User login
Variations in blood cancer survival across Europe

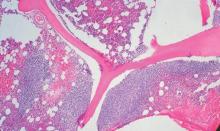
chemotherapy
Photo by Rhoda Baer
VIENNA—Results of the EUROCARE-5 study have revealed regional differences in survival for European patients with hematologic malignancies.
The data showed regional variations in 5-year relative survival rates for a number of cancers.
But the differences were particularly pronounced for leukemias, non-Hodgkin lymphomas (NHLs), and plasma cell neoplasms (PCNs).
Milena Sant, MD, of the Fondazione IRCCS Istituto Nazionale dei Tumori in Milan, Italy, presented these results at the 2015 European Cancer Congress (LBA 1).
Data from this study have also been published in several articles in the October 2015 issue of the European Journal of Cancer.
EUROCARE-5 includes records from 22 million cancer patients diagnosed between 1978 and 2007. The latest data encompass more than 10 million patients (ages 15 and older) diagnosed from 1995 to 2007 and followed up to 2008.
The data came from 107 cancer registries in 29 countries. The researchers estimated 5-year relative survival and trends from 1999 to 2007 according to region—Ireland/UK, Northern Europe, Central Europe, Southern Europe, and Eastern Europe.
“In general, 5-year relative survival—survival that is adjusted for causes of death other than cancer—increased steadily over time in Europe, particularly in Eastern Europe, for most cancers,” Dr Sant said.
“However, the most dramatic geographical variations were observed for cancers of the blood where there have been recent advances in treatment, such as chronic myeloid and lymphocytic leukemias, non-Hodgkin lymphoma and 2 of its subtypes (follicular and diffuse large B-cell lymphoma), and multiple myeloma. Hodgkin lymphoma was the exception, with smaller regional variations and a fairly good prognosis in most countries.”
Hodgkin lymphoma and NHL
Of all the hematologic malignancies, 5-year relative survival was highest for Hodgkin lymphoma, at 80.8% (40,625 cases). Five-year survival was 79.4% in Ireland and the UK, 85% in Northern countries, and 74.3% in Eastern Europe, which was significantly below the European average (P<0.0001).
For NHL, the 5-year relative survival was 59.4% (329,204 cases). Survival rates for NHL patients ranged from 49.7% in Eastern Europe to 63.3% in Northern Europe.
CLL/SLL
For chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), the 5-year relative survival was 70.4% (81,914 cases). CLL/SLL survival ranged from 58% in Eastern Europe to about 74% in Central and Northern Europe.
The researchers noted that between-country variations in CLL/SLL survival were high in all regions. Outliers that were significantly below the regional average were Austria (67%), Croatia (52%), and Bulgaria (45.5%).
PCNs
PCNs included multiple myeloma, plasmacytoma, and plasma cell leukemias. The 5-year relative survival for all PCNs was 39.2% (94,024 cases).
PCN survival rates were lowest in Eastern Europe (31.7%), slightly higher in the UK/Ireland (35.9%), and between 39.1% and 42% in the rest of Europe.
Myeloid leukemias
Of all the hematologic malignancies, 5-year relative survival was poorest for patients with acute myeloid leukemia (AML), at 17.1% (57,026 cases).
AML survival rates in Ireland/UK (15.0%) and Eastern Europe (13.0%) were significantly below the European average. But AML survival in Sweden, Belgium, France, and Germany was significantly higher than the average (P<0.005).
Five-year relative survival for chronic myeloid leukemia (CML) was 52.9% (17,713 cases).
Of all the hematologic malignancies, the survival gap between Eastern Europe and the rest of Europe was highest for CML. Five-year survival for CML patients was 33% in Eastern Europe and ranged from 51% to 58% in the rest of Europe.
The researchers also said there were striking survival variations by country in all areas. They found significant deviations from the regional average in Sweden (69.7%), Scotland (64.6%), France (71.7%), Austria (48.2%), Croatia (37.8%), Estonia (48.9%), Czech Republic (45.2%), and Latvia (22.1%).
“Results from EUROCARE can help to identify regions of low survival where action is needed to improve patients’ outcomes,” Dr Sant noted.
“Population-based survival information is essential for physicians, policy-makers, administrators, researchers, and patient organizations who deal with the needs of cancer patients, as well as with the issue of the growing expenditure on healthcare.” ![]()

chemotherapy
Photo by Rhoda Baer
VIENNA—Results of the EUROCARE-5 study have revealed regional differences in survival for European patients with hematologic malignancies.
The data showed regional variations in 5-year relative survival rates for a number of cancers.
But the differences were particularly pronounced for leukemias, non-Hodgkin lymphomas (NHLs), and plasma cell neoplasms (PCNs).
Milena Sant, MD, of the Fondazione IRCCS Istituto Nazionale dei Tumori in Milan, Italy, presented these results at the 2015 European Cancer Congress (LBA 1).
Data from this study have also been published in several articles in the October 2015 issue of the European Journal of Cancer.
EUROCARE-5 includes records from 22 million cancer patients diagnosed between 1978 and 2007. The latest data encompass more than 10 million patients (ages 15 and older) diagnosed from 1995 to 2007 and followed up to 2008.
The data came from 107 cancer registries in 29 countries. The researchers estimated 5-year relative survival and trends from 1999 to 2007 according to region—Ireland/UK, Northern Europe, Central Europe, Southern Europe, and Eastern Europe.
“In general, 5-year relative survival—survival that is adjusted for causes of death other than cancer—increased steadily over time in Europe, particularly in Eastern Europe, for most cancers,” Dr Sant said.
“However, the most dramatic geographical variations were observed for cancers of the blood where there have been recent advances in treatment, such as chronic myeloid and lymphocytic leukemias, non-Hodgkin lymphoma and 2 of its subtypes (follicular and diffuse large B-cell lymphoma), and multiple myeloma. Hodgkin lymphoma was the exception, with smaller regional variations and a fairly good prognosis in most countries.”
Hodgkin lymphoma and NHL
Of all the hematologic malignancies, 5-year relative survival was highest for Hodgkin lymphoma, at 80.8% (40,625 cases). Five-year survival was 79.4% in Ireland and the UK, 85% in Northern countries, and 74.3% in Eastern Europe, which was significantly below the European average (P<0.0001).
For NHL, the 5-year relative survival was 59.4% (329,204 cases). Survival rates for NHL patients ranged from 49.7% in Eastern Europe to 63.3% in Northern Europe.
CLL/SLL
For chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), the 5-year relative survival was 70.4% (81,914 cases). CLL/SLL survival ranged from 58% in Eastern Europe to about 74% in Central and Northern Europe.
The researchers noted that between-country variations in CLL/SLL survival were high in all regions. Outliers that were significantly below the regional average were Austria (67%), Croatia (52%), and Bulgaria (45.5%).
PCNs
PCNs included multiple myeloma, plasmacytoma, and plasma cell leukemias. The 5-year relative survival for all PCNs was 39.2% (94,024 cases).
PCN survival rates were lowest in Eastern Europe (31.7%), slightly higher in the UK/Ireland (35.9%), and between 39.1% and 42% in the rest of Europe.
Myeloid leukemias
Of all the hematologic malignancies, 5-year relative survival was poorest for patients with acute myeloid leukemia (AML), at 17.1% (57,026 cases).
AML survival rates in Ireland/UK (15.0%) and Eastern Europe (13.0%) were significantly below the European average. But AML survival in Sweden, Belgium, France, and Germany was significantly higher than the average (P<0.005).
Five-year relative survival for chronic myeloid leukemia (CML) was 52.9% (17,713 cases).
Of all the hematologic malignancies, the survival gap between Eastern Europe and the rest of Europe was highest for CML. Five-year survival for CML patients was 33% in Eastern Europe and ranged from 51% to 58% in the rest of Europe.
The researchers also said there were striking survival variations by country in all areas. They found significant deviations from the regional average in Sweden (69.7%), Scotland (64.6%), France (71.7%), Austria (48.2%), Croatia (37.8%), Estonia (48.9%), Czech Republic (45.2%), and Latvia (22.1%).
“Results from EUROCARE can help to identify regions of low survival where action is needed to improve patients’ outcomes,” Dr Sant noted.
“Population-based survival information is essential for physicians, policy-makers, administrators, researchers, and patient organizations who deal with the needs of cancer patients, as well as with the issue of the growing expenditure on healthcare.” ![]()

