User login
CDC updates Zika guidance for managing pregnant women
Updated guidelines released by the Centers for Disease Control and Prevention outline how to diagnose suspected cases of Zika virus infection among pregnant women based on how quickly they present with symptoms.
The guidance was updated in light of “the emerging data indicating that Zika virus RNA can be detected for prolonged periods in some pregnant women,” the CDC wrote in the July 25 issue of the Morbidity and Mortality Weekly Report (doi: 10.15585/mmwr.mm6529e1).
All pregnant women should be assessed for Zika virus at each of their prenatal care visits, regardless of their recent travel history or exposure to mosquitoes, by being evaluated for signs and symptoms of infection, such as fever, rash, and arthralgia. From there, management can take one of two directions.
The first direction involves women who are tested within 2 weeks of either symptom onset, or their suspected exposure to the virus. Pregnant women who are asymptomatic and do not live in an area with an ongoing Zika virus outbreak, as well as women who are symptomatic, should have their serum and urine analyzed using a real-time reverse transcription–polymerase chain reaction (rRT-PCR) test. If the result of this test is positive, it should be considered as confirmation that the woman has a “recent Zika virus infection.”
However, if the test results are negative, symptomatic women should undergo immunoglobin M testing for both Zika virus and dengue virus, while asymptomatic women should undergo just Zika virus IgM testing within 2-12 weeks of the possible exposure. In either case, if the tests come back negative, then the patient can be definitively cleared of any recent Zika virus infection. However, if either the Zika virus or dengue virus tests are positive or equivocal, then there is a “presumptive recent Zika virus or dengue virus or Flavivirus infection” in the woman, at which point plaque reduction neutralization testing (PRNT) must be conducted.
The second direction for management involves pregnant women who are initially tested within 2-12 weeks of either symptom onset or suspected exposure to the virus. Asymptomatic women who do not live in an area with active Zika virus transmission, or do live in an area with ongoing Zika virus cases but are already in the first or second trimester of their pregnancy – along with any women who are symptomatic – should have their serum analyzed through IgM testing for both Zika virus and dengue virus.
If both results are negative, then there is no Zika virus infection. If the Zika virus test is negative but the dengue virus test is either positive or equivocal, the woman has a “presumptive dengue virus infection” and should undergo PRNT. If the Zika virus test is either positive or equivocal, then the woman has a “presumptive recent Zika virus or Flavivirus infection,” regardless of the dengue virus IgM result. In the latter case, the next step is to conduct a reflex Zika virus rRT-PCR test on both serum and urine. A negative result on the serum test should be followed by PRNT; a positive result should be taken as proof of a “recent Zika virus infection.”
For any diagnostic chain that ends with a PRNT, the results of that test can be interpreted in one of three ways. If the Zika virus PRNT result is at least 10 and the dengue virus result is less than 10, then there is a recent Zika virus infection. If both the Zika virus and dengue virus PRNT results are 10 or greater, than there is a Flavivirus infection, but the specific one cannot be determined. Finally, if both results are less than 10, then there is no evidence of a recent Zika virus infection.
“For symptomatic and asymptomatic pregnant women with possible Zika virus exposure who seek care [more than] 12 weeks after symptom onset or possible exposure, IgM antibody testing might be considered,” the CDC wrote. “If fetal abnormalities are present, rRT-PCR testing should also be performed on maternal serum and urine [but] a negative IgM antibody test or rRT-PCR result [more than] 12 weeks after symptom onset or possible exposure does not rule out recent Zika virus infection.”
For pregnant women with a diagnosis of a confirmed or presumptive Flavivirus infection, regardless of whether it’s specifically Zika virus or not, the CDC recommends getting serial ultrasounds every 3-4 weeks during pregnancy in order to monitor the fetus’s development, while “decisions regarding amniocentesis should be individualized for each clinical circumstance.” After the child’s birth, rRT-PCR should be conducted on the child’s cord blood and serum; Zika virus and dengue virus IgM are also recommended.
Pregnant women without a diagnosis of either Zika virus or dengue virus should have a prenatal ultrasound; if abnormalities are found in the fetus, CDC recommends that they have a repeat Zika virus rRT-PCR and IgM test and that clinicians base management on corresponding laboratory results. If nothing is found, however, then standard care can resume with ongoing vigilance to avoid Zika virus infections. Women with dengue virus diagnoses should follow the guidance that is currently in place.
“Pregnant women with laboratory evidence of confirmed or possible Zika virus infection who experience a fetal loss or stillbirth should be offered pathology testing for Zika virus infection,” the CDC added. “This testing might provide insight into the etiology of the fetal loss, which could inform a woman’s future pregnancy planning.”
The CDC also issued updated guidance for preventing sexual transmission of Zika virus and that applies to all men and women who have traveled to or reside in areas with active Zika virus transmission and their sex partners (MMWR. ePub: 2016 25 Jul. doi: 10.15585/mmwr.mm6529e2). The CDC advises couples in which a woman is pregnant to use barriers methods or abstain from sex for the duration of the pregnancy. For couples not planning pregnancy and in which there is a male partner with confirmed Zika virus infection or symptoms of infection, the men should use barrier methods or abstain from sex for at least 6 months after the onset of illness. For women with Zika virus infection, they should use barrier protection or abstain from sex for at least 8 weeks after the onset of illness.
Updated guidelines released by the Centers for Disease Control and Prevention outline how to diagnose suspected cases of Zika virus infection among pregnant women based on how quickly they present with symptoms.
The guidance was updated in light of “the emerging data indicating that Zika virus RNA can be detected for prolonged periods in some pregnant women,” the CDC wrote in the July 25 issue of the Morbidity and Mortality Weekly Report (doi: 10.15585/mmwr.mm6529e1).
All pregnant women should be assessed for Zika virus at each of their prenatal care visits, regardless of their recent travel history or exposure to mosquitoes, by being evaluated for signs and symptoms of infection, such as fever, rash, and arthralgia. From there, management can take one of two directions.
The first direction involves women who are tested within 2 weeks of either symptom onset, or their suspected exposure to the virus. Pregnant women who are asymptomatic and do not live in an area with an ongoing Zika virus outbreak, as well as women who are symptomatic, should have their serum and urine analyzed using a real-time reverse transcription–polymerase chain reaction (rRT-PCR) test. If the result of this test is positive, it should be considered as confirmation that the woman has a “recent Zika virus infection.”
However, if the test results are negative, symptomatic women should undergo immunoglobin M testing for both Zika virus and dengue virus, while asymptomatic women should undergo just Zika virus IgM testing within 2-12 weeks of the possible exposure. In either case, if the tests come back negative, then the patient can be definitively cleared of any recent Zika virus infection. However, if either the Zika virus or dengue virus tests are positive or equivocal, then there is a “presumptive recent Zika virus or dengue virus or Flavivirus infection” in the woman, at which point plaque reduction neutralization testing (PRNT) must be conducted.
The second direction for management involves pregnant women who are initially tested within 2-12 weeks of either symptom onset or suspected exposure to the virus. Asymptomatic women who do not live in an area with active Zika virus transmission, or do live in an area with ongoing Zika virus cases but are already in the first or second trimester of their pregnancy – along with any women who are symptomatic – should have their serum analyzed through IgM testing for both Zika virus and dengue virus.
If both results are negative, then there is no Zika virus infection. If the Zika virus test is negative but the dengue virus test is either positive or equivocal, the woman has a “presumptive dengue virus infection” and should undergo PRNT. If the Zika virus test is either positive or equivocal, then the woman has a “presumptive recent Zika virus or Flavivirus infection,” regardless of the dengue virus IgM result. In the latter case, the next step is to conduct a reflex Zika virus rRT-PCR test on both serum and urine. A negative result on the serum test should be followed by PRNT; a positive result should be taken as proof of a “recent Zika virus infection.”
For any diagnostic chain that ends with a PRNT, the results of that test can be interpreted in one of three ways. If the Zika virus PRNT result is at least 10 and the dengue virus result is less than 10, then there is a recent Zika virus infection. If both the Zika virus and dengue virus PRNT results are 10 or greater, than there is a Flavivirus infection, but the specific one cannot be determined. Finally, if both results are less than 10, then there is no evidence of a recent Zika virus infection.
“For symptomatic and asymptomatic pregnant women with possible Zika virus exposure who seek care [more than] 12 weeks after symptom onset or possible exposure, IgM antibody testing might be considered,” the CDC wrote. “If fetal abnormalities are present, rRT-PCR testing should also be performed on maternal serum and urine [but] a negative IgM antibody test or rRT-PCR result [more than] 12 weeks after symptom onset or possible exposure does not rule out recent Zika virus infection.”
For pregnant women with a diagnosis of a confirmed or presumptive Flavivirus infection, regardless of whether it’s specifically Zika virus or not, the CDC recommends getting serial ultrasounds every 3-4 weeks during pregnancy in order to monitor the fetus’s development, while “decisions regarding amniocentesis should be individualized for each clinical circumstance.” After the child’s birth, rRT-PCR should be conducted on the child’s cord blood and serum; Zika virus and dengue virus IgM are also recommended.
Pregnant women without a diagnosis of either Zika virus or dengue virus should have a prenatal ultrasound; if abnormalities are found in the fetus, CDC recommends that they have a repeat Zika virus rRT-PCR and IgM test and that clinicians base management on corresponding laboratory results. If nothing is found, however, then standard care can resume with ongoing vigilance to avoid Zika virus infections. Women with dengue virus diagnoses should follow the guidance that is currently in place.
