User login
Low-calorie tastes sweeter with a little salt
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
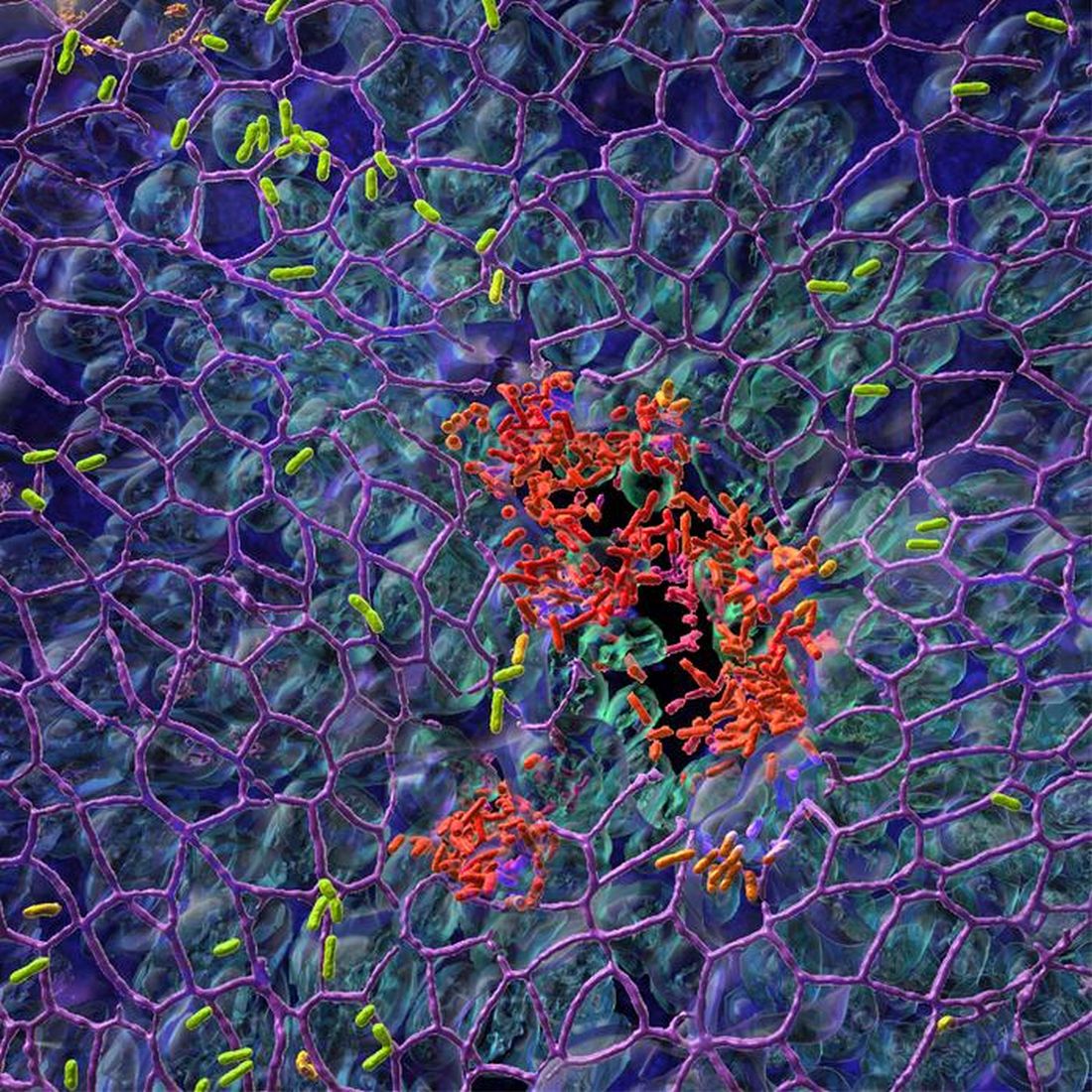
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Cases of potentially deadly fungus jump 200%: CDC
prompting the Centers for Disease Control and Prevention to issue a warning to health care facilities about the rising threat.
C. auris is a yeast that spreads easily from touching it on a surface like a countertop. It can also spread from person to person. It isn’t a threat to healthy people, but people in hospitals and nursing homes are at a heightened risk because they might have weakened immune systems or be using invasive medical devices that can introduce the fungus inside their bodies. When C. auris progresses to causing an infection that reaches the brain, blood, or lungs, more than one in three people die.
The worrying increase was detailed in the journal Annals of Internal Medicine. In 2021, cases reached a count of 3,270 with an active infection, and 7,413 cases showed the fungus was present but hadn’t caused an infection. Infection counts were up 95% over the previous year, and the fungus showed up on screenings three times as often. The number of cases resistant to medication also tripled.
The CDC called the figures “alarming,” noting that the fungus was only detected in the United States in 2016.
“The timing of this increase and findings from public health investigations suggest C. auris spread may have worsened due to strain on health care and public health systems during the COVID-19 pandemic,” the CDC explained in a news release.
Another potential reason for the jump could be that screening for C. auris has simply increased and it’s being found more often because it’s being looked for more often. But researchers believe that, even with the increase in testing, the reported counts are underestimated. That’s because even though screening has increased, health care providers still aren’t looking for the presence of the fungus as often as the CDC would like.
“The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control,” said study author Meghan Lyman, MD, a CDC epidemiologist in Atlanta, in a statement.
Cases of C. auris continued to rise in 2022, the CDC said. A map on the agency’s website of reported cases from 2022 shows it was found in more than half of U.S. states, with the highest counts occurring in California, Florida, Illinois, Nevada, New York, and Texas. The fungus is a problem worldwide and is listed among the most threatening treatment-resistant fungi by the World Health Organization.
The study authors concluded that screening capacity for the fungus needs to be expanded nationwide so that when C. auris is detected, measures can be taken to prevent its spread.
A version of this article originally appeared on WebMD.com.
prompting the Centers for Disease Control and Prevention to issue a warning to health care facilities about the rising threat.
C. auris is a yeast that spreads easily from touching it on a surface like a countertop. It can also spread from person to person. It isn’t a threat to healthy people, but people in hospitals and nursing homes are at a heightened risk because they might have weakened immune systems or be using invasive medical devices that can introduce the fungus inside their bodies. When C. auris progresses to causing an infection that reaches the brain, blood, or lungs, more than one in three people die.
The worrying increase was detailed in the journal Annals of Internal Medicine. In 2021, cases reached a count of 3,270 with an active infection, and 7,413 cases showed the fungus was present but hadn’t caused an infection. Infection counts were up 95% over the previous year, and the fungus showed up on screenings three times as often. The number of cases resistant to medication also tripled.
The CDC called the figures “alarming,” noting that the fungus was only detected in the United States in 2016.
“The timing of this increase and findings from public health investigations suggest C. auris spread may have worsened due to strain on health care and public health systems during the COVID-19 pandemic,” the CDC explained in a news release.
Another potential reason for the jump could be that screening for C. auris has simply increased and it’s being found more often because it’s being looked for more often. But researchers believe that, even with the increase in testing, the reported counts are underestimated. That’s because even though screening has increased, health care providers still aren’t looking for the presence of the fungus as often as the CDC would like.
“The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control,” said study author Meghan Lyman, MD, a CDC epidemiologist in Atlanta, in a statement.
Cases of C. auris continued to rise in 2022, the CDC said. A map on the agency’s website of reported cases from 2022 shows it was found in more than half of U.S. states, with the highest counts occurring in California, Florida, Illinois, Nevada, New York, and Texas. The fungus is a problem worldwide and is listed among the most threatening treatment-resistant fungi by the World Health Organization.
The study authors concluded that screening capacity for the fungus needs to be expanded nationwide so that when C. auris is detected, measures can be taken to prevent its spread.
A version of this article originally appeared on WebMD.com.
prompting the Centers for Disease Control and Prevention to issue a warning to health care facilities about the rising threat.
C. auris is a yeast that spreads easily from touching it on a surface like a countertop. It can also spread from person to person. It isn’t a threat to healthy people, but people in hospitals and nursing homes are at a heightened risk because they might have weakened immune systems or be using invasive medical devices that can introduce the fungus inside their bodies. When C. auris progresses to causing an infection that reaches the brain, blood, or lungs, more than one in three people die.
The worrying increase was detailed in the journal Annals of Internal Medicine. In 2021, cases reached a count of 3,270 with an active infection, and 7,413 cases showed the fungus was present but hadn’t caused an infection. Infection counts were up 95% over the previous year, and the fungus showed up on screenings three times as often. The number of cases resistant to medication also tripled.
The CDC called the figures “alarming,” noting that the fungus was only detected in the United States in 2016.
“The timing of this increase and findings from public health investigations suggest C. auris spread may have worsened due to strain on health care and public health systems during the COVID-19 pandemic,” the CDC explained in a news release.
Another potential reason for the jump could be that screening for C. auris has simply increased and it’s being found more often because it’s being looked for more often. But researchers believe that, even with the increase in testing, the reported counts are underestimated. That’s because even though screening has increased, health care providers still aren’t looking for the presence of the fungus as often as the CDC would like.
“The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control,” said study author Meghan Lyman, MD, a CDC epidemiologist in Atlanta, in a statement.
Cases of C. auris continued to rise in 2022, the CDC said. A map on the agency’s website of reported cases from 2022 shows it was found in more than half of U.S. states, with the highest counts occurring in California, Florida, Illinois, Nevada, New York, and Texas. The fungus is a problem worldwide and is listed among the most threatening treatment-resistant fungi by the World Health Organization.
The study authors concluded that screening capacity for the fungus needs to be expanded nationwide so that when C. auris is detected, measures can be taken to prevent its spread.
A version of this article originally appeared on WebMD.com.
Droplet dispersal in sterile processing units far exceeds guideline limit
In the era of Ebola, COVID-19, and even Legionnaires, technicians and other staff working behind the scenes to ensure provider and patient safety continue to face a long-recognized but under addressed challenge: splashes and airborne droplets.
Granted, National Institute for Occupational Safety and Health (NIOSH) standards, industry standards, and professional guidelines are all in place to prevent unintentional exposure to pathogens. However, findings from a newly published study in the American Journal of Infection Control suggest they fall short.
In the study, researchers found that simulated manual cleaning of medical devices generated a drenching splash throughout the process with droplet dispersal exceeding 7 feet (2.1 meters).
Cori L. Ofstead, MSPH, lead author and president/CEO of Ofstead & Associates, Bloomington, Minn., told this news organization. “That’s the problem with having standards and guidelines that are not based on relevant evidence, [which] in this case, is a single study that was done in an intensive care area where they had an infection outbreak.”
Ms. Ofstead was referring to a report in the journal Infection Control and Hospital Epidemiology, detailing a Canadian investigation involving a multidrug-resistant Pseudomonas aeruginosa outbreak in an ICU. The report implicated the faucets over the hand hygiene sinks, with fluorescent dye showing droplet dispersal roughly 3 feet away from the sinks.
“Somehow it [the 3-feet rule] got implemented in guidelines in sterile processing decontamination areas, which are not the same as hand hygiene,’’ Ms. Ofstead explained.
With a goal of providing more current evidence on droplet generation and dispersal, as well as personal protection equipment (PPE) exposure/effectiveness, she and her colleagues simulated manual cleaning of a decommissioned colonoscope and transvaginal ultrasound probe, using for the study location a new academic sterile processing unit.
To detect droplet generation and dispersal as well as splash following common technician activities (for example, colonoscope brushing, scrubbing, rinsing and transport to an automated endoscope reprocessor [AER] for sterilization), the researchers affixed blue moisture-detection paper to environmental surfaces, on carts positioned 4 feet (1.2 meters) from the sink (to simulate observers), and along a 15-foot pathway between the sink and AER.
They observed droplets everywhere.
Technician activities such as running the faucet and rinsing the probe under running water generated substantial splashing overall. Instrument rinsing in particular produced small and large droplets and confluent puddles of water around the sink and in the broad area surrounding the workspace. Droplets were also dispersed on the floor 7.25 feet (2.2 meters) away and along the entire 15-foot path from the sink to the AER.
At the sink, the technician risked drenching exposure from head to toe during most activities, and even observers positioned 3-4 feet away were found to have droplets on their gowns. In addition, saturated shoe covers reportedly tracked moisture away from the sink to the unit door – a distance of 13 feet (4 meters) – and 2 feet (0.6 meters) farther out into the PPE foyer for donning and doffing.
Although PPE gowns effectively repelled moisture during cleaning of a single device, Ms. Ofstead emphasized that technicians typically handle up to 10 instruments during a normal, 2-hour shift, further increasing exposure risk with each subsequent cleaning.
However, perhaps one of the most surprising findings was that despite an optimal unit design, including physical separation of clean and dirty activities and pressurized air flow to protect workers, droplets were still broadly dispersed.
Current efforts, however well-intentioned, might not be offering the degree of protection (and consideration) that sterile processing technicians need.
“The study was conducted in a new sterile processing area that had an extra excellent kind of distancing and three separate rooms, something that I think most of our hospitals are working toward,” Stella Hines, MD, associate professor at the University of Maryland School of Medicine, Baltimore, explained. Dr. Hines was not directly involved in the study.
“But it also really kind of highlighted what’s happening to workers potentially,” she added. “For example, we want to know if that spray or splatter has a live microbe it in that could cause a problem or ... in a highly wet environment, if that water has some kind of chemical in it that could pose an occupational hazard to the worker based on skin or mucous membrane exposure.”
Ms. Ofstead agreed. “We need to be thinking about the exposure of critically important workers and the environment in an era where we are worried about aerosol-generating procedures and superbugs,” she explained.
Dr. Hines and Ms. Ofstead also noted that the majority of staff involved in front-line patient care have never actually ventured into the sterile processing units nor do they recognize the risks that technicians working in these units face on a daily, or even hourly, basis.
