User login
Ultrasound helps predict gout flares over the next year
Adding ultrasound (US) to the clinical exam helps predict the likelihood of future gout flares, results of a prospective, observational study conducted in Italy suggest.
“Baseline US findings indicative of MSU [monosodium urate] burden and US-detected inflammation are independent predictors of gout flares over 12 months,” lead author Edoardo Cipolletta, MD, of the rheumatology unit, department of clinical and molecular sciences at Marche Polytechnic University in Ancona, Italy, and colleagues wrote in Rheumatology.
“We demonstrated that US findings provided an additional value over clinical data in estimating the risk of flares. Moreover, we reported an association between US findings at a joint and the occurrence of gout flares at the same joint,” they added.
Predicting risk of flares and reducing their occurrence are two main challenges in managing gout, the authors wrote. US can be used to scan multiple joints and is widely used in Europe as a low-cost, radiation-free imaging tool that’s easily integrated into clinical practice.
To investigate whether US can predict gout flares, the researchers enrolled 81 consecutive adult patients with gout in the study between April 2019 and March 2021 at one academic rheumatology treatment site in Italy and followed them for 12 months. The authors compared cases (who developed at least one flare within 12 months of the baseline visit) with controls (who self-reported no gout flares over that period).
Patients diagnosed with other inflammatory arthritis and those with coexisting calcium pyrophosphate deposition disease were excluded from the study.
The 71 participants who completed the study were, on average, in their early 60s, and in both groups, all but one were male. At the baseline visit, all had been on stable urate-lowering therapy for at least 6 months and had not had any gout flares in 4 weeks. The mean gout duration was 7 years in the case group and 8 years in controls.
At baseline, all participants underwent physical examination and US of elbows, wrists, second metacarpophalangeal joints, knees, ankles, and first metatarsophalangeal joints by a member of the research team who was blinded to the clinical and laboratory data.
Clinical assessments were scheduled at baseline and at 6-month intervals, and all participants were evaluated by a second researcher who was blinded to US findings.
During follow-up visits, participants were asked to report any gout flare, considered to meet at least three of four criteria: patient-defined flare, pain at rest score higher than 3 on a 0-10 scale, at least one swollen joint, and at least one warm joint. Patients not reaching their target serum urate goal received escalated urate-lowering therapy dosage and anti-inflammatory prophylaxis.
The US indicators of MSU deposits – aggregates, double contour sign, and tophi – were recorded as present or absent. The power Doppler signal was scored from 0 through 4, and summated scores for each US finding were calculated.
Over 12 months, the researchers found:
- Thirty (42.3%) patients had at least one flare, with a median of 2.0 flares. Patients with flares had higher a US median total MSU score (5.0 vs. 2.0; P = .01) and power Doppler signal (3.0 vs. 0; P < .01) than controls.
- In multivariate analysis, baseline US scores indicating MSU deposits and US-detected inflammation were significantly linked with the occurrence of flares. The adjusted odds ratio for total MSU score was 1.75 (95% confidence interval, 1.26-2.43) and for power Doppler score was 1.63 (95% CI, 1.12-2.40).
- Also in a multivariate analysis, baseline US scores indicating MSU deposits and US-detected inflammation were significantly linked with the number of flares. The incidence risk ratio for total MSU score adjusted was 1.17 (95% CI, 1.08-1.26) and for power Doppler score was 1.29 (95% CI, 1.19-1.40).
Four rheumatologists welcome findings
Gout remains the most common cause of inflammatory arthritis and a significant reason for hospital visits, noted Narender Annapureddy, MD, associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn..
“The study adds to the growing utility of musculoskeletal ultrasound in rheumatology practices to treat various diseases,” he said. “Data that could provide risk prediction for gout flares would be associated with significant benefits in terms of reducing ED visits, hospital admission, and lost work productivity.”
One study limitation, Dr. Annapureddy mentioned, was the single experienced US reader, “which may limit generalizability of results at this time, at least in the United States.”
Yeohan Song, MD, an instructor at Ohio State University Wexner Medical Center, Columbus, integrates US into his practice.
“In gout management, musculoskeletal ultrasound is a useful adjunct to the clinical exam and laboratory markers, particularly [in patients] with recurrent flares despite guideline-directed target serum urate levels,” he said.
Sara K. Tedeschi, MD, MPH, assistant professor of medicine at Harvard Medical School, Boston, pointed out that the US protocol in the study involved imaging knees, ankles, first metatarsophalangeal joints, elbows, wrists, and second metacarpophalangeal joints, and took around 30 minutes to complete.
“That would not be practical in the United States due to time constraints in most rheumatology clinics,” she said.
“The authors report that a ‘reduced scanning protocol’ of the bilateral knees, ankles, and first metatarsophalangeal joints demonstrated similar predictive ability as the full protocol,” she added, “although scanning six joints still might not be feasible during a typical return patient clinic visit in the United States.”
Philip Chu, MD, clinical associate at Duke University, Durham, N.C., uses diagnostic US to help differentiate borderline gout cases from other arthropathies.
“A baseline scan, a follow-up scan before deciding to stop prophylaxis, or a follow-up scan in the setting of recurrent gout flares despite reaching goal serum uric acid, may be cost-effective time points to perform diagnostic US,” he advised.
“Unfortunately,” he added, “reimbursement for diagnostic US has been decreasing over the years, which makes it challenging to increase diagnostic US to the [frequency of its use] in Europe.”
Asked how most gout care being provided by primary care doctors in the United States affects gout management, Dr. Chu said: “Depending on which guidelines one follows for treating gout – from the American College of Rheumatology or the American College of Physicians – one may be more or less likely to start urate-lowering therapy after the first gout flare.”
“Understanding MSU burden in each patient, or even seeing active inflammation at these sites by increased Doppler signal, may change the threshold for physicians to initiate therapy,” he added.
The study received no funding. Three study authors reported financial involvements with pharmaceutical companies. Dr. Cipolletta, Dr. Annapureddy, Dr. Song, Dr. Tedeschi, and Dr. Chu reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Adding ultrasound (US) to the clinical exam helps predict the likelihood of future gout flares, results of a prospective, observational study conducted in Italy suggest.
“Baseline US findings indicative of MSU [monosodium urate] burden and US-detected inflammation are independent predictors of gout flares over 12 months,” lead author Edoardo Cipolletta, MD, of the rheumatology unit, department of clinical and molecular sciences at Marche Polytechnic University in Ancona, Italy, and colleagues wrote in Rheumatology.
“We demonstrated that US findings provided an additional value over clinical data in estimating the risk of flares. Moreover, we reported an association between US findings at a joint and the occurrence of gout flares at the same joint,” they added.
Predicting risk of flares and reducing their occurrence are two main challenges in managing gout, the authors wrote. US can be used to scan multiple joints and is widely used in Europe as a low-cost, radiation-free imaging tool that’s easily integrated into clinical practice.
To investigate whether US can predict gout flares, the researchers enrolled 81 consecutive adult patients with gout in the study between April 2019 and March 2021 at one academic rheumatology treatment site in Italy and followed them for 12 months. The authors compared cases (who developed at least one flare within 12 months of the baseline visit) with controls (who self-reported no gout flares over that period).
Patients diagnosed with other inflammatory arthritis and those with coexisting calcium pyrophosphate deposition disease were excluded from the study.
The 71 participants who completed the study were, on average, in their early 60s, and in both groups, all but one were male. At the baseline visit, all had been on stable urate-lowering therapy for at least 6 months and had not had any gout flares in 4 weeks. The mean gout duration was 7 years in the case group and 8 years in controls.
At baseline, all participants underwent physical examination and US of elbows, wrists, second metacarpophalangeal joints, knees, ankles, and first metatarsophalangeal joints by a member of the research team who was blinded to the clinical and laboratory data.
Clinical assessments were scheduled at baseline and at 6-month intervals, and all participants were evaluated by a second researcher who was blinded to US findings.
During follow-up visits, participants were asked to report any gout flare, considered to meet at least three of four criteria: patient-defined flare, pain at rest score higher than 3 on a 0-10 scale, at least one swollen joint, and at least one warm joint. Patients not reaching their target serum urate goal received escalated urate-lowering therapy dosage and anti-inflammatory prophylaxis.
The US indicators of MSU deposits – aggregates, double contour sign, and tophi – were recorded as present or absent. The power Doppler signal was scored from 0 through 4, and summated scores for each US finding were calculated.
Over 12 months, the researchers found:
- Thirty (42.3%) patients had at least one flare, with a median of 2.0 flares. Patients with flares had higher a US median total MSU score (5.0 vs. 2.0; P = .01) and power Doppler signal (3.0 vs. 0; P < .01) than controls.
- In multivariate analysis, baseline US scores indicating MSU deposits and US-detected inflammation were significantly linked with the occurrence of flares. The adjusted odds ratio for total MSU score was 1.75 (95% confidence interval, 1.26-2.43) and for power Doppler score was 1.63 (95% CI, 1.12-2.40).
- Also in a multivariate analysis, baseline US scores indicating MSU deposits and US-detected inflammation were significantly linked with the number of flares. The incidence risk ratio for total MSU score adjusted was 1.17 (95% CI, 1.08-1.26) and for power Doppler score was 1.29 (95% CI, 1.19-1.40).
Four rheumatologists welcome findings
Gout remains the most common cause of inflammatory arthritis and a significant reason for hospital visits, noted Narender Annapureddy, MD, associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn..
“The study adds to the growing utility of musculoskeletal ultrasound in rheumatology practices to treat various diseases,” he said. “Data that could provide risk prediction for gout flares would be associated with significant benefits in terms of reducing ED visits, hospital admission, and lost work productivity.”
One study limitation, Dr. Annapureddy mentioned, was the single experienced US reader, “which may limit generalizability of results at this time, at least in the United States.”
Yeohan Song, MD, an instructor at Ohio State University Wexner Medical Center, Columbus, integrates US into his practice.
“In gout management, musculoskeletal ultrasound is a useful adjunct to the clinical exam and laboratory markers, particularly [in patients] with recurrent flares despite guideline-directed target serum urate levels,” he said.
Sara K. Tedeschi, MD, MPH, assistant professor of medicine at Harvard Medical School, Boston, pointed out that the US protocol in the study involved imaging knees, ankles, first metatarsophalangeal joints, elbows, wrists, and second metacarpophalangeal joints, and took around 30 minutes to complete.
“That would not be practical in the United States due to time constraints in most rheumatology clinics,” she said.
“The authors report that a ‘reduced scanning protocol’ of the bilateral knees, ankles, and first metatarsophalangeal joints demonstrated similar predictive ability as the full protocol,” she added, “although scanning six joints still might not be feasible during a typical return patient clinic visit in the United States.”
Philip Chu, MD, clinical associate at Duke University, Durham, N.C., uses diagnostic US to help differentiate borderline gout cases from other arthropathies.
“A baseline scan, a follow-up scan before deciding to stop prophylaxis, or a follow-up scan in the setting of recurrent gout flares despite reaching goal serum uric acid, may be cost-effective time points to perform diagnostic US,” he advised.
“Unfortunately,” he added, “reimbursement for diagnostic US has been decreasing over the years, which makes it challenging to increase diagnostic US to the [frequency of its use] in Europe.”
Asked how most gout care being provided by primary care doctors in the United States affects gout management, Dr. Chu said: “Depending on which guidelines one follows for treating gout – from the American College of Rheumatology or the American College of Physicians – one may be more or less likely to start urate-lowering therapy after the first gout flare.”
“Understanding MSU burden in each patient, or even seeing active inflammation at these sites by increased Doppler signal, may change the threshold for physicians to initiate therapy,” he added.
The study received no funding. Three study authors reported financial involvements with pharmaceutical companies. Dr. Cipolletta, Dr. Annapureddy, Dr. Song, Dr. Tedeschi, and Dr. Chu reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Adding ultrasound (US) to the clinical exam helps predict the likelihood of future gout flares, results of a prospective, observational study conducted in Italy suggest.
“Baseline US findings indicative of MSU [monosodium urate] burden and US-detected inflammation are independent predictors of gout flares over 12 months,” lead author Edoardo Cipolletta, MD, of the rheumatology unit, department of clinical and molecular sciences at Marche Polytechnic University in Ancona, Italy, and colleagues wrote in Rheumatology.
“We demonstrated that US findings provided an additional value over clinical data in estimating the risk of flares. Moreover, we reported an association between US findings at a joint and the occurrence of gout flares at the same joint,” they added.
Predicting risk of flares and reducing their occurrence are two main challenges in managing gout, the authors wrote. US can be used to scan multiple joints and is widely used in Europe as a low-cost, radiation-free imaging tool that’s easily integrated into clinical practice.
To investigate whether US can predict gout flares, the researchers enrolled 81 consecutive adult patients with gout in the study between April 2019 and March 2021 at one academic rheumatology treatment site in Italy and followed them for 12 months. The authors compared cases (who developed at least one flare within 12 months of the baseline visit) with controls (who self-reported no gout flares over that period).
Patients diagnosed with other inflammatory arthritis and those with coexisting calcium pyrophosphate deposition disease were excluded from the study.
The 71 participants who completed the study were, on average, in their early 60s, and in both groups, all but one were male. At the baseline visit, all had been on stable urate-lowering therapy for at least 6 months and had not had any gout flares in 4 weeks. The mean gout duration was 7 years in the case group and 8 years in controls.
At baseline, all participants underwent physical examination and US of elbows, wrists, second metacarpophalangeal joints, knees, ankles, and first metatarsophalangeal joints by a member of the research team who was blinded to the clinical and laboratory data.
Clinical assessments were scheduled at baseline and at 6-month intervals, and all participants were evaluated by a second researcher who was blinded to US findings.
During follow-up visits, participants were asked to report any gout flare, considered to meet at least three of four criteria: patient-defined flare, pain at rest score higher than 3 on a 0-10 scale, at least one swollen joint, and at least one warm joint. Patients not reaching their target serum urate goal received escalated urate-lowering therapy dosage and anti-inflammatory prophylaxis.
The US indicators of MSU deposits – aggregates, double contour sign, and tophi – were recorded as present or absent. The power Doppler signal was scored from 0 through 4, and summated scores for each US finding were calculated.
Over 12 months, the researchers found:
- Thirty (42.3%) patients had at least one flare, with a median of 2.0 flares. Patients with flares had higher a US median total MSU score (5.0 vs. 2.0; P = .01) and power Doppler signal (3.0 vs. 0; P < .01) than controls.
- In multivariate analysis, baseline US scores indicating MSU deposits and US-detected inflammation were significantly linked with the occurrence of flares. The adjusted odds ratio for total MSU score was 1.75 (95% confidence interval, 1.26-2.43) and for power Doppler score was 1.63 (95% CI, 1.12-2.40).
- Also in a multivariate analysis, baseline US scores indicating MSU deposits and US-detected inflammation were significantly linked with the number of flares. The incidence risk ratio for total MSU score adjusted was 1.17 (95% CI, 1.08-1.26) and for power Doppler score was 1.29 (95% CI, 1.19-1.40).
Four rheumatologists welcome findings
Gout remains the most common cause of inflammatory arthritis and a significant reason for hospital visits, noted Narender Annapureddy, MD, associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn..
“The study adds to the growing utility of musculoskeletal ultrasound in rheumatology practices to treat various diseases,” he said. “Data that could provide risk prediction for gout flares would be associated with significant benefits in terms of reducing ED visits, hospital admission, and lost work productivity.”
One study limitation, Dr. Annapureddy mentioned, was the single experienced US reader, “which may limit generalizability of results at this time, at least in the United States.”
Yeohan Song, MD, an instructor at Ohio State University Wexner Medical Center, Columbus, integrates US into his practice.
“In gout management, musculoskeletal ultrasound is a useful adjunct to the clinical exam and laboratory markers, particularly [in patients] with recurrent flares despite guideline-directed target serum urate levels,” he said.
Sara K. Tedeschi, MD, MPH, assistant professor of medicine at Harvard Medical School, Boston, pointed out that the US protocol in the study involved imaging knees, ankles, first metatarsophalangeal joints, elbows, wrists, and second metacarpophalangeal joints, and took around 30 minutes to complete.
“That would not be practical in the United States due to time constraints in most rheumatology clinics,” she said.
“The authors report that a ‘reduced scanning protocol’ of the bilateral knees, ankles, and first metatarsophalangeal joints demonstrated similar predictive ability as the full protocol,” she added, “although scanning six joints still might not be feasible during a typical return patient clinic visit in the United States.”
Philip Chu, MD, clinical associate at Duke University, Durham, N.C., uses diagnostic US to help differentiate borderline gout cases from other arthropathies.
“A baseline scan, a follow-up scan before deciding to stop prophylaxis, or a follow-up scan in the setting of recurrent gout flares despite reaching goal serum uric acid, may be cost-effective time points to perform diagnostic US,” he advised.
“Unfortunately,” he added, “reimbursement for diagnostic US has been decreasing over the years, which makes it challenging to increase diagnostic US to the [frequency of its use] in Europe.”
Asked how most gout care being provided by primary care doctors in the United States affects gout management, Dr. Chu said: “Depending on which guidelines one follows for treating gout – from the American College of Rheumatology or the American College of Physicians – one may be more or less likely to start urate-lowering therapy after the first gout flare.”
“Understanding MSU burden in each patient, or even seeing active inflammation at these sites by increased Doppler signal, may change the threshold for physicians to initiate therapy,” he added.
The study received no funding. Three study authors reported financial involvements with pharmaceutical companies. Dr. Cipolletta, Dr. Annapureddy, Dr. Song, Dr. Tedeschi, and Dr. Chu reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM RHEUMATOLOGY
Black Americans’ high gout rate stems from social causes
Gout prevalence is more common in Black Americans than White Americans, and the disparity in prevalence is attributable to social determinants of health, according to a recently published article in JAMA Network Open.