“Pregnant women with laboratory evidence of confirmed or possible Zika virus infection who experience a fetal loss or stillbirth should be offered pathology testing for Zika virus infection,” the CDC added. “This testing might provide insight into the etiology of the fetal loss, which could inform a woman’s future pregnancy planning.”
The CDC also issued updated guidance for preventing sexual transmission of Zika virus and that applies to all men and women who have traveled to or reside in areas with active Zika virus transmission and their sex partners (MMWR. ePub: 2016 25 Jul. doi: 10.15585/mmwr.mm6529e2). The CDC advises couples in which a woman is pregnant to use barriers methods or abstain from sex for the duration of the pregnancy. For couples not planning pregnancy and in which there is a male partner with confirmed Zika virus infection or symptoms of infection, the men should use barrier methods or abstain from sex for at least 6 months after the onset of illness. For women with Zika virus infection, they should use barrier protection or abstain from sex for at least 8 weeks after the onset of illness.
Updated guidelines released by the Centers for Disease Control and Prevention outline how to diagnose suspected cases of Zika virus infection among pregnant women based on how quickly they present with symptoms.
The guidance was updated in light of “the emerging data indicating that Zika virus RNA can be detected for prolonged periods in some pregnant women,” the CDC wrote in the July 25 issue of the Morbidity and Mortality Weekly Report (doi: 10.15585/mmwr.mm6529e1).
All pregnant women should be assessed for Zika virus at each of their prenatal care visits, regardless of their recent travel history or exposure to mosquitoes, by being evaluated for signs and symptoms of infection, such as fever, rash, and arthralgia. From there, management can take one of two directions.
The first direction involves women who are tested within 2 weeks of either symptom onset, or their suspected exposure to the virus. Pregnant women who are asymptomatic and do not live in an area with an ongoing Zika virus outbreak, as well as women who are symptomatic, should have their serum and urine analyzed using a real-time reverse transcription–polymerase chain reaction (rRT-PCR) test. If the result of this test is positive, it should be considered as confirmation that the woman has a “recent Zika virus infection.”
However, if the test results are negative, symptomatic women should undergo immunoglobin M testing for both Zika virus and dengue virus, while asymptomatic women should undergo just Zika virus IgM testing within 2-12 weeks of the possible exposure. In either case, if the tests come back negative, then the patient can be definitively cleared of any recent Zika virus infection. However, if either the Zika virus or dengue virus tests are positive or equivocal, then there is a “presumptive recent Zika virus or dengue virus or Flavivirus infection” in the woman, at which point plaque reduction neutralization testing (PRNT) must be conducted.
The second direction for management involves pregnant women who are initially tested within 2-12 weeks of either symptom onset or suspected exposure to the virus. Asymptomatic women who do not live in an area with active Zika virus transmission, or do live in an area with ongoing Zika virus cases but are already in the first or second trimester of their pregnancy – along with any women who are symptomatic – should have their serum analyzed through IgM testing for both Zika virus and dengue virus.
If both results are negative, then there is no Zika virus infection. If the Zika virus test is negative but the dengue virus test is either positive or equivocal, the woman has a “presumptive dengue virus infection” and should undergo PRNT. If the Zika virus test is either positive or equivocal, then the woman has a “presumptive recent Zika virus or Flavivirus infection,” regardless of the dengue virus IgM result. In the latter case, the next step is to conduct a reflex Zika virus rRT-PCR test on both serum and urine. A negative result on the serum test should be followed by PRNT; a positive result should be taken as proof of a “recent Zika virus infection.”
For any diagnostic chain that ends with a PRNT, the results of that test can be interpreted in one of three ways. If the Zika virus PRNT result is at least 10 and the dengue virus result is less than 10, then there is a recent Zika virus infection. If both the Zika virus and dengue virus PRNT results are 10 or greater, than there is a Flavivirus infection, but the specific one cannot be determined. Finally, if both results are less than 10, then there is no evidence of a recent Zika virus infection.
“For symptomatic and asymptomatic pregnant women with possible Zika virus exposure who seek care [more than] 12 weeks after symptom onset or possible exposure, IgM antibody testing might be considered,” the CDC wrote. “If fetal abnormalities are present, rRT-PCR testing should also be performed on maternal serum and urine [but] a negative IgM antibody test or rRT-PCR result [more than] 12 weeks after symptom onset or possible exposure does not rule out recent Zika virus infection.”
For pregnant women with a diagnosis of a confirmed or presumptive Flavivirus infection, regardless of whether it’s specifically Zika virus or not, the CDC recommends getting serial ultrasounds every 3-4 weeks during pregnancy in order to monitor the fetus’s development, while “decisions regarding amniocentesis should be individualized for each clinical circumstance.” After the child’s birth, rRT-PCR should be conducted on the child’s cord blood and serum; Zika virus and dengue virus IgM are also recommended.
Pregnant women without a diagnosis of either Zika virus or dengue virus should have a prenatal ultrasound; if abnormalities are found in the fetus, CDC recommends that they have a repeat Zika virus rRT-PCR and IgM test and that clinicians base management on corresponding laboratory results. If nothing is found, however, then standard care can resume with ongoing vigilance to avoid Zika virus infections. Women with dengue virus diagnoses should follow the guidance that is currently in place.
“Pregnant women with laboratory evidence of confirmed or possible Zika virus infection who experience a fetal loss or stillbirth should be offered pathology testing for Zika virus infection,” the CDC added. “This testing might provide insight into the etiology of the fetal loss, which could inform a woman’s future pregnancy planning.”
The CDC also issued updated guidance for preventing sexual transmission of Zika virus and that applies to all men and women who have traveled to or reside in areas with active Zika virus transmission and their sex partners (MMWR. ePub: 2016 25 Jul. doi: 10.15585/mmwr.mm6529e2). The CDC advises couples in which a woman is pregnant to use barriers methods or abstain from sex for the duration of the pregnancy. For couples not planning pregnancy and in which there is a male partner with confirmed Zika virus infection or symptoms of infection, the men should use barrier methods or abstain from sex for at least 6 months after the onset of illness. For women with Zika virus infection, they should use barrier protection or abstain from sex for at least 8 weeks after the onset of illness.
FROM MMWR
CDC: Infants with Zika symptoms should get specialized care
Diagnostic testing of infants with suspected congenital Zika virus should include both immunoglobulin M (IgM) and polymerase chain reaction (PCR) testing, according to initial recommendations from a work group of federal health officials and pediatric specialists.
The group also called for infants with Zika virus symptoms to be transferred to facilities with pediatric subspecialty services.
Officials at the Centers for Disease Control and Prevention, along with pediatric specialists, reviewed the CDC’s existing guidelines for diagnosing, treating, and preventing Zika virus infections in both pregnant mothers and their infants during a 2-day meeting at the agency’s headquarters in Atlanta July 21-22.
“We want to make sure in the evaluation of symptomatic infants that we’re opening up a thorough differential, and that people are thinking about other things, particularly as we know that some of these issues, especially in terms of diagnosis, may be complex,” said Wanda D. Barfield, MD, director of the division of reproductive health at the CDC’s National Center for Chronic Disease Prevention and Health Promotion.
Although final recommendations are forthcoming, the consensus of the work group is that diagnostic testing of infants with suspected congenital Zika virus infection should include IgM and PCR testing of cerebrospinal fluid, urine, saliva and other infant specimens.
Asymptomatic infants should continue to receive care consistent with that of a normal, newborn infant, along with comprehensive physical exams, hearing tests, and head ultrasounds.
Symptomatic infants, however, should undergo different clinical and laboratory evaluations. Any symptomatic infant should be transferred to a pediatric subspecialty facility, which would allow for more specific care and services than would a primary care office. These services would include: neonatal/pediatric intensive care; endocrinologists to treat hypothyroidism, hypoaldosteronism, and growth hormone deficiency; orthopedists to treat arthrogryposis; neurologists to perform neuroimaging and EEGs, and to treat microcephaly and seizures; and other specialists to handle infectious disease, pulmonology, genetics, and feeding issues. These facilities would also offer family and social support, including palliative care options.
Infants with anomalies associated with congenital Zika virus infection should see a primary care physician every month for “routine care and increased surveillance,” said Janet Cragan, MD, of the CDC’s National Center on Birth Defects and Developmental Disorders. These visits should include measurements of weight, length, and head circumference, and should continue through 6 months of age. After that, the frequency of visits can be reevaluated.
During subsequent visits, providers should continue to monitor the infant’s development, as certain abnormalities take longer to become evident. These include sleep issues, excessive irritability, seizures, and “subtle symptoms” such as infantile spasms.
“In terms of coordination of care, there was discussion about the need to close the loop [to] ensure that the needed testing and consultations are done, [and] that the primary physician obtain those results,” Dr. Cragan said.
Similar monitoring – though less complex and stringent – should be done for children with congenital Zika virus infection who do not exhibit abnormalities and may not be symptomatic, the work group recommended. In addition, outpatient care is another critical component in managing congenital Zika virus infections, particularly in children who display no abnormalities at birth. Specifically, hearing evaluations should be performed regularly, and if any abnormalities are found, children should be referred for repeat hearing evaluations.
