User login
Iowa Gambling Task differentiates bipolar patients from controls
A significant difference in oxygenated hemoglobin (oxy-Hb) rates was found between bipolar disorder patients and a control group during the Iowa Gambling Task, Dr. Yasuki Ono and associates reported.
While performing the Iowa Gambling Task (IGT), patients with bipolar disorder had significantly lower oxy-Hb levels in the bilateral orbitofrontal cortex and left prefrontal cortex than did those in the control group. Changes in oxy-Hb levels in the orbitofrontal cortex and profrontal cortex during the IGT were negatively correlated with total scores on the Hamilton Rating Scale for Depression. Oxy-Hb levels, however, were similar in both the bipolar disorder group and control group while taking a verbal fluency task.
“Although the IGT was useful for differentiating patients with [bipolar disorder] from control subjects, no significant differences in autonomic activity were observed,” noted Dr. Ono of the department of psychiatry and neurobiology at Kanazawa (Japan) University and associates.
Find the full study in Psychiatry Research: Neuroimaging (2015;233:1-8 [doi:10.1016/j.pscychresns.2015.04.003]).
A significant difference in oxygenated hemoglobin (oxy-Hb) rates was found between bipolar disorder patients and a control group during the Iowa Gambling Task, Dr. Yasuki Ono and associates reported.
While performing the Iowa Gambling Task (IGT), patients with bipolar disorder had significantly lower oxy-Hb levels in the bilateral orbitofrontal cortex and left prefrontal cortex than did those in the control group. Changes in oxy-Hb levels in the orbitofrontal cortex and profrontal cortex during the IGT were negatively correlated with total scores on the Hamilton Rating Scale for Depression. Oxy-Hb levels, however, were similar in both the bipolar disorder group and control group while taking a verbal fluency task.
“Although the IGT was useful for differentiating patients with [bipolar disorder] from control subjects, no significant differences in autonomic activity were observed,” noted Dr. Ono of the department of psychiatry and neurobiology at Kanazawa (Japan) University and associates.
Find the full study in Psychiatry Research: Neuroimaging (2015;233:1-8 [doi:10.1016/j.pscychresns.2015.04.003]).
A significant difference in oxygenated hemoglobin (oxy-Hb) rates was found between bipolar disorder patients and a control group during the Iowa Gambling Task, Dr. Yasuki Ono and associates reported.
While performing the Iowa Gambling Task (IGT), patients with bipolar disorder had significantly lower oxy-Hb levels in the bilateral orbitofrontal cortex and left prefrontal cortex than did those in the control group. Changes in oxy-Hb levels in the orbitofrontal cortex and profrontal cortex during the IGT were negatively correlated with total scores on the Hamilton Rating Scale for Depression. Oxy-Hb levels, however, were similar in both the bipolar disorder group and control group while taking a verbal fluency task.
“Although the IGT was useful for differentiating patients with [bipolar disorder] from control subjects, no significant differences in autonomic activity were observed,” noted Dr. Ono of the department of psychiatry and neurobiology at Kanazawa (Japan) University and associates.
Find the full study in Psychiatry Research: Neuroimaging (2015;233:1-8 [doi:10.1016/j.pscychresns.2015.04.003]).
ASCP: Brain imaging findings provide new guidance for neural outcomes research
MIAMI BEACH – Different brain regions appear to be responsible for processing emotional and cognitive stimuli during a common cognitive task used in psychiatric research, a new medical imaging study shows. Further, the activation of subcortical structures changed over time with repeated exposure to the task. The work has implications for researchers and clinicians involved with identifying new targets to treat mood disorders.
Functional magnetic resonance imaging (fMRI) gives detailed anatomic and physiologic data about the brain and has increasing importance for neural outcomes research, according to David Fleck, Ph.D., research associate professor with the Center for Imaging Research at the University of Cincinnati. His work, presented in a poster session, built on previous imaging research that showed differential activation of brain structures when emotional distraction interrupts a cognitive task.
Imaging offers investigators a “completely objective” measure of changes in brain function, and thus is an important tool in clinical trials for medications and treatments for mood disorders, Dr. Fleck said at a meeting of the American Society of Clinical Psychopharmacology, formerly known as the New Clinical Drug Evaluation Unit meeting. He noted that there can be variability in clinician assessments, and patients can both under- and overreport symptoms. Neuroimaging provides a means to measure absolute change in brain activity or structure, or both, over time.
Forty-one healthy subjects were recruited for the study, which obtained baseline, 1 week, and 8 week fMRI brain scans. During the scans, participants completed the Continuous Performance Task with Emotional and Neutral Distractor (CPT-END). This is a “visual oddball” task where participants are asked to differentiate a target – an image of a circle – from images of a square, and also from distracting images. Seventy percent of the time, subjects were shown a square. They saw the target circle 10% of the time and were presented either a neutral or an emotionally laden image, at a 10% rate for each image type, the remainder of the time.
Dr. Fleck and his colleagues at the University of Cincinnati identified the amygdala and the interior prefrontal gyrus as areas that showed more activation with both the neutral and the emotional distractors at baseline than with either the target circle or the square. However, at weeks 1 and 8, the emotional distractors elicited significantly more activation, particularly in the inferior frontal gyrus.
Deeper brain structures also showed differences between attentional and emotional stimuli, and activation changed over time: “Finally, targets elicited more caudate activation at baseline but not week 8 relative to both distractor types, while emotional distractors elicited more thalamic activation at week 8 but not baseline relative to neutrals and targets,” said Dr. Fleck and coinvestigators.
The study partly replicated and extended a study done more than a decade ago that looked at differential brain activation in cognitive attention versus emotional processes. This is important in mood disorder research, Dr. Fleck said in an interview. Bipolar disorder, for example, has significant cognitive and emotional components that contribute to the disease process. “It is hoped that this work will form the basis for a cognitive/emotional fMRI probe of pharmacological targets in mood disorders,” said Dr. Fleck and coinvestigators.
Dr. Fleck noted that advances in imaging technology since 2002 mean that the image analysis in this study could be much more fine-tuned in its identification of regions of interest, saying, “These findings will form the basis for further work characterizing the neurofunctional signature of mood-disordered patients over time.”
Dr. Fleck reported no conflicts of interest.
On Twitter @karioakes
MIAMI BEACH – Different brain regions appear to be responsible for processing emotional and cognitive stimuli during a common cognitive task used in psychiatric research, a new medical imaging study shows. Further, the activation of subcortical structures changed over time with repeated exposure to the task. The work has implications for researchers and clinicians involved with identifying new targets to treat mood disorders.
Functional magnetic resonance imaging (fMRI) gives detailed anatomic and physiologic data about the brain and has increasing importance for neural outcomes research, according to David Fleck, Ph.D., research associate professor with the Center for Imaging Research at the University of Cincinnati. His work, presented in a poster session, built on previous imaging research that showed differential activation of brain structures when emotional distraction interrupts a cognitive task.
Imaging offers investigators a “completely objective” measure of changes in brain function, and thus is an important tool in clinical trials for medications and treatments for mood disorders, Dr. Fleck said at a meeting of the American Society of Clinical Psychopharmacology, formerly known as the New Clinical Drug Evaluation Unit meeting. He noted that there can be variability in clinician assessments, and patients can both under- and overreport symptoms. Neuroimaging provides a means to measure absolute change in brain activity or structure, or both, over time.
Forty-one healthy subjects were recruited for the study, which obtained baseline, 1 week, and 8 week fMRI brain scans. During the scans, participants completed the Continuous Performance Task with Emotional and Neutral Distractor (CPT-END). This is a “visual oddball” task where participants are asked to differentiate a target – an image of a circle – from images of a square, and also from distracting images. Seventy percent of the time, subjects were shown a square. They saw the target circle 10% of the time and were presented either a neutral or an emotionally laden image, at a 10% rate for each image type, the remainder of the time.
Dr. Fleck and his colleagues at the University of Cincinnati identified the amygdala and the interior prefrontal gyrus as areas that showed more activation with both the neutral and the emotional distractors at baseline than with either the target circle or the square. However, at weeks 1 and 8, the emotional distractors elicited significantly more activation, particularly in the inferior frontal gyrus.
Deeper brain structures also showed differences between attentional and emotional stimuli, and activation changed over time: “Finally, targets elicited more caudate activation at baseline but not week 8 relative to both distractor types, while emotional distractors elicited more thalamic activation at week 8 but not baseline relative to neutrals and targets,” said Dr. Fleck and coinvestigators.
The study partly replicated and extended a study done more than a decade ago that looked at differential brain activation in cognitive attention versus emotional processes. This is important in mood disorder research, Dr. Fleck said in an interview. Bipolar disorder, for example, has significant cognitive and emotional components that contribute to the disease process. “It is hoped that this work will form the basis for a cognitive/emotional fMRI probe of pharmacological targets in mood disorders,” said Dr. Fleck and coinvestigators.
Dr. Fleck noted that advances in imaging technology since 2002 mean that the image analysis in this study could be much more fine-tuned in its identification of regions of interest, saying, “These findings will form the basis for further work characterizing the neurofunctional signature of mood-disordered patients over time.”
Dr. Fleck reported no conflicts of interest.
On Twitter @karioakes
MIAMI BEACH – Different brain regions appear to be responsible for processing emotional and cognitive stimuli during a common cognitive task used in psychiatric research, a new medical imaging study shows. Further, the activation of subcortical structures changed over time with repeated exposure to the task. The work has implications for researchers and clinicians involved with identifying new targets to treat mood disorders.
Functional magnetic resonance imaging (fMRI) gives detailed anatomic and physiologic data about the brain and has increasing importance for neural outcomes research, according to David Fleck, Ph.D., research associate professor with the Center for Imaging Research at the University of Cincinnati. His work, presented in a poster session, built on previous imaging research that showed differential activation of brain structures when emotional distraction interrupts a cognitive task.
Imaging offers investigators a “completely objective” measure of changes in brain function, and thus is an important tool in clinical trials for medications and treatments for mood disorders, Dr. Fleck said at a meeting of the American Society of Clinical Psychopharmacology, formerly known as the New Clinical Drug Evaluation Unit meeting. He noted that there can be variability in clinician assessments, and patients can both under- and overreport symptoms. Neuroimaging provides a means to measure absolute change in brain activity or structure, or both, over time.
Forty-one healthy subjects were recruited for the study, which obtained baseline, 1 week, and 8 week fMRI brain scans. During the scans, participants completed the Continuous Performance Task with Emotional and Neutral Distractor (CPT-END). This is a “visual oddball” task where participants are asked to differentiate a target – an image of a circle – from images of a square, and also from distracting images. Seventy percent of the time, subjects were shown a square. They saw the target circle 10% of the time and were presented either a neutral or an emotionally laden image, at a 10% rate for each image type, the remainder of the time.
Dr. Fleck and his colleagues at the University of Cincinnati identified the amygdala and the interior prefrontal gyrus as areas that showed more activation with both the neutral and the emotional distractors at baseline than with either the target circle or the square. However, at weeks 1 and 8, the emotional distractors elicited significantly more activation, particularly in the inferior frontal gyrus.
Deeper brain structures also showed differences between attentional and emotional stimuli, and activation changed over time: “Finally, targets elicited more caudate activation at baseline but not week 8 relative to both distractor types, while emotional distractors elicited more thalamic activation at week 8 but not baseline relative to neutrals and targets,” said Dr. Fleck and coinvestigators.
The study partly replicated and extended a study done more than a decade ago that looked at differential brain activation in cognitive attention versus emotional processes. This is important in mood disorder research, Dr. Fleck said in an interview. Bipolar disorder, for example, has significant cognitive and emotional components that contribute to the disease process. “It is hoped that this work will form the basis for a cognitive/emotional fMRI probe of pharmacological targets in mood disorders,” said Dr. Fleck and coinvestigators.
Dr. Fleck noted that advances in imaging technology since 2002 mean that the image analysis in this study could be much more fine-tuned in its identification of regions of interest, saying, “These findings will form the basis for further work characterizing the neurofunctional signature of mood-disordered patients over time.”
Dr. Fleck reported no conflicts of interest.
On Twitter @karioakes
AT THE ASCP ANNUAL MEETING
Key clinical point: Emotional disruptors to a cognitive attention task activated different brain regions, and emotional activation increased with time.
Major finding: The amygdala and the inferior prefrontal gyrus showed more activation over time with exposure to emotional stimuli during a cognitive attention task.
Data source: fMRI study of 41 healthy subjects given a cognitive/emotional task at baseline, 1, and 8 weeks.
Disclosures: Dr. Fleck reported no relevant financial disclosures.
Avoiding common drug−drug interactions
Mr. T, age 23, was given a diagnosis of bipolar disorder 1 year ago. After he experienced inadequate symptom relief with valproate, you switched him to extended-release lithium, 1,200 mg/d. Mr. T reported improved mood and stability with this medication adjustment. These positive changes led him to resume activities he enjoyed before onset of bipolar disorder, such as running, reading, and going out to dinner with friends.