“There has been evidence from recent cohort studies in the U.S. that was suggesting that the prevalence and incidence [of gout] was growing among non-White populations,” said Natalie McCormick, PhD, the study’s lead author and postdoctoral research fellow in medicine in the division of rheumatology, allergy, and immunology at Massachusetts General Hospital and Harvard Medical School, both in Boston. “We wanted to do this at the general population level to see how generalizable [that evidence] is.”
Alvin Wells, MD, PhD, director of the department of rheumatology at Advocate Aurora Medical Group, Franklin, Wisc., noted the findings highlight inequities in care for patients with gout that could be improved with greater emphasis on educating patients about their condition.
“I think that what this shows is that in the U.S. ... there still are some disparities in treating gout,” said Dr. Wells, who was not involved with the study. “And that we have ways to mitigate that, with not only aggressive therapy, but also with other tools like counseling patients. At the end of the day, people all want to be educated about the disease.”
Greater prevalence disappears with adjustment for socioclinical factors
The cross-sectional analysis involved data from U.S. adult participants in the National Health and Nutrition Examination Survey (NHANES) from 2007 to 2016 who self-reported Black or White race.
Investigators considered factors such as excess body mass index (BMI), chronic kidney disease (defined as estimated glomerular filtration rate less than 60 mL/min per 1.73 m2), poverty, poor-quality diet, lower educational level, alcohol consumption, and diuretic use in their analysis.
Dr. McCormick and coinvestigators included a total of 18,693 participants, consisting of 3,304 Black women, 6,195 White women, 3,085 Black men, and 6,109 White men.
They determined that the age-standardized prevalence of gout was 3.5% (95% confidence interval, 2.7%-4.3%) in Black women and 2.0% (95% CI, 1.5% - 2.5%) in White women (age-adjusted odds ratio, 1.81; 95% CI, 1.29-2.53). They calculated that the prevalence was 7.0% (95% CI, 6.2%-7.9%) in Black men and 5.4% (95% CI, 4.7%-6.2%) in White men (age-adjusted OR, 1.26; 95% CI, 1.02-1.55). They found similar differences in the prevalence of hyperuricemia between Black and White Americans.
The increased prevalence of gout in Black Americans, compared with White Americans, does not arise from genetics, according to McCormick. “Our conclusion was that it was due to social determinants of health,” she said. “When we adjusted for all socioclinical risk factors, the racial differences in gout and hyperuricemia prevalence disappeared. Importantly, stepwise regression analysis showed the two biggest drivers of the racial difference in gout prevalence among women were poverty itself, and excess BMI, which can be influenced by poverty.”
Dr. McCormick pointed out that in contrast to the current data, there was no racial difference in the prevalence of gout approximately 2 decades earlier, looking at data from the 1988-1994 NHANES III.
Given the findings, which included the fact that significantly more Black women and men were currently taking diuretics, compared with their White counterparts, Dr. McCormick pointed out clinicians should give more thought to medical therapies prescribed for conditions like high blood pressure to patients with gout or at risk for gout.
“One thing we found was that diuretic use was a driver” of gout, Dr. McCormick said. A prescriber “may want to consider different therapies that present a lower risk of gout if someone has hypertension. There could be greater consideration for prescribing alternatives to diuretics.”
More patient education and rheumatology referrals needed
An impediment to providing that education to patients with gout is unconscious bias on the part of the primary care provider, Dr. Wells said.
“It is about what your perspectives are and what you bring to the table,” he explained. “If you saw [a patient] who looked like someone in your family, that person will be treated differently [than someone who does not look like a family member]. That is where the whole concept [of unconscious bias] comes in.”
Primary care providers need to adopt a holistic approach to gout management that involves counseling about good nutrition, smoking cessation, regular exercise, and limiting alcohol consumption, in addition to medication adherence. Primary care providers may have a bias in treating their Black patients, failing to devote sufficient time and attention to assist them in getting their disease under control, he said.
“Gout should be just like any other chronic disease,” Dr. Wells said. “You need to have a target in mind, and you and your patient need to work together to get to that target. When [patients] end up in rheumatology offices, it is almost too late. I think the take-home message here is that in 2022 ... for any patient who has gout, that patient probably needs to be seen by a rheumatologist because, indeed, with aggressive therapy, preventive therapy, [and] education, and if they are on the right medications, they won’t end up with these crippling joints that we see all the time.”
Dr. McCormick and Dr. Wells disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Gout prevalence is more common in Black Americans than White Americans, and the disparity in prevalence is attributable to social determinants of health, according to a recently published article in JAMA Network Open.
“There has been evidence from recent cohort studies in the U.S. that was suggesting that the prevalence and incidence [of gout] was growing among non-White populations,” said Natalie McCormick, PhD, the study’s lead author and postdoctoral research fellow in medicine in the division of rheumatology, allergy, and immunology at Massachusetts General Hospital and Harvard Medical School, both in Boston. “We wanted to do this at the general population level to see how generalizable [that evidence] is.”
Alvin Wells, MD, PhD, director of the department of rheumatology at Advocate Aurora Medical Group, Franklin, Wisc., noted the findings highlight inequities in care for patients with gout that could be improved with greater emphasis on educating patients about their condition.
“I think that what this shows is that in the U.S. ... there still are some disparities in treating gout,” said Dr. Wells, who was not involved with the study. “And that we have ways to mitigate that, with not only aggressive therapy, but also with other tools like counseling patients. At the end of the day, people all want to be educated about the disease.”
Greater prevalence disappears with adjustment for socioclinical factors
The cross-sectional analysis involved data from U.S. adult participants in the National Health and Nutrition Examination Survey (NHANES) from 2007 to 2016 who self-reported Black or White race.
Investigators considered factors such as excess body mass index (BMI), chronic kidney disease (defined as estimated glomerular filtration rate less than 60 mL/min per 1.73 m2), poverty, poor-quality diet, lower educational level, alcohol consumption, and diuretic use in their analysis.
Dr. McCormick and coinvestigators included a total of 18,693 participants, consisting of 3,304 Black women, 6,195 White women, 3,085 Black men, and 6,109 White men.
They determined that the age-standardized prevalence of gout was 3.5% (95% confidence interval, 2.7%-4.3%) in Black women and 2.0% (95% CI, 1.5% - 2.5%) in White women (age-adjusted odds ratio, 1.81; 95% CI, 1.29-2.53). They calculated that the prevalence was 7.0% (95% CI, 6.2%-7.9%) in Black men and 5.4% (95% CI, 4.7%-6.2%) in White men (age-adjusted OR, 1.26; 95% CI, 1.02-1.55). They found similar differences in the prevalence of hyperuricemia between Black and White Americans.
The increased prevalence of gout in Black Americans, compared with White Americans, does not arise from genetics, according to McCormick. “Our conclusion was that it was due to social determinants of health,” she said. “When we adjusted for all socioclinical risk factors, the racial differences in gout and hyperuricemia prevalence disappeared. Importantly, stepwise regression analysis showed the two biggest drivers of the racial difference in gout prevalence among women were poverty itself, and excess BMI, which can be influenced by poverty.”
Dr. McCormick pointed out that in contrast to the current data, there was no racial difference in the prevalence of gout approximately 2 decades earlier, looking at data from the 1988-1994 NHANES III.
Given the findings, which included the fact that significantly more Black women and men were currently taking diuretics, compared with their White counterparts, Dr. McCormick pointed out clinicians should give more thought to medical therapies prescribed for conditions like high blood pressure to patients with gout or at risk for gout.
“One thing we found was that diuretic use was a driver” of gout, Dr. McCormick said. A prescriber “may want to consider different therapies that present a lower risk of gout if someone has hypertension. There could be greater consideration for prescribing alternatives to diuretics.”
More patient education and rheumatology referrals needed
An impediment to providing that education to patients with gout is unconscious bias on the part of the primary care provider, Dr. Wells said.
“It is about what your perspectives are and what you bring to the table,” he explained. “If you saw [a patient] who looked like someone in your family, that person will be treated differently [than someone who does not look like a family member]. That is where the whole concept [of unconscious bias] comes in.”
Primary care providers need to adopt a holistic approach to gout management that involves counseling about good nutrition, smoking cessation, regular exercise, and limiting alcohol consumption, in addition to medication adherence. Primary care providers may have a bias in treating their Black patients, failing to devote sufficient time and attention to assist them in getting their disease under control, he said.
“Gout should be just like any other chronic disease,” Dr. Wells said. “You need to have a target in mind, and you and your patient need to work together to get to that target. When [patients] end up in rheumatology offices, it is almost too late. I think the take-home message here is that in 2022 ... for any patient who has gout, that patient probably needs to be seen by a rheumatologist because, indeed, with aggressive therapy, preventive therapy, [and] education, and if they are on the right medications, they won’t end up with these crippling joints that we see all the time.”
Dr. McCormick and Dr. Wells disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Gout prevalence is more common in Black Americans than White Americans, and the disparity in prevalence is attributable to social determinants of health, according to a recently published article in JAMA Network Open.
“There has been evidence from recent cohort studies in the U.S. that was suggesting that the prevalence and incidence [of gout] was growing among non-White populations,” said Natalie McCormick, PhD, the study’s lead author and postdoctoral research fellow in medicine in the division of rheumatology, allergy, and immunology at Massachusetts General Hospital and Harvard Medical School, both in Boston. “We wanted to do this at the general population level to see how generalizable [that evidence] is.”
Alvin Wells, MD, PhD, director of the department of rheumatology at Advocate Aurora Medical Group, Franklin, Wisc., noted the findings highlight inequities in care for patients with gout that could be improved with greater emphasis on educating patients about their condition.
“I think that what this shows is that in the U.S. ... there still are some disparities in treating gout,” said Dr. Wells, who was not involved with the study. “And that we have ways to mitigate that, with not only aggressive therapy, but also with other tools like counseling patients. At the end of the day, people all want to be educated about the disease.”
Greater prevalence disappears with adjustment for socioclinical factors
The cross-sectional analysis involved data from U.S. adult participants in the National Health and Nutrition Examination Survey (NHANES) from 2007 to 2016 who self-reported Black or White race.
Investigators considered factors such as excess body mass index (BMI), chronic kidney disease (defined as estimated glomerular filtration rate less than 60 mL/min per 1.73 m2), poverty, poor-quality diet, lower educational level, alcohol consumption, and diuretic use in their analysis.
Dr. McCormick and coinvestigators included a total of 18,693 participants, consisting of 3,304 Black women, 6,195 White women, 3,085 Black men, and 6,109 White men.
They determined that the age-standardized prevalence of gout was 3.5% (95% confidence interval, 2.7%-4.3%) in Black women and 2.0% (95% CI, 1.5% - 2.5%) in White women (age-adjusted odds ratio, 1.81; 95% CI, 1.29-2.53). They calculated that the prevalence was 7.0% (95% CI, 6.2%-7.9%) in Black men and 5.4% (95% CI, 4.7%-6.2%) in White men (age-adjusted OR, 1.26; 95% CI, 1.02-1.55). They found similar differences in the prevalence of hyperuricemia between Black and White Americans.
The increased prevalence of gout in Black Americans, compared with White Americans, does not arise from genetics, according to McCormick. “Our conclusion was that it was due to social determinants of health,” she said. “When we adjusted for all socioclinical risk factors, the racial differences in gout and hyperuricemia prevalence disappeared. Importantly, stepwise regression analysis showed the two biggest drivers of the racial difference in gout prevalence among women were poverty itself, and excess BMI, which can be influenced by poverty.”
Dr. McCormick pointed out that in contrast to the current data, there was no racial difference in the prevalence of gout approximately 2 decades earlier, looking at data from the 1988-1994 NHANES III.
Given the findings, which included the fact that significantly more Black women and men were currently taking diuretics, compared with their White counterparts, Dr. McCormick pointed out clinicians should give more thought to medical therapies prescribed for conditions like high blood pressure to patients with gout or at risk for gout.
“One thing we found was that diuretic use was a driver” of gout, Dr. McCormick said. A prescriber “may want to consider different therapies that present a lower risk of gout if someone has hypertension. There could be greater consideration for prescribing alternatives to diuretics.”
More patient education and rheumatology referrals needed
An impediment to providing that education to patients with gout is unconscious bias on the part of the primary care provider, Dr. Wells said.
“It is about what your perspectives are and what you bring to the table,” he explained. “If you saw [a patient] who looked like someone in your family, that person will be treated differently [than someone who does not look like a family member]. That is where the whole concept [of unconscious bias] comes in.”
Primary care providers need to adopt a holistic approach to gout management that involves counseling about good nutrition, smoking cessation, regular exercise, and limiting alcohol consumption, in addition to medication adherence. Primary care providers may have a bias in treating their Black patients, failing to devote sufficient time and attention to assist them in getting their disease under control, he said.
“Gout should be just like any other chronic disease,” Dr. Wells said. “You need to have a target in mind, and you and your patient need to work together to get to that target. When [patients] end up in rheumatology offices, it is almost too late. I think the take-home message here is that in 2022 ... for any patient who has gout, that patient probably needs to be seen by a rheumatologist because, indeed, with aggressive therapy, preventive therapy, [and] education, and if they are on the right medications, they won’t end up with these crippling joints that we see all the time.”
Dr. McCormick and Dr. Wells disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Gout flares linked to transient jump in MI, stroke risk
There is evidence that gout and heart disease are mechanistically linked by inflammation and patients with gout are at elevated risk for cardiovascular disease (CVD). But do gout flares, on their own, affect short-term risk for CV events? A new analysis based on records from British medical practices suggests that might be the case.
Risk for myocardial infarction or stroke climbed in the weeks after individual gout flare-ups in the study’s more than 60,000 patients with a recent gout diagnosis. The jump in risk, significant but small in absolute terms, held for about 4 months in the case-control study before going away.
A sensitivity analysis that excluded patients who already had CVD when their gout was diagnosed yielded similar results.
The observational study isn’t able to show that gout flares themselves transiently raise the risk for MI or stroke, but it’s enough to send a cautionary message to physicians who care for patients with gout, rheumatologist Abhishek Abhishek, PhD, Nottingham (England) City Hospital, said in an interview.
In such patients who also have conditions like hypertension, diabetes, or dyslipidemia, or a history of heart disease, he said, it’s important “to manage risk factors really aggressively, knowing that when these patients have a gout flare, there’s a temporary increase in risk of a cardiovascular event.”
Managing their absolute CV risk – whether with drug therapy, lifestyle changes, or other interventions – should help limit the transient jump in risk for MI or stroke following a gout flare, proposed Dr. Abhishek, who is senior author on the study published in JAMA, with lead author Edoardo Cipolletta, MD, also from Nottingham City Hospital.
First robust evidence
The case-control study, which involved more than 60,000 patients with a recent gout diagnosis, some who went on to have MI or stroke, looked at rates of such events at different time intervals after gout flares. Those who experienced such events showed a more than 90% increased likelihood of a gout flare-up in the preceding 60 days, a greater than 50% chance of a flare between 60 and 120 days before the event, but no increased likelihood prior to 120 days before the event.
Such a link between gout flares and CV events “has been suspected but never proven,” observed rheumatologist Hyon K. Choi, MD, Harvard Medical School, Boston, who was not associated with the analysis. “This is the first time it has actually been shown in a robust way,” he said in an interview.
The study suggests a “likely causative relationship” between gout flares and CV events, but – as the published report noted – has limitations like any observational study, said Dr. Choi, who also directs the Gout & Crystal Arthropathy Center at Massachusetts General Hospital, Boston. “Hopefully, this can be replicated in other cohorts.”
The analysis controlled for a number of relevant potential confounders, he noted, but couldn’t account for all issues that could argue against gout flares as a direct cause of the MIs and strokes.
Gout attacks are a complex experience with a range of potential indirect effects on CV risk, Dr. Choi observed. They can immobilize patients, possibly raising their risk for thrombotic events, for example. They can be exceptionally painful, which causes stress and can lead to frequent or chronic use of glucocorticoids or NSAIDs, all of which can exacerbate high blood pressure and possibly worsen CV risk.
A unique insight
The timing of gout flares relative to acute vascular events hasn’t been fully explored, observed an accompanying editorial. The current study’s “unique insight,” it stated, “is that disease activity from gout was associated with an incremental increase in risk for acute vascular events during the time period immediately following the gout flare.”
Although the study is observational, a “large body of evidence from animal and human research, mechanistic insights, and clinical interventions” support an association between flares and vascular events and “make a causal link eminently reasonable,” stated the editorialists, Jeffrey L. Anderson, MD, and Kirk U. Knowlton, MD, both with Intermountain Medical Center, Salt Lake City, Utah.
The findings, they wrote, “should alert clinicians and patients to the increased cardiovascular risk in the weeks beginning after a gout flare and should focus attention on optimizing preventive measures.” Those can include “lifestyle measures and standard risk-factor control including adherence to diet, statins, anti-inflammatory drugs (e.g., aspirin, colchicine), smoking cessation, diabetic and blood pressure control, and antithrombotic medications as indicated.”
Dr. Choi said the current results argue for more liberal use of colchicine, and for preferring colchicine over other anti-inflammatories, in patients with gout and traditional CV risk factors, given multiple randomized trials supporting the drug’s use in such cases. “If you use colchicine, you are covering their heart disease risk as well as their gout. It’s two birds with one stone.”
Nested case-control study
The investigators accessed electronic health records from 96,153 patients with recently diagnosed gout in England from 1997 to 2020; the cohort’s mean age was about 76 years, and 69% of participants were men. They matched 10,475 patients with at least one CV event to 52,099 others who didn’t have such an event by age, sex, and time from gout diagnosis. In each matched set of patients, those not experiencing a CV event were assigned a flare-to-event interval based on their matching with patients who did experience such an event.
