User login
Intensive gout treatment meets urate goal, lowers tophi burden
PHILADELPHIA – Patients with gout who underwent an intensive treat-to-target regimen of monthly up-titration of urate-lowering therapy (ULT) to reach a target serum urate level were significantly more likely to reach that goal at 1 year than were patients who received conventional gout management in a randomized, controlled trial.
These results came from the TICOG (Tight Control of Gout) trial, one of a handful of recent trials to test a treat-to-target strategy with ULT in the management of gout. Beyond the primary outcome of reaching target serum urate level of < 5 mg/dL (< 300 micromol/L), the results also showed that the tight-control strategy significantly lowered urate to a greater extent than conventional management, reduced tophus size in the first metatarsophalangeal (MTP) joint, and improved gray scale synovitis on ultrasound significantly more than with conventional management, Sarah Black, MBBS, a rheumatology trainee at Musgrave Park Hospital, Belfast, Northern Ireland, reported at the American College of Rheumatology annual meeting.
“Based on these outcomes, we question whether gout is best managed in primary or secondary care. We think there is an argument for establishing specialist gout clinics with more time to focus on patient education to help improve outcomes. These clinics could be led by allied health care professionals, such as specialist nurses and pharmacists,” Dr. Black said at the meeting.
Gout management guidelines issued by the British Society for Rheumatology in 2017 call for a target serum urate level of < 5 mg/dL, whereas the ACR’s 2020 guideline for the management of gout endorses a treat-to-target management strategy that aims for a serum urate level of < 6 mg/dL.
The single-center, nonblinded trial recruited 110 patients aged 18-85 years over a 3-year period to take ULT with allopurinol as first-line therapy starting at 100 mg/day. Everyone received the same advice regarding ULT up-titration, lifestyle changes, and gout education at baseline. The second-line agent for ULT was febuxostat (Uloric) 80 mg daily, with uricosuric drugs as third-line agents. All patients received colchicine or NSAID prophylaxis for gout flares for the first 6 months, depending on their comorbidities.
The trial excluded patients who had been treated with ULT within the past 6 months or had experienced prior hypersensitivity to ULT, severe renal impairment (creatinine clearance < 30 mL/min as measured by estimated glomerular filtration rate), significant liver impairment, or any other significant medical disease affecting life expectancy shorter than 1 year.
Conventional management consisted of urate level review at 0, 6, and 12 months with up-titration at each visit and primary care management of ULT between reviews until the target serum urate level was reached. In the tight-control group, monthly up-titrations occurred at the Musgrave Park Hospital at visits with the study team that were led by a rheumatologist and a specialist pharmacist.
A total of 48 patients in the conventional arm and 47 in the tight-control arm completed the trial. At baseline, monosodium urate crystals were detected in joint aspirates in 56% of patients receiving tight control and in 58.5% of those receiving conventional management. The mean serum urate level was 490 micromol/L (8.24 mg/dL) for tight-control patients and 470 micromol/L (7.9 mg/dL) for conventionally managed patients.
By 1 year, 89.4% of patients in the tight-control group had achieved the target urate level, compared with 39.6% in the conventional-management group (P < .001). At 6 months, serum urate had declined by 37.6% with tight control vs. 18% with conventional management. By the end of the trial, the median allopurinol dose was 400 mg with tight control (range, 200-900 mg) and 200 mg with conventional management (range, 0-400 mg). A total of 89% of patients were taking allopurinol at the end of the trial.
As expected, tight control led to more flares per month on average (0.35 vs. 0.13) in the 79 patients for whom complete data on flare frequency were available.
On blinded ultrasound evaluations, the median diameter of the first MTP tophus declined significantly more with tight control than with conventional management (–4.65 mm vs. –0.30 mm; P = .003). Gray scale synovitis in the knee improved in 63% of patients undergoing tight control, compared with 14% of conventionally managed patients (P = .043). The researchers observed no difference in resolution of the double-contour sign or in the number of erosions between the groups, although the 1-year time frame may not have been long enough to see resolution and improvement, Dr. Black said.
Dr. Black said that a follow-up study is planned with the same patient cohort at 3 years.
When asked about the feasibility of monthly ULT titration visits for gout management, audience member Tuhina Neogi, MD, professor of epidemiology at Boston University and chief of rheumatology at Boston Medical Center, told this news organization, “We don’t have a lot of data to guide us in that regard, and I also think it depends on what the increment of the dose titration is, but we generally do recognize that therapeutic inertia is bad – keeping someone on a dose for a long time. For me, I don’t think monthly is unreasonable if you have good prophylaxis [against acute flares].”
Dr. Neogi also noted that such monthly assessments don’t have to take place at a hospital. “I think there are many different practice models in which it could be implemented [that are not physician-driven].”
The study had no outside funding. Dr. Black has disclosed no relevant financial relationships. Dr. Neogi has received consulting fees from a variety of pharmaceutical companies, including Alnylam, Regeneron, Eli Lilly, EMD Serono, Novartis, Pfizer, and GlaxoSmithKline.
A version of this article first appeared on Medscape.com.
PHILADELPHIA – Patients with gout who underwent an intensive treat-to-target regimen of monthly up-titration of urate-lowering therapy (ULT) to reach a target serum urate level were significantly more likely to reach that goal at 1 year than were patients who received conventional gout management in a randomized, controlled trial.
These results came from the TICOG (Tight Control of Gout) trial, one of a handful of recent trials to test a treat-to-target strategy with ULT in the management of gout. Beyond the primary outcome of reaching target serum urate level of < 5 mg/dL (< 300 micromol/L), the results also showed that the tight-control strategy significantly lowered urate to a greater extent than conventional management, reduced tophus size in the first metatarsophalangeal (MTP) joint, and improved gray scale synovitis on ultrasound significantly more than with conventional management, Sarah Black, MBBS, a rheumatology trainee at Musgrave Park Hospital, Belfast, Northern Ireland, reported at the American College of Rheumatology annual meeting.
“Based on these outcomes, we question whether gout is best managed in primary or secondary care. We think there is an argument for establishing specialist gout clinics with more time to focus on patient education to help improve outcomes. These clinics could be led by allied health care professionals, such as specialist nurses and pharmacists,” Dr. Black said at the meeting.
Gout management guidelines issued by the British Society for Rheumatology in 2017 call for a target serum urate level of < 5 mg/dL, whereas the ACR’s 2020 guideline for the management of gout endorses a treat-to-target management strategy that aims for a serum urate level of < 6 mg/dL.
The single-center, nonblinded trial recruited 110 patients aged 18-85 years over a 3-year period to take ULT with allopurinol as first-line therapy starting at 100 mg/day. Everyone received the same advice regarding ULT up-titration, lifestyle changes, and gout education at baseline. The second-line agent for ULT was febuxostat (Uloric) 80 mg daily, with uricosuric drugs as third-line agents. All patients received colchicine or NSAID prophylaxis for gout flares for the first 6 months, depending on their comorbidities.
The trial excluded patients who had been treated with ULT within the past 6 months or had experienced prior hypersensitivity to ULT, severe renal impairment (creatinine clearance < 30 mL/min as measured by estimated glomerular filtration rate), significant liver impairment, or any other significant medical disease affecting life expectancy shorter than 1 year.
Conventional management consisted of urate level review at 0, 6, and 12 months with up-titration at each visit and primary care management of ULT between reviews until the target serum urate level was reached. In the tight-control group, monthly up-titrations occurred at the Musgrave Park Hospital at visits with the study team that were led by a rheumatologist and a specialist pharmacist.
A total of 48 patients in the conventional arm and 47 in the tight-control arm completed the trial. At baseline, monosodium urate crystals were detected in joint aspirates in 56% of patients receiving tight control and in 58.5% of those receiving conventional management. The mean serum urate level was 490 micromol/L (8.24 mg/dL) for tight-control patients and 470 micromol/L (7.9 mg/dL) for conventionally managed patients.
By 1 year, 89.4% of patients in the tight-control group had achieved the target urate level, compared with 39.6% in the conventional-management group (P < .001). At 6 months, serum urate had declined by 37.6% with tight control vs. 18% with conventional management. By the end of the trial, the median allopurinol dose was 400 mg with tight control (range, 200-900 mg) and 200 mg with conventional management (range, 0-400 mg). A total of 89% of patients were taking allopurinol at the end of the trial.
As expected, tight control led to more flares per month on average (0.35 vs. 0.13) in the 79 patients for whom complete data on flare frequency were available.
On blinded ultrasound evaluations, the median diameter of the first MTP tophus declined significantly more with tight control than with conventional management (–4.65 mm vs. –0.30 mm; P = .003). Gray scale synovitis in the knee improved in 63% of patients undergoing tight control, compared with 14% of conventionally managed patients (P = .043). The researchers observed no difference in resolution of the double-contour sign or in the number of erosions between the groups, although the 1-year time frame may not have been long enough to see resolution and improvement, Dr. Black said.
Dr. Black said that a follow-up study is planned with the same patient cohort at 3 years.
When asked about the feasibility of monthly ULT titration visits for gout management, audience member Tuhina Neogi, MD, professor of epidemiology at Boston University and chief of rheumatology at Boston Medical Center, told this news organization, “We don’t have a lot of data to guide us in that regard, and I also think it depends on what the increment of the dose titration is, but we generally do recognize that therapeutic inertia is bad – keeping someone on a dose for a long time. For me, I don’t think monthly is unreasonable if you have good prophylaxis [against acute flares].”
Dr. Neogi also noted that such monthly assessments don’t have to take place at a hospital. “I think there are many different practice models in which it could be implemented [that are not physician-driven].”
The study had no outside funding. Dr. Black has disclosed no relevant financial relationships. Dr. Neogi has received consulting fees from a variety of pharmaceutical companies, including Alnylam, Regeneron, Eli Lilly, EMD Serono, Novartis, Pfizer, and GlaxoSmithKline.
A version of this article first appeared on Medscape.com.
PHILADELPHIA – Patients with gout who underwent an intensive treat-to-target regimen of monthly up-titration of urate-lowering therapy (ULT) to reach a target serum urate level were significantly more likely to reach that goal at 1 year than were patients who received conventional gout management in a randomized, controlled trial.
These results came from the TICOG (Tight Control of Gout) trial, one of a handful of recent trials to test a treat-to-target strategy with ULT in the management of gout. Beyond the primary outcome of reaching target serum urate level of < 5 mg/dL (< 300 micromol/L), the results also showed that the tight-control strategy significantly lowered urate to a greater extent than conventional management, reduced tophus size in the first metatarsophalangeal (MTP) joint, and improved gray scale synovitis on ultrasound significantly more than with conventional management, Sarah Black, MBBS, a rheumatology trainee at Musgrave Park Hospital, Belfast, Northern Ireland, reported at the American College of Rheumatology annual meeting.
“Based on these outcomes, we question whether gout is best managed in primary or secondary care. We think there is an argument for establishing specialist gout clinics with more time to focus on patient education to help improve outcomes. These clinics could be led by allied health care professionals, such as specialist nurses and pharmacists,” Dr. Black said at the meeting.
Gout management guidelines issued by the British Society for Rheumatology in 2017 call for a target serum urate level of < 5 mg/dL, whereas the ACR’s 2020 guideline for the management of gout endorses a treat-to-target management strategy that aims for a serum urate level of < 6 mg/dL.
The single-center, nonblinded trial recruited 110 patients aged 18-85 years over a 3-year period to take ULT with allopurinol as first-line therapy starting at 100 mg/day. Everyone received the same advice regarding ULT up-titration, lifestyle changes, and gout education at baseline. The second-line agent for ULT was febuxostat (Uloric) 80 mg daily, with uricosuric drugs as third-line agents. All patients received colchicine or NSAID prophylaxis for gout flares for the first 6 months, depending on their comorbidities.
The trial excluded patients who had been treated with ULT within the past 6 months or had experienced prior hypersensitivity to ULT, severe renal impairment (creatinine clearance < 30 mL/min as measured by estimated glomerular filtration rate), significant liver impairment, or any other significant medical disease affecting life expectancy shorter than 1 year.
Conventional management consisted of urate level review at 0, 6, and 12 months with up-titration at each visit and primary care management of ULT between reviews until the target serum urate level was reached. In the tight-control group, monthly up-titrations occurred at the Musgrave Park Hospital at visits with the study team that were led by a rheumatologist and a specialist pharmacist.
A total of 48 patients in the conventional arm and 47 in the tight-control arm completed the trial. At baseline, monosodium urate crystals were detected in joint aspirates in 56% of patients receiving tight control and in 58.5% of those receiving conventional management. The mean serum urate level was 490 micromol/L (8.24 mg/dL) for tight-control patients and 470 micromol/L (7.9 mg/dL) for conventionally managed patients.
By 1 year, 89.4% of patients in the tight-control group had achieved the target urate level, compared with 39.6% in the conventional-management group (P < .001). At 6 months, serum urate had declined by 37.6% with tight control vs. 18% with conventional management. By the end of the trial, the median allopurinol dose was 400 mg with tight control (range, 200-900 mg) and 200 mg with conventional management (range, 0-400 mg). A total of 89% of patients were taking allopurinol at the end of the trial.
As expected, tight control led to more flares per month on average (0.35 vs. 0.13) in the 79 patients for whom complete data on flare frequency were available.
On blinded ultrasound evaluations, the median diameter of the first MTP tophus declined significantly more with tight control than with conventional management (–4.65 mm vs. –0.30 mm; P = .003). Gray scale synovitis in the knee improved in 63% of patients undergoing tight control, compared with 14% of conventionally managed patients (P = .043). The researchers observed no difference in resolution of the double-contour sign or in the number of erosions between the groups, although the 1-year time frame may not have been long enough to see resolution and improvement, Dr. Black said.
Dr. Black said that a follow-up study is planned with the same patient cohort at 3 years.
When asked about the feasibility of monthly ULT titration visits for gout management, audience member Tuhina Neogi, MD, professor of epidemiology at Boston University and chief of rheumatology at Boston Medical Center, told this news organization, “We don’t have a lot of data to guide us in that regard, and I also think it depends on what the increment of the dose titration is, but we generally do recognize that therapeutic inertia is bad – keeping someone on a dose for a long time. For me, I don’t think monthly is unreasonable if you have good prophylaxis [against acute flares].”
Dr. Neogi also noted that such monthly assessments don’t have to take place at a hospital. “I think there are many different practice models in which it could be implemented [that are not physician-driven].”
The study had no outside funding. Dr. Black has disclosed no relevant financial relationships. Dr. Neogi has received consulting fees from a variety of pharmaceutical companies, including Alnylam, Regeneron, Eli Lilly, EMD Serono, Novartis, Pfizer, and GlaxoSmithKline.
A version of this article first appeared on Medscape.com.
AT ACR 2022
Prednisone, colchicine equivalent in efficacy for CPP crystal arthritis
PHILADELPHIA – Prednisone appears to have the edge over colchicine for control of pain in patients with acute calcium pyrophosphate (CPP) crystal arthritis, an intensely painful rheumatic disease primarily affecting older patients.
Among 111 patients with acute CPP crystal arthritis randomized to receive either prednisone or colchicine for control of acute pain in a multicenter study, 2 days of therapy with the oral agents provided equivalent pain relief on the second day, and patients generally tolerated each agent well, reported Tristan Pascart, MD, from the Groupement Hospitalier de l’Institut Catholique de Lille (France).
“Almost three-fourths of patients are considered to be good responders to both drugs on day 3, and, maybe, safety is the key issue distinguishing the two treatments: Colchicine was generally well tolerated, but even with this very short time frame of treatment, one patient out of five had diarrhea, which is more of a concern in this elderly population at risk of dehydration,” he said in an oral abstract session at the annual meeting of the American College of Rheumatology.
In contrast, only about 6% of patients assigned to prednisone had diarrhea, and other adverse events that occurred more frequently with the corticosteroid, including hypertension, hyperglycemia, and insomnia all resolved after the therapy was stopped.
Common and acutely painful
Acute CPP crystal arthritis is a common complication that often occurs during hospitalization for primarily nonrheumatologic causes, Dr. Pascart said, and “in the absence of clinical trials, the management relies on expert opinion, which stems from extrapolated data from gap studies” primarily with prednisone or colchicine, Dr. Pascart said.
To fill in the knowledge gap, Dr. Pascart and colleagues conducted the COLCHICORT study to evaluate whether the two drugs were comparable in efficacy and safety for control of acute pain in a vulnerable population.
The multicenter, open-label trial included patients older than age 65 years with an estimated glomerular filtration rate above 30 mL/min per 1.73 m2 who presented with acute CPP deposition arthritis with symptoms occurring within the previous 36 hours. CPP arthritis was defined by the identification of CPP crystals on synovial fluid analysis or typical clinical presentation with evidence of chondrocalcinosis on x-rays or ultrasound.
Patients with a history of gout, cognitive decline that could impair pain assessment, or contraindications to either of the study drugs were excluded.
The participants were randomized to receive either colchicine 1.5 mg (1 mg to start, then 0.5 mg one hour later) at baseline and then 1 mg on day 1, or oral prednisone 30 mg at baseline and on day 1. The patients also received 1 g of systemic acetaminophen, and three 50-mg doses of tramadol during the first 24 hours.
Of the 111 patients randomized, 54 were assigned to receive prednisone, and 57 were assigned to receive colchicine. Baseline characteristics were similar between the groups, with a mean age of about 86 years, body mass index of around 25 kg/m2, and blood pressure in the range of 130/69 mm Hg.
For nearly half of all patients in study each arm the most painful joint was the knee, followed by wrists and ankles.
There was no difference between the groups in the primary efficacy outcome of a change at 24 hours over baseline in visual analog scale (VAS) (0-100 mm) scores, either in a per-protocol analysis or modified intention-to-treat analysis. The mean change in VAS at 24 hours in the colchicine group was –36.6 mm, compared with –37.7 mm in the prednisone group. The investigators had previously determined that any difference between the two drugs of less than 13 mm on pain VAS at 24 hours would meet the definition for equivalent efficacy.
In both groups, a majority of patients had either an improvement greater than 50% in pain VAS scores and/or a pain VAS score less than 40 mm at both 24 and 48 hours.
At 7 days of follow-up, 21.8% of patients assigned to colchicine had diarrhea, compared with 5.6% of those assigned to prednisone. Adverse events occurring more frequently with prednisone included hyperglycemia, hypertension, and insomnia.
Patients who received colchicine and were also on statins had a trend toward a higher risk for diarrhea, but the study was not adequately powered to detect an association, and the trend was not statistically significant, Dr. Pascart said.
“Taken together, safety issues suggest that prednisone should be considered as the first-line therapy in acute CPP crystal arthritis. Future research is warranted to determine factors increasing the risk of colchicine-induced diarrhea,” he concluded.
Both drugs are used
Sara K. Tedeschi, MD, from Brigham & Women’s Hospital in Boston, who attended the session where the data were presented, has a special clinical interest in CPP deposition disease. She applauded Dr. Pascart and colleagues for conducting a rare clinical trial in CPP crystal arthritis.
In an interview, she said that the study suggests “we can keep in mind shorter courses of treatment for acute CPP crystal arthritis; I think that’s one big takeaway from this study.”
Asked whether she would change her practice based on the findings, Dr. Tedeschi replied: “I personally am not sure that I would be moved to use prednisone more than colchicine; I actually take away from this that colchicine is equivalent to prednisone for short-term use for CPP arthritis, but I think it’s also really important to note that this is in the context of quite a lot of acetaminophen and quite a lot of tramadol, and frankly I don’t usually use tramadol with my patients, but I might consider doing that, especially as there were no delirium events in this population.”
Dr. Tedeschi was not involved in the study.
Asked the same question, Michael Toprover, MD, from New York University Langone Medical Center, a moderator of the session who was not involved in the study, said: “I usually use a combination of medications. I generally, in someone who is hospitalized in particular and is in such severe pain, use a combination of colchicine and prednisone, unless I’m worried about infection, in which case I’ll start colchicine until we’ve proven that it’s CPPD, and then I’ll add prednisone.”
The study was funded by PHRC-1 GIRCI Nord Ouest, a clinical research program funded by the Ministry of Health in France. Dr. Pascart, Dr. Tedeschi, and Dr. Toprover all reported having no relevant conflicts of interest.
PHILADELPHIA – Prednisone appears to have the edge over colchicine for control of pain in patients with acute calcium pyrophosphate (CPP) crystal arthritis, an intensely painful rheumatic disease primarily affecting older patients.
Among 111 patients with acute CPP crystal arthritis randomized to receive either prednisone or colchicine for control of acute pain in a multicenter study, 2 days of therapy with the oral agents provided equivalent pain relief on the second day, and patients generally tolerated each agent well, reported Tristan Pascart, MD, from the Groupement Hospitalier de l’Institut Catholique de Lille (France).
“Almost three-fourths of patients are considered to be good responders to both drugs on day 3, and, maybe, safety is the key issue distinguishing the two treatments: Colchicine was generally well tolerated, but even with this very short time frame of treatment, one patient out of five had diarrhea, which is more of a concern in this elderly population at risk of dehydration,” he said in an oral abstract session at the annual meeting of the American College of Rheumatology.
In contrast, only about 6% of patients assigned to prednisone had diarrhea, and other adverse events that occurred more frequently with the corticosteroid, including hypertension, hyperglycemia, and insomnia all resolved after the therapy was stopped.
Common and acutely painful
Acute CPP crystal arthritis is a common complication that often occurs during hospitalization for primarily nonrheumatologic causes, Dr. Pascart said, and “in the absence of clinical trials, the management relies on expert opinion, which stems from extrapolated data from gap studies” primarily with prednisone or colchicine, Dr. Pascart said.
To fill in the knowledge gap, Dr. Pascart and colleagues conducted the COLCHICORT study to evaluate whether the two drugs were comparable in efficacy and safety for control of acute pain in a vulnerable population.
The multicenter, open-label trial included patients older than age 65 years with an estimated glomerular filtration rate above 30 mL/min per 1.73 m2 who presented with acute CPP deposition arthritis with symptoms occurring within the previous 36 hours. CPP arthritis was defined by the identification of CPP crystals on synovial fluid analysis or typical clinical presentation with evidence of chondrocalcinosis on x-rays or ultrasound.
Patients with a history of gout, cognitive decline that could impair pain assessment, or contraindications to either of the study drugs were excluded.