Now, Mr. T’s mother calls your office to express concern about her son’s slight
hand tremor, which appeared after 2 days of gastrointestinal distress. She tells you that Mr. T sprained his ankle while running 1 week ago and has been taking over-the-counter ibuprofen for pain relief, which he did often in the past.
You suspect that Mr. T is experiencing lithium toxicity as a result of ibuprofen use.
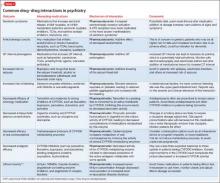
Although mental health providers can easily recognize the drug−drug interaction between lithium and nonsteroidal anti-inflammatory drugs (NSAIDs) that Mr. T experienced, interpreting the safety of a medication regimen with respect to drug− drug interactions before prescribing often is more daunting. This article reviews the basics of drug−drug interactions, while briefly highlighting common examples in psychiatric medicine (Table 11-5). We also provide an outline of additional points to consider when reviewing your patients’ medication regimens and encountering unfamiliar drug−drug interactions.
Types of drug−drug interactions
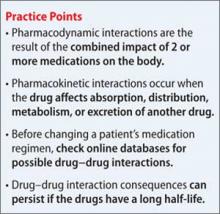
Drug−drug interactions fall into 2 categories: pharmacodynamic (PD) and pharmacokinetic (PK):
• PD interactions are a result of the combined impact of medications on the body when there is no direct effect on absorption, distribution, metabolism, or excretion characteristics, such as 2 medications that act at the same receptor or lead to similar or opposing pharmacologic effects.
• PK interactions occur when a drug affects the absorption, distribution, metabolism, or excretion characteristics of another drug.
Although it is possible that drug−drug interactions will have no clinical effect, when the impact of a PD or PK drug−drug interaction is evident, it likely is the result of additive, synergistic, or antagonistic consequences on the medications’ intended impact or side-effect profile.
Pharmacodynamic interactions
Serotonin syndrome. The potential for serotonin syndrome occurs when medications that increase synaptic serotonin concentration are used concomitantly.1 This can occur through several mechanisms, including increased serotonin release, decreased reuptake, or decreased serotonin metabolism. A high serotonin concentration in the CNS and in the periphery overstimulates serotonin receptors, leading to signs and symptoms that can include diarrhea, fever, delirium, coma, and potentially death.
QT prolongation and anticholinergic toxicity are further examples of additive PD drug−drug interactions. Anticholinergic toxicity is possible when multiple medications contribute to inhibition of the neuro-transmitter acetylcholine at muscarinic receptors. This leads to adverse effects such as dry mouth, constipation, confusion, and urinary retention.
QT prolongation, which can lead to arrhythmia, occurs when a patient is taking several medications that can increase the QT interval. Consider close monitoring and using alternative agents with less potential to increase the QT interval in patients at risk of arrhythmias (geriatric patients, those with an increased QT interval at baseline, etc.).
Decreased seizure threshold. The increased risk of seizures with bupropion and other medications that lower the seizure threshold is another example of an additive PD drug interaction. Bupropion can increase the risk of seizures in a dose-dependent manner, which increases when bupropion is taken with other drugs that lower the seizure threshold.6 Seizure risk associated with alcohol or benzodiazepine withdrawal also may increase the risk for this interaction.
Of note, the increased risk of seizures with the combination of bupropion and alcohol in the absence of withdrawal is not well studied in humans, but positive correlation has been seen in an animal study.6
Decreased platelet function. Another example of a PD drug−drug interaction is increased risk of bleeding when a selective serotonin reuptake inhibitor is used with a NSAID or oral anticoagulant. The proposed mechanism for this interaction is that blocking serotonin reuptake on platelets leads to decreased platelet function and an increased risk for prolonged bleeding.7 This is somewhat controversial because, first, it has been noted that drugs with the highest degree of serotonin reuptake inhibition do not always cause the highest risk of bleeding and, second, most of the evidence for this interaction is from observational studies.7
This potential interaction could be most important for patients who need an antidepressant, are on chronic NSAID or anticoagulant therapy, and are at high risk of bleeding.
Pharmacokinetic interactions
PK interactions in psychiatry often are caused by interference of drug metabolizing enzymes. The cytochrome P450 (CYP450) family of metabolizing enzymes in particular is important to the breakdown of medications in the body. Many drug−drug interactions involve medications that can inhibit or induce metabolism of other drugs through their effect on the CYP450 system.
Inhibition interactions. When a drug’s metabolism is inhibited, the result is usually increased serum concentration of that medication (because of less breakdown) and a more potent impact on the primary mechanism of action or adverse effects. Sometimes, inhibiting metabolism can lead to decreased clinical effect. Tamoxifen (an oral agent used to treat breast cancer) and certain analgesics when used in combination with moderate or strong inhibitors of the CYP2D6 subfamily of CYP450 metabolizing enzymes are 2 examples of metabolism inhibition leading to decreased efficacy.8 Both tamoxifen and the analgesics listed in Table 11-5 are prodrugs; that is, they must be metabolized to be active. When the enzymes that metabolize these drugs into their active form are inhibited, the concentration of active drug decreases.
Induction interactions. Alternatively, there is an increased rate of drug breakdown and resulting decrease in effect when drugs that induce the activity of metabolizing enzymes are used with medications that are substrates of the same enzyme. Carbamazepine is commonly involved in this type of drug interaction because it is a strong inducer of CYP 1A2, 2B6, 2C19, 2C9, and 3A4, and the p-glycoprotein drug efflux pump.9 As a result of this rampant induction, carbamazepine can decrease the serum concentration of oral contraceptives below a reliably effective level. Therefore, it is recommended that women of childbearing potential use other contraceptive methods, such as a progestin implant or an intrauterine device.10
In addition, the polycyclic aromatic hydrocarbons found in cigarettes induce activity of CYP1A2. Patients who smoke and use medications metabolized by this enzyme, such as clozapine and olanzapine, may need a higher dosage.
Drug elimination interactions
The last drug−drug interaction discussed here returns the discussion to Mr. T and involves drug elimination.2 The NSAIDs Mr. T was using for pain likely caused decreased renal excretion of lithium. Because lithium is primarily excreted through the kidneys, Mr. T’s NSAID use, possibly in combination with dehydration caused by gastrointestinal distress, resulted in lithium toxicity. This class of analgesics should be avoided or used cautiously in patients taking lithium.
Clinical applications
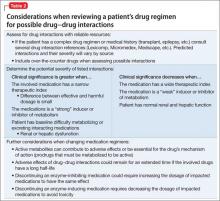
The relatively common drug−drug interactions discussed here are just a fraction of the potential interactions mental health practitioners see on a daily basis. Understanding the basics of PD and PK interactions in the setting of patient-specific factors can help to clarify the information found in drug−drug interaction databases, such as Micromedex, Lexicomp, Facts and Comparisons, and Epocrates. Table 2 lists additional insights into drug interactions.
Related Resources
• CredibleMeds. Online resource on QT prolonging drugs. http://crediblemeds.org.
• Madhusoodanan S, Velama U, Parmar J, et al. A current review of cytochrome P450 interactions of psychotropic drugs. Ann Clin Psychiatry. 2014;26(2):120-138.
Drug Brand Names
Benztropine • Cogentin Olanzapine • Zyprexa
Bupropion • Wellbutrin Oxycodone • Oxycontin
Carbamazepine • Tegretol Paroxetine • Paxil
Clozapine • Clozaril Quetiapine • Seroquel
Diphenhydramine • Benadryl Sertraline • Zoloft
Duloxetine • Cymbalta Tamoxifen • Soltamox
Fluoxetine • Prozac Trazodone • Desyrel
Lithium • Eskalith, Lithobid Valproate • Divalproex
Haloperidol • Haldol Ziprasidone • Geodon
Hydrocodone • Vicodin
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Buckley NA, Dawson AH, Isbister GK. Serotonin syndrome. BMJ. 2014;348:g1626. doi: 10.1136/bmj.g1626.
2. Eskalith [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2003.
3. Handler J. Lithium and antihypertensive medication: a potentially dangerous interaction. J Clin Hypertens (Greenwich). 2009;11(12):738-742.
4. Blanche P, Raynaud E, Kerob D, et al. Lithium intoxication in an elderly patient after combined treatment with losartan. Eur J Clin Pharmacol. 1997;52(6):501.
5. Atacand [package insert]. Wilmington, DE: AstraZeneca LP; 2013.
6. Silverstone PH, Williams R, McMahon L, et al. Alcohol significantly lowers the seizure threshold in mice when co-administered with bupropion hydrochloride. Ann Gen Psychiatry. 2008;7:11.
7. Spina E, Trifirò G, Caraci F. Clinically significant drug interactions with newer antidepressants. CNS Drugs. 2012;26(1):39-67.
8. Ereshefsky L, Sloan DM. Drug-drug interactions with the use of psychotropic medications. CNS Spectr. 2009;14(suppl Q and A forum 8):1-8.
9. Carbamazepine. Drug facts and comparisons database. St. Louis, MO: Wolters Kluwer Health Inc; November 2014.
10. Pennell PB. Pregnancy, epilepsy, and women’s issues. Continuum (Minneap Minn). 2013;19(3 Epilepsy):697-714.
Mr. T, age 23, was given a diagnosis of bipolar disorder 1 year ago. After he experienced inadequate symptom relief with valproate, you switched him to extended-release lithium, 1,200 mg/d. Mr. T reported improved mood and stability with this medication adjustment. These positive changes led him to resume activities he enjoyed before onset of bipolar disorder, such as running, reading, and going out to dinner with friends.
Now, Mr. T’s mother calls your office to express concern about her son’s slight
hand tremor, which appeared after 2 days of gastrointestinal distress. She tells you that Mr. T sprained his ankle while running 1 week ago and has been taking over-the-counter ibuprofen for pain relief, which he did often in the past.
You suspect that Mr. T is experiencing lithium toxicity as a result of ibuprofen use.
Although mental health providers can easily recognize the drug−drug interaction between lithium and nonsteroidal anti-inflammatory drugs (NSAIDs) that Mr. T experienced, interpreting the safety of a medication regimen with respect to drug− drug interactions before prescribing often is more daunting. This article reviews the basics of drug−drug interactions, while briefly highlighting common examples in psychiatric medicine (Table 11-5). We also provide an outline of additional points to consider when reviewing your patients’ medication regimens and encountering unfamiliar drug−drug interactions.
Types of drug−drug interactions
Drug−drug interactions fall into 2 categories: pharmacodynamic (PD) and pharmacokinetic (PK):
• PD interactions are a result of the combined impact of medications on the body when there is no direct effect on absorption, distribution, metabolism, or excretion characteristics, such as 2 medications that act at the same receptor or lead to similar or opposing pharmacologic effects.
• PK interactions occur when a drug affects the absorption, distribution, metabolism, or excretion characteristics of another drug.
Although it is possible that drug−drug interactions will have no clinical effect, when the impact of a PD or PK drug−drug interaction is evident, it likely is the result of additive, synergistic, or antagonistic consequences on the medications’ intended impact or side-effect profile.
Pharmacodynamic interactions
Serotonin syndrome. The potential for serotonin syndrome occurs when medications that increase synaptic serotonin concentration are used concomitantly.1 This can occur through several mechanisms, including increased serotonin release, decreased reuptake, or decreased serotonin metabolism. A high serotonin concentration in the CNS and in the periphery overstimulates serotonin receptors, leading to signs and symptoms that can include diarrhea, fever, delirium, coma, and potentially death.
QT prolongation and anticholinergic toxicity are further examples of additive PD drug−drug interactions. Anticholinergic toxicity is possible when multiple medications contribute to inhibition of the neuro-transmitter acetylcholine at muscarinic receptors. This leads to adverse effects such as dry mouth, constipation, confusion, and urinary retention.
QT prolongation, which can lead to arrhythmia, occurs when a patient is taking several medications that can increase the QT interval. Consider close monitoring and using alternative agents with less potential to increase the QT interval in patients at risk of arrhythmias (geriatric patients, those with an increased QT interval at baseline, etc.).
Decreased seizure threshold. The increased risk of seizures with bupropion and other medications that lower the seizure threshold is another example of an additive PD drug interaction. Bupropion can increase the risk of seizures in a dose-dependent manner, which increases when bupropion is taken with other drugs that lower the seizure threshold.6 Seizure risk associated with alcohol or benzodiazepine withdrawal also may increase the risk for this interaction.
