User login
Lymphocyte, monocyte data can predict treatment response in follicular lymphoma
Absolute lymphocyte cell (ALC) and absolute monocyte cell (AMC) counts, as well as their ratio (LMR) proved to be prognostic factors for treatment results, as shown by a database analysis of follicular lymphoma (FL) patients.
Progressive disease and stable disease after first-line therapy, as well as the mortality rate, were significantly associated with lower ALC, higher AMC, and higher LMR, according to the report published online.
Researchers analyzed the data of 100 FL variant patients admitted and treated between January 2009 and June 2018 at a single center.
Area under the curve analysis for discriminating between survival times showed 0.57 x 109 cells/L was the most discriminative ALC cutoff value, 1.24 x 109/L was the most discriminative AMC cutoff value, and 1.63 x 109/L was the most discriminative LMR cutoff value.
Shorter overall survival (OS) was significantly associated with lower ALC, compared with those having higher ALC. Shorter OS and progression-free survival (PFS) were significantly associated with higher AMC, compared with those having lower AMC. Shorter OS and PFS were also significantly associated with lower LMR, compared with those having higher LMR.
Overall, a high-risk score in the Follicular Lymphoma International Prognostic Index (FLIPI) and having a low LMR were considered risk factors for prediction of OS in all the studied FL patients in univariate analysis and multivariate analysis, according to the researchers.
“Our results prove the effect of lymphocyte and monocyte in the tumor immune response, which gives opportunity to several therapeutic strategies that target myeloid-derived suppressor cells (MDSCs), including monocytes and their progeny and improves the T-cell function in eradication strategies,” the researchers concluded.
No study funding or disclosure details were provided.
SOURCE: Mohsen A et al. Clin Lymphoma Myeloma Leuk. 2020 Mar 20. doi: 10.1016/j.clml.2020.03.007.
Absolute lymphocyte cell (ALC) and absolute monocyte cell (AMC) counts, as well as their ratio (LMR) proved to be prognostic factors for treatment results, as shown by a database analysis of follicular lymphoma (FL) patients.
Progressive disease and stable disease after first-line therapy, as well as the mortality rate, were significantly associated with lower ALC, higher AMC, and higher LMR, according to the report published online.
Researchers analyzed the data of 100 FL variant patients admitted and treated between January 2009 and June 2018 at a single center.
Area under the curve analysis for discriminating between survival times showed 0.57 x 109 cells/L was the most discriminative ALC cutoff value, 1.24 x 109/L was the most discriminative AMC cutoff value, and 1.63 x 109/L was the most discriminative LMR cutoff value.
Shorter overall survival (OS) was significantly associated with lower ALC, compared with those having higher ALC. Shorter OS and progression-free survival (PFS) were significantly associated with higher AMC, compared with those having lower AMC. Shorter OS and PFS were also significantly associated with lower LMR, compared with those having higher LMR.
Overall, a high-risk score in the Follicular Lymphoma International Prognostic Index (FLIPI) and having a low LMR were considered risk factors for prediction of OS in all the studied FL patients in univariate analysis and multivariate analysis, according to the researchers.
“Our results prove the effect of lymphocyte and monocyte in the tumor immune response, which gives opportunity to several therapeutic strategies that target myeloid-derived suppressor cells (MDSCs), including monocytes and their progeny and improves the T-cell function in eradication strategies,” the researchers concluded.
No study funding or disclosure details were provided.
SOURCE: Mohsen A et al. Clin Lymphoma Myeloma Leuk. 2020 Mar 20. doi: 10.1016/j.clml.2020.03.007.
Absolute lymphocyte cell (ALC) and absolute monocyte cell (AMC) counts, as well as their ratio (LMR) proved to be prognostic factors for treatment results, as shown by a database analysis of follicular lymphoma (FL) patients.
Progressive disease and stable disease after first-line therapy, as well as the mortality rate, were significantly associated with lower ALC, higher AMC, and higher LMR, according to the report published online.
Researchers analyzed the data of 100 FL variant patients admitted and treated between January 2009 and June 2018 at a single center.
Area under the curve analysis for discriminating between survival times showed 0.57 x 109 cells/L was the most discriminative ALC cutoff value, 1.24 x 109/L was the most discriminative AMC cutoff value, and 1.63 x 109/L was the most discriminative LMR cutoff value.
Shorter overall survival (OS) was significantly associated with lower ALC, compared with those having higher ALC. Shorter OS and progression-free survival (PFS) were significantly associated with higher AMC, compared with those having lower AMC. Shorter OS and PFS were also significantly associated with lower LMR, compared with those having higher LMR.
Overall, a high-risk score in the Follicular Lymphoma International Prognostic Index (FLIPI) and having a low LMR were considered risk factors for prediction of OS in all the studied FL patients in univariate analysis and multivariate analysis, according to the researchers.
“Our results prove the effect of lymphocyte and monocyte in the tumor immune response, which gives opportunity to several therapeutic strategies that target myeloid-derived suppressor cells (MDSCs), including monocytes and their progeny and improves the T-cell function in eradication strategies,” the researchers concluded.
No study funding or disclosure details were provided.
SOURCE: Mohsen A et al. Clin Lymphoma Myeloma Leuk. 2020 Mar 20. doi: 10.1016/j.clml.2020.03.007.
FROM CLINICAL LYMPHOMA, MYELOMA AND LEUKEMIA
Follicular lymphoma treatment can benefit patients 80 years and older
Follicular lymphoma (FL) treatment was associated with improved survival among patients diagnosed with FL at aged 80 years and older, according to the results of a large, retrospective database cohort study.
Researchers used the linked Surveillance, Epidemiology, and End Results–Medicare dataset to identify patients 80 years of age and older, diagnosed with FL between 2000 and 2013, identifying FL-directed treatments based on published guidelines. They used a propensity-score matched sample to compare treated and untreated patient cohorts who had similar observed characteristics.
They assessed 3,705 older patients with FL and a mean age of 84 years). Over a median follow-up of 2.9 years, 68% of the sample received FL-directed therapy and the most common regimen was rituximab monotherapy, which 21% (768 patients) received.
The median overall survival for the treated group was 4.31 years (95% confidence interval [CI], 4.00-4.61) vs. 2.86 years (95% CI, 2.59-3.16) for the untreated group, according to the report, published in the Journal of Geriatric Oncology.
The 3-year restricted mean survival time for the treated group was 2.36 years (95% CI, 2.30-2.41), vs. 2.05 years (95% CI, 1.98-2.11) for the untreated group. Treatment was associated with a 23% reduction in the hazard of death (HR: 0.77; P < .001).
Multivariable analysis showed that older age and a Charlson Comorbidity Index score of two or higher, and a proxy indicator for poor performance status, were inversely associated with receiving treatment. “These factors are expected to discourage physicians from providing FL-directed therapy,” the researchers suggested.
“We observed that, in a cohort of FL patients aged 80 years or older, FL-directed therapy was associated with an overall survival benefit, which persisted in important subgroups,” the researchers concluded.
Financial support for this study was provided by Bayer. One of the authors is employed by Bayer.
SOURCE: Albarmawi H et al. J Geriatric Oncol. 2020;11:55-61.
Follicular lymphoma (FL) treatment was associated with improved survival among patients diagnosed with FL at aged 80 years and older, according to the results of a large, retrospective database cohort study.
Researchers used the linked Surveillance, Epidemiology, and End Results–Medicare dataset to identify patients 80 years of age and older, diagnosed with FL between 2000 and 2013, identifying FL-directed treatments based on published guidelines. They used a propensity-score matched sample to compare treated and untreated patient cohorts who had similar observed characteristics.
They assessed 3,705 older patients with FL and a mean age of 84 years). Over a median follow-up of 2.9 years, 68% of the sample received FL-directed therapy and the most common regimen was rituximab monotherapy, which 21% (768 patients) received.
The median overall survival for the treated group was 4.31 years (95% confidence interval [CI], 4.00-4.61) vs. 2.86 years (95% CI, 2.59-3.16) for the untreated group, according to the report, published in the Journal of Geriatric Oncology.
The 3-year restricted mean survival time for the treated group was 2.36 years (95% CI, 2.30-2.41), vs. 2.05 years (95% CI, 1.98-2.11) for the untreated group. Treatment was associated with a 23% reduction in the hazard of death (HR: 0.77; P < .001).
Multivariable analysis showed that older age and a Charlson Comorbidity Index score of two or higher, and a proxy indicator for poor performance status, were inversely associated with receiving treatment. “These factors are expected to discourage physicians from providing FL-directed therapy,” the researchers suggested.
“We observed that, in a cohort of FL patients aged 80 years or older, FL-directed therapy was associated with an overall survival benefit, which persisted in important subgroups,” the researchers concluded.
Financial support for this study was provided by Bayer. One of the authors is employed by Bayer.
SOURCE: Albarmawi H et al. J Geriatric Oncol. 2020;11:55-61.
Follicular lymphoma (FL) treatment was associated with improved survival among patients diagnosed with FL at aged 80 years and older, according to the results of a large, retrospective database cohort study.
Researchers used the linked Surveillance, Epidemiology, and End Results–Medicare dataset to identify patients 80 years of age and older, diagnosed with FL between 2000 and 2013, identifying FL-directed treatments based on published guidelines. They used a propensity-score matched sample to compare treated and untreated patient cohorts who had similar observed characteristics.
They assessed 3,705 older patients with FL and a mean age of 84 years). Over a median follow-up of 2.9 years, 68% of the sample received FL-directed therapy and the most common regimen was rituximab monotherapy, which 21% (768 patients) received.
The median overall survival for the treated group was 4.31 years (95% confidence interval [CI], 4.00-4.61) vs. 2.86 years (95% CI, 2.59-3.16) for the untreated group, according to the report, published in the Journal of Geriatric Oncology.
The 3-year restricted mean survival time for the treated group was 2.36 years (95% CI, 2.30-2.41), vs. 2.05 years (95% CI, 1.98-2.11) for the untreated group. Treatment was associated with a 23% reduction in the hazard of death (HR: 0.77; P < .001).
Multivariable analysis showed that older age and a Charlson Comorbidity Index score of two or higher, and a proxy indicator for poor performance status, were inversely associated with receiving treatment. “These factors are expected to discourage physicians from providing FL-directed therapy,” the researchers suggested.
“We observed that, in a cohort of FL patients aged 80 years or older, FL-directed therapy was associated with an overall survival benefit, which persisted in important subgroups,” the researchers concluded.
Financial support for this study was provided by Bayer. One of the authors is employed by Bayer.
SOURCE: Albarmawi H et al. J Geriatric Oncol. 2020;11:55-61.
