User login
Rural Cancer Survivors Are More Likely to Have Chronic Pain
TOPLINE:
Rural cancer survivors experience significantly higher rates of chronic pain at 43.0% than those among urban survivors at 33.5%. Even after controlling for demographics and health conditions, rural residents showed 21% higher odds of experiencing chronic pain.
METHODOLOGY:
- Chronic pain prevalence among cancer survivors is twice that of the general US population and is associated with numerous negative outcomes. Rural residence is frequently linked to debilitating long-term survivorship effects, and current data lack information on whether chronic pain disparity exists specifically for rural cancer survivors.
- Researchers pooled data from the 2019–2021 and 2023 National Health Interview Survey, a cross–sectional survey conducted by the National Center for Health Statistics.
- Analysis included 5542 adult cancer survivors diagnosed within the previous 5 years, with 51.6% female participants and 48.4% male participants.
- Chronic pain was defined as pain experienced on most or all days over the past 3 months, following National Center for Health Statistics conventions.
- Rural residence classification was based on noncore or nonmetropolitan counties using the modified National Center for Health Statistics Urban–Rural Classification Scheme for Counties.
TAKEAWAY:
- Rural cancer survivors showed significantly higher odds of experiencing chronic pain compared with urban survivors (odds ratio [OR], 1.21; 95% CI, 1.01-1.45).
- Rural survivors were more likely to be non–Hispanic White, have less than a 4-year college degree, have an income below 200% of the federal poverty level, and have slightly more chronic health conditions.
- Having an income below 100% of the federal poverty level was associated with doubled odds of chronic pain (OR, 2.07; 95% CI, 1.54-2.77) compared with having an income at least four times the federal poverty level.
- Each additional health condition increased the odds of experiencing chronic pain by 32% (OR, 1.32; 95% CI, 1.26-1.39).
IN PRACTICE:
“Policymakers and health systems should work to close this gap by increasing the availability of pain management resources for rural cancer survivors. Approaches could include innovative payment models for integrative medicine in rural areas or supporting rural clinician access to pain specialists,” the authors of the study wrote.
SOURCE:
This study was led by Hyojin Choi, PhD, Department of Family Medicine, The Robert Larner MD College of Medicine, University of Vermont in Burlington, Vermont. It was published online in JAMA Network Open.
LIMITATIONS:
The authors note that the cross–sectional design of the study and limited information on individual respondents’ use of multimodal pain treatment options constrain the interpretation of findings.
DISCLOSURES:
The authors did not report any relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
Rural cancer survivors experience significantly higher rates of chronic pain at 43.0% than those among urban survivors at 33.5%. Even after controlling for demographics and health conditions, rural residents showed 21% higher odds of experiencing chronic pain.
METHODOLOGY:
- Chronic pain prevalence among cancer survivors is twice that of the general US population and is associated with numerous negative outcomes. Rural residence is frequently linked to debilitating long-term survivorship effects, and current data lack information on whether chronic pain disparity exists specifically for rural cancer survivors.
- Researchers pooled data from the 2019–2021 and 2023 National Health Interview Survey, a cross–sectional survey conducted by the National Center for Health Statistics.
- Analysis included 5542 adult cancer survivors diagnosed within the previous 5 years, with 51.6% female participants and 48.4% male participants.
- Chronic pain was defined as pain experienced on most or all days over the past 3 months, following National Center for Health Statistics conventions.
- Rural residence classification was based on noncore or nonmetropolitan counties using the modified National Center for Health Statistics Urban–Rural Classification Scheme for Counties.
TAKEAWAY:
- Rural cancer survivors showed significantly higher odds of experiencing chronic pain compared with urban survivors (odds ratio [OR], 1.21; 95% CI, 1.01-1.45).
- Rural survivors were more likely to be non–Hispanic White, have less than a 4-year college degree, have an income below 200% of the federal poverty level, and have slightly more chronic health conditions.
- Having an income below 100% of the federal poverty level was associated with doubled odds of chronic pain (OR, 2.07; 95% CI, 1.54-2.77) compared with having an income at least four times the federal poverty level.
- Each additional health condition increased the odds of experiencing chronic pain by 32% (OR, 1.32; 95% CI, 1.26-1.39).
IN PRACTICE:
“Policymakers and health systems should work to close this gap by increasing the availability of pain management resources for rural cancer survivors. Approaches could include innovative payment models for integrative medicine in rural areas or supporting rural clinician access to pain specialists,” the authors of the study wrote.
SOURCE:
This study was led by Hyojin Choi, PhD, Department of Family Medicine, The Robert Larner MD College of Medicine, University of Vermont in Burlington, Vermont. It was published online in JAMA Network Open.
LIMITATIONS:
The authors note that the cross–sectional design of the study and limited information on individual respondents’ use of multimodal pain treatment options constrain the interpretation of findings.
DISCLOSURES:
The authors did not report any relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
Rural cancer survivors experience significantly higher rates of chronic pain at 43.0% than those among urban survivors at 33.5%. Even after controlling for demographics and health conditions, rural residents showed 21% higher odds of experiencing chronic pain.
METHODOLOGY:
- Chronic pain prevalence among cancer survivors is twice that of the general US population and is associated with numerous negative outcomes. Rural residence is frequently linked to debilitating long-term survivorship effects, and current data lack information on whether chronic pain disparity exists specifically for rural cancer survivors.
- Researchers pooled data from the 2019–2021 and 2023 National Health Interview Survey, a cross–sectional survey conducted by the National Center for Health Statistics.
- Analysis included 5542 adult cancer survivors diagnosed within the previous 5 years, with 51.6% female participants and 48.4% male participants.
- Chronic pain was defined as pain experienced on most or all days over the past 3 months, following National Center for Health Statistics conventions.
- Rural residence classification was based on noncore or nonmetropolitan counties using the modified National Center for Health Statistics Urban–Rural Classification Scheme for Counties.
TAKEAWAY:
- Rural cancer survivors showed significantly higher odds of experiencing chronic pain compared with urban survivors (odds ratio [OR], 1.21; 95% CI, 1.01-1.45).
- Rural survivors were more likely to be non–Hispanic White, have less than a 4-year college degree, have an income below 200% of the federal poverty level, and have slightly more chronic health conditions.
- Having an income below 100% of the federal poverty level was associated with doubled odds of chronic pain (OR, 2.07; 95% CI, 1.54-2.77) compared with having an income at least four times the federal poverty level.
- Each additional health condition increased the odds of experiencing chronic pain by 32% (OR, 1.32; 95% CI, 1.26-1.39).
IN PRACTICE:
“Policymakers and health systems should work to close this gap by increasing the availability of pain management resources for rural cancer survivors. Approaches could include innovative payment models for integrative medicine in rural areas or supporting rural clinician access to pain specialists,” the authors of the study wrote.
SOURCE:
This study was led by Hyojin Choi, PhD, Department of Family Medicine, The Robert Larner MD College of Medicine, University of Vermont in Burlington, Vermont. It was published online in JAMA Network Open.
LIMITATIONS:
The authors note that the cross–sectional design of the study and limited information on individual respondents’ use of multimodal pain treatment options constrain the interpretation of findings.
DISCLOSURES:
The authors did not report any relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
NICE Endorses Chemo-Free First-Line Options for EGFR NSCLC
NICE Endorses Chemo-Free First-Line Options for EGFR NSCLC
The National Institute for Health and Care Excellence (NICE) has recommended amivantamab (Rybrevant) plus lazertinib (Lazcluze) as a first-line option for adults with previously untreated advanced non–small-cell lung cancer (NSCLC) harboring epidermal growth factor receptor (EGFR) exon 19 deletions or exon 21 L858R substitution mutations.
In final draft guidance, NICE said the combination therapy should be funded by the NHS in England for eligible patients when it is the most appropriate option. Around 1115 people are expected to benefit.
Lung cancer is the third most common cancer and the leading cause of cancer mortality in the UK. It accounted for 10% of all new cancer diagnoses and 20% of cancer deaths in 2020. Approximately 31,000 people received NSCLC diagnoses in England in 2021, comprising 91% of all lung cancer cases. EGFR mutation-positive NSCLC is more common in women, non-smokers, and individuals from Asian ethnic backgrounds.
Welcoming the decision, Virginia Harrison, research trustee, EGFR+ UK, said, “This is a meaningful advance for patients and their families facing this diagnosis. [It] provides something the EGFR community urgently needs: more choice in first-line treatment.”
How Practice May Shift
The recommendation adds an alternative to existing standards, including osimertinib monotherapy or osimertinib plus pemetrexed/platinum-based chemotherapy. Clinical specialists noted that no single standard care exists for this patient group.
Younger patients and those willing to accept greater side effects may choose between amivantamab plus lazertinib or osimertinib plus chemotherapy. Patients older than 80 years might prefer osimertinib monotherapy due to adverse event considerations.
Mechanism of Action and Clinical Evidence
Amivantamab is a bispecific antibody that simultaneously binds EGFR and mesenchymal-epithelial transition receptors, blocking downstream signaling pathways that drive tumor growth and promoting immune-mediated cancer cell killing. Lazertinib is an oral third-generation EGFR TKI that selectively inhibits mutant EGFR signaling. Together, the agents provides complementary suppression of EGFR-driven tumour growth and resistance mechanisms.
The NICE recommendation is supported by results from the phase 3 MARIPOSA trial, which met its primary endpoint of progression-free survival (PFS). Treatment with amivantamab plus lazertinib significantly prolonged median PFS to 23.7 months compared with 16.6 months with osimertinib. The combination also demonstrated a significant improvement in overall survival, reducing the risk for death by 25% vs osimertinib. Median OS was not reached in the combination arm and was 36.7 months with osimertinib.
The most common adverse reactions with the combination included rash, nail toxicity, hypoalbuminaemia, hepatotoxicity, and stomatitis.
A Medicines and Healthcare products Regulatory Agency-approved subcutaneous formulation of amivantamab, authorized after the committee’s initial meeting, may further improve tolerability and convenience. Administration-related reactions occurred in 63% of patients with the intravenous formulation vs 14% with the subcutaneous formulation. Clinicians expect subcutaneous dosing to replace intravenous use in practice.
Dosing, Access, and Implementation
Amivantamab is administered every 2 weeks, either intravenously or subcutaneously. Lazertinib is taken as a daily oral tablet.
Rybrevant costs £1079 for a 350-mg per 7-mL vial. Lazcluze is priced at £4128.50 for 56 x 80-mg tablets and £6192.75 for 28 x 240-mg tablets. Confidential NHS discounts are available through simple patient access schemes.
Integrated care boards, NHS England, and local authorities must implement the guidance within 90 days of publication. For drugs receiving positive draft recommendations for routine commissioning, interim funding becomes accessible from the Cancer Drugs Fund budget starting from the point of marketing authorisation or publication of draft guidance.
The National Institute for Health and Care Excellence (NICE) has recommended amivantamab (Rybrevant) plus lazertinib (Lazcluze) as a first-line option for adults with previously untreated advanced non–small-cell lung cancer (NSCLC) harboring epidermal growth factor receptor (EGFR) exon 19 deletions or exon 21 L858R substitution mutations.
In final draft guidance, NICE said the combination therapy should be funded by the NHS in England for eligible patients when it is the most appropriate option. Around 1115 people are expected to benefit.
Lung cancer is the third most common cancer and the leading cause of cancer mortality in the UK. It accounted for 10% of all new cancer diagnoses and 20% of cancer deaths in 2020. Approximately 31,000 people received NSCLC diagnoses in England in 2021, comprising 91% of all lung cancer cases. EGFR mutation-positive NSCLC is more common in women, non-smokers, and individuals from Asian ethnic backgrounds.
Welcoming the decision, Virginia Harrison, research trustee, EGFR+ UK, said, “This is a meaningful advance for patients and their families facing this diagnosis. [It] provides something the EGFR community urgently needs: more choice in first-line treatment.”
How Practice May Shift
The recommendation adds an alternative to existing standards, including osimertinib monotherapy or osimertinib plus pemetrexed/platinum-based chemotherapy. Clinical specialists noted that no single standard care exists for this patient group.
Younger patients and those willing to accept greater side effects may choose between amivantamab plus lazertinib or osimertinib plus chemotherapy. Patients older than 80 years might prefer osimertinib monotherapy due to adverse event considerations.
Mechanism of Action and Clinical Evidence
Amivantamab is a bispecific antibody that simultaneously binds EGFR and mesenchymal-epithelial transition receptors, blocking downstream signaling pathways that drive tumor growth and promoting immune-mediated cancer cell killing. Lazertinib is an oral third-generation EGFR TKI that selectively inhibits mutant EGFR signaling. Together, the agents provides complementary suppression of EGFR-driven tumour growth and resistance mechanisms.
The NICE recommendation is supported by results from the phase 3 MARIPOSA trial, which met its primary endpoint of progression-free survival (PFS). Treatment with amivantamab plus lazertinib significantly prolonged median PFS to 23.7 months compared with 16.6 months with osimertinib. The combination also demonstrated a significant improvement in overall survival, reducing the risk for death by 25% vs osimertinib. Median OS was not reached in the combination arm and was 36.7 months with osimertinib.
The most common adverse reactions with the combination included rash, nail toxicity, hypoalbuminaemia, hepatotoxicity, and stomatitis.
A Medicines and Healthcare products Regulatory Agency-approved subcutaneous formulation of amivantamab, authorized after the committee’s initial meeting, may further improve tolerability and convenience. Administration-related reactions occurred in 63% of patients with the intravenous formulation vs 14% with the subcutaneous formulation. Clinicians expect subcutaneous dosing to replace intravenous use in practice.
Dosing, Access, and Implementation
Amivantamab is administered every 2 weeks, either intravenously or subcutaneously. Lazertinib is taken as a daily oral tablet.
Rybrevant costs £1079 for a 350-mg per 7-mL vial. Lazcluze is priced at £4128.50 for 56 x 80-mg tablets and £6192.75 for 28 x 240-mg tablets. Confidential NHS discounts are available through simple patient access schemes.
Integrated care boards, NHS England, and local authorities must implement the guidance within 90 days of publication. For drugs receiving positive draft recommendations for routine commissioning, interim funding becomes accessible from the Cancer Drugs Fund budget starting from the point of marketing authorisation or publication of draft guidance.
The National Institute for Health and Care Excellence (NICE) has recommended amivantamab (Rybrevant) plus lazertinib (Lazcluze) as a first-line option for adults with previously untreated advanced non–small-cell lung cancer (NSCLC) harboring epidermal growth factor receptor (EGFR) exon 19 deletions or exon 21 L858R substitution mutations.
In final draft guidance, NICE said the combination therapy should be funded by the NHS in England for eligible patients when it is the most appropriate option. Around 1115 people are expected to benefit.
Lung cancer is the third most common cancer and the leading cause of cancer mortality in the UK. It accounted for 10% of all new cancer diagnoses and 20% of cancer deaths in 2020. Approximately 31,000 people received NSCLC diagnoses in England in 2021, comprising 91% of all lung cancer cases. EGFR mutation-positive NSCLC is more common in women, non-smokers, and individuals from Asian ethnic backgrounds.
Welcoming the decision, Virginia Harrison, research trustee, EGFR+ UK, said, “This is a meaningful advance for patients and their families facing this diagnosis. [It] provides something the EGFR community urgently needs: more choice in first-line treatment.”
How Practice May Shift
The recommendation adds an alternative to existing standards, including osimertinib monotherapy or osimertinib plus pemetrexed/platinum-based chemotherapy. Clinical specialists noted that no single standard care exists for this patient group.
Younger patients and those willing to accept greater side effects may choose between amivantamab plus lazertinib or osimertinib plus chemotherapy. Patients older than 80 years might prefer osimertinib monotherapy due to adverse event considerations.
Mechanism of Action and Clinical Evidence
Amivantamab is a bispecific antibody that simultaneously binds EGFR and mesenchymal-epithelial transition receptors, blocking downstream signaling pathways that drive tumor growth and promoting immune-mediated cancer cell killing. Lazertinib is an oral third-generation EGFR TKI that selectively inhibits mutant EGFR signaling. Together, the agents provides complementary suppression of EGFR-driven tumour growth and resistance mechanisms.
The NICE recommendation is supported by results from the phase 3 MARIPOSA trial, which met its primary endpoint of progression-free survival (PFS). Treatment with amivantamab plus lazertinib significantly prolonged median PFS to 23.7 months compared with 16.6 months with osimertinib. The combination also demonstrated a significant improvement in overall survival, reducing the risk for death by 25% vs osimertinib. Median OS was not reached in the combination arm and was 36.7 months with osimertinib.
The most common adverse reactions with the combination included rash, nail toxicity, hypoalbuminaemia, hepatotoxicity, and stomatitis.
A Medicines and Healthcare products Regulatory Agency-approved subcutaneous formulation of amivantamab, authorized after the committee’s initial meeting, may further improve tolerability and convenience. Administration-related reactions occurred in 63% of patients with the intravenous formulation vs 14% with the subcutaneous formulation. Clinicians expect subcutaneous dosing to replace intravenous use in practice.
Dosing, Access, and Implementation
Amivantamab is administered every 2 weeks, either intravenously or subcutaneously. Lazertinib is taken as a daily oral tablet.
Rybrevant costs £1079 for a 350-mg per 7-mL vial. Lazcluze is priced at £4128.50 for 56 x 80-mg tablets and £6192.75 for 28 x 240-mg tablets. Confidential NHS discounts are available through simple patient access schemes.
Integrated care boards, NHS England, and local authorities must implement the guidance within 90 days of publication. For drugs receiving positive draft recommendations for routine commissioning, interim funding becomes accessible from the Cancer Drugs Fund budget starting from the point of marketing authorisation or publication of draft guidance.