Of note, the increased risk of seizures with the combination of bupropion and alcohol in the absence of withdrawal is not well studied in humans, but positive correlation has been seen in an animal study.6
Decreased platelet function. Another example of a PD drug−drug interaction is increased risk of bleeding when a selective serotonin reuptake inhibitor is used with a NSAID or oral anticoagulant. The proposed mechanism for this interaction is that blocking serotonin reuptake on platelets leads to decreased platelet function and an increased risk for prolonged bleeding.7 This is somewhat controversial because, first, it has been noted that drugs with the highest degree of serotonin reuptake inhibition do not always cause the highest risk of bleeding and, second, most of the evidence for this interaction is from observational studies.7
This potential interaction could be most important for patients who need an antidepressant, are on chronic NSAID or anticoagulant therapy, and are at high risk of bleeding.
Pharmacokinetic interactions
PK interactions in psychiatry often are caused by interference of drug metabolizing enzymes. The cytochrome P450 (CYP450) family of metabolizing enzymes in particular is important to the breakdown of medications in the body. Many drug−drug interactions involve medications that can inhibit or induce metabolism of other drugs through their effect on the CYP450 system.
Inhibition interactions. When a drug’s metabolism is inhibited, the result is usually increased serum concentration of that medication (because of less breakdown) and a more potent impact on the primary mechanism of action or adverse effects. Sometimes, inhibiting metabolism can lead to decreased clinical effect. Tamoxifen (an oral agent used to treat breast cancer) and certain analgesics when used in combination with moderate or strong inhibitors of the CYP2D6 subfamily of CYP450 metabolizing enzymes are 2 examples of metabolism inhibition leading to decreased efficacy.8 Both tamoxifen and the analgesics listed in Table 11-5 are prodrugs; that is, they must be metabolized to be active. When the enzymes that metabolize these drugs into their active form are inhibited, the concentration of active drug decreases.
Induction interactions. Alternatively, there is an increased rate of drug breakdown and resulting decrease in effect when drugs that induce the activity of metabolizing enzymes are used with medications that are substrates of the same enzyme. Carbamazepine is commonly involved in this type of drug interaction because it is a strong inducer of CYP 1A2, 2B6, 2C19, 2C9, and 3A4, and the p-glycoprotein drug efflux pump.9 As a result of this rampant induction, carbamazepine can decrease the serum concentration of oral contraceptives below a reliably effective level. Therefore, it is recommended that women of childbearing potential use other contraceptive methods, such as a progestin implant or an intrauterine device.10
In addition, the polycyclic aromatic hydrocarbons found in cigarettes induce activity of CYP1A2. Patients who smoke and use medications metabolized by this enzyme, such as clozapine and olanzapine, may need a higher dosage.
Drug elimination interactions
The last drug−drug interaction discussed here returns the discussion to Mr. T and involves drug elimination.2 The NSAIDs Mr. T was using for pain likely caused decreased renal excretion of lithium. Because lithium is primarily excreted through the kidneys, Mr. T’s NSAID use, possibly in combination with dehydration caused by gastrointestinal distress, resulted in lithium toxicity. This class of analgesics should be avoided or used cautiously in patients taking lithium.
Clinical applications
The relatively common drug−drug interactions discussed here are just a fraction of the potential interactions mental health practitioners see on a daily basis. Understanding the basics of PD and PK interactions in the setting of patient-specific factors can help to clarify the information found in drug−drug interaction databases, such as Micromedex, Lexicomp, Facts and Comparisons, and Epocrates. Table 2 lists additional insights into drug interactions.
Related Resources
• CredibleMeds. Online resource on QT prolonging drugs. http://crediblemeds.org.
• Madhusoodanan S, Velama U, Parmar J, et al. A current review of cytochrome P450 interactions of psychotropic drugs. Ann Clin Psychiatry. 2014;26(2):120-138.
Drug Brand Names
Benztropine • Cogentin Olanzapine • Zyprexa
Bupropion • Wellbutrin Oxycodone • Oxycontin
Carbamazepine • Tegretol Paroxetine • Paxil
Clozapine • Clozaril Quetiapine • Seroquel
Diphenhydramine • Benadryl Sertraline • Zoloft
Duloxetine • Cymbalta Tamoxifen • Soltamox
Fluoxetine • Prozac Trazodone • Desyrel
Lithium • Eskalith, Lithobid Valproate • Divalproex
Haloperidol • Haldol Ziprasidone • Geodon
Hydrocodone • Vicodin
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Mr. T, age 23, was given a diagnosis of bipolar disorder 1 year ago. After he experienced inadequate symptom relief with valproate, you switched him to extended-release lithium, 1,200 mg/d. Mr. T reported improved mood and stability with this medication adjustment. These positive changes led him to resume activities he enjoyed before onset of bipolar disorder, such as running, reading, and going out to dinner with friends.
Now, Mr. T’s mother calls your office to express concern about her son’s slight
hand tremor, which appeared after 2 days of gastrointestinal distress. She tells you that Mr. T sprained his ankle while running 1 week ago and has been taking over-the-counter ibuprofen for pain relief, which he did often in the past.
You suspect that Mr. T is experiencing lithium toxicity as a result of ibuprofen use.
Although mental health providers can easily recognize the drug−drug interaction between lithium and nonsteroidal anti-inflammatory drugs (NSAIDs) that Mr. T experienced, interpreting the safety of a medication regimen with respect to drug− drug interactions before prescribing often is more daunting. This article reviews the basics of drug−drug interactions, while briefly highlighting common examples in psychiatric medicine (Table 11-5). We also provide an outline of additional points to consider when reviewing your patients’ medication regimens and encountering unfamiliar drug−drug interactions.
Types of drug−drug interactions
Drug−drug interactions fall into 2 categories: pharmacodynamic (PD) and pharmacokinetic (PK):
• PD interactions are a result of the combined impact of medications on the body when there is no direct effect on absorption, distribution, metabolism, or excretion characteristics, such as 2 medications that act at the same receptor or lead to similar or opposing pharmacologic effects.
• PK interactions occur when a drug affects the absorption, distribution, metabolism, or excretion characteristics of another drug.
Although it is possible that drug−drug interactions will have no clinical effect, when the impact of a PD or PK drug−drug interaction is evident, it likely is the result of additive, synergistic, or antagonistic consequences on the medications’ intended impact or side-effect profile.
Pharmacodynamic interactions
Serotonin syndrome. The potential for serotonin syndrome occurs when medications that increase synaptic serotonin concentration are used concomitantly.1 This can occur through several mechanisms, including increased serotonin release, decreased reuptake, or decreased serotonin metabolism. A high serotonin concentration in the CNS and in the periphery overstimulates serotonin receptors, leading to signs and symptoms that can include diarrhea, fever, delirium, coma, and potentially death.
QT prolongation and anticholinergic toxicity are further examples of additive PD drug−drug interactions. Anticholinergic toxicity is possible when multiple medications contribute to inhibition of the neuro-transmitter acetylcholine at muscarinic receptors. This leads to adverse effects such as dry mouth, constipation, confusion, and urinary retention.
QT prolongation, which can lead to arrhythmia, occurs when a patient is taking several medications that can increase the QT interval. Consider close monitoring and using alternative agents with less potential to increase the QT interval in patients at risk of arrhythmias (geriatric patients, those with an increased QT interval at baseline, etc.).
Decreased seizure threshold. The increased risk of seizures with bupropion and other medications that lower the seizure threshold is another example of an additive PD drug interaction. Bupropion can increase the risk of seizures in a dose-dependent manner, which increases when bupropion is taken with other drugs that lower the seizure threshold.6 Seizure risk associated with alcohol or benzodiazepine withdrawal also may increase the risk for this interaction.
Of note, the increased risk of seizures with the combination of bupropion and alcohol in the absence of withdrawal is not well studied in humans, but positive correlation has been seen in an animal study.6
Decreased platelet function. Another example of a PD drug−drug interaction is increased risk of bleeding when a selective serotonin reuptake inhibitor is used with a NSAID or oral anticoagulant. The proposed mechanism for this interaction is that blocking serotonin reuptake on platelets leads to decreased platelet function and an increased risk for prolonged bleeding.7 This is somewhat controversial because, first, it has been noted that drugs with the highest degree of serotonin reuptake inhibition do not always cause the highest risk of bleeding and, second, most of the evidence for this interaction is from observational studies.7
This potential interaction could be most important for patients who need an antidepressant, are on chronic NSAID or anticoagulant therapy, and are at high risk of bleeding.
Pharmacokinetic interactions
PK interactions in psychiatry often are caused by interference of drug metabolizing enzymes. The cytochrome P450 (CYP450) family of metabolizing enzymes in particular is important to the breakdown of medications in the body. Many drug−drug interactions involve medications that can inhibit or induce metabolism of other drugs through their effect on the CYP450 system.
Inhibition interactions. When a drug’s metabolism is inhibited, the result is usually increased serum concentration of that medication (because of less breakdown) and a more potent impact on the primary mechanism of action or adverse effects. Sometimes, inhibiting metabolism can lead to decreased clinical effect. Tamoxifen (an oral agent used to treat breast cancer) and certain analgesics when used in combination with moderate or strong inhibitors of the CYP2D6 subfamily of CYP450 metabolizing enzymes are 2 examples of metabolism inhibition leading to decreased efficacy.8 Both tamoxifen and the analgesics listed in Table 11-5 are prodrugs; that is, they must be metabolized to be active. When the enzymes that metabolize these drugs into their active form are inhibited, the concentration of active drug decreases.
Induction interactions. Alternatively, there is an increased rate of drug breakdown and resulting decrease in effect when drugs that induce the activity of metabolizing enzymes are used with medications that are substrates of the same enzyme. Carbamazepine is commonly involved in this type of drug interaction because it is a strong inducer of CYP 1A2, 2B6, 2C19, 2C9, and 3A4, and the p-glycoprotein drug efflux pump.9 As a result of this rampant induction, carbamazepine can decrease the serum concentration of oral contraceptives below a reliably effective level. Therefore, it is recommended that women of childbearing potential use other contraceptive methods, such as a progestin implant or an intrauterine device.10
In addition, the polycyclic aromatic hydrocarbons found in cigarettes induce activity of CYP1A2. Patients who smoke and use medications metabolized by this enzyme, such as clozapine and olanzapine, may need a higher dosage.
Drug elimination interactions
The last drug−drug interaction discussed here returns the discussion to Mr. T and involves drug elimination.2 The NSAIDs Mr. T was using for pain likely caused decreased renal excretion of lithium. Because lithium is primarily excreted through the kidneys, Mr. T’s NSAID use, possibly in combination with dehydration caused by gastrointestinal distress, resulted in lithium toxicity. This class of analgesics should be avoided or used cautiously in patients taking lithium.
Clinical applications
The relatively common drug−drug interactions discussed here are just a fraction of the potential interactions mental health practitioners see on a daily basis. Understanding the basics of PD and PK interactions in the setting of patient-specific factors can help to clarify the information found in drug−drug interaction databases, such as Micromedex, Lexicomp, Facts and Comparisons, and Epocrates. Table 2 lists additional insights into drug interactions.
Related Resources
• CredibleMeds. Online resource on QT prolonging drugs. http://crediblemeds.org.
• Madhusoodanan S, Velama U, Parmar J, et al. A current review of cytochrome P450 interactions of psychotropic drugs. Ann Clin Psychiatry. 2014;26(2):120-138.
Drug Brand Names
Benztropine • Cogentin Olanzapine • Zyprexa
Bupropion • Wellbutrin Oxycodone • Oxycontin
Carbamazepine • Tegretol Paroxetine • Paxil
Clozapine • Clozaril Quetiapine • Seroquel
Diphenhydramine • Benadryl Sertraline • Zoloft
Duloxetine • Cymbalta Tamoxifen • Soltamox
Fluoxetine • Prozac Trazodone • Desyrel
Lithium • Eskalith, Lithobid Valproate • Divalproex
Haloperidol • Haldol Ziprasidone • Geodon
Hydrocodone • Vicodin
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Buckley NA, Dawson AH, Isbister GK. Serotonin syndrome. BMJ. 2014;348:g1626. doi: 10.1136/bmj.g1626.
2. Eskalith [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2003.
3. Handler J. Lithium and antihypertensive medication: a potentially dangerous interaction. J Clin Hypertens (Greenwich). 2009;11(12):738-742.
4. Blanche P, Raynaud E, Kerob D, et al. Lithium intoxication in an elderly patient after combined treatment with losartan. Eur J Clin Pharmacol. 1997;52(6):501.
5. Atacand [package insert]. Wilmington, DE: AstraZeneca LP; 2013.
6. Silverstone PH, Williams R, McMahon L, et al. Alcohol significantly lowers the seizure threshold in mice when co-administered with bupropion hydrochloride. Ann Gen Psychiatry. 2008;7:11.
7. Spina E, Trifirò G, Caraci F. Clinically significant drug interactions with newer antidepressants. CNS Drugs. 2012;26(1):39-67.