FROM THE JOURNAL OF GERIATRIC ONCOLOGY
Adding lymphopenia component ‘improves’ FLIPI
Incorporating lymphopenia into the Follicular Lymphoma International Prognostic Index (FLIPI) can improve prognostication, according to researchers.
The team added lymphopenia as a point in a revised FLIPI scoring system, called FLIPI-L, and found the new system could better predict overall survival (OS), progression-free survival, and histologic transformation in patients with follicular lymphoma.
George Yang, MD, of Moffitt Cancer Center in Tampa, Fla., and his colleagues described results with the FLIPI-L in a letter published in Blood Cancer Journal.
“Prior studies have demonstrated that lymphopenia was associated with worsened OS in [follicular lymphoma],” Dr. Yang and his colleagues wrote. “Therefore, we hypothesized that lymphopenia may be integrated with existing FLIPI to better stratify long-term survival outcomes and predict for transformation.”
The researchers tested this theory in 736 follicular lymphoma patients who were followed for a median of 72 months (range, 2-211 months). The 5-year OS in this cohort was 81.3%, the 10-year OS was 67.3%, and 18% of patients experienced transformation to high-grade lymphoma.
The researchers defined absolute lymphopenia as less than 1.0 × 109 lymphocytes per liter. In multivariate analyses, lymphopenia was an independent predictor of OS (hazard ratio, 1.74; P less than .01) and transformation (odds ratio, 2.1; P less than .01).
To incorporate lymphopenia into the FLIPI, the researchers created a model in which 1 point was given for each of the standard FLIPI components (age, Ann Arbor stage, number of nodal areas, lactate dehydrogenase, and hemoglobin level), and one point was given for the presence of lymphopenia. Patients in the low-risk FLIPI-L category had 0-1 points, those in the intermediate-risk category had 2-3 points, and patients in the high-risk FLIPI-L category had 4-6 points.
Using the original FLIPI, the 5-year OS was 91% in the low-risk group (0-1), 82.7% in the intermediate-risk group (2), and 66% in the high-risk group (3-5). The 10-year OS was 80.4%, 66%, and 45.8%, respectively.
Using the FLIPI-L, the 5-year OS was 94.5% in the low-risk group (0-1), 89% in the intermediate-risk group (2-3), and 61% in the high-risk group (4-6). The 10-year OS was 83.9%, 68.5%, and 34.5%, respectively.
In a univariate Cox regression analysis of OS, each point increase in FLIPI-L score was associated with a significant increase in hazard ratio. For example, the hazard ratio was 3.4 for patients with a FLIPI-L score of 1 and 30.9 for those with a FLIPI-L score of 6 (P less than .02 for all FLIPI-L scores). Conversely, increases in hazard ratio were not significant with the original FLIPI (P greater than .05 for all FLIPI scores).
The FLIPI-L was prognostic for OS in different treatment groups. In patients who received rituximab alone, radiation alone, or rituximab plus chemotherapy, the scoring system differentiated low-, intermediate-, and high-risk groups (P less than .04). In patients under observation, the FLIPI-L distinguished low/intermediate-risk and high-risk groups (P less than .01).
For patients who progressed within 24 months, the FLIPI-L was more predictive of progression-free survival (P = .05) than was the original FLIPI (P = .11).
Increasing FLIPI-L was an independent predictor of transformation, both when assessed as a continuous variable (P less than .01) and stepwise for FLIPI-L 3-5 (P = .004-.01). The original FLIPI, on the other hand, was not an independent predictor of transformation.
“Our analysis of a lymphopenia cutoff as an addition to the original FLIPI is simple yet improves risk stratification to differentiate between prognostic groups and, importantly, to predict transformation,” Dr. Yang and his colleagues wrote.
The authors reported having no conflicts of interest.
SOURCE: Yang G et al. Blood Cancer J. 2020 Jan 2;9(12):104. doi: 10.1038/s41408-019-0269-6.
Incorporating lymphopenia into the Follicular Lymphoma International Prognostic Index (FLIPI) can improve prognostication, according to researchers.
The team added lymphopenia as a point in a revised FLIPI scoring system, called FLIPI-L, and found the new system could better predict overall survival (OS), progression-free survival, and histologic transformation in patients with follicular lymphoma.
George Yang, MD, of Moffitt Cancer Center in Tampa, Fla., and his colleagues described results with the FLIPI-L in a letter published in Blood Cancer Journal.
“Prior studies have demonstrated that lymphopenia was associated with worsened OS in [follicular lymphoma],” Dr. Yang and his colleagues wrote. “Therefore, we hypothesized that lymphopenia may be integrated with existing FLIPI to better stratify long-term survival outcomes and predict for transformation.”
The researchers tested this theory in 736 follicular lymphoma patients who were followed for a median of 72 months (range, 2-211 months). The 5-year OS in this cohort was 81.3%, the 10-year OS was 67.3%, and 18% of patients experienced transformation to high-grade lymphoma.
The researchers defined absolute lymphopenia as less than 1.0 × 109 lymphocytes per liter. In multivariate analyses, lymphopenia was an independent predictor of OS (hazard ratio, 1.74; P less than .01) and transformation (odds ratio, 2.1; P less than .01).
To incorporate lymphopenia into the FLIPI, the researchers created a model in which 1 point was given for each of the standard FLIPI components (age, Ann Arbor stage, number of nodal areas, lactate dehydrogenase, and hemoglobin level), and one point was given for the presence of lymphopenia. Patients in the low-risk FLIPI-L category had 0-1 points, those in the intermediate-risk category had 2-3 points, and patients in the high-risk FLIPI-L category had 4-6 points.
Using the original FLIPI, the 5-year OS was 91% in the low-risk group (0-1), 82.7% in the intermediate-risk group (2), and 66% in the high-risk group (3-5). The 10-year OS was 80.4%, 66%, and 45.8%, respectively.
Using the FLIPI-L, the 5-year OS was 94.5% in the low-risk group (0-1), 89% in the intermediate-risk group (2-3), and 61% in the high-risk group (4-6). The 10-year OS was 83.9%, 68.5%, and 34.5%, respectively.
In a univariate Cox regression analysis of OS, each point increase in FLIPI-L score was associated with a significant increase in hazard ratio. For example, the hazard ratio was 3.4 for patients with a FLIPI-L score of 1 and 30.9 for those with a FLIPI-L score of 6 (P less than .02 for all FLIPI-L scores). Conversely, increases in hazard ratio were not significant with the original FLIPI (P greater than .05 for all FLIPI scores).
The FLIPI-L was prognostic for OS in different treatment groups. In patients who received rituximab alone, radiation alone, or rituximab plus chemotherapy, the scoring system differentiated low-, intermediate-, and high-risk groups (P less than .04). In patients under observation, the FLIPI-L distinguished low/intermediate-risk and high-risk groups (P less than .01).
For patients who progressed within 24 months, the FLIPI-L was more predictive of progression-free survival (P = .05) than was the original FLIPI (P = .11).
Increasing FLIPI-L was an independent predictor of transformation, both when assessed as a continuous variable (P less than .01) and stepwise for FLIPI-L 3-5 (P = .004-.01). The original FLIPI, on the other hand, was not an independent predictor of transformation.
“Our analysis of a lymphopenia cutoff as an addition to the original FLIPI is simple yet improves risk stratification to differentiate between prognostic groups and, importantly, to predict transformation,” Dr. Yang and his colleagues wrote.
The authors reported having no conflicts of interest.
SOURCE: Yang G et al. Blood Cancer J. 2020 Jan 2;9(12):104. doi: 10.1038/s41408-019-0269-6.
Incorporating lymphopenia into the Follicular Lymphoma International Prognostic Index (FLIPI) can improve prognostication, according to researchers.
The team added lymphopenia as a point in a revised FLIPI scoring system, called FLIPI-L, and found the new system could better predict overall survival (OS), progression-free survival, and histologic transformation in patients with follicular lymphoma.
George Yang, MD, of Moffitt Cancer Center in Tampa, Fla., and his colleagues described results with the FLIPI-L in a letter published in Blood Cancer Journal.
“Prior studies have demonstrated that lymphopenia was associated with worsened OS in [follicular lymphoma],” Dr. Yang and his colleagues wrote. “Therefore, we hypothesized that lymphopenia may be integrated with existing FLIPI to better stratify long-term survival outcomes and predict for transformation.”
The researchers tested this theory in 736 follicular lymphoma patients who were followed for a median of 72 months (range, 2-211 months). The 5-year OS in this cohort was 81.3%, the 10-year OS was 67.3%, and 18% of patients experienced transformation to high-grade lymphoma.
The researchers defined absolute lymphopenia as less than 1.0 × 109 lymphocytes per liter. In multivariate analyses, lymphopenia was an independent predictor of OS (hazard ratio, 1.74; P less than .01) and transformation (odds ratio, 2.1; P less than .01).
To incorporate lymphopenia into the FLIPI, the researchers created a model in which 1 point was given for each of the standard FLIPI components (age, Ann Arbor stage, number of nodal areas, lactate dehydrogenase, and hemoglobin level), and one point was given for the presence of lymphopenia. Patients in the low-risk FLIPI-L category had 0-1 points, those in the intermediate-risk category had 2-3 points, and patients in the high-risk FLIPI-L category had 4-6 points.
Using the original FLIPI, the 5-year OS was 91% in the low-risk group (0-1), 82.7% in the intermediate-risk group (2), and 66% in the high-risk group (3-5). The 10-year OS was 80.4%, 66%, and 45.8%, respectively.
Using the FLIPI-L, the 5-year OS was 94.5% in the low-risk group (0-1), 89% in the intermediate-risk group (2-3), and 61% in the high-risk group (4-6). The 10-year OS was 83.9%, 68.5%, and 34.5%, respectively.
In a univariate Cox regression analysis of OS, each point increase in FLIPI-L score was associated with a significant increase in hazard ratio. For example, the hazard ratio was 3.4 for patients with a FLIPI-L score of 1 and 30.9 for those with a FLIPI-L score of 6 (P less than .02 for all FLIPI-L scores). Conversely, increases in hazard ratio were not significant with the original FLIPI (P greater than .05 for all FLIPI scores).
The FLIPI-L was prognostic for OS in different treatment groups. In patients who received rituximab alone, radiation alone, or rituximab plus chemotherapy, the scoring system differentiated low-, intermediate-, and high-risk groups (P less than .04). In patients under observation, the FLIPI-L distinguished low/intermediate-risk and high-risk groups (P less than .01).
