User login
Trial of ofatumumab in FL stopped early

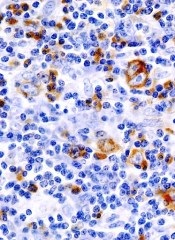
Photo courtesy of GSK
Genmab A/S said it is stopping a phase 3 trial of ofatumumab in follicular lymphoma (FL) after a planned interim analysis suggested the drug was unlikely to demonstrate superiority over rituximab.
The trial was designed to compare these 2 drugs as single-agent treatment in FL patients who had relapsed at least 6 months after completing treatment with a rituximab-containing regimen.
An interim analysis performed by an independent data monitoring committee indicated that, if the trial was to be completed as planned, it was unlikely that ofatumumab would improve progression-free survival (PFS) when compared to rituximab.
Genmab noted that this analysis did not reveal any new safety signals associated with ofatumumab, and no other ongoing trials of ofatumumab will be affected by the results of this analysis.
“The outcome of the interim analysis in this study is disappointing, as we had hoped to see superiority of ofatumumab,” said Jan van de Winkel, PhD, chief executive officer of Genmab. “The data from the study will now be prepared so that it can be presented at a future scientific conference.”
The goal of the study was to randomize up to 516 patients to receive ofatumumab (at 1000 mg) or rituximab (at 375 mg/m2) by intravenous infusion for 4 weekly doses.
Patients who had stable or responsive disease would then receive single infusions of ofatumumab or rituximab every 2 months for 4 additional doses—a total of 8 doses over 9 months. The primary endpoint of the study was PFS.
Past disappointments
This is not the first time ofatumumab has fallen short of expectations. Last year, the drug failed to meet the primary endpoint in two phase 3 trials.
In the OMB114242 trial, ofatumumab failed to improve PFS when compared to physicians’ choice in patients with bulky, fludarabine-refractory chronic lymphocytic leukemia (CLL).
In the ORCHARRD trial, ofatumumab plus chemotherapy failed to improve PFS when compared to rituximab plus chemotherapy in patients with relapsed or refractory diffuse large B-cell lymphoma.
About ofatumumab
Ofatumumab is a human monoclonal antibody designed to target the CD20 molecule found on the surface of CLL cells and normal B lymphocytes.
In the US, ofatumumab is approved for use in combination with chlorambucil to treat previously untreated patients with CLL for whom fludarabine-based therapy is considered inappropriate.
In the European Union (EU), ofatumumab is approved for use in combination with chlorambucil or bendamustine to treat patients with CLL who have not received prior therapy and who are not eligible for fludarabine-based therapy.
In more than 50 countries worldwide, including the US and EU member countries, ofatumumab is approved as monotherapy for the treatment of patients with CLL who are refractory after prior treatment with fludarabine and alemtuzumab.
Ofatumumab is marketed as Arzerra under a collaboration agreement between Genmab and Novartis (formerly GSK). ![]()

Photo courtesy of GSK
Genmab A/S said it is stopping a phase 3 trial of ofatumumab in follicular lymphoma (FL) after a planned interim analysis suggested the drug was unlikely to demonstrate superiority over rituximab.
The trial was designed to compare these 2 drugs as single-agent treatment in FL patients who had relapsed at least 6 months after completing treatment with a rituximab-containing regimen.
An interim analysis performed by an independent data monitoring committee indicated that, if the trial was to be completed as planned, it was unlikely that ofatumumab would improve progression-free survival (PFS) when compared to rituximab.
Genmab noted that this analysis did not reveal any new safety signals associated with ofatumumab, and no other ongoing trials of ofatumumab will be affected by the results of this analysis.
“The outcome of the interim analysis in this study is disappointing, as we had hoped to see superiority of ofatumumab,” said Jan van de Winkel, PhD, chief executive officer of Genmab. “The data from the study will now be prepared so that it can be presented at a future scientific conference.”
The goal of the study was to randomize up to 516 patients to receive ofatumumab (at 1000 mg) or rituximab (at 375 mg/m2) by intravenous infusion for 4 weekly doses.
Patients who had stable or responsive disease would then receive single infusions of ofatumumab or rituximab every 2 months for 4 additional doses—a total of 8 doses over 9 months. The primary endpoint of the study was PFS.
Past disappointments
This is not the first time ofatumumab has fallen short of expectations. Last year, the drug failed to meet the primary endpoint in two phase 3 trials.
In the OMB114242 trial, ofatumumab failed to improve PFS when compared to physicians’ choice in patients with bulky, fludarabine-refractory chronic lymphocytic leukemia (CLL).
In the ORCHARRD trial, ofatumumab plus chemotherapy failed to improve PFS when compared to rituximab plus chemotherapy in patients with relapsed or refractory diffuse large B-cell lymphoma.
About ofatumumab
Ofatumumab is a human monoclonal antibody designed to target the CD20 molecule found on the surface of CLL cells and normal B lymphocytes.
In the US, ofatumumab is approved for use in combination with chlorambucil to treat previously untreated patients with CLL for whom fludarabine-based therapy is considered inappropriate.
In the European Union (EU), ofatumumab is approved for use in combination with chlorambucil or bendamustine to treat patients with CLL who have not received prior therapy and who are not eligible for fludarabine-based therapy.
In more than 50 countries worldwide, including the US and EU member countries, ofatumumab is approved as monotherapy for the treatment of patients with CLL who are refractory after prior treatment with fludarabine and alemtuzumab.
Ofatumumab is marketed as Arzerra under a collaboration agreement between Genmab and Novartis (formerly GSK). ![]()

Photo courtesy of GSK
Genmab A/S said it is stopping a phase 3 trial of ofatumumab in follicular lymphoma (FL) after a planned interim analysis suggested the drug was unlikely to demonstrate superiority over rituximab.
The trial was designed to compare these 2 drugs as single-agent treatment in FL patients who had relapsed at least 6 months after completing treatment with a rituximab-containing regimen.
An interim analysis performed by an independent data monitoring committee indicated that, if the trial was to be completed as planned, it was unlikely that ofatumumab would improve progression-free survival (PFS) when compared to rituximab.
Genmab noted that this analysis did not reveal any new safety signals associated with ofatumumab, and no other ongoing trials of ofatumumab will be affected by the results of this analysis.
“The outcome of the interim analysis in this study is disappointing, as we had hoped to see superiority of ofatumumab,” said Jan van de Winkel, PhD, chief executive officer of Genmab. “The data from the study will now be prepared so that it can be presented at a future scientific conference.”
The goal of the study was to randomize up to 516 patients to receive ofatumumab (at 1000 mg) or rituximab (at 375 mg/m2) by intravenous infusion for 4 weekly doses.
Patients who had stable or responsive disease would then receive single infusions of ofatumumab or rituximab every 2 months for 4 additional doses—a total of 8 doses over 9 months. The primary endpoint of the study was PFS.
Past disappointments
This is not the first time ofatumumab has fallen short of expectations. Last year, the drug failed to meet the primary endpoint in two phase 3 trials.
In the OMB114242 trial, ofatumumab failed to improve PFS when compared to physicians’ choice in patients with bulky, fludarabine-refractory chronic lymphocytic leukemia (CLL).
In the ORCHARRD trial, ofatumumab plus chemotherapy failed to improve PFS when compared to rituximab plus chemotherapy in patients with relapsed or refractory diffuse large B-cell lymphoma.
About ofatumumab
Ofatumumab is a human monoclonal antibody designed to target the CD20 molecule found on the surface of CLL cells and normal B lymphocytes.
In the US, ofatumumab is approved for use in combination with chlorambucil to treat previously untreated patients with CLL for whom fludarabine-based therapy is considered inappropriate.
In the European Union (EU), ofatumumab is approved for use in combination with chlorambucil or bendamustine to treat patients with CLL who have not received prior therapy and who are not eligible for fludarabine-based therapy.
In more than 50 countries worldwide, including the US and EU member countries, ofatumumab is approved as monotherapy for the treatment of patients with CLL who are refractory after prior treatment with fludarabine and alemtuzumab.
Ofatumumab is marketed as Arzerra under a collaboration agreement between Genmab and Novartis (formerly GSK). ![]()
Companies abuse orphan drug designation, team says

Photo by Steven Harbour
Health experts are calling on US lawmakers and regulators to “close loopholes” in the Orphan Drug Act.
The experts say the loopholes can provide pharmaceutical companies with millions of dollars in unintended subsidies and tax breaks and fuel skyrocketing medication costs.
They argue that companies are exploiting gaps in the law by claiming orphan status for drugs that end up being marketed for more common conditions.
“The industry has been gaming the system by slicing and dicing indications so that drugs qualify for lucrative orphan status benefits,” says Martin Makary, MD, of Johns Hopkins Hospital in Baltimore, Maryland.
“As a result, funding support intended for rare disease medicine is diverted to fund the development of blockbuster drugs.”
Dr Makary and his colleagues express this viewpoint in a commentary published in the American Journal of Clinical Oncology.
The US Food and Drug Administration (FDA) grants orphan designation to encourage the development of drugs for diseases that affect fewer than 200,000 people in the US. The Orphan Drug Act was enacted in 1983 to provide incentives for drug companies to develop treatments for so-called orphan diseases that would be unprofitable because of the limited market.
Dr Makary and his colleagues say the legislation has accomplished that mission and sparked the development of life-saving therapies for a range of rare disorders. However, the authors say the law has also invited abuse.
Under the terms of the act, companies can receive federal taxpayer subsidies of up to half a million dollars a year for up to 4 years per drug, large tax credits, and waivers of marketing application fees that can cost more than $2 million. In addition, the FDA can grant companies 7 years of marketing exclusivity for an orphan drug to ensure that companies recoup the costs of research and development.
Dr Makary says companies exploit the law by initially listing only a single indication for a drug’s use—one narrow enough to qualify for orphan disease benefits. After FDA approval, however, some such drugs are marketed and used off-label more broadly, thus turning large profits.
“This is a financially toxic practice that is also unethical,” says study author Michael Daniel, also of Johns Hopkins.
“It’s time to ensure that we also render it illegal. The practice inflates drug prices, and the costs are passed on to consumers in the form of higher health insurance premiums.”
For example, the drug rituximab was originally approved to treat follicular B-cell non-Hodgkin lymphoma, a disease that affects about 14,000 patients a year. Now, rituximab is also used to treat several other types of cancer, organ rejection following kidney transplant, and autoimmune diseases, including rheumatoid arthritis, which affects 1.3 million Americans.
Rituximab, marketed under several trade names, is the top-selling medication approved as an orphan drug, the 12th all-time drug best-seller in the US, and it generated $3.7 billion in domestic sales in 2014.
In fact, 7 of the top 10 best-selling drugs in the US for 2014 came on the market with an orphan designation, according to Dr Makary and his colleagues.
Of the 41 drugs approved by the FDA in 2014, 18 had orphan status designations. The authors predict that, in 2015, orphan drugs will generate sales totaling $107 billion. And that number is expected to reach $176 billion by 2020.
Dr Makary says this projection represents a yearly growth rate of nearly 11%, or double the growth rate of the overall prescription drug market. The authors also cite data showing that, by 2020, orphan drugs are expected to account for 19% of global prescription drug sales, up from 6% in the year 2000.
Although the reasons for this boom in orphan drugs are likely multifactorial, the exploitation of the orphan drug act is an important catalyst behind this trend, the authors say.
Because orphan designation guarantees a 7-year exclusivity deal to market the drug and protects it from generic competition, the price tags for such medications often balloon rapidly.
For example, the drug imatinib was initially priced at $30,000 per year in 2001. By 2012, it cost $92,000 a year.
The drug’s original designation was for chronic myelogenous leukemia, and it would therefore treat 9000 patients a year in the US. Subsequently, imatinib was given 6 additional orphan designations for various conditions, including gastric cancers and immune disorders.
Dr Makary says, in essence, the exclusivity clause guarantees a hyperextended government-sponsored monopoly. So it’s not surprising that the median cost for orphan drugs is more than $98,000 per patient per year, compared with a median cost of just over $5000 per patient per year for drugs without orphan status.
Overall, nearly 15% of already approved orphan drugs subsequently add far more common diseases to their treatment repertoires.
Dr Makary and his colleagues recommend that, once a drug exceeds the basic tenets of the act—to treat fewer than 200,000 people—it should no longer receive government support or marketing exclusivity.
This can be achieved, the authors say, through pricing negotiations, clauses that reduce marketing exclusivity, and leveling of taxes once a medication becomes a blockbuster treatment for conditions not listed in the original FDA approval.
They say such measures would ensure the spirit of the original act is followed while continuing to provide critical economic incentives for truly rare diseases. ![]()

Photo by Steven Harbour
Health experts are calling on US lawmakers and regulators to “close loopholes” in the Orphan Drug Act.
The experts say the loopholes can provide pharmaceutical companies with millions of dollars in unintended subsidies and tax breaks and fuel skyrocketing medication costs.
They argue that companies are exploiting gaps in the law by claiming orphan status for drugs that end up being marketed for more common conditions.
“The industry has been gaming the system by slicing and dicing indications so that drugs qualify for lucrative orphan status benefits,” says Martin Makary, MD, of Johns Hopkins Hospital in Baltimore, Maryland.
“As a result, funding support intended for rare disease medicine is diverted to fund the development of blockbuster drugs.”
Dr Makary and his colleagues express this viewpoint in a commentary published in the American Journal of Clinical Oncology.
The US Food and Drug Administration (FDA) grants orphan designation to encourage the development of drugs for diseases that affect fewer than 200,000 people in the US. The Orphan Drug Act was enacted in 1983 to provide incentives for drug companies to develop treatments for so-called orphan diseases that would be unprofitable because of the limited market.
Dr Makary and his colleagues say the legislation has accomplished that mission and sparked the development of life-saving therapies for a range of rare disorders. However, the authors say the law has also invited abuse.
Under the terms of the act, companies can receive federal taxpayer subsidies of up to half a million dollars a year for up to 4 years per drug, large tax credits, and waivers of marketing application fees that can cost more than $2 million. In addition, the FDA can grant companies 7 years of marketing exclusivity for an orphan drug to ensure that companies recoup the costs of research and development.
Dr Makary says companies exploit the law by initially listing only a single indication for a drug’s use—one narrow enough to qualify for orphan disease benefits. After FDA approval, however, some such drugs are marketed and used off-label more broadly, thus turning large profits.
“This is a financially toxic practice that is also unethical,” says study author Michael Daniel, also of Johns Hopkins.
“It’s time to ensure that we also render it illegal. The practice inflates drug prices, and the costs are passed on to consumers in the form of higher health insurance premiums.”
For example, the drug rituximab was originally approved to treat follicular B-cell non-Hodgkin lymphoma, a disease that affects about 14,000 patients a year. Now, rituximab is also used to treat several other types of cancer, organ rejection following kidney transplant, and autoimmune diseases, including rheumatoid arthritis, which affects 1.3 million Americans.
Rituximab, marketed under several trade names, is the top-selling medication approved as an orphan drug, the 12th all-time drug best-seller in the US, and it generated $3.7 billion in domestic sales in 2014.
In fact, 7 of the top 10 best-selling drugs in the US for 2014 came on the market with an orphan designation, according to Dr Makary and his colleagues.
Of the 41 drugs approved by the FDA in 2014, 18 had orphan status designations. The authors predict that, in 2015, orphan drugs will generate sales totaling $107 billion. And that number is expected to reach $176 billion by 2020.
Dr Makary says this projection represents a yearly growth rate of nearly 11%, or double the growth rate of the overall prescription drug market. The authors also cite data showing that, by 2020, orphan drugs are expected to account for 19% of global prescription drug sales, up from 6% in the year 2000.
Although the reasons for this boom in orphan drugs are likely multifactorial, the exploitation of the orphan drug act is an important catalyst behind this trend, the authors say.
Because orphan designation guarantees a 7-year exclusivity deal to market the drug and protects it from generic competition, the price tags for such medications often balloon rapidly.
For example, the drug imatinib was initially priced at $30,000 per year in 2001. By 2012, it cost $92,000 a year.
The drug’s original designation was for chronic myelogenous leukemia, and it would therefore treat 9000 patients a year in the US. Subsequently, imatinib was given 6 additional orphan designations for various conditions, including gastric cancers and immune disorders.
Dr Makary says, in essence, the exclusivity clause guarantees a hyperextended government-sponsored monopoly. So it’s not surprising that the median cost for orphan drugs is more than $98,000 per patient per year, compared with a median cost of just over $5000 per patient per year for drugs without orphan status.
Overall, nearly 15% of already approved orphan drugs subsequently add far more common diseases to their treatment repertoires.
Dr Makary and his colleagues recommend that, once a drug exceeds the basic tenets of the act—to treat fewer than 200,000 people—it should no longer receive government support or marketing exclusivity.
This can be achieved, the authors say, through pricing negotiations, clauses that reduce marketing exclusivity, and leveling of taxes once a medication becomes a blockbuster treatment for conditions not listed in the original FDA approval.
They say such measures would ensure the spirit of the original act is followed while continuing to provide critical economic incentives for truly rare diseases. ![]()

Photo by Steven Harbour
Health experts are calling on US lawmakers and regulators to “close loopholes” in the Orphan Drug Act.
The experts say the loopholes can provide pharmaceutical companies with millions of dollars in unintended subsidies and tax breaks and fuel skyrocketing medication costs.
They argue that companies are exploiting gaps in the law by claiming orphan status for drugs that end up being marketed for more common conditions.
“The industry has been gaming the system by slicing and dicing indications so that drugs qualify for lucrative orphan status benefits,” says Martin Makary, MD, of Johns Hopkins Hospital in Baltimore, Maryland.
“As a result, funding support intended for rare disease medicine is diverted to fund the development of blockbuster drugs.”
Dr Makary and his colleagues express this viewpoint in a commentary published in the American Journal of Clinical Oncology.
The US Food and Drug Administration (FDA) grants orphan designation to encourage the development of drugs for diseases that affect fewer than 200,000 people in the US. The Orphan Drug Act was enacted in 1983 to provide incentives for drug companies to develop treatments for so-called orphan diseases that would be unprofitable because of the limited market.
Dr Makary and his colleagues say the legislation has accomplished that mission and sparked the development of life-saving therapies for a range of rare disorders. However, the authors say the law has also invited abuse.
Under the terms of the act, companies can receive federal taxpayer subsidies of up to half a million dollars a year for up to 4 years per drug, large tax credits, and waivers of marketing application fees that can cost more than $2 million. In addition, the FDA can grant companies 7 years of marketing exclusivity for an orphan drug to ensure that companies recoup the costs of research and development.
Dr Makary says companies exploit the law by initially listing only a single indication for a drug’s use—one narrow enough to qualify for orphan disease benefits. After FDA approval, however, some such drugs are marketed and used off-label more broadly, thus turning large profits.
“This is a financially toxic practice that is also unethical,” says study author Michael Daniel, also of Johns Hopkins.
“It’s time to ensure that we also render it illegal. The practice inflates drug prices, and the costs are passed on to consumers in the form of higher health insurance premiums.”
For example, the drug rituximab was originally approved to treat follicular B-cell non-Hodgkin lymphoma, a disease that affects about 14,000 patients a year. Now, rituximab is also used to treat several other types of cancer, organ rejection following kidney transplant, and autoimmune diseases, including rheumatoid arthritis, which affects 1.3 million Americans.
Rituximab, marketed under several trade names, is the top-selling medication approved as an orphan drug, the 12th all-time drug best-seller in the US, and it generated $3.7 billion in domestic sales in 2014.
In fact, 7 of the top 10 best-selling drugs in the US for 2014 came on the market with an orphan designation, according to Dr Makary and his colleagues.
Of the 41 drugs approved by the FDA in 2014, 18 had orphan status designations. The authors predict that, in 2015, orphan drugs will generate sales totaling $107 billion. And that number is expected to reach $176 billion by 2020.
Dr Makary says this projection represents a yearly growth rate of nearly 11%, or double the growth rate of the overall prescription drug market. The authors also cite data showing that, by 2020, orphan drugs are expected to account for 19% of global prescription drug sales, up from 6% in the year 2000.
Although the reasons for this boom in orphan drugs are likely multifactorial, the exploitation of the orphan drug act is an important catalyst behind this trend, the authors say.
Because orphan designation guarantees a 7-year exclusivity deal to market the drug and protects it from generic competition, the price tags for such medications often balloon rapidly.
For example, the drug imatinib was initially priced at $30,000 per year in 2001. By 2012, it cost $92,000 a year.
The drug’s original designation was for chronic myelogenous leukemia, and it would therefore treat 9000 patients a year in the US. Subsequently, imatinib was given 6 additional orphan designations for various conditions, including gastric cancers and immune disorders.
Dr Makary says, in essence, the exclusivity clause guarantees a hyperextended government-sponsored monopoly. So it’s not surprising that the median cost for orphan drugs is more than $98,000 per patient per year, compared with a median cost of just over $5000 per patient per year for drugs without orphan status.
Overall, nearly 15% of already approved orphan drugs subsequently add far more common diseases to their treatment repertoires.
Dr Makary and his colleagues recommend that, once a drug exceeds the basic tenets of the act—to treat fewer than 200,000 people—it should no longer receive government support or marketing exclusivity.
This can be achieved, the authors say, through pricing negotiations, clauses that reduce marketing exclusivity, and leveling of taxes once a medication becomes a blockbuster treatment for conditions not listed in the original FDA approval.
They say such measures would ensure the spirit of the original act is followed while continuing to provide critical economic incentives for truly rare diseases. ![]()
Inhibitor exhibits ‘modest’ activity in lymphoma
A small-molecule inhibitor has shown modest anticancer activity in a phase 1 trial of patients with relapsed/refractory lymphoma or multiple myeloma (MM), according to an investigator involved in the study.
A majority of patients who recieved the drug, pevonedistat, achieved stable disease, and a few patients with lymphoma experienced partial responses.
Investigators said pevonedistat could be given safely, although 100% of patients experienced adverse events (AEs), and a majority experienced grade 3 or higher AEs.
“The most important findings from our study are that pevonedistat hits its target in cancer cells in patients, can be given safely, and has modest activity in heavily pretreated patients with relapsed/refractory lymphoma, suggesting that we are on the right path,” said Jatin J. Shah, MD, of The University of Texas MD Anderson Cancer Center in Houston.
Dr Shah and his colleagues reported these findings in Clinical Cancer Research. The trial was sponsored by Millennium Pharmaceuticals, Inc., the company developing pevonedistat.
Pevonedistat is a first-in-class, investigational, small-molecule inhibitor of the NEDD8-activating enzyme.
“This enzyme is part of the ubiquitin-proteasome system, which is the target of a number of FDA-approved anticancer therapeutics, including bortezomib . . . ,” Dr Shah explained. “Pevonedistat also alters the ability of cancer cells to repair damaged DNA.”
Patient and treatment characteristics
Dr Shah and his colleagues enrolled 44 patients on this trial. Seventeen patients had relapsed/refractory MM, and 27 had relapsed/refractory lymphoma.
The types of lymphoma were diffuse large B-cell lymphoma (n=10), follicular lymphoma (n=5), Hodgkin lymphoma (n=5), small lymphocytic lymphoma/chronic lymphocytic leukemia (n=2), mantle cell lymphoma (n=1), lymphoplasmacytic lymphoma (n=1), peripheral T-cell lymphoma (n=1), splenic marginal zone B-cell lymphoma (n=1), and “other” (n=1).
Twenty-seven patients received escalating doses of pevonedistat on schedule A, which was days 1, 2, 8, and 9 of a 21-day cycle, and 17 patients received escalating doses of the drug on schedule B, which was days 1, 4, 8, and 11 of a 21-day cycle.
Safety
The maximum tolerated doses were 110 mg/m2 and 196 mg/m2 on schedule A and B, respectively. The dose-limiting toxicities were febrile neutropenia, transaminase elevations, and muscle cramps on schedule A, and thrombocytopenia on schedule B.
On schedule A, 100% of patients experienced AEs, and 59% had AEs of grade 3 or higher. The grade 3 or higher AEs were anemia (19%), thrombocytopenia (4%), neutropenia (7%), fatigue (7%), ALT increase (4%), AST increase (7%), diarrhea (4%), pain (4%), dyspnea (4%), hypercalcemia (7%), hypophosphatemia (11%), hyperkalemia (4%), muscle spasms (4%), abdominal discomfort (4%), and pneumonia (4%).
On schedule B, 100% of patients experienced AEs, and 71% had grade 3 or higher AEs. The grade 3 or higher AEs were anemia (6%), thrombocytopenia (6%), neutropenia (12%), fatigue (6%), ALT increase (6%), pyrexia (6%), pain (6%), dyspnea (6%), hypophosphatemia (6%), muscle spasms (6%), upper respiratory tract infection (6%), dehydration (6%), hyperbilirubinemia (6%), and pneumonia (12%).
Efficacy
Three patients had a partial response to treatment, including 1 patient with relapsed nodular sclerosis Hodgkin lymphoma, 1 with relapsed diffuse large B-cell lymphoma, and 1 with relapsed peripheral T-cell lymphoma.
Another 30 patients, 17 with lymphoma and 13 with MM, had stable disease.
“Although pevonedistat had modest activity as a single-agent treatment, we expect greater activity when it is given in combination with standard therapy,” Dr Shah said.
“The pharmacodynamics data showed that pevonedistat hit its target in cancer cells in patients at low doses. This is important because it may mean that we do not need to escalate the dose in future trials to increase anticancer activity. This has the potential to increase the risk-benefit ratio of pevonedistat.”
Dr Shah said a limitation of this study is that it included a small number of patients, all of whom were very heavily pretreated, which may limit assessment of how active pevonedistat could be. ![]()
A small-molecule inhibitor has shown modest anticancer activity in a phase 1 trial of patients with relapsed/refractory lymphoma or multiple myeloma (MM), according to an investigator involved in the study.
A majority of patients who recieved the drug, pevonedistat, achieved stable disease, and a few patients with lymphoma experienced partial responses.
Investigators said pevonedistat could be given safely, although 100% of patients experienced adverse events (AEs), and a majority experienced grade 3 or higher AEs.
“The most important findings from our study are that pevonedistat hits its target in cancer cells in patients, can be given safely, and has modest activity in heavily pretreated patients with relapsed/refractory lymphoma, suggesting that we are on the right path,” said Jatin J. Shah, MD, of The University of Texas MD Anderson Cancer Center in Houston.
Dr Shah and his colleagues reported these findings in Clinical Cancer Research. The trial was sponsored by Millennium Pharmaceuticals, Inc., the company developing pevonedistat.
Pevonedistat is a first-in-class, investigational, small-molecule inhibitor of the NEDD8-activating enzyme.
“This enzyme is part of the ubiquitin-proteasome system, which is the target of a number of FDA-approved anticancer therapeutics, including bortezomib . . . ,” Dr Shah explained. “Pevonedistat also alters the ability of cancer cells to repair damaged DNA.”
Patient and treatment characteristics
Dr Shah and his colleagues enrolled 44 patients on this trial. Seventeen patients had relapsed/refractory MM, and 27 had relapsed/refractory lymphoma.
The types of lymphoma were diffuse large B-cell lymphoma (n=10), follicular lymphoma (n=5), Hodgkin lymphoma (n=5), small lymphocytic lymphoma/chronic lymphocytic leukemia (n=2), mantle cell lymphoma (n=1), lymphoplasmacytic lymphoma (n=1), peripheral T-cell lymphoma (n=1), splenic marginal zone B-cell lymphoma (n=1), and “other” (n=1).
Twenty-seven patients received escalating doses of pevonedistat on schedule A, which was days 1, 2, 8, and 9 of a 21-day cycle, and 17 patients received escalating doses of the drug on schedule B, which was days 1, 4, 8, and 11 of a 21-day cycle.
Safety
The maximum tolerated doses were 110 mg/m2 and 196 mg/m2 on schedule A and B, respectively. The dose-limiting toxicities were febrile neutropenia, transaminase elevations, and muscle cramps on schedule A, and thrombocytopenia on schedule B.
On schedule A, 100% of patients experienced AEs, and 59% had AEs of grade 3 or higher. The grade 3 or higher AEs were anemia (19%), thrombocytopenia (4%), neutropenia (7%), fatigue (7%), ALT increase (4%), AST increase (7%), diarrhea (4%), pain (4%), dyspnea (4%), hypercalcemia (7%), hypophosphatemia (11%), hyperkalemia (4%), muscle spasms (4%), abdominal discomfort (4%), and pneumonia (4%).
On schedule B, 100% of patients experienced AEs, and 71% had grade 3 or higher AEs. The grade 3 or higher AEs were anemia (6%), thrombocytopenia (6%), neutropenia (12%), fatigue (6%), ALT increase (6%), pyrexia (6%), pain (6%), dyspnea (6%), hypophosphatemia (6%), muscle spasms (6%), upper respiratory tract infection (6%), dehydration (6%), hyperbilirubinemia (6%), and pneumonia (12%).
Efficacy
Three patients had a partial response to treatment, including 1 patient with relapsed nodular sclerosis Hodgkin lymphoma, 1 with relapsed diffuse large B-cell lymphoma, and 1 with relapsed peripheral T-cell lymphoma.
Another 30 patients, 17 with lymphoma and 13 with MM, had stable disease.
“Although pevonedistat had modest activity as a single-agent treatment, we expect greater activity when it is given in combination with standard therapy,” Dr Shah said.
“The pharmacodynamics data showed that pevonedistat hit its target in cancer cells in patients at low doses. This is important because it may mean that we do not need to escalate the dose in future trials to increase anticancer activity. This has the potential to increase the risk-benefit ratio of pevonedistat.”
Dr Shah said a limitation of this study is that it included a small number of patients, all of whom were very heavily pretreated, which may limit assessment of how active pevonedistat could be. ![]()
A small-molecule inhibitor has shown modest anticancer activity in a phase 1 trial of patients with relapsed/refractory lymphoma or multiple myeloma (MM), according to an investigator involved in the study.
A majority of patients who recieved the drug, pevonedistat, achieved stable disease, and a few patients with lymphoma experienced partial responses.
Investigators said pevonedistat could be given safely, although 100% of patients experienced adverse events (AEs), and a majority experienced grade 3 or higher AEs.
“The most important findings from our study are that pevonedistat hits its target in cancer cells in patients, can be given safely, and has modest activity in heavily pretreated patients with relapsed/refractory lymphoma, suggesting that we are on the right path,” said Jatin J. Shah, MD, of The University of Texas MD Anderson Cancer Center in Houston.
Dr Shah and his colleagues reported these findings in Clinical Cancer Research. The trial was sponsored by Millennium Pharmaceuticals, Inc., the company developing pevonedistat.
Pevonedistat is a first-in-class, investigational, small-molecule inhibitor of the NEDD8-activating enzyme.
“This enzyme is part of the ubiquitin-proteasome system, which is the target of a number of FDA-approved anticancer therapeutics, including bortezomib . . . ,” Dr Shah explained. “Pevonedistat also alters the ability of cancer cells to repair damaged DNA.”
Patient and treatment characteristics
Dr Shah and his colleagues enrolled 44 patients on this trial. Seventeen patients had relapsed/refractory MM, and 27 had relapsed/refractory lymphoma.
The types of lymphoma were diffuse large B-cell lymphoma (n=10), follicular lymphoma (n=5), Hodgkin lymphoma (n=5), small lymphocytic lymphoma/chronic lymphocytic leukemia (n=2), mantle cell lymphoma (n=1), lymphoplasmacytic lymphoma (n=1), peripheral T-cell lymphoma (n=1), splenic marginal zone B-cell lymphoma (n=1), and “other” (n=1).
Twenty-seven patients received escalating doses of pevonedistat on schedule A, which was days 1, 2, 8, and 9 of a 21-day cycle, and 17 patients received escalating doses of the drug on schedule B, which was days 1, 4, 8, and 11 of a 21-day cycle.
Safety
The maximum tolerated doses were 110 mg/m2 and 196 mg/m2 on schedule A and B, respectively. The dose-limiting toxicities were febrile neutropenia, transaminase elevations, and muscle cramps on schedule A, and thrombocytopenia on schedule B.
On schedule A, 100% of patients experienced AEs, and 59% had AEs of grade 3 or higher. The grade 3 or higher AEs were anemia (19%), thrombocytopenia (4%), neutropenia (7%), fatigue (7%), ALT increase (4%), AST increase (7%), diarrhea (4%), pain (4%), dyspnea (4%), hypercalcemia (7%), hypophosphatemia (11%), hyperkalemia (4%), muscle spasms (4%), abdominal discomfort (4%), and pneumonia (4%).
On schedule B, 100% of patients experienced AEs, and 71% had grade 3 or higher AEs. The grade 3 or higher AEs were anemia (6%), thrombocytopenia (6%), neutropenia (12%), fatigue (6%), ALT increase (6%), pyrexia (6%), pain (6%), dyspnea (6%), hypophosphatemia (6%), muscle spasms (6%), upper respiratory tract infection (6%), dehydration (6%), hyperbilirubinemia (6%), and pneumonia (12%).
Efficacy
Three patients had a partial response to treatment, including 1 patient with relapsed nodular sclerosis Hodgkin lymphoma, 1 with relapsed diffuse large B-cell lymphoma, and 1 with relapsed peripheral T-cell lymphoma.
Another 30 patients, 17 with lymphoma and 13 with MM, had stable disease.
“Although pevonedistat had modest activity as a single-agent treatment, we expect greater activity when it is given in combination with standard therapy,” Dr Shah said.
“The pharmacodynamics data showed that pevonedistat hit its target in cancer cells in patients at low doses. This is important because it may mean that we do not need to escalate the dose in future trials to increase anticancer activity. This has the potential to increase the risk-benefit ratio of pevonedistat.”
Dr Shah said a limitation of this study is that it included a small number of patients, all of whom were very heavily pretreated, which may limit assessment of how active pevonedistat could be. ![]()
Drug ‘life-changing’ for CLL patients in phase 1 trial

