User login
Massage therapy seems to benefit cancer patients

Photo courtesy of Barbara
E. Carver/New York College
of Health Professions
Massage therapy can reduce pain, fatigue, and anxiety in cancer patients, according to a review and meta-analysis published in Pain Medicine.
Massage therapy is commonly used among people seeking pain management, and research has generally supported its use.
However, there has been no published, rigorous review of the available research and evidence for massage therapy’s efficacy for pain populations, especially for cancer populations.
So Courtney Boyd, of the Samueli Institute in Alexandria, Virginia, and her colleagues set out to conduct just such a review.
The team assessed the quality of massage therapy research and evidence for its efficacy in treating pain, function-related quality of life, and health-related quality of life in cancer patients.
The researchers reviewed data from 12 high-quality studies and 4 low-quality studies.
The team said they could not assess health-related quality of life, emotional stress, or activity outcomes because too few of the studies examined these outcomes.
However, the data suggested that massage therapy can effectively reduce pain intensity or severity when compared to no treatment (standardized mean difference [SMD]=-0.20) or active comparators (SMD=-0.55).
Massage therapy also proved effective for reducing fatigue (SMD=-1.06) and anxiety (SMD=-1.24) when compared to active comparators.
Based on these results, the researchers concluded that massage therapy may have beneficial effects in cancer patients, so they should consider it as an option.
However, before definitive clinical conclusions and recommendations can be made at a policy level, specific factors surrounding the massage protocol, as well as selection of appropriate controls and standard outcomes, need to be well-understood. ![]()

Photo courtesy of Barbara
E. Carver/New York College
of Health Professions
Massage therapy can reduce pain, fatigue, and anxiety in cancer patients, according to a review and meta-analysis published in Pain Medicine.
Massage therapy is commonly used among people seeking pain management, and research has generally supported its use.
However, there has been no published, rigorous review of the available research and evidence for massage therapy’s efficacy for pain populations, especially for cancer populations.
So Courtney Boyd, of the Samueli Institute in Alexandria, Virginia, and her colleagues set out to conduct just such a review.
The team assessed the quality of massage therapy research and evidence for its efficacy in treating pain, function-related quality of life, and health-related quality of life in cancer patients.
The researchers reviewed data from 12 high-quality studies and 4 low-quality studies.
The team said they could not assess health-related quality of life, emotional stress, or activity outcomes because too few of the studies examined these outcomes.
However, the data suggested that massage therapy can effectively reduce pain intensity or severity when compared to no treatment (standardized mean difference [SMD]=-0.20) or active comparators (SMD=-0.55).
Massage therapy also proved effective for reducing fatigue (SMD=-1.06) and anxiety (SMD=-1.24) when compared to active comparators.
Based on these results, the researchers concluded that massage therapy may have beneficial effects in cancer patients, so they should consider it as an option.
However, before definitive clinical conclusions and recommendations can be made at a policy level, specific factors surrounding the massage protocol, as well as selection of appropriate controls and standard outcomes, need to be well-understood. ![]()

Photo courtesy of Barbara
E. Carver/New York College
of Health Professions
Massage therapy can reduce pain, fatigue, and anxiety in cancer patients, according to a review and meta-analysis published in Pain Medicine.
Massage therapy is commonly used among people seeking pain management, and research has generally supported its use.
However, there has been no published, rigorous review of the available research and evidence for massage therapy’s efficacy for pain populations, especially for cancer populations.
So Courtney Boyd, of the Samueli Institute in Alexandria, Virginia, and her colleagues set out to conduct just such a review.
The team assessed the quality of massage therapy research and evidence for its efficacy in treating pain, function-related quality of life, and health-related quality of life in cancer patients.
The researchers reviewed data from 12 high-quality studies and 4 low-quality studies.
The team said they could not assess health-related quality of life, emotional stress, or activity outcomes because too few of the studies examined these outcomes.
However, the data suggested that massage therapy can effectively reduce pain intensity or severity when compared to no treatment (standardized mean difference [SMD]=-0.20) or active comparators (SMD=-0.55).
Massage therapy also proved effective for reducing fatigue (SMD=-1.06) and anxiety (SMD=-1.24) when compared to active comparators.
Based on these results, the researchers concluded that massage therapy may have beneficial effects in cancer patients, so they should consider it as an option.
However, before definitive clinical conclusions and recommendations can be made at a policy level, specific factors surrounding the massage protocol, as well as selection of appropriate controls and standard outcomes, need to be well-understood. ![]()
Cancer survivors have ‘normal’ sex lives, survey says

receiving treatment
Photo by Rhoda Baer
A new study suggests cancer survivors and the general population have comparable sex lives, although cancer survivors don’t realize it.
According to a survey of more than 6500 people, cancer survivors over the age of 49 have just as much sex and similar levels of sexual function as individuals of the same age who never had cancer.
However, the cancer survivors were more likely to report being dissatisfied with their sex lives.
“We hope our findings will put cancer survivors’ concerns to rest—showing that they are just as sexually active and function just as well as others their age,” said Sarah Jackson, PhD, of University College London in the UK.
“The next stage of our research will look at why cancer patients feel less satisfied with their sex lives.”
Dr Jackson and her colleagues reported their current findings in Cancer.
The researchers set out to explore differences in sexual activity and function, as well as concerns about sex, between cancer survivors and cancer-free controls in a population-based study.
The team surveyed 3708 women (341 cancer survivors and 3367 controls) and 2982 men (220 cancer survivors and 2762 controls) aged 50 and older. Male and female cancer survivors were significantly older than controls (P<0.001 for both) and reported more comorbidities (P=0.003 for both).
Frequency
There were no significant differences in levels of sexual activity between cancer survivors and controls of either sex.
Among women, 58.2% of cancer survivors and 55.5% of controls reported having any sexual activity in the last year. Among men, the rates were 76.0% and 78.5%, respectively.
Overall, about half of the people surveyed reported having “frequent” sexual intercourse, which was defined as 2 to 3 times a month or more.
This included 49.1% of female cancer survivors, 50.1% of female controls, 49% of male cancer survivors, and 48% of male controls.
Function
The incidence of sexual problems was similar in cancer survivors and controls—both male and female.
For example, around a third of the women said they had problems becoming aroused (31.4% of cancer survivors and 31.8% of controls), and about 40% of the men had erectile dysfunction (40.3% of cancer survivors and 39.3% of controls).
Satisfaction
Despite similar levels of sexual activity and function, cancer survivors were more likely than controls to report feeling dissatisfied with their sex lives.
Among the women, 18.2% of cancer survivors and 11.8% of controls reported dissatisfaction (P=0.034). Among the men, the rates were 30.9% and 19.8%, respectively (P=0.023).
In addition, female cancer survivors were more likely to be concerned about their libido than female controls—10.2% and 7.1%, respectively (P=0.006). But there was no significant difference for the men.
Time from cancer diagnosis
The researchers also found the amount of time from cancer diagnosis was a factor affecting sexual function and concern among women but not men.
Females diagnosed with cancer less than 5 years from the time they were surveyed were more likely than female controls to report difficulty becoming aroused (55.4% and 31.8%, respectively, P=0.016) and achieving orgasm (60.6% and 28.3%, respectively, P<0.001).
The recently diagnosed females were also more likely than controls to be concerned about sexual desire (14.8% and 7.1%, respectively, P=0.007) and orgasmic experience (17.6% and 7.1%, respectively, P=0.042).
“Although some cancer treatments are known to impact on sexual function, this study suggests that the majority of cancer patients have similar sexual function and activity as the general population,” said Martin Ledwick, of Cancer Research UK, which sponsored this study.
“However, cancer patients in the study were more likely to be dissatisfied with their sex lives . . . . This highlights the need for health professionals to make sure they talk about sex with all patients—not just the ones whose sexual function is likely to be affected by their cancer or its treatment.” ![]()

