User login
Hospitalist-Specific Data Shows Rise in Use of Some CPT Codes
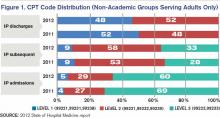
Before 2011, hospitalists had only Centers for Medicare & Medicaid Services’ (CMS) specialty-specific CPT distribution data, and no hospitalist-specific data, available when looking for benchmarks against which to compare their billing practices. Thanks to recent State of Hospital Medicine surveys, however, we now have hospitalist-specific data for the distribution of commonly used CPT codes. It’s interesting to analyze how 2011 data compares to 2012, and how the use of high-level codes varies by geographic region, employment model, compensation structure, and practice size.
In 2012, the use of the higher-level inpatient (IP) discharge code (99239) increased to 52% from 48% in 2011 among HM groups serving adults only, and the use of the highest-level IP subsequent code (99233) increased to 33% from 28% in the same comparison. This increase is in keeping with national trends. According to a May 2012 report by the Department of Health and Human Services’ Office of Inspector General, from 2001 to 2010, physicians’ billing shifted from lower-level to higher-level codes. For example, the billing of the lowest-level code (99231) decreased 16%, while the billing of the two higher-level codes (99232 and 99233) increased 6% and 9%, respectively.
Possible drivers of this change include:
- Expanded use of electronic health records (EHRs);
- Increased physician education about documentation requirements; and
- A sicker hospitalized patient population due to expanded outpatient care capabilities.
Although the proportion of high-level subsequent and discharge codes reported by SHM increased in 2012, the percent of highest-level IP admission codes (99223) actually decreased to 66% from 69%. There are many possible reasons for this. First, the elimination of consult codes by CMS in 2010 increased the overall use of admission codes but might have decreased the proportion of highest-level admission codes. Additionally, there may be an increased use of higher RVU-generating critical-care codes preferentially over billing of the highest-level admission codes. Third, there is the possibility that the extra documentation required for high-level admissions is a billing deterrent. Similarly, higher-level codes may be downcoded if documentation is lacking or incomplete.
Source: 2012 State of Hospital Medicine report
Comparatively, my health system, Allina Health, showed an increase in the use of highest-level codes for all three CPT codes analyzed.
With the increasing sophistication of EHRs and coding technology tools, it will be interesting to see the future impact on coding distribution as providers adapt to new documentation processes that support health information exchange across systems.
Comparing geographic regions, the West uses the highest proportion of high-level codes for admission, follow-up, and discharge, followed by the Midwest.
Interestingly, variation in billing by group size is only correlated directly to admission codes, but not to follow-up or discharge codes—with larger services tending to bill more of the highest-level admission codes.
Admission code use correlates directly with compensation structure; groups providing 100% of total compensation in the form of salary bill the lowest percentage of high-level admission codes. As compensation trends away from straight salaries, the percentage of high-level admission codes increases. The picture is less clear for high-level follow-up and discharge codes.
Comparing academic and nonacademic HM groups shows greater use of the highest- level admission, follow-up, and discharge codes for nonacademic HM groups. This is likely because academic hospitalists can only bill for their own time and not for time spent by medical residents.
Employment model (e.g. hospital system, private hospitalist-only groups, management companies, etc.) showed no categorical effect on CPT distribution.
Dr. Stephan is regional hospitalist medical director for Allina Health in Minneapolis and the incoming chair of SHM’s Practice Analysis Committee.
Before 2011, hospitalists had only Centers for Medicare & Medicaid Services’ (CMS) specialty-specific CPT distribution data, and no hospitalist-specific data, available when looking for benchmarks against which to compare their billing practices. Thanks to recent State of Hospital Medicine surveys, however, we now have hospitalist-specific data for the distribution of commonly used CPT codes. It’s interesting to analyze how 2011 data compares to 2012, and how the use of high-level codes varies by geographic region, employment model, compensation structure, and practice size.
In 2012, the use of the higher-level inpatient (IP) discharge code (99239) increased to 52% from 48% in 2011 among HM groups serving adults only, and the use of the highest-level IP subsequent code (99233) increased to 33% from 28% in the same comparison. This increase is in keeping with national trends. According to a May 2012 report by the Department of Health and Human Services’ Office of Inspector General, from 2001 to 2010, physicians’ billing shifted from lower-level to higher-level codes. For example, the billing of the lowest-level code (99231) decreased 16%, while the billing of the two higher-level codes (99232 and 99233) increased 6% and 9%, respectively.
Possible drivers of this change include:
- Expanded use of electronic health records (EHRs);
- Increased physician education about documentation requirements; and
- A sicker hospitalized patient population due to expanded outpatient care capabilities.
Although the proportion of high-level subsequent and discharge codes reported by SHM increased in 2012, the percent of highest-level IP admission codes (99223) actually decreased to 66% from 69%. There are many possible reasons for this. First, the elimination of consult codes by CMS in 2010 increased the overall use of admission codes but might have decreased the proportion of highest-level admission codes. Additionally, there may be an increased use of higher RVU-generating critical-care codes preferentially over billing of the highest-level admission codes. Third, there is the possibility that the extra documentation required for high-level admissions is a billing deterrent. Similarly, higher-level codes may be downcoded if documentation is lacking or incomplete.
Source: 2012 State of Hospital Medicine report
Comparatively, my health system, Allina Health, showed an increase in the use of highest-level codes for all three CPT codes analyzed.
With the increasing sophistication of EHRs and coding technology tools, it will be interesting to see the future impact on coding distribution as providers adapt to new documentation processes that support health information exchange across systems.
Comparing geographic regions, the West uses the highest proportion of high-level codes for admission, follow-up, and discharge, followed by the Midwest.
Interestingly, variation in billing by group size is only correlated directly to admission codes, but not to follow-up or discharge codes—with larger services tending to bill more of the highest-level admission codes.
Admission code use correlates directly with compensation structure; groups providing 100% of total compensation in the form of salary bill the lowest percentage of high-level admission codes. As compensation trends away from straight salaries, the percentage of high-level admission codes increases. The picture is less clear for high-level follow-up and discharge codes.
Comparing academic and nonacademic HM groups shows greater use of the highest- level admission, follow-up, and discharge codes for nonacademic HM groups. This is likely because academic hospitalists can only bill for their own time and not for time spent by medical residents.
Employment model (e.g. hospital system, private hospitalist-only groups, management companies, etc.) showed no categorical effect on CPT distribution.
Dr. Stephan is regional hospitalist medical director for Allina Health in Minneapolis and the incoming chair of SHM’s Practice Analysis Committee.
Before 2011, hospitalists had only Centers for Medicare & Medicaid Services’ (CMS) specialty-specific CPT distribution data, and no hospitalist-specific data, available when looking for benchmarks against which to compare their billing practices. Thanks to recent State of Hospital Medicine surveys, however, we now have hospitalist-specific data for the distribution of commonly used CPT codes. It’s interesting to analyze how 2011 data compares to 2012, and how the use of high-level codes varies by geographic region, employment model, compensation structure, and practice size.
In 2012, the use of the higher-level inpatient (IP) discharge code (99239) increased to 52% from 48% in 2011 among HM groups serving adults only, and the use of the highest-level IP subsequent code (99233) increased to 33% from 28% in the same comparison. This increase is in keeping with national trends. According to a May 2012 report by the Department of Health and Human Services’ Office of Inspector General, from 2001 to 2010, physicians’ billing shifted from lower-level to higher-level codes. For example, the billing of the lowest-level code (99231) decreased 16%, while the billing of the two higher-level codes (99232 and 99233) increased 6% and 9%, respectively.
Possible drivers of this change include:
- Expanded use of electronic health records (EHRs);
- Increased physician education about documentation requirements; and
- A sicker hospitalized patient population due to expanded outpatient care capabilities.
Although the proportion of high-level subsequent and discharge codes reported by SHM increased in 2012, the percent of highest-level IP admission codes (99223) actually decreased to 66% from 69%. There are many possible reasons for this. First, the elimination of consult codes by CMS in 2010 increased the overall use of admission codes but might have decreased the proportion of highest-level admission codes. Additionally, there may be an increased use of higher RVU-generating critical-care codes preferentially over billing of the highest-level admission codes. Third, there is the possibility that the extra documentation required for high-level admissions is a billing deterrent. Similarly, higher-level codes may be downcoded if documentation is lacking or incomplete.
Source: 2012 State of Hospital Medicine report
Comparatively, my health system, Allina Health, showed an increase in the use of highest-level codes for all three CPT codes analyzed.
With the increasing sophistication of EHRs and coding technology tools, it will be interesting to see the future impact on coding distribution as providers adapt to new documentation processes that support health information exchange across systems.
Comparing geographic regions, the West uses the highest proportion of high-level codes for admission, follow-up, and discharge, followed by the Midwest.
Interestingly, variation in billing by group size is only correlated directly to admission codes, but not to follow-up or discharge codes—with larger services tending to bill more of the highest-level admission codes.
Admission code use correlates directly with compensation structure; groups providing 100% of total compensation in the form of salary bill the lowest percentage of high-level admission codes. As compensation trends away from straight salaries, the percentage of high-level admission codes increases. The picture is less clear for high-level follow-up and discharge codes.
Comparing academic and nonacademic HM groups shows greater use of the highest- level admission, follow-up, and discharge codes for nonacademic HM groups. This is likely because academic hospitalists can only bill for their own time and not for time spent by medical residents.
Employment model (e.g. hospital system, private hospitalist-only groups, management companies, etc.) showed no categorical effect on CPT distribution.
Dr. Stephan is regional hospitalist medical director for Allina Health in Minneapolis and the incoming chair of SHM’s Practice Analysis Committee.
Peer Benchmarking Network May Reduce Overutilization in Pediatric Bronchiolitis
Clinical question: What is the impact of a peer benchmarking network on resource utilization in acute bronchiolitis?
Background: Acute bronchiolitis is the most common illness requiring hospitalization in children. Despite the publication of national evidence-based guidelines, variation and overuse of common therapies remains. Despite one report of successful implementation of evidence-based guidelines in a collaborative of freestanding children’s hospitals, most children are hospitalized outside of such institutions, and large-scale, lower-resource efforts have not been described.
Study design: Voluntary, quality-improvement (QI), and benchmarking collaborative.
Setting: Seventeen hospitals, including both community and freestanding children’s facilities.