8. Ereshefsky L, Sloan DM. Drug-drug interactions with the use of psychotropic medications. CNS Spectr. 2009;14(suppl Q and A forum 8):1-8.
9. Carbamazepine. Drug facts and comparisons database. St. Louis, MO: Wolters Kluwer Health Inc; November 2014.
10. Pennell PB. Pregnancy, epilepsy, and women’s issues. Continuum (Minneap Minn). 2013;19(3 Epilepsy):697-714.
1. Buckley NA, Dawson AH, Isbister GK. Serotonin syndrome. BMJ. 2014;348:g1626. doi: 10.1136/bmj.g1626.
2. Eskalith [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2003.
3. Handler J. Lithium and antihypertensive medication: a potentially dangerous interaction. J Clin Hypertens (Greenwich). 2009;11(12):738-742.
4. Blanche P, Raynaud E, Kerob D, et al. Lithium intoxication in an elderly patient after combined treatment with losartan. Eur J Clin Pharmacol. 1997;52(6):501.
5. Atacand [package insert]. Wilmington, DE: AstraZeneca LP; 2013.
6. Silverstone PH, Williams R, McMahon L, et al. Alcohol significantly lowers the seizure threshold in mice when co-administered with bupropion hydrochloride. Ann Gen Psychiatry. 2008;7:11.
7. Spina E, Trifirò G, Caraci F. Clinically significant drug interactions with newer antidepressants. CNS Drugs. 2012;26(1):39-67.
8. Ereshefsky L, Sloan DM. Drug-drug interactions with the use of psychotropic medications. CNS Spectr. 2009;14(suppl Q and A forum 8):1-8.
9. Carbamazepine. Drug facts and comparisons database. St. Louis, MO: Wolters Kluwer Health Inc; November 2014.
10. Pennell PB. Pregnancy, epilepsy, and women’s issues. Continuum (Minneap Minn). 2013;19(3 Epilepsy):697-714.
ASCP: Moving from treatment to prevention in mental illness – an achievable goal?
MIAMI BEACH – Researchers reporting early work in three areas of chronic mental illness or disability – autism spectrum disorder, schizophrenia, and bipolar disorder – shared the promising results of early detection and intervention programs during a plenary session at a meeting of the American Society for Clinical Psychopharmacology, formerly known as the New Clinical Drug Evaluation Unit meeting. Common themes across research in these disparate illnesses included the benefit of early identification of at-risk individuals and the hope that early intervention might modify the disease course of lifelong illnesses.
Geraldine Dawson, Ph.D., of Duke University in Durham, N.C., shared the results of her early detection and intervention programs. Since siblings of individuals with autism spectrum disorders are at increased risk for autism spectrum disorder (ASD), researchers began using eye-tracking exercises in very young infants. Some studies have reported differences in attention and gaze in infants as young as 4 months old; infants who went on to develop ASD spent less time focusing on the eyes of faces. Infants who later developed ASD also showed less differential in EEG tracings to direct versus averted gaze than normally developing infants. Dr. Dawson’s work found that toddlers with ASD showed distinctly more EEG reactivity to familiar versus unfamiliar objects, but not faces, indicating a lack of ability to differentiate faces.
Those changes, said Dr. Dawson, might indicate a fundamental biologic underpinning to ASD. Further, the lack of interaction with the social environment that’s seen so early might result in overall reduced input and stimulation for the developing prefrontal cortex, influencing development. “We have a double whammy going on here,” said Dr. Dawson, professor in the department of psychiatry and behavioral sciences at Duke.
Dr. Dawson found that early intensive behavioral intervention that started before age 2 and lasted for 2 years resulted in improved cognitive, language, and social behavior. In addition, brain activity of these children in response to social stimuli by the age of 4 was indistinguishable from that of a typical 4-year-old, said Dr. Dawson, also a professor in the departments of psychology and neuroscience, and pediatrics at the university.
She also shared the results of a small pilot study with parents of infants at risk for ASD who were coached in strategies that promote interaction with the social environment. She found that among at-risk infants, by 12 months of age, they showed more normal EEG responses to social stimuli.
Dr. Dawson emphasized that it is not yet known whether the early stimulation reduces later symptoms of autism. She said she hopes that a combination of pharmacologic and behavioral interventions will emerge that will enhance synaptic plasticity and improve outcomes for greater numbers of children.
Dr. John M. Kane spoke to the effectiveness of the NAVIGATE structured team-based assessment and treatment program for individuals newly diagnosed with schizophrenia. The program also incorporated COMPASS, a web-based documentation, shared decision making, and decision support tool. Using a cluster-randomized protocol comparing NAVIGATE to community care for first-episode schizophrenia, Dr. Kane and his colleagues assessed 404 patients at 34 sites in 21 states over a 2-year-year period.
In early results, NAVIGATE enrollees were strikingly more likely to be asked regularly about medication use, side effects, and symptoms; to receive counseling about work or school options; and to have family counseling and support than those receiving usual treatment in the community-based centers participating in the program over the 2 years of the study period.
Early and standardized delivery of the coordinated specialty care model, said Dr. Kane, was associated with patients staying in treatment significantly longer, being more likely to be working or in school, and experiencing symptom improvement. Patients receiving the NAVIGATE intervention had significant improvement in the study’s primary outcome measure, quality of life, said Dr. Kane, professor of psychiatry, neurology, and neuroscience at the Albert Einstein College of Medicine, New York.
Ellen Frank, Ph.D., of the University of Pittsburgh, began her presentation by expressing frank envy for her colleagues’ relatively advanced understanding of the pathophysiology of autism and schizophrenia. By contrast, she said, very little is known about the bipolar disorders.
One thing that is known, however, is the high degree of heritability of bipolar disorder. Her work, she said, begins to assess whether prediagnosis behavioral interventions among children of parents with bipolar disorder might impact the course of the disorder or even prevent its development.
Building on the knowledge that anxiety, depression, and emotional ability in adolescence are predictors for the development of bipolar disorder, Dr. Frank developed and implemented an intervention that focused on regularizing sleep and social rhythms for these at-risk adolescents.
The open pilot study of 42 evenly split adolescents compared those who received the usual appropriate referrals alone with those who received these referrals, plus sleep and social rhythm–targeted education and support for families and the teens themselves. These interventions, dubbed interpersonal and social rhythm therapy (IPRST), have been shown to reduce illness recurrence in adults with bipolar disorder, said Dr. Frank, also director of the depression and manic-depression prevention program at the Western Psychiatric Institute and Clinic in Pittsburgh.
Over the 6-month follow-up period, Dr. Frank said, IPRST recipients had significantly fewer subclinical symptoms of depression and hypomania (P <.05 for both) than their controls, according to assessors who were blinded as to intervention. Participants and their families were satisfied overall with the IPRST therapy, and Dr. Frank noted that the adolescents were “remarkably willing to be open” during the sessions.
Dr. Frank reiterated the less mature state of knowledge about the etiology and natural history of bipolar disorders. Even so, she said, this small pilot study showed an encouraging improvement in sleep patterns and a global improvement in mood and functioning among teens at significantly increased risk for bipolar disorder.
Dr. Dawson serves on the scientific advisory boards of several entities, including Janssen Research and Development and Roche Pharmaceuticals. She also receives royalties from Guilford Press and Oxford University Press. Dr. Kane has served as a consultant to several companies, including Forest Pharmaceuticals. Dr. Frank’s disclosures include Guilford Press and Servier International.
On Twitter @karioakes
MIAMI BEACH – Researchers reporting early work in three areas of chronic mental illness or disability – autism spectrum disorder, schizophrenia, and bipolar disorder – shared the promising results of early detection and intervention programs during a plenary session at a meeting of the American Society for Clinical Psychopharmacology, formerly known as the New Clinical Drug Evaluation Unit meeting. Common themes across research in these disparate illnesses included the benefit of early identification of at-risk individuals and the hope that early intervention might modify the disease course of lifelong illnesses.
Geraldine Dawson, Ph.D., of Duke University in Durham, N.C., shared the results of her early detection and intervention programs. Since siblings of individuals with autism spectrum disorders are at increased risk for autism spectrum disorder (ASD), researchers began using eye-tracking exercises in very young infants. Some studies have reported differences in attention and gaze in infants as young as 4 months old; infants who went on to develop ASD spent less time focusing on the eyes of faces. Infants who later developed ASD also showed less differential in EEG tracings to direct versus averted gaze than normally developing infants. Dr. Dawson’s work found that toddlers with ASD showed distinctly more EEG reactivity to familiar versus unfamiliar objects, but not faces, indicating a lack of ability to differentiate faces.
Those changes, said Dr. Dawson, might indicate a fundamental biologic underpinning to ASD. Further, the lack of interaction with the social environment that’s seen so early might result in overall reduced input and stimulation for the developing prefrontal cortex, influencing development. “We have a double whammy going on here,” said Dr. Dawson, professor in the department of psychiatry and behavioral sciences at Duke.
Dr. Dawson found that early intensive behavioral intervention that started before age 2 and lasted for 2 years resulted in improved cognitive, language, and social behavior. In addition, brain activity of these children in response to social stimuli by the age of 4 was indistinguishable from that of a typical 4-year-old, said Dr. Dawson, also a professor in the departments of psychology and neuroscience, and pediatrics at the university.
She also shared the results of a small pilot study with parents of infants at risk for ASD who were coached in strategies that promote interaction with the social environment. She found that among at-risk infants, by 12 months of age, they showed more normal EEG responses to social stimuli.
Dr. Dawson emphasized that it is not yet known whether the early stimulation reduces later symptoms of autism. She said she hopes that a combination of pharmacologic and behavioral interventions will emerge that will enhance synaptic plasticity and improve outcomes for greater numbers of children.
Dr. John M. Kane spoke to the effectiveness of the NAVIGATE structured team-based assessment and treatment program for individuals newly diagnosed with schizophrenia. The program also incorporated COMPASS, a web-based documentation, shared decision making, and decision support tool. Using a cluster-randomized protocol comparing NAVIGATE to community care for first-episode schizophrenia, Dr. Kane and his colleagues assessed 404 patients at 34 sites in 21 states over a 2-year-year period.
In early results, NAVIGATE enrollees were strikingly more likely to be asked regularly about medication use, side effects, and symptoms; to receive counseling about work or school options; and to have family counseling and support than those receiving usual treatment in the community-based centers participating in the program over the 2 years of the study period.
Early and standardized delivery of the coordinated specialty care model, said Dr. Kane, was associated with patients staying in treatment significantly longer, being more likely to be working or in school, and experiencing symptom improvement. Patients receiving the NAVIGATE intervention had significant improvement in the study’s primary outcome measure, quality of life, said Dr. Kane, professor of psychiatry, neurology, and neuroscience at the Albert Einstein College of Medicine, New York.
Ellen Frank, Ph.D., of the University of Pittsburgh, began her presentation by expressing frank envy for her colleagues’ relatively advanced understanding of the pathophysiology of autism and schizophrenia. By contrast, she said, very little is known about the bipolar disorders.
One thing that is known, however, is the high degree of heritability of bipolar disorder. Her work, she said, begins to assess whether prediagnosis behavioral interventions among children of parents with bipolar disorder might impact the course of the disorder or even prevent its development.
Building on the knowledge that anxiety, depression, and emotional ability in adolescence are predictors for the development of bipolar disorder, Dr. Frank developed and implemented an intervention that focused on regularizing sleep and social rhythms for these at-risk adolescents.
The open pilot study of 42 evenly split adolescents compared those who received the usual appropriate referrals alone with those who received these referrals, plus sleep and social rhythm–targeted education and support for families and the teens themselves. These interventions, dubbed interpersonal and social rhythm therapy (IPRST), have been shown to reduce illness recurrence in adults with bipolar disorder, said Dr. Frank, also director of the depression and manic-depression prevention program at the Western Psychiatric Institute and Clinic in Pittsburgh.
Over the 6-month follow-up period, Dr. Frank said, IPRST recipients had significantly fewer subclinical symptoms of depression and hypomania (P <.05 for both) than their controls, according to assessors who were blinded as to intervention. Participants and their families were satisfied overall with the IPRST therapy, and Dr. Frank noted that the adolescents were “remarkably willing to be open” during the sessions.
Dr. Frank reiterated the less mature state of knowledge about the etiology and natural history of bipolar disorders. Even so, she said, this small pilot study showed an encouraging improvement in sleep patterns and a global improvement in mood and functioning among teens at significantly increased risk for bipolar disorder.
Dr. Dawson serves on the scientific advisory boards of several entities, including Janssen Research and Development and Roche Pharmaceuticals. She also receives royalties from Guilford Press and Oxford University Press. Dr. Kane has served as a consultant to several companies, including Forest Pharmaceuticals. Dr. Frank’s disclosures include Guilford Press and Servier International.