receiving treatment
Photo by Rhoda Baer
A new study suggests cancer survivors and the general population have comparable sex lives, although cancer survivors don’t realize it.
According to a survey of more than 6500 people, cancer survivors over the age of 49 have just as much sex and similar levels of sexual function as individuals of the same age who never had cancer.
However, the cancer survivors were more likely to report being dissatisfied with their sex lives.
“We hope our findings will put cancer survivors’ concerns to rest—showing that they are just as sexually active and function just as well as others their age,” said Sarah Jackson, PhD, of University College London in the UK.
“The next stage of our research will look at why cancer patients feel less satisfied with their sex lives.”
Dr Jackson and her colleagues reported their current findings in Cancer.
The researchers set out to explore differences in sexual activity and function, as well as concerns about sex, between cancer survivors and cancer-free controls in a population-based study.
The team surveyed 3708 women (341 cancer survivors and 3367 controls) and 2982 men (220 cancer survivors and 2762 controls) aged 50 and older. Male and female cancer survivors were significantly older than controls (P<0.001 for both) and reported more comorbidities (P=0.003 for both).
Frequency
There were no significant differences in levels of sexual activity between cancer survivors and controls of either sex.
Among women, 58.2% of cancer survivors and 55.5% of controls reported having any sexual activity in the last year. Among men, the rates were 76.0% and 78.5%, respectively.
Overall, about half of the people surveyed reported having “frequent” sexual intercourse, which was defined as 2 to 3 times a month or more.
This included 49.1% of female cancer survivors, 50.1% of female controls, 49% of male cancer survivors, and 48% of male controls.
Function
The incidence of sexual problems was similar in cancer survivors and controls—both male and female.
For example, around a third of the women said they had problems becoming aroused (31.4% of cancer survivors and 31.8% of controls), and about 40% of the men had erectile dysfunction (40.3% of cancer survivors and 39.3% of controls).
Satisfaction
Despite similar levels of sexual activity and function, cancer survivors were more likely than controls to report feeling dissatisfied with their sex lives.
Among the women, 18.2% of cancer survivors and 11.8% of controls reported dissatisfaction (P=0.034). Among the men, the rates were 30.9% and 19.8%, respectively (P=0.023).
In addition, female cancer survivors were more likely to be concerned about their libido than female controls—10.2% and 7.1%, respectively (P=0.006). But there was no significant difference for the men.
Time from cancer diagnosis
The researchers also found the amount of time from cancer diagnosis was a factor affecting sexual function and concern among women but not men.
Females diagnosed with cancer less than 5 years from the time they were surveyed were more likely than female controls to report difficulty becoming aroused (55.4% and 31.8%, respectively, P=0.016) and achieving orgasm (60.6% and 28.3%, respectively, P<0.001).
The recently diagnosed females were also more likely than controls to be concerned about sexual desire (14.8% and 7.1%, respectively, P=0.007) and orgasmic experience (17.6% and 7.1%, respectively, P=0.042).
“Although some cancer treatments are known to impact on sexual function, this study suggests that the majority of cancer patients have similar sexual function and activity as the general population,” said Martin Ledwick, of Cancer Research UK, which sponsored this study.
“However, cancer patients in the study were more likely to be dissatisfied with their sex lives . . . . This highlights the need for health professionals to make sure they talk about sex with all patients—not just the ones whose sexual function is likely to be affected by their cancer or its treatment.” ![]()

receiving treatment
Photo by Rhoda Baer
A new study suggests cancer survivors and the general population have comparable sex lives, although cancer survivors don’t realize it.
According to a survey of more than 6500 people, cancer survivors over the age of 49 have just as much sex and similar levels of sexual function as individuals of the same age who never had cancer.
However, the cancer survivors were more likely to report being dissatisfied with their sex lives.
“We hope our findings will put cancer survivors’ concerns to rest—showing that they are just as sexually active and function just as well as others their age,” said Sarah Jackson, PhD, of University College London in the UK.
“The next stage of our research will look at why cancer patients feel less satisfied with their sex lives.”
Dr Jackson and her colleagues reported their current findings in Cancer.
The researchers set out to explore differences in sexual activity and function, as well as concerns about sex, between cancer survivors and cancer-free controls in a population-based study.
The team surveyed 3708 women (341 cancer survivors and 3367 controls) and 2982 men (220 cancer survivors and 2762 controls) aged 50 and older. Male and female cancer survivors were significantly older than controls (P<0.001 for both) and reported more comorbidities (P=0.003 for both).
Frequency
There were no significant differences in levels of sexual activity between cancer survivors and controls of either sex.
Among women, 58.2% of cancer survivors and 55.5% of controls reported having any sexual activity in the last year. Among men, the rates were 76.0% and 78.5%, respectively.
Overall, about half of the people surveyed reported having “frequent” sexual intercourse, which was defined as 2 to 3 times a month or more.
This included 49.1% of female cancer survivors, 50.1% of female controls, 49% of male cancer survivors, and 48% of male controls.
Function
The incidence of sexual problems was similar in cancer survivors and controls—both male and female.
For example, around a third of the women said they had problems becoming aroused (31.4% of cancer survivors and 31.8% of controls), and about 40% of the men had erectile dysfunction (40.3% of cancer survivors and 39.3% of controls).
Satisfaction
Despite similar levels of sexual activity and function, cancer survivors were more likely than controls to report feeling dissatisfied with their sex lives.
Among the women, 18.2% of cancer survivors and 11.8% of controls reported dissatisfaction (P=0.034). Among the men, the rates were 30.9% and 19.8%, respectively (P=0.023).
In addition, female cancer survivors were more likely to be concerned about their libido than female controls—10.2% and 7.1%, respectively (P=0.006). But there was no significant difference for the men.
Time from cancer diagnosis
The researchers also found the amount of time from cancer diagnosis was a factor affecting sexual function and concern among women but not men.
Females diagnosed with cancer less than 5 years from the time they were surveyed were more likely than female controls to report difficulty becoming aroused (55.4% and 31.8%, respectively, P=0.016) and achieving orgasm (60.6% and 28.3%, respectively, P<0.001).
The recently diagnosed females were also more likely than controls to be concerned about sexual desire (14.8% and 7.1%, respectively, P=0.007) and orgasmic experience (17.6% and 7.1%, respectively, P=0.042).
“Although some cancer treatments are known to impact on sexual function, this study suggests that the majority of cancer patients have similar sexual function and activity as the general population,” said Martin Ledwick, of Cancer Research UK, which sponsored this study.
“However, cancer patients in the study were more likely to be dissatisfied with their sex lives . . . . This highlights the need for health professionals to make sure they talk about sex with all patients—not just the ones whose sexual function is likely to be affected by their cancer or its treatment.” ![]()
Music may alleviate cancer patients’ symptoms

