 mutations, or in FLT3 WT cells.
With CG’086, the IC50s in human AML cell lines were 0.17 nM for MV4-11 (FLT3-ITD) and 0.82 nM for MOLM13 (FLT3-ITD).
The IC50s in the murine leukemia cell lines were 9.49 nM for Ba/F3 (FLT3-WT), 0.30 nM for Ba/F3 (FLT3-ITD), 8.26 nM for Ba/F3 (FLT3-D835Y), 9.72 nM for Ba/F3 (FLT3-ITD+D835Y), and 0.43 nM for Ba/F3 (FLT3-ITD+F691L).
The researchers also found that CG’806 “triggers marked apoptosis” in FLT3-ITD-mutated primary AML samples but minimal apoptosis in normal bone marrow cells.
Another finding was that once-daily oral dosing of CG’806 in a murine model of AML (MV4-11) resulted in sustained micromolar plasma concentration over a 24-hour period.
This was accompanied by complete elimination of AML FLT3-ITD tumors without toxicity, the researchers said.
Poster 44
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented poster 44, “CG’806, a First-in-Class FLT3/BTK Inhibitor, Exhibits Potent Activity against AML Patient Samples with Mutant or Wild-Type FLT3, as well as Other Hematologic Malignancy Subtypes.”
The researchers tested CG’806 in samples from patients with AML (n=82), MDS/MPNs (n=15), acute lymphoblastic leukemia (ALL, n=17), chronic lymphocytic leukemia (CLL, n=58), and chronic myeloid leukemia (CML, n=4).
The team observed “broad sensitivity” to CG’806, with 59% (48/82) of AML, 53% (8/15) of MDS/MPN, 40% (23/58) of CLL, 29% (5/17) of ALL, and 25% (1/4) of CML cases exhibiting an IC50 of less than 100 nM.
Among the 38 tested AML samples with known FLT3 mutational status, the FLT3-ITD+ AML samples tended to have enhanced sensitivity to CG’806 (median IC50 = 20 nM, n=8) relative to the FLT3-WT samples (median IC50 = 120 nM, n=30).
The researchers also found that CG’806 exerted potent anti-proliferative activity against human AML, B-ALL, mantle cell lymphoma, Burkitt lymphoma, and diffuse large B-cell lymphoma cell lines.
“The analyses of CG’806 against primary hematologic malignancy patient samples and cultured cell lines show evidence of potent and broad drug activity in AML and other disease subtypes and support further development of this agent for hematologic malignancies,” Dr Kurtz said. ![]()
Study shows similar outcomes with RIC and MAC in MDS
Results of a phase 3 trial revealed similar outcomes in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) to treat myelodysplastic syndromes (MDS), regardless of the conditioning regimen they received.
Rates of engraftment, graft-vs-host disease (GVHD), relapse, and survival were similar between patients who received reduced-intensity conditioning (RIC) and those who received standard myeloablative conditioning (MAC) before HSCT.
Researchers reported these results in the Journal of Clinical Oncology.
“Our study shed new light on expected benefits of a reduced-intensity conditioning regimen that can be offered as a curative treatment approach, especially in older patients with MDS,” said study author Nicolaus Kröger, MD, of University Hospital Eppendorf in Hamburg, Germany.
Patient characteristics
The study, known as RICMAC, involved 129 patients who underwent HSCT between May 2004 and December 2012 at 18 transplant units in 7 countries.
Patients were randomized in a 1:1 ratio to RIC (n=65) or MAC (n=64) and were stratified according to donor type, age, and blast count.
The median age was 50 (range, 19-64) in the MAC arm and 51 (range, 22-63) in the RIC arm. The median blast percentage was 4% (range, 0-18) and 5% (range, 0-18), respectively.
According to IPSS, most patients in both arms had intermediate-I-risk disease (28 MAC, 25 RIC) or intermediate-II-risk disease (18 MAC, 24 RIC).
Similar numbers of patients in each arm had low cytogenetic risk (24 MAC, 28 RIC), intermediate cytogenetic risk (17 MAC, 13 RIC), and high cytogenetic risk (17 MAC, 18 RIC).
Thirty-three patients in the MAC arm and 32 in the RIC arm received ATG as GVHD prophylaxis.
Patients received grafts from matched related donors (17 MAC, 16 RIC), matched unrelated donors (36 MAC, 38 RIC), or mismatched related/unrelated donors (11 in both arms).