chemotherapy
Photo by Rhoda Baer
VIENNA—Results of the EUROCARE-5 study have revealed regional differences in survival for European patients with hematologic malignancies.
The data showed regional variations in 5-year relative survival rates for a number of cancers.
But the differences were particularly pronounced for leukemias, non-Hodgkin lymphomas (NHLs), and plasma cell neoplasms (PCNs).
Milena Sant, MD, of the Fondazione IRCCS Istituto Nazionale dei Tumori in Milan, Italy, presented these results at the 2015 European Cancer Congress (LBA 1).
Data from this study have also been published in several articles in the October 2015 issue of the European Journal of Cancer.
EUROCARE-5 includes records from 22 million cancer patients diagnosed between 1978 and 2007. The latest data encompass more than 10 million patients (ages 15 and older) diagnosed from 1995 to 2007 and followed up to 2008.
The data came from 107 cancer registries in 29 countries. The researchers estimated 5-year relative survival and trends from 1999 to 2007 according to region—Ireland/UK, Northern Europe, Central Europe, Southern Europe, and Eastern Europe.
“In general, 5-year relative survival—survival that is adjusted for causes of death other than cancer—increased steadily over time in Europe, particularly in Eastern Europe, for most cancers,” Dr Sant said.
“However, the most dramatic geographical variations were observed for cancers of the blood where there have been recent advances in treatment, such as chronic myeloid and lymphocytic leukemias, non-Hodgkin lymphoma and 2 of its subtypes (follicular and diffuse large B-cell lymphoma), and multiple myeloma. Hodgkin lymphoma was the exception, with smaller regional variations and a fairly good prognosis in most countries.”
Hodgkin lymphoma and NHL
Of all the hematologic malignancies, 5-year relative survival was highest for Hodgkin lymphoma, at 80.8% (40,625 cases). Five-year survival was 79.4% in Ireland and the UK, 85% in Northern countries, and 74.3% in Eastern Europe, which was significantly below the European average (P<0.0001).
For NHL, the 5-year relative survival was 59.4% (329,204 cases). Survival rates for NHL patients ranged from 49.7% in Eastern Europe to 63.3% in Northern Europe.
CLL/SLL
For chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), the 5-year relative survival was 70.4% (81,914 cases). CLL/SLL survival ranged from 58% in Eastern Europe to about 74% in Central and Northern Europe.
The researchers noted that between-country variations in CLL/SLL survival were high in all regions. Outliers that were significantly below the regional average were Austria (67%), Croatia (52%), and Bulgaria (45.5%).
PCNs
PCNs included multiple myeloma, plasmacytoma, and plasma cell leukemias. The 5-year relative survival for all PCNs was 39.2% (94,024 cases).
PCN survival rates were lowest in Eastern Europe (31.7%), slightly higher in the UK/Ireland (35.9%), and between 39.1% and 42% in the rest of Europe.
Myeloid leukemias
Of all the hematologic malignancies, 5-year relative survival was poorest for patients with acute myeloid leukemia (AML), at 17.1% (57,026 cases).
AML survival rates in Ireland/UK (15.0%) and Eastern Europe (13.0%) were significantly below the European average. But AML survival in Sweden, Belgium, France, and Germany was significantly higher than the average (P<0.005).
Five-year relative survival for chronic myeloid leukemia (CML) was 52.9% (17,713 cases).
Of all the hematologic malignancies, the survival gap between Eastern Europe and the rest of Europe was highest for CML. Five-year survival for CML patients was 33% in Eastern Europe and ranged from 51% to 58% in the rest of Europe.
The researchers also said there were striking survival variations by country in all areas. They found significant deviations from the regional average in Sweden (69.7%), Scotland (64.6%), France (71.7%), Austria (48.2%), Croatia (37.8%), Estonia (48.9%), Czech Republic (45.2%), and Latvia (22.1%).
“Results from EUROCARE can help to identify regions of low survival where action is needed to improve patients’ outcomes,” Dr Sant noted.
“Population-based survival information is essential for physicians, policy-makers, administrators, researchers, and patient organizations who deal with the needs of cancer patients, as well as with the issue of the growing expenditure on healthcare.” ![]()
CAR T-cell therapy tested in Sweden
NEW YORK—For the first time, according to researchers, chimeric antigen receptor (CAR) T-cell therapy has been tested in a clinical trial in Sweden.
Early results have shown the treatment can produce complete responses (CRs) in leukemia and lymphoma, although most patients ultimately progressed.
Hannah Karlsson, PhD, of Uppsala University in Sweden, presented data from the phase 1/2a trial of the third-generation CD19 CAR T-cell therapy (abstract A041*) at the inaugural CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference.
The trial is a collaboration between Uppsala University and Baylor College of Medicine and was funded by AFA Insurances AB and the Swedish Cancer Society.
“Third-generation CAR T cells are being tested in clinical trials for leukemia patients in the United States with success,” said senior study author Angelica Loskog, PhD, also of Uppsala University.
“[T]he main purpose of our clinical trial was to evaluate whether we could reproduce the successful results in leukemia patients in Sweden and to also test if patients with lymphoma will also respond to this treatment.”
So the investigators enrolled 13 patients, 11 of whom were evaluable for efficacy at 3 months after CAR T-cell infusion. All patients had relapsed or refractory, CD19-positive, B-cell disease.
Two patients had acute lymphoblastic leukemia (ALL), 2 had chronic lymphocytic leukemia (CLL), and 7 had lymphoma—3 with diffuse large B-cell lymphoma (DLBCL), 2 with mantle cell lymphoma (MCL), 1 with follicular lymphoma (FL)/DLBCL, and 1 with Burkitt lymphoma.
All of the lymphoma patients received chemotherapy before CAR T-cell infusion to shrink their tumors. Seven patients—3 with leukemia and 4 with lymphoma—received pre-conditioning with cyclophosphamide plus fludarabine to reduce their immunosuppressive cell counts.
The investigators used CAR T cells containing signaling domains from both CD28 and 4-1BB and manufactured using a gamma retrovirus.
Patients received a single infusion of the CAR T cells, 2 patients at a dose of 2 x 107 cells/m2, 4 at a dose of 1 x 108 cells/m2, and 5 at 2 x 108 cells/m2.
Response and toxicity
Six patients had achieved a CR at the time of evaluation.
One patient with DLBCL experienced mild cytokine release syndrome (CRS) before achieving CR. However, the patient relapsed after a second CRS occurred (after 3 months).
Another DLBCL patient achieved a CR prior to T-cell infusion and remained in CR for 6 months before progressing.
One CLL patient and another DLBCL patient responded prior to T-cell infusion and remained in CR for more than 3 months. The CLL patient was still in CR at the time of the meeting.
One of the ALL patients achieved a CR after transient central nervous system toxicity but relapsed at 3 months with CD19-negative ALL. The other ALL patient was in CR for more than a month after experiencing CRS but ultimately progressed.
One CLL patient and 2 MCL patients had all progressed by 3 months.
The FL/DLBCL patient progressed after 1 month, with mild CRS. And the patient with Burkitt lymphoma had major CRS and progressive disease.
The investigators noted that 5 of the 6 patients who received pre-conditioning treatment had initial CRs.
The team is now analyzing whether there is any correlation between the level of immunosuppressive cells and patient response. ![]()
*Information presented at the meeting differs from the abstract.
NEW YORK—For the first time, according to researchers, chimeric antigen receptor (CAR) T-cell therapy has been tested in a clinical trial in Sweden.
Early results have shown the treatment can produce complete responses (CRs) in leukemia and lymphoma, although most patients ultimately progressed.
Hannah Karlsson, PhD, of Uppsala University in Sweden, presented data from the phase 1/2a trial of the third-generation CD19 CAR T-cell therapy (abstract A041*) at the inaugural CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference.
The trial is a collaboration between Uppsala University and Baylor College of Medicine and was funded by AFA Insurances AB and the Swedish Cancer Society.
“Third-generation CAR T cells are being tested in clinical trials for leukemia patients in the United States with success,” said senior study author Angelica Loskog, PhD, also of Uppsala University.
“[T]he main purpose of our clinical trial was to evaluate whether we could reproduce the successful results in leukemia patients in Sweden and to also test if patients with lymphoma will also respond to this treatment.”
So the investigators enrolled 13 patients, 11 of whom were evaluable for efficacy at 3 months after CAR T-cell infusion. All patients had relapsed or refractory, CD19-positive, B-cell disease.
Two patients had acute lymphoblastic leukemia (ALL), 2 had chronic lymphocytic leukemia (CLL), and 7 had lymphoma—3 with diffuse large B-cell lymphoma (DLBCL), 2 with mantle cell lymphoma (MCL), 1 with follicular lymphoma (FL)/DLBCL, and 1 with Burkitt lymphoma.
All of the lymphoma patients received chemotherapy before CAR T-cell infusion to shrink their tumors. Seven patients—3 with leukemia and 4 with lymphoma—received pre-conditioning with cyclophosphamide plus fludarabine to reduce their immunosuppressive cell counts.
The investigators used CAR T cells containing signaling domains from both CD28 and 4-1BB and manufactured using a gamma retrovirus.
Patients received a single infusion of the CAR T cells, 2 patients at a dose of 2 x 107 cells/m2, 4 at a dose of 1 x 108 cells/m2, and 5 at 2 x 108 cells/m2.
Response and toxicity
Six patients had achieved a CR at the time of evaluation.
One patient with DLBCL experienced mild cytokine release syndrome (CRS) before achieving CR. However, the patient relapsed after a second CRS occurred (after 3 months).
Another DLBCL patient achieved a CR prior to T-cell infusion and remained in CR for 6 months before progressing.
One CLL patient and another DLBCL patient responded prior to T-cell infusion and remained in CR for more than 3 months. The CLL patient was still in CR at the time of the meeting.
One of the ALL patients achieved a CR after transient central nervous system toxicity but relapsed at 3 months with CD19-negative ALL. The other ALL patient was in CR for more than a month after experiencing CRS but ultimately progressed.
One CLL patient and 2 MCL patients had all progressed by 3 months.
The FL/DLBCL patient progressed after 1 month, with mild CRS. And the patient with Burkitt lymphoma had major CRS and progressive disease.
The investigators noted that 5 of the 6 patients who received pre-conditioning treatment had initial CRs.
The team is now analyzing whether there is any correlation between the level of immunosuppressive cells and patient response. ![]()
*Information presented at the meeting differs from the abstract.
NEW YORK—For the first time, according to researchers, chimeric antigen receptor (CAR) T-cell therapy has been tested in a clinical trial in Sweden.
Early results have shown the treatment can produce complete responses (CRs) in leukemia and lymphoma, although most patients ultimately progressed.
Hannah Karlsson, PhD, of Uppsala University in Sweden, presented data from the phase 1/2a trial of the third-generation CD19 CAR T-cell therapy (abstract A041*) at the inaugural CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference.
The trial is a collaboration between Uppsala University and Baylor College of Medicine and was funded by AFA Insurances AB and the Swedish Cancer Society.
“Third-generation CAR T cells are being tested in clinical trials for leukemia patients in the United States with success,” said senior study author Angelica Loskog, PhD, also of Uppsala University.
“[T]he main purpose of our clinical trial was to evaluate whether we could reproduce the successful results in leukemia patients in Sweden and to also test if patients with lymphoma will also respond to this treatment.”
So the investigators enrolled 13 patients, 11 of whom were evaluable for efficacy at 3 months after CAR T-cell infusion. All patients had relapsed or refractory, CD19-positive, B-cell disease.
Two patients had acute lymphoblastic leukemia (ALL), 2 had chronic lymphocytic leukemia (CLL), and 7 had lymphoma—3 with diffuse large B-cell lymphoma (DLBCL), 2 with mantle cell lymphoma (MCL), 1 with follicular lymphoma (FL)/DLBCL, and 1 with Burkitt lymphoma.
All of the lymphoma patients received chemotherapy before CAR T-cell infusion to shrink their tumors. Seven patients—3 with leukemia and 4 with lymphoma—received pre-conditioning with cyclophosphamide plus fludarabine to reduce their immunosuppressive cell counts.
The investigators used CAR T cells containing signaling domains from both CD28 and 4-1BB and manufactured using a gamma retrovirus.
Patients received a single infusion of the CAR T cells, 2 patients at a dose of 2 x 107 cells/m2, 4 at a dose of 1 x 108 cells/m2, and 5 at 2 x 108 cells/m2.
Response and toxicity
Six patients had achieved a CR at the time of evaluation.
One patient with DLBCL experienced mild cytokine release syndrome (CRS) before achieving CR. However, the patient relapsed after a second CRS occurred (after 3 months).
Another DLBCL patient achieved a CR prior to T-cell infusion and remained in CR for 6 months before progressing.
One CLL patient and another DLBCL patient responded prior to T-cell infusion and remained in CR for more than 3 months. The CLL patient was still in CR at the time of the meeting.
One of the ALL patients achieved a CR after transient central nervous system toxicity but relapsed at 3 months with CD19-negative ALL. The other ALL patient was in CR for more than a month after experiencing CRS but ultimately progressed.
One CLL patient and 2 MCL patients had all progressed by 3 months.
The FL/DLBCL patient progressed after 1 month, with mild CRS. And the patient with Burkitt lymphoma had major CRS and progressive disease.
The investigators noted that 5 of the 6 patients who received pre-conditioning treatment had initial CRs.
The team is now analyzing whether there is any correlation between the level of immunosuppressive cells and patient response. ![]()
*Information presented at the meeting differs from the abstract.
Obinutuzumab trends better than rituxumab in relapsed indolent lymphoma
Patients with relapsed follicular lymphoma who were treated with obinutuzumab experienced higher response rates than did patients given rituximab with an acceptable safety profile, according to new findings.
However, the difference did not translate into an improvement in progression-free survival, so the clinical value of obinutuzumab in this patient population is still unclear.
The quality of remissions was better with obinutuzumab, with an almost twofold higher complete response/unconfirmed complete response rate (41.9% vs. 22.7%; P = .006),” wrote Dr. Laurie Sehn from the Centre for Lymphoid Cancer, British Columbia Cancer Agency and the University of British Columbia, Vancouver, and her colleagues (J Clin Oncol. 2015 Aug 17. doi:10.1200/JCO.2014.59.2139).
On the basis of an independent review, the best overall response was better in the obinutuzumab arm (P = .04), but the complete response/unconfirmed response rate was not different for the two groups.
The study was published online Aug. 17 in the Journal of Clinical Oncology.
A total of 175 patients with relapsed CD20+ indolent lymphoma were randomized 1:1 to four once-per-week infusions of either obinutuzumab (1,000 mg) or rituximab (375 mg/m2). Those without any evidence of disease progression after completing induction therapy received obinutuzumab or rituximab maintenance therapy every 2 months for up to 2 years.
At the end of induction, the investigator assessed overall response rate was 44.6% in the obinutuzumab arm and 33.3% in the rituximab arm (P = .08); nine patients receiving obinutuzumab (12.2%) and four given rituximab (5.3%) achieved complete response or unconfirmed complete response, but the difference was not significant (P = .07).
Independent review also found the overall response rate to be higher with obinutuzumab vs. rituximab (44.6% vs. 26.7%; P = .01), but with no difference in complete response/unconfirmed complete response rate (5.4 vs. 4.0; P = .34).
Adverse events were similar in each group, and most episodes were grade 1 to 2. Higher rates of infusion-related reactions (74% vs. 51%) and cough (24% vs. 9%) were observed in the obinutuzumab vs. the rituximab arm.
Dr. Sehn receives research funding and honoraria from, and serves in a consulting or advisory role to, Roche/Genentech, the maker of obinutuzumab (Gyzyva) and rituximab (Rituxan). She also receives honoraria from and serves in a consulting or advisory role to Amgen, Janssen, Seattle Genetics, Lundbeck, and Celgene.
Patients with relapsed follicular lymphoma who were treated with obinutuzumab experienced higher response rates than did patients given rituximab with an acceptable safety profile, according to new findings.
However, the difference did not translate into an improvement in progression-free survival, so the clinical value of obinutuzumab in this patient population is still unclear.
The quality of remissions was better with obinutuzumab, with an almost twofold higher complete response/unconfirmed complete response rate (41.9% vs. 22.7%; P = .006),” wrote Dr. Laurie Sehn from the Centre for Lymphoid Cancer, British Columbia Cancer Agency and the University of British Columbia, Vancouver, and her colleagues (J Clin Oncol. 2015 Aug 17. doi:10.1200/JCO.2014.59.2139).
On the basis of an independent review, the best overall response was better in the obinutuzumab arm (P = .04), but the complete response/unconfirmed response rate was not different for the two groups.
The study was published online Aug. 17 in the Journal of Clinical Oncology.
A total of 175 patients with relapsed CD20+ indolent lymphoma were randomized 1:1 to four once-per-week infusions of either obinutuzumab (1,000 mg) or rituximab (375 mg/m2). Those without any evidence of disease progression after completing induction therapy received obinutuzumab or rituximab maintenance therapy every 2 months for up to 2 years.
At the end of induction, the investigator assessed overall response rate was 44.6% in the obinutuzumab arm and 33.3% in the rituximab arm (P = .08); nine patients receiving obinutuzumab (12.2%) and four given rituximab (5.3%) achieved complete response or unconfirmed complete response, but the difference was not significant (P = .07).
Independent review also found the overall response rate to be higher with obinutuzumab vs. rituximab (44.6% vs. 26.7%; P = .01), but with no difference in complete response/unconfirmed complete response rate (5.4 vs. 4.0; P = .34).
Adverse events were similar in each group, and most episodes were grade 1 to 2. Higher rates of infusion-related reactions (74% vs. 51%) and cough (24% vs. 9%) were observed in the obinutuzumab vs. the rituximab arm.
Dr. Sehn receives research funding and honoraria from, and serves in a consulting or advisory role to, Roche/Genentech, the maker of obinutuzumab (Gyzyva) and rituximab (Rituxan). She also receives honoraria from and serves in a consulting or advisory role to Amgen, Janssen, Seattle Genetics, Lundbeck, and Celgene.
Patients with relapsed follicular lymphoma who were treated with obinutuzumab experienced higher response rates than did patients given rituximab with an acceptable safety profile, according to new findings.
However, the difference did not translate into an improvement in progression-free survival, so the clinical value of obinutuzumab in this patient population is still unclear.
The quality of remissions was better with obinutuzumab, with an almost twofold higher complete response/unconfirmed complete response rate (41.9% vs. 22.7%; P = .006),” wrote Dr. Laurie Sehn from the Centre for Lymphoid Cancer, British Columbia Cancer Agency and the University of British Columbia, Vancouver, and her colleagues (J Clin Oncol. 2015 Aug 17. doi:10.1200/JCO.2014.59.2139).
On the basis of an independent review, the best overall response was better in the obinutuzumab arm (P = .04), but the complete response/unconfirmed response rate was not different for the two groups.
The study was published online Aug. 17 in the Journal of Clinical Oncology.
A total of 175 patients with relapsed CD20+ indolent lymphoma were randomized 1:1 to four once-per-week infusions of either obinutuzumab (1,000 mg) or rituximab (375 mg/m2). Those without any evidence of disease progression after completing induction therapy received obinutuzumab or rituximab maintenance therapy every 2 months for up to 2 years.
At the end of induction, the investigator assessed overall response rate was 44.6% in the obinutuzumab arm and 33.3% in the rituximab arm (P = .08); nine patients receiving obinutuzumab (12.2%) and four given rituximab (5.3%) achieved complete response or unconfirmed complete response, but the difference was not significant (P = .07).
Independent review also found the overall response rate to be higher with obinutuzumab vs. rituximab (44.6% vs. 26.7%; P = .01), but with no difference in complete response/unconfirmed complete response rate (5.4 vs. 4.0; P = .34).
Adverse events were similar in each group, and most episodes were grade 1 to 2. Higher rates of infusion-related reactions (74% vs. 51%) and cough (24% vs. 9%) were observed in the obinutuzumab vs. the rituximab arm.
Dr. Sehn receives research funding and honoraria from, and serves in a consulting or advisory role to, Roche/Genentech, the maker of obinutuzumab (Gyzyva) and rituximab (Rituxan). She also receives honoraria from and serves in a consulting or advisory role to Amgen, Janssen, Seattle Genetics, Lundbeck, and Celgene.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Obinutuzumab was associated with a higher overall response rate as compared with rituximab, but obinutuzumab’s clinical benefit in non–Hodgkin lymphoma is still unclear.
Major finding: Among patients with follicular lymphoma (n = 149), overall response rate trended higher for obinutuzumab, compared with rituximab (44.6% vs. 33.3%; P = .08).
Data source: An open-label, multicenter, randomized, phase II study of 175 patients with relapsed CD20+ indolent lymphoma that compared induction with obinutuzumab vs. rituximab.
Disclosures: Dr. Sehn receives research funding and honoraria from, and serves in a consulting or advisory role to Roche/Genentech, the maker of obinutuzumab (Gyzyva) and rituximab (Rituxan). She also receives honoraria from and serves in a consulting or advisory role to Amgen, Janssen, Seattle Genetics, Lundbeck, and Celgene.
Lenalidomide + rituximab combo effective in recurrent follicular lymphoma
The combination of lenalidomide and rituximab was more active in patients with recurrent follicular lymphoma, compared with lenalidomide alone, and significantly increased the overall response rate, according to new data published online Aug. 24 in the Journal of Clinical Oncology.
Although both lenalidomide and rituximab are active agents in follicular lymphoma, their combined use in recurrent follicular lymphoma has not been previously evaluated in randomized clinical trials, said Dr. John P. Leonard of Cornell University, New York, and his colleagues.
The overall response rate of patients receiving the combination regimen was significantly higher than that of patients who received lenalidomide alone (P = .029). In the cohort receiving lenalidomide alone, 24 patients (53%) achieved an objective response (9 complete responses [20%]), while 35 patients (76%) in the lenalidomide/rituximab group were responders (18 complete responses [39%]).
At a median follow-up of 2.5 years (range, 0.1-4.8 years), the addition of rituximab to lenalidomide in this population also significantly increased the median time to progression: 1.1 year for lenalidomide alone versus 2 years for the combined therapy (P = .002).
Overall survival was 4.5 years for lenalidomide alone and has not yet been reached for the combination arm (P = .149.
This trial helps to establish the safety profile of single-agent lenalidomide in follicular lymphoma, while its “randomized nature also allows a direct assessment of potential toxicity resulting from the addition of rituximab to lenalidomide,” wrote Dr. Leonard and his associates (J Clin Oncol. 2015 Aug 24. doi: 10.1200/JCO.2014.59.9258).
“There was no evidence of increased toxicity from the lenalidomide/rituximab combination compared with lenalidomide alone,” they pointed out.
Both lenalidomide alone and lenalidomide/rituximab were well tolerated, with grade 3-4 adverse events occurring in 58% and 53% of patients, respectively, with 9% and 11% of patients experiencing grade 4 toxicity, respectively. The most common grade 3-4 adverse events included neutropenia (16% vs. 20%), fatigue (9% vs. 13%), and rash (4% vs. 4%).
The study was supported in part by grants from the National Cancer Institute to the Alliance for Clinical Trials in Oncology. Dr. Leonard reported financial relationships with Celgene and Genentech, and several coauthors also reported relationships with industry.
The combination of lenalidomide and rituximab was more active in patients with recurrent follicular lymphoma, compared with lenalidomide alone, and significantly increased the overall response rate, according to new data published online Aug. 24 in the Journal of Clinical Oncology.
Although both lenalidomide and rituximab are active agents in follicular lymphoma, their combined use in recurrent follicular lymphoma has not been previously evaluated in randomized clinical trials, said Dr. John P. Leonard of Cornell University, New York, and his colleagues.
The overall response rate of patients receiving the combination regimen was significantly higher than that of patients who received lenalidomide alone (P = .029). In the cohort receiving lenalidomide alone, 24 patients (53%) achieved an objective response (9 complete responses [20%]), while 35 patients (76%) in the lenalidomide/rituximab group were responders (18 complete responses [39%]).
At a median follow-up of 2.5 years (range, 0.1-4.8 years), the addition of rituximab to lenalidomide in this population also significantly increased the median time to progression: 1.1 year for lenalidomide alone versus 2 years for the combined therapy (P = .002).
Overall survival was 4.5 years for lenalidomide alone and has not yet been reached for the combination arm (P = .149.
This trial helps to establish the safety profile of single-agent lenalidomide in follicular lymphoma, while its “randomized nature also allows a direct assessment of potential toxicity resulting from the addition of rituximab to lenalidomide,” wrote Dr. Leonard and his associates (J Clin Oncol. 2015 Aug 24. doi: 10.1200/JCO.2014.59.9258).
“There was no evidence of increased toxicity from the lenalidomide/rituximab combination compared with lenalidomide alone,” they pointed out.
Both lenalidomide alone and lenalidomide/rituximab were well tolerated, with grade 3-4 adverse events occurring in 58% and 53% of patients, respectively, with 9% and 11% of patients experiencing grade 4 toxicity, respectively. The most common grade 3-4 adverse events included neutropenia (16% vs. 20%), fatigue (9% vs. 13%), and rash (4% vs. 4%).
The study was supported in part by grants from the National Cancer Institute to the Alliance for Clinical Trials in Oncology. Dr. Leonard reported financial relationships with Celgene and Genentech, and several coauthors also reported relationships with industry.
The combination of lenalidomide and rituximab was more active in patients with recurrent follicular lymphoma, compared with lenalidomide alone, and significantly increased the overall response rate, according to new data published online Aug. 24 in the Journal of Clinical Oncology.
Although both lenalidomide and rituximab are active agents in follicular lymphoma, their combined use in recurrent follicular lymphoma has not been previously evaluated in randomized clinical trials, said Dr. John P. Leonard of Cornell University, New York, and his colleagues.
The overall response rate of patients receiving the combination regimen was significantly higher than that of patients who received lenalidomide alone (P = .029). In the cohort receiving lenalidomide alone, 24 patients (53%) achieved an objective response (9 complete responses [20%]), while 35 patients (76%) in the lenalidomide/rituximab group were responders (18 complete responses [39%]).
At a median follow-up of 2.5 years (range, 0.1-4.8 years), the addition of rituximab to lenalidomide in this population also significantly increased the median time to progression: 1.1 year for lenalidomide alone versus 2 years for the combined therapy (P = .002).
Overall survival was 4.5 years for lenalidomide alone and has not yet been reached for the combination arm (P = .149.
This trial helps to establish the safety profile of single-agent lenalidomide in follicular lymphoma, while its “randomized nature also allows a direct assessment of potential toxicity resulting from the addition of rituximab to lenalidomide,” wrote Dr. Leonard and his associates (J Clin Oncol. 2015 Aug 24. doi: 10.1200/JCO.2014.59.9258).
“There was no evidence of increased toxicity from the lenalidomide/rituximab combination compared with lenalidomide alone,” they pointed out.
Both lenalidomide alone and lenalidomide/rituximab were well tolerated, with grade 3-4 adverse events occurring in 58% and 53% of patients, respectively, with 9% and 11% of patients experiencing grade 4 toxicity, respectively. The most common grade 3-4 adverse events included neutropenia (16% vs. 20%), fatigue (9% vs. 13%), and rash (4% vs. 4%).
The study was supported in part by grants from the National Cancer Institute to the Alliance for Clinical Trials in Oncology. Dr. Leonard reported financial relationships with Celgene and Genentech, and several coauthors also reported relationships with industry.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Lenalidomide combined with rituximab is more active in recurrent follicular lymphoma, compared with lenalidomide monotherapy.
Major finding: Overall response rate was 53% (20% complete response) for lenalidomide alone versus 76% (39% complete response) for lenalidomide and rituximab (P = .029).
Data source: Randomized phase II clinical trial of 91 patients with follicular lymphoma who were assigned to receive lenalidomide alone or lenalidomide combined with rituximab.
Disclosures: The study was supported in part by grants from the National Cancer Institute to the Alliance for Clinical Trials in Oncology. Dr. Leonard reported financial relationships with Celgene and Genentech, and several coauthors also reported relationships with industry.
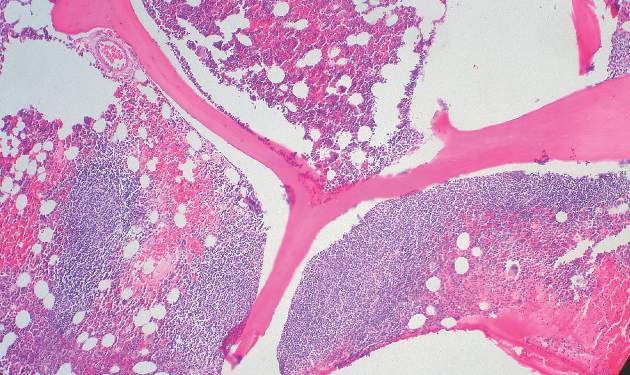
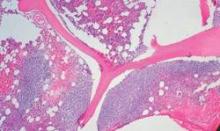
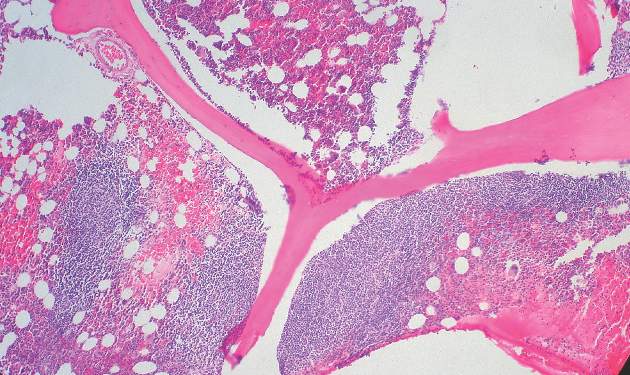
New prognostic model for follicular lymphoma