Photo by Lars Frantzen
Results of a systematic review suggest music can help alleviate symptoms of anxiety, pain, and fatigue in cancer patients.
The review included more than 50 studies investigating the impact of music therapy—a personalized music experience offered by trained music therapists—and music medicine—listening to pre-recorded music provided by a doctor or nurse—on psychological and physical outcomes in people with cancer.
“We found that music therapy interventions specifically help improve patients’ quality of life,” said study author Joke Bradt, PhD, of Drexel University in Philadelphia, Pennsylvania.
“These are important findings, as these outcomes play an important role in patients’ overall well-being.”
Dr Bradt and her colleagues reported their findings in Cochrane Database of Systematic Reviews.
The researchers examined 52 trials including 3731 cancer patients. The music interventions were classified as music therapy in 23 of the trials and as music medicine in 29 trials.
Analyses suggested that both types of music interventions positively impacted patients. The interventions had a moderate-to-strong effect on anxiety, a strong effect on pain reduction, and a small-to-moderate effect on fatigue.
Small reductions in heart and respiratory rates, as well as lowered blood pressure, were linked to the interventions as well.
In addition, the researchers observed a moderate increase in patients’ quality of life with music therapy but not music medicine.
The team could not determine the effect of music interventions on depression due to the low quality of evidence. And there was no evidence that the interventions improve mood, distress, or physical functioning, but there were few trials investigating these outcomes.
Similarly, the researchers said they could not draw any conclusions about the effect of music interventions on immunologic functioning, coping, resilience, or communication because there were not enough trials evaluating these outcomes.
Still, the researchers hope music interventions will become more widely used, in light of the potential benefits to cancer patients.
“We hope that the findings of this review will encourage healthcare providers in medical settings to seriously consider the use of music therapy in the psychosocial care of people with cancer,” Dr Bradt said. ![]()

Photo by Lars Frantzen
Results of a systematic review suggest music can help alleviate symptoms of anxiety, pain, and fatigue in cancer patients.
The review included more than 50 studies investigating the impact of music therapy—a personalized music experience offered by trained music therapists—and music medicine—listening to pre-recorded music provided by a doctor or nurse—on psychological and physical outcomes in people with cancer.
“We found that music therapy interventions specifically help improve patients’ quality of life,” said study author Joke Bradt, PhD, of Drexel University in Philadelphia, Pennsylvania.
“These are important findings, as these outcomes play an important role in patients’ overall well-being.”
Dr Bradt and her colleagues reported their findings in Cochrane Database of Systematic Reviews.
The researchers examined 52 trials including 3731 cancer patients. The music interventions were classified as music therapy in 23 of the trials and as music medicine in 29 trials.
Analyses suggested that both types of music interventions positively impacted patients. The interventions had a moderate-to-strong effect on anxiety, a strong effect on pain reduction, and a small-to-moderate effect on fatigue.
Small reductions in heart and respiratory rates, as well as lowered blood pressure, were linked to the interventions as well.
In addition, the researchers observed a moderate increase in patients’ quality of life with music therapy but not music medicine.
The team could not determine the effect of music interventions on depression due to the low quality of evidence. And there was no evidence that the interventions improve mood, distress, or physical functioning, but there were few trials investigating these outcomes.
Similarly, the researchers said they could not draw any conclusions about the effect of music interventions on immunologic functioning, coping, resilience, or communication because there were not enough trials evaluating these outcomes.
Still, the researchers hope music interventions will become more widely used, in light of the potential benefits to cancer patients.
“We hope that the findings of this review will encourage healthcare providers in medical settings to seriously consider the use of music therapy in the psychosocial care of people with cancer,” Dr Bradt said. ![]()

Photo by Lars Frantzen
Results of a systematic review suggest music can help alleviate symptoms of anxiety, pain, and fatigue in cancer patients.
The review included more than 50 studies investigating the impact of music therapy—a personalized music experience offered by trained music therapists—and music medicine—listening to pre-recorded music provided by a doctor or nurse—on psychological and physical outcomes in people with cancer.
“We found that music therapy interventions specifically help improve patients’ quality of life,” said study author Joke Bradt, PhD, of Drexel University in Philadelphia, Pennsylvania.
“These are important findings, as these outcomes play an important role in patients’ overall well-being.”
Dr Bradt and her colleagues reported their findings in Cochrane Database of Systematic Reviews.
The researchers examined 52 trials including 3731 cancer patients. The music interventions were classified as music therapy in 23 of the trials and as music medicine in 29 trials.
Analyses suggested that both types of music interventions positively impacted patients. The interventions had a moderate-to-strong effect on anxiety, a strong effect on pain reduction, and a small-to-moderate effect on fatigue.
Small reductions in heart and respiratory rates, as well as lowered blood pressure, were linked to the interventions as well.
In addition, the researchers observed a moderate increase in patients’ quality of life with music therapy but not music medicine.
The team could not determine the effect of music interventions on depression due to the low quality of evidence. And there was no evidence that the interventions improve mood, distress, or physical functioning, but there were few trials investigating these outcomes.
Similarly, the researchers said they could not draw any conclusions about the effect of music interventions on immunologic functioning, coping, resilience, or communication because there were not enough trials evaluating these outcomes.
Still, the researchers hope music interventions will become more widely used, in light of the potential benefits to cancer patients.
“We hope that the findings of this review will encourage healthcare providers in medical settings to seriously consider the use of music therapy in the psychosocial care of people with cancer,” Dr Bradt said. ![]()
Microneedle system could replace blood draws, team says
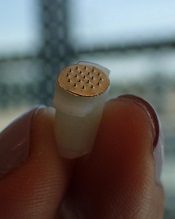
Photo courtesy of
Sahan Ranamukhaarachchi
A new microneedle drug monitoring system could one day replace invasive blood draws, according to researchers.
The system consists of a small, thin patch that is pressed against a patient’s arm during medical treatment and measures drugs in the bloodstream painlessly without drawing any blood.
The tiny projections on this patch resemble hollow cones and don’t pierce the skin like a standard hypodermic needle.
The researchers described this system in Scientific Reports.
“Many groups are researching microneedle technology for painless vaccines and drug delivery,” said study author Sahan Ranamukhaarachchi, a PhD student at the University of British Columbia (UBC) in Vancouver, British Columbia, Canada. “Using them to painlessly monitor drugs is a newer idea.”
The microneedle system Ranamukhaarachchi and his colleagues created was developed to monitor the antibiotic vancomycin. Patients taking vancomycin must be closely monitored because the drug can cause life-threatening side effects, so the patients undergo 3 to 4 blood draws per day.
The researchers discovered they could use fluid found just below the outer layer of skin, instead of blood, to monitor levels of vancomycin in the bloodstream.
The microneedle patch collects a tiny amount of the fluid, less than 1 nL, and a reaction occurs on the inside of the microneedles that can be detected using an optical sensor. This allows the user to quickly determine the concentration of vancomycin.
“This is probably one of the smallest probe volumes ever recorded for a medically relevant analysis,” said study author Urs Häfeli, PhD, of UBC.
This microneedle drug monitoring system was developed out of a research collaboration between Dr Häfeli and Boris Stoeber, PhD, also of UBC. The system is being commercialized by the UBC spin-off Microdermics Inc. ![]()
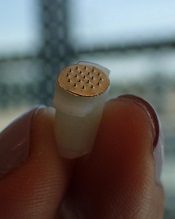
Photo courtesy of
Sahan Ranamukhaarachchi
A new microneedle drug monitoring system could one day replace invasive blood draws, according to researchers.
The system consists of a small, thin patch that is pressed against a patient’s arm during medical treatment and measures drugs in the bloodstream painlessly without drawing any blood.
The tiny projections on this patch resemble hollow cones and don’t pierce the skin like a standard hypodermic needle.
The researchers described this system in Scientific Reports.
“Many groups are researching microneedle technology for painless vaccines and drug delivery,” said study author Sahan Ranamukhaarachchi, a PhD student at the University of British Columbia (UBC) in Vancouver, British Columbia, Canada. “Using them to painlessly monitor drugs is a newer idea.”
The microneedle system Ranamukhaarachchi and his colleagues created was developed to monitor the antibiotic vancomycin. Patients taking vancomycin must be closely monitored because the drug can cause life-threatening side effects, so the patients undergo 3 to 4 blood draws per day.
The researchers discovered they could use fluid found just below the outer layer of skin, instead of blood, to monitor levels of vancomycin in the bloodstream.
The microneedle patch collects a tiny amount of the fluid, less than 1 nL, and a reaction occurs on the inside of the microneedles that can be detected using an optical sensor. This allows the user to quickly determine the concentration of vancomycin.
“This is probably one of the smallest probe volumes ever recorded for a medically relevant analysis,” said study author Urs Häfeli, PhD, of UBC.
This microneedle drug monitoring system was developed out of a research collaboration between Dr Häfeli and Boris Stoeber, PhD, also of UBC. The system is being commercialized by the UBC spin-off Microdermics Inc. ![]()
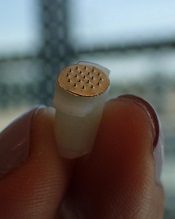
Photo courtesy of
Sahan Ranamukhaarachchi
A new microneedle drug monitoring system could one day replace invasive blood draws, according to researchers.
The system consists of a small, thin patch that is pressed against a patient’s arm during medical treatment and measures drugs in the bloodstream painlessly without drawing any blood.
The tiny projections on this patch resemble hollow cones and don’t pierce the skin like a standard hypodermic needle.
The researchers described this system in Scientific Reports.
“Many groups are researching microneedle technology for painless vaccines and drug delivery,” said study author Sahan Ranamukhaarachchi, a PhD student at the University of British Columbia (UBC) in Vancouver, British Columbia, Canada. “Using them to painlessly monitor drugs is a newer idea.”
The microneedle system Ranamukhaarachchi and his colleagues created was developed to monitor the antibiotic vancomycin. Patients taking vancomycin must be closely monitored because the drug can cause life-threatening side effects, so the patients undergo 3 to 4 blood draws per day.
The researchers discovered they could use fluid found just below the outer layer of skin, instead of blood, to monitor levels of vancomycin in the bloodstream.
The microneedle patch collects a tiny amount of the fluid, less than 1 nL, and a reaction occurs on the inside of the microneedles that can be detected using an optical sensor. This allows the user to quickly determine the concentration of vancomycin.
“This is probably one of the smallest probe volumes ever recorded for a medically relevant analysis,” said study author Urs Häfeli, PhD, of UBC.
This microneedle drug monitoring system was developed out of a research collaboration between Dr Häfeli and Boris Stoeber, PhD, also of UBC. The system is being commercialized by the UBC spin-off Microdermics Inc. ![]()
Blood disorders prove costly for European economy