For patients who progressed within 24 months, the FLIPI-L was more predictive of progression-free survival (P = .05) than was the original FLIPI (P = .11).
Increasing FLIPI-L was an independent predictor of transformation, both when assessed as a continuous variable (P less than .01) and stepwise for FLIPI-L 3-5 (P = .004-.01). The original FLIPI, on the other hand, was not an independent predictor of transformation.
“Our analysis of a lymphopenia cutoff as an addition to the original FLIPI is simple yet improves risk stratification to differentiate between prognostic groups and, importantly, to predict transformation,” Dr. Yang and his colleagues wrote.
The authors reported having no conflicts of interest.
SOURCE: Yang G et al. Blood Cancer J. 2020 Jan 2;9(12):104. doi: 10.1038/s41408-019-0269-6.
FROM BLOOD CANCER JOURNAL
REGN1979 shows good activity in pretreated aggressive B-NHL
ORLANDO – A novel bispecific antibody directed against CD20 and CD3 was associated in a phase 1 trial with a high overall response rate among patients with relapsed or refractory B-cell non-Hodgkin lymphomas in early clinical trials, including patients with diffuse large B-cell lymphoma (DLBCL) that had progressed following chimeric antigen receptor (CAR) T-cell therapy.
Among 22 patients previously treated for relapsed/refractory follicular lymphoma of grade 1-3a, there were 21 responses (95%), including 17 complete responses (CR) and 4 partial responses (PR), with the remaining patient having stable disease at 12 weeks of follow-up, reported Rajat Bannerji, MD, PhD, from the Rutgers Cancer Institute of New Jersey in New Brunswick.
“We had activity that was fairly robust in this heavily pretreated population with follicular lymphoma, large-cell patients who had not received CAR T and large-cell patients who had received CAR T, mantle cell, and marginal zone [lymphoma],” he said at the annual meeting of the American Society of Hematology.
REGN1979 is an anti-CD20 and anti-CD3 bispecific IgG4 antibody. It is designed to cross-link and activate CD3-expressing T cells on contact with CD20-positive B cells to kill CD20-positive tumor cells independent of T-cell receptor recognition.
The antibody is administered via an escalating dose schedule consisting of initial, intermediate, and step-up doses.
In addition to the follicular lymphoma response rates noted before, patients with heavily pretreated DLBCL who received the antibody at a dose of 80 mg or higher had an overall response rate of 57.9% (11 patients) including 42.1% CR (8 patients), and 15.8% PR (3 patients). Two patients had stable disease at the 12-week assessment, three had disease progression, and three were not available for assessment.
Among seven patients with DLBCL treated at 80 mg or above who had not received CAR T therapy, five had a CR, one had stable disease, and one had disease progression. Of 12 patients with prior CAR T exposure, 3 had complete responses, 3 had partial responses, 1 had stable disease, 2 had progressive disease, and 3 were not available for assessment.
Among six patients with mantle cell lymphoma and six with marginal zone lymphoma treated across all disease levels, the ORR in each cohort was 67%, with two of six patients in each cohort having a complete response, and two having a partial response.
The safety analysis of all 110 patients enrolled showed that no patients experience a dose-limiting toxicity during the escalation phase, and no maximum tolerated doses were identified.
The most common treatment-related adverse events (AEs) were pyrexia in 88 patients, cytokine release syndrome in 65, chills in 56, fatigue in 40, and anemia in 39.
The most common grade 3-4 AEs were anemia in 24, and hypophosphatemia, lymphopenia, and neutropenia in 21 patients each.
Neurologic AEs were transient and did not require treatment discontinuation, and there were no grade 4 neurologic AEs or deaths from neurologic side effects.
Six patients discontinued the study drug because of treatment-related AEs that included cytomegalovirus infection, grade 3 hemolysis, fatigue, pneumonia, and toxoplasmosis.
A total of 15 patients died during the study, 10 of which were caused by progressive disease, with other deaths caused by gastric perforation, cardiac arrest, lung infection, pneumonia, and 1 from fungal pneumonia 7 months after treatment discontinuation. In addition, after the data cutoff, one patient with mantle cell lymphoma blastoid variant with bone-marrow involvement and bulky disease who was enrolled in an expansion cohort died from tumor lysis syndrome.
The dose-escalation portion of the trial has been completed and expansion cohorts are being enrolled. In addition, REGN1979 is being investigated in a phase 2 global multiarm trial.
The study is supported by Regeneron Pharmaceuticals. Dr. Bannerji reported research funding, travel support, and consulting fees from Regeneron and others.
SOURCE: Bannerji R et al. ASH 2019, Abstract 762.
ORLANDO – A novel bispecific antibody directed against CD20 and CD3 was associated in a phase 1 trial with a high overall response rate among patients with relapsed or refractory B-cell non-Hodgkin lymphomas in early clinical trials, including patients with diffuse large B-cell lymphoma (DLBCL) that had progressed following chimeric antigen receptor (CAR) T-cell therapy.
Among 22 patients previously treated for relapsed/refractory follicular lymphoma of grade 1-3a, there were 21 responses (95%), including 17 complete responses (CR) and 4 partial responses (PR), with the remaining patient having stable disease at 12 weeks of follow-up, reported Rajat Bannerji, MD, PhD, from the Rutgers Cancer Institute of New Jersey in New Brunswick.
“We had activity that was fairly robust in this heavily pretreated population with follicular lymphoma, large-cell patients who had not received CAR T and large-cell patients who had received CAR T, mantle cell, and marginal zone [lymphoma],” he said at the annual meeting of the American Society of Hematology.
REGN1979 is an anti-CD20 and anti-CD3 bispecific IgG4 antibody. It is designed to cross-link and activate CD3-expressing T cells on contact with CD20-positive B cells to kill CD20-positive tumor cells independent of T-cell receptor recognition.
The antibody is administered via an escalating dose schedule consisting of initial, intermediate, and step-up doses.
In addition to the follicular lymphoma response rates noted before, patients with heavily pretreated DLBCL who received the antibody at a dose of 80 mg or higher had an overall response rate of 57.9% (11 patients) including 42.1% CR (8 patients), and 15.8% PR (3 patients). Two patients had stable disease at the 12-week assessment, three had disease progression, and three were not available for assessment.
Among seven patients with DLBCL treated at 80 mg or above who had not received CAR T therapy, five had a CR, one had stable disease, and one had disease progression. Of 12 patients with prior CAR T exposure, 3 had complete responses, 3 had partial responses, 1 had stable disease, 2 had progressive disease, and 3 were not available for assessment.
Among six patients with mantle cell lymphoma and six with marginal zone lymphoma treated across all disease levels, the ORR in each cohort was 67%, with two of six patients in each cohort having a complete response, and two having a partial response.
The safety analysis of all 110 patients enrolled showed that no patients experience a dose-limiting toxicity during the escalation phase, and no maximum tolerated doses were identified.
The most common treatment-related adverse events (AEs) were pyrexia in 88 patients, cytokine release syndrome in 65, chills in 56, fatigue in 40, and anemia in 39.
The most common grade 3-4 AEs were anemia in 24, and hypophosphatemia, lymphopenia, and neutropenia in 21 patients each.
Neurologic AEs were transient and did not require treatment discontinuation, and there were no grade 4 neurologic AEs or deaths from neurologic side effects.
Six patients discontinued the study drug because of treatment-related AEs that included cytomegalovirus infection, grade 3 hemolysis, fatigue, pneumonia, and toxoplasmosis.
A total of 15 patients died during the study, 10 of which were caused by progressive disease, with other deaths caused by gastric perforation, cardiac arrest, lung infection, pneumonia, and 1 from fungal pneumonia 7 months after treatment discontinuation. In addition, after the data cutoff, one patient with mantle cell lymphoma blastoid variant with bone-marrow involvement and bulky disease who was enrolled in an expansion cohort died from tumor lysis syndrome.
The dose-escalation portion of the trial has been completed and expansion cohorts are being enrolled. In addition, REGN1979 is being investigated in a phase 2 global multiarm trial.
The study is supported by Regeneron Pharmaceuticals. Dr. Bannerji reported research funding, travel support, and consulting fees from Regeneron and others.
SOURCE: Bannerji R et al. ASH 2019, Abstract 762.
ORLANDO – A novel bispecific antibody directed against CD20 and CD3 was associated in a phase 1 trial with a high overall response rate among patients with relapsed or refractory B-cell non-Hodgkin lymphomas in early clinical trials, including patients with diffuse large B-cell lymphoma (DLBCL) that had progressed following chimeric antigen receptor (CAR) T-cell therapy.
Among 22 patients previously treated for relapsed/refractory follicular lymphoma of grade 1-3a, there were 21 responses (95%), including 17 complete responses (CR) and 4 partial responses (PR), with the remaining patient having stable disease at 12 weeks of follow-up, reported Rajat Bannerji, MD, PhD, from the Rutgers Cancer Institute of New Jersey in New Brunswick.
“We had activity that was fairly robust in this heavily pretreated population with follicular lymphoma, large-cell patients who had not received CAR T and large-cell patients who had received CAR T, mantle cell, and marginal zone [lymphoma],” he said at the annual meeting of the American Society of Hematology.
REGN1979 is an anti-CD20 and anti-CD3 bispecific IgG4 antibody. It is designed to cross-link and activate CD3-expressing T cells on contact with CD20-positive B cells to kill CD20-positive tumor cells independent of T-cell receptor recognition.
The antibody is administered via an escalating dose schedule consisting of initial, intermediate, and step-up doses.
In addition to the follicular lymphoma response rates noted before, patients with heavily pretreated DLBCL who received the antibody at a dose of 80 mg or higher had an overall response rate of 57.9% (11 patients) including 42.1% CR (8 patients), and 15.8% PR (3 patients). Two patients had stable disease at the 12-week assessment, three had disease progression, and three were not available for assessment.
Among seven patients with DLBCL treated at 80 mg or above who had not received CAR T therapy, five had a CR, one had stable disease, and one had disease progression. Of 12 patients with prior CAR T exposure, 3 had complete responses, 3 had partial responses, 1 had stable disease, 2 had progressive disease, and 3 were not available for assessment.
Among six patients with mantle cell lymphoma and six with marginal zone lymphoma treated across all disease levels, the ORR in each cohort was 67%, with two of six patients in each cohort having a complete response, and two having a partial response.
The safety analysis of all 110 patients enrolled showed that no patients experience a dose-limiting toxicity during the escalation phase, and no maximum tolerated doses were identified.
The most common treatment-related adverse events (AEs) were pyrexia in 88 patients, cytokine release syndrome in 65, chills in 56, fatigue in 40, and anemia in 39.
