User login
AACN releases updated resource on VTE

caring for a patient in
an intensive care unit
The American Association of Critical-Care Nurses (AACN) has released updated resources aimed at helping nurses prevent serious complications facing critically ill patients.
The resources, or “practice alerts,” address venous thromboembolism (VTE), delirium, and catheter-associated urinary tract infections (CAUTIs).
Each alert outlines the scope of the problem, summarizes the expected nursing practice, and provides supporting evidence and research.
These documents are available on the AACN website.
The VTE practice alert, “Preventing Venous Thromboembolism in Adults,” notes that VTE affects approximately 900,000 adult patients in the US annually and results in an estimated 300,000 deaths. Furthermore, VTE prevalence is predicted to more than double in the next 35 years.
The document also reviews risk factors for VTE and methods of VTE prophylaxis, including medications and compression devices.
The CAUTI practice alert, “Prevention of Catheter-Associated Urinary Tract Infections in Adults,” notes that urinary tract infections are the most common healthcare-associated infection, and prolonged indwelling catheterization is the major risk factor for CAUTIs.
The document outlines preliminary and ongoing assessment, documentation, and adherence to infection control protocols.
The delirium practice alert, “Assessment and Management of Delirium Across the Life Span,” states that delirium affects up to 80% of critically ill patients in the US, with associated annual costs between $4 billion and $16 billion.
The document reviews risk factors for pediatric and adult patients and the use of validated tools to assess for delirium.
According to AACN, each practice alert is supported by authoritative evidence and seeks to ensure excellence in practice along with promotion of a safe and humane work environment.
Topics address both nursing and interprofessional activities of importance for patients in acute and critical care environments. Some alerts include additional resources for staff education and performance-improvement activities. ![]()

caring for a patient in
an intensive care unit
The American Association of Critical-Care Nurses (AACN) has released updated resources aimed at helping nurses prevent serious complications facing critically ill patients.
The resources, or “practice alerts,” address venous thromboembolism (VTE), delirium, and catheter-associated urinary tract infections (CAUTIs).
Each alert outlines the scope of the problem, summarizes the expected nursing practice, and provides supporting evidence and research.
These documents are available on the AACN website.
The VTE practice alert, “Preventing Venous Thromboembolism in Adults,” notes that VTE affects approximately 900,000 adult patients in the US annually and results in an estimated 300,000 deaths. Furthermore, VTE prevalence is predicted to more than double in the next 35 years.
The document also reviews risk factors for VTE and methods of VTE prophylaxis, including medications and compression devices.
The CAUTI practice alert, “Prevention of Catheter-Associated Urinary Tract Infections in Adults,” notes that urinary tract infections are the most common healthcare-associated infection, and prolonged indwelling catheterization is the major risk factor for CAUTIs.
The document outlines preliminary and ongoing assessment, documentation, and adherence to infection control protocols.
The delirium practice alert, “Assessment and Management of Delirium Across the Life Span,” states that delirium affects up to 80% of critically ill patients in the US, with associated annual costs between $4 billion and $16 billion.
The document reviews risk factors for pediatric and adult patients and the use of validated tools to assess for delirium.
According to AACN, each practice alert is supported by authoritative evidence and seeks to ensure excellence in practice along with promotion of a safe and humane work environment.
Topics address both nursing and interprofessional activities of importance for patients in acute and critical care environments. Some alerts include additional resources for staff education and performance-improvement activities. ![]()

caring for a patient in
an intensive care unit
The American Association of Critical-Care Nurses (AACN) has released updated resources aimed at helping nurses prevent serious complications facing critically ill patients.
The resources, or “practice alerts,” address venous thromboembolism (VTE), delirium, and catheter-associated urinary tract infections (CAUTIs).
Each alert outlines the scope of the problem, summarizes the expected nursing practice, and provides supporting evidence and research.
These documents are available on the AACN website.
The VTE practice alert, “Preventing Venous Thromboembolism in Adults,” notes that VTE affects approximately 900,000 adult patients in the US annually and results in an estimated 300,000 deaths. Furthermore, VTE prevalence is predicted to more than double in the next 35 years.
The document also reviews risk factors for VTE and methods of VTE prophylaxis, including medications and compression devices.
The CAUTI practice alert, “Prevention of Catheter-Associated Urinary Tract Infections in Adults,” notes that urinary tract infections are the most common healthcare-associated infection, and prolonged indwelling catheterization is the major risk factor for CAUTIs.
The document outlines preliminary and ongoing assessment, documentation, and adherence to infection control protocols.
The delirium practice alert, “Assessment and Management of Delirium Across the Life Span,” states that delirium affects up to 80% of critically ill patients in the US, with associated annual costs between $4 billion and $16 billion.
The document reviews risk factors for pediatric and adult patients and the use of validated tools to assess for delirium.
According to AACN, each practice alert is supported by authoritative evidence and seeks to ensure excellence in practice along with promotion of a safe and humane work environment.
Topics address both nursing and interprofessional activities of importance for patients in acute and critical care environments. Some alerts include additional resources for staff education and performance-improvement activities. ![]()
NCCN issues challenge to ‘bag’ vincristine
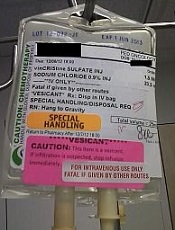
Photo courtesy of ISMP
PHILADELPHIA—To ensure proper administration of vincristine, the National Comprehensive Cancer Network (NCCN) has issued a challenge to hospitals, medical centers, and oncology practices as part of its “Just Bag It!” campaign.
Vincristine—the “O” for Oncovin in the CHOP regimen—is widely used to treat patients with leukemia or lymphoma.
It is considered an important chemotherapeutic agent. However, if administered incorrectly, vincristine is uniformly fatal, usually within a week, according to the NCCN.
Vincristine is highly neurotoxic and should always be administered intravenously. If it is mistakenly given intrathecally along with other chemotherapy drugs, it causes ascending paralysis, neurological defects, and death.
Therefore, the NCCN recommends always diluting and administering vincristine in a mini IV-drip bag, never through a syringe.
This precaution decreases the chances of improper dosage and makes it impossible to accidentally administer vincristine into the spinal fluid.
The NCCN initiated the safe-handling campaign in response to the death 11 years ago of a 21-year-old patient who received vincristine incorrectly administered into his spinal fluid. He was referred to Robert W. Carlson, MD, NCCN’s chief executive officer, who, at the time, was at Stanford Hospital, not the hospital where the error occurred.
The patient, Christopher Wibeto, had a “likely curable” non-Hodgkin lymphoma and died 4 days later.
“When I first met Christopher, he was doing well,” Dr Carlson said. “He was a delightful young gentleman, very articulate. He was funny. Even in the ICU, he had me chuckling and laughing at what he was saying.”
“But we knew that the medical error would almost certainly lead to his death. Shortly thereafter, I met his parents, Debra and Robin, . . . and had to tell them what the consequences of that medical error were likely to be. And they joined me in Christopher’s room while we talked with him about what the consequences of that medical error were likely to be.”
Making the situation even more painful, Dr Carlson, at that time, was the father of a young son who is now almost the age Christopher was then.
Dr Carlson said he realized that “we needed to come up with systems to assure that this did not happen, not today or tomorrow or ever again.”
Motivated by the tragedy, Dr Carlson spearheaded a national effort to address this mistake when he joined NCCN as CEO, enlisting the help of NCCN’s Best Practices Committee.
The NCCN developed and issued guidelines, and all 27 member institutions have adopted policies in line with the guidelines.
The Institute for Safe Medication Practices (ISMP) has undertaken efforts over more than a decade to implement procedures for safe vincristine administration.
ISMP conducted surveys and follow-up self-assessments regarding use of IV bags for vincristine at oncology practice sites. They found that only about half the institutions surveyed dilute IV vincristine for administration in a small-volume bag.
Some practitioners associate the use of an IV bag with an increased risk of extravasation (when the chemotherapy agent leaks into the tissue surrounding the administration site). Research shows, however, that the risk of extravasation is extremely low (less than 0.5%), regardless of how vincristine is administered.
And cost is not an issue when implementing the mini-bag policy, according to the president of ISMP, Michael R. Cohen, RPh.
“It cost a few pennies more,” he said. “And I mean pennies. I think probably what is an issue is just the age-old habit of putting vincristine in a syringe and being able to change that habit.”
Since the introduction of vincristine use in the 1960s, 125 documented cases of accidental death in the US and abroad have been reported. While the error is relatively rare, it is preventable and unique in its level of mortality.
“It’s hard to understand why this idea of ‘Just Bag It’ hasn’t permeated healthcare at this point,” Cohen said. “Because it is a sure-fire way to prevent this type of error.”
The ISMP, the Joint Commission, the World Health Organization, and the Oncology Nursing Society also recommend the bag-it policy. ![]()
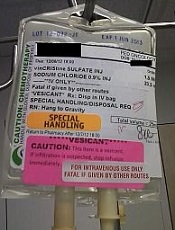
Photo courtesy of ISMP
PHILADELPHIA—To ensure proper administration of vincristine, the National Comprehensive Cancer Network (NCCN) has issued a challenge to hospitals, medical centers, and oncology practices as part of its “Just Bag It!” campaign.
Vincristine—the “O” for Oncovin in the CHOP regimen—is widely used to treat patients with leukemia or lymphoma.
It is considered an important chemotherapeutic agent. However, if administered incorrectly, vincristine is uniformly fatal, usually within a week, according to the NCCN.
Vincristine is highly neurotoxic and should always be administered intravenously. If it is mistakenly given intrathecally along with other chemotherapy drugs, it causes ascending paralysis, neurological defects, and death.
Therefore, the NCCN recommends always diluting and administering vincristine in a mini IV-drip bag, never through a syringe.
This precaution decreases the chances of improper dosage and makes it impossible to accidentally administer vincristine into the spinal fluid.
The NCCN initiated the safe-handling campaign in response to the death 11 years ago of a 21-year-old patient who received vincristine incorrectly administered into his spinal fluid. He was referred to Robert W. Carlson, MD, NCCN’s chief executive officer, who, at the time, was at Stanford Hospital, not the hospital where the error occurred.
The patient, Christopher Wibeto, had a “likely curable” non-Hodgkin lymphoma and died 4 days later.
“When I first met Christopher, he was doing well,” Dr Carlson said. “He was a delightful young gentleman, very articulate. He was funny. Even in the ICU, he had me chuckling and laughing at what he was saying.”
“But we knew that the medical error would almost certainly lead to his death. Shortly thereafter, I met his parents, Debra and Robin, . . . and had to tell them what the consequences of that medical error were likely to be. And they joined me in Christopher’s room while we talked with him about what the consequences of that medical error were likely to be.”
Making the situation even more painful, Dr Carlson, at that time, was the father of a young son who is now almost the age Christopher was then.
Dr Carlson said he realized that “we needed to come up with systems to assure that this did not happen, not today or tomorrow or ever again.”
Motivated by the tragedy, Dr Carlson spearheaded a national effort to address this mistake when he joined NCCN as CEO, enlisting the help of NCCN’s Best Practices Committee.
The NCCN developed and issued guidelines, and all 27 member institutions have adopted policies in line with the guidelines.
The Institute for Safe Medication Practices (ISMP) has undertaken efforts over more than a decade to implement procedures for safe vincristine administration.
ISMP conducted surveys and follow-up self-assessments regarding use of IV bags for vincristine at oncology practice sites. They found that only about half the institutions surveyed dilute IV vincristine for administration in a small-volume bag.
Some practitioners associate the use of an IV bag with an increased risk of extravasation (when the chemotherapy agent leaks into the tissue surrounding the administration site). Research shows, however, that the risk of extravasation is extremely low (less than 0.5%), regardless of how vincristine is administered.
And cost is not an issue when implementing the mini-bag policy, according to the president of ISMP, Michael R. Cohen, RPh.
“It cost a few pennies more,” he said. “And I mean pennies. I think probably what is an issue is just the age-old habit of putting vincristine in a syringe and being able to change that habit.”
Since the introduction of vincristine use in the 1960s, 125 documented cases of accidental death in the US and abroad have been reported. While the error is relatively rare, it is preventable and unique in its level of mortality.
“It’s hard to understand why this idea of ‘Just Bag It’ hasn’t permeated healthcare at this point,” Cohen said. “Because it is a sure-fire way to prevent this type of error.”
The ISMP, the Joint Commission, the World Health Organization, and the Oncology Nursing Society also recommend the bag-it policy. ![]()
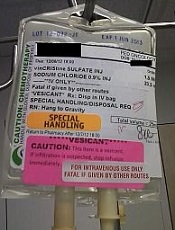
Photo courtesy of ISMP
PHILADELPHIA—To ensure proper administration of vincristine, the National Comprehensive Cancer Network (NCCN) has issued a challenge to hospitals, medical centers, and oncology practices as part of its “Just Bag It!” campaign.
Vincristine—the “O” for Oncovin in the CHOP regimen—is widely used to treat patients with leukemia or lymphoma.
It is considered an important chemotherapeutic agent. However, if administered incorrectly, vincristine is uniformly fatal, usually within a week, according to the NCCN.
Vincristine is highly neurotoxic and should always be administered intravenously. If it is mistakenly given intrathecally along with other chemotherapy drugs, it causes ascending paralysis, neurological defects, and death.
Therefore, the NCCN recommends always diluting and administering vincristine in a mini IV-drip bag, never through a syringe.
This precaution decreases the chances of improper dosage and makes it impossible to accidentally administer vincristine into the spinal fluid.
The NCCN initiated the safe-handling campaign in response to the death 11 years ago of a 21-year-old patient who received vincristine incorrectly administered into his spinal fluid. He was referred to Robert W. Carlson, MD, NCCN’s chief executive officer, who, at the time, was at Stanford Hospital, not the hospital where the error occurred.
The patient, Christopher Wibeto, had a “likely curable” non-Hodgkin lymphoma and died 4 days later.
“When I first met Christopher, he was doing well,” Dr Carlson said. “He was a delightful young gentleman, very articulate. He was funny. Even in the ICU, he had me chuckling and laughing at what he was saying.”
“But we knew that the medical error would almost certainly lead to his death. Shortly thereafter, I met his parents, Debra and Robin, . . . and had to tell them what the consequences of that medical error were likely to be. And they joined me in Christopher’s room while we talked with him about what the consequences of that medical error were likely to be.”
Making the situation even more painful, Dr Carlson, at that time, was the father of a young son who is now almost the age Christopher was then.
Dr Carlson said he realized that “we needed to come up with systems to assure that this did not happen, not today or tomorrow or ever again.”
Motivated by the tragedy, Dr Carlson spearheaded a national effort to address this mistake when he joined NCCN as CEO, enlisting the help of NCCN’s Best Practices Committee.
The NCCN developed and issued guidelines, and all 27 member institutions have adopted policies in line with the guidelines.
The Institute for Safe Medication Practices (ISMP) has undertaken efforts over more than a decade to implement procedures for safe vincristine administration.
ISMP conducted surveys and follow-up self-assessments regarding use of IV bags for vincristine at oncology practice sites. They found that only about half the institutions surveyed dilute IV vincristine for administration in a small-volume bag.
Some practitioners associate the use of an IV bag with an increased risk of extravasation (when the chemotherapy agent leaks into the tissue surrounding the administration site). Research shows, however, that the risk of extravasation is extremely low (less than 0.5%), regardless of how vincristine is administered.
And cost is not an issue when implementing the mini-bag policy, according to the president of ISMP, Michael R. Cohen, RPh.
“It cost a few pennies more,” he said. “And I mean pennies. I think probably what is an issue is just the age-old habit of putting vincristine in a syringe and being able to change that habit.”
Since the introduction of vincristine use in the 1960s, 125 documented cases of accidental death in the US and abroad have been reported. While the error is relatively rare, it is preventable and unique in its level of mortality.
“It’s hard to understand why this idea of ‘Just Bag It’ hasn’t permeated healthcare at this point,” Cohen said. “Because it is a sure-fire way to prevent this type of error.”
The ISMP, the Joint Commission, the World Health Organization, and the Oncology Nursing Society also recommend the bag-it policy. ![]()
Supportive care isn’t palliative care, speaker says