chemotherapy
Photo by Rhoda Baer
Malignant and non-malignant blood disorders cost 31 European countries a total of €23 billion in 2012, according to a pair of papers published in The Lancet Haematology.
Healthcare costs accounted for €16 billion of the total costs, with €7 billion for hospital inpatient care and €4 billion for medications.
Informal care (from friends and relatives) cost €1.6 billion, productivity losses due to mortality cost €2.5 billion, and morbidity cost €3 billion.
Researchers determined these figures by analyzing data from international health organizations (WHO and EUROSTAT), as well as national ministries of health and statistical institutes.
The team estimated the economic burden of malignant and non-malignant blood disorders in 2012 for all 28 countries in the European Union (EU), as well as Iceland, Norway, and Switzerland.
The costs considered were healthcare costs (primary care, accident and emergency care, hospital inpatient and outpatient care, and drugs), informal care costs (from friends and relatives), and productivity losses (due to premature death and people being unable to work due to illness).
Malignant blood disorders
In one paper, the researchers noted that the total economic cost of blood cancers to the 31 countries studied was €12 billion in 2012. Healthcare costs measured €7.3 billion (62% of total costs), productivity losses cost €3.6 billion (30%), and informal care cost €1 billion (8%).
In the 28 EU countries, blood cancers represented 8% of the total cancer costs (€143 billion), meaning that blood cancers are the fourth most expensive type of cancer after lung (15%), breast (12%), and colorectal (10%) cancers.
When considering healthcare costs alone, blood cancers were second only to breast cancers (12% vs 13% of healthcare costs for all cancers).
In 2012, blood cancers cost, on average, €14,674 per patient in the EU (€15,126 in all 31 countries), which is almost 2 times higher than the average cost per patient across all cancers (€7929 in the EU).
The researchers said this difference may be due to the longer length of hospital stay observed for patients with blood cancers (14 days, on average, compared to 8 days across all cancers).
Another potential reason is that blood cancers are increasingly treated with complex, long-term treatments (including stem cell transplants, multi-agent chemotherapy, and radiotherapy) and diagnosed via extensive procedures.
The costs of blood cancers varied widely between the countries studied, but the reasons for this were unclear. For instance, the average healthcare costs in Finland were nearly twice as high as in Belgium (€18,014 vs €9596), despite both countries having similar national income per capita.
Non-malignant blood disorders
In the other paper, the researchers said the total economic cost of non-malignant blood disorders to the 31 countries studied was €11 billion in 2012. Healthcare costs accounted for €8 billion (75% of total costs), productivity losses for €2 billion (19%), and informal care for €618 million (6%).
Averaged across the population studied, non-malignant blood disorders represented an annual healthcare cost of €159 per 10 citizens.
“Non-malignant blood disorders cost the European economy nearly as much as all blood cancers combined,” said Jose Leal, DPhil, of the University of Oxford in the UK.
“We found wide differences in the cost of treating blood disorders in different countries, likely linked to the significant differences in the access and delivery of care for patients with blood disorders. Our findings suggest there is a need to harmonize care of blood disorders across Europe in a cost-effective way.” ![]()

chemotherapy
Photo by Rhoda Baer
Malignant and non-malignant blood disorders cost 31 European countries a total of €23 billion in 2012, according to a pair of papers published in The Lancet Haematology.
Healthcare costs accounted for €16 billion of the total costs, with €7 billion for hospital inpatient care and €4 billion for medications.
Informal care (from friends and relatives) cost €1.6 billion, productivity losses due to mortality cost €2.5 billion, and morbidity cost €3 billion.
Researchers determined these figures by analyzing data from international health organizations (WHO and EUROSTAT), as well as national ministries of health and statistical institutes.
The team estimated the economic burden of malignant and non-malignant blood disorders in 2012 for all 28 countries in the European Union (EU), as well as Iceland, Norway, and Switzerland.
The costs considered were healthcare costs (primary care, accident and emergency care, hospital inpatient and outpatient care, and drugs), informal care costs (from friends and relatives), and productivity losses (due to premature death and people being unable to work due to illness).
Malignant blood disorders
In one paper, the researchers noted that the total economic cost of blood cancers to the 31 countries studied was €12 billion in 2012. Healthcare costs measured €7.3 billion (62% of total costs), productivity losses cost €3.6 billion (30%), and informal care cost €1 billion (8%).
In the 28 EU countries, blood cancers represented 8% of the total cancer costs (€143 billion), meaning that blood cancers are the fourth most expensive type of cancer after lung (15%), breast (12%), and colorectal (10%) cancers.
When considering healthcare costs alone, blood cancers were second only to breast cancers (12% vs 13% of healthcare costs for all cancers).
In 2012, blood cancers cost, on average, €14,674 per patient in the EU (€15,126 in all 31 countries), which is almost 2 times higher than the average cost per patient across all cancers (€7929 in the EU).
The researchers said this difference may be due to the longer length of hospital stay observed for patients with blood cancers (14 days, on average, compared to 8 days across all cancers).
Another potential reason is that blood cancers are increasingly treated with complex, long-term treatments (including stem cell transplants, multi-agent chemotherapy, and radiotherapy) and diagnosed via extensive procedures.
The costs of blood cancers varied widely between the countries studied, but the reasons for this were unclear. For instance, the average healthcare costs in Finland were nearly twice as high as in Belgium (€18,014 vs €9596), despite both countries having similar national income per capita.
Non-malignant blood disorders
In the other paper, the researchers said the total economic cost of non-malignant blood disorders to the 31 countries studied was €11 billion in 2012. Healthcare costs accounted for €8 billion (75% of total costs), productivity losses for €2 billion (19%), and informal care for €618 million (6%).
Averaged across the population studied, non-malignant blood disorders represented an annual healthcare cost of €159 per 10 citizens.
“Non-malignant blood disorders cost the European economy nearly as much as all blood cancers combined,” said Jose Leal, DPhil, of the University of Oxford in the UK.
“We found wide differences in the cost of treating blood disorders in different countries, likely linked to the significant differences in the access and delivery of care for patients with blood disorders. Our findings suggest there is a need to harmonize care of blood disorders across Europe in a cost-effective way.” ![]()