Synopsis: Over a four-year period, data on 11,568 bronchiolitis hospitalizations were collected. The collaborative facilitated sharing of resources (e.g. scoring tools, guidelines), celebrated high performers on an annual basis, and encouraged regular data collection, primarily via conference calls and email. Notably, a common bundle of interventions were not used; groups worked on local improvement cycles, with only a few groups forming a small subcollaborative utilizing a shared pathway. A significant decrease in bronchodilator utilization and chest physiotherapy was seen over the course of the collaborative, although no change in chest radiography, steroid utilization, and RSV testing was noted.
This voluntary and low-resource effort by similarly motivated peers across a variety of inpatient settings demonstrated improvement over time. It is particularly notable as inpatient collaboratives with face-to-face meeting requirements, and annual fees, become more commonplace.
Study limitations include the lack of a conceptual model for studying contextual factors that might have led to improvement in the varied settings and secular changes over this time period. Additionally, EDs were not included in this initiative, which likely accounted for the lack of improvement in chest radiography and RSV testing. Nonetheless, scalable innovations such as this will become increasingly important as hospitalists search for value in health care.
Bottom line: Creating a national community of practice may reduce overutilization in bronchiolitis.
Citation: Ralston S, Garber M, Narang S, et al. Decreasing unnecessary utilization in acute bronchiolitis care: results from the Value in Inpatient Pediatrics Network. J Hosp Med. 2013;8(1):25-30.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Clinical question: What is the impact of a peer benchmarking network on resource utilization in acute bronchiolitis?
Background: Acute bronchiolitis is the most common illness requiring hospitalization in children. Despite the publication of national evidence-based guidelines, variation and overuse of common therapies remains. Despite one report of successful implementation of evidence-based guidelines in a collaborative of freestanding children’s hospitals, most children are hospitalized outside of such institutions, and large-scale, lower-resource efforts have not been described.
Study design: Voluntary, quality-improvement (QI), and benchmarking collaborative.
Setting: Seventeen hospitals, including both community and freestanding children’s facilities.
Synopsis: Over a four-year period, data on 11,568 bronchiolitis hospitalizations were collected. The collaborative facilitated sharing of resources (e.g. scoring tools, guidelines), celebrated high performers on an annual basis, and encouraged regular data collection, primarily via conference calls and email. Notably, a common bundle of interventions were not used; groups worked on local improvement cycles, with only a few groups forming a small subcollaborative utilizing a shared pathway. A significant decrease in bronchodilator utilization and chest physiotherapy was seen over the course of the collaborative, although no change in chest radiography, steroid utilization, and RSV testing was noted.
This voluntary and low-resource effort by similarly motivated peers across a variety of inpatient settings demonstrated improvement over time. It is particularly notable as inpatient collaboratives with face-to-face meeting requirements, and annual fees, become more commonplace.
Study limitations include the lack of a conceptual model for studying contextual factors that might have led to improvement in the varied settings and secular changes over this time period. Additionally, EDs were not included in this initiative, which likely accounted for the lack of improvement in chest radiography and RSV testing. Nonetheless, scalable innovations such as this will become increasingly important as hospitalists search for value in health care.
Bottom line: Creating a national community of practice may reduce overutilization in bronchiolitis.
Citation: Ralston S, Garber M, Narang S, et al. Decreasing unnecessary utilization in acute bronchiolitis care: results from the Value in Inpatient Pediatrics Network. J Hosp Med. 2013;8(1):25-30.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Clinical question: What is the impact of a peer benchmarking network on resource utilization in acute bronchiolitis?
Background: Acute bronchiolitis is the most common illness requiring hospitalization in children. Despite the publication of national evidence-based guidelines, variation and overuse of common therapies remains. Despite one report of successful implementation of evidence-based guidelines in a collaborative of freestanding children’s hospitals, most children are hospitalized outside of such institutions, and large-scale, lower-resource efforts have not been described.
Study design: Voluntary, quality-improvement (QI), and benchmarking collaborative.
Setting: Seventeen hospitals, including both community and freestanding children’s facilities.
Synopsis: Over a four-year period, data on 11,568 bronchiolitis hospitalizations were collected. The collaborative facilitated sharing of resources (e.g. scoring tools, guidelines), celebrated high performers on an annual basis, and encouraged regular data collection, primarily via conference calls and email. Notably, a common bundle of interventions were not used; groups worked on local improvement cycles, with only a few groups forming a small subcollaborative utilizing a shared pathway. A significant decrease in bronchodilator utilization and chest physiotherapy was seen over the course of the collaborative, although no change in chest radiography, steroid utilization, and RSV testing was noted.
This voluntary and low-resource effort by similarly motivated peers across a variety of inpatient settings demonstrated improvement over time. It is particularly notable as inpatient collaboratives with face-to-face meeting requirements, and annual fees, become more commonplace.
Study limitations include the lack of a conceptual model for studying contextual factors that might have led to improvement in the varied settings and secular changes over this time period. Additionally, EDs were not included in this initiative, which likely accounted for the lack of improvement in chest radiography and RSV testing. Nonetheless, scalable innovations such as this will become increasingly important as hospitalists search for value in health care.
Bottom line: Creating a national community of practice may reduce overutilization in bronchiolitis.
Citation: Ralston S, Garber M, Narang S, et al. Decreasing unnecessary utilization in acute bronchiolitis care: results from the Value in Inpatient Pediatrics Network. J Hosp Med. 2013;8(1):25-30.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Hospitals' Battle Against Superbugs Goes Robotic
One in 20 hospitalized patients picks up an infection in the hospital, and a recent article by the Associated Press describes the emergence of new technologies to fight antibiotic-resistant superbugs: “They sweep. They swab. They sterilize. And still the germs persist.”1
Hospitals across the country are testing new approaches to stop the spread of superbugs, which are tied to an estimated 100,000 deaths per year, according to the CDC. New approaches include robotlike machines that emit ultraviolet light or hydrogen-peroxide vapors, germ-resistant copper bed rails and call buttons, antimicrobial linens and wall paint, and hydrogel post-surgical dressings infused with silver ions that have antimicrobial properties.
Research firm Frost & Sullivan estimates that the market for bug-killing products and technologies will grow to $80 million from $30 million in the next three years. And yet evidence of positive outcomes from them continues to be debated.
“In short, escalating antimicrobial-resistance issues have us facing the prospect of untreatable bacterial pathogens, particularly involving gram-negative organisms,” James Pile, MD, FACP, SFHM, a hospital medicine and infectious diseases physician at Cleveland Clinic, wrote in an email. “In fact, many of our hospitals already deal with a limited number of infections caused by bacteria we have no clearly effective antibiotics against; the issue is only going to get worse.”
As an example, the CDC recently issued a warning about carbapenum-resistant Enterobacteriaceae (CRE), which has a 40% mortality rate and last year was reported in 4.6% of U.S. hospitals.2 CDC recommends that hospitals use more of the existing prevention measures against CRE, including active-case detection and segregation of patients and the staff who care for them. Dr. Pile says health facilities need to do a better job of preventing infections involving multi-drug-resistant pathogens, but in the meantime, “proven technologies such as proper hand hygiene and antimicrobial stewardship are more important than ever.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
One in 20 hospitalized patients picks up an infection in the hospital, and a recent article by the Associated Press describes the emergence of new technologies to fight antibiotic-resistant superbugs: “They sweep. They swab. They sterilize. And still the germs persist.”1
Hospitals across the country are testing new approaches to stop the spread of superbugs, which are tied to an estimated 100,000 deaths per year, according to the CDC. New approaches include robotlike machines that emit ultraviolet light or hydrogen-peroxide vapors, germ-resistant copper bed rails and call buttons, antimicrobial linens and wall paint, and hydrogel post-surgical dressings infused with silver ions that have antimicrobial properties.
Research firm Frost & Sullivan estimates that the market for bug-killing products and technologies will grow to $80 million from $30 million in the next three years. And yet evidence of positive outcomes from them continues to be debated.
“In short, escalating antimicrobial-resistance issues have us facing the prospect of untreatable bacterial pathogens, particularly involving gram-negative organisms,” James Pile, MD, FACP, SFHM, a hospital medicine and infectious diseases physician at Cleveland Clinic, wrote in an email. “In fact, many of our hospitals already deal with a limited number of infections caused by bacteria we have no clearly effective antibiotics against; the issue is only going to get worse.”
As an example, the CDC recently issued a warning about carbapenum-resistant Enterobacteriaceae (CRE), which has a 40% mortality rate and last year was reported in 4.6% of U.S. hospitals.2 CDC recommends that hospitals use more of the existing prevention measures against CRE, including active-case detection and segregation of patients and the staff who care for them. Dr. Pile says health facilities need to do a better job of preventing infections involving multi-drug-resistant pathogens, but in the meantime, “proven technologies such as proper hand hygiene and antimicrobial stewardship are more important than ever.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
One in 20 hospitalized patients picks up an infection in the hospital, and a recent article by the Associated Press describes the emergence of new technologies to fight antibiotic-resistant superbugs: “They sweep. They swab. They sterilize. And still the germs persist.”1
Hospitals across the country are testing new approaches to stop the spread of superbugs, which are tied to an estimated 100,000 deaths per year, according to the CDC. New approaches include robotlike machines that emit ultraviolet light or hydrogen-peroxide vapors, germ-resistant copper bed rails and call buttons, antimicrobial linens and wall paint, and hydrogel post-surgical dressings infused with silver ions that have antimicrobial properties.
Research firm Frost & Sullivan estimates that the market for bug-killing products and technologies will grow to $80 million from $30 million in the next three years. And yet evidence of positive outcomes from them continues to be debated.
“In short, escalating antimicrobial-resistance issues have us facing the prospect of untreatable bacterial pathogens, particularly involving gram-negative organisms,” James Pile, MD, FACP, SFHM, a hospital medicine and infectious diseases physician at Cleveland Clinic, wrote in an email. “In fact, many of our hospitals already deal with a limited number of infections caused by bacteria we have no clearly effective antibiotics against; the issue is only going to get worse.”
As an example, the CDC recently issued a warning about carbapenum-resistant Enterobacteriaceae (CRE), which has a 40% mortality rate and last year was reported in 4.6% of U.S. hospitals.2 CDC recommends that hospitals use more of the existing prevention measures against CRE, including active-case detection and segregation of patients and the staff who care for them. Dr. Pile says health facilities need to do a better job of preventing infections involving multi-drug-resistant pathogens, but in the meantime, “proven technologies such as proper hand hygiene and antimicrobial stewardship are more important than ever.”