Those with CV events, compared with patients without an event, had a greater than 90% increased likelihood of experiencing a gout flare-up in the 60 days preceding the event, a more than 50% greater chance of a flare-up 60-120 days before the CV event, but no increased likelihood more than 120 days before the event.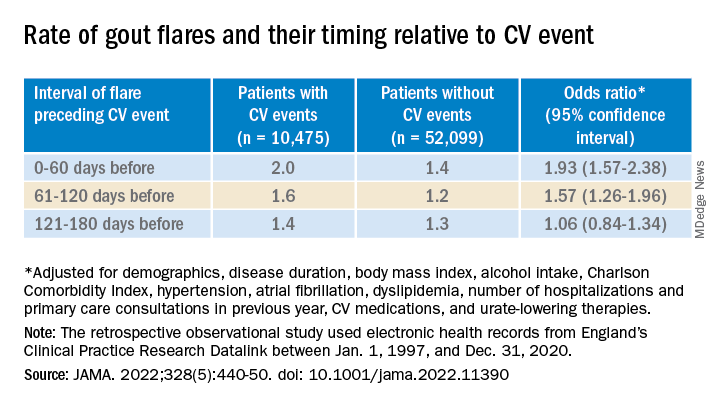
A self-controlled case series based on the same overall cohort with gout yielded similar results while sidestepping any potential for residual confounding, an inherent concern with any case–control analysis, the report notes. It involved 1,421 patients with one or more gout flare and at least one MI or stroke after the diagnosis of gout.
Among that cohort, the CV-event incidence rate ratio, adjusted for age and season of the year, by time interval after a gout flare, was 1.89 (95% confidence interval, 1.54-2.30) at 0-60 days, 1.64 (95% CI, 1.45-1.86) at 61-120 days, and1.29 (95% CI, 1.02-1.64) at 121-180 days.
Also similar, the report noted, were results of several sensitivity analyses, including one that excluded patients with confirmed CVD before their gout diagnosis; another that left out patients at low to moderate CV risk; and one that considered only gout flares treated with colchicine, corticosteroids, or NSAIDs.
The incremental CV event risks observed after flares in the study were small, which “has implications for both cost effectiveness and clinical relevance,” observed Dr. Anderson and Dr. Knowlton.
“An alternative to universal augmentation of cardiovascular risk prevention with therapies among patients with gout flares,” they wrote, would be “to further stratify risk by defining a group at highest near-term risk.” Such interventions could potentially be guided by markers of CV risk such as, for example, levels of high-sensitivity C-reactive protein or lipoprotein(a), or plaque burden on coronary-artery calcium scans.
Dr. Abhishek, Dr. Cipolletta, and the other authors reported no competing interests. Dr. Choi disclosed research support from Ironwood and Horizon; and consulting fees from Ironwood, Selecta, Horizon, Takeda, Kowa, and Vaxart. Dr. Anderson disclosed receiving grants to his institution from Novartis and Milestone.
A version of this article first appeared on Medscape.com.
There is evidence that gout and heart disease are mechanistically linked by inflammation and patients with gout are at elevated risk for cardiovascular disease (CVD). But do gout flares, on their own, affect short-term risk for CV events? A new analysis based on records from British medical practices suggests that might be the case.
Risk for myocardial infarction or stroke climbed in the weeks after individual gout flare-ups in the study’s more than 60,000 patients with a recent gout diagnosis. The jump in risk, significant but small in absolute terms, held for about 4 months in the case-control study before going away.
A sensitivity analysis that excluded patients who already had CVD when their gout was diagnosed yielded similar results.
The observational study isn’t able to show that gout flares themselves transiently raise the risk for MI or stroke, but it’s enough to send a cautionary message to physicians who care for patients with gout, rheumatologist Abhishek Abhishek, PhD, Nottingham (England) City Hospital, said in an interview.
In such patients who also have conditions like hypertension, diabetes, or dyslipidemia, or a history of heart disease, he said, it’s important “to manage risk factors really aggressively, knowing that when these patients have a gout flare, there’s a temporary increase in risk of a cardiovascular event.”
Managing their absolute CV risk – whether with drug therapy, lifestyle changes, or other interventions – should help limit the transient jump in risk for MI or stroke following a gout flare, proposed Dr. Abhishek, who is senior author on the study published in JAMA, with lead author Edoardo Cipolletta, MD, also from Nottingham City Hospital.
First robust evidence
The case-control study, which involved more than 60,000 patients with a recent gout diagnosis, some who went on to have MI or stroke, looked at rates of such events at different time intervals after gout flares. Those who experienced such events showed a more than 90% increased likelihood of a gout flare-up in the preceding 60 days, a greater than 50% chance of a flare between 60 and 120 days before the event, but no increased likelihood prior to 120 days before the event.
Such a link between gout flares and CV events “has been suspected but never proven,” observed rheumatologist Hyon K. Choi, MD, Harvard Medical School, Boston, who was not associated with the analysis. “This is the first time it has actually been shown in a robust way,” he said in an interview.
The study suggests a “likely causative relationship” between gout flares and CV events, but – as the published report noted – has limitations like any observational study, said Dr. Choi, who also directs the Gout & Crystal Arthropathy Center at Massachusetts General Hospital, Boston. “Hopefully, this can be replicated in other cohorts.”
The analysis controlled for a number of relevant potential confounders, he noted, but couldn’t account for all issues that could argue against gout flares as a direct cause of the MIs and strokes.
Gout attacks are a complex experience with a range of potential indirect effects on CV risk, Dr. Choi observed. They can immobilize patients, possibly raising their risk for thrombotic events, for example. They can be exceptionally painful, which causes stress and can lead to frequent or chronic use of glucocorticoids or NSAIDs, all of which can exacerbate high blood pressure and possibly worsen CV risk.
A unique insight
The timing of gout flares relative to acute vascular events hasn’t been fully explored, observed an accompanying editorial. The current study’s “unique insight,” it stated, “is that disease activity from gout was associated with an incremental increase in risk for acute vascular events during the time period immediately following the gout flare.”
Although the study is observational, a “large body of evidence from animal and human research, mechanistic insights, and clinical interventions” support an association between flares and vascular events and “make a causal link eminently reasonable,” stated the editorialists, Jeffrey L. Anderson, MD, and Kirk U. Knowlton, MD, both with Intermountain Medical Center, Salt Lake City, Utah.
The findings, they wrote, “should alert clinicians and patients to the increased cardiovascular risk in the weeks beginning after a gout flare and should focus attention on optimizing preventive measures.” Those can include “lifestyle measures and standard risk-factor control including adherence to diet, statins, anti-inflammatory drugs (e.g., aspirin, colchicine), smoking cessation, diabetic and blood pressure control, and antithrombotic medications as indicated.”
Dr. Choi said the current results argue for more liberal use of colchicine, and for preferring colchicine over other anti-inflammatories, in patients with gout and traditional CV risk factors, given multiple randomized trials supporting the drug’s use in such cases. “If you use colchicine, you are covering their heart disease risk as well as their gout. It’s two birds with one stone.”
Nested case-control study
The investigators accessed electronic health records from 96,153 patients with recently diagnosed gout in England from 1997 to 2020; the cohort’s mean age was about 76 years, and 69% of participants were men. They matched 10,475 patients with at least one CV event to 52,099 others who didn’t have such an event by age, sex, and time from gout diagnosis. In each matched set of patients, those not experiencing a CV event were assigned a flare-to-event interval based on their matching with patients who did experience such an event.
Those with CV events, compared with patients without an event, had a greater than 90% increased likelihood of experiencing a gout flare-up in the 60 days preceding the event, a more than 50% greater chance of a flare-up 60-120 days before the CV event, but no increased likelihood more than 120 days before the event.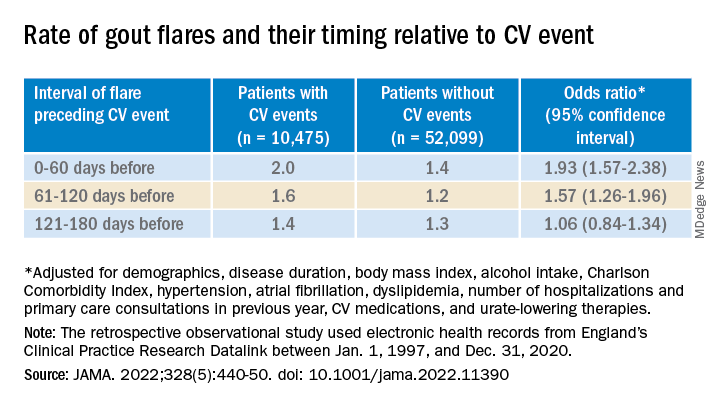
A self-controlled case series based on the same overall cohort with gout yielded similar results while sidestepping any potential for residual confounding, an inherent concern with any case–control analysis, the report notes. It involved 1,421 patients with one or more gout flare and at least one MI or stroke after the diagnosis of gout.
Among that cohort, the CV-event incidence rate ratio, adjusted for age and season of the year, by time interval after a gout flare, was 1.89 (95% confidence interval, 1.54-2.30) at 0-60 days, 1.64 (95% CI, 1.45-1.86) at 61-120 days, and1.29 (95% CI, 1.02-1.64) at 121-180 days.
Also similar, the report noted, were results of several sensitivity analyses, including one that excluded patients with confirmed CVD before their gout diagnosis; another that left out patients at low to moderate CV risk; and one that considered only gout flares treated with colchicine, corticosteroids, or NSAIDs.
The incremental CV event risks observed after flares in the study were small, which “has implications for both cost effectiveness and clinical relevance,” observed Dr. Anderson and Dr. Knowlton.
“An alternative to universal augmentation of cardiovascular risk prevention with therapies among patients with gout flares,” they wrote, would be “to further stratify risk by defining a group at highest near-term risk.” Such interventions could potentially be guided by markers of CV risk such as, for example, levels of high-sensitivity C-reactive protein or lipoprotein(a), or plaque burden on coronary-artery calcium scans.
Dr. Abhishek, Dr. Cipolletta, and the other authors reported no competing interests. Dr. Choi disclosed research support from Ironwood and Horizon; and consulting fees from Ironwood, Selecta, Horizon, Takeda, Kowa, and Vaxart. Dr. Anderson disclosed receiving grants to his institution from Novartis and Milestone.
A version of this article first appeared on Medscape.com.
There is evidence that gout and heart disease are mechanistically linked by inflammation and patients with gout are at elevated risk for cardiovascular disease (CVD). But do gout flares, on their own, affect short-term risk for CV events? A new analysis based on records from British medical practices suggests that might be the case.
Risk for myocardial infarction or stroke climbed in the weeks after individual gout flare-ups in the study’s more than 60,000 patients with a recent gout diagnosis. The jump in risk, significant but small in absolute terms, held for about 4 months in the case-control study before going away.
A sensitivity analysis that excluded patients who already had CVD when their gout was diagnosed yielded similar results.
The observational study isn’t able to show that gout flares themselves transiently raise the risk for MI or stroke, but it’s enough to send a cautionary message to physicians who care for patients with gout, rheumatologist Abhishek Abhishek, PhD, Nottingham (England) City Hospital, said in an interview.
In such patients who also have conditions like hypertension, diabetes, or dyslipidemia, or a history of heart disease, he said, it’s important “to manage risk factors really aggressively, knowing that when these patients have a gout flare, there’s a temporary increase in risk of a cardiovascular event.”
Managing their absolute CV risk – whether with drug therapy, lifestyle changes, or other interventions – should help limit the transient jump in risk for MI or stroke following a gout flare, proposed Dr. Abhishek, who is senior author on the study published in JAMA, with lead author Edoardo Cipolletta, MD, also from Nottingham City Hospital.
First robust evidence
The case-control study, which involved more than 60,000 patients with a recent gout diagnosis, some who went on to have MI or stroke, looked at rates of such events at different time intervals after gout flares. Those who experienced such events showed a more than 90% increased likelihood of a gout flare-up in the preceding 60 days, a greater than 50% chance of a flare between 60 and 120 days before the event, but no increased likelihood prior to 120 days before the event.
Such a link between gout flares and CV events “has been suspected but never proven,” observed rheumatologist Hyon K. Choi, MD, Harvard Medical School, Boston, who was not associated with the analysis. “This is the first time it has actually been shown in a robust way,” he said in an interview.
The study suggests a “likely causative relationship” between gout flares and CV events, but – as the published report noted – has limitations like any observational study, said Dr. Choi, who also directs the Gout & Crystal Arthropathy Center at Massachusetts General Hospital, Boston. “Hopefully, this can be replicated in other cohorts.”
The analysis controlled for a number of relevant potential confounders, he noted, but couldn’t account for all issues that could argue against gout flares as a direct cause of the MIs and strokes.
Gout attacks are a complex experience with a range of potential indirect effects on CV risk, Dr. Choi observed. They can immobilize patients, possibly raising their risk for thrombotic events, for example. They can be exceptionally painful, which causes stress and can lead to frequent or chronic use of glucocorticoids or NSAIDs, all of which can exacerbate high blood pressure and possibly worsen CV risk.
A unique insight
The timing of gout flares relative to acute vascular events hasn’t been fully explored, observed an accompanying editorial. The current study’s “unique insight,” it stated, “is that disease activity from gout was associated with an incremental increase in risk for acute vascular events during the time period immediately following the gout flare.”
Although the study is observational, a “large body of evidence from animal and human research, mechanistic insights, and clinical interventions” support an association between flares and vascular events and “make a causal link eminently reasonable,” stated the editorialists, Jeffrey L. Anderson, MD, and Kirk U. Knowlton, MD, both with Intermountain Medical Center, Salt Lake City, Utah.
The findings, they wrote, “should alert clinicians and patients to the increased cardiovascular risk in the weeks beginning after a gout flare and should focus attention on optimizing preventive measures.” Those can include “lifestyle measures and standard risk-factor control including adherence to diet, statins, anti-inflammatory drugs (e.g., aspirin, colchicine), smoking cessation, diabetic and blood pressure control, and antithrombotic medications as indicated.”
Dr. Choi said the current results argue for more liberal use of colchicine, and for preferring colchicine over other anti-inflammatories, in patients with gout and traditional CV risk factors, given multiple randomized trials supporting the drug’s use in such cases. “If you use colchicine, you are covering their heart disease risk as well as their gout. It’s two birds with one stone.”
Nested case-control study
The investigators accessed electronic health records from 96,153 patients with recently diagnosed gout in England from 1997 to 2020; the cohort’s mean age was about 76 years, and 69% of participants were men. They matched 10,475 patients with at least one CV event to 52,099 others who didn’t have such an event by age, sex, and time from gout diagnosis. In each matched set of patients, those not experiencing a CV event were assigned a flare-to-event interval based on their matching with patients who did experience such an event.
Those with CV events, compared with patients without an event, had a greater than 90% increased likelihood of experiencing a gout flare-up in the 60 days preceding the event, a more than 50% greater chance of a flare-up 60-120 days before the CV event, but no increased likelihood more than 120 days before the event.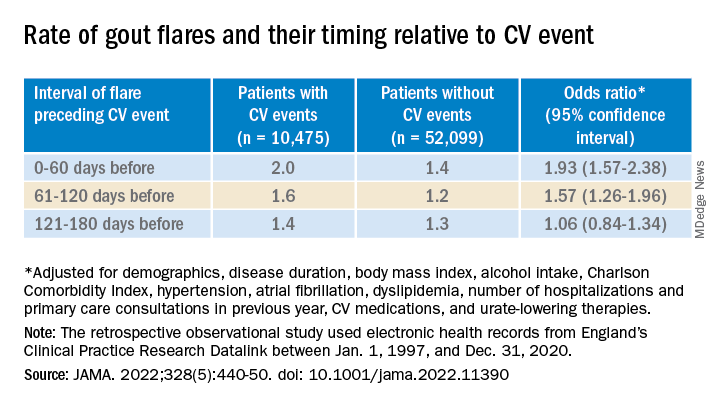
A self-controlled case series based on the same overall cohort with gout yielded similar results while sidestepping any potential for residual confounding, an inherent concern with any case–control analysis, the report notes. It involved 1,421 patients with one or more gout flare and at least one MI or stroke after the diagnosis of gout.
Among that cohort, the CV-event incidence rate ratio, adjusted for age and season of the year, by time interval after a gout flare, was 1.89 (95% confidence interval, 1.54-2.30) at 0-60 days, 1.64 (95% CI, 1.45-1.86) at 61-120 days, and1.29 (95% CI, 1.02-1.64) at 121-180 days.
Also similar, the report noted, were results of several sensitivity analyses, including one that excluded patients with confirmed CVD before their gout diagnosis; another that left out patients at low to moderate CV risk; and one that considered only gout flares treated with colchicine, corticosteroids, or NSAIDs.
The incremental CV event risks observed after flares in the study were small, which “has implications for both cost effectiveness and clinical relevance,” observed Dr. Anderson and Dr. Knowlton.
“An alternative to universal augmentation of cardiovascular risk prevention with therapies among patients with gout flares,” they wrote, would be “to further stratify risk by defining a group at highest near-term risk.” Such interventions could potentially be guided by markers of CV risk such as, for example, levels of high-sensitivity C-reactive protein or lipoprotein(a), or plaque burden on coronary-artery calcium scans.
Dr. Abhishek, Dr. Cipolletta, and the other authors reported no competing interests. Dr. Choi disclosed research support from Ironwood and Horizon; and consulting fees from Ironwood, Selecta, Horizon, Takeda, Kowa, and Vaxart. Dr. Anderson disclosed receiving grants to his institution from Novartis and Milestone.