On Twitter @karioakes
MIAMI BEACH – Researchers reporting early work in three areas of chronic mental illness or disability – autism spectrum disorder, schizophrenia, and bipolar disorder – shared the promising results of early detection and intervention programs during a plenary session at a meeting of the American Society for Clinical Psychopharmacology, formerly known as the New Clinical Drug Evaluation Unit meeting. Common themes across research in these disparate illnesses included the benefit of early identification of at-risk individuals and the hope that early intervention might modify the disease course of lifelong illnesses.
Geraldine Dawson, Ph.D., of Duke University in Durham, N.C., shared the results of her early detection and intervention programs. Since siblings of individuals with autism spectrum disorders are at increased risk for autism spectrum disorder (ASD), researchers began using eye-tracking exercises in very young infants. Some studies have reported differences in attention and gaze in infants as young as 4 months old; infants who went on to develop ASD spent less time focusing on the eyes of faces. Infants who later developed ASD also showed less differential in EEG tracings to direct versus averted gaze than normally developing infants. Dr. Dawson’s work found that toddlers with ASD showed distinctly more EEG reactivity to familiar versus unfamiliar objects, but not faces, indicating a lack of ability to differentiate faces.
Those changes, said Dr. Dawson, might indicate a fundamental biologic underpinning to ASD. Further, the lack of interaction with the social environment that’s seen so early might result in overall reduced input and stimulation for the developing prefrontal cortex, influencing development. “We have a double whammy going on here,” said Dr. Dawson, professor in the department of psychiatry and behavioral sciences at Duke.
Dr. Dawson found that early intensive behavioral intervention that started before age 2 and lasted for 2 years resulted in improved cognitive, language, and social behavior. In addition, brain activity of these children in response to social stimuli by the age of 4 was indistinguishable from that of a typical 4-year-old, said Dr. Dawson, also a professor in the departments of psychology and neuroscience, and pediatrics at the university.
She also shared the results of a small pilot study with parents of infants at risk for ASD who were coached in strategies that promote interaction with the social environment. She found that among at-risk infants, by 12 months of age, they showed more normal EEG responses to social stimuli.
Dr. Dawson emphasized that it is not yet known whether the early stimulation reduces later symptoms of autism. She said she hopes that a combination of pharmacologic and behavioral interventions will emerge that will enhance synaptic plasticity and improve outcomes for greater numbers of children.
Dr. John M. Kane spoke to the effectiveness of the NAVIGATE structured team-based assessment and treatment program for individuals newly diagnosed with schizophrenia. The program also incorporated COMPASS, a web-based documentation, shared decision making, and decision support tool. Using a cluster-randomized protocol comparing NAVIGATE to community care for first-episode schizophrenia, Dr. Kane and his colleagues assessed 404 patients at 34 sites in 21 states over a 2-year-year period.
In early results, NAVIGATE enrollees were strikingly more likely to be asked regularly about medication use, side effects, and symptoms; to receive counseling about work or school options; and to have family counseling and support than those receiving usual treatment in the community-based centers participating in the program over the 2 years of the study period.
Early and standardized delivery of the coordinated specialty care model, said Dr. Kane, was associated with patients staying in treatment significantly longer, being more likely to be working or in school, and experiencing symptom improvement. Patients receiving the NAVIGATE intervention had significant improvement in the study’s primary outcome measure, quality of life, said Dr. Kane, professor of psychiatry, neurology, and neuroscience at the Albert Einstein College of Medicine, New York.
Ellen Frank, Ph.D., of the University of Pittsburgh, began her presentation by expressing frank envy for her colleagues’ relatively advanced understanding of the pathophysiology of autism and schizophrenia. By contrast, she said, very little is known about the bipolar disorders.
One thing that is known, however, is the high degree of heritability of bipolar disorder. Her work, she said, begins to assess whether prediagnosis behavioral interventions among children of parents with bipolar disorder might impact the course of the disorder or even prevent its development.
Building on the knowledge that anxiety, depression, and emotional ability in adolescence are predictors for the development of bipolar disorder, Dr. Frank developed and implemented an intervention that focused on regularizing sleep and social rhythms for these at-risk adolescents.
The open pilot study of 42 evenly split adolescents compared those who received the usual appropriate referrals alone with those who received these referrals, plus sleep and social rhythm–targeted education and support for families and the teens themselves. These interventions, dubbed interpersonal and social rhythm therapy (IPRST), have been shown to reduce illness recurrence in adults with bipolar disorder, said Dr. Frank, also director of the depression and manic-depression prevention program at the Western Psychiatric Institute and Clinic in Pittsburgh.
Over the 6-month follow-up period, Dr. Frank said, IPRST recipients had significantly fewer subclinical symptoms of depression and hypomania (P <.05 for both) than their controls, according to assessors who were blinded as to intervention. Participants and their families were satisfied overall with the IPRST therapy, and Dr. Frank noted that the adolescents were “remarkably willing to be open” during the sessions.
Dr. Frank reiterated the less mature state of knowledge about the etiology and natural history of bipolar disorders. Even so, she said, this small pilot study showed an encouraging improvement in sleep patterns and a global improvement in mood and functioning among teens at significantly increased risk for bipolar disorder.
Dr. Dawson serves on the scientific advisory boards of several entities, including Janssen Research and Development and Roche Pharmaceuticals. She also receives royalties from Guilford Press and Oxford University Press. Dr. Kane has served as a consultant to several companies, including Forest Pharmaceuticals. Dr. Frank’s disclosures include Guilford Press and Servier International.
On Twitter @karioakes
Initial symptoms, BMI among factors may predict bipolar mania outcomes
Doctors looking for treatment options for bipolar mania would be wise to keep the following in mind: The presence of psychotic symptoms during the manic index episode, the number of past depressive episodes, and body mass index may be the best predictors of functional outcome at 6 months’ follow-up after a manic episode.
A team of researchers led by Dr. C. Mar Bonn<scaps>í</scaps>n of the University of Barcelona examined 169 patients with bipolar disorder I who suffered an acute manic episode and were treated clinically and followed up at 6 months. Bipolar severity was assessed using scores from the Functioning Assessment Short Test (FAST) scale. The researchers then used a multivariate analysis to identify six variables that best predicted functional outcome at 6-month follow-up after a manic episode. Only three of the variables were found to be statistically significant: the number of previous depressive episodes (P = .002), the presence of psychotic symptoms during the index manic episode (P = .031), and body mass index (P = .041).
“The effective prevention of depressive episodes may be crucial to prevent further disability. Moreover, early treatment of psychotic symptoms may be of importance to avoid the progression and further worsening of the manic episode. Finally, educating patients in healthy lifestyle, including exercise and eating habits, may also help to avoid long-term treatment side effects of those drugs often associated with weight increase or other comorbidities associated to weight gain,” wrote the investigators.
Read the full article here: Journal of Affective Disorders 2015;182:121-5 (http://dx.doi.org/10.1016/j.jad.2015.04.043).
Doctors looking for treatment options for bipolar mania would be wise to keep the following in mind: The presence of psychotic symptoms during the manic index episode, the number of past depressive episodes, and body mass index may be the best predictors of functional outcome at 6 months’ follow-up after a manic episode.
A team of researchers led by Dr. C. Mar Bonn<scaps>í</scaps>n of the University of Barcelona examined 169 patients with bipolar disorder I who suffered an acute manic episode and were treated clinically and followed up at 6 months. Bipolar severity was assessed using scores from the Functioning Assessment Short Test (FAST) scale. The researchers then used a multivariate analysis to identify six variables that best predicted functional outcome at 6-month follow-up after a manic episode. Only three of the variables were found to be statistically significant: the number of previous depressive episodes (P = .002), the presence of psychotic symptoms during the index manic episode (P = .031), and body mass index (P = .041).
“The effective prevention of depressive episodes may be crucial to prevent further disability. Moreover, early treatment of psychotic symptoms may be of importance to avoid the progression and further worsening of the manic episode. Finally, educating patients in healthy lifestyle, including exercise and eating habits, may also help to avoid long-term treatment side effects of those drugs often associated with weight increase or other comorbidities associated to weight gain,” wrote the investigators.
Read the full article here: Journal of Affective Disorders 2015;182:121-5 (http://dx.doi.org/10.1016/j.jad.2015.04.043).
Doctors looking for treatment options for bipolar mania would be wise to keep the following in mind: The presence of psychotic symptoms during the manic index episode, the number of past depressive episodes, and body mass index may be the best predictors of functional outcome at 6 months’ follow-up after a manic episode.
A team of researchers led by Dr. C. Mar Bonn<scaps>í</scaps>n of the University of Barcelona examined 169 patients with bipolar disorder I who suffered an acute manic episode and were treated clinically and followed up at 6 months. Bipolar severity was assessed using scores from the Functioning Assessment Short Test (FAST) scale. The researchers then used a multivariate analysis to identify six variables that best predicted functional outcome at 6-month follow-up after a manic episode. Only three of the variables were found to be statistically significant: the number of previous depressive episodes (P = .002), the presence of psychotic symptoms during the index manic episode (P = .031), and body mass index (P = .041).
“The effective prevention of depressive episodes may be crucial to prevent further disability. Moreover, early treatment of psychotic symptoms may be of importance to avoid the progression and further worsening of the manic episode. Finally, educating patients in healthy lifestyle, including exercise and eating habits, may also help to avoid long-term treatment side effects of those drugs often associated with weight increase or other comorbidities associated to weight gain,” wrote the investigators.
Read the full article here: Journal of Affective Disorders 2015;182:121-5 (http://dx.doi.org/10.1016/j.jad.2015.04.043).
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Impulsivity related to medication nonadherence in bipolar patients
Euthymic bipolar disorder patients with poor medication adherence are more likely to experience nonplanning impulsivity, according to Dr. Raoul Belzeaux and his associates.
Dr. Belzeaux and his associates conducted a cross-sectional study at nine centers across France. They collected data from 260 outpatients in symptomatic remission who had been diagnosed with bipolar disorder type I, type II, or not otherwise specified based on DSM-IV criteria.
The Medication Adherence Rating Scale total mean score for the study was 7.6, which is suboptimal. The standardized coefficient between nonplanning impulsivity score and MARS score was 0.156. Factors outside medication adherence, such as lifetime anxiety disorders, had little effect on impulsivity and medication adherence.
“The association between impulsivity and adherence to medication may lead to systematically evaluate impulsivity” for example, with standardized questionnaires such as the Barratt Impulsiveness Scale “in clinical practice to better predict risk of nonadherence and, thus, contribute to promote personalized treatment strategy,” the investigators concluded.
Find the full study in the Journal of Affective Disorders (doi: 10.1016/j.jad.2015.05.041).
Euthymic bipolar disorder patients with poor medication adherence are more likely to experience nonplanning impulsivity, according to Dr. Raoul Belzeaux and his associates.
Dr. Belzeaux and his associates conducted a cross-sectional study at nine centers across France. They collected data from 260 outpatients in symptomatic remission who had been diagnosed with bipolar disorder type I, type II, or not otherwise specified based on DSM-IV criteria.
The Medication Adherence Rating Scale total mean score for the study was 7.6, which is suboptimal. The standardized coefficient between nonplanning impulsivity score and MARS score was 0.156. Factors outside medication adherence, such as lifetime anxiety disorders, had little effect on impulsivity and medication adherence.
“The association between impulsivity and adherence to medication may lead to systematically evaluate impulsivity” for example, with standardized questionnaires such as the Barratt Impulsiveness Scale “in clinical practice to better predict risk of nonadherence and, thus, contribute to promote personalized treatment strategy,” the investigators concluded.
Find the full study in the Journal of Affective Disorders (doi: 10.1016/j.jad.2015.05.041).
Euthymic bipolar disorder patients with poor medication adherence are more likely to experience nonplanning impulsivity, according to Dr. Raoul Belzeaux and his associates.
Dr. Belzeaux and his associates conducted a cross-sectional study at nine centers across France. They collected data from 260 outpatients in symptomatic remission who had been diagnosed with bipolar disorder type I, type II, or not otherwise specified based on DSM-IV criteria.
The Medication Adherence Rating Scale total mean score for the study was 7.6, which is suboptimal. The standardized coefficient between nonplanning impulsivity score and MARS score was 0.156. Factors outside medication adherence, such as lifetime anxiety disorders, had little effect on impulsivity and medication adherence.
“The association between impulsivity and adherence to medication may lead to systematically evaluate impulsivity” for example, with standardized questionnaires such as the Barratt Impulsiveness Scale “in clinical practice to better predict risk of nonadherence and, thus, contribute to promote personalized treatment strategy,” the investigators concluded.
Find the full study in the Journal of Affective Disorders (doi: 10.1016/j.jad.2015.05.041).