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Stobbe, M. Germ-zapping “robots”: Hospitals combat superbugs. Associated Press website. Available at: http://bigstory.ap.org/article/hospitals-see-surge-superbug-fighting-products. Accessed June 7, 2013.
- Centers for Disease Control and Prevention. Vital Signs: Carbapenem-Resistant Enterobacteriaceae. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6209a3.htm?s_cid=mm6209a3_w. Accessed June 7, 2013.
- Wise ME, Scott RD, Baggs JM, et al. National estimates of central line-associated bloodstream infections in critical care patients. Infect Control Hosp Epidemiol, 2013;34(6):547-554.
- Hsu E, Lin D, Evans SJ, et al. Doing well by doing good: assessing the cost savings of an intervention to reduce central line-associated bloodstream infections in a Hawaii hospital. Am J Med Qual, 2013 May 7 [Epub ahead of print].
- Association of American Medical Colleges. Medical school enrollment on pace to reach 30 percent increase by 2017. Association of American Medical Colleges website. Available at: https://www.aamc.org/newsroom/newsreleases/ 335244/050213.html. Accessed June 7, 2013.
Reduced Estimate to Fix SGR Formula Brings Hope for Change
The tiresome cycle of the sustainable growth rate (SGR) continues and, as a result, providers are facing a pay cut of approximately 25% at the end of 2013. With virtually universal agreement that something must be done to permanently repeal the SGR, the insurmountable barrier to a solution has been the cost, which is estimated at $245 billion.
However, a bright spot has emerged.
Several months ago, the Congressional Budget Office produced an anomalous, revised SGR repeal estimate of $138 billion. At nearly half the cost of previous estimates, this is a much less daunting budgetary hole to fill. Needless to say, this revised estimate has breathed new life into the potential to permanently fix the SGR this year. The only catch is that this low estimate is unlikely to persist, so a flurry of activity is expected to last throughout the summer months before the window of opportunity closes.
One of the earliest proposals to move away from fee-for-service to a payment system rooted in quality and value came from the reintroduction of legislation by U.S. Reps. Allyson Schwartz (D-Pa.) and Joe Heck (R-Nev.). SHM is actively supporting this legislation and will continue to do so, but it will give the same attention to other reasonable plans designed to move away from the SGR by incorporating the concepts of quality and value as laid out by Schwartz and Heck.
Along these lines, a joint effort by House Energy and Commerce Committee chairman
Fred Upton (R-Mich.) and House Ways and Means Committee chairman Dave Camp (R-Mich.) would repeal the SGR and replace it with a more sustainable payment system. The plan is being developed iteratively, with opportunities for specialty societies, such as SHM, to provide input along the way. Clear details have yet to emerge because the plan is still in its early stages, but broadly, it will repeal the SGR, replacing it with quality and resource use metrics coupled with value-based payment, and somehow incorporate alternative payment models, such as accountable-care organizations (ACOs). This may sound familiar
because much of it is.
The Centers for Medicare & Medicaid Services (CMS) is developing programs, guided by the Affordable Care Act (ACA), to meet many of these systemic needs in the absence of a repeal of the SGR. The Physician Quality Reporting System (PQRS) is transitioning into a mandatory program, and it’s coupling with Quality and Resource Use Reports (QRURs) brings value into the equation. Both of these programs are a part of the ACA-mandated Physician Value-Based Payment Modifier (VBPM), which implements a level of value-based payment to all physicians by 2017. Additionally, the Center for Medicare & Medicaid Innovation, along with Medicare itself, is developing and testing many alternative models, such as ACOs, bundled payments, and patient-centered medical homes, to name a few.
Upton and Camp have expressed that their goal is to not only repeal the SGR, but also to establish a system that pays for value and is less piecemeal and confusing than what is currently being implemented. For example, they are looking at ways to potentially unify the often disparate yet overlapping reporting requirements placed on physicians through such programs as PQRS, Meaningful Use, and VBPM. This is a great opportunity to take the knowledge and experience hospitalists have with these current CMS programs and advocate for aligning programs, ensuring the usefulness of quality measurement, and reducing administrative barriers and burdens.
Ultimately, the repeal of the SGR will take much thought and legislative will to accomplish. With a broad framework in place, the process has at least begun. It remains to be seen whether Congress will act now on the SGR “sale” and help the health-care system transition into something more sustainable and stable.
Josh Boswell is SHM’s senior manager of government relations
The tiresome cycle of the sustainable growth rate (SGR) continues and, as a result, providers are facing a pay cut of approximately 25% at the end of 2013. With virtually universal agreement that something must be done to permanently repeal the SGR, the insurmountable barrier to a solution has been the cost, which is estimated at $245 billion.
However, a bright spot has emerged.
Several months ago, the Congressional Budget Office produced an anomalous, revised SGR repeal estimate of $138 billion. At nearly half the cost of previous estimates, this is a much less daunting budgetary hole to fill. Needless to say, this revised estimate has breathed new life into the potential to permanently fix the SGR this year. The only catch is that this low estimate is unlikely to persist, so a flurry of activity is expected to last throughout the summer months before the window of opportunity closes.
One of the earliest proposals to move away from fee-for-service to a payment system rooted in quality and value came from the reintroduction of legislation by U.S. Reps. Allyson Schwartz (D-Pa.) and Joe Heck (R-Nev.). SHM is actively supporting this legislation and will continue to do so, but it will give the same attention to other reasonable plans designed to move away from the SGR by incorporating the concepts of quality and value as laid out by Schwartz and Heck.
Along these lines, a joint effort by House Energy and Commerce Committee chairman
Fred Upton (R-Mich.) and House Ways and Means Committee chairman Dave Camp (R-Mich.) would repeal the SGR and replace it with a more sustainable payment system. The plan is being developed iteratively, with opportunities for specialty societies, such as SHM, to provide input along the way. Clear details have yet to emerge because the plan is still in its early stages, but broadly, it will repeal the SGR, replacing it with quality and resource use metrics coupled with value-based payment, and somehow incorporate alternative payment models, such as accountable-care organizations (ACOs). This may sound familiar
because much of it is.
The Centers for Medicare & Medicaid Services (CMS) is developing programs, guided by the Affordable Care Act (ACA), to meet many of these systemic needs in the absence of a repeal of the SGR. The Physician Quality Reporting System (PQRS) is transitioning into a mandatory program, and it’s coupling with Quality and Resource Use Reports (QRURs) brings value into the equation. Both of these programs are a part of the ACA-mandated Physician Value-Based Payment Modifier (VBPM), which implements a level of value-based payment to all physicians by 2017. Additionally, the Center for Medicare & Medicaid Innovation, along with Medicare itself, is developing and testing many alternative models, such as ACOs, bundled payments, and patient-centered medical homes, to name a few.
Upton and Camp have expressed that their goal is to not only repeal the SGR, but also to establish a system that pays for value and is less piecemeal and confusing than what is currently being implemented. For example, they are looking at ways to potentially unify the often disparate yet overlapping reporting requirements placed on physicians through such programs as PQRS, Meaningful Use, and VBPM. This is a great opportunity to take the knowledge and experience hospitalists have with these current CMS programs and advocate for aligning programs, ensuring the usefulness of quality measurement, and reducing administrative barriers and burdens.
Ultimately, the repeal of the SGR will take much thought and legislative will to accomplish. With a broad framework in place, the process has at least begun. It remains to be seen whether Congress will act now on the SGR “sale” and help the health-care system transition into something more sustainable and stable.
Josh Boswell is SHM’s senior manager of government relations
The tiresome cycle of the sustainable growth rate (SGR) continues and, as a result, providers are facing a pay cut of approximately 25% at the end of 2013. With virtually universal agreement that something must be done to permanently repeal the SGR, the insurmountable barrier to a solution has been the cost, which is estimated at $245 billion.
However, a bright spot has emerged.
Several months ago, the Congressional Budget Office produced an anomalous, revised SGR repeal estimate of $138 billion. At nearly half the cost of previous estimates, this is a much less daunting budgetary hole to fill. Needless to say, this revised estimate has breathed new life into the potential to permanently fix the SGR this year. The only catch is that this low estimate is unlikely to persist, so a flurry of activity is expected to last throughout the summer months before the window of opportunity closes.
One of the earliest proposals to move away from fee-for-service to a payment system rooted in quality and value came from the reintroduction of legislation by U.S. Reps. Allyson Schwartz (D-Pa.) and Joe Heck (R-Nev.). SHM is actively supporting this legislation and will continue to do so, but it will give the same attention to other reasonable plans designed to move away from the SGR by incorporating the concepts of quality and value as laid out by Schwartz and Heck.
Along these lines, a joint effort by House Energy and Commerce Committee chairman
Fred Upton (R-Mich.) and House Ways and Means Committee chairman Dave Camp (R-Mich.) would repeal the SGR and replace it with a more sustainable payment system. The plan is being developed iteratively, with opportunities for specialty societies, such as SHM, to provide input along the way. Clear details have yet to emerge because the plan is still in its early stages, but broadly, it will repeal the SGR, replacing it with quality and resource use metrics coupled with value-based payment, and somehow incorporate alternative payment models, such as accountable-care organizations (ACOs). This may sound familiar
because much of it is.
The Centers for Medicare & Medicaid Services (CMS) is developing programs, guided by the Affordable Care Act (ACA), to meet many of these systemic needs in the absence of a repeal of the SGR. The Physician Quality Reporting System (PQRS) is transitioning into a mandatory program, and it’s coupling with Quality and Resource Use Reports (QRURs) brings value into the equation. Both of these programs are a part of the ACA-mandated Physician Value-Based Payment Modifier (VBPM), which implements a level of value-based payment to all physicians by 2017. Additionally, the Center for Medicare & Medicaid Innovation, along with Medicare itself, is developing and testing many alternative models, such as ACOs, bundled payments, and patient-centered medical homes, to name a few.
Upton and Camp have expressed that their goal is to not only repeal the SGR, but also to establish a system that pays for value and is less piecemeal and confusing than what is currently being implemented. For example, they are looking at ways to potentially unify the often disparate yet overlapping reporting requirements placed on physicians through such programs as PQRS, Meaningful Use, and VBPM. This is a great opportunity to take the knowledge and experience hospitalists have with these current CMS programs and advocate for aligning programs, ensuring the usefulness of quality measurement, and reducing administrative barriers and burdens.
Ultimately, the repeal of the SGR will take much thought and legislative will to accomplish. With a broad framework in place, the process has at least begun. It remains to be seen whether Congress will act now on the SGR “sale” and help the health-care system transition into something more sustainable and stable.