The participants were randomized to receive either colchicine 1.5 mg (1 mg to start, then 0.5 mg one hour later) at baseline and then 1 mg on day 1, or oral prednisone 30 mg at baseline and on day 1. The patients also received 1 g of systemic acetaminophen, and three 50-mg doses of tramadol during the first 24 hours.
Of the 111 patients randomized, 54 were assigned to receive prednisone, and 57 were assigned to receive colchicine. Baseline characteristics were similar between the groups, with a mean age of about 86 years, body mass index of around 25 kg/m2, and blood pressure in the range of 130/69 mm Hg.
For nearly half of all patients in study each arm the most painful joint was the knee, followed by wrists and ankles.
There was no difference between the groups in the primary efficacy outcome of a change at 24 hours over baseline in visual analog scale (VAS) (0-100 mm) scores, either in a per-protocol analysis or modified intention-to-treat analysis. The mean change in VAS at 24 hours in the colchicine group was –36.6 mm, compared with –37.7 mm in the prednisone group. The investigators had previously determined that any difference between the two drugs of less than 13 mm on pain VAS at 24 hours would meet the definition for equivalent efficacy.
In both groups, a majority of patients had either an improvement greater than 50% in pain VAS scores and/or a pain VAS score less than 40 mm at both 24 and 48 hours.
At 7 days of follow-up, 21.8% of patients assigned to colchicine had diarrhea, compared with 5.6% of those assigned to prednisone. Adverse events occurring more frequently with prednisone included hyperglycemia, hypertension, and insomnia.
Patients who received colchicine and were also on statins had a trend toward a higher risk for diarrhea, but the study was not adequately powered to detect an association, and the trend was not statistically significant, Dr. Pascart said.
“Taken together, safety issues suggest that prednisone should be considered as the first-line therapy in acute CPP crystal arthritis. Future research is warranted to determine factors increasing the risk of colchicine-induced diarrhea,” he concluded.
Both drugs are used
Sara K. Tedeschi, MD, from Brigham & Women’s Hospital in Boston, who attended the session where the data were presented, has a special clinical interest in CPP deposition disease. She applauded Dr. Pascart and colleagues for conducting a rare clinical trial in CPP crystal arthritis.
In an interview, she said that the study suggests “we can keep in mind shorter courses of treatment for acute CPP crystal arthritis; I think that’s one big takeaway from this study.”
Asked whether she would change her practice based on the findings, Dr. Tedeschi replied: “I personally am not sure that I would be moved to use prednisone more than colchicine; I actually take away from this that colchicine is equivalent to prednisone for short-term use for CPP arthritis, but I think it’s also really important to note that this is in the context of quite a lot of acetaminophen and quite a lot of tramadol, and frankly I don’t usually use tramadol with my patients, but I might consider doing that, especially as there were no delirium events in this population.”
Dr. Tedeschi was not involved in the study.
Asked the same question, Michael Toprover, MD, from New York University Langone Medical Center, a moderator of the session who was not involved in the study, said: “I usually use a combination of medications. I generally, in someone who is hospitalized in particular and is in such severe pain, use a combination of colchicine and prednisone, unless I’m worried about infection, in which case I’ll start colchicine until we’ve proven that it’s CPPD, and then I’ll add prednisone.”
The study was funded by PHRC-1 GIRCI Nord Ouest, a clinical research program funded by the Ministry of Health in France. Dr. Pascart, Dr. Tedeschi, and Dr. Toprover all reported having no relevant conflicts of interest.
PHILADELPHIA – Prednisone appears to have the edge over colchicine for control of pain in patients with acute calcium pyrophosphate (CPP) crystal arthritis, an intensely painful rheumatic disease primarily affecting older patients.
Among 111 patients with acute CPP crystal arthritis randomized to receive either prednisone or colchicine for control of acute pain in a multicenter study, 2 days of therapy with the oral agents provided equivalent pain relief on the second day, and patients generally tolerated each agent well, reported Tristan Pascart, MD, from the Groupement Hospitalier de l’Institut Catholique de Lille (France).
“Almost three-fourths of patients are considered to be good responders to both drugs on day 3, and, maybe, safety is the key issue distinguishing the two treatments: Colchicine was generally well tolerated, but even with this very short time frame of treatment, one patient out of five had diarrhea, which is more of a concern in this elderly population at risk of dehydration,” he said in an oral abstract session at the annual meeting of the American College of Rheumatology.
In contrast, only about 6% of patients assigned to prednisone had diarrhea, and other adverse events that occurred more frequently with the corticosteroid, including hypertension, hyperglycemia, and insomnia all resolved after the therapy was stopped.
Common and acutely painful
Acute CPP crystal arthritis is a common complication that often occurs during hospitalization for primarily nonrheumatologic causes, Dr. Pascart said, and “in the absence of clinical trials, the management relies on expert opinion, which stems from extrapolated data from gap studies” primarily with prednisone or colchicine, Dr. Pascart said.
To fill in the knowledge gap, Dr. Pascart and colleagues conducted the COLCHICORT study to evaluate whether the two drugs were comparable in efficacy and safety for control of acute pain in a vulnerable population.
The multicenter, open-label trial included patients older than age 65 years with an estimated glomerular filtration rate above 30 mL/min per 1.73 m2 who presented with acute CPP deposition arthritis with symptoms occurring within the previous 36 hours. CPP arthritis was defined by the identification of CPP crystals on synovial fluid analysis or typical clinical presentation with evidence of chondrocalcinosis on x-rays or ultrasound.
Patients with a history of gout, cognitive decline that could impair pain assessment, or contraindications to either of the study drugs were excluded.
The participants were randomized to receive either colchicine 1.5 mg (1 mg to start, then 0.5 mg one hour later) at baseline and then 1 mg on day 1, or oral prednisone 30 mg at baseline and on day 1. The patients also received 1 g of systemic acetaminophen, and three 50-mg doses of tramadol during the first 24 hours.
Of the 111 patients randomized, 54 were assigned to receive prednisone, and 57 were assigned to receive colchicine. Baseline characteristics were similar between the groups, with a mean age of about 86 years, body mass index of around 25 kg/m2, and blood pressure in the range of 130/69 mm Hg.
For nearly half of all patients in study each arm the most painful joint was the knee, followed by wrists and ankles.
There was no difference between the groups in the primary efficacy outcome of a change at 24 hours over baseline in visual analog scale (VAS) (0-100 mm) scores, either in a per-protocol analysis or modified intention-to-treat analysis. The mean change in VAS at 24 hours in the colchicine group was –36.6 mm, compared with –37.7 mm in the prednisone group. The investigators had previously determined that any difference between the two drugs of less than 13 mm on pain VAS at 24 hours would meet the definition for equivalent efficacy.
In both groups, a majority of patients had either an improvement greater than 50% in pain VAS scores and/or a pain VAS score less than 40 mm at both 24 and 48 hours.
At 7 days of follow-up, 21.8% of patients assigned to colchicine had diarrhea, compared with 5.6% of those assigned to prednisone. Adverse events occurring more frequently with prednisone included hyperglycemia, hypertension, and insomnia.
Patients who received colchicine and were also on statins had a trend toward a higher risk for diarrhea, but the study was not adequately powered to detect an association, and the trend was not statistically significant, Dr. Pascart said.
“Taken together, safety issues suggest that prednisone should be considered as the first-line therapy in acute CPP crystal arthritis. Future research is warranted to determine factors increasing the risk of colchicine-induced diarrhea,” he concluded.
Both drugs are used
Sara K. Tedeschi, MD, from Brigham & Women’s Hospital in Boston, who attended the session where the data were presented, has a special clinical interest in CPP deposition disease. She applauded Dr. Pascart and colleagues for conducting a rare clinical trial in CPP crystal arthritis.
In an interview, she said that the study suggests “we can keep in mind shorter courses of treatment for acute CPP crystal arthritis; I think that’s one big takeaway from this study.”
Asked whether she would change her practice based on the findings, Dr. Tedeschi replied: “I personally am not sure that I would be moved to use prednisone more than colchicine; I actually take away from this that colchicine is equivalent to prednisone for short-term use for CPP arthritis, but I think it’s also really important to note that this is in the context of quite a lot of acetaminophen and quite a lot of tramadol, and frankly I don’t usually use tramadol with my patients, but I might consider doing that, especially as there were no delirium events in this population.”
Dr. Tedeschi was not involved in the study.
Asked the same question, Michael Toprover, MD, from New York University Langone Medical Center, a moderator of the session who was not involved in the study, said: “I usually use a combination of medications. I generally, in someone who is hospitalized in particular and is in such severe pain, use a combination of colchicine and prednisone, unless I’m worried about infection, in which case I’ll start colchicine until we’ve proven that it’s CPPD, and then I’ll add prednisone.”
The study was funded by PHRC-1 GIRCI Nord Ouest, a clinical research program funded by the Ministry of Health in France. Dr. Pascart, Dr. Tedeschi, and Dr. Toprover all reported having no relevant conflicts of interest.
AT ACR 2022
Gout too often treated only in emergency department
Only about one in three patients seen in the emergency department of an academic health system for acute gout had a follow-up visit that addressed this condition, Lesley Jackson, MD, of the University of Alabama at Birmingham, reported at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network (G-CAN).
Dr. Jackson presented research done on patients seen within her university’s health system, looking at 72 patients seen in the ED between September 2021 and February 2022. Medications prescribed at discharge from the ED included corticosteroids (46 patients, or 64%), opioids (45 patients, 63%), NSAIDs (31 patients, 43%), and colchicine (23 patients, 32%).
Only 26 patients, or about 36%, had a subsequent outpatient visit in the UAB health system addressing gout, she said. Of 33 patients with any outpatient follow-up visit within the UAB system, 21 were within 1 month after the index ED visit, followed by 3 more prior to 3 months, and 9 more after 3 months.
The limitations of the study includes its collection of data from a single institution. But the results highlight the need for improved quality of care for gout, with too many people being treated for this condition primarily in the ED, she said.
In an email exchange arranged by the Arthritis Foundation, Herbert S. B. Baraf, MD, said he agreed that patients too often limit their treatment for gout to seeking care for acute attacks in the ED.
Because of competing demands, physicians working there are more to take a “Band-Aid” approach and not impress upon patients that gout is a lifelong condition that needs follow-up and monitoring, said Dr. Baraf, clinical professor of medicine at George Washington University, Washington, and an associate clinical professor at the University of Maryland, Baltimore. He retired from private practice in 2022.
“This problem is akin to the patient who has a hip fracture due to osteoporosis who gets a surgical repair but is never referred for osteoporotic management,” wrote Dr. Baraf, who is a former board member of the Arthritis Foundation.
He suggested viewing gout as a form of arthritis that has two components.
“The first, that which brings the patient to seek medical care, is the often exquisitely painful attack of pain and swelling in a joint or joints that comes on acutely,” he wrote. “Calming these attacks are the focus of the patient and the doctor, who does the evaluation as relief of pain and inflammation is the most pressing task at hand.”
But equally important is the second element, addressing the cause of these flare ups of arthritis, he wrote. Elevated uric acid leads to crystalline deposits of urate in the joints, particularly in the feet, ankles, knees, and hands. Over time, these deposits generate seemingly random flare ups of acute joint pain in one or more of these areas.
“Thus, when a patient presents to an emergency room with a first or second attack of gout, pain relief is the primary focus of the visit,” Dr. Baraf wrote. “But if over time that is the only focus, and the elevation of serum uric acid is not addressed, deposits will continue to mount and flare ups will occur with increasing frequency and severity.”
This study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Jackson has no relevant financial disclosures.
Only about one in three patients seen in the emergency department of an academic health system for acute gout had a follow-up visit that addressed this condition, Lesley Jackson, MD, of the University of Alabama at Birmingham, reported at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network (G-CAN).
Dr. Jackson presented research done on patients seen within her university’s health system, looking at 72 patients seen in the ED between September 2021 and February 2022. Medications prescribed at discharge from the ED included corticosteroids (46 patients, or 64%), opioids (45 patients, 63%), NSAIDs (31 patients, 43%), and colchicine (23 patients, 32%).
Only 26 patients, or about 36%, had a subsequent outpatient visit in the UAB health system addressing gout, she said. Of 33 patients with any outpatient follow-up visit within the UAB system, 21 were within 1 month after the index ED visit, followed by 3 more prior to 3 months, and 9 more after 3 months.
The limitations of the study includes its collection of data from a single institution. But the results highlight the need for improved quality of care for gout, with too many people being treated for this condition primarily in the ED, she said.
In an email exchange arranged by the Arthritis Foundation, Herbert S. B. Baraf, MD, said he agreed that patients too often limit their treatment for gout to seeking care for acute attacks in the ED.
Because of competing demands, physicians working there are more to take a “Band-Aid” approach and not impress upon patients that gout is a lifelong condition that needs follow-up and monitoring, said Dr. Baraf, clinical professor of medicine at George Washington University, Washington, and an associate clinical professor at the University of Maryland, Baltimore. He retired from private practice in 2022.
“This problem is akin to the patient who has a hip fracture due to osteoporosis who gets a surgical repair but is never referred for osteoporotic management,” wrote Dr. Baraf, who is a former board member of the Arthritis Foundation.
He suggested viewing gout as a form of arthritis that has two components.
“The first, that which brings the patient to seek medical care, is the often exquisitely painful attack of pain and swelling in a joint or joints that comes on acutely,” he wrote. “Calming these attacks are the focus of the patient and the doctor, who does the evaluation as relief of pain and inflammation is the most pressing task at hand.”
But equally important is the second element, addressing the cause of these flare ups of arthritis, he wrote. Elevated uric acid leads to crystalline deposits of urate in the joints, particularly in the feet, ankles, knees, and hands. Over time, these deposits generate seemingly random flare ups of acute joint pain in one or more of these areas.
“Thus, when a patient presents to an emergency room with a first or second attack of gout, pain relief is the primary focus of the visit,” Dr. Baraf wrote. “But if over time that is the only focus, and the elevation of serum uric acid is not addressed, deposits will continue to mount and flare ups will occur with increasing frequency and severity.”
This study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Jackson has no relevant financial disclosures.
Only about one in three patients seen in the emergency department of an academic health system for acute gout had a follow-up visit that addressed this condition, Lesley Jackson, MD, of the University of Alabama at Birmingham, reported at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network (G-CAN).
Dr. Jackson presented research done on patients seen within her university’s health system, looking at 72 patients seen in the ED between September 2021 and February 2022. Medications prescribed at discharge from the ED included corticosteroids (46 patients, or 64%), opioids (45 patients, 63%), NSAIDs (31 patients, 43%), and colchicine (23 patients, 32%).
Only 26 patients, or about 36%, had a subsequent outpatient visit in the UAB health system addressing gout, she said. Of 33 patients with any outpatient follow-up visit within the UAB system, 21 were within 1 month after the index ED visit, followed by 3 more prior to 3 months, and 9 more after 3 months.
The limitations of the study includes its collection of data from a single institution. But the results highlight the need for improved quality of care for gout, with too many people being treated for this condition primarily in the ED, she said.
In an email exchange arranged by the Arthritis Foundation, Herbert S. B. Baraf, MD, said he agreed that patients too often limit their treatment for gout to seeking care for acute attacks in the ED.
Because of competing demands, physicians working there are more to take a “Band-Aid” approach and not impress upon patients that gout is a lifelong condition that needs follow-up and monitoring, said Dr. Baraf, clinical professor of medicine at George Washington University, Washington, and an associate clinical professor at the University of Maryland, Baltimore. He retired from private practice in 2022.
“This problem is akin to the patient who has a hip fracture due to osteoporosis who gets a surgical repair but is never referred for osteoporotic management,” wrote Dr. Baraf, who is a former board member of the Arthritis Foundation.
He suggested viewing gout as a form of arthritis that has two components.
“The first, that which brings the patient to seek medical care, is the often exquisitely painful attack of pain and swelling in a joint or joints that comes on acutely,” he wrote. “Calming these attacks are the focus of the patient and the doctor, who does the evaluation as relief of pain and inflammation is the most pressing task at hand.”
But equally important is the second element, addressing the cause of these flare ups of arthritis, he wrote. Elevated uric acid leads to crystalline deposits of urate in the joints, particularly in the feet, ankles, knees, and hands. Over time, these deposits generate seemingly random flare ups of acute joint pain in one or more of these areas.
“Thus, when a patient presents to an emergency room with a first or second attack of gout, pain relief is the primary focus of the visit,” Dr. Baraf wrote. “But if over time that is the only focus, and the elevation of serum uric acid is not addressed, deposits will continue to mount and flare ups will occur with increasing frequency and severity.”
This study was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Jackson has no relevant financial disclosures.
FROM G-CAN 2022
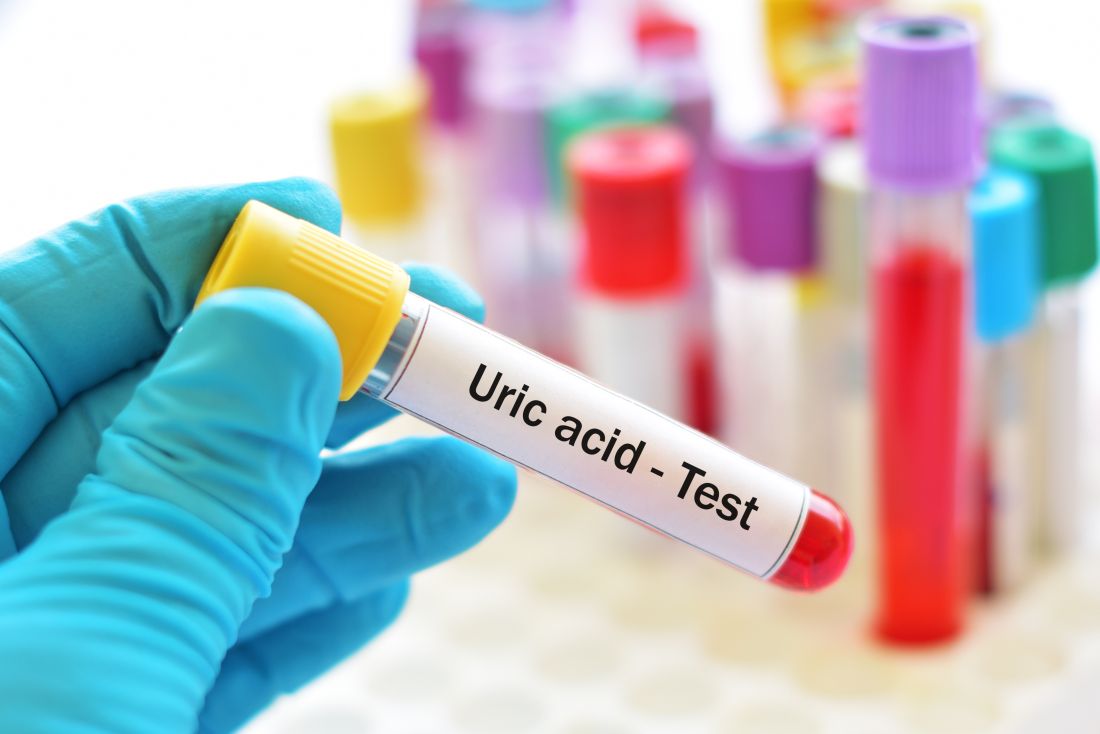
Poor control of serum urate linked to cardiovascular risk in patients with gout
A new study based on U.S. veterans’ medical records adds to the evidence for a link between gout – especially poorly controlled cases – and cardiovascular disease (CVD) risk, Tate Johnson, MD, reported at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network.
Gout was associated with a 68% increased risk of heart failure (HF) hospitalization, 25% increased risk of HF-related death, and a 22% increased risk of major adverse cardiovascular events (MACE), said Dr. Johnson, of the division of rheumatology at the University of Nebraska, Omaha.
Poorly controlled serum urate was associated with a higher risk of cardiovascular events, regardless of the use of urate-lowering therapy (ULT). He said more research is needed to see if there is a causal link between gout, hyperuricemia – or its treatment – and CVD risk.
Dr. Johnson and colleagues used records from the Veterans Health Administration for this study. They created a retrospective, matched cohort study that looked at records dating from January 1999 to September 2015. Patients with gout (≥ 2 ICD-9 codes) were matched 1:10 on age, sex, and year of VHA enrollment to patients without a gout ICD-9 code or a record of receiving ULT. They matched 559,243 people with gout to 5,407,379 people who did not have a diagnosis or a recorded treatment for this condition.
Over 43,331,604 person-years, Dr. Johnson and colleagues observed 137,162 CVD events in gout (incidence rate 33.96 per 1,000 person-years) vs. 879,903 in non-gout patients (IR 22.37 per 1,000 person-years). Gout was most strongly associated with HF hospitalization, with a nearly threefold higher risk (hazard ratio, 2.78; 95% confidence interval, 2.73-2.83), which attenuated but persisted after adjustment for additional CVD risk factors (adjusted hazard ratio, 1.68; 95% CI, 1.65-1.70) and excluding patients with prevalent HF (aHR, 1.60; 95% CI, 1.57-1.64).
People with gout were also at higher risk of HF-related death (aHR, 1.25; 95% CI, 1.21-1.29), MACE (aHR, 1.22; 95% CI, 1.21-1.23), and coronary artery disease–related death (aHR, 1.21; 95% CI, 1.20-1.22).
Among people with gout in the study, poor serum urate control was associated with a higher risk of all CVD events, with the highest CVD risk occurring in patients with inadequately controlled serum urate despite receipt of ULT, particularly related to HF hospitalization (aHR, 1.43; 95% CI, 1.34-1.52) and HF-related death (aHR, 1.47; 95% CI, 1.34-1.61).
Limits of the study include the generalizability of the study population. Reflecting the VHA’s patient population, 99% of the cohort were men, with 62% of the gout group and 59.4% of the control group identifying as White and non-Hispanic.
The study provides evidence that may be found only by studying medical records, Richard J. Johnson, MD, of the University of Colorado at Denver, Aurora, said in an interview.
Dr. Richard Johnson, who is not related to the author, said that only about one-third of people with gout are adequately treated, and about another one-third take urate-lowering therapy (ULT) but fail to get their serum urate level under control. But it would be unethical to design a clinical trial to study CVD risk and poorly controlled serum urate without ULT treatment.
“The only way you can figure out if uric acid lowering is going to help these guys is to actually do a study like this where you see the ones who don’t get adequate treatment versus adequate treatment and you show that there’s going to be a difference in outcome,” he said.
