User login
Remote ischemic preconditioning does no good
Remote ischemic preconditioning failed to improve outcomes among higher-risk patients undergoing elective cardiac surgery in two separate large clinical trials reported online Oct. 5 in the New England Journal of Medicine.
Both studies clearly showed that the technique did not provide greater protection of the heart, brain, or kidneys than did a sham technique, failing to improve any of the numerous primary or secondary endpoints or to produce a benefit in any of several subgroups of patients.
Remote ischemic preconditioning involves protecting the heart and other organs against surgery-related acute ischemia/reperfusion injury by first applying brief cycles of ischemia and reperfusion to a remote organ or tissue. It is thought that this stimulus produces a blood-borne response that conveys a protective effect from the remote area to the target organs. This remote preconditioning can be accomplished noninvasively by inflating and deflating a standard blood pressure cuff on the upper arm or thigh for brief periods.
Some early studies indicated that using this technique during cardiovascular surgery improved serum cardiac and renal biomarkers, which implied protection of these organs against ischemia/reperfusion injury. But more recent prospective clinical trials have shown no such benefit. None of these studies were adequately powered to assess the effect on hard clinical endpoints, and most were single center, unblinded, and had no standardized anesthesia regimen.
RIPHeart study
To address these study limitations, the RIPHeart Study investigators performed a prospective double-blind controlled trial among 1,385 adults undergoing elective cardiovascular surgery requiring cardiopulmonary bypass at 14 university hospitals in Germany during a 3-year period. The participants had a mean EuroSCORE (European System for Cardiac Operative Risk Evaluation) of 6 or higher, indicating that most of them were at higher than average risk, and all received the same anesthetic, intravenous propofol. A total of 692 patients were randomly assigned to undergo four 5-minute cycles of upper-arm ischemia/reperfusion after being anesthetized and 693 to undergo sham ischemia/reperfusion on a dummy arm hidden by surgical drapes, said Dr. Patrick Meybohm of the department of anesthesiology, intensive care medicine, and pain therapy at University Hospital Frankfurt and his associates.
The primary endpoint – a composite of death from any cause, nonfatal MI, stroke, or acute renal failure before hospital discharge – occurred in 14.3% of the intervention group and 14.6% of the control group, a nonsignificant difference. Furthermore, no significant differences between the two study groups were seen in any of the individual components of this composite measure, or in any secondary endpoints such as duration of mechanical ventilation, ICU length of stay, hospital length of stay, troponin levels, creatinine levels, onset of atrial fibrillation, or incidence of postoperative delirium. All outcome measures remained similar between the two study groups at 30-day, 90-day, and 1-year follow-ups (N Engl J Med 2015 Oct 5. doi: 10.1056/NEJMoa1413579).
In addition, estimated event-free survival at 30 days was 85.2% with the true intervention and 85.0% with the sham intervention, another nonsignificant difference. These estimates remained similar between the two study groups at 90 days and 1 year. The findings of the primary analysis were confirmed in the “completely concordant” per-protocol analysis, Dr. Meybohm and his associates noted.
ERICCA trial
In the Effect of Remote Ischemic Preconditioning on Clinical Outcomes in Patients Undergoing CABG (ERICCA) study, investigators assessed 1,612 adults undergoing on-pump CABG (with or without valve surgery) using blood cardioplegia at 30 cardiac surgery centers in the United Kingdom during a 3-year period. These patients were randomly assigned to undergo remote ischemic preconditioning with a standard blood pressure cuff on the upper arm for four 5-minute cycles (801 participants) or a sham procedure using a deactivated blood pressure cuff (811 participants) before surgery but while anesthetized, said Dr. Derek J. Hausenloy of the Hatter Cardiovascular Institute, University College London, and his associates.
The primary endpoint – a composite of death from cardiovascular causes, nonfatal MI, coronary revascularization, or stroke within 1 year – was 26.5% with true preconditioning and 27.7% with the sham procedure, a nonsignificant difference. There were no significant differences between the two study groups in any of the individual components of this composite or according to type of anesthesia or the interval between preconditioning and surgical incision.
These findings remained strongly consistent across all subgroups of patients evaluated, regardless of troponin levels, inotrope score, presence or absence of kidney injury, degree of kidney injury, length of ICU stay, length of hospital stay, or performance on 6-minute walk test, Dr. Hausenloy and his associates said (N Engl J Med. 2015 Oct 5. doi: 10.1056/NEJMoa1413534).
In both trials, the rate of adverse effects from remote ischemic preconditioning was the same between the true and the sham procedures, and the only adverse effect considered to be related to preconditioning was an increased incidence of skin petechiae (4.4% vs. 0.2%) in the ERICCA study.
The investigators’ financial disclosures are available at NEJM.org.
The conclusions from the RIPHeart study and the ERRICA study are definitive: Remote ischemic preconditioning is ineffective in adults undergoing on-pump cardiac surgery.
We do not yet understand why. Cardiopulmonary bypass itself, as well as hypothermia and cardioplegia, are known to be cardioprotective, so it may be that further cardioprotection is simply not possible. It also might be that concomitant medications, particularly propofol and opioids, diminish or even block the cardioprotective effects of remote ischemic preconditioning.
The most obvious explanation for the negative results of these two large trials is that other cardioprotective measures may have masked the effect of remote ischemic preconditioning or rendered it redundant.
Dr. Michael Zaugg and Eliana Lucchinetti, Ph.D., of the departments of anesthesiology and pain medicine and in the Cardiovascular Research Centre at the University of Alberta, Edmonton, made these remarks in an editorial accompanying the two reports on remote ischemic preconditioning (N Engl J Med. 2015 Oct 5. doi: 10.1056/MEJMe1510338). Their financial disclosures are available at NEJM.org.
The conclusions from the RIPHeart study and the ERRICA study are definitive: Remote ischemic preconditioning is ineffective in adults undergoing on-pump cardiac surgery.
We do not yet understand why. Cardiopulmonary bypass itself, as well as hypothermia and cardioplegia, are known to be cardioprotective, so it may be that further cardioprotection is simply not possible. It also might be that concomitant medications, particularly propofol and opioids, diminish or even block the cardioprotective effects of remote ischemic preconditioning.
The most obvious explanation for the negative results of these two large trials is that other cardioprotective measures may have masked the effect of remote ischemic preconditioning or rendered it redundant.
Dr. Michael Zaugg and Eliana Lucchinetti, Ph.D., of the departments of anesthesiology and pain medicine and in the Cardiovascular Research Centre at the University of Alberta, Edmonton, made these remarks in an editorial accompanying the two reports on remote ischemic preconditioning (N Engl J Med. 2015 Oct 5. doi: 10.1056/MEJMe1510338). Their financial disclosures are available at NEJM.org.
The conclusions from the RIPHeart study and the ERRICA study are definitive: Remote ischemic preconditioning is ineffective in adults undergoing on-pump cardiac surgery.
We do not yet understand why. Cardiopulmonary bypass itself, as well as hypothermia and cardioplegia, are known to be cardioprotective, so it may be that further cardioprotection is simply not possible. It also might be that concomitant medications, particularly propofol and opioids, diminish or even block the cardioprotective effects of remote ischemic preconditioning.
The most obvious explanation for the negative results of these two large trials is that other cardioprotective measures may have masked the effect of remote ischemic preconditioning or rendered it redundant.
Dr. Michael Zaugg and Eliana Lucchinetti, Ph.D., of the departments of anesthesiology and pain medicine and in the Cardiovascular Research Centre at the University of Alberta, Edmonton, made these remarks in an editorial accompanying the two reports on remote ischemic preconditioning (N Engl J Med. 2015 Oct 5. doi: 10.1056/MEJMe1510338). Their financial disclosures are available at NEJM.org.
Remote ischemic preconditioning failed to improve outcomes among higher-risk patients undergoing elective cardiac surgery in two separate large clinical trials reported online Oct. 5 in the New England Journal of Medicine.
Both studies clearly showed that the technique did not provide greater protection of the heart, brain, or kidneys than did a sham technique, failing to improve any of the numerous primary or secondary endpoints or to produce a benefit in any of several subgroups of patients.
Remote ischemic preconditioning involves protecting the heart and other organs against surgery-related acute ischemia/reperfusion injury by first applying brief cycles of ischemia and reperfusion to a remote organ or tissue. It is thought that this stimulus produces a blood-borne response that conveys a protective effect from the remote area to the target organs. This remote preconditioning can be accomplished noninvasively by inflating and deflating a standard blood pressure cuff on the upper arm or thigh for brief periods.
Some early studies indicated that using this technique during cardiovascular surgery improved serum cardiac and renal biomarkers, which implied protection of these organs against ischemia/reperfusion injury. But more recent prospective clinical trials have shown no such benefit. None of these studies were adequately powered to assess the effect on hard clinical endpoints, and most were single center, unblinded, and had no standardized anesthesia regimen.
RIPHeart study
To address these study limitations, the RIPHeart Study investigators performed a prospective double-blind controlled trial among 1,385 adults undergoing elective cardiovascular surgery requiring cardiopulmonary bypass at 14 university hospitals in Germany during a 3-year period. The participants had a mean EuroSCORE (European System for Cardiac Operative Risk Evaluation) of 6 or higher, indicating that most of them were at higher than average risk, and all received the same anesthetic, intravenous propofol. A total of 692 patients were randomly assigned to undergo four 5-minute cycles of upper-arm ischemia/reperfusion after being anesthetized and 693 to undergo sham ischemia/reperfusion on a dummy arm hidden by surgical drapes, said Dr. Patrick Meybohm of the department of anesthesiology, intensive care medicine, and pain therapy at University Hospital Frankfurt and his associates.
The primary endpoint – a composite of death from any cause, nonfatal MI, stroke, or acute renal failure before hospital discharge – occurred in 14.3% of the intervention group and 14.6% of the control group, a nonsignificant difference. Furthermore, no significant differences between the two study groups were seen in any of the individual components of this composite measure, or in any secondary endpoints such as duration of mechanical ventilation, ICU length of stay, hospital length of stay, troponin levels, creatinine levels, onset of atrial fibrillation, or incidence of postoperative delirium. All outcome measures remained similar between the two study groups at 30-day, 90-day, and 1-year follow-ups (N Engl J Med 2015 Oct 5. doi: 10.1056/NEJMoa1413579).
In addition, estimated event-free survival at 30 days was 85.2% with the true intervention and 85.0% with the sham intervention, another nonsignificant difference. These estimates remained similar between the two study groups at 90 days and 1 year. The findings of the primary analysis were confirmed in the “completely concordant” per-protocol analysis, Dr. Meybohm and his associates noted.
ERICCA trial
In the Effect of Remote Ischemic Preconditioning on Clinical Outcomes in Patients Undergoing CABG (ERICCA) study, investigators assessed 1,612 adults undergoing on-pump CABG (with or without valve surgery) using blood cardioplegia at 30 cardiac surgery centers in the United Kingdom during a 3-year period. These patients were randomly assigned to undergo remote ischemic preconditioning with a standard blood pressure cuff on the upper arm for four 5-minute cycles (801 participants) or a sham procedure using a deactivated blood pressure cuff (811 participants) before surgery but while anesthetized, said Dr. Derek J. Hausenloy of the Hatter Cardiovascular Institute, University College London, and his associates.
The primary endpoint – a composite of death from cardiovascular causes, nonfatal MI, coronary revascularization, or stroke within 1 year – was 26.5% with true preconditioning and 27.7% with the sham procedure, a nonsignificant difference. There were no significant differences between the two study groups in any of the individual components of this composite or according to type of anesthesia or the interval between preconditioning and surgical incision.
These findings remained strongly consistent across all subgroups of patients evaluated, regardless of troponin levels, inotrope score, presence or absence of kidney injury, degree of kidney injury, length of ICU stay, length of hospital stay, or performance on 6-minute walk test, Dr. Hausenloy and his associates said (N Engl J Med. 2015 Oct 5. doi: 10.1056/NEJMoa1413534).
In both trials, the rate of adverse effects from remote ischemic preconditioning was the same between the true and the sham procedures, and the only adverse effect considered to be related to preconditioning was an increased incidence of skin petechiae (4.4% vs. 0.2%) in the ERICCA study.
The investigators’ financial disclosures are available at NEJM.org.
Remote ischemic preconditioning failed to improve outcomes among higher-risk patients undergoing elective cardiac surgery in two separate large clinical trials reported online Oct. 5 in the New England Journal of Medicine.
Both studies clearly showed that the technique did not provide greater protection of the heart, brain, or kidneys than did a sham technique, failing to improve any of the numerous primary or secondary endpoints or to produce a benefit in any of several subgroups of patients.
Remote ischemic preconditioning involves protecting the heart and other organs against surgery-related acute ischemia/reperfusion injury by first applying brief cycles of ischemia and reperfusion to a remote organ or tissue. It is thought that this stimulus produces a blood-borne response that conveys a protective effect from the remote area to the target organs. This remote preconditioning can be accomplished noninvasively by inflating and deflating a standard blood pressure cuff on the upper arm or thigh for brief periods.
Some early studies indicated that using this technique during cardiovascular surgery improved serum cardiac and renal biomarkers, which implied protection of these organs against ischemia/reperfusion injury. But more recent prospective clinical trials have shown no such benefit. None of these studies were adequately powered to assess the effect on hard clinical endpoints, and most were single center, unblinded, and had no standardized anesthesia regimen.
RIPHeart study
To address these study limitations, the RIPHeart Study investigators performed a prospective double-blind controlled trial among 1,385 adults undergoing elective cardiovascular surgery requiring cardiopulmonary bypass at 14 university hospitals in Germany during a 3-year period. The participants had a mean EuroSCORE (European System for Cardiac Operative Risk Evaluation) of 6 or higher, indicating that most of them were at higher than average risk, and all received the same anesthetic, intravenous propofol. A total of 692 patients were randomly assigned to undergo four 5-minute cycles of upper-arm ischemia/reperfusion after being anesthetized and 693 to undergo sham ischemia/reperfusion on a dummy arm hidden by surgical drapes, said Dr. Patrick Meybohm of the department of anesthesiology, intensive care medicine, and pain therapy at University Hospital Frankfurt and his associates.
The primary endpoint – a composite of death from any cause, nonfatal MI, stroke, or acute renal failure before hospital discharge – occurred in 14.3% of the intervention group and 14.6% of the control group, a nonsignificant difference. Furthermore, no significant differences between the two study groups were seen in any of the individual components of this composite measure, or in any secondary endpoints such as duration of mechanical ventilation, ICU length of stay, hospital length of stay, troponin levels, creatinine levels, onset of atrial fibrillation, or incidence of postoperative delirium. All outcome measures remained similar between the two study groups at 30-day, 90-day, and 1-year follow-ups (N Engl J Med 2015 Oct 5. doi: 10.1056/NEJMoa1413579).
In addition, estimated event-free survival at 30 days was 85.2% with the true intervention and 85.0% with the sham intervention, another nonsignificant difference. These estimates remained similar between the two study groups at 90 days and 1 year. The findings of the primary analysis were confirmed in the “completely concordant” per-protocol analysis, Dr. Meybohm and his associates noted.
ERICCA trial
In the Effect of Remote Ischemic Preconditioning on Clinical Outcomes in Patients Undergoing CABG (ERICCA) study, investigators assessed 1,612 adults undergoing on-pump CABG (with or without valve surgery) using blood cardioplegia at 30 cardiac surgery centers in the United Kingdom during a 3-year period. These patients were randomly assigned to undergo remote ischemic preconditioning with a standard blood pressure cuff on the upper arm for four 5-minute cycles (801 participants) or a sham procedure using a deactivated blood pressure cuff (811 participants) before surgery but while anesthetized, said Dr. Derek J. Hausenloy of the Hatter Cardiovascular Institute, University College London, and his associates.
The primary endpoint – a composite of death from cardiovascular causes, nonfatal MI, coronary revascularization, or stroke within 1 year – was 26.5% with true preconditioning and 27.7% with the sham procedure, a nonsignificant difference. There were no significant differences between the two study groups in any of the individual components of this composite or according to type of anesthesia or the interval between preconditioning and surgical incision.
These findings remained strongly consistent across all subgroups of patients evaluated, regardless of troponin levels, inotrope score, presence or absence of kidney injury, degree of kidney injury, length of ICU stay, length of hospital stay, or performance on 6-minute walk test, Dr. Hausenloy and his associates said (N Engl J Med. 2015 Oct 5. doi: 10.1056/NEJMoa1413534).
In both trials, the rate of adverse effects from remote ischemic preconditioning was the same between the true and the sham procedures, and the only adverse effect considered to be related to preconditioning was an increased incidence of skin petechiae (4.4% vs. 0.2%) in the ERICCA study.
The investigators’ financial disclosures are available at NEJM.org.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Adverse cardiac events increased during surgery while on beta-blockers
For patients who underwent noncardiac surgery, a two-drug antihypertensive treatment regimen with a beta-blocker was associated with an increased risk of perioperative major adverse cardiovascular events (MACEs) and all-cause mortality, according to research published in JAMA Internal Medicine.
Mads E. JØrgensen of Copenhagen University Hospital and his associates examined data from 671,242 surgeries performed in Denmark from 2005-2011; ultimately, 14,644 patients treated with beta-blockers and the 40,676 patients treated with other antihypertensive drugs (or 55,320 hypertensive patients using at least two antihypertensive drugs) were included in the analysis.