“The people who run these operations are very well trained and knowledgeable. I think that it would be helpful for them to know that they’re appreciated and for the people upstairs on the front lines using the equipment to see what goes on downstairs and all of the painstaking steps that need to be in place for the equipment to come out of sterile processing and be ready to go,” said Dr. Hines.
In the meantime, hospital leaders need to address the challenges and danger posed by migrating infectious droplets, especially for workers involved in processes that stir them up in the first place – workers who by the end of their shifts are unavoidably drenched with infectious blood and tissue secretions.
“I think that it’s going to take a much bigger kind of worldview from hospital leadership,” Dr. Hines said.
The study was supported in part by a grant from Healthmark Industries. Ms. Ofstead reports research grants or consulting fees through her organization with 3M Company, Ambu, Boston Scientific, Cleanis, Fortive/Advanced Sterilization Products, Healthmark Industries, Pentax, and Steris/Cantel/Medviators. Dr. Hines reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In the era of Ebola, COVID-19, and even Legionnaires, technicians and other staff working behind the scenes to ensure provider and patient safety continue to face a long-recognized but under addressed challenge: splashes and airborne droplets.
Granted, National Institute for Occupational Safety and Health (NIOSH) standards, industry standards, and professional guidelines are all in place to prevent unintentional exposure to pathogens. However, findings from a newly published study in the American Journal of Infection Control suggest they fall short.
In the study, researchers found that simulated manual cleaning of medical devices generated a drenching splash throughout the process with droplet dispersal exceeding 7 feet (2.1 meters).
Cori L. Ofstead, MSPH, lead author and president/CEO of Ofstead & Associates, Bloomington, Minn., told this news organization. “That’s the problem with having standards and guidelines that are not based on relevant evidence, [which] in this case, is a single study that was done in an intensive care area where they had an infection outbreak.”
Ms. Ofstead was referring to a report in the journal Infection Control and Hospital Epidemiology, detailing a Canadian investigation involving a multidrug-resistant Pseudomonas aeruginosa outbreak in an ICU. The report implicated the faucets over the hand hygiene sinks, with fluorescent dye showing droplet dispersal roughly 3 feet away from the sinks.
“Somehow it [the 3-feet rule] got implemented in guidelines in sterile processing decontamination areas, which are not the same as hand hygiene,’’ Ms. Ofstead explained.
With a goal of providing more current evidence on droplet generation and dispersal, as well as personal protection equipment (PPE) exposure/effectiveness, she and her colleagues simulated manual cleaning of a decommissioned colonoscope and transvaginal ultrasound probe, using for the study location a new academic sterile processing unit.
To detect droplet generation and dispersal as well as splash following common technician activities (for example, colonoscope brushing, scrubbing, rinsing and transport to an automated endoscope reprocessor [AER] for sterilization), the researchers affixed blue moisture-detection paper to environmental surfaces, on carts positioned 4 feet (1.2 meters) from the sink (to simulate observers), and along a 15-foot pathway between the sink and AER.
They observed droplets everywhere.
Technician activities such as running the faucet and rinsing the probe under running water generated substantial splashing overall. Instrument rinsing in particular produced small and large droplets and confluent puddles of water around the sink and in the broad area surrounding the workspace. Droplets were also dispersed on the floor 7.25 feet (2.2 meters) away and along the entire 15-foot path from the sink to the AER.
At the sink, the technician risked drenching exposure from head to toe during most activities, and even observers positioned 3-4 feet away were found to have droplets on their gowns. In addition, saturated shoe covers reportedly tracked moisture away from the sink to the unit door – a distance of 13 feet (4 meters) – and 2 feet (0.6 meters) farther out into the PPE foyer for donning and doffing.
Although PPE gowns effectively repelled moisture during cleaning of a single device, Ms. Ofstead emphasized that technicians typically handle up to 10 instruments during a normal, 2-hour shift, further increasing exposure risk with each subsequent cleaning.
However, perhaps one of the most surprising findings was that despite an optimal unit design, including physical separation of clean and dirty activities and pressurized air flow to protect workers, droplets were still broadly dispersed.
Current efforts, however well-intentioned, might not be offering the degree of protection (and consideration) that sterile processing technicians need.
“The study was conducted in a new sterile processing area that had an extra excellent kind of distancing and three separate rooms, something that I think most of our hospitals are working toward,” Stella Hines, MD, associate professor at the University of Maryland School of Medicine, Baltimore, explained. Dr. Hines was not directly involved in the study.
“But it also really kind of highlighted what’s happening to workers potentially,” she added. “For example, we want to know if that spray or splatter has a live microbe it in that could cause a problem or ... in a highly wet environment, if that water has some kind of chemical in it that could pose an occupational hazard to the worker based on skin or mucous membrane exposure.”
Ms. Ofstead agreed. “We need to be thinking about the exposure of critically important workers and the environment in an era where we are worried about aerosol-generating procedures and superbugs,” she explained.
Dr. Hines and Ms. Ofstead also noted that the majority of staff involved in front-line patient care have never actually ventured into the sterile processing units nor do they recognize the risks that technicians working in these units face on a daily, or even hourly, basis.
“The people who run these operations are very well trained and knowledgeable. I think that it would be helpful for them to know that they’re appreciated and for the people upstairs on the front lines using the equipment to see what goes on downstairs and all of the painstaking steps that need to be in place for the equipment to come out of sterile processing and be ready to go,” said Dr. Hines.
In the meantime, hospital leaders need to address the challenges and danger posed by migrating infectious droplets, especially for workers involved in processes that stir them up in the first place – workers who by the end of their shifts are unavoidably drenched with infectious blood and tissue secretions.
“I think that it’s going to take a much bigger kind of worldview from hospital leadership,” Dr. Hines said.
The study was supported in part by a grant from Healthmark Industries. Ms. Ofstead reports research grants or consulting fees through her organization with 3M Company, Ambu, Boston Scientific, Cleanis, Fortive/Advanced Sterilization Products, Healthmark Industries, Pentax, and Steris/Cantel/Medviators. Dr. Hines reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In the era of Ebola, COVID-19, and even Legionnaires, technicians and other staff working behind the scenes to ensure provider and patient safety continue to face a long-recognized but under addressed challenge: splashes and airborne droplets.
Granted, National Institute for Occupational Safety and Health (NIOSH) standards, industry standards, and professional guidelines are all in place to prevent unintentional exposure to pathogens. However, findings from a newly published study in the American Journal of Infection Control suggest they fall short.
In the study, researchers found that simulated manual cleaning of medical devices generated a drenching splash throughout the process with droplet dispersal exceeding 7 feet (2.1 meters).
Cori L. Ofstead, MSPH, lead author and president/CEO of Ofstead & Associates, Bloomington, Minn., told this news organization. “That’s the problem with having standards and guidelines that are not based on relevant evidence, [which] in this case, is a single study that was done in an intensive care area where they had an infection outbreak.”
Ms. Ofstead was referring to a report in the journal Infection Control and Hospital Epidemiology, detailing a Canadian investigation involving a multidrug-resistant Pseudomonas aeruginosa outbreak in an ICU. The report implicated the faucets over the hand hygiene sinks, with fluorescent dye showing droplet dispersal roughly 3 feet away from the sinks.
“Somehow it [the 3-feet rule] got implemented in guidelines in sterile processing decontamination areas, which are not the same as hand hygiene,’’ Ms. Ofstead explained.
With a goal of providing more current evidence on droplet generation and dispersal, as well as personal protection equipment (PPE) exposure/effectiveness, she and her colleagues simulated manual cleaning of a decommissioned colonoscope and transvaginal ultrasound probe, using for the study location a new academic sterile processing unit.
To detect droplet generation and dispersal as well as splash following common technician activities (for example, colonoscope brushing, scrubbing, rinsing and transport to an automated endoscope reprocessor [AER] for sterilization), the researchers affixed blue moisture-detection paper to environmental surfaces, on carts positioned 4 feet (1.2 meters) from the sink (to simulate observers), and along a 15-foot pathway between the sink and AER.
They observed droplets everywhere.
Technician activities such as running the faucet and rinsing the probe under running water generated substantial splashing overall. Instrument rinsing in particular produced small and large droplets and confluent puddles of water around the sink and in the broad area surrounding the workspace. Droplets were also dispersed on the floor 7.25 feet (2.2 meters) away and along the entire 15-foot path from the sink to the AER.
At the sink, the technician risked drenching exposure from head to toe during most activities, and even observers positioned 3-4 feet away were found to have droplets on their gowns. In addition, saturated shoe covers reportedly tracked moisture away from the sink to the unit door – a distance of 13 feet (4 meters) – and 2 feet (0.6 meters) farther out into the PPE foyer for donning and doffing.
Although PPE gowns effectively repelled moisture during cleaning of a single device, Ms. Ofstead emphasized that technicians typically handle up to 10 instruments during a normal, 2-hour shift, further increasing exposure risk with each subsequent cleaning.
However, perhaps one of the most surprising findings was that despite an optimal unit design, including physical separation of clean and dirty activities and pressurized air flow to protect workers, droplets were still broadly dispersed.
Current efforts, however well-intentioned, might not be offering the degree of protection (and consideration) that sterile processing technicians need.
“The study was conducted in a new sterile processing area that had an extra excellent kind of distancing and three separate rooms, something that I think most of our hospitals are working toward,” Stella Hines, MD, associate professor at the University of Maryland School of Medicine, Baltimore, explained. Dr. Hines was not directly involved in the study.
“But it also really kind of highlighted what’s happening to workers potentially,” she added. “For example, we want to know if that spray or splatter has a live microbe it in that could cause a problem or ... in a highly wet environment, if that water has some kind of chemical in it that could pose an occupational hazard to the worker based on skin or mucous membrane exposure.”
Ms. Ofstead agreed. “We need to be thinking about the exposure of critically important workers and the environment in an era where we are worried about aerosol-generating procedures and superbugs,” she explained.
Dr. Hines and Ms. Ofstead also noted that the majority of staff involved in front-line patient care have never actually ventured into the sterile processing units nor do they recognize the risks that technicians working in these units face on a daily, or even hourly, basis.
“The people who run these operations are very well trained and knowledgeable. I think that it would be helpful for them to know that they’re appreciated and for the people upstairs on the front lines using the equipment to see what goes on downstairs and all of the painstaking steps that need to be in place for the equipment to come out of sterile processing and be ready to go,” said Dr. Hines.
In the meantime, hospital leaders need to address the challenges and danger posed by migrating infectious droplets, especially for workers involved in processes that stir them up in the first place – workers who by the end of their shifts are unavoidably drenched with infectious blood and tissue secretions.
“I think that it’s going to take a much bigger kind of worldview from hospital leadership,” Dr. Hines said.
The study was supported in part by a grant from Healthmark Industries. Ms. Ofstead reports research grants or consulting fees through her organization with 3M Company, Ambu, Boston Scientific, Cleanis, Fortive/Advanced Sterilization Products, Healthmark Industries, Pentax, and Steris/Cantel/Medviators. Dr. Hines reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF INFECTION CONTROL
C. diff recurrence drops with highly targeted ridinilazole
WASHINGTON – (CDI), according to phase 3 trial results presented at an annual scientific meeting on infectious diseases.
According to the Centers for Disease Control and Prevention, CDI is the top cause of antibiotic-associated diarrhea and one of the most common health care–associated infections in the United States. About 200,000 people in the United States are infected with C. difficile every year in the hospital or clinical care setting.
Most infections are currently treated with vancomycin. Although vancomycin has been shown to be more than 80% effective, it has been linked with recurrence rates ranging from 20% to 30% and interferes with the protective role of the gut microbiome against infection. The current study compared ridinilazole with vancomycin.
Results of the global, double-blinded, randomized trial were presented by Pablo C. Okhuysen, MD, professor of infectious disease at the University of Texas MD Anderson Cancer Center, Houston.
Participants with CDI received a 10-day course of ridinilazole 200 mg twice a day plus placebo or vancomycin 125 mg four times a day. The primary endpoint was sustained clinical response, defined as a clinical response with no recurrent CDI through 30 days after the end of treatment. Recurrent CDI was defined as a new episode of diarrhea with confirmed positive free toxin test requiring additional therapy.
Of the 759 patients enrolled, 745 were included in the modified intention-to-treat population (ridinilazole, n = 370; vancomycin, n = 375). Ridinilazole achieved a numerically higher rate of sustained clinical response than vancomycin (73.0% vs. 70.7%; P = .467), although the difference was not significant. Ridinilazole also resulted in a significant reduction in recurrence rate (8.1% vs. 17.3%; P < .001).
Ridinilazole’s effect was most notable in a subgroup of patients who were not receiving other antibiotics at time of enrollment – about 70% of participants. In that subgroup, the recurrence rate was 6.7% with ridinilazole versus 16.5% with vancomycin (P < .001), Dr. Okhuysen reported.
“That resulted in a relative risk reduction of 60%,” Dr. Okhuysen told this news organization.
Dr. Okhuysen pointed out that there are currently very few treatment options for CDI other than vancomycin.
“We need new agents to treat C. difficile,” he said, “particularly for those at risk of recurrence. In our study, we found that those exposed to vancomycin had very dramatic shifts in their microbiome.”
Vancomycin depletes the gut microbiome, which decreases the conversion of primary acids to secondary bile acids, the researchers noted.
“A dysbiotic microbiome is fertile ground for C. difficile to grow,” Dr. Okhuysen said. Ridinilazole does not disrupt the microbiome, he added.
Ridinilazole was well-tolerated in the study. The proportion of patients with at least one treatment-emergent adverse effect was 36.4% versus 35.5%, respectively, in the ridinilazole and vancomycin groups. And the proportion who stopped treatment because of treatment-related side effects was 0.8% versus 2.9%.
Mary Hayden, MD, pathology director in the division of infectious diseases at Rush University Medical Center, Chicago, who was not involved with the study, said the results are encouraging as “alternative agents or strategies to prevent recurrence are important to reduce CDI morbidity.”