NICE Endorses Chemo-Free First-Line Options for EGFR NSCLC
NICE Endorses Chemo-Free First-Line Options for EGFR NSCLC
Turning the Cancer Research Problem Into an Opportunity
Turning the Cancer Research Problem Into an Opportunity
The War on Cancer, declared by President Richard Nixon some 50 years ago, has been canceled during the second Trump administration in 2025 — so saith The New York Times Sunday magazine cover story on September 14, 2025. This war seems now to be best described as "The War on Cancer Research."
To our horror and disbelief, we've witnessed the slow but persistent drift of much of the United States citizenry away from science and the sudden and severe movement of the US government to crush much medical research. But it is not as if we were not warned.
In August 2024, on these pages and without political bias, I urged Medscape readers to pay attention to Project 2025. A great deal of what we as a population are now experiencing was laid out as a carefully constructed plan.
What is surprising is the cruel ruthlessness of the "move fast and break things" approach, taken with little apparent concern about the resultant human tragedies (workforce and patients) and no clear care about the resulting fallout. As we've now learned, destroying something as grand as our cancer research enterprise can be accomplished very quickly. Rebuilding it is certain to be slow and difficult and perhaps can never be accomplished.
In this new anti-science, anti-research, and anti-researcher reality, what can we now do?
First and foremost, we must recognize that the war on cancer is not over. Cancer is not canceled, even if much of the US government's research effort/funding has been. Those of us in medicine and public health often speak in quantification of causes of death of our populations. As such, I'll remind Medscape readers that cancer afflicts some 20 million humans worldwide each year, killing nearly 10 million. Although two-thirds of Americans diagnosed with a potentially lethal malignancy are cured, cancer still kills roughly 600,000 Americans each year. Cancer has been the second most frequent cause of death of Americans for 75 years.
Being inevitable and immutable, death itself is not the enemy. We all die. Disease, disability, pain, and human suffering are the real enemies of us all. Cancer maims, pains, diabetes, and torments some 20 million humans worldwide each year. That is a huge humanitarian problem that should be recognized by individuals of all creeds and backgrounds.
With this depletion of our domestic government basic and applied cancer research program, what can we do?
- Think globally and look to the international scientific research enterprises — relying on them, much as they have relied on us.
- Defend the universal importance of reliable and available literature on medical science.
- Continue to translate and apply the vast amount of available published research in clinical practice and publish the results.
- Urge private industries to expand their research budgets into areas of study that may not produce quickly tangible positive bottom-line results.
- Remind the Secretary of the Department of Health and Human Services (for whom chronic diseases seem paramount) that cancer is the second leading American chronic disease by morbidity.
- Redouble efforts of cancer prevention, especially urging the FDA to ban combustible tobacco and strive more diligently to decrease obesity.
- Appeal to our vast philanthropic universe to increase its funding of nonprofit organizations active in the cancer investigation, diagnosis, and management space.
One such 501c3 organization is California-based Cancer Commons. (Disclosure: I named it in 2010 and serve as its editor in chief).
A commons is a space shared by a community to use for the common interest. As we originally envisioned it, a cancer commons is an open access internet location where individuals and organizations (eg, corporations, universities, government agencies, philanthropies) will voluntarily share their data to work together to defeat the common enemy of humans: cancer.
On September 8, 2025, Cancer Commons was the 15th annual Lundberg Institute Lecturer at the Commonwealth Club of California in San Francisco. At the lecture, Cancer Commons founder (and long-term survivor of metastatic malignant melanoma), Jay Martin "Martin" Tenenbaum, PhD, spoke of the need for a cancer commons and the founder's vision. Emma Shtivelman, PhD, the long-time compassionate chief scientist, described some of the thousands of patients with advanced cancer that she has helped — all free of charge. And newly named CEO Clifford Reid, MBA, PhD, used his entrepreneurial prowess to envision an ambitious future.
Cancer Commons has always focused on patients with cancer who are beyond standards of curative care. As Cancer Commons evolves, it anticipates focusing on patients with cancer who are beyond National Comprehensive Cancer Network Guidelines. The organization intends to greatly expand its 1000 patients per year with "high touch" engagement with PhD clinical scientists to many thousands by including artificial intelligence. It plans to extend its N-of-One approach to create new knowledge — especially regarding the hundreds of drugs that are FDA-approved for use in treating cancer but have not been further assessed for the utility in actually treating patients with cancer.
The war on cancer is not over. It remains a persistent foe that causes immense disability, pain, and human suffering. With government support depleted, the burden now shifts to the private sector and philanthropic organizations, such as Cancer Commons, to serve as the new vital infrastructure in the fight for a cure. Now, we must redouble our efforts to ensure that these research endeavors are supported if the US government will not do its part.
A version of this article first appeared on Medscape.com.
The War on Cancer, declared by President Richard Nixon some 50 years ago, has been canceled during the second Trump administration in 2025 — so saith The New York Times Sunday magazine cover story on September 14, 2025. This war seems now to be best described as "The War on Cancer Research."
To our horror and disbelief, we've witnessed the slow but persistent drift of much of the United States citizenry away from science and the sudden and severe movement of the US government to crush much medical research. But it is not as if we were not warned.
In August 2024, on these pages and without political bias, I urged Medscape readers to pay attention to Project 2025. A great deal of what we as a population are now experiencing was laid out as a carefully constructed plan.
What is surprising is the cruel ruthlessness of the "move fast and break things" approach, taken with little apparent concern about the resultant human tragedies (workforce and patients) and no clear care about the resulting fallout. As we've now learned, destroying something as grand as our cancer research enterprise can be accomplished very quickly. Rebuilding it is certain to be slow and difficult and perhaps can never be accomplished.
In this new anti-science, anti-research, and anti-researcher reality, what can we now do?
First and foremost, we must recognize that the war on cancer is not over. Cancer is not canceled, even if much of the US government's research effort/funding has been. Those of us in medicine and public health often speak in quantification of causes of death of our populations. As such, I'll remind Medscape readers that cancer afflicts some 20 million humans worldwide each year, killing nearly 10 million. Although two-thirds of Americans diagnosed with a potentially lethal malignancy are cured, cancer still kills roughly 600,000 Americans each year. Cancer has been the second most frequent cause of death of Americans for 75 years.
Being inevitable and immutable, death itself is not the enemy. We all die. Disease, disability, pain, and human suffering are the real enemies of us all. Cancer maims, pains, diabetes, and torments some 20 million humans worldwide each year. That is a huge humanitarian problem that should be recognized by individuals of all creeds and backgrounds.
With this depletion of our domestic government basic and applied cancer research program, what can we do?
- Think globally and look to the international scientific research enterprises — relying on them, much as they have relied on us.
- Defend the universal importance of reliable and available literature on medical science.
- Continue to translate and apply the vast amount of available published research in clinical practice and publish the results.
- Urge private industries to expand their research budgets into areas of study that may not produce quickly tangible positive bottom-line results.
- Remind the Secretary of the Department of Health and Human Services (for whom chronic diseases seem paramount) that cancer is the second leading American chronic disease by morbidity.
- Redouble efforts of cancer prevention, especially urging the FDA to ban combustible tobacco and strive more diligently to decrease obesity.
- Appeal to our vast philanthropic universe to increase its funding of nonprofit organizations active in the cancer investigation, diagnosis, and management space.
One such 501c3 organization is California-based Cancer Commons. (Disclosure: I named it in 2010 and serve as its editor in chief).
A commons is a space shared by a community to use for the common interest. As we originally envisioned it, a cancer commons is an open access internet location where individuals and organizations (eg, corporations, universities, government agencies, philanthropies) will voluntarily share their data to work together to defeat the common enemy of humans: cancer.
On September 8, 2025, Cancer Commons was the 15th annual Lundberg Institute Lecturer at the Commonwealth Club of California in San Francisco. At the lecture, Cancer Commons founder (and long-term survivor of metastatic malignant melanoma), Jay Martin "Martin" Tenenbaum, PhD, spoke of the need for a cancer commons and the founder's vision. Emma Shtivelman, PhD, the long-time compassionate chief scientist, described some of the thousands of patients with advanced cancer that she has helped — all free of charge. And newly named CEO Clifford Reid, MBA, PhD, used his entrepreneurial prowess to envision an ambitious future.
Cancer Commons has always focused on patients with cancer who are beyond standards of curative care. As Cancer Commons evolves, it anticipates focusing on patients with cancer who are beyond National Comprehensive Cancer Network Guidelines. The organization intends to greatly expand its 1000 patients per year with "high touch" engagement with PhD clinical scientists to many thousands by including artificial intelligence. It plans to extend its N-of-One approach to create new knowledge — especially regarding the hundreds of drugs that are FDA-approved for use in treating cancer but have not been further assessed for the utility in actually treating patients with cancer.
The war on cancer is not over. It remains a persistent foe that causes immense disability, pain, and human suffering. With government support depleted, the burden now shifts to the private sector and philanthropic organizations, such as Cancer Commons, to serve as the new vital infrastructure in the fight for a cure. Now, we must redouble our efforts to ensure that these research endeavors are supported if the US government will not do its part.
A version of this article first appeared on Medscape.com.
The War on Cancer, declared by President Richard Nixon some 50 years ago, has been canceled during the second Trump administration in 2025 — so saith The New York Times Sunday magazine cover story on September 14, 2025. This war seems now to be best described as "The War on Cancer Research."
To our horror and disbelief, we've witnessed the slow but persistent drift of much of the United States citizenry away from science and the sudden and severe movement of the US government to crush much medical research. But it is not as if we were not warned.
In August 2024, on these pages and without political bias, I urged Medscape readers to pay attention to Project 2025. A great deal of what we as a population are now experiencing was laid out as a carefully constructed plan.
What is surprising is the cruel ruthlessness of the "move fast and break things" approach, taken with little apparent concern about the resultant human tragedies (workforce and patients) and no clear care about the resulting fallout. As we've now learned, destroying something as grand as our cancer research enterprise can be accomplished very quickly. Rebuilding it is certain to be slow and difficult and perhaps can never be accomplished.
In this new anti-science, anti-research, and anti-researcher reality, what can we now do?
First and foremost, we must recognize that the war on cancer is not over. Cancer is not canceled, even if much of the US government's research effort/funding has been. Those of us in medicine and public health often speak in quantification of causes of death of our populations. As such, I'll remind Medscape readers that cancer afflicts some 20 million humans worldwide each year, killing nearly 10 million. Although two-thirds of Americans diagnosed with a potentially lethal malignancy are cured, cancer still kills roughly 600,000 Americans each year. Cancer has been the second most frequent cause of death of Americans for 75 years.
Being inevitable and immutable, death itself is not the enemy. We all die. Disease, disability, pain, and human suffering are the real enemies of us all. Cancer maims, pains, diabetes, and torments some 20 million humans worldwide each year. That is a huge humanitarian problem that should be recognized by individuals of all creeds and backgrounds.
With this depletion of our domestic government basic and applied cancer research program, what can we do?
- Think globally and look to the international scientific research enterprises — relying on them, much as they have relied on us.
- Defend the universal importance of reliable and available literature on medical science.
- Continue to translate and apply the vast amount of available published research in clinical practice and publish the results.
- Urge private industries to expand their research budgets into areas of study that may not produce quickly tangible positive bottom-line results.
- Remind the Secretary of the Department of Health and Human Services (for whom chronic diseases seem paramount) that cancer is the second leading American chronic disease by morbidity.
- Redouble efforts of cancer prevention, especially urging the FDA to ban combustible tobacco and strive more diligently to decrease obesity.
- Appeal to our vast philanthropic universe to increase its funding of nonprofit organizations active in the cancer investigation, diagnosis, and management space.
One such 501c3 organization is California-based Cancer Commons. (Disclosure: I named it in 2010 and serve as its editor in chief).
A commons is a space shared by a community to use for the common interest. As we originally envisioned it, a cancer commons is an open access internet location where individuals and organizations (eg, corporations, universities, government agencies, philanthropies) will voluntarily share their data to work together to defeat the common enemy of humans: cancer.
On September 8, 2025, Cancer Commons was the 15th annual Lundberg Institute Lecturer at the Commonwealth Club of California in San Francisco. At the lecture, Cancer Commons founder (and long-term survivor of metastatic malignant melanoma), Jay Martin "Martin" Tenenbaum, PhD, spoke of the need for a cancer commons and the founder's vision. Emma Shtivelman, PhD, the long-time compassionate chief scientist, described some of the thousands of patients with advanced cancer that she has helped — all free of charge. And newly named CEO Clifford Reid, MBA, PhD, used his entrepreneurial prowess to envision an ambitious future.
Cancer Commons has always focused on patients with cancer who are beyond standards of curative care. As Cancer Commons evolves, it anticipates focusing on patients with cancer who are beyond National Comprehensive Cancer Network Guidelines. The organization intends to greatly expand its 1000 patients per year with "high touch" engagement with PhD clinical scientists to many thousands by including artificial intelligence. It plans to extend its N-of-One approach to create new knowledge — especially regarding the hundreds of drugs that are FDA-approved for use in treating cancer but have not been further assessed for the utility in actually treating patients with cancer.
The war on cancer is not over. It remains a persistent foe that causes immense disability, pain, and human suffering. With government support depleted, the burden now shifts to the private sector and philanthropic organizations, such as Cancer Commons, to serve as the new vital infrastructure in the fight for a cure. Now, we must redouble our efforts to ensure that these research endeavors are supported if the US government will not do its part.
A version of this article first appeared on Medscape.com.
Turning the Cancer Research Problem Into an Opportunity
Turning the Cancer Research Problem Into an Opportunity
Impact of Retroactive Application of Updated Surveillance Guidelines on Endoscopy Center Capacity at a Large VA Health Care System
Impact of Retroactive Application of Updated Surveillance Guidelines on Endoscopy Center Capacity at a Large VA Health Care System
In 2020, the US Multi-Society Task Force (USMSTF) on Colorectal Cancer (CRC) increased the recommended colon polyp surveillance interval for 1 to 2 subcentimeter tubular adenomas from 5 to 10 years to 7 to 10 years.1 This change was prompted by emerging research indicating that rates of CRC and advanced neoplasia among patients with a history of only 1 to 2 subcentimeter tubular adenomas are lower than initially estimated.2,3 This extension provides an opportunity to increase endoscopy capacity and improve access to colonoscopies by retroactively applying the 2020 guidelines to surveillance interval recommendations made before their introduction. For example, based on the updated guidelines, patients previously recommended to undergo colon polyp surveillance colonoscopy 5 years after an index colonoscopy could extend their surveillance interval by 2 to 5 years. Increasing endoscopic capacity could address the growing demand for colonoscopies from new screening guidelines that reduced the age of initial CRC screening from 50 years to 45 years and the backlog of procedures due to COVID-19 restrictions.4
As part of a project to increase endoscopic capacity at the US Department of Veterans Affairs (VA) Pittsburgh Healthcare System (VAPHS), this study assessed the potential impact of retroactively applying the 2020 USMSTF polyp surveillance guidelines on endoscopic capacity. These results may be informative for other VA and private-sector health care systems seeking to identify strategies to improve endoscopy capacity.
Methods
VAPHS is an integrated health care system in the Veterans Health Administration (VHA) serving 85,000 patients across 8 health care institutions in Pennsylvania, Ohio, and West Virginia. VAPHS manages colorectal screening recommendations for patients receiving medical care in the health care system regardless of whether their prior colonoscopy was performed at VAPHS or external facilities. The VA maintains a national CRC screening and surveillance electronic medical record reminder that prompts health care practitioners to order colon polyp surveillance based on interval recommendations from the index colonoscopy. This study reviewed all patients from the VAPHS panel with a reminder to undergo colonoscopy for screening for CRC or surveillance of colon polyps within 12 months from September 1, 2022.
Among patients with a reminder, 3 investigators reviewed index colonoscopy and pathology reports to identify CRC risk category, colonoscopy indication, procedural quality, and recommended repeat colonoscopy interval. Per the USMSTF guidelines, patients with incomplete colonoscopy or pathology records, high-risk indications (ie, personal history of inflammatory bowel disease, personal history of CRC, or family history of CRC), or inadequate bowel preparation (Boston Bowel Preparation Score < 6) were excluded. Additionally, patients who had CRC screening or surveillance discontinued due to age or comorbidities, had completed a subsequent follow-up colonoscopy, or were deceased at the time of review were excluded.
Retroactive Interval Reclassification
Among eligible patients, this study compared the repeat colonoscopy interval recommended by the prior endoscopist with those from the 2020 USMSTF guidelines. In cases where the interval was documented as a range of years, the lower end was considered the recommendation. Similarly, the lower end of the range from the 2020 USMSTF guidelines was used for the reclassified surveillance interval. Years extended per patient were quantified relative to September 1, 2023 (ie, 1 year after the review date). For example, if the index colonoscopy was completed on September 1, 2016, the initial surveillance recommendation was 5 years, and the reclassified recommendation was 7 years, the interval extension beyond September 1, 2023, was 0 years.
Furthermore, because index surveillance recommendations are not always guideline concordant, the years extended per patient were calculated by harmonizing the index endoscopist’s recommendations with the guidelines at the time of the index colonoscopy.5 For example, if the index colonoscopy was completed on September 1, 2018, and the endoscopist recommended a 5-year follow-up for a patient with average risk for CRC, adequate bowel preparation, and no colorectal polyps, that patient is eligible to extend their colonoscopy to September 1, 2028, based on guideline recommendations at the time of index endoscopy recommending that the next colonoscopy occur in 10 years. In this analysis the 2012 USMSTF guidelines were applied to all index colonoscopies completed in 2021 or earlier to allow time for adoption of the 2020 guidelines.
This project fulfilled a facility mandate to increase capacity to conduct endoscopic procedures. Institutional review board approval was not required by VAPHS policy relating to clinical operations projects. Approval for publication of clinical operations activity was obtained from the VAPHS facility director.