The most common grade 3-4 AEs were anemia in 24, and hypophosphatemia, lymphopenia, and neutropenia in 21 patients each.
Neurologic AEs were transient and did not require treatment discontinuation, and there were no grade 4 neurologic AEs or deaths from neurologic side effects.
Six patients discontinued the study drug because of treatment-related AEs that included cytomegalovirus infection, grade 3 hemolysis, fatigue, pneumonia, and toxoplasmosis.
A total of 15 patients died during the study, 10 of which were caused by progressive disease, with other deaths caused by gastric perforation, cardiac arrest, lung infection, pneumonia, and 1 from fungal pneumonia 7 months after treatment discontinuation. In addition, after the data cutoff, one patient with mantle cell lymphoma blastoid variant with bone-marrow involvement and bulky disease who was enrolled in an expansion cohort died from tumor lysis syndrome.
The dose-escalation portion of the trial has been completed and expansion cohorts are being enrolled. In addition, REGN1979 is being investigated in a phase 2 global multiarm trial.
The study is supported by Regeneron Pharmaceuticals. Dr. Bannerji reported research funding, travel support, and consulting fees from Regeneron and others.
SOURCE: Bannerji R et al. ASH 2019, Abstract 762.
REPORTING FROM ASH 2019
Survival data reported from largest CAR T trial in B-cell lymphoma
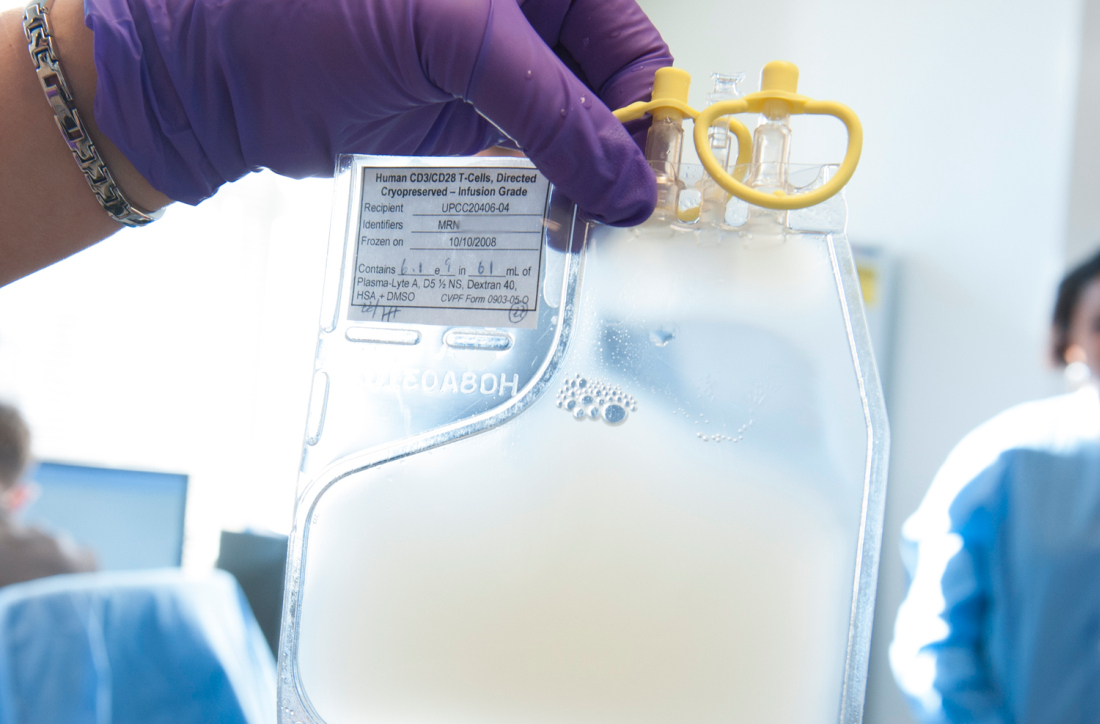
ORLANDO – Updated results from the TRANSCEND NHL trial include survival data with lisocabtagene maraleucel (liso-cel), an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, in patients with relapsed/refractory B-cell lymphomas.
The median progression-free survival (PFS) was 6.8 months, and the median overall survival was 21.1 months. PFS results were best among complete responders and among patients with primary mediastinal large B-cell lymphoma or transformed follicular lymphoma.
Jeremy S. Abramson, MD, of Massachusetts General Hospital in Boston, presented these results at the annual meeting of the American Society of Hematology.
“TRANSCEND NHL is the largest clinical study to date of CD19-directed CAR T cells in patients with relapsed/refractory aggressive B-cell lymphoma,” Dr. Abramson said.
The phase 1 trial (NCT02631044) includes 269 patients who received liso-cel. They were diagnosed with transformed follicular lymphoma (22%) or other indolent lymphoma (7%), high-grade B-cell lymphoma (13%), primary mediastinal large B-cell lymphoma (6%), grade 3B follicular lymphoma (1%), or diffuse large B-cell lymphoma not otherwise specified (51%).
At baseline, patients had received a median of three prior systemic therapies (range, one to eight). Some patients had received autologous (33%) or allogeneic (3%) transplant. Many patients were chemotherapy refractory (67%) or had never achieved a complete response to prior therapy (44%).
More than half of patients (59%) received bridging therapy during liso-cel manufacturing. All patients received lymphodepletion with fludarabine and cyclophosphamide, followed by liso-cel at 50 x 106 CAR T cells, 100 x 106 CAR T cells, or 150 x 106 CAR T cells.
Response and survival
The median follow-up was 12.0 months. The overall response rate was 73%, and the complete response rate was 53%.
“Remissions were rapid, with a median of 1 month from CAR T-cell infusion, and durable, with a median duration of response that has not been reached and 55% of patients remaining in response at 1 year,” Dr. Abramson said.
The median PFS was 6.8 months overall, not reached for patients who achieved a complete response, 2.8 months for patients with a partial response, and 1.1 months for patients with stable disease or progressive disease.
The median PFS was not reached for patients with primary mediastinal large B-cell lymphoma or transformed follicular lymphoma, 5.0 months for high-grade B-cell lymphoma, 3.0 months for diffuse large B-cell lymphoma not otherwise specified, and 2.9 months in transformed indolent non-Hodgkin lymphoma.
The median overall survival was 21.1 months overall, not reached for patients who achieved a complete response, 9.0 months for patients who had a partial response, and 5.1 months for patients with stable disease or progressive disease.
Safety
Common treatment-emergent adverse events were neutropenia (63%), anemia (48%), fatigue (44%), nausea (33%), thrombocytopenia (31%), headache (30%), decreased appetite (28%), and diarrhea (26%).
Cytokine release syndrome (CRS) occurred in 42% of patients, and neurologic events occurred in 30%. Grade 3-4 CRS occurred in 2% of patients, and grade 3-4 neurologic events occurred in 10%. There were no cases of grade 5 CRS or neurologic events.
The median time to CRS onset was 5 days, and the median time to onset of neurologic events was 9 days. The median time to resolution of CRS and neurologic events was 5 days and 11 days, respectively.
“The low incidence of severe CRS and neurologic events and their late time of onset support using this product in a large range of patients and in the outpatient setting,” Dr. Abramson said.
There were seven grade 5 treatment-related adverse events, including diffuse alveolar damage, pulmonary hemorrhage, multiple organ dysfunction syndrome, cardiomyopathy, fludarabine leukoencephalopathy, septic shock, and progressive multifocal leukoencephalopathy.
This trial is sponsored by Bristol-Myers Squibb. Dr. Abramson reported relationships with Juno Therapeutics and Celgene, now owned by Bristol-Myers Squibb, and a range of other companies.
SOURCE: Abramson JS et al. ASH 2019, Abstract 241.
ORLANDO – Updated results from the TRANSCEND NHL trial include survival data with lisocabtagene maraleucel (liso-cel), an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, in patients with relapsed/refractory B-cell lymphomas.
The median progression-free survival (PFS) was 6.8 months, and the median overall survival was 21.1 months. PFS results were best among complete responders and among patients with primary mediastinal large B-cell lymphoma or transformed follicular lymphoma.
Jeremy S. Abramson, MD, of Massachusetts General Hospital in Boston, presented these results at the annual meeting of the American Society of Hematology.
“TRANSCEND NHL is the largest clinical study to date of CD19-directed CAR T cells in patients with relapsed/refractory aggressive B-cell lymphoma,” Dr. Abramson said.
The phase 1 trial (NCT02631044) includes 269 patients who received liso-cel. They were diagnosed with transformed follicular lymphoma (22%) or other indolent lymphoma (7%), high-grade B-cell lymphoma (13%), primary mediastinal large B-cell lymphoma (6%), grade 3B follicular lymphoma (1%), or diffuse large B-cell lymphoma not otherwise specified (51%).
At baseline, patients had received a median of three prior systemic therapies (range, one to eight). Some patients had received autologous (33%) or allogeneic (3%) transplant. Many patients were chemotherapy refractory (67%) or had never achieved a complete response to prior therapy (44%).
More than half of patients (59%) received bridging therapy during liso-cel manufacturing. All patients received lymphodepletion with fludarabine and cyclophosphamide, followed by liso-cel at 50 x 106 CAR T cells, 100 x 106 CAR T cells, or 150 x 106 CAR T cells.
Response and survival
The median follow-up was 12.0 months. The overall response rate was 73%, and the complete response rate was 53%.
“Remissions were rapid, with a median of 1 month from CAR T-cell infusion, and durable, with a median duration of response that has not been reached and 55% of patients remaining in response at 1 year,” Dr. Abramson said.
The median PFS was 6.8 months overall, not reached for patients who achieved a complete response, 2.8 months for patients with a partial response, and 1.1 months for patients with stable disease or progressive disease.
The median PFS was not reached for patients with primary mediastinal large B-cell lymphoma or transformed follicular lymphoma, 5.0 months for high-grade B-cell lymphoma, 3.0 months for diffuse large B-cell lymphoma not otherwise specified, and 2.9 months in transformed indolent non-Hodgkin lymphoma.
The median overall survival was 21.1 months overall, not reached for patients who achieved a complete response, 9.0 months for patients who had a partial response, and 5.1 months for patients with stable disease or progressive disease.
Safety
Common treatment-emergent adverse events were neutropenia (63%), anemia (48%), fatigue (44%), nausea (33%), thrombocytopenia (31%), headache (30%), decreased appetite (28%), and diarrhea (26%).
Cytokine release syndrome (CRS) occurred in 42% of patients, and neurologic events occurred in 30%. Grade 3-4 CRS occurred in 2% of patients, and grade 3-4 neurologic events occurred in 10%. There were no cases of grade 5 CRS or neurologic events.