Josh Boswell is SHM’s senior manager of government relations
Quality Improvement (QI) Remains a Central Theme at HM13
Like a grinning child at a carnival, Iqbal M. Binoj, MD, steps right up and gives it a try—except instead of tossing rings, he’s gripping an intraosseous infusion drill.
A tutor shows him how the device, which looks remarkably like a glue gun, inserts into the bones of the shoulder or knee and drills down until it hits the marrow. He is guided on using a steady speed to maintain the integrity of the cavity. He’s also taught about the maneuver’s low complication rates and ability to expedite workups.
“I’ve seen it used before, but I never did it,” says Dr. Binoj, a hospitalist with Cogent HMG at Genesis Medical Center in Davenport, Iowa.
Well, he never did it before a hands-on pre-course at HM13 that focused on improving hospitalists’ proficiency at such procedures as lumbar punctures and ultrasound-guided vascular access. Quality improvement (QI) is always a focus of SHM’s annual meeting, but sometimes the science of improving care is viewed from up on high.
Not everything needs to be a national imitative, an institution-wide project, or even a unit-based intervention. Sometimes, it’s as simple as teaching a room full of hospitalists how to use an intraosseous infusion drill, says Michelle Fox, RN, BSN, senior director of clinical affairs with Vidacare, which manufactures the drill used in the demonstration.
“Hospitalists have an increasing role in doing these procedures, not only in the environment they predominantly support but in other areas of the hospital,” Fox says, adding that “the primary goal of this course is to give them the opportunity to perfect those skills.”
Hospitalist Bradley Rosen, MD, MBA, FHM, medical of the inpatient specialty program at Cedars-Sinai in Los Angeles, says the point of hands-on demonstrations is to translate QI to the bedside. Take ultrasound devices, he says. In the past few years, the technology has become less expensive, better in resolution, more common, and more portable. Hospitalists must ensure hands-on training that keeps pace with that technology.
“We actually want people to get gloves on, hands on, learn where they may have challenges in terms of their own dexterity or workflow, which hand is dominant, and how to visualize on the ultrasound machine a three-dimensional structure in 2D,” he says. “We don’t want people watching from the sidelines. ... We try to get people in it and engaged.”
And once hospitalists master procedures or diagnostic maneuvers, they invariably are sought out by other physicians to pass that knowledge on to others, Dr. Rosen says.
“In so doing, we get involved in larger quality initiatives and systemwide changes that can go top-down,” he adds, “but from our perspective, it starts with the individual practitioner. And I think SHM has always advocated and preached the importance of the individual hospitalist doing the best possible job for your patient, and the group, and the institution.”
Shared Excellence
What’s best for individual institutions moving forward is what worries SHM immediate past president Shaun Frost, MD, SFHM. He fears CMS’ Value-Based Payment Modifier (VBPM) program could have the unintended consequence of spurring some hospitals to hang on to innovative ideas in order to keep a competitive business advantage.
In health care, where quality and affordability have long been viewed as valuable for nonmonetary reasons, “the medical profession willingly shares new information” to improve patient care, Dr. Frost said in his farewell speech. But he is concerned that commodification—imbuing monetary value into something that previously had none—could change that dynamic, a situation he says is “ethically not acceptable.”
“When somebody builds a better mousetrap, it should be freely shared so that all patients have the opportunity to benefit,” Dr. Frost said. “The pursuit of economic competitive advantage should not prevent us from collaborating and sharing new ideas that hopefully make the health system better.”
Kendall Rogers, MD, FACP, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque, N.M., says part of that improvement in quality and patient safety will come via hospitalists pushing for improvements to health information technology (HIT), particularly to maximize computerized physician order entry (CPOE) and order sets. He empathizes with those who complain about the operability of existing systems but urges physicians to stop complaining and take action.
“We need to stop accepting what our existing limitations are, and we need to be the innovators,” he says. “Many of us aren’t even thinking about, ‘What are the products we need?’ We’re just reacting to the products we currently have and stating how they don’t meet our needs.”
He suggests people communally report safety or troubleshooting issues, in part via Hospital Medicine Exchange (HMX), an online community SHM launched last year to discuss HM issues (www.hmxchange.org). He also wants hospitalists to push HIT vendors to provide improved functionality, and for institutions to provide necessary training.
“We just need to be vocal,” says Dr. Rogers, chair of SHM’s IT Executive Committee. “I do believe this is all leading us to a good place, but there’s a dip down before we have a swing up.”
Frustration Surge
In the long run, hospitalist Anuj Mehta, MD, medical director of the adult hospitalist program at Nyack Hospital in New York, agrees with Dr. Rogers. But as a provider seeing patients day after day, he says it’s often easier to not engage HIT than it is to slog through it.
“We try to work around the system, and sometimes it’s a much longer workaround,” he says. “So what happens is loss of productivity, greater length of stay, poor patient satisfaction, more screen time, and less bedside time.”
Dr. Mehta says frustration is building as society—outside of medicine—moves rapidly through such technology as smartphones, tablets, and other intuitive devices that make actions easier. He notes that his toddler daughter could learn how to navigate an iPad in a fraction of the time it takes him to complete an HIT training course.
“You cannot have physicians going through learning for four hours, learning a system to do step one before step two before step three,” he laments. “It should flow naturally. I don’t think the IT people have realized that as of yet.”
Richard Quinn is a freelance writer in New Jersey.
Like a grinning child at a carnival, Iqbal M. Binoj, MD, steps right up and gives it a try—except instead of tossing rings, he’s gripping an intraosseous infusion drill.
A tutor shows him how the device, which looks remarkably like a glue gun, inserts into the bones of the shoulder or knee and drills down until it hits the marrow. He is guided on using a steady speed to maintain the integrity of the cavity. He’s also taught about the maneuver’s low complication rates and ability to expedite workups.
“I’ve seen it used before, but I never did it,” says Dr. Binoj, a hospitalist with Cogent HMG at Genesis Medical Center in Davenport, Iowa.
Well, he never did it before a hands-on pre-course at HM13 that focused on improving hospitalists’ proficiency at such procedures as lumbar punctures and ultrasound-guided vascular access. Quality improvement (QI) is always a focus of SHM’s annual meeting, but sometimes the science of improving care is viewed from up on high.
Not everything needs to be a national imitative, an institution-wide project, or even a unit-based intervention. Sometimes, it’s as simple as teaching a room full of hospitalists how to use an intraosseous infusion drill, says Michelle Fox, RN, BSN, senior director of clinical affairs with Vidacare, which manufactures the drill used in the demonstration.
“Hospitalists have an increasing role in doing these procedures, not only in the environment they predominantly support but in other areas of the hospital,” Fox says, adding that “the primary goal of this course is to give them the opportunity to perfect those skills.”
Hospitalist Bradley Rosen, MD, MBA, FHM, medical of the inpatient specialty program at Cedars-Sinai in Los Angeles, says the point of hands-on demonstrations is to translate QI to the bedside. Take ultrasound devices, he says. In the past few years, the technology has become less expensive, better in resolution, more common, and more portable. Hospitalists must ensure hands-on training that keeps pace with that technology.
“We actually want people to get gloves on, hands on, learn where they may have challenges in terms of their own dexterity or workflow, which hand is dominant, and how to visualize on the ultrasound machine a three-dimensional structure in 2D,” he says. “We don’t want people watching from the sidelines. ... We try to get people in it and engaged.”
And once hospitalists master procedures or diagnostic maneuvers, they invariably are sought out by other physicians to pass that knowledge on to others, Dr. Rosen says.
“In so doing, we get involved in larger quality initiatives and systemwide changes that can go top-down,” he adds, “but from our perspective, it starts with the individual practitioner. And I think SHM has always advocated and preached the importance of the individual hospitalist doing the best possible job for your patient, and the group, and the institution.”
Shared Excellence
What’s best for individual institutions moving forward is what worries SHM immediate past president Shaun Frost, MD, SFHM. He fears CMS’ Value-Based Payment Modifier (VBPM) program could have the unintended consequence of spurring some hospitals to hang on to innovative ideas in order to keep a competitive business advantage.
In health care, where quality and affordability have long been viewed as valuable for nonmonetary reasons, “the medical profession willingly shares new information” to improve patient care, Dr. Frost said in his farewell speech. But he is concerned that commodification—imbuing monetary value into something that previously had none—could change that dynamic, a situation he says is “ethically not acceptable.”
“When somebody builds a better mousetrap, it should be freely shared so that all patients have the opportunity to benefit,” Dr. Frost said. “The pursuit of economic competitive advantage should not prevent us from collaborating and sharing new ideas that hopefully make the health system better.”
Kendall Rogers, MD, FACP, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque, N.M., says part of that improvement in quality and patient safety will come via hospitalists pushing for improvements to health information technology (HIT), particularly to maximize computerized physician order entry (CPOE) and order sets. He empathizes with those who complain about the operability of existing systems but urges physicians to stop complaining and take action.
“We need to stop accepting what our existing limitations are, and we need to be the innovators,” he says. “Many of us aren’t even thinking about, ‘What are the products we need?’ We’re just reacting to the products we currently have and stating how they don’t meet our needs.”
He suggests people communally report safety or troubleshooting issues, in part via Hospital Medicine Exchange (HMX), an online community SHM launched last year to discuss HM issues (www.hmxchange.org). He also wants hospitalists to push HIT vendors to provide improved functionality, and for institutions to provide necessary training.
“We just need to be vocal,” says Dr. Rogers, chair of SHM’s IT Executive Committee. “I do believe this is all leading us to a good place, but there’s a dip down before we have a swing up.”
Frustration Surge
In the long run, hospitalist Anuj Mehta, MD, medical director of the adult hospitalist program at Nyack Hospital in New York, agrees with Dr. Rogers. But as a provider seeing patients day after day, he says it’s often easier to not engage HIT than it is to slog through it.
“We try to work around the system, and sometimes it’s a much longer workaround,” he says. “So what happens is loss of productivity, greater length of stay, poor patient satisfaction, more screen time, and less bedside time.”
Dr. Mehta says frustration is building as society—outside of medicine—moves rapidly through such technology as smartphones, tablets, and other intuitive devices that make actions easier. He notes that his toddler daughter could learn how to navigate an iPad in a fraction of the time it takes him to complete an HIT training course.
“You cannot have physicians going through learning for four hours, learning a system to do step one before step two before step three,” he laments. “It should flow naturally. I don’t think the IT people have realized that as of yet.”
Richard Quinn is a freelance writer in New Jersey.