Photo courtesy of NIH
A novel Bruton’s tyrosine kinase inhibitor has proven life-changing for patients with chronic lymphocytic leukemia (CLL) who received the drug as part of a phase 1 trial, according to the study’s lead author.
The inhibitor, ONO/GS-4059, produced a response in 96% of evaluable CLL patients.
Most CLL patients are still on the study after 3 years, although a handful withdrew due to adverse events (AEs) or disease progression.
“These patients were confronted with a cruel reality: they had failed multiple chemotherapy lines, and there were no other treatment options available for them,” said lead study author Harriet Walter, MBChB, of the University of Leicester in the UK.
“This drug has changed their lives. From desperate and tired, they are now leading a normal and really active life. This is hugely rewarding and encouraging.”
Dr Walter and her colleagues reported these results in Blood. The trial was funded by ONO Pharmaceuticals, the company developing ONO/GS-4059.
This study opened in January 2012, and 90 patients were enrolled at centers in the UK and France. There were 28 patients with CLL and 62 with non-Hodgkin lymphoma (NHL), including 16 with mantle cell lymphoma (MCL) and 35 with diffuse large B-cell lymphoma (DLBCL).
The study also included patients with follicular lymphoma, marginal zone lymphoma, small lymphocytic lymphoma, and Waldenstrom’s macroglobulinemia, but patient numbers were small for these groups, so the results were not discussed in detail.
There were 9 dose-escalation cohorts in this study. ONO/GS-4059 was given once-daily at doses ranging from 20 mg to 600 mg. Or the drug was given twice daily at doses of 240 mg or 300 mg.
Results
The maximum tolerated dose was not reached in the CLL cohort, but it was 480 mg once-daily in the NHL cohort. Four NHL patients had a dose-limiting toxicity.
In the CLL cohort, 2 patients went off study due to progression and 5 due to AEs.
In the NHL cohort, 49 patients discontinued treatment, 32 due to progression and 5 due to dose-limiting toxicities or AEs. The other 12 NHL patients discontinued due to patient or investigator decision, proceeding to transplant (n=1), or death due to progressive disease.
The median duration of follow-up was 560 days for CLL patients, 309 days for MCL patients, and 60 days for DLBCL patients.
The overall estimated mean progression-free survival was 874 days for CLL patients, 341 days for MCL patients, and 54 days for DLBCL patients.
CLL patients
Of all 28 CLL patients, 16 had relapsed CLL, 11 had refractory disease, and 1 had unknown status. The median number of prior therapies was 3.5 (range, 2-7).
Twenty-five patients were evaluable. Of the 3 who were not evaluable, 1 had not reached cycle 3 disease assessment at the time of data analysis, 1 progressed during cycle 1, and 1 was withdrawn due to an AE (idiopathic thrombocytopenia).
Of the 25 evaluable patients, 24 (96%) responded to ONO/GS-4059. The researchers said they observed rapid resolution of bulky lymphadenopathy within the first 3 months of treatment, but improvement in lymphadenopathy continued for up to 18 months in most patients.
The median treatment duration for these patients is 80 weeks, and 21 patients are still on treatment. Two of the evaluable patients progressed during therapy, one at cycle 3 and one at cycle 12.
MCL patients
Of the 16 MCL patients enrolled, 7 were refractory to their last course of immuno-chemotherapy. The median number of prior therapies was 3 (range, 2-7).
Eleven of 12 (92%) evaluable patients with MCL responded to ONO/GS-4059. Six patients had a partial response, and 5 had a complete response (CR) or unconfirmed CR.
Three patients progressed after an initial response. Four patients were not evaluable because they progressed.
The median treatment duration for MCL patients is 40 weeks, and 8 patients remain on study.
DLBCL patients
All 35 DLBCL patients had relapsed or refractory disease. The median number of prior treatments was 3
(range, 2-10), and 30 patients were refractory to their last line of chemotherapy.
Eleven of 31 (35%) patients with non-germinal center B-cell (non-GCB) DLBCL responded to ONO/GS-4059. Two non-GCB DLBCL patients had a confirmed CR, 1 had an unconfirmed CR, and the rest had partial responses.
The median duration of response was 54 days. And, among responders, the median treatment duration was 12 weeks.
The majority of non-GCB DLBCL patients progressed. There were no responses among the 2 patients with GCB DLBCL, and there were no responses among patients with primary mediastinal B-cell lymphoma or plasmablastic DLBCL.
Toxicity
AEs in this study were mostly grade 1/2—75% in the CLL cohort and 50% in the NHL cohort. However, treatment-related grade 3/4 AEs occurred in 14.3% of CLL patients and 16.1% of NHL patients.
Grade 3/4 events were mainly hematologic in nature and included neutropenia (10%), anemia (13.3%), and thrombocytopenia (13.3%).
There was a grade 3 episode of drug-related hemorrhage in a CLL patient, which resulted in a psoas hematoma (with concomitant CLL progression) in the presence of a normal platelet count. This patient was among those taken off the study.
“The next step is now to see how best we can improve on these outstanding results,” said study author Martin Dyer, DPhil, of the University of Leicester.
“A further study using this drug in combination with additional targeted agents is shortly to open in Leicester with the aim of achieving cure. In parallel with the clinical development of the drug, our team of scientists at the Haematological Research Institute are studying how this drug is working and how to overcome potential resistance.” ![]()

Photo courtesy of NIH
A novel Bruton’s tyrosine kinase inhibitor has proven life-changing for patients with chronic lymphocytic leukemia (CLL) who received the drug as part of a phase 1 trial, according to the study’s lead author.
The inhibitor, ONO/GS-4059, produced a response in 96% of evaluable CLL patients.
Most CLL patients are still on the study after 3 years, although a handful withdrew due to adverse events (AEs) or disease progression.
“These patients were confronted with a cruel reality: they had failed multiple chemotherapy lines, and there were no other treatment options available for them,” said lead study author Harriet Walter, MBChB, of the University of Leicester in the UK.
“This drug has changed their lives. From desperate and tired, they are now leading a normal and really active life. This is hugely rewarding and encouraging.”
Dr Walter and her colleagues reported these results in Blood. The trial was funded by ONO Pharmaceuticals, the company developing ONO/GS-4059.
This study opened in January 2012, and 90 patients were enrolled at centers in the UK and France. There were 28 patients with CLL and 62 with non-Hodgkin lymphoma (NHL), including 16 with mantle cell lymphoma (MCL) and 35 with diffuse large B-cell lymphoma (DLBCL).
The study also included patients with follicular lymphoma, marginal zone lymphoma, small lymphocytic lymphoma, and Waldenstrom’s macroglobulinemia, but patient numbers were small for these groups, so the results were not discussed in detail.
There were 9 dose-escalation cohorts in this study. ONO/GS-4059 was given once-daily at doses ranging from 20 mg to 600 mg. Or the drug was given twice daily at doses of 240 mg or 300 mg.
Results
The maximum tolerated dose was not reached in the CLL cohort, but it was 480 mg once-daily in the NHL cohort. Four NHL patients had a dose-limiting toxicity.
In the CLL cohort, 2 patients went off study due to progression and 5 due to AEs.
In the NHL cohort, 49 patients discontinued treatment, 32 due to progression and 5 due to dose-limiting toxicities or AEs. The other 12 NHL patients discontinued due to patient or investigator decision, proceeding to transplant (n=1), or death due to progressive disease.
The median duration of follow-up was 560 days for CLL patients, 309 days for MCL patients, and 60 days for DLBCL patients.
The overall estimated mean progression-free survival was 874 days for CLL patients, 341 days for MCL patients, and 54 days for DLBCL patients.
CLL patients
Of all 28 CLL patients, 16 had relapsed CLL, 11 had refractory disease, and 1 had unknown status. The median number of prior therapies was 3.5 (range, 2-7).
Twenty-five patients were evaluable. Of the 3 who were not evaluable, 1 had not reached cycle 3 disease assessment at the time of data analysis, 1 progressed during cycle 1, and 1 was withdrawn due to an AE (idiopathic thrombocytopenia).
Of the 25 evaluable patients, 24 (96%) responded to ONO/GS-4059. The researchers said they observed rapid resolution of bulky lymphadenopathy within the first 3 months of treatment, but improvement in lymphadenopathy continued for up to 18 months in most patients.
The median treatment duration for these patients is 80 weeks, and 21 patients are still on treatment. Two of the evaluable patients progressed during therapy, one at cycle 3 and one at cycle 12.
MCL patients
Of the 16 MCL patients enrolled, 7 were refractory to their last course of immuno-chemotherapy. The median number of prior therapies was 3 (range, 2-7).
Eleven of 12 (92%) evaluable patients with MCL responded to ONO/GS-4059. Six patients had a partial response, and 5 had a complete response (CR) or unconfirmed CR.
Three patients progressed after an initial response. Four patients were not evaluable because they progressed.
The median treatment duration for MCL patients is 40 weeks, and 8 patients remain on study.
DLBCL patients
All 35 DLBCL patients had relapsed or refractory disease. The median number of prior treatments was 3
(range, 2-10), and 30 patients were refractory to their last line of chemotherapy.
Eleven of 31 (35%) patients with non-germinal center B-cell (non-GCB) DLBCL responded to ONO/GS-4059. Two non-GCB DLBCL patients had a confirmed CR, 1 had an unconfirmed CR, and the rest had partial responses.
The median duration of response was 54 days. And, among responders, the median treatment duration was 12 weeks.
The majority of non-GCB DLBCL patients progressed. There were no responses among the 2 patients with GCB DLBCL, and there were no responses among patients with primary mediastinal B-cell lymphoma or plasmablastic DLBCL.
Toxicity
AEs in this study were mostly grade 1/2—75% in the CLL cohort and 50% in the NHL cohort. However, treatment-related grade 3/4 AEs occurred in 14.3% of CLL patients and 16.1% of NHL patients.
Grade 3/4 events were mainly hematologic in nature and included neutropenia (10%), anemia (13.3%), and thrombocytopenia (13.3%).
There was a grade 3 episode of drug-related hemorrhage in a CLL patient, which resulted in a psoas hematoma (with concomitant CLL progression) in the presence of a normal platelet count. This patient was among those taken off the study.
“The next step is now to see how best we can improve on these outstanding results,” said study author Martin Dyer, DPhil, of the University of Leicester.
“A further study using this drug in combination with additional targeted agents is shortly to open in Leicester with the aim of achieving cure. In parallel with the clinical development of the drug, our team of scientists at the Haematological Research Institute are studying how this drug is working and how to overcome potential resistance.” ![]()