“We’re talking about a group of infants that we have very little to no information about,” said Kate Russell, MD, of Duke University, Durham, N.C. “Our discussion revolved around what’s known about infants who do have apparent abnormalities and are symptomatic, and trying to infer from that what could be done for these infants with asymptomatic infections.”
Telemedicine is another potentially powerful tool that physicians can use, “particularly in areas where there is limited direct access to pediatric subspecialty care,” Dr. Cragan said. Examples include taking videos of an infant and sending them to a neurologist to determine if symptoms were consistent with Zika, or sharing audio of the crying of Zika-infected children in Brazil so that primary care physicians can compare that with their patients.
“This is an area of very new and growing research and literature, and so this is going to be a continuous process [to] make sure that the people who are going to be seeing these infants on the front line are aware of what’s known,” Dr. Russell said.
Diagnostic testing of infants with suspected congenital Zika virus should include both immunoglobulin M (IgM) and polymerase chain reaction (PCR) testing, according to initial recommendations from a work group of federal health officials and pediatric specialists.
The group also called for infants with Zika virus symptoms to be transferred to facilities with pediatric subspecialty services.
Officials at the Centers for Disease Control and Prevention, along with pediatric specialists, reviewed the CDC’s existing guidelines for diagnosing, treating, and preventing Zika virus infections in both pregnant mothers and their infants during a 2-day meeting at the agency’s headquarters in Atlanta July 21-22.
“We want to make sure in the evaluation of symptomatic infants that we’re opening up a thorough differential, and that people are thinking about other things, particularly as we know that some of these issues, especially in terms of diagnosis, may be complex,” said Wanda D. Barfield, MD, director of the division of reproductive health at the CDC’s National Center for Chronic Disease Prevention and Health Promotion.
Although final recommendations are forthcoming, the consensus of the work group is that diagnostic testing of infants with suspected congenital Zika virus infection should include IgM and PCR testing of cerebrospinal fluid, urine, saliva and other infant specimens.
Asymptomatic infants should continue to receive care consistent with that of a normal, newborn infant, along with comprehensive physical exams, hearing tests, and head ultrasounds.
Symptomatic infants, however, should undergo different clinical and laboratory evaluations. Any symptomatic infant should be transferred to a pediatric subspecialty facility, which would allow for more specific care and services than would a primary care office. These services would include: neonatal/pediatric intensive care; endocrinologists to treat hypothyroidism, hypoaldosteronism, and growth hormone deficiency; orthopedists to treat arthrogryposis; neurologists to perform neuroimaging and EEGs, and to treat microcephaly and seizures; and other specialists to handle infectious disease, pulmonology, genetics, and feeding issues. These facilities would also offer family and social support, including palliative care options.
Infants with anomalies associated with congenital Zika virus infection should see a primary care physician every month for “routine care and increased surveillance,” said Janet Cragan, MD, of the CDC’s National Center on Birth Defects and Developmental Disorders. These visits should include measurements of weight, length, and head circumference, and should continue through 6 months of age. After that, the frequency of visits can be reevaluated.
During subsequent visits, providers should continue to monitor the infant’s development, as certain abnormalities take longer to become evident. These include sleep issues, excessive irritability, seizures, and “subtle symptoms” such as infantile spasms.
“In terms of coordination of care, there was discussion about the need to close the loop [to] ensure that the needed testing and consultations are done, [and] that the primary physician obtain those results,” Dr. Cragan said.
Similar monitoring – though less complex and stringent – should be done for children with congenital Zika virus infection who do not exhibit abnormalities and may not be symptomatic, the work group recommended. In addition, outpatient care is another critical component in managing congenital Zika virus infections, particularly in children who display no abnormalities at birth. Specifically, hearing evaluations should be performed regularly, and if any abnormalities are found, children should be referred for repeat hearing evaluations.
“We’re talking about a group of infants that we have very little to no information about,” said Kate Russell, MD, of Duke University, Durham, N.C. “Our discussion revolved around what’s known about infants who do have apparent abnormalities and are symptomatic, and trying to infer from that what could be done for these infants with asymptomatic infections.”
Telemedicine is another potentially powerful tool that physicians can use, “particularly in areas where there is limited direct access to pediatric subspecialty care,” Dr. Cragan said. Examples include taking videos of an infant and sending them to a neurologist to determine if symptoms were consistent with Zika, or sharing audio of the crying of Zika-infected children in Brazil so that primary care physicians can compare that with their patients.
“This is an area of very new and growing research and literature, and so this is going to be a continuous process [to] make sure that the people who are going to be seeing these infants on the front line are aware of what’s known,” Dr. Russell said.
Diagnostic testing of infants with suspected congenital Zika virus should include both immunoglobulin M (IgM) and polymerase chain reaction (PCR) testing, according to initial recommendations from a work group of federal health officials and pediatric specialists.
The group also called for infants with Zika virus symptoms to be transferred to facilities with pediatric subspecialty services.
Officials at the Centers for Disease Control and Prevention, along with pediatric specialists, reviewed the CDC’s existing guidelines for diagnosing, treating, and preventing Zika virus infections in both pregnant mothers and their infants during a 2-day meeting at the agency’s headquarters in Atlanta July 21-22.
“We want to make sure in the evaluation of symptomatic infants that we’re opening up a thorough differential, and that people are thinking about other things, particularly as we know that some of these issues, especially in terms of diagnosis, may be complex,” said Wanda D. Barfield, MD, director of the division of reproductive health at the CDC’s National Center for Chronic Disease Prevention and Health Promotion.
Although final recommendations are forthcoming, the consensus of the work group is that diagnostic testing of infants with suspected congenital Zika virus infection should include IgM and PCR testing of cerebrospinal fluid, urine, saliva and other infant specimens.
Asymptomatic infants should continue to receive care consistent with that of a normal, newborn infant, along with comprehensive physical exams, hearing tests, and head ultrasounds.
Symptomatic infants, however, should undergo different clinical and laboratory evaluations. Any symptomatic infant should be transferred to a pediatric subspecialty facility, which would allow for more specific care and services than would a primary care office. These services would include: neonatal/pediatric intensive care; endocrinologists to treat hypothyroidism, hypoaldosteronism, and growth hormone deficiency; orthopedists to treat arthrogryposis; neurologists to perform neuroimaging and EEGs, and to treat microcephaly and seizures; and other specialists to handle infectious disease, pulmonology, genetics, and feeding issues. These facilities would also offer family and social support, including palliative care options.
Infants with anomalies associated with congenital Zika virus infection should see a primary care physician every month for “routine care and increased surveillance,” said Janet Cragan, MD, of the CDC’s National Center on Birth Defects and Developmental Disorders. These visits should include measurements of weight, length, and head circumference, and should continue through 6 months of age. After that, the frequency of visits can be reevaluated.
During subsequent visits, providers should continue to monitor the infant’s development, as certain abnormalities take longer to become evident. These include sleep issues, excessive irritability, seizures, and “subtle symptoms” such as infantile spasms.
“In terms of coordination of care, there was discussion about the need to close the loop [to] ensure that the needed testing and consultations are done, [and] that the primary physician obtain those results,” Dr. Cragan said.
Similar monitoring – though less complex and stringent – should be done for children with congenital Zika virus infection who do not exhibit abnormalities and may not be symptomatic, the work group recommended. In addition, outpatient care is another critical component in managing congenital Zika virus infections, particularly in children who display no abnormalities at birth. Specifically, hearing evaluations should be performed regularly, and if any abnormalities are found, children should be referred for repeat hearing evaluations.
“We’re talking about a group of infants that we have very little to no information about,” said Kate Russell, MD, of Duke University, Durham, N.C. “Our discussion revolved around what’s known about infants who do have apparent abnormalities and are symptomatic, and trying to infer from that what could be done for these infants with asymptomatic infections.”
Telemedicine is another potentially powerful tool that physicians can use, “particularly in areas where there is limited direct access to pediatric subspecialty care,” Dr. Cragan said. Examples include taking videos of an infant and sending them to a neurologist to determine if symptoms were consistent with Zika, or sharing audio of the crying of Zika-infected children in Brazil so that primary care physicians can compare that with their patients.
“This is an area of very new and growing research and literature, and so this is going to be a continuous process [to] make sure that the people who are going to be seeing these infants on the front line are aware of what’s known,” Dr. Russell said.
CDC reports three new cases of Zika-related birth defects
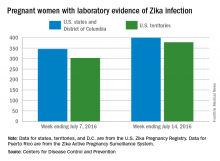
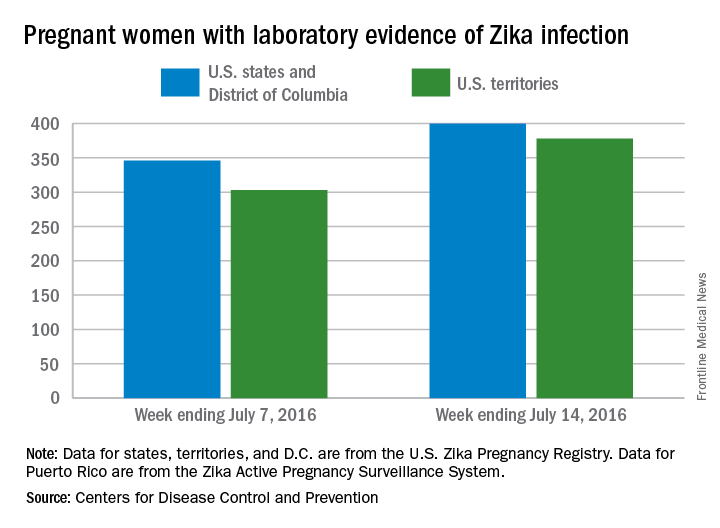
Three new cases of infants born with Zika virus–related birth defects were reported in the United States for the week ending July 14, 2016, along with 129 new infections in pregnant women, according to the Centers for Disease Control and Prevention.