Photo courtesy of NIH
A newly developed prognostic model can identify follicular lymphoma (FL) patients at the highest risk for treatment failure, according to researchers.
To create this model, called m7-FLIPI, the team combined the Follicular Lymphoma International Prognostic Index (FLIPI), Eastern Cooperative Oncology Group (ECOG) performance status, and the mutation status of 7 genes—EZH2, ARID1A, MEF2B, EP300, FOXO1, CREBBP, and CARD11.
The researchers said this is the first prognostic model for FL that accounts for both clinical factors and genetic mutations.
They described the creation and testing of the model in The Lancet Oncology.
“We set out to determine, at the time of diagnosis, which patients’ disease will have sustained responses after treatment and whether new genetic data could help inform which patients are at risk for developing progressive lymphoma so clinicians would be able to offer these high-risk patients more effective therapies,” said Randy Gascoyne, MD, of the British Columbia Cancer Agency in Vancouver, Canada.
He and his colleagues created the m7-FLIPI by conducting a retrospective analysis of genetic mutations and clinical risk factors in 2 cohorts of patients with symptomatic, advanced stage, or bulky FL grade 1, 2, or 3A.
The patients had a biopsy specimen collected 12 months or less before they began first-line treatment with an immunochemotherapy regimen containing rituximab.
Training cohort
The training cohort consisted of 151 FL patients who received R-CHOP. The median follow-up for these patients was 7.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found 28% of patients (43/151) were defined as high-risk, with a 5-year failure-free survival (FFS) rate of 38.29%.
And 72% of patients (108/151) were defined as low-risk, with a 5-year FFS of 77.21%. The hazard ratio was 4.14 (P<0.0001).
The positive predictive value for 5-year FFS was 64%, and the negative predictive value was 78%. The m7-FLIPI outperformed a prognostic model of only gene mutations and the FLIPI-2.
Validation cohort
The validation cohort consisted of 107 patients who received R-CVP. The median follow-up for these patients was 6.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found that 22% of patients (24/107) were defined as high-risk, with a 5-year FFS of 25%.
And 78% of patients (83/107) were defined as low-risk, with a 5-year FFS of 68.24%. The hazard ratio was 3.58 (P<0.0001).
The positive predictive value for 5-year FFS was 72%, and the negative predictive value was 68%. The m7-FLIPI outperformed the FLIPI alone and the FLIPI combined with ECOG performance status.
Overall survival
Although the m7-FLIPI was designed specifically for FFS, the researchers also tested its prognostic utility for overall survival (OS).
In the training cohort, high-risk disease according to the m7-FLIPI was associated with a 5-year OS of 65.25%, compared to 89.98% for low-risk disease (P=0.00031).
In the validation cohort, 5-year OS was 41.67% for patients with high-risk disease and 84.01% for patients with low-risk disease (P<0.0001). In both cohorts, the m7-FLIPI outperformed the FLIPI alone.
Based on these results, the researchers believe the m7-FLIPI could be utilized in a clinical setting to test all new FL patients at diagnosis and identify patients who harbor the most aggressive disease.
“The m7-FLIPI could be extremely significant for the medical community,” Dr Gascoyne said, “changing the story for high-risk patients who are currently destined to not respond well to standard treatment.” ![]()