chemotherapy
Photo by Rhoda Baer
Malignant and non-malignant blood disorders cost 31 European countries a total of €23 billion in 2012, according to a pair of papers published in The Lancet Haematology.
Healthcare costs accounted for €16 billion of the total costs, with €7 billion for hospital inpatient care and €4 billion for medications.
Informal care (from friends and relatives) cost €1.6 billion, productivity losses due to mortality cost €2.5 billion, and morbidity cost €3 billion.
Researchers determined these figures by analyzing data from international health organizations (WHO and EUROSTAT), as well as national ministries of health and statistical institutes.
The team estimated the economic burden of malignant and non-malignant blood disorders in 2012 for all 28 countries in the European Union (EU), as well as Iceland, Norway, and Switzerland.
The costs considered were healthcare costs (primary care, accident and emergency care, hospital inpatient and outpatient care, and drugs), informal care costs (from friends and relatives), and productivity losses (due to premature death and people being unable to work due to illness).
Malignant blood disorders
In one paper, the researchers noted that the total economic cost of blood cancers to the 31 countries studied was €12 billion in 2012. Healthcare costs measured €7.3 billion (62% of total costs), productivity losses cost €3.6 billion (30%), and informal care cost €1 billion (8%).
In the 28 EU countries, blood cancers represented 8% of the total cancer costs (€143 billion), meaning that blood cancers are the fourth most expensive type of cancer after lung (15%), breast (12%), and colorectal (10%) cancers.
When considering healthcare costs alone, blood cancers were second only to breast cancers (12% vs 13% of healthcare costs for all cancers).
In 2012, blood cancers cost, on average, €14,674 per patient in the EU (€15,126 in all 31 countries), which is almost 2 times higher than the average cost per patient across all cancers (€7929 in the EU).
The researchers said this difference may be due to the longer length of hospital stay observed for patients with blood cancers (14 days, on average, compared to 8 days across all cancers).
Another potential reason is that blood cancers are increasingly treated with complex, long-term treatments (including stem cell transplants, multi-agent chemotherapy, and radiotherapy) and diagnosed via extensive procedures.
The costs of blood cancers varied widely between the countries studied, but the reasons for this were unclear. For instance, the average healthcare costs in Finland were nearly twice as high as in Belgium (€18,014 vs €9596), despite both countries having similar national income per capita.
Non-malignant blood disorders
In the other paper, the researchers said the total economic cost of non-malignant blood disorders to the 31 countries studied was €11 billion in 2012. Healthcare costs accounted for €8 billion (75% of total costs), productivity losses for €2 billion (19%), and informal care for €618 million (6%).
Averaged across the population studied, non-malignant blood disorders represented an annual healthcare cost of €159 per 10 citizens.
“Non-malignant blood disorders cost the European economy nearly as much as all blood cancers combined,” said Jose Leal, DPhil, of the University of Oxford in the UK.
“We found wide differences in the cost of treating blood disorders in different countries, likely linked to the significant differences in the access and delivery of care for patients with blood disorders. Our findings suggest there is a need to harmonize care of blood disorders across Europe in a cost-effective way.” ![]()
Fertility concerns of female cancer survivors

Photo by Vera Kratochvil
A new study indicates that many young adult female cancer survivors do not receive adequate information about their fertility as part of their survivorship care, despite having concerns about their ability to bear children in the future.
The research, published in Cancer, suggests a need for better resources to support cancer survivors in making informed decisions about their reproductive options after they complete treatment.
To conduct this study, Catherine Benedict, PhD, of North Shore-Long Island Jewish Medical Center in Manhasset, New York, and her colleagues asked female cancer survivors to complete a web-based, anonymous survey.
There were 346 participants. They had an average age of 29.9 and had completed treatment an average of 4.9 years earlier.
The investigators focused on a subgroup of 179 women with uncertain fertility status who had not previously undergone or attempted fertility preservation, either before or after their cancer treatment, and who either wanted future children or were unsure.
Many of these women said they did not have enough information concerning their risk of infertility (58%), risk of early menopause (60%), options to assess their fertility (62%), options to preserve their fertility (51%), or options for alternative family building (43%).
The women’s greatest reproductive concerns were potential fertility problems and the health of a future child. Sixty-four percent of the women said they were concerned about not being able to have children (or more children), and 59% were worried about passing the risk of cancer on to their future children.
Only 13% of women said they were well informed about options for preserving fertility, and 74% were unclear about their personal values regarding fertility preservation.
Seventy percent of the women said they hadn’t received enough advice on fertility preservation, and 35% said they didn’t have enough support to make a decision about fertility preservation.
The investigators found a significant association between greater unmet information needs and higher levels of decisional conflict about fertility preservation (P<0.001).
On the other hand, having undergone a fertility evaluation after treatment was associated with lower decisional conflict (P=0.02).
The investigators said these findings establish the need for support services to help young female cancer survivors make decisions about fertility preservation and family-building as part of survivorship care.
The literature has largely focused on the clinical and support needs of women making fertility decisions before their treatment begins, but most patients do not preserve their fertility before treatment for a number of reasons, despite wanting children in the future.
“The potential loss of fertility has been described in the literature as being almost as painful, if not more so, than the cancer diagnosis itself,” Dr Benedict said.
“Failure to provide information and address concerns with respect to fertility-related decisions may have lasting consequences for young women who hope to move on from their cancer experience to achieve important life goals such as having children. For women at risk for early menopause, delaying fertility-related decisions may cause them to miss their narrowed window of opportunity to preserve their fertility, if desired.” ![]()