Results
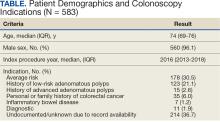
Within 1 year of the September 1, 2022, review date, 637 patients receiving care at VAPHS had clinical reminders for an upcoming colonoscopy. Of these, 54 (8.4%) were already up to date or were deceased at the time of review. Of the 583 eligible patients, 96% were male, the median age was 74 years, the median index colonoscopy year was 2016, and 178 (30.5%) had an average-risk CRC screening indication at the index colonoscopy (Table).
Of the 583 patients due for colonoscopy, 331 (56.7%) had both colonoscopy and pathology reports available. The majority of those with incomplete records had the index colonoscopy completed outside VAPHS. Among these patients, 222 (67.0%) had adequate bowel preparation. Of those with adequate bowel preparation, 43 were not eligible for interval extension because of high-risk conditions and 13 were not eligible because there was no index surveillance interval recommendation from the index endoscopist. Of the patients due for colonoscopy, 166 (28.4%) were potentially eligible for surveillance interval extension (Figure).
Sixty-five (39.2%) of the 166 patients had 1 to 2 subcentimeter tubular adenomas on their index colonoscopy. Sixty-two patients were eligible for interval extension to 7 years, but this only resulted in ≥ 1 year of extension beyond the review date for 36 (6% of all 583 patients due for colonoscopy). The 36 patients were extended 63 years. By harmonizing the index endoscopists’ surveillance interval recommendation with the guideline at the time of the index colonoscopy, 29 additional patients could have their colonoscopy extended by ≥ 1 year. Harmonization extended colonoscopy intervals by 93 years. Retroactively applying the 2020 USMSTF polyp surveillance guidelines and harmonizing recommendations to guidelines extended the time of index colonoscopy by 153 years.
Discussion
With retroactive application of the 2020 USMSTF polyp surveillance guidelines, 6% of patients due for an upcoming colonoscopy could extend their follow-up by ≥ 1 year by extending the surveillance interval for 1 to 2 subcentimeter tubular adenomas to 7 years. An additional 5% of patients could extend their interval by harmonizing the index endoscopist’s interval recommendation with polyp surveillance guidelines at the time of the index colonoscopy. These findings are consistent with the results of 2 studies that demonstrated that about 14% of patients due for colonoscopy could have their interval extended.6,7 The current study enhances those insights by separating the contribution of 2020 USMSTF polyp surveillance guidelines from the contribution of harmonizing surveillance intervals with guidelines for other polyp histologies. This study found that there is an opportunity to improve endoscopic capacity by harmonizing recommendations with guidelines. This complements a 2023 study showing that even when knowledgeable about guidelines, clinicians do not necessarily follow recommendations.8 While this and previous research have identified that 11% to 14% of patients are eligible for extension, these individuals would also have to be willing to have their polyp surveillance intervals extended for there to be a real-world impact on endoscopic capacity. A 2024 study found that only 19% to 37% of patients with 1 to 2 small tubular adenomas were willing to have polyps surveillance interval extension.9 This suggests the actual effect on capacity may be even lower than reported.
Limitations
The overall impact of the 2020 USMSTF polyp surveillance guidelines on endoscopic capacity was blunted by the high prevalence of incomplete index colonoscopy records among the study population. Without data on bowel preparation quality or procedure indications, this study could not assess whether 43% of patients were eligible for surveillance interval extension. Most index colonoscopies with incomplete documentation were completed at community-care gastroenterology facilities. This high rate of incomplete documentation is likely generalizable to other VA health care systems—especially in the era of the Veterans Access, Choice, and Accountability Act of 2014, which increased veteran access to non-VA community care.10 Veterans due for colon polyp surveillance colonoscopies are more likely to have had their prior colonoscopy in community care compared with prior eras.11 Furthermore, because the VHA is among the most established integrated health care systems offering primary and subspecialty care in the US, private sector health care systems may have even greater rates of care fragmentation for longitudinal CRC screening and colon polyp surveillance, as these systems have only begun to regionally integrate recently.12,13
Another limitation is that nearly one-third of the individuals with documentation had inadequate bowel preparation for surveillance recommendations. This results in shorter surveillance follow-up colonoscopies and increases downstream demand for future colonoscopies. The low yield of extending colon polyp surveillance interval in this study emphasizes that improved efforts to obtain colonoscopy and pathology reports from community care, right-sizing the colon polyp surveillance intervals recommended by endoscopists, and improving quality of bowel preparation could have downstream health care system benefits in the future. These efforts could increase colonoscopy capacity at VA health care systems, thereby shortening colonoscopy wait times, decreasing fragmentation of care, and increasing the number of veterans who receive high-quality colonoscopies at VA health care systems.14
Conclusions
Eleven percent of patients in this study due for a colonoscopy could extend their follow-up by ≥ 1 year. About half of these extensions were directly due to the 2020 USMSTF polyp surveillance interval extension for 1 to 2 subcentimeter tubular adenomas. The rest resulted from harmonizing recommendations with guidelines at the time of the procedure. To determine whether retroactively applying polyp surveillance guidelines to follow-up interval recommendations will result in improved endoscopic capacity, health care system administrators should consider the degree of CRC screening care fragmentation in their patient population. Greater long-term gains in endoscopic capacity may be achieved by proactively supporting endoscopists in making guideline-concordant screening recommendations at the time of colonoscopy.
Gupta S, Lieberman D, Anderson JC, et al. Recommendations for follow-up after colonoscopy and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc. 2020;91:463-485. doi:10.1016/j.gie.2020.01.014
Dubé C, Yakubu M, McCurdy BR, et al. Risk of advanced adenoma, colorectal cancer, and colorectal cancer mortality in people with low-risk adenomas at baseline colonoscopy: a systematic review and meta-analysis. Am J Gastroenterol. 2017;112:1790-1801. doi:10.1038/ajg.2017.360
Click B, Pinsky PF, Hickey T, Doroudi M, Shoen RE. Association of colonoscopy adenoma findings with long-term colorectal cancer incidence. JAMA. 2018;319:2021-2031. doi:10.1001/jama.2018.5809
US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2021;325:1965-1977. doi:10.1001/jama.2021.6238
Djinbachian R, Dubé AJ, Durand M, et al. Adherence to post-polypectomy surveillance guidelines: a systematic review and meta-analysis. Endoscopy. 2019;51:673-683. doi:10.1055/a-0865-2082
Gawron AJ, Kaltenbach T, Dominitz JA. The impact of the coronavirus disease-19 pandemic on access to endoscopy procedures in the VA healthcare system. Gastroenterology. 2020;159:1216-1220.e1. doi:10.1053/j.gastro.2020.07.033
Xiao AH, Chang SY, Stevoff CG, Komanduri S, Pandolfino JE, Keswani RN. Adoption of multi-society guidelines facilitates value-based reduction in screening and surveillance colonoscopy volume during COVID-19 pandemic. Dig Dis Sci. 2021;66:2578-2584. doi:10.1007/s10620-020-06539-1
Dong J, Wang LF, Ardolino E, Feuerstein JD. Real-world compliance with the 2020 U.S. Multi-Society Task Force on Colorectal Cancer polypectomy surveillance guidelines: an observational study. Gastrointest Endosc. 2023;97:350-356.e3. doi:10.1016/j.gie.2022.08.020
Lee JK, Koripella PC, Jensen CD, et al. Randomized trial of patient outreach approaches to de-implement outdated colonoscopy surveillance intervals. Clin Gastroenterol Hepatol. 2024;22:1315-1322.e7. doi:10.1016/j.cgh.2023.12.027
Veterans Access, Choice, and Accountability Act of 2014, HR 3230, 113th Cong (2014). Accessed September 8, 2025. https://www.congress.gov/bill/113th-congress/house-bill/3230
Dueker JM, Khalid A. Performance of the Veterans Choice Program for improving access to colonoscopy at a tertiary VA facility. Fed Pract. 2020;37:224-228.
Oliver A. The Veterans Health Administration: an American success story? Milbank Q. 2007;85:5-35. doi:10.1111/j.1468-0009.2007.00475.x
Furukawa MF, Machta RM, Barrett KA, et al. Landscape of health systems in the United States. Med Care Res Rev. 2020;77:357-366. doi:10.1177/1077558718823130
Petros V, Tsambikos E, Madhoun M, Tierney WM. Impact of community referral on colonoscopy quality metrics in a Veterans Affairs Medical Center. Clin Transl Gastroenterol. 2022;13:e00460. doi:10.14309/ctg.0000000000000460
In 2020, the US Multi-Society Task Force (USMSTF) on Colorectal Cancer (CRC) increased the recommended colon polyp surveillance interval for 1 to 2 subcentimeter tubular adenomas from 5 to 10 years to 7 to 10 years.1 This change was prompted by emerging research indicating that rates of CRC and advanced neoplasia among patients with a history of only 1 to 2 subcentimeter tubular adenomas are lower than initially estimated.2,3 This extension provides an opportunity to increase endoscopy capacity and improve access to colonoscopies by retroactively applying the 2020 guidelines to surveillance interval recommendations made before their introduction. For example, based on the updated guidelines, patients previously recommended to undergo colon polyp surveillance colonoscopy 5 years after an index colonoscopy could extend their surveillance interval by 2 to 5 years. Increasing endoscopic capacity could address the growing demand for colonoscopies from new screening guidelines that reduced the age of initial CRC screening from 50 years to 45 years and the backlog of procedures due to COVID-19 restrictions.4
As part of a project to increase endoscopic capacity at the US Department of Veterans Affairs (VA) Pittsburgh Healthcare System (VAPHS), this study assessed the potential impact of retroactively applying the 2020 USMSTF polyp surveillance guidelines on endoscopic capacity. These results may be informative for other VA and private-sector health care systems seeking to identify strategies to improve endoscopy capacity.
Methods
VAPHS is an integrated health care system in the Veterans Health Administration (VHA) serving 85,000 patients across 8 health care institutions in Pennsylvania, Ohio, and West Virginia. VAPHS manages colorectal screening recommendations for patients receiving medical care in the health care system regardless of whether their prior colonoscopy was performed at VAPHS or external facilities. The VA maintains a national CRC screening and surveillance electronic medical record reminder that prompts health care practitioners to order colon polyp surveillance based on interval recommendations from the index colonoscopy. This study reviewed all patients from the VAPHS panel with a reminder to undergo colonoscopy for screening for CRC or surveillance of colon polyps within 12 months from September 1, 2022.
Among patients with a reminder, 3 investigators reviewed index colonoscopy and pathology reports to identify CRC risk category, colonoscopy indication, procedural quality, and recommended repeat colonoscopy interval. Per the USMSTF guidelines, patients with incomplete colonoscopy or pathology records, high-risk indications (ie, personal history of inflammatory bowel disease, personal history of CRC, or family history of CRC), or inadequate bowel preparation (Boston Bowel Preparation Score < 6) were excluded. Additionally, patients who had CRC screening or surveillance discontinued due to age or comorbidities, had completed a subsequent follow-up colonoscopy, or were deceased at the time of review were excluded.
Retroactive Interval Reclassification
Among eligible patients, this study compared the repeat colonoscopy interval recommended by the prior endoscopist with those from the 2020 USMSTF guidelines. In cases where the interval was documented as a range of years, the lower end was considered the recommendation. Similarly, the lower end of the range from the 2020 USMSTF guidelines was used for the reclassified surveillance interval. Years extended per patient were quantified relative to September 1, 2023 (ie, 1 year after the review date). For example, if the index colonoscopy was completed on September 1, 2016, the initial surveillance recommendation was 5 years, and the reclassified recommendation was 7 years, the interval extension beyond September 1, 2023, was 0 years.
Furthermore, because index surveillance recommendations are not always guideline concordant, the years extended per patient were calculated by harmonizing the index endoscopist’s recommendations with the guidelines at the time of the index colonoscopy.5 For example, if the index colonoscopy was completed on September 1, 2018, and the endoscopist recommended a 5-year follow-up for a patient with average risk for CRC, adequate bowel preparation, and no colorectal polyps, that patient is eligible to extend their colonoscopy to September 1, 2028, based on guideline recommendations at the time of index endoscopy recommending that the next colonoscopy occur in 10 years. In this analysis the 2012 USMSTF guidelines were applied to all index colonoscopies completed in 2021 or earlier to allow time for adoption of the 2020 guidelines.
This project fulfilled a facility mandate to increase capacity to conduct endoscopic procedures. Institutional review board approval was not required by VAPHS policy relating to clinical operations projects. Approval for publication of clinical operations activity was obtained from the VAPHS facility director.
Results
Within 1 year of the September 1, 2022, review date, 637 patients receiving care at VAPHS had clinical reminders for an upcoming colonoscopy. Of these, 54 (8.4%) were already up to date or were deceased at the time of review. Of the 583 eligible patients, 96% were male, the median age was 74 years, the median index colonoscopy year was 2016, and 178 (30.5%) had an average-risk CRC screening indication at the index colonoscopy (Table).
Of the 583 patients due for colonoscopy, 331 (56.7%) had both colonoscopy and pathology reports available. The majority of those with incomplete records had the index colonoscopy completed outside VAPHS. Among these patients, 222 (67.0%) had adequate bowel preparation. Of those with adequate bowel preparation, 43 were not eligible for interval extension because of high-risk conditions and 13 were not eligible because there was no index surveillance interval recommendation from the index endoscopist. Of the patients due for colonoscopy, 166 (28.4%) were potentially eligible for surveillance interval extension (Figure).
Sixty-five (39.2%) of the 166 patients had 1 to 2 subcentimeter tubular adenomas on their index colonoscopy. Sixty-two patients were eligible for interval extension to 7 years, but this only resulted in ≥ 1 year of extension beyond the review date for 36 (6% of all 583 patients due for colonoscopy). The 36 patients were extended 63 years. By harmonizing the index endoscopists’ surveillance interval recommendation with the guideline at the time of the index colonoscopy, 29 additional patients could have their colonoscopy extended by ≥ 1 year. Harmonization extended colonoscopy intervals by 93 years. Retroactively applying the 2020 USMSTF polyp surveillance guidelines and harmonizing recommendations to guidelines extended the time of index colonoscopy by 153 years.
Discussion
With retroactive application of the 2020 USMSTF polyp surveillance guidelines, 6% of patients due for an upcoming colonoscopy could extend their follow-up by ≥ 1 year by extending the surveillance interval for 1 to 2 subcentimeter tubular adenomas to 7 years. An additional 5% of patients could extend their interval by harmonizing the index endoscopist’s interval recommendation with polyp surveillance guidelines at the time of the index colonoscopy. These findings are consistent with the results of 2 studies that demonstrated that about 14% of patients due for colonoscopy could have their interval extended.6,7 The current study enhances those insights by separating the contribution of 2020 USMSTF polyp surveillance guidelines from the contribution of harmonizing surveillance intervals with guidelines for other polyp histologies. This study found that there is an opportunity to improve endoscopic capacity by harmonizing recommendations with guidelines. This complements a 2023 study showing that even when knowledgeable about guidelines, clinicians do not necessarily follow recommendations.8 While this and previous research have identified that 11% to 14% of patients are eligible for extension, these individuals would also have to be willing to have their polyp surveillance intervals extended for there to be a real-world impact on endoscopic capacity. A 2024 study found that only 19% to 37% of patients with 1 to 2 small tubular adenomas were willing to have polyps surveillance interval extension.9 This suggests the actual effect on capacity may be even lower than reported.
Limitations
The overall impact of the 2020 USMSTF polyp surveillance guidelines on endoscopic capacity was blunted by the high prevalence of incomplete index colonoscopy records among the study population. Without data on bowel preparation quality or procedure indications, this study could not assess whether 43% of patients were eligible for surveillance interval extension. Most index colonoscopies with incomplete documentation were completed at community-care gastroenterology facilities. This high rate of incomplete documentation is likely generalizable to other VA health care systems—especially in the era of the Veterans Access, Choice, and Accountability Act of 2014, which increased veteran access to non-VA community care.10 Veterans due for colon polyp surveillance colonoscopies are more likely to have had their prior colonoscopy in community care compared with prior eras.11 Furthermore, because the VHA is among the most established integrated health care systems offering primary and subspecialty care in the US, private sector health care systems may have even greater rates of care fragmentation for longitudinal CRC screening and colon polyp surveillance, as these systems have only begun to regionally integrate recently.12,13
Another limitation is that nearly one-third of the individuals with documentation had inadequate bowel preparation for surveillance recommendations. This results in shorter surveillance follow-up colonoscopies and increases downstream demand for future colonoscopies. The low yield of extending colon polyp surveillance interval in this study emphasizes that improved efforts to obtain colonoscopy and pathology reports from community care, right-sizing the colon polyp surveillance intervals recommended by endoscopists, and improving quality of bowel preparation could have downstream health care system benefits in the future. These efforts could increase colonoscopy capacity at VA health care systems, thereby shortening colonoscopy wait times, decreasing fragmentation of care, and increasing the number of veterans who receive high-quality colonoscopies at VA health care systems.14
Conclusions
Eleven percent of patients in this study due for a colonoscopy could extend their follow-up by ≥ 1 year. About half of these extensions were directly due to the 2020 USMSTF polyp surveillance interval extension for 1 to 2 subcentimeter tubular adenomas. The rest resulted from harmonizing recommendations with guidelines at the time of the procedure. To determine whether retroactively applying polyp surveillance guidelines to follow-up interval recommendations will result in improved endoscopic capacity, health care system administrators should consider the degree of CRC screening care fragmentation in their patient population. Greater long-term gains in endoscopic capacity may be achieved by proactively supporting endoscopists in making guideline-concordant screening recommendations at the time of colonoscopy.