Most patients received peripheral blood stem cell grafts—61 in the MAC arm and 59 in the RIC arm.
Results
The researchers said engraftment was comparable between the arms. There were 4 graft failures in the MAC arm and 3 in the RIC arm (P=0.72). The median time to leukocyte engraftment was 15 days in both arms. The median time to platelet engraftment was 15 days in the RIC arm and 16 in the MAC arm (P=0.33).
There was no significant difference in the cumulative incidence of GVHD between the RIC and MAC arms:
- Grade 2-4 acute GVHD—32.3% and 37.5%, respectively
- Grade 3-4 acute GVHD—15% and 14%, respectively (P=0.35 for between-arm difference for all acute GVHD)
- Chronic GVHD—61.6% and 64.7%, respectively (P=0.76).
Though the occurrence of infection was similar between the MAC and RIC arms (48 and 44, respectively), the rate of infection was higher in the MAC arm than the RIC arm.
The rate of infection in the first 100 days was 6.9 per 100 person-years in the MAC arm and 4.3 in the RIC arm (P=0.002). The rate of infection during the total follow-up was 2.0 per 100 person-years in the MAC arm and 1.4 in the RIC arm (P=0.002).
There was no significant difference between the RIC and MAC arms with regard to the cumulative incidence of nonrelapse mortality after 1 year—16.9% and 25.3%, respectively (P=0.29).
And there was no significant difference in the cumulative incidence of relapse at 2 years—17% and 14.8%, respectively (P=0.6).
The 2-year relapse-free survival rate was similar in the MAC and RIC arms—58.3% and 62.4% (P=0.58)—as was the 2-year overall survival rate—63.2% and 76.3%, respectively (P=0.08). ![]()
Results of a phase 3 trial revealed similar outcomes in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) to treat myelodysplastic syndromes (MDS), regardless of the conditioning regimen they received.
Rates of engraftment, graft-vs-host disease (GVHD), relapse, and survival were similar between patients who received reduced-intensity conditioning (RIC) and those who received standard myeloablative conditioning (MAC) before HSCT.
Researchers reported these results in the Journal of Clinical Oncology.
“Our study shed new light on expected benefits of a reduced-intensity conditioning regimen that can be offered as a curative treatment approach, especially in older patients with MDS,” said study author Nicolaus Kröger, MD, of University Hospital Eppendorf in Hamburg, Germany.
Patient characteristics
The study, known as RICMAC, involved 129 patients who underwent HSCT between May 2004 and December 2012 at 18 transplant units in 7 countries.
Patients were randomized in a 1:1 ratio to RIC (n=65) or MAC (n=64) and were stratified according to donor type, age, and blast count.
The median age was 50 (range, 19-64) in the MAC arm and 51 (range, 22-63) in the RIC arm. The median blast percentage was 4% (range, 0-18) and 5% (range, 0-18), respectively.
According to IPSS, most patients in both arms had intermediate-I-risk disease (28 MAC, 25 RIC) or intermediate-II-risk disease (18 MAC, 24 RIC).
Similar numbers of patients in each arm had low cytogenetic risk (24 MAC, 28 RIC), intermediate cytogenetic risk (17 MAC, 13 RIC), and high cytogenetic risk (17 MAC, 18 RIC).
Thirty-three patients in the MAC arm and 32 in the RIC arm received ATG as GVHD prophylaxis.
Patients received grafts from matched related donors (17 MAC, 16 RIC), matched unrelated donors (36 MAC, 38 RIC), or mismatched related/unrelated donors (11 in both arms).
Most patients received peripheral blood stem cell grafts—61 in the MAC arm and 59 in the RIC arm.
Results
The researchers said engraftment was comparable between the arms. There were 4 graft failures in the MAC arm and 3 in the RIC arm (P=0.72). The median time to leukocyte engraftment was 15 days in both arms. The median time to platelet engraftment was 15 days in the RIC arm and 16 in the MAC arm (P=0.33).
There was no significant difference in the cumulative incidence of GVHD between the RIC and MAC arms:
- Grade 2-4 acute GVHD—32.3% and 37.5%, respectively
- Grade 3-4 acute GVHD—15% and 14%, respectively (P=0.35 for between-arm difference for all acute GVHD)
- Chronic GVHD—61.6% and 64.7%, respectively (P=0.76).