Photo by Vera Kratochvil
A new study indicates that many young adult female cancer survivors do not receive adequate information about their fertility as part of their survivorship care, despite having concerns about their ability to bear children in the future.
The research, published in Cancer, suggests a need for better resources to support cancer survivors in making informed decisions about their reproductive options after they complete treatment.
To conduct this study, Catherine Benedict, PhD, of North Shore-Long Island Jewish Medical Center in Manhasset, New York, and her colleagues asked female cancer survivors to complete a web-based, anonymous survey.
There were 346 participants. They had an average age of 29.9 and had completed treatment an average of 4.9 years earlier.
The investigators focused on a subgroup of 179 women with uncertain fertility status who had not previously undergone or attempted fertility preservation, either before or after their cancer treatment, and who either wanted future children or were unsure.
Many of these women said they did not have enough information concerning their risk of infertility (58%), risk of early menopause (60%), options to assess their fertility (62%), options to preserve their fertility (51%), or options for alternative family building (43%).
The women’s greatest reproductive concerns were potential fertility problems and the health of a future child. Sixty-four percent of the women said they were concerned about not being able to have children (or more children), and 59% were worried about passing the risk of cancer on to their future children.
Only 13% of women said they were well informed about options for preserving fertility, and 74% were unclear about their personal values regarding fertility preservation.
Seventy percent of the women said they hadn’t received enough advice on fertility preservation, and 35% said they didn’t have enough support to make a decision about fertility preservation.
The investigators found a significant association between greater unmet information needs and higher levels of decisional conflict about fertility preservation (P<0.001).
On the other hand, having undergone a fertility evaluation after treatment was associated with lower decisional conflict (P=0.02).
The investigators said these findings establish the need for support services to help young female cancer survivors make decisions about fertility preservation and family-building as part of survivorship care.
The literature has largely focused on the clinical and support needs of women making fertility decisions before their treatment begins, but most patients do not preserve their fertility before treatment for a number of reasons, despite wanting children in the future.
“The potential loss of fertility has been described in the literature as being almost as painful, if not more so, than the cancer diagnosis itself,” Dr Benedict said.
“Failure to provide information and address concerns with respect to fertility-related decisions may have lasting consequences for young women who hope to move on from their cancer experience to achieve important life goals such as having children. For women at risk for early menopause, delaying fertility-related decisions may cause them to miss their narrowed window of opportunity to preserve their fertility, if desired.” ![]()

Photo by Vera Kratochvil
A new study indicates that many young adult female cancer survivors do not receive adequate information about their fertility as part of their survivorship care, despite having concerns about their ability to bear children in the future.
The research, published in Cancer, suggests a need for better resources to support cancer survivors in making informed decisions about their reproductive options after they complete treatment.
To conduct this study, Catherine Benedict, PhD, of North Shore-Long Island Jewish Medical Center in Manhasset, New York, and her colleagues asked female cancer survivors to complete a web-based, anonymous survey.
There were 346 participants. They had an average age of 29.9 and had completed treatment an average of 4.9 years earlier.
The investigators focused on a subgroup of 179 women with uncertain fertility status who had not previously undergone or attempted fertility preservation, either before or after their cancer treatment, and who either wanted future children or were unsure.
Many of these women said they did not have enough information concerning their risk of infertility (58%), risk of early menopause (60%), options to assess their fertility (62%), options to preserve their fertility (51%), or options for alternative family building (43%).
The women’s greatest reproductive concerns were potential fertility problems and the health of a future child. Sixty-four percent of the women said they were concerned about not being able to have children (or more children), and 59% were worried about passing the risk of cancer on to their future children.
Only 13% of women said they were well informed about options for preserving fertility, and 74% were unclear about their personal values regarding fertility preservation.
Seventy percent of the women said they hadn’t received enough advice on fertility preservation, and 35% said they didn’t have enough support to make a decision about fertility preservation.
The investigators found a significant association between greater unmet information needs and higher levels of decisional conflict about fertility preservation (P<0.001).
On the other hand, having undergone a fertility evaluation after treatment was associated with lower decisional conflict (P=0.02).
The investigators said these findings establish the need for support services to help young female cancer survivors make decisions about fertility preservation and family-building as part of survivorship care.
The literature has largely focused on the clinical and support needs of women making fertility decisions before their treatment begins, but most patients do not preserve their fertility before treatment for a number of reasons, despite wanting children in the future.
“The potential loss of fertility has been described in the literature as being almost as painful, if not more so, than the cancer diagnosis itself,” Dr Benedict said.
“Failure to provide information and address concerns with respect to fertility-related decisions may have lasting consequences for young women who hope to move on from their cancer experience to achieve important life goals such as having children. For women at risk for early menopause, delaying fertility-related decisions may cause them to miss their narrowed window of opportunity to preserve their fertility, if desired.” ![]()
Patients may be uninformed about risks of warfarin

ATHENS—A study of patients taking warfarin suggests many do not fully understand the risks associated with the drug.
Researchers asked patients to complete a questionnaire on warfarin use and found that, on average, patients answered 64% of the questions correctly.
The patients tended to be the least informed about food and drug interactions and which side effects necessitate a call or visit to the doctor.
Kjersti Oterhals, RN, PhD, of Haukeland University Hospital in Bergen, Norway, and her colleagues presented these findings at EuroHeartCare 2016 (abstract 36).
“The stroke and bleeding complications from warfarin can be fatal,” Dr Oterhals noted. “Worldwide, warfarin causes the most deaths from drug-related side effects. Patients need to know what foods and drugs have an impact on how warfarin works and what to do if they have symptoms of an overdose or underdose.”
Dr Oterhals and her colleagues evaluated warfarin knowledge in 404 patients with aortic stenosis. The patients’ mean age was 68, and 70% were male.
Nearly two-thirds of the patients (63%) were taking warfarin because they had a mechanical valve, and 24% were taking the drug because they had atrial fibrillation. The remaining patients were taking the drug for unknown reasons (6%) or “other” reasons (7%).
The patients received a postal questionnaire with 28 multiple-choice questions about warfarin. On average, patients answered 18 of the 28 questions correctly. However, 22% of patients answered less than half of the questions correctly.
The questions that were most often answered incorrectly were those concerning food and drug interactions and when to call or see a doctor.
For example, patients were asked which of the following foods would interfere with warfarin: celery, carrots, coleslaw, or green beans. Only 25% correctly said coleslaw. Most patients answered green beans.
“Patients often think green vegetables have the most vitamin K, but that’s not true,” Dr Oterhals said. “Brassica vegetables such as cabbage, broccoli, and cauliflower are rich sources.”
“Patients do not have to avoid these foods, but they should eat an equal amount every week because the vitamin K will decrease their INR and put them at increased risk of thrombosis or embolism. Patients who like to eat a lot of vitamin K-containing foods can take a higher warfarin dosage, but they need to be consistent.”
Dr Oterhals and her colleagues also found that 80% of patients knew they should go directly to the emergency room if they had nose bleeding that would not stop. However, only 45% of patients correctly said diarrhea for more than one day necessitates a visit to the doctor.
The study also showed that increased age was associated with a decrease in correct answers.
“We can only speculate why,” Dr Oterhals said. “Younger people tend to seek out information about how to manage their disease, while the older generation wants the doctor to tell them what to do.”
“Motivated patients should be offered an INR testing kit so that they can monitor their levels and adjust the warfarin dose themselves, just as patients with diabetes who use insulin do. It enables patients to travel and try new foods without having to find a clinic to get tested. Patients tell me that hot weather increases their INR, while another found out while in Asia that nori decreased his INR.”
“Warfarin is a life-saving drug but can be deadly if not used carefully. Health professionals have a responsibility to educate patients, but, unfortunately, even cardiac nurses do not know enough. There is an urgent need to improve health professionals’ warfarin knowledge so they can educate patients.” ![]()