Dr. Richard Johnson contrasted this approach with the one used in the recently reported study that appeared to cast doubt on the link between serum uric acid levels and cardiovascular disease. The ALL-HEART trial found that allopurinol, a drug commonly used to treat gout, provided no benefit in terms of reducing cardiovascular events in patients with ischemic heart disease. But these patients did not have gout, and that was a critical difference, he said.
He noted that it was not surprising that the results of ALL-HEART were negative, given the study design.
“The ALL-HEART study treated people regardless of their uric acid level, and they also excluded subjects who had a history of gout,” he said. “Yet the risk associated with uric acid occurs primarily among those with elevated serum uric acid levels and those with gout.”
The study received funding from the Rheumatology Research Foundation and the VHA. Neither Dr. Tate Johnson nor Dr. Richard Johnson had any relevant disclosures.
A new study based on U.S. veterans’ medical records adds to the evidence for a link between gout – especially poorly controlled cases – and cardiovascular disease (CVD) risk, Tate Johnson, MD, reported at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network.
Gout was associated with a 68% increased risk of heart failure (HF) hospitalization, 25% increased risk of HF-related death, and a 22% increased risk of major adverse cardiovascular events (MACE), said Dr. Johnson, of the division of rheumatology at the University of Nebraska, Omaha.
Poorly controlled serum urate was associated with a higher risk of cardiovascular events, regardless of the use of urate-lowering therapy (ULT). He said more research is needed to see if there is a causal link between gout, hyperuricemia – or its treatment – and CVD risk.
Dr. Johnson and colleagues used records from the Veterans Health Administration for this study. They created a retrospective, matched cohort study that looked at records dating from January 1999 to September 2015. Patients with gout (≥ 2 ICD-9 codes) were matched 1:10 on age, sex, and year of VHA enrollment to patients without a gout ICD-9 code or a record of receiving ULT. They matched 559,243 people with gout to 5,407,379 people who did not have a diagnosis or a recorded treatment for this condition.
Over 43,331,604 person-years, Dr. Johnson and colleagues observed 137,162 CVD events in gout (incidence rate 33.96 per 1,000 person-years) vs. 879,903 in non-gout patients (IR 22.37 per 1,000 person-years). Gout was most strongly associated with HF hospitalization, with a nearly threefold higher risk (hazard ratio, 2.78; 95% confidence interval, 2.73-2.83), which attenuated but persisted after adjustment for additional CVD risk factors (adjusted hazard ratio, 1.68; 95% CI, 1.65-1.70) and excluding patients with prevalent HF (aHR, 1.60; 95% CI, 1.57-1.64).
People with gout were also at higher risk of HF-related death (aHR, 1.25; 95% CI, 1.21-1.29), MACE (aHR, 1.22; 95% CI, 1.21-1.23), and coronary artery disease–related death (aHR, 1.21; 95% CI, 1.20-1.22).
Among people with gout in the study, poor serum urate control was associated with a higher risk of all CVD events, with the highest CVD risk occurring in patients with inadequately controlled serum urate despite receipt of ULT, particularly related to HF hospitalization (aHR, 1.43; 95% CI, 1.34-1.52) and HF-related death (aHR, 1.47; 95% CI, 1.34-1.61).
Limits of the study include the generalizability of the study population. Reflecting the VHA’s patient population, 99% of the cohort were men, with 62% of the gout group and 59.4% of the control group identifying as White and non-Hispanic.
The study provides evidence that may be found only by studying medical records, Richard J. Johnson, MD, of the University of Colorado at Denver, Aurora, said in an interview.
Dr. Richard Johnson, who is not related to the author, said that only about one-third of people with gout are adequately treated, and about another one-third take urate-lowering therapy (ULT) but fail to get their serum urate level under control. But it would be unethical to design a clinical trial to study CVD risk and poorly controlled serum urate without ULT treatment.
“The only way you can figure out if uric acid lowering is going to help these guys is to actually do a study like this where you see the ones who don’t get adequate treatment versus adequate treatment and you show that there’s going to be a difference in outcome,” he said.
Dr. Richard Johnson contrasted this approach with the one used in the recently reported study that appeared to cast doubt on the link between serum uric acid levels and cardiovascular disease. The ALL-HEART trial found that allopurinol, a drug commonly used to treat gout, provided no benefit in terms of reducing cardiovascular events in patients with ischemic heart disease. But these patients did not have gout, and that was a critical difference, he said.
He noted that it was not surprising that the results of ALL-HEART were negative, given the study design.
“The ALL-HEART study treated people regardless of their uric acid level, and they also excluded subjects who had a history of gout,” he said. “Yet the risk associated with uric acid occurs primarily among those with elevated serum uric acid levels and those with gout.”
The study received funding from the Rheumatology Research Foundation and the VHA. Neither Dr. Tate Johnson nor Dr. Richard Johnson had any relevant disclosures.
A new study based on U.S. veterans’ medical records adds to the evidence for a link between gout – especially poorly controlled cases – and cardiovascular disease (CVD) risk, Tate Johnson, MD, reported at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network.
Gout was associated with a 68% increased risk of heart failure (HF) hospitalization, 25% increased risk of HF-related death, and a 22% increased risk of major adverse cardiovascular events (MACE), said Dr. Johnson, of the division of rheumatology at the University of Nebraska, Omaha.
Poorly controlled serum urate was associated with a higher risk of cardiovascular events, regardless of the use of urate-lowering therapy (ULT). He said more research is needed to see if there is a causal link between gout, hyperuricemia – or its treatment – and CVD risk.
Dr. Johnson and colleagues used records from the Veterans Health Administration for this study. They created a retrospective, matched cohort study that looked at records dating from January 1999 to September 2015. Patients with gout (≥ 2 ICD-9 codes) were matched 1:10 on age, sex, and year of VHA enrollment to patients without a gout ICD-9 code or a record of receiving ULT. They matched 559,243 people with gout to 5,407,379 people who did not have a diagnosis or a recorded treatment for this condition.
Over 43,331,604 person-years, Dr. Johnson and colleagues observed 137,162 CVD events in gout (incidence rate 33.96 per 1,000 person-years) vs. 879,903 in non-gout patients (IR 22.37 per 1,000 person-years). Gout was most strongly associated with HF hospitalization, with a nearly threefold higher risk (hazard ratio, 2.78; 95% confidence interval, 2.73-2.83), which attenuated but persisted after adjustment for additional CVD risk factors (adjusted hazard ratio, 1.68; 95% CI, 1.65-1.70) and excluding patients with prevalent HF (aHR, 1.60; 95% CI, 1.57-1.64).
People with gout were also at higher risk of HF-related death (aHR, 1.25; 95% CI, 1.21-1.29), MACE (aHR, 1.22; 95% CI, 1.21-1.23), and coronary artery disease–related death (aHR, 1.21; 95% CI, 1.20-1.22).
Among people with gout in the study, poor serum urate control was associated with a higher risk of all CVD events, with the highest CVD risk occurring in patients with inadequately controlled serum urate despite receipt of ULT, particularly related to HF hospitalization (aHR, 1.43; 95% CI, 1.34-1.52) and HF-related death (aHR, 1.47; 95% CI, 1.34-1.61).
Limits of the study include the generalizability of the study population. Reflecting the VHA’s patient population, 99% of the cohort were men, with 62% of the gout group and 59.4% of the control group identifying as White and non-Hispanic.
The study provides evidence that may be found only by studying medical records, Richard J. Johnson, MD, of the University of Colorado at Denver, Aurora, said in an interview.
Dr. Richard Johnson, who is not related to the author, said that only about one-third of people with gout are adequately treated, and about another one-third take urate-lowering therapy (ULT) but fail to get their serum urate level under control. But it would be unethical to design a clinical trial to study CVD risk and poorly controlled serum urate without ULT treatment.
“The only way you can figure out if uric acid lowering is going to help these guys is to actually do a study like this where you see the ones who don’t get adequate treatment versus adequate treatment and you show that there’s going to be a difference in outcome,” he said.
Dr. Richard Johnson contrasted this approach with the one used in the recently reported study that appeared to cast doubt on the link between serum uric acid levels and cardiovascular disease. The ALL-HEART trial found that allopurinol, a drug commonly used to treat gout, provided no benefit in terms of reducing cardiovascular events in patients with ischemic heart disease. But these patients did not have gout, and that was a critical difference, he said.
He noted that it was not surprising that the results of ALL-HEART were negative, given the study design.
“The ALL-HEART study treated people regardless of their uric acid level, and they also excluded subjects who had a history of gout,” he said. “Yet the risk associated with uric acid occurs primarily among those with elevated serum uric acid levels and those with gout.”
The study received funding from the Rheumatology Research Foundation and the VHA. Neither Dr. Tate Johnson nor Dr. Richard Johnson had any relevant disclosures.
FROM G-CAN 2022
Research ties gout in women to comorbidities more than genetics
Comorbidities may play a greater role than genetics women with gout, although this appears not to be true for men, Nicholas Sumpter, MSc, of the University of Alabama at Birmingham said at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network (G-CAN).
Mr. Sumpter was among the authors of a recent paper in Arthritis & Rheumatology that suggested that earlier gout onset involves the accumulation of certain allelic variants in men. This genetic risk was shared across multiple ancestral groups in the study, conducted with men of European and Polynesian ancestry, Mr. Sumpter and colleagues reported.
“There might be more than one factor in gout in men, but in women we’ve been getting at this idea that comorbidities are the big thing,” he said.
During his presentation, Mr. Sumpter offered a hypothesis that in men there might be a kind of “two-pronged attack,” with increases in serum urate linked to genetic risk, but comorbidities also playing a role. “But that may not be the case for women.”
In his presentation, Mr. Sumpter noted a paper published in March 2022 from his University of Alabama at Birmingham colleagues, Aakash V. Patel, MD, and Angelo L. Gaffo, MD. In the article, Dr. Patel and Dr. Gaffo delved into the challenges of treating women with gout given “the paucity of appropriately well-powered, randomized-controlled trials investigating the efficacy” of commonly used treatments.
“This poses major challenges for the management of female gout patients since they carry a greater burden of cardiovascular and renal morbidity, which is known to modulate the pathophysiology of gout; as such, conclusions regarding the efficacy of treatments for females cannot be extrapolated from investigative studies that are predominantly male,” they wrote, calling for increased efforts to enroll women in studies of treatments for this condition.
There’s increased interest in how gout affects women, including findings in a paper published in September in Arthritis & Rheumatology that found people with gout, especially women, appear to be at higher risk for poor COVID-19 outcomes, including hospitalization and death, regardless of COVID-19 vaccination status.
Gout has become more common in women, although this remains a condition that is far more likely to strike men.
The age-standardized prevalence of gout among women rose from 233.52 per 100,000 in 1990 to 253.49 in 2017, a gain of about 9%, according to a systematic analysis of the Global Burden of Disease Study.
That topped the roughly 5% gain seen for men in the same time frame, with the rate going from 747.48 per 100,000 to 790.90. With the aging of the global population, gout’s burden in terms of prevalence and disability is expected to increase.
Impact of obesity and healthy eating patterns
Obesity, or excess adiposity, appears to be of particular concern for women in terms of gout risk.
While obesity and genetic predisposition both are strongly associated with a higher risk of gout, the excess risk of both combined was higher than the sum of each, particularly among women, Natalie McCormick, PhD, of Massachusetts General Hospital, Boston, and coauthors reported in Annals of the Rheumatic Diseases.
These findings suggested that “addressing excess adiposity could prevent a large proportion of female gout cases in particular, as well as its cardiometabolic comorbidities, and the benefit could be greater in genetically predisposed women,” they wrote.
In general, there’s a need to re-examine the advice given by many clinicians in the past that people with gout, or those at risk for it, should follow a low-protein diet to avoid purines, Dr. McCormick said in an interview.
“Now we’re finding that a healthier diet that balances protein as well as fat intake can actually be better both for cardiovascular health and for gout prevention,” she said.
Dr. McCormick’s research on this topic includes a 2022 JAMA Internal Medicine article, and a 2021 article in Current Rheumatology Reports. In the latter article, Dr. McCormick and colleagues examined the benefits of changing habits for patients, such as following one of several well-established healthy eating patterns, including the Mediterranean and DASH diets.
With excess weight and associated cardiovascular and endocrine risks already elevated among people with gout, especially women, the “conventional low-purine (i.e., low-protein) approach to gout dietary guidance is neither helpful nor sustainable and may lead to detrimental effects related to worsening insulin resistance as a result of substitution of healthy proteins with unhealthy carbohydrates or fats,” they wrote. “Rather, by focusing our dietary recommendations on healthy eating patterns which have been proven to reduce cardiometabolic risk factors, as opposed to singular ‘good’ or ‘bad’ food items or groups, the beneficial effects of such diets on relevant gout endpoints should naturally follow for the majority of typical gout cases, mediated through changes in insulin resistance.”
Mr. Sumpter and Dr. McCormick had no competing interests to declare.
Comorbidities may play a greater role than genetics women with gout, although this appears not to be true for men, Nicholas Sumpter, MSc, of the University of Alabama at Birmingham said at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network (G-CAN).
Mr. Sumpter was among the authors of a recent paper in Arthritis & Rheumatology that suggested that earlier gout onset involves the accumulation of certain allelic variants in men. This genetic risk was shared across multiple ancestral groups in the study, conducted with men of European and Polynesian ancestry, Mr. Sumpter and colleagues reported.
“There might be more than one factor in gout in men, but in women we’ve been getting at this idea that comorbidities are the big thing,” he said.
During his presentation, Mr. Sumpter offered a hypothesis that in men there might be a kind of “two-pronged attack,” with increases in serum urate linked to genetic risk, but comorbidities also playing a role. “But that may not be the case for women.”
In his presentation, Mr. Sumpter noted a paper published in March 2022 from his University of Alabama at Birmingham colleagues, Aakash V. Patel, MD, and Angelo L. Gaffo, MD. In the article, Dr. Patel and Dr. Gaffo delved into the challenges of treating women with gout given “the paucity of appropriately well-powered, randomized-controlled trials investigating the efficacy” of commonly used treatments.
“This poses major challenges for the management of female gout patients since they carry a greater burden of cardiovascular and renal morbidity, which is known to modulate the pathophysiology of gout; as such, conclusions regarding the efficacy of treatments for females cannot be extrapolated from investigative studies that are predominantly male,” they wrote, calling for increased efforts to enroll women in studies of treatments for this condition.
There’s increased interest in how gout affects women, including findings in a paper published in September in Arthritis & Rheumatology that found people with gout, especially women, appear to be at higher risk for poor COVID-19 outcomes, including hospitalization and death, regardless of COVID-19 vaccination status.
Gout has become more common in women, although this remains a condition that is far more likely to strike men.
The age-standardized prevalence of gout among women rose from 233.52 per 100,000 in 1990 to 253.49 in 2017, a gain of about 9%, according to a systematic analysis of the Global Burden of Disease Study.
That topped the roughly 5% gain seen for men in the same time frame, with the rate going from 747.48 per 100,000 to 790.90. With the aging of the global population, gout’s burden in terms of prevalence and disability is expected to increase.
Impact of obesity and healthy eating patterns
Obesity, or excess adiposity, appears to be of particular concern for women in terms of gout risk.
While obesity and genetic predisposition both are strongly associated with a higher risk of gout, the excess risk of both combined was higher than the sum of each, particularly among women, Natalie McCormick, PhD, of Massachusetts General Hospital, Boston, and coauthors reported in Annals of the Rheumatic Diseases.
These findings suggested that “addressing excess adiposity could prevent a large proportion of female gout cases in particular, as well as its cardiometabolic comorbidities, and the benefit could be greater in genetically predisposed women,” they wrote.
In general, there’s a need to re-examine the advice given by many clinicians in the past that people with gout, or those at risk for it, should follow a low-protein diet to avoid purines, Dr. McCormick said in an interview.
“Now we’re finding that a healthier diet that balances protein as well as fat intake can actually be better both for cardiovascular health and for gout prevention,” she said.
Dr. McCormick’s research on this topic includes a 2022 JAMA Internal Medicine article, and a 2021 article in Current Rheumatology Reports. In the latter article, Dr. McCormick and colleagues examined the benefits of changing habits for patients, such as following one of several well-established healthy eating patterns, including the Mediterranean and DASH diets.
With excess weight and associated cardiovascular and endocrine risks already elevated among people with gout, especially women, the “conventional low-purine (i.e., low-protein) approach to gout dietary guidance is neither helpful nor sustainable and may lead to detrimental effects related to worsening insulin resistance as a result of substitution of healthy proteins with unhealthy carbohydrates or fats,” they wrote. “Rather, by focusing our dietary recommendations on healthy eating patterns which have been proven to reduce cardiometabolic risk factors, as opposed to singular ‘good’ or ‘bad’ food items or groups, the beneficial effects of such diets on relevant gout endpoints should naturally follow for the majority of typical gout cases, mediated through changes in insulin resistance.”
Mr. Sumpter and Dr. McCormick had no competing interests to declare.
Comorbidities may play a greater role than genetics women with gout, although this appears not to be true for men, Nicholas Sumpter, MSc, of the University of Alabama at Birmingham said at the annual research symposium of the Gout, Hyperuricemia, and Crystal Associated Disease Network (G-CAN).
Mr. Sumpter was among the authors of a recent paper in Arthritis & Rheumatology that suggested that earlier gout onset involves the accumulation of certain allelic variants in men. This genetic risk was shared across multiple ancestral groups in the study, conducted with men of European and Polynesian ancestry, Mr. Sumpter and colleagues reported.
“There might be more than one factor in gout in men, but in women we’ve been getting at this idea that comorbidities are the big thing,” he said.
During his presentation, Mr. Sumpter offered a hypothesis that in men there might be a kind of “two-pronged attack,” with increases in serum urate linked to genetic risk, but comorbidities also playing a role. “But that may not be the case for women.”
In his presentation, Mr. Sumpter noted a paper published in March 2022 from his University of Alabama at Birmingham colleagues, Aakash V. Patel, MD, and Angelo L. Gaffo, MD. In the article, Dr. Patel and Dr. Gaffo delved into the challenges of treating women with gout given “the paucity of appropriately well-powered, randomized-controlled trials investigating the efficacy” of commonly used treatments.
“This poses major challenges for the management of female gout patients since they carry a greater burden of cardiovascular and renal morbidity, which is known to modulate the pathophysiology of gout; as such, conclusions regarding the efficacy of treatments for females cannot be extrapolated from investigative studies that are predominantly male,” they wrote, calling for increased efforts to enroll women in studies of treatments for this condition.
There’s increased interest in how gout affects women, including findings in a paper published in September in Arthritis & Rheumatology that found people with gout, especially women, appear to be at higher risk for poor COVID-19 outcomes, including hospitalization and death, regardless of COVID-19 vaccination status.
Gout has become more common in women, although this remains a condition that is far more likely to strike men.
The age-standardized prevalence of gout among women rose from 233.52 per 100,000 in 1990 to 253.49 in 2017, a gain of about 9%, according to a systematic analysis of the Global Burden of Disease Study.
That topped the roughly 5% gain seen for men in the same time frame, with the rate going from 747.48 per 100,000 to 790.90. With the aging of the global population, gout’s burden in terms of prevalence and disability is expected to increase.
Impact of obesity and healthy eating patterns
Obesity, or excess adiposity, appears to be of particular concern for women in terms of gout risk.
While obesity and genetic predisposition both are strongly associated with a higher risk of gout, the excess risk of both combined was higher than the sum of each, particularly among women, Natalie McCormick, PhD, of Massachusetts General Hospital, Boston, and coauthors reported in Annals of the Rheumatic Diseases.
These findings suggested that “addressing excess adiposity could prevent a large proportion of female gout cases in particular, as well as its cardiometabolic comorbidities, and the benefit could be greater in genetically predisposed women,” they wrote.
In general, there’s a need to re-examine the advice given by many clinicians in the past that people with gout, or those at risk for it, should follow a low-protein diet to avoid purines, Dr. McCormick said in an interview.
“Now we’re finding that a healthier diet that balances protein as well as fat intake can actually be better both for cardiovascular health and for gout prevention,” she said.
Dr. McCormick’s research on this topic includes a 2022 JAMA Internal Medicine article, and a 2021 article in Current Rheumatology Reports. In the latter article, Dr. McCormick and colleagues examined the benefits of changing habits for patients, such as following one of several well-established healthy eating patterns, including the Mediterranean and DASH diets.
With excess weight and associated cardiovascular and endocrine risks already elevated among people with gout, especially women, the “conventional low-purine (i.e., low-protein) approach to gout dietary guidance is neither helpful nor sustainable and may lead to detrimental effects related to worsening insulin resistance as a result of substitution of healthy proteins with unhealthy carbohydrates or fats,” they wrote. “Rather, by focusing our dietary recommendations on healthy eating patterns which have been proven to reduce cardiometabolic risk factors, as opposed to singular ‘good’ or ‘bad’ food items or groups, the beneficial effects of such diets on relevant gout endpoints should naturally follow for the majority of typical gout cases, mediated through changes in insulin resistance.”
Mr. Sumpter and Dr. McCormick had no competing interests to declare.
FROM G-CAN 2022
Worse COVID outcomes seen with gout, particularly in women
People with gout, especially women, appear to be at higher risk for poor COVID-19 outcomes, including hospitalization and death, regardless of COVID-19 vaccination status, researchers suggest.
“We found that the risks of SARS-CoV-2 infection, 30-day hospitalization, and 30-day death among individuals with gout were higher than the general population irrespective of the vaccination status,” lead study author Dongxing Xie, MD, PhD, Xiangya Hospital, Central South University, Changsha, China, and his colleagues write in their large population study. “This finding informs individuals with gout, especially women, that additional measures, even after vaccination, should be considered in order to mitigate the risk of SARS-CoV-2 infection and its severe sequelae.”
People with gout, the most common inflammatory arthritis, often have other conditions that are linked to higher risk for SARS-CoV-2 infection and poor outcomes as well, including obesity, cardiovascular disease, and chronic kidney disease, the authors write. And elevated serum urate may contribute to inflammation and possible COVID-19 complications. But unlike in the case of diseases such as lupus and rheumatoid arthritis, little is known about SARS-CoV-2 infection risk among patients with gout.