The median time to CRS onset was 5 days, and the median time to onset of neurologic events was 9 days. The median time to resolution of CRS and neurologic events was 5 days and 11 days, respectively.
“The low incidence of severe CRS and neurologic events and their late time of onset support using this product in a large range of patients and in the outpatient setting,” Dr. Abramson said.
There were seven grade 5 treatment-related adverse events, including diffuse alveolar damage, pulmonary hemorrhage, multiple organ dysfunction syndrome, cardiomyopathy, fludarabine leukoencephalopathy, septic shock, and progressive multifocal leukoencephalopathy.
This trial is sponsored by Bristol-Myers Squibb. Dr. Abramson reported relationships with Juno Therapeutics and Celgene, now owned by Bristol-Myers Squibb, and a range of other companies.
SOURCE: Abramson JS et al. ASH 2019, Abstract 241.
ORLANDO – Updated results from the TRANSCEND NHL trial include survival data with lisocabtagene maraleucel (liso-cel), an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, in patients with relapsed/refractory B-cell lymphomas.
The median progression-free survival (PFS) was 6.8 months, and the median overall survival was 21.1 months. PFS results were best among complete responders and among patients with primary mediastinal large B-cell lymphoma or transformed follicular lymphoma.
Jeremy S. Abramson, MD, of Massachusetts General Hospital in Boston, presented these results at the annual meeting of the American Society of Hematology.
“TRANSCEND NHL is the largest clinical study to date of CD19-directed CAR T cells in patients with relapsed/refractory aggressive B-cell lymphoma,” Dr. Abramson said.
The phase 1 trial (NCT02631044) includes 269 patients who received liso-cel. They were diagnosed with transformed follicular lymphoma (22%) or other indolent lymphoma (7%), high-grade B-cell lymphoma (13%), primary mediastinal large B-cell lymphoma (6%), grade 3B follicular lymphoma (1%), or diffuse large B-cell lymphoma not otherwise specified (51%).
At baseline, patients had received a median of three prior systemic therapies (range, one to eight). Some patients had received autologous (33%) or allogeneic (3%) transplant. Many patients were chemotherapy refractory (67%) or had never achieved a complete response to prior therapy (44%).
More than half of patients (59%) received bridging therapy during liso-cel manufacturing. All patients received lymphodepletion with fludarabine and cyclophosphamide, followed by liso-cel at 50 x 106 CAR T cells, 100 x 106 CAR T cells, or 150 x 106 CAR T cells.
Response and survival
The median follow-up was 12.0 months. The overall response rate was 73%, and the complete response rate was 53%.
“Remissions were rapid, with a median of 1 month from CAR T-cell infusion, and durable, with a median duration of response that has not been reached and 55% of patients remaining in response at 1 year,” Dr. Abramson said.
The median PFS was 6.8 months overall, not reached for patients who achieved a complete response, 2.8 months for patients with a partial response, and 1.1 months for patients with stable disease or progressive disease.
The median PFS was not reached for patients with primary mediastinal large B-cell lymphoma or transformed follicular lymphoma, 5.0 months for high-grade B-cell lymphoma, 3.0 months for diffuse large B-cell lymphoma not otherwise specified, and 2.9 months in transformed indolent non-Hodgkin lymphoma.
The median overall survival was 21.1 months overall, not reached for patients who achieved a complete response, 9.0 months for patients who had a partial response, and 5.1 months for patients with stable disease or progressive disease.
Safety
Common treatment-emergent adverse events were neutropenia (63%), anemia (48%), fatigue (44%), nausea (33%), thrombocytopenia (31%), headache (30%), decreased appetite (28%), and diarrhea (26%).
Cytokine release syndrome (CRS) occurred in 42% of patients, and neurologic events occurred in 30%. Grade 3-4 CRS occurred in 2% of patients, and grade 3-4 neurologic events occurred in 10%. There were no cases of grade 5 CRS or neurologic events.
The median time to CRS onset was 5 days, and the median time to onset of neurologic events was 9 days. The median time to resolution of CRS and neurologic events was 5 days and 11 days, respectively.
“The low incidence of severe CRS and neurologic events and their late time of onset support using this product in a large range of patients and in the outpatient setting,” Dr. Abramson said.
There were seven grade 5 treatment-related adverse events, including diffuse alveolar damage, pulmonary hemorrhage, multiple organ dysfunction syndrome, cardiomyopathy, fludarabine leukoencephalopathy, septic shock, and progressive multifocal leukoencephalopathy.
This trial is sponsored by Bristol-Myers Squibb. Dr. Abramson reported relationships with Juno Therapeutics and Celgene, now owned by Bristol-Myers Squibb, and a range of other companies.
SOURCE: Abramson JS et al. ASH 2019, Abstract 241.
REPORTING FROM ASH 2019
New evidence informs discussions on FL treatment and breast screening
In this edition of “How I Will Treat My Next Patient,” I highlight two recent studies that reinforce prior diagnostic and treatment preferences among many oncologists and will certainly influence the discussions we all will have with our patients in the coming weeks and months.
Rituximab maintenance in follicular lymphoma
The largest trial addressing the role of maintenance CD20-targeted antibody therapy was the Primary Rituximab and Maintenance (PRIMA) phase 3, intergroup study in 1,018 advanced follicular lymphoma patients with an initial response to induction chemoimmunotherapy. The induction regimen could be either of three commonly used regimens plus rituximab. Importantly, none of the induction regimens included bendamustine.
Patients were randomized to 2 years of rituximab maintenance or observation. Prior interim analyses at 3 and 6 years showed improvements for the rituximab maintenance patients in progression-free survival and other secondary endpoints, but no improvement in overall survival. Emmanuel Bachy, MD, PhD, and colleagues published the final survival data after 9 years of follow-up, including a final safety analysis (J Clin Oncol. 2019 Nov 1;37[31]:2815-24).
Among the 607 patients consenting to extended follow-up, median progression-free survival was 10.5 years with rituximab maintenance, compared with 4.1 years for observation (hazard ratio, 0.61; P less than .001). There were more patients with progression-free survival at 3 years, complete response or unconfirmed complete response at 2 years, longer time to next antilymphoma treatment, and later time to next chemotherapy. But the 10-year overall survival was similar in the two groups, as were the quality of life ratings.
In all, 503 patients experienced disease progression. Overall survival after progression was shorter in the rituximab maintenance arm versus the observation arm. Among the approximately 4% of patients experiencing transformation from follicular lymphoma to a more aggressive histology, there was no difference observed in time to transformation. Results were independent of the induction regimen received, response to induction, Follicular Lymphoma International Prognostic Index score, and other clinical factors.
In the safety analysis, there were more grade 3-4 adverse events among the rituximab maintenance patients – primarily cytopenia and infections – more serious adverse events, and more adverse events overall. Fatal adverse events were low in both groups (1.6 vs. 0.6%).
How these results influence practice
Many years ago, a senior mentor of mine taught that “progression-free survival is an important endpoint since the quality of life for patients is generally superior before relapse than afterwards.”
With that mantra playing in my mind and with the reality that discussions about relapse and subsequent treatment are never easy, the results of PRIMA seem straightforward: Rituximab maintenance is beneficial, despite the absence of an overall survival benefit, in a disease with multiple options for subsequent therapy and a long natural history. In this 9-year, final analysis of PRIMA, rituximab maintenance seems to have achieved its goals of deepening responses with low (but not inconsequential) toxicity and delaying substantially those difficult conversations with patients about how to proceed after relapse.
The influence of the final analysis of PRIMA, however, may be more complicated that it would initially seem. Bendamustine-containing regimens were not employed, are commonly used now, and some studies with bendamustine have suggested higher nonrelapse mortality with rituximab maintenance.
Low-grade adverse events take on greater importance for patients on long-term therapy than they do for patients receiving abbreviated treatment, and with noncurative treatment, the higher adverse event profile with 2 years of rituximab maintenance needs to be taken seriously. Induction and maintenance regimens involving rituximab alone, lenalidomide, or obinutuzumab may be preferred for some patients. For all of those reasons, the discussion about rituximab with advanced follicular lymphoma patients remains a long one, demanding detailed descriptions of risks, benefits, limitations of the data, and multiple modern day alternatives to the treatments employed in PRIMA.
Supplemental MRI for dense breast tissue
In the DENSE trial, investigators assigned 40,373 women with extremely dense breast tissue and negative results on screening mammography to be offered either supplemental MRI or mammography screening every other year only. The women were 50-75 years old and were enrolled in the Dutch population-based digital mammography screening program. The primary outcome was the difference in the number of cancers that developed in the 2-year interval between mammograms (N Engl J Med 2019;381:2091-102).
The interval cancer rate was 2.5 per 1,000 screenings among 4,783 women in the “MRI-invitation” group (41% of whom did not actually agree to have an MRI), and 5 per 1,000 in the 32,312 women in the “mammography-only” group, a difference of 2.5 per 1,000 screenings (P less than .001).
Of the 20 interval cancers diagnosed in the MRI-invitation group, 4 were diagnosed in the 59% of women who had undergone MRI (0.8 per 1,000 screenings). The remaining 16 were diagnosed in those who had declined an MRI (4.9 per 1,000 screenings) – virtually identical to the rate of interval cancers in the group that was not invited to have an MRI. This speaks against nonrandom allocation of patients between the mammography-only and the supplemental MRI groups.
Although supplemental MRI was associated with a cancer-detection rate of 16.5 per 1,000 screenings, there was a false positive rate of 8.0% (79.8 per 1,000 screenings). Of the women who underwent a breast biopsy after MRI, 73.7% did not have cancer. Among the women who had MRI-detected cancers, in general, the malignancies diagnosed were smaller, more likely node negative, better differentiated, and more often hormone receptor–positive, compared with those in the mammography-only group.
At the next screening mammogram, the cancer detection rate was lower in the MRI-screened group (2 per 1,000 screenings) than in the MRI–“offered but declined” (7.1 per 1,000 screenings) or mammogram-only groups (6 per 1,000 screenings).
How these results influence practice
American physicians are obligated to inform women with dense breast tissue about the limitations (for them) of conventional mammography, an unquantified, but elevated, risk of breast cancer in women with dense breast tissue, and the fact that there are no universally accepted recommended subsequent steps those women should take.
One side benefit of the requirement to disclose information about breast density, however, is that disclosure can prompt discussions about breast cancer risk reduction – an important discussion with multiple possible health-maintaining interventions.