In 2020, the US Multi-Society Task Force (USMSTF) on Colorectal Cancer (CRC) increased the recommended colon polyp surveillance interval for 1 to 2 subcentimeter tubular adenomas from 5 to 10 years to 7 to 10 years.1 This change was prompted by emerging research indicating that rates of CRC and advanced neoplasia among patients with a history of only 1 to 2 subcentimeter tubular adenomas are lower than initially estimated.2,3 This extension provides an opportunity to increase endoscopy capacity and improve access to colonoscopies by retroactively applying the 2020 guidelines to surveillance interval recommendations made before their introduction. For example, based on the updated guidelines, patients previously recommended to undergo colon polyp surveillance colonoscopy 5 years after an index colonoscopy could extend their surveillance interval by 2 to 5 years. Increasing endoscopic capacity could address the growing demand for colonoscopies from new screening guidelines that reduced the age of initial CRC screening from 50 years to 45 years and the backlog of procedures due to COVID-19 restrictions.4
As part of a project to increase endoscopic capacity at the US Department of Veterans Affairs (VA) Pittsburgh Healthcare System (VAPHS), this study assessed the potential impact of retroactively applying the 2020 USMSTF polyp surveillance guidelines on endoscopic capacity. These results may be informative for other VA and private-sector health care systems seeking to identify strategies to improve endoscopy capacity.
Methods
VAPHS is an integrated health care system in the Veterans Health Administration (VHA) serving 85,000 patients across 8 health care institutions in Pennsylvania, Ohio, and West Virginia. VAPHS manages colorectal screening recommendations for patients receiving medical care in the health care system regardless of whether their prior colonoscopy was performed at VAPHS or external facilities. The VA maintains a national CRC screening and surveillance electronic medical record reminder that prompts health care practitioners to order colon polyp surveillance based on interval recommendations from the index colonoscopy. This study reviewed all patients from the VAPHS panel with a reminder to undergo colonoscopy for screening for CRC or surveillance of colon polyps within 12 months from September 1, 2022.
Among patients with a reminder, 3 investigators reviewed index colonoscopy and pathology reports to identify CRC risk category, colonoscopy indication, procedural quality, and recommended repeat colonoscopy interval. Per the USMSTF guidelines, patients with incomplete colonoscopy or pathology records, high-risk indications (ie, personal history of inflammatory bowel disease, personal history of CRC, or family history of CRC), or inadequate bowel preparation (Boston Bowel Preparation Score < 6) were excluded. Additionally, patients who had CRC screening or surveillance discontinued due to age or comorbidities, had completed a subsequent follow-up colonoscopy, or were deceased at the time of review were excluded.
Retroactive Interval Reclassification
Among eligible patients, this study compared the repeat colonoscopy interval recommended by the prior endoscopist with those from the 2020 USMSTF guidelines. In cases where the interval was documented as a range of years, the lower end was considered the recommendation. Similarly, the lower end of the range from the 2020 USMSTF guidelines was used for the reclassified surveillance interval. Years extended per patient were quantified relative to September 1, 2023 (ie, 1 year after the review date). For example, if the index colonoscopy was completed on September 1, 2016, the initial surveillance recommendation was 5 years, and the reclassified recommendation was 7 years, the interval extension beyond September 1, 2023, was 0 years.
Furthermore, because index surveillance recommendations are not always guideline concordant, the years extended per patient were calculated by harmonizing the index endoscopist’s recommendations with the guidelines at the time of the index colonoscopy.5 For example, if the index colonoscopy was completed on September 1, 2018, and the endoscopist recommended a 5-year follow-up for a patient with average risk for CRC, adequate bowel preparation, and no colorectal polyps, that patient is eligible to extend their colonoscopy to September 1, 2028, based on guideline recommendations at the time of index endoscopy recommending that the next colonoscopy occur in 10 years. In this analysis the 2012 USMSTF guidelines were applied to all index colonoscopies completed in 2021 or earlier to allow time for adoption of the 2020 guidelines.
This project fulfilled a facility mandate to increase capacity to conduct endoscopic procedures. Institutional review board approval was not required by VAPHS policy relating to clinical operations projects. Approval for publication of clinical operations activity was obtained from the VAPHS facility director.
Results
Within 1 year of the September 1, 2022, review date, 637 patients receiving care at VAPHS had clinical reminders for an upcoming colonoscopy. Of these, 54 (8.4%) were already up to date or were deceased at the time of review. Of the 583 eligible patients, 96% were male, the median age was 74 years, the median index colonoscopy year was 2016, and 178 (30.5%) had an average-risk CRC screening indication at the index colonoscopy (Table).
Of the 583 patients due for colonoscopy, 331 (56.7%) had both colonoscopy and pathology reports available. The majority of those with incomplete records had the index colonoscopy completed outside VAPHS. Among these patients, 222 (67.0%) had adequate bowel preparation. Of those with adequate bowel preparation, 43 were not eligible for interval extension because of high-risk conditions and 13 were not eligible because there was no index surveillance interval recommendation from the index endoscopist. Of the patients due for colonoscopy, 166 (28.4%) were potentially eligible for surveillance interval extension (Figure).
Sixty-five (39.2%) of the 166 patients had 1 to 2 subcentimeter tubular adenomas on their index colonoscopy. Sixty-two patients were eligible for interval extension to 7 years, but this only resulted in ≥ 1 year of extension beyond the review date for 36 (6% of all 583 patients due for colonoscopy). The 36 patients were extended 63 years. By harmonizing the index endoscopists’ surveillance interval recommendation with the guideline at the time of the index colonoscopy, 29 additional patients could have their colonoscopy extended by ≥ 1 year. Harmonization extended colonoscopy intervals by 93 years. Retroactively applying the 2020 USMSTF polyp surveillance guidelines and harmonizing recommendations to guidelines extended the time of index colonoscopy by 153 years.
Discussion
With retroactive application of the 2020 USMSTF polyp surveillance guidelines, 6% of patients due for an upcoming colonoscopy could extend their follow-up by ≥ 1 year by extending the surveillance interval for 1 to 2 subcentimeter tubular adenomas to 7 years. An additional 5% of patients could extend their interval by harmonizing the index endoscopist’s interval recommendation with polyp surveillance guidelines at the time of the index colonoscopy. These findings are consistent with the results of 2 studies that demonstrated that about 14% of patients due for colonoscopy could have their interval extended.6,7 The current study enhances those insights by separating the contribution of 2020 USMSTF polyp surveillance guidelines from the contribution of harmonizing surveillance intervals with guidelines for other polyp histologies. This study found that there is an opportunity to improve endoscopic capacity by harmonizing recommendations with guidelines. This complements a 2023 study showing that even when knowledgeable about guidelines, clinicians do not necessarily follow recommendations.8 While this and previous research have identified that 11% to 14% of patients are eligible for extension, these individuals would also have to be willing to have their polyp surveillance intervals extended for there to be a real-world impact on endoscopic capacity. A 2024 study found that only 19% to 37% of patients with 1 to 2 small tubular adenomas were willing to have polyps surveillance interval extension.9 This suggests the actual effect on capacity may be even lower than reported.
Limitations
The overall impact of the 2020 USMSTF polyp surveillance guidelines on endoscopic capacity was blunted by the high prevalence of incomplete index colonoscopy records among the study population. Without data on bowel preparation quality or procedure indications, this study could not assess whether 43% of patients were eligible for surveillance interval extension. Most index colonoscopies with incomplete documentation were completed at community-care gastroenterology facilities. This high rate of incomplete documentation is likely generalizable to other VA health care systems—especially in the era of the Veterans Access, Choice, and Accountability Act of 2014, which increased veteran access to non-VA community care.10 Veterans due for colon polyp surveillance colonoscopies are more likely to have had their prior colonoscopy in community care compared with prior eras.11 Furthermore, because the VHA is among the most established integrated health care systems offering primary and subspecialty care in the US, private sector health care systems may have even greater rates of care fragmentation for longitudinal CRC screening and colon polyp surveillance, as these systems have only begun to regionally integrate recently.12,13
Another limitation is that nearly one-third of the individuals with documentation had inadequate bowel preparation for surveillance recommendations. This results in shorter surveillance follow-up colonoscopies and increases downstream demand for future colonoscopies. The low yield of extending colon polyp surveillance interval in this study emphasizes that improved efforts to obtain colonoscopy and pathology reports from community care, right-sizing the colon polyp surveillance intervals recommended by endoscopists, and improving quality of bowel preparation could have downstream health care system benefits in the future. These efforts could increase colonoscopy capacity at VA health care systems, thereby shortening colonoscopy wait times, decreasing fragmentation of care, and increasing the number of veterans who receive high-quality colonoscopies at VA health care systems.14
Conclusions
Eleven percent of patients in this study due for a colonoscopy could extend their follow-up by ≥ 1 year. About half of these extensions were directly due to the 2020 USMSTF polyp surveillance interval extension for 1 to 2 subcentimeter tubular adenomas. The rest resulted from harmonizing recommendations with guidelines at the time of the procedure. To determine whether retroactively applying polyp surveillance guidelines to follow-up interval recommendations will result in improved endoscopic capacity, health care system administrators should consider the degree of CRC screening care fragmentation in their patient population. Greater long-term gains in endoscopic capacity may be achieved by proactively supporting endoscopists in making guideline-concordant screening recommendations at the time of colonoscopy.
Gupta S, Lieberman D, Anderson JC, et al. Recommendations for follow-up after colonoscopy and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc. 2020;91:463-485. doi:10.1016/j.gie.2020.01.014
Dubé C, Yakubu M, McCurdy BR, et al. Risk of advanced adenoma, colorectal cancer, and colorectal cancer mortality in people with low-risk adenomas at baseline colonoscopy: a systematic review and meta-analysis. Am J Gastroenterol. 2017;112:1790-1801. doi:10.1038/ajg.2017.360
Click B, Pinsky PF, Hickey T, Doroudi M, Shoen RE. Association of colonoscopy adenoma findings with long-term colorectal cancer incidence. JAMA. 2018;319:2021-2031. doi:10.1001/jama.2018.5809
US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2021;325:1965-1977. doi:10.1001/jama.2021.6238
Djinbachian R, Dubé AJ, Durand M, et al. Adherence to post-polypectomy surveillance guidelines: a systematic review and meta-analysis. Endoscopy. 2019;51:673-683. doi:10.1055/a-0865-2082
Gawron AJ, Kaltenbach T, Dominitz JA. The impact of the coronavirus disease-19 pandemic on access to endoscopy procedures in the VA healthcare system. Gastroenterology. 2020;159:1216-1220.e1. doi:10.1053/j.gastro.2020.07.033
Xiao AH, Chang SY, Stevoff CG, Komanduri S, Pandolfino JE, Keswani RN. Adoption of multi-society guidelines facilitates value-based reduction in screening and surveillance colonoscopy volume during COVID-19 pandemic. Dig Dis Sci. 2021;66:2578-2584. doi:10.1007/s10620-020-06539-1
Dong J, Wang LF, Ardolino E, Feuerstein JD. Real-world compliance with the 2020 U.S. Multi-Society Task Force on Colorectal Cancer polypectomy surveillance guidelines: an observational study. Gastrointest Endosc. 2023;97:350-356.e3. doi:10.1016/j.gie.2022.08.020
Lee JK, Koripella PC, Jensen CD, et al. Randomized trial of patient outreach approaches to de-implement outdated colonoscopy surveillance intervals. Clin Gastroenterol Hepatol. 2024;22:1315-1322.e7. doi:10.1016/j.cgh.2023.12.027
Veterans Access, Choice, and Accountability Act of 2014, HR 3230, 113th Cong (2014). Accessed September 8, 2025. https://www.congress.gov/bill/113th-congress/house-bill/3230
Dueker JM, Khalid A. Performance of the Veterans Choice Program for improving access to colonoscopy at a tertiary VA facility. Fed Pract. 2020;37:224-228.
Oliver A. The Veterans Health Administration: an American success story? Milbank Q. 2007;85:5-35. doi:10.1111/j.1468-0009.2007.00475.x
Furukawa MF, Machta RM, Barrett KA, et al. Landscape of health systems in the United States. Med Care Res Rev. 2020;77:357-366. doi:10.1177/1077558718823130
Petros V, Tsambikos E, Madhoun M, Tierney WM. Impact of community referral on colonoscopy quality metrics in a Veterans Affairs Medical Center. Clin Transl Gastroenterol. 2022;13:e00460. doi:10.14309/ctg.0000000000000460
Gupta S, Lieberman D, Anderson JC, et al. Recommendations for follow-up after colonoscopy and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc. 2020;91:463-485. doi:10.1016/j.gie.2020.01.014
Dubé C, Yakubu M, McCurdy BR, et al. Risk of advanced adenoma, colorectal cancer, and colorectal cancer mortality in people with low-risk adenomas at baseline colonoscopy: a systematic review and meta-analysis. Am J Gastroenterol. 2017;112:1790-1801. doi:10.1038/ajg.2017.360
Click B, Pinsky PF, Hickey T, Doroudi M, Shoen RE. Association of colonoscopy adenoma findings with long-term colorectal cancer incidence. JAMA. 2018;319:2021-2031. doi:10.1001/jama.2018.5809
US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2021;325:1965-1977. doi:10.1001/jama.2021.6238
Djinbachian R, Dubé AJ, Durand M, et al. Adherence to post-polypectomy surveillance guidelines: a systematic review and meta-analysis. Endoscopy. 2019;51:673-683. doi:10.1055/a-0865-2082
Gawron AJ, Kaltenbach T, Dominitz JA. The impact of the coronavirus disease-19 pandemic on access to endoscopy procedures in the VA healthcare system. Gastroenterology. 2020;159:1216-1220.e1. doi:10.1053/j.gastro.2020.07.033
Xiao AH, Chang SY, Stevoff CG, Komanduri S, Pandolfino JE, Keswani RN. Adoption of multi-society guidelines facilitates value-based reduction in screening and surveillance colonoscopy volume during COVID-19 pandemic. Dig Dis Sci. 2021;66:2578-2584. doi:10.1007/s10620-020-06539-1
Dong J, Wang LF, Ardolino E, Feuerstein JD. Real-world compliance with the 2020 U.S. Multi-Society Task Force on Colorectal Cancer polypectomy surveillance guidelines: an observational study. Gastrointest Endosc. 2023;97:350-356.e3. doi:10.1016/j.gie.2022.08.020
Lee JK, Koripella PC, Jensen CD, et al. Randomized trial of patient outreach approaches to de-implement outdated colonoscopy surveillance intervals. Clin Gastroenterol Hepatol. 2024;22:1315-1322.e7. doi:10.1016/j.cgh.2023.12.027
Veterans Access, Choice, and Accountability Act of 2014, HR 3230, 113th Cong (2014). Accessed September 8, 2025. https://www.congress.gov/bill/113th-congress/house-bill/3230
Dueker JM, Khalid A. Performance of the Veterans Choice Program for improving access to colonoscopy at a tertiary VA facility. Fed Pract. 2020;37:224-228.
Oliver A. The Veterans Health Administration: an American success story? Milbank Q. 2007;85:5-35. doi:10.1111/j.1468-0009.2007.00475.x
Furukawa MF, Machta RM, Barrett KA, et al. Landscape of health systems in the United States. Med Care Res Rev. 2020;77:357-366. doi:10.1177/1077558718823130
Petros V, Tsambikos E, Madhoun M, Tierney WM. Impact of community referral on colonoscopy quality metrics in a Veterans Affairs Medical Center. Clin Transl Gastroenterol. 2022;13:e00460. doi:10.14309/ctg.0000000000000460
Impact of Retroactive Application of Updated Surveillance Guidelines on Endoscopy Center Capacity at a Large VA Health Care System
Impact of Retroactive Application of Updated Surveillance Guidelines on Endoscopy Center Capacity at a Large VA Health Care System
mRNA Cancer Vaccines: Pipeline Insights for Clinicians
Since 1965, messenger RNA (mRNA) vaccines have been studied for cancer treatment, but it was the technological advances in vaccines during the COVID pandemic that helped accelerate research. Currently, no vaccine has been approved for tumor treatment, although many clinical studies are ongoing worldwide. According to experts consulted by Medscape’s Portuguese edition, the outlook is very promising, and these studies are expected to open doors for personalized therapies.
In cancer treatment, the vaccine would function as an immunotherapy, in which the immune system can be “trained” to act against an invader. Just as with pathogens, the platform would use parts of the tumor — which have altered proteins or are expressed at abnormal levels — to teach the body to defend itself against cancer.
Vladmir Lima, MD, PhD, clinical oncologist at A.C. Camargo Cancer Center, São Paulo, Brazil, explained that with this technology it will be possible to produce personalized vaccines, which prevents, for example, large-scale manufacturing. “In theory, these vaccines can be developed for any tumor type, but this does not mean that efficacy will be the same for all,” he said. Because cancer has specific characteristics in each individual, it is difficult to envision a single vaccine that works for all cancers.
Current evidence suggests the vaccine could be administered after chemotherapy or radiotherapy, with the goal of reducing tumor mass and increasing the effectiveness of mRNA-based treatment, according to Ana Paula Lepique, professor and researcher in tumor immunology at the Institute of Biomedical Sciences, University of São Paulo, São Paulo.
“There is also a study with pancreatic cancer patients, in which the vaccine was administered after surgery,” she explained. “It would not work, for example, to give chemotherapy or radiotherapy while the immune response is being triggered by the vaccine. This would make the vaccine ineffective, since chemotherapy and radiotherapy are toxic to lymphocytes.”
Lepique also clarified that it is possible to combine the vaccine with immunotherapy targeting immune regulatory molecules. “In this case, in addition to administering the mRNA with the antigen, a strategy is used to improve the patient’s immune response.”
Challenges With mRNA Vaccines
Despite being a promising technology, there are challenges, warned Lepique. mRNA molecules degrade quickly when injected into the body, which can compromise vaccine efficacy. To overcome this, researchers have developed nanoencapsulation technologies that protect the molecules and allow safe use in vaccines. “Another alternative is transferring the mRNA into dendritic cells, known as antigen-presenting cells, and then administering these cells to the patient,” she explained.
Global Research Status
According to a study published this year in Med, over 120 clinical trials are exploring mRNA vaccines to treat lung, breast, prostate, and pancreatic tumors, as well as melanoma.