As reported in Arthritis & Rheumatology, Dr. Xie and his research team used the Health Improvement Network ([THIN], now called IQVIA Medical Research Database) repository of medical conditions, demographics, and other details of around 17 million people in the United Kingdom to estimate the risk for SARS-CoV-2 infection, hospitalization, and death in people with gout. They compared those outcomes with outcomes of people without gout and compared outcomes of vaccinated vs. nonvaccinated participants.
From December 2020 through October 2021, the researchers investigated the risk for SARS-CoV-2 breakthrough infection in vaccinated people between age 18 and 90 years who had gout and were hospitalized within 30 days after the infection diagnosis or who died within 30 days after the diagnosis. They compared these outcomes with the outcomes of people in the general population without gout after COVID-19 vaccination. They also compared the risk for SARS-CoV-2 infection and its severe outcomes between individuals with gout and the general population among unvaccinated people.
They weighted these comparisons on the basis of age, sex, body mass index, socioeconomic deprivation index score, region, and number of previous COVID-19 tests in one model. A more fully adjusted model also weighted the comparisons for lifestyle factors, comorbidities, medications, and healthcare utilization.
The vaccinated cohort consisted of 54,576 people with gout and 1,336,377 without gout from the general population. The unvaccinated cohort included 61,111 individuals with gout and 1,697,168 individuals without gout from the general population.
Women more likely to be hospitalized and die
The risk for breakthrough infection in the vaccinated cohort was significantly higher among people with gout than among those without gout in the general population, particularly for men, who had hazard ratios (HRs) ranging from 1.22 with a fully adjusted exposure score to 1.30 with a partially adjusted score, but this was not seen in women. The overall incidence of breakthrough infection per 1,000 person-months for these groups was 4.68 with gout vs. 3.76 without gout.
The researchers showed a similar pattern of a higher rate of hospitalizations for people with gout vs. without (0.42/1,000 person-months vs. 0.28); in this case, women had higher risks than did men, with HRs for women ranging from 1.55 with a fully adjusted exposure score to 1.91 with a partially adjusted score, compared with 1.22 and 1.43 for men, respectively.
People with gout had significantly higher mortality than did those without (0.06/1,000 person-months vs. 0.04), but the risk for death was only higher for women, with HRs calculated to be 2.23 in fully adjusted exposure scores and 3.01 in partially adjusted scores.
These same comparisons in the unvaccinated cohort all went in the same direction as did those in the vaccinated cohort but showed higher rates for infection (8.69/1,000 person-months vs. 6.89), hospitalization (2.57/1,000 person-months vs. 1.71), and death (0.65/1,000 person-months vs. 0.53). Similar sex-specific links between gout and risks for SARS-CoV-2 infection, hospitalization, and death were seen in the unvaccinated cohort.
Patients with gout and COVID-19 need close monitoring
Four experts who were not involved in the study encourage greater attention to the needs of patients with gout.
Pamela B. Davis, MD, PhD, research professor at Case Western Reserve University, Cleveland, told this news organization, “This study brings to attention yet another potentially vulnerable group for physicians to monitor closely if they are infected with SARS-CoV-2.
“It is not clear why women with gout are more vulnerable, but fewer women than men were in the cohort with gout, and the confidence intervals for the results in women were, in general, larger,” she said.
“The authors suggest that women with gout tend to be older and have more comorbidities than men with gout,” Dr. Davis added. “The excess risk diminishes when the model is fully adjusted for comorbidities, such as obesity, hypertension, or heart disease, suggesting that already-known antecedents of infection severity account for a great deal of the excess risk.”
Kevin D. Deane, MD, PhD, associate professor of medicine and chair in rheumatology research at the University of Colorado at Denver, Aurora, advises physicians to keep in mind other conditions linked with increased risk for severe COVID-19, including advanced age; heart, lung, or kidney problems; and autoimmune diseases.
“I would be very cautious about the finding that there was not a difference in outcomes in individuals with gout based on vaccination status,” he cautioned, urging clinicians to “still strongly recommend vaccines according to guidelines.”
Sarah E. Waldman, MD, associate clinical professor of infectious diseases at UC Davis Health in Sacramento, Calif., called the study interesting but not surprising.
“The reason for increased risk for COVID-19 infection among those with gout may have to do with their underlying inflammatory state. Additional research needs to be done on this topic.
“Retrospective population-based cohort studies can be difficult to interpret due to biases,” she added. Associations identified in this type of study do not determine causation.
“As the researchers noted, those with gout tend to have additional comorbidities as well as advanced age,” she said. “They may also seek medical care more often and be tested for SARS-CoV-2 more frequently.”
Dr. Waldman advises clinicians to counsel patients with gout about their potential increased infection risk and ways they can protect themselves, including COVID-19 vaccinations.
“The strong association between gout and COVID-19 infection could involve coexisting conditions such as diabetes, hypertension, cardiovascular disease, and chronic kidney disease,” Dr. Aung added.
Earlier studies show links between gout and severe COVID-19 outcomes
Lead author Kanon Jatuworapruk, MD, PhD, of Thammasat University in Pathumthani, Thailand, and his colleagues investigated characteristics and outcomes of people with gout who were hospitalized for COVID-19 between March 2020 and October 2021, using data from the COVID-19 Global Rheumatology Alliance registry.
“This cohort of people with gout and COVID-19 who were hospitalized had high frequencies of ventilatory support and death,” the authors write in ACR Open Rheumatology . “This suggests that patients with gout who were hospitalized for COVID-19 may be at risk of poor outcomes, perhaps related to known risk factors for poor outcomes, such as age and presence of comorbidity.”
In their study, the average age of the 163 patients was 63 years, and 85% were men. Most lived in the Western Pacific Region and North America, and 46% had two or more comorbidities, most commonly hypertension, cardiovascular disease, diabetes, chronic kidney disease, and obesity. The researchers found that:
- Sixty-eight percent of the cohort required supplemental oxygen or ventilatory support during hospitalization.
- Sixteen percent of deaths were related to COVID-19, with 73% of deaths occurring in people with two or more comorbidities.
Ruth K. Topless, assistant research fellow in the department of biochemistry at the University of Otago in Dunedin, New Zealand, is the lead author on a study she and her colleagues are conducting using the UK Biobank databases of 459,837 participants in the United Kingdom, including 15,871 people with gout, through April 6, 2021, to investigate whether gout is a risk factor for diagnosis of COVID-19 and COVID-19–related death.
“Gout is a risk factor for COVID-19-related death in the UK Biobank cohort, with an increased risk in women with gout, which was driven by risk factors independent of the metabolic comorbidities of gout,” the researchers conclude in The Lancet Rheumatology.
In their study, gout was linked with COVID-19 diagnosis (odds ratio, 1.20; 95% confidence interval, 1.11-1.29) but not with risk for COVID-19–related death in the group of patients with COVID-19 (OR, 1.20; 95% CI, 0.96-1.51). In the entire cohort, gout was linked with COVID-19–related death (OR, 1.29; 95% CI, 1.06-1.56); women with gout were at increased risk for COVID-19–related death (OR, 1.98; 95% CI, 1.34-2.94), but men with gout were not (OR, 1.16; 95% CI, 0.93-1.45). The risk for COVID-19 diagnosis was significant in the nonvaccinated group (OR, 1.21; 95% CI, 1.11-1.30) but not in the vaccinated group (OR, 1.09; 95% CI, 0.65-1.85).
Editorial authors join in recommending further related research
In a commentary in The Lancet Rheumatology about the UK Biobank and other related research, Christoffer B. Nissen, MD, of University Hospital of Southern Denmark in Sonderborg, and his co-authors call the Topless and colleagues study “an elegantly conducted analysis of data from the UK Biobank supporting the hypothesis that gout needs attention in patients with COVID-19.”
Further studies are needed to investigate to what degree a diagnosis of gout is a risk factor for COVID-19 and whether treatment modifies the risk of a severe disease course,” they write. “However, in the interim, the results of this study could be considered when risk stratifying patients with gout in view of vaccination recommendations and early treatment interventions.”
Each of the three studies received grant funding. Several of the authors of the studies report financial involvements with pharmaceutical companies. All outside experts commented by email and report no relevant financial involvements.
A version of this article first appeared on Medscape.com.
People with gout, especially women, appear to be at higher risk for poor COVID-19 outcomes, including hospitalization and death, regardless of COVID-19 vaccination status, researchers suggest.
“We found that the risks of SARS-CoV-2 infection, 30-day hospitalization, and 30-day death among individuals with gout were higher than the general population irrespective of the vaccination status,” lead study author Dongxing Xie, MD, PhD, Xiangya Hospital, Central South University, Changsha, China, and his colleagues write in their large population study. “This finding informs individuals with gout, especially women, that additional measures, even after vaccination, should be considered in order to mitigate the risk of SARS-CoV-2 infection and its severe sequelae.”
People with gout, the most common inflammatory arthritis, often have other conditions that are linked to higher risk for SARS-CoV-2 infection and poor outcomes as well, including obesity, cardiovascular disease, and chronic kidney disease, the authors write. And elevated serum urate may contribute to inflammation and possible COVID-19 complications. But unlike in the case of diseases such as lupus and rheumatoid arthritis, little is known about SARS-CoV-2 infection risk among patients with gout.
As reported in Arthritis & Rheumatology, Dr. Xie and his research team used the Health Improvement Network ([THIN], now called IQVIA Medical Research Database) repository of medical conditions, demographics, and other details of around 17 million people in the United Kingdom to estimate the risk for SARS-CoV-2 infection, hospitalization, and death in people with gout. They compared those outcomes with outcomes of people without gout and compared outcomes of vaccinated vs. nonvaccinated participants.
From December 2020 through October 2021, the researchers investigated the risk for SARS-CoV-2 breakthrough infection in vaccinated people between age 18 and 90 years who had gout and were hospitalized within 30 days after the infection diagnosis or who died within 30 days after the diagnosis. They compared these outcomes with the outcomes of people in the general population without gout after COVID-19 vaccination. They also compared the risk for SARS-CoV-2 infection and its severe outcomes between individuals with gout and the general population among unvaccinated people.
They weighted these comparisons on the basis of age, sex, body mass index, socioeconomic deprivation index score, region, and number of previous COVID-19 tests in one model. A more fully adjusted model also weighted the comparisons for lifestyle factors, comorbidities, medications, and healthcare utilization.
The vaccinated cohort consisted of 54,576 people with gout and 1,336,377 without gout from the general population. The unvaccinated cohort included 61,111 individuals with gout and 1,697,168 individuals without gout from the general population.
Women more likely to be hospitalized and die
The risk for breakthrough infection in the vaccinated cohort was significantly higher among people with gout than among those without gout in the general population, particularly for men, who had hazard ratios (HRs) ranging from 1.22 with a fully adjusted exposure score to 1.30 with a partially adjusted score, but this was not seen in women. The overall incidence of breakthrough infection per 1,000 person-months for these groups was 4.68 with gout vs. 3.76 without gout.
The researchers showed a similar pattern of a higher rate of hospitalizations for people with gout vs. without (0.42/1,000 person-months vs. 0.28); in this case, women had higher risks than did men, with HRs for women ranging from 1.55 with a fully adjusted exposure score to 1.91 with a partially adjusted score, compared with 1.22 and 1.43 for men, respectively.
People with gout had significantly higher mortality than did those without (0.06/1,000 person-months vs. 0.04), but the risk for death was only higher for women, with HRs calculated to be 2.23 in fully adjusted exposure scores and 3.01 in partially adjusted scores.
These same comparisons in the unvaccinated cohort all went in the same direction as did those in the vaccinated cohort but showed higher rates for infection (8.69/1,000 person-months vs. 6.89), hospitalization (2.57/1,000 person-months vs. 1.71), and death (0.65/1,000 person-months vs. 0.53). Similar sex-specific links between gout and risks for SARS-CoV-2 infection, hospitalization, and death were seen in the unvaccinated cohort.
Patients with gout and COVID-19 need close monitoring
Four experts who were not involved in the study encourage greater attention to the needs of patients with gout.
Pamela B. Davis, MD, PhD, research professor at Case Western Reserve University, Cleveland, told this news organization, “This study brings to attention yet another potentially vulnerable group for physicians to monitor closely if they are infected with SARS-CoV-2.
“It is not clear why women with gout are more vulnerable, but fewer women than men were in the cohort with gout, and the confidence intervals for the results in women were, in general, larger,” she said.
“The authors suggest that women with gout tend to be older and have more comorbidities than men with gout,” Dr. Davis added. “The excess risk diminishes when the model is fully adjusted for comorbidities, such as obesity, hypertension, or heart disease, suggesting that already-known antecedents of infection severity account for a great deal of the excess risk.”
Kevin D. Deane, MD, PhD, associate professor of medicine and chair in rheumatology research at the University of Colorado at Denver, Aurora, advises physicians to keep in mind other conditions linked with increased risk for severe COVID-19, including advanced age; heart, lung, or kidney problems; and autoimmune diseases.
“I would be very cautious about the finding that there was not a difference in outcomes in individuals with gout based on vaccination status,” he cautioned, urging clinicians to “still strongly recommend vaccines according to guidelines.”
Sarah E. Waldman, MD, associate clinical professor of infectious diseases at UC Davis Health in Sacramento, Calif., called the study interesting but not surprising.
“The reason for increased risk for COVID-19 infection among those with gout may have to do with their underlying inflammatory state. Additional research needs to be done on this topic.
“Retrospective population-based cohort studies can be difficult to interpret due to biases,” she added. Associations identified in this type of study do not determine causation.
“As the researchers noted, those with gout tend to have additional comorbidities as well as advanced age,” she said. “They may also seek medical care more often and be tested for SARS-CoV-2 more frequently.”
Dr. Waldman advises clinicians to counsel patients with gout about their potential increased infection risk and ways they can protect themselves, including COVID-19 vaccinations.
“The strong association between gout and COVID-19 infection could involve coexisting conditions such as diabetes, hypertension, cardiovascular disease, and chronic kidney disease,” Dr. Aung added.
Earlier studies show links between gout and severe COVID-19 outcomes
Lead author Kanon Jatuworapruk, MD, PhD, of Thammasat University in Pathumthani, Thailand, and his colleagues investigated characteristics and outcomes of people with gout who were hospitalized for COVID-19 between March 2020 and October 2021, using data from the COVID-19 Global Rheumatology Alliance registry.
“This cohort of people with gout and COVID-19 who were hospitalized had high frequencies of ventilatory support and death,” the authors write in ACR Open Rheumatology . “This suggests that patients with gout who were hospitalized for COVID-19 may be at risk of poor outcomes, perhaps related to known risk factors for poor outcomes, such as age and presence of comorbidity.”
In their study, the average age of the 163 patients was 63 years, and 85% were men. Most lived in the Western Pacific Region and North America, and 46% had two or more comorbidities, most commonly hypertension, cardiovascular disease, diabetes, chronic kidney disease, and obesity. The researchers found that:
- Sixty-eight percent of the cohort required supplemental oxygen or ventilatory support during hospitalization.
- Sixteen percent of deaths were related to COVID-19, with 73% of deaths occurring in people with two or more comorbidities.
Ruth K. Topless, assistant research fellow in the department of biochemistry at the University of Otago in Dunedin, New Zealand, is the lead author on a study she and her colleagues are conducting using the UK Biobank databases of 459,837 participants in the United Kingdom, including 15,871 people with gout, through April 6, 2021, to investigate whether gout is a risk factor for diagnosis of COVID-19 and COVID-19–related death.
“Gout is a risk factor for COVID-19-related death in the UK Biobank cohort, with an increased risk in women with gout, which was driven by risk factors independent of the metabolic comorbidities of gout,” the researchers conclude in The Lancet Rheumatology.
In their study, gout was linked with COVID-19 diagnosis (odds ratio, 1.20; 95% confidence interval, 1.11-1.29) but not with risk for COVID-19–related death in the group of patients with COVID-19 (OR, 1.20; 95% CI, 0.96-1.51). In the entire cohort, gout was linked with COVID-19–related death (OR, 1.29; 95% CI, 1.06-1.56); women with gout were at increased risk for COVID-19–related death (OR, 1.98; 95% CI, 1.34-2.94), but men with gout were not (OR, 1.16; 95% CI, 0.93-1.45). The risk for COVID-19 diagnosis was significant in the nonvaccinated group (OR, 1.21; 95% CI, 1.11-1.30) but not in the vaccinated group (OR, 1.09; 95% CI, 0.65-1.85).
Editorial authors join in recommending further related research
In a commentary in The Lancet Rheumatology about the UK Biobank and other related research, Christoffer B. Nissen, MD, of University Hospital of Southern Denmark in Sonderborg, and his co-authors call the Topless and colleagues study “an elegantly conducted analysis of data from the UK Biobank supporting the hypothesis that gout needs attention in patients with COVID-19.”
Further studies are needed to investigate to what degree a diagnosis of gout is a risk factor for COVID-19 and whether treatment modifies the risk of a severe disease course,” they write. “However, in the interim, the results of this study could be considered when risk stratifying patients with gout in view of vaccination recommendations and early treatment interventions.”
Each of the three studies received grant funding. Several of the authors of the studies report financial involvements with pharmaceutical companies. All outside experts commented by email and report no relevant financial involvements.
A version of this article first appeared on Medscape.com.
People with gout, especially women, appear to be at higher risk for poor COVID-19 outcomes, including hospitalization and death, regardless of COVID-19 vaccination status, researchers suggest.
“We found that the risks of SARS-CoV-2 infection, 30-day hospitalization, and 30-day death among individuals with gout were higher than the general population irrespective of the vaccination status,” lead study author Dongxing Xie, MD, PhD, Xiangya Hospital, Central South University, Changsha, China, and his colleagues write in their large population study. “This finding informs individuals with gout, especially women, that additional measures, even after vaccination, should be considered in order to mitigate the risk of SARS-CoV-2 infection and its severe sequelae.”
People with gout, the most common inflammatory arthritis, often have other conditions that are linked to higher risk for SARS-CoV-2 infection and poor outcomes as well, including obesity, cardiovascular disease, and chronic kidney disease, the authors write. And elevated serum urate may contribute to inflammation and possible COVID-19 complications. But unlike in the case of diseases such as lupus and rheumatoid arthritis, little is known about SARS-CoV-2 infection risk among patients with gout.
As reported in Arthritis & Rheumatology, Dr. Xie and his research team used the Health Improvement Network ([THIN], now called IQVIA Medical Research Database) repository of medical conditions, demographics, and other details of around 17 million people in the United Kingdom to estimate the risk for SARS-CoV-2 infection, hospitalization, and death in people with gout. They compared those outcomes with outcomes of people without gout and compared outcomes of vaccinated vs. nonvaccinated participants.
From December 2020 through October 2021, the researchers investigated the risk for SARS-CoV-2 breakthrough infection in vaccinated people between age 18 and 90 years who had gout and were hospitalized within 30 days after the infection diagnosis or who died within 30 days after the diagnosis. They compared these outcomes with the outcomes of people in the general population without gout after COVID-19 vaccination. They also compared the risk for SARS-CoV-2 infection and its severe outcomes between individuals with gout and the general population among unvaccinated people.
They weighted these comparisons on the basis of age, sex, body mass index, socioeconomic deprivation index score, region, and number of previous COVID-19 tests in one model. A more fully adjusted model also weighted the comparisons for lifestyle factors, comorbidities, medications, and healthcare utilization.
The vaccinated cohort consisted of 54,576 people with gout and 1,336,377 without gout from the general population. The unvaccinated cohort included 61,111 individuals with gout and 1,697,168 individuals without gout from the general population.
Women more likely to be hospitalized and die
The risk for breakthrough infection in the vaccinated cohort was significantly higher among people with gout than among those without gout in the general population, particularly for men, who had hazard ratios (HRs) ranging from 1.22 with a fully adjusted exposure score to 1.30 with a partially adjusted score, but this was not seen in women. The overall incidence of breakthrough infection per 1,000 person-months for these groups was 4.68 with gout vs. 3.76 without gout.
The researchers showed a similar pattern of a higher rate of hospitalizations for people with gout vs. without (0.42/1,000 person-months vs. 0.28); in this case, women had higher risks than did men, with HRs for women ranging from 1.55 with a fully adjusted exposure score to 1.91 with a partially adjusted score, compared with 1.22 and 1.43 for men, respectively.
People with gout had significantly higher mortality than did those without (0.06/1,000 person-months vs. 0.04), but the risk for death was only higher for women, with HRs calculated to be 2.23 in fully adjusted exposure scores and 3.01 in partially adjusted scores.
These same comparisons in the unvaccinated cohort all went in the same direction as did those in the vaccinated cohort but showed higher rates for infection (8.69/1,000 person-months vs. 6.89), hospitalization (2.57/1,000 person-months vs. 1.71), and death (0.65/1,000 person-months vs. 0.53). Similar sex-specific links between gout and risks for SARS-CoV-2 infection, hospitalization, and death were seen in the unvaccinated cohort.
Patients with gout and COVID-19 need close monitoring
Four experts who were not involved in the study encourage greater attention to the needs of patients with gout.
Pamela B. Davis, MD, PhD, research professor at Case Western Reserve University, Cleveland, told this news organization, “This study brings to attention yet another potentially vulnerable group for physicians to monitor closely if they are infected with SARS-CoV-2.
“It is not clear why women with gout are more vulnerable, but fewer women than men were in the cohort with gout, and the confidence intervals for the results in women were, in general, larger,” she said.
“The authors suggest that women with gout tend to be older and have more comorbidities than men with gout,” Dr. Davis added. “The excess risk diminishes when the model is fully adjusted for comorbidities, such as obesity, hypertension, or heart disease, suggesting that already-known antecedents of infection severity account for a great deal of the excess risk.”
Kevin D. Deane, MD, PhD, associate professor of medicine and chair in rheumatology research at the University of Colorado at Denver, Aurora, advises physicians to keep in mind other conditions linked with increased risk for severe COVID-19, including advanced age; heart, lung, or kidney problems; and autoimmune diseases.
“I would be very cautious about the finding that there was not a difference in outcomes in individuals with gout based on vaccination status,” he cautioned, urging clinicians to “still strongly recommend vaccines according to guidelines.”
Sarah E. Waldman, MD, associate clinical professor of infectious diseases at UC Davis Health in Sacramento, Calif., called the study interesting but not surprising.
“The reason for increased risk for COVID-19 infection among those with gout may have to do with their underlying inflammatory state. Additional research needs to be done on this topic.
“Retrospective population-based cohort studies can be difficult to interpret due to biases,” she added. Associations identified in this type of study do not determine causation.