Like a grinning child at a carnival, Iqbal M. Binoj, MD, steps right up and gives it a try—except instead of tossing rings, he’s gripping an intraosseous infusion drill.
A tutor shows him how the device, which looks remarkably like a glue gun, inserts into the bones of the shoulder or knee and drills down until it hits the marrow. He is guided on using a steady speed to maintain the integrity of the cavity. He’s also taught about the maneuver’s low complication rates and ability to expedite workups.
“I’ve seen it used before, but I never did it,” says Dr. Binoj, a hospitalist with Cogent HMG at Genesis Medical Center in Davenport, Iowa.
Well, he never did it before a hands-on pre-course at HM13 that focused on improving hospitalists’ proficiency at such procedures as lumbar punctures and ultrasound-guided vascular access. Quality improvement (QI) is always a focus of SHM’s annual meeting, but sometimes the science of improving care is viewed from up on high.
Not everything needs to be a national imitative, an institution-wide project, or even a unit-based intervention. Sometimes, it’s as simple as teaching a room full of hospitalists how to use an intraosseous infusion drill, says Michelle Fox, RN, BSN, senior director of clinical affairs with Vidacare, which manufactures the drill used in the demonstration.
“Hospitalists have an increasing role in doing these procedures, not only in the environment they predominantly support but in other areas of the hospital,” Fox says, adding that “the primary goal of this course is to give them the opportunity to perfect those skills.”
Hospitalist Bradley Rosen, MD, MBA, FHM, medical of the inpatient specialty program at Cedars-Sinai in Los Angeles, says the point of hands-on demonstrations is to translate QI to the bedside. Take ultrasound devices, he says. In the past few years, the technology has become less expensive, better in resolution, more common, and more portable. Hospitalists must ensure hands-on training that keeps pace with that technology.
“We actually want people to get gloves on, hands on, learn where they may have challenges in terms of their own dexterity or workflow, which hand is dominant, and how to visualize on the ultrasound machine a three-dimensional structure in 2D,” he says. “We don’t want people watching from the sidelines. ... We try to get people in it and engaged.”
And once hospitalists master procedures or diagnostic maneuvers, they invariably are sought out by other physicians to pass that knowledge on to others, Dr. Rosen says.
“In so doing, we get involved in larger quality initiatives and systemwide changes that can go top-down,” he adds, “but from our perspective, it starts with the individual practitioner. And I think SHM has always advocated and preached the importance of the individual hospitalist doing the best possible job for your patient, and the group, and the institution.”
Shared Excellence
What’s best for individual institutions moving forward is what worries SHM immediate past president Shaun Frost, MD, SFHM. He fears CMS’ Value-Based Payment Modifier (VBPM) program could have the unintended consequence of spurring some hospitals to hang on to innovative ideas in order to keep a competitive business advantage.
In health care, where quality and affordability have long been viewed as valuable for nonmonetary reasons, “the medical profession willingly shares new information” to improve patient care, Dr. Frost said in his farewell speech. But he is concerned that commodification—imbuing monetary value into something that previously had none—could change that dynamic, a situation he says is “ethically not acceptable.”
“When somebody builds a better mousetrap, it should be freely shared so that all patients have the opportunity to benefit,” Dr. Frost said. “The pursuit of economic competitive advantage should not prevent us from collaborating and sharing new ideas that hopefully make the health system better.”
Kendall Rogers, MD, FACP, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque, N.M., says part of that improvement in quality and patient safety will come via hospitalists pushing for improvements to health information technology (HIT), particularly to maximize computerized physician order entry (CPOE) and order sets. He empathizes with those who complain about the operability of existing systems but urges physicians to stop complaining and take action.
“We need to stop accepting what our existing limitations are, and we need to be the innovators,” he says. “Many of us aren’t even thinking about, ‘What are the products we need?’ We’re just reacting to the products we currently have and stating how they don’t meet our needs.”
He suggests people communally report safety or troubleshooting issues, in part via Hospital Medicine Exchange (HMX), an online community SHM launched last year to discuss HM issues (www.hmxchange.org). He also wants hospitalists to push HIT vendors to provide improved functionality, and for institutions to provide necessary training.
“We just need to be vocal,” says Dr. Rogers, chair of SHM’s IT Executive Committee. “I do believe this is all leading us to a good place, but there’s a dip down before we have a swing up.”
Frustration Surge
In the long run, hospitalist Anuj Mehta, MD, medical director of the adult hospitalist program at Nyack Hospital in New York, agrees with Dr. Rogers. But as a provider seeing patients day after day, he says it’s often easier to not engage HIT than it is to slog through it.
“We try to work around the system, and sometimes it’s a much longer workaround,” he says. “So what happens is loss of productivity, greater length of stay, poor patient satisfaction, more screen time, and less bedside time.”
Dr. Mehta says frustration is building as society—outside of medicine—moves rapidly through such technology as smartphones, tablets, and other intuitive devices that make actions easier. He notes that his toddler daughter could learn how to navigate an iPad in a fraction of the time it takes him to complete an HIT training course.
“You cannot have physicians going through learning for four hours, learning a system to do step one before step two before step three,” he laments. “It should flow naturally. I don’t think the IT people have realized that as of yet.”
Richard Quinn is a freelance writer in New Jersey.
Health-Care Journalists Tackle Barriers to Hospital Safety Records
The Association of Health Care Journalists, a professional association that includes 1,400 journalists, is tackling some of the barriers consumers and advocates face when trying to access such information as hospital safety records. AHCJ’s www.HospitalInfections.org is a free, searchable news application that went live in March with detailed reports of deficiencies cited in federal inspection visits for acute- and critical-access hospitals nationwide.
Through years of advocacy, AHCJ has filed Freedom of Information Act requests and negotiated with the Centers for Medicare & Medicaid Services (CMS) to get access to hospital safety information in electronic form.
CMS’ Hospital Compare website (www.medicare.gov/hospitalcompare) and the Joint Commission’s Quality Check (www.qualitycheck.org) program both publicly report hospital quality data, but they have significant time lags and data that are difficult for the average consumer to understand, according to AHCJ. The association touts its new site as an “early attempt by an advocacy group to make hospital safety information easier to access and more consumer-driven.”
“Being able to easily review the performance of your local hospital is vital for health-care journalists and for the public,” AHCJ president Charles Ornstein, a senior reporter at ProPublica in New York, said in a statement.
Larry Beresford is a freelance writer in San Francisco
References
- Weigel C, Suen W, Gupta G. Using Lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013 Feb 4 [Epub ahead of print].
- Morganti KG, Lovejoy S, Beckjord EB, Haviland AM, Haas AC, Farley DO. A retrospective evaluation of the Perfecting Patient Care University training program for health care organizations. Am J Med Qual. 2013 Apr 9 [Epub ahead of print].
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators’ Academy: fulfilling an unmet need for faculty development. Am J Med Qual. 2013 Apr 11 [Epub ahead of print].
- Dong XQ, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 Apr 8:1-7. doi: 10.1001/jamainternmed.2013.238 [Epub ahead of print].
- Cisco mConcierge. 90% American workers use their own smartphones for work. Cisco mConcierge website. Available at: http://www.ciscomcon.com/sw/swchannel/registration/internet/registrationcfm?SWAPPID=91&RegPageID=350200&SWTHEMEID=12949. Accessed
The Association of Health Care Journalists, a professional association that includes 1,400 journalists, is tackling some of the barriers consumers and advocates face when trying to access such information as hospital safety records. AHCJ’s www.HospitalInfections.org is a free, searchable news application that went live in March with detailed reports of deficiencies cited in federal inspection visits for acute- and critical-access hospitals nationwide.
Through years of advocacy, AHCJ has filed Freedom of Information Act requests and negotiated with the Centers for Medicare & Medicaid Services (CMS) to get access to hospital safety information in electronic form.
CMS’ Hospital Compare website (www.medicare.gov/hospitalcompare) and the Joint Commission’s Quality Check (www.qualitycheck.org) program both publicly report hospital quality data, but they have significant time lags and data that are difficult for the average consumer to understand, according to AHCJ. The association touts its new site as an “early attempt by an advocacy group to make hospital safety information easier to access and more consumer-driven.”
“Being able to easily review the performance of your local hospital is vital for health-care journalists and for the public,” AHCJ president Charles Ornstein, a senior reporter at ProPublica in New York, said in a statement.
Larry Beresford is a freelance writer in San Francisco
References
- Weigel C, Suen W, Gupta G. Using Lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013 Feb 4 [Epub ahead of print].
- Morganti KG, Lovejoy S, Beckjord EB, Haviland AM, Haas AC, Farley DO. A retrospective evaluation of the Perfecting Patient Care University training program for health care organizations. Am J Med Qual. 2013 Apr 9 [Epub ahead of print].
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators’ Academy: fulfilling an unmet need for faculty development. Am J Med Qual. 2013 Apr 11 [Epub ahead of print].
- Dong XQ, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 Apr 8:1-7. doi: 10.1001/jamainternmed.2013.238 [Epub ahead of print].
- Cisco mConcierge. 90% American workers use their own smartphones for work. Cisco mConcierge website. Available at: http://www.ciscomcon.com/sw/swchannel/registration/internet/registrationcfm?SWAPPID=91&RegPageID=350200&SWTHEMEID=12949. Accessed
The Association of Health Care Journalists, a professional association that includes 1,400 journalists, is tackling some of the barriers consumers and advocates face when trying to access such information as hospital safety records. AHCJ’s www.HospitalInfections.org is a free, searchable news application that went live in March with detailed reports of deficiencies cited in federal inspection visits for acute- and critical-access hospitals nationwide.
Through years of advocacy, AHCJ has filed Freedom of Information Act requests and negotiated with the Centers for Medicare & Medicaid Services (CMS) to get access to hospital safety information in electronic form.
CMS’ Hospital Compare website (www.medicare.gov/hospitalcompare) and the Joint Commission’s Quality Check (www.qualitycheck.org) program both publicly report hospital quality data, but they have significant time lags and data that are difficult for the average consumer to understand, according to AHCJ. The association touts its new site as an “early attempt by an advocacy group to make hospital safety information easier to access and more consumer-driven.”
“Being able to easily review the performance of your local hospital is vital for health-care journalists and for the public,” AHCJ president Charles Ornstein, a senior reporter at ProPublica in New York, said in a statement.