The DENSE trial is very important news, with potential for even more value in future years. It is finite (2 years of study, with only one MRI scan mandated), narrow (Vopara or BI-RADs breast density grade 4 only), and oligo-institutional (eight participating centers in the Netherlands). Still, it provides randomized, rigorously gathered and analyzed data where there were previously none. Importantly, it answers the question, “So what can I do now, doctor?”
I have some concerns about whether we, as a medical community, have the discipline to restrict application of supplemental MRI screening beyond the population that was studied in the Netherlands. Will we be able to restrain ourselves from ordering MRI scans in women with heterogeneously dense – but not extremely dense – breasts? Will we truly manage patients whose MRI scans had BI-RADs readings of less than 4 in the rigorous, but conservative, fashion employed in the trial? Would we miss fewer significant cancers and subject fewer patients to potential expense and harm with annual mammography, instead of the biennial screening performed in the Netherlands? Does tomo-synthesis improve the interpretation of screening mammograms so much that the interval cancer rate is a lot closer to the rate obtained with supplemental MRI scans? Is the expense of MRI scanning, with the resultant subsequent tests and procedures, justified by the reduction in detecting relatively favorable breast cancers that may not materially impact overall survival?
The DENSE study promises to be a “gift that keeps on giving” as the investigators continue to assess a number of factors including: the value of ongoing supplemental MRI scans (compared with the one-time-only screening reported here); whether there will be a reduction in the advanced cancers and subsequent mortality benefit; the extent of over diagnosis, costs, and impact on quality-of-life; and the applicability of artificial intelligence techniques to reduce false positive MRI results.
While the study may not be practice changing in the United States at the present time, it may be just that as subsequent analyses emerge.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I Will Treat My Next Patient,” I highlight two recent studies that reinforce prior diagnostic and treatment preferences among many oncologists and will certainly influence the discussions we all will have with our patients in the coming weeks and months.
Rituximab maintenance in follicular lymphoma
The largest trial addressing the role of maintenance CD20-targeted antibody therapy was the Primary Rituximab and Maintenance (PRIMA) phase 3, intergroup study in 1,018 advanced follicular lymphoma patients with an initial response to induction chemoimmunotherapy. The induction regimen could be either of three commonly used regimens plus rituximab. Importantly, none of the induction regimens included bendamustine.
Patients were randomized to 2 years of rituximab maintenance or observation. Prior interim analyses at 3 and 6 years showed improvements for the rituximab maintenance patients in progression-free survival and other secondary endpoints, but no improvement in overall survival. Emmanuel Bachy, MD, PhD, and colleagues published the final survival data after 9 years of follow-up, including a final safety analysis (J Clin Oncol. 2019 Nov 1;37[31]:2815-24).
Among the 607 patients consenting to extended follow-up, median progression-free survival was 10.5 years with rituximab maintenance, compared with 4.1 years for observation (hazard ratio, 0.61; P less than .001). There were more patients with progression-free survival at 3 years, complete response or unconfirmed complete response at 2 years, longer time to next antilymphoma treatment, and later time to next chemotherapy. But the 10-year overall survival was similar in the two groups, as were the quality of life ratings.
In all, 503 patients experienced disease progression. Overall survival after progression was shorter in the rituximab maintenance arm versus the observation arm. Among the approximately 4% of patients experiencing transformation from follicular lymphoma to a more aggressive histology, there was no difference observed in time to transformation. Results were independent of the induction regimen received, response to induction, Follicular Lymphoma International Prognostic Index score, and other clinical factors.
In the safety analysis, there were more grade 3-4 adverse events among the rituximab maintenance patients – primarily cytopenia and infections – more serious adverse events, and more adverse events overall. Fatal adverse events were low in both groups (1.6 vs. 0.6%).
How these results influence practice
Many years ago, a senior mentor of mine taught that “progression-free survival is an important endpoint since the quality of life for patients is generally superior before relapse than afterwards.”
With that mantra playing in my mind and with the reality that discussions about relapse and subsequent treatment are never easy, the results of PRIMA seem straightforward: Rituximab maintenance is beneficial, despite the absence of an overall survival benefit, in a disease with multiple options for subsequent therapy and a long natural history. In this 9-year, final analysis of PRIMA, rituximab maintenance seems to have achieved its goals of deepening responses with low (but not inconsequential) toxicity and delaying substantially those difficult conversations with patients about how to proceed after relapse.
The influence of the final analysis of PRIMA, however, may be more complicated that it would initially seem. Bendamustine-containing regimens were not employed, are commonly used now, and some studies with bendamustine have suggested higher nonrelapse mortality with rituximab maintenance.
Low-grade adverse events take on greater importance for patients on long-term therapy than they do for patients receiving abbreviated treatment, and with noncurative treatment, the higher adverse event profile with 2 years of rituximab maintenance needs to be taken seriously. Induction and maintenance regimens involving rituximab alone, lenalidomide, or obinutuzumab may be preferred for some patients. For all of those reasons, the discussion about rituximab with advanced follicular lymphoma patients remains a long one, demanding detailed descriptions of risks, benefits, limitations of the data, and multiple modern day alternatives to the treatments employed in PRIMA.
Supplemental MRI for dense breast tissue
In the DENSE trial, investigators assigned 40,373 women with extremely dense breast tissue and negative results on screening mammography to be offered either supplemental MRI or mammography screening every other year only. The women were 50-75 years old and were enrolled in the Dutch population-based digital mammography screening program. The primary outcome was the difference in the number of cancers that developed in the 2-year interval between mammograms (N Engl J Med 2019;381:2091-102).
The interval cancer rate was 2.5 per 1,000 screenings among 4,783 women in the “MRI-invitation” group (41% of whom did not actually agree to have an MRI), and 5 per 1,000 in the 32,312 women in the “mammography-only” group, a difference of 2.5 per 1,000 screenings (P less than .001).
Of the 20 interval cancers diagnosed in the MRI-invitation group, 4 were diagnosed in the 59% of women who had undergone MRI (0.8 per 1,000 screenings). The remaining 16 were diagnosed in those who had declined an MRI (4.9 per 1,000 screenings) – virtually identical to the rate of interval cancers in the group that was not invited to have an MRI. This speaks against nonrandom allocation of patients between the mammography-only and the supplemental MRI groups.
Although supplemental MRI was associated with a cancer-detection rate of 16.5 per 1,000 screenings, there was a false positive rate of 8.0% (79.8 per 1,000 screenings). Of the women who underwent a breast biopsy after MRI, 73.7% did not have cancer. Among the women who had MRI-detected cancers, in general, the malignancies diagnosed were smaller, more likely node negative, better differentiated, and more often hormone receptor–positive, compared with those in the mammography-only group.
At the next screening mammogram, the cancer detection rate was lower in the MRI-screened group (2 per 1,000 screenings) than in the MRI–“offered but declined” (7.1 per 1,000 screenings) or mammogram-only groups (6 per 1,000 screenings).
How these results influence practice
American physicians are obligated to inform women with dense breast tissue about the limitations (for them) of conventional mammography, an unquantified, but elevated, risk of breast cancer in women with dense breast tissue, and the fact that there are no universally accepted recommended subsequent steps those women should take.
One side benefit of the requirement to disclose information about breast density, however, is that disclosure can prompt discussions about breast cancer risk reduction – an important discussion with multiple possible health-maintaining interventions.
The DENSE trial is very important news, with potential for even more value in future years. It is finite (2 years of study, with only one MRI scan mandated), narrow (Vopara or BI-RADs breast density grade 4 only), and oligo-institutional (eight participating centers in the Netherlands). Still, it provides randomized, rigorously gathered and analyzed data where there were previously none. Importantly, it answers the question, “So what can I do now, doctor?”
I have some concerns about whether we, as a medical community, have the discipline to restrict application of supplemental MRI screening beyond the population that was studied in the Netherlands. Will we be able to restrain ourselves from ordering MRI scans in women with heterogeneously dense – but not extremely dense – breasts? Will we truly manage patients whose MRI scans had BI-RADs readings of less than 4 in the rigorous, but conservative, fashion employed in the trial? Would we miss fewer significant cancers and subject fewer patients to potential expense and harm with annual mammography, instead of the biennial screening performed in the Netherlands? Does tomo-synthesis improve the interpretation of screening mammograms so much that the interval cancer rate is a lot closer to the rate obtained with supplemental MRI scans? Is the expense of MRI scanning, with the resultant subsequent tests and procedures, justified by the reduction in detecting relatively favorable breast cancers that may not materially impact overall survival?
The DENSE study promises to be a “gift that keeps on giving” as the investigators continue to assess a number of factors including: the value of ongoing supplemental MRI scans (compared with the one-time-only screening reported here); whether there will be a reduction in the advanced cancers and subsequent mortality benefit; the extent of over diagnosis, costs, and impact on quality-of-life; and the applicability of artificial intelligence techniques to reduce false positive MRI results.
While the study may not be practice changing in the United States at the present time, it may be just that as subsequent analyses emerge.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I Will Treat My Next Patient,” I highlight two recent studies that reinforce prior diagnostic and treatment preferences among many oncologists and will certainly influence the discussions we all will have with our patients in the coming weeks and months.
Rituximab maintenance in follicular lymphoma
The largest trial addressing the role of maintenance CD20-targeted antibody therapy was the Primary Rituximab and Maintenance (PRIMA) phase 3, intergroup study in 1,018 advanced follicular lymphoma patients with an initial response to induction chemoimmunotherapy. The induction regimen could be either of three commonly used regimens plus rituximab. Importantly, none of the induction regimens included bendamustine.
Patients were randomized to 2 years of rituximab maintenance or observation. Prior interim analyses at 3 and 6 years showed improvements for the rituximab maintenance patients in progression-free survival and other secondary endpoints, but no improvement in overall survival. Emmanuel Bachy, MD, PhD, and colleagues published the final survival data after 9 years of follow-up, including a final safety analysis (J Clin Oncol. 2019 Nov 1;37[31]:2815-24).
Among the 607 patients consenting to extended follow-up, median progression-free survival was 10.5 years with rituximab maintenance, compared with 4.1 years for observation (hazard ratio, 0.61; P less than .001). There were more patients with progression-free survival at 3 years, complete response or unconfirmed complete response at 2 years, longer time to next antilymphoma treatment, and later time to next chemotherapy. But the 10-year overall survival was similar in the two groups, as were the quality of life ratings.
In all, 503 patients experienced disease progression. Overall survival after progression was shorter in the rituximab maintenance arm versus the observation arm. Among the approximately 4% of patients experiencing transformation from follicular lymphoma to a more aggressive histology, there was no difference observed in time to transformation. Results were independent of the induction regimen received, response to induction, Follicular Lymphoma International Prognostic Index score, and other clinical factors.