“As the researchers noted, those with gout tend to have additional comorbidities as well as advanced age,” she said. “They may also seek medical care more often and be tested for SARS-CoV-2 more frequently.”
Dr. Waldman advises clinicians to counsel patients with gout about their potential increased infection risk and ways they can protect themselves, including COVID-19 vaccinations.
“The strong association between gout and COVID-19 infection could involve coexisting conditions such as diabetes, hypertension, cardiovascular disease, and chronic kidney disease,” Dr. Aung added.
Earlier studies show links between gout and severe COVID-19 outcomes
Lead author Kanon Jatuworapruk, MD, PhD, of Thammasat University in Pathumthani, Thailand, and his colleagues investigated characteristics and outcomes of people with gout who were hospitalized for COVID-19 between March 2020 and October 2021, using data from the COVID-19 Global Rheumatology Alliance registry.
“This cohort of people with gout and COVID-19 who were hospitalized had high frequencies of ventilatory support and death,” the authors write in ACR Open Rheumatology . “This suggests that patients with gout who were hospitalized for COVID-19 may be at risk of poor outcomes, perhaps related to known risk factors for poor outcomes, such as age and presence of comorbidity.”
In their study, the average age of the 163 patients was 63 years, and 85% were men. Most lived in the Western Pacific Region and North America, and 46% had two or more comorbidities, most commonly hypertension, cardiovascular disease, diabetes, chronic kidney disease, and obesity. The researchers found that:
- Sixty-eight percent of the cohort required supplemental oxygen or ventilatory support during hospitalization.
- Sixteen percent of deaths were related to COVID-19, with 73% of deaths occurring in people with two or more comorbidities.
Ruth K. Topless, assistant research fellow in the department of biochemistry at the University of Otago in Dunedin, New Zealand, is the lead author on a study she and her colleagues are conducting using the UK Biobank databases of 459,837 participants in the United Kingdom, including 15,871 people with gout, through April 6, 2021, to investigate whether gout is a risk factor for diagnosis of COVID-19 and COVID-19–related death.
“Gout is a risk factor for COVID-19-related death in the UK Biobank cohort, with an increased risk in women with gout, which was driven by risk factors independent of the metabolic comorbidities of gout,” the researchers conclude in The Lancet Rheumatology.
In their study, gout was linked with COVID-19 diagnosis (odds ratio, 1.20; 95% confidence interval, 1.11-1.29) but not with risk for COVID-19–related death in the group of patients with COVID-19 (OR, 1.20; 95% CI, 0.96-1.51). In the entire cohort, gout was linked with COVID-19–related death (OR, 1.29; 95% CI, 1.06-1.56); women with gout were at increased risk for COVID-19–related death (OR, 1.98; 95% CI, 1.34-2.94), but men with gout were not (OR, 1.16; 95% CI, 0.93-1.45). The risk for COVID-19 diagnosis was significant in the nonvaccinated group (OR, 1.21; 95% CI, 1.11-1.30) but not in the vaccinated group (OR, 1.09; 95% CI, 0.65-1.85).
Editorial authors join in recommending further related research
In a commentary in The Lancet Rheumatology about the UK Biobank and other related research, Christoffer B. Nissen, MD, of University Hospital of Southern Denmark in Sonderborg, and his co-authors call the Topless and colleagues study “an elegantly conducted analysis of data from the UK Biobank supporting the hypothesis that gout needs attention in patients with COVID-19.”
Further studies are needed to investigate to what degree a diagnosis of gout is a risk factor for COVID-19 and whether treatment modifies the risk of a severe disease course,” they write. “However, in the interim, the results of this study could be considered when risk stratifying patients with gout in view of vaccination recommendations and early treatment interventions.”
Each of the three studies received grant funding. Several of the authors of the studies report financial involvements with pharmaceutical companies. All outside experts commented by email and report no relevant financial involvements.
A version of this article first appeared on Medscape.com.
Could vitamin C help reduce gout?
Could taking vitamin C help reduce the chances of developing gout? A new study sheds light on this possibility.
Gout is a form of inflammatory arthritis that has been on the rise in the United States in recent decades. Considered a lifestyle disease, some research has shown that instances of the condition have more than doubled in recent years as rates of obesity have skyrocketed. It’s caused by uric acid in the blood that builds up and crystallizes in the joints. Flare-ups are so intense that the joints can turn a cherry red and vibrate with intense – and sometimes seemingly intolerable – pain.
While there are effective treatments, many people fail to take their medications when they’re not in pain, and if the condition goes unchecked, it can get much worse and cause permanent damage to the joints.
“Gout can cause flare-ups that vary in frequency and severity; but sometimes when people aren’t experiencing them, they’re less likely to stay on top of their medications,” said Stephen Juraschek, MD, an assistant professor of medicine at Harvard Medical School, Boston.
That’s why lifestyle interventions are seen as particularly relevant to a disease like gout. Vitamin C, for example, has few side effects, and for those with higher levels of uric acid in the blood, it could reduce the likelihood of getting the condition. A recent study published in The American Journal of Clinical Nutrition found that people who were given 500 mg of vitamin C versus a placebo had a 12% reduced risk of getting gout. The study of over 14,000 male doctors showed that men who weren’t overweight had the most significant reduction in the risk of getting the condition. (Excess weight has been shown to increase the risk of gout.)
As part of the study, participants responded to a questionnaire that asked whether they had ever been diagnosed with gout. Other studies have shown that vitamin C reduced the levels of urate in people without gout and broke down uric crystals in the blood, but this study took it a step further to show that the supplement actually reduced the risk of getting the condition.
“In addition to lowering levels of uric acid in the body, it’s thought that vitamin C may also minimize the inflammatory response to urate crystals,” said Dr. Juraschek. That’s because when flare-ups develop in joints throughout the body, much of the painful irritation is caused by the immune system’s response as it fights to break down the crystals.
Dr. Juraschek said this likely wouldn’t change recommendations for patients with serious gout, but it could still have an impact.
“For individuals who were told that they have gout but have had fewer flare-ups, they might be more open to taking vitamin C,” he said.
Will Settle, 42, of Hilton Head, S.C., was not involved in the study, but he said he would be inclined to try most any safe preventive method. Gout runs in his family. His father and grandfather had it, and now, so does he. His flare-ups have slowed in recent years, which he said has a lot to do with his diet and lifestyle. He stopped eating seafood, started drinking more water, and stopped drinking as much alcohol – all of which he thinks has had a huge impact on the severity of his condition. (Both seafood and beer contain high levels of purines, which have been shown to increase the buildup of uric acid in the blood.) Mr. Settle said that other simple lifestyle changes like vitamin C would be an easy addition to his routine with few downsides. Plus, he hates having to take colchicine, a medication that’s meant to relieve pain but causes him intense diarrhea when he takes it.
“Anything to reduce my flare-ups without having to take colchicine,” he said.
But the jury is still out as to whether vitamin C will have any real benefits. Study coauthor Robert H. Shmerling, MD, is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center, New York. He said the study shows that the effect of vitamin C in those undiagnosed with gout was rather modest. Also, vitamin C did not show a reduction in gout flare-ups in those who were already diagnosed with the condition. Not to mention that the study lacked diversity, as the people in it were all male and mostly white. Still, there’s little downside risk to taking vitamin C, and it might end up being worthwhile.
“Maybe it will turn out to be an effective treatment in those who are at high risk, but we’re not there yet,” he said.
Robert Terkeltaub, MD, chief of rheumatology at the Veterans Administration Medical Center in San Diego and a professor of medicine at the University of California, San Diego, said there’s an unmet need when it comes to tools for gout prevention.
“The disease impacts some 10 million Americans, and we need to better identify these individuals so we can intervene earlier,” he said.
While vitamin C had a small but significant association with fewer new cases of gout, it did not lower it in those who already had the disease, said Dr. Terkeltaub. What’s more, researchers didn’t measure the levels of uric acid in the blood, which would have painted a more accurate picture of whether vitamin C actually reduced it in the body.
“There remains no clarity on the potential role of vitamin C in either prevention or treatment of gout. That said, future research would be of interest,” he said.
Still, gout patients like Mr. Settle aren’t ruling it out. Anything to avoid the pain that, at times, makes it difficult for him to get out of bed. He’s seen the benefit that simple lifestyle changes can make, and he’s willing to try just about anything to live a normal, arthritis-free life.
“I’m always looking for simple ways to keep my flare-ups at bay,” he said.
A version of this article first appeared on WebMD.com.
Could taking vitamin C help reduce the chances of developing gout? A new study sheds light on this possibility.
Gout is a form of inflammatory arthritis that has been on the rise in the United States in recent decades. Considered a lifestyle disease, some research has shown that instances of the condition have more than doubled in recent years as rates of obesity have skyrocketed. It’s caused by uric acid in the blood that builds up and crystallizes in the joints. Flare-ups are so intense that the joints can turn a cherry red and vibrate with intense – and sometimes seemingly intolerable – pain.
While there are effective treatments, many people fail to take their medications when they’re not in pain, and if the condition goes unchecked, it can get much worse and cause permanent damage to the joints.
“Gout can cause flare-ups that vary in frequency and severity; but sometimes when people aren’t experiencing them, they’re less likely to stay on top of their medications,” said Stephen Juraschek, MD, an assistant professor of medicine at Harvard Medical School, Boston.
That’s why lifestyle interventions are seen as particularly relevant to a disease like gout. Vitamin C, for example, has few side effects, and for those with higher levels of uric acid in the blood, it could reduce the likelihood of getting the condition. A recent study published in The American Journal of Clinical Nutrition found that people who were given 500 mg of vitamin C versus a placebo had a 12% reduced risk of getting gout. The study of over 14,000 male doctors showed that men who weren’t overweight had the most significant reduction in the risk of getting the condition. (Excess weight has been shown to increase the risk of gout.)
As part of the study, participants responded to a questionnaire that asked whether they had ever been diagnosed with gout. Other studies have shown that vitamin C reduced the levels of urate in people without gout and broke down uric crystals in the blood, but this study took it a step further to show that the supplement actually reduced the risk of getting the condition.
“In addition to lowering levels of uric acid in the body, it’s thought that vitamin C may also minimize the inflammatory response to urate crystals,” said Dr. Juraschek. That’s because when flare-ups develop in joints throughout the body, much of the painful irritation is caused by the immune system’s response as it fights to break down the crystals.
Dr. Juraschek said this likely wouldn’t change recommendations for patients with serious gout, but it could still have an impact.
“For individuals who were told that they have gout but have had fewer flare-ups, they might be more open to taking vitamin C,” he said.
Will Settle, 42, of Hilton Head, S.C., was not involved in the study, but he said he would be inclined to try most any safe preventive method. Gout runs in his family. His father and grandfather had it, and now, so does he. His flare-ups have slowed in recent years, which he said has a lot to do with his diet and lifestyle. He stopped eating seafood, started drinking more water, and stopped drinking as much alcohol – all of which he thinks has had a huge impact on the severity of his condition. (Both seafood and beer contain high levels of purines, which have been shown to increase the buildup of uric acid in the blood.) Mr. Settle said that other simple lifestyle changes like vitamin C would be an easy addition to his routine with few downsides. Plus, he hates having to take colchicine, a medication that’s meant to relieve pain but causes him intense diarrhea when he takes it.
“Anything to reduce my flare-ups without having to take colchicine,” he said.
But the jury is still out as to whether vitamin C will have any real benefits. Study coauthor Robert H. Shmerling, MD, is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center, New York. He said the study shows that the effect of vitamin C in those undiagnosed with gout was rather modest. Also, vitamin C did not show a reduction in gout flare-ups in those who were already diagnosed with the condition. Not to mention that the study lacked diversity, as the people in it were all male and mostly white. Still, there’s little downside risk to taking vitamin C, and it might end up being worthwhile.
“Maybe it will turn out to be an effective treatment in those who are at high risk, but we’re not there yet,” he said.
Robert Terkeltaub, MD, chief of rheumatology at the Veterans Administration Medical Center in San Diego and a professor of medicine at the University of California, San Diego, said there’s an unmet need when it comes to tools for gout prevention.
“The disease impacts some 10 million Americans, and we need to better identify these individuals so we can intervene earlier,” he said.
While vitamin C had a small but significant association with fewer new cases of gout, it did not lower it in those who already had the disease, said Dr. Terkeltaub. What’s more, researchers didn’t measure the levels of uric acid in the blood, which would have painted a more accurate picture of whether vitamin C actually reduced it in the body.
“There remains no clarity on the potential role of vitamin C in either prevention or treatment of gout. That said, future research would be of interest,” he said.
Still, gout patients like Mr. Settle aren’t ruling it out. Anything to avoid the pain that, at times, makes it difficult for him to get out of bed. He’s seen the benefit that simple lifestyle changes can make, and he’s willing to try just about anything to live a normal, arthritis-free life.
“I’m always looking for simple ways to keep my flare-ups at bay,” he said.
A version of this article first appeared on WebMD.com.
Could taking vitamin C help reduce the chances of developing gout? A new study sheds light on this possibility.
Gout is a form of inflammatory arthritis that has been on the rise in the United States in recent decades. Considered a lifestyle disease, some research has shown that instances of the condition have more than doubled in recent years as rates of obesity have skyrocketed. It’s caused by uric acid in the blood that builds up and crystallizes in the joints. Flare-ups are so intense that the joints can turn a cherry red and vibrate with intense – and sometimes seemingly intolerable – pain.
While there are effective treatments, many people fail to take their medications when they’re not in pain, and if the condition goes unchecked, it can get much worse and cause permanent damage to the joints.
“Gout can cause flare-ups that vary in frequency and severity; but sometimes when people aren’t experiencing them, they’re less likely to stay on top of their medications,” said Stephen Juraschek, MD, an assistant professor of medicine at Harvard Medical School, Boston.
That’s why lifestyle interventions are seen as particularly relevant to a disease like gout. Vitamin C, for example, has few side effects, and for those with higher levels of uric acid in the blood, it could reduce the likelihood of getting the condition. A recent study published in The American Journal of Clinical Nutrition found that people who were given 500 mg of vitamin C versus a placebo had a 12% reduced risk of getting gout. The study of over 14,000 male doctors showed that men who weren’t overweight had the most significant reduction in the risk of getting the condition. (Excess weight has been shown to increase the risk of gout.)
As part of the study, participants responded to a questionnaire that asked whether they had ever been diagnosed with gout. Other studies have shown that vitamin C reduced the levels of urate in people without gout and broke down uric crystals in the blood, but this study took it a step further to show that the supplement actually reduced the risk of getting the condition.
“In addition to lowering levels of uric acid in the body, it’s thought that vitamin C may also minimize the inflammatory response to urate crystals,” said Dr. Juraschek. That’s because when flare-ups develop in joints throughout the body, much of the painful irritation is caused by the immune system’s response as it fights to break down the crystals.
Dr. Juraschek said this likely wouldn’t change recommendations for patients with serious gout, but it could still have an impact.
“For individuals who were told that they have gout but have had fewer flare-ups, they might be more open to taking vitamin C,” he said.
Will Settle, 42, of Hilton Head, S.C., was not involved in the study, but he said he would be inclined to try most any safe preventive method. Gout runs in his family. His father and grandfather had it, and now, so does he. His flare-ups have slowed in recent years, which he said has a lot to do with his diet and lifestyle. He stopped eating seafood, started drinking more water, and stopped drinking as much alcohol – all of which he thinks has had a huge impact on the severity of his condition. (Both seafood and beer contain high levels of purines, which have been shown to increase the buildup of uric acid in the blood.) Mr. Settle said that other simple lifestyle changes like vitamin C would be an easy addition to his routine with few downsides. Plus, he hates having to take colchicine, a medication that’s meant to relieve pain but causes him intense diarrhea when he takes it.
“Anything to reduce my flare-ups without having to take colchicine,” he said.
But the jury is still out as to whether vitamin C will have any real benefits. Study coauthor Robert H. Shmerling, MD, is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center, New York. He said the study shows that the effect of vitamin C in those undiagnosed with gout was rather modest. Also, vitamin C did not show a reduction in gout flare-ups in those who were already diagnosed with the condition. Not to mention that the study lacked diversity, as the people in it were all male and mostly white. Still, there’s little downside risk to taking vitamin C, and it might end up being worthwhile.
“Maybe it will turn out to be an effective treatment in those who are at high risk, but we’re not there yet,” he said.
Robert Terkeltaub, MD, chief of rheumatology at the Veterans Administration Medical Center in San Diego and a professor of medicine at the University of California, San Diego, said there’s an unmet need when it comes to tools for gout prevention.
“The disease impacts some 10 million Americans, and we need to better identify these individuals so we can intervene earlier,” he said.
While vitamin C had a small but significant association with fewer new cases of gout, it did not lower it in those who already had the disease, said Dr. Terkeltaub. What’s more, researchers didn’t measure the levels of uric acid in the blood, which would have painted a more accurate picture of whether vitamin C actually reduced it in the body.
“There remains no clarity on the potential role of vitamin C in either prevention or treatment of gout. That said, future research would be of interest,” he said.
Still, gout patients like Mr. Settle aren’t ruling it out. Anything to avoid the pain that, at times, makes it difficult for him to get out of bed. He’s seen the benefit that simple lifestyle changes can make, and he’s willing to try just about anything to live a normal, arthritis-free life.
“I’m always looking for simple ways to keep my flare-ups at bay,” he said.
A version of this article first appeared on WebMD.com.
FROM THE AMERICAN JOURNAL OF CLINICAL NUTRITION
OMERACT continues to set standards on research outcomes, enhancing the patient voice
Clinical research in rheumatology was suffering from an identity crisis of sorts 40 years ago. A lack of consensus across continents resulted in differing views about clinical outcome measures and judgments about treatments.
Patients were not allowed to be the generating source of a clinical outcome, according to Peter Tugwell, MSc, MD. “The only outcomes that were acceptable were clinician assessments, blood tests, and imaging,” said Dr. Tugwell, professor of medicine, epidemiology, and public health at the University of Ottawa (Ont.) and a practicing rheumatologist at Ottawa Hospital.
Clinicians were coming to different conclusions about patient responses to treatment when managing rheumatoid arthritis in clinical practice.
OMERACT sought to address this lack of uniformity. This international group, formed in 1992, leverages stakeholder groups to improve outcome measurement in rheumatology endpoints through a consensus-building, data-driven format.
It was originally known as “Outcome Measures in Rheumatoid Arthritis Clinical Trials,” but its leaders have since broadened its scope to “Outcome Measures in Rheumatology.” Over the years, it has evolved into an international network that assesses measurement across a wide variety of intervention studies. Now 30 years old, the network spans 40 active working groups and has influenced work in patient outcomes across 500 peer-reviewed publications.
The network meets every 2 years to address what is always a challenging agenda, said Dr. Tugwell, one of its founding members and chair. “There’s lots of strong opinions.” Participating in the discussions are individuals from all stages of seniority in rheumatology and clinical epidemiology, patient research partners, industry, approval agencies, and many countries who are committed to the spirit of OMERACT.
“The secret to our success has been getting world leaders to come together and have those discussions, work them through, and identify common ground in such a way that the approval agencies accept these outcome measures in clinical trials,” he added.
“My impression was the founders perceived a problem in the early 1990s and devised a consensus method in an attempt to quantify clinical parameters to define disease activity in rheumatoid arthritis – an important first step to do clinical trials and allow comparisons between them,” said Patricia Woo, CBE, FMedSci, FRCP, emeritus professor of pediatric rheumatology and previous head of the Centre for Paediatric and Adolescent Rheumatology at UCL, London. At that time, even disease definitions varied between the United States and Europe and other parts of the world, said Dr. Woo, who is not a part of OMERACT. “This was especially true for pediatric rheumatology.”
Fusing the continental divide
OMERACT arose from a need to streamline clinical outcome measures in rheumatology. Research papers during the 1980s demonstrated a lack of coherence in managing patients with rheumatoid arthritis in routine practice. In addition, the measures used to define clinical endpoints in clinical trials operated in silos – they were either too specific to a certain trial, overlapped with other concepts, or didn’t reflect changes in treatment.
Approval agencies in Europe and North America were approving only outcomes measures developed by their respective researchers. This was also true of patients they tested on. “This seemed crazy,” Dr. Tugwell said.
Dr. Tugwell was involved in the Cochrane collaboration, which conducts systematic reviews of best evidence across the world that assesses the magnitude of benefits versus harms.
To achieve this goal, “you need to pull studies from around the world,” he said. Maarten Boers, MD, PhD, a rheumatologist (and later professor of clinical epidemiology at Amsterdam University Medical Center) from the Netherlands, spent a year in Ontario, Canada, to train as a clinical epidemiologist. Together, Dr. Tugwell and Dr. Boers began discussing options to develop more streamlined outcome measures.
They initiated the first OMERACT conference in Maastricht, the Netherlands, in 1992. The Food and Drug Administration and European Medicines Agency participated, along with leaders of outcomes measurement in Europe and in North America.
Discussions centered on methods to develop outcomes in a meaningful fashion. During the first meeting, North American and European approval agencies agreed to accept each other’s studies and endpoints and patient reported outcomes.
Agreement was achieved on a preliminary set of outcome domains and measures that later became known as the WHO-ILAR (World Health Organization–International League of Associations for Rheumatology) core set. The set included seven outcome domains: tender joints, swollen joints, pain, physician global assessment, patient global assessment, physical disability, and acute phase reactants, and one additional outcome domain for studies lasting 1 year or more: radiographs of the joints.
“A proactive program was planned to test not only the validity of these endpoints, but also the methods for their measurement. This was the start of a continuing process,” OMERACT members said in a joint statement for this article. Meetings have since taken place every 2 years.

OMERACT accomplishments
OMERACT now requires buy-in from four continents: Asia, Australia, Europe, and North America.
Its leaders have developed an explicit process for gaining endorsement of core outcome domains and instrument measurement sets. To fully capture the possibilities of “what to measure,” i.e., “measurable aspects of health conditions,” OMERACT has developed a framework of concepts, core areas, and outcome domains. The key concepts are pathophysiology (with a core area termed “manifestations/abnormalities”) and impact (with core areas of “death/lifespan,” and “life impact,” and the optional area of “societal/resource use”). An outcome domain defines an element of a core area to measure the effects of a treatment, such as blood markers, pain intensity, physical function, or emotional well-being.