Though the occurrence of infection was similar between the MAC and RIC arms (48 and 44, respectively), the rate of infection was higher in the MAC arm than the RIC arm.
The rate of infection in the first 100 days was 6.9 per 100 person-years in the MAC arm and 4.3 in the RIC arm (P=0.002). The rate of infection during the total follow-up was 2.0 per 100 person-years in the MAC arm and 1.4 in the RIC arm (P=0.002).
There was no significant difference between the RIC and MAC arms with regard to the cumulative incidence of nonrelapse mortality after 1 year—16.9% and 25.3%, respectively (P=0.29).
And there was no significant difference in the cumulative incidence of relapse at 2 years—17% and 14.8%, respectively (P=0.6).
The 2-year relapse-free survival rate was similar in the MAC and RIC arms—58.3% and 62.4% (P=0.58)—as was the 2-year overall survival rate—63.2% and 76.3%, respectively (P=0.08). ![]()
Results of a phase 3 trial revealed similar outcomes in patients who underwent allogeneic hematopoietic stem cell transplant (HSCT) to treat myelodysplastic syndromes (MDS), regardless of the conditioning regimen they received.
Rates of engraftment, graft-vs-host disease (GVHD), relapse, and survival were similar between patients who received reduced-intensity conditioning (RIC) and those who received standard myeloablative conditioning (MAC) before HSCT.
Researchers reported these results in the Journal of Clinical Oncology.
“Our study shed new light on expected benefits of a reduced-intensity conditioning regimen that can be offered as a curative treatment approach, especially in older patients with MDS,” said study author Nicolaus Kröger, MD, of University Hospital Eppendorf in Hamburg, Germany.
Patient characteristics
The study, known as RICMAC, involved 129 patients who underwent HSCT between May 2004 and December 2012 at 18 transplant units in 7 countries.
Patients were randomized in a 1:1 ratio to RIC (n=65) or MAC (n=64) and were stratified according to donor type, age, and blast count.
The median age was 50 (range, 19-64) in the MAC arm and 51 (range, 22-63) in the RIC arm. The median blast percentage was 4% (range, 0-18) and 5% (range, 0-18), respectively.
According to IPSS, most patients in both arms had intermediate-I-risk disease (28 MAC, 25 RIC) or intermediate-II-risk disease (18 MAC, 24 RIC).
Similar numbers of patients in each arm had low cytogenetic risk (24 MAC, 28 RIC), intermediate cytogenetic risk (17 MAC, 13 RIC), and high cytogenetic risk (17 MAC, 18 RIC).
Thirty-three patients in the MAC arm and 32 in the RIC arm received ATG as GVHD prophylaxis.
Patients received grafts from matched related donors (17 MAC, 16 RIC), matched unrelated donors (36 MAC, 38 RIC), or mismatched related/unrelated donors (11 in both arms).
Most patients received peripheral blood stem cell grafts—61 in the MAC arm and 59 in the RIC arm.
Results
The researchers said engraftment was comparable between the arms. There were 4 graft failures in the MAC arm and 3 in the RIC arm (P=0.72). The median time to leukocyte engraftment was 15 days in both arms. The median time to platelet engraftment was 15 days in the RIC arm and 16 in the MAC arm (P=0.33).
There was no significant difference in the cumulative incidence of GVHD between the RIC and MAC arms:
- Grade 2-4 acute GVHD—32.3% and 37.5%, respectively
- Grade 3-4 acute GVHD—15% and 14%, respectively (P=0.35 for between-arm difference for all acute GVHD)
- Chronic GVHD—61.6% and 64.7%, respectively (P=0.76).
Though the occurrence of infection was similar between the MAC and RIC arms (48 and 44, respectively), the rate of infection was higher in the MAC arm than the RIC arm.
The rate of infection in the first 100 days was 6.9 per 100 person-years in the MAC arm and 4.3 in the RIC arm (P=0.002). The rate of infection during the total follow-up was 2.0 per 100 person-years in the MAC arm and 1.4 in the RIC arm (P=0.002).
There was no significant difference between the RIC and MAC arms with regard to the cumulative incidence of nonrelapse mortality after 1 year—16.9% and 25.3%, respectively (P=0.29).
And there was no significant difference in the cumulative incidence of relapse at 2 years—17% and 14.8%, respectively (P=0.6).