ATHENS—A study of patients taking warfarin suggests many do not fully understand the risks associated with the drug.
Researchers asked patients to complete a questionnaire on warfarin use and found that, on average, patients answered 64% of the questions correctly.
The patients tended to be the least informed about food and drug interactions and which side effects necessitate a call or visit to the doctor.
Kjersti Oterhals, RN, PhD, of Haukeland University Hospital in Bergen, Norway, and her colleagues presented these findings at EuroHeartCare 2016 (abstract 36).
“The stroke and bleeding complications from warfarin can be fatal,” Dr Oterhals noted. “Worldwide, warfarin causes the most deaths from drug-related side effects. Patients need to know what foods and drugs have an impact on how warfarin works and what to do if they have symptoms of an overdose or underdose.”
Dr Oterhals and her colleagues evaluated warfarin knowledge in 404 patients with aortic stenosis. The patients’ mean age was 68, and 70% were male.
Nearly two-thirds of the patients (63%) were taking warfarin because they had a mechanical valve, and 24% were taking the drug because they had atrial fibrillation. The remaining patients were taking the drug for unknown reasons (6%) or “other” reasons (7%).
The patients received a postal questionnaire with 28 multiple-choice questions about warfarin. On average, patients answered 18 of the 28 questions correctly. However, 22% of patients answered less than half of the questions correctly.
The questions that were most often answered incorrectly were those concerning food and drug interactions and when to call or see a doctor.
For example, patients were asked which of the following foods would interfere with warfarin: celery, carrots, coleslaw, or green beans. Only 25% correctly said coleslaw. Most patients answered green beans.
“Patients often think green vegetables have the most vitamin K, but that’s not true,” Dr Oterhals said. “Brassica vegetables such as cabbage, broccoli, and cauliflower are rich sources.”
“Patients do not have to avoid these foods, but they should eat an equal amount every week because the vitamin K will decrease their INR and put them at increased risk of thrombosis or embolism. Patients who like to eat a lot of vitamin K-containing foods can take a higher warfarin dosage, but they need to be consistent.”
Dr Oterhals and her colleagues also found that 80% of patients knew they should go directly to the emergency room if they had nose bleeding that would not stop. However, only 45% of patients correctly said diarrhea for more than one day necessitates a visit to the doctor.
The study also showed that increased age was associated with a decrease in correct answers.
“We can only speculate why,” Dr Oterhals said. “Younger people tend to seek out information about how to manage their disease, while the older generation wants the doctor to tell them what to do.”
“Motivated patients should be offered an INR testing kit so that they can monitor their levels and adjust the warfarin dose themselves, just as patients with diabetes who use insulin do. It enables patients to travel and try new foods without having to find a clinic to get tested. Patients tell me that hot weather increases their INR, while another found out while in Asia that nori decreased his INR.”
“Warfarin is a life-saving drug but can be deadly if not used carefully. Health professionals have a responsibility to educate patients, but, unfortunately, even cardiac nurses do not know enough. There is an urgent need to improve health professionals’ warfarin knowledge so they can educate patients.” ![]()

ATHENS—A study of patients taking warfarin suggests many do not fully understand the risks associated with the drug.
Researchers asked patients to complete a questionnaire on warfarin use and found that, on average, patients answered 64% of the questions correctly.
The patients tended to be the least informed about food and drug interactions and which side effects necessitate a call or visit to the doctor.
Kjersti Oterhals, RN, PhD, of Haukeland University Hospital in Bergen, Norway, and her colleagues presented these findings at EuroHeartCare 2016 (abstract 36).
“The stroke and bleeding complications from warfarin can be fatal,” Dr Oterhals noted. “Worldwide, warfarin causes the most deaths from drug-related side effects. Patients need to know what foods and drugs have an impact on how warfarin works and what to do if they have symptoms of an overdose or underdose.”
Dr Oterhals and her colleagues evaluated warfarin knowledge in 404 patients with aortic stenosis. The patients’ mean age was 68, and 70% were male.
Nearly two-thirds of the patients (63%) were taking warfarin because they had a mechanical valve, and 24% were taking the drug because they had atrial fibrillation. The remaining patients were taking the drug for unknown reasons (6%) or “other” reasons (7%).
The patients received a postal questionnaire with 28 multiple-choice questions about warfarin. On average, patients answered 18 of the 28 questions correctly. However, 22% of patients answered less than half of the questions correctly.
The questions that were most often answered incorrectly were those concerning food and drug interactions and when to call or see a doctor.
For example, patients were asked which of the following foods would interfere with warfarin: celery, carrots, coleslaw, or green beans. Only 25% correctly said coleslaw. Most patients answered green beans.
“Patients often think green vegetables have the most vitamin K, but that’s not true,” Dr Oterhals said. “Brassica vegetables such as cabbage, broccoli, and cauliflower are rich sources.”
“Patients do not have to avoid these foods, but they should eat an equal amount every week because the vitamin K will decrease their INR and put them at increased risk of thrombosis or embolism. Patients who like to eat a lot of vitamin K-containing foods can take a higher warfarin dosage, but they need to be consistent.”
Dr Oterhals and her colleagues also found that 80% of patients knew they should go directly to the emergency room if they had nose bleeding that would not stop. However, only 45% of patients correctly said diarrhea for more than one day necessitates a visit to the doctor.
The study also showed that increased age was associated with a decrease in correct answers.
“We can only speculate why,” Dr Oterhals said. “Younger people tend to seek out information about how to manage their disease, while the older generation wants the doctor to tell them what to do.”
“Motivated patients should be offered an INR testing kit so that they can monitor their levels and adjust the warfarin dose themselves, just as patients with diabetes who use insulin do. It enables patients to travel and try new foods without having to find a clinic to get tested. Patients tell me that hot weather increases their INR, while another found out while in Asia that nori decreased his INR.”
“Warfarin is a life-saving drug but can be deadly if not used carefully. Health professionals have a responsibility to educate patients, but, unfortunately, even cardiac nurses do not know enough. There is an urgent need to improve health professionals’ warfarin knowledge so they can educate patients.”
Intervention helps parents cope with kids’ HSCT

Photo by Chad McNeeley
A new social-cognitive intervention can reduce stress in parents of children undergoing hematopoietic stem cell transplant (HSCT), according to research published in the Journal of Consulting and Clinical Psychology.
In the short-term, the parent social-cognitive intervention program (P-SCIP) appeared more effective than the current best-practice psychosocial care (BPC) for reducing anxiety, depression, and traumatic distress.
However, there was not much difference between P-SCIP and BPC when it came to long-term results.
Certain subgroups of parents seemed to derive more benefit from P-SCIP than other parents.
“[P]revious research from our team and others has shown that between 20% and 66% of caregivers have elevated depression and/or anxiety prior to their child’s transplant procedure,” said study author Sharon Manne, PhD, of the Rutgers Cancer Institute of New Jersey in New Brunswick.
“It was our aim in this study to develop and test an individual intervention program that targets cognitive and social processing strategies associated with caregiver adjustment and compare that to available best-practice psychosocial care.”
Interventions
This study included 218 biological or foster parents of HSCT recipients under age 19. The parents were assigned to receive P-SCIP or BPC.
P-SCIP required parents to view an interactive CD-ROM for five 60-minute sessions over a 2- to 3-week period following the child’s transplant.
The CD-ROM addressed parents’ worries about their child, coping with solvable concerns related to HSCT, coping with unchangeable problems related to HSCT, and communication and the importance of expressing feelings and needs.
Parents receiving BPC viewed a 1-hour video guide to pediatric HSCT and received a pamphlet covering common caregiver issues. The parents were also given the option of having someone watch their child for up to 5 hours and the use of walkie-talkies so the parents could communicate with their child when they were not in the room.
All participants were asked to complete an in-person survey within a month’s time of their child receiving the transplant and to complete follow-up surveys by phone or mail at 1 month, 6 months, and 1 year post-HSCT.
One hundred and ten parents were randomized to P-SCIP and 108 to BPC. Sixty-six parents completed P-SCIP through the last follow-up, as did 72 parents assigned to BPC.
Results
The researchers found that P-SCIP could reduce anxiety, depression, and—to a marginal degree—traumatic distress more than BPC.
However, the beneficial effects of P-SCIP relative to BPC were only seen at the first follow-up. The overall psychological benefits of P-SCIP were no longer evident at the 6-month or 1-year follow ups.
Still, anxiety, depression, and traumatic distress declined among all the parents over the 1-year follow-up period, which is consistent with other research on caregiver distress after pediatric HSCT.
“Our study suggests that our intervention had an impact when primary caregivers were experiencing high levels of trauma and stress—during the time of the actual transplant and hospitalization—and that the intervention was more beneficial for specific subgroups of caregivers,” Dr Manne said.
P-SCIP had a stronger effect than BPC among parents who began the study reporting higher depression and anxiety and among parents whose children developed graft-versus-host disease.
Similarly, P-SCIP had long-term effects on traumatic distress among parents who reported higher anxiety pre-HSCT and among parents whose children had graft-versus-host disease at HSCT discharge.
“Our findings suggest that screening caregivers for elevations in anxiety and targeting interventions specifically to them may prove beneficial,” Dr Manne said.
She added that a next step for this research might be to examine possible differences between mothers and fathers in the caregiver role, as most of the primary caregivers in this study were mothers.
Additionally, if this intervention is carried into the clinical setting, methods of improving intervention attendance might be considered. Utilizing phone or web-based contact that would allow the parent to remain in the room with the child during hospitalization might help the caregivers more easily access the intervention.