A core outcome domain set is developed by agreeing to at least one outcome domain within one of the three core areas. Subsequently, a core outcome measurement set is developed by agreeing to at least one applicable measurement instrument for each core outcome domain. This requires documentation of validity, summarized under three metrics: truth, discrimination, and feasibility.
OMERACT’s handbook provides tutelage on establishing and implementing core outcomes, and several workbooks offer guidance on developing core outcome domain sets, selecting instruments for core outcome measurement sets, and OMERACT methodology.
All this work has led to widespread adoption.
Approval agencies have accepted OMERACT’s filter and methods advances, which have been adopted by many research groups in rheumatology and among nonrheumatology research groups. Organizations such as the U.S. National Institutes of Health’s National Institute of Neurological Disorders and Stroke have sought its advice.
Its core outcomes have been adopted and used for approval in the great majority of studies on rheumatoid arthritis, Dr. Tugwell said.
Several BMJ articles underscore the influence and uptake of OMERACT’s core outcome set. One 2017 paper, which analyzed 273 randomized trials of rheumatoid arthritis drug treatments on ClinicalTrials.gov, found that the WHO-ILAR arthritis core outcome set was reported in 81% of the studies. “The adoption of a core outcome set has the potential to increase consistency in outcomes measured across trials and ensure that trials are more likely to measure appropriate outcomes,” the authors concluded.
Since the initial 1992 meeting, OMERACT has broadened its focus from rheumatoid arthritis to 25 other musculoskeletal conditions.
For example, other OMERACT conferences have led to consensus on core sets of measures for osteoarthritis and osteoporosis, psoriasis/psoriatic arthritis, psychosocial measures, and a core set of data for cost-effectiveness evaluations.
‘Speed is a limitation’
OMERACT is a bottom-up volunteer organization. It doesn’t represent any official organization of any clinical society. “We’ve not asked to be adopted by the American College of Rheumatology, EULAR [European Alliance of Associations for Rheumatology], or other international organizations,” Dr. Tugwell said. It offers a chance for patients, users, and doers of research to work together to agree on rigorous criteria accepted by the approval agencies and take the necessary time to work things through.
This is not a fast process, usually taking 4-6 years to initiate and establish an outcome domain set, he emphasized. “It would be beneficial to do it faster if we had the resources to meet every year. The fact is we’re a volunteer organization that meets every 2 years.”
Speed is a limitation, he acknowledged, but it’s an acceptable trade-off for doing things correctly.
The group has faced other challenges during the COVID-19 pandemic, pivoting to a virtual format that had benefits and limitations.
In one respect, moving to a virtual meeting increased uptake in participation and voting, Dr. Tugwell said. Patient participants with severe rheumatoid arthritis no longer faced the challenges of travel. “On the other hand, we didn’t have the same opportunity to achieve common ground virtually,” he said. “Where there are strong disagreements, I’m a great believer that people need to know one another. There needs to be relationship building.”
OMERACT’s emerging leader program has been a cornerstone of its in-person meetings, engaging young rheumatologists to interact with some of the leaders of outcome measurement. The virtual format dampened this process somewhat, eliminating those important “café chats” between the stakeholders.
The hope is to bring people face-to-face once more at the next meeting in May 2023. The agenda will focus on relationship building, identifying controversial areas, and bringing younger people to develop relationships, Dr. Tugwell said. OMERACT will retain a virtual option for the worldwide voting, “which will allow for more buy-in from so many more people,” he added.
A consensus on pain
The onus of developing outcome measures that move with the times is sometimes too great for one group to manage. In 2018, OMERACT became a part of the Red Hat Group (RHG), an organization conceived at the COMET (Core Outcome Measures in Effectiveness Trials) VII meeting in Amsterdam.
RHG aims to improve the choice of outcomes in health research. It includes eight groups: COMET; OMERACT; the Cochrane Skin Core Outcome Set Initiative; Grading of Recommendations, Assessment, Development and Evaluations; Center for Medical Technology Policy; COnsensus-based Standards for the selection of health Measurement Instruments; Clinical Data Interchange Standards Consortium; and Standardized Outcomes in Nephrology.
The collaboration between groups offers a “very interesting interface between consensus building as well as hard evidence,” Dr. Tugwell said. The focus goes beyond rheumatology to other clinical areas of common interest, exploring how one classifies outcome domains in terms of symptoms, life impact, or death.
Pain is an important common denominator that the RHG has evaluated.
“We believe it’s too general. We’re trying to define pain across all Red Hat Groups because it’s clear that the research community has all these different scales for defining pain severity,” Dr. Tugwell said. “We have to find a way to make ruthless decisions and rules for doing it. And of course, it has to be transparent.”
Looking ahead
As part of its ongoing work, OMERACT is evaluating the robustness of instruments that rheumatologists use as outcome measures in clinical trials, which can be a laborious process. The OMERACT Filter 2.0, part of the latest iteration of the handbook, offers strong guidance for researchers but needs a long-term strategy and key methodological support. “To that end, we set up a technical advisory group to help people in the instrument selection work and that remains an ongoing process,” OMERACT leaders said in their joint statement.
OMERACT is looking at opportunities to create benchmark processes for developing core sets outside of rheumatology and a methodology around outcome measures such as contextual factors, composites, and surrogates.
It will also be taking a step back to solicit opinions from the approval agencies represented by the OMERACT membership on the OMERACT handbook.
The goal is to make sure the handbook aligns with everyone else’s approval and labeling requirements.
OMERACT’s patient participants bring important perspectives
OMERACT over the years has sought to become a more patient-centered group. Patients have been involved in OMERACT activities since its sixth meeting, forming an independent, yet integrated, group within the network. They have their own steering committee and produced and helped to update a glossary for OMERACT patients and professionals.
Catherine (McGowan) Hofstetter, who was diagnosed with rheumatoid arthritis 30 years ago, chairs OMERACT’s Patient Research Partners Support Team. In a Q&A, she discussed the importance of patient voices and OMERACT’s plans to further educate and include patients in the dialogue on outcomes.
Question: Have patients always been a part of OMERACT meetings?
Answer: Patients have been involved with OMERACT since 2002. The patient voice adds relevance to all the work that OMERACT does. You can’t begin to talk about outcomes unless there is a patient at the table with lived experience.
Q: Can you cite a few examples of how the patient voice enriches the conversation on outcomes research?
A: Outcomes and priorities that are important to patients are often completely different than those of the clinician. For instance, a work outcome is important to someone who doesn’t have any medical insurance or disability insurance, so that you can ensure that there is food on the table and a roof over your head. Or it may be important to someone because the employment provides medical and disability insurance to provide security for them and their family. These are two different perspectives on work and therefore work priorities and outcomes.
Q: What have been some of the challenges of getting patients to participate?
A: Training patients is one challenge. OMERACT’s work has a very steep learning curve, and while the basics are the same between the groups in terms of looking at what we measure and how we measure it, the nuances of different working groups require a lot of time and energy to be comfortable enough with the work, and then be confident enough to bring your perspective and lived experience to the table. It’s also a very accomplished group, which can be quite intimidating. Self-disclosure is a very personal and intimate undertaking that requires patience, compassion, and respect.
Q: Are there any plans to enhance patient engagement?
A: When we had OMERACT 2020 it was a virtual conference that took place over about 6 months. We had far more patient research partners [PRPs] participate than we have ever had at any OMERACT face-to-face meeting. There is a desire and passion on the part of patients to lend their voices to the work. The working groups meet virtually throughout the year to advance their agendas, and PRPs are a part of each of the working groups.
Hopefully, we can start working toward including more voices at the conferences by enabling a hybrid model. The PRP Support Team will begin engaging patients this fall with education, mentoring, and team-building exercises so by the time we meet in person in May 2023, they will have enough background knowledge and information to give them the confidence that will enhance their experience at the face-to-face meeting.
We also need to ensure that those patients who want to stay engaged can. This means that the education and training should continue long after the face-to-face meeting is over. We need to build capacity in the PRP group and look to succession planning and be a resource to working groups struggling to find PRPs to work with them on a longer-term basis.
Clinical research in rheumatology was suffering from an identity crisis of sorts 40 years ago. A lack of consensus across continents resulted in differing views about clinical outcome measures and judgments about treatments.
Patients were not allowed to be the generating source of a clinical outcome, according to Peter Tugwell, MSc, MD. “The only outcomes that were acceptable were clinician assessments, blood tests, and imaging,” said Dr. Tugwell, professor of medicine, epidemiology, and public health at the University of Ottawa (Ont.) and a practicing rheumatologist at Ottawa Hospital.
Clinicians were coming to different conclusions about patient responses to treatment when managing rheumatoid arthritis in clinical practice.
OMERACT sought to address this lack of uniformity. This international group, formed in 1992, leverages stakeholder groups to improve outcome measurement in rheumatology endpoints through a consensus-building, data-driven format.
It was originally known as “Outcome Measures in Rheumatoid Arthritis Clinical Trials,” but its leaders have since broadened its scope to “Outcome Measures in Rheumatology.” Over the years, it has evolved into an international network that assesses measurement across a wide variety of intervention studies. Now 30 years old, the network spans 40 active working groups and has influenced work in patient outcomes across 500 peer-reviewed publications.
The network meets every 2 years to address what is always a challenging agenda, said Dr. Tugwell, one of its founding members and chair. “There’s lots of strong opinions.” Participating in the discussions are individuals from all stages of seniority in rheumatology and clinical epidemiology, patient research partners, industry, approval agencies, and many countries who are committed to the spirit of OMERACT.
“The secret to our success has been getting world leaders to come together and have those discussions, work them through, and identify common ground in such a way that the approval agencies accept these outcome measures in clinical trials,” he added.
“My impression was the founders perceived a problem in the early 1990s and devised a consensus method in an attempt to quantify clinical parameters to define disease activity in rheumatoid arthritis – an important first step to do clinical trials and allow comparisons between them,” said Patricia Woo, CBE, FMedSci, FRCP, emeritus professor of pediatric rheumatology and previous head of the Centre for Paediatric and Adolescent Rheumatology at UCL, London. At that time, even disease definitions varied between the United States and Europe and other parts of the world, said Dr. Woo, who is not a part of OMERACT. “This was especially true for pediatric rheumatology.”
Fusing the continental divide
OMERACT arose from a need to streamline clinical outcome measures in rheumatology. Research papers during the 1980s demonstrated a lack of coherence in managing patients with rheumatoid arthritis in routine practice. In addition, the measures used to define clinical endpoints in clinical trials operated in silos – they were either too specific to a certain trial, overlapped with other concepts, or didn’t reflect changes in treatment.
Approval agencies in Europe and North America were approving only outcomes measures developed by their respective researchers. This was also true of patients they tested on. “This seemed crazy,” Dr. Tugwell said.
Dr. Tugwell was involved in the Cochrane collaboration, which conducts systematic reviews of best evidence across the world that assesses the magnitude of benefits versus harms.
To achieve this goal, “you need to pull studies from around the world,” he said. Maarten Boers, MD, PhD, a rheumatologist (and later professor of clinical epidemiology at Amsterdam University Medical Center) from the Netherlands, spent a year in Ontario, Canada, to train as a clinical epidemiologist. Together, Dr. Tugwell and Dr. Boers began discussing options to develop more streamlined outcome measures.
They initiated the first OMERACT conference in Maastricht, the Netherlands, in 1992. The Food and Drug Administration and European Medicines Agency participated, along with leaders of outcomes measurement in Europe and in North America.
Discussions centered on methods to develop outcomes in a meaningful fashion. During the first meeting, North American and European approval agencies agreed to accept each other’s studies and endpoints and patient reported outcomes.
Agreement was achieved on a preliminary set of outcome domains and measures that later became known as the WHO-ILAR (World Health Organization–International League of Associations for Rheumatology) core set. The set included seven outcome domains: tender joints, swollen joints, pain, physician global assessment, patient global assessment, physical disability, and acute phase reactants, and one additional outcome domain for studies lasting 1 year or more: radiographs of the joints.
“A proactive program was planned to test not only the validity of these endpoints, but also the methods for their measurement. This was the start of a continuing process,” OMERACT members said in a joint statement for this article. Meetings have since taken place every 2 years.

OMERACT accomplishments
OMERACT now requires buy-in from four continents: Asia, Australia, Europe, and North America.
Its leaders have developed an explicit process for gaining endorsement of core outcome domains and instrument measurement sets. To fully capture the possibilities of “what to measure,” i.e., “measurable aspects of health conditions,” OMERACT has developed a framework of concepts, core areas, and outcome domains. The key concepts are pathophysiology (with a core area termed “manifestations/abnormalities”) and impact (with core areas of “death/lifespan,” and “life impact,” and the optional area of “societal/resource use”). An outcome domain defines an element of a core area to measure the effects of a treatment, such as blood markers, pain intensity, physical function, or emotional well-being.
A core outcome domain set is developed by agreeing to at least one outcome domain within one of the three core areas. Subsequently, a core outcome measurement set is developed by agreeing to at least one applicable measurement instrument for each core outcome domain. This requires documentation of validity, summarized under three metrics: truth, discrimination, and feasibility.
OMERACT’s handbook provides tutelage on establishing and implementing core outcomes, and several workbooks offer guidance on developing core outcome domain sets, selecting instruments for core outcome measurement sets, and OMERACT methodology.
All this work has led to widespread adoption.
Approval agencies have accepted OMERACT’s filter and methods advances, which have been adopted by many research groups in rheumatology and among nonrheumatology research groups. Organizations such as the U.S. National Institutes of Health’s National Institute of Neurological Disorders and Stroke have sought its advice.
Its core outcomes have been adopted and used for approval in the great majority of studies on rheumatoid arthritis, Dr. Tugwell said.
Several BMJ articles underscore the influence and uptake of OMERACT’s core outcome set. One 2017 paper, which analyzed 273 randomized trials of rheumatoid arthritis drug treatments on ClinicalTrials.gov, found that the WHO-ILAR arthritis core outcome set was reported in 81% of the studies. “The adoption of a core outcome set has the potential to increase consistency in outcomes measured across trials and ensure that trials are more likely to measure appropriate outcomes,” the authors concluded.
Since the initial 1992 meeting, OMERACT has broadened its focus from rheumatoid arthritis to 25 other musculoskeletal conditions.
For example, other OMERACT conferences have led to consensus on core sets of measures for osteoarthritis and osteoporosis, psoriasis/psoriatic arthritis, psychosocial measures, and a core set of data for cost-effectiveness evaluations.
‘Speed is a limitation’
OMERACT is a bottom-up volunteer organization. It doesn’t represent any official organization of any clinical society. “We’ve not asked to be adopted by the American College of Rheumatology, EULAR [European Alliance of Associations for Rheumatology], or other international organizations,” Dr. Tugwell said. It offers a chance for patients, users, and doers of research to work together to agree on rigorous criteria accepted by the approval agencies and take the necessary time to work things through.
This is not a fast process, usually taking 4-6 years to initiate and establish an outcome domain set, he emphasized. “It would be beneficial to do it faster if we had the resources to meet every year. The fact is we’re a volunteer organization that meets every 2 years.”
Speed is a limitation, he acknowledged, but it’s an acceptable trade-off for doing things correctly.
The group has faced other challenges during the COVID-19 pandemic, pivoting to a virtual format that had benefits and limitations.
In one respect, moving to a virtual meeting increased uptake in participation and voting, Dr. Tugwell said. Patient participants with severe rheumatoid arthritis no longer faced the challenges of travel. “On the other hand, we didn’t have the same opportunity to achieve common ground virtually,” he said. “Where there are strong disagreements, I’m a great believer that people need to know one another. There needs to be relationship building.”
OMERACT’s emerging leader program has been a cornerstone of its in-person meetings, engaging young rheumatologists to interact with some of the leaders of outcome measurement. The virtual format dampened this process somewhat, eliminating those important “café chats” between the stakeholders.
The hope is to bring people face-to-face once more at the next meeting in May 2023. The agenda will focus on relationship building, identifying controversial areas, and bringing younger people to develop relationships, Dr. Tugwell said. OMERACT will retain a virtual option for the worldwide voting, “which will allow for more buy-in from so many more people,” he added.
A consensus on pain
The onus of developing outcome measures that move with the times is sometimes too great for one group to manage. In 2018, OMERACT became a part of the Red Hat Group (RHG), an organization conceived at the COMET (Core Outcome Measures in Effectiveness Trials) VII meeting in Amsterdam.
RHG aims to improve the choice of outcomes in health research. It includes eight groups: COMET; OMERACT; the Cochrane Skin Core Outcome Set Initiative; Grading of Recommendations, Assessment, Development and Evaluations; Center for Medical Technology Policy; COnsensus-based Standards for the selection of health Measurement Instruments; Clinical Data Interchange Standards Consortium; and Standardized Outcomes in Nephrology.
The collaboration between groups offers a “very interesting interface between consensus building as well as hard evidence,” Dr. Tugwell said. The focus goes beyond rheumatology to other clinical areas of common interest, exploring how one classifies outcome domains in terms of symptoms, life impact, or death.
Pain is an important common denominator that the RHG has evaluated.
“We believe it’s too general. We’re trying to define pain across all Red Hat Groups because it’s clear that the research community has all these different scales for defining pain severity,” Dr. Tugwell said. “We have to find a way to make ruthless decisions and rules for doing it. And of course, it has to be transparent.”
Looking ahead
As part of its ongoing work, OMERACT is evaluating the robustness of instruments that rheumatologists use as outcome measures in clinical trials, which can be a laborious process. The OMERACT Filter 2.0, part of the latest iteration of the handbook, offers strong guidance for researchers but needs a long-term strategy and key methodological support. “To that end, we set up a technical advisory group to help people in the instrument selection work and that remains an ongoing process,” OMERACT leaders said in their joint statement.
OMERACT is looking at opportunities to create benchmark processes for developing core sets outside of rheumatology and a methodology around outcome measures such as contextual factors, composites, and surrogates.
It will also be taking a step back to solicit opinions from the approval agencies represented by the OMERACT membership on the OMERACT handbook.
The goal is to make sure the handbook aligns with everyone else’s approval and labeling requirements.
OMERACT’s patient participants bring important perspectives
OMERACT over the years has sought to become a more patient-centered group. Patients have been involved in OMERACT activities since its sixth meeting, forming an independent, yet integrated, group within the network. They have their own steering committee and produced and helped to update a glossary for OMERACT patients and professionals.
Catherine (McGowan) Hofstetter, who was diagnosed with rheumatoid arthritis 30 years ago, chairs OMERACT’s Patient Research Partners Support Team. In a Q&A, she discussed the importance of patient voices and OMERACT’s plans to further educate and include patients in the dialogue on outcomes.
Question: Have patients always been a part of OMERACT meetings?
Answer: Patients have been involved with OMERACT since 2002. The patient voice adds relevance to all the work that OMERACT does. You can’t begin to talk about outcomes unless there is a patient at the table with lived experience.
Q: Can you cite a few examples of how the patient voice enriches the conversation on outcomes research?
A: Outcomes and priorities that are important to patients are often completely different than those of the clinician. For instance, a work outcome is important to someone who doesn’t have any medical insurance or disability insurance, so that you can ensure that there is food on the table and a roof over your head. Or it may be important to someone because the employment provides medical and disability insurance to provide security for them and their family. These are two different perspectives on work and therefore work priorities and outcomes.
Q: What have been some of the challenges of getting patients to participate?
A: Training patients is one challenge. OMERACT’s work has a very steep learning curve, and while the basics are the same between the groups in terms of looking at what we measure and how we measure it, the nuances of different working groups require a lot of time and energy to be comfortable enough with the work, and then be confident enough to bring your perspective and lived experience to the table. It’s also a very accomplished group, which can be quite intimidating. Self-disclosure is a very personal and intimate undertaking that requires patience, compassion, and respect.
Q: Are there any plans to enhance patient engagement?
A: When we had OMERACT 2020 it was a virtual conference that took place over about 6 months. We had far more patient research partners [PRPs] participate than we have ever had at any OMERACT face-to-face meeting. There is a desire and passion on the part of patients to lend their voices to the work. The working groups meet virtually throughout the year to advance their agendas, and PRPs are a part of each of the working groups.
Hopefully, we can start working toward including more voices at the conferences by enabling a hybrid model. The PRP Support Team will begin engaging patients this fall with education, mentoring, and team-building exercises so by the time we meet in person in May 2023, they will have enough background knowledge and information to give them the confidence that will enhance their experience at the face-to-face meeting.
We also need to ensure that those patients who want to stay engaged can. This means that the education and training should continue long after the face-to-face meeting is over. We need to build capacity in the PRP group and look to succession planning and be a resource to working groups struggling to find PRPs to work with them on a longer-term basis.
Clinical research in rheumatology was suffering from an identity crisis of sorts 40 years ago. A lack of consensus across continents resulted in differing views about clinical outcome measures and judgments about treatments.
Patients were not allowed to be the generating source of a clinical outcome, according to Peter Tugwell, MSc, MD. “The only outcomes that were acceptable were clinician assessments, blood tests, and imaging,” said Dr. Tugwell, professor of medicine, epidemiology, and public health at the University of Ottawa (Ont.) and a practicing rheumatologist at Ottawa Hospital.
Clinicians were coming to different conclusions about patient responses to treatment when managing rheumatoid arthritis in clinical practice.
OMERACT sought to address this lack of uniformity. This international group, formed in 1992, leverages stakeholder groups to improve outcome measurement in rheumatology endpoints through a consensus-building, data-driven format.
It was originally known as “Outcome Measures in Rheumatoid Arthritis Clinical Trials,” but its leaders have since broadened its scope to “Outcome Measures in Rheumatology.” Over the years, it has evolved into an international network that assesses measurement across a wide variety of intervention studies. Now 30 years old, the network spans 40 active working groups and has influenced work in patient outcomes across 500 peer-reviewed publications.
The network meets every 2 years to address what is always a challenging agenda, said Dr. Tugwell, one of its founding members and chair. “There’s lots of strong opinions.” Participating in the discussions are individuals from all stages of seniority in rheumatology and clinical epidemiology, patient research partners, industry, approval agencies, and many countries who are committed to the spirit of OMERACT.
“The secret to our success has been getting world leaders to come together and have those discussions, work them through, and identify common ground in such a way that the approval agencies accept these outcome measures in clinical trials,” he added.