Photo courtesy of NCI
NEW YORK—Two presentations at the NCCN 11th Annual Congress: Hematologic Malignancies addressed the importance of supportive care in the treatment of patients with T-cell lymphomas and multiple myeloma.
Erin Kopp, ACNP-BC, of City of Hope Comprehensive Cancer Center in Duarte, California, reminded the audience that supportive care is not palliative care.
Supportive care “complements critical care so that the patient doesn’t have to stop treatment,” she said.
Kopp focused primarily on cutaneous T-cell lymphoma (CTCL) in her presentation, with some recommendations for managing tumor lysis syndrome in patients undergoing therapy for peripheral T-cell lymphoma (PTCL).
And Kathleen Colson, RN, of the Dana-Farber Cancer Institute in Boston, Massachusetts, discussed supportive care for patients with multiple myeloma (MM).
T-cell lymphomas
Most T-cell lymphoma patients will require multiple treatment regimens over their lifetimes, Kopp said. And each type of therapy brings different treatment-related toxicities, which in turn require distinct supportive care measures to manage them.
Topical steroids, for example, may cause skin-thinning, stretch marks, skin irritation, and may be absorbed systemically when a high-potency formulation is used. So the lowest potency steroid that provides the maximum efficacy should be utilized. Practitioners should assess systemic effects if high-potency steroids are utilized.
Topical nitrogen mustard can darken the skin, which often occurs as the lesions resolve, Kopp said. She cautioned that patients experiencing hyperpigmentation often stop treatment without telling their physicians.
So Kopp recommends appropriate patient education to go along with the treatment. With nitrogen mustard, this includes applying a thin layer only to the affected areas and refrigerating the topical ointment to increase soothing.
Topical retinoids may cause redness, itching, warmth, swelling, burning, scaling or other irritation. They also increase the patients’ sensitivity to light. Kopp indicated that for the first week, topical retinoids should be applied once every other day and then titrated as tolerated.
Phototherapy with PUVA or narrowband-UVB may also cause itching, in addition to skin burn, nausea, and other side effects.
“Do not underestimate emollients,” Kopp said, for relief of pruritus. And skin baths with bleach significantly decrease infections that may result from treatment.
Systemic therapy with retinoids, interferon, cytotoxic agents, monoclonal antibodies, and HDAC inhibitors may also cause distinct reactions. For example, the retinoid bexarotene may cause primary hypothyroidism and major lipid abnormalities. Therefore, TSH, free T4, and triglycerides should be monitored every 8 weeks.
Cytotoxic agents such as pralatrexate and methotrexate significantly increase the risk for infection.
Monoclonal antibodies can reactivate previous viral infection, induce tumor lysis syndrome (TLS), and cause progressive multifocal leukoencephalopathy.
HDAC inhibitors such as vorinostat and romidepsin may cause QT prolongation and myelosuppression, among other side effects.
Practitioners need to assess symptoms and side effects thoroughly and often and provide options for supportive care management.
PTCL is an under recognized risk for TLS, Kopp said.
“It should be addressed aggressively,” she added, with monitoring and correction of electrolyte imbalance.
Patients should be rigorously hydrated, and allopurinol should be administered 2-3 days prior to treatment and adjusted based on the patient response and uric acid level.
Multiple myeloma
Colson described supportive care as “keeping all the pieces together.” MM itself can result in a broad spectrum of clinical manifestations, including renal compromise, neuropathy, infection, hypercalcemia, bone pain, lytic lesions, and anemia.
To preserve renal health, patients should drink plenty of water and avoid certain medications, such as IV contrast and nonsteroidal anti-inflammatory drugs.
Peripheral neuropathy can be a side effect of treatment or be caused by the disease itself. Bortezomib-related neuropathy can be reduced with weekly instead of twice weekly dosing and with subcutaneous administration.
Duration of higher doses of thalidomide treatment also impacts neuropathy. Carfilzomib and pomalidomide have a lower incidence of neuropathy.
Myeloma patients have a 15-fold increased risk of recurrent infection because white blood cell production is decreased and the normal immune role of plasma cells is lost.
Supportive therapy includes antibiotics and IVIG therapy. In addition, Colson said pneumonia and influenza vaccines should be considered, as well as prophylaxis for Pneumocystis carinii, herpes zoster, and fungal infections.
Hypercalcemia results from increased bone deterioration. Symptoms include loss of appetite, fatigue, vomiting, muscle weakness, confusion, constipation, increased thirst, and increased urine output. Supportive measures are adequate hydration, furosemide, bisphosphonates, and steroids.
Supportive therapy for bone pain includes bisphosphonates, radiation, pain medication, kyphoplasty, and vertebroplasty. Bisphosphonates, such as pamidronate and zoledronic acid, inhibit bone destruction and are recommended for all myeloma patients with bone disease. However, patients should be monitored for renal dysfunction and osteonecrosis of the jaw when taking bisphosphonates.
And Colson advises, “Hold bisphosphonate therapy if the patient needs a root canal or extraction.” Additionally, dental implants are not recommended for MM patients.
Anemia is another common presenting symptom of myeloma and may also be a result of decreased kidney function. Colson said the use of red blood cell supplements may be used with caution to ameliorate the symptom. Red blood cell transfusion may be considered and a reduction in the medication dose may be required.
MM is a hypercoagulable disease, and measures should be taken to avoid deep vein thrombosis (DVT) and pulmonary embolism (PE). Patients should wear anti-embolism stockings, exercise regularly, take low-dose aspirin, and move about frequently instead of sitting for long periods. Immunomodulatory medications may be adjusted to reduce the risk of a blot clot forming.
Infusion-related reactions are also a risk of therapy, and symptoms of a reaction need to be managed immediately and appropriately, with antihistamines, corticosteroids, interruption of the infusion, slowing of the infusion rate after symptom resolution, and permanent discontinuation in the case of grade 4 reactions.
The potential for longer survival exists, Colson said, due to appropriate supportive care measures. ![]()