Lepique noted that the countries leading this research are the US, UK, Germany, China, and Japan. “Unfortunately, the US government recently cut funding for mRNA vaccine development and testing, which will likely have significant consequences,” she said.
Lepique reported that Brazilian researchers are collaborating with international institutions to develop these vaccines. “The Brazilian government, through the Ministry of Health and the Ministry of Science, Technology, and Innovation, recently announced investments in mRNA technologies for vaccines. While not specifically targeting cancer, these investments could also benefit this field,” she clarified.
Leading Studies
Lepique highlighted the most advanced studies to date:
- Pancreatic cancer: A study published in Nature in February demonstrated that a personalized mRNA vaccine reduced the risk for recurrence after surgery in 16 patients, with 3 years of follow-up.
- Melanoma: A study published in The Lancet reported improved survival in melanoma patients after mRNA vaccine administration combined with the checkpoint inhibitor pembrolizumab applied after surgical tumor resection.
- Universal vaccine: A study in Nature Biomedical Engineering described the creation of a “generic” vaccine capable of activating the patient’s immune system and inducing tumor regression. Lepique explained that this vaccine acts more as an immune response modulator than a classical neoantigen-specific vaccine. “Because it is not limited to a single neoantigen, it could potentially be universal, though further testing is needed to determine efficacy across all cancer types,” she added.
Lima highlighted a 2024 study being conducted by MSD and Moderna against lung cancer, with results yet to be published. “Patients first receive immunotherapy after surgery. Once the vaccine is ready, it is added to the ongoing immunotherapy,” he explained. The global phase 3 study involves 868 patients with resected lung cancer who previously underwent chemotherapy. Participants receive the vaccine (1 mg every 3 weeks, up to nine doses) alongside pembrolizumab (400 mg every 6 weeks, up to nine cycles) over approximately 1 year.
Other mRNA vaccines remain in early-stage development. For example, in May 2024, the UK National Health Service recruited participants for a personalized colorectal cancer mRNA vaccine trial.
Advantages of mRNA Technology
Experts noted that mRNA-based cancer vaccines are considered safer for patients because the tumor mRNA is synthesized in the laboratory. According to Lepique, these vaccines are more specific than many other cancer therapies, and therefore carry a lower risk for serious side effects.
“Clinical studies have shown that these vaccines can generate immunological memory, meaning lymphocytes that recognize tumor antigens remain in the body and can respond to recurrence,” she explained.
It is also possible to combine multiple mRNA molecules in a single vaccine, creating a platform that targets several tumor antigens simultaneously. “Formulations can additionally include adjuvants to further enhance immune responses against tumors,” she said. However, as a personalized therapy, costs are high, and vaccine formulation requires considerable time.
Lima emphasized the customization advantage: “We can take a portion of the patient’s tumor, sequence it to identify alterations, and develop a vaccine specifically for that tumor.” He also highlighted safety data, noting that the platform has been widely used in SARS-CoV-2 vaccine development, providing confidence in large-scale application. “The potential exists to achieve more personalized, tumor-directed immunotherapy with greater scalability,” he explained.
Outlook and Limitations
Lima noted that although the projected efficacy is promising, definitive results are still pending.
“We have very positive expectations, but we must wait for study outcomes. Efficacy may vary across scenarios and among patients. The immune system may also respond against the vaccine itself, potentially reducing effectiveness at times,” he explained.
According to Lima, mRNA vaccines are expected to complement current treatments, enhancing outcomes without replacing conventional approaches entirely.
“It will not be a panacea. These vaccines are likely to add to and improve strategies we already use, but they will not work for all patients in every scenario,” he concluded.
Lepique highlighted the promise of combination strategies. “The outlook is positive, particularly because multiple mRNA types can be combined in a single formulation and used alongside drugs that enhance immune responses,” she explained.
Although mRNA vaccine research has been ongoing for many years, prior results have brought both progress and setbacks. “This new protocol appears more effective [and] capable of generating immunological memory and is also safe,” she noted. Still, she cautioned that cancer presents unique challenges: “The disease has multiple mechanisms to evade immune responses. Additionally, some tumors are naturally unrecognized by the immune system, the so-called ‘cold tumors.’”
This story was translated from Medscape’s Portuguese edition. A version of this article appeared on Medscape.com.
Since 1965, messenger RNA (mRNA) vaccines have been studied for cancer treatment, but it was the technological advances in vaccines during the COVID pandemic that helped accelerate research. Currently, no vaccine has been approved for tumor treatment, although many clinical studies are ongoing worldwide. According to experts consulted by Medscape’s Portuguese edition, the outlook is very promising, and these studies are expected to open doors for personalized therapies.
In cancer treatment, the vaccine would function as an immunotherapy, in which the immune system can be “trained” to act against an invader. Just as with pathogens, the platform would use parts of the tumor — which have altered proteins or are expressed at abnormal levels — to teach the body to defend itself against cancer.
Vladmir Lima, MD, PhD, clinical oncologist at A.C. Camargo Cancer Center, São Paulo, Brazil, explained that with this technology it will be possible to produce personalized vaccines, which prevents, for example, large-scale manufacturing. “In theory, these vaccines can be developed for any tumor type, but this does not mean that efficacy will be the same for all,” he said. Because cancer has specific characteristics in each individual, it is difficult to envision a single vaccine that works for all cancers.
Current evidence suggests the vaccine could be administered after chemotherapy or radiotherapy, with the goal of reducing tumor mass and increasing the effectiveness of mRNA-based treatment, according to Ana Paula Lepique, professor and researcher in tumor immunology at the Institute of Biomedical Sciences, University of São Paulo, São Paulo.
“There is also a study with pancreatic cancer patients, in which the vaccine was administered after surgery,” she explained. “It would not work, for example, to give chemotherapy or radiotherapy while the immune response is being triggered by the vaccine. This would make the vaccine ineffective, since chemotherapy and radiotherapy are toxic to lymphocytes.”
Lepique also clarified that it is possible to combine the vaccine with immunotherapy targeting immune regulatory molecules. “In this case, in addition to administering the mRNA with the antigen, a strategy is used to improve the patient’s immune response.”
Challenges With mRNA Vaccines
Despite being a promising technology, there are challenges, warned Lepique. mRNA molecules degrade quickly when injected into the body, which can compromise vaccine efficacy. To overcome this, researchers have developed nanoencapsulation technologies that protect the molecules and allow safe use in vaccines. “Another alternative is transferring the mRNA into dendritic cells, known as antigen-presenting cells, and then administering these cells to the patient,” she explained.
Global Research Status
According to a study published this year in Med, over 120 clinical trials are exploring mRNA vaccines to treat lung, breast, prostate, and pancreatic tumors, as well as melanoma.
Lepique noted that the countries leading this research are the US, UK, Germany, China, and Japan. “Unfortunately, the US government recently cut funding for mRNA vaccine development and testing, which will likely have significant consequences,” she said.
Lepique reported that Brazilian researchers are collaborating with international institutions to develop these vaccines. “The Brazilian government, through the Ministry of Health and the Ministry of Science, Technology, and Innovation, recently announced investments in mRNA technologies for vaccines. While not specifically targeting cancer, these investments could also benefit this field,” she clarified.
Leading Studies
Lepique highlighted the most advanced studies to date:
- Pancreatic cancer: A study published in Nature in February demonstrated that a personalized mRNA vaccine reduced the risk for recurrence after surgery in 16 patients, with 3 years of follow-up.
- Melanoma: A study published in The Lancet reported improved survival in melanoma patients after mRNA vaccine administration combined with the checkpoint inhibitor pembrolizumab applied after surgical tumor resection.
- Universal vaccine: A study in Nature Biomedical Engineering described the creation of a “generic” vaccine capable of activating the patient’s immune system and inducing tumor regression. Lepique explained that this vaccine acts more as an immune response modulator than a classical neoantigen-specific vaccine. “Because it is not limited to a single neoantigen, it could potentially be universal, though further testing is needed to determine efficacy across all cancer types,” she added.
Lima highlighted a 2024 study being conducted by MSD and Moderna against lung cancer, with results yet to be published. “Patients first receive immunotherapy after surgery. Once the vaccine is ready, it is added to the ongoing immunotherapy,” he explained. The global phase 3 study involves 868 patients with resected lung cancer who previously underwent chemotherapy. Participants receive the vaccine (1 mg every 3 weeks, up to nine doses) alongside pembrolizumab (400 mg every 6 weeks, up to nine cycles) over approximately 1 year.
Other mRNA vaccines remain in early-stage development. For example, in May 2024, the UK National Health Service recruited participants for a personalized colorectal cancer mRNA vaccine trial.
Advantages of mRNA Technology
Experts noted that mRNA-based cancer vaccines are considered safer for patients because the tumor mRNA is synthesized in the laboratory. According to Lepique, these vaccines are more specific than many other cancer therapies, and therefore carry a lower risk for serious side effects.
“Clinical studies have shown that these vaccines can generate immunological memory, meaning lymphocytes that recognize tumor antigens remain in the body and can respond to recurrence,” she explained.
It is also possible to combine multiple mRNA molecules in a single vaccine, creating a platform that targets several tumor antigens simultaneously. “Formulations can additionally include adjuvants to further enhance immune responses against tumors,” she said. However, as a personalized therapy, costs are high, and vaccine formulation requires considerable time.
Lima emphasized the customization advantage: “We can take a portion of the patient’s tumor, sequence it to identify alterations, and develop a vaccine specifically for that tumor.” He also highlighted safety data, noting that the platform has been widely used in SARS-CoV-2 vaccine development, providing confidence in large-scale application. “The potential exists to achieve more personalized, tumor-directed immunotherapy with greater scalability,” he explained.
Outlook and Limitations
Lima noted that although the projected efficacy is promising, definitive results are still pending.
“We have very positive expectations, but we must wait for study outcomes. Efficacy may vary across scenarios and among patients. The immune system may also respond against the vaccine itself, potentially reducing effectiveness at times,” he explained.
According to Lima, mRNA vaccines are expected to complement current treatments, enhancing outcomes without replacing conventional approaches entirely.
“It will not be a panacea. These vaccines are likely to add to and improve strategies we already use, but they will not work for all patients in every scenario,” he concluded.
Lepique highlighted the promise of combination strategies. “The outlook is positive, particularly because multiple mRNA types can be combined in a single formulation and used alongside drugs that enhance immune responses,” she explained.
Although mRNA vaccine research has been ongoing for many years, prior results have brought both progress and setbacks. “This new protocol appears more effective [and] capable of generating immunological memory and is also safe,” she noted. Still, she cautioned that cancer presents unique challenges: “The disease has multiple mechanisms to evade immune responses. Additionally, some tumors are naturally unrecognized by the immune system, the so-called ‘cold tumors.’”
This story was translated from Medscape’s Portuguese edition. A version of this article appeared on Medscape.com.
Since 1965, messenger RNA (mRNA) vaccines have been studied for cancer treatment, but it was the technological advances in vaccines during the COVID pandemic that helped accelerate research. Currently, no vaccine has been approved for tumor treatment, although many clinical studies are ongoing worldwide. According to experts consulted by Medscape’s Portuguese edition, the outlook is very promising, and these studies are expected to open doors for personalized therapies.
In cancer treatment, the vaccine would function as an immunotherapy, in which the immune system can be “trained” to act against an invader. Just as with pathogens, the platform would use parts of the tumor — which have altered proteins or are expressed at abnormal levels — to teach the body to defend itself against cancer.
Vladmir Lima, MD, PhD, clinical oncologist at A.C. Camargo Cancer Center, São Paulo, Brazil, explained that with this technology it will be possible to produce personalized vaccines, which prevents, for example, large-scale manufacturing. “In theory, these vaccines can be developed for any tumor type, but this does not mean that efficacy will be the same for all,” he said. Because cancer has specific characteristics in each individual, it is difficult to envision a single vaccine that works for all cancers.
Current evidence suggests the vaccine could be administered after chemotherapy or radiotherapy, with the goal of reducing tumor mass and increasing the effectiveness of mRNA-based treatment, according to Ana Paula Lepique, professor and researcher in tumor immunology at the Institute of Biomedical Sciences, University of São Paulo, São Paulo.
“There is also a study with pancreatic cancer patients, in which the vaccine was administered after surgery,” she explained. “It would not work, for example, to give chemotherapy or radiotherapy while the immune response is being triggered by the vaccine. This would make the vaccine ineffective, since chemotherapy and radiotherapy are toxic to lymphocytes.”
Lepique also clarified that it is possible to combine the vaccine with immunotherapy targeting immune regulatory molecules. “In this case, in addition to administering the mRNA with the antigen, a strategy is used to improve the patient’s immune response.”
Challenges With mRNA Vaccines
Despite being a promising technology, there are challenges, warned Lepique. mRNA molecules degrade quickly when injected into the body, which can compromise vaccine efficacy. To overcome this, researchers have developed nanoencapsulation technologies that protect the molecules and allow safe use in vaccines. “Another alternative is transferring the mRNA into dendritic cells, known as antigen-presenting cells, and then administering these cells to the patient,” she explained.
Global Research Status
According to a study published this year in Med, over 120 clinical trials are exploring mRNA vaccines to treat lung, breast, prostate, and pancreatic tumors, as well as melanoma.
Lepique noted that the countries leading this research are the US, UK, Germany, China, and Japan. “Unfortunately, the US government recently cut funding for mRNA vaccine development and testing, which will likely have significant consequences,” she said.
Lepique reported that Brazilian researchers are collaborating with international institutions to develop these vaccines. “The Brazilian government, through the Ministry of Health and the Ministry of Science, Technology, and Innovation, recently announced investments in mRNA technologies for vaccines. While not specifically targeting cancer, these investments could also benefit this field,” she clarified.
Leading Studies
Lepique highlighted the most advanced studies to date:
- Pancreatic cancer: A study published in Nature in February demonstrated that a personalized mRNA vaccine reduced the risk for recurrence after surgery in 16 patients, with 3 years of follow-up.
- Melanoma: A study published in The Lancet reported improved survival in melanoma patients after mRNA vaccine administration combined with the checkpoint inhibitor pembrolizumab applied after surgical tumor resection.
- Universal vaccine: A study in Nature Biomedical Engineering described the creation of a “generic” vaccine capable of activating the patient’s immune system and inducing tumor regression. Lepique explained that this vaccine acts more as an immune response modulator than a classical neoantigen-specific vaccine. “Because it is not limited to a single neoantigen, it could potentially be universal, though further testing is needed to determine efficacy across all cancer types,” she added.
Lima highlighted a 2024 study being conducted by MSD and Moderna against lung cancer, with results yet to be published. “Patients first receive immunotherapy after surgery. Once the vaccine is ready, it is added to the ongoing immunotherapy,” he explained. The global phase 3 study involves 868 patients with resected lung cancer who previously underwent chemotherapy. Participants receive the vaccine (1 mg every 3 weeks, up to nine doses) alongside pembrolizumab (400 mg every 6 weeks, up to nine cycles) over approximately 1 year.
Other mRNA vaccines remain in early-stage development. For example, in May 2024, the UK National Health Service recruited participants for a personalized colorectal cancer mRNA vaccine trial.
Advantages of mRNA Technology
Experts noted that mRNA-based cancer vaccines are considered safer for patients because the tumor mRNA is synthesized in the laboratory. According to Lepique, these vaccines are more specific than many other cancer therapies, and therefore carry a lower risk for serious side effects.
“Clinical studies have shown that these vaccines can generate immunological memory, meaning lymphocytes that recognize tumor antigens remain in the body and can respond to recurrence,” she explained.
It is also possible to combine multiple mRNA molecules in a single vaccine, creating a platform that targets several tumor antigens simultaneously. “Formulations can additionally include adjuvants to further enhance immune responses against tumors,” she said. However, as a personalized therapy, costs are high, and vaccine formulation requires considerable time.
Lima emphasized the customization advantage: “We can take a portion of the patient’s tumor, sequence it to identify alterations, and develop a vaccine specifically for that tumor.” He also highlighted safety data, noting that the platform has been widely used in SARS-CoV-2 vaccine development, providing confidence in large-scale application. “The potential exists to achieve more personalized, tumor-directed immunotherapy with greater scalability,” he explained.
Outlook and Limitations
Lima noted that although the projected efficacy is promising, definitive results are still pending.
“We have very positive expectations, but we must wait for study outcomes. Efficacy may vary across scenarios and among patients. The immune system may also respond against the vaccine itself, potentially reducing effectiveness at times,” he explained.
According to Lima, mRNA vaccines are expected to complement current treatments, enhancing outcomes without replacing conventional approaches entirely.
“It will not be a panacea. These vaccines are likely to add to and improve strategies we already use, but they will not work for all patients in every scenario,” he concluded.
Lepique highlighted the promise of combination strategies. “The outlook is positive, particularly because multiple mRNA types can be combined in a single formulation and used alongside drugs that enhance immune responses,” she explained.
Although mRNA vaccine research has been ongoing for many years, prior results have brought both progress and setbacks. “This new protocol appears more effective [and] capable of generating immunological memory and is also safe,” she noted. Still, she cautioned that cancer presents unique challenges: “The disease has multiple mechanisms to evade immune responses. Additionally, some tumors are naturally unrecognized by the immune system, the so-called ‘cold tumors.’”
This story was translated from Medscape’s Portuguese edition. A version of this article appeared on Medscape.com.
Hepatitis D Virus Classified as Carcinogenic: Implications
The International Agency for Research on Cancer (IARC) of the World Health Organization has classified hepatitis D virus (HDV) as carcinogenic, citing sufficient evidence and placing it alongside hepatitis B virus (HBV) and hepatitis C virus (HCV) as a cause of hepatocellular carcinoma (HCC).
Individuals with HBV-HDV coinfection face an elevated risk for liver cancer, highlighting the need for HBV vaccination, systematic screening, and early antiviral treatment to reduce the progression to cirrhosis and HCC.