“My impression was the founders perceived a problem in the early 1990s and devised a consensus method in an attempt to quantify clinical parameters to define disease activity in rheumatoid arthritis – an important first step to do clinical trials and allow comparisons between them,” said Patricia Woo, CBE, FMedSci, FRCP, emeritus professor of pediatric rheumatology and previous head of the Centre for Paediatric and Adolescent Rheumatology at UCL, London. At that time, even disease definitions varied between the United States and Europe and other parts of the world, said Dr. Woo, who is not a part of OMERACT. “This was especially true for pediatric rheumatology.”
Fusing the continental divide
OMERACT arose from a need to streamline clinical outcome measures in rheumatology. Research papers during the 1980s demonstrated a lack of coherence in managing patients with rheumatoid arthritis in routine practice. In addition, the measures used to define clinical endpoints in clinical trials operated in silos – they were either too specific to a certain trial, overlapped with other concepts, or didn’t reflect changes in treatment.
Approval agencies in Europe and North America were approving only outcomes measures developed by their respective researchers. This was also true of patients they tested on. “This seemed crazy,” Dr. Tugwell said.
Dr. Tugwell was involved in the Cochrane collaboration, which conducts systematic reviews of best evidence across the world that assesses the magnitude of benefits versus harms.
To achieve this goal, “you need to pull studies from around the world,” he said. Maarten Boers, MD, PhD, a rheumatologist (and later professor of clinical epidemiology at Amsterdam University Medical Center) from the Netherlands, spent a year in Ontario, Canada, to train as a clinical epidemiologist. Together, Dr. Tugwell and Dr. Boers began discussing options to develop more streamlined outcome measures.
They initiated the first OMERACT conference in Maastricht, the Netherlands, in 1992. The Food and Drug Administration and European Medicines Agency participated, along with leaders of outcomes measurement in Europe and in North America.
Discussions centered on methods to develop outcomes in a meaningful fashion. During the first meeting, North American and European approval agencies agreed to accept each other’s studies and endpoints and patient reported outcomes.
Agreement was achieved on a preliminary set of outcome domains and measures that later became known as the WHO-ILAR (World Health Organization–International League of Associations for Rheumatology) core set. The set included seven outcome domains: tender joints, swollen joints, pain, physician global assessment, patient global assessment, physical disability, and acute phase reactants, and one additional outcome domain for studies lasting 1 year or more: radiographs of the joints.
“A proactive program was planned to test not only the validity of these endpoints, but also the methods for their measurement. This was the start of a continuing process,” OMERACT members said in a joint statement for this article. Meetings have since taken place every 2 years.

OMERACT accomplishments
OMERACT now requires buy-in from four continents: Asia, Australia, Europe, and North America.
Its leaders have developed an explicit process for gaining endorsement of core outcome domains and instrument measurement sets. To fully capture the possibilities of “what to measure,” i.e., “measurable aspects of health conditions,” OMERACT has developed a framework of concepts, core areas, and outcome domains. The key concepts are pathophysiology (with a core area termed “manifestations/abnormalities”) and impact (with core areas of “death/lifespan,” and “life impact,” and the optional area of “societal/resource use”). An outcome domain defines an element of a core area to measure the effects of a treatment, such as blood markers, pain intensity, physical function, or emotional well-being.
A core outcome domain set is developed by agreeing to at least one outcome domain within one of the three core areas. Subsequently, a core outcome measurement set is developed by agreeing to at least one applicable measurement instrument for each core outcome domain. This requires documentation of validity, summarized under three metrics: truth, discrimination, and feasibility.
OMERACT’s handbook provides tutelage on establishing and implementing core outcomes, and several workbooks offer guidance on developing core outcome domain sets, selecting instruments for core outcome measurement sets, and OMERACT methodology.
All this work has led to widespread adoption.
Approval agencies have accepted OMERACT’s filter and methods advances, which have been adopted by many research groups in rheumatology and among nonrheumatology research groups. Organizations such as the U.S. National Institutes of Health’s National Institute of Neurological Disorders and Stroke have sought its advice.
Its core outcomes have been adopted and used for approval in the great majority of studies on rheumatoid arthritis, Dr. Tugwell said.
Several BMJ articles underscore the influence and uptake of OMERACT’s core outcome set. One 2017 paper, which analyzed 273 randomized trials of rheumatoid arthritis drug treatments on ClinicalTrials.gov, found that the WHO-ILAR arthritis core outcome set was reported in 81% of the studies. “The adoption of a core outcome set has the potential to increase consistency in outcomes measured across trials and ensure that trials are more likely to measure appropriate outcomes,” the authors concluded.
Since the initial 1992 meeting, OMERACT has broadened its focus from rheumatoid arthritis to 25 other musculoskeletal conditions.
For example, other OMERACT conferences have led to consensus on core sets of measures for osteoarthritis and osteoporosis, psoriasis/psoriatic arthritis, psychosocial measures, and a core set of data for cost-effectiveness evaluations.
‘Speed is a limitation’
OMERACT is a bottom-up volunteer organization. It doesn’t represent any official organization of any clinical society. “We’ve not asked to be adopted by the American College of Rheumatology, EULAR [European Alliance of Associations for Rheumatology], or other international organizations,” Dr. Tugwell said. It offers a chance for patients, users, and doers of research to work together to agree on rigorous criteria accepted by the approval agencies and take the necessary time to work things through.
This is not a fast process, usually taking 4-6 years to initiate and establish an outcome domain set, he emphasized. “It would be beneficial to do it faster if we had the resources to meet every year. The fact is we’re a volunteer organization that meets every 2 years.”
Speed is a limitation, he acknowledged, but it’s an acceptable trade-off for doing things correctly.
The group has faced other challenges during the COVID-19 pandemic, pivoting to a virtual format that had benefits and limitations.
In one respect, moving to a virtual meeting increased uptake in participation and voting, Dr. Tugwell said. Patient participants with severe rheumatoid arthritis no longer faced the challenges of travel. “On the other hand, we didn’t have the same opportunity to achieve common ground virtually,” he said. “Where there are strong disagreements, I’m a great believer that people need to know one another. There needs to be relationship building.”
OMERACT’s emerging leader program has been a cornerstone of its in-person meetings, engaging young rheumatologists to interact with some of the leaders of outcome measurement. The virtual format dampened this process somewhat, eliminating those important “café chats” between the stakeholders.
The hope is to bring people face-to-face once more at the next meeting in May 2023. The agenda will focus on relationship building, identifying controversial areas, and bringing younger people to develop relationships, Dr. Tugwell said. OMERACT will retain a virtual option for the worldwide voting, “which will allow for more buy-in from so many more people,” he added.
A consensus on pain
The onus of developing outcome measures that move with the times is sometimes too great for one group to manage. In 2018, OMERACT became a part of the Red Hat Group (RHG), an organization conceived at the COMET (Core Outcome Measures in Effectiveness Trials) VII meeting in Amsterdam.
RHG aims to improve the choice of outcomes in health research. It includes eight groups: COMET; OMERACT; the Cochrane Skin Core Outcome Set Initiative; Grading of Recommendations, Assessment, Development and Evaluations; Center for Medical Technology Policy; COnsensus-based Standards for the selection of health Measurement Instruments; Clinical Data Interchange Standards Consortium; and Standardized Outcomes in Nephrology.
The collaboration between groups offers a “very interesting interface between consensus building as well as hard evidence,” Dr. Tugwell said. The focus goes beyond rheumatology to other clinical areas of common interest, exploring how one classifies outcome domains in terms of symptoms, life impact, or death.
Pain is an important common denominator that the RHG has evaluated.
“We believe it’s too general. We’re trying to define pain across all Red Hat Groups because it’s clear that the research community has all these different scales for defining pain severity,” Dr. Tugwell said. “We have to find a way to make ruthless decisions and rules for doing it. And of course, it has to be transparent.”
Looking ahead
As part of its ongoing work, OMERACT is evaluating the robustness of instruments that rheumatologists use as outcome measures in clinical trials, which can be a laborious process. The OMERACT Filter 2.0, part of the latest iteration of the handbook, offers strong guidance for researchers but needs a long-term strategy and key methodological support. “To that end, we set up a technical advisory group to help people in the instrument selection work and that remains an ongoing process,” OMERACT leaders said in their joint statement.
OMERACT is looking at opportunities to create benchmark processes for developing core sets outside of rheumatology and a methodology around outcome measures such as contextual factors, composites, and surrogates.
It will also be taking a step back to solicit opinions from the approval agencies represented by the OMERACT membership on the OMERACT handbook.
The goal is to make sure the handbook aligns with everyone else’s approval and labeling requirements.
OMERACT’s patient participants bring important perspectives
OMERACT over the years has sought to become a more patient-centered group. Patients have been involved in OMERACT activities since its sixth meeting, forming an independent, yet integrated, group within the network. They have their own steering committee and produced and helped to update a glossary for OMERACT patients and professionals.
Catherine (McGowan) Hofstetter, who was diagnosed with rheumatoid arthritis 30 years ago, chairs OMERACT’s Patient Research Partners Support Team. In a Q&A, she discussed the importance of patient voices and OMERACT’s plans to further educate and include patients in the dialogue on outcomes.
Question: Have patients always been a part of OMERACT meetings?
Answer: Patients have been involved with OMERACT since 2002. The patient voice adds relevance to all the work that OMERACT does. You can’t begin to talk about outcomes unless there is a patient at the table with lived experience.
Q: Can you cite a few examples of how the patient voice enriches the conversation on outcomes research?
A: Outcomes and priorities that are important to patients are often completely different than those of the clinician. For instance, a work outcome is important to someone who doesn’t have any medical insurance or disability insurance, so that you can ensure that there is food on the table and a roof over your head. Or it may be important to someone because the employment provides medical and disability insurance to provide security for them and their family. These are two different perspectives on work and therefore work priorities and outcomes.
Q: What have been some of the challenges of getting patients to participate?
A: Training patients is one challenge. OMERACT’s work has a very steep learning curve, and while the basics are the same between the groups in terms of looking at what we measure and how we measure it, the nuances of different working groups require a lot of time and energy to be comfortable enough with the work, and then be confident enough to bring your perspective and lived experience to the table. It’s also a very accomplished group, which can be quite intimidating. Self-disclosure is a very personal and intimate undertaking that requires patience, compassion, and respect.
Q: Are there any plans to enhance patient engagement?
A: When we had OMERACT 2020 it was a virtual conference that took place over about 6 months. We had far more patient research partners [PRPs] participate than we have ever had at any OMERACT face-to-face meeting. There is a desire and passion on the part of patients to lend their voices to the work. The working groups meet virtually throughout the year to advance their agendas, and PRPs are a part of each of the working groups.
Hopefully, we can start working toward including more voices at the conferences by enabling a hybrid model. The PRP Support Team will begin engaging patients this fall with education, mentoring, and team-building exercises so by the time we meet in person in May 2023, they will have enough background knowledge and information to give them the confidence that will enhance their experience at the face-to-face meeting.
We also need to ensure that those patients who want to stay engaged can. This means that the education and training should continue long after the face-to-face meeting is over. We need to build capacity in the PRP group and look to succession planning and be a resource to working groups struggling to find PRPs to work with them on a longer-term basis.
ALL-HEART: No benefit of allopurinol in ischemic heart disease
Allopurinol, a drug commonly used to treat gout, provided no benefit in terms of reducing cardiovascular (CV) events in patients with ischemic heart disease, new randomized trial results show.
Treatment of these patients without gout with 600 mg of allopurinol daily had no effect on composite primary endpoint outcomes, including nonfatal MI, nonfatal stroke, or CV death.
“ALL-HEART is the first large, prospective, randomized trial of the effect of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease and provides robust evidence on the role of allopurinol in these patients,” principal investigator Isla Shelagh Mackenzie, MBChB (Honors), PhD, University of Dundee (Scotland), concluded at a press conference.
Their results suggest allopurinol should not be recommended for secondary prevention of events in this group, Dr. Mackenzie said. Although it remains an important treatment for gout, she added, “other avenues for treatment of ischemic heart disease should be explored in future.”
Results of the ALL-HEART (Allopurinol and Cardiovascular Outcomes in Ischemic Heart Disease) trial were presented at the annual congress of the European Society of Cardiology.
Gout treatment
Allopurinol is a xanthine oxidase inhibitor and acts by reducing serum uric acid levels and oxidative stress. Treatment is generally well tolerated, Dr. Mackenzie noted in her presentation, but some patients develop a rash, which can in some cases be serious or even fatal, progressing to Stevens-Johnson syndrome or toxic epidermal necrolysis, “particularly in certain ethnicities.” If rash develops, the advice is to stop treatment immediately.
“The importance of serum uric acid levels in cardiovascular disease is controversial, and there have been different reports over the years of how important they may be,” Dr. Mackenzie explained.
Observational studies have shown variable results, whereas intervention trials, most with fewer than 100 participants, have suggested potential improvements in factors such as blood pressure, endothelial function, left ventricular hypertrophy, or carotid intima-media thickness. Some have reported benefits in acute coronary syndrome and coronary artery bypass grafting, but others have not, she said. A previous study by their own group suggested an improvement in chest pain and exercise time in patients with chronic stable angina and documented coronary artery disease (CAD).
“So, until now, there have been no large prospective randomized trials of the effects of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease,” Dr. Mackenzie said, and this was the aim of ALL-HEART.
ALL-HEART was a prospective, randomized, open-label, blinded-endpoint, multicenter trial. Patients with ischemia heart disease but no history of gout were recruited from 424 general practices across the United Kingdom, starting in February 2014 and with follow-up ending in September 2021. Participants were randomly assigned 1:1 to receive 600 mg of allopurinol daily or usual care.
“It was a decentralized trial, so the follow-up was largely remote after the first 6 weeks, and that included using record linkage data collected from centralized NHS [National Health Service] databases for hospitalizations and deaths in Scotland and England,” she said. The average follow-up was 4.8 years.
During that time, 258 (9.0%) participants in the allopurinol group and 76 (2.6%) in usual care withdrew from follow-up. By the end of the trial, 57.4% of patients in the allopurinol arm withdrew from randomized treatment.
Mean serum uric acid levels dropped from 0.34 mmol/L at baseline to 0.18 mmol/L at 6 weeks of treatment, “so we can see that the treatment was effective at lowering uric acid,” she noted.
In total, there were 5,721 patients in the final intention-to-treat analysis, and 639 patients had a first primary event.
For the primary outcome of nonfatal MI, nonfatal stroke, and cardiovascular death, there was no difference between the groups, the researchers reported, with a hazard ratio of 1.04 (95% confidence interval, 0.89-1.21; P = .65). Similarly, in secondary analyses, there were no differences in any of the component endpoints making up the primary outcome (nonfatal MI: HR, 0.97; 95% CI, 0.78-1.21; P = .81; nonfatal stroke: HR, 1.20; 95% CI, 0.89-1.60; P = .23; cardiovascular death: HR, 1.10; 95% CI, 0.85-1.43; P = .48), or in all-cause mortality (HR, 1.02; 95% CI, 0.87-1.20; P = .77), between the two groups, Dr. Mackenzie noted, “so a definitively neutral trial all round.”
In addition, no differences were seen in prespecified subgroups, including age, sex, estimated glomerular filtration rate, or diabetes, MI, heart failure, peripheral arterial disease, stroke, and stroke or transient ischemic attack at baseline.
There were also no significant effects on quality of life outcomes. Cost-effectiveness analyses are ongoing, although no differences are expected there, Dr. Mackenzie noted.
In terms of safety, incident cancers and all-cause mortality did not differ between groups. Serious adverse events were also similar between groups, Dr. Mackenzie said, “and there were no fatal treatment-related SAEs [serious adverse events] in the study.”
Another negative antioxidant trial
Invited discussant for the presentation, Leslie Cho, MD, of the Cleveland Clinic said that ALL-HEART, while an excellent trial with a pragmatic design, constitutes yet another negative antioxidant trial.
She pointed to three problems with this study and antioxidant trials in general. “First, the problem is with the antioxidant,” a xanthine oxidase inhibitor. “Xanthine oxidase is not a major trigger of oxidative stress. In a field of major players,” including nitric oxide, uncoupled endothelial nitric oxide synthase, and mitochondria myeloperoxidase, Dr. Cho said, “xanthine oxidase is a minor player.”
“Moreover, 57% of the patients stopped taking allopurinol, and rightfully so,” she said. Patients were receiving optimal medical therapies, many of which are also antioxidants, including statins, ACE inhibitors, angiotensin receptor blockers, and beta-blockers.
Second, the patient population was older, with an average age of 72 years. “This makes the ALL-HEART study a chronic angina study, chronic CAD study, one of the oldest modern day CAD trials. If you look at LoDoCo or ISCHEMIA trials, the average age is 63.” Patients also had established disease, many with previous revascularization.
The final issue seen with this trial, and all antioxidant trials, is that patient selection is not based on oxidative stress or antioxidant level. “The antioxidant trials have been disappointing at best. There is clear and convincing evidence that oxidative stress is involved in the pathogenesis of atherosclerosis, and yet study after study of antioxidant trials have been negative,” she said.
“Currently, there is no reliable measurement of global level of oxidative stress,” Dr. Cho noted. “Moreover, dose response was not tested, and if we cannot test the baseline antioxidant stress level of patients, we also cannot measure the effect of treatment on the global oxidative stress.”
So, “is there no hope for antioxidant trials?” she asked. Three factors will be required for future success, she said. “No. 1, selecting the right patient at the right time. No. 2, a reliable biomarker to measure oxidative stress to guide who should get therapy, and if the therapy is working. And lastly, targeted therapies that work on major triggers of oxidative stress.”
Also commenting on the results, B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute/Atrium Health, clinical professor of medicine at the University of North Carolina at Chapel Hill, and vice president of the American College of Cardiology, called ALL-HEART “an important and interesting study.”
“For years, cardiologists and others have been interested in allopurinol as an anti-inflammatory, xanthine oxidase inhibitor ... to prevent coronary ischemic events,” he said in an interview.
But this was a well-designed, well-conducted study, and “unfortunately there was no improvement in the primary outcome, no reduction in major cardiovascular events like myocardial infarction or stroke or cardiovascular death,” Dr. Wilson said. “So, it’s a bit of a disappointment that it’s not there as an important medication to help us with these patients with ischemic heart disease, but it’s also an important question answered — that we need to look at treatments for ischemic heart disease other than allopurinol.”
The trial was supported by the National Institute for Health and Care Research Health Technology Assessment Program in the United Kingdom. Dr. Mackenzie reported research contracts to her institution from NIHR HTA for this work, and other disclosures related to other work. Dr. Cho and Dr. Wilson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Allopurinol, a drug commonly used to treat gout, provided no benefit in terms of reducing cardiovascular (CV) events in patients with ischemic heart disease, new randomized trial results show.
Treatment of these patients without gout with 600 mg of allopurinol daily had no effect on composite primary endpoint outcomes, including nonfatal MI, nonfatal stroke, or CV death.
“ALL-HEART is the first large, prospective, randomized trial of the effect of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease and provides robust evidence on the role of allopurinol in these patients,” principal investigator Isla Shelagh Mackenzie, MBChB (Honors), PhD, University of Dundee (Scotland), concluded at a press conference.
Their results suggest allopurinol should not be recommended for secondary prevention of events in this group, Dr. Mackenzie said. Although it remains an important treatment for gout, she added, “other avenues for treatment of ischemic heart disease should be explored in future.”
Results of the ALL-HEART (Allopurinol and Cardiovascular Outcomes in Ischemic Heart Disease) trial were presented at the annual congress of the European Society of Cardiology.
Gout treatment
Allopurinol is a xanthine oxidase inhibitor and acts by reducing serum uric acid levels and oxidative stress. Treatment is generally well tolerated, Dr. Mackenzie noted in her presentation, but some patients develop a rash, which can in some cases be serious or even fatal, progressing to Stevens-Johnson syndrome or toxic epidermal necrolysis, “particularly in certain ethnicities.” If rash develops, the advice is to stop treatment immediately.
“The importance of serum uric acid levels in cardiovascular disease is controversial, and there have been different reports over the years of how important they may be,” Dr. Mackenzie explained.
Observational studies have shown variable results, whereas intervention trials, most with fewer than 100 participants, have suggested potential improvements in factors such as blood pressure, endothelial function, left ventricular hypertrophy, or carotid intima-media thickness. Some have reported benefits in acute coronary syndrome and coronary artery bypass grafting, but others have not, she said. A previous study by their own group suggested an improvement in chest pain and exercise time in patients with chronic stable angina and documented coronary artery disease (CAD).
“So, until now, there have been no large prospective randomized trials of the effects of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease,” Dr. Mackenzie said, and this was the aim of ALL-HEART.
ALL-HEART was a prospective, randomized, open-label, blinded-endpoint, multicenter trial. Patients with ischemia heart disease but no history of gout were recruited from 424 general practices across the United Kingdom, starting in February 2014 and with follow-up ending in September 2021. Participants were randomly assigned 1:1 to receive 600 mg of allopurinol daily or usual care.
“It was a decentralized trial, so the follow-up was largely remote after the first 6 weeks, and that included using record linkage data collected from centralized NHS [National Health Service] databases for hospitalizations and deaths in Scotland and England,” she said. The average follow-up was 4.8 years.
During that time, 258 (9.0%) participants in the allopurinol group and 76 (2.6%) in usual care withdrew from follow-up. By the end of the trial, 57.4% of patients in the allopurinol arm withdrew from randomized treatment.
Mean serum uric acid levels dropped from 0.34 mmol/L at baseline to 0.18 mmol/L at 6 weeks of treatment, “so we can see that the treatment was effective at lowering uric acid,” she noted.
In total, there were 5,721 patients in the final intention-to-treat analysis, and 639 patients had a first primary event.
For the primary outcome of nonfatal MI, nonfatal stroke, and cardiovascular death, there was no difference between the groups, the researchers reported, with a hazard ratio of 1.04 (95% confidence interval, 0.89-1.21; P = .65). Similarly, in secondary analyses, there were no differences in any of the component endpoints making up the primary outcome (nonfatal MI: HR, 0.97; 95% CI, 0.78-1.21; P = .81; nonfatal stroke: HR, 1.20; 95% CI, 0.89-1.60; P = .23; cardiovascular death: HR, 1.10; 95% CI, 0.85-1.43; P = .48), or in all-cause mortality (HR, 1.02; 95% CI, 0.87-1.20; P = .77), between the two groups, Dr. Mackenzie noted, “so a definitively neutral trial all round.”