Photo courtesy of NIH
A novel Bruton’s tyrosine kinase inhibitor has proven life-changing for patients with chronic lymphocytic leukemia (CLL) who received the drug as part of a phase 1 trial, according to the study’s lead author.
The inhibitor, ONO/GS-4059, produced a response in 96% of evaluable CLL patients.
Most CLL patients are still on the study after 3 years, although a handful withdrew due to adverse events (AEs) or disease progression.
“These patients were confronted with a cruel reality: they had failed multiple chemotherapy lines, and there were no other treatment options available for them,” said lead study author Harriet Walter, MBChB, of the University of Leicester in the UK.
“This drug has changed their lives. From desperate and tired, they are now leading a normal and really active life. This is hugely rewarding and encouraging.”
Dr Walter and her colleagues reported these results in Blood. The trial was funded by ONO Pharmaceuticals, the company developing ONO/GS-4059.
This study opened in January 2012, and 90 patients were enrolled at centers in the UK and France. There were 28 patients with CLL and 62 with non-Hodgkin lymphoma (NHL), including 16 with mantle cell lymphoma (MCL) and 35 with diffuse large B-cell lymphoma (DLBCL).
The study also included patients with follicular lymphoma, marginal zone lymphoma, small lymphocytic lymphoma, and Waldenstrom’s macroglobulinemia, but patient numbers were small for these groups, so the results were not discussed in detail.
There were 9 dose-escalation cohorts in this study. ONO/GS-4059 was given once-daily at doses ranging from 20 mg to 600 mg. Or the drug was given twice daily at doses of 240 mg or 300 mg.
Results
The maximum tolerated dose was not reached in the CLL cohort, but it was 480 mg once-daily in the NHL cohort. Four NHL patients had a dose-limiting toxicity.
In the CLL cohort, 2 patients went off study due to progression and 5 due to AEs.
In the NHL cohort, 49 patients discontinued treatment, 32 due to progression and 5 due to dose-limiting toxicities or AEs. The other 12 NHL patients discontinued due to patient or investigator decision, proceeding to transplant (n=1), or death due to progressive disease.
The median duration of follow-up was 560 days for CLL patients, 309 days for MCL patients, and 60 days for DLBCL patients.
The overall estimated mean progression-free survival was 874 days for CLL patients, 341 days for MCL patients, and 54 days for DLBCL patients.
CLL patients
Of all 28 CLL patients, 16 had relapsed CLL, 11 had refractory disease, and 1 had unknown status. The median number of prior therapies was 3.5 (range, 2-7).
Twenty-five patients were evaluable. Of the 3 who were not evaluable, 1 had not reached cycle 3 disease assessment at the time of data analysis, 1 progressed during cycle 1, and 1 was withdrawn due to an AE (idiopathic thrombocytopenia).
Of the 25 evaluable patients, 24 (96%) responded to ONO/GS-4059. The researchers said they observed rapid resolution of bulky lymphadenopathy within the first 3 months of treatment, but improvement in lymphadenopathy continued for up to 18 months in most patients.
The median treatment duration for these patients is 80 weeks, and 21 patients are still on treatment. Two of the evaluable patients progressed during therapy, one at cycle 3 and one at cycle 12.
MCL patients
Of the 16 MCL patients enrolled, 7 were refractory to their last course of immuno-chemotherapy. The median number of prior therapies was 3 (range, 2-7).
Eleven of 12 (92%) evaluable patients with MCL responded to ONO/GS-4059. Six patients had a partial response, and 5 had a complete response (CR) or unconfirmed CR.
Three patients progressed after an initial response. Four patients were not evaluable because they progressed.
The median treatment duration for MCL patients is 40 weeks, and 8 patients remain on study.
DLBCL patients
All 35 DLBCL patients had relapsed or refractory disease. The median number of prior treatments was 3
(range, 2-10), and 30 patients were refractory to their last line of chemotherapy.
Eleven of 31 (35%) patients with non-germinal center B-cell (non-GCB) DLBCL responded to ONO/GS-4059. Two non-GCB DLBCL patients had a confirmed CR, 1 had an unconfirmed CR, and the rest had partial responses.
The median duration of response was 54 days. And, among responders, the median treatment duration was 12 weeks.
The majority of non-GCB DLBCL patients progressed. There were no responses among the 2 patients with GCB DLBCL, and there were no responses among patients with primary mediastinal B-cell lymphoma or plasmablastic DLBCL.
Toxicity
AEs in this study were mostly grade 1/2—75% in the CLL cohort and 50% in the NHL cohort. However, treatment-related grade 3/4 AEs occurred in 14.3% of CLL patients and 16.1% of NHL patients.
Grade 3/4 events were mainly hematologic in nature and included neutropenia (10%), anemia (13.3%), and thrombocytopenia (13.3%).
There was a grade 3 episode of drug-related hemorrhage in a CLL patient, which resulted in a psoas hematoma (with concomitant CLL progression) in the presence of a normal platelet count. This patient was among those taken off the study.
“The next step is now to see how best we can improve on these outstanding results,” said study author Martin Dyer, DPhil, of the University of Leicester.
“A further study using this drug in combination with additional targeted agents is shortly to open in Leicester with the aim of achieving cure. In parallel with the clinical development of the drug, our team of scientists at the Haematological Research Institute are studying how this drug is working and how to overcome potential resistance.” ![]()
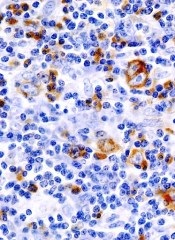
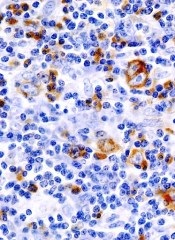
ITC 2015: Review IDs features to aid thyroid lymphoma diagnosis
LAKE BUENA VISTA, FLA. – Rapidly enlarging thyroid masses with compressive symptoms may signal thyroid lymphoma, according to findings from a review of cases at the Mayo Clinic.
Radiologically, these masses tend to present as large, unilateral, thyroid-centered masses that are hypoechoic on ultrasound and that expand into adjacent soft tissue, Dr. Anu Sharma reported at the International Thyroid Congress.
The findings are based on a review of 75 patients with biopsy-proven thyroid lymphoma – a relatively rare disease, accounting for between 1% and 5% of all thyroid malignancies, and less than 1% of all lymphomas – who presented to the Mayo Clinic between 2000 and 2014.
“Thyroid lymphoma can sometimes present very similar to anaplastic carcinoma, and we wanted to see if there are any unique identification factors that you can use to increase your suspicion of thyroid lymphoma,” Dr. Sharma of the Mayo Clinic, Rochester, Minn., said.
Indeed, rapid enlargement and compressive symptoms are also common presenting features of anaplastic carcinoma, she said.
Of the 75 cases included in the review – compromising all cases presenting during the study period – 70.7% involved primary thyroid lymphoma. A neck mass was present in 88% of cases, dysphagia in 45%, and hoarseness in 37%.
The typical presentation included a solid, hypoechoic mass with mildly increased vascularity, no internal calcifications, and edge characteristics that ranged from well-defined (80%) to ill-defined (20%). Median tumor volume was 64 cm3, Dr. Sharma said.
This differs from anaplastic carcinoma in that most patients with anaplastic carcinoma have ill-defined edges, she noted.
Another difference between thyroid lymphoma and anaplastic carcinoma as noted in this study involves necrosis; none of the patients in the current study had areas of necrosis, whereas 78% of anaplastic carcinoma patients in another study had areas of necrosis, she explained.
The patients in the current study had a median age of 67 years, although the ages varied widely. About half (50.7%) were men, and 54.7% had a history of Hashimoto’s thyroiditis. Fifty-seven of the patients had an ultrasound before treatment.
The first diagnostic procedure performed was fine needle aspiration (FNA) in 65 subjects, and the FNA biopsies were abnormal in 69% of those, with 42% suggesting a specific lymphoma subtype. The subtype diagnosis was accurate, based on final tissue analysis, in 89% of those.
“While this is quite impressive, all patients who had FNA ended up having further tissue biopsy for subtype confirmation and for treatment, and this is important, because the subtype of the lymphoma is important in determining the type of treatment uses as well as determining prognosis,” she said.
The diagnosis was confirmed by core biopsy in 46.7% of cases, by incisional biopsy in 9.3%, by partial or total thyroidectomy in 25.3%, and by lymph node biopsy in 13.3%; percentages total 94.6% due to downward rounding. Histologic subtypes included diffuse large B-cell lymphoma (DLBCL) in 73.3% of cases, follicular lymphoma in 5.3%, mucosa-associated lymphoid tissue (MALT) in 10.7%, MALT/DLBCL in 2.6%, T-cell lymphoma in 2.6%, and Hodgkin’s lymphoma in 1.3%; percentages total 95.8% rather than 100% due to downward rounding.
In addition to rapid enlargement of a neck mass with compressive symptoms, findings that should raise suspicion of thyroid lymphoma include a history of Hashimoto’s thyroiditis and the ultrasound findings characterized by this study, Dr. Sharma said.
“Once you have that increased suspicion, you should move toward going to core biopsy rather than FNA to save the patient from having two diagnostic steps rather than one,” she concluded.
Dr. Sharma reported having no disclosures.
LAKE BUENA VISTA, FLA. – Rapidly enlarging thyroid masses with compressive symptoms may signal thyroid lymphoma, according to findings from a review of cases at the Mayo Clinic.
Radiologically, these masses tend to present as large, unilateral, thyroid-centered masses that are hypoechoic on ultrasound and that expand into adjacent soft tissue, Dr. Anu Sharma reported at the International Thyroid Congress.
The findings are based on a review of 75 patients with biopsy-proven thyroid lymphoma – a relatively rare disease, accounting for between 1% and 5% of all thyroid malignancies, and less than 1% of all lymphomas – who presented to the Mayo Clinic between 2000 and 2014.
“Thyroid lymphoma can sometimes present very similar to anaplastic carcinoma, and we wanted to see if there are any unique identification factors that you can use to increase your suspicion of thyroid lymphoma,” Dr. Sharma of the Mayo Clinic, Rochester, Minn., said.
Indeed, rapid enlargement and compressive symptoms are also common presenting features of anaplastic carcinoma, she said.
Of the 75 cases included in the review – compromising all cases presenting during the study period – 70.7% involved primary thyroid lymphoma. A neck mass was present in 88% of cases, dysphagia in 45%, and hoarseness in 37%.
The typical presentation included a solid, hypoechoic mass with mildly increased vascularity, no internal calcifications, and edge characteristics that ranged from well-defined (80%) to ill-defined (20%). Median tumor volume was 64 cm3, Dr. Sharma said.
This differs from anaplastic carcinoma in that most patients with anaplastic carcinoma have ill-defined edges, she noted.
Another difference between thyroid lymphoma and anaplastic carcinoma as noted in this study involves necrosis; none of the patients in the current study had areas of necrosis, whereas 78% of anaplastic carcinoma patients in another study had areas of necrosis, she explained.
The patients in the current study had a median age of 67 years, although the ages varied widely. About half (50.7%) were men, and 54.7% had a history of Hashimoto’s thyroiditis. Fifty-seven of the patients had an ultrasound before treatment.
The first diagnostic procedure performed was fine needle aspiration (FNA) in 65 subjects, and the FNA biopsies were abnormal in 69% of those, with 42% suggesting a specific lymphoma subtype. The subtype diagnosis was accurate, based on final tissue analysis, in 89% of those.
“While this is quite impressive, all patients who had FNA ended up having further tissue biopsy for subtype confirmation and for treatment, and this is important, because the subtype of the lymphoma is important in determining the type of treatment uses as well as determining prognosis,” she said.
The diagnosis was confirmed by core biopsy in 46.7% of cases, by incisional biopsy in 9.3%, by partial or total thyroidectomy in 25.3%, and by lymph node biopsy in 13.3%; percentages total 94.6% due to downward rounding. Histologic subtypes included diffuse large B-cell lymphoma (DLBCL) in 73.3% of cases, follicular lymphoma in 5.3%, mucosa-associated lymphoid tissue (MALT) in 10.7%, MALT/DLBCL in 2.6%, T-cell lymphoma in 2.6%, and Hodgkin’s lymphoma in 1.3%; percentages total 95.8% rather than 100% due to downward rounding.
In addition to rapid enlargement of a neck mass with compressive symptoms, findings that should raise suspicion of thyroid lymphoma include a history of Hashimoto’s thyroiditis and the ultrasound findings characterized by this study, Dr. Sharma said.
“Once you have that increased suspicion, you should move toward going to core biopsy rather than FNA to save the patient from having two diagnostic steps rather than one,” she concluded.
Dr. Sharma reported having no disclosures.
LAKE BUENA VISTA, FLA. – Rapidly enlarging thyroid masses with compressive symptoms may signal thyroid lymphoma, according to findings from a review of cases at the Mayo Clinic.
Radiologically, these masses tend to present as large, unilateral, thyroid-centered masses that are hypoechoic on ultrasound and that expand into adjacent soft tissue, Dr. Anu Sharma reported at the International Thyroid Congress.
The findings are based on a review of 75 patients with biopsy-proven thyroid lymphoma – a relatively rare disease, accounting for between 1% and 5% of all thyroid malignancies, and less than 1% of all lymphomas – who presented to the Mayo Clinic between 2000 and 2014.
“Thyroid lymphoma can sometimes present very similar to anaplastic carcinoma, and we wanted to see if there are any unique identification factors that you can use to increase your suspicion of thyroid lymphoma,” Dr. Sharma of the Mayo Clinic, Rochester, Minn., said.
Indeed, rapid enlargement and compressive symptoms are also common presenting features of anaplastic carcinoma, she said.
Of the 75 cases included in the review – compromising all cases presenting during the study period – 70.7% involved primary thyroid lymphoma. A neck mass was present in 88% of cases, dysphagia in 45%, and hoarseness in 37%.
The typical presentation included a solid, hypoechoic mass with mildly increased vascularity, no internal calcifications, and edge characteristics that ranged from well-defined (80%) to ill-defined (20%). Median tumor volume was 64 cm3, Dr. Sharma said.
This differs from anaplastic carcinoma in that most patients with anaplastic carcinoma have ill-defined edges, she noted.
Another difference between thyroid lymphoma and anaplastic carcinoma as noted in this study involves necrosis; none of the patients in the current study had areas of necrosis, whereas 78% of anaplastic carcinoma patients in another study had areas of necrosis, she explained.
The patients in the current study had a median age of 67 years, although the ages varied widely. About half (50.7%) were men, and 54.7% had a history of Hashimoto’s thyroiditis. Fifty-seven of the patients had an ultrasound before treatment.
The first diagnostic procedure performed was fine needle aspiration (FNA) in 65 subjects, and the FNA biopsies were abnormal in 69% of those, with 42% suggesting a specific lymphoma subtype. The subtype diagnosis was accurate, based on final tissue analysis, in 89% of those.
“While this is quite impressive, all patients who had FNA ended up having further tissue biopsy for subtype confirmation and for treatment, and this is important, because the subtype of the lymphoma is important in determining the type of treatment uses as well as determining prognosis,” she said.
The diagnosis was confirmed by core biopsy in 46.7% of cases, by incisional biopsy in 9.3%, by partial or total thyroidectomy in 25.3%, and by lymph node biopsy in 13.3%; percentages total 94.6% due to downward rounding. Histologic subtypes included diffuse large B-cell lymphoma (DLBCL) in 73.3% of cases, follicular lymphoma in 5.3%, mucosa-associated lymphoid tissue (MALT) in 10.7%, MALT/DLBCL in 2.6%, T-cell lymphoma in 2.6%, and Hodgkin’s lymphoma in 1.3%; percentages total 95.8% rather than 100% due to downward rounding.
In addition to rapid enlargement of a neck mass with compressive symptoms, findings that should raise suspicion of thyroid lymphoma include a history of Hashimoto’s thyroiditis and the ultrasound findings characterized by this study, Dr. Sharma said.
“Once you have that increased suspicion, you should move toward going to core biopsy rather than FNA to save the patient from having two diagnostic steps rather than one,” she concluded.
Dr. Sharma reported having no disclosures.
AT ITC 2015
Key clinical point: Rapidly enlarging thyroid masses with compressive symptoms may signal thyroid lymphoma, according to findings from a review of cases at the Mayo Clinic.
Major finding: Typical presentation included a solid, hypoechoic mass with mildly increased vascularity, no internal calcifications, and edge characteristics that ranged from well-defined (80%) to ill-defined (20%).
Data source: A retrospective review of 75 cases.
Disclosures: Dr. Sharma reported having no disclosures.
New therapies finding their place in management of follicular lymphoma
SAN FRANCISCO – A variety of emerging therapies are being incorporated into the management of follicular lymphoma, which is typically a long-term endeavor requiring strategic use of multiple treatments, Dr. Andrew D. Zelenetz said at the National Comprehensive Cancer Network (NCCN) 10th Annual Congress: Hematologic Malignancies.
“Follicular lymphoma is a disease of paradox. The reality is that overall survival is excellent, but patients are not going to be able to do that with one treatment; they are going to get a series of treatments,” he said. “Survival is the sum of your exposures to treatment, time on active therapy, time in remission, and actually time with relapse not needing treatment.”
Risk stratification
Overall survival for patients with follicular lymphoma diagnosed today and treated with modern therapy is only slightly inferior to that for age-matched controls, noted Dr. Zelenetz of the department of medicine at Memorial Sloan-Kettering Cancer Center and professor of medicine at Cornell University, both in New York.
But patients who are faring poorly at 12 months (American Society of Hematology [ASH] 2014, Abstract 1664) or at 24 months (J Clin Oncol. 2015;33[23]:2516-22) into care have a much worse prognosis. “This shows the importance of identifying those patients with poor biology, and [the question of] whether we can identify them without treating them first and having them progress,” he said.
Hematologists have historically looked to the Follicular Lymphoma International Prognostic Index (FLIPI) to estimate outcome. “The FLIPI clearly works; it’s an important clinical tool. But the FLIPI high-risk patients are still identifying more than those very high-risk patients,” he said.
Therefore, a clinicogenomic risk model was developed that incorporates seven mutations having poor prognostic impact, the m7-FLIPI (Lancet Oncol. 2015;16[9]:1111-22). Adding the mutations split the previously defined high-risk patients into a group with a prognosis similar to that of low-risk patients and a small group with a very poor prognosis.
“This actually represents something very close to the 20% of patients that we think have bad biology,” Dr. Zelenetz noted. “There will be some additional data at ASH looking at this exact question, because the holy grail is to know when you diagnose someone if they are in that bad-risk group because those are the patients you want to do novel clinical trials on. If your overall survival is equivalent to the general population, it’s going to be hard to ever prove an overall survival advantage for an intervention in an unselected group of patients.”
Advanced-stage disease with low tumor bulk
For patients who have advanced-stage follicular lymphoma but with low tumor bulk, the NCCN endorses a modification of criteria developed by the Follicular Lymphoma Study Group (GELF) in deciding when to start treatment (J Clin Oncol. 1998;16[7]:2332-8).
Roughly a fifth of patients who are eligible for and managed with a watch-and-wait approach will not need chemotherapy or die of their disease in the next 10 years (Lancet. 2003;362[9383]:516-22). Furthermore, this strategy nets a median delay in the need for chemotherapy of 2.6 years.
Compared with observation, treatment with the anti-CD20 antibody rituximab (Rituxan) improves progression-free survival but not overall survival in this setting (ASH 2010, Abstract 6). “Though in selected patients, rituximab may be appropriate as initial treatment for the observable patient, I would argue for the observable patient with no survival disadvantage, the standard of care remains observation,” Dr. Zelenetz said.
Advanced-stage disease requiring treatment
A meta-analysis has shown a clear survival benefit from adding rituximab to chemotherapy (R-chemo) in patients with advanced follicular lymphoma who need treatment (J Natl Cancer Inst. 2007;99[9]:706-14). “Based on the results, it is the standard of care to add rituximab to a chemotherapy backbone, but the optimum R-chemo actually remains undefined and would be customized to the individual clinical situation,” he commented.
A variety of emerging agents are being tested in this setting. Among the subset of patients with untreated follicular lymphoma in a single-center trial, the combination of rituximab with the immunomodulator lenalidomide (Revlimid) yielded an overall response rate of 98% and a complete response rate of 87%, as well as excellent progression-free and overall survival (Lancet Oncol. 2014;15[12]:1311-8). The main grade 3 or 4 toxicity was neutropenia, seen in 35% of all patients studied. Efficacy results were much the same in a multicenter trial (International Conference on Malignant Lymphoma [ICML] 2013, Abstract 63).
This combination is now being tested as front-line therapy for follicular lymphoma in the RELEVANCE (Rituximab and Lenalidomide Versus Any Chemotherapy) phase III trial. “The trial is now done, but we don’t have results, and we won’t have results until 2019, so don’t hold your breath,” Dr. Zelenetz commented. “That’s because this was an unselected trial; we took all patients, all comers. And if you don’t try to identify bad-risk patients, you actually have to do very large trials, and the effect size is relatively small.”
Relapsed and refractory disease
“Many times when patients with follicular lymphoma relapse, they are immediately started on treatment. It’s not necessary and probably in most cases not appropriate. If patients are asymptomatic and have a low tumor burden, they can have a second and a third and even a fourth period of observation, where they don’t need active treatment,” he said. “So I would encourage you to …wait until they actually meet GELF criteria again.”
A key question in this setting is whether patients previously given rituximab can derive benefit from an alternative anti-CD20 antibody. Taking on this question, the GADOLIN trial tested the addition of obinutuzumab (induction plus maintenance) to bendamustine among patients with rituximab-refractory disease (American Society of Clinical Oncology [ASCO] 2015, Abstract LBA8502; ICML 2015, Abstract 123).
Toxicities were generally similar by arm, except for a higher rate of infusion-related reactions with obinutuzumab. The overall response rates were comparable for the two arms, but progression-free survival was better with the combination (median event-free survival, not reached, vs. 14.9 months; hazard ratio, 0.55), and there was a trend for overall survival.
“These curves start separating after 6 months, and 6 months is the time of chemotherapy,” Dr. Zelenetz noted. “So I would argue from these data that the obinutuzumab didn’t add very much to the bendamustine backbone, but actually the obinutuzumab maintenance was effective even in rituximab-refractory patients.”
The combination of lenalidomide and rituximab has been compared with lenalidomide alone in patients with relapsed follicular lymphoma (ASCO 2012, Abstract 8000). The results showed a trend toward better median event-free survival with the combination (2.0 vs. 1.2 years; hazard ratio, 1.9; P = .061) but not overall survival.
In a phase II trial, idelalisib (Zydelig) was tested among patients with indolent non-Hodgkin lymphomas (60% with follicular lymphoma) that were refractory to both rituximab and an alkylator (N Engl J Med. 2014;370:1008-18). Noteworthy grade 3 or worse toxicities included pneumonia and transaminase elevations. The overall response rate was 57%, and the complete response rate was 6%; median progression-free survival was 11 months.
“Idelalisib can be safely combined with other agents including rituximab and bendamustine,” Dr. Zelenetz added (ASH 2014, Abstract 3063). “Interestingly, the overall response seems to be a little higher when you combine it, but it doesn’t seem to matter which drug you combine it with – rituximab, bendamustine, or [both] – you get good overall responses,” ranging from 71% to 85%.
The BCL-2 inhibitor venetoclax (formerly ABT-199/GDC-199) has been tested in non-Hodgkin lymphomas, where it has not been associated with the life-threatening tumor lysis syndrome seen in some other hematologic malignancies (European Hematology Association [EHA] 2015, Davis et al). It yielded an overall response rate of 31% in patients with relatively refractory follicular lymphoma. “This will lead to additional studies in this area,” he predicted.
Finally, nivolumab (Opdivo), a PD-1 immune checkpoint inhibitor, has been evaluated in a phase I study in relapsed or refractory hematologic malignancies, where it was well tolerated (ASH 2014, Abstract 291). Among the small subset of patients with follicular lymphoma, the overall response rate was 40%, prompting initiation of more trials.
Although chimeric antigen receptor (CAR) T-cell therapy is showing promise in various malignancies, Dr. Zelenetz said that other options are probably better avenues for research in follicular lymphoma at present.
“I’m much more interested in the tools that we have now, between the checkpoint inhibitors, the T-cell activators, and the bispecific monoclonal antibodies. I think I can [apply these therapies] with less money for probably less toxicity without the complexity of having to make a customized drug for the patient,” he said. “So I’m not very enthusiastic about CAR T cells in follicular lymphoma.”
SAN FRANCISCO – A variety of emerging therapies are being incorporated into the management of follicular lymphoma, which is typically a long-term endeavor requiring strategic use of multiple treatments, Dr. Andrew D. Zelenetz said at the National Comprehensive Cancer Network (NCCN) 10th Annual Congress: Hematologic Malignancies.
“Follicular lymphoma is a disease of paradox. The reality is that overall survival is excellent, but patients are not going to be able to do that with one treatment; they are going to get a series of treatments,” he said. “Survival is the sum of your exposures to treatment, time on active therapy, time in remission, and actually time with relapse not needing treatment.”
Risk stratification
Overall survival for patients with follicular lymphoma diagnosed today and treated with modern therapy is only slightly inferior to that for age-matched controls, noted Dr. Zelenetz of the department of medicine at Memorial Sloan-Kettering Cancer Center and professor of medicine at Cornell University, both in New York.
But patients who are faring poorly at 12 months (American Society of Hematology [ASH] 2014, Abstract 1664) or at 24 months (J Clin Oncol. 2015;33[23]:2516-22) into care have a much worse prognosis. “This shows the importance of identifying those patients with poor biology, and [the question of] whether we can identify them without treating them first and having them progress,” he said.
Hematologists have historically looked to the Follicular Lymphoma International Prognostic Index (FLIPI) to estimate outcome. “The FLIPI clearly works; it’s an important clinical tool. But the FLIPI high-risk patients are still identifying more than those very high-risk patients,” he said.
Therefore, a clinicogenomic risk model was developed that incorporates seven mutations having poor prognostic impact, the m7-FLIPI (Lancet Oncol. 2015;16[9]:1111-22). Adding the mutations split the previously defined high-risk patients into a group with a prognosis similar to that of low-risk patients and a small group with a very poor prognosis.
“This actually represents something very close to the 20% of patients that we think have bad biology,” Dr. Zelenetz noted. “There will be some additional data at ASH looking at this exact question, because the holy grail is to know when you diagnose someone if they are in that bad-risk group because those are the patients you want to do novel clinical trials on. If your overall survival is equivalent to the general population, it’s going to be hard to ever prove an overall survival advantage for an intervention in an unselected group of patients.”
Advanced-stage disease with low tumor bulk
For patients who have advanced-stage follicular lymphoma but with low tumor bulk, the NCCN endorses a modification of criteria developed by the Follicular Lymphoma Study Group (GELF) in deciding when to start treatment (J Clin Oncol. 1998;16[7]:2332-8).
Roughly a fifth of patients who are eligible for and managed with a watch-and-wait approach will not need chemotherapy or die of their disease in the next 10 years (Lancet. 2003;362[9383]:516-22). Furthermore, this strategy nets a median delay in the need for chemotherapy of 2.6 years.
Compared with observation, treatment with the anti-CD20 antibody rituximab (Rituxan) improves progression-free survival but not overall survival in this setting (ASH 2010, Abstract 6). “Though in selected patients, rituximab may be appropriate as initial treatment for the observable patient, I would argue for the observable patient with no survival disadvantage, the standard of care remains observation,” Dr. Zelenetz said.
Advanced-stage disease requiring treatment
A meta-analysis has shown a clear survival benefit from adding rituximab to chemotherapy (R-chemo) in patients with advanced follicular lymphoma who need treatment (J Natl Cancer Inst. 2007;99[9]:706-14). “Based on the results, it is the standard of care to add rituximab to a chemotherapy backbone, but the optimum R-chemo actually remains undefined and would be customized to the individual clinical situation,” he commented.
A variety of emerging agents are being tested in this setting. Among the subset of patients with untreated follicular lymphoma in a single-center trial, the combination of rituximab with the immunomodulator lenalidomide (Revlimid) yielded an overall response rate of 98% and a complete response rate of 87%, as well as excellent progression-free and overall survival (Lancet Oncol. 2014;15[12]:1311-8). The main grade 3 or 4 toxicity was neutropenia, seen in 35% of all patients studied. Efficacy results were much the same in a multicenter trial (International Conference on Malignant Lymphoma [ICML] 2013, Abstract 63).
This combination is now being tested as front-line therapy for follicular lymphoma in the RELEVANCE (Rituximab and Lenalidomide Versus Any Chemotherapy) phase III trial. “The trial is now done, but we don’t have results, and we won’t have results until 2019, so don’t hold your breath,” Dr. Zelenetz commented. “That’s because this was an unselected trial; we took all patients, all comers. And if you don’t try to identify bad-risk patients, you actually have to do very large trials, and the effect size is relatively small.”
Relapsed and refractory disease
“Many times when patients with follicular lymphoma relapse, they are immediately started on treatment. It’s not necessary and probably in most cases not appropriate. If patients are asymptomatic and have a low tumor burden, they can have a second and a third and even a fourth period of observation, where they don’t need active treatment,” he said. “So I would encourage you to …wait until they actually meet GELF criteria again.”
A key question in this setting is whether patients previously given rituximab can derive benefit from an alternative anti-CD20 antibody. Taking on this question, the GADOLIN trial tested the addition of obinutuzumab (induction plus maintenance) to bendamustine among patients with rituximab-refractory disease (American Society of Clinical Oncology [ASCO] 2015, Abstract LBA8502; ICML 2015, Abstract 123).
Toxicities were generally similar by arm, except for a higher rate of infusion-related reactions with obinutuzumab. The overall response rates were comparable for the two arms, but progression-free survival was better with the combination (median event-free survival, not reached, vs. 14.9 months; hazard ratio, 0.55), and there was a trend for overall survival.
“These curves start separating after 6 months, and 6 months is the time of chemotherapy,” Dr. Zelenetz noted. “So I would argue from these data that the obinutuzumab didn’t add very much to the bendamustine backbone, but actually the obinutuzumab maintenance was effective even in rituximab-refractory patients.”
The combination of lenalidomide and rituximab has been compared with lenalidomide alone in patients with relapsed follicular lymphoma (ASCO 2012, Abstract 8000). The results showed a trend toward better median event-free survival with the combination (2.0 vs. 1.2 years; hazard ratio, 1.9; P = .061) but not overall survival.
In a phase II trial, idelalisib (Zydelig) was tested among patients with indolent non-Hodgkin lymphomas (60% with follicular lymphoma) that were refractory to both rituximab and an alkylator (N Engl J Med. 2014;370:1008-18). Noteworthy grade 3 or worse toxicities included pneumonia and transaminase elevations. The overall response rate was 57%, and the complete response rate was 6%; median progression-free survival was 11 months.
“Idelalisib can be safely combined with other agents including rituximab and bendamustine,” Dr. Zelenetz added (ASH 2014, Abstract 3063). “Interestingly, the overall response seems to be a little higher when you combine it, but it doesn’t seem to matter which drug you combine it with – rituximab, bendamustine, or [both] – you get good overall responses,” ranging from 71% to 85%.
The BCL-2 inhibitor venetoclax (formerly ABT-199/GDC-199) has been tested in non-Hodgkin lymphomas, where it has not been associated with the life-threatening tumor lysis syndrome seen in some other hematologic malignancies (European Hematology Association [EHA] 2015, Davis et al). It yielded an overall response rate of 31% in patients with relatively refractory follicular lymphoma. “This will lead to additional studies in this area,” he predicted.
Finally, nivolumab (Opdivo), a PD-1 immune checkpoint inhibitor, has been evaluated in a phase I study in relapsed or refractory hematologic malignancies, where it was well tolerated (ASH 2014, Abstract 291). Among the small subset of patients with follicular lymphoma, the overall response rate was 40%, prompting initiation of more trials.
Although chimeric antigen receptor (CAR) T-cell therapy is showing promise in various malignancies, Dr. Zelenetz said that other options are probably better avenues for research in follicular lymphoma at present.
“I’m much more interested in the tools that we have now, between the checkpoint inhibitors, the T-cell activators, and the bispecific monoclonal antibodies. I think I can [apply these therapies] with less money for probably less toxicity without the complexity of having to make a customized drug for the patient,” he said. “So I’m not very enthusiastic about CAR T cells in follicular lymphoma.”
SAN FRANCISCO – A variety of emerging therapies are being incorporated into the management of follicular lymphoma, which is typically a long-term endeavor requiring strategic use of multiple treatments, Dr. Andrew D. Zelenetz said at the National Comprehensive Cancer Network (NCCN) 10th Annual Congress: Hematologic Malignancies.
“Follicular lymphoma is a disease of paradox. The reality is that overall survival is excellent, but patients are not going to be able to do that with one treatment; they are going to get a series of treatments,” he said. “Survival is the sum of your exposures to treatment, time on active therapy, time in remission, and actually time with relapse not needing treatment.”
Risk stratification
Overall survival for patients with follicular lymphoma diagnosed today and treated with modern therapy is only slightly inferior to that for age-matched controls, noted Dr. Zelenetz of the department of medicine at Memorial Sloan-Kettering Cancer Center and professor of medicine at Cornell University, both in New York.
But patients who are faring poorly at 12 months (American Society of Hematology [ASH] 2014, Abstract 1664) or at 24 months (J Clin Oncol. 2015;33[23]:2516-22) into care have a much worse prognosis. “This shows the importance of identifying those patients with poor biology, and [the question of] whether we can identify them without treating them first and having them progress,” he said.
Hematologists have historically looked to the Follicular Lymphoma International Prognostic Index (FLIPI) to estimate outcome. “The FLIPI clearly works; it’s an important clinical tool. But the FLIPI high-risk patients are still identifying more than those very high-risk patients,” he said.
Therefore, a clinicogenomic risk model was developed that incorporates seven mutations having poor prognostic impact, the m7-FLIPI (Lancet Oncol. 2015;16[9]:1111-22). Adding the mutations split the previously defined high-risk patients into a group with a prognosis similar to that of low-risk patients and a small group with a very poor prognosis.
“This actually represents something very close to the 20% of patients that we think have bad biology,” Dr. Zelenetz noted. “There will be some additional data at ASH looking at this exact question, because the holy grail is to know when you diagnose someone if they are in that bad-risk group because those are the patients you want to do novel clinical trials on. If your overall survival is equivalent to the general population, it’s going to be hard to ever prove an overall survival advantage for an intervention in an unselected group of patients.”
Advanced-stage disease with low tumor bulk
For patients who have advanced-stage follicular lymphoma but with low tumor bulk, the NCCN endorses a modification of criteria developed by the Follicular Lymphoma Study Group (GELF) in deciding when to start treatment (J Clin Oncol. 1998;16[7]:2332-8).
Roughly a fifth of patients who are eligible for and managed with a watch-and-wait approach will not need chemotherapy or die of their disease in the next 10 years (Lancet. 2003;362[9383]:516-22). Furthermore, this strategy nets a median delay in the need for chemotherapy of 2.6 years.
Compared with observation, treatment with the anti-CD20 antibody rituximab (Rituxan) improves progression-free survival but not overall survival in this setting (ASH 2010, Abstract 6). “Though in selected patients, rituximab may be appropriate as initial treatment for the observable patient, I would argue for the observable patient with no survival disadvantage, the standard of care remains observation,” Dr. Zelenetz said.
Advanced-stage disease requiring treatment
A meta-analysis has shown a clear survival benefit from adding rituximab to chemotherapy (R-chemo) in patients with advanced follicular lymphoma who need treatment (J Natl Cancer Inst. 2007;99[9]:706-14). “Based on the results, it is the standard of care to add rituximab to a chemotherapy backbone, but the optimum R-chemo actually remains undefined and would be customized to the individual clinical situation,” he commented.
A variety of emerging agents are being tested in this setting. Among the subset of patients with untreated follicular lymphoma in a single-center trial, the combination of rituximab with the immunomodulator lenalidomide (Revlimid) yielded an overall response rate of 98% and a complete response rate of 87%, as well as excellent progression-free and overall survival (Lancet Oncol. 2014;15[12]:1311-8). The main grade 3 or 4 toxicity was neutropenia, seen in 35% of all patients studied. Efficacy results were much the same in a multicenter trial (International Conference on Malignant Lymphoma [ICML] 2013, Abstract 63).
This combination is now being tested as front-line therapy for follicular lymphoma in the RELEVANCE (Rituximab and Lenalidomide Versus Any Chemotherapy) phase III trial. “The trial is now done, but we don’t have results, and we won’t have results until 2019, so don’t hold your breath,” Dr. Zelenetz commented. “That’s because this was an unselected trial; we took all patients, all comers. And if you don’t try to identify bad-risk patients, you actually have to do very large trials, and the effect size is relatively small.”
Relapsed and refractory disease
“Many times when patients with follicular lymphoma relapse, they are immediately started on treatment. It’s not necessary and probably in most cases not appropriate. If patients are asymptomatic and have a low tumor burden, they can have a second and a third and even a fourth period of observation, where they don’t need active treatment,” he said. “So I would encourage you to …wait until they actually meet GELF criteria again.”
A key question in this setting is whether patients previously given rituximab can derive benefit from an alternative anti-CD20 antibody. Taking on this question, the GADOLIN trial tested the addition of obinutuzumab (induction plus maintenance) to bendamustine among patients with rituximab-refractory disease (American Society of Clinical Oncology [ASCO] 2015, Abstract LBA8502; ICML 2015, Abstract 123).
Toxicities were generally similar by arm, except for a higher rate of infusion-related reactions with obinutuzumab. The overall response rates were comparable for the two arms, but progression-free survival was better with the combination (median event-free survival, not reached, vs. 14.9 months; hazard ratio, 0.55), and there was a trend for overall survival.
“These curves start separating after 6 months, and 6 months is the time of chemotherapy,” Dr. Zelenetz noted. “So I would argue from these data that the obinutuzumab didn’t add very much to the bendamustine backbone, but actually the obinutuzumab maintenance was effective even in rituximab-refractory patients.”
The combination of lenalidomide and rituximab has been compared with lenalidomide alone in patients with relapsed follicular lymphoma (ASCO 2012, Abstract 8000). The results showed a trend toward better median event-free survival with the combination (2.0 vs. 1.2 years; hazard ratio, 1.9; P = .061) but not overall survival.
In a phase II trial, idelalisib (Zydelig) was tested among patients with indolent non-Hodgkin lymphomas (60% with follicular lymphoma) that were refractory to both rituximab and an alkylator (N Engl J Med. 2014;370:1008-18). Noteworthy grade 3 or worse toxicities included pneumonia and transaminase elevations. The overall response rate was 57%, and the complete response rate was 6%; median progression-free survival was 11 months.
“Idelalisib can be safely combined with other agents including rituximab and bendamustine,” Dr. Zelenetz added (ASH 2014, Abstract 3063). “Interestingly, the overall response seems to be a little higher when you combine it, but it doesn’t seem to matter which drug you combine it with – rituximab, bendamustine, or [both] – you get good overall responses,” ranging from 71% to 85%.
The BCL-2 inhibitor venetoclax (formerly ABT-199/GDC-199) has been tested in non-Hodgkin lymphomas, where it has not been associated with the life-threatening tumor lysis syndrome seen in some other hematologic malignancies (European Hematology Association [EHA] 2015, Davis et al). It yielded an overall response rate of 31% in patients with relatively refractory follicular lymphoma. “This will lead to additional studies in this area,” he predicted.
Finally, nivolumab (Opdivo), a PD-1 immune checkpoint inhibitor, has been evaluated in a phase I study in relapsed or refractory hematologic malignancies, where it was well tolerated (ASH 2014, Abstract 291). Among the small subset of patients with follicular lymphoma, the overall response rate was 40%, prompting initiation of more trials.
Although chimeric antigen receptor (CAR) T-cell therapy is showing promise in various malignancies, Dr. Zelenetz said that other options are probably better avenues for research in follicular lymphoma at present.
“I’m much more interested in the tools that we have now, between the checkpoint inhibitors, the T-cell activators, and the bispecific monoclonal antibodies. I think I can [apply these therapies] with less money for probably less toxicity without the complexity of having to make a customized drug for the patient,” he said. “So I’m not very enthusiastic about CAR T cells in follicular lymphoma.”
AT NCCN ANNUAL CONGRESS: HEMATOLOGIC MALIGNANCIES
Reprogramming the immune system