A version of this article first appeared on Medscape.com.
FROM JAMA
Benzbromarone tops febuxostat for gout?
Benzbromarone is not approved in the United States because of concerns of acute liver injury but is approved in several other countries, including China, Brazil, and New Zealand.
“The results suggest that low dosing of benzbromarone may warrant stronger consideration as a safe and effective therapy to achieve serum urate target in gout without moderate chronic kidney disease,” the study team writes.
“Benzbromarone is severely hepatotoxic in some individuals and unlikely to ever gain approval in the United States,” one of the study’s investigators, Robert Terkeltaub, MD, professor of medicine, University of California, San Diego, told this news organization.
However, this study “illustrates the value and impact of uricosuric therapy in general in gout, including potentially as an initial urate-lowering monotherapy strategy, and the sheer number of subjects reaching urate target with low-dose uricosuric monotherapy was impressive,” Dr. Terkeltaub said.
The study was published online in Arthritis & Rheumatology.
“Renal uric acid underexcretion is the chief mechanism driving hyperuricemia in gout, yet the standard urate-lowering therapy recommendation is first-line xanthine oxidase inhibition irrespective of the cause of hyperuricemia,” the study team explains in their article.
Their prospective, randomized, single-center, open-labeled trial was conducted at the Gout Clinic of the Affiliated Hospital of Qingdao University, China.
A total of 196 relatively young healthy men with gout and uric acid underexcretion were randomly assigned to receive low-dose benzbromarone (25 mg/d) or low-dose febuxostat (20 mg/d) for 12 weeks.
Renal uric acid underexcretion was defined as fractional excretion of urate less than 5.5% and uric acid excretion less than or equal to 600 mg/d/1.73 m2.
A “major aspect” of this comparative effectiveness trial was its specific focus on gout-associated renal uric acid underexcretion, where the uricosuric targeted the dominant abnormality promoting the hyperuricemia, Dr. Terkeltaub told this news organization.
In addition, all participants received daily urine alkalinization with oral sodium bicarbonate. “This is not always done in clinical practice, nor in clinical trials of uricosuric agents,” Dr. Terkeltaub said.
The results showed that more participants in the benzbromarone group achieved the serum urate target of less than 6 mg/dL, compared with those in the febuxostat group (primary endpoint, 61% vs. 32%, P < .001).
Adverse events, including gout flares and urolithiasis, did not differ significantly between the two groups, with the exception of more transaminase elevation in the febuxostat group (15% vs. 4%; P = .008).
“We did not find severe hepatotoxicity with low-dose benzbromarone, but ethnic background may affect drug responses, and severe hepatotoxicity of benzbromarone has rarely been reported in Asia,” the authors write.
The incidence of urolithiasis was numerically, but not significantly, higher in the benzbromarone group (5% vs. 2%).
This study found no significant changes in participants’ triglyceride levels, though a previous study suggested febuxostat could increase serum triglycerides.
The investigators caution that the study only included patients who had baseline serum urate levels ranging from 8.0 to 10 mg/dL, who were relatively young and with few comorbidities.
The authors further noted that the “... results may not be generalizable to patients with higher serum urate levels or impaired kidney function, as well [as] patients from other geographical regions, age, and ethnicity groups. The study only included men, and the findings may not be generalizable to women with gout.”
‘Very useful’ in select cases
Weighing in on the results, Valderilio Feijó Azevedo, MD, PhD, adjunct professor of rheumatology, Federal University of Paraná, Brazil, noted that in some specific clinical circumstances, benzbromarone has been “a very useful medication, alone or combined, to treat gout patients.”
“We have great experience with the drug in Brazil. However, it is not used to treat all patients. Patients must be very well-selected in our clinical practice,” Dr. Azevedo said in an interview.
“For most patients, benzbromarone is effective for those who have failed to achieve serum uric acid goals with allopurinol treatment. We do not use it to treat patients with asymptomatic hyperuricemia. In general, we avoid patients with hepatic dysfunction due to previous hepatotoxicity reports. In every patient, we do active monitoring of enzymes,” Dr. Azevedo explained.
“We also avoid using it in patients with severe kidney disease. However, we have used it in some patients with estimated glomerular filtration rate less than 30. We also avoid dosage over 200 mg per day. On average, we use 100 mg per day combined with allopurinol or alone,” said Dr. Azevedo, who was not involved with the study.
Also weighing in, Michael Pillinger, MD, rheumatologist at NYU Langone Health, noted that while benzbromarone is not used in the United States, “in many parts of the world, it is used and is felt to be effective.” Dr. Pillinger was not associated with this current research.
This study, Dr. Pillinger said, “does underline the fact that an alternative drug that lowers urate by promoting urate excretion, if it could gain [U.S. Food and Drug Association] approval and if it were safe, could present a viable new option for therapy.”
He added, “If one conclusion to the study is that determining the basis of hyperuricemia is helpful in guiding benzbromarone use, that implies an additional layer of effort for physicians and patients in a disease that is already notoriously known for patient noncompliance – and in a case where febuxostat and allopurinol will work for both overproducers and underexcreters and would not need this additional assessment.”
The study was sponsored by Shandong Provincial Key Research and Development Plan, the National Natural Science Foundation of China, and Shandong Provincial Science Foundation for Outstanding Youth Scholarship. Dr. Terkeltaub was supported by the National Institutes of Health and the VA Research Service. Dr. Terkeltaub has received research funding from AstraZeneca, and has consulted with Horizon, Selecta, SOBI, Dyve BioSciences, Fortress, AstraZeneca, Allena, Fortress Biotech, and LG Life Sciences. Dr. Azevedo and Dr. Pillinger have no reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Benzbromarone is not approved in the United States because of concerns of acute liver injury but is approved in several other countries, including China, Brazil, and New Zealand.
“The results suggest that low dosing of benzbromarone may warrant stronger consideration as a safe and effective therapy to achieve serum urate target in gout without moderate chronic kidney disease,” the study team writes.
“Benzbromarone is severely hepatotoxic in some individuals and unlikely to ever gain approval in the United States,” one of the study’s investigators, Robert Terkeltaub, MD, professor of medicine, University of California, San Diego, told this news organization.
However, this study “illustrates the value and impact of uricosuric therapy in general in gout, including potentially as an initial urate-lowering monotherapy strategy, and the sheer number of subjects reaching urate target with low-dose uricosuric monotherapy was impressive,” Dr. Terkeltaub said.
The study was published online in Arthritis & Rheumatology.
“Renal uric acid underexcretion is the chief mechanism driving hyperuricemia in gout, yet the standard urate-lowering therapy recommendation is first-line xanthine oxidase inhibition irrespective of the cause of hyperuricemia,” the study team explains in their article.
Their prospective, randomized, single-center, open-labeled trial was conducted at the Gout Clinic of the Affiliated Hospital of Qingdao University, China.
A total of 196 relatively young healthy men with gout and uric acid underexcretion were randomly assigned to receive low-dose benzbromarone (25 mg/d) or low-dose febuxostat (20 mg/d) for 12 weeks.
Renal uric acid underexcretion was defined as fractional excretion of urate less than 5.5% and uric acid excretion less than or equal to 600 mg/d/1.73 m2.
A “major aspect” of this comparative effectiveness trial was its specific focus on gout-associated renal uric acid underexcretion, where the uricosuric targeted the dominant abnormality promoting the hyperuricemia, Dr. Terkeltaub told this news organization.
In addition, all participants received daily urine alkalinization with oral sodium bicarbonate. “This is not always done in clinical practice, nor in clinical trials of uricosuric agents,” Dr. Terkeltaub said.
The results showed that more participants in the benzbromarone group achieved the serum urate target of less than 6 mg/dL, compared with those in the febuxostat group (primary endpoint, 61% vs. 32%, P < .001).
Adverse events, including gout flares and urolithiasis, did not differ significantly between the two groups, with the exception of more transaminase elevation in the febuxostat group (15% vs. 4%; P = .008).
“We did not find severe hepatotoxicity with low-dose benzbromarone, but ethnic background may affect drug responses, and severe hepatotoxicity of benzbromarone has rarely been reported in Asia,” the authors write.
The incidence of urolithiasis was numerically, but not significantly, higher in the benzbromarone group (5% vs. 2%).
This study found no significant changes in participants’ triglyceride levels, though a previous study suggested febuxostat could increase serum triglycerides.
The investigators caution that the study only included patients who had baseline serum urate levels ranging from 8.0 to 10 mg/dL, who were relatively young and with few comorbidities.
The authors further noted that the “... results may not be generalizable to patients with higher serum urate levels or impaired kidney function, as well [as] patients from other geographical regions, age, and ethnicity groups. The study only included men, and the findings may not be generalizable to women with gout.”
‘Very useful’ in select cases
Weighing in on the results, Valderilio Feijó Azevedo, MD, PhD, adjunct professor of rheumatology, Federal University of Paraná, Brazil, noted that in some specific clinical circumstances, benzbromarone has been “a very useful medication, alone or combined, to treat gout patients.”
“We have great experience with the drug in Brazil. However, it is not used to treat all patients. Patients must be very well-selected in our clinical practice,” Dr. Azevedo said in an interview.
“For most patients, benzbromarone is effective for those who have failed to achieve serum uric acid goals with allopurinol treatment. We do not use it to treat patients with asymptomatic hyperuricemia. In general, we avoid patients with hepatic dysfunction due to previous hepatotoxicity reports. In every patient, we do active monitoring of enzymes,” Dr. Azevedo explained.
“We also avoid using it in patients with severe kidney disease. However, we have used it in some patients with estimated glomerular filtration rate less than 30. We also avoid dosage over 200 mg per day. On average, we use 100 mg per day combined with allopurinol or alone,” said Dr. Azevedo, who was not involved with the study.
Also weighing in, Michael Pillinger, MD, rheumatologist at NYU Langone Health, noted that while benzbromarone is not used in the United States, “in many parts of the world, it is used and is felt to be effective.” Dr. Pillinger was not associated with this current research.
This study, Dr. Pillinger said, “does underline the fact that an alternative drug that lowers urate by promoting urate excretion, if it could gain [U.S. Food and Drug Association] approval and if it were safe, could present a viable new option for therapy.”
He added, “If one conclusion to the study is that determining the basis of hyperuricemia is helpful in guiding benzbromarone use, that implies an additional layer of effort for physicians and patients in a disease that is already notoriously known for patient noncompliance – and in a case where febuxostat and allopurinol will work for both overproducers and underexcreters and would not need this additional assessment.”
The study was sponsored by Shandong Provincial Key Research and Development Plan, the National Natural Science Foundation of China, and Shandong Provincial Science Foundation for Outstanding Youth Scholarship. Dr. Terkeltaub was supported by the National Institutes of Health and the VA Research Service. Dr. Terkeltaub has received research funding from AstraZeneca, and has consulted with Horizon, Selecta, SOBI, Dyve BioSciences, Fortress, AstraZeneca, Allena, Fortress Biotech, and LG Life Sciences. Dr. Azevedo and Dr. Pillinger have no reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Benzbromarone is not approved in the United States because of concerns of acute liver injury but is approved in several other countries, including China, Brazil, and New Zealand.
“The results suggest that low dosing of benzbromarone may warrant stronger consideration as a safe and effective therapy to achieve serum urate target in gout without moderate chronic kidney disease,” the study team writes.
“Benzbromarone is severely hepatotoxic in some individuals and unlikely to ever gain approval in the United States,” one of the study’s investigators, Robert Terkeltaub, MD, professor of medicine, University of California, San Diego, told this news organization.
However, this study “illustrates the value and impact of uricosuric therapy in general in gout, including potentially as an initial urate-lowering monotherapy strategy, and the sheer number of subjects reaching urate target with low-dose uricosuric monotherapy was impressive,” Dr. Terkeltaub said.
The study was published online in Arthritis & Rheumatology.
“Renal uric acid underexcretion is the chief mechanism driving hyperuricemia in gout, yet the standard urate-lowering therapy recommendation is first-line xanthine oxidase inhibition irrespective of the cause of hyperuricemia,” the study team explains in their article.
Their prospective, randomized, single-center, open-labeled trial was conducted at the Gout Clinic of the Affiliated Hospital of Qingdao University, China.
A total of 196 relatively young healthy men with gout and uric acid underexcretion were randomly assigned to receive low-dose benzbromarone (25 mg/d) or low-dose febuxostat (20 mg/d) for 12 weeks.
Renal uric acid underexcretion was defined as fractional excretion of urate less than 5.5% and uric acid excretion less than or equal to 600 mg/d/1.73 m2.
A “major aspect” of this comparative effectiveness trial was its specific focus on gout-associated renal uric acid underexcretion, where the uricosuric targeted the dominant abnormality promoting the hyperuricemia, Dr. Terkeltaub told this news organization.
In addition, all participants received daily urine alkalinization with oral sodium bicarbonate. “This is not always done in clinical practice, nor in clinical trials of uricosuric agents,” Dr. Terkeltaub said.
The results showed that more participants in the benzbromarone group achieved the serum urate target of less than 6 mg/dL, compared with those in the febuxostat group (primary endpoint, 61% vs. 32%, P < .001).
Adverse events, including gout flares and urolithiasis, did not differ significantly between the two groups, with the exception of more transaminase elevation in the febuxostat group (15% vs. 4%; P = .008).
“We did not find severe hepatotoxicity with low-dose benzbromarone, but ethnic background may affect drug responses, and severe hepatotoxicity of benzbromarone has rarely been reported in Asia,” the authors write.
The incidence of urolithiasis was numerically, but not significantly, higher in the benzbromarone group (5% vs. 2%).
This study found no significant changes in participants’ triglyceride levels, though a previous study suggested febuxostat could increase serum triglycerides.
The investigators caution that the study only included patients who had baseline serum urate levels ranging from 8.0 to 10 mg/dL, who were relatively young and with few comorbidities.
The authors further noted that the “... results may not be generalizable to patients with higher serum urate levels or impaired kidney function, as well [as] patients from other geographical regions, age, and ethnicity groups. The study only included men, and the findings may not be generalizable to women with gout.”
‘Very useful’ in select cases
Weighing in on the results, Valderilio Feijó Azevedo, MD, PhD, adjunct professor of rheumatology, Federal University of Paraná, Brazil, noted that in some specific clinical circumstances, benzbromarone has been “a very useful medication, alone or combined, to treat gout patients.”
“We have great experience with the drug in Brazil. However, it is not used to treat all patients. Patients must be very well-selected in our clinical practice,” Dr. Azevedo said in an interview.
“For most patients, benzbromarone is effective for those who have failed to achieve serum uric acid goals with allopurinol treatment. We do not use it to treat patients with asymptomatic hyperuricemia. In general, we avoid patients with hepatic dysfunction due to previous hepatotoxicity reports. In every patient, we do active monitoring of enzymes,” Dr. Azevedo explained.
“We also avoid using it in patients with severe kidney disease. However, we have used it in some patients with estimated glomerular filtration rate less than 30. We also avoid dosage over 200 mg per day. On average, we use 100 mg per day combined with allopurinol or alone,” said Dr. Azevedo, who was not involved with the study.
Also weighing in, Michael Pillinger, MD, rheumatologist at NYU Langone Health, noted that while benzbromarone is not used in the United States, “in many parts of the world, it is used and is felt to be effective.” Dr. Pillinger was not associated with this current research.
This study, Dr. Pillinger said, “does underline the fact that an alternative drug that lowers urate by promoting urate excretion, if it could gain [U.S. Food and Drug Association] approval and if it were safe, could present a viable new option for therapy.”
He added, “If one conclusion to the study is that determining the basis of hyperuricemia is helpful in guiding benzbromarone use, that implies an additional layer of effort for physicians and patients in a disease that is already notoriously known for patient noncompliance – and in a case where febuxostat and allopurinol will work for both overproducers and underexcreters and would not need this additional assessment.”
The study was sponsored by Shandong Provincial Key Research and Development Plan, the National Natural Science Foundation of China, and Shandong Provincial Science Foundation for Outstanding Youth Scholarship. Dr. Terkeltaub was supported by the National Institutes of Health and the VA Research Service. Dr. Terkeltaub has received research funding from AstraZeneca, and has consulted with Horizon, Selecta, SOBI, Dyve BioSciences, Fortress, AstraZeneca, Allena, Fortress Biotech, and LG Life Sciences. Dr. Azevedo and Dr. Pillinger have no reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA approves combination pegloticase and methotrexate for refractory gout
Pegloticase, which has been available for 12 years, is a pegylated uric acid specific enzyme that lowers sUA by converting it to allantoin.
Though pegloticase is effective in treating chronic gout in patients refractory to conventional treatment, approximately 92% of patients develop antibodies against the drug, resulting in reduced efficacy.
Based on the immunomodulatory effects of methotrexate, researchers of the randomized, placebo-controlled MIRROR trial sought to determine whether combination treatment of pegloticase with methotrexate (multiple brands) would prevent the development of anti-drug antibodies.
Findings from the phase 4 trial found that co-administration of pegloticase and methotrexate reduced the formation of new anti-PEG antibodies. In the group receiving methotrexate and pegloticase, 23.2% (22 out of 95) of patients had an increase in anti-PEG antibodies, compared with 50% (24 of 48) in the pegloticase plus placebo group, according to a recent company press release.
Nearly three-quarters (71%) of participants in the group pretreated with methotrexate, followed by combination pegloticase-methotrexate, had sUA levels that dopped to below 6 mg/dL during the 52-week study. By comparison, 38.5% of participants in the pegloticase and placebo group reached the endpoint. Though gout flare occurred in both groups, methotrexate did not appear to increase the risk for adverse events or gout flare.