Photo courtesy of NCI
NEW YORK—Two presentations at the NCCN 11th Annual Congress: Hematologic Malignancies addressed the importance of supportive care in the treatment of patients with T-cell lymphomas and multiple myeloma.
Erin Kopp, ACNP-BC, of City of Hope Comprehensive Cancer Center in Duarte, California, reminded the audience that supportive care is not palliative care.
Supportive care “complements critical care so that the patient doesn’t have to stop treatment,” she said.
Kopp focused primarily on cutaneous T-cell lymphoma (CTCL) in her presentation, with some recommendations for managing tumor lysis syndrome in patients undergoing therapy for peripheral T-cell lymphoma (PTCL).
And Kathleen Colson, RN, of the Dana-Farber Cancer Institute in Boston, Massachusetts, discussed supportive care for patients with multiple myeloma (MM).
T-cell lymphomas
Most T-cell lymphoma patients will require multiple treatment regimens over their lifetimes, Kopp said. And each type of therapy brings different treatment-related toxicities, which in turn require distinct supportive care measures to manage them.
Topical steroids, for example, may cause skin-thinning, stretch marks, skin irritation, and may be absorbed systemically when a high-potency formulation is used. So the lowest potency steroid that provides the maximum efficacy should be utilized. Practitioners should assess systemic effects if high-potency steroids are utilized.
Topical nitrogen mustard can darken the skin, which often occurs as the lesions resolve, Kopp said. She cautioned that patients experiencing hyperpigmentation often stop treatment without telling their physicians.
So Kopp recommends appropriate patient education to go along with the treatment. With nitrogen mustard, this includes applying a thin layer only to the affected areas and refrigerating the topical ointment to increase soothing.
Topical retinoids may cause redness, itching, warmth, swelling, burning, scaling or other irritation. They also increase the patients’ sensitivity to light. Kopp indicated that for the first week, topical retinoids should be applied once every other day and then titrated as tolerated.
Phototherapy with PUVA or narrowband-UVB may also cause itching, in addition to skin burn, nausea, and other side effects.
“Do not underestimate emollients,” Kopp said, for relief of pruritus. And skin baths with bleach significantly decrease infections that may result from treatment.
Systemic therapy with retinoids, interferon, cytotoxic agents, monoclonal antibodies, and HDAC inhibitors may also cause distinct reactions. For example, the retinoid bexarotene may cause primary hypothyroidism and major lipid abnormalities. Therefore, TSH, free T4, and triglycerides should be monitored every 8 weeks.
Cytotoxic agents such as pralatrexate and methotrexate significantly increase the risk for infection.
Monoclonal antibodies can reactivate previous viral infection, induce tumor lysis syndrome (TLS), and cause progressive multifocal leukoencephalopathy.
HDAC inhibitors such as vorinostat and romidepsin may cause QT prolongation and myelosuppression, among other side effects.
Practitioners need to assess symptoms and side effects thoroughly and often and provide options for supportive care management.
PTCL is an under recognized risk for TLS, Kopp said.
“It should be addressed aggressively,” she added, with monitoring and correction of electrolyte imbalance.
Patients should be rigorously hydrated, and allopurinol should be administered 2-3 days prior to treatment and adjusted based on the patient response and uric acid level.
Multiple myeloma
Colson described supportive care as “keeping all the pieces together.” MM itself can result in a broad spectrum of clinical manifestations, including renal compromise, neuropathy, infection, hypercalcemia, bone pain, lytic lesions, and anemia.
To preserve renal health, patients should drink plenty of water and avoid certain medications, such as IV contrast and nonsteroidal anti-inflammatory drugs.
Peripheral neuropathy can be a side effect of treatment or be caused by the disease itself. Bortezomib-related neuropathy can be reduced with weekly instead of twice weekly dosing and with subcutaneous administration.
Duration of higher doses of thalidomide treatment also impacts neuropathy. Carfilzomib and pomalidomide have a lower incidence of neuropathy.
Myeloma patients have a 15-fold increased risk of recurrent infection because white blood cell production is decreased and the normal immune role of plasma cells is lost.
Supportive therapy includes antibiotics and IVIG therapy. In addition, Colson said pneumonia and influenza vaccines should be considered, as well as prophylaxis for Pneumocystis carinii, herpes zoster, and fungal infections.
Hypercalcemia results from increased bone deterioration. Symptoms include loss of appetite, fatigue, vomiting, muscle weakness, confusion, constipation, increased thirst, and increased urine output. Supportive measures are adequate hydration, furosemide, bisphosphonates, and steroids.
Supportive therapy for bone pain includes bisphosphonates, radiation, pain medication, kyphoplasty, and vertebroplasty. Bisphosphonates, such as pamidronate and zoledronic acid, inhibit bone destruction and are recommended for all myeloma patients with bone disease. However, patients should be monitored for renal dysfunction and osteonecrosis of the jaw when taking bisphosphonates.
And Colson advises, “Hold bisphosphonate therapy if the patient needs a root canal or extraction.” Additionally, dental implants are not recommended for MM patients.
Anemia is another common presenting symptom of myeloma and may also be a result of decreased kidney function. Colson said the use of red blood cell supplements may be used with caution to ameliorate the symptom. Red blood cell transfusion may be considered and a reduction in the medication dose may be required.
MM is a hypercoagulable disease, and measures should be taken to avoid deep vein thrombosis (DVT) and pulmonary embolism (PE). Patients should wear anti-embolism stockings, exercise regularly, take low-dose aspirin, and move about frequently instead of sitting for long periods. Immunomodulatory medications may be adjusted to reduce the risk of a blot clot forming.
Infusion-related reactions are also a risk of therapy, and symptoms of a reaction need to be managed immediately and appropriately, with antihistamines, corticosteroids, interruption of the infusion, slowing of the infusion rate after symptom resolution, and permanent discontinuation in the case of grade 4 reactions.
The potential for longer survival exists, Colson said, due to appropriate supportive care measures. ![]()