The three infants were born in the 50 states and the District of Columbia, with no new pregnancy losses reported in the states or U.S. territories. Totals for the year are 12 infants with birth defects, all in the states, and seven pregnancy losses, of which six occurred in the states, the CDC reported July 21. State- or territorial-level data are not being reported to protect the privacy of affected women and children.
Of the 129 new infections in pregnant women for the week, 54 occurred in the states and 75 occurred in the U.S. territories. Those new cases bring the U.S. total to 778 for the year: 400 in the states and 378 in territories, the CDC also reported on July 21.
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
Three new cases of infants born with Zika virus–related birth defects were reported in the United States for the week ending July 14, 2016, along with 129 new infections in pregnant women, according to the Centers for Disease Control and Prevention.
The three infants were born in the 50 states and the District of Columbia, with no new pregnancy losses reported in the states or U.S. territories. Totals for the year are 12 infants with birth defects, all in the states, and seven pregnancy losses, of which six occurred in the states, the CDC reported July 21. State- or territorial-level data are not being reported to protect the privacy of affected women and children.
Of the 129 new infections in pregnant women for the week, 54 occurred in the states and 75 occurred in the U.S. territories. Those new cases bring the U.S. total to 778 for the year: 400 in the states and 378 in territories, the CDC also reported on July 21.
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
Three new cases of infants born with Zika virus–related birth defects were reported in the United States for the week ending July 14, 2016, along with 129 new infections in pregnant women, according to the Centers for Disease Control and Prevention.
The three infants were born in the 50 states and the District of Columbia, with no new pregnancy losses reported in the states or U.S. territories. Totals for the year are 12 infants with birth defects, all in the states, and seven pregnancy losses, of which six occurred in the states, the CDC reported July 21. State- or territorial-level data are not being reported to protect the privacy of affected women and children.
Of the 129 new infections in pregnant women for the week, 54 occurred in the states and 75 occurred in the U.S. territories. Those new cases bring the U.S. total to 778 for the year: 400 in the states and 378 in territories, the CDC also reported on July 21.
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
Health officials investigating mysterious Zika infection
Health officials are looking into a case of Zika virus infection in Utah, where a person was infected after caring for an elderly family member with the virus.
In the new case, the person had not recently traveled to an area with Zika and had not had sex with anyone with Zika infection or who had traveled to an area with Zika. Also, there is no current evidence that the Aedes mosquitoes, known to spread Zika virus, have been active in Utah.
The elderly Utah man who was first infected with Zika died in late June of unknown causes. He had traveled to an area with Zika, and laboratory tests revealed that he had virus levels more than 100,000 times higher than seen in other samples of infected people, according to the Centers for Disease Control and Prevention.
The Utah Department of Health and the CDC are investigating the possible cause of infection.
“We are trying to determine if the contact between the very sick elderly patient and the person played a role in how the person got sick,” Satish Pillai, PhD, deputy incident manager with CDC’s Zika response, said during a news conference. “We don’t have all of the answers right now, but we will continue to share the information as it comes available.”
CDC currently is not altering its instructions on the use of personal protective equipment.
“I think what this highlights is the fact that when you have an infection like Zika virus ... wherein a good percentage of patients don’t actually have symptoms, it means that it’s as important as ever to stick with good adherence to standard precautions,” Dr. Pillai said. “Just like we assume anybody might carry hepatitis or HIV, we don’t wait for a positive diagnosis in order to prevent blood or body fluid exposure. The same thing is true with Zika virus, and I think this is a great example of why we should never take chances, but always adhere to careful standards of touching.”
“The new case in Utah is a surprise, showing that we still have more to learn about Zika,” Erin Staples, MD, PhD, CDC medical epidemiologist on the ground in Utah, said in a statement. “Fortunately, the patient recovered quickly, and from what we have seen with more than 1,300 travel-associated cases of Zika in the continental United States and Hawaii, nonsexual spread from one person to another does not appear to be common.”
On Twitter @maryellenny
Health officials are looking into a case of Zika virus infection in Utah, where a person was infected after caring for an elderly family member with the virus.
In the new case, the person had not recently traveled to an area with Zika and had not had sex with anyone with Zika infection or who had traveled to an area with Zika. Also, there is no current evidence that the Aedes mosquitoes, known to spread Zika virus, have been active in Utah.
The elderly Utah man who was first infected with Zika died in late June of unknown causes. He had traveled to an area with Zika, and laboratory tests revealed that he had virus levels more than 100,000 times higher than seen in other samples of infected people, according to the Centers for Disease Control and Prevention.
The Utah Department of Health and the CDC are investigating the possible cause of infection.
“We are trying to determine if the contact between the very sick elderly patient and the person played a role in how the person got sick,” Satish Pillai, PhD, deputy incident manager with CDC’s Zika response, said during a news conference. “We don’t have all of the answers right now, but we will continue to share the information as it comes available.”
CDC currently is not altering its instructions on the use of personal protective equipment.
“I think what this highlights is the fact that when you have an infection like Zika virus ... wherein a good percentage of patients don’t actually have symptoms, it means that it’s as important as ever to stick with good adherence to standard precautions,” Dr. Pillai said. “Just like we assume anybody might carry hepatitis or HIV, we don’t wait for a positive diagnosis in order to prevent blood or body fluid exposure. The same thing is true with Zika virus, and I think this is a great example of why we should never take chances, but always adhere to careful standards of touching.”
“The new case in Utah is a surprise, showing that we still have more to learn about Zika,” Erin Staples, MD, PhD, CDC medical epidemiologist on the ground in Utah, said in a statement. “Fortunately, the patient recovered quickly, and from what we have seen with more than 1,300 travel-associated cases of Zika in the continental United States and Hawaii, nonsexual spread from one person to another does not appear to be common.”
On Twitter @maryellenny
Health officials are looking into a case of Zika virus infection in Utah, where a person was infected after caring for an elderly family member with the virus.
In the new case, the person had not recently traveled to an area with Zika and had not had sex with anyone with Zika infection or who had traveled to an area with Zika. Also, there is no current evidence that the Aedes mosquitoes, known to spread Zika virus, have been active in Utah.
The elderly Utah man who was first infected with Zika died in late June of unknown causes. He had traveled to an area with Zika, and laboratory tests revealed that he had virus levels more than 100,000 times higher than seen in other samples of infected people, according to the Centers for Disease Control and Prevention.
The Utah Department of Health and the CDC are investigating the possible cause of infection.
“We are trying to determine if the contact between the very sick elderly patient and the person played a role in how the person got sick,” Satish Pillai, PhD, deputy incident manager with CDC’s Zika response, said during a news conference. “We don’t have all of the answers right now, but we will continue to share the information as it comes available.”
CDC currently is not altering its instructions on the use of personal protective equipment.
“I think what this highlights is the fact that when you have an infection like Zika virus ... wherein a good percentage of patients don’t actually have symptoms, it means that it’s as important as ever to stick with good adherence to standard precautions,” Dr. Pillai said. “Just like we assume anybody might carry hepatitis or HIV, we don’t wait for a positive diagnosis in order to prevent blood or body fluid exposure. The same thing is true with Zika virus, and I think this is a great example of why we should never take chances, but always adhere to careful standards of touching.”
“The new case in Utah is a surprise, showing that we still have more to learn about Zika,” Erin Staples, MD, PhD, CDC medical epidemiologist on the ground in Utah, said in a statement. “Fortunately, the patient recovered quickly, and from what we have seen with more than 1,300 travel-associated cases of Zika in the continental United States and Hawaii, nonsexual spread from one person to another does not appear to be common.”
On Twitter @maryellenny
First female-to-male sexual transmission of Zika virus
A suspected case of sexual transmission of the Zika virus from a female to a male has occurred in New York City, according to the New York City Department of Health and Mental Hygiene (DOHMH).
“This case represents the first reported occurrence of female-to-male sexual transmission of Zika virus,” Alexander Davidson of the DOHMH and his coauthors stated in the CDC’s Morbidity and Mortality Weekly Report. “Current guidance to prevent sexual transmission of Zika virus is based on the assumption that transmission occurs from a male partner to a receptive partner.”
The woman, reportedly in her twenties and not pregnant at the time of infection, had traveled to a region experiencing high volumes of Zika virus transmission. Upon returning home, the woman engaged in condomless vaginal intercourse with her male partner, and subsequently developed symptoms consistent with a Zika virus infection. Three days after symptom onset, her primary care provider took blood and urine samples, from which a Zika virus infection was confirmed. (MMWR Morb Mortal Wkly Rep. 2016 Jul 15. doi: 10.15585/mmwr.mm6528e2)
A week after the sexual encounter, her partner – also in his twenties – began experiencing symptoms of Zika virus infection. Three days after the onset of his symptoms, he went to the same primary care provider as the woman. He confirmed that he had not traveled outside of the United States in the last year, had engaged in condomless vaginal sex with just one individual (the aforementioned female), had no blood on his penis to indicate vaginal bleeding or the presence of open lesions, and had no mosquito bites in the previous week.