Photo courtesy of NIH
A newly developed prognostic model can identify follicular lymphoma (FL) patients at the highest risk for treatment failure, according to researchers.
To create this model, called m7-FLIPI, the team combined the Follicular Lymphoma International Prognostic Index (FLIPI), Eastern Cooperative Oncology Group (ECOG) performance status, and the mutation status of 7 genes—EZH2, ARID1A, MEF2B, EP300, FOXO1, CREBBP, and CARD11.
The researchers said this is the first prognostic model for FL that accounts for both clinical factors and genetic mutations.
They described the creation and testing of the model in The Lancet Oncology.
“We set out to determine, at the time of diagnosis, which patients’ disease will have sustained responses after treatment and whether new genetic data could help inform which patients are at risk for developing progressive lymphoma so clinicians would be able to offer these high-risk patients more effective therapies,” said Randy Gascoyne, MD, of the British Columbia Cancer Agency in Vancouver, Canada.
He and his colleagues created the m7-FLIPI by conducting a retrospective analysis of genetic mutations and clinical risk factors in 2 cohorts of patients with symptomatic, advanced stage, or bulky FL grade 1, 2, or 3A.
The patients had a biopsy specimen collected 12 months or less before they began first-line treatment with an immunochemotherapy regimen containing rituximab.
Training cohort
The training cohort consisted of 151 FL patients who received R-CHOP. The median follow-up for these patients was 7.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found 28% of patients (43/151) were defined as high-risk, with a 5-year failure-free survival (FFS) rate of 38.29%.
And 72% of patients (108/151) were defined as low-risk, with a 5-year FFS of 77.21%. The hazard ratio was 4.14 (P<0.0001).
The positive predictive value for 5-year FFS was 64%, and the negative predictive value was 78%. The m7-FLIPI outperformed a prognostic model of only gene mutations and the FLIPI-2.
Validation cohort
The validation cohort consisted of 107 patients who received R-CVP. The median follow-up for these patients was 6.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found that 22% of patients (24/107) were defined as high-risk, with a 5-year FFS of 25%.
And 78% of patients (83/107) were defined as low-risk, with a 5-year FFS of 68.24%. The hazard ratio was 3.58 (P<0.0001).
The positive predictive value for 5-year FFS was 72%, and the negative predictive value was 68%. The m7-FLIPI outperformed the FLIPI alone and the FLIPI combined with ECOG performance status.
Overall survival
Although the m7-FLIPI was designed specifically for FFS, the researchers also tested its prognostic utility for overall survival (OS).
In the training cohort, high-risk disease according to the m7-FLIPI was associated with a 5-year OS of 65.25%, compared to 89.98% for low-risk disease (P=0.00031).
In the validation cohort, 5-year OS was 41.67% for patients with high-risk disease and 84.01% for patients with low-risk disease (P<0.0001). In both cohorts, the m7-FLIPI outperformed the FLIPI alone.
Based on these results, the researchers believe the m7-FLIPI could be utilized in a clinical setting to test all new FL patients at diagnosis and identify patients who harbor the most aggressive disease.
“The m7-FLIPI could be extremely significant for the medical community,” Dr Gascoyne said, “changing the story for high-risk patients who are currently destined to not respond well to standard treatment.” ![]()