The study, led by John Botson, MD, RPh, CCD, a rheumatologist in Anchorage, Alaska, concluded that these measurements demonstrated a significant improvement from traditional pegloticase-only treatment of gout. “This trial confirms not only improved efficacy but improved safety in patients treated with pegloticase in combination with methotrexate 15 mg orally once weekly,” Dr. Botson said last month in an interview with this news organization.
The study was funded by Horizon. Dr. Botson reports receiving research support from Horizon and Radius Health and speaker fees from AbbVie, Amgen, Aurinia, ChemoCentryx, Horizon, Eli Lilly, and Novartis.
A version of this article first appeared on Medscape.com.
Pegloticase, which has been available for 12 years, is a pegylated uric acid specific enzyme that lowers sUA by converting it to allantoin.
Though pegloticase is effective in treating chronic gout in patients refractory to conventional treatment, approximately 92% of patients develop antibodies against the drug, resulting in reduced efficacy.
Based on the immunomodulatory effects of methotrexate, researchers of the randomized, placebo-controlled MIRROR trial sought to determine whether combination treatment of pegloticase with methotrexate (multiple brands) would prevent the development of anti-drug antibodies.
Findings from the phase 4 trial found that co-administration of pegloticase and methotrexate reduced the formation of new anti-PEG antibodies. In the group receiving methotrexate and pegloticase, 23.2% (22 out of 95) of patients had an increase in anti-PEG antibodies, compared with 50% (24 of 48) in the pegloticase plus placebo group, according to a recent company press release.
Nearly three-quarters (71%) of participants in the group pretreated with methotrexate, followed by combination pegloticase-methotrexate, had sUA levels that dopped to below 6 mg/dL during the 52-week study. By comparison, 38.5% of participants in the pegloticase and placebo group reached the endpoint. Though gout flare occurred in both groups, methotrexate did not appear to increase the risk for adverse events or gout flare.
The study, led by John Botson, MD, RPh, CCD, a rheumatologist in Anchorage, Alaska, concluded that these measurements demonstrated a significant improvement from traditional pegloticase-only treatment of gout. “This trial confirms not only improved efficacy but improved safety in patients treated with pegloticase in combination with methotrexate 15 mg orally once weekly,” Dr. Botson said last month in an interview with this news organization.
The study was funded by Horizon. Dr. Botson reports receiving research support from Horizon and Radius Health and speaker fees from AbbVie, Amgen, Aurinia, ChemoCentryx, Horizon, Eli Lilly, and Novartis.
A version of this article first appeared on Medscape.com.
Pegloticase, which has been available for 12 years, is a pegylated uric acid specific enzyme that lowers sUA by converting it to allantoin.
Though pegloticase is effective in treating chronic gout in patients refractory to conventional treatment, approximately 92% of patients develop antibodies against the drug, resulting in reduced efficacy.
Based on the immunomodulatory effects of methotrexate, researchers of the randomized, placebo-controlled MIRROR trial sought to determine whether combination treatment of pegloticase with methotrexate (multiple brands) would prevent the development of anti-drug antibodies.
Findings from the phase 4 trial found that co-administration of pegloticase and methotrexate reduced the formation of new anti-PEG antibodies. In the group receiving methotrexate and pegloticase, 23.2% (22 out of 95) of patients had an increase in anti-PEG antibodies, compared with 50% (24 of 48) in the pegloticase plus placebo group, according to a recent company press release.
Nearly three-quarters (71%) of participants in the group pretreated with methotrexate, followed by combination pegloticase-methotrexate, had sUA levels that dopped to below 6 mg/dL during the 52-week study. By comparison, 38.5% of participants in the pegloticase and placebo group reached the endpoint. Though gout flare occurred in both groups, methotrexate did not appear to increase the risk for adverse events or gout flare.
The study, led by John Botson, MD, RPh, CCD, a rheumatologist in Anchorage, Alaska, concluded that these measurements demonstrated a significant improvement from traditional pegloticase-only treatment of gout. “This trial confirms not only improved efficacy but improved safety in patients treated with pegloticase in combination with methotrexate 15 mg orally once weekly,” Dr. Botson said last month in an interview with this news organization.
The study was funded by Horizon. Dr. Botson reports receiving research support from Horizon and Radius Health and speaker fees from AbbVie, Amgen, Aurinia, ChemoCentryx, Horizon, Eli Lilly, and Novartis.
A version of this article first appeared on Medscape.com.
Alcohol consumption habits can predict gout tophi
The more years a person drinks alcohol, the kind of alcohol consumed, and the amount consumed can help to predict gout tophi, researchers say in a newly published paper in Arthritis Care and Research.
The study, led by Lin Han, PhD, of the gout laboratory, Shandong provincial clinical research center for immune diseases and gout, Affiliated Hospital of Qingdao (China) University, helps clarify the already-established relationship between alcohol consumption and gout tophi.
Additionally, the effects of drinking alcohol on ultrasound (US)–detected tophi and subcutaneous tophi (subtophi) were evaluated separately for the first time in this work, the authors say.
Tophi may be underdiagnosed because they are hard to find with only a physical exam. US can help with early detection, especially with small clusters of crystals or those found deep in the tissues, and offers good diagnostic accuracy with high specificity.
“Unlike subtophi, which represent long-term subcutaneous MSU [monosodium urate] deposition over many years, US-detected tophi represent the early stage of tophi in both intra- and extra-articular settings,” the authors write.
This cross-sectional study in China included 554 patients with gout who had joint ultrasound and physical exams through the Affiliated Hospital of Qingdao University. Physicians gathered medical histories using the Biobank Information Management System.
Physicians also tracked alcohol consumption patterns through the biobank information, which included answers to a detailed drinking questionnaire.
Patients were classified as either nondrinkers (no history of drinking; n = 141), former drinkers (n = 60), or current regular drinkers (n = 353). Current regular drinkers were asked further questions about their drinking patterns, including how long they have been drinking, type of alcohol they drink, and how much and how often they drink. In China, the average drink is considered to contain 10 g of alcohol, according to the World Health Organization.
Results from US and clinically detected tophi
Compared with nondrinkers, excessive drinkers (more than 70 g/week); long-term drinkers (at least 10 years), and spirits drinkers had a greater proportion, size, and number of US-detected tophi and subtophi (all P < .05).
After adjusting for confounders, the researchers found that excessive drinking was significantly associated with having US-detected tophi (odds ratio, 1.79) and subtophi (OR, 2.00). Similar associations were found for consumption of alcohol for at least 10 years (OR, 1.96 for US-detected tophi; OR, 2.17 for sub-tophi) and drinking spirits (OR, 1.81 for US-detected tophi; OR, 2.10 for subtophi). All comparisons were P < .05.
Among patients who already have US-detected tophi or subtophi, moderate drinking (70 g/week or less) was linked with larger or multiple tophi (all P < .05).
Angelo Gaffo, MD, section chief of rheumatology at the Birmingham VA Medical Center and associate professor of medicine in the division of rheumatology at the University of Alabama at Birmingham, said in an interview that the results are likely generalizable.
“I wouldn’t expect them to be specific to the Chinese population,” he said.
Most of the 554 patients were male (97.8%) and had no family history of gout (79.8%). The median duration of gout was 4 years, and the average age was 45.1 years.
Dr. Gaffo noted the population age was fairly young and the average duration of gout in these patients was fairly short. He also noted most had small tophi that were detected only by ultrasound and small numbers of tophi overall.
“I would like to see how these results will replicate in a population that has had gout for, say, 10 years on average,” he said.
Dr. Gaffo says he explores alcohol history with his patients with gout. If they are frequent drinkers, he encourages them to cut back.
“At the very least,” he said, “you have to restrict your intake to no more than 1-2 servings per week,” he said. “For some patients, even minimal amounts of alcohol intake can be associated with the development of flares.”
Still, research like this, he says, can help physicians point to evidence in their advice to patients about alcohol use.
He noted that the authors found the association between different types of alcohol and tophi was independent of serum urate level.
“That surprised me,” Dr. Gaffo said. “That’s a very unique finding.”
This work was supported by grants from the National Natural Science Foundation of China, the Natural Science Foundation of Shandong Province, Qingdao applied basic research project, National College Students’ Innovation and Entrepreneurship Training Program, and Shandong Provincial Science Foundation for Outstanding Youth Scholars.
The authors of the study and Dr. Gaffo report no relevant financial relationships.
The more years a person drinks alcohol, the kind of alcohol consumed, and the amount consumed can help to predict gout tophi, researchers say in a newly published paper in Arthritis Care and Research.
The study, led by Lin Han, PhD, of the gout laboratory, Shandong provincial clinical research center for immune diseases and gout, Affiliated Hospital of Qingdao (China) University, helps clarify the already-established relationship between alcohol consumption and gout tophi.
Additionally, the effects of drinking alcohol on ultrasound (US)–detected tophi and subcutaneous tophi (subtophi) were evaluated separately for the first time in this work, the authors say.
Tophi may be underdiagnosed because they are hard to find with only a physical exam. US can help with early detection, especially with small clusters of crystals or those found deep in the tissues, and offers good diagnostic accuracy with high specificity.
“Unlike subtophi, which represent long-term subcutaneous MSU [monosodium urate] deposition over many years, US-detected tophi represent the early stage of tophi in both intra- and extra-articular settings,” the authors write.
This cross-sectional study in China included 554 patients with gout who had joint ultrasound and physical exams through the Affiliated Hospital of Qingdao University. Physicians gathered medical histories using the Biobank Information Management System.
Physicians also tracked alcohol consumption patterns through the biobank information, which included answers to a detailed drinking questionnaire.
Patients were classified as either nondrinkers (no history of drinking; n = 141), former drinkers (n = 60), or current regular drinkers (n = 353). Current regular drinkers were asked further questions about their drinking patterns, including how long they have been drinking, type of alcohol they drink, and how much and how often they drink. In China, the average drink is considered to contain 10 g of alcohol, according to the World Health Organization.
Results from US and clinically detected tophi
Compared with nondrinkers, excessive drinkers (more than 70 g/week); long-term drinkers (at least 10 years), and spirits drinkers had a greater proportion, size, and number of US-detected tophi and subtophi (all P < .05).
After adjusting for confounders, the researchers found that excessive drinking was significantly associated with having US-detected tophi (odds ratio, 1.79) and subtophi (OR, 2.00). Similar associations were found for consumption of alcohol for at least 10 years (OR, 1.96 for US-detected tophi; OR, 2.17 for sub-tophi) and drinking spirits (OR, 1.81 for US-detected tophi; OR, 2.10 for subtophi). All comparisons were P < .05.
Among patients who already have US-detected tophi or subtophi, moderate drinking (70 g/week or less) was linked with larger or multiple tophi (all P < .05).
Angelo Gaffo, MD, section chief of rheumatology at the Birmingham VA Medical Center and associate professor of medicine in the division of rheumatology at the University of Alabama at Birmingham, said in an interview that the results are likely generalizable.
“I wouldn’t expect them to be specific to the Chinese population,” he said.
Most of the 554 patients were male (97.8%) and had no family history of gout (79.8%). The median duration of gout was 4 years, and the average age was 45.1 years.
Dr. Gaffo noted the population age was fairly young and the average duration of gout in these patients was fairly short. He also noted most had small tophi that were detected only by ultrasound and small numbers of tophi overall.
“I would like to see how these results will replicate in a population that has had gout for, say, 10 years on average,” he said.
Dr. Gaffo says he explores alcohol history with his patients with gout. If they are frequent drinkers, he encourages them to cut back.
“At the very least,” he said, “you have to restrict your intake to no more than 1-2 servings per week,” he said. “For some patients, even minimal amounts of alcohol intake can be associated with the development of flares.”
Still, research like this, he says, can help physicians point to evidence in their advice to patients about alcohol use.
He noted that the authors found the association between different types of alcohol and tophi was independent of serum urate level.
“That surprised me,” Dr. Gaffo said. “That’s a very unique finding.”
This work was supported by grants from the National Natural Science Foundation of China, the Natural Science Foundation of Shandong Province, Qingdao applied basic research project, National College Students’ Innovation and Entrepreneurship Training Program, and Shandong Provincial Science Foundation for Outstanding Youth Scholars.
The authors of the study and Dr. Gaffo report no relevant financial relationships.
The more years a person drinks alcohol, the kind of alcohol consumed, and the amount consumed can help to predict gout tophi, researchers say in a newly published paper in Arthritis Care and Research.
The study, led by Lin Han, PhD, of the gout laboratory, Shandong provincial clinical research center for immune diseases and gout, Affiliated Hospital of Qingdao (China) University, helps clarify the already-established relationship between alcohol consumption and gout tophi.
Additionally, the effects of drinking alcohol on ultrasound (US)–detected tophi and subcutaneous tophi (subtophi) were evaluated separately for the first time in this work, the authors say.
Tophi may be underdiagnosed because they are hard to find with only a physical exam. US can help with early detection, especially with small clusters of crystals or those found deep in the tissues, and offers good diagnostic accuracy with high specificity.
“Unlike subtophi, which represent long-term subcutaneous MSU [monosodium urate] deposition over many years, US-detected tophi represent the early stage of tophi in both intra- and extra-articular settings,” the authors write.
This cross-sectional study in China included 554 patients with gout who had joint ultrasound and physical exams through the Affiliated Hospital of Qingdao University. Physicians gathered medical histories using the Biobank Information Management System.
Physicians also tracked alcohol consumption patterns through the biobank information, which included answers to a detailed drinking questionnaire.
Patients were classified as either nondrinkers (no history of drinking; n = 141), former drinkers (n = 60), or current regular drinkers (n = 353). Current regular drinkers were asked further questions about their drinking patterns, including how long they have been drinking, type of alcohol they drink, and how much and how often they drink. In China, the average drink is considered to contain 10 g of alcohol, according to the World Health Organization.
Results from US and clinically detected tophi
Compared with nondrinkers, excessive drinkers (more than 70 g/week); long-term drinkers (at least 10 years), and spirits drinkers had a greater proportion, size, and number of US-detected tophi and subtophi (all P < .05).
After adjusting for confounders, the researchers found that excessive drinking was significantly associated with having US-detected tophi (odds ratio, 1.79) and subtophi (OR, 2.00). Similar associations were found for consumption of alcohol for at least 10 years (OR, 1.96 for US-detected tophi; OR, 2.17 for sub-tophi) and drinking spirits (OR, 1.81 for US-detected tophi; OR, 2.10 for subtophi). All comparisons were P < .05.
Among patients who already have US-detected tophi or subtophi, moderate drinking (70 g/week or less) was linked with larger or multiple tophi (all P < .05).
Angelo Gaffo, MD, section chief of rheumatology at the Birmingham VA Medical Center and associate professor of medicine in the division of rheumatology at the University of Alabama at Birmingham, said in an interview that the results are likely generalizable.
“I wouldn’t expect them to be specific to the Chinese population,” he said.
Most of the 554 patients were male (97.8%) and had no family history of gout (79.8%). The median duration of gout was 4 years, and the average age was 45.1 years.
Dr. Gaffo noted the population age was fairly young and the average duration of gout in these patients was fairly short. He also noted most had small tophi that were detected only by ultrasound and small numbers of tophi overall.
“I would like to see how these results will replicate in a population that has had gout for, say, 10 years on average,” he said.
Dr. Gaffo says he explores alcohol history with his patients with gout. If they are frequent drinkers, he encourages them to cut back.
“At the very least,” he said, “you have to restrict your intake to no more than 1-2 servings per week,” he said. “For some patients, even minimal amounts of alcohol intake can be associated with the development of flares.”
Still, research like this, he says, can help physicians point to evidence in their advice to patients about alcohol use.
He noted that the authors found the association between different types of alcohol and tophi was independent of serum urate level.
“That surprised me,” Dr. Gaffo said. “That’s a very unique finding.”
This work was supported by grants from the National Natural Science Foundation of China, the Natural Science Foundation of Shandong Province, Qingdao applied basic research project, National College Students’ Innovation and Entrepreneurship Training Program, and Shandong Provincial Science Foundation for Outstanding Youth Scholars.
The authors of the study and Dr. Gaffo report no relevant financial relationships.
FROM ARTHRITIS CARE AND RESEARCH
Methotrexate enhances pegloticase response in uncontrolled gout
In patients with uncontrolled gout, response rates were increased by 32% when methotrexate was used in conjunction with pegloticase versus pegloticase plus a placebo, it was reported at the annual European Congress of Rheumatology.
In the phase 4 MIRROR trial, 71% of patients who received pretreatment with methotrexate and then the combination of methotrexate and pegloticase achieved uric-acid levels lower than 6 mg/dL for more than 80% of the time during weeks 20-24 of the 52-week study. By comparison, only 39% of those treated with pegloticase plus a placebo achieved this primary endpoint (P < .0001).
“This trial confirms not only improved efficacy but improved safety in patients treated with pegloticase in combination with methotrexate 15 mg orally once weekly,” study investigator John K. Botson, MD, RPh, CCD, said in reporting the trial’s findings.
This is good news for patients, suggested two rheumatologists who were not involved in the study. The combination appears “useful for a select group of gout patients,” observed Christian Ammitzbøll, MD, PhD, from Aarhus University Hospital, Denmark.
“Very promising in refractory gout,” agreed Emre Bilgin, MD, from Ankara, Turkey.
Rationale for using methotrexate
“Oral urate lowering agents are the mainstay of treatment of gout, but there are patients that just don’t respond to oral agents,” said Dr. Botson, a rheumatologist in private practice from Anchorage, Alaska.
“These patients are very difficult to treat,” he added. “They have a lot of physical disabilities, they have high medical comorbidities, and they have a low quality of life. Their treatment options are extremely limited.”
One of the few options they have is pegloticase, a pegylated uric acid specific enzyme sold under the brand name Krystexxa for the past 12 years. It lowers serum uric acid by converting it to allantoin, which is more water soluble and thus is easier to excrete from the body.