showing Hodgkin lymphoma
NEW YORK—Using a 3-pronged approach to reprogram the immune system—inhibition of critical pathways, activation of others, and depletion of malignant cells—may be the best strategy to optimize immune function in B-cell lymphomas, according to Stephen M. Ansell, MD, PhD, of the Mayo Clinic in Rochester, Minnesota.
“[A]ll told, there are multiple immunological barriers to an effective immune response,” Dr Ansell said at Lymphoma & Myeloma 2015.
“So the questions are how can you use an immune checkpoint approach to try and modulate this and improve the outcome.”
Dr Ansell discussed checkpoint inhibitors, immune signal activators, and the potential of combining the approaches in Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL) in a way that enhances rather than antagonizes their effects.
Blocking CTLA-4
Cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) functions as an immune checkpoint that downregulates the immune system. A receptor found on the surface of inhibitor T cells, it acts as an off switch when it binds to CD80 or CD86 on the surface of antigen-presenting cells.
Ipilimumab, an antibody that targets CTLA-4, has been approved by the US Food and Drug Administration for the treatment of melanoma and is in clinical trials for lung, bladder, and prostate cancer.
Investigators wanted to see whether it also works in lymphoma, so they conducted a phase 1 study in relapsed/refractory B-cell NHL.
Eighteen patients received 3 mg/kg of ipilimumab. Two patients responded, 1 with a complete response (CR) that lasted more than 31 months, and 1 with a partial response (PR) that lasted 19 months. In 5 of 16 patients (31%), T-cell proliferation to recall antigens increased more than 2-fold.
As Dr Ansell explained, “Immune response doesn’t always correlate directly with the clinical responses. So I think we really have a lot to learn about what is really a biomarker of efficacy.”
Ipilimumab was also evaluated to treat relapse after allogeneic hematopoietic stem cell transplantation (HSCT) in 29 patients with relapsed hematologic disease. Two patients with HL achieved a CR and 1 patient with mantle cell lymphoma achieved a PR.
The investigators observed that ipilimumab did not induce or exacerbate clinical graft-versus-host disease.
Blocking PD-1
Programmed cell death protein 1 (PD-1) is a surface receptor expressed on T cells and pro-B cells. PD-1 binds 2 ligands, PD-L1 and PD-L2.
PD-1 ligands are overexpressed in inflammatory environments and attenuate the immune response through PD-1 on immune effector cells. In addition, PD-L1 expressed on malignant cells or in the tumor microenvironment suppresses tumor-infiltrating lymphocyte activity.
Pidilizumab, a humanized monoclonal antibody that binds to PD-1, weakens the apoptotic processes in lymphocytes and augments the antitumor activities of NK cells.
Investigators conducted a phase 2 trial of pidilizumab in patients with diffuse large B-cell lymphoma (DLBCL) after autologous HSCT to modulate the immune system after a transplant.
The team treated 66 patients with the antibody. At 16 months, progression-free survival (PFS) was 72%. For the 24 high-risk patients who were PET-positive after salvage chemotherapy, the 16-month PFS was 70%.
“And I think that what was most interesting,” Dr Ansell said, when focusing on the 35 patients with measurable disease after transplant, pidilizumab produced a 51% response rate “even in patients that actually had active disease.”
When pidilizumab was combined with rituximab in another trial in patients with relapsed follicular lymphoma (FL), 19 of 29 evaluable patients (66%) achieved an objective response: 15 (52%) CRs and 4 (14%) PRs.
“You might say, ‘Who cares? That’s not that great,’” Dr Ansell said. “But I think what was pretty impressive is that 52% CR rate. And most of you who treat patients with rituximab would know that that’s quite surprising, suggesting that there may be additional benefit for the use of PD-1 blockade in this subset of patients.”
Nivolumab, another monoclonal antibody that blocks the PD-1 pathway, is being investigated in a number of lymphoid malignancies, including HL, DLBCL, and T-cell lymphomas.
In a phase 1 study of nivolumab in 81 patients with relapsed or refractory lymphoid malignancies, the best preliminary overall response has been in FL and DLBCL patients, with an objective response rate of 40% and 36%, respectively, including 1 PR and 3 PRs in each subtype.
“I think what is important,” Dr Ansell said, “is that the side effects, as expected, were mainly immune-mediated, not as dramatic as have been seen with other agents, and very similar to what has been seen in solid tumor studies.”
Dr Ansell pointed out that the response rates with nivolumab varied widely by histology, suggesting that “we have a lot to learn about why patients benefit and who exactly benefits.”
There were no responses in patients with multiple myeloma or primary mediastinal B-cell lymphoma, although many patients achieved stable disease.
“Hodgkin lymphoma was completely different,” Dr Ansell said, “and there were responses in virtually every patient.”
Of 23 patients treated with nivolumab, 20 responded—4 achieved a CR and 16 a PR—including patients who had failed autologous HSCT and brentuximab vedotin treatment. Eleven patients, including 2 with CRs, have an ongoing response, some approaching 2 years. So the responses have been durable, Dr Ansell noted.
Yet another PD-1 antibody, pembrolizumab, has prompted reduction in tumor burden in HL in all but 2 of 29 evaluable patients, including 6 CRs and 13 PRs. The median duration of response has not yet been reached, and the side effect profile was similar to what has been seen with nivolumab and in solid tumors.
Activating immune stimulatory signals
Another approach to boosting the immune system is to activate immune stimulatory signals, eg, CD27 and CD40, and get a benefit that way. Varlilumab (CDX-1127) is an unconjugated monoclonal antibody that binds CD27 and activates CD27-expressing T cells.
In a phase 1 trial of varlilumab in 24 lymphoma patients, investigators found no significant depletion in absolute lymphocyte counts, T cells, or B cells. “Not quite the same success story,” Dr Ansell said, with a response—a CR—in only 1 patient.
Investigators did observe, however, evidence of increased soluble CD27, a reduction of circulating Tregs, and the induction of pro-inflammatory cytokines.
And in a phase 1 study of the anti-CD40 monoclonal antibody dacetuzumab in recurrent NHL, “the response rate was disappointingly low,” Dr Ansell said.
Investigators observed 6 objective responses, including 1 CR and 5 PRs, and a decrease in tumor size in approximately one-third of the 50 patients treated.
The investigators of the subsequent phase 2 trial did not want to take the agent forward for further study, Dr Ansell noted, “but there are antibodies now being developed in this space that will hopefully be more effective and create a greater benefit.”
Optimizing immune function
Dr Ansell suggested there are 3 main approaches to treating patients. One is going directly after the malignant cells and depleting them. A second is to inhibit critical pathways that the malignant cell is dependent upon, “starving them, if you like.” The third way is to activate the immune system and thereby create a greater benefit for patients.
“[P]robably our best strategy is to use all 3 in a reprogram approach,” he said. “Because unless you target each one of these areas, the likelihood is that the other sides of the 3-legged stool will take over.”
“This is an encouraging and exciting time for immune checkpoints therapy and an encouraging and exciting time for immune therapies in general. I think this is really the new frontier in lymphomas.” ![]()

showing Hodgkin lymphoma
NEW YORK—Using a 3-pronged approach to reprogram the immune system—inhibition of critical pathways, activation of others, and depletion of malignant cells—may be the best strategy to optimize immune function in B-cell lymphomas, according to Stephen M. Ansell, MD, PhD, of the Mayo Clinic in Rochester, Minnesota.
“[A]ll told, there are multiple immunological barriers to an effective immune response,” Dr Ansell said at Lymphoma & Myeloma 2015.
“So the questions are how can you use an immune checkpoint approach to try and modulate this and improve the outcome.”
Dr Ansell discussed checkpoint inhibitors, immune signal activators, and the potential of combining the approaches in Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL) in a way that enhances rather than antagonizes their effects.
Blocking CTLA-4
Cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) functions as an immune checkpoint that downregulates the immune system. A receptor found on the surface of inhibitor T cells, it acts as an off switch when it binds to CD80 or CD86 on the surface of antigen-presenting cells.
Ipilimumab, an antibody that targets CTLA-4, has been approved by the US Food and Drug Administration for the treatment of melanoma and is in clinical trials for lung, bladder, and prostate cancer.
Investigators wanted to see whether it also works in lymphoma, so they conducted a phase 1 study in relapsed/refractory B-cell NHL.
Eighteen patients received 3 mg/kg of ipilimumab. Two patients responded, 1 with a complete response (CR) that lasted more than 31 months, and 1 with a partial response (PR) that lasted 19 months. In 5 of 16 patients (31%), T-cell proliferation to recall antigens increased more than 2-fold.
As Dr Ansell explained, “Immune response doesn’t always correlate directly with the clinical responses. So I think we really have a lot to learn about what is really a biomarker of efficacy.”
Ipilimumab was also evaluated to treat relapse after allogeneic hematopoietic stem cell transplantation (HSCT) in 29 patients with relapsed hematologic disease. Two patients with HL achieved a CR and 1 patient with mantle cell lymphoma achieved a PR.
The investigators observed that ipilimumab did not induce or exacerbate clinical graft-versus-host disease.
Blocking PD-1
Programmed cell death protein 1 (PD-1) is a surface receptor expressed on T cells and pro-B cells. PD-1 binds 2 ligands, PD-L1 and PD-L2.
PD-1 ligands are overexpressed in inflammatory environments and attenuate the immune response through PD-1 on immune effector cells. In addition, PD-L1 expressed on malignant cells or in the tumor microenvironment suppresses tumor-infiltrating lymphocyte activity.
Pidilizumab, a humanized monoclonal antibody that binds to PD-1, weakens the apoptotic processes in lymphocytes and augments the antitumor activities of NK cells.
Investigators conducted a phase 2 trial of pidilizumab in patients with diffuse large B-cell lymphoma (DLBCL) after autologous HSCT to modulate the immune system after a transplant.
The team treated 66 patients with the antibody. At 16 months, progression-free survival (PFS) was 72%. For the 24 high-risk patients who were PET-positive after salvage chemotherapy, the 16-month PFS was 70%.
“And I think that what was most interesting,” Dr Ansell said, when focusing on the 35 patients with measurable disease after transplant, pidilizumab produced a 51% response rate “even in patients that actually had active disease.”
When pidilizumab was combined with rituximab in another trial in patients with relapsed follicular lymphoma (FL), 19 of 29 evaluable patients (66%) achieved an objective response: 15 (52%) CRs and 4 (14%) PRs.
“You might say, ‘Who cares? That’s not that great,’” Dr Ansell said. “But I think what was pretty impressive is that 52% CR rate. And most of you who treat patients with rituximab would know that that’s quite surprising, suggesting that there may be additional benefit for the use of PD-1 blockade in this subset of patients.”
Nivolumab, another monoclonal antibody that blocks the PD-1 pathway, is being investigated in a number of lymphoid malignancies, including HL, DLBCL, and T-cell lymphomas.
In a phase 1 study of nivolumab in 81 patients with relapsed or refractory lymphoid malignancies, the best preliminary overall response has been in FL and DLBCL patients, with an objective response rate of 40% and 36%, respectively, including 1 PR and 3 PRs in each subtype.
“I think what is important,” Dr Ansell said, “is that the side effects, as expected, were mainly immune-mediated, not as dramatic as have been seen with other agents, and very similar to what has been seen in solid tumor studies.”
Dr Ansell pointed out that the response rates with nivolumab varied widely by histology, suggesting that “we have a lot to learn about why patients benefit and who exactly benefits.”
There were no responses in patients with multiple myeloma or primary mediastinal B-cell lymphoma, although many patients achieved stable disease.
“Hodgkin lymphoma was completely different,” Dr Ansell said, “and there were responses in virtually every patient.”
Of 23 patients treated with nivolumab, 20 responded—4 achieved a CR and 16 a PR—including patients who had failed autologous HSCT and brentuximab vedotin treatment. Eleven patients, including 2 with CRs, have an ongoing response, some approaching 2 years. So the responses have been durable, Dr Ansell noted.
Yet another PD-1 antibody, pembrolizumab, has prompted reduction in tumor burden in HL in all but 2 of 29 evaluable patients, including 6 CRs and 13 PRs. The median duration of response has not yet been reached, and the side effect profile was similar to what has been seen with nivolumab and in solid tumors.
Activating immune stimulatory signals
Another approach to boosting the immune system is to activate immune stimulatory signals, eg, CD27 and CD40, and get a benefit that way. Varlilumab (CDX-1127) is an unconjugated monoclonal antibody that binds CD27 and activates CD27-expressing T cells.
In a phase 1 trial of varlilumab in 24 lymphoma patients, investigators found no significant depletion in absolute lymphocyte counts, T cells, or B cells. “Not quite the same success story,” Dr Ansell said, with a response—a CR—in only 1 patient.
Investigators did observe, however, evidence of increased soluble CD27, a reduction of circulating Tregs, and the induction of pro-inflammatory cytokines.
And in a phase 1 study of the anti-CD40 monoclonal antibody dacetuzumab in recurrent NHL, “the response rate was disappointingly low,” Dr Ansell said.
Investigators observed 6 objective responses, including 1 CR and 5 PRs, and a decrease in tumor size in approximately one-third of the 50 patients treated.
The investigators of the subsequent phase 2 trial did not want to take the agent forward for further study, Dr Ansell noted, “but there are antibodies now being developed in this space that will hopefully be more effective and create a greater benefit.”
Optimizing immune function
Dr Ansell suggested there are 3 main approaches to treating patients. One is going directly after the malignant cells and depleting them. A second is to inhibit critical pathways that the malignant cell is dependent upon, “starving them, if you like.” The third way is to activate the immune system and thereby create a greater benefit for patients.
“[P]robably our best strategy is to use all 3 in a reprogram approach,” he said. “Because unless you target each one of these areas, the likelihood is that the other sides of the 3-legged stool will take over.”
“This is an encouraging and exciting time for immune checkpoints therapy and an encouraging and exciting time for immune therapies in general. I think this is really the new frontier in lymphomas.” ![]()

showing Hodgkin lymphoma
NEW YORK—Using a 3-pronged approach to reprogram the immune system—inhibition of critical pathways, activation of others, and depletion of malignant cells—may be the best strategy to optimize immune function in B-cell lymphomas, according to Stephen M. Ansell, MD, PhD, of the Mayo Clinic in Rochester, Minnesota.
“[A]ll told, there are multiple immunological barriers to an effective immune response,” Dr Ansell said at Lymphoma & Myeloma 2015.
“So the questions are how can you use an immune checkpoint approach to try and modulate this and improve the outcome.”
Dr Ansell discussed checkpoint inhibitors, immune signal activators, and the potential of combining the approaches in Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL) in a way that enhances rather than antagonizes their effects.
Blocking CTLA-4
Cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) functions as an immune checkpoint that downregulates the immune system. A receptor found on the surface of inhibitor T cells, it acts as an off switch when it binds to CD80 or CD86 on the surface of antigen-presenting cells.
Ipilimumab, an antibody that targets CTLA-4, has been approved by the US Food and Drug Administration for the treatment of melanoma and is in clinical trials for lung, bladder, and prostate cancer.
Investigators wanted to see whether it also works in lymphoma, so they conducted a phase 1 study in relapsed/refractory B-cell NHL.
Eighteen patients received 3 mg/kg of ipilimumab. Two patients responded, 1 with a complete response (CR) that lasted more than 31 months, and 1 with a partial response (PR) that lasted 19 months. In 5 of 16 patients (31%), T-cell proliferation to recall antigens increased more than 2-fold.
As Dr Ansell explained, “Immune response doesn’t always correlate directly with the clinical responses. So I think we really have a lot to learn about what is really a biomarker of efficacy.”
Ipilimumab was also evaluated to treat relapse after allogeneic hematopoietic stem cell transplantation (HSCT) in 29 patients with relapsed hematologic disease. Two patients with HL achieved a CR and 1 patient with mantle cell lymphoma achieved a PR.
The investigators observed that ipilimumab did not induce or exacerbate clinical graft-versus-host disease.
Blocking PD-1
Programmed cell death protein 1 (PD-1) is a surface receptor expressed on T cells and pro-B cells. PD-1 binds 2 ligands, PD-L1 and PD-L2.
PD-1 ligands are overexpressed in inflammatory environments and attenuate the immune response through PD-1 on immune effector cells. In addition, PD-L1 expressed on malignant cells or in the tumor microenvironment suppresses tumor-infiltrating lymphocyte activity.
Pidilizumab, a humanized monoclonal antibody that binds to PD-1, weakens the apoptotic processes in lymphocytes and augments the antitumor activities of NK cells.
Investigators conducted a phase 2 trial of pidilizumab in patients with diffuse large B-cell lymphoma (DLBCL) after autologous HSCT to modulate the immune system after a transplant.
The team treated 66 patients with the antibody. At 16 months, progression-free survival (PFS) was 72%. For the 24 high-risk patients who were PET-positive after salvage chemotherapy, the 16-month PFS was 70%.
“And I think that what was most interesting,” Dr Ansell said, when focusing on the 35 patients with measurable disease after transplant, pidilizumab produced a 51% response rate “even in patients that actually had active disease.”
When pidilizumab was combined with rituximab in another trial in patients with relapsed follicular lymphoma (FL), 19 of 29 evaluable patients (66%) achieved an objective response: 15 (52%) CRs and 4 (14%) PRs.
“You might say, ‘Who cares? That’s not that great,’” Dr Ansell said. “But I think what was pretty impressive is that 52% CR rate. And most of you who treat patients with rituximab would know that that’s quite surprising, suggesting that there may be additional benefit for the use of PD-1 blockade in this subset of patients.”
Nivolumab, another monoclonal antibody that blocks the PD-1 pathway, is being investigated in a number of lymphoid malignancies, including HL, DLBCL, and T-cell lymphomas.
In a phase 1 study of nivolumab in 81 patients with relapsed or refractory lymphoid malignancies, the best preliminary overall response has been in FL and DLBCL patients, with an objective response rate of 40% and 36%, respectively, including 1 PR and 3 PRs in each subtype.
“I think what is important,” Dr Ansell said, “is that the side effects, as expected, were mainly immune-mediated, not as dramatic as have been seen with other agents, and very similar to what has been seen in solid tumor studies.”
Dr Ansell pointed out that the response rates with nivolumab varied widely by histology, suggesting that “we have a lot to learn about why patients benefit and who exactly benefits.”
There were no responses in patients with multiple myeloma or primary mediastinal B-cell lymphoma, although many patients achieved stable disease.
“Hodgkin lymphoma was completely different,” Dr Ansell said, “and there were responses in virtually every patient.”
Of 23 patients treated with nivolumab, 20 responded—4 achieved a CR and 16 a PR—including patients who had failed autologous HSCT and brentuximab vedotin treatment. Eleven patients, including 2 with CRs, have an ongoing response, some approaching 2 years. So the responses have been durable, Dr Ansell noted.
Yet another PD-1 antibody, pembrolizumab, has prompted reduction in tumor burden in HL in all but 2 of 29 evaluable patients, including 6 CRs and 13 PRs. The median duration of response has not yet been reached, and the side effect profile was similar to what has been seen with nivolumab and in solid tumors.
Activating immune stimulatory signals
Another approach to boosting the immune system is to activate immune stimulatory signals, eg, CD27 and CD40, and get a benefit that way. Varlilumab (CDX-1127) is an unconjugated monoclonal antibody that binds CD27 and activates CD27-expressing T cells.
In a phase 1 trial of varlilumab in 24 lymphoma patients, investigators found no significant depletion in absolute lymphocyte counts, T cells, or B cells. “Not quite the same success story,” Dr Ansell said, with a response—a CR—in only 1 patient.
Investigators did observe, however, evidence of increased soluble CD27, a reduction of circulating Tregs, and the induction of pro-inflammatory cytokines.
And in a phase 1 study of the anti-CD40 monoclonal antibody dacetuzumab in recurrent NHL, “the response rate was disappointingly low,” Dr Ansell said.
Investigators observed 6 objective responses, including 1 CR and 5 PRs, and a decrease in tumor size in approximately one-third of the 50 patients treated.
The investigators of the subsequent phase 2 trial did not want to take the agent forward for further study, Dr Ansell noted, “but there are antibodies now being developed in this space that will hopefully be more effective and create a greater benefit.”
Optimizing immune function
Dr Ansell suggested there are 3 main approaches to treating patients. One is going directly after the malignant cells and depleting them. A second is to inhibit critical pathways that the malignant cell is dependent upon, “starving them, if you like.” The third way is to activate the immune system and thereby create a greater benefit for patients.
“[P]robably our best strategy is to use all 3 in a reprogram approach,” he said. “Because unless you target each one of these areas, the likelihood is that the other sides of the 3-legged stool will take over.”
“This is an encouraging and exciting time for immune checkpoints therapy and an encouraging and exciting time for immune therapies in general. I think this is really the new frontier in lymphomas.” ![]()
Radiation often underused in follicular lymphoma

woman for radiotherapy
Photo by Rhoda Baer
SAN ANTONIO—A new study indicates that patients with early stage follicular lymphoma (FL) are increasingly receiving no treatment or single-agent chemotherapy, despite evidence suggesting that radiation therapy can produce better outcomes.
Guidelines from the National Comprehensive Cancer Network and the European Society for Medical Oncology both list radiation therapy as the preferred treatment for low-grade FL.
However, investigators found that, in recent years, radiation has been replaced by alternative strategies.
“Our study highlights the increasing omission of radiation therapy in [FL] and its associated negative effect on overall survival at a national level,” said John Austin Vargo, MD, of the University of Pittsburg Cancer Institute in Pennsylvania.
“This increasing bias towards the omission of radiation therapy is despite proven efficacy and increasing adoption of lower radiation therapy doses and more modern radiation therapy techniques which decrease risk of side effects.”
Dr Vargo presented these findings at the 57th Annual Meeting of the American Society for Radiation Oncology (presentation #183).
He and his colleagues analyzed patterns of care and survival outcomes for 35,961 patients diagnosed with early stage FL as listed in the National Cancer Data Base. A majority of patients were older than 60 (61%), and most had stage I disease (63%).
The use of radiation therapy in this group of patients decreased from 37% in 1999 to 24% in 2012 (P<0.0001).
The use of observation increased from 34% in 1998 to 44% in 2012 (P<0.0001). And the use of single-agent chemotherapy increased from 5.4% in 1999 to 11.7% in 2006 (P=0.01).
The 5-year overall survival rate was 86% in patients who received radiation and 74% in those who did not (P<0.0001). Ten-year overall survival rates were 68% and 54%, respectively (P<0.0001).
In multivariate analysis, radiation therapy remained significantly associated with improved overall survival (P<0.0001). ![]()

woman for radiotherapy
Photo by Rhoda Baer
SAN ANTONIO—A new study indicates that patients with early stage follicular lymphoma (FL) are increasingly receiving no treatment or single-agent chemotherapy, despite evidence suggesting that radiation therapy can produce better outcomes.
Guidelines from the National Comprehensive Cancer Network and the European Society for Medical Oncology both list radiation therapy as the preferred treatment for low-grade FL.
However, investigators found that, in recent years, radiation has been replaced by alternative strategies.
“Our study highlights the increasing omission of radiation therapy in [FL] and its associated negative effect on overall survival at a national level,” said John Austin Vargo, MD, of the University of Pittsburg Cancer Institute in Pennsylvania.
“This increasing bias towards the omission of radiation therapy is despite proven efficacy and increasing adoption of lower radiation therapy doses and more modern radiation therapy techniques which decrease risk of side effects.”
Dr Vargo presented these findings at the 57th Annual Meeting of the American Society for Radiation Oncology (presentation #183).
He and his colleagues analyzed patterns of care and survival outcomes for 35,961 patients diagnosed with early stage FL as listed in the National Cancer Data Base. A majority of patients were older than 60 (61%), and most had stage I disease (63%).
The use of radiation therapy in this group of patients decreased from 37% in 1999 to 24% in 2012 (P<0.0001).
The use of observation increased from 34% in 1998 to 44% in 2012 (P<0.0001). And the use of single-agent chemotherapy increased from 5.4% in 1999 to 11.7% in 2006 (P=0.01).
The 5-year overall survival rate was 86% in patients who received radiation and 74% in those who did not (P<0.0001). Ten-year overall survival rates were 68% and 54%, respectively (P<0.0001).
In multivariate analysis, radiation therapy remained significantly associated with improved overall survival (P<0.0001). ![]()