The incidence of 30-day MACEs and mortality was 1.32% and 1.93%, respectively, in patients treated with beta-blockers, compared with 0.84% and 1.32%, respectively, in patients treated with other drugs only (both P less than .001).
The investigators also noted that patients over age 70, men, and patients undergoing acute surgery were at greater risk for MACEs.
“This observation may suggest that perioperative management of patients with hypertension should receive specific attention in clinical practice and future guidelines, but additional randomized clinical trials on this question may be warranted,” the investigators wrote.
Read the full article in JAMA Internal Medicine (doi:10.1001/jamainternmed.2015.5346.).
For patients who underwent noncardiac surgery, a two-drug antihypertensive treatment regimen with a beta-blocker was associated with an increased risk of perioperative major adverse cardiovascular events (MACEs) and all-cause mortality, according to research published in JAMA Internal Medicine.
Mads E. JØrgensen of Copenhagen University Hospital and his associates examined data from 671,242 surgeries performed in Denmark from 2005-2011; ultimately, 14,644 patients treated with beta-blockers and the 40,676 patients treated with other antihypertensive drugs (or 55,320 hypertensive patients using at least two antihypertensive drugs) were included in the analysis.
The incidence of 30-day MACEs and mortality was 1.32% and 1.93%, respectively, in patients treated with beta-blockers, compared with 0.84% and 1.32%, respectively, in patients treated with other drugs only (both P less than .001).
The investigators also noted that patients over age 70, men, and patients undergoing acute surgery were at greater risk for MACEs.
“This observation may suggest that perioperative management of patients with hypertension should receive specific attention in clinical practice and future guidelines, but additional randomized clinical trials on this question may be warranted,” the investigators wrote.
Read the full article in JAMA Internal Medicine (doi:10.1001/jamainternmed.2015.5346.).
For patients who underwent noncardiac surgery, a two-drug antihypertensive treatment regimen with a beta-blocker was associated with an increased risk of perioperative major adverse cardiovascular events (MACEs) and all-cause mortality, according to research published in JAMA Internal Medicine.
Mads E. JØrgensen of Copenhagen University Hospital and his associates examined data from 671,242 surgeries performed in Denmark from 2005-2011; ultimately, 14,644 patients treated with beta-blockers and the 40,676 patients treated with other antihypertensive drugs (or 55,320 hypertensive patients using at least two antihypertensive drugs) were included in the analysis.
The incidence of 30-day MACEs and mortality was 1.32% and 1.93%, respectively, in patients treated with beta-blockers, compared with 0.84% and 1.32%, respectively, in patients treated with other drugs only (both P less than .001).
The investigators also noted that patients over age 70, men, and patients undergoing acute surgery were at greater risk for MACEs.
“This observation may suggest that perioperative management of patients with hypertension should receive specific attention in clinical practice and future guidelines, but additional randomized clinical trials on this question may be warranted,” the investigators wrote.
Read the full article in JAMA Internal Medicine (doi:10.1001/jamainternmed.2015.5346.).
FROM JAMA INTERNAL MEDICINE
‘Minimalist’ TAVR has short learning curve
As a “minimalist” approach to transcatheter aortic valve replacement – known as MA-TAVR – gains in popularity at high-volume centers, questions persist about the surgeon’s learning curve. A small series of MA-TAVR cases at Emory University in Atlanta has shown that the leaning curve may be like the TAVR approach itself: minimal.
Dr. Hanna Jensen and her associates reported on 151 consecutive patients who had MA-TAVR in the October issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.07.078). They previously reported their findings at the annual meeting of the American Association for Thoracic Surgery in April in Seattle.
This study builds on an Emory study last year that reported the minimalist approach to TAVR cost about $10,000 less per patient than the standard transfemoral approach (JACC Cardiovasc Interv. 2014;7:898-904).
The operation the study authors evaluated is performed in the catheterization laboratory rather than the operating room, as in traditional TAVR. Both approaches use a femoral approach, but where traditional TAVR requires general anesthesia and transesophageal echocardiography (TEE), MA-TAVR uses local anesthesia, minimal conscious sedation, and transthoracic echocardiography (TTE).
The study authors acknowledged concerns that TTE may underestimate the severity of paravalvular leak after the procedure when compared with TEE. Their protocol relies on preoperative TTE and CT scans, or three-dimensional TEE if the case warrants it, to ensure optimal sizing of the transcatheter valve before the operation. “If any concerns arise, our threshold is low to perform intraoperative balloon-sizing,” Dr. Jensen and her coauthors said. They also use TTE, along with a root-angiogram after valve deployment, and invasively measure the aortic regurgitation index before and after deployment.
Most study patients were high-risk surgical candidates with a median Society of Thoracic Surgeons Predicted Risk of Mortality (STS PROM) score of 10%. The overall major stroke rate was 3.3%, while major vascular complications occurred in 3% of patients and the greater-than-mild paravalvular leak rate was 7%.
The study retrospectively evaluated 151 consecutive patients who were divided into three groups at different time points: May 2012 to January 2013, February to August 2013, and September 2013 to July 2014. Complications were similar among all three groups, but the third group had shorter hospital stays and less time in the intensive care unit (ICU).
The first group received only the first-generation SAPIEN valve system; use of the second-generation SAPIEN XT valve increased in latter two groups. The SAPIEN XT valve is available in 23, 26, or 29 mm, but the 29-mm size was not available in the first-generation SAPIEN implant.
A subgroup analysis looked at patients who were discharged within 48 hours of the operation or more than 48 hours afterward. The early-discharge patients had lower STS PROM scores (8.3% vs. 10.3%) and lower rates of diabetes (31% vs. 49%). They also had less need for postoperative pacemakers and less frequent rehospitalization. “This implies that in selected MA-TAVR patients early discharge is feasible and safe, but larger studies are required to identify the optimal profile of patients who can be sent home within the first two postoperative days,” Dr. Jensen and her colleagues said.
Early in the MA-TAVR protocol all patients were sent to the ICU. As the care team gained more experience with the procedure, the protocol changed to send all patients to a regular telemetry floor after surgery unless they had vascular issues or potential need for a pacemaker. The decreasing need for ICU “was the only indication of an institutional learning curve that was discovered, and demonstrated improved resource utilization over time,” the investigators said.
They encouraged other centers to pursue MA-TAVR. “As experience grows, we believe that this procedure can be done with less or no ICU support leading to a shorter hospital stay and improved resource utilization,” Dr. Jensen and her coauthors concluded. They called for further studies to determine the characteristics that make a patient most suitable for a short-admission MA-TAVR procedure.
Study coauthors Dr. Vasilis Babaliaros, Dr. Vinod Thourani, Amy Simone, and Patricia Keegan are research consultants with Edwards Lifesciences. The rest of the authors had no disclosures.
Calling this report an “early milestone in the relentless simplification” of transcatheter aortic valve replacement (TAVR), Dr. Craig Smith of Columbia University Medical Center/New York Presbyterian Hospital, wrote in his invited commentary that it nonetheless leaves a few questions unanswered – and may leave surgeons seeing their role in TAVR marginalized as the procedure moves from the operating room to the catheterization lab (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.07.082). .

|
Dr. Craig Smith |
One unanswered question revolves around the use of conscious sedation and transthoracic echocardiography (TTE) for the minimalist approach (MA), rather than general anesthesia and transesophageal echocardiography (TEE) of the traditional transfemoral approach. “MA requires reliance on [TTE] for assessment of paravalvular leak, and since TTE can’t be compared to TEE in the same patients and still be MA, the merits of this trade-off cannot be assessed in this population,” he said.
Further, he said that the study data do not conclusively link MA to early discharge because the early discharge patients had lower Society of Thoracic Surgery scores.
Another important unanswered question is whether endocarditis is more frequent in TAVR when it’s performed outside the operating room.
“While I suspect the answer will be ‘yes,’ this question will be left dangling until large numbers have been done in hybrid cath labs, because the frequency will be low, and because the forces propelling a ‘cath lab’ alternative to surgical or transcatheter valve replacement done in an operating room will be too powerful to retard on a hunch,” Dr. Smith wrote. “What will the departure of TAVR from operating rooms mean for the role of the surgeon? That is for surgeons to determine. Stay involved, or say goodbye!”
Calling this report an “early milestone in the relentless simplification” of transcatheter aortic valve replacement (TAVR), Dr. Craig Smith of Columbia University Medical Center/New York Presbyterian Hospital, wrote in his invited commentary that it nonetheless leaves a few questions unanswered – and may leave surgeons seeing their role in TAVR marginalized as the procedure moves from the operating room to the catheterization lab (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.07.082). .

|
Dr. Craig Smith |
One unanswered question revolves around the use of conscious sedation and transthoracic echocardiography (TTE) for the minimalist approach (MA), rather than general anesthesia and transesophageal echocardiography (TEE) of the traditional transfemoral approach. “MA requires reliance on [TTE] for assessment of paravalvular leak, and since TTE can’t be compared to TEE in the same patients and still be MA, the merits of this trade-off cannot be assessed in this population,” he said.
Further, he said that the study data do not conclusively link MA to early discharge because the early discharge patients had lower Society of Thoracic Surgery scores.
Another important unanswered question is whether endocarditis is more frequent in TAVR when it’s performed outside the operating room.
“While I suspect the answer will be ‘yes,’ this question will be left dangling until large numbers have been done in hybrid cath labs, because the frequency will be low, and because the forces propelling a ‘cath lab’ alternative to surgical or transcatheter valve replacement done in an operating room will be too powerful to retard on a hunch,” Dr. Smith wrote. “What will the departure of TAVR from operating rooms mean for the role of the surgeon? That is for surgeons to determine. Stay involved, or say goodbye!”
Calling this report an “early milestone in the relentless simplification” of transcatheter aortic valve replacement (TAVR), Dr. Craig Smith of Columbia University Medical Center/New York Presbyterian Hospital, wrote in his invited commentary that it nonetheless leaves a few questions unanswered – and may leave surgeons seeing their role in TAVR marginalized as the procedure moves from the operating room to the catheterization lab (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.07.082). .

|
Dr. Craig Smith |
One unanswered question revolves around the use of conscious sedation and transthoracic echocardiography (TTE) for the minimalist approach (MA), rather than general anesthesia and transesophageal echocardiography (TEE) of the traditional transfemoral approach. “MA requires reliance on [TTE] for assessment of paravalvular leak, and since TTE can’t be compared to TEE in the same patients and still be MA, the merits of this trade-off cannot be assessed in this population,” he said.
Further, he said that the study data do not conclusively link MA to early discharge because the early discharge patients had lower Society of Thoracic Surgery scores.
Another important unanswered question is whether endocarditis is more frequent in TAVR when it’s performed outside the operating room.
“While I suspect the answer will be ‘yes,’ this question will be left dangling until large numbers have been done in hybrid cath labs, because the frequency will be low, and because the forces propelling a ‘cath lab’ alternative to surgical or transcatheter valve replacement done in an operating room will be too powerful to retard on a hunch,” Dr. Smith wrote. “What will the departure of TAVR from operating rooms mean for the role of the surgeon? That is for surgeons to determine. Stay involved, or say goodbye!”
As a “minimalist” approach to transcatheter aortic valve replacement – known as MA-TAVR – gains in popularity at high-volume centers, questions persist about the surgeon’s learning curve. A small series of MA-TAVR cases at Emory University in Atlanta has shown that the leaning curve may be like the TAVR approach itself: minimal.
Dr. Hanna Jensen and her associates reported on 151 consecutive patients who had MA-TAVR in the October issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.07.078). They previously reported their findings at the annual meeting of the American Association for Thoracic Surgery in April in Seattle.
This study builds on an Emory study last year that reported the minimalist approach to TAVR cost about $10,000 less per patient than the standard transfemoral approach (JACC Cardiovasc Interv. 2014;7:898-904).
The operation the study authors evaluated is performed in the catheterization laboratory rather than the operating room, as in traditional TAVR. Both approaches use a femoral approach, but where traditional TAVR requires general anesthesia and transesophageal echocardiography (TEE), MA-TAVR uses local anesthesia, minimal conscious sedation, and transthoracic echocardiography (TTE).
The study authors acknowledged concerns that TTE may underestimate the severity of paravalvular leak after the procedure when compared with TEE. Their protocol relies on preoperative TTE and CT scans, or three-dimensional TEE if the case warrants it, to ensure optimal sizing of the transcatheter valve before the operation. “If any concerns arise, our threshold is low to perform intraoperative balloon-sizing,” Dr. Jensen and her coauthors said. They also use TTE, along with a root-angiogram after valve deployment, and invasively measure the aortic regurgitation index before and after deployment.
Most study patients were high-risk surgical candidates with a median Society of Thoracic Surgeons Predicted Risk of Mortality (STS PROM) score of 10%. The overall major stroke rate was 3.3%, while major vascular complications occurred in 3% of patients and the greater-than-mild paravalvular leak rate was 7%.
The study retrospectively evaluated 151 consecutive patients who were divided into three groups at different time points: May 2012 to January 2013, February to August 2013, and September 2013 to July 2014. Complications were similar among all three groups, but the third group had shorter hospital stays and less time in the intensive care unit (ICU).
The first group received only the first-generation SAPIEN valve system; use of the second-generation SAPIEN XT valve increased in latter two groups. The SAPIEN XT valve is available in 23, 26, or 29 mm, but the 29-mm size was not available in the first-generation SAPIEN implant.
A subgroup analysis looked at patients who were discharged within 48 hours of the operation or more than 48 hours afterward. The early-discharge patients had lower STS PROM scores (8.3% vs. 10.3%) and lower rates of diabetes (31% vs. 49%). They also had less need for postoperative pacemakers and less frequent rehospitalization. “This implies that in selected MA-TAVR patients early discharge is feasible and safe, but larger studies are required to identify the optimal profile of patients who can be sent home within the first two postoperative days,” Dr. Jensen and her colleagues said.
Early in the MA-TAVR protocol all patients were sent to the ICU. As the care team gained more experience with the procedure, the protocol changed to send all patients to a regular telemetry floor after surgery unless they had vascular issues or potential need for a pacemaker. The decreasing need for ICU “was the only indication of an institutional learning curve that was discovered, and demonstrated improved resource utilization over time,” the investigators said.
They encouraged other centers to pursue MA-TAVR. “As experience grows, we believe that this procedure can be done with less or no ICU support leading to a shorter hospital stay and improved resource utilization,” Dr. Jensen and her coauthors concluded. They called for further studies to determine the characteristics that make a patient most suitable for a short-admission MA-TAVR procedure.
Study coauthors Dr. Vasilis Babaliaros, Dr. Vinod Thourani, Amy Simone, and Patricia Keegan are research consultants with Edwards Lifesciences. The rest of the authors had no disclosures.
As a “minimalist” approach to transcatheter aortic valve replacement – known as MA-TAVR – gains in popularity at high-volume centers, questions persist about the surgeon’s learning curve. A small series of MA-TAVR cases at Emory University in Atlanta has shown that the leaning curve may be like the TAVR approach itself: minimal.
Dr. Hanna Jensen and her associates reported on 151 consecutive patients who had MA-TAVR in the October issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.07.078). They previously reported their findings at the annual meeting of the American Association for Thoracic Surgery in April in Seattle.
This study builds on an Emory study last year that reported the minimalist approach to TAVR cost about $10,000 less per patient than the standard transfemoral approach (JACC Cardiovasc Interv. 2014;7:898-904).
The operation the study authors evaluated is performed in the catheterization laboratory rather than the operating room, as in traditional TAVR. Both approaches use a femoral approach, but where traditional TAVR requires general anesthesia and transesophageal echocardiography (TEE), MA-TAVR uses local anesthesia, minimal conscious sedation, and transthoracic echocardiography (TTE).
The study authors acknowledged concerns that TTE may underestimate the severity of paravalvular leak after the procedure when compared with TEE. Their protocol relies on preoperative TTE and CT scans, or three-dimensional TEE if the case warrants it, to ensure optimal sizing of the transcatheter valve before the operation. “If any concerns arise, our threshold is low to perform intraoperative balloon-sizing,” Dr. Jensen and her coauthors said. They also use TTE, along with a root-angiogram after valve deployment, and invasively measure the aortic regurgitation index before and after deployment.
Most study patients were high-risk surgical candidates with a median Society of Thoracic Surgeons Predicted Risk of Mortality (STS PROM) score of 10%. The overall major stroke rate was 3.3%, while major vascular complications occurred in 3% of patients and the greater-than-mild paravalvular leak rate was 7%.
The study retrospectively evaluated 151 consecutive patients who were divided into three groups at different time points: May 2012 to January 2013, February to August 2013, and September 2013 to July 2014. Complications were similar among all three groups, but the third group had shorter hospital stays and less time in the intensive care unit (ICU).
The first group received only the first-generation SAPIEN valve system; use of the second-generation SAPIEN XT valve increased in latter two groups. The SAPIEN XT valve is available in 23, 26, or 29 mm, but the 29-mm size was not available in the first-generation SAPIEN implant.