However, one of the problems of using the drug is that anti-drug antibodies frequently develop, meaning that discontinuation rates can be as high as 50%, with around a quarter of patients at high risk of experiencing an infusion reaction.
“Methotrexate is a medication we’re very familiar with for other rheumatologic conditions that use biologic medications, and we use this to prevent anti-drug antibodies. So, the MIRROR RCT was a study we performed to examine the pegloticase therapy in combination with methotrexate co therapy,” explained Dr. Botson.
In fact, co-administration of methotrexate and pegloticase was associated with fewer infusion reactions than using pegloticase alone (3% vs. 31%).
Study design and results
A total of 152 patients were included in the trial and were treated with methotrexate at a weekly dose of 15 mg for 2 weeks before being randomized, 2:1, to either continue methotrexate and then receive intravenous pegloticase or receive the latter with a placebo. Pegloticase was given at a dose of 8 mg every 2 weeks. Treatment was for 52 weeks, with the primary endpoint of serum uric acid response tested at 6 months.
The reason for the 2-week run-in period with methotrexate was to check that patients would be able to tolerate it, Dr. Botson explained.
The mean age of patients was around 54 years, the majority (> 84%) were male and were White (69%). The average duration of gout was about 14 years, with over 74% having tophi present at screening and experiencing 10-11 flares in the previous year. Baseline serum uric acid averaged at about 9 mg/dL.
Almost three-quarters of the 100 patients (73%) who were treated with the combination completed treatment to week 24 while the corresponding percentage in the placebo arm (n = 52) was 39%. The main reason for stopping was due to lack of efficacy (27% and 61% of cases, respectively), defined as having serum uric acid levels above 6 mg/dL on two consecutive measurements.
The median time to discontinuation was 69 days for those in the placebo arm; “it was non-estimable” in the methotrexate arm, Dr. Botson reported.
The mean change in serum uric acid through to week 24 was higher in the methotrexate than placebo arm, at a respective 7.66 and 5.23 mg/dL, giving a significant mean difference of 2.43 mg/dL.
There was a “dramatic resolution of tophaceous deposits,” Dr. Botson said. Complete resolution of tophi was seen in 34.6% of methotrexate-treated patients versus 13.8% of pegloticase-placebo–treated patients (P = .043).
One of the most common adverse events associated with pegloticase treatment is gout flare, which occurred in about 70% of participants in both study arms. Overall, the addition of methotrexate did not increase the risk for adverse events in general, and of the two deaths seen in the study – both in methotrexate-treated patients – one was because of a heart attack and another due COVID-19, so they were unrelated to study treatment.
In patients with renal insufficiency
Concern was raised during the discussion, however, on how to handle methotrexate use in patients with renal insufficiency.
“That’s been a debate that we’ve had in this study and others,” said Dr. Botson, acknowledging that “methotrexate is often a concern for the nephrologist that we’re co-treating these patients with.” However, no dose adjustments were needed in the study.
“There are some other studies with other immunomodulators that do suggest that other agents could be used that may be a little less potentially renal toxic, but we didn’t see any toxicity in the patients that we had, even in those that had a reduced [glomerular filtration rate],” he added.
Dr. Botson has received research support from Horizon and Radius Health. He also acknowledged receiving speakers fees from AbbVie, Amgen, Aurinia, ChemoCentryx*, Horizon, Eli Lilly, and Novartis.
Correction, 6/7/22: The name of the company ChemoCentryx was misstated.
In patients with uncontrolled gout, response rates were increased by 32% when methotrexate was used in conjunction with pegloticase versus pegloticase plus a placebo, it was reported at the annual European Congress of Rheumatology.
In the phase 4 MIRROR trial, 71% of patients who received pretreatment with methotrexate and then the combination of methotrexate and pegloticase achieved uric-acid levels lower than 6 mg/dL for more than 80% of the time during weeks 20-24 of the 52-week study. By comparison, only 39% of those treated with pegloticase plus a placebo achieved this primary endpoint (P < .0001).
“This trial confirms not only improved efficacy but improved safety in patients treated with pegloticase in combination with methotrexate 15 mg orally once weekly,” study investigator John K. Botson, MD, RPh, CCD, said in reporting the trial’s findings.
This is good news for patients, suggested two rheumatologists who were not involved in the study. The combination appears “useful for a select group of gout patients,” observed Christian Ammitzbøll, MD, PhD, from Aarhus University Hospital, Denmark.
“Very promising in refractory gout,” agreed Emre Bilgin, MD, from Ankara, Turkey.
Rationale for using methotrexate
“Oral urate lowering agents are the mainstay of treatment of gout, but there are patients that just don’t respond to oral agents,” said Dr. Botson, a rheumatologist in private practice from Anchorage, Alaska.
“These patients are very difficult to treat,” he added. “They have a lot of physical disabilities, they have high medical comorbidities, and they have a low quality of life. Their treatment options are extremely limited.”
One of the few options they have is pegloticase, a pegylated uric acid specific enzyme sold under the brand name Krystexxa for the past 12 years. It lowers serum uric acid by converting it to allantoin, which is more water soluble and thus is easier to excrete from the body.
However, one of the problems of using the drug is that anti-drug antibodies frequently develop, meaning that discontinuation rates can be as high as 50%, with around a quarter of patients at high risk of experiencing an infusion reaction.
“Methotrexate is a medication we’re very familiar with for other rheumatologic conditions that use biologic medications, and we use this to prevent anti-drug antibodies. So, the MIRROR RCT was a study we performed to examine the pegloticase therapy in combination with methotrexate co therapy,” explained Dr. Botson.
In fact, co-administration of methotrexate and pegloticase was associated with fewer infusion reactions than using pegloticase alone (3% vs. 31%).
Study design and results
A total of 152 patients were included in the trial and were treated with methotrexate at a weekly dose of 15 mg for 2 weeks before being randomized, 2:1, to either continue methotrexate and then receive intravenous pegloticase or receive the latter with a placebo. Pegloticase was given at a dose of 8 mg every 2 weeks. Treatment was for 52 weeks, with the primary endpoint of serum uric acid response tested at 6 months.
The reason for the 2-week run-in period with methotrexate was to check that patients would be able to tolerate it, Dr. Botson explained.
The mean age of patients was around 54 years, the majority (> 84%) were male and were White (69%). The average duration of gout was about 14 years, with over 74% having tophi present at screening and experiencing 10-11 flares in the previous year. Baseline serum uric acid averaged at about 9 mg/dL.
Almost three-quarters of the 100 patients (73%) who were treated with the combination completed treatment to week 24 while the corresponding percentage in the placebo arm (n = 52) was 39%. The main reason for stopping was due to lack of efficacy (27% and 61% of cases, respectively), defined as having serum uric acid levels above 6 mg/dL on two consecutive measurements.
The median time to discontinuation was 69 days for those in the placebo arm; “it was non-estimable” in the methotrexate arm, Dr. Botson reported.
The mean change in serum uric acid through to week 24 was higher in the methotrexate than placebo arm, at a respective 7.66 and 5.23 mg/dL, giving a significant mean difference of 2.43 mg/dL.
There was a “dramatic resolution of tophaceous deposits,” Dr. Botson said. Complete resolution of tophi was seen in 34.6% of methotrexate-treated patients versus 13.8% of pegloticase-placebo–treated patients (P = .043).
One of the most common adverse events associated with pegloticase treatment is gout flare, which occurred in about 70% of participants in both study arms. Overall, the addition of methotrexate did not increase the risk for adverse events in general, and of the two deaths seen in the study – both in methotrexate-treated patients – one was because of a heart attack and another due COVID-19, so they were unrelated to study treatment.
In patients with renal insufficiency
Concern was raised during the discussion, however, on how to handle methotrexate use in patients with renal insufficiency.
“That’s been a debate that we’ve had in this study and others,” said Dr. Botson, acknowledging that “methotrexate is often a concern for the nephrologist that we’re co-treating these patients with.” However, no dose adjustments were needed in the study.
“There are some other studies with other immunomodulators that do suggest that other agents could be used that may be a little less potentially renal toxic, but we didn’t see any toxicity in the patients that we had, even in those that had a reduced [glomerular filtration rate],” he added.
Dr. Botson has received research support from Horizon and Radius Health. He also acknowledged receiving speakers fees from AbbVie, Amgen, Aurinia, ChemoCentryx*, Horizon, Eli Lilly, and Novartis.
Correction, 6/7/22: The name of the company ChemoCentryx was misstated.
In patients with uncontrolled gout, response rates were increased by 32% when methotrexate was used in conjunction with pegloticase versus pegloticase plus a placebo, it was reported at the annual European Congress of Rheumatology.
In the phase 4 MIRROR trial, 71% of patients who received pretreatment with methotrexate and then the combination of methotrexate and pegloticase achieved uric-acid levels lower than 6 mg/dL for more than 80% of the time during weeks 20-24 of the 52-week study. By comparison, only 39% of those treated with pegloticase plus a placebo achieved this primary endpoint (P < .0001).
“This trial confirms not only improved efficacy but improved safety in patients treated with pegloticase in combination with methotrexate 15 mg orally once weekly,” study investigator John K. Botson, MD, RPh, CCD, said in reporting the trial’s findings.
This is good news for patients, suggested two rheumatologists who were not involved in the study. The combination appears “useful for a select group of gout patients,” observed Christian Ammitzbøll, MD, PhD, from Aarhus University Hospital, Denmark.
“Very promising in refractory gout,” agreed Emre Bilgin, MD, from Ankara, Turkey.
Rationale for using methotrexate
“Oral urate lowering agents are the mainstay of treatment of gout, but there are patients that just don’t respond to oral agents,” said Dr. Botson, a rheumatologist in private practice from Anchorage, Alaska.
“These patients are very difficult to treat,” he added. “They have a lot of physical disabilities, they have high medical comorbidities, and they have a low quality of life. Their treatment options are extremely limited.”
One of the few options they have is pegloticase, a pegylated uric acid specific enzyme sold under the brand name Krystexxa for the past 12 years. It lowers serum uric acid by converting it to allantoin, which is more water soluble and thus is easier to excrete from the body.
However, one of the problems of using the drug is that anti-drug antibodies frequently develop, meaning that discontinuation rates can be as high as 50%, with around a quarter of patients at high risk of experiencing an infusion reaction.
“Methotrexate is a medication we’re very familiar with for other rheumatologic conditions that use biologic medications, and we use this to prevent anti-drug antibodies. So, the MIRROR RCT was a study we performed to examine the pegloticase therapy in combination with methotrexate co therapy,” explained Dr. Botson.
In fact, co-administration of methotrexate and pegloticase was associated with fewer infusion reactions than using pegloticase alone (3% vs. 31%).
Study design and results
A total of 152 patients were included in the trial and were treated with methotrexate at a weekly dose of 15 mg for 2 weeks before being randomized, 2:1, to either continue methotrexate and then receive intravenous pegloticase or receive the latter with a placebo. Pegloticase was given at a dose of 8 mg every 2 weeks. Treatment was for 52 weeks, with the primary endpoint of serum uric acid response tested at 6 months.
The reason for the 2-week run-in period with methotrexate was to check that patients would be able to tolerate it, Dr. Botson explained.
The mean age of patients was around 54 years, the majority (> 84%) were male and were White (69%). The average duration of gout was about 14 years, with over 74% having tophi present at screening and experiencing 10-11 flares in the previous year. Baseline serum uric acid averaged at about 9 mg/dL.
Almost three-quarters of the 100 patients (73%) who were treated with the combination completed treatment to week 24 while the corresponding percentage in the placebo arm (n = 52) was 39%. The main reason for stopping was due to lack of efficacy (27% and 61% of cases, respectively), defined as having serum uric acid levels above 6 mg/dL on two consecutive measurements.
The median time to discontinuation was 69 days for those in the placebo arm; “it was non-estimable” in the methotrexate arm, Dr. Botson reported.
The mean change in serum uric acid through to week 24 was higher in the methotrexate than placebo arm, at a respective 7.66 and 5.23 mg/dL, giving a significant mean difference of 2.43 mg/dL.
There was a “dramatic resolution of tophaceous deposits,” Dr. Botson said. Complete resolution of tophi was seen in 34.6% of methotrexate-treated patients versus 13.8% of pegloticase-placebo–treated patients (P = .043).
One of the most common adverse events associated with pegloticase treatment is gout flare, which occurred in about 70% of participants in both study arms. Overall, the addition of methotrexate did not increase the risk for adverse events in general, and of the two deaths seen in the study – both in methotrexate-treated patients – one was because of a heart attack and another due COVID-19, so they were unrelated to study treatment.
In patients with renal insufficiency
Concern was raised during the discussion, however, on how to handle methotrexate use in patients with renal insufficiency.
“That’s been a debate that we’ve had in this study and others,” said Dr. Botson, acknowledging that “methotrexate is often a concern for the nephrologist that we’re co-treating these patients with.” However, no dose adjustments were needed in the study.
“There are some other studies with other immunomodulators that do suggest that other agents could be used that may be a little less potentially renal toxic, but we didn’t see any toxicity in the patients that we had, even in those that had a reduced [glomerular filtration rate],” he added.
Dr. Botson has received research support from Horizon and Radius Health. He also acknowledged receiving speakers fees from AbbVie, Amgen, Aurinia, ChemoCentryx*, Horizon, Eli Lilly, and Novartis.
Correction, 6/7/22: The name of the company ChemoCentryx was misstated.
FROM THE EULAR 2022 CONGRESS
Gout app improves treat to target, reduces flares
Self-management of gout using a smartphone app to record self-test urate levels and flares, and communicate those results to clinicians, could see more patients reaching target urate levels and even reducing flare frequency, a study has found.
Writing in The Lancet Rheumatology, Philip Riches, PhD, of the rheumatic disease unit at Western General Hospital in Edinburgh, and coauthors presented the findings of their randomized, controlled feasibility study of a new gout self-management approach aimed at helping patients treat to target.
While current rheumatology guidelines stress the importance of keeping urate below target levels to reduce flares and improve clinical outcomes, this isn’t always achieved in clinical practice. A previous trial of a nurse-led treat-to-target intervention did show a reduced incidence of flares and tophaceous disease, but the authors said, despite its cost-effectiveness, this approach has yet to be implemented in the United Kingdom.
Dr. Riches and colleagues developed a self-management strategy in which all 60 patients in the study self-tested their urate levels and were prompted to enter that data into the GoutSMART smartphone app once a month or opportunistically, along with information on disease severity and quality of life. All patients had been recommended for initiation or escalation of urate-lowering therapy, and had a serum urate of 0.36 mmol/L (6 mg/dL) or higher at baseline, and all received a gout management plan at the start of the study.
Patients in the intervention group who recorded a urate level above 0.30 mmol/L (5 mg/dL) via the app during the study were prompted to do a self-test every 2 weeks and given daily reminders in the app. Their urate levels were transmitted securely to the study team who then advised on dose escalation or treatment change. Those in the usual-care group also used the app but it only prompted them to record gout flares, keep quality of life diaries, or message the researchers.
At 24 weeks after the start of the study, 73% of 40 participants in the self-management group had reached the urate target of 0.30 mmol/L or below, compared with 15% of the 20 participants in the usual-care group (P < .0001).
The difference between the two groups was sustained even 1 year after starting the intervention, when 80% of those in the self-management group had reached that target, compared with 45% of those in the usual-care group.
Patients in the intervention group also had fewer flares, experiencing a mean of 2.03 flares in the first 24 weeks, compared with a mean of 3 among the control group, although the study didn’t report any difference in the rates of tophaceous disease.
Those in the self-management group had fewer medical appointments, but were prescribed higher doses of allopurinol at the 24- and 52-week visits.
“Qualitative feedback suggests that the self-monitoring approach was accepted by most participants and was enthusiastically endorsed by many,” the authors wrote. “The approach empowers patients and provides feedback on the effect of medication.”
It will be important to determine if the success of this self-management intervention can be replicated in an even broader patient population, Lisa K. Stamp, MBChB, PhD, of University of Otago, Christchurch, New Zealand, and Angelo L. Gaffo, MD, of University of Alabama at Birmingham, noted in an accompanying editorial. They wrote it was encouraging that only 7% of the 92 people screened for the trial did not have a smartphone and that it the patient sample had a mean age of 53 years. However, the trial did not include people with chronic kidney disease who make up nearly a quarter of all people with gout.
“It remains unknown whether the characteristics of those who did not reach target urate are the same or different as those who did, and a head-to-head comparison of these interventions would be of interest,” Dr. Stamp and Dr. Gaffo wrote. “A key challenge in managing gout is to determine which treatment strategy will be best suited to an individual with gout and to identify those for whom more support might be required.”
This study was supported by the University of Edinburgh and funded by NHS Lothian Health Foundation. No conflicts of interest were declared.
Self-management of gout using a smartphone app to record self-test urate levels and flares, and communicate those results to clinicians, could see more patients reaching target urate levels and even reducing flare frequency, a study has found.
Writing in The Lancet Rheumatology, Philip Riches, PhD, of the rheumatic disease unit at Western General Hospital in Edinburgh, and coauthors presented the findings of their randomized, controlled feasibility study of a new gout self-management approach aimed at helping patients treat to target.
While current rheumatology guidelines stress the importance of keeping urate below target levels to reduce flares and improve clinical outcomes, this isn’t always achieved in clinical practice. A previous trial of a nurse-led treat-to-target intervention did show a reduced incidence of flares and tophaceous disease, but the authors said, despite its cost-effectiveness, this approach has yet to be implemented in the United Kingdom.