Its double-blind, randomized, multicenter design strengthens the findings, she explained, adding that “the secondary outcomes of higher concentrations of secondary bile acids and microbiota diversity and composition lend biological plausibility.”
Ridinilazole’s narrow spectrum of activity “should result in less disruption of the colonic microbiota, which has theoretical benefit for both reducing CDI recurrence and for reducing risk of acquisition of multidrug-resistant organisms,” Dr. Hayden said.
Dr. Okhuysen shared that the team is in talks with the Food and Drug Administration and is preparing a manuscript for publication.
The study was supported by Summit Pharmaceuticals and funded by the Biomedical and Advanced Research and Development Authority. Dr. Okhuysen has reported receiving research support from and/or consulting for Summit, Merck, Deinove, Melinta, and Ferring Pharmaceuticals. Some of the coauthors have financial relationships with or received research support from Summit. Dr. Hayden has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
WASHINGTON – (CDI), according to phase 3 trial results presented at an annual scientific meeting on infectious diseases.
According to the Centers for Disease Control and Prevention, CDI is the top cause of antibiotic-associated diarrhea and one of the most common health care–associated infections in the United States. About 200,000 people in the United States are infected with C. difficile every year in the hospital or clinical care setting.
Most infections are currently treated with vancomycin. Although vancomycin has been shown to be more than 80% effective, it has been linked with recurrence rates ranging from 20% to 30% and interferes with the protective role of the gut microbiome against infection. The current study compared ridinilazole with vancomycin.
Results of the global, double-blinded, randomized trial were presented by Pablo C. Okhuysen, MD, professor of infectious disease at the University of Texas MD Anderson Cancer Center, Houston.
Participants with CDI received a 10-day course of ridinilazole 200 mg twice a day plus placebo or vancomycin 125 mg four times a day. The primary endpoint was sustained clinical response, defined as a clinical response with no recurrent CDI through 30 days after the end of treatment. Recurrent CDI was defined as a new episode of diarrhea with confirmed positive free toxin test requiring additional therapy.
Of the 759 patients enrolled, 745 were included in the modified intention-to-treat population (ridinilazole, n = 370; vancomycin, n = 375). Ridinilazole achieved a numerically higher rate of sustained clinical response than vancomycin (73.0% vs. 70.7%; P = .467), although the difference was not significant. Ridinilazole also resulted in a significant reduction in recurrence rate (8.1% vs. 17.3%; P < .001).
Ridinilazole’s effect was most notable in a subgroup of patients who were not receiving other antibiotics at time of enrollment – about 70% of participants. In that subgroup, the recurrence rate was 6.7% with ridinilazole versus 16.5% with vancomycin (P < .001), Dr. Okhuysen reported.
“That resulted in a relative risk reduction of 60%,” Dr. Okhuysen told this news organization.
Dr. Okhuysen pointed out that there are currently very few treatment options for CDI other than vancomycin.
“We need new agents to treat C. difficile,” he said, “particularly for those at risk of recurrence. In our study, we found that those exposed to vancomycin had very dramatic shifts in their microbiome.”
Vancomycin depletes the gut microbiome, which decreases the conversion of primary acids to secondary bile acids, the researchers noted.
“A dysbiotic microbiome is fertile ground for C. difficile to grow,” Dr. Okhuysen said. Ridinilazole does not disrupt the microbiome, he added.
Ridinilazole was well-tolerated in the study. The proportion of patients with at least one treatment-emergent adverse effect was 36.4% versus 35.5%, respectively, in the ridinilazole and vancomycin groups. And the proportion who stopped treatment because of treatment-related side effects was 0.8% versus 2.9%.
Mary Hayden, MD, pathology director in the division of infectious diseases at Rush University Medical Center, Chicago, who was not involved with the study, said the results are encouraging as “alternative agents or strategies to prevent recurrence are important to reduce CDI morbidity.”
Its double-blind, randomized, multicenter design strengthens the findings, she explained, adding that “the secondary outcomes of higher concentrations of secondary bile acids and microbiota diversity and composition lend biological plausibility.”
Ridinilazole’s narrow spectrum of activity “should result in less disruption of the colonic microbiota, which has theoretical benefit for both reducing CDI recurrence and for reducing risk of acquisition of multidrug-resistant organisms,” Dr. Hayden said.
Dr. Okhuysen shared that the team is in talks with the Food and Drug Administration and is preparing a manuscript for publication.
The study was supported by Summit Pharmaceuticals and funded by the Biomedical and Advanced Research and Development Authority. Dr. Okhuysen has reported receiving research support from and/or consulting for Summit, Merck, Deinove, Melinta, and Ferring Pharmaceuticals. Some of the coauthors have financial relationships with or received research support from Summit. Dr. Hayden has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
WASHINGTON – (CDI), according to phase 3 trial results presented at an annual scientific meeting on infectious diseases.
According to the Centers for Disease Control and Prevention, CDI is the top cause of antibiotic-associated diarrhea and one of the most common health care–associated infections in the United States. About 200,000 people in the United States are infected with C. difficile every year in the hospital or clinical care setting.
Most infections are currently treated with vancomycin. Although vancomycin has been shown to be more than 80% effective, it has been linked with recurrence rates ranging from 20% to 30% and interferes with the protective role of the gut microbiome against infection. The current study compared ridinilazole with vancomycin.
Results of the global, double-blinded, randomized trial were presented by Pablo C. Okhuysen, MD, professor of infectious disease at the University of Texas MD Anderson Cancer Center, Houston.
Participants with CDI received a 10-day course of ridinilazole 200 mg twice a day plus placebo or vancomycin 125 mg four times a day. The primary endpoint was sustained clinical response, defined as a clinical response with no recurrent CDI through 30 days after the end of treatment. Recurrent CDI was defined as a new episode of diarrhea with confirmed positive free toxin test requiring additional therapy.
Of the 759 patients enrolled, 745 were included in the modified intention-to-treat population (ridinilazole, n = 370; vancomycin, n = 375). Ridinilazole achieved a numerically higher rate of sustained clinical response than vancomycin (73.0% vs. 70.7%; P = .467), although the difference was not significant. Ridinilazole also resulted in a significant reduction in recurrence rate (8.1% vs. 17.3%; P < .001).
Ridinilazole’s effect was most notable in a subgroup of patients who were not receiving other antibiotics at time of enrollment – about 70% of participants. In that subgroup, the recurrence rate was 6.7% with ridinilazole versus 16.5% with vancomycin (P < .001), Dr. Okhuysen reported.
“That resulted in a relative risk reduction of 60%,” Dr. Okhuysen told this news organization.
Dr. Okhuysen pointed out that there are currently very few treatment options for CDI other than vancomycin.
“We need new agents to treat C. difficile,” he said, “particularly for those at risk of recurrence. In our study, we found that those exposed to vancomycin had very dramatic shifts in their microbiome.”
Vancomycin depletes the gut microbiome, which decreases the conversion of primary acids to secondary bile acids, the researchers noted.
“A dysbiotic microbiome is fertile ground for C. difficile to grow,” Dr. Okhuysen said. Ridinilazole does not disrupt the microbiome, he added.
Ridinilazole was well-tolerated in the study. The proportion of patients with at least one treatment-emergent adverse effect was 36.4% versus 35.5%, respectively, in the ridinilazole and vancomycin groups. And the proportion who stopped treatment because of treatment-related side effects was 0.8% versus 2.9%.
Mary Hayden, MD, pathology director in the division of infectious diseases at Rush University Medical Center, Chicago, who was not involved with the study, said the results are encouraging as “alternative agents or strategies to prevent recurrence are important to reduce CDI morbidity.”
Its double-blind, randomized, multicenter design strengthens the findings, she explained, adding that “the secondary outcomes of higher concentrations of secondary bile acids and microbiota diversity and composition lend biological plausibility.”
Ridinilazole’s narrow spectrum of activity “should result in less disruption of the colonic microbiota, which has theoretical benefit for both reducing CDI recurrence and for reducing risk of acquisition of multidrug-resistant organisms,” Dr. Hayden said.
Dr. Okhuysen shared that the team is in talks with the Food and Drug Administration and is preparing a manuscript for publication.
The study was supported by Summit Pharmaceuticals and funded by the Biomedical and Advanced Research and Development Authority. Dr. Okhuysen has reported receiving research support from and/or consulting for Summit, Merck, Deinove, Melinta, and Ferring Pharmaceuticals. Some of the coauthors have financial relationships with or received research support from Summit. Dr. Hayden has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT IDWEEK 2022
Hospitalizations for VAP rose prior to pandemic
Health care–associated infections are a significant burden, and “ventilator associated-pneumonia is a contributor to that,” said Namratha S. Meda, MBBS, in a presentation at the annual meeting of the American College of Chest Physicians.
VAP can affect length of stay and other costs, but factors related to VAP hospitalization have not been well studied, said Dr. Meda, of Medstar Health/Georgetown University Hospital, Washington.
To examine trends in hospitalization for VAP, Dr. Meda and colleagues reviewed data from the National Inpatient Sample from January 2013 to December 2019. The study population included adult patients with VAP as a primary or secondary diagnosis based on ICD-9 or ICD-10 codes.
Overall, the trend in hospitalizations showed a consistent increase, said Dr. Meda.
The researchers identified 128,025 adult hospitalizations with VAP during the study period, with an increase from 50 VAP cases per 100,000 hospitalizations in 2013 to 75 cases per 100,000 hospitalizations in 2019.
A total of 42,120 hospitalizations were associated with tracheostomy, ventilator dependence, or both. Hospitalizations in these categories increased by 80% during the study period, from 15 cases per 100,000 hospitalizations in 2013 to 27 cases per 100,000 hospitalizations in 2019.
The median cost for each hospitalization was $83,311, and showed a 2.9% increase from 2013 to 2019. The estimated annual cost of VAP hospitalizations was approximately $2.8 billion in 2019, Dr. Meda emphasized. However, all-cause hospital mortality remained unchanged over the study period, at approximately 20%.
The mean age of the hospitalized VAP patients was 58 years across all VAP-related hospitalizations, and 36.5% were women. More than half (58%) were White, 21% were Black, and 12% were Hispanic.
The researchers noted some sex and racial disparities; the median age was lower for Black and Hispanic patients, compared with White patients, but all-cause mortality was lower. Men had a significantly longer median length of stay, compared with women (21 days vs. 19 days), and higher median costs ($87,981 vs. $74,889) with a P <.001 for both, but the all-cause in-hospital mortality was not significantly different between sexes.
The steady increase in hospitalization for VAP without a significant change in all-cause mortality, might be driven by hospitals with higher levels of tracheostomy and ventilator dependence, but more research is needed, Dr. Meda noted.
The study was limited by the observational design, which allowed the researchers to report an association, but not causality, said Dr. Meda. However, the results reflect the ongoing financial burden of VAP on the health care system, although “it would be interesting to see how the trend might change if we just looked at the clinical definition versus billing data,” she noted.
The study did not include data since the advent of COVID-19, but COVID is likely to drive the trend of increasing VAP hospitalization higher, Dr. Meda added.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Health care–associated infections are a significant burden, and “ventilator associated-pneumonia is a contributor to that,” said Namratha S. Meda, MBBS, in a presentation at the annual meeting of the American College of Chest Physicians.
VAP can affect length of stay and other costs, but factors related to VAP hospitalization have not been well studied, said Dr. Meda, of Medstar Health/Georgetown University Hospital, Washington.
To examine trends in hospitalization for VAP, Dr. Meda and colleagues reviewed data from the National Inpatient Sample from January 2013 to December 2019. The study population included adult patients with VAP as a primary or secondary diagnosis based on ICD-9 or ICD-10 codes.
Overall, the trend in hospitalizations showed a consistent increase, said Dr. Meda.
The researchers identified 128,025 adult hospitalizations with VAP during the study period, with an increase from 50 VAP cases per 100,000 hospitalizations in 2013 to 75 cases per 100,000 hospitalizations in 2019.
A total of 42,120 hospitalizations were associated with tracheostomy, ventilator dependence, or both. Hospitalizations in these categories increased by 80% during the study period, from 15 cases per 100,000 hospitalizations in 2013 to 27 cases per 100,000 hospitalizations in 2019.
The median cost for each hospitalization was $83,311, and showed a 2.9% increase from 2013 to 2019. The estimated annual cost of VAP hospitalizations was approximately $2.8 billion in 2019, Dr. Meda emphasized. However, all-cause hospital mortality remained unchanged over the study period, at approximately 20%.
The mean age of the hospitalized VAP patients was 58 years across all VAP-related hospitalizations, and 36.5% were women. More than half (58%) were White, 21% were Black, and 12% were Hispanic.
The researchers noted some sex and racial disparities; the median age was lower for Black and Hispanic patients, compared with White patients, but all-cause mortality was lower. Men had a significantly longer median length of stay, compared with women (21 days vs. 19 days), and higher median costs ($87,981 vs. $74,889) with a P <.001 for both, but the all-cause in-hospital mortality was not significantly different between sexes.
The steady increase in hospitalization for VAP without a significant change in all-cause mortality, might be driven by hospitals with higher levels of tracheostomy and ventilator dependence, but more research is needed, Dr. Meda noted.
The study was limited by the observational design, which allowed the researchers to report an association, but not causality, said Dr. Meda. However, the results reflect the ongoing financial burden of VAP on the health care system, although “it would be interesting to see how the trend might change if we just looked at the clinical definition versus billing data,” she noted.
The study did not include data since the advent of COVID-19, but COVID is likely to drive the trend of increasing VAP hospitalization higher, Dr. Meda added.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Health care–associated infections are a significant burden, and “ventilator associated-pneumonia is a contributor to that,” said Namratha S. Meda, MBBS, in a presentation at the annual meeting of the American College of Chest Physicians.
VAP can affect length of stay and other costs, but factors related to VAP hospitalization have not been well studied, said Dr. Meda, of Medstar Health/Georgetown University Hospital, Washington.