A subgroup analysis looked at patients who were discharged within 48 hours of the operation or more than 48 hours afterward. The early-discharge patients had lower STS PROM scores (8.3% vs. 10.3%) and lower rates of diabetes (31% vs. 49%). They also had less need for postoperative pacemakers and less frequent rehospitalization. “This implies that in selected MA-TAVR patients early discharge is feasible and safe, but larger studies are required to identify the optimal profile of patients who can be sent home within the first two postoperative days,” Dr. Jensen and her colleagues said.
Early in the MA-TAVR protocol all patients were sent to the ICU. As the care team gained more experience with the procedure, the protocol changed to send all patients to a regular telemetry floor after surgery unless they had vascular issues or potential need for a pacemaker. The decreasing need for ICU “was the only indication of an institutional learning curve that was discovered, and demonstrated improved resource utilization over time,” the investigators said.
They encouraged other centers to pursue MA-TAVR. “As experience grows, we believe that this procedure can be done with less or no ICU support leading to a shorter hospital stay and improved resource utilization,” Dr. Jensen and her coauthors concluded. They called for further studies to determine the characteristics that make a patient most suitable for a short-admission MA-TAVR procedure.
Study coauthors Dr. Vasilis Babaliaros, Dr. Vinod Thourani, Amy Simone, and Patricia Keegan are research consultants with Edwards Lifesciences. The rest of the authors had no disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: A minimalist approach to transcatheter aortic valve replacement (MA-TAVR) is feasible with acceptable outcomes.
Major finding: Transition to MA-TAVR in a high-volume center had a relatively small learning curve.
Data source: A review of 151 consecutive patients who had MA-TAVR at Emory University between May 2012 and July 2014.
Disclosures: Study coauthors Dr. Vasilis Babaliaros, Dr. Vinod Thourani, Amy Simone, and Patricia Keegan are research consultants with Edwards Lifesciences. The rest of the authors had no disclosures.
HFSA: Next-generation LVAD meets survival goal
NATIONAL HARBOR, MD. – A next-generation left-ventricular assist device, the HeartMate 3, gave a solid debut performance in an uncontrolled series of the first 50 recipients, which was designed to gain the device CE mark approval in Europe.
In this study, run at 10 sites in Australia, Austria, Canada, Czech Republic, Germany, and Kazakhstan, the new-design left ventricular assist device (LVAD) numerically surpassed the study’s prespecified primary endpoint with 6-month recipient survival of 92%. This bested the target survival rate of 88% that the trial’s designers derived from the survival rate among 50 matched patients who had received a LVAD during 2012-2014 and had entered the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS), Dr. Ivan Netuka said at the annual meeting of the Heart Failure Society of America.
Other notable findings of the HeartMate 3’s performance in the first 50 patients followed for 6 months were no pump malfunctions, no thrombosis within the pump, and no evidence of hemolysis, said Dr. Netuka, deputy director of cardiovascular surgery at IKEM hospital in Prague.
HeartMate 3 features several improvements over the HeartMate II model, such as a fully magnetically levitated rotor designed to eliminate friction and wear within the pump. The device also is engineered to produce an artificial pulse of 30 beats per minute, and it can deliver a wide blood-flow range of 2-10 L/min. Larger and consistent pump gaps are designed to reduced shear stress on blood components.
The study enrolled patients during June-November 2014 with NYHA class IIIB or IV heart failure and stage D heart failure, with a left ventricular ejection fraction of 25% or less. The 50 patients averaged 59 years of age and 90% were men; they were divided about equally between patients who received the device as a bridge to transplant and those who received the LVAD as destination therapy.
During 6 months of follow-up, two patients received a heart transplant. Twenty-one (42%) of the enrolled patients classified as INTERMACS patient profile 3, 20 (40%) as profile 4, and 5 (10%) as profile 2 patients, with the remaining four patients falling into other profile levels. Twenty-one patients had concomitant heart surgery when they received their LVAD, usually valve replacement. All patients received warfarin treatment and aspirin following device placement. Dr. Netuka and his associates calculated an expected 6-month survival of 78% for the enrolled patients without LVAD intervention.
The four deaths included a patient who died from cardiac arrest following a stroke on day 19 – a complication judged attributable to the device-placement procedure, a patient with circulatory failure on day 48, a suicide on day 113, and a patient with multiorgan failure on day 144.
After 6 months of follow-up, notable adverse events included bleeding in 19 patients (38%) – including gastrointestinal bleeds in 4 patients (8%) – strokes in 6 patients (12%), and infections in 18 patients (36%). Most of the adverse events occurred in the first 7 days following LVAD placement. Three of the six strokes were judged procedure associated, Dr. Netuka said.
Following device placement, patients showed improvements in their NYHA class and quality of life; their 6-minute walk distance improved by an average of 231 m.
The HeartMate 3 device is currently undergoing U.S. assessment in comparison to HeartMate II prior to submission to the Food and Drug Administration. The randomized trial, known as MOMENTUM 3, plans to enroll 1,028 patients with completion scheduled for 2018.
The study was sponsored by Thoratec, which is developing the HeartMate 3 device. Dr. Netuka is a speaker for and consultant to Thoratec.
On Twitter @mitchelzoler
It is extremely exciting to see this next-generation left ventricular assist device move forward, but it is important not to overinterpret the findings because the number of patients treated was relatively small and, as a result, the findings are limited by very wide confidence limits.

|
| Mitchel L. Zoler/Frontline Medical News Dr. Marvin A. Konstam |
The HeartMate 3 device probably represents an important advance beyond currently available technology. Its attractive features include full magnetic levitation of the rotor, production of an artificial pulse, and the ability to deliver a wide range of blood-flow rates. These features may improve performance and could have favorable effects on thrombus and stroke rates.
The device clearly achieved its primary performance goal of 88% 6-month survival. The INTERMACS profiles of the enrolled patients included 40% of patients with profile 4 and 10% with profile 2. This does not exactly mimic the typical U.S. population receiving these devices, which recently had 15% of patients with a level 4 profile and 36% of patients with more severe disease at level 2. I applaud the decision to include patients who received their devices as destination therapy as well as patients who received it as a bridge to transplant.
The technologic advances that this new device represents are a step in the right direction, and the results provide a green light for further assessment. I look forward to seeing results from the U.S. randomized trial.
Dr. Marvin A. Konstam is professor and chief physician executive of the CardioVascular Center at Tufts Medical Center in Boston. He made these comments as designated discussant for Dr. Netuka’s report. Dr. Konstam has been a consultant to Merck, Novartis, Amgen, Johnson & Johnson, Arbor, Mast, and Cardioxyl.
It is extremely exciting to see this next-generation left ventricular assist device move forward, but it is important not to overinterpret the findings because the number of patients treated was relatively small and, as a result, the findings are limited by very wide confidence limits.

|
| Mitchel L. Zoler/Frontline Medical News Dr. Marvin A. Konstam |
The HeartMate 3 device probably represents an important advance beyond currently available technology. Its attractive features include full magnetic levitation of the rotor, production of an artificial pulse, and the ability to deliver a wide range of blood-flow rates. These features may improve performance and could have favorable effects on thrombus and stroke rates.
The device clearly achieved its primary performance goal of 88% 6-month survival. The INTERMACS profiles of the enrolled patients included 40% of patients with profile 4 and 10% with profile 2. This does not exactly mimic the typical U.S. population receiving these devices, which recently had 15% of patients with a level 4 profile and 36% of patients with more severe disease at level 2. I applaud the decision to include patients who received their devices as destination therapy as well as patients who received it as a bridge to transplant.
The technologic advances that this new device represents are a step in the right direction, and the results provide a green light for further assessment. I look forward to seeing results from the U.S. randomized trial.
Dr. Marvin A. Konstam is professor and chief physician executive of the CardioVascular Center at Tufts Medical Center in Boston. He made these comments as designated discussant for Dr. Netuka’s report. Dr. Konstam has been a consultant to Merck, Novartis, Amgen, Johnson & Johnson, Arbor, Mast, and Cardioxyl.
It is extremely exciting to see this next-generation left ventricular assist device move forward, but it is important not to overinterpret the findings because the number of patients treated was relatively small and, as a result, the findings are limited by very wide confidence limits.

|
| Mitchel L. Zoler/Frontline Medical News Dr. Marvin A. Konstam |
The HeartMate 3 device probably represents an important advance beyond currently available technology. Its attractive features include full magnetic levitation of the rotor, production of an artificial pulse, and the ability to deliver a wide range of blood-flow rates. These features may improve performance and could have favorable effects on thrombus and stroke rates.
The device clearly achieved its primary performance goal of 88% 6-month survival. The INTERMACS profiles of the enrolled patients included 40% of patients with profile 4 and 10% with profile 2. This does not exactly mimic the typical U.S. population receiving these devices, which recently had 15% of patients with a level 4 profile and 36% of patients with more severe disease at level 2. I applaud the decision to include patients who received their devices as destination therapy as well as patients who received it as a bridge to transplant.
The technologic advances that this new device represents are a step in the right direction, and the results provide a green light for further assessment. I look forward to seeing results from the U.S. randomized trial.
Dr. Marvin A. Konstam is professor and chief physician executive of the CardioVascular Center at Tufts Medical Center in Boston. He made these comments as designated discussant for Dr. Netuka’s report. Dr. Konstam has been a consultant to Merck, Novartis, Amgen, Johnson & Johnson, Arbor, Mast, and Cardioxyl.
NATIONAL HARBOR, MD. – A next-generation left-ventricular assist device, the HeartMate 3, gave a solid debut performance in an uncontrolled series of the first 50 recipients, which was designed to gain the device CE mark approval in Europe.
In this study, run at 10 sites in Australia, Austria, Canada, Czech Republic, Germany, and Kazakhstan, the new-design left ventricular assist device (LVAD) numerically surpassed the study’s prespecified primary endpoint with 6-month recipient survival of 92%. This bested the target survival rate of 88% that the trial’s designers derived from the survival rate among 50 matched patients who had received a LVAD during 2012-2014 and had entered the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS), Dr. Ivan Netuka said at the annual meeting of the Heart Failure Society of America.
Other notable findings of the HeartMate 3’s performance in the first 50 patients followed for 6 months were no pump malfunctions, no thrombosis within the pump, and no evidence of hemolysis, said Dr. Netuka, deputy director of cardiovascular surgery at IKEM hospital in Prague.
HeartMate 3 features several improvements over the HeartMate II model, such as a fully magnetically levitated rotor designed to eliminate friction and wear within the pump. The device also is engineered to produce an artificial pulse of 30 beats per minute, and it can deliver a wide blood-flow range of 2-10 L/min. Larger and consistent pump gaps are designed to reduced shear stress on blood components.
The study enrolled patients during June-November 2014 with NYHA class IIIB or IV heart failure and stage D heart failure, with a left ventricular ejection fraction of 25% or less. The 50 patients averaged 59 years of age and 90% were men; they were divided about equally between patients who received the device as a bridge to transplant and those who received the LVAD as destination therapy.
During 6 months of follow-up, two patients received a heart transplant. Twenty-one (42%) of the enrolled patients classified as INTERMACS patient profile 3, 20 (40%) as profile 4, and 5 (10%) as profile 2 patients, with the remaining four patients falling into other profile levels. Twenty-one patients had concomitant heart surgery when they received their LVAD, usually valve replacement. All patients received warfarin treatment and aspirin following device placement. Dr. Netuka and his associates calculated an expected 6-month survival of 78% for the enrolled patients without LVAD intervention.
The four deaths included a patient who died from cardiac arrest following a stroke on day 19 – a complication judged attributable to the device-placement procedure, a patient with circulatory failure on day 48, a suicide on day 113, and a patient with multiorgan failure on day 144.
After 6 months of follow-up, notable adverse events included bleeding in 19 patients (38%) – including gastrointestinal bleeds in 4 patients (8%) – strokes in 6 patients (12%), and infections in 18 patients (36%). Most of the adverse events occurred in the first 7 days following LVAD placement. Three of the six strokes were judged procedure associated, Dr. Netuka said.
Following device placement, patients showed improvements in their NYHA class and quality of life; their 6-minute walk distance improved by an average of 231 m.
The HeartMate 3 device is currently undergoing U.S. assessment in comparison to HeartMate II prior to submission to the Food and Drug Administration. The randomized trial, known as MOMENTUM 3, plans to enroll 1,028 patients with completion scheduled for 2018.
The study was sponsored by Thoratec, which is developing the HeartMate 3 device. Dr. Netuka is a speaker for and consultant to Thoratec.
On Twitter @mitchelzoler
NATIONAL HARBOR, MD. – A next-generation left-ventricular assist device, the HeartMate 3, gave a solid debut performance in an uncontrolled series of the first 50 recipients, which was designed to gain the device CE mark approval in Europe.
In this study, run at 10 sites in Australia, Austria, Canada, Czech Republic, Germany, and Kazakhstan, the new-design left ventricular assist device (LVAD) numerically surpassed the study’s prespecified primary endpoint with 6-month recipient survival of 92%. This bested the target survival rate of 88% that the trial’s designers derived from the survival rate among 50 matched patients who had received a LVAD during 2012-2014 and had entered the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS), Dr. Ivan Netuka said at the annual meeting of the Heart Failure Society of America.
Other notable findings of the HeartMate 3’s performance in the first 50 patients followed for 6 months were no pump malfunctions, no thrombosis within the pump, and no evidence of hemolysis, said Dr. Netuka, deputy director of cardiovascular surgery at IKEM hospital in Prague.
HeartMate 3 features several improvements over the HeartMate II model, such as a fully magnetically levitated rotor designed to eliminate friction and wear within the pump. The device also is engineered to produce an artificial pulse of 30 beats per minute, and it can deliver a wide blood-flow range of 2-10 L/min. Larger and consistent pump gaps are designed to reduced shear stress on blood components.
The study enrolled patients during June-November 2014 with NYHA class IIIB or IV heart failure and stage D heart failure, with a left ventricular ejection fraction of 25% or less. The 50 patients averaged 59 years of age and 90% were men; they were divided about equally between patients who received the device as a bridge to transplant and those who received the LVAD as destination therapy.
During 6 months of follow-up, two patients received a heart transplant. Twenty-one (42%) of the enrolled patients classified as INTERMACS patient profile 3, 20 (40%) as profile 4, and 5 (10%) as profile 2 patients, with the remaining four patients falling into other profile levels. Twenty-one patients had concomitant heart surgery when they received their LVAD, usually valve replacement. All patients received warfarin treatment and aspirin following device placement. Dr. Netuka and his associates calculated an expected 6-month survival of 78% for the enrolled patients without LVAD intervention.
The four deaths included a patient who died from cardiac arrest following a stroke on day 19 – a complication judged attributable to the device-placement procedure, a patient with circulatory failure on day 48, a suicide on day 113, and a patient with multiorgan failure on day 144.
After 6 months of follow-up, notable adverse events included bleeding in 19 patients (38%) – including gastrointestinal bleeds in 4 patients (8%) – strokes in 6 patients (12%), and infections in 18 patients (36%). Most of the adverse events occurred in the first 7 days following LVAD placement. Three of the six strokes were judged procedure associated, Dr. Netuka said.
Following device placement, patients showed improvements in their NYHA class and quality of life; their 6-minute walk distance improved by an average of 231 m.
The HeartMate 3 device is currently undergoing U.S. assessment in comparison to HeartMate II prior to submission to the Food and Drug Administration. The randomized trial, known as MOMENTUM 3, plans to enroll 1,028 patients with completion scheduled for 2018.
The study was sponsored by Thoratec, which is developing the HeartMate 3 device. Dr. Netuka is a speaker for and consultant to Thoratec.
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point: A next-generation left ventricular assist device, HeartMate 3, met its 6-month survival goal to receive CE mark approval in Europe.
Major finding: The advanced heart failure patients who received the HeartMate 3 LVAD had a 92% survival rate after 6 months.
Data source: A prospective series of 50 patients enrolled at 10 centers in six countries.
Disclosures: The study was sponsored by Thoratec, which is developing the HeartMate 3 device. Dr. Netuka is a speaker for and consultant to Thoratec.
Mentoring that takes it up a notch
Everything seems to be extreme nowadays – “Extreme Makeover: Home Edition,” “Extreme Weight Loss,” even “Extreme Fishing” and “Extreme Couponing” – so it was only a matter of time that extreme came to cardiothoracic surgery.
Dr. Michael K. Pasque of Washington University in St. Louis explored “Extreme Mentoring in Cardiothoracic Surgery” in his commentary published online ahead of print for the October issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2015 doi: 10.1016/j.jtcvs.2015.04.056).
Meaningful mentoring “carries with it considerable responsibility. Extreme mentoring comes only at a price – it is going to cost us,” Dr. Pasque wrote, calling on academic cardiothoracic surgical mentors to perform a self-appraisal of their commitment and mentoring skills. He even developed a self-appraisal checklist that involves 37 different markers in four different categories: general; goals, pathways, and meetings; milestone timelines and taking action; and clinical assistance.
The first step in extreme mentoring for the academic cardiothoracic surgeon is to focus exclusively on the mentee. “As cardiothoracic surgeons, we are used to having the attention focused on us,” Dr. Pasque noted, but mentoring is different: the “energy of our relationship” must focus on the mentee.