“The timing and sequence of events support female-to-male Zika virus transmission through condomless vaginal intercourse,” the coauthors conclude, adding that “virus present in either vaginal fluids or menstrual blood might have been transmitted during exposure to her male partner’s urethral mucosa or undetected abrasions on his penis.”
Both the female and male were tested via real-time reverse transcription–polymerase chain reaction (rRT-PCR), with serum testing done via the Zika immunoglobulin M antibody capture enzyme-linked immunosorbent assay (Zika MAC-ELISA). The rRT-PCR testing showed Zika virus RNA in the woman’s serum, despite being collected three days after the sexual encounter, meaning she was viremic at the time. Studies on nonhuman primates have shown that Zika virus RNA can remain present in vaginal fluid for up to a week, according to the report.
The CDC is cautioning pregnant women against travel to Zika-heavy areas, in particular the 2016 Summer Olympic Games in Rio de Janeiro. Health care providers who receive patients with Zika-like symptoms should ask if the patient has had sexual contact with someone who has traveled to an affected region, if the patient did not travel to such a region.
A suspected case of sexual transmission of the Zika virus from a female to a male has occurred in New York City, according to the New York City Department of Health and Mental Hygiene (DOHMH).
“This case represents the first reported occurrence of female-to-male sexual transmission of Zika virus,” Alexander Davidson of the DOHMH and his coauthors stated in the CDC’s Morbidity and Mortality Weekly Report. “Current guidance to prevent sexual transmission of Zika virus is based on the assumption that transmission occurs from a male partner to a receptive partner.”
The woman, reportedly in her twenties and not pregnant at the time of infection, had traveled to a region experiencing high volumes of Zika virus transmission. Upon returning home, the woman engaged in condomless vaginal intercourse with her male partner, and subsequently developed symptoms consistent with a Zika virus infection. Three days after symptom onset, her primary care provider took blood and urine samples, from which a Zika virus infection was confirmed. (MMWR Morb Mortal Wkly Rep. 2016 Jul 15. doi: 10.15585/mmwr.mm6528e2)
A week after the sexual encounter, her partner – also in his twenties – began experiencing symptoms of Zika virus infection. Three days after the onset of his symptoms, he went to the same primary care provider as the woman. He confirmed that he had not traveled outside of the United States in the last year, had engaged in condomless vaginal sex with just one individual (the aforementioned female), had no blood on his penis to indicate vaginal bleeding or the presence of open lesions, and had no mosquito bites in the previous week.
“The timing and sequence of events support female-to-male Zika virus transmission through condomless vaginal intercourse,” the coauthors conclude, adding that “virus present in either vaginal fluids or menstrual blood might have been transmitted during exposure to her male partner’s urethral mucosa or undetected abrasions on his penis.”
Both the female and male were tested via real-time reverse transcription–polymerase chain reaction (rRT-PCR), with serum testing done via the Zika immunoglobulin M antibody capture enzyme-linked immunosorbent assay (Zika MAC-ELISA). The rRT-PCR testing showed Zika virus RNA in the woman’s serum, despite being collected three days after the sexual encounter, meaning she was viremic at the time. Studies on nonhuman primates have shown that Zika virus RNA can remain present in vaginal fluid for up to a week, according to the report.
The CDC is cautioning pregnant women against travel to Zika-heavy areas, in particular the 2016 Summer Olympic Games in Rio de Janeiro. Health care providers who receive patients with Zika-like symptoms should ask if the patient has had sexual contact with someone who has traveled to an affected region, if the patient did not travel to such a region.
A suspected case of sexual transmission of the Zika virus from a female to a male has occurred in New York City, according to the New York City Department of Health and Mental Hygiene (DOHMH).
“This case represents the first reported occurrence of female-to-male sexual transmission of Zika virus,” Alexander Davidson of the DOHMH and his coauthors stated in the CDC’s Morbidity and Mortality Weekly Report. “Current guidance to prevent sexual transmission of Zika virus is based on the assumption that transmission occurs from a male partner to a receptive partner.”
The woman, reportedly in her twenties and not pregnant at the time of infection, had traveled to a region experiencing high volumes of Zika virus transmission. Upon returning home, the woman engaged in condomless vaginal intercourse with her male partner, and subsequently developed symptoms consistent with a Zika virus infection. Three days after symptom onset, her primary care provider took blood and urine samples, from which a Zika virus infection was confirmed. (MMWR Morb Mortal Wkly Rep. 2016 Jul 15. doi: 10.15585/mmwr.mm6528e2)
A week after the sexual encounter, her partner – also in his twenties – began experiencing symptoms of Zika virus infection. Three days after the onset of his symptoms, he went to the same primary care provider as the woman. He confirmed that he had not traveled outside of the United States in the last year, had engaged in condomless vaginal sex with just one individual (the aforementioned female), had no blood on his penis to indicate vaginal bleeding or the presence of open lesions, and had no mosquito bites in the previous week.
“The timing and sequence of events support female-to-male Zika virus transmission through condomless vaginal intercourse,” the coauthors conclude, adding that “virus present in either vaginal fluids or menstrual blood might have been transmitted during exposure to her male partner’s urethral mucosa or undetected abrasions on his penis.”
Both the female and male were tested via real-time reverse transcription–polymerase chain reaction (rRT-PCR), with serum testing done via the Zika immunoglobulin M antibody capture enzyme-linked immunosorbent assay (Zika MAC-ELISA). The rRT-PCR testing showed Zika virus RNA in the woman’s serum, despite being collected three days after the sexual encounter, meaning she was viremic at the time. Studies on nonhuman primates have shown that Zika virus RNA can remain present in vaginal fluid for up to a week, according to the report.
The CDC is cautioning pregnant women against travel to Zika-heavy areas, in particular the 2016 Summer Olympic Games in Rio de Janeiro. Health care providers who receive patients with Zika-like symptoms should ask if the patient has had sexual contact with someone who has traveled to an affected region, if the patient did not travel to such a region.
FROM MMWR
Number of U.S. Zika-related poor pregnancy outcomes rise to 16
One pregnancy loss with birth defects related to Zika virus was reported in the week ending July 7, 2016, along with two liveborn infants with Zika-related birth defects, according to the Centers for Disease Control and Prevention.
That brings the total number of Zika-related poor birth outcomes in the United States to seven pregnancy losses and nine liveborn infants with birth defects, the CDC reported July 14.
All three of the latest Zika-related poor outcomes occurred in the 50 states and the District of Columbia. Of the 16 total poor outcomes so far, 15 have occurred in the 50 states and D.C.; one pregnancy loss has been reported in the U.S. territories. State- or territorial-level data are not being reported to protect the privacy of affected women and children, the CDC said.
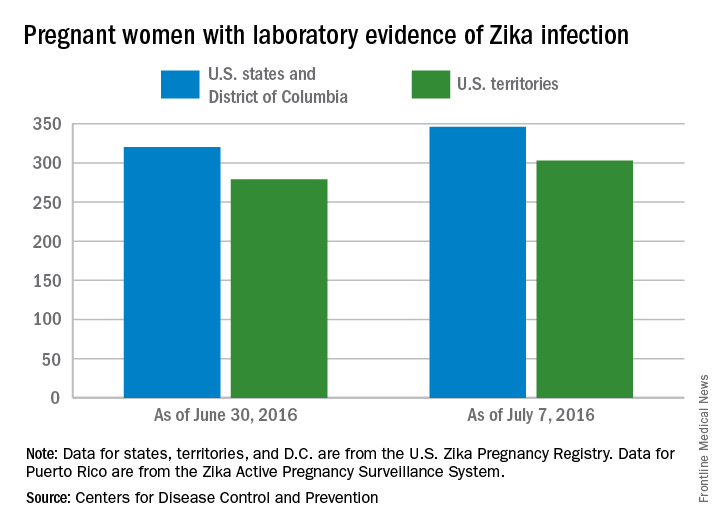
The CDC also reported that 346 pregnant women in the 50 states and D.C. and 303 women in U.S. territories have had laboratory evidence of Zika virus infection, for a total of 649 nationwide as of July 7.
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
One pregnancy loss with birth defects related to Zika virus was reported in the week ending July 7, 2016, along with two liveborn infants with Zika-related birth defects, according to the Centers for Disease Control and Prevention.
That brings the total number of Zika-related poor birth outcomes in the United States to seven pregnancy losses and nine liveborn infants with birth defects, the CDC reported July 14.
All three of the latest Zika-related poor outcomes occurred in the 50 states and the District of Columbia. Of the 16 total poor outcomes so far, 15 have occurred in the 50 states and D.C.; one pregnancy loss has been reported in the U.S. territories. State- or territorial-level data are not being reported to protect the privacy of affected women and children, the CDC said.
The CDC also reported that 346 pregnant women in the 50 states and D.C. and 303 women in U.S. territories have had laboratory evidence of Zika virus infection, for a total of 649 nationwide as of July 7.
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
One pregnancy loss with birth defects related to Zika virus was reported in the week ending July 7, 2016, along with two liveborn infants with Zika-related birth defects, according to the Centers for Disease Control and Prevention.