The 2-year relapse-free survival rate was similar in the MAC and RIC arms—58.3% and 62.4% (P=0.58)—as was the 2-year overall survival rate—63.2% and 76.3%, respectively (P=0.08).
In sickle cell disease, osteomyelitis is a tough call
MONTREAL – Osteomyelitis is an especially challenging diagnosis in children with sickle cell disease (SCD) because the bone and joint signs, elevated white cell counts, and C-reactive protein levels that are commonly used to diagnose bone infection are frequently features of SCD as well.
As a result, most patients with SCD and suspected osteomyelitis are treated without a confirmation of the diagnosis.
Among 30 patients with SCD who were followed at a single center over a decade, 29 patients had elevated ESR, but only 13 patients had leukocytosis, and only 13 had elevated CRP.
“Prior studies on sickle cell disease have shown that it is very difficult to differentiate between osteoarticular infection and bone infarction. Therefore, oftentimes, this diagnosis is very difficult to make,” Dr. Weisman said at the annual meeting of the American Society of Pediatric Hematology/Oncology.
Laboratory findings for osteomyelitis in SCD are often nonspecific, including leukocytosis, elevated CRP and ESR, and blood cultures positive for Staphylococcus aureus (the predominant pathogen in children with osteomyelitis), or, in children with hemoglobinopathies, salmonella.
In children with SCD, CRP levels can vary from normal to elevated. ESR is similarly variable, as low hematocrit values can result in higher ESR values. Additionally, sickle erythrocytes can fail to aggregate, which can lead to lower ESR values.
A decade of data
The researchers set out to get a better handle on the characteristics and outcomes of osteomyelitis in patients with SCD and to see which laboratory and imaging findings might prove most useful for diagnosing osteomyelitis in this population. They reviewed data on 59 patients who were identified with indeterminate or likely osteomyelitis over a 10-year span. Of those, 30 were diagnosed and treated for osteomyelitis, and 29 were tentatively diagnosed but not treated. The latter group likely had symptoms caused by a bone infarction or vaso-occlusive crisis, Dr. Weisman said.
Among the 30 treated patients, osteomyelitis was confirmed by bone biopsy in 3, and an organism was isolated from blood or an abscess in 6. In the other 21, osteomyelitis was presumed based on clinical, laboratory, and MRI findings.
The median patient age was 12 years (range, 8 months to 18 years), 18 were male, and all but three patients have the HbSS genotype. Of the remaining patients, two had the HbSC and one the HbSF genotypes.
Infections occurred in the lower extremities in 11 patients, in the upper extremities in 10, in the pelvis or vertebrae in 2 each, and in the scapula, clavicle, hand, rib, or mandible in 1 patient each.
Just 13 of the 30 patients (43%) had lab findings of leukocytosis (more than 15,000 cells/mm2), and an equal number had elevated CRP (greater than 10 mg/L).
In contrast, 29 patients had an ESR above 20 mm/hour, and, in three of these patients, the rate was higher than 100 mm/hour.
When the researchers compared white blood cell counts and CRP levels between the treated patients and the 29 untreated controls, they found no significant differences for either measure of inflammation. In contrast, ESR was significantly higher among treated patients (P = .03).
Looking at the receiver operating characteristic curve for ESR, they found that an ESR of more than 100 mm/hour had 100% specificity for osteomyelitis in this group of patients.
Only 6 of the 30 (20%) had bacteremia. In 9 patients, nontyphoidal salmonella was isolated from cultures of either bone biopsy (3), abscess (3), or blood (6), but no possible causative organism could be isolated in the remaining 21 patients.
All patients were treated with prolonged antibiotic therapy. Surgical drainage and/or debridement were required in 6 patients. Two patients developed chronic osteomyelitis, but infection eventually resolved in all patients.
Recommendations
Dr. Weisman recommended early consultation with infectious disease experts and orthopedists; labs studies with complete blood counts, CRP, and ESR; and imaging studies with MRI when there is clinical suspicion of osteomyelitis in patients with SCD.
When an SCD patient has indeterminate findings, a blood culture can be performed. If it is positive for salmonella and the ESR is above 100 mm/hour, the patient can then go on to treatment. If the blood culture is negative and the ESR is below 100 mm hour but the suspicion of osteomyelitis remains high, a bone biopsy can be considered, they concluded.
The study was internally funded. Dr. Weisman reported no conflicts of interest to disclose.