Incidence of first-ever bipolar diagnoses rose, researchers find
Both the incidence of bipolar disorder and the standardized mortality ratio of patients with bipolar disorder, compared with the general population, significantly increased, according to a Danish cohort study.
The study was of 15,334 patients with a first-ever diagnosis of bipolar disorder, according to the International Classification of Diseases (ICD)-10 criteria, between Jan. 1, 1995, and Dec. 31, 2012. Patients were followed until Dec. 31, 2012, or death, whichever came first. Data came from the Danish Psychiatric Central Research Register, a national electronic registry containing all psychiatric hospitalizations since 1969 and all psychiatric outpatient contacts and emergency room visits since 1995. Those diagnosed with schizophrenia subsequent to being diagnosed with bipolar disorder and patients who received one of several specific ICD-8 diagnoses before 1995 (when the ICD-8 was in use) were excluded.
Bipolar disorder became significantly more common, especially throughout the 2000s. The total incidence rate was 18.5/100,000 person-years (PY) in 1995 and, at its lowest, was 14.8/100,000 PY in 1997. The most recent and highest incidence of the disorder was 28.4/100,000 PY in 2012. Such findings represent a higher incidence of bipolar disorder than was found in studies conducted in England during the same period, according to Clara Reece Medici of Aarhus University Hospital, in Risskov, Denmark, and her colleagues.
Significantly more females than males were diagnosed with bipolar disorder, with 9,132 females and 6,202 males having suffered from the disease.
Mortality in patients with bipolar disorder was higher, compared with the general population, with the mean standardized mortality ratio (SMR) for patients with bipolar disorder vs. the general population having been 1.7. Deaths of the bipolar patients were mostly tied to natural causes, but as many as 9% of the bipolar patients committed suicide.
Another of the study’s findings was that age at diagnosis of bipolar disorder decreased by more than 10 years, with the average age at diagnosis having been 54.5 in 1995, compared with 42.4 in 2012. The researchers said increased awareness among clinicians may explain this, but that they will test whether “increased use of antidepressants and medication against [attention-deficit/hyperactivity disorder] in Denmark in the same time period may have contributed to unmasking a latent bipolar episode earlier.”
According to the researchers, “studies on lowering physical illlness in patients with bipolar disorder are needed to lower death by natural causes.”
Read the full study in the Journal of Affective Disorders (doi:http://dx.doi.org/10.1016/j.jad.2015.04.032).
Both the incidence of bipolar disorder and the standardized mortality ratio of patients with bipolar disorder, compared with the general population, significantly increased, according to a Danish cohort study.
The study was of 15,334 patients with a first-ever diagnosis of bipolar disorder, according to the International Classification of Diseases (ICD)-10 criteria, between Jan. 1, 1995, and Dec. 31, 2012. Patients were followed until Dec. 31, 2012, or death, whichever came first. Data came from the Danish Psychiatric Central Research Register, a national electronic registry containing all psychiatric hospitalizations since 1969 and all psychiatric outpatient contacts and emergency room visits since 1995. Those diagnosed with schizophrenia subsequent to being diagnosed with bipolar disorder and patients who received one of several specific ICD-8 diagnoses before 1995 (when the ICD-8 was in use) were excluded.
Bipolar disorder became significantly more common, especially throughout the 2000s. The total incidence rate was 18.5/100,000 person-years (PY) in 1995 and, at its lowest, was 14.8/100,000 PY in 1997. The most recent and highest incidence of the disorder was 28.4/100,000 PY in 2012. Such findings represent a higher incidence of bipolar disorder than was found in studies conducted in England during the same period, according to Clara Reece Medici of Aarhus University Hospital, in Risskov, Denmark, and her colleagues.
Significantly more females than males were diagnosed with bipolar disorder, with 9,132 females and 6,202 males having suffered from the disease.
Mortality in patients with bipolar disorder was higher, compared with the general population, with the mean standardized mortality ratio (SMR) for patients with bipolar disorder vs. the general population having been 1.7. Deaths of the bipolar patients were mostly tied to natural causes, but as many as 9% of the bipolar patients committed suicide.
Another of the study’s findings was that age at diagnosis of bipolar disorder decreased by more than 10 years, with the average age at diagnosis having been 54.5 in 1995, compared with 42.4 in 2012. The researchers said increased awareness among clinicians may explain this, but that they will test whether “increased use of antidepressants and medication against [attention-deficit/hyperactivity disorder] in Denmark in the same time period may have contributed to unmasking a latent bipolar episode earlier.”
According to the researchers, “studies on lowering physical illlness in patients with bipolar disorder are needed to lower death by natural causes.”
Read the full study in the Journal of Affective Disorders (doi:http://dx.doi.org/10.1016/j.jad.2015.04.032).
Both the incidence of bipolar disorder and the standardized mortality ratio of patients with bipolar disorder, compared with the general population, significantly increased, according to a Danish cohort study.
The study was of 15,334 patients with a first-ever diagnosis of bipolar disorder, according to the International Classification of Diseases (ICD)-10 criteria, between Jan. 1, 1995, and Dec. 31, 2012. Patients were followed until Dec. 31, 2012, or death, whichever came first. Data came from the Danish Psychiatric Central Research Register, a national electronic registry containing all psychiatric hospitalizations since 1969 and all psychiatric outpatient contacts and emergency room visits since 1995. Those diagnosed with schizophrenia subsequent to being diagnosed with bipolar disorder and patients who received one of several specific ICD-8 diagnoses before 1995 (when the ICD-8 was in use) were excluded.
Bipolar disorder became significantly more common, especially throughout the 2000s. The total incidence rate was 18.5/100,000 person-years (PY) in 1995 and, at its lowest, was 14.8/100,000 PY in 1997. The most recent and highest incidence of the disorder was 28.4/100,000 PY in 2012. Such findings represent a higher incidence of bipolar disorder than was found in studies conducted in England during the same period, according to Clara Reece Medici of Aarhus University Hospital, in Risskov, Denmark, and her colleagues.
Significantly more females than males were diagnosed with bipolar disorder, with 9,132 females and 6,202 males having suffered from the disease.
Mortality in patients with bipolar disorder was higher, compared with the general population, with the mean standardized mortality ratio (SMR) for patients with bipolar disorder vs. the general population having been 1.7. Deaths of the bipolar patients were mostly tied to natural causes, but as many as 9% of the bipolar patients committed suicide.
Another of the study’s findings was that age at diagnosis of bipolar disorder decreased by more than 10 years, with the average age at diagnosis having been 54.5 in 1995, compared with 42.4 in 2012. The researchers said increased awareness among clinicians may explain this, but that they will test whether “increased use of antidepressants and medication against [attention-deficit/hyperactivity disorder] in Denmark in the same time period may have contributed to unmasking a latent bipolar episode earlier.”
According to the researchers, “studies on lowering physical illlness in patients with bipolar disorder are needed to lower death by natural causes.”
Read the full study in the Journal of Affective Disorders (doi:http://dx.doi.org/10.1016/j.jad.2015.04.032).
FROM JOURNAL OF AFFECTIVE DISORDERS
In recent-onset bipolar disorder, tailored CBT reduced relapses
Recovery-focused cognitive-behavioral therapy can delay and reduce relapses for patients with recent-onset bipolar disorder, Steven H. Jones, Ph.D., and his associates reported in a pilot study that compared 33 patients who received up to 18 hours of tailored CBT and 34 patients who received treatment as usual (TAU).
“This study highlights the potential benefits of taking a formulation-based approach to bipolar disorder, in which a range of evidence-informed techniques are available to the clinician but the relative emphasis given to each is determined on an individual client basis,” the researchers noted in the British Journal of Psychiatry (doi:10.1192/bjp.bp.113.141259).
Dr. Jones of Lancaster (England) University and his colleagues studied participants who met the DSM-IV diagnosis of primary bipolar with onset within the past 5 years. The recovery-focused CBT approach included core items whose use was determined by individual patient needs. The recovery approach was explained, information was gathered about current and historical mood and functioning, the meaning and relevance of the diagnosis were discussed, recovery-informed therapy goals were identified, relationships between mood experiences and progress towards recovery goals were addressed, CBT techniques were identified and applied to facilitate positive coping, and wider functioning issues in relation to recovery were considered. The information was used to develop a recovery plan and lessons from therapy were shared with key stakeholders.
Unlike standard CBT for bipolar disorder, which focuses on preventing relapse, the tailored CBT approach elicited client-focused goals and the freedom to work within whatever model the client brings. The model could address functioning and comorbidity issues as well as mood problems, and emphasized supporting clients to move away from self-critical and stigmatizing language, especially around diagnosis and behavior in acute episodes.
The primary clinical outcomes were measured using the Bipolar Recovery Questionnaire (33-item version, 0-100 scale with higher score indicating higher personal recovery), time to bipolar relapse measured by the Structural Clinical Interview for DSM-IV (SCID)-LIFE, and mood symptoms as measured by the Hamilton Rating Scale for Depression and Bech-Rafaelsen Mania Scale.
After 12 months, the CBT group’s Bipolar Recovery Questionnaire mean score was 2,351 – a 30% improvement from baseline (1,797), while the TAU group’s mean score was 2,193 – an 8% improvement from baseline(1,935).
Both manic and depressive relapses were less common and took longer to occur in the CBT group. There were 11 depressive relapses in the CBT group, occurring after a median of 60 weeks. There were 19 relapses in the TAU group, occurring after a median of 18 weeks. There were 3 manic relapses in the CBT group, occurring after a median of 60 weeks, and 10 manic relapses in the TAU group occurring after a median of 33 weeks.
Recovery-focused cognitive-behavioral therapy can delay and reduce relapses for patients with recent-onset bipolar disorder, Steven H. Jones, Ph.D., and his associates reported in a pilot study that compared 33 patients who received up to 18 hours of tailored CBT and 34 patients who received treatment as usual (TAU).
“This study highlights the potential benefits of taking a formulation-based approach to bipolar disorder, in which a range of evidence-informed techniques are available to the clinician but the relative emphasis given to each is determined on an individual client basis,” the researchers noted in the British Journal of Psychiatry (doi:10.1192/bjp.bp.113.141259).
Dr. Jones of Lancaster (England) University and his colleagues studied participants who met the DSM-IV diagnosis of primary bipolar with onset within the past 5 years. The recovery-focused CBT approach included core items whose use was determined by individual patient needs. The recovery approach was explained, information was gathered about current and historical mood and functioning, the meaning and relevance of the diagnosis were discussed, recovery-informed therapy goals were identified, relationships between mood experiences and progress towards recovery goals were addressed, CBT techniques were identified and applied to facilitate positive coping, and wider functioning issues in relation to recovery were considered. The information was used to develop a recovery plan and lessons from therapy were shared with key stakeholders.
Unlike standard CBT for bipolar disorder, which focuses on preventing relapse, the tailored CBT approach elicited client-focused goals and the freedom to work within whatever model the client brings. The model could address functioning and comorbidity issues as well as mood problems, and emphasized supporting clients to move away from self-critical and stigmatizing language, especially around diagnosis and behavior in acute episodes.
The primary clinical outcomes were measured using the Bipolar Recovery Questionnaire (33-item version, 0-100 scale with higher score indicating higher personal recovery), time to bipolar relapse measured by the Structural Clinical Interview for DSM-IV (SCID)-LIFE, and mood symptoms as measured by the Hamilton Rating Scale for Depression and Bech-Rafaelsen Mania Scale.
After 12 months, the CBT group’s Bipolar Recovery Questionnaire mean score was 2,351 – a 30% improvement from baseline (1,797), while the TAU group’s mean score was 2,193 – an 8% improvement from baseline(1,935).
Both manic and depressive relapses were less common and took longer to occur in the CBT group. There were 11 depressive relapses in the CBT group, occurring after a median of 60 weeks. There were 19 relapses in the TAU group, occurring after a median of 18 weeks. There were 3 manic relapses in the CBT group, occurring after a median of 60 weeks, and 10 manic relapses in the TAU group occurring after a median of 33 weeks.
Recovery-focused cognitive-behavioral therapy can delay and reduce relapses for patients with recent-onset bipolar disorder, Steven H. Jones, Ph.D., and his associates reported in a pilot study that compared 33 patients who received up to 18 hours of tailored CBT and 34 patients who received treatment as usual (TAU).
“This study highlights the potential benefits of taking a formulation-based approach to bipolar disorder, in which a range of evidence-informed techniques are available to the clinician but the relative emphasis given to each is determined on an individual client basis,” the researchers noted in the British Journal of Psychiatry (doi:10.1192/bjp.bp.113.141259).