woman for radiotherapy
Photo by Rhoda Baer
SAN ANTONIO—A new study indicates that patients with early stage follicular lymphoma (FL) are increasingly receiving no treatment or single-agent chemotherapy, despite evidence suggesting that radiation therapy can produce better outcomes.
Guidelines from the National Comprehensive Cancer Network and the European Society for Medical Oncology both list radiation therapy as the preferred treatment for low-grade FL.
However, investigators found that, in recent years, radiation has been replaced by alternative strategies.
“Our study highlights the increasing omission of radiation therapy in [FL] and its associated negative effect on overall survival at a national level,” said John Austin Vargo, MD, of the University of Pittsburg Cancer Institute in Pennsylvania.
“This increasing bias towards the omission of radiation therapy is despite proven efficacy and increasing adoption of lower radiation therapy doses and more modern radiation therapy techniques which decrease risk of side effects.”
Dr Vargo presented these findings at the 57th Annual Meeting of the American Society for Radiation Oncology (presentation #183).
He and his colleagues analyzed patterns of care and survival outcomes for 35,961 patients diagnosed with early stage FL as listed in the National Cancer Data Base. A majority of patients were older than 60 (61%), and most had stage I disease (63%).
The use of radiation therapy in this group of patients decreased from 37% in 1999 to 24% in 2012 (P<0.0001).
The use of observation increased from 34% in 1998 to 44% in 2012 (P<0.0001). And the use of single-agent chemotherapy increased from 5.4% in 1999 to 11.7% in 2006 (P=0.01).
The 5-year overall survival rate was 86% in patients who received radiation and 74% in those who did not (P<0.0001). Ten-year overall survival rates were 68% and 54%, respectively (P<0.0001).
In multivariate analysis, radiation therapy remained significantly associated with improved overall survival (P<0.0001). ![]()
Medical Roundtable: The Changing Pharmacologic Treatment Landscape in Chronic Lymphocytic Leukemia
Moderated by: Jennifer R. Brown, MD, PhD1
Discussants: Jeffrey A. Jones, MD, MPH2; Jacqueline C. Barrientos, MD3
From the Dana-Farber Cancer Institute and Harvard Medical School, Boston, MA1; Ohio State University, Columbus, OH2; Hofstra North Shore-LIJ School of Medicine, Lake Success, NY
Address for correspondence: Jennifer R. Brown, MD, PhD, Dana-Farber Cancer Institute, 450 Brookline Avenue, Boston, MA 02215
E-mail: [email protected]
Biographical Sketch
From Dana-Farber Cancer Institute and Harvard Medical School:
Jennifer R. Brown, MD, PhD is the Director of the CLL Center of the Division of Hematologic Malignancies at Dana-Farber Cancer Institute and an Associate Professor of Medicine at Harvard Medical School in Boston, Massachusetts. Dr. Brown completed a BS and MS simultaneously in molecular biophysics and biochemistry (MB&B) at Yale, graduating summa cum laude with distinction in MB&B. She proceeded to Harvard Medical School where she received her MD and PhD in molecular genetics in 1998 and was awarded the James Tolbert Shipley Prize for research accomplishment in the graduating class. She then served as an intern and resident in Internal Medicine at Massachusetts General Hospital followed by fellowship in Hematology and Medical Oncology at the Dana-Farber Cancer Institute. Dr. Brown joined the faculty of DFCI and Harvard Medical School in 2004, where she has an active clinical-translational research program in CLL.
Her particular interests include the development of novel targeted therapeutics for CLL, as well as the genomics of CLL. She has been instrumental in the clinical development of both idelalisib and ibrutinib, leading to their regulatory approvals in CLL.
In the area of genomics she has been instrumental in the description of the somatic mutation profile of CLL, and is now particularly interested in the implementation of genomic technology in the clinic, including for prognosis and targeted therapy. She also has a longstanding research interest and focus on the inherited predisposition to CLL.
To date she has published over 130 papers in the scientific literature, predominantly in CLL. She is an active member of the CLL Research Consortium and serves on the Alliance Leukemia and Leukemia Correlative Science Committees as well as the NIH Cancer Biomarkers Study Section. In 2014 she was the recipient of two awards from Dana-Farber Cancer Institute, the Clinical Innovation Award, as well as the George Canellos Award for Excellence in Clinical Investigation and Patient Care. She enjoys a worldwide reputation as a CLL expert and is in much demand as an international speaker.
From Hofstra North Shore-LIJ School of Medicine:
Jacqueline C. Barrientos, MD, is Attending Physician at the Chronic Lymphocytic Leukemia (CLL) Research & Treatment Program of the Division of Hematology and Medical Oncology, Department of Medicine, in the North Shore – LIJ Cancer Institute in Lake Success, New York. She is also Assistant Professor of Medicine at the Hofstra North Shore-LIJ School of Medicine. Dr. Barrientos works in close collaboration with her mentors, Dr. Kanti R. Rai and Dr. Nicholas Chiorazzi of the Feinstein Institute for Medical Research.
Dr. Barrientos received her medical degree at the Ponce School of Medicine in Puerto Rico, where she was elected vice-president of Alpha Omega Alpha Honor Medical Society. During her medical studies, she was the recipient of two Research Fellowship Awards from the Howard Hughes Medical Institute. She completed her internship and residency in internal medicine at Yale-New Haven Hospital of the Yale School of Medicine, and her fellowship in Hematology/Oncology at New York Presbyterian Hospital of Weill Cornell Medical College in New York City, where she also served as Chief Fellow. She is board certified in internal medicine, hematology and oncology.
Dr. Barrientos’ research focus is on chronic lymphocytic leukemia and lymphoma. She has extensive experience with the new promising agents targeting the B-cell receptor signaling pathway in B-cell malignancies, serving as Principal Investigator on several phase I-III clinical trials.
Dr. Barrientos actively participates in multi-institutional clinical trials with the Chronic Lymphocytic Leukemia Research Consortium (CRC) and the Alliance for Clinical Trials in Oncology. She is a cadre member of the Leukemia Committee of the Alliance for Clinical Trials in Oncology and in this capacity is co-chair of a study comparing chemoimmunotherapy against a combination of targeted agents. She is a member of the American Society of Clinical Oncology (ASCO) and the American Society of Hematology (ASH).
She has been an invited speaker for ASCO University “CLL Tumor Board”, ASH “State of the Art Symposium”, and “Highlights of ASH in Latin America”. Dr. Barrientos is the recipient of a 2015 American Society of Hematology-Harold Amos Medical Faculty Development Program (ASH-AMFDP) Fellowship award.
DR. BROWN: I am Jennifer Brown, Director of the Chronic Lymphocytic Leukemia (CLL) Center at Dana-Farber Cancer Institute, and Associate Professor of Medicine at Harvard Medical School. Today, I will be speaking with two of my esteemed CLL colleagues, Drs. Jeffrey Jones and Jacqueline Barrientos, about the new drug approvals in CLL.
DR. BARRIENTOS: I’m Jacqueline Barrientos, Assistant Professor of Hematology/Oncology at the Hofstra North Shore-LIJ School of Medicine, and Attending Hematologist at the CLL Research and Treatment Program in Long Island, NY. Our center participates in clinical trials and we perform correlative basic research. I’m very happy to participate in this expert roundtable discussion.
DR. JONES: I’m Dr. Jeffrey Jones, Associate Professor of Internal Medicine and Section Chief for CLL in the Division of Hematology at The Ohio State University.
DR. BROWN: Thank you Jeff and Jacquie for joining me today. I think we’re all aware what an exciting time this is in CLL with the approvals last year of the targeted inhibitors ibrutinib and idelalisib as well as the new antibody approval obinutuzumab as well as the additional indication for ofatumumab. Let’s start our discussion with ibrutinib and idelalisib. Jeff, please introduce the approvals that these inhibitors received and get us started.
DR. JONES: February 2014 marked a really important time in CLL medicine with the approval of the first oral kinase inhibitor, ibrutinib, for the treatment of CLL after one prior therapy.1,2 This ushered in an entirely new era of molecularly-targeted therapy for CLL. Later that year, ibrutinib received approval for deletion 17p CLL, the highest risk genetic subtype of CLL, whether previously untreated or relapsed disease. The drug has rapidly entered the clinic, although I think most of us are still trying to determine how best to incorporate them into our practice.
DR. BROWN: Jacquie, please comment on how you’re using ibrutinib now in your practice.
DR. BARRIENTOS: In CLL patients with the presence of a mutation of TP53 or deletion 17p, we use ibrutinib. We essentially do not use chemotherapy on this particular set of patients. If, for any reason, they are not able to tolerate the drug, then we consider idelalisib, which is not approved separately for this 17p deletion indication. Idelalisib is approved for use in combination with rituximab for the treatment of relapsed or refractory CLL patients. Idelalisib has shown clinical activity in several clinical trials in patients with deletion 17p.
At this moment, we mainly are using ibrutinib or idelalisib for our relapsed or refractory CLL patients. Clinical trials are underway in the frontline setting and we hope to see the results of the frontline use of ibrutinib in elderly patients soon. As of right now, we don’t use ibrutinib as a frontline therapy unless there is a reason, and usually it’s that they carry the 17p deletion or they are participating in a clinical trial.
DR. JONES: Outside of clinical trials our practice has really been to follow the label indications for ibrutinib. For previously untreated patients, our use has been limited to patients with deletion 17p or TP53 mutated disease, as Jacquie said, since that is the group for which the drug has been approved in the frontline.
DR. BROWN: I would agree. That’s been my practice as well. We should perhaps review the data from the registration trial that led to the ibrutinib approval for relapsed refractory CLL. The initial approval was from the stage IB2 study and was an accelerated approval.1 The confirmatory registration trial, RESONATE, randomized relapsed refractory CLL patients to ibrutinib versus the anti-CD20 antibody ofatumumab.2 Ibrutinib was found to be significantly better in improving both progression free and overall survival, although there was crossover later. As a result, this has moved into our relapse refractory use very rapidly. Although we still use chemoimmunotherapy for upfront therapy for patients without 17p deletion, for those in relapse we have moved entirely to targeted inhibitors. Would you both agree?
DR. JONES: For sure. I think it is very hard in 2015 to think of the patient for whom chemo-immunotherapy is the better choice than ibrutinib for relapsed disease.I think it is very hard in 2015 to think of the patient for whom chemoimmunotherapy is the better choice than ibrutinib for relapsed disease. The benefit is most marked for the group with higher-risk disease as characterized by genetic risk features, not just deletion 17p, but patients with complex abnormal karyotype or deletions of chromosome 11q. All of these patients particularly benefit from treatment with ibrutinib in the second line vs chemoimmunotherapy, as do patients who had either a suboptimal response to frontline chemoimmunotherapy or a brief duration of first remission. All of us are sometimes asked, “Well, who is the patient with relapsed CLL for whom ibrutinib is the best choice?” Right now, in most clinical situations, my response is, “For which patient is ibrutinib not the best choice in first relapse?”
DR. BROWN: That’s actually a good question. Jacquie, how would you answer that? Are there patients for whom you would not choose ibrutinib in first relapse?
DR. BARRIENTOS: I feel a hesitant to use ibrutinib in some patients with a particular comorbidity or medical history. For example, patients with a previous intracranial bleed or a recent history of bleeding, I would prefer to avoid using ibrutinib because there have been rare cases of spontaneous intracranial bleed or severe bleeding after trauma. The other type of patient where I would be cautious is a patient with uncontrolled atrial fibrillation because there are data that in the minority of patients (up to 10% of patients), atrial fibrillation has been an issue. We have some patients that are so frail that they couldn’t tolerate another episode of uncontrolled atrial fibrillation and as such they would not be ideal candidates for the drug. For that type of patient, I would probably abstain from using ibrutinib and consider the use of another therapy. Finally, I would be careful in patients on antiplatelet and anticoagulation therapy because ibrutinib affects platelet functions increasing the risk of bleeding. The bleeding events seen with ibrutinib are mostly grade 1 or grade 2. If the patients have had a serious bleed or serious gastrointestinal bleed or a recent surgery, then I would preferably use another agent.
DR. BROWN:Yes, so that gets to the toxicities of ibrutinib. The more medically significant ones do include perhaps a 5% to 10% risk of atrial fibrillation as well as bleeding risks, which as Jacquie points out are low and usually low grade, but there are occasional higher-risk bleeds. I personally still try to avoid combining anticoagulation with ibrutinib, as we don’t fully understand the mechanism or the risk factors for the more serious bleeds. Jeff, please comment.
DR. JONES: I think the data from the randomized study are actually the most helpful since, as you say, mild bleeding events (grade 1 or 2) were indeed more common amongst the group of patients who were treated with ibrutinib.2 Major bleeding events—which are typically defined as intracranial hemorrhage, bleeding requiring transfusion, or inpatient management—were actually similar between the two arms of the trial. An important caveat in interpreting these data is to know that patients in this trial were excluded if they were anticoagulated with warfarin, if they had an antecedent history of intracranial hemorrhage or recent bleeding, or recent surgery. In line with those exclusions, we will often consider other options. If there is any specific concern for bleeding, such as a patient who has experienced bleeding complications during routine anticoagulation, which is also a patient for whom ibrutinib may not be the best choice. In these clinical situations, it is important to involve the patient in discussing the balance of risks and benefits.
DR. BROWN: Yes. Jacquie, please comment on some of the side effects the patients on ibrutinib have, and how you manage those.
DR. BARRIENTOS: I usually mention to my patients that over the first 2 or 3 months about half of them will have a possible change in their bowel movements. Usually they report some diarrhea or loose stools. Usually these episodes are mild, nothing that requires hospitalization. In any case, if it becomes severe, I definitely make sure that it’s not an infection. We all know that our patients with CLL are prone to infections. The other thing I tell the patients is that in some cases patients may develop a rash on the skin. Many times it may look like a rash, but it’s actually ecchymosis—an effect from the drug on the platelets. Essentially, they are grade 1 and don’t require intervention. I just tell them that eventually they will go away. It can be scary for the patients if they are not expecting these. We have had patients with large areas of hematomas in the arms or in the legs. That is unexpected with a drug that they are taking by mouth. They usually expect that with other drugs like warfarin, but not with ibrutinib, so it is important to mention before they start the drug.
Last but not least, I mention the fact that they may get arthralgias—joint pain—in different areas of their bodies. I would say that I see that in about 20% to 30% of patients. Usually it’s very mild, but on occasion I’ve had patients with arthritis so severe that we’ve had to hold the drug and give them some steroids to help them improve their ability to maneuver their hands or move their joints. I’m sure you have seen some of those same side effects.
DR. BROWN: Yes, definitely. In general, it’s pretty well tolerated but it’s best to warn the patients, then there are no surprises. Let’s turn our attention for a moment back to the highest risk genetic subgroup, the 17p deleted patients—which Jeff had mentioned get particularly strong benefit from ibrutinib. This is certainly true, although it’s also the case that it appears, depending on the data set you look at, that they may relapse earlier than other patients on ibrutinib. In the original phase IB2, the median progression survival for the 17p deleted patients was 28 months. More recent data from Ohio State and MD Anderson suggest that complex karyotype may be a risk factor.3,4 Given these data, how are you two handling the question of allogeneic stem cell transplantation for these patients in this new era?
DR. BARRIENTOS: At our center, if the patient is young and they have access and are fit to tolerate a reduced-intensity allogeneic transplant, we recommend that they be evaluated for a transplant. Unfortunately, if they lose the response to the best drug available for their particular genetic mutation, then we have limited options of salvage therapy. It’s risky to think that they will not relapse at some point, and then what do we do at the time of relapse? We can use other targeted agents that are available, like idelalisib, with the knowledge that they may not always respond to the salvage therapy. Promising clinical activity has been reported for patients with 17p deletion treated with venetoclax in clinical trials. Venetoclax is a new targeted agent in development stages but the drug is only available in clinical trials.Promising clinical activity has been reported for patients with 17p deletion treated with venetoclax in clinical trials. Venetoclax is a new targeted agent in development stages but the drug is only available in clinical trials. One problem is that in order to participate in a clinical trial the patient needs to be able to get to the center to get the drug. Additionally, the patient needs to satisfy certain eligibility criteria for study entry. For these patients that stop responding to ibrutinib, the options of care are very limited at this time. This is the reason why I send all my young patients with a 17p deletion for a transplant evaluation.
At the end of the day it is tough to convince the patients to go for a transplant when they’re feeling in excellent shape. It’s still difficult to make a case to go for a procedure that may have its complications on its own. It is well known that there are some increased mortality risks and infection risks that can arise as a result of a transplant. They may not want to do it because they are feeling so great with their routine. I still sit down and have a long frank talk with the patients, especially if they have complex karyotype and 17p deletion. I am concerned that at some point they’re going to stop responding to ibrutinib.
DR. BROWN: That’s generally my practice as well. What about you, Jeff?
DR. JONES: Until there is greater clarity regarding which of the newer agents can salvage patients progressing after ibrutinib, I think it is still important for younger, transplant eligible patients with deletion 17p disease to undergo evaluation for allograft. It remains potentially curative therapy, and I think the availability of ibrutinib has not really changed the importance of that evaluation.
DR. BROWN: Yes, I would agree. I think that was a good discussion on ibrutinib. Why don’t we turn our attention now to idelalisib, the phosphoinositide 3-kinase (PI3K) inhibitor. How are you using idelalisib in your practices? Is this after ibrutinib in general?
DR. JONES: Published data regarding the sequencing of the new agents are relatively limited since all of the registration trials for idelalisib excluded patients who had received prior therapy with an inhibitor of B-cell receptor signaling, including Bruton’s tyrosine kinase inhibitors like ibrutinib.5,6 A small number of patients enrolled on the phase IB2 trial of ibrutinib, as well as the subsequent randomized trial, had received prior therapy with idelalisib and responded similarly to patients who had not received prior idelalisib.1,2 In our practice, the use of idelalisib has pretty much been limited to patients who have either received prior ibrutinib or patients who are not eligible to receive ibrutinib because of some important contraindication, such as an inherited bleeding defect, perceived increased bleeding, or history of difficult to control atrial fibrillation, since that event also seems to be more likely among patients treated with ibrutinib.
DR. BROWN: How about you, Jacquie?
DR. BARRIENTOS: The same type of patient with the addition of patients with kidney disease. The rationale for this is based on the phase III trial for idelalisib and rituximab, the enrollment allowed participation of patients with decreased renal function, that was one of the entry criteria for eligibility to participate in the trial.6 In most of the ibrutinib trials the creatinine clearance needed to be adequate, whereas this was allowed to be lower on the idelalisib trials. For those patients with severe renal impairment, I tend to prefer idelalisib rather than ibrutinib—only because I feel more comfortable and have more experience treating patients with impaired kidney function with idelalisib.
DR. BROWN: I have seen some episodic elevations in creatinine in patients on ibrutinib, but they’re fairly sporadic and it’s a little hard to assess the direct drug relationship. It is true that the patients in the idelalisib studies had a high level of comorbidity deliberately on the initial registration trial and generally did reasonably well with idelalisib. The toxicity profile of idelalisib is pretty characteristic, and is potentially harder to manage than that of ibrutinib. I think it also dictates some of how it’s being used in later line therapy. Does one of you wish to comment on the pattern of the key toxicities?
DR. BARRIENTOS: One key toxicity that is very particular to this drug that may happen overnight and is very striking is transaminitis. It usually happens more with non-Hodgkin lymphoma patients compared to relapsed CLL patients, but transaminitis can still be very severe. Patients can develop transaminitis even after more than a cycle on therapy even if they were tolerating the drug well without other issues. It’s very important to educate physicians and healthcare providers about the need to monitor the liver function tests, at least every 2 weeks for the first 2 months. Transaminitis events can be very prompt, very rapid, and usually asymptomatic. My patients that developed transaminitis never complained and had we not been cautious about it, we may have missed it.
DR. BROWN: Yes, I even check weekly. The recent safety analysis said the overall incidence of grade 3 to 4 transaminitis is about 15% in relapse patients.7 That’s pretty significant.
DR. JONES: I think it’s important to know that the transaminitis, if monitored carefully and managed with drug interruption and/or dose reduction upon reintroduction, need not lead to discontinuation. Discontinuations for transaminitis are actually the minority of patients who experience the side effect.
DR. BROWN: Absolutely. Do you want to comment on some of the other side effects that may more often lead to discontinuation?
DR. JONES: We should mention that there are some preclinical animal data suggesting that the molecular target of idelalisib, the PI3K delta isoform, is an important signaling molecule in regulatory T cells important for self-tolerance. While it has efficacy in treating B-cell disorders, inhibiting PI3K-delta may also be impairing T regulatory cell function. That may be what leads to the more characteristic later side effects of idelalisib, including pneumonitis and colitis. Pneumonitis is relatively rare, but because it can masquerade as other respiratory ailments in an older patient population with comorbid medical illnesses like chronic obstructive pulmonary disease and preexisting immune dysfunction because of CLL or prior therapy, inflammatory pneumonitis can be misdiagnosed. This rare but potentially life-threatening complication of idelalisib treatment requires prompt recognition, discontinuation of the drug, and appears to be most effectively managed with corticosteroids.
The other commonly occurring late toxicity, colitis, is often one that also eludes prompt recognition since many times patients are seen by primary care practitioners between oncology visits, and these doctors may not yet be aware that colitis can occur as a late side effect of idelalisib. Sometimes the colitis is misdiagnosed as gastroenteritis or Clostridium difficile colitis and eludes initial management. Like the pneumonitis, this problem, which may occur in more than a quarter of patients, is really best managed by prompt recognition and, in many cases, interruption of the drug. In some cases, patients have been managed with interruption of the drug and perhaps rechallenge at a lower dose, but in many other cases, colitis has been a treatment-limiting side effect and is a leading cause of drug discontinuation for toxicity.
DR. BROWN: Yes, I would agree. It can occur even at much later times in people who have tolerated the drug for even a couple of years, which is surprising compared to typical drug-related diarrhea.
DR. JONES: Right. With many other drugs, a patient starts taking the drug and expects the treatment-related side effects to become manifest very early. The diarrhea and rash associated with ibrutinib, for instance, are really timed very close to drug initiation, similar to antibiotics and other medications that we commonly prescribe. When side effects occur late in the course of treatment, I think it is just not on anyone’s radar to suspect that they could be related to a drug that they have been receiving for some time. That is an important message to communicate to patients, as well as to doctors who are just beginning to prescribe these new drugs for the first time.
DR. BROWN: Exactly. Why don’t we turn our attention now to the approval of obinutuzumab, and review the registration trial data there and then how you’re using that in practice. Jacquie?
DR. BARRIENTOS: Obinutuzumab is a third generation monoclonal antibody targeting the CD20 receptor on B cells. It was approved in November of 2013 by the US Food and Drug Administration for use in combination with chlorambucil to treat patients with previously untreated CLL.8 The trial enrolled patients with comorbidities as measured by the Cumulative Index Rating Scale, the scale helps define fitness. The patients that participated in the registration trial were patients that due to their comorbidities would not tolerate well a chemoimmunotherapy regimen like fludarabine, cyclophosphamide, and rituximab (FCR), and possibly the combination of bendamustine and rituximab. In patients older than age 65 with multiple comorbidities, chlorambucil monotherapy is widely used worldwide due to concerns of complications from the use of other chemoimmunotherapy regimens like the ones mentioned above. In the United States, we usually see that physicians prefer to use rituximab as a single agent in frail patients with multiple comorbidities.
The combination of obinutuzumab with chlorambucil compared to chlorambucil as a single agent showed that the patients treated with the combination therapy had a higher rate of response, a higher rate of progression free survival, and an improved overall survival. The main issue with obinutuzumab is the fact that the infusion reactions are much greater than what we traditionally see with rituximab. Severe and life-threatening infusion reactions have been reported. The reactions can also be more abrupt, although they typically occur very early in infusion, so they are more predictable. If the patient develops an infusion reaction or can’t tolerate the drug, the infusion needs to be interrupted. If the patient does not experience any further infusion reaction symptoms, the infusion may be restarted at a lower rate. I believe grade 3 to grade 4 events were higher than 10% in the registration trial, with infusion reactions of any grade seen in 50%–70%, so it can be common—usually within the first day. By the third infusion, the rate of reaction decreases significantly. Most of the time after that third infusion, most patients won’t have any more issues with tolerability.
Who are the patients that develop these infusion reactions? It has been noted that the level of interleukin 6 is elevated in patients that develop an infusion reaction. That’s the reason why all patients should be premedicated with potent steroids (methylprednisolone or dexamethasone, not hydrocortisone). In addition, patients need to be premedicated with acetaminophen and an antihistamine. In the future hopefully we will be able to use other agents like tocilizumab to lessen the risk of infusion reactions, this is currently being tested in clinical trials as its use is theoretical at this point based on the observation of the elevated interleukin 6 levels.
There are other important side effects with this combination regimen that were noted in the registration trial. There was a higher rate of neutropenia in the patients receiving obinutuzumab and chlorambucil, although this did not correlate with a higher rate of grade 3 or grade 4 infections. The rate of grade 3 or 4 infections was the same all across the board in patients that received chlorambucil, chlorambucil in combination with rituximab, or chlorambucil in combination with obinutuzumab.
DR. BROWN: Are you using much obinutuzumab chlorambucil in your practice?
DR. BARRIENTOS: In select patients, yes. For untreated patients with comorbidities that are not participating in a clinical trial, we discuss with them data from the frontline bendamustine and rituximab combination and obinutuzumab and chlorambucil combination. For the most part, most patients prefer obinutuzumab with chlorambucil because the obinutuzumab chlorambucil combination might be better tolerated and possibly less myelosuppressive than the bendamustine rituximab combination. Unfortunately, most of my patients have already been treated by the time we see them. We have a minority of patients that come recently diagnosed, we just don’t see that many untreated patients.
DR. BROWN: How about you, Jeff? Are you using it?
DR. JONES: Yes, it is a consideration for frontline therapy in patients who don’t have deletion 17p. As we discussed before, most of us have already adopted ibrutinib as our first choice in that 17p deleted population outside of clinical trial. For the remainder of patients, I think the first question remains whether their age and health are permissive to safely give FCR, since that regimen has been associated with the best survival outcomes, even some really long survival, in a group of patients with IgVH mutated, favorable cytogenetic risk disease.
For patients who are not eligible or willing to receive FCR, I think the choice between bendumustine and rituximab (BR) and chlorambucil and obinutuzumab is a relatively challenging one. Part of the reason is that while the overall response rates and complete response rates are lower with obinutuzumab and chlorambucil, the toxicity is also a bit lower. That makes it an appealing choice, particularly when we have the availability of drugs like ibrutinib and idelalisib in the second line. For older patients with comorbid medical illnesses in particular, it may be that the duration of first remission after chemotherapy may not matter as much when we have more effective second line options.
DR. BROWN: Yes, I think that’s definitely true. I just want to highlight two points. Your point about the long-term efficacy of FCR, particularly in the IgVH mutated patients—it is important to note that we now have data from both MD Anderson and the German CLL Study Group. The MD Anderson data with 10 year follow up, 60% of that genetic subgroup are progression free after FCR suggesting that a subset of them may in fact be cured. We don’t want to forget that with the excitement of the new inhibitors. I would second your point also about the potential toxicities of BR which can be as myelosuppressive as FCR even though it is not in every case. Again, it’s very important to assess the comorbidities of the patient not just for FCR but also for BR, particularly when FCR has this chance of very long-term remission which is not seen with BR.
DR. JONES: Yes, and there’s also a risk for opportunistic infections with both regimens. Like fludarabine-treated patients, there are patients treated with bendumustine who experience pneumocystis pneumonia or viral reactivation from immune suppression beyond just the neutropenia.
DR. BROWN: Yes, absolutely. Let’s talk briefly about where we see CLL therapy going in the next few years given these exciting new drugs. I’ll just leave that open and see what you have to say. Jacquie?
DR. BARRIENTOS: Some of the possible developments that we may see over the next couple of years are the use of these targeted agents or small molecules as initial therapy either as monotherapy or in combination regimens. We are expecting to see the data of the clinical trial of frontline ibrutinib against chlorambucil in patients that are older than age 65. Idelalisib has other ongoing clinical trials in the frontline setting as monotherapy and in combination therapy. Data have been presented of idelalisib in combination with rituximab as frontline therapy. It was interesting to note that some of these side effects that we saw in the relapsed or refractory setting occurred more often in patients in the frontline setting, although efficacy was very high. These promising data may eventually lead to a change in the way that we treat patients in the frontline, not only as monotherapy. There are several clinical trials that incorporate chemoimmunotherapy with these new targeted agents to see if maybe we will obtain deeper remissions or longer duration of response.
DR. JONES: What preliminary data exist in small phase 1 or phase 2 studies suggest that the new agents may be even more effective in previously untreated disease, with higher overall response rates, higher complete response rates, and more durable remissions than observed among patients with relapsed and refractory disease.9,10 These results underscore that the individual agents are among the most effective drugs that have been developed for CLL in terms of their single-agent activity. If you include the oral BCL-2 inhibitor in development, venetoclax, these drugs have really had remarkable single-agent efficacy. If these newer agents are like older cytotoxic chemotherapy agents, like fludarabine, they may become superstars when used in combination. While we will soon see these drugs move into the frontline setting as single agents, I think the real potential for magic is when they get combined. There we may see the kinds of deep remissions that we only achieve now with chemoimmunotherapy, remissions that will allow similar long-term treatment-free survival without cytotoxic chemotherapy. I’d like nothing more than to see a 60% 10 year survival after a nonchemotherapy-containing combination that emerges when we use these new drugs in ways that maximize their benefit in combination.