The next step involves an objective assessment of the mentee. “If we are to throw our support wholeheartedly behind our mentee, we must genuinely believe in them,” he said. This assessment leads to setting goals for the mentee. “My formula is to honestly estimate the surgical, research, teaching and academic life goals that are both desired by and within reach of our mentee – and then double them,” he said. “We must set very aggressive goals for our mentee.”
Achieving those goals involves directing mentees to the right pathway and then helping them stay on that pathway despite obstacles. “When their progress through these barriers is discussed – and that should be often – then ours should be the voice that reminds them that despite the momentary setbacks, the goals we have set are going to happen,” Dr. Pasque said.
The process involves frequent “and substantive” meetings between mentor and mentee and establishing timelines for achieving milestones and goals. The mentor must back up what happens in those meetings with action – both overt, like assisting them in surgery or introducing them to influential colleagues, and covert in ways the mentee may never know about.
One “clandestine” operation involves the mentor keeping an updated list of 10 individuals who have the most to offer the mentee, “especially in areas in which we have limited or no influence,” and habitually following up with them. The mentor must be willing to “pick a fight” so the mentee doesn’t get left behind on call while senior colleagues attend meetings.
“We must be the senior voice that speaks up for them,” Dr. Pasque wrote. “They need to attend these meetings, even if it is we who must stay behind in their place.”
The mentoring process involves being across the operating room table from them at key milestones in their surgical development and being on-call 24/7 for the mentee. That may seem like extreme handholding to some critics, but Dr. Pasque said that letting a patient suffer or die is inexcusable. “Our first priority is always the patient’s well-being.”
The mentor must show respect to the mentee and practice “extreme encouragement,” especially in the operating room. “There is something magical about being told you are a good surgeon,” he said. “You become one.” This isn’t about falsely building up the mentee, but instilling the confidence to act on the patient’s behalf. The mentee will face enough doubters. “We must be the voice that assures them otherwise,” he said.
Teaching leadership also is key for the mentor. Mentors teach leadership by modeling it. “The best leaders are always those who place the needs of others above their own,” Dr. Pasque pointed out, harkening back to putting the focus on the mentee. “We can’t teach them to put the needs of others above their own without putting their needs about ours.”
Ultimately, the mentor’s greatest desire should be that the mentee exceeds them, “that they make everyone forget about us,” Dr. Pasque said. That would be the “crowning achievement” that would make the mentor “most unforgettable.”
Dr. Pasque had no disclosures.
Everything seems to be extreme nowadays – “Extreme Makeover: Home Edition,” “Extreme Weight Loss,” even “Extreme Fishing” and “Extreme Couponing” – so it was only a matter of time that extreme came to cardiothoracic surgery.
Dr. Michael K. Pasque of Washington University in St. Louis explored “Extreme Mentoring in Cardiothoracic Surgery” in his commentary published online ahead of print for the October issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2015 doi: 10.1016/j.jtcvs.2015.04.056).
Meaningful mentoring “carries with it considerable responsibility. Extreme mentoring comes only at a price – it is going to cost us,” Dr. Pasque wrote, calling on academic cardiothoracic surgical mentors to perform a self-appraisal of their commitment and mentoring skills. He even developed a self-appraisal checklist that involves 37 different markers in four different categories: general; goals, pathways, and meetings; milestone timelines and taking action; and clinical assistance.
The first step in extreme mentoring for the academic cardiothoracic surgeon is to focus exclusively on the mentee. “As cardiothoracic surgeons, we are used to having the attention focused on us,” Dr. Pasque noted, but mentoring is different: the “energy of our relationship” must focus on the mentee.
The next step involves an objective assessment of the mentee. “If we are to throw our support wholeheartedly behind our mentee, we must genuinely believe in them,” he said. This assessment leads to setting goals for the mentee. “My formula is to honestly estimate the surgical, research, teaching and academic life goals that are both desired by and within reach of our mentee – and then double them,” he said. “We must set very aggressive goals for our mentee.”
Achieving those goals involves directing mentees to the right pathway and then helping them stay on that pathway despite obstacles. “When their progress through these barriers is discussed – and that should be often – then ours should be the voice that reminds them that despite the momentary setbacks, the goals we have set are going to happen,” Dr. Pasque said.
The process involves frequent “and substantive” meetings between mentor and mentee and establishing timelines for achieving milestones and goals. The mentor must back up what happens in those meetings with action – both overt, like assisting them in surgery or introducing them to influential colleagues, and covert in ways the mentee may never know about.
One “clandestine” operation involves the mentor keeping an updated list of 10 individuals who have the most to offer the mentee, “especially in areas in which we have limited or no influence,” and habitually following up with them. The mentor must be willing to “pick a fight” so the mentee doesn’t get left behind on call while senior colleagues attend meetings.
“We must be the senior voice that speaks up for them,” Dr. Pasque wrote. “They need to attend these meetings, even if it is we who must stay behind in their place.”
The mentoring process involves being across the operating room table from them at key milestones in their surgical development and being on-call 24/7 for the mentee. That may seem like extreme handholding to some critics, but Dr. Pasque said that letting a patient suffer or die is inexcusable. “Our first priority is always the patient’s well-being.”
The mentor must show respect to the mentee and practice “extreme encouragement,” especially in the operating room. “There is something magical about being told you are a good surgeon,” he said. “You become one.” This isn’t about falsely building up the mentee, but instilling the confidence to act on the patient’s behalf. The mentee will face enough doubters. “We must be the voice that assures them otherwise,” he said.
Teaching leadership also is key for the mentor. Mentors teach leadership by modeling it. “The best leaders are always those who place the needs of others above their own,” Dr. Pasque pointed out, harkening back to putting the focus on the mentee. “We can’t teach them to put the needs of others above their own without putting their needs about ours.”
Ultimately, the mentor’s greatest desire should be that the mentee exceeds them, “that they make everyone forget about us,” Dr. Pasque said. That would be the “crowning achievement” that would make the mentor “most unforgettable.”
Dr. Pasque had no disclosures.
Everything seems to be extreme nowadays – “Extreme Makeover: Home Edition,” “Extreme Weight Loss,” even “Extreme Fishing” and “Extreme Couponing” – so it was only a matter of time that extreme came to cardiothoracic surgery.
Dr. Michael K. Pasque of Washington University in St. Louis explored “Extreme Mentoring in Cardiothoracic Surgery” in his commentary published online ahead of print for the October issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2015 doi: 10.1016/j.jtcvs.2015.04.056).
Meaningful mentoring “carries with it considerable responsibility. Extreme mentoring comes only at a price – it is going to cost us,” Dr. Pasque wrote, calling on academic cardiothoracic surgical mentors to perform a self-appraisal of their commitment and mentoring skills. He even developed a self-appraisal checklist that involves 37 different markers in four different categories: general; goals, pathways, and meetings; milestone timelines and taking action; and clinical assistance.
The first step in extreme mentoring for the academic cardiothoracic surgeon is to focus exclusively on the mentee. “As cardiothoracic surgeons, we are used to having the attention focused on us,” Dr. Pasque noted, but mentoring is different: the “energy of our relationship” must focus on the mentee.
The next step involves an objective assessment of the mentee. “If we are to throw our support wholeheartedly behind our mentee, we must genuinely believe in them,” he said. This assessment leads to setting goals for the mentee. “My formula is to honestly estimate the surgical, research, teaching and academic life goals that are both desired by and within reach of our mentee – and then double them,” he said. “We must set very aggressive goals for our mentee.”
Achieving those goals involves directing mentees to the right pathway and then helping them stay on that pathway despite obstacles. “When their progress through these barriers is discussed – and that should be often – then ours should be the voice that reminds them that despite the momentary setbacks, the goals we have set are going to happen,” Dr. Pasque said.
The process involves frequent “and substantive” meetings between mentor and mentee and establishing timelines for achieving milestones and goals. The mentor must back up what happens in those meetings with action – both overt, like assisting them in surgery or introducing them to influential colleagues, and covert in ways the mentee may never know about.
One “clandestine” operation involves the mentor keeping an updated list of 10 individuals who have the most to offer the mentee, “especially in areas in which we have limited or no influence,” and habitually following up with them. The mentor must be willing to “pick a fight” so the mentee doesn’t get left behind on call while senior colleagues attend meetings.
“We must be the senior voice that speaks up for them,” Dr. Pasque wrote. “They need to attend these meetings, even if it is we who must stay behind in their place.”
The mentoring process involves being across the operating room table from them at key milestones in their surgical development and being on-call 24/7 for the mentee. That may seem like extreme handholding to some critics, but Dr. Pasque said that letting a patient suffer or die is inexcusable. “Our first priority is always the patient’s well-being.”
The mentor must show respect to the mentee and practice “extreme encouragement,” especially in the operating room. “There is something magical about being told you are a good surgeon,” he said. “You become one.” This isn’t about falsely building up the mentee, but instilling the confidence to act on the patient’s behalf. The mentee will face enough doubters. “We must be the voice that assures them otherwise,” he said.
Teaching leadership also is key for the mentor. Mentors teach leadership by modeling it. “The best leaders are always those who place the needs of others above their own,” Dr. Pasque pointed out, harkening back to putting the focus on the mentee. “We can’t teach them to put the needs of others above their own without putting their needs about ours.”
Ultimately, the mentor’s greatest desire should be that the mentee exceeds them, “that they make everyone forget about us,” Dr. Pasque said. That would be the “crowning achievement” that would make the mentor “most unforgettable.”
Dr. Pasque had no disclosures.
Point/Counterpoint: Does surgery play a role in N2 disease treatment following induction therapy?
POINT: Surgery has its uses for some
BY DR. STEPHEN G. SWISHER
When talking about the role of surgery after induction therapy with persistent N2 disease, one must acknowledge that this is such a heterogeneous disease. You can have single-station N2; resectable, bulky multistation N2; and so on. Then there’s unresectable stage IIIA, but let’s focus mainly on resectable stage IIIA disease.
I can’t tell you how many audiences I’ve faced that absolutely believe the myth that surgery plays no role in Stage IIIA non–small cell lung cancer based on data from stage IIIA disease patients randomized to chemoradiation followed by surgery. The problem with these study results is the high mortality in the pneumonectomy subset. There’s no difference in the overall survival of the two groups, but that doesn’t mean that everyone in that group wouldn’t benefit from surgery.
The curve showed that pneumonectomy did not benefit after chemoradiation in a non–high-volume center. You can see a steep drop in the mortality early on, but it catches up again at the end. If you look at the overall 5-year survival rate, even in the pneumonectomy subset, you’re looking at 22% vs. 24%.
But in the lobectomy set, you see something completely different. You’ve got a doubling of survivors and no mortality early on, and a doubling of 5-year survival from 18% to 36%.
And yet, people continue saying that there’s no role for surgery. Well, I think there is a role for surgery, and there are subsets of N2 for which surgery can be particularly beneficial. We have to move more toward what the medical oncologists do, which is personalize therapy and look at subsets of N2 disease so that we know which patients we can benefit and which ones we can’t.
Moving on to the second myth: Surgery plays no role in N2 residual disease after induction therapy. This myth is based on the results of a couple of prospective studies in the 1980s and ’90s that showed residual N2 disease after chemo- and radiotherapy leads to survival of 16-35 months in most cases. I’d say that those results are true, but it’s not to say there aren’t subsets within these populations that benefited. With preoperative chemo and radiation, it’s basically the same thing – poor prognoses in patients with N2 or N3 disease, so the standard becomes never to operate on these individuals.
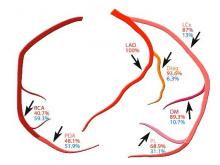
A European study prospectively took 30 patients and treated them with induction chemotherapy. They saw a 5-year survival rate of 62% if a patient downgrades to lymph node–negative disease and the positron-emission tomographic (PET) findings were good. But they also saw a subset with a small amount of disease within the lymph nodes at the N2 stage and a poor response on PET; Their 5-year survival rate was around 19%. So I’d argue that PET response and the number of lymph nodes involved are the key criteria, and you shouldn’t routinely deny surgery to these patients.
Our experience at MD Anderson Cancer Center over the last 10 years has been to treat N2 and N3 admissions, with surgery, followed by postoperative radiation of 50 Gy. We’re able to achieve very-low morbidity with this regimen, and no mortality after 30 and 90 days. Just to show the heterogeneity: Single-station, microscopic N2 disease should really be resected.
You just can’t lump together everyone with residual N2 after induction therapy, since PET-CTs and most other diagnostic procedures have high false-negative rates. And like I’ve said, it doesn’t matter because N2 disease is really a subset disease. Microscopic N2 disease behaves in a completely different way than does macroscopic, multiple-level N2 disease. And even more important is how the patient’s primary tumor responds to the chemotherapy or chemoradiation; that will tell you how well they’re going to do even if they have a small amount of residual disease in the lymph nodes.
Dr. Swisher is at the University of Texas MD Anderson Cancer Center in Houston. He disclosed that he is a consultant/advisory board member for GlaxoSmithKline.
COUNTERPOINT: Surgery seems to have little value, adds risk.
BY DR. SCOTT J. SWANSON
Dr. Swisher and I probably agree more than we disagree, but I’m going to start by saying that N2 disease is bad, and most of these populations are heterogeneous. But if you feel that a curve toward the bottom of a graph is good, then you should think twice. Anywhere from a 15%-30% survival rate is not great and shows that we have a long way to go. The overall impression among oncologists in several countries is that it’s not really clear whether surgery adds value. Even in very good centers like MD Anderson where there is minimal risk, surgery inherently still involves some risk.
So then, what do we do with persistent N2 disease? I’d say that most of the time, it should be treated with chemotherapy or chemotherapy and radiation. In some cases, N2 disease can be treated with a creative, mutation-driven immunotherapy approach. Most of the time though, surgery is just not a good idea.
Interestingly, about one-third of lung cancer patients present with stage IIIA disease, so it’s important that we as a medical community sort out these treatment options. I think we’re all in agreement that single-station, microscopic, PET-negative/CT-negative disease is not the same as extranodal or multistation PET-positive disease, so we’ve got to begin to substratify N2 disease.
In an intergroup trial of about 200 patients per arm published in the Lancet, patients went to surgery if they didn’t regress after evaluation. The progression-free survival rate did seem to favor surgery; and, if you look at the lobectomy subset, the results are certainly strong. But again, we’re dealing with curves that are pretty low. The pneumonectomy subset drops off and then starts to catch up, but clearly pneumonectomy was a problem in this multicenter trial. The most important graph to this debate shows subjects that persistently had nodal disease had very poor survival. It’s hard to argue for surgery when results show that only about 24% of them are going to be alive down the road. If oncologists across most of the United States say they believe that surgery isn’t a good idea, we’re not going to use this graph to change their minds; we need to change our way of thinking.
So the conclusion to take away from that presentation is that N0 status at surgery significantly predicts greater 5-year survival. So, conversely, surgery is not helpful for the patient with node-positive disease. Surgical resection should only be considered if lobectomy is the operation in question. Pneumonectomy carries risk, and surgery has no beneficial value, compared with chemotherapy unless the patient has been downstaged.
Our experience at Brigham and Women’s Hospital in Boston is similar to Dr. Swisher’s at MD Anderson. During the first 8 years of our thoracic division, we looked at 103 patients who had surgery after induction therapy for N2 disease. The induction plan in those patients was chemotherapy only for 75, radiation only for 18, and chemoradiation for 10. Almost 40% of patients had pneumonectomies, and the rest had lobectomies.
Mortality was 3.9%, major morbidity was 7%, and about 30% were downstaged. Those 5-year survival rates were about 36%. Persistent nodal disease, either N1 or N2, was seen in about 75%, and most of them were N2; the 5-year survival rate there was about 9% with a median of about 15.9 months. Beauty is in the eye of the beholder, so you may look at that and say that 15.9 months isn’t bad, but there’s still a huge subgroup that’s node positive, so here I’d say that pushing surgery is not the best strategy. We also found in this group that adenocarcinomas were much harder to clear.
We’re on very-safe ground to push surgery in the node-negative group, but you’ve got to be careful in the node-positive group.
Survival is relatively limited in N2 disease in general. Surgery may be of value if you downstage the patient, if you’re doing a lobectomy or if you see squamous cell carcinoma. Going forward, we really ought to focus our attention on identifying responders more reliably and improving downstaging – with different or individualized chemotherapy, or perhaps even immunologic therapy.
For the present, we can talk about radiation dosing. High-dose radiation is clearly a viable option for some patients. In addition, we can improve identification of N2 subgroups. Not all N2 disease is the same, so it should not be treated the same across the board.
Dr. Swanson is at Brigham and Women’s Hospital in Boston. He disclosed that he is a consultant/advisory board member for Covidien and Ethicon Endo-Surgery.
This article grew out of the debate by Dr. Swisher and Dr. Swanson at the annual meeting of the Society of Thoracic Surgeons.
POINT: Surgery has its uses for some
BY DR. STEPHEN G. SWISHER
When talking about the role of surgery after induction therapy with persistent N2 disease, one must acknowledge that this is such a heterogeneous disease. You can have single-station N2; resectable, bulky multistation N2; and so on. Then there’s unresectable stage IIIA, but let’s focus mainly on resectable stage IIIA disease.