Dr. Riches and colleagues developed a self-management strategy in which all 60 patients in the study self-tested their urate levels and were prompted to enter that data into the GoutSMART smartphone app once a month or opportunistically, along with information on disease severity and quality of life. All patients had been recommended for initiation or escalation of urate-lowering therapy, and had a serum urate of 0.36 mmol/L (6 mg/dL) or higher at baseline, and all received a gout management plan at the start of the study.
Patients in the intervention group who recorded a urate level above 0.30 mmol/L (5 mg/dL) via the app during the study were prompted to do a self-test every 2 weeks and given daily reminders in the app. Their urate levels were transmitted securely to the study team who then advised on dose escalation or treatment change. Those in the usual-care group also used the app but it only prompted them to record gout flares, keep quality of life diaries, or message the researchers.
At 24 weeks after the start of the study, 73% of 40 participants in the self-management group had reached the urate target of 0.30 mmol/L or below, compared with 15% of the 20 participants in the usual-care group (P < .0001).
The difference between the two groups was sustained even 1 year after starting the intervention, when 80% of those in the self-management group had reached that target, compared with 45% of those in the usual-care group.
Patients in the intervention group also had fewer flares, experiencing a mean of 2.03 flares in the first 24 weeks, compared with a mean of 3 among the control group, although the study didn’t report any difference in the rates of tophaceous disease.
Those in the self-management group had fewer medical appointments, but were prescribed higher doses of allopurinol at the 24- and 52-week visits.
“Qualitative feedback suggests that the self-monitoring approach was accepted by most participants and was enthusiastically endorsed by many,” the authors wrote. “The approach empowers patients and provides feedback on the effect of medication.”
It will be important to determine if the success of this self-management intervention can be replicated in an even broader patient population, Lisa K. Stamp, MBChB, PhD, of University of Otago, Christchurch, New Zealand, and Angelo L. Gaffo, MD, of University of Alabama at Birmingham, noted in an accompanying editorial. They wrote it was encouraging that only 7% of the 92 people screened for the trial did not have a smartphone and that it the patient sample had a mean age of 53 years. However, the trial did not include people with chronic kidney disease who make up nearly a quarter of all people with gout.
“It remains unknown whether the characteristics of those who did not reach target urate are the same or different as those who did, and a head-to-head comparison of these interventions would be of interest,” Dr. Stamp and Dr. Gaffo wrote. “A key challenge in managing gout is to determine which treatment strategy will be best suited to an individual with gout and to identify those for whom more support might be required.”
This study was supported by the University of Edinburgh and funded by NHS Lothian Health Foundation. No conflicts of interest were declared.
Self-management of gout using a smartphone app to record self-test urate levels and flares, and communicate those results to clinicians, could see more patients reaching target urate levels and even reducing flare frequency, a study has found.
Writing in The Lancet Rheumatology, Philip Riches, PhD, of the rheumatic disease unit at Western General Hospital in Edinburgh, and coauthors presented the findings of their randomized, controlled feasibility study of a new gout self-management approach aimed at helping patients treat to target.
While current rheumatology guidelines stress the importance of keeping urate below target levels to reduce flares and improve clinical outcomes, this isn’t always achieved in clinical practice. A previous trial of a nurse-led treat-to-target intervention did show a reduced incidence of flares and tophaceous disease, but the authors said, despite its cost-effectiveness, this approach has yet to be implemented in the United Kingdom.
Dr. Riches and colleagues developed a self-management strategy in which all 60 patients in the study self-tested their urate levels and were prompted to enter that data into the GoutSMART smartphone app once a month or opportunistically, along with information on disease severity and quality of life. All patients had been recommended for initiation or escalation of urate-lowering therapy, and had a serum urate of 0.36 mmol/L (6 mg/dL) or higher at baseline, and all received a gout management plan at the start of the study.
Patients in the intervention group who recorded a urate level above 0.30 mmol/L (5 mg/dL) via the app during the study were prompted to do a self-test every 2 weeks and given daily reminders in the app. Their urate levels were transmitted securely to the study team who then advised on dose escalation or treatment change. Those in the usual-care group also used the app but it only prompted them to record gout flares, keep quality of life diaries, or message the researchers.
At 24 weeks after the start of the study, 73% of 40 participants in the self-management group had reached the urate target of 0.30 mmol/L or below, compared with 15% of the 20 participants in the usual-care group (P < .0001).
The difference between the two groups was sustained even 1 year after starting the intervention, when 80% of those in the self-management group had reached that target, compared with 45% of those in the usual-care group.
Patients in the intervention group also had fewer flares, experiencing a mean of 2.03 flares in the first 24 weeks, compared with a mean of 3 among the control group, although the study didn’t report any difference in the rates of tophaceous disease.
Those in the self-management group had fewer medical appointments, but were prescribed higher doses of allopurinol at the 24- and 52-week visits.
“Qualitative feedback suggests that the self-monitoring approach was accepted by most participants and was enthusiastically endorsed by many,” the authors wrote. “The approach empowers patients and provides feedback on the effect of medication.”
It will be important to determine if the success of this self-management intervention can be replicated in an even broader patient population, Lisa K. Stamp, MBChB, PhD, of University of Otago, Christchurch, New Zealand, and Angelo L. Gaffo, MD, of University of Alabama at Birmingham, noted in an accompanying editorial. They wrote it was encouraging that only 7% of the 92 people screened for the trial did not have a smartphone and that it the patient sample had a mean age of 53 years. However, the trial did not include people with chronic kidney disease who make up nearly a quarter of all people with gout.
“It remains unknown whether the characteristics of those who did not reach target urate are the same or different as those who did, and a head-to-head comparison of these interventions would be of interest,” Dr. Stamp and Dr. Gaffo wrote. “A key challenge in managing gout is to determine which treatment strategy will be best suited to an individual with gout and to identify those for whom more support might be required.”
This study was supported by the University of Edinburgh and funded by NHS Lothian Health Foundation. No conflicts of interest were declared.
FROM THE LANCET RHEUMATOLOGY
EULAR CVD management guidance focuses on gout, lupus, vasculitis
New recommendations from the European Alliance of Associations for Rheumatology provide both broad and detailed advice for cardiovascular risk management in various rheumatic and musculoskeletal diseases (RMDs), many of which can lead to an increased possibility of cardiovascular disease (CVD).
“The panel believes that these recommendations will enable health care providers and patients to mutually engage in a long-term care pathway tailored to patients’ needs and expectations for improving cardiovascular health in RMDs,” write George C. Drosos, National and Kapodistrian University of Athens, and colleagues. The recommendations were published in February in Annals of the Rheumatic Diseases).
EULAR assembled a task force to generate best practices for preventing CVD in patients with gout, vasculitis, systemic sclerosis (SSc), myositis, mixed connective tissue disease (MCTD), Sjögren syndrome (SS), systemic lupus erythematosus (SLE), and antiphospholipid syndrome (APS).
The cardiovascular risk management of patients with rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis was covered in prior EULAR recommendations.
The task force included 20 members from 11 European countries, including 12 rheumatologists, 2 cardiologists, 1 metabolic medicine physician, 1 health care professional, 2 patient representatives, and 2 EMEUNET (Emerging EULAR Network) members. One group of task force members conducted a systematic literature review of 105 articles about gout, vasculitis, SSc, myositis, MCTD, and SS, and another group evaluated 75 articles about SLE and APS. Together, they decided on four overarching principles:
Clinicians need to be aware of increased cardiovascular risk in patients with RMDs, with disease reduction likely decreasing risk.
Rheumatologists – in tandem with other health care providers – are responsible for their patients’ cardiovascular risk assessment and management.
Screening for cardiovascular risk should be performed regularly in all patients with RMDs, with an emphasis on factors like smoking and blood pressure management.
Patient education and counseling on cardiovascular risk, including important lifestyle modifications, is key for RMD patients.
Specific recommendations from the gout, vasculitis, SSc, myositis, MCTD, and SS group include deploying existing cardiovascular prediction tools as they are used in the general population, with the European Vasculitis Society model suggesting to supplement the Framingham Risk Score for patients with antineutrophil cytoplasmic antibody–associated vasculitis. They also recommended avoiding diuretics in patients with gout and beta-blockers in patients with SSc, as well as following the same blood pressure and lipid management strategies that are used among the general population.
Recommendations from the SLE and APS group include thoroughly assessing traditional cardiovascular risk factors in all patients, following typical blood pressure management strategies in patients with APS, and setting a blood pressure target of less than 130/80 mm Hg in patients with SLE. They also recommended administering the lowest possible glucocorticoid dose in patients with SLE, along with treatment with hydroxychloroquine – unless contraindicated – and even common preventive strategies like low-dose aspirin if it suits their cardiovascular risk profile.
As for next steps, the task force noted several areas where additional focus is needed, such as identifying patient subgroups with increased cardiovascular risk. This could include patients with a longer disease duration or more flare-ups, older patients, and those with certain disease characteristics like antiphospholipid positivity in SLE.
Can EULAR’s recommendations be implemented in U.S. rheumatology practices?
“We have been hearing for years that patients with rheumatic diseases have an increased risk of cardiovascular disease,” Ali A. Duarte Garcia, MD, a rheumatologist at the Mayo Clinic in Rochester, Minn., told this news organization. “That has been consistently published for more than a decade now. But any further guidance about it has not been issued. I think there was a void there.”
“Certainly, cardiovascular disease risk in rheumatoid and psoriatic arthritis has been front of mind for the last decade or so,” Christie M. Bartels, MD, chief of the division of rheumatology at the University of Wisconsin, Madison, said when asked to comment on the recommendations. “But in some of these other conditions, it hasn’t been.”
When asked if rheumatologists would be ready and willing to implement these recommendations, Dr. Duarte Garcia acknowledged that it could be challenging for some.
“It’s a different workflow,” he said. “You’ve been trained traditionally to assess inflammation, to keep the disease under control, which is something they recommend, by the way. If you control the disease, patients do better. But I think lipid screening, for example, and testing for cholesterol, smoking cessation, those well-established programs are harder to bring to a rheumatology clinic. It’s doable, but it’s something that needs to be implemented within the current workflows and could take a few years to take hold.”
Dr. Bartels, however, noted that her group has done extensive work over the last 5 years incorporating certain interventions into practice, including sending patients with high blood pressure back to primary care.
“It’s a sustainable intervention in our clinic that basically our medical assistants and nurses do as a routine operation,” she said. “Our primary care providers are grateful to get these patients back. Our patients are grateful because otherwise when they come to the rheumatologist, get their blood pressure measured, and don’t get feedback, they assume they’re OK. So, we’re giving them a false signal.
“We have a similar intervention with smoking,” she added. “Often our patients aren’t even aware that they’re at increased risk of cardiovascular disease or that smoking might make their rheumatic disease and their cardiovascular outcomes worse. No one has had that conversation with them. They really welcome engaging in those discussions.
“Our tobacco intervention takes 90 seconds at point of care. Our blood pressure intervention at point of care, we’ve timed it, takes 3 minutes. There are ways that we can hardwire this into care.”
Along those lines, Dr. Duarte Garcia stated that the recommendations – although released by EULAR – are largely intuitive and should be very adaptable to an American health care context. He also recognized this moment as an opportunity for rheumatologists to consider patient outcomes beyond what they usually encounter firsthand.
“I don’t think we have many rheumatologists with patients who get a stroke or heart attack because if that happens, it’s in a hospital context or they go see a cardiologist,” he said. “You may see it once it happens if they survive and come and see you – or perhaps if you’re in a more integrated practice – but I don’t think it’s as apparent in our clinics because it is a predominantly outpatient practice and many times those are emergencies or inpatient complications.
“The bottom line,” he added, “is these are practical guidelines. It’s a push in the right direction, but there is still work to be done. And hopefully some of the recommendations, like measuring high blood pressure and addressing it just as in the general population, are something we can start to implement.”
Dr. Duarte Garcia reported receiving grant funding from the Rheumatology Research Foundation and the Centers for Disease Control and Prevention. Dr. Bartels reported that her group’s tobacco cessation work is funded by Pfizer’s Independent Grants for Learning and Change.
A version of this article first appeared on Medscape.com.
New recommendations from the European Alliance of Associations for Rheumatology provide both broad and detailed advice for cardiovascular risk management in various rheumatic and musculoskeletal diseases (RMDs), many of which can lead to an increased possibility of cardiovascular disease (CVD).
“The panel believes that these recommendations will enable health care providers and patients to mutually engage in a long-term care pathway tailored to patients’ needs and expectations for improving cardiovascular health in RMDs,” write George C. Drosos, National and Kapodistrian University of Athens, and colleagues. The recommendations were published in February in Annals of the Rheumatic Diseases).
EULAR assembled a task force to generate best practices for preventing CVD in patients with gout, vasculitis, systemic sclerosis (SSc), myositis, mixed connective tissue disease (MCTD), Sjögren syndrome (SS), systemic lupus erythematosus (SLE), and antiphospholipid syndrome (APS).
The cardiovascular risk management of patients with rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis was covered in prior EULAR recommendations.
The task force included 20 members from 11 European countries, including 12 rheumatologists, 2 cardiologists, 1 metabolic medicine physician, 1 health care professional, 2 patient representatives, and 2 EMEUNET (Emerging EULAR Network) members. One group of task force members conducted a systematic literature review of 105 articles about gout, vasculitis, SSc, myositis, MCTD, and SS, and another group evaluated 75 articles about SLE and APS. Together, they decided on four overarching principles:
Clinicians need to be aware of increased cardiovascular risk in patients with RMDs, with disease reduction likely decreasing risk.
Rheumatologists – in tandem with other health care providers – are responsible for their patients’ cardiovascular risk assessment and management.
Screening for cardiovascular risk should be performed regularly in all patients with RMDs, with an emphasis on factors like smoking and blood pressure management.
Patient education and counseling on cardiovascular risk, including important lifestyle modifications, is key for RMD patients.
Specific recommendations from the gout, vasculitis, SSc, myositis, MCTD, and SS group include deploying existing cardiovascular prediction tools as they are used in the general population, with the European Vasculitis Society model suggesting to supplement the Framingham Risk Score for patients with antineutrophil cytoplasmic antibody–associated vasculitis. They also recommended avoiding diuretics in patients with gout and beta-blockers in patients with SSc, as well as following the same blood pressure and lipid management strategies that are used among the general population.
Recommendations from the SLE and APS group include thoroughly assessing traditional cardiovascular risk factors in all patients, following typical blood pressure management strategies in patients with APS, and setting a blood pressure target of less than 130/80 mm Hg in patients with SLE. They also recommended administering the lowest possible glucocorticoid dose in patients with SLE, along with treatment with hydroxychloroquine – unless contraindicated – and even common preventive strategies like low-dose aspirin if it suits their cardiovascular risk profile.
As for next steps, the task force noted several areas where additional focus is needed, such as identifying patient subgroups with increased cardiovascular risk. This could include patients with a longer disease duration or more flare-ups, older patients, and those with certain disease characteristics like antiphospholipid positivity in SLE.
Can EULAR’s recommendations be implemented in U.S. rheumatology practices?
“We have been hearing for years that patients with rheumatic diseases have an increased risk of cardiovascular disease,” Ali A. Duarte Garcia, MD, a rheumatologist at the Mayo Clinic in Rochester, Minn., told this news organization. “That has been consistently published for more than a decade now. But any further guidance about it has not been issued. I think there was a void there.”
“Certainly, cardiovascular disease risk in rheumatoid and psoriatic arthritis has been front of mind for the last decade or so,” Christie M. Bartels, MD, chief of the division of rheumatology at the University of Wisconsin, Madison, said when asked to comment on the recommendations. “But in some of these other conditions, it hasn’t been.”
When asked if rheumatologists would be ready and willing to implement these recommendations, Dr. Duarte Garcia acknowledged that it could be challenging for some.
“It’s a different workflow,” he said. “You’ve been trained traditionally to assess inflammation, to keep the disease under control, which is something they recommend, by the way. If you control the disease, patients do better. But I think lipid screening, for example, and testing for cholesterol, smoking cessation, those well-established programs are harder to bring to a rheumatology clinic. It’s doable, but it’s something that needs to be implemented within the current workflows and could take a few years to take hold.”
Dr. Bartels, however, noted that her group has done extensive work over the last 5 years incorporating certain interventions into practice, including sending patients with high blood pressure back to primary care.
“It’s a sustainable intervention in our clinic that basically our medical assistants and nurses do as a routine operation,” she said. “Our primary care providers are grateful to get these patients back. Our patients are grateful because otherwise when they come to the rheumatologist, get their blood pressure measured, and don’t get feedback, they assume they’re OK. So, we’re giving them a false signal.
“We have a similar intervention with smoking,” she added. “Often our patients aren’t even aware that they’re at increased risk of cardiovascular disease or that smoking might make their rheumatic disease and their cardiovascular outcomes worse. No one has had that conversation with them. They really welcome engaging in those discussions.
“Our tobacco intervention takes 90 seconds at point of care. Our blood pressure intervention at point of care, we’ve timed it, takes 3 minutes. There are ways that we can hardwire this into care.”
Along those lines, Dr. Duarte Garcia stated that the recommendations – although released by EULAR – are largely intuitive and should be very adaptable to an American health care context. He also recognized this moment as an opportunity for rheumatologists to consider patient outcomes beyond what they usually encounter firsthand.
“I don’t think we have many rheumatologists with patients who get a stroke or heart attack because if that happens, it’s in a hospital context or they go see a cardiologist,” he said. “You may see it once it happens if they survive and come and see you – or perhaps if you’re in a more integrated practice – but I don’t think it’s as apparent in our clinics because it is a predominantly outpatient practice and many times those are emergencies or inpatient complications.
“The bottom line,” he added, “is these are practical guidelines. It’s a push in the right direction, but there is still work to be done. And hopefully some of the recommendations, like measuring high blood pressure and addressing it just as in the general population, are something we can start to implement.”