Photo courtesy of NCI
NEW YORK—Two presentations at the NCCN 11th Annual Congress: Hematologic Malignancies addressed the importance of supportive care in the treatment of patients with T-cell lymphomas and multiple myeloma.
Erin Kopp, ACNP-BC, of City of Hope Comprehensive Cancer Center in Duarte, California, reminded the audience that supportive care is not palliative care.
Supportive care “complements critical care so that the patient doesn’t have to stop treatment,” she said.
Kopp focused primarily on cutaneous T-cell lymphoma (CTCL) in her presentation, with some recommendations for managing tumor lysis syndrome in patients undergoing therapy for peripheral T-cell lymphoma (PTCL).
And Kathleen Colson, RN, of the Dana-Farber Cancer Institute in Boston, Massachusetts, discussed supportive care for patients with multiple myeloma (MM).
T-cell lymphomas
Most T-cell lymphoma patients will require multiple treatment regimens over their lifetimes, Kopp said. And each type of therapy brings different treatment-related toxicities, which in turn require distinct supportive care measures to manage them.
Topical steroids, for example, may cause skin-thinning, stretch marks, skin irritation, and may be absorbed systemically when a high-potency formulation is used. So the lowest potency steroid that provides the maximum efficacy should be utilized. Practitioners should assess systemic effects if high-potency steroids are utilized.
Topical nitrogen mustard can darken the skin, which often occurs as the lesions resolve, Kopp said. She cautioned that patients experiencing hyperpigmentation often stop treatment without telling their physicians.
So Kopp recommends appropriate patient education to go along with the treatment. With nitrogen mustard, this includes applying a thin layer only to the affected areas and refrigerating the topical ointment to increase soothing.
Topical retinoids may cause redness, itching, warmth, swelling, burning, scaling or other irritation. They also increase the patients’ sensitivity to light. Kopp indicated that for the first week, topical retinoids should be applied once every other day and then titrated as tolerated.
Phototherapy with PUVA or narrowband-UVB may also cause itching, in addition to skin burn, nausea, and other side effects.
“Do not underestimate emollients,” Kopp said, for relief of pruritus. And skin baths with bleach significantly decrease infections that may result from treatment.
Systemic therapy with retinoids, interferon, cytotoxic agents, monoclonal antibodies, and HDAC inhibitors may also cause distinct reactions. For example, the retinoid bexarotene may cause primary hypothyroidism and major lipid abnormalities. Therefore, TSH, free T4, and triglycerides should be monitored every 8 weeks.
Cytotoxic agents such as pralatrexate and methotrexate significantly increase the risk for infection.
Monoclonal antibodies can reactivate previous viral infection, induce tumor lysis syndrome (TLS), and cause progressive multifocal leukoencephalopathy.
HDAC inhibitors such as vorinostat and romidepsin may cause QT prolongation and myelosuppression, among other side effects.
Practitioners need to assess symptoms and side effects thoroughly and often and provide options for supportive care management.
PTCL is an under recognized risk for TLS, Kopp said.
“It should be addressed aggressively,” she added, with monitoring and correction of electrolyte imbalance.
Patients should be rigorously hydrated, and allopurinol should be administered 2-3 days prior to treatment and adjusted based on the patient response and uric acid level.
Multiple myeloma
Colson described supportive care as “keeping all the pieces together.” MM itself can result in a broad spectrum of clinical manifestations, including renal compromise, neuropathy, infection, hypercalcemia, bone pain, lytic lesions, and anemia.
To preserve renal health, patients should drink plenty of water and avoid certain medications, such as IV contrast and nonsteroidal anti-inflammatory drugs.
Peripheral neuropathy can be a side effect of treatment or be caused by the disease itself. Bortezomib-related neuropathy can be reduced with weekly instead of twice weekly dosing and with subcutaneous administration.
Duration of higher doses of thalidomide treatment also impacts neuropathy. Carfilzomib and pomalidomide have a lower incidence of neuropathy.
Myeloma patients have a 15-fold increased risk of recurrent infection because white blood cell production is decreased and the normal immune role of plasma cells is lost.
Supportive therapy includes antibiotics and IVIG therapy. In addition, Colson said pneumonia and influenza vaccines should be considered, as well as prophylaxis for Pneumocystis carinii, herpes zoster, and fungal infections.
Hypercalcemia results from increased bone deterioration. Symptoms include loss of appetite, fatigue, vomiting, muscle weakness, confusion, constipation, increased thirst, and increased urine output. Supportive measures are adequate hydration, furosemide, bisphosphonates, and steroids.
Supportive therapy for bone pain includes bisphosphonates, radiation, pain medication, kyphoplasty, and vertebroplasty. Bisphosphonates, such as pamidronate and zoledronic acid, inhibit bone destruction and are recommended for all myeloma patients with bone disease. However, patients should be monitored for renal dysfunction and osteonecrosis of the jaw when taking bisphosphonates.
And Colson advises, “Hold bisphosphonate therapy if the patient needs a root canal or extraction.” Additionally, dental implants are not recommended for MM patients.
Anemia is another common presenting symptom of myeloma and may also be a result of decreased kidney function. Colson said the use of red blood cell supplements may be used with caution to ameliorate the symptom. Red blood cell transfusion may be considered and a reduction in the medication dose may be required.
MM is a hypercoagulable disease, and measures should be taken to avoid deep vein thrombosis (DVT) and pulmonary embolism (PE). Patients should wear anti-embolism stockings, exercise regularly, take low-dose aspirin, and move about frequently instead of sitting for long periods. Immunomodulatory medications may be adjusted to reduce the risk of a blot clot forming.
Infusion-related reactions are also a risk of therapy, and symptoms of a reaction need to be managed immediately and appropriately, with antihistamines, corticosteroids, interruption of the infusion, slowing of the infusion rate after symptom resolution, and permanent discontinuation in the case of grade 4 reactions.
The potential for longer survival exists, Colson said, due to appropriate supportive care measures. ![]()
Patients may have high expectations of phase 1 trials

Photo courtesy of NCI Clinical
Center/Mathews Media Group
Expectations may not correspond to reality for cancer patients considering enrollment in phase 1 trials, according to a study published in Cancer.
The study showed that, even after consulting with clinicians, nearly half of patients expected their tumors would shrink during the trial, and some patients expected to be cured.
In reality, the typical response rates of phase 1 cancer trials range from 4% to 20%, and patients survive for a median of 6 months.
Udai Banerji, MD, PhD, of The Institute of Cancer Research in London, England, and his colleagues conducted this study.
The team explored patients’ motivations for considering participation in phase 1 trials and assessed their expectations both before and after they consulted with clinicians.
The study included 396 patients who were considering enrollment in a phase 1 trial. All of these patients completed questionnaires prior to a consultation with a clinician, and 301 completed an abbreviated follow-up questionnaire after their consultation.
A majority of the patients said they were willing to enroll in a trial—72% pre-consultation and 84% after.
Before their consultation, 84% of patients ranked the possibility of tumor shrinkage as the most important reason for considering a phase 1 trial.
Fifty-six percent of patients said the most important reason was a lack of alternative treatments, 44% said it was their physician’s recommendation, and 38% said it was the possibility that the research might benefit others. (Patients could give the same rank to multiple reasons.)
Before their consultation, 43% of patients predicted their tumors would shrink if they participated in a trial. After the consultation, this increased to 47%, and 14% of patients thought they would be cured by participating in the trial. (Patients were not asked about the possibility of cure in the pre-consultation questionnaire.)
Before their consultation, 71% of patients said they expected moderate side effects related to the treatment being tested. This increased to 77% after the consultation. Only 11% of patients expected severe side effects pre-consultation, a figure that decreased to 7% after consultation.
Before consultation, about half of patients did not expect that weekly hospital visits would be required for participation in the trial. After the consultation, 93% of patients expected weekly visits.
“There is a positive message in this [study], which is that 84% of patients are willing to participate in phase 1 oncology studies after a discussion with clinical and nursing staff who lay out the conservative estimates of benefit and requirements of hospital visits,” Dr Banerji said.
“This is good for current and future patients and cancer medicine in general. [However,] the high percentage of patients expecting their tumors to shrink was a sobering finding. This creates a challenge for healthcare professionals to manage expectations but to do so without being patronizing or dismissing human hope.” ![]()

Photo courtesy of NCI Clinical
Center/Mathews Media Group
Expectations may not correspond to reality for cancer patients considering enrollment in phase 1 trials, according to a study published in Cancer.
The study showed that, even after consulting with clinicians, nearly half of patients expected their tumors would shrink during the trial, and some patients expected to be cured.
In reality, the typical response rates of phase 1 cancer trials range from 4% to 20%, and patients survive for a median of 6 months.
Udai Banerji, MD, PhD, of The Institute of Cancer Research in London, England, and his colleagues conducted this study.
The team explored patients’ motivations for considering participation in phase 1 trials and assessed their expectations both before and after they consulted with clinicians.
The study included 396 patients who were considering enrollment in a phase 1 trial. All of these patients completed questionnaires prior to a consultation with a clinician, and 301 completed an abbreviated follow-up questionnaire after their consultation.
A majority of the patients said they were willing to enroll in a trial—72% pre-consultation and 84% after.
Before their consultation, 84% of patients ranked the possibility of tumor shrinkage as the most important reason for considering a phase 1 trial.
Fifty-six percent of patients said the most important reason was a lack of alternative treatments, 44% said it was their physician’s recommendation, and 38% said it was the possibility that the research might benefit others. (Patients could give the same rank to multiple reasons.)
Before their consultation, 43% of patients predicted their tumors would shrink if they participated in a trial. After the consultation, this increased to 47%, and 14% of patients thought they would be cured by participating in the trial. (Patients were not asked about the possibility of cure in the pre-consultation questionnaire.)
Before their consultation, 71% of patients said they expected moderate side effects related to the treatment being tested. This increased to 77% after the consultation. Only 11% of patients expected severe side effects pre-consultation, a figure that decreased to 7% after consultation.
Before consultation, about half of patients did not expect that weekly hospital visits would be required for participation in the trial. After the consultation, 93% of patients expected weekly visits.
“There is a positive message in this [study], which is that 84% of patients are willing to participate in phase 1 oncology studies after a discussion with clinical and nursing staff who lay out the conservative estimates of benefit and requirements of hospital visits,” Dr Banerji said.
“This is good for current and future patients and cancer medicine in general. [However,] the high percentage of patients expecting their tumors to shrink was a sobering finding. This creates a challenge for healthcare professionals to manage expectations but to do so without being patronizing or dismissing human hope.” ![]()

Photo courtesy of NCI Clinical
Center/Mathews Media Group
Expectations may not correspond to reality for cancer patients considering enrollment in phase 1 trials, according to a study published in Cancer.
The study showed that, even after consulting with clinicians, nearly half of patients expected their tumors would shrink during the trial, and some patients expected to be cured.
In reality, the typical response rates of phase 1 cancer trials range from 4% to 20%, and patients survive for a median of 6 months.
Udai Banerji, MD, PhD, of The Institute of Cancer Research in London, England, and his colleagues conducted this study.
The team explored patients’ motivations for considering participation in phase 1 trials and assessed their expectations both before and after they consulted with clinicians.
The study included 396 patients who were considering enrollment in a phase 1 trial. All of these patients completed questionnaires prior to a consultation with a clinician, and 301 completed an abbreviated follow-up questionnaire after their consultation.
A majority of the patients said they were willing to enroll in a trial—72% pre-consultation and 84% after.
Before their consultation, 84% of patients ranked the possibility of tumor shrinkage as the most important reason for considering a phase 1 trial.
Fifty-six percent of patients said the most important reason was a lack of alternative treatments, 44% said it was their physician’s recommendation, and 38% said it was the possibility that the research might benefit others. (Patients could give the same rank to multiple reasons.)
Before their consultation, 43% of patients predicted their tumors would shrink if they participated in a trial. After the consultation, this increased to 47%, and 14% of patients thought they would be cured by participating in the trial. (Patients were not asked about the possibility of cure in the pre-consultation questionnaire.)
Before their consultation, 71% of patients said they expected moderate side effects related to the treatment being tested. This increased to 77% after the consultation. Only 11% of patients expected severe side effects pre-consultation, a figure that decreased to 7% after consultation.
Before consultation, about half of patients did not expect that weekly hospital visits would be required for participation in the trial. After the consultation, 93% of patients expected weekly visits.
“There is a positive message in this [study], which is that 84% of patients are willing to participate in phase 1 oncology studies after a discussion with clinical and nursing staff who lay out the conservative estimates of benefit and requirements of hospital visits,” Dr Banerji said.
“This is good for current and future patients and cancer medicine in general. [However,] the high percentage of patients expecting their tumors to shrink was a sobering finding. This creates a challenge for healthcare professionals to manage expectations but to do so without being patronizing or dismissing human hope.” ![]()
Cancer report details progress, predicts problems