Photo courtesy of NIH
A newly developed prognostic model can identify follicular lymphoma (FL) patients at the highest risk for treatment failure, according to researchers.
To create this model, called m7-FLIPI, the team combined the Follicular Lymphoma International Prognostic Index (FLIPI), Eastern Cooperative Oncology Group (ECOG) performance status, and the mutation status of 7 genes—EZH2, ARID1A, MEF2B, EP300, FOXO1, CREBBP, and CARD11.
The researchers said this is the first prognostic model for FL that accounts for both clinical factors and genetic mutations.
They described the creation and testing of the model in The Lancet Oncology.
“We set out to determine, at the time of diagnosis, which patients’ disease will have sustained responses after treatment and whether new genetic data could help inform which patients are at risk for developing progressive lymphoma so clinicians would be able to offer these high-risk patients more effective therapies,” said Randy Gascoyne, MD, of the British Columbia Cancer Agency in Vancouver, Canada.
He and his colleagues created the m7-FLIPI by conducting a retrospective analysis of genetic mutations and clinical risk factors in 2 cohorts of patients with symptomatic, advanced stage, or bulky FL grade 1, 2, or 3A.
The patients had a biopsy specimen collected 12 months or less before they began first-line treatment with an immunochemotherapy regimen containing rituximab.
Training cohort
The training cohort consisted of 151 FL patients who received R-CHOP. The median follow-up for these patients was 7.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found 28% of patients (43/151) were defined as high-risk, with a 5-year failure-free survival (FFS) rate of 38.29%.
And 72% of patients (108/151) were defined as low-risk, with a 5-year FFS of 77.21%. The hazard ratio was 4.14 (P<0.0001).
The positive predictive value for 5-year FFS was 64%, and the negative predictive value was 78%. The m7-FLIPI outperformed a prognostic model of only gene mutations and the FLIPI-2.
Validation cohort
The validation cohort consisted of 107 patients who received R-CVP. The median follow-up for these patients was 6.7 years.
When the researchers applied the m7-FLIPI to this cohort, they found that 22% of patients (24/107) were defined as high-risk, with a 5-year FFS of 25%.
And 78% of patients (83/107) were defined as low-risk, with a 5-year FFS of 68.24%. The hazard ratio was 3.58 (P<0.0001).
The positive predictive value for 5-year FFS was 72%, and the negative predictive value was 68%. The m7-FLIPI outperformed the FLIPI alone and the FLIPI combined with ECOG performance status.
Overall survival
Although the m7-FLIPI was designed specifically for FFS, the researchers also tested its prognostic utility for overall survival (OS).
In the training cohort, high-risk disease according to the m7-FLIPI was associated with a 5-year OS of 65.25%, compared to 89.98% for low-risk disease (P=0.00031).
In the validation cohort, 5-year OS was 41.67% for patients with high-risk disease and 84.01% for patients with low-risk disease (P<0.0001). In both cohorts, the m7-FLIPI outperformed the FLIPI alone.
Based on these results, the researchers believe the m7-FLIPI could be utilized in a clinical setting to test all new FL patients at diagnosis and identify patients who harbor the most aggressive disease.
“The m7-FLIPI could be extremely significant for the medical community,” Dr Gascoyne said, “changing the story for high-risk patients who are currently destined to not respond well to standard treatment.” ![]()
Early follicular lymphoma progression signals poor outcomes
For patients with follicular lymphoma treated with a rituximab-based combination chemotherapy regimen, early disease progression is associated with significantly worse overall survival, suggesting the need for additional interventions, according to results of a multicenter study.
Among 588 patients with stage 2-4 follicular lymphoma treated with first-line R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone) and followed for a median of 7 years in the National LymphoCare Study, overall survival (OS) at 2 years was 68% for those who had disease progression within 2 years, compared with 97% for patients with no disease progression during that time.
Similarly, 5-year overall survival was 50% for patients with early progression of disease, compared with 90% for patients with no early progression, write Dr. Carla Casulo of the University of Rochester (N.Y.) Medical Center and colleagues. The study is in anearly online publication in the Journal of Clinical Oncology.
“Given our findings, early relapse after diagnosis in patients treated with first-line chemoimmunotherapy is a powerful prognostic indicator of outcome and should be used to stratify the risk of patients in studies of relapsed follicular lymphoma,” the authors wrote.
The findings were validated in an independent cohort of patients with follicular lymphoma treated with R-CHOP from the University of Iowa and Mayo Clinical Molecular Epidemiology Resource, and are consistent with findings from other studies of patients treated with different rituximab-based regimens, the investigators reported.
In unadjusted analysis, early disease progression was associated with a hazard ratio (HR) of 7.17 (95% confidence interval [CI] 4.83-10.65); the effect remained after adjustment for the Follicular Lymphoma International Prognostic Index (FLIPI) score (HR 6.44, 95% CI, 4.33-9.58).
Factors associated with early progression included age, Eastern Cooperative Oncology Group performance score, nodal sites, and disease stage.
Early use of aggressive salvage therapies or autologous stem-cell transplantation could improve outcomes in patients with early disease progression, the authors wrote. However, only 8 patients among the 110 with early progression went on to transplant, not a large enough sample for meaningful analysis, they added.
“This newly defined high-risk group of patients represents a distinct population in whom further study is warranted in both directed prospective clinical trials of follicular lymphoma biology and treatment. Moreover, we propose that 2-year progression-free survival may be a practical and meaningful clinical end point for trials involving a chemoimmunotherapy backbone,” they concluded.
If, in studying the immunologic and inflammatory host response to, and the genetic landscape of, these lymphomas, we are able to define this high-risk subgroup of patients with follicular lymphoma, the question becomes whether we could use this information to effectively treat these patients differently. Although high-dose chemotherapy and autologous stem-cell transplantation (HDC-ASCT) in first remission seems to have no effect on OS in all comers, results might be different for this cohort of high-risk patients. To study this would require an ability to identify these patients at diagnosis. Given that the efficacy of HDC-ASCT is maintained in the case of chemosensitive relapse, reserving HDC-ASCT for patients who relapse within the first 2 years of their initial therapy may be a more prudent strategy.
However, it may be that this is a particularly chemoresistant population and that, instead, attention should be paid to targeting the biologic and genetic factors that contribute to the poor prognosis of this group. Given the negative differential outcomes in patients with decreased tumor-infiltrating lymphocytes and increased monocyte/macrophage activation, immunologic approaches in the salvage setting, including immune checkpoint blockade drugs, chimeric antigen receptor T cells, and allogeneic transplantation may be biologically relevant.
Dr. Caron A. Jacobson and Dr. Arnold S. Freedman, of the Dana-Farber Cancer Institute and Harvard Medical School, Boston, made their remarks in an editorial accompanying the study.
If, in studying the immunologic and inflammatory host response to, and the genetic landscape of, these lymphomas, we are able to define this high-risk subgroup of patients with follicular lymphoma, the question becomes whether we could use this information to effectively treat these patients differently. Although high-dose chemotherapy and autologous stem-cell transplantation (HDC-ASCT) in first remission seems to have no effect on OS in all comers, results might be different for this cohort of high-risk patients. To study this would require an ability to identify these patients at diagnosis. Given that the efficacy of HDC-ASCT is maintained in the case of chemosensitive relapse, reserving HDC-ASCT for patients who relapse within the first 2 years of their initial therapy may be a more prudent strategy.
However, it may be that this is a particularly chemoresistant population and that, instead, attention should be paid to targeting the biologic and genetic factors that contribute to the poor prognosis of this group. Given the negative differential outcomes in patients with decreased tumor-infiltrating lymphocytes and increased monocyte/macrophage activation, immunologic approaches in the salvage setting, including immune checkpoint blockade drugs, chimeric antigen receptor T cells, and allogeneic transplantation may be biologically relevant.
Dr. Caron A. Jacobson and Dr. Arnold S. Freedman, of the Dana-Farber Cancer Institute and Harvard Medical School, Boston, made their remarks in an editorial accompanying the study.
If, in studying the immunologic and inflammatory host response to, and the genetic landscape of, these lymphomas, we are able to define this high-risk subgroup of patients with follicular lymphoma, the question becomes whether we could use this information to effectively treat these patients differently. Although high-dose chemotherapy and autologous stem-cell transplantation (HDC-ASCT) in first remission seems to have no effect on OS in all comers, results might be different for this cohort of high-risk patients. To study this would require an ability to identify these patients at diagnosis. Given that the efficacy of HDC-ASCT is maintained in the case of chemosensitive relapse, reserving HDC-ASCT for patients who relapse within the first 2 years of their initial therapy may be a more prudent strategy.
However, it may be that this is a particularly chemoresistant population and that, instead, attention should be paid to targeting the biologic and genetic factors that contribute to the poor prognosis of this group. Given the negative differential outcomes in patients with decreased tumor-infiltrating lymphocytes and increased monocyte/macrophage activation, immunologic approaches in the salvage setting, including immune checkpoint blockade drugs, chimeric antigen receptor T cells, and allogeneic transplantation may be biologically relevant.
Dr. Caron A. Jacobson and Dr. Arnold S. Freedman, of the Dana-Farber Cancer Institute and Harvard Medical School, Boston, made their remarks in an editorial accompanying the study.
For patients with follicular lymphoma treated with a rituximab-based combination chemotherapy regimen, early disease progression is associated with significantly worse overall survival, suggesting the need for additional interventions, according to results of a multicenter study.
Among 588 patients with stage 2-4 follicular lymphoma treated with first-line R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone) and followed for a median of 7 years in the National LymphoCare Study, overall survival (OS) at 2 years was 68% for those who had disease progression within 2 years, compared with 97% for patients with no disease progression during that time.
Similarly, 5-year overall survival was 50% for patients with early progression of disease, compared with 90% for patients with no early progression, write Dr. Carla Casulo of the University of Rochester (N.Y.) Medical Center and colleagues. The study is in anearly online publication in the Journal of Clinical Oncology.
“Given our findings, early relapse after diagnosis in patients treated with first-line chemoimmunotherapy is a powerful prognostic indicator of outcome and should be used to stratify the risk of patients in studies of relapsed follicular lymphoma,” the authors wrote.
The findings were validated in an independent cohort of patients with follicular lymphoma treated with R-CHOP from the University of Iowa and Mayo Clinical Molecular Epidemiology Resource, and are consistent with findings from other studies of patients treated with different rituximab-based regimens, the investigators reported.
In unadjusted analysis, early disease progression was associated with a hazard ratio (HR) of 7.17 (95% confidence interval [CI] 4.83-10.65); the effect remained after adjustment for the Follicular Lymphoma International Prognostic Index (FLIPI) score (HR 6.44, 95% CI, 4.33-9.58).
Factors associated with early progression included age, Eastern Cooperative Oncology Group performance score, nodal sites, and disease stage.
Early use of aggressive salvage therapies or autologous stem-cell transplantation could improve outcomes in patients with early disease progression, the authors wrote. However, only 8 patients among the 110 with early progression went on to transplant, not a large enough sample for meaningful analysis, they added.
“This newly defined high-risk group of patients represents a distinct population in whom further study is warranted in both directed prospective clinical trials of follicular lymphoma biology and treatment. Moreover, we propose that 2-year progression-free survival may be a practical and meaningful clinical end point for trials involving a chemoimmunotherapy backbone,” they concluded.
For patients with follicular lymphoma treated with a rituximab-based combination chemotherapy regimen, early disease progression is associated with significantly worse overall survival, suggesting the need for additional interventions, according to results of a multicenter study.
Among 588 patients with stage 2-4 follicular lymphoma treated with first-line R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone) and followed for a median of 7 years in the National LymphoCare Study, overall survival (OS) at 2 years was 68% for those who had disease progression within 2 years, compared with 97% for patients with no disease progression during that time.
Similarly, 5-year overall survival was 50% for patients with early progression of disease, compared with 90% for patients with no early progression, write Dr. Carla Casulo of the University of Rochester (N.Y.) Medical Center and colleagues. The study is in anearly online publication in the Journal of Clinical Oncology.
“Given our findings, early relapse after diagnosis in patients treated with first-line chemoimmunotherapy is a powerful prognostic indicator of outcome and should be used to stratify the risk of patients in studies of relapsed follicular lymphoma,” the authors wrote.
The findings were validated in an independent cohort of patients with follicular lymphoma treated with R-CHOP from the University of Iowa and Mayo Clinical Molecular Epidemiology Resource, and are consistent with findings from other studies of patients treated with different rituximab-based regimens, the investigators reported.
In unadjusted analysis, early disease progression was associated with a hazard ratio (HR) of 7.17 (95% confidence interval [CI] 4.83-10.65); the effect remained after adjustment for the Follicular Lymphoma International Prognostic Index (FLIPI) score (HR 6.44, 95% CI, 4.33-9.58).
Factors associated with early progression included age, Eastern Cooperative Oncology Group performance score, nodal sites, and disease stage.
Early use of aggressive salvage therapies or autologous stem-cell transplantation could improve outcomes in patients with early disease progression, the authors wrote. However, only 8 patients among the 110 with early progression went on to transplant, not a large enough sample for meaningful analysis, they added.
“This newly defined high-risk group of patients represents a distinct population in whom further study is warranted in both directed prospective clinical trials of follicular lymphoma biology and treatment. Moreover, we propose that 2-year progression-free survival may be a practical and meaningful clinical end point for trials involving a chemoimmunotherapy backbone,” they concluded.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Disease progression within 2 years of chemotherapy for follicular lymphoma is associated with poor outcomes.
Major finding: Five-year overall survival was 50% for patients with follicular lymphoma with disease progression within 2-years of R-CHOP, vs. 90% for patients with no early progression.
Data source: Retrospective review involving 588 patients in the longitudinal National LymphoCare Study.
Disclosures: Genentech and F. Hoffmann-La Roche supported the study. Dr. Casulo and Dr. Jacobson reported no relevant disclosures. Dr. Freedman reported ties with UpToDate, Axio, and Immunogen.
Prenatal test results linked to cancer in mothers

Photo by Nina Matthews
Researchers have again found evidence to suggest that tests used to identify chromosomal fetal disorders can detect occult malignancies in pregnant women.
In a study made public last month, non-invasive prenatal tests (NIPTs) revealed 2 cases of lymphoma and a case of ovarian cancer in expectant mothers.
In the new study, researchers showed that positive NIPT results were due to leukemia, lymphoma, or solid tumors in 10 expectant mothers.
The research was published in JAMA and presented at the 19th International Conference on Prenatal Diagnosis and Therapy in Washington, DC. Funding for the study was provided by Illumina, and company employees were involved in the research.
“We did this study because noninvasive prenatal testing using sequencing of cell-free DNA in the mother’s plasma is the fastest-growing area of prenatal testing and, indeed, of genomic medicine,” said study author Diana W. Bianchi, MD, of Tufts Medical Center in Boston, Massachusetts.
“As the volume of tests has expanded, we’ve become increasingly aware of the so-called “false-positive” cases. [A]pproximately 0.2% of the time, there is a discrepancy between the results of the prenatal test—in which an aneuploidy is reported—and the result from the diagnostic fetal procedure, the amniocentesis or the chorionic villus sampling.”
“So we’re interested in the situation where the fetal chromosomes are normal, but the prenatal test shows that there’s an aneuploidy detected. We’re interested in the possible explanations for that discrepancy.”
To gain some insight, Dr Bianchi and her colleagues evaluated 125,426 samples from asymptomatic pregnant women who underwent plasma cell-free DNA sequencing for clinical prenatal aneuploidy screening using Illumina’s verifi Prenatal Test.
In all, 3757 samples (3%) were positive for 1 or more aneuploidies involving chromosomes 13, 18, 21, X, or Y. These were reported to the ordering physician with recommendations for further evaluation.
“In a small minority of women, [subsequent tests analyzing only fetal DNA] showed that the fetal chromosomes were normal, and that disagreed with [results of the NIPT],” Dr Bianchi said. “We were examining whether cancer could explain the discrepancy between these two test results.”
The researchers found that 10 of the women with discordant test results were subsequently diagnosed with cancer. There were 3 cases of B-cell lymphoma and 1 case each of T-cell leukemia, Hodgkin lymphoma, unspecified adenocarcinoma, leiomyosarcoma, and neuroendocrine, colorectal, and anal carcinomas.
Dr Bianchi and her colleagues were able to obtain detailed clinical and sequencing data for 8 of these cases. In the other 2 cases (leiomyosarcoma and unspecified adenocarcinoma), the women were critically ill and were not approached about participating in the study.
The researchers found that maternal cancers most frequently occurred when the NIPT detected more than 1 aneuploidy. There were 7 known cancers among 39 cases of multiple aneuploidies by NIPT. In 1 case, blood was sampled after the patient completed treatment for colorectal cancer, and the abnormal pattern was no longer evident.
When the researchers examined additional genetic information for the women with cancer, they found unique patterns of nonspecific copy-number gains and losses across multiple chromosomes.
“[These women] had DNA imbalances all across the genome,” Dr Bianchi said. “The [NIPT] normally is only looking at DNA material from the chromosomes of clinical interest—chromosomes 13, 18, 21, X, and Y.”
“When we opened up their results to look at all of the chromosomes, there were multiple abnormalities in other places, such as chromosome 8, chromosome 6, etc. Each woman had a unique pattern that was abnormal in many places. This suggested that it was the tumor DNA that was being shed into her blood and was contributing to the abnormal pattern.”
Dr Bianchi stressed that the tumor DNA did not affect the babies. She said all were born healthy, although labor was induced early in one mother to facilitate her cancer treatment. ![]()