DR. BROWN: I would certainly agree. I think that although we have remarkable single-agent activity of these drugs, we know that in the context of single-agent activity, resistance is likely to develop over time. For a subset of patients that may not matter. If they’re older and have comorbidities, they may get enough durability of response from their first single agent that it doesn’t matter, particularly the patients with lower risk CLL. For our younger patients, I think the combinations will have the opportunity to minimize the development of resistance and also allow shorter courses of therapy so that patients can be off treatment still with deep remissions. That is what most excites me about the future of these agents.
Let’s just talk about the future of watch and wait. We now have great drugs and great therapies. Are you considering treatment earlier in any of your patients at this point, Jacquie?
DR. BARRIENTOS: I have been very hesitant to start our patients on any drug before they develop symptoms from the disease. I still wait to initiate therapy according to the International Workshop on CLL (IWCLL) guidelines.11 The reason is that anytime that we start a new agent, the patients may develop some mutation that is driven by these new agents. At this point, there are no data for us to start therapy before symptoms develop. The German CLL study group is currently doing a high risk study in patients that are asymptomatic but have a high risk profile like 17p deletion to see if maybe a drug like ibrutinib could have a benefit. I think that will be very interesting once the data come out. There are certain patients with whom you are always wondering, “Am I doing more harm by withholding therapy at this moment?” So far, early intervention with chemotherapy before symptoms has not shown any additional benefit. We still do the watch and wait for the time being, but this may change in the future for certain patients with certain high-risk characteristics.
DR. BROWN: Yes, I share your concerns about the possibility of evolution of the disease in the context of any treatment. Even though we hope that there will be less clonal evolution with these targeted inhibitors, there is some increasing evidence that some adverse clones like TP53 mutated or 17p deleted clones are preexisting in many cases. Then, under the influence of treatment, these mutations become more evident, ie a higher percentage of the disease. Personally, I would like to see overall survival data before we start treating patients earlier.
DR. JONES: I would absolutely agree. I think if you want to undertake the systematic treatment of patients before they actually progress clinically, those are the kind of data that you want. You want to know whether you are impacting the natural history of the disease. I’ll take a slightly contrarian point of view in talking about elderly patients in particular. Some of our colleagues who treat low-grade lymphoma—where watch and wait is often employed in the initial asymptomatic setting—have argued that there is a strong rationale to treat earlier rather than later because you may find that toxicity becomes more prohibitive if you wait until the patients become ill. There’s a somewhat perverse logic underlying our current approach to therapy—we don’t treat to maintain health, we treat when patients become sick. I think there is room for a slightly different approach still operating within current consensus guidelines. There is a group of elderly patients with comorbid medical illnesses that as it seems their disease is starting to progress, I am inclined to consider—at least discuss—the feasibility of treatment then as a way of limiting both the morbidity from the disease, as well as the morbidity of treatment. When the only available treatments were chemotherapy drugs like fludarabine, which has not clearly resulted in survival benefits for elderly patients, that was as feasible as when the treatment is perhaps obinutuzumab and chlorambucil, or maybe in the near future drugs like ibrutinib and idelalisib. Therefore I think we may all want to start rethinking our approach, cautiously. Ultimately, this is a research question.
DR. BROWN: That’s interesting. I certainly agree that in the setting of chemotherapy or chemoimmunotherapy patients with a higher disease burden have a lot harder time getting started on therapy. If in fact the targeted inhibitors move to upfront therapy, it’s not so clear to me that those drugs have more initial toxicity in patients with a greater disease burden—at least for ibrutinib. Do you disagree?
DR. JONES: No, I think that’s true. You will even hear an argument sometimes that a single-agent rituximab for follicular lymphoma or obinutuzumab and chlorambucil would be better tolerated, and you have more room for management of toxicity when you give them to patients who are healthier at baseline. Part of that is with less extensive disease, but you’re right. I agree that there is no indication right now that the novel, targeted agents are more toxic in older patients. However, I will say that our own retrospective analysis from Ohio State suggested that age was one of the factors associated with early discontinuation among our patients.4
DR. BROWN: Right, but to me, the fact that age is a predictor of less tolerability of therapy suggests that maybe we should save the therapy until the patient really needs it. The toxicities of ibrutinib are not as clearly disease-burden related necessarily.
DR. JONES: Yeah, I think that our disagreement really suggests that it’s a question to study.
As the treatment becomes more manageable and potentially more effective, you start to question whether our goal is to treat patients as they become ill, or to prevent them from ever becoming ill in the first place.DR. BROWN: Oh, absolutely.
DR. JONES: These are important questions that we will necessarily revisit. As the treatment becomes more manageable and potentially more effective, you start to question whether our goal is to treat patients as they become ill, or to prevent them from ever becoming ill in the first place.
DR. BROWN: Right, absolutely. I would say that I feel that we don’t always let the patients become symptomatically ill even in following IWCLL criteria. For example, their counts may be relatively poor, requiring treatment, but the patients are not yet suffering from that.
DR. JONES: Right.
DR. BROWN: I think this was a great discussion. It’s obviously an extremely exciting time in CLL research as we learn how to use our targeted inhibitors, our new antibodies, and hopefully soon we’ll have another targeted inhibitor with ABT199 the BCL-2 inhibitor. Jacquie or Jeff, do you have any points you would like to add before we wrap up?
DR. BARRIENTOS: No. I think we covered most of the important concepts.
DR. JONES: I will just say that with analogy to a cousin disease, chronic myeloid leukemia, after imatinib and the subsequent oral kinase inhibitors were introduced in that disease people thought that the final chapter of the story had been. I think we’re going to find the same thing in CLL medicine. These phenomenally effective agents, safer than the ones we have had available to employ before, are going to open up a whole new range of investigations that we will continue innovating over the next decade.
DR. BROWN: To summarize, in 2014 we saw four new drug approvals for CLL, including two new antibodies for upfront therapy, obinutuzumab and ofatumumab, and two new targeted inhibitors for relapsed therapy, ibrutinib and idelalisib. These innovations are starting to revolutionize the treatment of CLL for the benefit of our patients. However, many questions remain about how best to use each of these drugs, about toxicity, and about resistance. The next 5 years in CLL research will be a very exciting time as we start to answer these questions. Hopefully, ultimately, we will cure more and more of our patients, maybe eventually all of them.
References
1. Byrd JC, Furman RR, Coutre SE, et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med. 2013;369(1):32–42.
2. Byrd JC, Brown JR, O’Brien S, et al. for the RESONATE Investigators. Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med. 2014;371(3):213–223.
3. Jain P, Keating M, Wierda W, et al. Outcomes of patients with chronic lymphocytic leukemia after discontinuing ibrutinib. Blood. 2015;125(13):2062–2067.
4. Maddocks KJ, Ruppert AS, Lozanski G, et al. Etiology of ibrutinib therapy discontinuation and outcomes in patients with chronic lymphocytic leukemia. JAMA Oncol. 2015;1(1):80–87.
5. Brown JR, Byrd JC, Coutre SE, et al. Idelalisib, an inhibitor of phosphatidylinositol 3-kinase p110δ, for relapsed/refractory chronic lymphocytic leukemia. Blood. 2014;123(22):3390–3397.
6. Furman RR, Sharman JP, Coutre SE, et al. Idelalisib and rituximab in relapsed in chronic lymphocytic leukemia. N Engl J Med. 2014;370(11):997–1007.
7. Coutre S, Leonard J, Flowers C, et al. Idelalisib monotherapy results in durable responses in patients with relapsed or refractory Waldenstrom’s macroglobulinemia (WM). Poster presented at: 20th Congress of European Hematology Association; June 11–14, 2015; Vienna, Austria. Abstract P690.
8. Goede V, Fischer K, Busch R, et al. Obinutuzumab plus chlorambucil in patients with CLL and coexisting conditions. N Engl J Med. 2014;370(12):1101–1110.
9. O’Brien S, Furman RR, Coutre SE, et al. Ibrutinib as initial therapy for elderly patients with chronic lymphocytic leukaemia or small lymphocytic lymphoma: an open-label, multicentre, phase 1b/2 trial. Lancet Oncol. 2014;15(1):48–58.
10. O’Brien S, Lamanna N, Kipps TJ, et al. Update of a phase 2 study of idelalisib in combination with rituximab in treatment-naïve patients ≥65 years with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL). Program and abstracts of the 56th ASH Annual Meeting and Exposition; December 6–9, 2014; San Francisco, CA. Abstract 1994.
11. Hallek M, Cheson BD, Catovsky D, et al. for the International Workshop on Chronic Lymphocytic Leukemia. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood. 2008;111(12):5446–5456.
Moderated by: Jennifer R. Brown, MD, PhD1
Discussants: Jeffrey A. Jones, MD, MPH2; Jacqueline C. Barrientos, MD3
From the Dana-Farber Cancer Institute and Harvard Medical School, Boston, MA1; Ohio State University, Columbus, OH2; Hofstra North Shore-LIJ School of Medicine, Lake Success, NY
Address for correspondence: Jennifer R. Brown, MD, PhD, Dana-Farber Cancer Institute, 450 Brookline Avenue, Boston, MA 02215
E-mail: [email protected]
Biographical Sketch
From Dana-Farber Cancer Institute and Harvard Medical School:
Jennifer R. Brown, MD, PhD is the Director of the CLL Center of the Division of Hematologic Malignancies at Dana-Farber Cancer Institute and an Associate Professor of Medicine at Harvard Medical School in Boston, Massachusetts. Dr. Brown completed a BS and MS simultaneously in molecular biophysics and biochemistry (MB&B) at Yale, graduating summa cum laude with distinction in MB&B. She proceeded to Harvard Medical School where she received her MD and PhD in molecular genetics in 1998 and was awarded the James Tolbert Shipley Prize for research accomplishment in the graduating class. She then served as an intern and resident in Internal Medicine at Massachusetts General Hospital followed by fellowship in Hematology and Medical Oncology at the Dana-Farber Cancer Institute. Dr. Brown joined the faculty of DFCI and Harvard Medical School in 2004, where she has an active clinical-translational research program in CLL.
Her particular interests include the development of novel targeted therapeutics for CLL, as well as the genomics of CLL. She has been instrumental in the clinical development of both idelalisib and ibrutinib, leading to their regulatory approvals in CLL.
In the area of genomics she has been instrumental in the description of the somatic mutation profile of CLL, and is now particularly interested in the implementation of genomic technology in the clinic, including for prognosis and targeted therapy. She also has a longstanding research interest and focus on the inherited predisposition to CLL.
To date she has published over 130 papers in the scientific literature, predominantly in CLL. She is an active member of the CLL Research Consortium and serves on the Alliance Leukemia and Leukemia Correlative Science Committees as well as the NIH Cancer Biomarkers Study Section. In 2014 she was the recipient of two awards from Dana-Farber Cancer Institute, the Clinical Innovation Award, as well as the George Canellos Award for Excellence in Clinical Investigation and Patient Care. She enjoys a worldwide reputation as a CLL expert and is in much demand as an international speaker.
From Hofstra North Shore-LIJ School of Medicine:
Jacqueline C. Barrientos, MD, is Attending Physician at the Chronic Lymphocytic Leukemia (CLL) Research & Treatment Program of the Division of Hematology and Medical Oncology, Department of Medicine, in the North Shore – LIJ Cancer Institute in Lake Success, New York. She is also Assistant Professor of Medicine at the Hofstra North Shore-LIJ School of Medicine. Dr. Barrientos works in close collaboration with her mentors, Dr. Kanti R. Rai and Dr. Nicholas Chiorazzi of the Feinstein Institute for Medical Research.
Dr. Barrientos received her medical degree at the Ponce School of Medicine in Puerto Rico, where she was elected vice-president of Alpha Omega Alpha Honor Medical Society. During her medical studies, she was the recipient of two Research Fellowship Awards from the Howard Hughes Medical Institute. She completed her internship and residency in internal medicine at Yale-New Haven Hospital of the Yale School of Medicine, and her fellowship in Hematology/Oncology at New York Presbyterian Hospital of Weill Cornell Medical College in New York City, where she also served as Chief Fellow. She is board certified in internal medicine, hematology and oncology.
Dr. Barrientos’ research focus is on chronic lymphocytic leukemia and lymphoma. She has extensive experience with the new promising agents targeting the B-cell receptor signaling pathway in B-cell malignancies, serving as Principal Investigator on several phase I-III clinical trials.
Dr. Barrientos actively participates in multi-institutional clinical trials with the Chronic Lymphocytic Leukemia Research Consortium (CRC) and the Alliance for Clinical Trials in Oncology. She is a cadre member of the Leukemia Committee of the Alliance for Clinical Trials in Oncology and in this capacity is co-chair of a study comparing chemoimmunotherapy against a combination of targeted agents. She is a member of the American Society of Clinical Oncology (ASCO) and the American Society of Hematology (ASH).
She has been an invited speaker for ASCO University “CLL Tumor Board”, ASH “State of the Art Symposium”, and “Highlights of ASH in Latin America”. Dr. Barrientos is the recipient of a 2015 American Society of Hematology-Harold Amos Medical Faculty Development Program (ASH-AMFDP) Fellowship award.
DR. BROWN: I am Jennifer Brown, Director of the Chronic Lymphocytic Leukemia (CLL) Center at Dana-Farber Cancer Institute, and Associate Professor of Medicine at Harvard Medical School. Today, I will be speaking with two of my esteemed CLL colleagues, Drs. Jeffrey Jones and Jacqueline Barrientos, about the new drug approvals in CLL.
DR. BARRIENTOS: I’m Jacqueline Barrientos, Assistant Professor of Hematology/Oncology at the Hofstra North Shore-LIJ School of Medicine, and Attending Hematologist at the CLL Research and Treatment Program in Long Island, NY. Our center participates in clinical trials and we perform correlative basic research. I’m very happy to participate in this expert roundtable discussion.
DR. JONES: I’m Dr. Jeffrey Jones, Associate Professor of Internal Medicine and Section Chief for CLL in the Division of Hematology at The Ohio State University.
DR. BROWN: Thank you Jeff and Jacquie for joining me today. I think we’re all aware what an exciting time this is in CLL with the approvals last year of the targeted inhibitors ibrutinib and idelalisib as well as the new antibody approval obinutuzumab as well as the additional indication for ofatumumab. Let’s start our discussion with ibrutinib and idelalisib. Jeff, please introduce the approvals that these inhibitors received and get us started.
DR. JONES: February 2014 marked a really important time in CLL medicine with the approval of the first oral kinase inhibitor, ibrutinib, for the treatment of CLL after one prior therapy.1,2 This ushered in an entirely new era of molecularly-targeted therapy for CLL. Later that year, ibrutinib received approval for deletion 17p CLL, the highest risk genetic subtype of CLL, whether previously untreated or relapsed disease. The drug has rapidly entered the clinic, although I think most of us are still trying to determine how best to incorporate them into our practice.
DR. BROWN: Jacquie, please comment on how you’re using ibrutinib now in your practice.
DR. BARRIENTOS: In CLL patients with the presence of a mutation of TP53 or deletion 17p, we use ibrutinib. We essentially do not use chemotherapy on this particular set of patients. If, for any reason, they are not able to tolerate the drug, then we consider idelalisib, which is not approved separately for this 17p deletion indication. Idelalisib is approved for use in combination with rituximab for the treatment of relapsed or refractory CLL patients. Idelalisib has shown clinical activity in several clinical trials in patients with deletion 17p.
At this moment, we mainly are using ibrutinib or idelalisib for our relapsed or refractory CLL patients. Clinical trials are underway in the frontline setting and we hope to see the results of the frontline use of ibrutinib in elderly patients soon. As of right now, we don’t use ibrutinib as a frontline therapy unless there is a reason, and usually it’s that they carry the 17p deletion or they are participating in a clinical trial.
DR. JONES: Outside of clinical trials our practice has really been to follow the label indications for ibrutinib. For previously untreated patients, our use has been limited to patients with deletion 17p or TP53 mutated disease, as Jacquie said, since that is the group for which the drug has been approved in the frontline.
DR. BROWN: I would agree. That’s been my practice as well. We should perhaps review the data from the registration trial that led to the ibrutinib approval for relapsed refractory CLL. The initial approval was from the stage IB2 study and was an accelerated approval.1 The confirmatory registration trial, RESONATE, randomized relapsed refractory CLL patients to ibrutinib versus the anti-CD20 antibody ofatumumab.2 Ibrutinib was found to be significantly better in improving both progression free and overall survival, although there was crossover later. As a result, this has moved into our relapse refractory use very rapidly. Although we still use chemoimmunotherapy for upfront therapy for patients without 17p deletion, for those in relapse we have moved entirely to targeted inhibitors. Would you both agree?
DR. JONES: For sure. I think it is very hard in 2015 to think of the patient for whom chemo-immunotherapy is the better choice than ibrutinib for relapsed disease.I think it is very hard in 2015 to think of the patient for whom chemoimmunotherapy is the better choice than ibrutinib for relapsed disease. The benefit is most marked for the group with higher-risk disease as characterized by genetic risk features, not just deletion 17p, but patients with complex abnormal karyotype or deletions of chromosome 11q. All of these patients particularly benefit from treatment with ibrutinib in the second line vs chemoimmunotherapy, as do patients who had either a suboptimal response to frontline chemoimmunotherapy or a brief duration of first remission. All of us are sometimes asked, “Well, who is the patient with relapsed CLL for whom ibrutinib is the best choice?” Right now, in most clinical situations, my response is, “For which patient is ibrutinib not the best choice in first relapse?”
DR. BROWN: That’s actually a good question. Jacquie, how would you answer that? Are there patients for whom you would not choose ibrutinib in first relapse?
DR. BARRIENTOS: I feel a hesitant to use ibrutinib in some patients with a particular comorbidity or medical history. For example, patients with a previous intracranial bleed or a recent history of bleeding, I would prefer to avoid using ibrutinib because there have been rare cases of spontaneous intracranial bleed or severe bleeding after trauma. The other type of patient where I would be cautious is a patient with uncontrolled atrial fibrillation because there are data that in the minority of patients (up to 10% of patients), atrial fibrillation has been an issue. We have some patients that are so frail that they couldn’t tolerate another episode of uncontrolled atrial fibrillation and as such they would not be ideal candidates for the drug. For that type of patient, I would probably abstain from using ibrutinib and consider the use of another therapy. Finally, I would be careful in patients on antiplatelet and anticoagulation therapy because ibrutinib affects platelet functions increasing the risk of bleeding. The bleeding events seen with ibrutinib are mostly grade 1 or grade 2. If the patients have had a serious bleed or serious gastrointestinal bleed or a recent surgery, then I would preferably use another agent.
DR. BROWN:Yes, so that gets to the toxicities of ibrutinib. The more medically significant ones do include perhaps a 5% to 10% risk of atrial fibrillation as well as bleeding risks, which as Jacquie points out are low and usually low grade, but there are occasional higher-risk bleeds. I personally still try to avoid combining anticoagulation with ibrutinib, as we don’t fully understand the mechanism or the risk factors for the more serious bleeds. Jeff, please comment.
DR. JONES: I think the data from the randomized study are actually the most helpful since, as you say, mild bleeding events (grade 1 or 2) were indeed more common amongst the group of patients who were treated with ibrutinib.2 Major bleeding events—which are typically defined as intracranial hemorrhage, bleeding requiring transfusion, or inpatient management—were actually similar between the two arms of the trial. An important caveat in interpreting these data is to know that patients in this trial were excluded if they were anticoagulated with warfarin, if they had an antecedent history of intracranial hemorrhage or recent bleeding, or recent surgery. In line with those exclusions, we will often consider other options. If there is any specific concern for bleeding, such as a patient who has experienced bleeding complications during routine anticoagulation, which is also a patient for whom ibrutinib may not be the best choice. In these clinical situations, it is important to involve the patient in discussing the balance of risks and benefits.
DR. BROWN: Yes. Jacquie, please comment on some of the side effects the patients on ibrutinib have, and how you manage those.
DR. BARRIENTOS: I usually mention to my patients that over the first 2 or 3 months about half of them will have a possible change in their bowel movements. Usually they report some diarrhea or loose stools. Usually these episodes are mild, nothing that requires hospitalization. In any case, if it becomes severe, I definitely make sure that it’s not an infection. We all know that our patients with CLL are prone to infections. The other thing I tell the patients is that in some cases patients may develop a rash on the skin. Many times it may look like a rash, but it’s actually ecchymosis—an effect from the drug on the platelets. Essentially, they are grade 1 and don’t require intervention. I just tell them that eventually they will go away. It can be scary for the patients if they are not expecting these. We have had patients with large areas of hematomas in the arms or in the legs. That is unexpected with a drug that they are taking by mouth. They usually expect that with other drugs like warfarin, but not with ibrutinib, so it is important to mention before they start the drug.
Last but not least, I mention the fact that they may get arthralgias—joint pain—in different areas of their bodies. I would say that I see that in about 20% to 30% of patients. Usually it’s very mild, but on occasion I’ve had patients with arthritis so severe that we’ve had to hold the drug and give them some steroids to help them improve their ability to maneuver their hands or move their joints. I’m sure you have seen some of those same side effects.
DR. BROWN: Yes, definitely. In general, it’s pretty well tolerated but it’s best to warn the patients, then there are no surprises. Let’s turn our attention for a moment back to the highest risk genetic subgroup, the 17p deleted patients—which Jeff had mentioned get particularly strong benefit from ibrutinib. This is certainly true, although it’s also the case that it appears, depending on the data set you look at, that they may relapse earlier than other patients on ibrutinib. In the original phase IB2, the median progression survival for the 17p deleted patients was 28 months. More recent data from Ohio State and MD Anderson suggest that complex karyotype may be a risk factor.3,4 Given these data, how are you two handling the question of allogeneic stem cell transplantation for these patients in this new era?
DR. BARRIENTOS: At our center, if the patient is young and they have access and are fit to tolerate a reduced-intensity allogeneic transplant, we recommend that they be evaluated for a transplant. Unfortunately, if they lose the response to the best drug available for their particular genetic mutation, then we have limited options of salvage therapy. It’s risky to think that they will not relapse at some point, and then what do we do at the time of relapse? We can use other targeted agents that are available, like idelalisib, with the knowledge that they may not always respond to the salvage therapy. Promising clinical activity has been reported for patients with 17p deletion treated with venetoclax in clinical trials. Venetoclax is a new targeted agent in development stages but the drug is only available in clinical trials.Promising clinical activity has been reported for patients with 17p deletion treated with venetoclax in clinical trials. Venetoclax is a new targeted agent in development stages but the drug is only available in clinical trials. One problem is that in order to participate in a clinical trial the patient needs to be able to get to the center to get the drug. Additionally, the patient needs to satisfy certain eligibility criteria for study entry. For these patients that stop responding to ibrutinib, the options of care are very limited at this time. This is the reason why I send all my young patients with a 17p deletion for a transplant evaluation.
At the end of the day it is tough to convince the patients to go for a transplant when they’re feeling in excellent shape. It’s still difficult to make a case to go for a procedure that may have its complications on its own. It is well known that there are some increased mortality risks and infection risks that can arise as a result of a transplant. They may not want to do it because they are feeling so great with their routine. I still sit down and have a long frank talk with the patients, especially if they have complex karyotype and 17p deletion. I am concerned that at some point they’re going to stop responding to ibrutinib.
DR. BROWN: That’s generally my practice as well. What about you, Jeff?
DR. JONES: Until there is greater clarity regarding which of the newer agents can salvage patients progressing after ibrutinib, I think it is still important for younger, transplant eligible patients with deletion 17p disease to undergo evaluation for allograft. It remains potentially curative therapy, and I think the availability of ibrutinib has not really changed the importance of that evaluation.
DR. BROWN: Yes, I would agree. I think that was a good discussion on ibrutinib. Why don’t we turn our attention now to idelalisib, the phosphoinositide 3-kinase (PI3K) inhibitor. How are you using idelalisib in your practices? Is this after ibrutinib in general?
DR. JONES: Published data regarding the sequencing of the new agents are relatively limited since all of the registration trials for idelalisib excluded patients who had received prior therapy with an inhibitor of B-cell receptor signaling, including Bruton’s tyrosine kinase inhibitors like ibrutinib.5,6 A small number of patients enrolled on the phase IB2 trial of ibrutinib, as well as the subsequent randomized trial, had received prior therapy with idelalisib and responded similarly to patients who had not received prior idelalisib.1,2 In our practice, the use of idelalisib has pretty much been limited to patients who have either received prior ibrutinib or patients who are not eligible to receive ibrutinib because of some important contraindication, such as an inherited bleeding defect, perceived increased bleeding, or history of difficult to control atrial fibrillation, since that event also seems to be more likely among patients treated with ibrutinib.
DR. BROWN: How about you, Jacquie?
DR. BARRIENTOS: The same type of patient with the addition of patients with kidney disease. The rationale for this is based on the phase III trial for idelalisib and rituximab, the enrollment allowed participation of patients with decreased renal function, that was one of the entry criteria for eligibility to participate in the trial.6 In most of the ibrutinib trials the creatinine clearance needed to be adequate, whereas this was allowed to be lower on the idelalisib trials. For those patients with severe renal impairment, I tend to prefer idelalisib rather than ibrutinib—only because I feel more comfortable and have more experience treating patients with impaired kidney function with idelalisib.
DR. BROWN: I have seen some episodic elevations in creatinine in patients on ibrutinib, but they’re fairly sporadic and it’s a little hard to assess the direct drug relationship. It is true that the patients in the idelalisib studies had a high level of comorbidity deliberately on the initial registration trial and generally did reasonably well with idelalisib. The toxicity profile of idelalisib is pretty characteristic, and is potentially harder to manage than that of ibrutinib. I think it also dictates some of how it’s being used in later line therapy. Does one of you wish to comment on the pattern of the key toxicities?
DR. BARRIENTOS: One key toxicity that is very particular to this drug that may happen overnight and is very striking is transaminitis. It usually happens more with non-Hodgkin lymphoma patients compared to relapsed CLL patients, but transaminitis can still be very severe. Patients can develop transaminitis even after more than a cycle on therapy even if they were tolerating the drug well without other issues. It’s very important to educate physicians and healthcare providers about the need to monitor the liver function tests, at least every 2 weeks for the first 2 months. Transaminitis events can be very prompt, very rapid, and usually asymptomatic. My patients that developed transaminitis never complained and had we not been cautious about it, we may have missed it.
DR. BROWN: Yes, I even check weekly. The recent safety analysis said the overall incidence of grade 3 to 4 transaminitis is about 15% in relapse patients.7 That’s pretty significant.
DR. JONES: I think it’s important to know that the transaminitis, if monitored carefully and managed with drug interruption and/or dose reduction upon reintroduction, need not lead to discontinuation. Discontinuations for transaminitis are actually the minority of patients who experience the side effect.
DR. BROWN: Absolutely. Do you want to comment on some of the other side effects that may more often lead to discontinuation?
DR. JONES: We should mention that there are some preclinical animal data suggesting that the molecular target of idelalisib, the PI3K delta isoform, is an important signaling molecule in regulatory T cells important for self-tolerance. While it has efficacy in treating B-cell disorders, inhibiting PI3K-delta may also be impairing T regulatory cell function. That may be what leads to the more characteristic later side effects of idelalisib, including pneumonitis and colitis. Pneumonitis is relatively rare, but because it can masquerade as other respiratory ailments in an older patient population with comorbid medical illnesses like chronic obstructive pulmonary disease and preexisting immune dysfunction because of CLL or prior therapy, inflammatory pneumonitis can be misdiagnosed. This rare but potentially life-threatening complication of idelalisib treatment requires prompt recognition, discontinuation of the drug, and appears to be most effectively managed with corticosteroids.
The other commonly occurring late toxicity, colitis, is often one that also eludes prompt recognition since many times patients are seen by primary care practitioners between oncology visits, and these doctors may not yet be aware that colitis can occur as a late side effect of idelalisib. Sometimes the colitis is misdiagnosed as gastroenteritis or Clostridium difficile colitis and eludes initial management. Like the pneumonitis, this problem, which may occur in more than a quarter of patients, is really best managed by prompt recognition and, in many cases, interruption of the drug. In some cases, patients have been managed with interruption of the drug and perhaps rechallenge at a lower dose, but in many other cases, colitis has been a treatment-limiting side effect and is a leading cause of drug discontinuation for toxicity.
DR. BROWN: Yes, I would agree. It can occur even at much later times in people who have tolerated the drug for even a couple of years, which is surprising compared to typical drug-related diarrhea.
DR. JONES: Right. With many other drugs, a patient starts taking the drug and expects the treatment-related side effects to become manifest very early. The diarrhea and rash associated with ibrutinib, for instance, are really timed very close to drug initiation, similar to antibiotics and other medications that we commonly prescribe. When side effects occur late in the course of treatment, I think it is just not on anyone’s radar to suspect that they could be related to a drug that they have been receiving for some time. That is an important message to communicate to patients, as well as to doctors who are just beginning to prescribe these new drugs for the first time.
DR. BROWN: Exactly. Why don’t we turn our attention now to the approval of obinutuzumab, and review the registration trial data there and then how you’re using that in practice. Jacquie?