Photo by Rhoda Baer
A new report highlights recent advances made in the fight against cancer but suggests the burden of cancer in the US is still on the rise.
The AACR Cancer Progress Report 2016 states that the number of cancer survivors in the US rose by 1 million from 2014 to 2016, reaching an estimated 15.5 million.
Meanwhile, the US Food and Drug Administration (FDA) approved new treatments for a range of cancers.
Between August 1, 2015, and July 31, 2016, the FDA approved 13 new anticancer therapies and new uses for 11 previously approved anticancer therapies.
Six of these drugs were approved to treat hematologic malignancies:
- Venetoclax for chronic lymphocytic leukemia
- Daratumumab for multiple myeloma
- Elotuzumab for multiple myeloma
- Ixazomib for multiple myeloma
- Obinutuzumab for follicular lymphoma
- Nivolumab for classical Hodgkin lymphoma.
The report notes that the use of immunotherapy, in particular, is on the rise. For example, on August 1, 2015, checkpoint inhibitors were approved for just 2 cancers—melanoma and lung cancer.
As of September 1, 2016, checkpoint inhibitors have been approved for 6 cancers—Hodgkin lymphoma, bladder cancer, head and neck cancer, kidney cancer, lung cancer, and melanoma.
“The promise of immunotherapy for cancer therapy has never been greater, and the opportunity to make significant progress in this critical area is real,” said Nancy E. Davidson, MD, president of the AACR and director of the University of Pittsburgh Cancer Institute in Pennsylvania.
“However, continued progress is going to require a sustained federal commitment to the research agenda. And in fact, if the necessary funding is provided, we will accelerate the pace of progress and, in turn, markedly reduce morbidity and mortality from cancer.”
Growing burden of cancer
The report emphasizes that although advances are being made against cancers, these diseases continue to exert an immense personal and economic toll, and the burden of cancer is expected to grow in the coming decades.
According to the report:
- More than 595,000 people in the US are projected to die from cancer in 2016
- Cancer is the number one cause of disease-related death among US children
- The number of new cancer cases in the US is predicted to rise from 1.7 million in 2015 to 2.4 million in 2035
- It is estimated that the direct medical costs of cancer care in the US in 2010 were nearly $125 billion, and these costs will rise to $156 billion in 2020.
The report states that the increasing economic and personal burden of cancer underscores the need for more research to develop new approaches to cancer prevention and treatment.
The report also highlights the recommendations of the National Cancer Moonshot Initiative Blue Ribbon Panel for accelerating the pace of progress in cancer research.
“Research has made tremendous advances against cancer,” said Margaret Foti, PhD, MD, chief executive officer of the AACR.
“However, we need to accelerate the pace of progress because it is unacceptable that 1 American will die of cancer every minute of every day this year.” ![]()

Photo by Rhoda Baer
A new report highlights recent advances made in the fight against cancer but suggests the burden of cancer in the US is still on the rise.
The AACR Cancer Progress Report 2016 states that the number of cancer survivors in the US rose by 1 million from 2014 to 2016, reaching an estimated 15.5 million.
Meanwhile, the US Food and Drug Administration (FDA) approved new treatments for a range of cancers.
Between August 1, 2015, and July 31, 2016, the FDA approved 13 new anticancer therapies and new uses for 11 previously approved anticancer therapies.
Six of these drugs were approved to treat hematologic malignancies:
- Venetoclax for chronic lymphocytic leukemia
- Daratumumab for multiple myeloma
- Elotuzumab for multiple myeloma
- Ixazomib for multiple myeloma
- Obinutuzumab for follicular lymphoma
- Nivolumab for classical Hodgkin lymphoma.
The report notes that the use of immunotherapy, in particular, is on the rise. For example, on August 1, 2015, checkpoint inhibitors were approved for just 2 cancers—melanoma and lung cancer.
As of September 1, 2016, checkpoint inhibitors have been approved for 6 cancers—Hodgkin lymphoma, bladder cancer, head and neck cancer, kidney cancer, lung cancer, and melanoma.
“The promise of immunotherapy for cancer therapy has never been greater, and the opportunity to make significant progress in this critical area is real,” said Nancy E. Davidson, MD, president of the AACR and director of the University of Pittsburgh Cancer Institute in Pennsylvania.
“However, continued progress is going to require a sustained federal commitment to the research agenda. And in fact, if the necessary funding is provided, we will accelerate the pace of progress and, in turn, markedly reduce morbidity and mortality from cancer.”
Growing burden of cancer
The report emphasizes that although advances are being made against cancers, these diseases continue to exert an immense personal and economic toll, and the burden of cancer is expected to grow in the coming decades.
According to the report:
- More than 595,000 people in the US are projected to die from cancer in 2016
- Cancer is the number one cause of disease-related death among US children
- The number of new cancer cases in the US is predicted to rise from 1.7 million in 2015 to 2.4 million in 2035
- It is estimated that the direct medical costs of cancer care in the US in 2010 were nearly $125 billion, and these costs will rise to $156 billion in 2020.
The report states that the increasing economic and personal burden of cancer underscores the need for more research to develop new approaches to cancer prevention and treatment.
The report also highlights the recommendations of the National Cancer Moonshot Initiative Blue Ribbon Panel for accelerating the pace of progress in cancer research.
“Research has made tremendous advances against cancer,” said Margaret Foti, PhD, MD, chief executive officer of the AACR.
“However, we need to accelerate the pace of progress because it is unacceptable that 1 American will die of cancer every minute of every day this year.” ![]()

Photo by Rhoda Baer
A new report highlights recent advances made in the fight against cancer but suggests the burden of cancer in the US is still on the rise.
The AACR Cancer Progress Report 2016 states that the number of cancer survivors in the US rose by 1 million from 2014 to 2016, reaching an estimated 15.5 million.
Meanwhile, the US Food and Drug Administration (FDA) approved new treatments for a range of cancers.
Between August 1, 2015, and July 31, 2016, the FDA approved 13 new anticancer therapies and new uses for 11 previously approved anticancer therapies.
Six of these drugs were approved to treat hematologic malignancies:
- Venetoclax for chronic lymphocytic leukemia
- Daratumumab for multiple myeloma
- Elotuzumab for multiple myeloma
- Ixazomib for multiple myeloma
- Obinutuzumab for follicular lymphoma
- Nivolumab for classical Hodgkin lymphoma.
The report notes that the use of immunotherapy, in particular, is on the rise. For example, on August 1, 2015, checkpoint inhibitors were approved for just 2 cancers—melanoma and lung cancer.
As of September 1, 2016, checkpoint inhibitors have been approved for 6 cancers—Hodgkin lymphoma, bladder cancer, head and neck cancer, kidney cancer, lung cancer, and melanoma.
“The promise of immunotherapy for cancer therapy has never been greater, and the opportunity to make significant progress in this critical area is real,” said Nancy E. Davidson, MD, president of the AACR and director of the University of Pittsburgh Cancer Institute in Pennsylvania.
“However, continued progress is going to require a sustained federal commitment to the research agenda. And in fact, if the necessary funding is provided, we will accelerate the pace of progress and, in turn, markedly reduce morbidity and mortality from cancer.”
Growing burden of cancer
The report emphasizes that although advances are being made against cancers, these diseases continue to exert an immense personal and economic toll, and the burden of cancer is expected to grow in the coming decades.
According to the report:
- More than 595,000 people in the US are projected to die from cancer in 2016
- Cancer is the number one cause of disease-related death among US children
- The number of new cancer cases in the US is predicted to rise from 1.7 million in 2015 to 2.4 million in 2035
- It is estimated that the direct medical costs of cancer care in the US in 2010 were nearly $125 billion, and these costs will rise to $156 billion in 2020.
The report states that the increasing economic and personal burden of cancer underscores the need for more research to develop new approaches to cancer prevention and treatment.
The report also highlights the recommendations of the National Cancer Moonshot Initiative Blue Ribbon Panel for accelerating the pace of progress in cancer research.
“Research has made tremendous advances against cancer,” said Margaret Foti, PhD, MD, chief executive officer of the AACR.
“However, we need to accelerate the pace of progress because it is unacceptable that 1 American will die of cancer every minute of every day this year.” ![]()
Dying cancer patients may be under-treated for pain

Photo courtesy of CDC
New research suggests that many patients who die of cancer do not receive strong opioid medications in their last year of life, despite the fact that these drugs are the recommended treatment for cancer-related pain.
Researchers used UK Cancer Registry Data to study more than 6000 cancer patients who died over a 7-year period.
Less than half of these patients received prescriptions for strong opioid medications in their last year of life.
Among those patients who did receive such prescriptions, many received them late.
Lucy Ziegler, PhD, of the University of Leeds in the UK, and her colleagues conducted this study and reported the results in PAIN.
The study included 6080 cancer patients who died between 2005 and 2012.
About 76% (n=4610) of these patients had received one or more prescriptions for analgesics, including 48% (n=2919) who received a strong opioid and 28% (n=1691) who received a non-opioid or weak opioid. The remaining 24% (n=1470) did not receive any prescription analgesic.
The chance of receiving strong opioids was not affected by patients’ age or sex.
However, patients who died in a hospital were 60% less likely to have a prescription for strong opioids during the last year of life, when compared with those who died in hospice.
And patients who received chemotherapy in the last year of life were 30% more likely to receive a strong opioid than patients who did not receive chemotherapy.
Timing of therapy
Among the patients who did receive strong opioids, the median time between receiving the medication and death was 9 weeks. By 6 weeks before death, just 30% of patients had been prescribed a strong opioid.
The researchers noted that these figures don’t match up with previous studies reporting that severe pain can occur “much earlier in the cancer trajectory.”
Older patients were more likely to receive their strong opioid prescription late (defined as later than 9 weeks before death). After other factors were taken into account, patients age 60 or older were about 2 to 4 times more likely to be in the late-prescribing group, compared with those age 50 or younger.
Compared to patients who died in hospice, patients who died in a hospital were 40% more likely to receive a late prescription for a strong opioid. Patients who died in their own home were 2.6 times more likely to receive a late prescription, and patients who died in a care home were 2.8 times more likely to receive a late prescription.
Patients who had surgery were 40% more likely to receive a late prescription than patients who did not undergo surgery.
But patients who received chemotherapy and/or radiotherapy were 30% more likely to have received an early prescription for a strong opioid than patients who did not receive chemo/radiotherapy.
Dr Ziegler and her colleagues noted that this study had its limitations; in particular, the lack of data on pain severity.
Still, the researchers believe their results support the hypothesis of potential under-treatment of cancer pain and suggest that many more patients with advanced cancer and pain may benefit from a strong opioid analgesic. ![]()