Photo by Nina Matthews
Researchers have again found evidence to suggest that tests used to identify chromosomal fetal disorders can detect occult malignancies in pregnant women.
In a study made public last month, non-invasive prenatal tests (NIPTs) revealed 2 cases of lymphoma and a case of ovarian cancer in expectant mothers.
In the new study, researchers showed that positive NIPT results were due to leukemia, lymphoma, or solid tumors in 10 expectant mothers.
The research was published in JAMA and presented at the 19th International Conference on Prenatal Diagnosis and Therapy in Washington, DC. Funding for the study was provided by Illumina, and company employees were involved in the research.
“We did this study because noninvasive prenatal testing using sequencing of cell-free DNA in the mother’s plasma is the fastest-growing area of prenatal testing and, indeed, of genomic medicine,” said study author Diana W. Bianchi, MD, of Tufts Medical Center in Boston, Massachusetts.
“As the volume of tests has expanded, we’ve become increasingly aware of the so-called “false-positive” cases. [A]pproximately 0.2% of the time, there is a discrepancy between the results of the prenatal test—in which an aneuploidy is reported—and the result from the diagnostic fetal procedure, the amniocentesis or the chorionic villus sampling.”
“So we’re interested in the situation where the fetal chromosomes are normal, but the prenatal test shows that there’s an aneuploidy detected. We’re interested in the possible explanations for that discrepancy.”
To gain some insight, Dr Bianchi and her colleagues evaluated 125,426 samples from asymptomatic pregnant women who underwent plasma cell-free DNA sequencing for clinical prenatal aneuploidy screening using Illumina’s verifi Prenatal Test.
In all, 3757 samples (3%) were positive for 1 or more aneuploidies involving chromosomes 13, 18, 21, X, or Y. These were reported to the ordering physician with recommendations for further evaluation.
“In a small minority of women, [subsequent tests analyzing only fetal DNA] showed that the fetal chromosomes were normal, and that disagreed with [results of the NIPT],” Dr Bianchi said. “We were examining whether cancer could explain the discrepancy between these two test results.”
The researchers found that 10 of the women with discordant test results were subsequently diagnosed with cancer. There were 3 cases of B-cell lymphoma and 1 case each of T-cell leukemia, Hodgkin lymphoma, unspecified adenocarcinoma, leiomyosarcoma, and neuroendocrine, colorectal, and anal carcinomas.
Dr Bianchi and her colleagues were able to obtain detailed clinical and sequencing data for 8 of these cases. In the other 2 cases (leiomyosarcoma and unspecified adenocarcinoma), the women were critically ill and were not approached about participating in the study.
The researchers found that maternal cancers most frequently occurred when the NIPT detected more than 1 aneuploidy. There were 7 known cancers among 39 cases of multiple aneuploidies by NIPT. In 1 case, blood was sampled after the patient completed treatment for colorectal cancer, and the abnormal pattern was no longer evident.
When the researchers examined additional genetic information for the women with cancer, they found unique patterns of nonspecific copy-number gains and losses across multiple chromosomes.
“[These women] had DNA imbalances all across the genome,” Dr Bianchi said. “The [NIPT] normally is only looking at DNA material from the chromosomes of clinical interest—chromosomes 13, 18, 21, X, and Y.”
“When we opened up their results to look at all of the chromosomes, there were multiple abnormalities in other places, such as chromosome 8, chromosome 6, etc. Each woman had a unique pattern that was abnormal in many places. This suggested that it was the tumor DNA that was being shed into her blood and was contributing to the abnormal pattern.”
Dr Bianchi stressed that the tumor DNA did not affect the babies. She said all were born healthy, although labor was induced early in one mother to facilitate her cancer treatment. ![]()

Photo by Nina Matthews
Researchers have again found evidence to suggest that tests used to identify chromosomal fetal disorders can detect occult malignancies in pregnant women.
In a study made public last month, non-invasive prenatal tests (NIPTs) revealed 2 cases of lymphoma and a case of ovarian cancer in expectant mothers.
In the new study, researchers showed that positive NIPT results were due to leukemia, lymphoma, or solid tumors in 10 expectant mothers.
The research was published in JAMA and presented at the 19th International Conference on Prenatal Diagnosis and Therapy in Washington, DC. Funding for the study was provided by Illumina, and company employees were involved in the research.
“We did this study because noninvasive prenatal testing using sequencing of cell-free DNA in the mother’s plasma is the fastest-growing area of prenatal testing and, indeed, of genomic medicine,” said study author Diana W. Bianchi, MD, of Tufts Medical Center in Boston, Massachusetts.
“As the volume of tests has expanded, we’ve become increasingly aware of the so-called “false-positive” cases. [A]pproximately 0.2% of the time, there is a discrepancy between the results of the prenatal test—in which an aneuploidy is reported—and the result from the diagnostic fetal procedure, the amniocentesis or the chorionic villus sampling.”
“So we’re interested in the situation where the fetal chromosomes are normal, but the prenatal test shows that there’s an aneuploidy detected. We’re interested in the possible explanations for that discrepancy.”
To gain some insight, Dr Bianchi and her colleagues evaluated 125,426 samples from asymptomatic pregnant women who underwent plasma cell-free DNA sequencing for clinical prenatal aneuploidy screening using Illumina’s verifi Prenatal Test.
In all, 3757 samples (3%) were positive for 1 or more aneuploidies involving chromosomes 13, 18, 21, X, or Y. These were reported to the ordering physician with recommendations for further evaluation.
“In a small minority of women, [subsequent tests analyzing only fetal DNA] showed that the fetal chromosomes were normal, and that disagreed with [results of the NIPT],” Dr Bianchi said. “We were examining whether cancer could explain the discrepancy between these two test results.”
The researchers found that 10 of the women with discordant test results were subsequently diagnosed with cancer. There were 3 cases of B-cell lymphoma and 1 case each of T-cell leukemia, Hodgkin lymphoma, unspecified adenocarcinoma, leiomyosarcoma, and neuroendocrine, colorectal, and anal carcinomas.
Dr Bianchi and her colleagues were able to obtain detailed clinical and sequencing data for 8 of these cases. In the other 2 cases (leiomyosarcoma and unspecified adenocarcinoma), the women were critically ill and were not approached about participating in the study.
The researchers found that maternal cancers most frequently occurred when the NIPT detected more than 1 aneuploidy. There were 7 known cancers among 39 cases of multiple aneuploidies by NIPT. In 1 case, blood was sampled after the patient completed treatment for colorectal cancer, and the abnormal pattern was no longer evident.
When the researchers examined additional genetic information for the women with cancer, they found unique patterns of nonspecific copy-number gains and losses across multiple chromosomes.
“[These women] had DNA imbalances all across the genome,” Dr Bianchi said. “The [NIPT] normally is only looking at DNA material from the chromosomes of clinical interest—chromosomes 13, 18, 21, X, and Y.”
“When we opened up their results to look at all of the chromosomes, there were multiple abnormalities in other places, such as chromosome 8, chromosome 6, etc. Each woman had a unique pattern that was abnormal in many places. This suggested that it was the tumor DNA that was being shed into her blood and was contributing to the abnormal pattern.”
Dr Bianchi stressed that the tumor DNA did not affect the babies. She said all were born healthy, although labor was induced early in one mother to facilitate her cancer treatment. ![]()
Early progression predicts overall survival in FL

Photo by Rhoda Baer
The goal for many cancer patients is to reach the 5-year mark without progression, but a new study suggests 2 years might be a more appropriate goal for patients with follicular lymphoma (FL).
Previous research indicated that about 20% of FL patients relapse within 2 years of treatment.
Now, researchers have found these patients have a significantly worse 5-year survival rate than patients who make it past the 2-year mark without progressing.
Carla Casulo, MD, of the University of Rochester in New York, and her colleagues recounted these findings in the Journal of Clinical Oncology.
The team analyzed data from 588 patients with stage 2-4 FL who received first-line therapy with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP).
These patients could be separated into 2 groups: those with disease progression within 2 years of diagnosis (19%, n=110) and those who did not progress within the 2-year period (71%, n=420).
Eight percent of patients (n=46) were lost to follow-up, and 2% (n=12) died of causes other than progression within the 2-year period.
At 2 years, the overall survival (OS) rate was 68% in the early progression group and 97% in the group that did not progress. At 5 years, OS rates were 50% and 90%, respectively.
In unadjusted Cox regression analysis, early progression was associated with lower OS (hazard ratio[HR]=7.17). The same was true after the researchers adjusted for FLIPI score (HR=6.44).
The team observed similar results in a validation cohort of 147 FL patients who received first-line R-CHOP. At 2 years, the OS rate was 64% in the early progression group and 98% in the group that did not progress. At 5 years, OS rates were 34% and 94%, respectively.
Again, in an unadjusted analysis, early progression was associated with lower OS (HR=20.0). And this trend was maintained after the researchers adjusted for FLIPI score (HR=19.8).
The researchers also found that, for patients in the early progression group, clinical factors that were predictive of inferior OS were age, ECOG performance score, nodal sites, and disease stage. For the group that did not progress within 2 years, clinical factors that were predictive of OS were age and extranodal sites.
In a Cox regression analysis that encompassed these factors and early progression, only early progression, age, and ECOG performance scores remained significantly predictive of OS.
“[W]e have confirmed that all relapsed patients are not equal and therefore should not be approached the same at diagnosis, nor at the time of relapse, in terms of therapies,” Dr Casulo said.
“It will be critical to predict who is most likely to relapse early. We believe that targeted sequencing or gene-expression profiling will be important to understanding how to improve the outcomes of this group.” ![]()

Photo by Rhoda Baer
The goal for many cancer patients is to reach the 5-year mark without progression, but a new study suggests 2 years might be a more appropriate goal for patients with follicular lymphoma (FL).
Previous research indicated that about 20% of FL patients relapse within 2 years of treatment.
Now, researchers have found these patients have a significantly worse 5-year survival rate than patients who make it past the 2-year mark without progressing.
Carla Casulo, MD, of the University of Rochester in New York, and her colleagues recounted these findings in the Journal of Clinical Oncology.
The team analyzed data from 588 patients with stage 2-4 FL who received first-line therapy with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP).
These patients could be separated into 2 groups: those with disease progression within 2 years of diagnosis (19%, n=110) and those who did not progress within the 2-year period (71%, n=420).
Eight percent of patients (n=46) were lost to follow-up, and 2% (n=12) died of causes other than progression within the 2-year period.
At 2 years, the overall survival (OS) rate was 68% in the early progression group and 97% in the group that did not progress. At 5 years, OS rates were 50% and 90%, respectively.
In unadjusted Cox regression analysis, early progression was associated with lower OS (hazard ratio[HR]=7.17). The same was true after the researchers adjusted for FLIPI score (HR=6.44).
The team observed similar results in a validation cohort of 147 FL patients who received first-line R-CHOP. At 2 years, the OS rate was 64% in the early progression group and 98% in the group that did not progress. At 5 years, OS rates were 34% and 94%, respectively.
Again, in an unadjusted analysis, early progression was associated with lower OS (HR=20.0). And this trend was maintained after the researchers adjusted for FLIPI score (HR=19.8).
The researchers also found that, for patients in the early progression group, clinical factors that were predictive of inferior OS were age, ECOG performance score, nodal sites, and disease stage. For the group that did not progress within 2 years, clinical factors that were predictive of OS were age and extranodal sites.
In a Cox regression analysis that encompassed these factors and early progression, only early progression, age, and ECOG performance scores remained significantly predictive of OS.
“[W]e have confirmed that all relapsed patients are not equal and therefore should not be approached the same at diagnosis, nor at the time of relapse, in terms of therapies,” Dr Casulo said.
“It will be critical to predict who is most likely to relapse early. We believe that targeted sequencing or gene-expression profiling will be important to understanding how to improve the outcomes of this group.” ![]()