To examine trends in hospitalization for VAP, Dr. Meda and colleagues reviewed data from the National Inpatient Sample from January 2013 to December 2019. The study population included adult patients with VAP as a primary or secondary diagnosis based on ICD-9 or ICD-10 codes.
Overall, the trend in hospitalizations showed a consistent increase, said Dr. Meda.
The researchers identified 128,025 adult hospitalizations with VAP during the study period, with an increase from 50 VAP cases per 100,000 hospitalizations in 2013 to 75 cases per 100,000 hospitalizations in 2019.
A total of 42,120 hospitalizations were associated with tracheostomy, ventilator dependence, or both. Hospitalizations in these categories increased by 80% during the study period, from 15 cases per 100,000 hospitalizations in 2013 to 27 cases per 100,000 hospitalizations in 2019.
The median cost for each hospitalization was $83,311, and showed a 2.9% increase from 2013 to 2019. The estimated annual cost of VAP hospitalizations was approximately $2.8 billion in 2019, Dr. Meda emphasized. However, all-cause hospital mortality remained unchanged over the study period, at approximately 20%.
The mean age of the hospitalized VAP patients was 58 years across all VAP-related hospitalizations, and 36.5% were women. More than half (58%) were White, 21% were Black, and 12% were Hispanic.
The researchers noted some sex and racial disparities; the median age was lower for Black and Hispanic patients, compared with White patients, but all-cause mortality was lower. Men had a significantly longer median length of stay, compared with women (21 days vs. 19 days), and higher median costs ($87,981 vs. $74,889) with a P <.001 for both, but the all-cause in-hospital mortality was not significantly different between sexes.
The steady increase in hospitalization for VAP without a significant change in all-cause mortality, might be driven by hospitals with higher levels of tracheostomy and ventilator dependence, but more research is needed, Dr. Meda noted.
The study was limited by the observational design, which allowed the researchers to report an association, but not causality, said Dr. Meda. However, the results reflect the ongoing financial burden of VAP on the health care system, although “it would be interesting to see how the trend might change if we just looked at the clinical definition versus billing data,” she noted.
The study did not include data since the advent of COVID-19, but COVID is likely to drive the trend of increasing VAP hospitalization higher, Dr. Meda added.
The study received no outside funding. The researchers had no financial conflicts to disclose.
FROM CHEST 2022
Sepsis transition program may lower mortality in patients discharged to post-acute care
Sepsis survivors discharged to post-acute care facilities are at high risk for mortality and hospital readmission, according to Nicholas Colucciello, MD, and few interventions have been shown to reduce these adverse outcomes.
Dr. Colucciello and colleagues compared the effects of a Sepsis Transition And Recovery (STAR) program versus Usual Care (UC) alone on 30-day mortality and hospital readmission among sepsis survivors discharged to post-acute care.
In a study presented at the annual meeting of the American College of Chest Physicians (CHEST), Dr. Colucciello, a primary care physician in Toledo, Ohio, presented data suggesting that
Study of IMPACTS
The study was a secondary analysis of patients from the IMPACTS (Improving Morbidity During Post-Acute Care Transitions for Sepsis) randomized clinical trial, focusing only on those patients who were discharged to a post-acute care facility. IMPACTS evaluated the effectiveness of STAR, a post-sepsis transition program using nurse navigators to deliver best-practice post-sepsis care during and after hospitalization, Dr. Colucciello said. The interventions included comorbidity monitoring, medication review, evaluation for new impairments/symptoms, and goals of care assessment.
“Over one-third of sepsis survivors are discharged to post-acute care as they are not stable enough to go home,” said Dr. Colucciello, and among these patients there is a high risk for mortality and hospital readmission.
Dr. Colucciello and his colleagues randomly assigned patients hospitalized with sepsis and deemed high risk for post-discharge readmission or mortality to either STAR or usual care. The primary outcome was a composite of 30-day readmission and mortality, which was assessed from the electronic health record and social security death master file.
Of the 175 (21%) IMPACTS patients discharged to post-acute care facilities, 143 (82%) were sent to skilled nursing facilities, and 12 (7%) were sent to long-term acute care hospitals. The remaining 20 patients (11%) were sent to inpatient rehabilitation. A total of 88 of these patients received the STAR intervention and 87 received usual care.
Suggestive results
The study showed that the composite primary endpoint occurred in 26 (30.6%) patients in the usual care group versus 18 (20.7%) patients in the STAR group, for a risk difference of –9.9% (95% CI, –22.9 to 3.1), according to Dr. Colucciello. As individual factors, 30-day all-cause mortality was 8.2% in the UC group, compared with 5.8% in the STAR group, for a risk difference of –2.5% (95% CI, –10.1 to 5.0) and the 30-day all-cause readmission was 27.1% in the UC group, compared with 17.2% in the STAR program, for a risk difference of –9.8% (95% CI, –22.2 to 2.5). On average, patients receiving UC experienced 26.5 hospital-free days, compared with 27.4 hospital-free days in the STAR group, he added.
The biggest limitation of the study was the fact that it was underpowered to detect statistically significant differences, despite the suggestive results, said Dr. Colucciello. However, he added: “This secondary analysis of the IMPACTS randomized trial found that the STAR intervention may decrease 30-day mortality and readmission rates among sepsis patients discharged to a post-acute care facility,” he concluded.
Dr. Colucciello and colleagues report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sepsis survivors discharged to post-acute care facilities are at high risk for mortality and hospital readmission, according to Nicholas Colucciello, MD, and few interventions have been shown to reduce these adverse outcomes.
Dr. Colucciello and colleagues compared the effects of a Sepsis Transition And Recovery (STAR) program versus Usual Care (UC) alone on 30-day mortality and hospital readmission among sepsis survivors discharged to post-acute care.
In a study presented at the annual meeting of the American College of Chest Physicians (CHEST), Dr. Colucciello, a primary care physician in Toledo, Ohio, presented data suggesting that
Study of IMPACTS
The study was a secondary analysis of patients from the IMPACTS (Improving Morbidity During Post-Acute Care Transitions for Sepsis) randomized clinical trial, focusing only on those patients who were discharged to a post-acute care facility. IMPACTS evaluated the effectiveness of STAR, a post-sepsis transition program using nurse navigators to deliver best-practice post-sepsis care during and after hospitalization, Dr. Colucciello said. The interventions included comorbidity monitoring, medication review, evaluation for new impairments/symptoms, and goals of care assessment.
“Over one-third of sepsis survivors are discharged to post-acute care as they are not stable enough to go home,” said Dr. Colucciello, and among these patients there is a high risk for mortality and hospital readmission.
Dr. Colucciello and his colleagues randomly assigned patients hospitalized with sepsis and deemed high risk for post-discharge readmission or mortality to either STAR or usual care. The primary outcome was a composite of 30-day readmission and mortality, which was assessed from the electronic health record and social security death master file.
Of the 175 (21%) IMPACTS patients discharged to post-acute care facilities, 143 (82%) were sent to skilled nursing facilities, and 12 (7%) were sent to long-term acute care hospitals. The remaining 20 patients (11%) were sent to inpatient rehabilitation. A total of 88 of these patients received the STAR intervention and 87 received usual care.
Suggestive results
The study showed that the composite primary endpoint occurred in 26 (30.6%) patients in the usual care group versus 18 (20.7%) patients in the STAR group, for a risk difference of –9.9% (95% CI, –22.9 to 3.1), according to Dr. Colucciello. As individual factors, 30-day all-cause mortality was 8.2% in the UC group, compared with 5.8% in the STAR group, for a risk difference of –2.5% (95% CI, –10.1 to 5.0) and the 30-day all-cause readmission was 27.1% in the UC group, compared with 17.2% in the STAR program, for a risk difference of –9.8% (95% CI, –22.2 to 2.5). On average, patients receiving UC experienced 26.5 hospital-free days, compared with 27.4 hospital-free days in the STAR group, he added.
The biggest limitation of the study was the fact that it was underpowered to detect statistically significant differences, despite the suggestive results, said Dr. Colucciello. However, he added: “This secondary analysis of the IMPACTS randomized trial found that the STAR intervention may decrease 30-day mortality and readmission rates among sepsis patients discharged to a post-acute care facility,” he concluded.
Dr. Colucciello and colleagues report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sepsis survivors discharged to post-acute care facilities are at high risk for mortality and hospital readmission, according to Nicholas Colucciello, MD, and few interventions have been shown to reduce these adverse outcomes.
Dr. Colucciello and colleagues compared the effects of a Sepsis Transition And Recovery (STAR) program versus Usual Care (UC) alone on 30-day mortality and hospital readmission among sepsis survivors discharged to post-acute care.
In a study presented at the annual meeting of the American College of Chest Physicians (CHEST), Dr. Colucciello, a primary care physician in Toledo, Ohio, presented data suggesting that
Study of IMPACTS
The study was a secondary analysis of patients from the IMPACTS (Improving Morbidity During Post-Acute Care Transitions for Sepsis) randomized clinical trial, focusing only on those patients who were discharged to a post-acute care facility. IMPACTS evaluated the effectiveness of STAR, a post-sepsis transition program using nurse navigators to deliver best-practice post-sepsis care during and after hospitalization, Dr. Colucciello said. The interventions included comorbidity monitoring, medication review, evaluation for new impairments/symptoms, and goals of care assessment.
“Over one-third of sepsis survivors are discharged to post-acute care as they are not stable enough to go home,” said Dr. Colucciello, and among these patients there is a high risk for mortality and hospital readmission.
Dr. Colucciello and his colleagues randomly assigned patients hospitalized with sepsis and deemed high risk for post-discharge readmission or mortality to either STAR or usual care. The primary outcome was a composite of 30-day readmission and mortality, which was assessed from the electronic health record and social security death master file.
Of the 175 (21%) IMPACTS patients discharged to post-acute care facilities, 143 (82%) were sent to skilled nursing facilities, and 12 (7%) were sent to long-term acute care hospitals. The remaining 20 patients (11%) were sent to inpatient rehabilitation. A total of 88 of these patients received the STAR intervention and 87 received usual care.
Suggestive results
The study showed that the composite primary endpoint occurred in 26 (30.6%) patients in the usual care group versus 18 (20.7%) patients in the STAR group, for a risk difference of –9.9% (95% CI, –22.9 to 3.1), according to Dr. Colucciello. As individual factors, 30-day all-cause mortality was 8.2% in the UC group, compared with 5.8% in the STAR group, for a risk difference of –2.5% (95% CI, –10.1 to 5.0) and the 30-day all-cause readmission was 27.1% in the UC group, compared with 17.2% in the STAR program, for a risk difference of –9.8% (95% CI, –22.2 to 2.5). On average, patients receiving UC experienced 26.5 hospital-free days, compared with 27.4 hospital-free days in the STAR group, he added.
The biggest limitation of the study was the fact that it was underpowered to detect statistically significant differences, despite the suggestive results, said Dr. Colucciello. However, he added: “This secondary analysis of the IMPACTS randomized trial found that the STAR intervention may decrease 30-day mortality and readmission rates among sepsis patients discharged to a post-acute care facility,” he concluded.
Dr. Colucciello and colleagues report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CHEST 2022
Sepsis predictor tool falls short in emergency setting
Use of a sepsis predictor made little difference in time to antibiotic administration for septic patients in the emergency department, based on data from more than 200 patients.
“One of the big problems with sepsis is the lack of current tools for early and accurate diagnoses,” said Daniel Burgin, MD, an internal medicine resident at Louisiana State University, Baton Rouge, in a presentation at the annual meeting of the American College of Chest Physicians.
The EPIC Sepsis Model (ESM) was designed to help facilitate earlier detection of sepsis and speed time to the start of antibiotics, but its effectiveness has not been well studied, Dr. Burgin said.
In Dr. Burgin’s facility, the ESM is mainly driven by systemic inflammatory response syndrome (SIRS) and blood pressure and is calculated every 15 minutes; the system triggers a best-practice advisory if needed, with an alert that sepsis may be suspected.
To assess the impact of ESM on time to antibiotics, Dr. Burgin and colleagues reviewed data from 226 adult patients who presented to a single emergency department between February 2019 and June 2019. All patients presented with at least two criteria for SIRS. An ESM threshold of 6 was designed to trigger a set of orders to guide providers on a treatment plan that included antibiotics.
The researchers compared times to the ordering and the administration of antibiotics for patients with ESM scores of 6 or higher vs. less than 6 within 6 hours of triage in the ED. A total of 109 patients (48.2%) received antibiotics in the ED. Of these, 71 (74.5%) had ESM less than 6 and 38 (40.6%) had ESM of 6 or higher. The times from triage to antibiotics ordered and administered was significantly less in patients with ESM of 6 or higher (90.5 minutes vs. 131.5 minutes; 136 minutes vs. 186 minutes, respectively; P = .011 for both).
A total of 188 patients were evaluated for infection, and 86 met Sepsis-2 criteria based on physician chart review. These patients were significantly more likely than those not meeting the Sepsis-2 criteria to receive antibiotics in the ED (76.7% vs. 22.8%; P <.001).
Another 21 patients met criteria for Sepsis-3 based on a physician panel. Although all 21 received antibiotics, 5 did not receive them within 6 hours of triage in the ED, Dr. Burgin said. The median times to ordering and administration of antibiotics for Sepsis-3 patients with an ESM of 6 or higher were –5 and 38.5 (interquartile range), respectively.
“We hope that the ESM would prompt providers to start the order [for antibiotics],” Dr. Burgin said in his presentation. However, the researchers found no consistent patterns, and in many cases the ESM alerts occurred after the orders had been initiated, he noted.
The study findings were limited by the use of data from a single center; the implementation of the EPIC tool is hospital specific, said Dr. Burgin. However, the results suggest that he said.
“While this research proved useful in assessing the impact of ESM on time to antibiotics, more research is needed to understand how to operationalize predictive analytics,” Dr. Burgin said of the study findings. “The goal is to find the balance between early identification of sepsis and timely antimicrobial therapy and the potential harm of overalerting treatment teams.”