Dr. Jones of Lancaster (England) University and his colleagues studied participants who met the DSM-IV diagnosis of primary bipolar with onset within the past 5 years. The recovery-focused CBT approach included core items whose use was determined by individual patient needs. The recovery approach was explained, information was gathered about current and historical mood and functioning, the meaning and relevance of the diagnosis were discussed, recovery-informed therapy goals were identified, relationships between mood experiences and progress towards recovery goals were addressed, CBT techniques were identified and applied to facilitate positive coping, and wider functioning issues in relation to recovery were considered. The information was used to develop a recovery plan and lessons from therapy were shared with key stakeholders.
Unlike standard CBT for bipolar disorder, which focuses on preventing relapse, the tailored CBT approach elicited client-focused goals and the freedom to work within whatever model the client brings. The model could address functioning and comorbidity issues as well as mood problems, and emphasized supporting clients to move away from self-critical and stigmatizing language, especially around diagnosis and behavior in acute episodes.
The primary clinical outcomes were measured using the Bipolar Recovery Questionnaire (33-item version, 0-100 scale with higher score indicating higher personal recovery), time to bipolar relapse measured by the Structural Clinical Interview for DSM-IV (SCID)-LIFE, and mood symptoms as measured by the Hamilton Rating Scale for Depression and Bech-Rafaelsen Mania Scale.
After 12 months, the CBT group’s Bipolar Recovery Questionnaire mean score was 2,351 – a 30% improvement from baseline (1,797), while the TAU group’s mean score was 2,193 – an 8% improvement from baseline(1,935).
Both manic and depressive relapses were less common and took longer to occur in the CBT group. There were 11 depressive relapses in the CBT group, occurring after a median of 60 weeks. There were 19 relapses in the TAU group, occurring after a median of 18 weeks. There were 3 manic relapses in the CBT group, occurring after a median of 60 weeks, and 10 manic relapses in the TAU group occurring after a median of 33 weeks.
Key clinical point: Patient-focused CBT may reduce relapses in recent-onset bipolar disorder.
Major finding: After 12 months, the CBT group’s Bipolar Recovery Questionnaire mean score was 2,351 – a 30% improvement from baseline (1,797), while the usual treatment group’s mean score was 2,193 – an 8% improvement from baseline(1,935).
Data source: A prospective study of 67 patients with recent-onset bipolar disorder, 33 given CBT and 34 given usual therapy.
Disclosures: The researchers had no relevant financial disclosures.
Legislation aims to improve treatment of serious mental illness
WASHINGTON – A new bill sponsored by Rep. Tim Murphy (R-Pa.) aims to improve the treatment of serious mental illness by providing access and assistance to families and caregivers, improving mental health and substance abuse treatment parity, and encouraging evidence-based mental health care.
H.R. 2646, the Helping Families in Mental Health Crisis Act of 2015, also would increase the number of psychiatric hospital beds for those in acute crisis, allocate funds to mental and behavioral health workforce development, and reform oversight of mental health care delivery.
The bill was originally introduced in the last Congress, after the mass shooting in Newtown, Conn. It is based on the findings of a report commissioned by the House Energy & Commerce Committee’s Subcommittee on Oversight & Investigations, which cited high levels of untreated serious mental illness nationwide.
During a June 16 hearing on the bill, Virginia state senator Creigh Deeds, a Democrat, testified about his son’s serious mental illness. Sen. Deeds said that it wasn’t until after his son had stabbed him multiple times, then killed himself, that the senator learned the details of his son’s treatment for bipolar disorder. Those details might have allowed him to successfully intervene and save his son, Sen. Deeds said. The information he did get often came anonymously, he added, due to providers’ fears of violating HIPAA (Health Insurance Portability and Accountability Act).
“HIPAA prevented me from accessing the information I needed to keep him safe and help him towards recovery. Even though I was the one who cared for him, fed him, housed him, transported him, insured him, I was not privy to any information that could clarify for me his behaviors, his treatment plan, and symptoms to be vigilant about,” Sen. Deeds testified. “I was in the dark as I tried to advocate for him in the best way I could with the best information I had.”
H.R. 2646 would amend HIPAA and FERPA (Family Educational Rights and Privacy Act) to allow family members and other caregivers access to diagnoses, treatment plans, and prescribed medications without patient consent. Release of psychotherapy notes would remain prohibited, however.
Meanwhile, patient privacy legislation (H.R. 2690) introduced by Rep. Doris Matsui (D-Calif.) and considered during the same hearing would clarify and strengthen existing language in HIPAA law by amending but not rewriting it. H.R. 2690 would de-escalate the fears of medical personnel surrounding HIPAA, which Rep. Matsui said was appropriately written but not always applied as intended.
Dr. Jeffrey Lieberman*, chair of the psychiatry department at Columbia University, New York, testified that “simply educating doctors” would not be enough to impact how HIPAA-protected information was shared with concerned families because of “the fear of God placed in doctors by personal injury lawyers who often challenge doctors” even when doctors are doing “the common-sense thing to do.”
H.R. 2646 also calls for medical records and mental health records to be integrated. “If a primary care physician doesn’t know that a patient is recovering from an opiate addiction, that provider might misprescribe the patient an opiate and start that patient into a relapse,” Rep. Murphy said in an interview. “Instead of making the files separate but equal, you make them the same. You can’t treat the brain without treating the body.”
The bill also would change the way Medicaid pays for acute care psychiatric services. Currently, under the institutions of mental disease exclusion, federal Medicaid funds can be used for no more than 16 beds in an inpatient psychiatric facility. According to Dr. Lorenzo Norris, director of inpatient psychiatric services at George Washington University Hospital, Washington, D.C., the result is that state-funded facilities often turn away patients experiencing acute mental health crises. H.R. 2646 would lift the 16-bed limit for inpatient stays of 30 days or less.
Such a change would be “huge. It would definitely increase access to services,” Dr. Norris said in an interview. The bill also calls for the elimination of the 190-day lifetime cap on inpatient psychiatric care covered by Medicare.
The overall aim of the bill, according to Rep. Murphy, is to reinforce existing mental health parity laws and to create more integrated evidence-based interventions for mental disorders, especially serious mental illnesses such as schizophrenia or bipolar disorder. The bill would implement primary care– and community health center–based schizophrenia screening and treatment protocols derived from two projects sponsored by the National Institute of Mental Health: the North American Prodrome Longitudinal Study (NAPLS) and the Recovery After Initial Schizophrenia Episode (RAISE) project.
The bill would increase and consolidate federal oversight of mental health care by doing away with the current top job at the Substance Abuse and Mental Health Services Administration and creating an assistant secretary appointed by the Senate to oversee mental health and substance abuse treatment within the Health and Human Services department. Further, the bill stipulates that the position must be held by a psychiatrist or psychologist. The assistant secretary would administer the current SAMHSA. “I don’t want to eliminate SAMHSA, I want to elevate it,” Rep. Murphy said in an interview.
Several key provisions of the bill have been modified since it was introduced in the last Congress. Previously, Rep. Murphy called for eliminating funds for patients-rights groups, saying they were aligned with the “antipsychiatry movement” that would go as far as advocating people with severe mental illness not take their prescribed medications. Instead, H.R. 2646 would restrict funds to groups that investigate patient abuse and neglect only, which Rep. Murphy said would prevent antipsychiatry activists and others from giving dangerous counsel to those who lack insight into their condition.
The new bill has bipartisan support among subcommittee members. “It’s different than we saw last Congress,” Lauren Alfred, policy director for the Kennedy Forum, said in an interview. “Last time it was more about reacting to crisis, this time it’s more about the future. The focus is on what will happen in primary care offices and across the system if comprehensive mental health care reform goes forward.”
Despite that support, there is some dissent.
Rep. Frank Pallone Jr. (D-N.J.), ranking member of the Energy & Commerce Committee, testified that he favors the language on workforce development and parity enforcement but is opposed to predicating community mental health block grant funding on the existence of state treatment standard and assisted outpatient treatment laws, which Rep. Murphy’s proposed legislation would do.
The bill also raised some alarm with references to antiabortion language. Subcommittee member Rep. Jan Schakowsky (D-Ill.) noted that H.R. 2646 would expand existing restrictions on the use of grant funds to pay for abortions by reauthorizing the Garrett Lee Smith Memorial Act, a suicide prevention law. Rep. Murphy dismissed this claim in an interview, noting that to remove the antiabortion language would mean rewriting the existing suicide prevention law. “It’s existing law from a decade ago and we simply reference that whole bill,” he said. “We haven’t changed anything. There’s nothing partisan or sneaky about it.”
On Twitter @whitneymcknight
*Correction, 6/22/2015: An earlier version of this article misstated Dr. Jeffrey Lieberman's name.
WASHINGTON – A new bill sponsored by Rep. Tim Murphy (R-Pa.) aims to improve the treatment of serious mental illness by providing access and assistance to families and caregivers, improving mental health and substance abuse treatment parity, and encouraging evidence-based mental health care.
H.R. 2646, the Helping Families in Mental Health Crisis Act of 2015, also would increase the number of psychiatric hospital beds for those in acute crisis, allocate funds to mental and behavioral health workforce development, and reform oversight of mental health care delivery.
The bill was originally introduced in the last Congress, after the mass shooting in Newtown, Conn. It is based on the findings of a report commissioned by the House Energy & Commerce Committee’s Subcommittee on Oversight & Investigations, which cited high levels of untreated serious mental illness nationwide.
During a June 16 hearing on the bill, Virginia state senator Creigh Deeds, a Democrat, testified about his son’s serious mental illness. Sen. Deeds said that it wasn’t until after his son had stabbed him multiple times, then killed himself, that the senator learned the details of his son’s treatment for bipolar disorder. Those details might have allowed him to successfully intervene and save his son, Sen. Deeds said. The information he did get often came anonymously, he added, due to providers’ fears of violating HIPAA (Health Insurance Portability and Accountability Act).
“HIPAA prevented me from accessing the information I needed to keep him safe and help him towards recovery. Even though I was the one who cared for him, fed him, housed him, transported him, insured him, I was not privy to any information that could clarify for me his behaviors, his treatment plan, and symptoms to be vigilant about,” Sen. Deeds testified. “I was in the dark as I tried to advocate for him in the best way I could with the best information I had.”
H.R. 2646 would amend HIPAA and FERPA (Family Educational Rights and Privacy Act) to allow family members and other caregivers access to diagnoses, treatment plans, and prescribed medications without patient consent. Release of psychotherapy notes would remain prohibited, however.
Meanwhile, patient privacy legislation (H.R. 2690) introduced by Rep. Doris Matsui (D-Calif.) and considered during the same hearing would clarify and strengthen existing language in HIPAA law by amending but not rewriting it. H.R. 2690 would de-escalate the fears of medical personnel surrounding HIPAA, which Rep. Matsui said was appropriately written but not always applied as intended.
Dr. Jeffrey Lieberman*, chair of the psychiatry department at Columbia University, New York, testified that “simply educating doctors” would not be enough to impact how HIPAA-protected information was shared with concerned families because of “the fear of God placed in doctors by personal injury lawyers who often challenge doctors” even when doctors are doing “the common-sense thing to do.”
H.R. 2646 also calls for medical records and mental health records to be integrated. “If a primary care physician doesn’t know that a patient is recovering from an opiate addiction, that provider might misprescribe the patient an opiate and start that patient into a relapse,” Rep. Murphy said in an interview. “Instead of making the files separate but equal, you make them the same. You can’t treat the brain without treating the body.”
The bill also would change the way Medicaid pays for acute care psychiatric services. Currently, under the institutions of mental disease exclusion, federal Medicaid funds can be used for no more than 16 beds in an inpatient psychiatric facility. According to Dr. Lorenzo Norris, director of inpatient psychiatric services at George Washington University Hospital, Washington, D.C., the result is that state-funded facilities often turn away patients experiencing acute mental health crises. H.R. 2646 would lift the 16-bed limit for inpatient stays of 30 days or less.
Such a change would be “huge. It would definitely increase access to services,” Dr. Norris said in an interview. The bill also calls for the elimination of the 190-day lifetime cap on inpatient psychiatric care covered by Medicare.
The overall aim of the bill, according to Rep. Murphy, is to reinforce existing mental health parity laws and to create more integrated evidence-based interventions for mental disorders, especially serious mental illnesses such as schizophrenia or bipolar disorder. The bill would implement primary care– and community health center–based schizophrenia screening and treatment protocols derived from two projects sponsored by the National Institute of Mental Health: the North American Prodrome Longitudinal Study (NAPLS) and the Recovery After Initial Schizophrenia Episode (RAISE) project.
The bill would increase and consolidate federal oversight of mental health care by doing away with the current top job at the Substance Abuse and Mental Health Services Administration and creating an assistant secretary appointed by the Senate to oversee mental health and substance abuse treatment within the Health and Human Services department. Further, the bill stipulates that the position must be held by a psychiatrist or psychologist. The assistant secretary would administer the current SAMHSA. “I don’t want to eliminate SAMHSA, I want to elevate it,” Rep. Murphy said in an interview.