In addition, no differences were seen in prespecified subgroups, including age, sex, estimated glomerular filtration rate, or diabetes, MI, heart failure, peripheral arterial disease, stroke, and stroke or transient ischemic attack at baseline.
There were also no significant effects on quality of life outcomes. Cost-effectiveness analyses are ongoing, although no differences are expected there, Dr. Mackenzie noted.
In terms of safety, incident cancers and all-cause mortality did not differ between groups. Serious adverse events were also similar between groups, Dr. Mackenzie said, “and there were no fatal treatment-related SAEs [serious adverse events] in the study.”
Another negative antioxidant trial
Invited discussant for the presentation, Leslie Cho, MD, of the Cleveland Clinic said that ALL-HEART, while an excellent trial with a pragmatic design, constitutes yet another negative antioxidant trial.
She pointed to three problems with this study and antioxidant trials in general. “First, the problem is with the antioxidant,” a xanthine oxidase inhibitor. “Xanthine oxidase is not a major trigger of oxidative stress. In a field of major players,” including nitric oxide, uncoupled endothelial nitric oxide synthase, and mitochondria myeloperoxidase, Dr. Cho said, “xanthine oxidase is a minor player.”
“Moreover, 57% of the patients stopped taking allopurinol, and rightfully so,” she said. Patients were receiving optimal medical therapies, many of which are also antioxidants, including statins, ACE inhibitors, angiotensin receptor blockers, and beta-blockers.
Second, the patient population was older, with an average age of 72 years. “This makes the ALL-HEART study a chronic angina study, chronic CAD study, one of the oldest modern day CAD trials. If you look at LoDoCo or ISCHEMIA trials, the average age is 63.” Patients also had established disease, many with previous revascularization.
The final issue seen with this trial, and all antioxidant trials, is that patient selection is not based on oxidative stress or antioxidant level. “The antioxidant trials have been disappointing at best. There is clear and convincing evidence that oxidative stress is involved in the pathogenesis of atherosclerosis, and yet study after study of antioxidant trials have been negative,” she said.
“Currently, there is no reliable measurement of global level of oxidative stress,” Dr. Cho noted. “Moreover, dose response was not tested, and if we cannot test the baseline antioxidant stress level of patients, we also cannot measure the effect of treatment on the global oxidative stress.”
So, “is there no hope for antioxidant trials?” she asked. Three factors will be required for future success, she said. “No. 1, selecting the right patient at the right time. No. 2, a reliable biomarker to measure oxidative stress to guide who should get therapy, and if the therapy is working. And lastly, targeted therapies that work on major triggers of oxidative stress.”
Also commenting on the results, B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute/Atrium Health, clinical professor of medicine at the University of North Carolina at Chapel Hill, and vice president of the American College of Cardiology, called ALL-HEART “an important and interesting study.”
“For years, cardiologists and others have been interested in allopurinol as an anti-inflammatory, xanthine oxidase inhibitor ... to prevent coronary ischemic events,” he said in an interview.
But this was a well-designed, well-conducted study, and “unfortunately there was no improvement in the primary outcome, no reduction in major cardiovascular events like myocardial infarction or stroke or cardiovascular death,” Dr. Wilson said. “So, it’s a bit of a disappointment that it’s not there as an important medication to help us with these patients with ischemic heart disease, but it’s also an important question answered — that we need to look at treatments for ischemic heart disease other than allopurinol.”
The trial was supported by the National Institute for Health and Care Research Health Technology Assessment Program in the United Kingdom. Dr. Mackenzie reported research contracts to her institution from NIHR HTA for this work, and other disclosures related to other work. Dr. Cho and Dr. Wilson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Allopurinol, a drug commonly used to treat gout, provided no benefit in terms of reducing cardiovascular (CV) events in patients with ischemic heart disease, new randomized trial results show.
Treatment of these patients without gout with 600 mg of allopurinol daily had no effect on composite primary endpoint outcomes, including nonfatal MI, nonfatal stroke, or CV death.
“ALL-HEART is the first large, prospective, randomized trial of the effect of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease and provides robust evidence on the role of allopurinol in these patients,” principal investigator Isla Shelagh Mackenzie, MBChB (Honors), PhD, University of Dundee (Scotland), concluded at a press conference.
Their results suggest allopurinol should not be recommended for secondary prevention of events in this group, Dr. Mackenzie said. Although it remains an important treatment for gout, she added, “other avenues for treatment of ischemic heart disease should be explored in future.”
Results of the ALL-HEART (Allopurinol and Cardiovascular Outcomes in Ischemic Heart Disease) trial were presented at the annual congress of the European Society of Cardiology.
Gout treatment
Allopurinol is a xanthine oxidase inhibitor and acts by reducing serum uric acid levels and oxidative stress. Treatment is generally well tolerated, Dr. Mackenzie noted in her presentation, but some patients develop a rash, which can in some cases be serious or even fatal, progressing to Stevens-Johnson syndrome or toxic epidermal necrolysis, “particularly in certain ethnicities.” If rash develops, the advice is to stop treatment immediately.
“The importance of serum uric acid levels in cardiovascular disease is controversial, and there have been different reports over the years of how important they may be,” Dr. Mackenzie explained.
Observational studies have shown variable results, whereas intervention trials, most with fewer than 100 participants, have suggested potential improvements in factors such as blood pressure, endothelial function, left ventricular hypertrophy, or carotid intima-media thickness. Some have reported benefits in acute coronary syndrome and coronary artery bypass grafting, but others have not, she said. A previous study by their own group suggested an improvement in chest pain and exercise time in patients with chronic stable angina and documented coronary artery disease (CAD).
“So, until now, there have been no large prospective randomized trials of the effects of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease,” Dr. Mackenzie said, and this was the aim of ALL-HEART.
ALL-HEART was a prospective, randomized, open-label, blinded-endpoint, multicenter trial. Patients with ischemia heart disease but no history of gout were recruited from 424 general practices across the United Kingdom, starting in February 2014 and with follow-up ending in September 2021. Participants were randomly assigned 1:1 to receive 600 mg of allopurinol daily or usual care.
“It was a decentralized trial, so the follow-up was largely remote after the first 6 weeks, and that included using record linkage data collected from centralized NHS [National Health Service] databases for hospitalizations and deaths in Scotland and England,” she said. The average follow-up was 4.8 years.
During that time, 258 (9.0%) participants in the allopurinol group and 76 (2.6%) in usual care withdrew from follow-up. By the end of the trial, 57.4% of patients in the allopurinol arm withdrew from randomized treatment.
Mean serum uric acid levels dropped from 0.34 mmol/L at baseline to 0.18 mmol/L at 6 weeks of treatment, “so we can see that the treatment was effective at lowering uric acid,” she noted.
In total, there were 5,721 patients in the final intention-to-treat analysis, and 639 patients had a first primary event.
For the primary outcome of nonfatal MI, nonfatal stroke, and cardiovascular death, there was no difference between the groups, the researchers reported, with a hazard ratio of 1.04 (95% confidence interval, 0.89-1.21; P = .65). Similarly, in secondary analyses, there were no differences in any of the component endpoints making up the primary outcome (nonfatal MI: HR, 0.97; 95% CI, 0.78-1.21; P = .81; nonfatal stroke: HR, 1.20; 95% CI, 0.89-1.60; P = .23; cardiovascular death: HR, 1.10; 95% CI, 0.85-1.43; P = .48), or in all-cause mortality (HR, 1.02; 95% CI, 0.87-1.20; P = .77), between the two groups, Dr. Mackenzie noted, “so a definitively neutral trial all round.”
In addition, no differences were seen in prespecified subgroups, including age, sex, estimated glomerular filtration rate, or diabetes, MI, heart failure, peripheral arterial disease, stroke, and stroke or transient ischemic attack at baseline.
There were also no significant effects on quality of life outcomes. Cost-effectiveness analyses are ongoing, although no differences are expected there, Dr. Mackenzie noted.
In terms of safety, incident cancers and all-cause mortality did not differ between groups. Serious adverse events were also similar between groups, Dr. Mackenzie said, “and there were no fatal treatment-related SAEs [serious adverse events] in the study.”
Another negative antioxidant trial
Invited discussant for the presentation, Leslie Cho, MD, of the Cleveland Clinic said that ALL-HEART, while an excellent trial with a pragmatic design, constitutes yet another negative antioxidant trial.
She pointed to three problems with this study and antioxidant trials in general. “First, the problem is with the antioxidant,” a xanthine oxidase inhibitor. “Xanthine oxidase is not a major trigger of oxidative stress. In a field of major players,” including nitric oxide, uncoupled endothelial nitric oxide synthase, and mitochondria myeloperoxidase, Dr. Cho said, “xanthine oxidase is a minor player.”
“Moreover, 57% of the patients stopped taking allopurinol, and rightfully so,” she said. Patients were receiving optimal medical therapies, many of which are also antioxidants, including statins, ACE inhibitors, angiotensin receptor blockers, and beta-blockers.
Second, the patient population was older, with an average age of 72 years. “This makes the ALL-HEART study a chronic angina study, chronic CAD study, one of the oldest modern day CAD trials. If you look at LoDoCo or ISCHEMIA trials, the average age is 63.” Patients also had established disease, many with previous revascularization.
The final issue seen with this trial, and all antioxidant trials, is that patient selection is not based on oxidative stress or antioxidant level. “The antioxidant trials have been disappointing at best. There is clear and convincing evidence that oxidative stress is involved in the pathogenesis of atherosclerosis, and yet study after study of antioxidant trials have been negative,” she said.
“Currently, there is no reliable measurement of global level of oxidative stress,” Dr. Cho noted. “Moreover, dose response was not tested, and if we cannot test the baseline antioxidant stress level of patients, we also cannot measure the effect of treatment on the global oxidative stress.”
So, “is there no hope for antioxidant trials?” she asked. Three factors will be required for future success, she said. “No. 1, selecting the right patient at the right time. No. 2, a reliable biomarker to measure oxidative stress to guide who should get therapy, and if the therapy is working. And lastly, targeted therapies that work on major triggers of oxidative stress.”
Also commenting on the results, B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute/Atrium Health, clinical professor of medicine at the University of North Carolina at Chapel Hill, and vice president of the American College of Cardiology, called ALL-HEART “an important and interesting study.”
“For years, cardiologists and others have been interested in allopurinol as an anti-inflammatory, xanthine oxidase inhibitor ... to prevent coronary ischemic events,” he said in an interview.
But this was a well-designed, well-conducted study, and “unfortunately there was no improvement in the primary outcome, no reduction in major cardiovascular events like myocardial infarction or stroke or cardiovascular death,” Dr. Wilson said. “So, it’s a bit of a disappointment that it’s not there as an important medication to help us with these patients with ischemic heart disease, but it’s also an important question answered — that we need to look at treatments for ischemic heart disease other than allopurinol.”
The trial was supported by the National Institute for Health and Care Research Health Technology Assessment Program in the United Kingdom. Dr. Mackenzie reported research contracts to her institution from NIHR HTA for this work, and other disclosures related to other work. Dr. Cho and Dr. Wilson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2022
Low urate limits for gout questioned in study
Lower limits on serum urate levels applied in gout management may be based on a misreading of data on mortality risks, researchers say.
Low urate levels may not in themselves pose a risk of death but may be a sign of some other illness, said Joshua F. Baker, MD, MSCE, associate professor of rheumatology and epidemiology at the University of Pennsylvania in Philadelphia.
“It points us towards being more reassured that we can be aggressive in treating gout without a concern about long-term effects for our patients,” he said in an interview. He and colleagues published their findings online in Arthritis & Rheumatology.
Previous research has linked high levels of urate with excessive fat and low levels of urate with loss of skeletal muscle mass. And epidemiologic studies have shown a U-shaped relationship between urate levels and mortality, suggesting that very high and very low levels of urate could be harmful.
Based on this correlation, and the theory that urate could have antioxidant benefits, some professional societies have recommended not lowering urate levels below a defined threshold when treating gout. The European Alliance of Associations for Rheumatology has recommended a lower limit of 3 mg/dL.
But the evidence doesn’t entirely support this caution. For example, in a clinical trial of pegloticase (Krystexxa) in patients with refractory gout, patients whose mean serum urate dropped below 2 mg/dL did not die in higher proportions than patients with higher urate levels.
To better understand the risk of low urate, Dr. Baker and colleagues analyzed data on 13,979 participants in the National Health and Nutrition Examination Survey (NHANES) during 1999-2006. The dataset included whole-body dual-energy x-ray absorptiometry (DXA) body composition measures as well as urate levels.
The researchers argue this measurement reveals more about a person’s overall health than body mass index (BMI), which doesn’t distinguish between mass from fat and mass from muscle.
They defined low lean body mass, or sarcopenia, as an appendicular lean mass index relative to fat mass index z score of –1. And they defined low urate as less than 2.5 mg/dL in women and less than 3.5 mg/dL in men.
They found that 29% of people with low urate had low lean body mass, compared with 16% of people with normal urate levels. The difference was statistically significant (P = .001).
They found an association between low urate and increased mortality (hazard ratio, 1.61; 95% confidence interval, 1.14-2.28; P = .008). But that association lost its statistical significance when the researchers adjusted for body composition and weight loss (HR, 1.30; 95% CI, 0.92-1.85; P = .13).
Dr. Baker thinks the association between elevated mortality and low urate can be explained by conditions such as cancer or lung inflammation that might on one hand increase the risk of death and on the other hand lower urate levels by lowering muscle mass. “Low uric acid levels are observed in people who have lost weight for unhealthy reasons, and that can explain relationships with long-term outcomes,” he said.
Proportions of muscle and fat could not account for the risk of mortality associated with high levels of urate, the researchers found. Those participants with urate levels above 5.7 mg/dL had a higher risk of death with higher levels of urate, and this persisted even after statistical adjustment for body composition.
The study sheds light on an important area of controversy, said Mehdi Fini, MD, of the department of medicine at the University of Colorado at Denver, Aurora, who was not involved in the research.
But body composition does not entirely explain the relationship between urate and mortality, he told this news organization. Medications used to lower urate can cause side effects that might increase mortality, he said.
Also, he said, it’s important to understand the role of comorbidities. He cited evidence that low urate is associated with renal, cardiovascular, and pulmonary conditions. Safe levels of urate might differ depending on these factors. So rather than applying the same target serum level to all patients, perhaps researchers should investigate whether lowering urate by a percentage of the patient’s current level is safer and more effective, he suggested.
He agreed with an editorial that also appeared in Arthritis & Rheumatology saying that there is no evidence for a benefit in lowering urate much below 5 mg/dL. “No matter what, I think we should just be careful,” Dr. Fini said.
Dr. Fini and Dr. Baker report no relevant financial relationships. Dr. Baker acknowledged support from a VA Clinical Science Research & Development Merit Award and a Rehabilitation R&D Merit Award.
A version of this article first appeared on Medscape.com.
Lower limits on serum urate levels applied in gout management may be based on a misreading of data on mortality risks, researchers say.
Low urate levels may not in themselves pose a risk of death but may be a sign of some other illness, said Joshua F. Baker, MD, MSCE, associate professor of rheumatology and epidemiology at the University of Pennsylvania in Philadelphia.
“It points us towards being more reassured that we can be aggressive in treating gout without a concern about long-term effects for our patients,” he said in an interview. He and colleagues published their findings online in Arthritis & Rheumatology.
Previous research has linked high levels of urate with excessive fat and low levels of urate with loss of skeletal muscle mass. And epidemiologic studies have shown a U-shaped relationship between urate levels and mortality, suggesting that very high and very low levels of urate could be harmful.
Based on this correlation, and the theory that urate could have antioxidant benefits, some professional societies have recommended not lowering urate levels below a defined threshold when treating gout. The European Alliance of Associations for Rheumatology has recommended a lower limit of 3 mg/dL.
But the evidence doesn’t entirely support this caution. For example, in a clinical trial of pegloticase (Krystexxa) in patients with refractory gout, patients whose mean serum urate dropped below 2 mg/dL did not die in higher proportions than patients with higher urate levels.
To better understand the risk of low urate, Dr. Baker and colleagues analyzed data on 13,979 participants in the National Health and Nutrition Examination Survey (NHANES) during 1999-2006. The dataset included whole-body dual-energy x-ray absorptiometry (DXA) body composition measures as well as urate levels.
The researchers argue this measurement reveals more about a person’s overall health than body mass index (BMI), which doesn’t distinguish between mass from fat and mass from muscle.
They defined low lean body mass, or sarcopenia, as an appendicular lean mass index relative to fat mass index z score of –1. And they defined low urate as less than 2.5 mg/dL in women and less than 3.5 mg/dL in men.
They found that 29% of people with low urate had low lean body mass, compared with 16% of people with normal urate levels. The difference was statistically significant (P = .001).
They found an association between low urate and increased mortality (hazard ratio, 1.61; 95% confidence interval, 1.14-2.28; P = .008). But that association lost its statistical significance when the researchers adjusted for body composition and weight loss (HR, 1.30; 95% CI, 0.92-1.85; P = .13).
Dr. Baker thinks the association between elevated mortality and low urate can be explained by conditions such as cancer or lung inflammation that might on one hand increase the risk of death and on the other hand lower urate levels by lowering muscle mass. “Low uric acid levels are observed in people who have lost weight for unhealthy reasons, and that can explain relationships with long-term outcomes,” he said.
Proportions of muscle and fat could not account for the risk of mortality associated with high levels of urate, the researchers found. Those participants with urate levels above 5.7 mg/dL had a higher risk of death with higher levels of urate, and this persisted even after statistical adjustment for body composition.
The study sheds light on an important area of controversy, said Mehdi Fini, MD, of the department of medicine at the University of Colorado at Denver, Aurora, who was not involved in the research.
But body composition does not entirely explain the relationship between urate and mortality, he told this news organization. Medications used to lower urate can cause side effects that might increase mortality, he said.
Also, he said, it’s important to understand the role of comorbidities. He cited evidence that low urate is associated with renal, cardiovascular, and pulmonary conditions. Safe levels of urate might differ depending on these factors. So rather than applying the same target serum level to all patients, perhaps researchers should investigate whether lowering urate by a percentage of the patient’s current level is safer and more effective, he suggested.
He agreed with an editorial that also appeared in Arthritis & Rheumatology saying that there is no evidence for a benefit in lowering urate much below 5 mg/dL. “No matter what, I think we should just be careful,” Dr. Fini said.
Dr. Fini and Dr. Baker report no relevant financial relationships. Dr. Baker acknowledged support from a VA Clinical Science Research & Development Merit Award and a Rehabilitation R&D Merit Award.
A version of this article first appeared on Medscape.com.
Lower limits on serum urate levels applied in gout management may be based on a misreading of data on mortality risks, researchers say.
Low urate levels may not in themselves pose a risk of death but may be a sign of some other illness, said Joshua F. Baker, MD, MSCE, associate professor of rheumatology and epidemiology at the University of Pennsylvania in Philadelphia.
“It points us towards being more reassured that we can be aggressive in treating gout without a concern about long-term effects for our patients,” he said in an interview. He and colleagues published their findings online in Arthritis & Rheumatology.
Previous research has linked high levels of urate with excessive fat and low levels of urate with loss of skeletal muscle mass. And epidemiologic studies have shown a U-shaped relationship between urate levels and mortality, suggesting that very high and very low levels of urate could be harmful.
Based on this correlation, and the theory that urate could have antioxidant benefits, some professional societies have recommended not lowering urate levels below a defined threshold when treating gout. The European Alliance of Associations for Rheumatology has recommended a lower limit of 3 mg/dL.
But the evidence doesn’t entirely support this caution. For example, in a clinical trial of pegloticase (Krystexxa) in patients with refractory gout, patients whose mean serum urate dropped below 2 mg/dL did not die in higher proportions than patients with higher urate levels.
To better understand the risk of low urate, Dr. Baker and colleagues analyzed data on 13,979 participants in the National Health and Nutrition Examination Survey (NHANES) during 1999-2006. The dataset included whole-body dual-energy x-ray absorptiometry (DXA) body composition measures as well as urate levels.
The researchers argue this measurement reveals more about a person’s overall health than body mass index (BMI), which doesn’t distinguish between mass from fat and mass from muscle.
They defined low lean body mass, or sarcopenia, as an appendicular lean mass index relative to fat mass index z score of –1. And they defined low urate as less than 2.5 mg/dL in women and less than 3.5 mg/dL in men.
They found that 29% of people with low urate had low lean body mass, compared with 16% of people with normal urate levels. The difference was statistically significant (P = .001).
They found an association between low urate and increased mortality (hazard ratio, 1.61; 95% confidence interval, 1.14-2.28; P = .008). But that association lost its statistical significance when the researchers adjusted for body composition and weight loss (HR, 1.30; 95% CI, 0.92-1.85; P = .13).
Dr. Baker thinks the association between elevated mortality and low urate can be explained by conditions such as cancer or lung inflammation that might on one hand increase the risk of death and on the other hand lower urate levels by lowering muscle mass. “Low uric acid levels are observed in people who have lost weight for unhealthy reasons, and that can explain relationships with long-term outcomes,” he said.
Proportions of muscle and fat could not account for the risk of mortality associated with high levels of urate, the researchers found. Those participants with urate levels above 5.7 mg/dL had a higher risk of death with higher levels of urate, and this persisted even after statistical adjustment for body composition.
The study sheds light on an important area of controversy, said Mehdi Fini, MD, of the department of medicine at the University of Colorado at Denver, Aurora, who was not involved in the research.
But body composition does not entirely explain the relationship between urate and mortality, he told this news organization. Medications used to lower urate can cause side effects that might increase mortality, he said.
Also, he said, it’s important to understand the role of comorbidities. He cited evidence that low urate is associated with renal, cardiovascular, and pulmonary conditions. Safe levels of urate might differ depending on these factors. So rather than applying the same target serum level to all patients, perhaps researchers should investigate whether lowering urate by a percentage of the patient’s current level is safer and more effective, he suggested.
He agreed with an editorial that also appeared in Arthritis & Rheumatology saying that there is no evidence for a benefit in lowering urate much below 5 mg/dL. “No matter what, I think we should just be careful,” Dr. Fini said.
Dr. Fini and Dr. Baker report no relevant financial relationships. Dr. Baker acknowledged support from a VA Clinical Science Research & Development Merit Award and a Rehabilitation R&D Merit Award.
A version of this article first appeared on Medscape.com.
FROM ARTHRITIS & RHEUMATOLOGY