MONTREAL – Osteomyelitis is an especially challenging diagnosis in children with sickle cell disease (SCD) because the bone and joint signs, elevated white cell counts, and C-reactive protein levels that are commonly used to diagnose bone infection are frequently features of SCD as well.
As a result, most patients with SCD and suspected osteomyelitis are treated without a confirmation of the diagnosis.
Among 30 patients with SCD who were followed at a single center over a decade, 29 patients had elevated ESR, but only 13 patients had leukocytosis, and only 13 had elevated CRP.
“Prior studies on sickle cell disease have shown that it is very difficult to differentiate between osteoarticular infection and bone infarction. Therefore, oftentimes, this diagnosis is very difficult to make,” Dr. Weisman said at the annual meeting of the American Society of Pediatric Hematology/Oncology.
Laboratory findings for osteomyelitis in SCD are often nonspecific, including leukocytosis, elevated CRP and ESR, and blood cultures positive for Staphylococcus aureus (the predominant pathogen in children with osteomyelitis), or, in children with hemoglobinopathies, salmonella.
In children with SCD, CRP levels can vary from normal to elevated. ESR is similarly variable, as low hematocrit values can result in higher ESR values. Additionally, sickle erythrocytes can fail to aggregate, which can lead to lower ESR values.
A decade of data
The researchers set out to get a better handle on the characteristics and outcomes of osteomyelitis in patients with SCD and to see which laboratory and imaging findings might prove most useful for diagnosing osteomyelitis in this population. They reviewed data on 59 patients who were identified with indeterminate or likely osteomyelitis over a 10-year span. Of those, 30 were diagnosed and treated for osteomyelitis, and 29 were tentatively diagnosed but not treated. The latter group likely had symptoms caused by a bone infarction or vaso-occlusive crisis, Dr. Weisman said.
Among the 30 treated patients, osteomyelitis was confirmed by bone biopsy in 3, and an organism was isolated from blood or an abscess in 6. In the other 21, osteomyelitis was presumed based on clinical, laboratory, and MRI findings.
The median patient age was 12 years (range, 8 months to 18 years), 18 were male, and all but three patients have the HbSS genotype. Of the remaining patients, two had the HbSC and one the HbSF genotypes.
Infections occurred in the lower extremities in 11 patients, in the upper extremities in 10, in the pelvis or vertebrae in 2 each, and in the scapula, clavicle, hand, rib, or mandible in 1 patient each.
Just 13 of the 30 patients (43%) had lab findings of leukocytosis (more than 15,000 cells/mm2), and an equal number had elevated CRP (greater than 10 mg/L).
In contrast, 29 patients had an ESR above 20 mm/hour, and, in three of these patients, the rate was higher than 100 mm/hour.
When the researchers compared white blood cell counts and CRP levels between the treated patients and the 29 untreated controls, they found no significant differences for either measure of inflammation. In contrast, ESR was significantly higher among treated patients (P = .03).
Looking at the receiver operating characteristic curve for ESR, they found that an ESR of more than 100 mm/hour had 100% specificity for osteomyelitis in this group of patients.
Only 6 of the 30 (20%) had bacteremia. In 9 patients, nontyphoidal salmonella was isolated from cultures of either bone biopsy (3), abscess (3), or blood (6), but no possible causative organism could be isolated in the remaining 21 patients.
All patients were treated with prolonged antibiotic therapy. Surgical drainage and/or debridement were required in 6 patients. Two patients developed chronic osteomyelitis, but infection eventually resolved in all patients.
Recommendations
Dr. Weisman recommended early consultation with infectious disease experts and orthopedists; labs studies with complete blood counts, CRP, and ESR; and imaging studies with MRI when there is clinical suspicion of osteomyelitis in patients with SCD.
When an SCD patient has indeterminate findings, a blood culture can be performed. If it is positive for salmonella and the ESR is above 100 mm/hour, the patient can then go on to treatment. If the blood culture is negative and the ESR is below 100 mm hour but the suspicion of osteomyelitis remains high, a bone biopsy can be considered, they concluded.
The study was internally funded. Dr. Weisman reported no conflicts of interest to disclose.
MONTREAL – Osteomyelitis is an especially challenging diagnosis in children with sickle cell disease (SCD) because the bone and joint signs, elevated white cell counts, and C-reactive protein levels that are commonly used to diagnose bone infection are frequently features of SCD as well.