That brings the total number of Zika-related poor birth outcomes in the United States to seven pregnancy losses and nine liveborn infants with birth defects, the CDC reported July 14.
All three of the latest Zika-related poor outcomes occurred in the 50 states and the District of Columbia. Of the 16 total poor outcomes so far, 15 have occurred in the 50 states and D.C.; one pregnancy loss has been reported in the U.S. territories. State- or territorial-level data are not being reported to protect the privacy of affected women and children, the CDC said.
The CDC also reported that 346 pregnant women in the 50 states and D.C. and 303 women in U.S. territories have had laboratory evidence of Zika virus infection, for a total of 649 nationwide as of July 7.
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
Case study: Zika virus may persist in female genital tract
Zika virus appears to be able to persist in a woman’s genital tract even after it is no longer detectable in blood and urine, according to a new case study.
The findings raise the possibility of woman-to-man sexual transmission of the virus, as well as mother-to-child vertical transmission.
Nadia Prisant, MD, of the University Hospital Center Pointe à Pitre, Guadeloupe, France, and her colleagues reported the case of a 27-year-old woman in France who tested positive for Zika virus infection in May. The initial blood test was positive, while the urine sample was negative (Lancet Infect Dis. 2016 Jul 11. doi: 10.1016/S1473-3099[16]30193-1).
A genital swab, endocervical swab, and a cervical mucus sample were collected 3 days after symptom onset and all tested positive for Zika virus RNA. On day 11 after symptom onset, the woman’s blood and urine samples both tested negative, but her cervical mucus continued to test positive for Zika virus RNA.
The researchers stated that this is the first report of the presence of Zika virus in the genital tract of a woman, as well as its possible persistence after the virus is no longer detectable in blood and urine samples.
“Although we have not tested the infectiousness of a locally situated vaginal virus, its very presence in the female genital tract poses notable challenges, implying that sexual transmission from women to men could occur, as is the case for other viral infections,” the researchers wrote. “Zika virus presence in the female genital tract also means that vertical transmission from mother to fetus needs to be assessed, since this virus is a member of the Flaviviridae family, which includes hepatitis C, in which vertical transmission from mother to child can occur in up to 10% of pregnancies.”
The researchers reported having no relevant financial disclosures.
On Twitter @maryellenny
Zika virus appears to be able to persist in a woman’s genital tract even after it is no longer detectable in blood and urine, according to a new case study.
The findings raise the possibility of woman-to-man sexual transmission of the virus, as well as mother-to-child vertical transmission.
Nadia Prisant, MD, of the University Hospital Center Pointe à Pitre, Guadeloupe, France, and her colleagues reported the case of a 27-year-old woman in France who tested positive for Zika virus infection in May. The initial blood test was positive, while the urine sample was negative (Lancet Infect Dis. 2016 Jul 11. doi: 10.1016/S1473-3099[16]30193-1).
A genital swab, endocervical swab, and a cervical mucus sample were collected 3 days after symptom onset and all tested positive for Zika virus RNA. On day 11 after symptom onset, the woman’s blood and urine samples both tested negative, but her cervical mucus continued to test positive for Zika virus RNA.
The researchers stated that this is the first report of the presence of Zika virus in the genital tract of a woman, as well as its possible persistence after the virus is no longer detectable in blood and urine samples.
“Although we have not tested the infectiousness of a locally situated vaginal virus, its very presence in the female genital tract poses notable challenges, implying that sexual transmission from women to men could occur, as is the case for other viral infections,” the researchers wrote. “Zika virus presence in the female genital tract also means that vertical transmission from mother to fetus needs to be assessed, since this virus is a member of the Flaviviridae family, which includes hepatitis C, in which vertical transmission from mother to child can occur in up to 10% of pregnancies.”
The researchers reported having no relevant financial disclosures.
On Twitter @maryellenny
Zika virus appears to be able to persist in a woman’s genital tract even after it is no longer detectable in blood and urine, according to a new case study.
The findings raise the possibility of woman-to-man sexual transmission of the virus, as well as mother-to-child vertical transmission.
Nadia Prisant, MD, of the University Hospital Center Pointe à Pitre, Guadeloupe, France, and her colleagues reported the case of a 27-year-old woman in France who tested positive for Zika virus infection in May. The initial blood test was positive, while the urine sample was negative (Lancet Infect Dis. 2016 Jul 11. doi: 10.1016/S1473-3099[16]30193-1).
A genital swab, endocervical swab, and a cervical mucus sample were collected 3 days after symptom onset and all tested positive for Zika virus RNA. On day 11 after symptom onset, the woman’s blood and urine samples both tested negative, but her cervical mucus continued to test positive for Zika virus RNA.
The researchers stated that this is the first report of the presence of Zika virus in the genital tract of a woman, as well as its possible persistence after the virus is no longer detectable in blood and urine samples.
“Although we have not tested the infectiousness of a locally situated vaginal virus, its very presence in the female genital tract poses notable challenges, implying that sexual transmission from women to men could occur, as is the case for other viral infections,” the researchers wrote. “Zika virus presence in the female genital tract also means that vertical transmission from mother to fetus needs to be assessed, since this virus is a member of the Flaviviridae family, which includes hepatitis C, in which vertical transmission from mother to child can occur in up to 10% of pregnancies.”
The researchers reported having no relevant financial disclosures.
On Twitter @maryellenny
FROM THE LANCET INFECTIOUS DISEASES
Key clinical point: Zika virus RNA was found in a woman’s genital tract.
Major finding: On day 11 after symptom onset, the woman’s blood and urine samples both tested negative, but her cervical mucus continued to test positive for Zika virus RNA.
Data source: A case study of a 27-year-old woman in Guadeloupe, France with Zika virus.
Disclosures: The researchers reported having no relevant financial disclosures.
Olympic Games create novel opportunity to study Zika virus
Behind the competition and pageantry of the 2016 Summer Olympics and Paralympics in Rio de Janeiro, researchers at the University of Utah will be busy monitoring a subset of athletes, coaches, and other U.S. Olympic Committee staff for potential Zika virus exposure.
“Of everyone I talk to who’s at risk for Zika virus, their No. 1 question is, what are the risks to my reproductive health?” said the study’s principal investigator Carrie L. Byington, MD, a pediatrician and infectious disease specialist who is codirector of Utah Center for Clinical and Translational Science at the University of Utah in Salt Lake City. “Can I have a healthy baby? How can I protect that opportunity to reproduce? We are dedicated to trying to find some answers.”
In a study funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Dr. Byington and a team of six other clinicians will recruit up to 1,000 athletes, coaches, and other U.S. Olympic Committee (USOC) staff attending the games to complete health surveys and undergo pre- and post-travel periodic antibody testing for Zika virus, a mosquito-borne flavivirus that has emerged in the Americas with local transmission identified in 30 countries and territories as of April 2016, including Brazil. From that group they expect to identify infected individuals. “Hopefully, it’s a very small proportion of the group but we think that we will identify some, because it is going to be impossible to prevent all mosquito exposure, even over the short term,” Dr. Byington said. Those found to harbor Zika virus by antibody testing will be followed for up to 2 years and will be asked to submit self-collected samples of blood, urine, saliva, semen, and vaginal secretions monthly. Affected individuals who wish to conceive after the games will have access to the study personnel, who include four infectious disease specialists, two obstetrician-gynecologists, and a laboratory expert. “We will have monthly testing and direct consultation with them regarding their test results and help them make the best reproductive decisions they can,” Dr. Byington said.
In April 2016, the Centers for Disease Control and Prevention confirmed that fetal infection with Zika virus was the cause of microcephaly and other severe brain anomalies that result in permanent morbidity in surviving infants. According to a description of the current study published by the National Institutes of Health, many questions remain regarding infection with Zika virus, including the duration and potential for sexual or perinatal transmission from body fluids; the short and long-term reproductive outcomes of individuals infected with Zika virus; and the outcomes for infants born to men and women with either symptomatic or asymptomatic Zika virus infection. The researchers consider each study participant as equally susceptible to Zika virus exposure, regardless of his or her sport or role with the USOC. “People will be both indoors and outdoors, and these are indoor-dwelling mosquitoes, so I don’t think we can completely eliminate the risk for any type of traveler,” Dr. Byington said. “We’re very interested in the water venues, but we’re also concerned about standing water outside other venues or hotel rooms.” If a study participant falls ill in Rio de Janeiro with symptoms consistent with Zika virus, USOC medical personnel will send samples of blood, urine, and saliva to the Utah-based research team for confirmatory polymerase chain reaction testing.
The idea for the current study grew out of a pilot trial that Dr. Byington and her associates conducted in 150 individuals affiliated with the USOC who were traveling back and forth to Brazil in preparation for the games during March and April of 2016. It enabled the researchers to develop online web-based tools for consenting, tracking, and returning test results. “It allowed us to do some work with our laboratory facilities for shipping and receiving specimens and processing and running specimens and returning some results,” Dr. Byington said. “That work has been really important. We found that about one-third of our pilot was interested in becoming pregnant very shortly after the games, so that was very important information that we were able to share with the USOC and the NIH. This is a group that is very interested in their reproductive health, which makes an ideal cohort for the study.”