Photo courtesy of CDC
New research suggests that many patients who die of cancer do not receive strong opioid medications in their last year of life, despite the fact that these drugs are the recommended treatment for cancer-related pain.
Researchers used UK Cancer Registry Data to study more than 6000 cancer patients who died over a 7-year period.
Less than half of these patients received prescriptions for strong opioid medications in their last year of life.
Among those patients who did receive such prescriptions, many received them late.
Lucy Ziegler, PhD, of the University of Leeds in the UK, and her colleagues conducted this study and reported the results in PAIN.
The study included 6080 cancer patients who died between 2005 and 2012.
About 76% (n=4610) of these patients had received one or more prescriptions for analgesics, including 48% (n=2919) who received a strong opioid and 28% (n=1691) who received a non-opioid or weak opioid. The remaining 24% (n=1470) did not receive any prescription analgesic.
The chance of receiving strong opioids was not affected by patients’ age or sex.
However, patients who died in a hospital were 60% less likely to have a prescription for strong opioids during the last year of life, when compared with those who died in hospice.
And patients who received chemotherapy in the last year of life were 30% more likely to receive a strong opioid than patients who did not receive chemotherapy.
Timing of therapy
Among the patients who did receive strong opioids, the median time between receiving the medication and death was 9 weeks. By 6 weeks before death, just 30% of patients had been prescribed a strong opioid.
The researchers noted that these figures don’t match up with previous studies reporting that severe pain can occur “much earlier in the cancer trajectory.”
Older patients were more likely to receive their strong opioid prescription late (defined as later than 9 weeks before death). After other factors were taken into account, patients age 60 or older were about 2 to 4 times more likely to be in the late-prescribing group, compared with those age 50 or younger.
Compared to patients who died in hospice, patients who died in a hospital were 40% more likely to receive a late prescription for a strong opioid. Patients who died in their own home were 2.6 times more likely to receive a late prescription, and patients who died in a care home were 2.8 times more likely to receive a late prescription.
Patients who had surgery were 40% more likely to receive a late prescription than patients who did not undergo surgery.
But patients who received chemotherapy and/or radiotherapy were 30% more likely to have received an early prescription for a strong opioid than patients who did not receive chemo/radiotherapy.
Dr Ziegler and her colleagues noted that this study had its limitations; in particular, the lack of data on pain severity.
Still, the researchers believe their results support the hypothesis of potential under-treatment of cancer pain and suggest that many more patients with advanced cancer and pain may benefit from a strong opioid analgesic. ![]()

Photo courtesy of CDC
New research suggests that many patients who die of cancer do not receive strong opioid medications in their last year of life, despite the fact that these drugs are the recommended treatment for cancer-related pain.
Researchers used UK Cancer Registry Data to study more than 6000 cancer patients who died over a 7-year period.
Less than half of these patients received prescriptions for strong opioid medications in their last year of life.
Among those patients who did receive such prescriptions, many received them late.
Lucy Ziegler, PhD, of the University of Leeds in the UK, and her colleagues conducted this study and reported the results in PAIN.
The study included 6080 cancer patients who died between 2005 and 2012.
About 76% (n=4610) of these patients had received one or more prescriptions for analgesics, including 48% (n=2919) who received a strong opioid and 28% (n=1691) who received a non-opioid or weak opioid. The remaining 24% (n=1470) did not receive any prescription analgesic.
The chance of receiving strong opioids was not affected by patients’ age or sex.
However, patients who died in a hospital were 60% less likely to have a prescription for strong opioids during the last year of life, when compared with those who died in hospice.
And patients who received chemotherapy in the last year of life were 30% more likely to receive a strong opioid than patients who did not receive chemotherapy.
Timing of therapy
Among the patients who did receive strong opioids, the median time between receiving the medication and death was 9 weeks. By 6 weeks before death, just 30% of patients had been prescribed a strong opioid.
The researchers noted that these figures don’t match up with previous studies reporting that severe pain can occur “much earlier in the cancer trajectory.”
Older patients were more likely to receive their strong opioid prescription late (defined as later than 9 weeks before death). After other factors were taken into account, patients age 60 or older were about 2 to 4 times more likely to be in the late-prescribing group, compared with those age 50 or younger.
Compared to patients who died in hospice, patients who died in a hospital were 40% more likely to receive a late prescription for a strong opioid. Patients who died in their own home were 2.6 times more likely to receive a late prescription, and patients who died in a care home were 2.8 times more likely to receive a late prescription.
Patients who had surgery were 40% more likely to receive a late prescription than patients who did not undergo surgery.
But patients who received chemotherapy and/or radiotherapy were 30% more likely to have received an early prescription for a strong opioid than patients who did not receive chemo/radiotherapy.
Dr Ziegler and her colleagues noted that this study had its limitations; in particular, the lack of data on pain severity.
Still, the researchers believe their results support the hypothesis of potential under-treatment of cancer pain and suggest that many more patients with advanced cancer and pain may benefit from a strong opioid analgesic. ![]()
Effects of caring for advanced cancer patients
SAN FRANCISCO—Family caregivers of patients with high-mortality cancers may often experience high levels of depression and anxiety, results of a survey suggest.
The survey showed that caregivers can spend more than 8 hours a day providing care.
And as caregiving time increases, self-care behaviors such as sleep and exercise decline, which may confer poorer mental health.
These findings were presented at the 2016 Palliative Care in Oncology Symposium (abstract 239).
“Caregivers and patients are faced with an enormous physical and emotional toll when dealing with advanced cancer,” said study investigator J. Nicholas Dionne-Odom, PhD, RN, of the University of Alabama at Birmingham.
“When they put their own health and well-being on the back burner, it can affect their care to the patient.”
Dr Dionne-Odom and his colleagues conducted a cross-sectional survey of 294 family caregivers of Medicare beneficiaries diagnosed with pancreatic, lung, brain, ovarian, head and neck, hematologic, or stage IV cancers.
The survey was fielded across 8 cancer centers in Alabama, Florida, and Tennessee. Survey questions explored measures of self-care behaviors and quality of life.
The caregivers had an average age of 66. They were mostly female (72.8%), white (91.2%), retired (54.4%), and the patient’s spouse/partner (60.2%). Nearly half of the caregivers lived in rural areas (46.9%), and more than half had annual incomes less than $50,000 (53.8%).
Most of the caregivers said they provided care 6 to 7 days a week (71%) for more than 1 year (68%).
Twenty-three percent of caregivers reported a high level of depressive symptoms, and 34% reported borderline or high levels of anxiety symptoms, associated with significantly lower scores for self-care.
Lower self-care behavior scores were associated with a longer overall duration of caregiving, more hours in the day spent caregiving, more days of the week spent caregiving, and with fair or poor patient health.
“We hope our research rallies the oncology palliative care communities to develop assessment tools and services that support caregivers,” Dr Dionne-Odom said. “These efforts would help ensure that caregivers are supported and healthy when they take on the important role of caring for an individual with advanced cancer.” ![]()
SAN FRANCISCO—Family caregivers of patients with high-mortality cancers may often experience high levels of depression and anxiety, results of a survey suggest.
The survey showed that caregivers can spend more than 8 hours a day providing care.
And as caregiving time increases, self-care behaviors such as sleep and exercise decline, which may confer poorer mental health.
These findings were presented at the 2016 Palliative Care in Oncology Symposium (abstract 239).
“Caregivers and patients are faced with an enormous physical and emotional toll when dealing with advanced cancer,” said study investigator J. Nicholas Dionne-Odom, PhD, RN, of the University of Alabama at Birmingham.
“When they put their own health and well-being on the back burner, it can affect their care to the patient.”
Dr Dionne-Odom and his colleagues conducted a cross-sectional survey of 294 family caregivers of Medicare beneficiaries diagnosed with pancreatic, lung, brain, ovarian, head and neck, hematologic, or stage IV cancers.
The survey was fielded across 8 cancer centers in Alabama, Florida, and Tennessee. Survey questions explored measures of self-care behaviors and quality of life.
The caregivers had an average age of 66. They were mostly female (72.8%), white (91.2%), retired (54.4%), and the patient’s spouse/partner (60.2%). Nearly half of the caregivers lived in rural areas (46.9%), and more than half had annual incomes less than $50,000 (53.8%).
Most of the caregivers said they provided care 6 to 7 days a week (71%) for more than 1 year (68%).
Twenty-three percent of caregivers reported a high level of depressive symptoms, and 34% reported borderline or high levels of anxiety symptoms, associated with significantly lower scores for self-care.
Lower self-care behavior scores were associated with a longer overall duration of caregiving, more hours in the day spent caregiving, more days of the week spent caregiving, and with fair or poor patient health.
“We hope our research rallies the oncology palliative care communities to develop assessment tools and services that support caregivers,” Dr Dionne-Odom said. “These efforts would help ensure that caregivers are supported and healthy when they take on the important role of caring for an individual with advanced cancer.” ![]()
SAN FRANCISCO—Family caregivers of patients with high-mortality cancers may often experience high levels of depression and anxiety, results of a survey suggest.
The survey showed that caregivers can spend more than 8 hours a day providing care.
And as caregiving time increases, self-care behaviors such as sleep and exercise decline, which may confer poorer mental health.
These findings were presented at the 2016 Palliative Care in Oncology Symposium (abstract 239).
“Caregivers and patients are faced with an enormous physical and emotional toll when dealing with advanced cancer,” said study investigator J. Nicholas Dionne-Odom, PhD, RN, of the University of Alabama at Birmingham.
“When they put their own health and well-being on the back burner, it can affect their care to the patient.”
Dr Dionne-Odom and his colleagues conducted a cross-sectional survey of 294 family caregivers of Medicare beneficiaries diagnosed with pancreatic, lung, brain, ovarian, head and neck, hematologic, or stage IV cancers.
The survey was fielded across 8 cancer centers in Alabama, Florida, and Tennessee. Survey questions explored measures of self-care behaviors and quality of life.
The caregivers had an average age of 66. They were mostly female (72.8%), white (91.2%), retired (54.4%), and the patient’s spouse/partner (60.2%). Nearly half of the caregivers lived in rural areas (46.9%), and more than half had annual incomes less than $50,000 (53.8%).
Most of the caregivers said they provided care 6 to 7 days a week (71%) for more than 1 year (68%).
Twenty-three percent of caregivers reported a high level of depressive symptoms, and 34% reported borderline or high levels of anxiety symptoms, associated with significantly lower scores for self-care.
Lower self-care behavior scores were associated with a longer overall duration of caregiving, more hours in the day spent caregiving, more days of the week spent caregiving, and with fair or poor patient health.
“We hope our research rallies the oncology palliative care communities to develop assessment tools and services that support caregivers,” Dr Dionne-Odom said. “These efforts would help ensure that caregivers are supported and healthy when they take on the important role of caring for an individual with advanced cancer.”
Study reveals barriers to accessing palliative care services