Larry Beresford is a freelance writer in San Francisco
References
- Weigel C, Suen W, Gupta G. Using Lean methodology to teach quality improvement to internal medicine residents at a safety net hospital. Am J Med Qual. 2013 Feb 4 [Epub ahead of print].
- Morganti KG, Lovejoy S, Beckjord EB, Haviland AM, Haas AC, Farley DO. A retrospective evaluation of the Perfecting Patient Care University training program for health care organizations. Am J Med Qual. 2013 Apr 9 [Epub ahead of print].
- Myers JS, Tess A, Glasheen JJ, et al. The Quality and Safety Educators’ Academy: fulfilling an unmet need for faculty development. Am J Med Qual. 2013 Apr 11 [Epub ahead of print].
- Dong XQ, Simon MA. Elder abuse as a risk factor for hospitalization in older persons. JAMA Intern Med. 2013 Apr 8:1-7. doi: 10.1001/jamainternmed.2013.238 [Epub ahead of print].
- Cisco mConcierge. 90% American workers use their own smartphones for work. Cisco mConcierge website. Available at: http://www.ciscomcon.com/sw/swchannel/registration/internet/registrationcfm?SWAPPID=91&RegPageID=350200&SWTHEMEID=12949. Accessed
Letters: Medicare Official Says 'Physician Compare' Website Does Not Provide Performance Data on Individual Doctors
I read the article “Call for Transparency in Health-Care Performance Results to Impact Hospitalists” (January 2013, p. 47) by Shaun Frost, MD, SFHM, president of the Society of Hospital Medicine, with interest. I’d like to clarify a key point about Physician Compare. In the article, the statement that the Physician Compare website (www.medicare.gov/find-a-doctor) provides performance information on individual doctors is inaccurate.
The Affordable Care Act (ACA) states that the Centers for Medicare & Medicaid Services (CMS) must have a plan in place by Jan. 1, 2013, to include quality-of-care information on the site. To meet that requirement, CMS has established a plan that initiates a phased approach to public reporting. The 2012 Physician Fee Schedule (PFS) Final Rule was the first step in that phased approach. This rule established that the first measures to be reported on the site would be group-level measures for data collected no sooner than program year 2012. A second critical step is the 2013 PFS Proposed Rule, which outlines a longer-term public reporting plan. According to this plan, we expect the first set of group-level quality measure data to be included on the site in calendar year 2014. We are targeting publishing individual-level quality measures no sooner than 2015 reflecting data collected in program year 2014, if technically feasible.
As you may be aware, Physician Compare is undergoing a redesign to significantly improve the underlying database and thus the information on Physician Compare, as well as the ease of use and functionality of the site. We’ll be unveiling the redesigned site soon. We welcome your feedback and look forward to maintaining a dialogue with you as Physician Compare continues to evolve.
Rashaan Byers, MPH, social science research analyst, Centers forMedicare & Medicaid Services, Center for Clinical Standards & Quality, Quality Measurement & Health Assessment Group
Dr. Frost responds:
I thank Mr. Byers for his clarification regarding the current content on the CMS Physician Compare website, and agree that at the present time the website does not report individual physician clinical performance data.
Physician Compare, however, does currently report if an individual physician participated in the CMS Physician Quality Reporting System (PQRS) by stating “this professional chose to take part in Medicare’s PQRS, and reported quality information satisfactorily for the year 2010.” For those physicians who did not participate in PQRS, their personal website pages do not make reference to the PQRS program.
As the intent of transparency is to educate consumers to make informed choices about where to seek health care, care providers should know that their participation in PQRS is currently publically reported. It is, therefore, possible that patient decisions about whom to seek care from may be influenced by this.
As acknowledged in my January 2013 column in The Hospitalist, Physician Compare currently reports very little information. We should expect this to change, however, as Medicare moves forward with developing a plan to publically report valid and reliable individual physician performance metrics. CMS’ clarification of the timeline by which we can expect to see more detailed information is thus greatly appreciated.
The take-home message for hospitalists is that public reporting of care provider performance will become increasingly comprehensive and transparent in the future. As pointed out, CMS’ present plan targets the publication of individual, physician-level quality measures as soon as 2015, which will reflect actual performance during program year 2014. The measurement period is thus less than one year away, so it behooves us all to focus ever more intently on delivering high-value healthcare.
Shaun Frost, MD, SFHM, past president, SHM
I read the article “Call for Transparency in Health-Care Performance Results to Impact Hospitalists” (January 2013, p. 47) by Shaun Frost, MD, SFHM, president of the Society of Hospital Medicine, with interest. I’d like to clarify a key point about Physician Compare. In the article, the statement that the Physician Compare website (www.medicare.gov/find-a-doctor) provides performance information on individual doctors is inaccurate.
The Affordable Care Act (ACA) states that the Centers for Medicare & Medicaid Services (CMS) must have a plan in place by Jan. 1, 2013, to include quality-of-care information on the site. To meet that requirement, CMS has established a plan that initiates a phased approach to public reporting. The 2012 Physician Fee Schedule (PFS) Final Rule was the first step in that phased approach. This rule established that the first measures to be reported on the site would be group-level measures for data collected no sooner than program year 2012. A second critical step is the 2013 PFS Proposed Rule, which outlines a longer-term public reporting plan. According to this plan, we expect the first set of group-level quality measure data to be included on the site in calendar year 2014. We are targeting publishing individual-level quality measures no sooner than 2015 reflecting data collected in program year 2014, if technically feasible.
As you may be aware, Physician Compare is undergoing a redesign to significantly improve the underlying database and thus the information on Physician Compare, as well as the ease of use and functionality of the site. We’ll be unveiling the redesigned site soon. We welcome your feedback and look forward to maintaining a dialogue with you as Physician Compare continues to evolve.
Rashaan Byers, MPH, social science research analyst, Centers forMedicare & Medicaid Services, Center for Clinical Standards & Quality, Quality Measurement & Health Assessment Group
Dr. Frost responds:
I thank Mr. Byers for his clarification regarding the current content on the CMS Physician Compare website, and agree that at the present time the website does not report individual physician clinical performance data.
Physician Compare, however, does currently report if an individual physician participated in the CMS Physician Quality Reporting System (PQRS) by stating “this professional chose to take part in Medicare’s PQRS, and reported quality information satisfactorily for the year 2010.” For those physicians who did not participate in PQRS, their personal website pages do not make reference to the PQRS program.
As the intent of transparency is to educate consumers to make informed choices about where to seek health care, care providers should know that their participation in PQRS is currently publically reported. It is, therefore, possible that patient decisions about whom to seek care from may be influenced by this.
As acknowledged in my January 2013 column in The Hospitalist, Physician Compare currently reports very little information. We should expect this to change, however, as Medicare moves forward with developing a plan to publically report valid and reliable individual physician performance metrics. CMS’ clarification of the timeline by which we can expect to see more detailed information is thus greatly appreciated.
The take-home message for hospitalists is that public reporting of care provider performance will become increasingly comprehensive and transparent in the future. As pointed out, CMS’ present plan targets the publication of individual, physician-level quality measures as soon as 2015, which will reflect actual performance during program year 2014. The measurement period is thus less than one year away, so it behooves us all to focus ever more intently on delivering high-value healthcare.
Shaun Frost, MD, SFHM, past president, SHM
I read the article “Call for Transparency in Health-Care Performance Results to Impact Hospitalists” (January 2013, p. 47) by Shaun Frost, MD, SFHM, president of the Society of Hospital Medicine, with interest. I’d like to clarify a key point about Physician Compare. In the article, the statement that the Physician Compare website (www.medicare.gov/find-a-doctor) provides performance information on individual doctors is inaccurate.
The Affordable Care Act (ACA) states that the Centers for Medicare & Medicaid Services (CMS) must have a plan in place by Jan. 1, 2013, to include quality-of-care information on the site. To meet that requirement, CMS has established a plan that initiates a phased approach to public reporting. The 2012 Physician Fee Schedule (PFS) Final Rule was the first step in that phased approach. This rule established that the first measures to be reported on the site would be group-level measures for data collected no sooner than program year 2012. A second critical step is the 2013 PFS Proposed Rule, which outlines a longer-term public reporting plan. According to this plan, we expect the first set of group-level quality measure data to be included on the site in calendar year 2014. We are targeting publishing individual-level quality measures no sooner than 2015 reflecting data collected in program year 2014, if technically feasible.
As you may be aware, Physician Compare is undergoing a redesign to significantly improve the underlying database and thus the information on Physician Compare, as well as the ease of use and functionality of the site. We’ll be unveiling the redesigned site soon. We welcome your feedback and look forward to maintaining a dialogue with you as Physician Compare continues to evolve.
Rashaan Byers, MPH, social science research analyst, Centers forMedicare & Medicaid Services, Center for Clinical Standards & Quality, Quality Measurement & Health Assessment Group
Dr. Frost responds:
I thank Mr. Byers for his clarification regarding the current content on the CMS Physician Compare website, and agree that at the present time the website does not report individual physician clinical performance data.
Physician Compare, however, does currently report if an individual physician participated in the CMS Physician Quality Reporting System (PQRS) by stating “this professional chose to take part in Medicare’s PQRS, and reported quality information satisfactorily for the year 2010.” For those physicians who did not participate in PQRS, their personal website pages do not make reference to the PQRS program.
As the intent of transparency is to educate consumers to make informed choices about where to seek health care, care providers should know that their participation in PQRS is currently publically reported. It is, therefore, possible that patient decisions about whom to seek care from may be influenced by this.
As acknowledged in my January 2013 column in The Hospitalist, Physician Compare currently reports very little information. We should expect this to change, however, as Medicare moves forward with developing a plan to publically report valid and reliable individual physician performance metrics. CMS’ clarification of the timeline by which we can expect to see more detailed information is thus greatly appreciated.
The take-home message for hospitalists is that public reporting of care provider performance will become increasingly comprehensive and transparent in the future. As pointed out, CMS’ present plan targets the publication of individual, physician-level quality measures as soon as 2015, which will reflect actual performance during program year 2014. The measurement period is thus less than one year away, so it behooves us all to focus ever more intently on delivering high-value healthcare.
Shaun Frost, MD, SFHM, past president, SHM
Documentation, CMS-Approved Language Key to Getting Paid for Hospitalist Teaching Services
When hospitalists work in academic centers, medical and surgical services are furnished, in part, by a resident within the scope of the hospitalists’ training program. A resident is “an individual who participates in an approved graduate medical education (GME) program or a physician who is not in an approved GME program but who is authorized to practice only in a hospital setting.”1 Resident services are covered by Centers for Medicare & Medicaid Services (CMS) and paid by the Fiscal Intermediary through direct GME and Indirect Medical Education (IME) payments. These services are not billed or paid using the Medicare Physician Fee Schedule. The teaching physician is responsible for supervising the resident’s health-care delivery but is not paid for the resident’s work. The teaching physician is paid for their personal and medically necessary service in providing patient care. The teaching physician has the option to perform the entire service, or perform the self-determined critical or key portion(s) of the service.