In the safety analysis, there were more grade 3-4 adverse events among the rituximab maintenance patients – primarily cytopenia and infections – more serious adverse events, and more adverse events overall. Fatal adverse events were low in both groups (1.6 vs. 0.6%).
How these results influence practice
Many years ago, a senior mentor of mine taught that “progression-free survival is an important endpoint since the quality of life for patients is generally superior before relapse than afterwards.”
With that mantra playing in my mind and with the reality that discussions about relapse and subsequent treatment are never easy, the results of PRIMA seem straightforward: Rituximab maintenance is beneficial, despite the absence of an overall survival benefit, in a disease with multiple options for subsequent therapy and a long natural history. In this 9-year, final analysis of PRIMA, rituximab maintenance seems to have achieved its goals of deepening responses with low (but not inconsequential) toxicity and delaying substantially those difficult conversations with patients about how to proceed after relapse.
The influence of the final analysis of PRIMA, however, may be more complicated that it would initially seem. Bendamustine-containing regimens were not employed, are commonly used now, and some studies with bendamustine have suggested higher nonrelapse mortality with rituximab maintenance.
Low-grade adverse events take on greater importance for patients on long-term therapy than they do for patients receiving abbreviated treatment, and with noncurative treatment, the higher adverse event profile with 2 years of rituximab maintenance needs to be taken seriously. Induction and maintenance regimens involving rituximab alone, lenalidomide, or obinutuzumab may be preferred for some patients. For all of those reasons, the discussion about rituximab with advanced follicular lymphoma patients remains a long one, demanding detailed descriptions of risks, benefits, limitations of the data, and multiple modern day alternatives to the treatments employed in PRIMA.
Supplemental MRI for dense breast tissue
In the DENSE trial, investigators assigned 40,373 women with extremely dense breast tissue and negative results on screening mammography to be offered either supplemental MRI or mammography screening every other year only. The women were 50-75 years old and were enrolled in the Dutch population-based digital mammography screening program. The primary outcome was the difference in the number of cancers that developed in the 2-year interval between mammograms (N Engl J Med 2019;381:2091-102).
The interval cancer rate was 2.5 per 1,000 screenings among 4,783 women in the “MRI-invitation” group (41% of whom did not actually agree to have an MRI), and 5 per 1,000 in the 32,312 women in the “mammography-only” group, a difference of 2.5 per 1,000 screenings (P less than .001).
Of the 20 interval cancers diagnosed in the MRI-invitation group, 4 were diagnosed in the 59% of women who had undergone MRI (0.8 per 1,000 screenings). The remaining 16 were diagnosed in those who had declined an MRI (4.9 per 1,000 screenings) – virtually identical to the rate of interval cancers in the group that was not invited to have an MRI. This speaks against nonrandom allocation of patients between the mammography-only and the supplemental MRI groups.
Although supplemental MRI was associated with a cancer-detection rate of 16.5 per 1,000 screenings, there was a false positive rate of 8.0% (79.8 per 1,000 screenings). Of the women who underwent a breast biopsy after MRI, 73.7% did not have cancer. Among the women who had MRI-detected cancers, in general, the malignancies diagnosed were smaller, more likely node negative, better differentiated, and more often hormone receptor–positive, compared with those in the mammography-only group.
At the next screening mammogram, the cancer detection rate was lower in the MRI-screened group (2 per 1,000 screenings) than in the MRI–“offered but declined” (7.1 per 1,000 screenings) or mammogram-only groups (6 per 1,000 screenings).
How these results influence practice
American physicians are obligated to inform women with dense breast tissue about the limitations (for them) of conventional mammography, an unquantified, but elevated, risk of breast cancer in women with dense breast tissue, and the fact that there are no universally accepted recommended subsequent steps those women should take.
One side benefit of the requirement to disclose information about breast density, however, is that disclosure can prompt discussions about breast cancer risk reduction – an important discussion with multiple possible health-maintaining interventions.
The DENSE trial is very important news, with potential for even more value in future years. It is finite (2 years of study, with only one MRI scan mandated), narrow (Vopara or BI-RADs breast density grade 4 only), and oligo-institutional (eight participating centers in the Netherlands). Still, it provides randomized, rigorously gathered and analyzed data where there were previously none. Importantly, it answers the question, “So what can I do now, doctor?”
I have some concerns about whether we, as a medical community, have the discipline to restrict application of supplemental MRI screening beyond the population that was studied in the Netherlands. Will we be able to restrain ourselves from ordering MRI scans in women with heterogeneously dense – but not extremely dense – breasts? Will we truly manage patients whose MRI scans had BI-RADs readings of less than 4 in the rigorous, but conservative, fashion employed in the trial? Would we miss fewer significant cancers and subject fewer patients to potential expense and harm with annual mammography, instead of the biennial screening performed in the Netherlands? Does tomo-synthesis improve the interpretation of screening mammograms so much that the interval cancer rate is a lot closer to the rate obtained with supplemental MRI scans? Is the expense of MRI scanning, with the resultant subsequent tests and procedures, justified by the reduction in detecting relatively favorable breast cancers that may not materially impact overall survival?
The DENSE study promises to be a “gift that keeps on giving” as the investigators continue to assess a number of factors including: the value of ongoing supplemental MRI scans (compared with the one-time-only screening reported here); whether there will be a reduction in the advanced cancers and subsequent mortality benefit; the extent of over diagnosis, costs, and impact on quality-of-life; and the applicability of artificial intelligence techniques to reduce false positive MRI results.
While the study may not be practice changing in the United States at the present time, it may be just that as subsequent analyses emerge.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
Newly identified genetic changes contribute to transformation of follicular lymphoma
A molecular analysis of a patient with follicular lymphoma (FL) that became B-lymphoblastic leukemia/lymphoma (B-ALL/LBL) uncovered genetic changes that may improve understanding of this transformation.
“The study provides new insights into the pathogenesis of FL-B-ALL/LBL transformation and suggests novel, disease biology–based therapeutic approaches to this aggressive and currently incurable disease,” wrote Jonathan Belman, MD, PhD, of the Hospital of the University of Pennsylvania, Philadelphia, and coauthors. Their findings were published in Cold Spring Harbor Molecular Case Studies.
To further understand the rare occasions when FL transforms into a more aggressive form of lymphoma, the researchers investigated a 36-year-old man with low-grade FL that became B-ALL/LBL roughly 1 year after diagnosis. Their analysis included immunoglobulin (Ig) gene rearrangement studies, cytogenetic analysis, and whole exome sequencing of the patient’s FL, B-ALL/LBL, and normal cells.
Next generation sequencing of Ig rearrangements from normal, FL, and B-ALL/LBL specimens revealed considerable somatic hypermutation (SHM) in a single neoplastic clone – IgHV4-34_JH6 – in the FL cells. By comparison, though no dominant clone was found in the B-ALL/LBL specimen, there was even more extensive SHM, along with clones that could be traced to the FL lineage.
In addition, fluorescence in situ hybridization (FISH) studies on the FL specimen were positive for rearrangements of BCL2 and BCL6 genes; a rearrangement of BCL6 is associated with clinical aggressiveness. Those same two rearrangements were found in the B-ALL/LBL specimen, along with a MYC gene rearrangement unseen in the FL.
“MYC translocations are well known to contribute to high aggressiveness of lymphomas, and are hallmark of FL-B-ALL/LBL transformation,” the researchers wrote.
Finally, comparative whole exome sequencing of normal tissue plus the cancerous specimens identified 751 single nucleotide variants. The normal tissue contained 111 of those mutations, while the FL specimens contained 116 mutations – 11 of which were shared solely with B-ALL/LBL – and the B-ALL/LBL specimens contained a striking 575 unique mutations. Notably, a nonsense mutation in the KMT2D gene that was shared by FL and B-ALL/LBL may have contributed to lymphomagenesis.
The study was funded by a grant from the National Institutes of Health, the Abramson Cancer Center Translational Center in Lymphoma, the Daniel B. Allanoff Foundation, and a Hematopathology Divisional Training grant.
SOURCE: Belman JP et al. Cold Spring Harb Mol Case Stud. 2019 Nov 27. doi: 10.1101/mcs.a004614.
A molecular analysis of a patient with follicular lymphoma (FL) that became B-lymphoblastic leukemia/lymphoma (B-ALL/LBL) uncovered genetic changes that may improve understanding of this transformation.
“The study provides new insights into the pathogenesis of FL-B-ALL/LBL transformation and suggests novel, disease biology–based therapeutic approaches to this aggressive and currently incurable disease,” wrote Jonathan Belman, MD, PhD, of the Hospital of the University of Pennsylvania, Philadelphia, and coauthors. Their findings were published in Cold Spring Harbor Molecular Case Studies.
To further understand the rare occasions when FL transforms into a more aggressive form of lymphoma, the researchers investigated a 36-year-old man with low-grade FL that became B-ALL/LBL roughly 1 year after diagnosis. Their analysis included immunoglobulin (Ig) gene rearrangement studies, cytogenetic analysis, and whole exome sequencing of the patient’s FL, B-ALL/LBL, and normal cells.
Next generation sequencing of Ig rearrangements from normal, FL, and B-ALL/LBL specimens revealed considerable somatic hypermutation (SHM) in a single neoplastic clone – IgHV4-34_JH6 – in the FL cells. By comparison, though no dominant clone was found in the B-ALL/LBL specimen, there was even more extensive SHM, along with clones that could be traced to the FL lineage.
In addition, fluorescence in situ hybridization (FISH) studies on the FL specimen were positive for rearrangements of BCL2 and BCL6 genes; a rearrangement of BCL6 is associated with clinical aggressiveness. Those same two rearrangements were found in the B-ALL/LBL specimen, along with a MYC gene rearrangement unseen in the FL.
“MYC translocations are well known to contribute to high aggressiveness of lymphomas, and are hallmark of FL-B-ALL/LBL transformation,” the researchers wrote.
Finally, comparative whole exome sequencing of normal tissue plus the cancerous specimens identified 751 single nucleotide variants. The normal tissue contained 111 of those mutations, while the FL specimens contained 116 mutations – 11 of which were shared solely with B-ALL/LBL – and the B-ALL/LBL specimens contained a striking 575 unique mutations. Notably, a nonsense mutation in the KMT2D gene that was shared by FL and B-ALL/LBL may have contributed to lymphomagenesis.
The study was funded by a grant from the National Institutes of Health, the Abramson Cancer Center Translational Center in Lymphoma, the Daniel B. Allanoff Foundation, and a Hematopathology Divisional Training grant.