As a result, most patients with SCD and suspected osteomyelitis are treated without a confirmation of the diagnosis.
Among 30 patients with SCD who were followed at a single center over a decade, 29 patients had elevated ESR, but only 13 patients had leukocytosis, and only 13 had elevated CRP.
“Prior studies on sickle cell disease have shown that it is very difficult to differentiate between osteoarticular infection and bone infarction. Therefore, oftentimes, this diagnosis is very difficult to make,” Dr. Weisman said at the annual meeting of the American Society of Pediatric Hematology/Oncology.
Laboratory findings for osteomyelitis in SCD are often nonspecific, including leukocytosis, elevated CRP and ESR, and blood cultures positive for Staphylococcus aureus (the predominant pathogen in children with osteomyelitis), or, in children with hemoglobinopathies, salmonella.
In children with SCD, CRP levels can vary from normal to elevated. ESR is similarly variable, as low hematocrit values can result in higher ESR values. Additionally, sickle erythrocytes can fail to aggregate, which can lead to lower ESR values.
A decade of data
The researchers set out to get a better handle on the characteristics and outcomes of osteomyelitis in patients with SCD and to see which laboratory and imaging findings might prove most useful for diagnosing osteomyelitis in this population. They reviewed data on 59 patients who were identified with indeterminate or likely osteomyelitis over a 10-year span. Of those, 30 were diagnosed and treated for osteomyelitis, and 29 were tentatively diagnosed but not treated. The latter group likely had symptoms caused by a bone infarction or vaso-occlusive crisis, Dr. Weisman said.
Among the 30 treated patients, osteomyelitis was confirmed by bone biopsy in 3, and an organism was isolated from blood or an abscess in 6. In the other 21, osteomyelitis was presumed based on clinical, laboratory, and MRI findings.
The median patient age was 12 years (range, 8 months to 18 years), 18 were male, and all but three patients have the HbSS genotype. Of the remaining patients, two had the HbSC and one the HbSF genotypes.
Infections occurred in the lower extremities in 11 patients, in the upper extremities in 10, in the pelvis or vertebrae in 2 each, and in the scapula, clavicle, hand, rib, or mandible in 1 patient each.
Just 13 of the 30 patients (43%) had lab findings of leukocytosis (more than 15,000 cells/mm2), and an equal number had elevated CRP (greater than 10 mg/L).
In contrast, 29 patients had an ESR above 20 mm/hour, and, in three of these patients, the rate was higher than 100 mm/hour.
When the researchers compared white blood cell counts and CRP levels between the treated patients and the 29 untreated controls, they found no significant differences for either measure of inflammation. In contrast, ESR was significantly higher among treated patients (P = .03).
Looking at the receiver operating characteristic curve for ESR, they found that an ESR of more than 100 mm/hour had 100% specificity for osteomyelitis in this group of patients.
Only 6 of the 30 (20%) had bacteremia. In 9 patients, nontyphoidal salmonella was isolated from cultures of either bone biopsy (3), abscess (3), or blood (6), but no possible causative organism could be isolated in the remaining 21 patients.
All patients were treated with prolonged antibiotic therapy. Surgical drainage and/or debridement were required in 6 patients. Two patients developed chronic osteomyelitis, but infection eventually resolved in all patients.
Recommendations
Dr. Weisman recommended early consultation with infectious disease experts and orthopedists; labs studies with complete blood counts, CRP, and ESR; and imaging studies with MRI when there is clinical suspicion of osteomyelitis in patients with SCD.
When an SCD patient has indeterminate findings, a blood culture can be performed. If it is positive for salmonella and the ESR is above 100 mm/hour, the patient can then go on to treatment. If the blood culture is negative and the ESR is below 100 mm hour but the suspicion of osteomyelitis remains high, a bone biopsy can be considered, they concluded.
The study was internally funded. Dr. Weisman reported no conflicts of interest to disclose.
Key clinical point: ESR may be a better lab marker for osteomyelitis in sickle cell disease than either WBC or CRP.
Major finding: An ESR greater than 100 mm/hr was 100% specific for osteomyelitis in this study.
Data source: A retrospective review of data on 59 patients with sickle cell disease and suspected or probable osteomyelitis.
Disclosures: The study was internally funded. Dr. Weisman reported having no conflicts of interest to disclose.