©ASCO/Todd Buchanan 2016
SAN FRANCISCO—Patients may face challenges when trying to access palliative and supportive care services at cancer centers, a new study suggests.
Researchers took a “mystery shopper” approach and placed calls to cancer centers inquiring about palliative and supportive care services for a family member.
The callers sometimes had difficulty obtaining information about these services, even though all of the centers offer them.
“It’s sobering to hear that such services are not readily accessible at many centers,” said study investigator Kathryn Hutchins, a medical student at Duke University in Durham, North Carolina.
“However, it provides an opportunity for cancer centers to empower their front-line staff, as well as the oncology care team, through education and training so that the entire enterprise has a common understanding of palliative care and how to access it.”
Hutchins and her colleagues presented this research at the 2016 Palliative Care in Oncology Symposium (abstract 122).
The researchers placed 160 calls to 40 major cancer centers. The team chose to focus on National Cancer Institute-designated cancer centers because they all provide palliative care services along with other supportive care services.
The researchers used the same script for every call, asking about services for a 58-year-old female who was recently diagnosed with inoperable liver cancer. The team called each center 4 times on different days.
In 38.2% of the calls, the researchers were not able to receive complete information about supportive care services.
In 9.5% of calls, cancer center staff gave an answer other than “yes” regarding the availability of palliative care services, even though such services were available.
The answers varied and included responses such as:
- Palliative care was for end-of-life patients only (n=2)
- No physicians specialized in symptom management (n=3)
- A medical record review would be needed first (n=2).
In addition, 10 staff members said they were unsure about the availability of palliative care, and 2 were unfamiliar with the term.
Overall, 37.6% of the callers were told that all 7 supportive care services they inquired about were offered.
“As oncologists, we like to believe that, when we refer patients to our institution’s helpline, they will get connected to the services they need, but that doesn’t always happen,” said study investigator Arif Kamal, MD, of Duke Cancer Institute.
“It’s important for oncologists to be aware of these barriers and to work to eliminate them.”

©ASCO/Todd Buchanan 2016
SAN FRANCISCO—Patients may face challenges when trying to access palliative and supportive care services at cancer centers, a new study suggests.
Researchers took a “mystery shopper” approach and placed calls to cancer centers inquiring about palliative and supportive care services for a family member.
The callers sometimes had difficulty obtaining information about these services, even though all of the centers offer them.
“It’s sobering to hear that such services are not readily accessible at many centers,” said study investigator Kathryn Hutchins, a medical student at Duke University in Durham, North Carolina.
“However, it provides an opportunity for cancer centers to empower their front-line staff, as well as the oncology care team, through education and training so that the entire enterprise has a common understanding of palliative care and how to access it.”
Hutchins and her colleagues presented this research at the 2016 Palliative Care in Oncology Symposium (abstract 122).
The researchers placed 160 calls to 40 major cancer centers. The team chose to focus on National Cancer Institute-designated cancer centers because they all provide palliative care services along with other supportive care services.
The researchers used the same script for every call, asking about services for a 58-year-old female who was recently diagnosed with inoperable liver cancer. The team called each center 4 times on different days.
In 38.2% of the calls, the researchers were not able to receive complete information about supportive care services.
In 9.5% of calls, cancer center staff gave an answer other than “yes” regarding the availability of palliative care services, even though such services were available.
The answers varied and included responses such as:
- Palliative care was for end-of-life patients only (n=2)
- No physicians specialized in symptom management (n=3)
- A medical record review would be needed first (n=2).
In addition, 10 staff members said they were unsure about the availability of palliative care, and 2 were unfamiliar with the term.
Overall, 37.6% of the callers were told that all 7 supportive care services they inquired about were offered.
“As oncologists, we like to believe that, when we refer patients to our institution’s helpline, they will get connected to the services they need, but that doesn’t always happen,” said study investigator Arif Kamal, MD, of Duke Cancer Institute.
“It’s important for oncologists to be aware of these barriers and to work to eliminate them.”

©ASCO/Todd Buchanan 2016
SAN FRANCISCO—Patients may face challenges when trying to access palliative and supportive care services at cancer centers, a new study suggests.
Researchers took a “mystery shopper” approach and placed calls to cancer centers inquiring about palliative and supportive care services for a family member.
The callers sometimes had difficulty obtaining information about these services, even though all of the centers offer them.
“It’s sobering to hear that such services are not readily accessible at many centers,” said study investigator Kathryn Hutchins, a medical student at Duke University in Durham, North Carolina.
“However, it provides an opportunity for cancer centers to empower their front-line staff, as well as the oncology care team, through education and training so that the entire enterprise has a common understanding of palliative care and how to access it.”
Hutchins and her colleagues presented this research at the 2016 Palliative Care in Oncology Symposium (abstract 122).
The researchers placed 160 calls to 40 major cancer centers. The team chose to focus on National Cancer Institute-designated cancer centers because they all provide palliative care services along with other supportive care services.
The researchers used the same script for every call, asking about services for a 58-year-old female who was recently diagnosed with inoperable liver cancer. The team called each center 4 times on different days.
In 38.2% of the calls, the researchers were not able to receive complete information about supportive care services.
In 9.5% of calls, cancer center staff gave an answer other than “yes” regarding the availability of palliative care services, even though such services were available.
The answers varied and included responses such as:
- Palliative care was for end-of-life patients only (n=2)
- No physicians specialized in symptom management (n=3)
- A medical record review would be needed first (n=2).
In addition, 10 staff members said they were unsure about the availability of palliative care, and 2 were unfamiliar with the term.
Overall, 37.6% of the callers were told that all 7 supportive care services they inquired about were offered.
“As oncologists, we like to believe that, when we refer patients to our institution’s helpline, they will get connected to the services they need, but that doesn’t always happen,” said study investigator Arif Kamal, MD, of Duke Cancer Institute.
“It’s important for oncologists to be aware of these barriers and to work to eliminate them.”
Cancer patients’ caregivers may carry greater burden

©ASCO/Todd Buchanan 2016
SAN FRANCISCO—New research suggests caring for a loved one with cancer may be more burdensome than caring for a loved one with a different condition.
Researchers analyzed data from “Caregiving in the U.S. 2015,” an online panel study of unpaid adult caregivers.
The team compared cancer and non-cancer caregivers to determine similarities and differences in characteristics and experiences.
The findings were presented at the 2016 Palliative Care in Oncology Symposium (abstract 4).
The study included 1248 caregivers, age 18 and older at the time they were surveyed, who provided care to an adult patient. Seven percent of these caregivers were looking after patients with cancer.
Cancer caregivers reported spending more hours per week providing care than non-cancer caregivers—32.9 and 23.9 hours, respectively.
In addition, cancer caregivers were more likely than other caregivers to communicate with healthcare professionals (82% and 62%, respectively), monitor and adjust patients’ care (76% and 66%, respectively), and advocate on behalf of patients (62% and 49%, respectively).
Despite high levels of engagement with providers, cancer caregivers were nearly twice as likely as non-cancer caregivers to report needing more help and information with making end-of-life decisions—40% and 21%, respectively.
“Our research demonstrates the ripple effect that cancer has on families and patient support systems,” said study investigator Erin Kent, PhD, of the National Cancer Institute in Rockville, Maryland.
“Caregiving can be extremely stressful and demanding—physically, emotionally, and financially. The data show we need to do a better job of supporting these individuals, as their wellbeing is essential to the patient’s quality of life and outcomes.”
Dr Kent emphasized the cyclical nature of cancer care, often requiring short, highly intense periods of time where patients undergo active treatment as a possible reason for the increased intensity in caregiving. She noted that such intensity is also associated with increased caregiver stress and depression.
“Based on our findings, it’s clear we need additional research on caregiving to better understand at what point providers and clinicians should intervene to assess the wellbeing of caregivers,” Dr Kent said.
“Technology, combined with use of a clinical distress rating system, could be promising in the future as a means to ensure caregivers are being supported in a meaningful way.”

©ASCO/Todd Buchanan 2016
SAN FRANCISCO—New research suggests caring for a loved one with cancer may be more burdensome than caring for a loved one with a different condition.
Researchers analyzed data from “Caregiving in the U.S. 2015,” an online panel study of unpaid adult caregivers.
The team compared cancer and non-cancer caregivers to determine similarities and differences in characteristics and experiences.
The findings were presented at the 2016 Palliative Care in Oncology Symposium (abstract 4).
The study included 1248 caregivers, age 18 and older at the time they were surveyed, who provided care to an adult patient. Seven percent of these caregivers were looking after patients with cancer.
Cancer caregivers reported spending more hours per week providing care than non-cancer caregivers—32.9 and 23.9 hours, respectively.
In addition, cancer caregivers were more likely than other caregivers to communicate with healthcare professionals (82% and 62%, respectively), monitor and adjust patients’ care (76% and 66%, respectively), and advocate on behalf of patients (62% and 49%, respectively).
Despite high levels of engagement with providers, cancer caregivers were nearly twice as likely as non-cancer caregivers to report needing more help and information with making end-of-life decisions—40% and 21%, respectively.
“Our research demonstrates the ripple effect that cancer has on families and patient support systems,” said study investigator Erin Kent, PhD, of the National Cancer Institute in Rockville, Maryland.
“Caregiving can be extremely stressful and demanding—physically, emotionally, and financially. The data show we need to do a better job of supporting these individuals, as their wellbeing is essential to the patient’s quality of life and outcomes.”
Dr Kent emphasized the cyclical nature of cancer care, often requiring short, highly intense periods of time where patients undergo active treatment as a possible reason for the increased intensity in caregiving. She noted that such intensity is also associated with increased caregiver stress and depression.
“Based on our findings, it’s clear we need additional research on caregiving to better understand at what point providers and clinicians should intervene to assess the wellbeing of caregivers,” Dr Kent said.
“Technology, combined with use of a clinical distress rating system, could be promising in the future as a means to ensure caregivers are being supported in a meaningful way.”