Several key provisions of the bill have been modified since it was introduced in the last Congress. Previously, Rep. Murphy called for eliminating funds for patients-rights groups, saying they were aligned with the “antipsychiatry movement” that would go as far as advocating people with severe mental illness not take their prescribed medications. Instead, H.R. 2646 would restrict funds to groups that investigate patient abuse and neglect only, which Rep. Murphy said would prevent antipsychiatry activists and others from giving dangerous counsel to those who lack insight into their condition.
The new bill has bipartisan support among subcommittee members. “It’s different than we saw last Congress,” Lauren Alfred, policy director for the Kennedy Forum, said in an interview. “Last time it was more about reacting to crisis, this time it’s more about the future. The focus is on what will happen in primary care offices and across the system if comprehensive mental health care reform goes forward.”
Despite that support, there is some dissent.
Rep. Frank Pallone Jr. (D-N.J.), ranking member of the Energy & Commerce Committee, testified that he favors the language on workforce development and parity enforcement but is opposed to predicating community mental health block grant funding on the existence of state treatment standard and assisted outpatient treatment laws, which Rep. Murphy’s proposed legislation would do.
The bill also raised some alarm with references to antiabortion language. Subcommittee member Rep. Jan Schakowsky (D-Ill.) noted that H.R. 2646 would expand existing restrictions on the use of grant funds to pay for abortions by reauthorizing the Garrett Lee Smith Memorial Act, a suicide prevention law. Rep. Murphy dismissed this claim in an interview, noting that to remove the antiabortion language would mean rewriting the existing suicide prevention law. “It’s existing law from a decade ago and we simply reference that whole bill,” he said. “We haven’t changed anything. There’s nothing partisan or sneaky about it.”
On Twitter @whitneymcknight
*Correction, 6/22/2015: An earlier version of this article misstated Dr. Jeffrey Lieberman's name.
WASHINGTON – A new bill sponsored by Rep. Tim Murphy (R-Pa.) aims to improve the treatment of serious mental illness by providing access and assistance to families and caregivers, improving mental health and substance abuse treatment parity, and encouraging evidence-based mental health care.
H.R. 2646, the Helping Families in Mental Health Crisis Act of 2015, also would increase the number of psychiatric hospital beds for those in acute crisis, allocate funds to mental and behavioral health workforce development, and reform oversight of mental health care delivery.
The bill was originally introduced in the last Congress, after the mass shooting in Newtown, Conn. It is based on the findings of a report commissioned by the House Energy & Commerce Committee’s Subcommittee on Oversight & Investigations, which cited high levels of untreated serious mental illness nationwide.
During a June 16 hearing on the bill, Virginia state senator Creigh Deeds, a Democrat, testified about his son’s serious mental illness. Sen. Deeds said that it wasn’t until after his son had stabbed him multiple times, then killed himself, that the senator learned the details of his son’s treatment for bipolar disorder. Those details might have allowed him to successfully intervene and save his son, Sen. Deeds said. The information he did get often came anonymously, he added, due to providers’ fears of violating HIPAA (Health Insurance Portability and Accountability Act).
“HIPAA prevented me from accessing the information I needed to keep him safe and help him towards recovery. Even though I was the one who cared for him, fed him, housed him, transported him, insured him, I was not privy to any information that could clarify for me his behaviors, his treatment plan, and symptoms to be vigilant about,” Sen. Deeds testified. “I was in the dark as I tried to advocate for him in the best way I could with the best information I had.”
H.R. 2646 would amend HIPAA and FERPA (Family Educational Rights and Privacy Act) to allow family members and other caregivers access to diagnoses, treatment plans, and prescribed medications without patient consent. Release of psychotherapy notes would remain prohibited, however.
Meanwhile, patient privacy legislation (H.R. 2690) introduced by Rep. Doris Matsui (D-Calif.) and considered during the same hearing would clarify and strengthen existing language in HIPAA law by amending but not rewriting it. H.R. 2690 would de-escalate the fears of medical personnel surrounding HIPAA, which Rep. Matsui said was appropriately written but not always applied as intended.
Dr. Jeffrey Lieberman*, chair of the psychiatry department at Columbia University, New York, testified that “simply educating doctors” would not be enough to impact how HIPAA-protected information was shared with concerned families because of “the fear of God placed in doctors by personal injury lawyers who often challenge doctors” even when doctors are doing “the common-sense thing to do.”
H.R. 2646 also calls for medical records and mental health records to be integrated. “If a primary care physician doesn’t know that a patient is recovering from an opiate addiction, that provider might misprescribe the patient an opiate and start that patient into a relapse,” Rep. Murphy said in an interview. “Instead of making the files separate but equal, you make them the same. You can’t treat the brain without treating the body.”
The bill also would change the way Medicaid pays for acute care psychiatric services. Currently, under the institutions of mental disease exclusion, federal Medicaid funds can be used for no more than 16 beds in an inpatient psychiatric facility. According to Dr. Lorenzo Norris, director of inpatient psychiatric services at George Washington University Hospital, Washington, D.C., the result is that state-funded facilities often turn away patients experiencing acute mental health crises. H.R. 2646 would lift the 16-bed limit for inpatient stays of 30 days or less.
Such a change would be “huge. It would definitely increase access to services,” Dr. Norris said in an interview. The bill also calls for the elimination of the 190-day lifetime cap on inpatient psychiatric care covered by Medicare.
The overall aim of the bill, according to Rep. Murphy, is to reinforce existing mental health parity laws and to create more integrated evidence-based interventions for mental disorders, especially serious mental illnesses such as schizophrenia or bipolar disorder. The bill would implement primary care– and community health center–based schizophrenia screening and treatment protocols derived from two projects sponsored by the National Institute of Mental Health: the North American Prodrome Longitudinal Study (NAPLS) and the Recovery After Initial Schizophrenia Episode (RAISE) project.
The bill would increase and consolidate federal oversight of mental health care by doing away with the current top job at the Substance Abuse and Mental Health Services Administration and creating an assistant secretary appointed by the Senate to oversee mental health and substance abuse treatment within the Health and Human Services department. Further, the bill stipulates that the position must be held by a psychiatrist or psychologist. The assistant secretary would administer the current SAMHSA. “I don’t want to eliminate SAMHSA, I want to elevate it,” Rep. Murphy said in an interview.
Several key provisions of the bill have been modified since it was introduced in the last Congress. Previously, Rep. Murphy called for eliminating funds for patients-rights groups, saying they were aligned with the “antipsychiatry movement” that would go as far as advocating people with severe mental illness not take their prescribed medications. Instead, H.R. 2646 would restrict funds to groups that investigate patient abuse and neglect only, which Rep. Murphy said would prevent antipsychiatry activists and others from giving dangerous counsel to those who lack insight into their condition.
The new bill has bipartisan support among subcommittee members. “It’s different than we saw last Congress,” Lauren Alfred, policy director for the Kennedy Forum, said in an interview. “Last time it was more about reacting to crisis, this time it’s more about the future. The focus is on what will happen in primary care offices and across the system if comprehensive mental health care reform goes forward.”
Despite that support, there is some dissent.
Rep. Frank Pallone Jr. (D-N.J.), ranking member of the Energy & Commerce Committee, testified that he favors the language on workforce development and parity enforcement but is opposed to predicating community mental health block grant funding on the existence of state treatment standard and assisted outpatient treatment laws, which Rep. Murphy’s proposed legislation would do.
The bill also raised some alarm with references to antiabortion language. Subcommittee member Rep. Jan Schakowsky (D-Ill.) noted that H.R. 2646 would expand existing restrictions on the use of grant funds to pay for abortions by reauthorizing the Garrett Lee Smith Memorial Act, a suicide prevention law. Rep. Murphy dismissed this claim in an interview, noting that to remove the antiabortion language would mean rewriting the existing suicide prevention law. “It’s existing law from a decade ago and we simply reference that whole bill,” he said. “We haven’t changed anything. There’s nothing partisan or sneaky about it.”
On Twitter @whitneymcknight
*Correction, 6/22/2015: An earlier version of this article misstated Dr. Jeffrey Lieberman's name.
AT A HOUSE ENERGY & COMMERCE SUBCOMMITTEE HEARING
Migraines are extremely common in bipolar disorder
About one-third of people with bipolar disorder are affected by comorbid migraine, and migraine is significantly more common among bipolar II disorder patients than among those with bipolar I disorder, a meta-analysis shows.
The meta-analysis covered 14 studies of 3,976 patients with some type of bipolar disorder from North America, Europe, and South America. Of the sample, 2,161 had bipolar I disorder and 647 had bipolar II disorder. The type of bipolar disorder the other patients had was either mixed or unknown. On average, each of the studies included 283.69 participants, and the mean age of a participant was 35.5 years. Studies that reported the prevalence of bipolar disorder among people with migraines were excluded.
Fifty-four percent of bipolar II disorder patients had migraines, compared with 32.7% of bipolar I disorder patients. An additional finding of the meta-analysis is that migraine was found significantly more often in studies that used standardized criteria to determine whether a bipolar patient had comorbid migraine than in studies that used nonstandardized criteria, such as self-report.
A meta-regression analysis of data from the studies showed that mean age moderated how frequently migraine occurred among the entire sample.
“The findings of this meta-analysis suggest that the prevalence of comorbid migraine among people with [bipolar disorder] is remarkably high, particularly among people with [bipolar II disorder],” according to Dr. Michele Fornaro and Brendon Stubbs.
The results of this meta-analysis “highlighted the need for further studies focusing on [migraine-bipolar II disorder] comobidity including well-matched control cases with or without rapid cycling features too,” according to the researchers.
Read the full study in Journal of Affective Disorders (doi:http://dx.doi.org/10.1016/j.jad.2015.02.032).
About one-third of people with bipolar disorder are affected by comorbid migraine, and migraine is significantly more common among bipolar II disorder patients than among those with bipolar I disorder, a meta-analysis shows.
The meta-analysis covered 14 studies of 3,976 patients with some type of bipolar disorder from North America, Europe, and South America. Of the sample, 2,161 had bipolar I disorder and 647 had bipolar II disorder. The type of bipolar disorder the other patients had was either mixed or unknown. On average, each of the studies included 283.69 participants, and the mean age of a participant was 35.5 years. Studies that reported the prevalence of bipolar disorder among people with migraines were excluded.
Fifty-four percent of bipolar II disorder patients had migraines, compared with 32.7% of bipolar I disorder patients. An additional finding of the meta-analysis is that migraine was found significantly more often in studies that used standardized criteria to determine whether a bipolar patient had comorbid migraine than in studies that used nonstandardized criteria, such as self-report.
A meta-regression analysis of data from the studies showed that mean age moderated how frequently migraine occurred among the entire sample.
“The findings of this meta-analysis suggest that the prevalence of comorbid migraine among people with [bipolar disorder] is remarkably high, particularly among people with [bipolar II disorder],” according to Dr. Michele Fornaro and Brendon Stubbs.
The results of this meta-analysis “highlighted the need for further studies focusing on [migraine-bipolar II disorder] comobidity including well-matched control cases with or without rapid cycling features too,” according to the researchers.
Read the full study in Journal of Affective Disorders (doi:http://dx.doi.org/10.1016/j.jad.2015.02.032).
About one-third of people with bipolar disorder are affected by comorbid migraine, and migraine is significantly more common among bipolar II disorder patients than among those with bipolar I disorder, a meta-analysis shows.
The meta-analysis covered 14 studies of 3,976 patients with some type of bipolar disorder from North America, Europe, and South America. Of the sample, 2,161 had bipolar I disorder and 647 had bipolar II disorder. The type of bipolar disorder the other patients had was either mixed or unknown. On average, each of the studies included 283.69 participants, and the mean age of a participant was 35.5 years. Studies that reported the prevalence of bipolar disorder among people with migraines were excluded.
Fifty-four percent of bipolar II disorder patients had migraines, compared with 32.7% of bipolar I disorder patients. An additional finding of the meta-analysis is that migraine was found significantly more often in studies that used standardized criteria to determine whether a bipolar patient had comorbid migraine than in studies that used nonstandardized criteria, such as self-report.
A meta-regression analysis of data from the studies showed that mean age moderated how frequently migraine occurred among the entire sample.
“The findings of this meta-analysis suggest that the prevalence of comorbid migraine among people with [bipolar disorder] is remarkably high, particularly among people with [bipolar II disorder],” according to Dr. Michele Fornaro and Brendon Stubbs.
The results of this meta-analysis “highlighted the need for further studies focusing on [migraine-bipolar II disorder] comobidity including well-matched control cases with or without rapid cycling features too,” according to the researchers.
Read the full study in Journal of Affective Disorders (doi:http://dx.doi.org/10.1016/j.jad.2015.02.032).
FROM JOURNAL OF AFFECTIVE DISORDERS