Dr. Duarte Garcia reported receiving grant funding from the Rheumatology Research Foundation and the Centers for Disease Control and Prevention. Dr. Bartels reported that her group’s tobacco cessation work is funded by Pfizer’s Independent Grants for Learning and Change.
A version of this article first appeared on Medscape.com.
New recommendations from the European Alliance of Associations for Rheumatology provide both broad and detailed advice for cardiovascular risk management in various rheumatic and musculoskeletal diseases (RMDs), many of which can lead to an increased possibility of cardiovascular disease (CVD).
“The panel believes that these recommendations will enable health care providers and patients to mutually engage in a long-term care pathway tailored to patients’ needs and expectations for improving cardiovascular health in RMDs,” write George C. Drosos, National and Kapodistrian University of Athens, and colleagues. The recommendations were published in February in Annals of the Rheumatic Diseases).
EULAR assembled a task force to generate best practices for preventing CVD in patients with gout, vasculitis, systemic sclerosis (SSc), myositis, mixed connective tissue disease (MCTD), Sjögren syndrome (SS), systemic lupus erythematosus (SLE), and antiphospholipid syndrome (APS).
The cardiovascular risk management of patients with rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis was covered in prior EULAR recommendations.
The task force included 20 members from 11 European countries, including 12 rheumatologists, 2 cardiologists, 1 metabolic medicine physician, 1 health care professional, 2 patient representatives, and 2 EMEUNET (Emerging EULAR Network) members. One group of task force members conducted a systematic literature review of 105 articles about gout, vasculitis, SSc, myositis, MCTD, and SS, and another group evaluated 75 articles about SLE and APS. Together, they decided on four overarching principles:
Clinicians need to be aware of increased cardiovascular risk in patients with RMDs, with disease reduction likely decreasing risk.
Rheumatologists – in tandem with other health care providers – are responsible for their patients’ cardiovascular risk assessment and management.
Screening for cardiovascular risk should be performed regularly in all patients with RMDs, with an emphasis on factors like smoking and blood pressure management.
Patient education and counseling on cardiovascular risk, including important lifestyle modifications, is key for RMD patients.
Specific recommendations from the gout, vasculitis, SSc, myositis, MCTD, and SS group include deploying existing cardiovascular prediction tools as they are used in the general population, with the European Vasculitis Society model suggesting to supplement the Framingham Risk Score for patients with antineutrophil cytoplasmic antibody–associated vasculitis. They also recommended avoiding diuretics in patients with gout and beta-blockers in patients with SSc, as well as following the same blood pressure and lipid management strategies that are used among the general population.
Recommendations from the SLE and APS group include thoroughly assessing traditional cardiovascular risk factors in all patients, following typical blood pressure management strategies in patients with APS, and setting a blood pressure target of less than 130/80 mm Hg in patients with SLE. They also recommended administering the lowest possible glucocorticoid dose in patients with SLE, along with treatment with hydroxychloroquine – unless contraindicated – and even common preventive strategies like low-dose aspirin if it suits their cardiovascular risk profile.
As for next steps, the task force noted several areas where additional focus is needed, such as identifying patient subgroups with increased cardiovascular risk. This could include patients with a longer disease duration or more flare-ups, older patients, and those with certain disease characteristics like antiphospholipid positivity in SLE.
Can EULAR’s recommendations be implemented in U.S. rheumatology practices?
“We have been hearing for years that patients with rheumatic diseases have an increased risk of cardiovascular disease,” Ali A. Duarte Garcia, MD, a rheumatologist at the Mayo Clinic in Rochester, Minn., told this news organization. “That has been consistently published for more than a decade now. But any further guidance about it has not been issued. I think there was a void there.”
“Certainly, cardiovascular disease risk in rheumatoid and psoriatic arthritis has been front of mind for the last decade or so,” Christie M. Bartels, MD, chief of the division of rheumatology at the University of Wisconsin, Madison, said when asked to comment on the recommendations. “But in some of these other conditions, it hasn’t been.”
When asked if rheumatologists would be ready and willing to implement these recommendations, Dr. Duarte Garcia acknowledged that it could be challenging for some.
“It’s a different workflow,” he said. “You’ve been trained traditionally to assess inflammation, to keep the disease under control, which is something they recommend, by the way. If you control the disease, patients do better. But I think lipid screening, for example, and testing for cholesterol, smoking cessation, those well-established programs are harder to bring to a rheumatology clinic. It’s doable, but it’s something that needs to be implemented within the current workflows and could take a few years to take hold.”
Dr. Bartels, however, noted that her group has done extensive work over the last 5 years incorporating certain interventions into practice, including sending patients with high blood pressure back to primary care.
“It’s a sustainable intervention in our clinic that basically our medical assistants and nurses do as a routine operation,” she said. “Our primary care providers are grateful to get these patients back. Our patients are grateful because otherwise when they come to the rheumatologist, get their blood pressure measured, and don’t get feedback, they assume they’re OK. So, we’re giving them a false signal.
“We have a similar intervention with smoking,” she added. “Often our patients aren’t even aware that they’re at increased risk of cardiovascular disease or that smoking might make their rheumatic disease and their cardiovascular outcomes worse. No one has had that conversation with them. They really welcome engaging in those discussions.
“Our tobacco intervention takes 90 seconds at point of care. Our blood pressure intervention at point of care, we’ve timed it, takes 3 minutes. There are ways that we can hardwire this into care.”
Along those lines, Dr. Duarte Garcia stated that the recommendations – although released by EULAR – are largely intuitive and should be very adaptable to an American health care context. He also recognized this moment as an opportunity for rheumatologists to consider patient outcomes beyond what they usually encounter firsthand.
“I don’t think we have many rheumatologists with patients who get a stroke or heart attack because if that happens, it’s in a hospital context or they go see a cardiologist,” he said. “You may see it once it happens if they survive and come and see you – or perhaps if you’re in a more integrated practice – but I don’t think it’s as apparent in our clinics because it is a predominantly outpatient practice and many times those are emergencies or inpatient complications.
“The bottom line,” he added, “is these are practical guidelines. It’s a push in the right direction, but there is still work to be done. And hopefully some of the recommendations, like measuring high blood pressure and addressing it just as in the general population, are something we can start to implement.”
Dr. Duarte Garcia reported receiving grant funding from the Rheumatology Research Foundation and the Centers for Disease Control and Prevention. Dr. Bartels reported that her group’s tobacco cessation work is funded by Pfizer’s Independent Grants for Learning and Change.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF THE RHEUMATIC DISEASES
A range of healthy dietary patterns can reduce risk of gout in women
A new study of thousands of women has found that sticking to recommended healthy dietary patterns can lessen the risk of new-onset gout.
“The identification of multiple patterns of eating that can similarly reduce a woman’s risk of incident gout in our study allows more choice for potential personalization of dietary recommendations according to culinary traditions and personal preferences to enhance adherence,” Chio Yokose, MD, of Harvard Medical School, Boston, and coauthors wrote. The study was published Jan. 31, 2022, in JAMA Internal Medicine.
To determine whether consistent healthy eating plays a role in preventing gout in women, the authors launched a prospective cohort study tied to the Nurses’ Health Study, an ongoing endeavor that has been questioning its participants’ food and beverage intake since 1984. Based on the 2020 to 2025 Dietary Guidelines for Americans, four healthy eating patterns were identified for assessment: the Dietary Approaches to Stop Hypertension (DASH), the Mediterranean diet, the Alternative Healthy Eating Index, and the Prudent diet, as well as the unhealthy Western dietary pattern for comparison.
Over 34 years of follow-up, the researchers identified 3,890 cases of gout among 80,039 women with an average age of 50.5 and an average body mass index (BMI) of 25.0 kg/m2. Women who strongly adhered to either of the four healthy dietary patterns had a significantly lower risk of gout, especially those who stuck to DASH (multivariable hazard ratio, 0.68; 95% confidence interval, 0.61-0.76) and Prudent (HR, 0.75; 95% CI, 0.73-0.90). In contrast, women with high Western diet scores had a 49% increased risk of gout (HR, 1.49; 95% CI, 1.33-1.68), compared with those who had low scores.
After additional analysis that factored in variables like diuretic use, alcohol use, and obesity, the associations between each diet and their risk of gout persisted in almost every instance. In particular, the most DASH-adherent women with normal BMI had a 68% lower risk of gout (HR, 0.32; 95% CI, 0.26-0.38), compared with the least-adherent women who were overweight or obese. Strong DASH adherence and no diuretic use also led to a 65% gout risk reduction (HR, 0.35; 95% CI, 0.30-0.41).
Healthy eating offers broad benefits for gout patients
“These results are consistent with a lot of the conversations we have on a day-to-day basis with patients,” Ted Mikuls, MD, of the University of Nebraska Medical Center, Omaha, said in an interview. “But I will say, I don’t get a lot of patients coming in saying: ‘Hey, what can I do to prevent gout?’ You’re usually seeing them after the fact.”
“These results shouldn’t be confused with that,” he said. “In other words, I wouldn’t want people interpreting this study to mean diet is always a satisfactory treatment for someone with established gout. The fact of the matter is, often it’s not. We need medication to effectively treat gout. I think this and other studies like it call for future research that can look at these dietary interventions as either standalone or probably adjuvant therapies in gout treatment.”
But, he added, that doesn’t mean conversations about diet aren’t of the utmost importance for gout patients.
“That shouldn’t stop clinicians from talking to patients about dietary changes that holistically are going to have positive benefits,” he said. “By the time you meet them, gout patients often already have other health conditions: high blood pressure, diabetes, obesity. The dietary changes that these authors studied are going to have a holistic benefit that goes well beyond gout risk, and that’s important. That’s a conversation that physicians and health care providers can and should be having right now with their patients.”
The authors acknowledged their study’s limitations, including the unmeasured or residual confounding that could come with any observational study as well as these rates of gout and these dietary patterns not necessarily being representative of a random sample of American women. “Future research could examine the population contributions of diets and other risk factors for incident female gout, as done in men.”
The study was funded by the National Institutes of Health. The authors reported several potential conflicts of interest, including receiving grants from the NIH and grants and personal fees from other organizations and pharmaceutical companies. Dr. Mikuls reported receiving past funding from Horizon Therapeutics and serving for them in a consulting capacity.
A new study of thousands of women has found that sticking to recommended healthy dietary patterns can lessen the risk of new-onset gout.
“The identification of multiple patterns of eating that can similarly reduce a woman’s risk of incident gout in our study allows more choice for potential personalization of dietary recommendations according to culinary traditions and personal preferences to enhance adherence,” Chio Yokose, MD, of Harvard Medical School, Boston, and coauthors wrote. The study was published Jan. 31, 2022, in JAMA Internal Medicine.
To determine whether consistent healthy eating plays a role in preventing gout in women, the authors launched a prospective cohort study tied to the Nurses’ Health Study, an ongoing endeavor that has been questioning its participants’ food and beverage intake since 1984. Based on the 2020 to 2025 Dietary Guidelines for Americans, four healthy eating patterns were identified for assessment: the Dietary Approaches to Stop Hypertension (DASH), the Mediterranean diet, the Alternative Healthy Eating Index, and the Prudent diet, as well as the unhealthy Western dietary pattern for comparison.
Over 34 years of follow-up, the researchers identified 3,890 cases of gout among 80,039 women with an average age of 50.5 and an average body mass index (BMI) of 25.0 kg/m2. Women who strongly adhered to either of the four healthy dietary patterns had a significantly lower risk of gout, especially those who stuck to DASH (multivariable hazard ratio, 0.68; 95% confidence interval, 0.61-0.76) and Prudent (HR, 0.75; 95% CI, 0.73-0.90). In contrast, women with high Western diet scores had a 49% increased risk of gout (HR, 1.49; 95% CI, 1.33-1.68), compared with those who had low scores.
After additional analysis that factored in variables like diuretic use, alcohol use, and obesity, the associations between each diet and their risk of gout persisted in almost every instance. In particular, the most DASH-adherent women with normal BMI had a 68% lower risk of gout (HR, 0.32; 95% CI, 0.26-0.38), compared with the least-adherent women who were overweight or obese. Strong DASH adherence and no diuretic use also led to a 65% gout risk reduction (HR, 0.35; 95% CI, 0.30-0.41).
Healthy eating offers broad benefits for gout patients
“These results are consistent with a lot of the conversations we have on a day-to-day basis with patients,” Ted Mikuls, MD, of the University of Nebraska Medical Center, Omaha, said in an interview. “But I will say, I don’t get a lot of patients coming in saying: ‘Hey, what can I do to prevent gout?’ You’re usually seeing them after the fact.”
“These results shouldn’t be confused with that,” he said. “In other words, I wouldn’t want people interpreting this study to mean diet is always a satisfactory treatment for someone with established gout. The fact of the matter is, often it’s not. We need medication to effectively treat gout. I think this and other studies like it call for future research that can look at these dietary interventions as either standalone or probably adjuvant therapies in gout treatment.”
But, he added, that doesn’t mean conversations about diet aren’t of the utmost importance for gout patients.
“That shouldn’t stop clinicians from talking to patients about dietary changes that holistically are going to have positive benefits,” he said. “By the time you meet them, gout patients often already have other health conditions: high blood pressure, diabetes, obesity. The dietary changes that these authors studied are going to have a holistic benefit that goes well beyond gout risk, and that’s important. That’s a conversation that physicians and health care providers can and should be having right now with their patients.”
The authors acknowledged their study’s limitations, including the unmeasured or residual confounding that could come with any observational study as well as these rates of gout and these dietary patterns not necessarily being representative of a random sample of American women. “Future research could examine the population contributions of diets and other risk factors for incident female gout, as done in men.”
The study was funded by the National Institutes of Health. The authors reported several potential conflicts of interest, including receiving grants from the NIH and grants and personal fees from other organizations and pharmaceutical companies. Dr. Mikuls reported receiving past funding from Horizon Therapeutics and serving for them in a consulting capacity.
A new study of thousands of women has found that sticking to recommended healthy dietary patterns can lessen the risk of new-onset gout.
“The identification of multiple patterns of eating that can similarly reduce a woman’s risk of incident gout in our study allows more choice for potential personalization of dietary recommendations according to culinary traditions and personal preferences to enhance adherence,” Chio Yokose, MD, of Harvard Medical School, Boston, and coauthors wrote. The study was published Jan. 31, 2022, in JAMA Internal Medicine.
To determine whether consistent healthy eating plays a role in preventing gout in women, the authors launched a prospective cohort study tied to the Nurses’ Health Study, an ongoing endeavor that has been questioning its participants’ food and beverage intake since 1984. Based on the 2020 to 2025 Dietary Guidelines for Americans, four healthy eating patterns were identified for assessment: the Dietary Approaches to Stop Hypertension (DASH), the Mediterranean diet, the Alternative Healthy Eating Index, and the Prudent diet, as well as the unhealthy Western dietary pattern for comparison.
Over 34 years of follow-up, the researchers identified 3,890 cases of gout among 80,039 women with an average age of 50.5 and an average body mass index (BMI) of 25.0 kg/m2. Women who strongly adhered to either of the four healthy dietary patterns had a significantly lower risk of gout, especially those who stuck to DASH (multivariable hazard ratio, 0.68; 95% confidence interval, 0.61-0.76) and Prudent (HR, 0.75; 95% CI, 0.73-0.90). In contrast, women with high Western diet scores had a 49% increased risk of gout (HR, 1.49; 95% CI, 1.33-1.68), compared with those who had low scores.
After additional analysis that factored in variables like diuretic use, alcohol use, and obesity, the associations between each diet and their risk of gout persisted in almost every instance. In particular, the most DASH-adherent women with normal BMI had a 68% lower risk of gout (HR, 0.32; 95% CI, 0.26-0.38), compared with the least-adherent women who were overweight or obese. Strong DASH adherence and no diuretic use also led to a 65% gout risk reduction (HR, 0.35; 95% CI, 0.30-0.41).
Healthy eating offers broad benefits for gout patients
“These results are consistent with a lot of the conversations we have on a day-to-day basis with patients,” Ted Mikuls, MD, of the University of Nebraska Medical Center, Omaha, said in an interview. “But I will say, I don’t get a lot of patients coming in saying: ‘Hey, what can I do to prevent gout?’ You’re usually seeing them after the fact.”
“These results shouldn’t be confused with that,” he said. “In other words, I wouldn’t want people interpreting this study to mean diet is always a satisfactory treatment for someone with established gout. The fact of the matter is, often it’s not. We need medication to effectively treat gout. I think this and other studies like it call for future research that can look at these dietary interventions as either standalone or probably adjuvant therapies in gout treatment.”
But, he added, that doesn’t mean conversations about diet aren’t of the utmost importance for gout patients.
“That shouldn’t stop clinicians from talking to patients about dietary changes that holistically are going to have positive benefits,” he said. “By the time you meet them, gout patients often already have other health conditions: high blood pressure, diabetes, obesity. The dietary changes that these authors studied are going to have a holistic benefit that goes well beyond gout risk, and that’s important. That’s a conversation that physicians and health care providers can and should be having right now with their patients.”
The authors acknowledged their study’s limitations, including the unmeasured or residual confounding that could come with any observational study as well as these rates of gout and these dietary patterns not necessarily being representative of a random sample of American women. “Future research could examine the population contributions of diets and other risk factors for incident female gout, as done in men.”
The study was funded by the National Institutes of Health. The authors reported several potential conflicts of interest, including receiving grants from the NIH and grants and personal fees from other organizations and pharmaceutical companies. Dr. Mikuls reported receiving past funding from Horizon Therapeutics and serving for them in a consulting capacity.
FROM JAMA INTERNAL MEDICINE