DR. BARRIENTOS: Obinutuzumab is a third generation monoclonal antibody targeting the CD20 receptor on B cells. It was approved in November of 2013 by the US Food and Drug Administration for use in combination with chlorambucil to treat patients with previously untreated CLL.8 The trial enrolled patients with comorbidities as measured by the Cumulative Index Rating Scale, the scale helps define fitness. The patients that participated in the registration trial were patients that due to their comorbidities would not tolerate well a chemoimmunotherapy regimen like fludarabine, cyclophosphamide, and rituximab (FCR), and possibly the combination of bendamustine and rituximab. In patients older than age 65 with multiple comorbidities, chlorambucil monotherapy is widely used worldwide due to concerns of complications from the use of other chemoimmunotherapy regimens like the ones mentioned above. In the United States, we usually see that physicians prefer to use rituximab as a single agent in frail patients with multiple comorbidities.
The combination of obinutuzumab with chlorambucil compared to chlorambucil as a single agent showed that the patients treated with the combination therapy had a higher rate of response, a higher rate of progression free survival, and an improved overall survival. The main issue with obinutuzumab is the fact that the infusion reactions are much greater than what we traditionally see with rituximab. Severe and life-threatening infusion reactions have been reported. The reactions can also be more abrupt, although they typically occur very early in infusion, so they are more predictable. If the patient develops an infusion reaction or can’t tolerate the drug, the infusion needs to be interrupted. If the patient does not experience any further infusion reaction symptoms, the infusion may be restarted at a lower rate. I believe grade 3 to grade 4 events were higher than 10% in the registration trial, with infusion reactions of any grade seen in 50%–70%, so it can be common—usually within the first day. By the third infusion, the rate of reaction decreases significantly. Most of the time after that third infusion, most patients won’t have any more issues with tolerability.
Who are the patients that develop these infusion reactions? It has been noted that the level of interleukin 6 is elevated in patients that develop an infusion reaction. That’s the reason why all patients should be premedicated with potent steroids (methylprednisolone or dexamethasone, not hydrocortisone). In addition, patients need to be premedicated with acetaminophen and an antihistamine. In the future hopefully we will be able to use other agents like tocilizumab to lessen the risk of infusion reactions, this is currently being tested in clinical trials as its use is theoretical at this point based on the observation of the elevated interleukin 6 levels.
There are other important side effects with this combination regimen that were noted in the registration trial. There was a higher rate of neutropenia in the patients receiving obinutuzumab and chlorambucil, although this did not correlate with a higher rate of grade 3 or grade 4 infections. The rate of grade 3 or 4 infections was the same all across the board in patients that received chlorambucil, chlorambucil in combination with rituximab, or chlorambucil in combination with obinutuzumab.
DR. BROWN: Are you using much obinutuzumab chlorambucil in your practice?
DR. BARRIENTOS: In select patients, yes. For untreated patients with comorbidities that are not participating in a clinical trial, we discuss with them data from the frontline bendamustine and rituximab combination and obinutuzumab and chlorambucil combination. For the most part, most patients prefer obinutuzumab with chlorambucil because the obinutuzumab chlorambucil combination might be better tolerated and possibly less myelosuppressive than the bendamustine rituximab combination. Unfortunately, most of my patients have already been treated by the time we see them. We have a minority of patients that come recently diagnosed, we just don’t see that many untreated patients.
DR. BROWN: How about you, Jeff? Are you using it?
DR. JONES: Yes, it is a consideration for frontline therapy in patients who don’t have deletion 17p. As we discussed before, most of us have already adopted ibrutinib as our first choice in that 17p deleted population outside of clinical trial. For the remainder of patients, I think the first question remains whether their age and health are permissive to safely give FCR, since that regimen has been associated with the best survival outcomes, even some really long survival, in a group of patients with IgVH mutated, favorable cytogenetic risk disease.
For patients who are not eligible or willing to receive FCR, I think the choice between bendumustine and rituximab (BR) and chlorambucil and obinutuzumab is a relatively challenging one. Part of the reason is that while the overall response rates and complete response rates are lower with obinutuzumab and chlorambucil, the toxicity is also a bit lower. That makes it an appealing choice, particularly when we have the availability of drugs like ibrutinib and idelalisib in the second line. For older patients with comorbid medical illnesses in particular, it may be that the duration of first remission after chemotherapy may not matter as much when we have more effective second line options.
DR. BROWN: Yes, I think that’s definitely true. I just want to highlight two points. Your point about the long-term efficacy of FCR, particularly in the IgVH mutated patients—it is important to note that we now have data from both MD Anderson and the German CLL Study Group. The MD Anderson data with 10 year follow up, 60% of that genetic subgroup are progression free after FCR suggesting that a subset of them may in fact be cured. We don’t want to forget that with the excitement of the new inhibitors. I would second your point also about the potential toxicities of BR which can be as myelosuppressive as FCR even though it is not in every case. Again, it’s very important to assess the comorbidities of the patient not just for FCR but also for BR, particularly when FCR has this chance of very long-term remission which is not seen with BR.
DR. JONES: Yes, and there’s also a risk for opportunistic infections with both regimens. Like fludarabine-treated patients, there are patients treated with bendumustine who experience pneumocystis pneumonia or viral reactivation from immune suppression beyond just the neutropenia.
DR. BROWN: Yes, absolutely. Let’s talk briefly about where we see CLL therapy going in the next few years given these exciting new drugs. I’ll just leave that open and see what you have to say. Jacquie?
DR. BARRIENTOS: Some of the possible developments that we may see over the next couple of years are the use of these targeted agents or small molecules as initial therapy either as monotherapy or in combination regimens. We are expecting to see the data of the clinical trial of frontline ibrutinib against chlorambucil in patients that are older than age 65. Idelalisib has other ongoing clinical trials in the frontline setting as monotherapy and in combination therapy. Data have been presented of idelalisib in combination with rituximab as frontline therapy. It was interesting to note that some of these side effects that we saw in the relapsed or refractory setting occurred more often in patients in the frontline setting, although efficacy was very high. These promising data may eventually lead to a change in the way that we treat patients in the frontline, not only as monotherapy. There are several clinical trials that incorporate chemoimmunotherapy with these new targeted agents to see if maybe we will obtain deeper remissions or longer duration of response.
DR. JONES: What preliminary data exist in small phase 1 or phase 2 studies suggest that the new agents may be even more effective in previously untreated disease, with higher overall response rates, higher complete response rates, and more durable remissions than observed among patients with relapsed and refractory disease.9,10 These results underscore that the individual agents are among the most effective drugs that have been developed for CLL in terms of their single-agent activity. If you include the oral BCL-2 inhibitor in development, venetoclax, these drugs have really had remarkable single-agent efficacy. If these newer agents are like older cytotoxic chemotherapy agents, like fludarabine, they may become superstars when used in combination. While we will soon see these drugs move into the frontline setting as single agents, I think the real potential for magic is when they get combined. There we may see the kinds of deep remissions that we only achieve now with chemoimmunotherapy, remissions that will allow similar long-term treatment-free survival without cytotoxic chemotherapy. I’d like nothing more than to see a 60% 10 year survival after a nonchemotherapy-containing combination that emerges when we use these new drugs in ways that maximize their benefit in combination.
DR. BROWN: I would certainly agree. I think that although we have remarkable single-agent activity of these drugs, we know that in the context of single-agent activity, resistance is likely to develop over time. For a subset of patients that may not matter. If they’re older and have comorbidities, they may get enough durability of response from their first single agent that it doesn’t matter, particularly the patients with lower risk CLL. For our younger patients, I think the combinations will have the opportunity to minimize the development of resistance and also allow shorter courses of therapy so that patients can be off treatment still with deep remissions. That is what most excites me about the future of these agents.
Let’s just talk about the future of watch and wait. We now have great drugs and great therapies. Are you considering treatment earlier in any of your patients at this point, Jacquie?
DR. BARRIENTOS: I have been very hesitant to start our patients on any drug before they develop symptoms from the disease. I still wait to initiate therapy according to the International Workshop on CLL (IWCLL) guidelines.11 The reason is that anytime that we start a new agent, the patients may develop some mutation that is driven by these new agents. At this point, there are no data for us to start therapy before symptoms develop. The German CLL study group is currently doing a high risk study in patients that are asymptomatic but have a high risk profile like 17p deletion to see if maybe a drug like ibrutinib could have a benefit. I think that will be very interesting once the data come out. There are certain patients with whom you are always wondering, “Am I doing more harm by withholding therapy at this moment?” So far, early intervention with chemotherapy before symptoms has not shown any additional benefit. We still do the watch and wait for the time being, but this may change in the future for certain patients with certain high-risk characteristics.
DR. BROWN: Yes, I share your concerns about the possibility of evolution of the disease in the context of any treatment. Even though we hope that there will be less clonal evolution with these targeted inhibitors, there is some increasing evidence that some adverse clones like TP53 mutated or 17p deleted clones are preexisting in many cases. Then, under the influence of treatment, these mutations become more evident, ie a higher percentage of the disease. Personally, I would like to see overall survival data before we start treating patients earlier.
DR. JONES: I would absolutely agree. I think if you want to undertake the systematic treatment of patients before they actually progress clinically, those are the kind of data that you want. You want to know whether you are impacting the natural history of the disease. I’ll take a slightly contrarian point of view in talking about elderly patients in particular. Some of our colleagues who treat low-grade lymphoma—where watch and wait is often employed in the initial asymptomatic setting—have argued that there is a strong rationale to treat earlier rather than later because you may find that toxicity becomes more prohibitive if you wait until the patients become ill. There’s a somewhat perverse logic underlying our current approach to therapy—we don’t treat to maintain health, we treat when patients become sick. I think there is room for a slightly different approach still operating within current consensus guidelines. There is a group of elderly patients with comorbid medical illnesses that as it seems their disease is starting to progress, I am inclined to consider—at least discuss—the feasibility of treatment then as a way of limiting both the morbidity from the disease, as well as the morbidity of treatment. When the only available treatments were chemotherapy drugs like fludarabine, which has not clearly resulted in survival benefits for elderly patients, that was as feasible as when the treatment is perhaps obinutuzumab and chlorambucil, or maybe in the near future drugs like ibrutinib and idelalisib. Therefore I think we may all want to start rethinking our approach, cautiously. Ultimately, this is a research question.
DR. BROWN: That’s interesting. I certainly agree that in the setting of chemotherapy or chemoimmunotherapy patients with a higher disease burden have a lot harder time getting started on therapy. If in fact the targeted inhibitors move to upfront therapy, it’s not so clear to me that those drugs have more initial toxicity in patients with a greater disease burden—at least for ibrutinib. Do you disagree?
DR. JONES: No, I think that’s true. You will even hear an argument sometimes that a single-agent rituximab for follicular lymphoma or obinutuzumab and chlorambucil would be better tolerated, and you have more room for management of toxicity when you give them to patients who are healthier at baseline. Part of that is with less extensive disease, but you’re right. I agree that there is no indication right now that the novel, targeted agents are more toxic in older patients. However, I will say that our own retrospective analysis from Ohio State suggested that age was one of the factors associated with early discontinuation among our patients.4
DR. BROWN: Right, but to me, the fact that age is a predictor of less tolerability of therapy suggests that maybe we should save the therapy until the patient really needs it. The toxicities of ibrutinib are not as clearly disease-burden related necessarily.
DR. JONES: Yeah, I think that our disagreement really suggests that it’s a question to study.
As the treatment becomes more manageable and potentially more effective, you start to question whether our goal is to treat patients as they become ill, or to prevent them from ever becoming ill in the first place.DR. BROWN: Oh, absolutely.
DR. JONES: These are important questions that we will necessarily revisit. As the treatment becomes more manageable and potentially more effective, you start to question whether our goal is to treat patients as they become ill, or to prevent them from ever becoming ill in the first place.
DR. BROWN: Right, absolutely. I would say that I feel that we don’t always let the patients become symptomatically ill even in following IWCLL criteria. For example, their counts may be relatively poor, requiring treatment, but the patients are not yet suffering from that.
DR. JONES: Right.
DR. BROWN: I think this was a great discussion. It’s obviously an extremely exciting time in CLL research as we learn how to use our targeted inhibitors, our new antibodies, and hopefully soon we’ll have another targeted inhibitor with ABT199 the BCL-2 inhibitor. Jacquie or Jeff, do you have any points you would like to add before we wrap up?
DR. BARRIENTOS: No. I think we covered most of the important concepts.
DR. JONES: I will just say that with analogy to a cousin disease, chronic myeloid leukemia, after imatinib and the subsequent oral kinase inhibitors were introduced in that disease people thought that the final chapter of the story had been. I think we’re going to find the same thing in CLL medicine. These phenomenally effective agents, safer than the ones we have had available to employ before, are going to open up a whole new range of investigations that we will continue innovating over the next decade.
DR. BROWN: To summarize, in 2014 we saw four new drug approvals for CLL, including two new antibodies for upfront therapy, obinutuzumab and ofatumumab, and two new targeted inhibitors for relapsed therapy, ibrutinib and idelalisib. These innovations are starting to revolutionize the treatment of CLL for the benefit of our patients. However, many questions remain about how best to use each of these drugs, about toxicity, and about resistance. The next 5 years in CLL research will be a very exciting time as we start to answer these questions. Hopefully, ultimately, we will cure more and more of our patients, maybe eventually all of them.
References
1. Byrd JC, Furman RR, Coutre SE, et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med. 2013;369(1):32–42.
2. Byrd JC, Brown JR, O’Brien S, et al. for the RESONATE Investigators. Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med. 2014;371(3):213–223.
3. Jain P, Keating M, Wierda W, et al. Outcomes of patients with chronic lymphocytic leukemia after discontinuing ibrutinib. Blood. 2015;125(13):2062–2067.
4. Maddocks KJ, Ruppert AS, Lozanski G, et al. Etiology of ibrutinib therapy discontinuation and outcomes in patients with chronic lymphocytic leukemia. JAMA Oncol. 2015;1(1):80–87.
5. Brown JR, Byrd JC, Coutre SE, et al. Idelalisib, an inhibitor of phosphatidylinositol 3-kinase p110δ, for relapsed/refractory chronic lymphocytic leukemia. Blood. 2014;123(22):3390–3397.
6. Furman RR, Sharman JP, Coutre SE, et al. Idelalisib and rituximab in relapsed in chronic lymphocytic leukemia. N Engl J Med. 2014;370(11):997–1007.
7. Coutre S, Leonard J, Flowers C, et al. Idelalisib monotherapy results in durable responses in patients with relapsed or refractory Waldenstrom’s macroglobulinemia (WM). Poster presented at: 20th Congress of European Hematology Association; June 11–14, 2015; Vienna, Austria. Abstract P690.
8. Goede V, Fischer K, Busch R, et al. Obinutuzumab plus chlorambucil in patients with CLL and coexisting conditions. N Engl J Med. 2014;370(12):1101–1110.
9. O’Brien S, Furman RR, Coutre SE, et al. Ibrutinib as initial therapy for elderly patients with chronic lymphocytic leukaemia or small lymphocytic lymphoma: an open-label, multicentre, phase 1b/2 trial. Lancet Oncol. 2014;15(1):48–58.
10. O’Brien S, Lamanna N, Kipps TJ, et al. Update of a phase 2 study of idelalisib in combination with rituximab in treatment-naïve patients ≥65 years with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL). Program and abstracts of the 56th ASH Annual Meeting and Exposition; December 6–9, 2014; San Francisco, CA. Abstract 1994.
11. Hallek M, Cheson BD, Catovsky D, et al. for the International Workshop on Chronic Lymphocytic Leukemia. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood. 2008;111(12):5446–5456.
Moderated by: Jennifer R. Brown, MD, PhD1
Discussants: Jeffrey A. Jones, MD, MPH2; Jacqueline C. Barrientos, MD3
From the Dana-Farber Cancer Institute and Harvard Medical School, Boston, MA1; Ohio State University, Columbus, OH2; Hofstra North Shore-LIJ School of Medicine, Lake Success, NY
Address for correspondence: Jennifer R. Brown, MD, PhD, Dana-Farber Cancer Institute, 450 Brookline Avenue, Boston, MA 02215
E-mail: [email protected]
Biographical Sketch
From Dana-Farber Cancer Institute and Harvard Medical School:
Jennifer R. Brown, MD, PhD is the Director of the CLL Center of the Division of Hematologic Malignancies at Dana-Farber Cancer Institute and an Associate Professor of Medicine at Harvard Medical School in Boston, Massachusetts. Dr. Brown completed a BS and MS simultaneously in molecular biophysics and biochemistry (MB&B) at Yale, graduating summa cum laude with distinction in MB&B. She proceeded to Harvard Medical School where she received her MD and PhD in molecular genetics in 1998 and was awarded the James Tolbert Shipley Prize for research accomplishment in the graduating class. She then served as an intern and resident in Internal Medicine at Massachusetts General Hospital followed by fellowship in Hematology and Medical Oncology at the Dana-Farber Cancer Institute. Dr. Brown joined the faculty of DFCI and Harvard Medical School in 2004, where she has an active clinical-translational research program in CLL.
Her particular interests include the development of novel targeted therapeutics for CLL, as well as the genomics of CLL. She has been instrumental in the clinical development of both idelalisib and ibrutinib, leading to their regulatory approvals in CLL.
In the area of genomics she has been instrumental in the description of the somatic mutation profile of CLL, and is now particularly interested in the implementation of genomic technology in the clinic, including for prognosis and targeted therapy. She also has a longstanding research interest and focus on the inherited predisposition to CLL.
To date she has published over 130 papers in the scientific literature, predominantly in CLL. She is an active member of the CLL Research Consortium and serves on the Alliance Leukemia and Leukemia Correlative Science Committees as well as the NIH Cancer Biomarkers Study Section. In 2014 she was the recipient of two awards from Dana-Farber Cancer Institute, the Clinical Innovation Award, as well as the George Canellos Award for Excellence in Clinical Investigation and Patient Care. She enjoys a worldwide reputation as a CLL expert and is in much demand as an international speaker.
From Hofstra North Shore-LIJ School of Medicine:
Jacqueline C. Barrientos, MD, is Attending Physician at the Chronic Lymphocytic Leukemia (CLL) Research & Treatment Program of the Division of Hematology and Medical Oncology, Department of Medicine, in the North Shore – LIJ Cancer Institute in Lake Success, New York. She is also Assistant Professor of Medicine at the Hofstra North Shore-LIJ School of Medicine. Dr. Barrientos works in close collaboration with her mentors, Dr. Kanti R. Rai and Dr. Nicholas Chiorazzi of the Feinstein Institute for Medical Research.
Dr. Barrientos received her medical degree at the Ponce School of Medicine in Puerto Rico, where she was elected vice-president of Alpha Omega Alpha Honor Medical Society. During her medical studies, she was the recipient of two Research Fellowship Awards from the Howard Hughes Medical Institute. She completed her internship and residency in internal medicine at Yale-New Haven Hospital of the Yale School of Medicine, and her fellowship in Hematology/Oncology at New York Presbyterian Hospital of Weill Cornell Medical College in New York City, where she also served as Chief Fellow. She is board certified in internal medicine, hematology and oncology.
Dr. Barrientos’ research focus is on chronic lymphocytic leukemia and lymphoma. She has extensive experience with the new promising agents targeting the B-cell receptor signaling pathway in B-cell malignancies, serving as Principal Investigator on several phase I-III clinical trials.
Dr. Barrientos actively participates in multi-institutional clinical trials with the Chronic Lymphocytic Leukemia Research Consortium (CRC) and the Alliance for Clinical Trials in Oncology. She is a cadre member of the Leukemia Committee of the Alliance for Clinical Trials in Oncology and in this capacity is co-chair of a study comparing chemoimmunotherapy against a combination of targeted agents. She is a member of the American Society of Clinical Oncology (ASCO) and the American Society of Hematology (ASH).
She has been an invited speaker for ASCO University “CLL Tumor Board”, ASH “State of the Art Symposium”, and “Highlights of ASH in Latin America”. Dr. Barrientos is the recipient of a 2015 American Society of Hematology-Harold Amos Medical Faculty Development Program (ASH-AMFDP) Fellowship award.
DR. BROWN: I am Jennifer Brown, Director of the Chronic Lymphocytic Leukemia (CLL) Center at Dana-Farber Cancer Institute, and Associate Professor of Medicine at Harvard Medical School. Today, I will be speaking with two of my esteemed CLL colleagues, Drs. Jeffrey Jones and Jacqueline Barrientos, about the new drug approvals in CLL.
DR. BARRIENTOS: I’m Jacqueline Barrientos, Assistant Professor of Hematology/Oncology at the Hofstra North Shore-LIJ School of Medicine, and Attending Hematologist at the CLL Research and Treatment Program in Long Island, NY. Our center participates in clinical trials and we perform correlative basic research. I’m very happy to participate in this expert roundtable discussion.
DR. JONES: I’m Dr. Jeffrey Jones, Associate Professor of Internal Medicine and Section Chief for CLL in the Division of Hematology at The Ohio State University.
DR. BROWN: Thank you Jeff and Jacquie for joining me today. I think we’re all aware what an exciting time this is in CLL with the approvals last year of the targeted inhibitors ibrutinib and idelalisib as well as the new antibody approval obinutuzumab as well as the additional indication for ofatumumab. Let’s start our discussion with ibrutinib and idelalisib. Jeff, please introduce the approvals that these inhibitors received and get us started.
DR. JONES: February 2014 marked a really important time in CLL medicine with the approval of the first oral kinase inhibitor, ibrutinib, for the treatment of CLL after one prior therapy.1,2 This ushered in an entirely new era of molecularly-targeted therapy for CLL. Later that year, ibrutinib received approval for deletion 17p CLL, the highest risk genetic subtype of CLL, whether previously untreated or relapsed disease. The drug has rapidly entered the clinic, although I think most of us are still trying to determine how best to incorporate them into our practice.
DR. BROWN: Jacquie, please comment on how you’re using ibrutinib now in your practice.
DR. BARRIENTOS: In CLL patients with the presence of a mutation of TP53 or deletion 17p, we use ibrutinib. We essentially do not use chemotherapy on this particular set of patients. If, for any reason, they are not able to tolerate the drug, then we consider idelalisib, which is not approved separately for this 17p deletion indication. Idelalisib is approved for use in combination with rituximab for the treatment of relapsed or refractory CLL patients. Idelalisib has shown clinical activity in several clinical trials in patients with deletion 17p.
At this moment, we mainly are using ibrutinib or idelalisib for our relapsed or refractory CLL patients. Clinical trials are underway in the frontline setting and we hope to see the results of the frontline use of ibrutinib in elderly patients soon. As of right now, we don’t use ibrutinib as a frontline therapy unless there is a reason, and usually it’s that they carry the 17p deletion or they are participating in a clinical trial.
DR. JONES: Outside of clinical trials our practice has really been to follow the label indications for ibrutinib. For previously untreated patients, our use has been limited to patients with deletion 17p or TP53 mutated disease, as Jacquie said, since that is the group for which the drug has been approved in the frontline.
DR. BROWN: I would agree. That’s been my practice as well. We should perhaps review the data from the registration trial that led to the ibrutinib approval for relapsed refractory CLL. The initial approval was from the stage IB2 study and was an accelerated approval.1 The confirmatory registration trial, RESONATE, randomized relapsed refractory CLL patients to ibrutinib versus the anti-CD20 antibody ofatumumab.2 Ibrutinib was found to be significantly better in improving both progression free and overall survival, although there was crossover later. As a result, this has moved into our relapse refractory use very rapidly. Although we still use chemoimmunotherapy for upfront therapy for patients without 17p deletion, for those in relapse we have moved entirely to targeted inhibitors. Would you both agree?
DR. JONES: For sure. I think it is very hard in 2015 to think of the patient for whom chemo-immunotherapy is the better choice than ibrutinib for relapsed disease.I think it is very hard in 2015 to think of the patient for whom chemoimmunotherapy is the better choice than ibrutinib for relapsed disease. The benefit is most marked for the group with higher-risk disease as characterized by genetic risk features, not just deletion 17p, but patients with complex abnormal karyotype or deletions of chromosome 11q. All of these patients particularly benefit from treatment with ibrutinib in the second line vs chemoimmunotherapy, as do patients who had either a suboptimal response to frontline chemoimmunotherapy or a brief duration of first remission. All of us are sometimes asked, “Well, who is the patient with relapsed CLL for whom ibrutinib is the best choice?” Right now, in most clinical situations, my response is, “For which patient is ibrutinib not the best choice in first relapse?”
DR. BROWN: That’s actually a good question. Jacquie, how would you answer that? Are there patients for whom you would not choose ibrutinib in first relapse?
DR. BARRIENTOS: I feel a hesitant to use ibrutinib in some patients with a particular comorbidity or medical history. For example, patients with a previous intracranial bleed or a recent history of bleeding, I would prefer to avoid using ibrutinib because there have been rare cases of spontaneous intracranial bleed or severe bleeding after trauma. The other type of patient where I would be cautious is a patient with uncontrolled atrial fibrillation because there are data that in the minority of patients (up to 10% of patients), atrial fibrillation has been an issue. We have some patients that are so frail that they couldn’t tolerate another episode of uncontrolled atrial fibrillation and as such they would not be ideal candidates for the drug. For that type of patient, I would probably abstain from using ibrutinib and consider the use of another therapy. Finally, I would be careful in patients on antiplatelet and anticoagulation therapy because ibrutinib affects platelet functions increasing the risk of bleeding. The bleeding events seen with ibrutinib are mostly grade 1 or grade 2. If the patients have had a serious bleed or serious gastrointestinal bleed or a recent surgery, then I would preferably use another agent.
DR. BROWN:Yes, so that gets to the toxicities of ibrutinib. The more medically significant ones do include perhaps a 5% to 10% risk of atrial fibrillation as well as bleeding risks, which as Jacquie points out are low and usually low grade, but there are occasional higher-risk bleeds. I personally still try to avoid combining anticoagulation with ibrutinib, as we don’t fully understand the mechanism or the risk factors for the more serious bleeds. Jeff, please comment.
DR. JONES: I think the data from the randomized study are actually the most helpful since, as you say, mild bleeding events (grade 1 or 2) were indeed more common amongst the group of patients who were treated with ibrutinib.2 Major bleeding events—which are typically defined as intracranial hemorrhage, bleeding requiring transfusion, or inpatient management—were actually similar between the two arms of the trial. An important caveat in interpreting these data is to know that patients in this trial were excluded if they were anticoagulated with warfarin, if they had an antecedent history of intracranial hemorrhage or recent bleeding, or recent surgery. In line with those exclusions, we will often consider other options. If there is any specific concern for bleeding, such as a patient who has experienced bleeding complications during routine anticoagulation, which is also a patient for whom ibrutinib may not be the best choice. In these clinical situations, it is important to involve the patient in discussing the balance of risks and benefits.
DR. BROWN: Yes. Jacquie, please comment on some of the side effects the patients on ibrutinib have, and how you manage those.
DR. BARRIENTOS: I usually mention to my patients that over the first 2 or 3 months about half of them will have a possible change in their bowel movements. Usually they report some diarrhea or loose stools. Usually these episodes are mild, nothing that requires hospitalization. In any case, if it becomes severe, I definitely make sure that it’s not an infection. We all know that our patients with CLL are prone to infections. The other thing I tell the patients is that in some cases patients may develop a rash on the skin. Many times it may look like a rash, but it’s actually ecchymosis—an effect from the drug on the platelets. Essentially, they are grade 1 and don’t require intervention. I just tell them that eventually they will go away. It can be scary for the patients if they are not expecting these. We have had patients with large areas of hematomas in the arms or in the legs. That is unexpected with a drug that they are taking by mouth. They usually expect that with other drugs like warfarin, but not with ibrutinib, so it is important to mention before they start the drug.
Last but not least, I mention the fact that they may get arthralgias—joint pain—in different areas of their bodies. I would say that I see that in about 20% to 30% of patients. Usually it’s very mild, but on occasion I’ve had patients with arthritis so severe that we’ve had to hold the drug and give them some steroids to help them improve their ability to maneuver their hands or move their joints. I’m sure you have seen some of those same side effects.
DR. BROWN: Yes, definitely. In general, it’s pretty well tolerated but it’s best to warn the patients, then there are no surprises. Let’s turn our attention for a moment back to the highest risk genetic subgroup, the 17p deleted patients—which Jeff had mentioned get particularly strong benefit from ibrutinib. This is certainly true, although it’s also the case that it appears, depending on the data set you look at, that they may relapse earlier than other patients on ibrutinib. In the original phase IB2, the median progression survival for the 17p deleted patients was 28 months. More recent data from Ohio State and MD Anderson suggest that complex karyotype may be a risk factor.3,4 Given these data, how are you two handling the question of allogeneic stem cell transplantation for these patients in this new era?
DR. BARRIENTOS: At our center, if the patient is young and they have access and are fit to tolerate a reduced-intensity allogeneic transplant, we recommend that they be evaluated for a transplant. Unfortunately, if they lose the response to the best drug available for their particular genetic mutation, then we have limited options of salvage therapy. It’s risky to think that they will not relapse at some point, and then what do we do at the time of relapse? We can use other targeted agents that are available, like idelalisib, with the knowledge that they may not always respond to the salvage therapy. Promising clinical activity has been reported for patients with 17p deletion treated with venetoclax in clinical trials. Venetoclax is a new targeted agent in development stages but the drug is only available in clinical trials.Promising clinical activity has been reported for patients with 17p deletion treated with venetoclax in clinical trials. Venetoclax is a new targeted agent in development stages but the drug is only available in clinical trials. One problem is that in order to participate in a clinical trial the patient needs to be able to get to the center to get the drug. Additionally, the patient needs to satisfy certain eligibility criteria for study entry. For these patients that stop responding to ibrutinib, the options of care are very limited at this time. This is the reason why I send all my young patients with a 17p deletion for a transplant evaluation.