About 12 million people globally have HBV-HDV coinfection, representing 5% of all chronic HBV cases. The prevalence of this condition varies regionally, with a likely underdiagnosis. True coinfection rates may reach 13%-14%, the highest in Europe’s Mediterranean region.
Virus Biology
HDV is an incomplete virus that infects hepatocytes and requires the envelope protein of hepatitis B surface antigen (HBsAg) for cell exit. Infection occurs only with chronic HBV infection, either as a superinfection or simultaneous acquisition. Humans are the only known natural host.
HDV coinfection worsens HBV-induced hepatic inflammation and prognosis, and up to 80% of patients develop cirrhosis. Triple infection with the HBV virus, HDV, and HIV further increases this risk, and the global prevalence is likely underestimated.
Cancer Risk
HDV infection significantly increases the risk for HCC compared with HBV infection alone. Many patients die from decompensated cirrhosis or HCC, reflecting the aggressive nature of coinfection.
The molecular mechanisms underlying HDV oncogenesis remain unclear. Research conducted over the past 15 years has provided insights that could inform the development of more effective treatments.
Early vaccination prophylaxis is critical for reducing the risk for HCC, despite limited options.
Treatment Options
Randomized controlled trials have demonstrated antiviral efficacy for:
- Pegylated interferon alpha (Peg-IFN) is approved for HBV and is active against HDV.
- Bulevirtide, a synthetic myristoylated lipopeptide entry inhibitor, is used alone or in combination with Peg-IFN.
Suppression of HBV remains central. Nucleoside and nucleotide analogs, such as entecavir, tenofovir alafenamide fumarate, and tenofovir disoproxil fumarate, significantly reduce HCC progression in treated patients compared with untreated patients at risk.
Promising therapeutics include lonafarnib, a farnesyltransferase inhibitor that blocks HDV particle formation, and nucleic acid polymers targeting the host chaperone DNAJB12 to inhibit HBV and HDV replication.
Guideline Updates
The 2023 addendum to the S3 guidelines covers the prophylaxis, diagnosis, and treatment of HBV, including HDV management.
IARC experts also re-evaluated the human cytomegalovirus and Merkel cell polyomavirus. Complete assessments are expected in the next edition of IARC Monographs.
HBV Vaccination
HBV vaccination is the only effective prophylaxis against HBV and HDV. Introduced in 1982 for high-risk groups, it reduced chronic infections, with the WHO expanding its recommendations from 1992 onward.
Infants and young children are at the highest risk of developing this disease. Acute HBV infection often resolves in adults, but infants face up to a 90% risk of developing chronic infection. Newborns of mothers with chronic or undiagnosed HBV infections are particularly vulnerable.
Routine infant immunization includes three doses, with the first dose administered within 12 hours of birth. In Germany, the Standing Committee on Vaccination (STIKO) recommends the administration of combination vaccines, with the hexavalent vaccine administered at 2, 4, and 11 months in a 2 + 1 schedule.
Timely vaccination is crucial because undetected chronic infections often lead to late-stage HCC diagnosis. Adults in high-risk groups should receive HBV vaccination counseling.
STIKO recommends vaccination for close contacts of individuals who are HBsAg-positive, individuals with high-risk sexual contacts, immunocompromised persons, and those with preexisting conditions that increase the risk for severe HBV infection.
Since 2021, insured adults aged 35 years or older in Germany have undergone one-time HBV and HCV screening. HDV testing is recommended for all HBsAg-positive patients. Current frameworks may miss cases, and additional or personalized screening could improve the detection of previously unrecognized infections.
This story was translated from Univadis Germany.
A version of this article appeared on Medscape.com.
The International Agency for Research on Cancer (IARC) of the World Health Organization has classified hepatitis D virus (HDV) as carcinogenic, citing sufficient evidence and placing it alongside hepatitis B virus (HBV) and hepatitis C virus (HCV) as a cause of hepatocellular carcinoma (HCC).
Individuals with HBV-HDV coinfection face an elevated risk for liver cancer, highlighting the need for HBV vaccination, systematic screening, and early antiviral treatment to reduce the progression to cirrhosis and HCC.
About 12 million people globally have HBV-HDV coinfection, representing 5% of all chronic HBV cases. The prevalence of this condition varies regionally, with a likely underdiagnosis. True coinfection rates may reach 13%-14%, the highest in Europe’s Mediterranean region.
Virus Biology
HDV is an incomplete virus that infects hepatocytes and requires the envelope protein of hepatitis B surface antigen (HBsAg) for cell exit. Infection occurs only with chronic HBV infection, either as a superinfection or simultaneous acquisition. Humans are the only known natural host.
HDV coinfection worsens HBV-induced hepatic inflammation and prognosis, and up to 80% of patients develop cirrhosis. Triple infection with the HBV virus, HDV, and HIV further increases this risk, and the global prevalence is likely underestimated.
Cancer Risk
HDV infection significantly increases the risk for HCC compared with HBV infection alone. Many patients die from decompensated cirrhosis or HCC, reflecting the aggressive nature of coinfection.
The molecular mechanisms underlying HDV oncogenesis remain unclear. Research conducted over the past 15 years has provided insights that could inform the development of more effective treatments.
Early vaccination prophylaxis is critical for reducing the risk for HCC, despite limited options.
Treatment Options
Randomized controlled trials have demonstrated antiviral efficacy for:
- Pegylated interferon alpha (Peg-IFN) is approved for HBV and is active against HDV.
- Bulevirtide, a synthetic myristoylated lipopeptide entry inhibitor, is used alone or in combination with Peg-IFN.
Suppression of HBV remains central. Nucleoside and nucleotide analogs, such as entecavir, tenofovir alafenamide fumarate, and tenofovir disoproxil fumarate, significantly reduce HCC progression in treated patients compared with untreated patients at risk.
Promising therapeutics include lonafarnib, a farnesyltransferase inhibitor that blocks HDV particle formation, and nucleic acid polymers targeting the host chaperone DNAJB12 to inhibit HBV and HDV replication.
Guideline Updates
The 2023 addendum to the S3 guidelines covers the prophylaxis, diagnosis, and treatment of HBV, including HDV management.
IARC experts also re-evaluated the human cytomegalovirus and Merkel cell polyomavirus. Complete assessments are expected in the next edition of IARC Monographs.
HBV Vaccination
HBV vaccination is the only effective prophylaxis against HBV and HDV. Introduced in 1982 for high-risk groups, it reduced chronic infections, with the WHO expanding its recommendations from 1992 onward.
Infants and young children are at the highest risk of developing this disease. Acute HBV infection often resolves in adults, but infants face up to a 90% risk of developing chronic infection. Newborns of mothers with chronic or undiagnosed HBV infections are particularly vulnerable.
Routine infant immunization includes three doses, with the first dose administered within 12 hours of birth. In Germany, the Standing Committee on Vaccination (STIKO) recommends the administration of combination vaccines, with the hexavalent vaccine administered at 2, 4, and 11 months in a 2 + 1 schedule.
Timely vaccination is crucial because undetected chronic infections often lead to late-stage HCC diagnosis. Adults in high-risk groups should receive HBV vaccination counseling.
STIKO recommends vaccination for close contacts of individuals who are HBsAg-positive, individuals with high-risk sexual contacts, immunocompromised persons, and those with preexisting conditions that increase the risk for severe HBV infection.
Since 2021, insured adults aged 35 years or older in Germany have undergone one-time HBV and HCV screening. HDV testing is recommended for all HBsAg-positive patients. Current frameworks may miss cases, and additional or personalized screening could improve the detection of previously unrecognized infections.
This story was translated from Univadis Germany.
A version of this article appeared on Medscape.com.
The International Agency for Research on Cancer (IARC) of the World Health Organization has classified hepatitis D virus (HDV) as carcinogenic, citing sufficient evidence and placing it alongside hepatitis B virus (HBV) and hepatitis C virus (HCV) as a cause of hepatocellular carcinoma (HCC).
Individuals with HBV-HDV coinfection face an elevated risk for liver cancer, highlighting the need for HBV vaccination, systematic screening, and early antiviral treatment to reduce the progression to cirrhosis and HCC.
About 12 million people globally have HBV-HDV coinfection, representing 5% of all chronic HBV cases. The prevalence of this condition varies regionally, with a likely underdiagnosis. True coinfection rates may reach 13%-14%, the highest in Europe’s Mediterranean region.
Virus Biology
HDV is an incomplete virus that infects hepatocytes and requires the envelope protein of hepatitis B surface antigen (HBsAg) for cell exit. Infection occurs only with chronic HBV infection, either as a superinfection or simultaneous acquisition. Humans are the only known natural host.
HDV coinfection worsens HBV-induced hepatic inflammation and prognosis, and up to 80% of patients develop cirrhosis. Triple infection with the HBV virus, HDV, and HIV further increases this risk, and the global prevalence is likely underestimated.
Cancer Risk
HDV infection significantly increases the risk for HCC compared with HBV infection alone. Many patients die from decompensated cirrhosis or HCC, reflecting the aggressive nature of coinfection.
The molecular mechanisms underlying HDV oncogenesis remain unclear. Research conducted over the past 15 years has provided insights that could inform the development of more effective treatments.
Early vaccination prophylaxis is critical for reducing the risk for HCC, despite limited options.
Treatment Options
Randomized controlled trials have demonstrated antiviral efficacy for:
- Pegylated interferon alpha (Peg-IFN) is approved for HBV and is active against HDV.
- Bulevirtide, a synthetic myristoylated lipopeptide entry inhibitor, is used alone or in combination with Peg-IFN.
Suppression of HBV remains central. Nucleoside and nucleotide analogs, such as entecavir, tenofovir alafenamide fumarate, and tenofovir disoproxil fumarate, significantly reduce HCC progression in treated patients compared with untreated patients at risk.
Promising therapeutics include lonafarnib, a farnesyltransferase inhibitor that blocks HDV particle formation, and nucleic acid polymers targeting the host chaperone DNAJB12 to inhibit HBV and HDV replication.
Guideline Updates
The 2023 addendum to the S3 guidelines covers the prophylaxis, diagnosis, and treatment of HBV, including HDV management.
IARC experts also re-evaluated the human cytomegalovirus and Merkel cell polyomavirus. Complete assessments are expected in the next edition of IARC Monographs.
HBV Vaccination
HBV vaccination is the only effective prophylaxis against HBV and HDV. Introduced in 1982 for high-risk groups, it reduced chronic infections, with the WHO expanding its recommendations from 1992 onward.
Infants and young children are at the highest risk of developing this disease. Acute HBV infection often resolves in adults, but infants face up to a 90% risk of developing chronic infection. Newborns of mothers with chronic or undiagnosed HBV infections are particularly vulnerable.
Routine infant immunization includes three doses, with the first dose administered within 12 hours of birth. In Germany, the Standing Committee on Vaccination (STIKO) recommends the administration of combination vaccines, with the hexavalent vaccine administered at 2, 4, and 11 months in a 2 + 1 schedule.
Timely vaccination is crucial because undetected chronic infections often lead to late-stage HCC diagnosis. Adults in high-risk groups should receive HBV vaccination counseling.
STIKO recommends vaccination for close contacts of individuals who are HBsAg-positive, individuals with high-risk sexual contacts, immunocompromised persons, and those with preexisting conditions that increase the risk for severe HBV infection.
Since 2021, insured adults aged 35 years or older in Germany have undergone one-time HBV and HCV screening. HDV testing is recommended for all HBsAg-positive patients. Current frameworks may miss cases, and additional or personalized screening could improve the detection of previously unrecognized infections.
This story was translated from Univadis Germany.
A version of this article appeared on Medscape.com.
Don't Treat Investigational Cancer Drugs Like Other Medications
Don't Treat Investigational Cancer Drugs Like Other Medications
PHOENIX – Medications used in oncology clinical trials pose unique challenges in areas such as labeling, packaging, and administration, a US Department of Veterans Affairs (VA) pharmacist cautioned colleagues, and placebos have special needs too.
Even basic safety protections can be lacking when a drug is investigational, said Emily Hennes, PharmD, BCOP, clinical pharmacy specialist for research at William S. Middleton Memorial Veterans Hospital in Shorewood Hills, Wisconsin, in a presentation at the annual meeting of the Association of VA Hematology/Oncology.
“All of the safety features that we have come to know and love in dispensing commercial drugs are absent. There’s no Tall Man lettering, there's no color differentiation, and there's no barcoding, because these are not registered drugs," she said.
A 2017 report found that 81% of pharmacists surveyed indicated some level of concern regarding the safety risk in using investigational drugs. At the same time, Hennes noted, the Joint Commission has mandated that pharmacists must control the storage, dispensing, labeling, and distribution of investigational medications.
Here are things to know about the use of investigational cancer drugs:
Drug Interactions Are Common
Hennes highlighted a 2023 study of medication reconciliation of 501 patients in 79 clinical trials that found alarming levels of drug interactions:
• 360 clinically relevant drug-drug interactions were identified among 189 patients, including 158 therapies that were prohibited by protocols. Of these, 57.7% involved cytochrome P450 enzymes, which are involved in metabolism.
• Reconciliation revealed that 35.2% of medications were not otherwise known or documented.
• A median of 2 previously unknown therapies per patient was discovered in 74% of patients.
• Alternative medicine products such as supplements and over-the-counter drugs were implicated in 60% of identified drug interactions.
• Only 41% of oncologists discussed alternative medicine use with patients, which Hennes attributed to “lack of familiarity with many alternative medicine products or insufficient training.”
To make things more complicated, “We sometimes don’t know the full pharmacokinetic and pharmacodynamic profile of an investigational agent,” she said.
Naming and Labeling May Not Be Standard
Investigational products may not have genetic names and instead have an alphanumeric identifier such as INV54826 that can be quite similar to other products, she said. Investigational drugs may even go through name changes, forcing pharmacists to be alerted to protect patients.
In addition, labeling may not be standardized. Drugs may arrive unlabeled, with the wrong volume and size, and lack of barcoding. In some cases, pharmacists choose to put new, patient-friendly labels on these products, Hennes said.
Information Distribution is Key
“Something that comes up in our practice quite a bit is that there’s no standard drug reference regarding investigational drugs,” Hennes said. “Finding ways to get key information to staff at the point of care is really critical to make sure we’re able to safely treat our patients.”
Precautions May Be Needed to Maintain Blinding Protocols
Hennes explained that pharmacists must use opaque brown bag covers to maintain blinding when parenteral products have distinctive colors. Lines may have to be covered too, which can create challenges during administration.
“Pumps aren’t meant to run lines that are covered,” she said, which can lead to jams. “If you don’t do education with your point of care staff, it can cause a lot of confusion.”
It’s also important for blinding purposes to keep an eye on how long it takes to prepare a treatment, she said. A study’s integrity, for example, could be violated if a complex investigational product takes an hour to equilibrate to room temperature and 20-30 minutes to prepare, while a placebo only requires “drawing a few mils of saline out of a bag and labeling it.”
Education for Patients Can Be Useful
Hennes urged colleagues to remind patients to save investigational medication at the end of each cycle and return it to the clinic site for accountability.
She also suggested creating treatment calendars/reminders for patients and discussing
Hennes reported no disclosures.
PHOENIX – Medications used in oncology clinical trials pose unique challenges in areas such as labeling, packaging, and administration, a US Department of Veterans Affairs (VA) pharmacist cautioned colleagues, and placebos have special needs too.
Even basic safety protections can be lacking when a drug is investigational, said Emily Hennes, PharmD, BCOP, clinical pharmacy specialist for research at William S. Middleton Memorial Veterans Hospital in Shorewood Hills, Wisconsin, in a presentation at the annual meeting of the Association of VA Hematology/Oncology.
“All of the safety features that we have come to know and love in dispensing commercial drugs are absent. There’s no Tall Man lettering, there's no color differentiation, and there's no barcoding, because these are not registered drugs," she said.
A 2017 report found that 81% of pharmacists surveyed indicated some level of concern regarding the safety risk in using investigational drugs. At the same time, Hennes noted, the Joint Commission has mandated that pharmacists must control the storage, dispensing, labeling, and distribution of investigational medications.
Here are things to know about the use of investigational cancer drugs:
Drug Interactions Are Common
Hennes highlighted a 2023 study of medication reconciliation of 501 patients in 79 clinical trials that found alarming levels of drug interactions:
• 360 clinically relevant drug-drug interactions were identified among 189 patients, including 158 therapies that were prohibited by protocols. Of these, 57.7% involved cytochrome P450 enzymes, which are involved in metabolism.
• Reconciliation revealed that 35.2% of medications were not otherwise known or documented.
• A median of 2 previously unknown therapies per patient was discovered in 74% of patients.
• Alternative medicine products such as supplements and over-the-counter drugs were implicated in 60% of identified drug interactions.
• Only 41% of oncologists discussed alternative medicine use with patients, which Hennes attributed to “lack of familiarity with many alternative medicine products or insufficient training.”
To make things more complicated, “We sometimes don’t know the full pharmacokinetic and pharmacodynamic profile of an investigational agent,” she said.
Naming and Labeling May Not Be Standard
Investigational products may not have genetic names and instead have an alphanumeric identifier such as INV54826 that can be quite similar to other products, she said. Investigational drugs may even go through name changes, forcing pharmacists to be alerted to protect patients.
In addition, labeling may not be standardized. Drugs may arrive unlabeled, with the wrong volume and size, and lack of barcoding. In some cases, pharmacists choose to put new, patient-friendly labels on these products, Hennes said.
Information Distribution is Key
“Something that comes up in our practice quite a bit is that there’s no standard drug reference regarding investigational drugs,” Hennes said. “Finding ways to get key information to staff at the point of care is really critical to make sure we’re able to safely treat our patients.”
Precautions May Be Needed to Maintain Blinding Protocols
Hennes explained that pharmacists must use opaque brown bag covers to maintain blinding when parenteral products have distinctive colors. Lines may have to be covered too, which can create challenges during administration.