I can’t tell you how many audiences I’ve faced that absolutely believe the myth that surgery plays no role in Stage IIIA non–small cell lung cancer based on data from stage IIIA disease patients randomized to chemoradiation followed by surgery. The problem with these study results is the high mortality in the pneumonectomy subset. There’s no difference in the overall survival of the two groups, but that doesn’t mean that everyone in that group wouldn’t benefit from surgery.
The curve showed that pneumonectomy did not benefit after chemoradiation in a non–high-volume center. You can see a steep drop in the mortality early on, but it catches up again at the end. If you look at the overall 5-year survival rate, even in the pneumonectomy subset, you’re looking at 22% vs. 24%.
But in the lobectomy set, you see something completely different. You’ve got a doubling of survivors and no mortality early on, and a doubling of 5-year survival from 18% to 36%.
And yet, people continue saying that there’s no role for surgery. Well, I think there is a role for surgery, and there are subsets of N2 for which surgery can be particularly beneficial. We have to move more toward what the medical oncologists do, which is personalize therapy and look at subsets of N2 disease so that we know which patients we can benefit and which ones we can’t.
Moving on to the second myth: Surgery plays no role in N2 residual disease after induction therapy. This myth is based on the results of a couple of prospective studies in the 1980s and ’90s that showed residual N2 disease after chemo- and radiotherapy leads to survival of 16-35 months in most cases. I’d say that those results are true, but it’s not to say there aren’t subsets within these populations that benefited. With preoperative chemo and radiation, it’s basically the same thing – poor prognoses in patients with N2 or N3 disease, so the standard becomes never to operate on these individuals.
A European study prospectively took 30 patients and treated them with induction chemotherapy. They saw a 5-year survival rate of 62% if a patient downgrades to lymph node–negative disease and the positron-emission tomographic (PET) findings were good. But they also saw a subset with a small amount of disease within the lymph nodes at the N2 stage and a poor response on PET; Their 5-year survival rate was around 19%. So I’d argue that PET response and the number of lymph nodes involved are the key criteria, and you shouldn’t routinely deny surgery to these patients.
Our experience at MD Anderson Cancer Center over the last 10 years has been to treat N2 and N3 admissions, with surgery, followed by postoperative radiation of 50 Gy. We’re able to achieve very-low morbidity with this regimen, and no mortality after 30 and 90 days. Just to show the heterogeneity: Single-station, microscopic N2 disease should really be resected.
You just can’t lump together everyone with residual N2 after induction therapy, since PET-CTs and most other diagnostic procedures have high false-negative rates. And like I’ve said, it doesn’t matter because N2 disease is really a subset disease. Microscopic N2 disease behaves in a completely different way than does macroscopic, multiple-level N2 disease. And even more important is how the patient’s primary tumor responds to the chemotherapy or chemoradiation; that will tell you how well they’re going to do even if they have a small amount of residual disease in the lymph nodes.
Dr. Swisher is at the University of Texas MD Anderson Cancer Center in Houston. He disclosed that he is a consultant/advisory board member for GlaxoSmithKline.
COUNTERPOINT: Surgery seems to have little value, adds risk.
BY DR. SCOTT J. SWANSON
Dr. Swisher and I probably agree more than we disagree, but I’m going to start by saying that N2 disease is bad, and most of these populations are heterogeneous. But if you feel that a curve toward the bottom of a graph is good, then you should think twice. Anywhere from a 15%-30% survival rate is not great and shows that we have a long way to go. The overall impression among oncologists in several countries is that it’s not really clear whether surgery adds value. Even in very good centers like MD Anderson where there is minimal risk, surgery inherently still involves some risk.
So then, what do we do with persistent N2 disease? I’d say that most of the time, it should be treated with chemotherapy or chemotherapy and radiation. In some cases, N2 disease can be treated with a creative, mutation-driven immunotherapy approach. Most of the time though, surgery is just not a good idea.
Interestingly, about one-third of lung cancer patients present with stage IIIA disease, so it’s important that we as a medical community sort out these treatment options. I think we’re all in agreement that single-station, microscopic, PET-negative/CT-negative disease is not the same as extranodal or multistation PET-positive disease, so we’ve got to begin to substratify N2 disease.
In an intergroup trial of about 200 patients per arm published in the Lancet, patients went to surgery if they didn’t regress after evaluation. The progression-free survival rate did seem to favor surgery; and, if you look at the lobectomy subset, the results are certainly strong. But again, we’re dealing with curves that are pretty low. The pneumonectomy subset drops off and then starts to catch up, but clearly pneumonectomy was a problem in this multicenter trial. The most important graph to this debate shows subjects that persistently had nodal disease had very poor survival. It’s hard to argue for surgery when results show that only about 24% of them are going to be alive down the road. If oncologists across most of the United States say they believe that surgery isn’t a good idea, we’re not going to use this graph to change their minds; we need to change our way of thinking.
So the conclusion to take away from that presentation is that N0 status at surgery significantly predicts greater 5-year survival. So, conversely, surgery is not helpful for the patient with node-positive disease. Surgical resection should only be considered if lobectomy is the operation in question. Pneumonectomy carries risk, and surgery has no beneficial value, compared with chemotherapy unless the patient has been downstaged.
Our experience at Brigham and Women’s Hospital in Boston is similar to Dr. Swisher’s at MD Anderson. During the first 8 years of our thoracic division, we looked at 103 patients who had surgery after induction therapy for N2 disease. The induction plan in those patients was chemotherapy only for 75, radiation only for 18, and chemoradiation for 10. Almost 40% of patients had pneumonectomies, and the rest had lobectomies.
Mortality was 3.9%, major morbidity was 7%, and about 30% were downstaged. Those 5-year survival rates were about 36%. Persistent nodal disease, either N1 or N2, was seen in about 75%, and most of them were N2; the 5-year survival rate there was about 9% with a median of about 15.9 months. Beauty is in the eye of the beholder, so you may look at that and say that 15.9 months isn’t bad, but there’s still a huge subgroup that’s node positive, so here I’d say that pushing surgery is not the best strategy. We also found in this group that adenocarcinomas were much harder to clear.
We’re on very-safe ground to push surgery in the node-negative group, but you’ve got to be careful in the node-positive group.
Survival is relatively limited in N2 disease in general. Surgery may be of value if you downstage the patient, if you’re doing a lobectomy or if you see squamous cell carcinoma. Going forward, we really ought to focus our attention on identifying responders more reliably and improving downstaging – with different or individualized chemotherapy, or perhaps even immunologic therapy.
For the present, we can talk about radiation dosing. High-dose radiation is clearly a viable option for some patients. In addition, we can improve identification of N2 subgroups. Not all N2 disease is the same, so it should not be treated the same across the board.
Dr. Swanson is at Brigham and Women’s Hospital in Boston. He disclosed that he is a consultant/advisory board member for Covidien and Ethicon Endo-Surgery.
This article grew out of the debate by Dr. Swisher and Dr. Swanson at the annual meeting of the Society of Thoracic Surgeons.
POINT: Surgery has its uses for some
BY DR. STEPHEN G. SWISHER
When talking about the role of surgery after induction therapy with persistent N2 disease, one must acknowledge that this is such a heterogeneous disease. You can have single-station N2; resectable, bulky multistation N2; and so on. Then there’s unresectable stage IIIA, but let’s focus mainly on resectable stage IIIA disease.
I can’t tell you how many audiences I’ve faced that absolutely believe the myth that surgery plays no role in Stage IIIA non–small cell lung cancer based on data from stage IIIA disease patients randomized to chemoradiation followed by surgery. The problem with these study results is the high mortality in the pneumonectomy subset. There’s no difference in the overall survival of the two groups, but that doesn’t mean that everyone in that group wouldn’t benefit from surgery.
The curve showed that pneumonectomy did not benefit after chemoradiation in a non–high-volume center. You can see a steep drop in the mortality early on, but it catches up again at the end. If you look at the overall 5-year survival rate, even in the pneumonectomy subset, you’re looking at 22% vs. 24%.
But in the lobectomy set, you see something completely different. You’ve got a doubling of survivors and no mortality early on, and a doubling of 5-year survival from 18% to 36%.
And yet, people continue saying that there’s no role for surgery. Well, I think there is a role for surgery, and there are subsets of N2 for which surgery can be particularly beneficial. We have to move more toward what the medical oncologists do, which is personalize therapy and look at subsets of N2 disease so that we know which patients we can benefit and which ones we can’t.
Moving on to the second myth: Surgery plays no role in N2 residual disease after induction therapy. This myth is based on the results of a couple of prospective studies in the 1980s and ’90s that showed residual N2 disease after chemo- and radiotherapy leads to survival of 16-35 months in most cases. I’d say that those results are true, but it’s not to say there aren’t subsets within these populations that benefited. With preoperative chemo and radiation, it’s basically the same thing – poor prognoses in patients with N2 or N3 disease, so the standard becomes never to operate on these individuals.
A European study prospectively took 30 patients and treated them with induction chemotherapy. They saw a 5-year survival rate of 62% if a patient downgrades to lymph node–negative disease and the positron-emission tomographic (PET) findings were good. But they also saw a subset with a small amount of disease within the lymph nodes at the N2 stage and a poor response on PET; Their 5-year survival rate was around 19%. So I’d argue that PET response and the number of lymph nodes involved are the key criteria, and you shouldn’t routinely deny surgery to these patients.
Our experience at MD Anderson Cancer Center over the last 10 years has been to treat N2 and N3 admissions, with surgery, followed by postoperative radiation of 50 Gy. We’re able to achieve very-low morbidity with this regimen, and no mortality after 30 and 90 days. Just to show the heterogeneity: Single-station, microscopic N2 disease should really be resected.
You just can’t lump together everyone with residual N2 after induction therapy, since PET-CTs and most other diagnostic procedures have high false-negative rates. And like I’ve said, it doesn’t matter because N2 disease is really a subset disease. Microscopic N2 disease behaves in a completely different way than does macroscopic, multiple-level N2 disease. And even more important is how the patient’s primary tumor responds to the chemotherapy or chemoradiation; that will tell you how well they’re going to do even if they have a small amount of residual disease in the lymph nodes.
Dr. Swisher is at the University of Texas MD Anderson Cancer Center in Houston. He disclosed that he is a consultant/advisory board member for GlaxoSmithKline.
COUNTERPOINT: Surgery seems to have little value, adds risk.
BY DR. SCOTT J. SWANSON
Dr. Swisher and I probably agree more than we disagree, but I’m going to start by saying that N2 disease is bad, and most of these populations are heterogeneous. But if you feel that a curve toward the bottom of a graph is good, then you should think twice. Anywhere from a 15%-30% survival rate is not great and shows that we have a long way to go. The overall impression among oncologists in several countries is that it’s not really clear whether surgery adds value. Even in very good centers like MD Anderson where there is minimal risk, surgery inherently still involves some risk.
So then, what do we do with persistent N2 disease? I’d say that most of the time, it should be treated with chemotherapy or chemotherapy and radiation. In some cases, N2 disease can be treated with a creative, mutation-driven immunotherapy approach. Most of the time though, surgery is just not a good idea.
Interestingly, about one-third of lung cancer patients present with stage IIIA disease, so it’s important that we as a medical community sort out these treatment options. I think we’re all in agreement that single-station, microscopic, PET-negative/CT-negative disease is not the same as extranodal or multistation PET-positive disease, so we’ve got to begin to substratify N2 disease.
In an intergroup trial of about 200 patients per arm published in the Lancet, patients went to surgery if they didn’t regress after evaluation. The progression-free survival rate did seem to favor surgery; and, if you look at the lobectomy subset, the results are certainly strong. But again, we’re dealing with curves that are pretty low. The pneumonectomy subset drops off and then starts to catch up, but clearly pneumonectomy was a problem in this multicenter trial. The most important graph to this debate shows subjects that persistently had nodal disease had very poor survival. It’s hard to argue for surgery when results show that only about 24% of them are going to be alive down the road. If oncologists across most of the United States say they believe that surgery isn’t a good idea, we’re not going to use this graph to change their minds; we need to change our way of thinking.
So the conclusion to take away from that presentation is that N0 status at surgery significantly predicts greater 5-year survival. So, conversely, surgery is not helpful for the patient with node-positive disease. Surgical resection should only be considered if lobectomy is the operation in question. Pneumonectomy carries risk, and surgery has no beneficial value, compared with chemotherapy unless the patient has been downstaged.
Our experience at Brigham and Women’s Hospital in Boston is similar to Dr. Swisher’s at MD Anderson. During the first 8 years of our thoracic division, we looked at 103 patients who had surgery after induction therapy for N2 disease. The induction plan in those patients was chemotherapy only for 75, radiation only for 18, and chemoradiation for 10. Almost 40% of patients had pneumonectomies, and the rest had lobectomies.
Mortality was 3.9%, major morbidity was 7%, and about 30% were downstaged. Those 5-year survival rates were about 36%. Persistent nodal disease, either N1 or N2, was seen in about 75%, and most of them were N2; the 5-year survival rate there was about 9% with a median of about 15.9 months. Beauty is in the eye of the beholder, so you may look at that and say that 15.9 months isn’t bad, but there’s still a huge subgroup that’s node positive, so here I’d say that pushing surgery is not the best strategy. We also found in this group that adenocarcinomas were much harder to clear.
We’re on very-safe ground to push surgery in the node-negative group, but you’ve got to be careful in the node-positive group.
Survival is relatively limited in N2 disease in general. Surgery may be of value if you downstage the patient, if you’re doing a lobectomy or if you see squamous cell carcinoma. Going forward, we really ought to focus our attention on identifying responders more reliably and improving downstaging – with different or individualized chemotherapy, or perhaps even immunologic therapy.
For the present, we can talk about radiation dosing. High-dose radiation is clearly a viable option for some patients. In addition, we can improve identification of N2 subgroups. Not all N2 disease is the same, so it should not be treated the same across the board.
Dr. Swanson is at Brigham and Women’s Hospital in Boston. He disclosed that he is a consultant/advisory board member for Covidien and Ethicon Endo-Surgery.
This article grew out of the debate by Dr. Swisher and Dr. Swanson at the annual meeting of the Society of Thoracic Surgeons.
Combined percutaneous procedures emerging in Europe
NEW YORK – Combined transcatheter mitral valve interventions with the potential to have results as good as cardiac surgery are beginning to emerge in Europe, where cardiac surgeons are also getting early experience with newer transcatheter systems that offer alternatives to existing mitral valve treatments, said Dr. Francesco Maisano.
Surgeons in Europe are investigating for mitral valve repair, as alternatives to the MitraClip (Abbott Vascular) percutaneous mitral valve system, and developers of these devices have met their share of challenges, Dr. Maisano of the University Hospital Zurich (Switzerland) said at the 2015 Mitral Valve Conclave, sponsored by the American Association for Thoracic Surgery.
“This list was much longer in the past, but some of the companies have lost their way in the past few years,” he said. “This is because it is difficult to pursue such a tremendous effort of doing a transcatheter repair that is competing with a device that has been commercially available.”
The NeoChord system (NeoChord) has been approved in Europe and has been implanted in about 200 patients so far. It is implanted through a small (2-3–inch) left thoracotomy and deploys implantation of multiple neochordae. “This is slowly getting into practice,” Dr. Maisano said. “The main problem with this technology is that it still is a hybrid procedure; it requires general anesthesia. It’s still doubtful what the role will be for this procedure in the spectrum of mitral interventions.”
The Carillon Mitral Contour System (Cardiac Dimension Inc.) is “the only coronary sinus annuloplasty technology that survived in these years,” he said. The device is in clinical trials in Europe and Australia. However, he noted, efficacy with the device “doesn’t happen at the implant, but it happens over time.” Group outcomes data is pending. “Enthusiasm around coronary sinus annuloplasty never took, so a lot of physicians are still reluctant to embrace this technology,” he said. Nonetheless, in some patients the device has show results ”as good as other procedures.”
Meanwhile, three other percutaneous systems that aim to reproduce surgical annuloplasty are in development: the Mitralign (Mitralign), a percutaneous system that selectively plicates the annulus using pledget sutures; the Accucinch (Guided Delivery Systems) which completes a full-seal annuloplasty using suture-connected mitral anchors; and Cardioband (ValtechCardio), which can perform surgery-like annuloplasty without sutures. Dr. Maisano said Mitralign is hopeful to get CE-mark approval possibly as early as this year, and the Cardioband has been implanted in 42 patients in Europe with an average 22% reduction in septal dimensions – “good outcomes in terms of reduction of mitral regurgitation and improvement of symptoms,” he said.
Helping to advance the development of percutaneous procedures and the promise of combining those procedures to replicate surgery is the integration of multimodal imaging in the cardiac suite, Dr. Maisano said.
“There are many problems to be solved” in pursuing combined percutaneous procedures to replicate surgical results, he said. “It’s not easy from a regulatory standpoint or from an economical standpoint, but there is the potential to simulate what is done today in surgery-associated procedures. This is something that is happening in Europe, which is land of freedom in terms of utilizing devices.”
He related the story of a patient in whom he implanted two mitral valve clips and then, to stop leakage, used a vascular plug to fill the gap in the subcommissure. European cardiac surgeons have pondered or attempted transcatheter aortic implantation (TAVI) in combination with other procedures, including left atrial appendage closure (LAAC) and mitral clip insertion in varied combinations. “This is still feasible and something that is getting done more in Europe in experienced centers,” Dr. Maisano said. Although feasibility, safety, and efficacy of such approaches need to be proved in larger series, combination therapy will evolve in the future, in an attempt to reproduce surgical standards, he said.