At the end of the day it is tough to convince the patients to go for a transplant when they’re feeling in excellent shape. It’s still difficult to make a case to go for a procedure that may have its complications on its own. It is well known that there are some increased mortality risks and infection risks that can arise as a result of a transplant. They may not want to do it because they are feeling so great with their routine. I still sit down and have a long frank talk with the patients, especially if they have complex karyotype and 17p deletion. I am concerned that at some point they’re going to stop responding to ibrutinib.
DR. BROWN: That’s generally my practice as well. What about you, Jeff?
DR. JONES: Until there is greater clarity regarding which of the newer agents can salvage patients progressing after ibrutinib, I think it is still important for younger, transplant eligible patients with deletion 17p disease to undergo evaluation for allograft. It remains potentially curative therapy, and I think the availability of ibrutinib has not really changed the importance of that evaluation.
DR. BROWN: Yes, I would agree. I think that was a good discussion on ibrutinib. Why don’t we turn our attention now to idelalisib, the phosphoinositide 3-kinase (PI3K) inhibitor. How are you using idelalisib in your practices? Is this after ibrutinib in general?
DR. JONES: Published data regarding the sequencing of the new agents are relatively limited since all of the registration trials for idelalisib excluded patients who had received prior therapy with an inhibitor of B-cell receptor signaling, including Bruton’s tyrosine kinase inhibitors like ibrutinib.5,6 A small number of patients enrolled on the phase IB2 trial of ibrutinib, as well as the subsequent randomized trial, had received prior therapy with idelalisib and responded similarly to patients who had not received prior idelalisib.1,2 In our practice, the use of idelalisib has pretty much been limited to patients who have either received prior ibrutinib or patients who are not eligible to receive ibrutinib because of some important contraindication, such as an inherited bleeding defect, perceived increased bleeding, or history of difficult to control atrial fibrillation, since that event also seems to be more likely among patients treated with ibrutinib.
DR. BROWN: How about you, Jacquie?
DR. BARRIENTOS: The same type of patient with the addition of patients with kidney disease. The rationale for this is based on the phase III trial for idelalisib and rituximab, the enrollment allowed participation of patients with decreased renal function, that was one of the entry criteria for eligibility to participate in the trial.6 In most of the ibrutinib trials the creatinine clearance needed to be adequate, whereas this was allowed to be lower on the idelalisib trials. For those patients with severe renal impairment, I tend to prefer idelalisib rather than ibrutinib—only because I feel more comfortable and have more experience treating patients with impaired kidney function with idelalisib.
DR. BROWN: I have seen some episodic elevations in creatinine in patients on ibrutinib, but they’re fairly sporadic and it’s a little hard to assess the direct drug relationship. It is true that the patients in the idelalisib studies had a high level of comorbidity deliberately on the initial registration trial and generally did reasonably well with idelalisib. The toxicity profile of idelalisib is pretty characteristic, and is potentially harder to manage than that of ibrutinib. I think it also dictates some of how it’s being used in later line therapy. Does one of you wish to comment on the pattern of the key toxicities?
DR. BARRIENTOS: One key toxicity that is very particular to this drug that may happen overnight and is very striking is transaminitis. It usually happens more with non-Hodgkin lymphoma patients compared to relapsed CLL patients, but transaminitis can still be very severe. Patients can develop transaminitis even after more than a cycle on therapy even if they were tolerating the drug well without other issues. It’s very important to educate physicians and healthcare providers about the need to monitor the liver function tests, at least every 2 weeks for the first 2 months. Transaminitis events can be very prompt, very rapid, and usually asymptomatic. My patients that developed transaminitis never complained and had we not been cautious about it, we may have missed it.
DR. BROWN: Yes, I even check weekly. The recent safety analysis said the overall incidence of grade 3 to 4 transaminitis is about 15% in relapse patients.7 That’s pretty significant.
DR. JONES: I think it’s important to know that the transaminitis, if monitored carefully and managed with drug interruption and/or dose reduction upon reintroduction, need not lead to discontinuation. Discontinuations for transaminitis are actually the minority of patients who experience the side effect.
DR. BROWN: Absolutely. Do you want to comment on some of the other side effects that may more often lead to discontinuation?
DR. JONES: We should mention that there are some preclinical animal data suggesting that the molecular target of idelalisib, the PI3K delta isoform, is an important signaling molecule in regulatory T cells important for self-tolerance. While it has efficacy in treating B-cell disorders, inhibiting PI3K-delta may also be impairing T regulatory cell function. That may be what leads to the more characteristic later side effects of idelalisib, including pneumonitis and colitis. Pneumonitis is relatively rare, but because it can masquerade as other respiratory ailments in an older patient population with comorbid medical illnesses like chronic obstructive pulmonary disease and preexisting immune dysfunction because of CLL or prior therapy, inflammatory pneumonitis can be misdiagnosed. This rare but potentially life-threatening complication of idelalisib treatment requires prompt recognition, discontinuation of the drug, and appears to be most effectively managed with corticosteroids.
The other commonly occurring late toxicity, colitis, is often one that also eludes prompt recognition since many times patients are seen by primary care practitioners between oncology visits, and these doctors may not yet be aware that colitis can occur as a late side effect of idelalisib. Sometimes the colitis is misdiagnosed as gastroenteritis or Clostridium difficile colitis and eludes initial management. Like the pneumonitis, this problem, which may occur in more than a quarter of patients, is really best managed by prompt recognition and, in many cases, interruption of the drug. In some cases, patients have been managed with interruption of the drug and perhaps rechallenge at a lower dose, but in many other cases, colitis has been a treatment-limiting side effect and is a leading cause of drug discontinuation for toxicity.
DR. BROWN: Yes, I would agree. It can occur even at much later times in people who have tolerated the drug for even a couple of years, which is surprising compared to typical drug-related diarrhea.
DR. JONES: Right. With many other drugs, a patient starts taking the drug and expects the treatment-related side effects to become manifest very early. The diarrhea and rash associated with ibrutinib, for instance, are really timed very close to drug initiation, similar to antibiotics and other medications that we commonly prescribe. When side effects occur late in the course of treatment, I think it is just not on anyone’s radar to suspect that they could be related to a drug that they have been receiving for some time. That is an important message to communicate to patients, as well as to doctors who are just beginning to prescribe these new drugs for the first time.
DR. BROWN: Exactly. Why don’t we turn our attention now to the approval of obinutuzumab, and review the registration trial data there and then how you’re using that in practice. Jacquie?
DR. BARRIENTOS: Obinutuzumab is a third generation monoclonal antibody targeting the CD20 receptor on B cells. It was approved in November of 2013 by the US Food and Drug Administration for use in combination with chlorambucil to treat patients with previously untreated CLL.8 The trial enrolled patients with comorbidities as measured by the Cumulative Index Rating Scale, the scale helps define fitness. The patients that participated in the registration trial were patients that due to their comorbidities would not tolerate well a chemoimmunotherapy regimen like fludarabine, cyclophosphamide, and rituximab (FCR), and possibly the combination of bendamustine and rituximab. In patients older than age 65 with multiple comorbidities, chlorambucil monotherapy is widely used worldwide due to concerns of complications from the use of other chemoimmunotherapy regimens like the ones mentioned above. In the United States, we usually see that physicians prefer to use rituximab as a single agent in frail patients with multiple comorbidities.
The combination of obinutuzumab with chlorambucil compared to chlorambucil as a single agent showed that the patients treated with the combination therapy had a higher rate of response, a higher rate of progression free survival, and an improved overall survival. The main issue with obinutuzumab is the fact that the infusion reactions are much greater than what we traditionally see with rituximab. Severe and life-threatening infusion reactions have been reported. The reactions can also be more abrupt, although they typically occur very early in infusion, so they are more predictable. If the patient develops an infusion reaction or can’t tolerate the drug, the infusion needs to be interrupted. If the patient does not experience any further infusion reaction symptoms, the infusion may be restarted at a lower rate. I believe grade 3 to grade 4 events were higher than 10% in the registration trial, with infusion reactions of any grade seen in 50%–70%, so it can be common—usually within the first day. By the third infusion, the rate of reaction decreases significantly. Most of the time after that third infusion, most patients won’t have any more issues with tolerability.
Who are the patients that develop these infusion reactions? It has been noted that the level of interleukin 6 is elevated in patients that develop an infusion reaction. That’s the reason why all patients should be premedicated with potent steroids (methylprednisolone or dexamethasone, not hydrocortisone). In addition, patients need to be premedicated with acetaminophen and an antihistamine. In the future hopefully we will be able to use other agents like tocilizumab to lessen the risk of infusion reactions, this is currently being tested in clinical trials as its use is theoretical at this point based on the observation of the elevated interleukin 6 levels.
There are other important side effects with this combination regimen that were noted in the registration trial. There was a higher rate of neutropenia in the patients receiving obinutuzumab and chlorambucil, although this did not correlate with a higher rate of grade 3 or grade 4 infections. The rate of grade 3 or 4 infections was the same all across the board in patients that received chlorambucil, chlorambucil in combination with rituximab, or chlorambucil in combination with obinutuzumab.
DR. BROWN: Are you using much obinutuzumab chlorambucil in your practice?
DR. BARRIENTOS: In select patients, yes. For untreated patients with comorbidities that are not participating in a clinical trial, we discuss with them data from the frontline bendamustine and rituximab combination and obinutuzumab and chlorambucil combination. For the most part, most patients prefer obinutuzumab with chlorambucil because the obinutuzumab chlorambucil combination might be better tolerated and possibly less myelosuppressive than the bendamustine rituximab combination. Unfortunately, most of my patients have already been treated by the time we see them. We have a minority of patients that come recently diagnosed, we just don’t see that many untreated patients.
DR. BROWN: How about you, Jeff? Are you using it?
DR. JONES: Yes, it is a consideration for frontline therapy in patients who don’t have deletion 17p. As we discussed before, most of us have already adopted ibrutinib as our first choice in that 17p deleted population outside of clinical trial. For the remainder of patients, I think the first question remains whether their age and health are permissive to safely give FCR, since that regimen has been associated with the best survival outcomes, even some really long survival, in a group of patients with IgVH mutated, favorable cytogenetic risk disease.
For patients who are not eligible or willing to receive FCR, I think the choice between bendumustine and rituximab (BR) and chlorambucil and obinutuzumab is a relatively challenging one. Part of the reason is that while the overall response rates and complete response rates are lower with obinutuzumab and chlorambucil, the toxicity is also a bit lower. That makes it an appealing choice, particularly when we have the availability of drugs like ibrutinib and idelalisib in the second line. For older patients with comorbid medical illnesses in particular, it may be that the duration of first remission after chemotherapy may not matter as much when we have more effective second line options.
DR. BROWN: Yes, I think that’s definitely true. I just want to highlight two points. Your point about the long-term efficacy of FCR, particularly in the IgVH mutated patients—it is important to note that we now have data from both MD Anderson and the German CLL Study Group. The MD Anderson data with 10 year follow up, 60% of that genetic subgroup are progression free after FCR suggesting that a subset of them may in fact be cured. We don’t want to forget that with the excitement of the new inhibitors. I would second your point also about the potential toxicities of BR which can be as myelosuppressive as FCR even though it is not in every case. Again, it’s very important to assess the comorbidities of the patient not just for FCR but also for BR, particularly when FCR has this chance of very long-term remission which is not seen with BR.
DR. JONES: Yes, and there’s also a risk for opportunistic infections with both regimens. Like fludarabine-treated patients, there are patients treated with bendumustine who experience pneumocystis pneumonia or viral reactivation from immune suppression beyond just the neutropenia.
DR. BROWN: Yes, absolutely. Let’s talk briefly about where we see CLL therapy going in the next few years given these exciting new drugs. I’ll just leave that open and see what you have to say. Jacquie?
DR. BARRIENTOS: Some of the possible developments that we may see over the next couple of years are the use of these targeted agents or small molecules as initial therapy either as monotherapy or in combination regimens. We are expecting to see the data of the clinical trial of frontline ibrutinib against chlorambucil in patients that are older than age 65. Idelalisib has other ongoing clinical trials in the frontline setting as monotherapy and in combination therapy. Data have been presented of idelalisib in combination with rituximab as frontline therapy. It was interesting to note that some of these side effects that we saw in the relapsed or refractory setting occurred more often in patients in the frontline setting, although efficacy was very high. These promising data may eventually lead to a change in the way that we treat patients in the frontline, not only as monotherapy. There are several clinical trials that incorporate chemoimmunotherapy with these new targeted agents to see if maybe we will obtain deeper remissions or longer duration of response.
DR. JONES: What preliminary data exist in small phase 1 or phase 2 studies suggest that the new agents may be even more effective in previously untreated disease, with higher overall response rates, higher complete response rates, and more durable remissions than observed among patients with relapsed and refractory disease.9,10 These results underscore that the individual agents are among the most effective drugs that have been developed for CLL in terms of their single-agent activity. If you include the oral BCL-2 inhibitor in development, venetoclax, these drugs have really had remarkable single-agent efficacy. If these newer agents are like older cytotoxic chemotherapy agents, like fludarabine, they may become superstars when used in combination. While we will soon see these drugs move into the frontline setting as single agents, I think the real potential for magic is when they get combined. There we may see the kinds of deep remissions that we only achieve now with chemoimmunotherapy, remissions that will allow similar long-term treatment-free survival without cytotoxic chemotherapy. I’d like nothing more than to see a 60% 10 year survival after a nonchemotherapy-containing combination that emerges when we use these new drugs in ways that maximize their benefit in combination.
DR. BROWN: I would certainly agree. I think that although we have remarkable single-agent activity of these drugs, we know that in the context of single-agent activity, resistance is likely to develop over time. For a subset of patients that may not matter. If they’re older and have comorbidities, they may get enough durability of response from their first single agent that it doesn’t matter, particularly the patients with lower risk CLL. For our younger patients, I think the combinations will have the opportunity to minimize the development of resistance and also allow shorter courses of therapy so that patients can be off treatment still with deep remissions. That is what most excites me about the future of these agents.
Let’s just talk about the future of watch and wait. We now have great drugs and great therapies. Are you considering treatment earlier in any of your patients at this point, Jacquie?
DR. BARRIENTOS: I have been very hesitant to start our patients on any drug before they develop symptoms from the disease. I still wait to initiate therapy according to the International Workshop on CLL (IWCLL) guidelines.11 The reason is that anytime that we start a new agent, the patients may develop some mutation that is driven by these new agents. At this point, there are no data for us to start therapy before symptoms develop. The German CLL study group is currently doing a high risk study in patients that are asymptomatic but have a high risk profile like 17p deletion to see if maybe a drug like ibrutinib could have a benefit. I think that will be very interesting once the data come out. There are certain patients with whom you are always wondering, “Am I doing more harm by withholding therapy at this moment?” So far, early intervention with chemotherapy before symptoms has not shown any additional benefit. We still do the watch and wait for the time being, but this may change in the future for certain patients with certain high-risk characteristics.
DR. BROWN: Yes, I share your concerns about the possibility of evolution of the disease in the context of any treatment. Even though we hope that there will be less clonal evolution with these targeted inhibitors, there is some increasing evidence that some adverse clones like TP53 mutated or 17p deleted clones are preexisting in many cases. Then, under the influence of treatment, these mutations become more evident, ie a higher percentage of the disease. Personally, I would like to see overall survival data before we start treating patients earlier.
DR. JONES: I would absolutely agree. I think if you want to undertake the systematic treatment of patients before they actually progress clinically, those are the kind of data that you want. You want to know whether you are impacting the natural history of the disease. I’ll take a slightly contrarian point of view in talking about elderly patients in particular. Some of our colleagues who treat low-grade lymphoma—where watch and wait is often employed in the initial asymptomatic setting—have argued that there is a strong rationale to treat earlier rather than later because you may find that toxicity becomes more prohibitive if you wait until the patients become ill. There’s a somewhat perverse logic underlying our current approach to therapy—we don’t treat to maintain health, we treat when patients become sick. I think there is room for a slightly different approach still operating within current consensus guidelines. There is a group of elderly patients with comorbid medical illnesses that as it seems their disease is starting to progress, I am inclined to consider—at least discuss—the feasibility of treatment then as a way of limiting both the morbidity from the disease, as well as the morbidity of treatment. When the only available treatments were chemotherapy drugs like fludarabine, which has not clearly resulted in survival benefits for elderly patients, that was as feasible as when the treatment is perhaps obinutuzumab and chlorambucil, or maybe in the near future drugs like ibrutinib and idelalisib. Therefore I think we may all want to start rethinking our approach, cautiously. Ultimately, this is a research question.
DR. BROWN: That’s interesting. I certainly agree that in the setting of chemotherapy or chemoimmunotherapy patients with a higher disease burden have a lot harder time getting started on therapy. If in fact the targeted inhibitors move to upfront therapy, it’s not so clear to me that those drugs have more initial toxicity in patients with a greater disease burden—at least for ibrutinib. Do you disagree?
DR. JONES: No, I think that’s true. You will even hear an argument sometimes that a single-agent rituximab for follicular lymphoma or obinutuzumab and chlorambucil would be better tolerated, and you have more room for management of toxicity when you give them to patients who are healthier at baseline. Part of that is with less extensive disease, but you’re right. I agree that there is no indication right now that the novel, targeted agents are more toxic in older patients. However, I will say that our own retrospective analysis from Ohio State suggested that age was one of the factors associated with early discontinuation among our patients.4
DR. BROWN: Right, but to me, the fact that age is a predictor of less tolerability of therapy suggests that maybe we should save the therapy until the patient really needs it. The toxicities of ibrutinib are not as clearly disease-burden related necessarily.
DR. JONES: Yeah, I think that our disagreement really suggests that it’s a question to study.
As the treatment becomes more manageable and potentially more effective, you start to question whether our goal is to treat patients as they become ill, or to prevent them from ever becoming ill in the first place.DR. BROWN: Oh, absolutely.
DR. JONES: These are important questions that we will necessarily revisit. As the treatment becomes more manageable and potentially more effective, you start to question whether our goal is to treat patients as they become ill, or to prevent them from ever becoming ill in the first place.
DR. BROWN: Right, absolutely. I would say that I feel that we don’t always let the patients become symptomatically ill even in following IWCLL criteria. For example, their counts may be relatively poor, requiring treatment, but the patients are not yet suffering from that.
DR. JONES: Right.
DR. BROWN: I think this was a great discussion. It’s obviously an extremely exciting time in CLL research as we learn how to use our targeted inhibitors, our new antibodies, and hopefully soon we’ll have another targeted inhibitor with ABT199 the BCL-2 inhibitor. Jacquie or Jeff, do you have any points you would like to add before we wrap up?
DR. BARRIENTOS: No. I think we covered most of the important concepts.
DR. JONES: I will just say that with analogy to a cousin disease, chronic myeloid leukemia, after imatinib and the subsequent oral kinase inhibitors were introduced in that disease people thought that the final chapter of the story had been. I think we’re going to find the same thing in CLL medicine. These phenomenally effective agents, safer than the ones we have had available to employ before, are going to open up a whole new range of investigations that we will continue innovating over the next decade.
DR. BROWN: To summarize, in 2014 we saw four new drug approvals for CLL, including two new antibodies for upfront therapy, obinutuzumab and ofatumumab, and two new targeted inhibitors for relapsed therapy, ibrutinib and idelalisib. These innovations are starting to revolutionize the treatment of CLL for the benefit of our patients. However, many questions remain about how best to use each of these drugs, about toxicity, and about resistance. The next 5 years in CLL research will be a very exciting time as we start to answer these questions. Hopefully, ultimately, we will cure more and more of our patients, maybe eventually all of them.
References
1. Byrd JC, Furman RR, Coutre SE, et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med. 2013;369(1):32–42.
2. Byrd JC, Brown JR, O’Brien S, et al. for the RESONATE Investigators. Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med. 2014;371(3):213–223.
3. Jain P, Keating M, Wierda W, et al. Outcomes of patients with chronic lymphocytic leukemia after discontinuing ibrutinib. Blood. 2015;125(13):2062–2067.
4. Maddocks KJ, Ruppert AS, Lozanski G, et al. Etiology of ibrutinib therapy discontinuation and outcomes in patients with chronic lymphocytic leukemia. JAMA Oncol. 2015;1(1):80–87.
5. Brown JR, Byrd JC, Coutre SE, et al. Idelalisib, an inhibitor of phosphatidylinositol 3-kinase p110δ, for relapsed/refractory chronic lymphocytic leukemia. Blood. 2014;123(22):3390–3397.
6. Furman RR, Sharman JP, Coutre SE, et al. Idelalisib and rituximab in relapsed in chronic lymphocytic leukemia. N Engl J Med. 2014;370(11):997–1007.
7. Coutre S, Leonard J, Flowers C, et al. Idelalisib monotherapy results in durable responses in patients with relapsed or refractory Waldenstrom’s macroglobulinemia (WM). Poster presented at: 20th Congress of European Hematology Association; June 11–14, 2015; Vienna, Austria. Abstract P690.
8. Goede V, Fischer K, Busch R, et al. Obinutuzumab plus chlorambucil in patients with CLL and coexisting conditions. N Engl J Med. 2014;370(12):1101–1110.
9. O’Brien S, Furman RR, Coutre SE, et al. Ibrutinib as initial therapy for elderly patients with chronic lymphocytic leukaemia or small lymphocytic lymphoma: an open-label, multicentre, phase 1b/2 trial. Lancet Oncol. 2014;15(1):48–58.
10. O’Brien S, Lamanna N, Kipps TJ, et al. Update of a phase 2 study of idelalisib in combination with rituximab in treatment-naïve patients ≥65 years with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL). Program and abstracts of the 56th ASH Annual Meeting and Exposition; December 6–9, 2014; San Francisco, CA. Abstract 1994.
11. Hallek M, Cheson BD, Catovsky D, et al. for the International Workshop on Chronic Lymphocytic Leukemia. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood. 2008;111(12):5446–5456.
Bacterium may increase risk of DLBCL, FL
Coxiella burnetii
Image courtesy of NIAID
The bacterium that causes Q fever may confer an increased risk of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), according to a study published in Blood.
Q fever is an infectious disease caused by Coxiella burnetii, a bacterium primarily transmitted through the excrements of cattle, sheep, and goats.
Because some patients with Q fever develop lymphoma, researchers believed the malignancy could be a risk factor for Q fever.
However, the experience of 1 patient prompted a group of researchers in France to consider the opposite—that the infection might cause the lymphoma.
“During a follow-up scan in a patient we had successfully treated for Q fever, we observed a tumor close to the location of the previous infection,” said study author Didier Raoult, MD, PhD, of Aix-Marseille University in Marseille, France.
“The discovery that it was a lymphoma tumor containing C burnetii encouraged us to consider that the infection might have contributed to the development of the cancer.”
To better understand the association between C burnetii and lymphoma, Dr Raoult and his colleagues screened 1468 patients treated at the French National Referral Center for Q Fever from 2004 to 2014.
The researchers imaged patient tissue samples and identified 7 people, including the initial patient, who developed lymphoma after C burnetii infection. Six patients were diagnosed with DLBCL and 1 with FL.
To determine if patients with Q fever have a higher risk of lymphoma than the general population, the researchers compared the incidence of lymphoma in the Q fever registry to the incidence reported in France’s general population.
This revealed an excess risk of DLBCL and FL in the Q fever population, with standardized incidence ratios of 25.4 for DLBCL and 6.7 for FL.
In addition, the odds of developing lymphoma were higher in patients with persistent, concentrated infections than in those with other forms of Q fever. The hazard ratio for patients with persistent, concentrated infection was 9.35.
Finally, the researchers observed interleukin-10 overproduction in Q fever patients with lymphoma. The team said this suggests that suppression of the immune system may have allowed the lymphoma cells to evade immune detection and multiply.
“As we continue to learn more about the association between C burnetii and lymphoma, these results should encourage clinicians to survey high-risk patients as early as possible for potential cancer,” Dr Raoult said.
“Ultimately, this early diagnosis and treatment would improve outcomes for Q fever patients who subsequently develop lymphoma, particularly those with B-cell non-Hodgkin lymphoma.” ![]()
Coxiella burnetii
Image courtesy of NIAID
The bacterium that causes Q fever may confer an increased risk of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), according to a study published in Blood.
Q fever is an infectious disease caused by Coxiella burnetii, a bacterium primarily transmitted through the excrements of cattle, sheep, and goats.
Because some patients with Q fever develop lymphoma, researchers believed the malignancy could be a risk factor for Q fever.
However, the experience of 1 patient prompted a group of researchers in France to consider the opposite—that the infection might cause the lymphoma.
“During a follow-up scan in a patient we had successfully treated for Q fever, we observed a tumor close to the location of the previous infection,” said study author Didier Raoult, MD, PhD, of Aix-Marseille University in Marseille, France.
“The discovery that it was a lymphoma tumor containing C burnetii encouraged us to consider that the infection might have contributed to the development of the cancer.”
To better understand the association between C burnetii and lymphoma, Dr Raoult and his colleagues screened 1468 patients treated at the French National Referral Center for Q Fever from 2004 to 2014.
The researchers imaged patient tissue samples and identified 7 people, including the initial patient, who developed lymphoma after C burnetii infection. Six patients were diagnosed with DLBCL and 1 with FL.
To determine if patients with Q fever have a higher risk of lymphoma than the general population, the researchers compared the incidence of lymphoma in the Q fever registry to the incidence reported in France’s general population.
This revealed an excess risk of DLBCL and FL in the Q fever population, with standardized incidence ratios of 25.4 for DLBCL and 6.7 for FL.
In addition, the odds of developing lymphoma were higher in patients with persistent, concentrated infections than in those with other forms of Q fever. The hazard ratio for patients with persistent, concentrated infection was 9.35.
Finally, the researchers observed interleukin-10 overproduction in Q fever patients with lymphoma. The team said this suggests that suppression of the immune system may have allowed the lymphoma cells to evade immune detection and multiply.
“As we continue to learn more about the association between C burnetii and lymphoma, these results should encourage clinicians to survey high-risk patients as early as possible for potential cancer,” Dr Raoult said.
“Ultimately, this early diagnosis and treatment would improve outcomes for Q fever patients who subsequently develop lymphoma, particularly those with B-cell non-Hodgkin lymphoma.” ![]()
Coxiella burnetii
Image courtesy of NIAID
The bacterium that causes Q fever may confer an increased risk of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL), according to a study published in Blood.
Q fever is an infectious disease caused by Coxiella burnetii, a bacterium primarily transmitted through the excrements of cattle, sheep, and goats.
Because some patients with Q fever develop lymphoma, researchers believed the malignancy could be a risk factor for Q fever.
However, the experience of 1 patient prompted a group of researchers in France to consider the opposite—that the infection might cause the lymphoma.
“During a follow-up scan in a patient we had successfully treated for Q fever, we observed a tumor close to the location of the previous infection,” said study author Didier Raoult, MD, PhD, of Aix-Marseille University in Marseille, France.
“The discovery that it was a lymphoma tumor containing C burnetii encouraged us to consider that the infection might have contributed to the development of the cancer.”
To better understand the association between C burnetii and lymphoma, Dr Raoult and his colleagues screened 1468 patients treated at the French National Referral Center for Q Fever from 2004 to 2014.
The researchers imaged patient tissue samples and identified 7 people, including the initial patient, who developed lymphoma after C burnetii infection. Six patients were diagnosed with DLBCL and 1 with FL.
To determine if patients with Q fever have a higher risk of lymphoma than the general population, the researchers compared the incidence of lymphoma in the Q fever registry to the incidence reported in France’s general population.
This revealed an excess risk of DLBCL and FL in the Q fever population, with standardized incidence ratios of 25.4 for DLBCL and 6.7 for FL.
In addition, the odds of developing lymphoma were higher in patients with persistent, concentrated infections than in those with other forms of Q fever. The hazard ratio for patients with persistent, concentrated infection was 9.35.
Finally, the researchers observed interleukin-10 overproduction in Q fever patients with lymphoma. The team said this suggests that suppression of the immune system may have allowed the lymphoma cells to evade immune detection and multiply.
“As we continue to learn more about the association between C burnetii and lymphoma, these results should encourage clinicians to survey high-risk patients as early as possible for potential cancer,” Dr Raoult said.
“Ultimately, this early diagnosis and treatment would improve outcomes for Q fever patients who subsequently develop lymphoma, particularly those with B-cell non-Hodgkin lymphoma.”