Comprehensive Service
Teaching physicians independently see the patient and perform all required elements to support the visit level (e.g. 99233: subsequent hospital care, per day, which requires at least two of the following three key components: a detailed interval history, a detailed examination, or high-complexity medical decision-making).2 The teaching physician writes a note independent of a resident encounter with the patient or documentation. The teaching physician note “stands alone” and does not rely on the resident’s documentation. If the resident saw the patient and documented the encounter, the teaching physician might choose to “link to” the resident note in lieu of personally documenting the entire service. The linking statement must demonstrate teaching physician involvement in the patient encounter and participation in patient management. Use of CMS-approved statements is best to meet these requirements. Statement examples include:3
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note, except the heart murmur is louder, so I will obtain an echo to evaluate.”
Each of these statements meets the minimum requirements for billing. However, teaching physicians should offer more information in support of other clinical, quality, and regulatory initiatives and mandates, better exemplified in the last example. The reported visit level will be supported by the combined documentation (teaching physician and resident).
The teaching physician submits a claim in their name and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99223-GC). This alerts the Medicare contractor that services were provided under teaching physician rules. Requests for documentation should include a response with medical record entries from the teaching physician and resident.
Critical/Key Portion
“Supervised” service: The resident and teaching physician can round together; they can see the patient at the same time. The teaching physician observes the resident’s performance during the patient encounter, or personally performs self-determined elements of patient care. The resident documents their patient care. The attending must still note their presence in the medical record, performance of the critical or key portions of the service, and involvement in patient management. CMS-accepted statements include:3
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
Although these statements demonstrate acceptable billing language, they lack patient-specific details that support the teaching physician’s personal contribution to patient care and the quality of their expertise. The teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99232-GC).
“Shared” service: The resident sees the patient unaccompanied and documents the corresponding care provided. The teaching physician sees the patient at a different time but performs only the critical or key portions of the service. The case is subsequently discussed with the resident. The teaching physician must document their presence and performance of the critical or key portions of the service, along with any patient management. Using CMS-quoted statements ensures regulatory compliance:3
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that the picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note, but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Once again, the teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99233-GC).
EHR Considerations
When seeing patients independent of one another, the timing of the teaching physician and resident encounters does not impact billing. However, the time that the resident encounter is documented in the medical record can significantly impact the payment when reviewed by external auditors. When the resident note is dated and timed later than the teaching physician’s entry, the teaching physician cannot consider the resident’s note for visit-level selection. The teaching physician should not “link to” a resident note that is viewed as “not having been written” prior to the teaching physician note. This would not fulfill the requirements represented in the CMS-approved language “I reviewed the resident’s note and agree.”
Electronic health record (EHR) systems sometimes hinder compliance. If the resident completes the note but does not “finalize” or “close” the encounter until after the teaching physician documents their own note, it can falsely appear that the resident note did not exist at the time the teaching physician created their entry. Because an auditor can only view the finalized entries, the timing of each entry might be erroneously represented. Proper training and closing of encounters can diminish these issues.
Additionally, scribing the attestation is not permitted. Residents cannot document the teaching physician attestation on behalf of the physician under any circumstance. CMS rules require the teaching physician to document their presence, participation, and management of the patient. In an EHR, the teaching physician must document this entry under his/her own log-in and password, which is not to be shared with anyone.
Students
CMS defines student as “an individual who participates in an accredited educational program [e.g. a medical school] that is not an approved GME program.”1 A student is not regarded as a “physician in training,” and the service is not eligible for reimbursement consideration under the teaching physician rules.
Per CMS guidelines, students can document services in the medical record, but the teaching physician may only refer to the student’s systems review and past/family/social history entries. The teaching physician must verify and redocument the history of present illness. A student’s physical exam findings or medical decision-making are not suitable for tethering, and the teaching physician must personally perform and redocument the physical exam and medical decision-making. The visit level reflects only the teaching physician’s personally performed and documented service.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Guidelines for Teaching Physicians, Interns, Residents. CMS website. Available at: http://www.cms.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf. Accessed Jan. 8, 2013.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 100. CMS website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2013.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 30.2. CMS website. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed Jan. 8, 2013.
When hospitalists work in academic centers, medical and surgical services are furnished, in part, by a resident within the scope of the hospitalists’ training program. A resident is “an individual who participates in an approved graduate medical education (GME) program or a physician who is not in an approved GME program but who is authorized to practice only in a hospital setting.”1 Resident services are covered by Centers for Medicare & Medicaid Services (CMS) and paid by the Fiscal Intermediary through direct GME and Indirect Medical Education (IME) payments. These services are not billed or paid using the Medicare Physician Fee Schedule. The teaching physician is responsible for supervising the resident’s health-care delivery but is not paid for the resident’s work. The teaching physician is paid for their personal and medically necessary service in providing patient care. The teaching physician has the option to perform the entire service, or perform the self-determined critical or key portion(s) of the service.
Comprehensive Service
Teaching physicians independently see the patient and perform all required elements to support the visit level (e.g. 99233: subsequent hospital care, per day, which requires at least two of the following three key components: a detailed interval history, a detailed examination, or high-complexity medical decision-making).2 The teaching physician writes a note independent of a resident encounter with the patient or documentation. The teaching physician note “stands alone” and does not rely on the resident’s documentation. If the resident saw the patient and documented the encounter, the teaching physician might choose to “link to” the resident note in lieu of personally documenting the entire service. The linking statement must demonstrate teaching physician involvement in the patient encounter and participation in patient management. Use of CMS-approved statements is best to meet these requirements. Statement examples include:3
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note, except the heart murmur is louder, so I will obtain an echo to evaluate.”
Each of these statements meets the minimum requirements for billing. However, teaching physicians should offer more information in support of other clinical, quality, and regulatory initiatives and mandates, better exemplified in the last example. The reported visit level will be supported by the combined documentation (teaching physician and resident).
The teaching physician submits a claim in their name and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99223-GC). This alerts the Medicare contractor that services were provided under teaching physician rules. Requests for documentation should include a response with medical record entries from the teaching physician and resident.
Critical/Key Portion
“Supervised” service: The resident and teaching physician can round together; they can see the patient at the same time. The teaching physician observes the resident’s performance during the patient encounter, or personally performs self-determined elements of patient care. The resident documents their patient care. The attending must still note their presence in the medical record, performance of the critical or key portions of the service, and involvement in patient management. CMS-accepted statements include:3
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
Although these statements demonstrate acceptable billing language, they lack patient-specific details that support the teaching physician’s personal contribution to patient care and the quality of their expertise. The teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99232-GC).
“Shared” service: The resident sees the patient unaccompanied and documents the corresponding care provided. The teaching physician sees the patient at a different time but performs only the critical or key portions of the service. The case is subsequently discussed with the resident. The teaching physician must document their presence and performance of the critical or key portions of the service, along with any patient management. Using CMS-quoted statements ensures regulatory compliance:3
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that the picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note, but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Once again, the teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99233-GC).
EHR Considerations
When seeing patients independent of one another, the timing of the teaching physician and resident encounters does not impact billing. However, the time that the resident encounter is documented in the medical record can significantly impact the payment when reviewed by external auditors. When the resident note is dated and timed later than the teaching physician’s entry, the teaching physician cannot consider the resident’s note for visit-level selection. The teaching physician should not “link to” a resident note that is viewed as “not having been written” prior to the teaching physician note. This would not fulfill the requirements represented in the CMS-approved language “I reviewed the resident’s note and agree.”
Electronic health record (EHR) systems sometimes hinder compliance. If the resident completes the note but does not “finalize” or “close” the encounter until after the teaching physician documents their own note, it can falsely appear that the resident note did not exist at the time the teaching physician created their entry. Because an auditor can only view the finalized entries, the timing of each entry might be erroneously represented. Proper training and closing of encounters can diminish these issues.
Additionally, scribing the attestation is not permitted. Residents cannot document the teaching physician attestation on behalf of the physician under any circumstance. CMS rules require the teaching physician to document their presence, participation, and management of the patient. In an EHR, the teaching physician must document this entry under his/her own log-in and password, which is not to be shared with anyone.
Students
CMS defines student as “an individual who participates in an accredited educational program [e.g. a medical school] that is not an approved GME program.”1 A student is not regarded as a “physician in training,” and the service is not eligible for reimbursement consideration under the teaching physician rules.
Per CMS guidelines, students can document services in the medical record, but the teaching physician may only refer to the student’s systems review and past/family/social history entries. The teaching physician must verify and redocument the history of present illness. A student’s physical exam findings or medical decision-making are not suitable for tethering, and the teaching physician must personally perform and redocument the physical exam and medical decision-making. The visit level reflects only the teaching physician’s personally performed and documented service.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Guidelines for Teaching Physicians, Interns, Residents. CMS website. Available at: http://www.cms.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf. Accessed Jan. 8, 2013.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 100. CMS website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2013.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 30.2. CMS website. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed Jan. 8, 2013.
When hospitalists work in academic centers, medical and surgical services are furnished, in part, by a resident within the scope of the hospitalists’ training program. A resident is “an individual who participates in an approved graduate medical education (GME) program or a physician who is not in an approved GME program but who is authorized to practice only in a hospital setting.”1 Resident services are covered by Centers for Medicare & Medicaid Services (CMS) and paid by the Fiscal Intermediary through direct GME and Indirect Medical Education (IME) payments. These services are not billed or paid using the Medicare Physician Fee Schedule. The teaching physician is responsible for supervising the resident’s health-care delivery but is not paid for the resident’s work. The teaching physician is paid for their personal and medically necessary service in providing patient care. The teaching physician has the option to perform the entire service, or perform the self-determined critical or key portion(s) of the service.