Findings were presented on behalf of the European Society of Cardiology. Dr. Maisano is a consultant for Abbott Vascular and ValtechCardio, among other companies. He receives royalties from Edwards Lifesciences.
NEW YORK – Combined transcatheter mitral valve interventions with the potential to have results as good as cardiac surgery are beginning to emerge in Europe, where cardiac surgeons are also getting early experience with newer transcatheter systems that offer alternatives to existing mitral valve treatments, said Dr. Francesco Maisano.
Surgeons in Europe are investigating for mitral valve repair, as alternatives to the MitraClip (Abbott Vascular) percutaneous mitral valve system, and developers of these devices have met their share of challenges, Dr. Maisano of the University Hospital Zurich (Switzerland) said at the 2015 Mitral Valve Conclave, sponsored by the American Association for Thoracic Surgery.
“This list was much longer in the past, but some of the companies have lost their way in the past few years,” he said. “This is because it is difficult to pursue such a tremendous effort of doing a transcatheter repair that is competing with a device that has been commercially available.”
The NeoChord system (NeoChord) has been approved in Europe and has been implanted in about 200 patients so far. It is implanted through a small (2-3–inch) left thoracotomy and deploys implantation of multiple neochordae. “This is slowly getting into practice,” Dr. Maisano said. “The main problem with this technology is that it still is a hybrid procedure; it requires general anesthesia. It’s still doubtful what the role will be for this procedure in the spectrum of mitral interventions.”
The Carillon Mitral Contour System (Cardiac Dimension Inc.) is “the only coronary sinus annuloplasty technology that survived in these years,” he said. The device is in clinical trials in Europe and Australia. However, he noted, efficacy with the device “doesn’t happen at the implant, but it happens over time.” Group outcomes data is pending. “Enthusiasm around coronary sinus annuloplasty never took, so a lot of physicians are still reluctant to embrace this technology,” he said. Nonetheless, in some patients the device has show results ”as good as other procedures.”
Meanwhile, three other percutaneous systems that aim to reproduce surgical annuloplasty are in development: the Mitralign (Mitralign), a percutaneous system that selectively plicates the annulus using pledget sutures; the Accucinch (Guided Delivery Systems) which completes a full-seal annuloplasty using suture-connected mitral anchors; and Cardioband (ValtechCardio), which can perform surgery-like annuloplasty without sutures. Dr. Maisano said Mitralign is hopeful to get CE-mark approval possibly as early as this year, and the Cardioband has been implanted in 42 patients in Europe with an average 22% reduction in septal dimensions – “good outcomes in terms of reduction of mitral regurgitation and improvement of symptoms,” he said.
Helping to advance the development of percutaneous procedures and the promise of combining those procedures to replicate surgery is the integration of multimodal imaging in the cardiac suite, Dr. Maisano said.
“There are many problems to be solved” in pursuing combined percutaneous procedures to replicate surgical results, he said. “It’s not easy from a regulatory standpoint or from an economical standpoint, but there is the potential to simulate what is done today in surgery-associated procedures. This is something that is happening in Europe, which is land of freedom in terms of utilizing devices.”
He related the story of a patient in whom he implanted two mitral valve clips and then, to stop leakage, used a vascular plug to fill the gap in the subcommissure. European cardiac surgeons have pondered or attempted transcatheter aortic implantation (TAVI) in combination with other procedures, including left atrial appendage closure (LAAC) and mitral clip insertion in varied combinations. “This is still feasible and something that is getting done more in Europe in experienced centers,” Dr. Maisano said. Although feasibility, safety, and efficacy of such approaches need to be proved in larger series, combination therapy will evolve in the future, in an attempt to reproduce surgical standards, he said.
Findings were presented on behalf of the European Society of Cardiology. Dr. Maisano is a consultant for Abbott Vascular and ValtechCardio, among other companies. He receives royalties from Edwards Lifesciences.
NEW YORK – Combined transcatheter mitral valve interventions with the potential to have results as good as cardiac surgery are beginning to emerge in Europe, where cardiac surgeons are also getting early experience with newer transcatheter systems that offer alternatives to existing mitral valve treatments, said Dr. Francesco Maisano.
Surgeons in Europe are investigating for mitral valve repair, as alternatives to the MitraClip (Abbott Vascular) percutaneous mitral valve system, and developers of these devices have met their share of challenges, Dr. Maisano of the University Hospital Zurich (Switzerland) said at the 2015 Mitral Valve Conclave, sponsored by the American Association for Thoracic Surgery.
“This list was much longer in the past, but some of the companies have lost their way in the past few years,” he said. “This is because it is difficult to pursue such a tremendous effort of doing a transcatheter repair that is competing with a device that has been commercially available.”
The NeoChord system (NeoChord) has been approved in Europe and has been implanted in about 200 patients so far. It is implanted through a small (2-3–inch) left thoracotomy and deploys implantation of multiple neochordae. “This is slowly getting into practice,” Dr. Maisano said. “The main problem with this technology is that it still is a hybrid procedure; it requires general anesthesia. It’s still doubtful what the role will be for this procedure in the spectrum of mitral interventions.”
The Carillon Mitral Contour System (Cardiac Dimension Inc.) is “the only coronary sinus annuloplasty technology that survived in these years,” he said. The device is in clinical trials in Europe and Australia. However, he noted, efficacy with the device “doesn’t happen at the implant, but it happens over time.” Group outcomes data is pending. “Enthusiasm around coronary sinus annuloplasty never took, so a lot of physicians are still reluctant to embrace this technology,” he said. Nonetheless, in some patients the device has show results ”as good as other procedures.”
Meanwhile, three other percutaneous systems that aim to reproduce surgical annuloplasty are in development: the Mitralign (Mitralign), a percutaneous system that selectively plicates the annulus using pledget sutures; the Accucinch (Guided Delivery Systems) which completes a full-seal annuloplasty using suture-connected mitral anchors; and Cardioband (ValtechCardio), which can perform surgery-like annuloplasty without sutures. Dr. Maisano said Mitralign is hopeful to get CE-mark approval possibly as early as this year, and the Cardioband has been implanted in 42 patients in Europe with an average 22% reduction in septal dimensions – “good outcomes in terms of reduction of mitral regurgitation and improvement of symptoms,” he said.
Helping to advance the development of percutaneous procedures and the promise of combining those procedures to replicate surgery is the integration of multimodal imaging in the cardiac suite, Dr. Maisano said.
“There are many problems to be solved” in pursuing combined percutaneous procedures to replicate surgical results, he said. “It’s not easy from a regulatory standpoint or from an economical standpoint, but there is the potential to simulate what is done today in surgery-associated procedures. This is something that is happening in Europe, which is land of freedom in terms of utilizing devices.”
He related the story of a patient in whom he implanted two mitral valve clips and then, to stop leakage, used a vascular plug to fill the gap in the subcommissure. European cardiac surgeons have pondered or attempted transcatheter aortic implantation (TAVI) in combination with other procedures, including left atrial appendage closure (LAAC) and mitral clip insertion in varied combinations. “This is still feasible and something that is getting done more in Europe in experienced centers,” Dr. Maisano said. Although feasibility, safety, and efficacy of such approaches need to be proved in larger series, combination therapy will evolve in the future, in an attempt to reproduce surgical standards, he said.
Findings were presented on behalf of the European Society of Cardiology. Dr. Maisano is a consultant for Abbott Vascular and ValtechCardio, among other companies. He receives royalties from Edwards Lifesciences.
EXPERT ANALYSIS FROM THE 2015 MITRAL VALVE CONCLAVE
ESC: CERTITUDE casts doubt on defibrillator benefit in CRT
LONDON – Heart failure patients who are candidates for cardiac resynchronization therapy in a routine clinical practice setting will likely not benefit from the addition of a defibrillator to a pacemaker, according to results of the CERTITUDE cohort study.
In CERTITUDE, most of the deaths in patients fitted with a cardiac resynchronization therapy–pacemaker (CRT-P) device were predominantly from causes other than sudden cardiac death (SCD), which is the main rationale for using a CRT-defibrillator (CRT-D) device, said lead investigator Jean-Yves Le Heuzey at the annual congress of the European Society of Cardiology.
“Our results should not be interpreted as a general lack of benefit from CRT-D vs. CRT-P or vice versa. Rather we demonstrate that given currently selected CRT-P patients in the French population, addition of a defibrillator may not significantly add to survival.” Therefore, patients who may be eligible for CRT should not “automatically” be considered as requiring a CRT-D, suggested Dr. Le Heuzey and his coinvestigators in an article that was published online at the time of the study’s presentation (Eur Heart J. 2015 Sep 1. doi: 10.1093/eurheartj/ehv455).
Current ESC guidelines on cardiac pacing and cardiac resynchronization therapy “leave flexibility for the physician” on the use of CRT-P and CRT-D” because there was no evidence of a superior effect of the latter over CRT alone, said Dr. Le Heuzey of René Descartes University in Paris at the meeting. A randomized, controlled trial would be the only way to determine this, but such a trial is unlikely to ever be conducted, he noted.
Despite the lack of evidence, however, CRT-D is widely used, more so in the United States than in Europe, Dr. Le Heuzey observed, where more than 90% of patients needing CRT would likely have a CRT-D rather than a CRT-P device implanted.
The aims of the CERTITUDE cohort study were to look at the extent to which CRT-P patients differ from CRT-D patients in a real-life setting, and to also see if there were patients in the CRT-P group that might have benefited from CRT-D.
The prospective, observational study involved 1,705 patients who were recruited at 41 centers throughout France over a 2-year period starting in January 2008. Of these, 31% were fitted with a CRT-P device and 69% with a CRT-D.
Results showed that patients who had a CRT-P versus a CRT-D implanted were significantly older, more often female, and more symptomatic. They were also significantly less likely to have coronary artery disease, more likely to have wider QRS intervals and to have atrial fibrillation, and more often had at least two comorbidities.
Analysis of the causes of death was performed at 2 years’ follow-up, which Dr. Le Heuzey conceded was a short period of time. At this point, 267 of 1,611 patients with complete follow-up data had died, giving an overall mortality rate of 8.4% per 100 patient-years for the entire cohort.
The crude mortality rate was found to be higher among CRT-P than CRT-D patients, at 13.1% versus 6.5% per 100 patient-years (relative risk, 2.01; 95% confidence interval, 1.56-2.58; P less than .0001). But when the cause of death was examined more closely, there was no significant difference in the number of SCDs between the groups (RR, 1.57; 95% CI, 0.71-3.46; P = .42) and no significant difference when a specific cause of death analysis was performed.
The main reasons for the almost doubled risk of death in the CRT-P group was an increase in non-SCD cardiovascular mortality, mainly progressive heart failure (RR, 0.27; 95% CI, 1.62-3.18) and other cardiovascular causes (RR, 4.4; 95% CI, 1.29-15.03), Dr. Le Heuzey and associates noted in the article.
“Overall, 95% of the excess mortality among CRT-P recipients was not related to SCD,” they wrote, noting that this “suggests that the presence of a back-up defibrillator would probably not have been beneficial in terms of improving survival for these patients.”
So where does this leave clinicians? Dr. Le Heuzey referred to Table 17 in the European guidelines (Eur Heart J. 2013;34:2281-2329) with guidance on factors favoring CRT-P or CRT-D. For instance, CRT-P might be favorable in a patient with advanced heart failure or one with severe renal insufficiency or on dialysis. Other major comorbidities or frailty or cachexia might veer a decision towards CRT without a defibrillator. On the other hand, factors favoring CRT-D include a life expectancy of more than 1 year; stable, moderate (New York Heart Association class II) disease; or low to moderate–risk ischemic heart disease, with a lack of comorbidities.
CERTITUDE was funded by grants from the French Institute of Health and Medical Research (INSERM) and from the French Cardiology Society. The latter received specific grants from Biotronik, Boston Scientific, Medtronic, Saint Jude Medical, and Sorin in order to perform the study. Dr. Le Heuzey disclosed receiving fees for participation in advisory boards and conferences from AstraZeneca, Bayer, Boehringer-Ingelheim, Bristol Myers Squibb/Pfizer, Correvio, Daiichi-Sankyo, Meda, Sanofi, and Servier.
LONDON – Heart failure patients who are candidates for cardiac resynchronization therapy in a routine clinical practice setting will likely not benefit from the addition of a defibrillator to a pacemaker, according to results of the CERTITUDE cohort study.
In CERTITUDE, most of the deaths in patients fitted with a cardiac resynchronization therapy–pacemaker (CRT-P) device were predominantly from causes other than sudden cardiac death (SCD), which is the main rationale for using a CRT-defibrillator (CRT-D) device, said lead investigator Jean-Yves Le Heuzey at the annual congress of the European Society of Cardiology.
“Our results should not be interpreted as a general lack of benefit from CRT-D vs. CRT-P or vice versa. Rather we demonstrate that given currently selected CRT-P patients in the French population, addition of a defibrillator may not significantly add to survival.” Therefore, patients who may be eligible for CRT should not “automatically” be considered as requiring a CRT-D, suggested Dr. Le Heuzey and his coinvestigators in an article that was published online at the time of the study’s presentation (Eur Heart J. 2015 Sep 1. doi: 10.1093/eurheartj/ehv455).
Current ESC guidelines on cardiac pacing and cardiac resynchronization therapy “leave flexibility for the physician” on the use of CRT-P and CRT-D” because there was no evidence of a superior effect of the latter over CRT alone, said Dr. Le Heuzey of René Descartes University in Paris at the meeting. A randomized, controlled trial would be the only way to determine this, but such a trial is unlikely to ever be conducted, he noted.
Despite the lack of evidence, however, CRT-D is widely used, more so in the United States than in Europe, Dr. Le Heuzey observed, where more than 90% of patients needing CRT would likely have a CRT-D rather than a CRT-P device implanted.
The aims of the CERTITUDE cohort study were to look at the extent to which CRT-P patients differ from CRT-D patients in a real-life setting, and to also see if there were patients in the CRT-P group that might have benefited from CRT-D.
The prospective, observational study involved 1,705 patients who were recruited at 41 centers throughout France over a 2-year period starting in January 2008. Of these, 31% were fitted with a CRT-P device and 69% with a CRT-D.
Results showed that patients who had a CRT-P versus a CRT-D implanted were significantly older, more often female, and more symptomatic. They were also significantly less likely to have coronary artery disease, more likely to have wider QRS intervals and to have atrial fibrillation, and more often had at least two comorbidities.
Analysis of the causes of death was performed at 2 years’ follow-up, which Dr. Le Heuzey conceded was a short period of time. At this point, 267 of 1,611 patients with complete follow-up data had died, giving an overall mortality rate of 8.4% per 100 patient-years for the entire cohort.
The crude mortality rate was found to be higher among CRT-P than CRT-D patients, at 13.1% versus 6.5% per 100 patient-years (relative risk, 2.01; 95% confidence interval, 1.56-2.58; P less than .0001). But when the cause of death was examined more closely, there was no significant difference in the number of SCDs between the groups (RR, 1.57; 95% CI, 0.71-3.46; P = .42) and no significant difference when a specific cause of death analysis was performed.
The main reasons for the almost doubled risk of death in the CRT-P group was an increase in non-SCD cardiovascular mortality, mainly progressive heart failure (RR, 0.27; 95% CI, 1.62-3.18) and other cardiovascular causes (RR, 4.4; 95% CI, 1.29-15.03), Dr. Le Heuzey and associates noted in the article.
“Overall, 95% of the excess mortality among CRT-P recipients was not related to SCD,” they wrote, noting that this “suggests that the presence of a back-up defibrillator would probably not have been beneficial in terms of improving survival for these patients.”
So where does this leave clinicians? Dr. Le Heuzey referred to Table 17 in the European guidelines (Eur Heart J. 2013;34:2281-2329) with guidance on factors favoring CRT-P or CRT-D. For instance, CRT-P might be favorable in a patient with advanced heart failure or one with severe renal insufficiency or on dialysis. Other major comorbidities or frailty or cachexia might veer a decision towards CRT without a defibrillator. On the other hand, factors favoring CRT-D include a life expectancy of more than 1 year; stable, moderate (New York Heart Association class II) disease; or low to moderate–risk ischemic heart disease, with a lack of comorbidities.
CERTITUDE was funded by grants from the French Institute of Health and Medical Research (INSERM) and from the French Cardiology Society. The latter received specific grants from Biotronik, Boston Scientific, Medtronic, Saint Jude Medical, and Sorin in order to perform the study. Dr. Le Heuzey disclosed receiving fees for participation in advisory boards and conferences from AstraZeneca, Bayer, Boehringer-Ingelheim, Bristol Myers Squibb/Pfizer, Correvio, Daiichi-Sankyo, Meda, Sanofi, and Servier.
LONDON – Heart failure patients who are candidates for cardiac resynchronization therapy in a routine clinical practice setting will likely not benefit from the addition of a defibrillator to a pacemaker, according to results of the CERTITUDE cohort study.