SOURCE: Belman JP et al. Cold Spring Harb Mol Case Stud. 2019 Nov 27. doi: 10.1101/mcs.a004614.
A molecular analysis of a patient with follicular lymphoma (FL) that became B-lymphoblastic leukemia/lymphoma (B-ALL/LBL) uncovered genetic changes that may improve understanding of this transformation.
“The study provides new insights into the pathogenesis of FL-B-ALL/LBL transformation and suggests novel, disease biology–based therapeutic approaches to this aggressive and currently incurable disease,” wrote Jonathan Belman, MD, PhD, of the Hospital of the University of Pennsylvania, Philadelphia, and coauthors. Their findings were published in Cold Spring Harbor Molecular Case Studies.
To further understand the rare occasions when FL transforms into a more aggressive form of lymphoma, the researchers investigated a 36-year-old man with low-grade FL that became B-ALL/LBL roughly 1 year after diagnosis. Their analysis included immunoglobulin (Ig) gene rearrangement studies, cytogenetic analysis, and whole exome sequencing of the patient’s FL, B-ALL/LBL, and normal cells.
Next generation sequencing of Ig rearrangements from normal, FL, and B-ALL/LBL specimens revealed considerable somatic hypermutation (SHM) in a single neoplastic clone – IgHV4-34_JH6 – in the FL cells. By comparison, though no dominant clone was found in the B-ALL/LBL specimen, there was even more extensive SHM, along with clones that could be traced to the FL lineage.
In addition, fluorescence in situ hybridization (FISH) studies on the FL specimen were positive for rearrangements of BCL2 and BCL6 genes; a rearrangement of BCL6 is associated with clinical aggressiveness. Those same two rearrangements were found in the B-ALL/LBL specimen, along with a MYC gene rearrangement unseen in the FL.
“MYC translocations are well known to contribute to high aggressiveness of lymphomas, and are hallmark of FL-B-ALL/LBL transformation,” the researchers wrote.
Finally, comparative whole exome sequencing of normal tissue plus the cancerous specimens identified 751 single nucleotide variants. The normal tissue contained 111 of those mutations, while the FL specimens contained 116 mutations – 11 of which were shared solely with B-ALL/LBL – and the B-ALL/LBL specimens contained a striking 575 unique mutations. Notably, a nonsense mutation in the KMT2D gene that was shared by FL and B-ALL/LBL may have contributed to lymphomagenesis.
The study was funded by a grant from the National Institutes of Health, the Abramson Cancer Center Translational Center in Lymphoma, the Daniel B. Allanoff Foundation, and a Hematopathology Divisional Training grant.
SOURCE: Belman JP et al. Cold Spring Harb Mol Case Stud. 2019 Nov 27. doi: 10.1101/mcs.a004614.
FROM COLD SPRING HARBOR MOLECULAR CASE STUDIES
Rituximab maintenance has a durable benefit in follicular lymphoma
The benefit of rituximab maintenance therapy in follicular lymphoma is long lasting and evident out to at least 9 years, according to the final efficacy analysis of the PRIMA phase 3, randomized, controlled trial.
Previously reported results of this pivotal trial showed prolongation of progression-free survival and time to next treatment with rituximab maintenance at a follow-up of 3 years and 6 years.
“Rituximab maintenance is now widely recommended for patients with follicular lymphoma responding to first-line rituximab-based immunochemotherapy,” Emmanuel Bachy, MD, PhD, of Institut National de la Santé et de la Recherche Médicale in Pierre-Bénite, France, and colleagues reported in the Journal of Clinical Oncology.
In PRIMA, patients with previously untreated high–tumor burden follicular lymphoma received any of three immunochemotherapy induction regimens. The 1,018 patients having a response were then randomly assigned to receive 2 years of rituximab (Rituxan) maintenance or observation only.
Dr. Bachy and colleagues performed the trial’s final efficacy analyses, now at a median follow-up of 9 years.
Among the 607 patients consenting to the extended follow-up, median progression-free survival was 10.5 years in the rituximab-maintenance group, compared with 4.1 years in the observation group (hazard ratio, 0.61; P less than .001).
“Subgroup analyses showed the substantial progression-free survival improvement associated with rituximab maintenance was independent of age, sex, induction immunochemotherapy regimen, response to induction, or [Follicular Lymphoma International Prognostic Index] risk score,” the investigators wrote.
Rituximab maintenance also prolonged the median time to next antilymphoma treatment (not reached vs. 6.1 years; hazard ratio, 0.66; P less than .001) and time to next chemotherapy treatment (not reached vs. 9.3 years; hazard ratio, 0.71; P less than .001).
But there was no significant difference in overall survival. Median overall survival was not reached in either group (hazard ratio, 1.04; P = .7948). The estimated 10-year overall survival rate was about 80% in both groups.
“This 9-year follow-up of the PRIMA study demonstrates that rituximab maintenance after induction immunochemotherapy provides a significant long-term [progression-free survival] benefit over observation,” the investigators wrote. “Despite the lack of [overall survival] advantage, it is noteworthy that more than half of the patients in the rituximab maintenance arm remain free of disease progression and have not required new antilymphoma treatment beyond 10 years.”
The trial was sponsored by the Lymphoma Study Association and supported by F. Hoffmann–La Roche and Biogen. Dr. Bachy reported financial disclosures related to Roche and other companies.
SOURCE: Bachy E et al. J Clin Oncol. 2019 Nov 1;37(31):2815-24.
The benefit of rituximab maintenance therapy in follicular lymphoma is long lasting and evident out to at least 9 years, according to the final efficacy analysis of the PRIMA phase 3, randomized, controlled trial.
Previously reported results of this pivotal trial showed prolongation of progression-free survival and time to next treatment with rituximab maintenance at a follow-up of 3 years and 6 years.
“Rituximab maintenance is now widely recommended for patients with follicular lymphoma responding to first-line rituximab-based immunochemotherapy,” Emmanuel Bachy, MD, PhD, of Institut National de la Santé et de la Recherche Médicale in Pierre-Bénite, France, and colleagues reported in the Journal of Clinical Oncology.
In PRIMA, patients with previously untreated high–tumor burden follicular lymphoma received any of three immunochemotherapy induction regimens. The 1,018 patients having a response were then randomly assigned to receive 2 years of rituximab (Rituxan) maintenance or observation only.
Dr. Bachy and colleagues performed the trial’s final efficacy analyses, now at a median follow-up of 9 years.
Among the 607 patients consenting to the extended follow-up, median progression-free survival was 10.5 years in the rituximab-maintenance group, compared with 4.1 years in the observation group (hazard ratio, 0.61; P less than .001).
“Subgroup analyses showed the substantial progression-free survival improvement associated with rituximab maintenance was independent of age, sex, induction immunochemotherapy regimen, response to induction, or [Follicular Lymphoma International Prognostic Index] risk score,” the investigators wrote.
Rituximab maintenance also prolonged the median time to next antilymphoma treatment (not reached vs. 6.1 years; hazard ratio, 0.66; P less than .001) and time to next chemotherapy treatment (not reached vs. 9.3 years; hazard ratio, 0.71; P less than .001).
But there was no significant difference in overall survival. Median overall survival was not reached in either group (hazard ratio, 1.04; P = .7948). The estimated 10-year overall survival rate was about 80% in both groups.
“This 9-year follow-up of the PRIMA study demonstrates that rituximab maintenance after induction immunochemotherapy provides a significant long-term [progression-free survival] benefit over observation,” the investigators wrote. “Despite the lack of [overall survival] advantage, it is noteworthy that more than half of the patients in the rituximab maintenance arm remain free of disease progression and have not required new antilymphoma treatment beyond 10 years.”
The trial was sponsored by the Lymphoma Study Association and supported by F. Hoffmann–La Roche and Biogen. Dr. Bachy reported financial disclosures related to Roche and other companies.
SOURCE: Bachy E et al. J Clin Oncol. 2019 Nov 1;37(31):2815-24.
The benefit of rituximab maintenance therapy in follicular lymphoma is long lasting and evident out to at least 9 years, according to the final efficacy analysis of the PRIMA phase 3, randomized, controlled trial.
Previously reported results of this pivotal trial showed prolongation of progression-free survival and time to next treatment with rituximab maintenance at a follow-up of 3 years and 6 years.
“Rituximab maintenance is now widely recommended for patients with follicular lymphoma responding to first-line rituximab-based immunochemotherapy,” Emmanuel Bachy, MD, PhD, of Institut National de la Santé et de la Recherche Médicale in Pierre-Bénite, France, and colleagues reported in the Journal of Clinical Oncology.
In PRIMA, patients with previously untreated high–tumor burden follicular lymphoma received any of three immunochemotherapy induction regimens. The 1,018 patients having a response were then randomly assigned to receive 2 years of rituximab (Rituxan) maintenance or observation only.
Dr. Bachy and colleagues performed the trial’s final efficacy analyses, now at a median follow-up of 9 years.
Among the 607 patients consenting to the extended follow-up, median progression-free survival was 10.5 years in the rituximab-maintenance group, compared with 4.1 years in the observation group (hazard ratio, 0.61; P less than .001).
“Subgroup analyses showed the substantial progression-free survival improvement associated with rituximab maintenance was independent of age, sex, induction immunochemotherapy regimen, response to induction, or [Follicular Lymphoma International Prognostic Index] risk score,” the investigators wrote.
Rituximab maintenance also prolonged the median time to next antilymphoma treatment (not reached vs. 6.1 years; hazard ratio, 0.66; P less than .001) and time to next chemotherapy treatment (not reached vs. 9.3 years; hazard ratio, 0.71; P less than .001).
But there was no significant difference in overall survival. Median overall survival was not reached in either group (hazard ratio, 1.04; P = .7948). The estimated 10-year overall survival rate was about 80% in both groups.
“This 9-year follow-up of the PRIMA study demonstrates that rituximab maintenance after induction immunochemotherapy provides a significant long-term [progression-free survival] benefit over observation,” the investigators wrote. “Despite the lack of [overall survival] advantage, it is noteworthy that more than half of the patients in the rituximab maintenance arm remain free of disease progression and have not required new antilymphoma treatment beyond 10 years.”
The trial was sponsored by the Lymphoma Study Association and supported by F. Hoffmann–La Roche and Biogen. Dr. Bachy reported financial disclosures related to Roche and other companies.
SOURCE: Bachy E et al. J Clin Oncol. 2019 Nov 1;37(31):2815-24.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Armored CAR T cells elicit responses in NHL patients
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
REPORTING FROM SITC 2019