Photo by Rhoda Baer
The goal for many cancer patients is to reach the 5-year mark without progression, but a new study suggests 2 years might be a more appropriate goal for patients with follicular lymphoma (FL).
Previous research indicated that about 20% of FL patients relapse within 2 years of treatment.
Now, researchers have found these patients have a significantly worse 5-year survival rate than patients who make it past the 2-year mark without progressing.
Carla Casulo, MD, of the University of Rochester in New York, and her colleagues recounted these findings in the Journal of Clinical Oncology.
The team analyzed data from 588 patients with stage 2-4 FL who received first-line therapy with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP).
These patients could be separated into 2 groups: those with disease progression within 2 years of diagnosis (19%, n=110) and those who did not progress within the 2-year period (71%, n=420).
Eight percent of patients (n=46) were lost to follow-up, and 2% (n=12) died of causes other than progression within the 2-year period.
At 2 years, the overall survival (OS) rate was 68% in the early progression group and 97% in the group that did not progress. At 5 years, OS rates were 50% and 90%, respectively.
In unadjusted Cox regression analysis, early progression was associated with lower OS (hazard ratio[HR]=7.17). The same was true after the researchers adjusted for FLIPI score (HR=6.44).
The team observed similar results in a validation cohort of 147 FL patients who received first-line R-CHOP. At 2 years, the OS rate was 64% in the early progression group and 98% in the group that did not progress. At 5 years, OS rates were 34% and 94%, respectively.
Again, in an unadjusted analysis, early progression was associated with lower OS (HR=20.0). And this trend was maintained after the researchers adjusted for FLIPI score (HR=19.8).
The researchers also found that, for patients in the early progression group, clinical factors that were predictive of inferior OS were age, ECOG performance score, nodal sites, and disease stage. For the group that did not progress within 2 years, clinical factors that were predictive of OS were age and extranodal sites.
In a Cox regression analysis that encompassed these factors and early progression, only early progression, age, and ECOG performance scores remained significantly predictive of OS.
“[W]e have confirmed that all relapsed patients are not equal and therefore should not be approached the same at diagnosis, nor at the time of relapse, in terms of therapies,” Dr Casulo said.
“It will be critical to predict who is most likely to relapse early. We believe that targeted sequencing or gene-expression profiling will be important to understanding how to improve the outcomes of this group.” ![]()
Novel mAb targeting CD70 shows activity in TCL

Photo by Linda Bartlett
LUGANO—The defucosylated monoclonal antibody (mAb) ARGX-110, which is active against CD70-bearing tumor cells and CD70-dependent stimulation of regulatory T cells, has shown activity in relapsed/refractory T-cell lymphoma (TCL), according to investigators.
Of the 8 TCL patients enrolled in a phase 1 trial of ARGX-110, 3 had a biological response to the mAb.
In this dose-escalation trial, the maximum tolerated dose of ARGX-110 was not reached.
Marie Maerevoet, MD, of the Institut Jules Bordet in Brussels, Belgium, presented results from the lymphoma cohort of this trial at the 13th International Congress on Malignant Lymphoma (abstract 040*). The study was sponsored by arGEN-X, the company developing ARGX-110.
Dr Maerevoet pointed out that more than half the tumor cells in 71% of patients with cutaneous T-cell lymphoma (CTCL) and 22% with peripheral T-cell lymphoma (PTCL) are CD70-positive. CD70 signaling occurs via CD27, and CD27 shedding is a biomarker for an active pathway.
Since ARGX-110 has an affinity for CD70, inhibits CD27 signaling, and mediates the lysis of TCL in Sézary syndrome (SS), mycosis fungoides, and anaplastic large cell lymphoma (ALCL) cell lines, researchers decided to investigate the safety and clinical pharmacology of ARGX-110 monotherapy in metastatic, relapsed or refractory, solid tumors and hematologic malignancies.
Patients’ tumors had to express CD70 by immunohistochemistry, defined as more than 10% tumor cells of 2+ or 3+ intensity.
The primary endpoint was to determine the maximum tolerated dose. Secondary endpoints were pharmacology, immunogenicity, and efficacy signals.
Patient demographics
Between February 2013 and April 2015, investigators assigned 63 patients to receive ARGX-110 at doses ranging from 0.1 to 10 mg/kg intravenously once every 3 weeks until disease progression or withdrawal due to toxicity. Patients were pre-medicated with corticoid regimens.
Eighteen patients had lymphoid malignancies—8 with B-cell lymphomas, 8 with TCL, and 2 with Hodgkin lymphoma.
The TCL cohort consisted of 1 patient with SS, 1 with transformed SS, 1 with T-helper CTCL, 2 with angioimmunoblastic T-cell lymphoma (AITL), 2 with PTCL not otherwise specified (NOS), and 1 with ALCL.
Patients were a median age of 62 (range, 55–78), had a median of 4 prior treatment regimens (range, 2–6), and received a median of 2 cycles of ARGX-110 (range, 1–6).
Dr Maerevoet noted that most lymphoma patients received a dose of 5 mg/kg every 3 weeks.
Safety
In the entire lymphoma cohort of 18 patients, 4 patients (22%) experienced a grade 1 or 2 infusion-related reaction. Three patients (18%) developed grade 3 sepsis—1 with Waldenstrom’s macroglobulinemia, 1 with AITL, and 1 with PTCL-NOS.
Two patients (11%) had hematologic toxicity consisting of a grade 3 decrease in hemoglobin and absolute neutrophil count, which was considered not related to treatment with ARGX-110.
“The maximum tolerated dose was not reached,” Dr Maerevoet said. “We didn’t observe auto-immune adverse events or impact on serum IgG or IgM.”
Efficacy outcomes
The main reason for withdrawal was progressive disease, which occurred in 14 lymphoma patients.
Two patients—1 with Waldenstrom’s macroglobulinemia and 1 with AITL—withdrew due to adverse events of sepsis (catheter infection, pneumonia), 1 patient with SS withdrew for social reasons, and 1 patient with follicular T-cell lymphoma (currently classified as PTCL-NOS) remains on study.
Dr Maerevoet described the 3 TCL patients who had a biologic response to ARGX-110. One patient with SS had a hematologic complete remission after 6 cycles at the 0.1 mg/kg dose.
Another patient with transformed SS experienced a depletion of circulating clones after 2 cycles of the 10 mg/kg dose. However, the patient ultimately died of progressive disease.
A third patient had resolution of autoimmune hemolytic anemia. This 61-year-old male with AITL achieved a partial response with normalization of LDH levels and an increase in hemoglobin to 7.9 g/dL without transfusion support after 2 doses of ARGX-110 at 5 mg/kg.
The patient became Coombs-negative and had a 16% reduction in tumor size by CT scan. However, the patient subsequently died of pneumonia.
The investigators also observed clinical activity in the peripheral blood, lymph nodes, and skin of 2 additional patients.
The biological activity of ARGX-110 as demonstrated by these TCL patients, in addition to the safety and tolerability of this mAb, led the team to conclude that further clinical investigation of ARGX-110 in TCL is warranted. ![]()
*Information in the abstract differs from that presented at the meeting.

Photo by Linda Bartlett
LUGANO—The defucosylated monoclonal antibody (mAb) ARGX-110, which is active against CD70-bearing tumor cells and CD70-dependent stimulation of regulatory T cells, has shown activity in relapsed/refractory T-cell lymphoma (TCL), according to investigators.
Of the 8 TCL patients enrolled in a phase 1 trial of ARGX-110, 3 had a biological response to the mAb.
In this dose-escalation trial, the maximum tolerated dose of ARGX-110 was not reached.
Marie Maerevoet, MD, of the Institut Jules Bordet in Brussels, Belgium, presented results from the lymphoma cohort of this trial at the 13th International Congress on Malignant Lymphoma (abstract 040*). The study was sponsored by arGEN-X, the company developing ARGX-110.
Dr Maerevoet pointed out that more than half the tumor cells in 71% of patients with cutaneous T-cell lymphoma (CTCL) and 22% with peripheral T-cell lymphoma (PTCL) are CD70-positive. CD70 signaling occurs via CD27, and CD27 shedding is a biomarker for an active pathway.
Since ARGX-110 has an affinity for CD70, inhibits CD27 signaling, and mediates the lysis of TCL in Sézary syndrome (SS), mycosis fungoides, and anaplastic large cell lymphoma (ALCL) cell lines, researchers decided to investigate the safety and clinical pharmacology of ARGX-110 monotherapy in metastatic, relapsed or refractory, solid tumors and hematologic malignancies.
Patients’ tumors had to express CD70 by immunohistochemistry, defined as more than 10% tumor cells of 2+ or 3+ intensity.
The primary endpoint was to determine the maximum tolerated dose. Secondary endpoints were pharmacology, immunogenicity, and efficacy signals.
Patient demographics
Between February 2013 and April 2015, investigators assigned 63 patients to receive ARGX-110 at doses ranging from 0.1 to 10 mg/kg intravenously once every 3 weeks until disease progression or withdrawal due to toxicity. Patients were pre-medicated with corticoid regimens.
Eighteen patients had lymphoid malignancies—8 with B-cell lymphomas, 8 with TCL, and 2 with Hodgkin lymphoma.
The TCL cohort consisted of 1 patient with SS, 1 with transformed SS, 1 with T-helper CTCL, 2 with angioimmunoblastic T-cell lymphoma (AITL), 2 with PTCL not otherwise specified (NOS), and 1 with ALCL.
Patients were a median age of 62 (range, 55–78), had a median of 4 prior treatment regimens (range, 2–6), and received a median of 2 cycles of ARGX-110 (range, 1–6).
Dr Maerevoet noted that most lymphoma patients received a dose of 5 mg/kg every 3 weeks.
Safety
In the entire lymphoma cohort of 18 patients, 4 patients (22%) experienced a grade 1 or 2 infusion-related reaction. Three patients (18%) developed grade 3 sepsis—1 with Waldenstrom’s macroglobulinemia, 1 with AITL, and 1 with PTCL-NOS.
Two patients (11%) had hematologic toxicity consisting of a grade 3 decrease in hemoglobin and absolute neutrophil count, which was considered not related to treatment with ARGX-110.
“The maximum tolerated dose was not reached,” Dr Maerevoet said. “We didn’t observe auto-immune adverse events or impact on serum IgG or IgM.”
Efficacy outcomes
The main reason for withdrawal was progressive disease, which occurred in 14 lymphoma patients.
Two patients—1 with Waldenstrom’s macroglobulinemia and 1 with AITL—withdrew due to adverse events of sepsis (catheter infection, pneumonia), 1 patient with SS withdrew for social reasons, and 1 patient with follicular T-cell lymphoma (currently classified as PTCL-NOS) remains on study.
Dr Maerevoet described the 3 TCL patients who had a biologic response to ARGX-110. One patient with SS had a hematologic complete remission after 6 cycles at the 0.1 mg/kg dose.
Another patient with transformed SS experienced a depletion of circulating clones after 2 cycles of the 10 mg/kg dose. However, the patient ultimately died of progressive disease.
A third patient had resolution of autoimmune hemolytic anemia. This 61-year-old male with AITL achieved a partial response with normalization of LDH levels and an increase in hemoglobin to 7.9 g/dL without transfusion support after 2 doses of ARGX-110 at 5 mg/kg.
The patient became Coombs-negative and had a 16% reduction in tumor size by CT scan. However, the patient subsequently died of pneumonia.
The investigators also observed clinical activity in the peripheral blood, lymph nodes, and skin of 2 additional patients.
The biological activity of ARGX-110 as demonstrated by these TCL patients, in addition to the safety and tolerability of this mAb, led the team to conclude that further clinical investigation of ARGX-110 in TCL is warranted. ![]()
*Information in the abstract differs from that presented at the meeting.