In CERTITUDE, most of the deaths in patients fitted with a cardiac resynchronization therapy–pacemaker (CRT-P) device were predominantly from causes other than sudden cardiac death (SCD), which is the main rationale for using a CRT-defibrillator (CRT-D) device, said lead investigator Jean-Yves Le Heuzey at the annual congress of the European Society of Cardiology.
“Our results should not be interpreted as a general lack of benefit from CRT-D vs. CRT-P or vice versa. Rather we demonstrate that given currently selected CRT-P patients in the French population, addition of a defibrillator may not significantly add to survival.” Therefore, patients who may be eligible for CRT should not “automatically” be considered as requiring a CRT-D, suggested Dr. Le Heuzey and his coinvestigators in an article that was published online at the time of the study’s presentation (Eur Heart J. 2015 Sep 1. doi: 10.1093/eurheartj/ehv455).
Current ESC guidelines on cardiac pacing and cardiac resynchronization therapy “leave flexibility for the physician” on the use of CRT-P and CRT-D” because there was no evidence of a superior effect of the latter over CRT alone, said Dr. Le Heuzey of René Descartes University in Paris at the meeting. A randomized, controlled trial would be the only way to determine this, but such a trial is unlikely to ever be conducted, he noted.
Despite the lack of evidence, however, CRT-D is widely used, more so in the United States than in Europe, Dr. Le Heuzey observed, where more than 90% of patients needing CRT would likely have a CRT-D rather than a CRT-P device implanted.
The aims of the CERTITUDE cohort study were to look at the extent to which CRT-P patients differ from CRT-D patients in a real-life setting, and to also see if there were patients in the CRT-P group that might have benefited from CRT-D.
The prospective, observational study involved 1,705 patients who were recruited at 41 centers throughout France over a 2-year period starting in January 2008. Of these, 31% were fitted with a CRT-P device and 69% with a CRT-D.
Results showed that patients who had a CRT-P versus a CRT-D implanted were significantly older, more often female, and more symptomatic. They were also significantly less likely to have coronary artery disease, more likely to have wider QRS intervals and to have atrial fibrillation, and more often had at least two comorbidities.
Analysis of the causes of death was performed at 2 years’ follow-up, which Dr. Le Heuzey conceded was a short period of time. At this point, 267 of 1,611 patients with complete follow-up data had died, giving an overall mortality rate of 8.4% per 100 patient-years for the entire cohort.
The crude mortality rate was found to be higher among CRT-P than CRT-D patients, at 13.1% versus 6.5% per 100 patient-years (relative risk, 2.01; 95% confidence interval, 1.56-2.58; P less than .0001). But when the cause of death was examined more closely, there was no significant difference in the number of SCDs between the groups (RR, 1.57; 95% CI, 0.71-3.46; P = .42) and no significant difference when a specific cause of death analysis was performed.
The main reasons for the almost doubled risk of death in the CRT-P group was an increase in non-SCD cardiovascular mortality, mainly progressive heart failure (RR, 0.27; 95% CI, 1.62-3.18) and other cardiovascular causes (RR, 4.4; 95% CI, 1.29-15.03), Dr. Le Heuzey and associates noted in the article.
“Overall, 95% of the excess mortality among CRT-P recipients was not related to SCD,” they wrote, noting that this “suggests that the presence of a back-up defibrillator would probably not have been beneficial in terms of improving survival for these patients.”
So where does this leave clinicians? Dr. Le Heuzey referred to Table 17 in the European guidelines (Eur Heart J. 2013;34:2281-2329) with guidance on factors favoring CRT-P or CRT-D. For instance, CRT-P might be favorable in a patient with advanced heart failure or one with severe renal insufficiency or on dialysis. Other major comorbidities or frailty or cachexia might veer a decision towards CRT without a defibrillator. On the other hand, factors favoring CRT-D include a life expectancy of more than 1 year; stable, moderate (New York Heart Association class II) disease; or low to moderate–risk ischemic heart disease, with a lack of comorbidities.
CERTITUDE was funded by grants from the French Institute of Health and Medical Research (INSERM) and from the French Cardiology Society. The latter received specific grants from Biotronik, Boston Scientific, Medtronic, Saint Jude Medical, and Sorin in order to perform the study. Dr. Le Heuzey disclosed receiving fees for participation in advisory boards and conferences from AstraZeneca, Bayer, Boehringer-Ingelheim, Bristol Myers Squibb/Pfizer, Correvio, Daiichi-Sankyo, Meda, Sanofi, and Servier.
AT THE ESC CONGRESS 2015
Key clinical point:There appears to be no survival benefit of cardiac resynchronization therapy with a defibrillator CRT-D over a pacemaker (CRT-P).
Major finding: Although there was a higher death rate among CRT-P recipients, 95% of the excess mortality, compared with CRT-D recipients, was not related to sudden cardiac death.
Data source: The prospective, observational CERTITUDE cohort study in 1,705 French patients fitted with a CRT-P or CRT-D.
Disclosures: CERTITUDE was funded by grants from the French Institute of Health and Medical Research (INSERM) and from the French Cardiology Society. The latter received specific grants from Biotronik, Boston Scientific, Medtronic, St. Jude Medical, and Sorin in order to perform the study. Dr. Le Heuzey disclosed receiving fees for participation in advisory boards and conferences from AstraZeneca, Bayer, Boehringer-Ingelheim, Bristol Myers Squibb/Pfizer, Correvio, Daiichi-Sankyo, Meda, Sanofi, and Servier.
Right-side mini-AVR an option for frail patients
Many patients with aortic valve disease still undergo conventional aortic valve replacement (AVR) with standard full sternotomy or seek out alternative treatments like transcatheter aortic valve insertion (TAVI). But a minimally invasive approach that uses a sutureless prostheses may reduce operation times and put AVR within reach of more frail patients.
Investigators from G. Pasquinucci Heart Hospital in Massa, Italy, reported on 593 patients who had AVR through right anterior minithoracotomy (RAMT) over 10 years at their institution (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.06.045). In 302 of the patients, the researchers used a sutureless or rapidly implantable biological prosthesis.
“More surgeons should enrich their armamentarium by RAMT AVR,” lead author Dr. Mattia Glauber and his coauthors said. “Sutureless prostheses can increase adoption of RAMT AVR.”
The authors acknowledged that minimally invasive approaches to AVR, including partial sternotomy, require longer operation times than open surgery despite reduced aortic cross-clamping and cardiopulmonary bypass times, but have resulted in better outcomes and lower death rates.
A new generation of aortic valve prostheses, including sutureless devices, have emerged in an attempt to further reduce operative times and improve outcomes, so the Italian investigators designed their study to compare early and midterm outcomes after minimally invasive AVR using sutured and sutureless repair at their institution between 2004 and 2014.
In 302 (50.9%) patients, sutureless or rapidly implantable biological prosthesis was used, 23 (3.9%) had a mechanical prosthesis, and the remainder received a conventional biological prosthesis.
The investigators determined patients were suitable for RAMT if CT scan showed specific anatomic features, including rightward positioning of the ascending aorta at the level of the main pulmonary artery. Once the sutureless prostheses became available in 2011, every patient undergoing AVR via RAMT was considered a potential candidate, although the investigators decided that patients with type 1 and 2 bicuspid aortic valves without raphe and asymmetric aortic root were not suitable for the sutureless approach.
The subgroup that underwent sutureless repair tended to be older and sicker than the overall study population and had a higher prevalence of tricuspid aortic valve and aortic stenosis, a slightly higher body mass index, and a higher propensity to be obese. The sutureless subgroup also had fewer smokers.
Cardiopulmonary bypass time averaged 88 minutes and aortic cross-clamping times 55 minutes in the sutureless subgroup vs. 107 and 74 minutes, respectively, in the overall RAMT study subgroup.
The death before discharge rate of patients who had RAMT repair was 1%, and the 30-day in-hospital death rate was 1.5%. Overall, 97% of patients who had RAMT did not require reoperation at 5 years.
Between the sutured and sutureless subgroups, hospital and intensive care unit lengths of stay were similar, as were bleeding rates and in-hospital mortality. One measure in which the two subgroups deviated was prolonged ICU stay – a rate of 11.3% in the sutureless subgroup and 6.6% in the sutured subgroup.
“To the best of our knowledge, this is the largest up-to-date single-center experience on minimally invasive AVR through RAMT,” Dr. Glauber and coauthors said. “Our data along with earlier reports confirm that minimally invasive AVR through RAMT is safe and reproducible. It is associated with low perioperative mortality and morbidity.”
Dr. Glauber and coauthor Dr. Marco Solinas disclosed a commercial/financial relationship with Sorin Group.
“Have we found the end of the road, and the future for isolated AVR is made up of RAMT with sutureless AVR?” asks Dr. Patrick M. McCarthy, chief of cardiac surgery at Northwestern University Feinberg School of Medicine in Chicago, in his invited commentary (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.07.007). “The cardiology literature serves as a reality check.”
He noted that results from the NOTION Trial of transaortic valve replacement (TAVR) vs. surgical AVR (J Am Coll Cardiol. 2015;65:2184-94) had 30-day results similar to the G. Pasquinucci Heart Hospital results. However, 34% in the TAVR group in NOTION needed pacemakers, and 16% had moderate or greater valvular regurgitation and higher rates of dyspnea.

|
Dr. Patrick M. McCarthy |
Right anterior minithoracotomy is different from other minimally invasive approaches, Dr. McCarthy said. “It’s more of a tunnel down to the aortic valve which is why patient selection based on anatomic factors determined by preoperative CT scan (which is an unnecessary expense for hemisternotomy) is so important,” he said.
The evolution of TAVR is still in the early stage, so the “flaws” involved in the approach can yet be eliminated, “but the message that TAVR outcomes today are still very different than [surgical] AVR in low-risk patients, the type that have a minimally invasive AVR, may be lost on many readers,” Dr. McCarthy said.
For isolated aortic stenosis, the era of minimally invasive procedures that involve bypass, cross-clamping and a difficult surgical approach may be fading, he said. “The handwriting is on the wall, or in the journals in this case.”
Dr. McCarthy disclosed relationships with Edwards Lifesciences and Abbott Vascular. He is the inventor of the Edwards MC3 Ring and dETlogix Ring and coinventor of the IMR ETlogix Ring.
“Have we found the end of the road, and the future for isolated AVR is made up of RAMT with sutureless AVR?” asks Dr. Patrick M. McCarthy, chief of cardiac surgery at Northwestern University Feinberg School of Medicine in Chicago, in his invited commentary (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.07.007). “The cardiology literature serves as a reality check.”
He noted that results from the NOTION Trial of transaortic valve replacement (TAVR) vs. surgical AVR (J Am Coll Cardiol. 2015;65:2184-94) had 30-day results similar to the G. Pasquinucci Heart Hospital results. However, 34% in the TAVR group in NOTION needed pacemakers, and 16% had moderate or greater valvular regurgitation and higher rates of dyspnea.

|
Dr. Patrick M. McCarthy |
Right anterior minithoracotomy is different from other minimally invasive approaches, Dr. McCarthy said. “It’s more of a tunnel down to the aortic valve which is why patient selection based on anatomic factors determined by preoperative CT scan (which is an unnecessary expense for hemisternotomy) is so important,” he said.
The evolution of TAVR is still in the early stage, so the “flaws” involved in the approach can yet be eliminated, “but the message that TAVR outcomes today are still very different than [surgical] AVR in low-risk patients, the type that have a minimally invasive AVR, may be lost on many readers,” Dr. McCarthy said.
For isolated aortic stenosis, the era of minimally invasive procedures that involve bypass, cross-clamping and a difficult surgical approach may be fading, he said. “The handwriting is on the wall, or in the journals in this case.”
Dr. McCarthy disclosed relationships with Edwards Lifesciences and Abbott Vascular. He is the inventor of the Edwards MC3 Ring and dETlogix Ring and coinventor of the IMR ETlogix Ring.
“Have we found the end of the road, and the future for isolated AVR is made up of RAMT with sutureless AVR?” asks Dr. Patrick M. McCarthy, chief of cardiac surgery at Northwestern University Feinberg School of Medicine in Chicago, in his invited commentary (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.07.007). “The cardiology literature serves as a reality check.”
He noted that results from the NOTION Trial of transaortic valve replacement (TAVR) vs. surgical AVR (J Am Coll Cardiol. 2015;65:2184-94) had 30-day results similar to the G. Pasquinucci Heart Hospital results. However, 34% in the TAVR group in NOTION needed pacemakers, and 16% had moderate or greater valvular regurgitation and higher rates of dyspnea.

|
Dr. Patrick M. McCarthy |
Right anterior minithoracotomy is different from other minimally invasive approaches, Dr. McCarthy said. “It’s more of a tunnel down to the aortic valve which is why patient selection based on anatomic factors determined by preoperative CT scan (which is an unnecessary expense for hemisternotomy) is so important,” he said.
The evolution of TAVR is still in the early stage, so the “flaws” involved in the approach can yet be eliminated, “but the message that TAVR outcomes today are still very different than [surgical] AVR in low-risk patients, the type that have a minimally invasive AVR, may be lost on many readers,” Dr. McCarthy said.
For isolated aortic stenosis, the era of minimally invasive procedures that involve bypass, cross-clamping and a difficult surgical approach may be fading, he said. “The handwriting is on the wall, or in the journals in this case.”
Dr. McCarthy disclosed relationships with Edwards Lifesciences and Abbott Vascular. He is the inventor of the Edwards MC3 Ring and dETlogix Ring and coinventor of the IMR ETlogix Ring.
Many patients with aortic valve disease still undergo conventional aortic valve replacement (AVR) with standard full sternotomy or seek out alternative treatments like transcatheter aortic valve insertion (TAVI). But a minimally invasive approach that uses a sutureless prostheses may reduce operation times and put AVR within reach of more frail patients.
Investigators from G. Pasquinucci Heart Hospital in Massa, Italy, reported on 593 patients who had AVR through right anterior minithoracotomy (RAMT) over 10 years at their institution (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.06.045). In 302 of the patients, the researchers used a sutureless or rapidly implantable biological prosthesis.
“More surgeons should enrich their armamentarium by RAMT AVR,” lead author Dr. Mattia Glauber and his coauthors said. “Sutureless prostheses can increase adoption of RAMT AVR.”
The authors acknowledged that minimally invasive approaches to AVR, including partial sternotomy, require longer operation times than open surgery despite reduced aortic cross-clamping and cardiopulmonary bypass times, but have resulted in better outcomes and lower death rates.
A new generation of aortic valve prostheses, including sutureless devices, have emerged in an attempt to further reduce operative times and improve outcomes, so the Italian investigators designed their study to compare early and midterm outcomes after minimally invasive AVR using sutured and sutureless repair at their institution between 2004 and 2014.
In 302 (50.9%) patients, sutureless or rapidly implantable biological prosthesis was used, 23 (3.9%) had a mechanical prosthesis, and the remainder received a conventional biological prosthesis.
The investigators determined patients were suitable for RAMT if CT scan showed specific anatomic features, including rightward positioning of the ascending aorta at the level of the main pulmonary artery. Once the sutureless prostheses became available in 2011, every patient undergoing AVR via RAMT was considered a potential candidate, although the investigators decided that patients with type 1 and 2 bicuspid aortic valves without raphe and asymmetric aortic root were not suitable for the sutureless approach.
The subgroup that underwent sutureless repair tended to be older and sicker than the overall study population and had a higher prevalence of tricuspid aortic valve and aortic stenosis, a slightly higher body mass index, and a higher propensity to be obese. The sutureless subgroup also had fewer smokers.
Cardiopulmonary bypass time averaged 88 minutes and aortic cross-clamping times 55 minutes in the sutureless subgroup vs. 107 and 74 minutes, respectively, in the overall RAMT study subgroup.
The death before discharge rate of patients who had RAMT repair was 1%, and the 30-day in-hospital death rate was 1.5%. Overall, 97% of patients who had RAMT did not require reoperation at 5 years.
Between the sutured and sutureless subgroups, hospital and intensive care unit lengths of stay were similar, as were bleeding rates and in-hospital mortality. One measure in which the two subgroups deviated was prolonged ICU stay – a rate of 11.3% in the sutureless subgroup and 6.6% in the sutured subgroup.
“To the best of our knowledge, this is the largest up-to-date single-center experience on minimally invasive AVR through RAMT,” Dr. Glauber and coauthors said. “Our data along with earlier reports confirm that minimally invasive AVR through RAMT is safe and reproducible. It is associated with low perioperative mortality and morbidity.”
Dr. Glauber and coauthor Dr. Marco Solinas disclosed a commercial/financial relationship with Sorin Group.
Many patients with aortic valve disease still undergo conventional aortic valve replacement (AVR) with standard full sternotomy or seek out alternative treatments like transcatheter aortic valve insertion (TAVI). But a minimally invasive approach that uses a sutureless prostheses may reduce operation times and put AVR within reach of more frail patients.
Investigators from G. Pasquinucci Heart Hospital in Massa, Italy, reported on 593 patients who had AVR through right anterior minithoracotomy (RAMT) over 10 years at their institution (J Thorac Cardiovasc Surg. 2015. doi: 10.1016/j.jtcvs.2015.06.045). In 302 of the patients, the researchers used a sutureless or rapidly implantable biological prosthesis.