The study was supported in part by Cytovale, a sepsis diagnostics company. Several coauthors disclosed financial relationships with Cytovale. Dr. Burgin reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Use of a sepsis predictor made little difference in time to antibiotic administration for septic patients in the emergency department, based on data from more than 200 patients.
“One of the big problems with sepsis is the lack of current tools for early and accurate diagnoses,” said Daniel Burgin, MD, an internal medicine resident at Louisiana State University, Baton Rouge, in a presentation at the annual meeting of the American College of Chest Physicians.
The EPIC Sepsis Model (ESM) was designed to help facilitate earlier detection of sepsis and speed time to the start of antibiotics, but its effectiveness has not been well studied, Dr. Burgin said.
In Dr. Burgin’s facility, the ESM is mainly driven by systemic inflammatory response syndrome (SIRS) and blood pressure and is calculated every 15 minutes; the system triggers a best-practice advisory if needed, with an alert that sepsis may be suspected.
To assess the impact of ESM on time to antibiotics, Dr. Burgin and colleagues reviewed data from 226 adult patients who presented to a single emergency department between February 2019 and June 2019. All patients presented with at least two criteria for SIRS. An ESM threshold of 6 was designed to trigger a set of orders to guide providers on a treatment plan that included antibiotics.
The researchers compared times to the ordering and the administration of antibiotics for patients with ESM scores of 6 or higher vs. less than 6 within 6 hours of triage in the ED. A total of 109 patients (48.2%) received antibiotics in the ED. Of these, 71 (74.5%) had ESM less than 6 and 38 (40.6%) had ESM of 6 or higher. The times from triage to antibiotics ordered and administered was significantly less in patients with ESM of 6 or higher (90.5 minutes vs. 131.5 minutes; 136 minutes vs. 186 minutes, respectively; P = .011 for both).
A total of 188 patients were evaluated for infection, and 86 met Sepsis-2 criteria based on physician chart review. These patients were significantly more likely than those not meeting the Sepsis-2 criteria to receive antibiotics in the ED (76.7% vs. 22.8%; P <.001).
Another 21 patients met criteria for Sepsis-3 based on a physician panel. Although all 21 received antibiotics, 5 did not receive them within 6 hours of triage in the ED, Dr. Burgin said. The median times to ordering and administration of antibiotics for Sepsis-3 patients with an ESM of 6 or higher were –5 and 38.5 (interquartile range), respectively.
“We hope that the ESM would prompt providers to start the order [for antibiotics],” Dr. Burgin said in his presentation. However, the researchers found no consistent patterns, and in many cases the ESM alerts occurred after the orders had been initiated, he noted.
The study findings were limited by the use of data from a single center; the implementation of the EPIC tool is hospital specific, said Dr. Burgin. However, the results suggest that he said.
“While this research proved useful in assessing the impact of ESM on time to antibiotics, more research is needed to understand how to operationalize predictive analytics,” Dr. Burgin said of the study findings. “The goal is to find the balance between early identification of sepsis and timely antimicrobial therapy and the potential harm of overalerting treatment teams.”
The study was supported in part by Cytovale, a sepsis diagnostics company. Several coauthors disclosed financial relationships with Cytovale. Dr. Burgin reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Use of a sepsis predictor made little difference in time to antibiotic administration for septic patients in the emergency department, based on data from more than 200 patients.
“One of the big problems with sepsis is the lack of current tools for early and accurate diagnoses,” said Daniel Burgin, MD, an internal medicine resident at Louisiana State University, Baton Rouge, in a presentation at the annual meeting of the American College of Chest Physicians.
The EPIC Sepsis Model (ESM) was designed to help facilitate earlier detection of sepsis and speed time to the start of antibiotics, but its effectiveness has not been well studied, Dr. Burgin said.
In Dr. Burgin’s facility, the ESM is mainly driven by systemic inflammatory response syndrome (SIRS) and blood pressure and is calculated every 15 minutes; the system triggers a best-practice advisory if needed, with an alert that sepsis may be suspected.
To assess the impact of ESM on time to antibiotics, Dr. Burgin and colleagues reviewed data from 226 adult patients who presented to a single emergency department between February 2019 and June 2019. All patients presented with at least two criteria for SIRS. An ESM threshold of 6 was designed to trigger a set of orders to guide providers on a treatment plan that included antibiotics.
The researchers compared times to the ordering and the administration of antibiotics for patients with ESM scores of 6 or higher vs. less than 6 within 6 hours of triage in the ED. A total of 109 patients (48.2%) received antibiotics in the ED. Of these, 71 (74.5%) had ESM less than 6 and 38 (40.6%) had ESM of 6 or higher. The times from triage to antibiotics ordered and administered was significantly less in patients with ESM of 6 or higher (90.5 minutes vs. 131.5 minutes; 136 minutes vs. 186 minutes, respectively; P = .011 for both).
A total of 188 patients were evaluated for infection, and 86 met Sepsis-2 criteria based on physician chart review. These patients were significantly more likely than those not meeting the Sepsis-2 criteria to receive antibiotics in the ED (76.7% vs. 22.8%; P <.001).
Another 21 patients met criteria for Sepsis-3 based on a physician panel. Although all 21 received antibiotics, 5 did not receive them within 6 hours of triage in the ED, Dr. Burgin said. The median times to ordering and administration of antibiotics for Sepsis-3 patients with an ESM of 6 or higher were –5 and 38.5 (interquartile range), respectively.
“We hope that the ESM would prompt providers to start the order [for antibiotics],” Dr. Burgin said in his presentation. However, the researchers found no consistent patterns, and in many cases the ESM alerts occurred after the orders had been initiated, he noted.
The study findings were limited by the use of data from a single center; the implementation of the EPIC tool is hospital specific, said Dr. Burgin. However, the results suggest that he said.
“While this research proved useful in assessing the impact of ESM on time to antibiotics, more research is needed to understand how to operationalize predictive analytics,” Dr. Burgin said of the study findings. “The goal is to find the balance between early identification of sepsis and timely antimicrobial therapy and the potential harm of overalerting treatment teams.”
The study was supported in part by Cytovale, a sepsis diagnostics company. Several coauthors disclosed financial relationships with Cytovale. Dr. Burgin reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CHEST 2022
Hospital-acquired pneumonia is killing patients, yet there is a simple way to stop it
Four years ago, when Dr. Karen Giuliano went to a Boston hospital for hip replacement surgery, she was given a pale-pink bucket of toiletries issued to patients in many hospitals. Inside were tissues, bar soap, deodorant, toothpaste, and, without a doubt, the worst toothbrush she’d ever seen.
“I couldn’t believe it. I got a toothbrush with no bristles,” she said. “It must have not gone through the bristle machine. It was just a stick.”
To most patients, a useless hospital toothbrush would be a mild inconvenience. But to Dr. Giuliano, a nursing professor at the University of Massachusetts, Amherst, it was a reminder of a pervasive “blind spot” in U.S. hospitals: the stunning consequences of unbrushed teeth.
Hospital patients not getting their teeth brushed, or not brushing their teeth themselves, is believed to be a leading cause of hundreds of thousands of cases of pneumonia a year in patients who have not been put on a ventilator. Pneumonia is among the most common infections that occur in health care facilities, and a majority of cases are nonventilator hospital-acquired pneumonia, or NVHAP, which kills up to 30% of those infected, Dr. Giuliano and other experts said.
But unlike many infections that strike within hospitals, the federal government doesn’t require hospitals to report cases of NVHAP. As a result, few hospitals understand the origin of the illness, track its occurrence, or actively work to prevent it, the experts said.
, according to a growing body of peer-reviewed research papers. Instead, many hospitals often skip teeth brushing to prioritize other tasks and provide only cheap, ineffective toothbrushes, often unaware of the consequences, said Dr. Dian Baker, a Sacramento (Calif.) State nursing professor who has spent more than a decade studying NVHAP.
“I’ll tell you that today the vast majority of the tens of thousands of nurses in hospitals have no idea that pneumonia comes from germs in the mouth,” Dr. Baker said.
Pneumonia occurs when germs trigger an infection in the lungs. Although NVHAP accounts for most of the cases that occur in hospitals, it historically has not received the same attention as pneumonia tied to ventilators, which is easier to identify and study because it occurs among a narrow subset of patients.
NVHAP, a risk for virtually all hospital patients, is often caused by bacteria from the mouth that gathers in the scummy biofilm on unbrushed teeth and is aspirated into the lungs. Patients face a higher risk if they lie flat or remain immobile for long periods, so NVHAP can also be prevented by elevating their heads and getting them out of bed more often.
According to the National Organization for NV-HAP Prevention, which was founded in 2020, this pneumonia infects about 1 in every 100 hospital patients and kills 15%-30% of them. For those who survive, the illness often extends their hospital stay by up to 15 days and makes it much more likely they will be readmitted within a month or transferred to an intensive care unit.
John McCleary, 83, of Millinocket, Maine, contracted a likely case of NVHAP in 2008 after he fractured his ankle in a fall and spent 12 days in rehabilitation at a hospital, said his daughter, Kathy Day, a retired nurse and advocate with the Patient Safety Action Network.
Mr. McCleary recovered from the fracture but not from pneumonia. Two days after he returned home, the infection in his lungs caused him to be rushed back to the hospital, where he went into sepsis and spent weeks in treatment before moving to an isolation unit in a nursing home.
He died weeks later, emaciated, largely deaf, unable to eat, and often “too weak to get water through a straw,” his daughter said. After contracting pneumonia, he never walked again.
“It was an astounding assault on his body, from him being here visiting me the week before his fall, to his death just a few months later,” Ms. Day said. “And the whole thing was avoidable.”
While experts describe NVHAP as a largely ignored threat, that appears to be changing.
Last year, a group of researchers – including Dr. Giuliano and Dr. Baker, plus officials from the Centers for Disease Control and Prevention, the Veterans Health Administration, and the Joint Commission – published a “call-to-action” research paper hoping to launch “a national health care conversation about NVHAP prevention.”
The Joint Commission, a nonprofit organization whose accreditation can make or break hospitals, is considering broadening the infection control standards to include more ailments, including NVHAP, said Sylvia Garcia-Houchins, its director of infection prevention and control.
Separately, ECRI, a nonprofit focused on health care safety, this year pinpointed NVHAP as one of its top patient safety concerns.
James Davis, an ECRI infection expert, said the prevalence of NVHAP, while already alarming, is likely “underestimated” and probably worsened as hospitals swelled with patients during the coronavirus pandemic.
“We only know what’s reported,” Mr. Davis said. “Could this be the tip of the iceberg? I would say, in my opinion, probably.”
To better measure the condition, some researchers call for a standardized surveillance definition of NVHAP, which could in time open the door for the federal government to mandate reporting of cases or incentivize prevention. With increasing urgency, researchers are pushing for hospitals not to wait for the federal government to act against NVHAP.
Dr. Baker said she has spoken with hundreds of hospitals about how to prevent NVHAP, but thousands more have yet to take up the cause.
“We are not asking for some big, $300,000 piece of equipment,” Dr. Baker said. “The two things that show the best evidence of preventing this harm are things that should be happening in standard care anyway – brushing teeth and getting patients mobilized.”
That evidence comes from a smattering of studies that show those two strategies can lead to sharp reductions in infection rates.
In California, a study at 21 Kaiser Permanente hospitals used a reprioritization of oral care and getting patients out of bed to reduce rates of hospital-acquired pneumonia by around 70%. At Sutter Medical Center in Sacramento, better oral care reduced NVHAP cases by a yearly average of 35%.
At Orlando Regional Medical Center in Florida, a medical unit and a surgical unit where patients received enhanced oral care reduced NVHAP rates by 85% and 56%, respectively, when compared with similar units that received normal care. A similar study is underway at two hospitals in Illinois.
And the most compelling results come from a veterans’ hospital in Salem, Va., where a 2016 oral care pilot program reduced rates of NVHAP by 92% – saving an estimated 13 lives in just 19 months. The program, the HAPPEN Initiative, has been expanded across the Veterans Health Administration, and experts say it could serve as a model for all U.S. hospitals.
Dr. Michelle Lucatorto, a nursing official who leads HAPPEN, said the program trains nurses to most effectively brush patients’ teeth and educates patients and families on the link between oral care and preventing NVHAP. While teeth brushing may not seem to require training, Dr. Lucatorto made comparisons to how the coronavirus revealed many Americans were doing a lackluster job of another routine hygienic practice: washing their hands.
“Sometimes we are searching for the most complicated intervention,” she said. “We are always looking for that new bypass surgery, or some new technical equipment. And sometimes I think we fail to look at the simple things we can do in our practice to save people’s lives.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Four years ago, when Dr. Karen Giuliano went to a Boston hospital for hip replacement surgery, she was given a pale-pink bucket of toiletries issued to patients in many hospitals. Inside were tissues, bar soap, deodorant, toothpaste, and, without a doubt, the worst toothbrush she’d ever seen.
“I couldn’t believe it. I got a toothbrush with no bristles,” she said. “It must have not gone through the bristle machine. It was just a stick.”
To most patients, a useless hospital toothbrush would be a mild inconvenience. But to Dr. Giuliano, a nursing professor at the University of Massachusetts, Amherst, it was a reminder of a pervasive “blind spot” in U.S. hospitals: the stunning consequences of unbrushed teeth.
Hospital patients not getting their teeth brushed, or not brushing their teeth themselves, is believed to be a leading cause of hundreds of thousands of cases of pneumonia a year in patients who have not been put on a ventilator. Pneumonia is among the most common infections that occur in health care facilities, and a majority of cases are nonventilator hospital-acquired pneumonia, or NVHAP, which kills up to 30% of those infected, Dr. Giuliano and other experts said.
But unlike many infections that strike within hospitals, the federal government doesn’t require hospitals to report cases of NVHAP. As a result, few hospitals understand the origin of the illness, track its occurrence, or actively work to prevent it, the experts said.