David Turok, MD, an ob.gyn. and member of the research team, planned long ago to attend the Olympic Games in Rio as a spectator with his wife and 14-year-old son. He intends to carry out those plans and described the current study as a unique opportunity to better understand the Zika virus. “The need for data on the topic is pressing,” said Dr. Turok, who directs the family planning fellowship at the University of Utah. “People who are Olympic athletes and coaches are probably more likely to plan their lives. We know from a wealth of epidemiologic data that people who plan their pregnancies have better outcomes. This is something that our society has done a really poor job in communicating: the challenges of parenting and the benefits of planning pregnancy and making the most effective methods of contraception available. This study is an opportunity to better our game. There’s probably no better opportunity for prospective evaluation of a group of people who we know are going to have some exposure [to Zika virus]. The known exposure and the known desired outcome make it a unique opportunity.”
The 2016 Summer Olympics will take place in Rio de Janeiro Aug. 5-21, while the Paralympic Games take place Sept. 7-18. Dr. Byington said that she hopes to be able to share preliminary study results with the public sometime in October.
Behind the competition and pageantry of the 2016 Summer Olympics and Paralympics in Rio de Janeiro, researchers at the University of Utah will be busy monitoring a subset of athletes, coaches, and other U.S. Olympic Committee staff for potential Zika virus exposure.
“Of everyone I talk to who’s at risk for Zika virus, their No. 1 question is, what are the risks to my reproductive health?” said the study’s principal investigator Carrie L. Byington, MD, a pediatrician and infectious disease specialist who is codirector of Utah Center for Clinical and Translational Science at the University of Utah in Salt Lake City. “Can I have a healthy baby? How can I protect that opportunity to reproduce? We are dedicated to trying to find some answers.”
In a study funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Dr. Byington and a team of six other clinicians will recruit up to 1,000 athletes, coaches, and other U.S. Olympic Committee (USOC) staff attending the games to complete health surveys and undergo pre- and post-travel periodic antibody testing for Zika virus, a mosquito-borne flavivirus that has emerged in the Americas with local transmission identified in 30 countries and territories as of April 2016, including Brazil. From that group they expect to identify infected individuals. “Hopefully, it’s a very small proportion of the group but we think that we will identify some, because it is going to be impossible to prevent all mosquito exposure, even over the short term,” Dr. Byington said. Those found to harbor Zika virus by antibody testing will be followed for up to 2 years and will be asked to submit self-collected samples of blood, urine, saliva, semen, and vaginal secretions monthly. Affected individuals who wish to conceive after the games will have access to the study personnel, who include four infectious disease specialists, two obstetrician-gynecologists, and a laboratory expert. “We will have monthly testing and direct consultation with them regarding their test results and help them make the best reproductive decisions they can,” Dr. Byington said.
In April 2016, the Centers for Disease Control and Prevention confirmed that fetal infection with Zika virus was the cause of microcephaly and other severe brain anomalies that result in permanent morbidity in surviving infants. According to a description of the current study published by the National Institutes of Health, many questions remain regarding infection with Zika virus, including the duration and potential for sexual or perinatal transmission from body fluids; the short and long-term reproductive outcomes of individuals infected with Zika virus; and the outcomes for infants born to men and women with either symptomatic or asymptomatic Zika virus infection. The researchers consider each study participant as equally susceptible to Zika virus exposure, regardless of his or her sport or role with the USOC. “People will be both indoors and outdoors, and these are indoor-dwelling mosquitoes, so I don’t think we can completely eliminate the risk for any type of traveler,” Dr. Byington said. “We’re very interested in the water venues, but we’re also concerned about standing water outside other venues or hotel rooms.” If a study participant falls ill in Rio de Janeiro with symptoms consistent with Zika virus, USOC medical personnel will send samples of blood, urine, and saliva to the Utah-based research team for confirmatory polymerase chain reaction testing.
The idea for the current study grew out of a pilot trial that Dr. Byington and her associates conducted in 150 individuals affiliated with the USOC who were traveling back and forth to Brazil in preparation for the games during March and April of 2016. It enabled the researchers to develop online web-based tools for consenting, tracking, and returning test results. “It allowed us to do some work with our laboratory facilities for shipping and receiving specimens and processing and running specimens and returning some results,” Dr. Byington said. “That work has been really important. We found that about one-third of our pilot was interested in becoming pregnant very shortly after the games, so that was very important information that we were able to share with the USOC and the NIH. This is a group that is very interested in their reproductive health, which makes an ideal cohort for the study.”
David Turok, MD, an ob.gyn. and member of the research team, planned long ago to attend the Olympic Games in Rio as a spectator with his wife and 14-year-old son. He intends to carry out those plans and described the current study as a unique opportunity to better understand the Zika virus. “The need for data on the topic is pressing,” said Dr. Turok, who directs the family planning fellowship at the University of Utah. “People who are Olympic athletes and coaches are probably more likely to plan their lives. We know from a wealth of epidemiologic data that people who plan their pregnancies have better outcomes. This is something that our society has done a really poor job in communicating: the challenges of parenting and the benefits of planning pregnancy and making the most effective methods of contraception available. This study is an opportunity to better our game. There’s probably no better opportunity for prospective evaluation of a group of people who we know are going to have some exposure [to Zika virus]. The known exposure and the known desired outcome make it a unique opportunity.”
The 2016 Summer Olympics will take place in Rio de Janeiro Aug. 5-21, while the Paralympic Games take place Sept. 7-18. Dr. Byington said that she hopes to be able to share preliminary study results with the public sometime in October.
Behind the competition and pageantry of the 2016 Summer Olympics and Paralympics in Rio de Janeiro, researchers at the University of Utah will be busy monitoring a subset of athletes, coaches, and other U.S. Olympic Committee staff for potential Zika virus exposure.
“Of everyone I talk to who’s at risk for Zika virus, their No. 1 question is, what are the risks to my reproductive health?” said the study’s principal investigator Carrie L. Byington, MD, a pediatrician and infectious disease specialist who is codirector of Utah Center for Clinical and Translational Science at the University of Utah in Salt Lake City. “Can I have a healthy baby? How can I protect that opportunity to reproduce? We are dedicated to trying to find some answers.”
In a study funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Dr. Byington and a team of six other clinicians will recruit up to 1,000 athletes, coaches, and other U.S. Olympic Committee (USOC) staff attending the games to complete health surveys and undergo pre- and post-travel periodic antibody testing for Zika virus, a mosquito-borne flavivirus that has emerged in the Americas with local transmission identified in 30 countries and territories as of April 2016, including Brazil. From that group they expect to identify infected individuals. “Hopefully, it’s a very small proportion of the group but we think that we will identify some, because it is going to be impossible to prevent all mosquito exposure, even over the short term,” Dr. Byington said. Those found to harbor Zika virus by antibody testing will be followed for up to 2 years and will be asked to submit self-collected samples of blood, urine, saliva, semen, and vaginal secretions monthly. Affected individuals who wish to conceive after the games will have access to the study personnel, who include four infectious disease specialists, two obstetrician-gynecologists, and a laboratory expert. “We will have monthly testing and direct consultation with them regarding their test results and help them make the best reproductive decisions they can,” Dr. Byington said.
In April 2016, the Centers for Disease Control and Prevention confirmed that fetal infection with Zika virus was the cause of microcephaly and other severe brain anomalies that result in permanent morbidity in surviving infants. According to a description of the current study published by the National Institutes of Health, many questions remain regarding infection with Zika virus, including the duration and potential for sexual or perinatal transmission from body fluids; the short and long-term reproductive outcomes of individuals infected with Zika virus; and the outcomes for infants born to men and women with either symptomatic or asymptomatic Zika virus infection. The researchers consider each study participant as equally susceptible to Zika virus exposure, regardless of his or her sport or role with the USOC. “People will be both indoors and outdoors, and these are indoor-dwelling mosquitoes, so I don’t think we can completely eliminate the risk for any type of traveler,” Dr. Byington said. “We’re very interested in the water venues, but we’re also concerned about standing water outside other venues or hotel rooms.” If a study participant falls ill in Rio de Janeiro with symptoms consistent with Zika virus, USOC medical personnel will send samples of blood, urine, and saliva to the Utah-based research team for confirmatory polymerase chain reaction testing.
The idea for the current study grew out of a pilot trial that Dr. Byington and her associates conducted in 150 individuals affiliated with the USOC who were traveling back and forth to Brazil in preparation for the games during March and April of 2016. It enabled the researchers to develop online web-based tools for consenting, tracking, and returning test results. “It allowed us to do some work with our laboratory facilities for shipping and receiving specimens and processing and running specimens and returning some results,” Dr. Byington said. “That work has been really important. We found that about one-third of our pilot was interested in becoming pregnant very shortly after the games, so that was very important information that we were able to share with the USOC and the NIH. This is a group that is very interested in their reproductive health, which makes an ideal cohort for the study.”
David Turok, MD, an ob.gyn. and member of the research team, planned long ago to attend the Olympic Games in Rio as a spectator with his wife and 14-year-old son. He intends to carry out those plans and described the current study as a unique opportunity to better understand the Zika virus. “The need for data on the topic is pressing,” said Dr. Turok, who directs the family planning fellowship at the University of Utah. “People who are Olympic athletes and coaches are probably more likely to plan their lives. We know from a wealth of epidemiologic data that people who plan their pregnancies have better outcomes. This is something that our society has done a really poor job in communicating: the challenges of parenting and the benefits of planning pregnancy and making the most effective methods of contraception available. This study is an opportunity to better our game. There’s probably no better opportunity for prospective evaluation of a group of people who we know are going to have some exposure [to Zika virus]. The known exposure and the known desired outcome make it a unique opportunity.”