Photo by Linda Bartlett
LUGANO—The defucosylated monoclonal antibody (mAb) ARGX-110, which is active against CD70-bearing tumor cells and CD70-dependent stimulation of regulatory T cells, has shown activity in relapsed/refractory T-cell lymphoma (TCL), according to investigators.
Of the 8 TCL patients enrolled in a phase 1 trial of ARGX-110, 3 had a biological response to the mAb.
In this dose-escalation trial, the maximum tolerated dose of ARGX-110 was not reached.
Marie Maerevoet, MD, of the Institut Jules Bordet in Brussels, Belgium, presented results from the lymphoma cohort of this trial at the 13th International Congress on Malignant Lymphoma (abstract 040*). The study was sponsored by arGEN-X, the company developing ARGX-110.
Dr Maerevoet pointed out that more than half the tumor cells in 71% of patients with cutaneous T-cell lymphoma (CTCL) and 22% with peripheral T-cell lymphoma (PTCL) are CD70-positive. CD70 signaling occurs via CD27, and CD27 shedding is a biomarker for an active pathway.
Since ARGX-110 has an affinity for CD70, inhibits CD27 signaling, and mediates the lysis of TCL in Sézary syndrome (SS), mycosis fungoides, and anaplastic large cell lymphoma (ALCL) cell lines, researchers decided to investigate the safety and clinical pharmacology of ARGX-110 monotherapy in metastatic, relapsed or refractory, solid tumors and hematologic malignancies.
Patients’ tumors had to express CD70 by immunohistochemistry, defined as more than 10% tumor cells of 2+ or 3+ intensity.
The primary endpoint was to determine the maximum tolerated dose. Secondary endpoints were pharmacology, immunogenicity, and efficacy signals.
Patient demographics
Between February 2013 and April 2015, investigators assigned 63 patients to receive ARGX-110 at doses ranging from 0.1 to 10 mg/kg intravenously once every 3 weeks until disease progression or withdrawal due to toxicity. Patients were pre-medicated with corticoid regimens.
Eighteen patients had lymphoid malignancies—8 with B-cell lymphomas, 8 with TCL, and 2 with Hodgkin lymphoma.
The TCL cohort consisted of 1 patient with SS, 1 with transformed SS, 1 with T-helper CTCL, 2 with angioimmunoblastic T-cell lymphoma (AITL), 2 with PTCL not otherwise specified (NOS), and 1 with ALCL.
Patients were a median age of 62 (range, 55–78), had a median of 4 prior treatment regimens (range, 2–6), and received a median of 2 cycles of ARGX-110 (range, 1–6).
Dr Maerevoet noted that most lymphoma patients received a dose of 5 mg/kg every 3 weeks.
Safety
In the entire lymphoma cohort of 18 patients, 4 patients (22%) experienced a grade 1 or 2 infusion-related reaction. Three patients (18%) developed grade 3 sepsis—1 with Waldenstrom’s macroglobulinemia, 1 with AITL, and 1 with PTCL-NOS.
Two patients (11%) had hematologic toxicity consisting of a grade 3 decrease in hemoglobin and absolute neutrophil count, which was considered not related to treatment with ARGX-110.
“The maximum tolerated dose was not reached,” Dr Maerevoet said. “We didn’t observe auto-immune adverse events or impact on serum IgG or IgM.”
Efficacy outcomes
The main reason for withdrawal was progressive disease, which occurred in 14 lymphoma patients.
Two patients—1 with Waldenstrom’s macroglobulinemia and 1 with AITL—withdrew due to adverse events of sepsis (catheter infection, pneumonia), 1 patient with SS withdrew for social reasons, and 1 patient with follicular T-cell lymphoma (currently classified as PTCL-NOS) remains on study.
Dr Maerevoet described the 3 TCL patients who had a biologic response to ARGX-110. One patient with SS had a hematologic complete remission after 6 cycles at the 0.1 mg/kg dose.
Another patient with transformed SS experienced a depletion of circulating clones after 2 cycles of the 10 mg/kg dose. However, the patient ultimately died of progressive disease.
A third patient had resolution of autoimmune hemolytic anemia. This 61-year-old male with AITL achieved a partial response with normalization of LDH levels and an increase in hemoglobin to 7.9 g/dL without transfusion support after 2 doses of ARGX-110 at 5 mg/kg.
The patient became Coombs-negative and had a 16% reduction in tumor size by CT scan. However, the patient subsequently died of pneumonia.
The investigators also observed clinical activity in the peripheral blood, lymph nodes, and skin of 2 additional patients.
The biological activity of ARGX-110 as demonstrated by these TCL patients, in addition to the safety and tolerability of this mAb, led the team to conclude that further clinical investigation of ARGX-110 in TCL is warranted. ![]()
*Information in the abstract differs from that presented at the meeting.
Second pathology review boosts diagnostic accuracy in lymphoma
In patients with newly diagnosed lymphoma and suspected lymphoma, a second pathological review found inaccuracies in the original diagnosis among 17% of more than 42,000 cases, based on data presented at the International Congress on Malignant Lymphoma in Lugano, Switzerland.
In more than 25% of all discrepancies, tumors were reclassified at the second pathology review as the result of findings from additional immunostaining and molecular studies – polymerase chain reaction and fluorescence in situ hybridization.
In 15% of cases, diagnostic changes were expected to result in a change in patient management.
“Our study highlights the importance of specialized centralized review of lymphoma diagnosis, not only in the setting of clinical trials but also in routine clinical practice, for optimal patient management,” reported Dr. Camille Laurent of the Institut Universitaire du Cancer Oncopole, Toulouse, France.
In 2010, the French National Cancer Agency (INCa) established the Lymphopath Network, comprising 33 reference centers, to provide a review by expert hematopathologists of every newly diagnosed lymphoma or suspected lymphoma prior to treatment. These new diagnoses were entered in a central national database. Between 2010 and 2015, 42,146 samples were reviewed: 35,753 were newly diagnosed as lymphomas, while the remaining 6,393 cases included 4,610 reactive lymphoid conditions and 1,783 nonlymphoid malignancies, including especially myeloma and leukemic disorders.
Discordant diagnoses among extra-cutaneous lymphomas were carefully examined by a hematologist and recorded as major or minor depending on the expected therapeutic impact. Dr. Laurent said.
The discordance rate between the referral diagnosis and the final diagnosis was 17.2%. Small B-cell lymphomas and peripheral T-cell lymphoma subtyping were the most common discrepancies; 6.4% of discordances were due to an unspecified lymphoma diagnosis, Dr. Laurent stated.
Less than 2% of discrepancies were due to misclassifications of benign versus malignant lymphoid conditions and of Hodgkin lymphoma versus non-Hodgkin lymphoma. There were minor discrepancies (2.2%) in follicular lymphoma misgrading and diffuse large B-cell lymphoma subtypes.
Given the complexity of lymphoma classification, it is not surprising that expert hematopathologists can refine diagnoses. As we progress in understanding the specific pathogenesis of lymphoma subtypes and utility of targeted therapy, it becomes even more critical to make correct diagnoses. This study reiterates the importance of expert review for many, if not all, lymphoma samples, particularly any T-cell lymphoma and non—follicular small B-cell lymphoma.
Given the complexity of lymphoma classification, it is not surprising that expert hematopathologists can refine diagnoses. As we progress in understanding the specific pathogenesis of lymphoma subtypes and utility of targeted therapy, it becomes even more critical to make correct diagnoses. This study reiterates the importance of expert review for many, if not all, lymphoma samples, particularly any T-cell lymphoma and non—follicular small B-cell lymphoma.
Given the complexity of lymphoma classification, it is not surprising that expert hematopathologists can refine diagnoses. As we progress in understanding the specific pathogenesis of lymphoma subtypes and utility of targeted therapy, it becomes even more critical to make correct diagnoses. This study reiterates the importance of expert review for many, if not all, lymphoma samples, particularly any T-cell lymphoma and non—follicular small B-cell lymphoma.
In patients with newly diagnosed lymphoma and suspected lymphoma, a second pathological review found inaccuracies in the original diagnosis among 17% of more than 42,000 cases, based on data presented at the International Congress on Malignant Lymphoma in Lugano, Switzerland.
In more than 25% of all discrepancies, tumors were reclassified at the second pathology review as the result of findings from additional immunostaining and molecular studies – polymerase chain reaction and fluorescence in situ hybridization.
In 15% of cases, diagnostic changes were expected to result in a change in patient management.
“Our study highlights the importance of specialized centralized review of lymphoma diagnosis, not only in the setting of clinical trials but also in routine clinical practice, for optimal patient management,” reported Dr. Camille Laurent of the Institut Universitaire du Cancer Oncopole, Toulouse, France.
In 2010, the French National Cancer Agency (INCa) established the Lymphopath Network, comprising 33 reference centers, to provide a review by expert hematopathologists of every newly diagnosed lymphoma or suspected lymphoma prior to treatment. These new diagnoses were entered in a central national database. Between 2010 and 2015, 42,146 samples were reviewed: 35,753 were newly diagnosed as lymphomas, while the remaining 6,393 cases included 4,610 reactive lymphoid conditions and 1,783 nonlymphoid malignancies, including especially myeloma and leukemic disorders.
Discordant diagnoses among extra-cutaneous lymphomas were carefully examined by a hematologist and recorded as major or minor depending on the expected therapeutic impact. Dr. Laurent said.
The discordance rate between the referral diagnosis and the final diagnosis was 17.2%. Small B-cell lymphomas and peripheral T-cell lymphoma subtyping were the most common discrepancies; 6.4% of discordances were due to an unspecified lymphoma diagnosis, Dr. Laurent stated.
Less than 2% of discrepancies were due to misclassifications of benign versus malignant lymphoid conditions and of Hodgkin lymphoma versus non-Hodgkin lymphoma. There were minor discrepancies (2.2%) in follicular lymphoma misgrading and diffuse large B-cell lymphoma subtypes.
In patients with newly diagnosed lymphoma and suspected lymphoma, a second pathological review found inaccuracies in the original diagnosis among 17% of more than 42,000 cases, based on data presented at the International Congress on Malignant Lymphoma in Lugano, Switzerland.
In more than 25% of all discrepancies, tumors were reclassified at the second pathology review as the result of findings from additional immunostaining and molecular studies – polymerase chain reaction and fluorescence in situ hybridization.
In 15% of cases, diagnostic changes were expected to result in a change in patient management.
“Our study highlights the importance of specialized centralized review of lymphoma diagnosis, not only in the setting of clinical trials but also in routine clinical practice, for optimal patient management,” reported Dr. Camille Laurent of the Institut Universitaire du Cancer Oncopole, Toulouse, France.
In 2010, the French National Cancer Agency (INCa) established the Lymphopath Network, comprising 33 reference centers, to provide a review by expert hematopathologists of every newly diagnosed lymphoma or suspected lymphoma prior to treatment. These new diagnoses were entered in a central national database. Between 2010 and 2015, 42,146 samples were reviewed: 35,753 were newly diagnosed as lymphomas, while the remaining 6,393 cases included 4,610 reactive lymphoid conditions and 1,783 nonlymphoid malignancies, including especially myeloma and leukemic disorders.
Discordant diagnoses among extra-cutaneous lymphomas were carefully examined by a hematologist and recorded as major or minor depending on the expected therapeutic impact. Dr. Laurent said.
The discordance rate between the referral diagnosis and the final diagnosis was 17.2%. Small B-cell lymphomas and peripheral T-cell lymphoma subtyping were the most common discrepancies; 6.4% of discordances were due to an unspecified lymphoma diagnosis, Dr. Laurent stated.
Less than 2% of discrepancies were due to misclassifications of benign versus malignant lymphoid conditions and of Hodgkin lymphoma versus non-Hodgkin lymphoma. There were minor discrepancies (2.2%) in follicular lymphoma misgrading and diffuse large B-cell lymphoma subtypes.
FROM 13-ICML
Key clinical point: A second pathological review of newly-diagnosed lymphoma or suspected lymphoma found discrepancies in 17% of cases.
Major finding: Small B-cell lymphomas and peripheral T-cell lymphoma subtyping were the most common discrepancies; 6.4% of discordances were due to an unspecified lymphoma diagnosis.
Data source: 42,146 samples from the French National Cancer Agency’s Lymphopath Network, comprising 33 reference centers.
Disclosures: Dr. Laurent had no relevant financial disclosures.