“Pumps aren’t meant to run lines that are covered,” she said, which can lead to jams. “If you don’t do education with your point of care staff, it can cause a lot of confusion.”
It’s also important for blinding purposes to keep an eye on how long it takes to prepare a treatment, she said. A study’s integrity, for example, could be violated if a complex investigational product takes an hour to equilibrate to room temperature and 20-30 minutes to prepare, while a placebo only requires “drawing a few mils of saline out of a bag and labeling it.”
Education for Patients Can Be Useful
Hennes urged colleagues to remind patients to save investigational medication at the end of each cycle and return it to the clinic site for accountability.
She also suggested creating treatment calendars/reminders for patients and discussing
Hennes reported no disclosures.
PHOENIX – Medications used in oncology clinical trials pose unique challenges in areas such as labeling, packaging, and administration, a US Department of Veterans Affairs (VA) pharmacist cautioned colleagues, and placebos have special needs too.
Even basic safety protections can be lacking when a drug is investigational, said Emily Hennes, PharmD, BCOP, clinical pharmacy specialist for research at William S. Middleton Memorial Veterans Hospital in Shorewood Hills, Wisconsin, in a presentation at the annual meeting of the Association of VA Hematology/Oncology.
“All of the safety features that we have come to know and love in dispensing commercial drugs are absent. There’s no Tall Man lettering, there's no color differentiation, and there's no barcoding, because these are not registered drugs," she said.
A 2017 report found that 81% of pharmacists surveyed indicated some level of concern regarding the safety risk in using investigational drugs. At the same time, Hennes noted, the Joint Commission has mandated that pharmacists must control the storage, dispensing, labeling, and distribution of investigational medications.
Here are things to know about the use of investigational cancer drugs:
Drug Interactions Are Common
Hennes highlighted a 2023 study of medication reconciliation of 501 patients in 79 clinical trials that found alarming levels of drug interactions:
• 360 clinically relevant drug-drug interactions were identified among 189 patients, including 158 therapies that were prohibited by protocols. Of these, 57.7% involved cytochrome P450 enzymes, which are involved in metabolism.
• Reconciliation revealed that 35.2% of medications were not otherwise known or documented.
• A median of 2 previously unknown therapies per patient was discovered in 74% of patients.
• Alternative medicine products such as supplements and over-the-counter drugs were implicated in 60% of identified drug interactions.
• Only 41% of oncologists discussed alternative medicine use with patients, which Hennes attributed to “lack of familiarity with many alternative medicine products or insufficient training.”
To make things more complicated, “We sometimes don’t know the full pharmacokinetic and pharmacodynamic profile of an investigational agent,” she said.
Naming and Labeling May Not Be Standard
Investigational products may not have genetic names and instead have an alphanumeric identifier such as INV54826 that can be quite similar to other products, she said. Investigational drugs may even go through name changes, forcing pharmacists to be alerted to protect patients.
In addition, labeling may not be standardized. Drugs may arrive unlabeled, with the wrong volume and size, and lack of barcoding. In some cases, pharmacists choose to put new, patient-friendly labels on these products, Hennes said.
Information Distribution is Key
“Something that comes up in our practice quite a bit is that there’s no standard drug reference regarding investigational drugs,” Hennes said. “Finding ways to get key information to staff at the point of care is really critical to make sure we’re able to safely treat our patients.”
Precautions May Be Needed to Maintain Blinding Protocols
Hennes explained that pharmacists must use opaque brown bag covers to maintain blinding when parenteral products have distinctive colors. Lines may have to be covered too, which can create challenges during administration.
“Pumps aren’t meant to run lines that are covered,” she said, which can lead to jams. “If you don’t do education with your point of care staff, it can cause a lot of confusion.”
It’s also important for blinding purposes to keep an eye on how long it takes to prepare a treatment, she said. A study’s integrity, for example, could be violated if a complex investigational product takes an hour to equilibrate to room temperature and 20-30 minutes to prepare, while a placebo only requires “drawing a few mils of saline out of a bag and labeling it.”
Education for Patients Can Be Useful
Hennes urged colleagues to remind patients to save investigational medication at the end of each cycle and return it to the clinic site for accountability.
She also suggested creating treatment calendars/reminders for patients and discussing
Hennes reported no disclosures.
Don't Treat Investigational Cancer Drugs Like Other Medications
Don't Treat Investigational Cancer Drugs Like Other Medications
Does Ethnicity Affect Skin Cancer Risk?
Does Ethnicity Affect Skin Cancer Risk?
TOPLINE:
The incidence of skin cancer in England varied by ethnicity: White individuals had higher rates of melanoma, cutaneous squamous cell carcinoma, and basal cell carcinoma than Asian or Black individuals. In contrast, acral lentiginous melanoma was most common among Black individuals, whereas cutaneous T-cell lymphoma and Kaposi sarcoma were highest among those in the "Other" ethnic group.
METHODOLOGY:
- Researchers analysed all cases of cutaneous melanoma (melanoma and acral lentiginous melanoma), basal cell carcinoma, cutaneous squamous cell carcinoma, cutaneous T-cell lymphoma, and Kaposi sarcoma using data from the NHS National Disease Registration Service cancer registry between 2013 and 2020.
- Data collection incorporated ethnicity information from multiple health care datasets, including Clinical Outcomes and Services Dataset, Patient Administration System, Radiotherapy Dataset, Diagnostic Imaging Dataset, and Hospital Episode Statistics.
- A population analysis categorised patients into 7 standardised ethnic groups (on the basis of Office for National Statistics classifications): White, Asian, Chinese, Black, mixed, other, and unknown groups, with ethnicity data being self-reported by patients.
- Outcomes included European age-standardised rates calculated using the 2013 European Standard Population and reported per 100,000 person-years (PYs).
TAKEAWAY:
- White Individuals had 13-fold higher rates of cutaneous squamous cell carcinoma (61.75 per 100,000 PYs), 26-fold and 27-fold higher rates of basal cell carcinoma (153.69 per 100,000 PYs), and 33-fold and 16-fold higher rates of cutaneous melanoma (27.29 per 100,000 PYs) than Asian and Black individuals, respectively.
- Black individuals had the highest incidence of acral lentiginous melanoma (0.85 per 100,000 PYs), and those in the other ethnic group had the highest incidence of cutaneous T-cell lymphoma (1.74 per 100,000 PYs) and Kaposi sarcoma (1.57 per 100,000 PYs).
- The presentation of early-stage melanoma was low among Asian (53.5%), Black (62.4%), mixed (62.5%), and other (76.4%) ethnic groups compared to that among White ethnicities (79.8%).
- Acral lentiginous melanomas were less likely to get urgent suspected cancer pathway referrals than overall melanoma (40.1% vs 44.6%; P < .001) and more likely to be diagnosed late than overall melanoma (stage I/II at diagnosis; 72% vs 80%; P < .0001).
IN PRACTICE:
"The findings emphasise the need for better, targeted ethnicity data collection strategies to address incidence, outcomes and health care equity for not just skin cancer but all health conditions in underserved populations," the authors wrote. "While projects like the Global Burden of Disease have improved global health care reporting, continuous audit and improvement of collected data are essential to provide better care across people of all ethnicities."
SOURCE:
This study was led by Shehnaz Ahmed, British Association of Dermatologists, London, England. It was published online on September 10, 2025, in the British Journal of Dermatology.
LIMITATIONS:
Census data collection after every 10 years could have contributed to inaccurate population estimates and incidence rates. Small sample sizes in certain ethnic groups could have led to potential confounders, requiring a cautious interpretation of relative incidence. The NHS data included only self-reported ethnicity data with no available details of skin phototypes, skin tones, or racial ancestry. This study lacked granular ethnicity census data and stage data for basal cell carcinoma, cutaneous small cell carcinoma, and Kaposi sarcoma.
DISCLOSURES:
This research was supported through a partnership between the British Association of Dermatologists and NHS England's National Disease Registration Service. Two authors reported being employees of the British Association of Dermatologists.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
The incidence of skin cancer in England varied by ethnicity: White individuals had higher rates of melanoma, cutaneous squamous cell carcinoma, and basal cell carcinoma than Asian or Black individuals. In contrast, acral lentiginous melanoma was most common among Black individuals, whereas cutaneous T-cell lymphoma and Kaposi sarcoma were highest among those in the "Other" ethnic group.
METHODOLOGY:
- Researchers analysed all cases of cutaneous melanoma (melanoma and acral lentiginous melanoma), basal cell carcinoma, cutaneous squamous cell carcinoma, cutaneous T-cell lymphoma, and Kaposi sarcoma using data from the NHS National Disease Registration Service cancer registry between 2013 and 2020.
- Data collection incorporated ethnicity information from multiple health care datasets, including Clinical Outcomes and Services Dataset, Patient Administration System, Radiotherapy Dataset, Diagnostic Imaging Dataset, and Hospital Episode Statistics.
- A population analysis categorised patients into 7 standardised ethnic groups (on the basis of Office for National Statistics classifications): White, Asian, Chinese, Black, mixed, other, and unknown groups, with ethnicity data being self-reported by patients.
- Outcomes included European age-standardised rates calculated using the 2013 European Standard Population and reported per 100,000 person-years (PYs).
TAKEAWAY:
- White Individuals had 13-fold higher rates of cutaneous squamous cell carcinoma (61.75 per 100,000 PYs), 26-fold and 27-fold higher rates of basal cell carcinoma (153.69 per 100,000 PYs), and 33-fold and 16-fold higher rates of cutaneous melanoma (27.29 per 100,000 PYs) than Asian and Black individuals, respectively.
- Black individuals had the highest incidence of acral lentiginous melanoma (0.85 per 100,000 PYs), and those in the other ethnic group had the highest incidence of cutaneous T-cell lymphoma (1.74 per 100,000 PYs) and Kaposi sarcoma (1.57 per 100,000 PYs).
- The presentation of early-stage melanoma was low among Asian (53.5%), Black (62.4%), mixed (62.5%), and other (76.4%) ethnic groups compared to that among White ethnicities (79.8%).
- Acral lentiginous melanomas were less likely to get urgent suspected cancer pathway referrals than overall melanoma (40.1% vs 44.6%; P < .001) and more likely to be diagnosed late than overall melanoma (stage I/II at diagnosis; 72% vs 80%; P < .0001).
IN PRACTICE:
"The findings emphasise the need for better, targeted ethnicity data collection strategies to address incidence, outcomes and health care equity for not just skin cancer but all health conditions in underserved populations," the authors wrote. "While projects like the Global Burden of Disease have improved global health care reporting, continuous audit and improvement of collected data are essential to provide better care across people of all ethnicities."
SOURCE:
This study was led by Shehnaz Ahmed, British Association of Dermatologists, London, England. It was published online on September 10, 2025, in the British Journal of Dermatology.
LIMITATIONS:
Census data collection after every 10 years could have contributed to inaccurate population estimates and incidence rates. Small sample sizes in certain ethnic groups could have led to potential confounders, requiring a cautious interpretation of relative incidence. The NHS data included only self-reported ethnicity data with no available details of skin phototypes, skin tones, or racial ancestry. This study lacked granular ethnicity census data and stage data for basal cell carcinoma, cutaneous small cell carcinoma, and Kaposi sarcoma.
DISCLOSURES:
This research was supported through a partnership between the British Association of Dermatologists and NHS England's National Disease Registration Service. Two authors reported being employees of the British Association of Dermatologists.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
The incidence of skin cancer in England varied by ethnicity: White individuals had higher rates of melanoma, cutaneous squamous cell carcinoma, and basal cell carcinoma than Asian or Black individuals. In contrast, acral lentiginous melanoma was most common among Black individuals, whereas cutaneous T-cell lymphoma and Kaposi sarcoma were highest among those in the "Other" ethnic group.
METHODOLOGY:
- Researchers analysed all cases of cutaneous melanoma (melanoma and acral lentiginous melanoma), basal cell carcinoma, cutaneous squamous cell carcinoma, cutaneous T-cell lymphoma, and Kaposi sarcoma using data from the NHS National Disease Registration Service cancer registry between 2013 and 2020.
- Data collection incorporated ethnicity information from multiple health care datasets, including Clinical Outcomes and Services Dataset, Patient Administration System, Radiotherapy Dataset, Diagnostic Imaging Dataset, and Hospital Episode Statistics.
- A population analysis categorised patients into 7 standardised ethnic groups (on the basis of Office for National Statistics classifications): White, Asian, Chinese, Black, mixed, other, and unknown groups, with ethnicity data being self-reported by patients.
- Outcomes included European age-standardised rates calculated using the 2013 European Standard Population and reported per 100,000 person-years (PYs).
TAKEAWAY:
- White Individuals had 13-fold higher rates of cutaneous squamous cell carcinoma (61.75 per 100,000 PYs), 26-fold and 27-fold higher rates of basal cell carcinoma (153.69 per 100,000 PYs), and 33-fold and 16-fold higher rates of cutaneous melanoma (27.29 per 100,000 PYs) than Asian and Black individuals, respectively.
- Black individuals had the highest incidence of acral lentiginous melanoma (0.85 per 100,000 PYs), and those in the other ethnic group had the highest incidence of cutaneous T-cell lymphoma (1.74 per 100,000 PYs) and Kaposi sarcoma (1.57 per 100,000 PYs).
- The presentation of early-stage melanoma was low among Asian (53.5%), Black (62.4%), mixed (62.5%), and other (76.4%) ethnic groups compared to that among White ethnicities (79.8%).
- Acral lentiginous melanomas were less likely to get urgent suspected cancer pathway referrals than overall melanoma (40.1% vs 44.6%; P < .001) and more likely to be diagnosed late than overall melanoma (stage I/II at diagnosis; 72% vs 80%; P < .0001).
IN PRACTICE:
"The findings emphasise the need for better, targeted ethnicity data collection strategies to address incidence, outcomes and health care equity for not just skin cancer but all health conditions in underserved populations," the authors wrote. "While projects like the Global Burden of Disease have improved global health care reporting, continuous audit and improvement of collected data are essential to provide better care across people of all ethnicities."
SOURCE:
This study was led by Shehnaz Ahmed, British Association of Dermatologists, London, England. It was published online on September 10, 2025, in the British Journal of Dermatology.
LIMITATIONS:
Census data collection after every 10 years could have contributed to inaccurate population estimates and incidence rates. Small sample sizes in certain ethnic groups could have led to potential confounders, requiring a cautious interpretation of relative incidence. The NHS data included only self-reported ethnicity data with no available details of skin phototypes, skin tones, or racial ancestry. This study lacked granular ethnicity census data and stage data for basal cell carcinoma, cutaneous small cell carcinoma, and Kaposi sarcoma.
DISCLOSURES:
This research was supported through a partnership between the British Association of Dermatologists and NHS England's National Disease Registration Service. Two authors reported being employees of the British Association of Dermatologists.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
Does Ethnicity Affect Skin Cancer Risk?
Does Ethnicity Affect Skin Cancer Risk?
Architect of VA Transformation Urges Innovation Amid Uncertainty
Architect of VA Transformation Urges Innovation Amid Uncertainty
PHOENIX – Three decades after he initiated the transformation of the Veterans Health Administration (VHA) into a model research and clinical health care system, former US Department of Veterans Affairs (VA) Under Secretary of Health Kenneth W. Kizer, MD, MPH, urged cancer specialists to embrace this challenging moment as an opportunity for bold innovation.
At the annual meeting of the Association of VA Hematology/Oncology (AVAHO), Kizer acknowledged that the VA faces an “uncertain and turbulent time” in areas such as funding, staffing, community care implementation, and the rollout of a new electronic health record system.
He also noted the grim rise of global instability, economic turmoil, climate change, infectious diseases, political violence, and mass shootings.
“This can be stressful. It can create negative energy. But this uncertainty can also be liberating, and it can prompt positive energy and innovation, depending on choices that we make,” said Kizer, who also has served as California’s top health official prior to leading the VHA from 1994 to 1999.
From “Bloated Bureaucracy’ to High-Quality Health Care System
Kizer has been credited with revitalizing VHA care through a greater commitment to quality, and harkened to his work with the VA as an example of how bold goals can lead to bold innovation.
“What were the perceptions of VA health care in 1994? Well, they weren’t very good, frankly,” Kizer recalled. He described the VA as having a reputation at that time as “highly dysfunctional” with “a very bloated and entrenched bureaucracy.” As for quality of care, it “wasn’t viewed as very good.”
The system’s problems were so severe that patients would park motorhomes in VA medical center parking lots as they waited for care. “While they might have an appointment for one day, they may not be seen for 3 or 4 or 5 days. So they would stay in their motorhome until they finally got into their clinic appointment,” Kizer said.
Overall, “the public viewed the VA as this bleak backwater of incompetence and difference and inefficiency, and there were very strong calls to privatize the VA,” Kizer said.
Kizer asked colleagues about what he should do after he was asked to take the under secretary job. “With one exception, they all said, don’t go near it. Don’t touch it. Walk away. That it’s impossible to change the organization.
“I looked at the VA and I saw an opportunity. When I told [members of the President Bill] Clinton [Administration] yes, my bold aim was that I would like to pursue this was to make VHA a model of excellent health care, an exemplary health care system. Most everyone else thought that I was totally delusional, but sometimes it’s good to be delusional.”
Revolutionary Changes Despite Opposition
Kizer sought reforms in 5 major strategic objectives, all without explicit congressional approval: creating an accountable management structure, decentralizing decision-making, integrating care, implementing universal primary care, and pursuing eligibility reform to create the current 8-tier VA system.
One major innovation was the implementation of community-based outpatient clinics (CBOCs): “Those were strongly opposed initially,” Kizer said. “Everyone, the veteran community in particular, had been led to believe that the only good care was in the hospital.”
The resistance was substantial. “There was a lot of opposition when we said we’re going to move out into the community where you live to make [care] easier to access,” Kizer said.