The 2016 Summer Olympics will take place in Rio de Janeiro Aug. 5-21, while the Paralympic Games take place Sept. 7-18. Dr. Byington said that she hopes to be able to share preliminary study results with the public sometime in October.
CDC forecasts low chance of mosquito-borne Zika infection at Olympics
With only a few weeks left until the 2016 Olympic Games get underway in Rio de Janeiro, officials at the Centers for Disease Control and Prevention are urging anyone traveling to the Olympics to take precautions to avoid contracting Zika virus infection or spreading it when they return home.
But the CDC estimates that there is a low probability of mosquito-borne Zika virus infections during the Olympics because Rio will be experiencing cooler, drier weather then, which typically reduces the mosquito population.
Along with lower mosquito activity, the CDC said that the number of visitors expected in Brazil for the Olympics represents only a fraction of the total travel volume to Zika-affected countries during 2015. The Brazilian Tourism Board is expecting anywhere between 350,000 and 500,000 visitors for the Olympic Games, coming from 207 countries. That represents less than 0.25% of the total travel volume to Zika-affected countries during the entirety of 2015, according to the CDC.
There are 19 countries that the CDC deems susceptible to sustained mosquito-borne transmission of the Zika virus, should the virus enter the country via an attendee of the Olympics (MMWR. 2016 Jul 13. doi: 10.15585/mmwr.mm6528e1).
Of these 19 – none of which are currently experiencing a Zika outbreak – 15 are “not estimated to increase substantially the level of risk above that incurred by the usual aviation travel baseline for these countries.” This leaves Chad, Djibouti, Eritrea, and Yemen at an elevated risk for a Zika outbreak. These four countries “are unique in that they do not have a substantial number of travelers to any country with local Zika virus transmission, except for anticipated travel to the Games,” according to the CDC.
The CDC is urging travelers to take protective measures for their entire stay in Rio and for at least 3 weeks after returning home. The measures include applying mosquito repellent, wearing long-sleeved shirts and long pants, staying in rooms that are air conditioned, and using either screen doors or a mosquito net for additional protection. Additionally, all travelers should take measures to prevent sexual transmission. The CDC continues to advise pregnant women not to travel to the Olympics.
With only a few weeks left until the 2016 Olympic Games get underway in Rio de Janeiro, officials at the Centers for Disease Control and Prevention are urging anyone traveling to the Olympics to take precautions to avoid contracting Zika virus infection or spreading it when they return home.
But the CDC estimates that there is a low probability of mosquito-borne Zika virus infections during the Olympics because Rio will be experiencing cooler, drier weather then, which typically reduces the mosquito population.
Along with lower mosquito activity, the CDC said that the number of visitors expected in Brazil for the Olympics represents only a fraction of the total travel volume to Zika-affected countries during 2015. The Brazilian Tourism Board is expecting anywhere between 350,000 and 500,000 visitors for the Olympic Games, coming from 207 countries. That represents less than 0.25% of the total travel volume to Zika-affected countries during the entirety of 2015, according to the CDC.
There are 19 countries that the CDC deems susceptible to sustained mosquito-borne transmission of the Zika virus, should the virus enter the country via an attendee of the Olympics (MMWR. 2016 Jul 13. doi: 10.15585/mmwr.mm6528e1).
Of these 19 – none of which are currently experiencing a Zika outbreak – 15 are “not estimated to increase substantially the level of risk above that incurred by the usual aviation travel baseline for these countries.” This leaves Chad, Djibouti, Eritrea, and Yemen at an elevated risk for a Zika outbreak. These four countries “are unique in that they do not have a substantial number of travelers to any country with local Zika virus transmission, except for anticipated travel to the Games,” according to the CDC.
The CDC is urging travelers to take protective measures for their entire stay in Rio and for at least 3 weeks after returning home. The measures include applying mosquito repellent, wearing long-sleeved shirts and long pants, staying in rooms that are air conditioned, and using either screen doors or a mosquito net for additional protection. Additionally, all travelers should take measures to prevent sexual transmission. The CDC continues to advise pregnant women not to travel to the Olympics.
With only a few weeks left until the 2016 Olympic Games get underway in Rio de Janeiro, officials at the Centers for Disease Control and Prevention are urging anyone traveling to the Olympics to take precautions to avoid contracting Zika virus infection or spreading it when they return home.
But the CDC estimates that there is a low probability of mosquito-borne Zika virus infections during the Olympics because Rio will be experiencing cooler, drier weather then, which typically reduces the mosquito population.
Along with lower mosquito activity, the CDC said that the number of visitors expected in Brazil for the Olympics represents only a fraction of the total travel volume to Zika-affected countries during 2015. The Brazilian Tourism Board is expecting anywhere between 350,000 and 500,000 visitors for the Olympic Games, coming from 207 countries. That represents less than 0.25% of the total travel volume to Zika-affected countries during the entirety of 2015, according to the CDC.
There are 19 countries that the CDC deems susceptible to sustained mosquito-borne transmission of the Zika virus, should the virus enter the country via an attendee of the Olympics (MMWR. 2016 Jul 13. doi: 10.15585/mmwr.mm6528e1).
Of these 19 – none of which are currently experiencing a Zika outbreak – 15 are “not estimated to increase substantially the level of risk above that incurred by the usual aviation travel baseline for these countries.” This leaves Chad, Djibouti, Eritrea, and Yemen at an elevated risk for a Zika outbreak. These four countries “are unique in that they do not have a substantial number of travelers to any country with local Zika virus transmission, except for anticipated travel to the Games,” according to the CDC.
The CDC is urging travelers to take protective measures for their entire stay in Rio and for at least 3 weeks after returning home. The measures include applying mosquito repellent, wearing long-sleeved shirts and long pants, staying in rooms that are air conditioned, and using either screen doors or a mosquito net for additional protection. Additionally, all travelers should take measures to prevent sexual transmission. The CDC continues to advise pregnant women not to travel to the Olympics.
FROM MMWR
Biomarkers more specific in severe EVD than in moderate disease
Biomarkers associated with severe Ebola virus disease (EVD) were more specific than were those associated with moderate EVD, in a small study, according to Dr. Anita K. McElroy and her associates.
In the study of seven (two severe, five moderate) patients with EVD, 54 biomarkers in plasma samples were analyzed to define the kinetics of inflammatory modulators. Of these, 6 had a statistically significant association with moderate disease and 17 with severe disease. The patients with severe disease had higher viremia (P = .0003). Among 16 biomarkers correlated with viremia, 11 were associated with severe disease.
The researchers noted that the interleukin-6 differences between moderate and severe disease were not statistically significant because of the small numbers of samples in the moderate group that had detectable levels; however, there is a direct association between severity and interleukin-6 levels.
“The results from this study illuminate the beneficial vs. harmful host immune responses in EVD,” the researchers concluded. “The next step is to generate testable hypotheses about these physiologic processes and evaluate them using relevant animal models.”
Find the full study in Clinical Infectious Diseases (doi: 10.1093/cid/ciw334).
Biomarkers associated with severe Ebola virus disease (EVD) were more specific than were those associated with moderate EVD, in a small study, according to Dr. Anita K. McElroy and her associates.
In the study of seven (two severe, five moderate) patients with EVD, 54 biomarkers in plasma samples were analyzed to define the kinetics of inflammatory modulators. Of these, 6 had a statistically significant association with moderate disease and 17 with severe disease. The patients with severe disease had higher viremia (P = .0003). Among 16 biomarkers correlated with viremia, 11 were associated with severe disease.
The researchers noted that the interleukin-6 differences between moderate and severe disease were not statistically significant because of the small numbers of samples in the moderate group that had detectable levels; however, there is a direct association between severity and interleukin-6 levels.
“The results from this study illuminate the beneficial vs. harmful host immune responses in EVD,” the researchers concluded. “The next step is to generate testable hypotheses about these physiologic processes and evaluate them using relevant animal models.”
Find the full study in Clinical Infectious Diseases (doi: 10.1093/cid/ciw334).
Biomarkers associated with severe Ebola virus disease (EVD) were more specific than were those associated with moderate EVD, in a small study, according to Dr. Anita K. McElroy and her associates.
In the study of seven (two severe, five moderate) patients with EVD, 54 biomarkers in plasma samples were analyzed to define the kinetics of inflammatory modulators. Of these, 6 had a statistically significant association with moderate disease and 17 with severe disease. The patients with severe disease had higher viremia (P = .0003). Among 16 biomarkers correlated with viremia, 11 were associated with severe disease.
The researchers noted that the interleukin-6 differences between moderate and severe disease were not statistically significant because of the small numbers of samples in the moderate group that had detectable levels; however, there is a direct association between severity and interleukin-6 levels.
“The results from this study illuminate the beneficial vs. harmful host immune responses in EVD,” the researchers concluded. “The next step is to generate testable hypotheses about these physiologic processes and evaluate them using relevant animal models.”
Find the full study in Clinical Infectious Diseases (doi: 10.1093/cid/ciw334).
FROM CLINICAL INFECTIOUS DISEASES