“More surgeons should enrich their armamentarium by RAMT AVR,” lead author Dr. Mattia Glauber and his coauthors said. “Sutureless prostheses can increase adoption of RAMT AVR.”
The authors acknowledged that minimally invasive approaches to AVR, including partial sternotomy, require longer operation times than open surgery despite reduced aortic cross-clamping and cardiopulmonary bypass times, but have resulted in better outcomes and lower death rates.
A new generation of aortic valve prostheses, including sutureless devices, have emerged in an attempt to further reduce operative times and improve outcomes, so the Italian investigators designed their study to compare early and midterm outcomes after minimally invasive AVR using sutured and sutureless repair at their institution between 2004 and 2014.
In 302 (50.9%) patients, sutureless or rapidly implantable biological prosthesis was used, 23 (3.9%) had a mechanical prosthesis, and the remainder received a conventional biological prosthesis.
The investigators determined patients were suitable for RAMT if CT scan showed specific anatomic features, including rightward positioning of the ascending aorta at the level of the main pulmonary artery. Once the sutureless prostheses became available in 2011, every patient undergoing AVR via RAMT was considered a potential candidate, although the investigators decided that patients with type 1 and 2 bicuspid aortic valves without raphe and asymmetric aortic root were not suitable for the sutureless approach.
The subgroup that underwent sutureless repair tended to be older and sicker than the overall study population and had a higher prevalence of tricuspid aortic valve and aortic stenosis, a slightly higher body mass index, and a higher propensity to be obese. The sutureless subgroup also had fewer smokers.
Cardiopulmonary bypass time averaged 88 minutes and aortic cross-clamping times 55 minutes in the sutureless subgroup vs. 107 and 74 minutes, respectively, in the overall RAMT study subgroup.
The death before discharge rate of patients who had RAMT repair was 1%, and the 30-day in-hospital death rate was 1.5%. Overall, 97% of patients who had RAMT did not require reoperation at 5 years.
Between the sutured and sutureless subgroups, hospital and intensive care unit lengths of stay were similar, as were bleeding rates and in-hospital mortality. One measure in which the two subgroups deviated was prolonged ICU stay – a rate of 11.3% in the sutureless subgroup and 6.6% in the sutured subgroup.
“To the best of our knowledge, this is the largest up-to-date single-center experience on minimally invasive AVR through RAMT,” Dr. Glauber and coauthors said. “Our data along with earlier reports confirm that minimally invasive AVR through RAMT is safe and reproducible. It is associated with low perioperative mortality and morbidity.”
Dr. Glauber and coauthor Dr. Marco Solinas disclosed a commercial/financial relationship with Sorin Group.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Aortic valve replacement through right anterior minithoracotomy provides excellent outcomes. Sutureless prostheses facilitate mini-AVR.
Major finding: Study subjects had a survival rate of 95% at 31.5 months follow-up on average, and operative times were significantly shorter with sutureless prostheses, compared with sutured prostheses.
Data source: A retrospective, observational cohort study with prospective data collection on 593 patients who had right anterior minithoracotomy for AVR at a single institution over a 10-yar period.
Disclosures: Study coauthors Mattia Glauber and Marco Solinas disclosed a commercial/financial relationship with Sorin Group.
SYNTAX: Early CABG results with arterial grafts similar to venous in matched groups
While single-center studies have supported the advantages of multiple arterial grafts over venous grafts in coronary artery bypass surgery, an analysis of patients in the international and multicenter SYNTAX trial has shown that, on propensity matching, rates of cardiac events and death are actually similar between the two groups.
These findings of the SYNTAX investigators, led by Dr. Catalina Parasca of Erasmus University in Rotterdam, the Netherlands, were published online in the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j.jtcvs.2015.05.010).
The SYNTAX trial compared percutaneous coronary intervention (PCI) with coronary artery bypass grafting (CABG) in patients with left main or three-vessel coronary artery disease (Lancet. 2013;381[9867]:629-38).
In the latest report, the SYNTAX investigators found that patients in unmatched groups who received arterial grafts in addition to an arterial graft of the left anterior descending artery (LAD) had noticeably lower rates of death and a composite endpoint of death-stroke-MI than did those who received a second venous graft. However, when the researchers applied propensity matching, the outcomes between the two groups were similar.
Because large randomized trials have yet to prove the superiority of multiarterial grafts, the adoption rate has been low, Dr. Parasca and colleagues said. “The objective of this study was to assess the effect of using a second arterial graft on 5-year outcomes in patients who underwent CABG in the SYNTAX trial and registry,” they said.
They looked at 1,322 SYNTAX trial patients who had CABG with 5-year follow-up. In unmatched groups, the safety endpoint of the death-stroke-MI composite was 13.3% in the multiarterial group vs. 18.7% in the vein graft group. Although the incidence of stroke, MI, and graft occlusion was similar between the unmatched groups, the second-graft arterial group had a higher revascularization rate at 5 years, 12.6% vs. 9.6%, mainly due to repeat PCI. The element of the composite where the two unmatched groups deviated was the all-cause death rate at 5 years: 8.9% in the second-graft arterial group and 13.1% in the venous group.
However, when the investigators applied propensity matching, the differences between the two groups were insignificant.
“The results of the present study must be seen in the light of a multicenter CABG cohort with complex coronary disease, where revascularization was performed according to surgeon’s personal experience and local practices,” Dr. Parasca and coauthors noted. “The result was a high heterogeneity of CABG techniques, which shows different understanding of the best ‘graft-target match’ across centers.”
While the SYNTAX analysis demonstrates the variation in patient selection and operator technique with regard to arterial revascularization typical of a multicenter study, “extended follow-up beyond 5 years is required to estimate its impact on long-term outcomes,” Dr. Parasca and colleagues said.
Boston Scientific supported the trial. Coauthor Keith Dawkins is employed by Boston Scientific and coauthor Ted Feldman has received consulting fees from the company. The other authors reported no disclosures.
That arterial grafts are a better long-term match in coronary bypass surgery has been a tenet in cardiac surgery, but multiple factors have prevented their more widespread acceptance, Dr. Davis C. Drinkwater Jr. said in his invited commentary (J Thorac Cardiovasc Surg. 2015.doi:10.1016/j.jtcvs.2015.06.014). Concerns about sternal wound healing, particularly in diabetic or obese patients, as well as the alternative generally good early and mid-term results in multivessel coronary artery disease using the left internal thoracic artery to LAD accompanied by saphenous vein grafts, have made surgeons hesitant to take up the approach more readily, said Dr. Drinkwater of Frist Cardiology, Tristar Centennial Medical Center, Nashville, Tenn.
The SYNTAX investigators’ main finding of no survival advantage among the matched groups at 5 years is in line with most reports comparing patency between arterial and venous grafts, “requiring between 5- and 10-year follow-up to show a divergence,” Dr. Drinkwater said.
He pointed out that the patients who had second arterial grafts in the unmatched group were younger and healthier – the average age was 62 years, and 27% of them had previous heart attacks, compared with 66 years of age and a heart attack rate of 35.6% in the venous graft group – and that may explain the higher reintervention rate in the former group. Another factor may be the younger and healthier patients had longer cardiopulmonary bypass and aortic cross clamp times despite a greater percentage having undergone the off-pump technique.
“This counterintuitive information underscores an inherent weakness of this multicenter trial that is without surgical randomization into the two arterial groups, and with potentially varied surgical experience using nonstandardized technical and management protocols,” Dr. Drinkwater said. “This is in stark contrast to the previous and well accepted single high-volume-center reports of the benefits of using multiple arterial bypass grafts.”
Because the report points out the technical challenges of achieving complete revascularization with multiple arterial grafting at “the early” interval of up to 5 years, the authors may be inappropriately discouraging centers that do not currently offer multiarterial grafting from embracing it, Dr. Drinkwater concluded.
He had no disclosures to report.
That arterial grafts are a better long-term match in coronary bypass surgery has been a tenet in cardiac surgery, but multiple factors have prevented their more widespread acceptance, Dr. Davis C. Drinkwater Jr. said in his invited commentary (J Thorac Cardiovasc Surg. 2015.doi:10.1016/j.jtcvs.2015.06.014). Concerns about sternal wound healing, particularly in diabetic or obese patients, as well as the alternative generally good early and mid-term results in multivessel coronary artery disease using the left internal thoracic artery to LAD accompanied by saphenous vein grafts, have made surgeons hesitant to take up the approach more readily, said Dr. Drinkwater of Frist Cardiology, Tristar Centennial Medical Center, Nashville, Tenn.
The SYNTAX investigators’ main finding of no survival advantage among the matched groups at 5 years is in line with most reports comparing patency between arterial and venous grafts, “requiring between 5- and 10-year follow-up to show a divergence,” Dr. Drinkwater said.
He pointed out that the patients who had second arterial grafts in the unmatched group were younger and healthier – the average age was 62 years, and 27% of them had previous heart attacks, compared with 66 years of age and a heart attack rate of 35.6% in the venous graft group – and that may explain the higher reintervention rate in the former group. Another factor may be the younger and healthier patients had longer cardiopulmonary bypass and aortic cross clamp times despite a greater percentage having undergone the off-pump technique.
“This counterintuitive information underscores an inherent weakness of this multicenter trial that is without surgical randomization into the two arterial groups, and with potentially varied surgical experience using nonstandardized technical and management protocols,” Dr. Drinkwater said. “This is in stark contrast to the previous and well accepted single high-volume-center reports of the benefits of using multiple arterial bypass grafts.”
Because the report points out the technical challenges of achieving complete revascularization with multiple arterial grafting at “the early” interval of up to 5 years, the authors may be inappropriately discouraging centers that do not currently offer multiarterial grafting from embracing it, Dr. Drinkwater concluded.
He had no disclosures to report.
That arterial grafts are a better long-term match in coronary bypass surgery has been a tenet in cardiac surgery, but multiple factors have prevented their more widespread acceptance, Dr. Davis C. Drinkwater Jr. said in his invited commentary (J Thorac Cardiovasc Surg. 2015.doi:10.1016/j.jtcvs.2015.06.014). Concerns about sternal wound healing, particularly in diabetic or obese patients, as well as the alternative generally good early and mid-term results in multivessel coronary artery disease using the left internal thoracic artery to LAD accompanied by saphenous vein grafts, have made surgeons hesitant to take up the approach more readily, said Dr. Drinkwater of Frist Cardiology, Tristar Centennial Medical Center, Nashville, Tenn.
The SYNTAX investigators’ main finding of no survival advantage among the matched groups at 5 years is in line with most reports comparing patency between arterial and venous grafts, “requiring between 5- and 10-year follow-up to show a divergence,” Dr. Drinkwater said.
He pointed out that the patients who had second arterial grafts in the unmatched group were younger and healthier – the average age was 62 years, and 27% of them had previous heart attacks, compared with 66 years of age and a heart attack rate of 35.6% in the venous graft group – and that may explain the higher reintervention rate in the former group. Another factor may be the younger and healthier patients had longer cardiopulmonary bypass and aortic cross clamp times despite a greater percentage having undergone the off-pump technique.
“This counterintuitive information underscores an inherent weakness of this multicenter trial that is without surgical randomization into the two arterial groups, and with potentially varied surgical experience using nonstandardized technical and management protocols,” Dr. Drinkwater said. “This is in stark contrast to the previous and well accepted single high-volume-center reports of the benefits of using multiple arterial bypass grafts.”
Because the report points out the technical challenges of achieving complete revascularization with multiple arterial grafting at “the early” interval of up to 5 years, the authors may be inappropriately discouraging centers that do not currently offer multiarterial grafting from embracing it, Dr. Drinkwater concluded.
He had no disclosures to report.
While single-center studies have supported the advantages of multiple arterial grafts over venous grafts in coronary artery bypass surgery, an analysis of patients in the international and multicenter SYNTAX trial has shown that, on propensity matching, rates of cardiac events and death are actually similar between the two groups.
These findings of the SYNTAX investigators, led by Dr. Catalina Parasca of Erasmus University in Rotterdam, the Netherlands, were published online in the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j.jtcvs.2015.05.010).
The SYNTAX trial compared percutaneous coronary intervention (PCI) with coronary artery bypass grafting (CABG) in patients with left main or three-vessel coronary artery disease (Lancet. 2013;381[9867]:629-38).
In the latest report, the SYNTAX investigators found that patients in unmatched groups who received arterial grafts in addition to an arterial graft of the left anterior descending artery (LAD) had noticeably lower rates of death and a composite endpoint of death-stroke-MI than did those who received a second venous graft. However, when the researchers applied propensity matching, the outcomes between the two groups were similar.
Because large randomized trials have yet to prove the superiority of multiarterial grafts, the adoption rate has been low, Dr. Parasca and colleagues said. “The objective of this study was to assess the effect of using a second arterial graft on 5-year outcomes in patients who underwent CABG in the SYNTAX trial and registry,” they said.
They looked at 1,322 SYNTAX trial patients who had CABG with 5-year follow-up. In unmatched groups, the safety endpoint of the death-stroke-MI composite was 13.3% in the multiarterial group vs. 18.7% in the vein graft group. Although the incidence of stroke, MI, and graft occlusion was similar between the unmatched groups, the second-graft arterial group had a higher revascularization rate at 5 years, 12.6% vs. 9.6%, mainly due to repeat PCI. The element of the composite where the two unmatched groups deviated was the all-cause death rate at 5 years: 8.9% in the second-graft arterial group and 13.1% in the venous group.
However, when the investigators applied propensity matching, the differences between the two groups were insignificant.
“The results of the present study must be seen in the light of a multicenter CABG cohort with complex coronary disease, where revascularization was performed according to surgeon’s personal experience and local practices,” Dr. Parasca and coauthors noted. “The result was a high heterogeneity of CABG techniques, which shows different understanding of the best ‘graft-target match’ across centers.”
While the SYNTAX analysis demonstrates the variation in patient selection and operator technique with regard to arterial revascularization typical of a multicenter study, “extended follow-up beyond 5 years is required to estimate its impact on long-term outcomes,” Dr. Parasca and colleagues said.
Boston Scientific supported the trial. Coauthor Keith Dawkins is employed by Boston Scientific and coauthor Ted Feldman has received consulting fees from the company. The other authors reported no disclosures.
While single-center studies have supported the advantages of multiple arterial grafts over venous grafts in coronary artery bypass surgery, an analysis of patients in the international and multicenter SYNTAX trial has shown that, on propensity matching, rates of cardiac events and death are actually similar between the two groups.
These findings of the SYNTAX investigators, led by Dr. Catalina Parasca of Erasmus University in Rotterdam, the Netherlands, were published online in the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j.jtcvs.2015.05.010).
The SYNTAX trial compared percutaneous coronary intervention (PCI) with coronary artery bypass grafting (CABG) in patients with left main or three-vessel coronary artery disease (Lancet. 2013;381[9867]:629-38).
In the latest report, the SYNTAX investigators found that patients in unmatched groups who received arterial grafts in addition to an arterial graft of the left anterior descending artery (LAD) had noticeably lower rates of death and a composite endpoint of death-stroke-MI than did those who received a second venous graft. However, when the researchers applied propensity matching, the outcomes between the two groups were similar.
Because large randomized trials have yet to prove the superiority of multiarterial grafts, the adoption rate has been low, Dr. Parasca and colleagues said. “The objective of this study was to assess the effect of using a second arterial graft on 5-year outcomes in patients who underwent CABG in the SYNTAX trial and registry,” they said.
They looked at 1,322 SYNTAX trial patients who had CABG with 5-year follow-up. In unmatched groups, the safety endpoint of the death-stroke-MI composite was 13.3% in the multiarterial group vs. 18.7% in the vein graft group. Although the incidence of stroke, MI, and graft occlusion was similar between the unmatched groups, the second-graft arterial group had a higher revascularization rate at 5 years, 12.6% vs. 9.6%, mainly due to repeat PCI. The element of the composite where the two unmatched groups deviated was the all-cause death rate at 5 years: 8.9% in the second-graft arterial group and 13.1% in the venous group.
However, when the investigators applied propensity matching, the differences between the two groups were insignificant.
“The results of the present study must be seen in the light of a multicenter CABG cohort with complex coronary disease, where revascularization was performed according to surgeon’s personal experience and local practices,” Dr. Parasca and coauthors noted. “The result was a high heterogeneity of CABG techniques, which shows different understanding of the best ‘graft-target match’ across centers.”
While the SYNTAX analysis demonstrates the variation in patient selection and operator technique with regard to arterial revascularization typical of a multicenter study, “extended follow-up beyond 5 years is required to estimate its impact on long-term outcomes,” Dr. Parasca and colleagues said.
Boston Scientific supported the trial. Coauthor Keith Dawkins is employed by Boston Scientific and coauthor Ted Feldman has received consulting fees from the company. The other authors reported no disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Surgeons should choose arterial grafts for multigraft coronary artery bypass surgery when feasible.
Major finding: Patients who received multiple arterial graft had significantly lower rates of death and other problems than did those who received venous grafts in unmatched groups, but results were similar between propensity matched groups.
Data source: Registry of 1,322 patients who had 5-year follow-up after coronary artery bypass surgery within the SYNTAX trial.
Disclosures: Boston Scientific supported the trial. Coauthor Keith Dawkins is employed by Boston Scientific and coauthor Ted Feldman has received consulting fees from the company. The other authors reported no disclosures.