To make things more difficult, Congress wouldn’t fund the project: “For the first 3 years, every CBOC had to be funded by redirected savings from other things that we could do within the system,” he said. “All of this was through redirected savings and finding ways to save and reinvest.”
Innovation From the Ground Up
Kizer emphasized that many breakthrough innovations came from frontline staff rather than executive mandates. He cited the example of Barcode Medication Administration, which originated from a nurse in Topeka, Kan.
The nurse saw a barcode scanner put to work at a rental car company where it was used to check cars in and out. She wondered, “Why can’t we do this with medications when they’re given on the floor? We followed up on it, pursued those things, tested it out, it worked.”
The results were dramatic. “I was told at a meeting that they had achieved close to 80% reduction in medication errors,” Kizer said. After verifying the results personally, he “authorized $20 million, and we moved forward with it systemwide.”
This experience reinforced his belief in harvesting ideas from staff at all levels.
Innovation remains part of the VA’s culture “despite what some people would have you believe,” Kizer said. Recently, the VA has made major advances in areas such as patient transportation and the climate crisis, he said.
Inside the Recipe for Innovation
Boldness, persistence, adaptability, and tolerance for risk are necessary ingredients for high-risk goals, Kizer said. Ambition is also part of the picture.
He highlighted examples such as the Apollo moon landing, the first sub-4-minute mile, and the first swim across the English Channel by a woman.
In medicine, Kizer pointed to a national patient safety campaign that saved an estimated 122,000 lives. He also mentioned recent progress in organ transplantation such as recommendations from the National Academies of Sciences, Engineering, and Medicine to establish national performance goals and the Organ Procurement and Transplantation Network’s target of 60,000 deceased donor transplants by 2026.
Bold doesn’t mean being reckless or careless, Kizer said. “But it does require innovation. And it does require that you try some new things, some of which aren’t going to work out.”
The key mindset, he explained, is to “embrace the unknown” because “you often really don’t know how you will accomplish the aim when you start. But you’ll figure it out as you go.”
Kizer highlighted 2 opposing strategies to handling challenging times.
According to him, the “negative energy” approach focuses on frustrations, limitations, and asking “Why is this happening to me?”
In contrast, a “positive energy” approach expects problems, focuses on available resources and capabilities, and asks, “What are the opportunities that these changes are creating for me?”
Kizer made it crystal clear which option he prefers.
Dr. Kizer disclosed that his comments represent his opinions only, and he noted his ongoing connections to the VA.
PHOENIX – Three decades after he initiated the transformation of the Veterans Health Administration (VHA) into a model research and clinical health care system, former US Department of Veterans Affairs (VA) Under Secretary of Health Kenneth W. Kizer, MD, MPH, urged cancer specialists to embrace this challenging moment as an opportunity for bold innovation.
At the annual meeting of the Association of VA Hematology/Oncology (AVAHO), Kizer acknowledged that the VA faces an “uncertain and turbulent time” in areas such as funding, staffing, community care implementation, and the rollout of a new electronic health record system.
He also noted the grim rise of global instability, economic turmoil, climate change, infectious diseases, political violence, and mass shootings.
“This can be stressful. It can create negative energy. But this uncertainty can also be liberating, and it can prompt positive energy and innovation, depending on choices that we make,” said Kizer, who also has served as California’s top health official prior to leading the VHA from 1994 to 1999.
From “Bloated Bureaucracy’ to High-Quality Health Care System
Kizer has been credited with revitalizing VHA care through a greater commitment to quality, and harkened to his work with the VA as an example of how bold goals can lead to bold innovation.
“What were the perceptions of VA health care in 1994? Well, they weren’t very good, frankly,” Kizer recalled. He described the VA as having a reputation at that time as “highly dysfunctional” with “a very bloated and entrenched bureaucracy.” As for quality of care, it “wasn’t viewed as very good.”
The system’s problems were so severe that patients would park motorhomes in VA medical center parking lots as they waited for care. “While they might have an appointment for one day, they may not be seen for 3 or 4 or 5 days. So they would stay in their motorhome until they finally got into their clinic appointment,” Kizer said.
Overall, “the public viewed the VA as this bleak backwater of incompetence and difference and inefficiency, and there were very strong calls to privatize the VA,” Kizer said.
Kizer asked colleagues about what he should do after he was asked to take the under secretary job. “With one exception, they all said, don’t go near it. Don’t touch it. Walk away. That it’s impossible to change the organization.
“I looked at the VA and I saw an opportunity. When I told [members of the President Bill] Clinton [Administration] yes, my bold aim was that I would like to pursue this was to make VHA a model of excellent health care, an exemplary health care system. Most everyone else thought that I was totally delusional, but sometimes it’s good to be delusional.”
Revolutionary Changes Despite Opposition
Kizer sought reforms in 5 major strategic objectives, all without explicit congressional approval: creating an accountable management structure, decentralizing decision-making, integrating care, implementing universal primary care, and pursuing eligibility reform to create the current 8-tier VA system.
One major innovation was the implementation of community-based outpatient clinics (CBOCs): “Those were strongly opposed initially,” Kizer said. “Everyone, the veteran community in particular, had been led to believe that the only good care was in the hospital.”
The resistance was substantial. “There was a lot of opposition when we said we’re going to move out into the community where you live to make [care] easier to access,” Kizer said.
To make things more difficult, Congress wouldn’t fund the project: “For the first 3 years, every CBOC had to be funded by redirected savings from other things that we could do within the system,” he said. “All of this was through redirected savings and finding ways to save and reinvest.”
Innovation From the Ground Up
Kizer emphasized that many breakthrough innovations came from frontline staff rather than executive mandates. He cited the example of Barcode Medication Administration, which originated from a nurse in Topeka, Kan.
The nurse saw a barcode scanner put to work at a rental car company where it was used to check cars in and out. She wondered, “Why can’t we do this with medications when they’re given on the floor? We followed up on it, pursued those things, tested it out, it worked.”
The results were dramatic. “I was told at a meeting that they had achieved close to 80% reduction in medication errors,” Kizer said. After verifying the results personally, he “authorized $20 million, and we moved forward with it systemwide.”
This experience reinforced his belief in harvesting ideas from staff at all levels.
Innovation remains part of the VA’s culture “despite what some people would have you believe,” Kizer said. Recently, the VA has made major advances in areas such as patient transportation and the climate crisis, he said.
Inside the Recipe for Innovation
Boldness, persistence, adaptability, and tolerance for risk are necessary ingredients for high-risk goals, Kizer said. Ambition is also part of the picture.
He highlighted examples such as the Apollo moon landing, the first sub-4-minute mile, and the first swim across the English Channel by a woman.
In medicine, Kizer pointed to a national patient safety campaign that saved an estimated 122,000 lives. He also mentioned recent progress in organ transplantation such as recommendations from the National Academies of Sciences, Engineering, and Medicine to establish national performance goals and the Organ Procurement and Transplantation Network’s target of 60,000 deceased donor transplants by 2026.
Bold doesn’t mean being reckless or careless, Kizer said. “But it does require innovation. And it does require that you try some new things, some of which aren’t going to work out.”
The key mindset, he explained, is to “embrace the unknown” because “you often really don’t know how you will accomplish the aim when you start. But you’ll figure it out as you go.”
Kizer highlighted 2 opposing strategies to handling challenging times.
According to him, the “negative energy” approach focuses on frustrations, limitations, and asking “Why is this happening to me?”
In contrast, a “positive energy” approach expects problems, focuses on available resources and capabilities, and asks, “What are the opportunities that these changes are creating for me?”
Kizer made it crystal clear which option he prefers.
Dr. Kizer disclosed that his comments represent his opinions only, and he noted his ongoing connections to the VA.
PHOENIX – Three decades after he initiated the transformation of the Veterans Health Administration (VHA) into a model research and clinical health care system, former US Department of Veterans Affairs (VA) Under Secretary of Health Kenneth W. Kizer, MD, MPH, urged cancer specialists to embrace this challenging moment as an opportunity for bold innovation.
At the annual meeting of the Association of VA Hematology/Oncology (AVAHO), Kizer acknowledged that the VA faces an “uncertain and turbulent time” in areas such as funding, staffing, community care implementation, and the rollout of a new electronic health record system.
He also noted the grim rise of global instability, economic turmoil, climate change, infectious diseases, political violence, and mass shootings.
“This can be stressful. It can create negative energy. But this uncertainty can also be liberating, and it can prompt positive energy and innovation, depending on choices that we make,” said Kizer, who also has served as California’s top health official prior to leading the VHA from 1994 to 1999.
From “Bloated Bureaucracy’ to High-Quality Health Care System
Kizer has been credited with revitalizing VHA care through a greater commitment to quality, and harkened to his work with the VA as an example of how bold goals can lead to bold innovation.
“What were the perceptions of VA health care in 1994? Well, they weren’t very good, frankly,” Kizer recalled. He described the VA as having a reputation at that time as “highly dysfunctional” with “a very bloated and entrenched bureaucracy.” As for quality of care, it “wasn’t viewed as very good.”
The system’s problems were so severe that patients would park motorhomes in VA medical center parking lots as they waited for care. “While they might have an appointment for one day, they may not be seen for 3 or 4 or 5 days. So they would stay in their motorhome until they finally got into their clinic appointment,” Kizer said.
Overall, “the public viewed the VA as this bleak backwater of incompetence and difference and inefficiency, and there were very strong calls to privatize the VA,” Kizer said.
Kizer asked colleagues about what he should do after he was asked to take the under secretary job. “With one exception, they all said, don’t go near it. Don’t touch it. Walk away. That it’s impossible to change the organization.
“I looked at the VA and I saw an opportunity. When I told [members of the President Bill] Clinton [Administration] yes, my bold aim was that I would like to pursue this was to make VHA a model of excellent health care, an exemplary health care system. Most everyone else thought that I was totally delusional, but sometimes it’s good to be delusional.”
Revolutionary Changes Despite Opposition
Kizer sought reforms in 5 major strategic objectives, all without explicit congressional approval: creating an accountable management structure, decentralizing decision-making, integrating care, implementing universal primary care, and pursuing eligibility reform to create the current 8-tier VA system.
One major innovation was the implementation of community-based outpatient clinics (CBOCs): “Those were strongly opposed initially,” Kizer said. “Everyone, the veteran community in particular, had been led to believe that the only good care was in the hospital.”
The resistance was substantial. “There was a lot of opposition when we said we’re going to move out into the community where you live to make [care] easier to access,” Kizer said.
To make things more difficult, Congress wouldn’t fund the project: “For the first 3 years, every CBOC had to be funded by redirected savings from other things that we could do within the system,” he said. “All of this was through redirected savings and finding ways to save and reinvest.”
Innovation From the Ground Up
Kizer emphasized that many breakthrough innovations came from frontline staff rather than executive mandates. He cited the example of Barcode Medication Administration, which originated from a nurse in Topeka, Kan.
The nurse saw a barcode scanner put to work at a rental car company where it was used to check cars in and out. She wondered, “Why can’t we do this with medications when they’re given on the floor? We followed up on it, pursued those things, tested it out, it worked.”
The results were dramatic. “I was told at a meeting that they had achieved close to 80% reduction in medication errors,” Kizer said. After verifying the results personally, he “authorized $20 million, and we moved forward with it systemwide.”
This experience reinforced his belief in harvesting ideas from staff at all levels.
Innovation remains part of the VA’s culture “despite what some people would have you believe,” Kizer said. Recently, the VA has made major advances in areas such as patient transportation and the climate crisis, he said.
Inside the Recipe for Innovation
Boldness, persistence, adaptability, and tolerance for risk are necessary ingredients for high-risk goals, Kizer said. Ambition is also part of the picture.
He highlighted examples such as the Apollo moon landing, the first sub-4-minute mile, and the first swim across the English Channel by a woman.
In medicine, Kizer pointed to a national patient safety campaign that saved an estimated 122,000 lives. He also mentioned recent progress in organ transplantation such as recommendations from the National Academies of Sciences, Engineering, and Medicine to establish national performance goals and the Organ Procurement and Transplantation Network’s target of 60,000 deceased donor transplants by 2026.
Bold doesn’t mean being reckless or careless, Kizer said. “But it does require innovation. And it does require that you try some new things, some of which aren’t going to work out.”
The key mindset, he explained, is to “embrace the unknown” because “you often really don’t know how you will accomplish the aim when you start. But you’ll figure it out as you go.”
Kizer highlighted 2 opposing strategies to handling challenging times.
According to him, the “negative energy” approach focuses on frustrations, limitations, and asking “Why is this happening to me?”
In contrast, a “positive energy” approach expects problems, focuses on available resources and capabilities, and asks, “What are the opportunities that these changes are creating for me?”
Kizer made it crystal clear which option he prefers.
Dr. Kizer disclosed that his comments represent his opinions only, and he noted his ongoing connections to the VA.
Architect of VA Transformation Urges Innovation Amid Uncertainty
Architect of VA Transformation Urges Innovation Amid Uncertainty
ERCC2, KDM6A, and TERT as Key Prognostic Factors in Bladder Cancer: Insights from the AACR Project GENIE Database
Background
Urothelial carcinoma (UC) is among the top 10 frequently diagnosed cancers in the world. Mutations in FGFR3, ARID1A, and TP53 are well documented as being some of the most frequent mutations found in UC. Despite advances in treatment, survival outcomes remain poor, especially in advanced stages. To promote future pharmacotherapeutic development, the molecular understanding of UC needs to be continually updated using more recently available databases.
Methods
This study utilizes the AACR Project GENIE database from the American Association for Cancer Research to explore the mutational profiles of patients with UC. Gene mutation frequencies were calculated, and two Kaplan-Meier curves were drawn for each gene, showing one curve for patients with the mutation and one for those without. Log-Rank tests were calculated with subsequent FDR (Benjamini–Hochberg) correction applied to account for multiple hypothesis testing. Data was analyzed using R 4.4.2 and statistical significance was set at α = 0.05.
Results
In this study, 4525 patients had histology consistent with UC. The 5 most common mutations were TERT (n = 1714, 37.9%), TP53 (n = 1689, 37.3%), KDM6A (n = 1091, 24.1%), ARID1A (n = 872, 19.3%), and FGFR3 (n = 762, 16.8%). Mutations associated with differential survival outcomes included ERCC2 (mutated n = 387, wild type n = 3751, p < 0.0001), KDM6A (mutated n = 1091, wild type n = 3047, p < 0.0001), TERT (mutated n = 1714, wild type n = 2424), and TP53 (mutated n = 1689, wild type n = 2449, p < 0.0001).
Conclusions
Interestingly, while mutations in TP53 and ERCC2 were associated with shorter median survival, mutations in KDM6A and TERT were associated with longer median survival.
Background
Urothelial carcinoma (UC) is among the top 10 frequently diagnosed cancers in the world. Mutations in FGFR3, ARID1A, and TP53 are well documented as being some of the most frequent mutations found in UC. Despite advances in treatment, survival outcomes remain poor, especially in advanced stages. To promote future pharmacotherapeutic development, the molecular understanding of UC needs to be continually updated using more recently available databases.
Methods
This study utilizes the AACR Project GENIE database from the American Association for Cancer Research to explore the mutational profiles of patients with UC. Gene mutation frequencies were calculated, and two Kaplan-Meier curves were drawn for each gene, showing one curve for patients with the mutation and one for those without. Log-Rank tests were calculated with subsequent FDR (Benjamini–Hochberg) correction applied to account for multiple hypothesis testing. Data was analyzed using R 4.4.2 and statistical significance was set at α = 0.05.
Results
In this study, 4525 patients had histology consistent with UC. The 5 most common mutations were TERT (n = 1714, 37.9%), TP53 (n = 1689, 37.3%), KDM6A (n = 1091, 24.1%), ARID1A (n = 872, 19.3%), and FGFR3 (n = 762, 16.8%). Mutations associated with differential survival outcomes included ERCC2 (mutated n = 387, wild type n = 3751, p < 0.0001), KDM6A (mutated n = 1091, wild type n = 3047, p < 0.0001), TERT (mutated n = 1714, wild type n = 2424), and TP53 (mutated n = 1689, wild type n = 2449, p < 0.0001).
Conclusions
Interestingly, while mutations in TP53 and ERCC2 were associated with shorter median survival, mutations in KDM6A and TERT were associated with longer median survival.
Background
Urothelial carcinoma (UC) is among the top 10 frequently diagnosed cancers in the world. Mutations in FGFR3, ARID1A, and TP53 are well documented as being some of the most frequent mutations found in UC. Despite advances in treatment, survival outcomes remain poor, especially in advanced stages. To promote future pharmacotherapeutic development, the molecular understanding of UC needs to be continually updated using more recently available databases.
Methods
This study utilizes the AACR Project GENIE database from the American Association for Cancer Research to explore the mutational profiles of patients with UC. Gene mutation frequencies were calculated, and two Kaplan-Meier curves were drawn for each gene, showing one curve for patients with the mutation and one for those without. Log-Rank tests were calculated with subsequent FDR (Benjamini–Hochberg) correction applied to account for multiple hypothesis testing. Data was analyzed using R 4.4.2 and statistical significance was set at α = 0.05.
Results
In this study, 4525 patients had histology consistent with UC. The 5 most common mutations were TERT (n = 1714, 37.9%), TP53 (n = 1689, 37.3%), KDM6A (n = 1091, 24.1%), ARID1A (n = 872, 19.3%), and FGFR3 (n = 762, 16.8%). Mutations associated with differential survival outcomes included ERCC2 (mutated n = 387, wild type n = 3751, p < 0.0001), KDM6A (mutated n = 1091, wild type n = 3047, p < 0.0001), TERT (mutated n = 1714, wild type n = 2424), and TP53 (mutated n = 1689, wild type n = 2449, p < 0.0001).
Conclusions
Interestingly, while mutations in TP53 and ERCC2 were associated with shorter median survival, mutations in KDM6A and TERT were associated with longer median survival.