, according to a growing body of peer-reviewed research papers. Instead, many hospitals often skip teeth brushing to prioritize other tasks and provide only cheap, ineffective toothbrushes, often unaware of the consequences, said Dr. Dian Baker, a Sacramento (Calif.) State nursing professor who has spent more than a decade studying NVHAP.
“I’ll tell you that today the vast majority of the tens of thousands of nurses in hospitals have no idea that pneumonia comes from germs in the mouth,” Dr. Baker said.
Pneumonia occurs when germs trigger an infection in the lungs. Although NVHAP accounts for most of the cases that occur in hospitals, it historically has not received the same attention as pneumonia tied to ventilators, which is easier to identify and study because it occurs among a narrow subset of patients.
NVHAP, a risk for virtually all hospital patients, is often caused by bacteria from the mouth that gathers in the scummy biofilm on unbrushed teeth and is aspirated into the lungs. Patients face a higher risk if they lie flat or remain immobile for long periods, so NVHAP can also be prevented by elevating their heads and getting them out of bed more often.
According to the National Organization for NV-HAP Prevention, which was founded in 2020, this pneumonia infects about 1 in every 100 hospital patients and kills 15%-30% of them. For those who survive, the illness often extends their hospital stay by up to 15 days and makes it much more likely they will be readmitted within a month or transferred to an intensive care unit.
John McCleary, 83, of Millinocket, Maine, contracted a likely case of NVHAP in 2008 after he fractured his ankle in a fall and spent 12 days in rehabilitation at a hospital, said his daughter, Kathy Day, a retired nurse and advocate with the Patient Safety Action Network.
Mr. McCleary recovered from the fracture but not from pneumonia. Two days after he returned home, the infection in his lungs caused him to be rushed back to the hospital, where he went into sepsis and spent weeks in treatment before moving to an isolation unit in a nursing home.
He died weeks later, emaciated, largely deaf, unable to eat, and often “too weak to get water through a straw,” his daughter said. After contracting pneumonia, he never walked again.
“It was an astounding assault on his body, from him being here visiting me the week before his fall, to his death just a few months later,” Ms. Day said. “And the whole thing was avoidable.”
While experts describe NVHAP as a largely ignored threat, that appears to be changing.
Last year, a group of researchers – including Dr. Giuliano and Dr. Baker, plus officials from the Centers for Disease Control and Prevention, the Veterans Health Administration, and the Joint Commission – published a “call-to-action” research paper hoping to launch “a national health care conversation about NVHAP prevention.”
The Joint Commission, a nonprofit organization whose accreditation can make or break hospitals, is considering broadening the infection control standards to include more ailments, including NVHAP, said Sylvia Garcia-Houchins, its director of infection prevention and control.
Separately, ECRI, a nonprofit focused on health care safety, this year pinpointed NVHAP as one of its top patient safety concerns.
James Davis, an ECRI infection expert, said the prevalence of NVHAP, while already alarming, is likely “underestimated” and probably worsened as hospitals swelled with patients during the coronavirus pandemic.
“We only know what’s reported,” Mr. Davis said. “Could this be the tip of the iceberg? I would say, in my opinion, probably.”
To better measure the condition, some researchers call for a standardized surveillance definition of NVHAP, which could in time open the door for the federal government to mandate reporting of cases or incentivize prevention. With increasing urgency, researchers are pushing for hospitals not to wait for the federal government to act against NVHAP.
Dr. Baker said she has spoken with hundreds of hospitals about how to prevent NVHAP, but thousands more have yet to take up the cause.
“We are not asking for some big, $300,000 piece of equipment,” Dr. Baker said. “The two things that show the best evidence of preventing this harm are things that should be happening in standard care anyway – brushing teeth and getting patients mobilized.”
That evidence comes from a smattering of studies that show those two strategies can lead to sharp reductions in infection rates.
In California, a study at 21 Kaiser Permanente hospitals used a reprioritization of oral care and getting patients out of bed to reduce rates of hospital-acquired pneumonia by around 70%. At Sutter Medical Center in Sacramento, better oral care reduced NVHAP cases by a yearly average of 35%.
At Orlando Regional Medical Center in Florida, a medical unit and a surgical unit where patients received enhanced oral care reduced NVHAP rates by 85% and 56%, respectively, when compared with similar units that received normal care. A similar study is underway at two hospitals in Illinois.
And the most compelling results come from a veterans’ hospital in Salem, Va., where a 2016 oral care pilot program reduced rates of NVHAP by 92% – saving an estimated 13 lives in just 19 months. The program, the HAPPEN Initiative, has been expanded across the Veterans Health Administration, and experts say it could serve as a model for all U.S. hospitals.
Dr. Michelle Lucatorto, a nursing official who leads HAPPEN, said the program trains nurses to most effectively brush patients’ teeth and educates patients and families on the link between oral care and preventing NVHAP. While teeth brushing may not seem to require training, Dr. Lucatorto made comparisons to how the coronavirus revealed many Americans were doing a lackluster job of another routine hygienic practice: washing their hands.
“Sometimes we are searching for the most complicated intervention,” she said. “We are always looking for that new bypass surgery, or some new technical equipment. And sometimes I think we fail to look at the simple things we can do in our practice to save people’s lives.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Four years ago, when Dr. Karen Giuliano went to a Boston hospital for hip replacement surgery, she was given a pale-pink bucket of toiletries issued to patients in many hospitals. Inside were tissues, bar soap, deodorant, toothpaste, and, without a doubt, the worst toothbrush she’d ever seen.
“I couldn’t believe it. I got a toothbrush with no bristles,” she said. “It must have not gone through the bristle machine. It was just a stick.”
To most patients, a useless hospital toothbrush would be a mild inconvenience. But to Dr. Giuliano, a nursing professor at the University of Massachusetts, Amherst, it was a reminder of a pervasive “blind spot” in U.S. hospitals: the stunning consequences of unbrushed teeth.
Hospital patients not getting their teeth brushed, or not brushing their teeth themselves, is believed to be a leading cause of hundreds of thousands of cases of pneumonia a year in patients who have not been put on a ventilator. Pneumonia is among the most common infections that occur in health care facilities, and a majority of cases are nonventilator hospital-acquired pneumonia, or NVHAP, which kills up to 30% of those infected, Dr. Giuliano and other experts said.
But unlike many infections that strike within hospitals, the federal government doesn’t require hospitals to report cases of NVHAP. As a result, few hospitals understand the origin of the illness, track its occurrence, or actively work to prevent it, the experts said.
, according to a growing body of peer-reviewed research papers. Instead, many hospitals often skip teeth brushing to prioritize other tasks and provide only cheap, ineffective toothbrushes, often unaware of the consequences, said Dr. Dian Baker, a Sacramento (Calif.) State nursing professor who has spent more than a decade studying NVHAP.
“I’ll tell you that today the vast majority of the tens of thousands of nurses in hospitals have no idea that pneumonia comes from germs in the mouth,” Dr. Baker said.
Pneumonia occurs when germs trigger an infection in the lungs. Although NVHAP accounts for most of the cases that occur in hospitals, it historically has not received the same attention as pneumonia tied to ventilators, which is easier to identify and study because it occurs among a narrow subset of patients.
NVHAP, a risk for virtually all hospital patients, is often caused by bacteria from the mouth that gathers in the scummy biofilm on unbrushed teeth and is aspirated into the lungs. Patients face a higher risk if they lie flat or remain immobile for long periods, so NVHAP can also be prevented by elevating their heads and getting them out of bed more often.
According to the National Organization for NV-HAP Prevention, which was founded in 2020, this pneumonia infects about 1 in every 100 hospital patients and kills 15%-30% of them. For those who survive, the illness often extends their hospital stay by up to 15 days and makes it much more likely they will be readmitted within a month or transferred to an intensive care unit.
John McCleary, 83, of Millinocket, Maine, contracted a likely case of NVHAP in 2008 after he fractured his ankle in a fall and spent 12 days in rehabilitation at a hospital, said his daughter, Kathy Day, a retired nurse and advocate with the Patient Safety Action Network.
Mr. McCleary recovered from the fracture but not from pneumonia. Two days after he returned home, the infection in his lungs caused him to be rushed back to the hospital, where he went into sepsis and spent weeks in treatment before moving to an isolation unit in a nursing home.
He died weeks later, emaciated, largely deaf, unable to eat, and often “too weak to get water through a straw,” his daughter said. After contracting pneumonia, he never walked again.
“It was an astounding assault on his body, from him being here visiting me the week before his fall, to his death just a few months later,” Ms. Day said. “And the whole thing was avoidable.”
While experts describe NVHAP as a largely ignored threat, that appears to be changing.
Last year, a group of researchers – including Dr. Giuliano and Dr. Baker, plus officials from the Centers for Disease Control and Prevention, the Veterans Health Administration, and the Joint Commission – published a “call-to-action” research paper hoping to launch “a national health care conversation about NVHAP prevention.”
The Joint Commission, a nonprofit organization whose accreditation can make or break hospitals, is considering broadening the infection control standards to include more ailments, including NVHAP, said Sylvia Garcia-Houchins, its director of infection prevention and control.
Separately, ECRI, a nonprofit focused on health care safety, this year pinpointed NVHAP as one of its top patient safety concerns.
James Davis, an ECRI infection expert, said the prevalence of NVHAP, while already alarming, is likely “underestimated” and probably worsened as hospitals swelled with patients during the coronavirus pandemic.
“We only know what’s reported,” Mr. Davis said. “Could this be the tip of the iceberg? I would say, in my opinion, probably.”
To better measure the condition, some researchers call for a standardized surveillance definition of NVHAP, which could in time open the door for the federal government to mandate reporting of cases or incentivize prevention. With increasing urgency, researchers are pushing for hospitals not to wait for the federal government to act against NVHAP.
Dr. Baker said she has spoken with hundreds of hospitals about how to prevent NVHAP, but thousands more have yet to take up the cause.
“We are not asking for some big, $300,000 piece of equipment,” Dr. Baker said. “The two things that show the best evidence of preventing this harm are things that should be happening in standard care anyway – brushing teeth and getting patients mobilized.”
That evidence comes from a smattering of studies that show those two strategies can lead to sharp reductions in infection rates.
In California, a study at 21 Kaiser Permanente hospitals used a reprioritization of oral care and getting patients out of bed to reduce rates of hospital-acquired pneumonia by around 70%. At Sutter Medical Center in Sacramento, better oral care reduced NVHAP cases by a yearly average of 35%.
At Orlando Regional Medical Center in Florida, a medical unit and a surgical unit where patients received enhanced oral care reduced NVHAP rates by 85% and 56%, respectively, when compared with similar units that received normal care. A similar study is underway at two hospitals in Illinois.
And the most compelling results come from a veterans’ hospital in Salem, Va., where a 2016 oral care pilot program reduced rates of NVHAP by 92% – saving an estimated 13 lives in just 19 months. The program, the HAPPEN Initiative, has been expanded across the Veterans Health Administration, and experts say it could serve as a model for all U.S. hospitals.
Dr. Michelle Lucatorto, a nursing official who leads HAPPEN, said the program trains nurses to most effectively brush patients’ teeth and educates patients and families on the link between oral care and preventing NVHAP. While teeth brushing may not seem to require training, Dr. Lucatorto made comparisons to how the coronavirus revealed many Americans were doing a lackluster job of another routine hygienic practice: washing their hands.
“Sometimes we are searching for the most complicated intervention,” she said. “We are always looking for that new bypass surgery, or some new technical equipment. And sometimes I think we fail to look at the simple things we can do in our practice to save people’s lives.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Transplanted pig hearts functioned normally in deceased persons on ventilator support
A team of surgeons successfully transplanted genetically engineered pig hearts into two recently deceased people whose bodies were being maintained on ventilatory support – not in the hope of restoring life, but as a proof-of-concept experiment in xenotransplantation that could eventually help to ease the critical shortage of donor organs.
The surgeries were performed on June 16 and July 6, 2022, using porcine hearts from animals genetically engineered to prevent organ rejection and promote adaptive immunity by human recipients
without utilizing unapproved devices or techniques or medications,” said Nader Moazami, MD, surgical director of heart transplantation and chief of the division of heart and lung transplantation and mechanical circulatory support at NYU Langone Health, New York.

Through 72 hours of postoperative monitoring “we evaluated the heart for functionality and the heart function was completely normal with excellent contractility,” he said at a press briefing announcing early results of the experimental program.
He acknowledged that for the first of the two procedures some surgical modification of the pig heart was required, primarily because of size differences between the donor and recipient.
“Nevertheless, we learned a tremendous amount from the first operation, and when that experience was translated into the second operation it even performed better,” he said.
Alex Reyentovich, MD, medical director of heart transplantation and director of the NYU Langone advanced heart failure program noted that “there are 6 million individuals with heart failure in the United States. About 100,000 of those individuals have end-stage heart failure, and we only do about 3,500 heart transplants a year in the United States, so we have a tremendous deficiency in organs, and there are many people dying waiting for a heart.”
Infection protocols
To date there has been only one xenotransplant of a genetically modified pig heart into a living human recipient, David Bennett Sr., age 57. The surgery, performed at the University of Maryland in January 2022, was initially successful, with the patient able to sit up in bed a few days after the procedure, and the heart performing like a “rock star” according to transplant surgeon Bartley Griffith, MD.
However, Mr. Bennett died 2 months after the procedure from compromise of the organ by an as yet undetermined cause, of which one may have been the heart's infection by porcine cytomegalovirus (CMV).

The NYU team, mindful of this potential setback, used more sensitive assays to screen the donor organs for porcine CMV, and implemented protocols to prevent and to monitor for potential zoonotic transmission of porcine endogenous retrovirus.
The procedure used a dedicated operating room and equipment that will not be used for clinical procedures, the team emphasized.
An organ transplant specialist who was not involved in the study commented that there can be unwelcome surprises even with the most rigorous infection prophylaxis protocols.