Comprehensive Service
Teaching physicians independently see the patient and perform all required elements to support the visit level (e.g. 99233: subsequent hospital care, per day, which requires at least two of the following three key components: a detailed interval history, a detailed examination, or high-complexity medical decision-making).2 The teaching physician writes a note independent of a resident encounter with the patient or documentation. The teaching physician note “stands alone” and does not rely on the resident’s documentation. If the resident saw the patient and documented the encounter, the teaching physician might choose to “link to” the resident note in lieu of personally documenting the entire service. The linking statement must demonstrate teaching physician involvement in the patient encounter and participation in patient management. Use of CMS-approved statements is best to meet these requirements. Statement examples include:3
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note, except the heart murmur is louder, so I will obtain an echo to evaluate.”
Each of these statements meets the minimum requirements for billing. However, teaching physicians should offer more information in support of other clinical, quality, and regulatory initiatives and mandates, better exemplified in the last example. The reported visit level will be supported by the combined documentation (teaching physician and resident).
The teaching physician submits a claim in their name and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99223-GC). This alerts the Medicare contractor that services were provided under teaching physician rules. Requests for documentation should include a response with medical record entries from the teaching physician and resident.
Critical/Key Portion
“Supervised” service: The resident and teaching physician can round together; they can see the patient at the same time. The teaching physician observes the resident’s performance during the patient encounter, or personally performs self-determined elements of patient care. The resident documents their patient care. The attending must still note their presence in the medical record, performance of the critical or key portions of the service, and involvement in patient management. CMS-accepted statements include:3
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
Although these statements demonstrate acceptable billing language, they lack patient-specific details that support the teaching physician’s personal contribution to patient care and the quality of their expertise. The teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99232-GC).
“Shared” service: The resident sees the patient unaccompanied and documents the corresponding care provided. The teaching physician sees the patient at a different time but performs only the critical or key portions of the service. The case is subsequently discussed with the resident. The teaching physician must document their presence and performance of the critical or key portions of the service, along with any patient management. Using CMS-quoted statements ensures regulatory compliance:3
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that the picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note, but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Once again, the teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99233-GC).
EHR Considerations
When seeing patients independent of one another, the timing of the teaching physician and resident encounters does not impact billing. However, the time that the resident encounter is documented in the medical record can significantly impact the payment when reviewed by external auditors. When the resident note is dated and timed later than the teaching physician’s entry, the teaching physician cannot consider the resident’s note for visit-level selection. The teaching physician should not “link to” a resident note that is viewed as “not having been written” prior to the teaching physician note. This would not fulfill the requirements represented in the CMS-approved language “I reviewed the resident’s note and agree.”
Electronic health record (EHR) systems sometimes hinder compliance. If the resident completes the note but does not “finalize” or “close” the encounter until after the teaching physician documents their own note, it can falsely appear that the resident note did not exist at the time the teaching physician created their entry. Because an auditor can only view the finalized entries, the timing of each entry might be erroneously represented. Proper training and closing of encounters can diminish these issues.
Additionally, scribing the attestation is not permitted. Residents cannot document the teaching physician attestation on behalf of the physician under any circumstance. CMS rules require the teaching physician to document their presence, participation, and management of the patient. In an EHR, the teaching physician must document this entry under his/her own log-in and password, which is not to be shared with anyone.
Students
CMS defines student as “an individual who participates in an accredited educational program [e.g. a medical school] that is not an approved GME program.”1 A student is not regarded as a “physician in training,” and the service is not eligible for reimbursement consideration under the teaching physician rules.
Per CMS guidelines, students can document services in the medical record, but the teaching physician may only refer to the student’s systems review and past/family/social history entries. The teaching physician must verify and redocument the history of present illness. A student’s physical exam findings or medical decision-making are not suitable for tethering, and the teaching physician must personally perform and redocument the physical exam and medical decision-making. The visit level reflects only the teaching physician’s personally performed and documented service.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Guidelines for Teaching Physicians, Interns, Residents. CMS website. Available at: http://www.cms.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf. Accessed Jan. 8, 2013.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 100. CMS website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2013.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 30.2. CMS website. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed Jan. 8, 2013.
Telehealth Technology Connects Specialists with First Responders in the Field
The VA Ann Arbor Healthcare System in Michigan is mobilizing telehealth technology for a disaster-relief initiative that aims to connect first responders in the field with medical specialists at the Ann Arbor Medical Center. As reported in Healthcare IT News, the Disaster Relief Telehealth System of Orion, Mich.-based JEMS Technology (www.jemstech.com) enables secure, live-streaming video to be sent to specialists, who can review the video and respond with medical advice.5
The Office of Emergency Management at the Ann Arbor VA supports emergency operations from four treatment sites serving 21 counties in Michigan and Ohio, as well as regional disaster preparedness.
In other technology news, the U.S. Army in March awarded a $2.5 million contract to brain-monitoring-device company NeuroWave Systems of Cleveland Heights, Ohio (www.neurowavesystems.com), to develop a wearable, miniaturized brain monitor to assess via electroencephalogram data for traumatic brain injury (TBI) in the field, directly at the point of suspected injury, such as on battlefronts. The device, called SeizTBI, is “small, lightweight, and designed for rapid deployment in austere environments,” explains NeuroWave principal investigator Stephan Bibian, MD. TBI accounted for 22% of U.S. troop casualties in the Iraq and Afghanistan conflicts, but fewer than half were identified in the field.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
The VA Ann Arbor Healthcare System in Michigan is mobilizing telehealth technology for a disaster-relief initiative that aims to connect first responders in the field with medical specialists at the Ann Arbor Medical Center. As reported in Healthcare IT News, the Disaster Relief Telehealth System of Orion, Mich.-based JEMS Technology (www.jemstech.com) enables secure, live-streaming video to be sent to specialists, who can review the video and respond with medical advice.5
The Office of Emergency Management at the Ann Arbor VA supports emergency operations from four treatment sites serving 21 counties in Michigan and Ohio, as well as regional disaster preparedness.
In other technology news, the U.S. Army in March awarded a $2.5 million contract to brain-monitoring-device company NeuroWave Systems of Cleveland Heights, Ohio (www.neurowavesystems.com), to develop a wearable, miniaturized brain monitor to assess via electroencephalogram data for traumatic brain injury (TBI) in the field, directly at the point of suspected injury, such as on battlefronts. The device, called SeizTBI, is “small, lightweight, and designed for rapid deployment in austere environments,” explains NeuroWave principal investigator Stephan Bibian, MD. TBI accounted for 22% of U.S. troop casualties in the Iraq and Afghanistan conflicts, but fewer than half were identified in the field.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
The VA Ann Arbor Healthcare System in Michigan is mobilizing telehealth technology for a disaster-relief initiative that aims to connect first responders in the field with medical specialists at the Ann Arbor Medical Center. As reported in Healthcare IT News, the Disaster Relief Telehealth System of Orion, Mich.-based JEMS Technology (www.jemstech.com) enables secure, live-streaming video to be sent to specialists, who can review the video and respond with medical advice.5
The Office of Emergency Management at the Ann Arbor VA supports emergency operations from four treatment sites serving 21 counties in Michigan and Ohio, as well as regional disaster preparedness.
In other technology news, the U.S. Army in March awarded a $2.5 million contract to brain-monitoring-device company NeuroWave Systems of Cleveland Heights, Ohio (www.neurowavesystems.com), to develop a wearable, miniaturized brain monitor to assess via electroencephalogram data for traumatic brain injury (TBI) in the field, directly at the point of suspected injury, such as on battlefronts. The device, called SeizTBI, is “small, lightweight, and designed for rapid deployment in austere environments,” explains NeuroWave principal investigator Stephan Bibian, MD. TBI accounted for 22% of U.S. troop casualties in the Iraq and Afghanistan conflicts, but fewer than half were identified in the field.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
AMA Report Offers Nine Steps to Help PCPs Prevent Readmissions
The American Medical Association recently released a report developed by a 21-member expert panel proposing a nine-step plan for primary-care-physician (PCP) practices to play an integral role in improving care transitions and preventing avoidable rehospitalizations.2 The report recommends focusing on more than just the hospital-admitting diagnosis, conducting a thorough patient health assessment, clarifying the patient’s short- and long-term goals, and coordinating care with other care settings.
With simultaneous research in JAMA concluding that the vast majority of readmissions are for reasons unrelated to the previous hospital stay, coordination between the inpatient and outpatient teams is crucial to successful transitions of care.3 Moreover, a recent survey showed that nearly 30% of PCPs say they miss alerts about patients’ test results from an electronic health record (EHR) notification system.4 According to the survey by Hardeep Singh, MD, MPH, and colleagues from the Michael E. DeBakey VA Medical Center in Houston, the doctors received on average 63 such alerts per day. Seventy percent reported that they cannot effectively manage the alerts, and more than half said that the current EHR notification system makes it possible to miss test results.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
The American Medical Association recently released a report developed by a 21-member expert panel proposing a nine-step plan for primary-care-physician (PCP) practices to play an integral role in improving care transitions and preventing avoidable rehospitalizations.2 The report recommends focusing on more than just the hospital-admitting diagnosis, conducting a thorough patient health assessment, clarifying the patient’s short- and long-term goals, and coordinating care with other care settings.
With simultaneous research in JAMA concluding that the vast majority of readmissions are for reasons unrelated to the previous hospital stay, coordination between the inpatient and outpatient teams is crucial to successful transitions of care.3 Moreover, a recent survey showed that nearly 30% of PCPs say they miss alerts about patients’ test results from an electronic health record (EHR) notification system.4 According to the survey by Hardeep Singh, MD, MPH, and colleagues from the Michael E. DeBakey VA Medical Center in Houston, the doctors received on average 63 such alerts per day. Seventy percent reported that they cannot effectively manage the alerts, and more than half said that the current EHR notification system makes it possible to miss test results.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
The American Medical Association recently released a report developed by a 21-member expert panel proposing a nine-step plan for primary-care-physician (PCP) practices to play an integral role in improving care transitions and preventing avoidable rehospitalizations.2 The report recommends focusing on more than just the hospital-admitting diagnosis, conducting a thorough patient health assessment, clarifying the patient’s short- and long-term goals, and coordinating care with other care settings.
With simultaneous research in JAMA concluding that the vast majority of readmissions are for reasons unrelated to the previous hospital stay, coordination between the inpatient and outpatient teams is crucial to successful transitions of care.3 Moreover, a recent survey showed that nearly 30% of PCPs say they miss alerts about patients’ test results from an electronic health record (EHR) notification system.4 According to the survey by Hardeep Singh, MD, MPH, and colleagues from the Michael E. DeBakey VA Medical Center in Houston, the doctors received on average 63 such alerts per day. Seventy percent reported that they cannot effectively manage the alerts, and more than half said that the current EHR notification system makes it possible to miss test results.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.