©ASCO/Todd Buchanan 2016
SAN FRANCISCO—New research suggests caring for a loved one with cancer may be more burdensome than caring for a loved one with a different condition.
Researchers analyzed data from “Caregiving in the U.S. 2015,” an online panel study of unpaid adult caregivers.
The team compared cancer and non-cancer caregivers to determine similarities and differences in characteristics and experiences.
The findings were presented at the 2016 Palliative Care in Oncology Symposium (abstract 4).
The study included 1248 caregivers, age 18 and older at the time they were surveyed, who provided care to an adult patient. Seven percent of these caregivers were looking after patients with cancer.
Cancer caregivers reported spending more hours per week providing care than non-cancer caregivers—32.9 and 23.9 hours, respectively.
In addition, cancer caregivers were more likely than other caregivers to communicate with healthcare professionals (82% and 62%, respectively), monitor and adjust patients’ care (76% and 66%, respectively), and advocate on behalf of patients (62% and 49%, respectively).
Despite high levels of engagement with providers, cancer caregivers were nearly twice as likely as non-cancer caregivers to report needing more help and information with making end-of-life decisions—40% and 21%, respectively.
“Our research demonstrates the ripple effect that cancer has on families and patient support systems,” said study investigator Erin Kent, PhD, of the National Cancer Institute in Rockville, Maryland.
“Caregiving can be extremely stressful and demanding—physically, emotionally, and financially. The data show we need to do a better job of supporting these individuals, as their wellbeing is essential to the patient’s quality of life and outcomes.”
Dr Kent emphasized the cyclical nature of cancer care, often requiring short, highly intense periods of time where patients undergo active treatment as a possible reason for the increased intensity in caregiving. She noted that such intensity is also associated with increased caregiver stress and depression.
“Based on our findings, it’s clear we need additional research on caregiving to better understand at what point providers and clinicians should intervene to assess the wellbeing of caregivers,” Dr Kent said.
“Technology, combined with use of a clinical distress rating system, could be promising in the future as a means to ensure caregivers are being supported in a meaningful way.”
BSIs costly for pediatric transplant, cancer patients

Staphylococcus infection
Photo by Bill Branson
Ambulatory bloodstream infections (BSIs) can be costly in young cancer patients and recipients of hematopoietic stem cell transplants, according to research published in Pediatric Blood & Cancer.
Among the 61 patients studied, the median cost for an ambulatory BSI was $40,852, and the median length of hospital stay was 7 days.
For patients who were hospitalized for BSI and other medical issues, the cost and length of stay were much higher.
“This issue has resonance beyond the pediatric stem cell transplant and oncology patient population,” said study author Amy Billett, MD, of the Dana–Farber Cancer Institute and Boston Children’s Hospital in Massachusetts.
“At a time when many aspects of care are being shifted to the home and of heightened attention to safety and cost, this is the new frontier. What we learn about preventing outpatient bloodstream infections in these patients could have broad relevance.”
To determine the economic and hospitalization impact of ambulatory BSIs, Dr Billet and her colleagues retrospectively analyzed data on outpatient BSIs at Dana-Farber/Boston Children’s that occurred between January 1, 2012, and December 31, 2013, and resulted in hospitalization.
The team identified 74 BSIs in 61 patients. Sixty-nine percent of these infections were classified as central-line-associated bloodstream infections.
In 43% of BSIs, the patient’s central line had to be surgically removed. In 15% of cases, the child was transferred to the intensive care unit. Four patients died during hospitalization, and 3 of these deaths were associated with the infections.
Most of the hospitalizations analyzed—62—were due solely to BSIs. The remainder involved at least 1 other medical issue.
The median total cost of BSIs was $40,852, and the median length of hospital stay was 7 days.
The median cost was $36,611 among patients who were hospitalized for BSIs alone (n=62) and $89,935 for patients who were hospitalized for other medical issues as well. The median lengths of hospital stay were 6 days and 15 days, respectively.
The top 3 drivers of cost for all BSIs were room and board (43%), non-chemotherapy medications (22%), and procedures (11%).
Room and board accounted for 42% of charges among patients who were hospitalized for BSIs alone and 44% among the other patients. Non-chemotherapy medications accounted for 20% and 25%, respectively. And procedures accounted for 11% and 10%, respectively.
“Behind these metrics are real and serious risks to patients’ health,” said study author Chris Wong, MD, of Dana-Farber/Boston Children’s.
“The bottom line is that the dollar cost and lengthy hospital stays signal complications that could become life-threatening or delay treatment of the children’s cancer. Reducing these infections is important both for cost containment and quality of care.”

Staphylococcus infection
Photo by Bill Branson
Ambulatory bloodstream infections (BSIs) can be costly in young cancer patients and recipients of hematopoietic stem cell transplants, according to research published in Pediatric Blood & Cancer.
Among the 61 patients studied, the median cost for an ambulatory BSI was $40,852, and the median length of hospital stay was 7 days.
For patients who were hospitalized for BSI and other medical issues, the cost and length of stay were much higher.
“This issue has resonance beyond the pediatric stem cell transplant and oncology patient population,” said study author Amy Billett, MD, of the Dana–Farber Cancer Institute and Boston Children’s Hospital in Massachusetts.
“At a time when many aspects of care are being shifted to the home and of heightened attention to safety and cost, this is the new frontier. What we learn about preventing outpatient bloodstream infections in these patients could have broad relevance.”
To determine the economic and hospitalization impact of ambulatory BSIs, Dr Billet and her colleagues retrospectively analyzed data on outpatient BSIs at Dana-Farber/Boston Children’s that occurred between January 1, 2012, and December 31, 2013, and resulted in hospitalization.
The team identified 74 BSIs in 61 patients. Sixty-nine percent of these infections were classified as central-line-associated bloodstream infections.
In 43% of BSIs, the patient’s central line had to be surgically removed. In 15% of cases, the child was transferred to the intensive care unit. Four patients died during hospitalization, and 3 of these deaths were associated with the infections.
Most of the hospitalizations analyzed—62—were due solely to BSIs. The remainder involved at least 1 other medical issue.
The median total cost of BSIs was $40,852, and the median length of hospital stay was 7 days.
The median cost was $36,611 among patients who were hospitalized for BSIs alone (n=62) and $89,935 for patients who were hospitalized for other medical issues as well. The median lengths of hospital stay were 6 days and 15 days, respectively.
The top 3 drivers of cost for all BSIs were room and board (43%), non-chemotherapy medications (22%), and procedures (11%).
Room and board accounted for 42% of charges among patients who were hospitalized for BSIs alone and 44% among the other patients. Non-chemotherapy medications accounted for 20% and 25%, respectively. And procedures accounted for 11% and 10%, respectively.
“Behind these metrics are real and serious risks to patients’ health,” said study author Chris Wong, MD, of Dana-Farber/Boston Children’s.
“The bottom line is that the dollar cost and lengthy hospital stays signal complications that could become life-threatening or delay treatment of the children’s cancer. Reducing these infections is important both for cost containment and quality of care.”

Staphylococcus infection
Photo by Bill Branson
Ambulatory bloodstream infections (BSIs) can be costly in young cancer patients and recipients of hematopoietic stem cell transplants, according to research published in Pediatric Blood & Cancer.
Among the 61 patients studied, the median cost for an ambulatory BSI was $40,852, and the median length of hospital stay was 7 days.
For patients who were hospitalized for BSI and other medical issues, the cost and length of stay were much higher.
“This issue has resonance beyond the pediatric stem cell transplant and oncology patient population,” said study author Amy Billett, MD, of the Dana–Farber Cancer Institute and Boston Children’s Hospital in Massachusetts.
“At a time when many aspects of care are being shifted to the home and of heightened attention to safety and cost, this is the new frontier. What we learn about preventing outpatient bloodstream infections in these patients could have broad relevance.”
To determine the economic and hospitalization impact of ambulatory BSIs, Dr Billet and her colleagues retrospectively analyzed data on outpatient BSIs at Dana-Farber/Boston Children’s that occurred between January 1, 2012, and December 31, 2013, and resulted in hospitalization.
The team identified 74 BSIs in 61 patients. Sixty-nine percent of these infections were classified as central-line-associated bloodstream infections.
In 43% of BSIs, the patient’s central line had to be surgically removed. In 15% of cases, the child was transferred to the intensive care unit. Four patients died during hospitalization, and 3 of these deaths were associated with the infections.
Most of the hospitalizations analyzed—62—were due solely to BSIs. The remainder involved at least 1 other medical issue.
The median total cost of BSIs was $40,852, and the median length of hospital stay was 7 days.
The median cost was $36,611 among patients who were hospitalized for BSIs alone (n=62) and $89,935 for patients who were hospitalized for other medical issues as well. The median lengths of hospital stay were 6 days and 15 days, respectively.
The top 3 drivers of cost for all BSIs were room and board (43%), non-chemotherapy medications (22%), and procedures (11%).
Room and board accounted for 42% of charges among patients who were hospitalized for BSIs alone and 44% among the other patients. Non-chemotherapy medications accounted for 20% and 25%, respectively. And procedures accounted for 11% and 10%, respectively.
“Behind these metrics are real and serious risks to patients’ health,” said study author Chris Wong, MD, of Dana-Farber/Boston Children’s.
“The bottom line is that the dollar cost and lengthy hospital stays signal complications that could become life-threatening or delay treatment of the children’s cancer. Reducing these infections is important both for cost containment and quality of care.”