“I think these are important steps, but they don’t resolve the question of infectious risk. Sometimes viruses or latent infections are only manifested later,” said Jay A. Fishman, MD, associate director of the Massachusetts General Hospital Transplant Center and director of the transplant infectious diseases and compromised host program at the hospital, which is in Boston.
“I think these are important steps, but as you may recall from the Maryland heart transplant experience, when porcine cytomegalovirus was activated, it was a long way into that patient’s course, and so we just don’t know whether something would have been reactivated later,” he said in an interview.
Dr. Fishman noted that experience with xenotransplantation at the University of Maryland and other centers has suggested that immunosuppressive regimens used for human-to-human transplants may not be suited for animal-to-human grafts.
The hearts were taken from pigs genetically modified with knockouts of four porcine genes to prevent rejection – including a gene for a growth hormone that would otherwise cause the heart to continue to expand in the recipient’s chest – and with the addition of six human transgenes encoding for expression of proteins regulating biologic pathways that might be disrupted by incompatibilities across species.
Vietnam veteran
The organ recipients were recently deceased patients who had expressed the clear wish to be organ donors but whose organs were for clinical reasons unsuitable for transplant.
The first recipient was Lawrence Kelly, a Vietnam War veteran and welder who died from heart failure at the age of 72.
“He was an organ donor, and would be so happy to know how much his contribution to this research will help people like him with this heart disease. He was a hero his whole life, and he went out a hero,” said Alice Michael, Mr. Kelly’s partner of 33 years, who also spoke at the briefing.
“It was, I think, one of the most incredible things to see a pig heart pounding away and beating inside the chest of a human being,” said Robert A. Montgomery, MD, DPhil, director of the NYU Transplant Institute, and himself a heart transplant recipient.
Dr. Fishman said he had no relevant conflicts of interest.
This article was updated on 7/12/22 and 7/14/22.
A team of surgeons successfully transplanted genetically engineered pig hearts into two recently deceased people whose bodies were being maintained on ventilatory support – not in the hope of restoring life, but as a proof-of-concept experiment in xenotransplantation that could eventually help to ease the critical shortage of donor organs.
The surgeries were performed on June 16 and July 6, 2022, using porcine hearts from animals genetically engineered to prevent organ rejection and promote adaptive immunity by human recipients
without utilizing unapproved devices or techniques or medications,” said Nader Moazami, MD, surgical director of heart transplantation and chief of the division of heart and lung transplantation and mechanical circulatory support at NYU Langone Health, New York.

Through 72 hours of postoperative monitoring “we evaluated the heart for functionality and the heart function was completely normal with excellent contractility,” he said at a press briefing announcing early results of the experimental program.
He acknowledged that for the first of the two procedures some surgical modification of the pig heart was required, primarily because of size differences between the donor and recipient.
“Nevertheless, we learned a tremendous amount from the first operation, and when that experience was translated into the second operation it even performed better,” he said.
Alex Reyentovich, MD, medical director of heart transplantation and director of the NYU Langone advanced heart failure program noted that “there are 6 million individuals with heart failure in the United States. About 100,000 of those individuals have end-stage heart failure, and we only do about 3,500 heart transplants a year in the United States, so we have a tremendous deficiency in organs, and there are many people dying waiting for a heart.”
Infection protocols
To date there has been only one xenotransplant of a genetically modified pig heart into a living human recipient, David Bennett Sr., age 57. The surgery, performed at the University of Maryland in January 2022, was initially successful, with the patient able to sit up in bed a few days after the procedure, and the heart performing like a “rock star” according to transplant surgeon Bartley Griffith, MD.
However, Mr. Bennett died 2 months after the procedure from compromise of the organ by an as yet undetermined cause, of which one may have been the heart's infection by porcine cytomegalovirus (CMV).

The NYU team, mindful of this potential setback, used more sensitive assays to screen the donor organs for porcine CMV, and implemented protocols to prevent and to monitor for potential zoonotic transmission of porcine endogenous retrovirus.
The procedure used a dedicated operating room and equipment that will not be used for clinical procedures, the team emphasized.
An organ transplant specialist who was not involved in the study commented that there can be unwelcome surprises even with the most rigorous infection prophylaxis protocols.
“I think these are important steps, but they don’t resolve the question of infectious risk. Sometimes viruses or latent infections are only manifested later,” said Jay A. Fishman, MD, associate director of the Massachusetts General Hospital Transplant Center and director of the transplant infectious diseases and compromised host program at the hospital, which is in Boston.
“I think these are important steps, but as you may recall from the Maryland heart transplant experience, when porcine cytomegalovirus was activated, it was a long way into that patient’s course, and so we just don’t know whether something would have been reactivated later,” he said in an interview.
Dr. Fishman noted that experience with xenotransplantation at the University of Maryland and other centers has suggested that immunosuppressive regimens used for human-to-human transplants may not be suited for animal-to-human grafts.
The hearts were taken from pigs genetically modified with knockouts of four porcine genes to prevent rejection – including a gene for a growth hormone that would otherwise cause the heart to continue to expand in the recipient’s chest – and with the addition of six human transgenes encoding for expression of proteins regulating biologic pathways that might be disrupted by incompatibilities across species.
Vietnam veteran
The organ recipients were recently deceased patients who had expressed the clear wish to be organ donors but whose organs were for clinical reasons unsuitable for transplant.
The first recipient was Lawrence Kelly, a Vietnam War veteran and welder who died from heart failure at the age of 72.
“He was an organ donor, and would be so happy to know how much his contribution to this research will help people like him with this heart disease. He was a hero his whole life, and he went out a hero,” said Alice Michael, Mr. Kelly’s partner of 33 years, who also spoke at the briefing.
“It was, I think, one of the most incredible things to see a pig heart pounding away and beating inside the chest of a human being,” said Robert A. Montgomery, MD, DPhil, director of the NYU Transplant Institute, and himself a heart transplant recipient.
Dr. Fishman said he had no relevant conflicts of interest.
This article was updated on 7/12/22 and 7/14/22.
A team of surgeons successfully transplanted genetically engineered pig hearts into two recently deceased people whose bodies were being maintained on ventilatory support – not in the hope of restoring life, but as a proof-of-concept experiment in xenotransplantation that could eventually help to ease the critical shortage of donor organs.
The surgeries were performed on June 16 and July 6, 2022, using porcine hearts from animals genetically engineered to prevent organ rejection and promote adaptive immunity by human recipients
without utilizing unapproved devices or techniques or medications,” said Nader Moazami, MD, surgical director of heart transplantation and chief of the division of heart and lung transplantation and mechanical circulatory support at NYU Langone Health, New York.

Through 72 hours of postoperative monitoring “we evaluated the heart for functionality and the heart function was completely normal with excellent contractility,” he said at a press briefing announcing early results of the experimental program.
He acknowledged that for the first of the two procedures some surgical modification of the pig heart was required, primarily because of size differences between the donor and recipient.
“Nevertheless, we learned a tremendous amount from the first operation, and when that experience was translated into the second operation it even performed better,” he said.
Alex Reyentovich, MD, medical director of heart transplantation and director of the NYU Langone advanced heart failure program noted that “there are 6 million individuals with heart failure in the United States. About 100,000 of those individuals have end-stage heart failure, and we only do about 3,500 heart transplants a year in the United States, so we have a tremendous deficiency in organs, and there are many people dying waiting for a heart.”
Infection protocols
To date there has been only one xenotransplant of a genetically modified pig heart into a living human recipient, David Bennett Sr., age 57. The surgery, performed at the University of Maryland in January 2022, was initially successful, with the patient able to sit up in bed a few days after the procedure, and the heart performing like a “rock star” according to transplant surgeon Bartley Griffith, MD.
However, Mr. Bennett died 2 months after the procedure from compromise of the organ by an as yet undetermined cause, of which one may have been the heart's infection by porcine cytomegalovirus (CMV).

The NYU team, mindful of this potential setback, used more sensitive assays to screen the donor organs for porcine CMV, and implemented protocols to prevent and to monitor for potential zoonotic transmission of porcine endogenous retrovirus.
The procedure used a dedicated operating room and equipment that will not be used for clinical procedures, the team emphasized.
An organ transplant specialist who was not involved in the study commented that there can be unwelcome surprises even with the most rigorous infection prophylaxis protocols.
“I think these are important steps, but they don’t resolve the question of infectious risk. Sometimes viruses or latent infections are only manifested later,” said Jay A. Fishman, MD, associate director of the Massachusetts General Hospital Transplant Center and director of the transplant infectious diseases and compromised host program at the hospital, which is in Boston.
“I think these are important steps, but as you may recall from the Maryland heart transplant experience, when porcine cytomegalovirus was activated, it was a long way into that patient’s course, and so we just don’t know whether something would have been reactivated later,” he said in an interview.
Dr. Fishman noted that experience with xenotransplantation at the University of Maryland and other centers has suggested that immunosuppressive regimens used for human-to-human transplants may not be suited for animal-to-human grafts.
The hearts were taken from pigs genetically modified with knockouts of four porcine genes to prevent rejection – including a gene for a growth hormone that would otherwise cause the heart to continue to expand in the recipient’s chest – and with the addition of six human transgenes encoding for expression of proteins regulating biologic pathways that might be disrupted by incompatibilities across species.
Vietnam veteran
The organ recipients were recently deceased patients who had expressed the clear wish to be organ donors but whose organs were for clinical reasons unsuitable for transplant.
The first recipient was Lawrence Kelly, a Vietnam War veteran and welder who died from heart failure at the age of 72.
“He was an organ donor, and would be so happy to know how much his contribution to this research will help people like him with this heart disease. He was a hero his whole life, and he went out a hero,” said Alice Michael, Mr. Kelly’s partner of 33 years, who also spoke at the briefing.
“It was, I think, one of the most incredible things to see a pig heart pounding away and beating inside the chest of a human being,” said Robert A. Montgomery, MD, DPhil, director of the NYU Transplant Institute, and himself a heart transplant recipient.
Dr. Fishman said he had no relevant conflicts of interest.
This article was updated on 7/12/22 and 7/14/22.
C. diff.: How did a community hospital cut infections by 77%?
Teamwork by a wide range of professional staff, coupled with support from leadership, enabled one academic community hospital to cut its rate of hospital-onset Clostridioides difficile infections (HO-CDIs) by almost two-thirds in 1 year and by over three-quarters in 3 years, a study published in the American Journal of Infection Control reports.
C. diff. is a major health threat. According to the U.S. Centers for Disease Control and Prevention, CDIs, mainly linked with hospitals, caused an estimated 223,900 cases in hospitalized patients and 12,800 deaths in the United States in 2017.
“The interventions and outcomes of the project improved patient care by ensuring early testing, diagnosis, treatment if warranted, and proper isolation, which helped reduce C. diff. transmission to staff and other patients,” lead study author Cherith Walter, MSN, RN, a clinical nurse specialist at Emory Saint Joseph’s Hospital, Atlanta, told this news organization. “Had we not worked together as a team, we would not have had the ability to carry out such a robust project,” she added in an email.
Each HO-CDI case costs a health care system an estimated $12,313, and high rates of HO-CDIs incur fines from the Hospital-Acquired Condition Reduction Program of the Centers for Medicare & Medicaid Services (CMS), the authors write.
A diverse staff team collaborated
Emory Saint Joseph’s, a 410-bed hospital in Atlanta, had a history of being above the national CMS benchmark for HO-CDIs. To reduce these infections, comply with CMS requirements, and avoid fines, Ms. Walter and colleagues launched a quality improvement project between 2015 and 2020.
With the approval of the chief nursing officer, chief quality officer, and hospital board, researchers mobilized a diverse team of professionals: a clinical nurse specialist, a physician champion, unit nurse champions, a hospital epidemiologist, an infection preventionist, a clinical microbiologist, an antimicrobial stewardship pharmacist, and an environmental services representative.
The team investigated what caused their hospital’s HO-CDIs from 2014 through 2016 and developed appropriate, evidence-based infection prevention interventions. The integrated approach involved:
- Diagnostic stewardship, including a diarrhea decision-tree algorithm that enabled nurses to order tests of any loose or unformed stool for C. diff. during the first 3 days of admission.
- Enhanced environmental cleaning, which involved switching from sporicidal disinfectant only in isolation rooms to using a more effective Environmental Protection Agency–approved sporicidal disinfectant containing hydrogen peroxide and peracetic acid in all patient rooms for daily cleaning and after discharge. Every day, high-touch surfaces in C. diff. isolation rooms were cleaned and shared equipment was disinfected with bleach wipes. After patient discharge, staff cleaned mattresses on all sides, wiped walls with disinfectant, and used ultraviolet light.
- Antimicrobial stewardship. Formulary fluoroquinolones were removed as standalone orders and made available only through order sets with built-in clinical decision support.
- Education of staff on best practices, through emails, flyers, meetings, and training sessions. Two nurses needed to approve the appropriateness of testing specific specimens for CDI. All HO-CDIs were reviewed and findings presented at CDI team meetings.
- Accountability. Staff on the team and units received emailed notices about compliance issues and held meetings to discuss how to improve compliance.
After 1 year, HO-CDI incidence dropped 63% from baseline, from above 12 cases per 10,000 patient-days to 4.72 per 10,000 patient-days. And after 3 years, infections dropped 77% to 2.80 per 10,000 patient-days.
The hospital’s HO-CDI standardized infection ratio – the total number of infections divided by the National Healthcare Safety Network’s risk-adjusted predicted number of infections – dropped below the national benchmark, from 1.11 in 2015 to 0.43 in 2020.
The hospital also increased testing of appropriate patients for CDI within the first 3 days of admission, from 54% in 2014 to 81% in late 2019.
“By testing patients within 3 days of admission, we discovered that many had acquired C. diff. before admission,” Ms. Walter said. “I don’t think we realized how prevalent C. diff. was in the community.”
Benjamin D. Galvan, MLS(ASCP), CIC, an infection preventionist at Tampa General Hospital and a member of the Association for Professionals in Infection Control and Epidemiology, welcomed the study’s results.
“Effective collaboration within the health care setting is a highly effective way to implement and sustain evidence-based practices related to infection reduction. When buy-in is obtained from the top, and pertinent stakeholders are engaged for their expertise, we can see sustainable change and improved patient outcomes,” Mr. Galvan, who was not involved in the study, said in an email.
“The researchers did a fantastic job,” he added. “I am grateful to see this important work addressed in the literature, as it will only improve buy-in for improvement efforts aimed at reducing infections moving forward across the health care continuum.”
Douglas S. Paauw, MD, a professor of medicine and chair for patient-centered clinical education at the University of Washington School of Medicine, Seattle, said that the team’s most important interventions were changing the environmental cleaning protocol and using agents that kill C. diff. spores.
“We know that as many as 10%-20% of hospitalized patients carry C. diff. Cleaning only the rooms where you know you have C. diff. (isolation rooms) will miss most of it,” said Dr. Paauw, who was also not involved in the study. “Cleaning every room with cleaners that actually work is very important but costs money.”
Handwashing with soap and water works, alcohol hand gels do not
“We know that handwashing with soap and water is the most important way to prevent hospital C. diff. transmission,” Dr. Paauw noted. “Handwashing protocols implemented prior to the study were probably a big part of the team’s success.”
Handwashing with soap and water works but alcohol hand gels do not, he cautioned.
“C. diff. rates in hospitals went up years ago when we started putting alcohol gels outside patients’ rooms,” Dr. Paauw explained. “Now, instead of washing their hands, staff quickly pump gel before they see patients. Applying gel is easy, but gel does not eliminate C. diff. spores. Handwashing is such a simple way to fix the C. diff. problem, but doctors don’t take the time.”
“We need to take the C. diff. problem seriously. We have enough information, and we know the right things to do. We need to wash our hands. We need to clean the rooms. We need to stop cutting corners if we want to give good care,” he said.
The authors plan to conduct further related research.
The study was not funded. All study authors, as well as Mr. Galvan and Dr. Paauw, have reported no relevant financial interests.
A version of this article first appeared on Medscape.com.
Teamwork by a wide range of professional staff, coupled with support from leadership, enabled one academic community hospital to cut its rate of hospital-onset Clostridioides difficile infections (HO-CDIs) by almost two-thirds in 1 year and by over three-quarters in 3 years, a study published in the American Journal of Infection Control reports.
C. diff. is a major health threat. According to the U.S. Centers for Disease Control and Prevention, CDIs, mainly linked with hospitals, caused an estimated 223,900 cases in hospitalized patients and 12,800 deaths in the United States in 2017.
“The interventions and outcomes of the project improved patient care by ensuring early testing, diagnosis, treatment if warranted, and proper isolation, which helped reduce C. diff. transmission to staff and other patients,” lead study author Cherith Walter, MSN, RN, a clinical nurse specialist at Emory Saint Joseph’s Hospital, Atlanta, told this news organization. “Had we not worked together as a team, we would not have had the ability to carry out such a robust project,” she added in an email.
Each HO-CDI case costs a health care system an estimated $12,313, and high rates of HO-CDIs incur fines from the Hospital-Acquired Condition Reduction Program of the Centers for Medicare & Medicaid Services (CMS), the authors write.
A diverse staff team collaborated
Emory Saint Joseph’s, a 410-bed hospital in Atlanta, had a history of being above the national CMS benchmark for HO-CDIs. To reduce these infections, comply with CMS requirements, and avoid fines, Ms. Walter and colleagues launched a quality improvement project between 2015 and 2020.
With the approval of the chief nursing officer, chief quality officer, and hospital board, researchers mobilized a diverse team of professionals: a clinical nurse specialist, a physician champion, unit nurse champions, a hospital epidemiologist, an infection preventionist, a clinical microbiologist, an antimicrobial stewardship pharmacist, and an environmental services representative.
The team investigated what caused their hospital’s HO-CDIs from 2014 through 2016 and developed appropriate, evidence-based infection prevention interventions. The integrated approach involved:
- Diagnostic stewardship, including a diarrhea decision-tree algorithm that enabled nurses to order tests of any loose or unformed stool for C. diff. during the first 3 days of admission.
- Enhanced environmental cleaning, which involved switching from sporicidal disinfectant only in isolation rooms to using a more effective Environmental Protection Agency–approved sporicidal disinfectant containing hydrogen peroxide and peracetic acid in all patient rooms for daily cleaning and after discharge. Every day, high-touch surfaces in C. diff. isolation rooms were cleaned and shared equipment was disinfected with bleach wipes. After patient discharge, staff cleaned mattresses on all sides, wiped walls with disinfectant, and used ultraviolet light.
- Antimicrobial stewardship. Formulary fluoroquinolones were removed as standalone orders and made available only through order sets with built-in clinical decision support.
- Education of staff on best practices, through emails, flyers, meetings, and training sessions. Two nurses needed to approve the appropriateness of testing specific specimens for CDI. All HO-CDIs were reviewed and findings presented at CDI team meetings.
- Accountability. Staff on the team and units received emailed notices about compliance issues and held meetings to discuss how to improve compliance.
After 1 year, HO-CDI incidence dropped 63% from baseline, from above 12 cases per 10,000 patient-days to 4.72 per 10,000 patient-days. And after 3 years, infections dropped 77% to 2.80 per 10,000 patient-days.
The hospital’s HO-CDI standardized infection ratio – the total number of infections divided by the National Healthcare Safety Network’s risk-adjusted predicted number of infections – dropped below the national benchmark, from 1.11 in 2015 to 0.43 in 2020.
The hospital also increased testing of appropriate patients for CDI within the first 3 days of admission, from 54% in 2014 to 81% in late 2019.
“By testing patients within 3 days of admission, we discovered that many had acquired C. diff. before admission,” Ms. Walter said. “I don’t think we realized how prevalent C. diff. was in the community.”
Benjamin D. Galvan, MLS(ASCP), CIC, an infection preventionist at Tampa General Hospital and a member of the Association for Professionals in Infection Control and Epidemiology, welcomed the study’s results.
“Effective collaboration within the health care setting is a highly effective way to implement and sustain evidence-based practices related to infection reduction. When buy-in is obtained from the top, and pertinent stakeholders are engaged for their expertise, we can see sustainable change and improved patient outcomes,” Mr. Galvan, who was not involved in the study, said in an email.
“The researchers did a fantastic job,” he added. “I am grateful to see this important work addressed in the literature, as it will only improve buy-in for improvement efforts aimed at reducing infections moving forward across the health care continuum.”
Douglas S. Paauw, MD, a professor of medicine and chair for patient-centered clinical education at the University of Washington School of Medicine, Seattle, said that the team’s most important interventions were changing the environmental cleaning protocol and using agents that kill C. diff. spores.
“We know that as many as 10%-20% of hospitalized patients carry C. diff. Cleaning only the rooms where you know you have C. diff. (isolation rooms) will miss most of it,” said Dr. Paauw, who was also not involved in the study. “Cleaning every room with cleaners that actually work is very important but costs money.”
Handwashing with soap and water works, alcohol hand gels do not
“We know that handwashing with soap and water is the most important way to prevent hospital C. diff. transmission,” Dr. Paauw noted. “Handwashing protocols implemented prior to the study were probably a big part of the team’s success.”
Handwashing with soap and water works but alcohol hand gels do not, he cautioned.
“C. diff. rates in hospitals went up years ago when we started putting alcohol gels outside patients’ rooms,” Dr. Paauw explained. “Now, instead of washing their hands, staff quickly pump gel before they see patients. Applying gel is easy, but gel does not eliminate C. diff. spores. Handwashing is such a simple way to fix the C. diff. problem, but doctors don’t take the time.”
“We need to take the C. diff. problem seriously. We have enough information, and we know the right things to do. We need to wash our hands. We need to clean the rooms. We need to stop cutting corners if we want to give good care,” he said.
The authors plan to conduct further related research.
The study was not funded. All study authors, as well as Mr. Galvan and Dr. Paauw, have reported no relevant financial interests.
A version of this article first appeared on Medscape.com.
Teamwork by a wide range of professional staff, coupled with support from leadership, enabled one academic community hospital to cut its rate of hospital-onset Clostridioides difficile infections (HO-CDIs) by almost two-thirds in 1 year and by over three-quarters in 3 years, a study published in the American Journal of Infection Control reports.
C. diff. is a major health threat. According to the U.S. Centers for Disease Control and Prevention, CDIs, mainly linked with hospitals, caused an estimated 223,900 cases in hospitalized patients and 12,800 deaths in the United States in 2017.
“The interventions and outcomes of the project improved patient care by ensuring early testing, diagnosis, treatment if warranted, and proper isolation, which helped reduce C. diff. transmission to staff and other patients,” lead study author Cherith Walter, MSN, RN, a clinical nurse specialist at Emory Saint Joseph’s Hospital, Atlanta, told this news organization. “Had we not worked together as a team, we would not have had the ability to carry out such a robust project,” she added in an email.
Each HO-CDI case costs a health care system an estimated $12,313, and high rates of HO-CDIs incur fines from the Hospital-Acquired Condition Reduction Program of the Centers for Medicare & Medicaid Services (CMS), the authors write.
A diverse staff team collaborated
Emory Saint Joseph’s, a 410-bed hospital in Atlanta, had a history of being above the national CMS benchmark for HO-CDIs. To reduce these infections, comply with CMS requirements, and avoid fines, Ms. Walter and colleagues launched a quality improvement project between 2015 and 2020.
With the approval of the chief nursing officer, chief quality officer, and hospital board, researchers mobilized a diverse team of professionals: a clinical nurse specialist, a physician champion, unit nurse champions, a hospital epidemiologist, an infection preventionist, a clinical microbiologist, an antimicrobial stewardship pharmacist, and an environmental services representative.
The team investigated what caused their hospital’s HO-CDIs from 2014 through 2016 and developed appropriate, evidence-based infection prevention interventions. The integrated approach involved:
- Diagnostic stewardship, including a diarrhea decision-tree algorithm that enabled nurses to order tests of any loose or unformed stool for C. diff. during the first 3 days of admission.
- Enhanced environmental cleaning, which involved switching from sporicidal disinfectant only in isolation rooms to using a more effective Environmental Protection Agency–approved sporicidal disinfectant containing hydrogen peroxide and peracetic acid in all patient rooms for daily cleaning and after discharge. Every day, high-touch surfaces in C. diff. isolation rooms were cleaned and shared equipment was disinfected with bleach wipes. After patient discharge, staff cleaned mattresses on all sides, wiped walls with disinfectant, and used ultraviolet light.
- Antimicrobial stewardship. Formulary fluoroquinolones were removed as standalone orders and made available only through order sets with built-in clinical decision support.
- Education of staff on best practices, through emails, flyers, meetings, and training sessions. Two nurses needed to approve the appropriateness of testing specific specimens for CDI. All HO-CDIs were reviewed and findings presented at CDI team meetings.
- Accountability. Staff on the team and units received emailed notices about compliance issues and held meetings to discuss how to improve compliance.
After 1 year, HO-CDI incidence dropped 63% from baseline, from above 12 cases per 10,000 patient-days to 4.72 per 10,000 patient-days. And after 3 years, infections dropped 77% to 2.80 per 10,000 patient-days.
The hospital’s HO-CDI standardized infection ratio – the total number of infections divided by the National Healthcare Safety Network’s risk-adjusted predicted number of infections – dropped below the national benchmark, from 1.11 in 2015 to 0.43 in 2020.
The hospital also increased testing of appropriate patients for CDI within the first 3 days of admission, from 54% in 2014 to 81% in late 2019.
“By testing patients within 3 days of admission, we discovered that many had acquired C. diff. before admission,” Ms. Walter said. “I don’t think we realized how prevalent C. diff. was in the community.”
Benjamin D. Galvan, MLS(ASCP), CIC, an infection preventionist at Tampa General Hospital and a member of the Association for Professionals in Infection Control and Epidemiology, welcomed the study’s results.
“Effective collaboration within the health care setting is a highly effective way to implement and sustain evidence-based practices related to infection reduction. When buy-in is obtained from the top, and pertinent stakeholders are engaged for their expertise, we can see sustainable change and improved patient outcomes,” Mr. Galvan, who was not involved in the study, said in an email.
“The researchers did a fantastic job,” he added. “I am grateful to see this important work addressed in the literature, as it will only improve buy-in for improvement efforts aimed at reducing infections moving forward across the health care continuum.”
Douglas S. Paauw, MD, a professor of medicine and chair for patient-centered clinical education at the University of Washington School of Medicine, Seattle, said that the team’s most important interventions were changing the environmental cleaning protocol and using agents that kill C. diff. spores.
“We know that as many as 10%-20% of hospitalized patients carry C. diff. Cleaning only the rooms where you know you have C. diff. (isolation rooms) will miss most of it,” said Dr. Paauw, who was also not involved in the study. “Cleaning every room with cleaners that actually work is very important but costs money.”
Handwashing with soap and water works, alcohol hand gels do not
“We know that handwashing with soap and water is the most important way to prevent hospital C. diff. transmission,” Dr. Paauw noted. “Handwashing protocols implemented prior to the study were probably a big part of the team’s success.”
Handwashing with soap and water works but alcohol hand gels do not, he cautioned.
“C. diff. rates in hospitals went up years ago when we started putting alcohol gels outside patients’ rooms,” Dr. Paauw explained. “Now, instead of washing their hands, staff quickly pump gel before they see patients. Applying gel is easy, but gel does not eliminate C. diff. spores. Handwashing is such a simple way to fix the C. diff. problem, but doctors don’t take the time.”
“We need to take the C. diff. problem seriously. We have enough information, and we know the right things to do. We need to wash our hands. We need to clean the rooms. We need to stop cutting corners if we want to give good care,” he said.
The authors plan to conduct further related research.
The study was not funded. All study authors, as well as Mr. Galvan and Dr. Paauw, have reported no relevant financial interests.
A version of this article first appeared on Medscape.com.