Photo by Chad McNeeley
A new social-cognitive intervention can reduce stress in parents of children undergoing hematopoietic stem cell transplant (HSCT), according to research published in the Journal of Consulting and Clinical Psychology.
In the short-term, the parent social-cognitive intervention program (P-SCIP) appeared more effective than the current best-practice psychosocial care (BPC) for reducing anxiety, depression, and traumatic distress.
However, there was not much difference between P-SCIP and BPC when it came to long-term results.
Certain subgroups of parents seemed to derive more benefit from P-SCIP than other parents.
“[P]revious research from our team and others has shown that between 20% and 66% of caregivers have elevated depression and/or anxiety prior to their child’s transplant procedure,” said study author Sharon Manne, PhD, of the Rutgers Cancer Institute of New Jersey in New Brunswick.
“It was our aim in this study to develop and test an individual intervention program that targets cognitive and social processing strategies associated with caregiver adjustment and compare that to available best-practice psychosocial care.”
Interventions
This study included 218 biological or foster parents of HSCT recipients under age 19. The parents were assigned to receive P-SCIP or BPC.
P-SCIP required parents to view an interactive CD-ROM for five 60-minute sessions over a 2- to 3-week period following the child’s transplant.
The CD-ROM addressed parents’ worries about their child, coping with solvable concerns related to HSCT, coping with unchangeable problems related to HSCT, and communication and the importance of expressing feelings and needs.
Parents receiving BPC viewed a 1-hour video guide to pediatric HSCT and received a pamphlet covering common caregiver issues. The parents were also given the option of having someone watch their child for up to 5 hours and the use of walkie-talkies so the parents could communicate with their child when they were not in the room.
All participants were asked to complete an in-person survey within a month’s time of their child receiving the transplant and to complete follow-up surveys by phone or mail at 1 month, 6 months, and 1 year post-HSCT.
One hundred and ten parents were randomized to P-SCIP and 108 to BPC. Sixty-six parents completed P-SCIP through the last follow-up, as did 72 parents assigned to BPC.
Results
The researchers found that P-SCIP could reduce anxiety, depression, and—to a marginal degree—traumatic distress more than BPC.
However, the beneficial effects of P-SCIP relative to BPC were only seen at the first follow-up. The overall psychological benefits of P-SCIP were no longer evident at the 6-month or 1-year follow ups.
Still, anxiety, depression, and traumatic distress declined among all the parents over the 1-year follow-up period, which is consistent with other research on caregiver distress after pediatric HSCT.
“Our study suggests that our intervention had an impact when primary caregivers were experiencing high levels of trauma and stress—during the time of the actual transplant and hospitalization—and that the intervention was more beneficial for specific subgroups of caregivers,” Dr Manne said.
P-SCIP had a stronger effect than BPC among parents who began the study reporting higher depression and anxiety and among parents whose children developed graft-versus-host disease.
Similarly, P-SCIP had long-term effects on traumatic distress among parents who reported higher anxiety pre-HSCT and among parents whose children had graft-versus-host disease at HSCT discharge.
“Our findings suggest that screening caregivers for elevations in anxiety and targeting interventions specifically to them may prove beneficial,” Dr Manne said.
She added that a next step for this research might be to examine possible differences between mothers and fathers in the caregiver role, as most of the primary caregivers in this study were mothers.
Additionally, if this intervention is carried into the clinical setting, methods of improving intervention attendance might be considered. Utilizing phone or web-based contact that would allow the parent to remain in the room with the child during hospitalization might help the caregivers more easily access the intervention.

Photo by Chad McNeeley
A new social-cognitive intervention can reduce stress in parents of children undergoing hematopoietic stem cell transplant (HSCT), according to research published in the Journal of Consulting and Clinical Psychology.
In the short-term, the parent social-cognitive intervention program (P-SCIP) appeared more effective than the current best-practice psychosocial care (BPC) for reducing anxiety, depression, and traumatic distress.
However, there was not much difference between P-SCIP and BPC when it came to long-term results.
Certain subgroups of parents seemed to derive more benefit from P-SCIP than other parents.
“[P]revious research from our team and others has shown that between 20% and 66% of caregivers have elevated depression and/or anxiety prior to their child’s transplant procedure,” said study author Sharon Manne, PhD, of the Rutgers Cancer Institute of New Jersey in New Brunswick.
“It was our aim in this study to develop and test an individual intervention program that targets cognitive and social processing strategies associated with caregiver adjustment and compare that to available best-practice psychosocial care.”
Interventions
This study included 218 biological or foster parents of HSCT recipients under age 19. The parents were assigned to receive P-SCIP or BPC.
P-SCIP required parents to view an interactive CD-ROM for five 60-minute sessions over a 2- to 3-week period following the child’s transplant.
The CD-ROM addressed parents’ worries about their child, coping with solvable concerns related to HSCT, coping with unchangeable problems related to HSCT, and communication and the importance of expressing feelings and needs.
Parents receiving BPC viewed a 1-hour video guide to pediatric HSCT and received a pamphlet covering common caregiver issues. The parents were also given the option of having someone watch their child for up to 5 hours and the use of walkie-talkies so the parents could communicate with their child when they were not in the room.
All participants were asked to complete an in-person survey within a month’s time of their child receiving the transplant and to complete follow-up surveys by phone or mail at 1 month, 6 months, and 1 year post-HSCT.
One hundred and ten parents were randomized to P-SCIP and 108 to BPC. Sixty-six parents completed P-SCIP through the last follow-up, as did 72 parents assigned to BPC.
Results
The researchers found that P-SCIP could reduce anxiety, depression, and—to a marginal degree—traumatic distress more than BPC.
However, the beneficial effects of P-SCIP relative to BPC were only seen at the first follow-up. The overall psychological benefits of P-SCIP were no longer evident at the 6-month or 1-year follow ups.
Still, anxiety, depression, and traumatic distress declined among all the parents over the 1-year follow-up period, which is consistent with other research on caregiver distress after pediatric HSCT.
“Our study suggests that our intervention had an impact when primary caregivers were experiencing high levels of trauma and stress—during the time of the actual transplant and hospitalization—and that the intervention was more beneficial for specific subgroups of caregivers,” Dr Manne said.
P-SCIP had a stronger effect than BPC among parents who began the study reporting higher depression and anxiety and among parents whose children developed graft-versus-host disease.
Similarly, P-SCIP had long-term effects on traumatic distress among parents who reported higher anxiety pre-HSCT and among parents whose children had graft-versus-host disease at HSCT discharge.
“Our findings suggest that screening caregivers for elevations in anxiety and targeting interventions specifically to them may prove beneficial,” Dr Manne said.
She added that a next step for this research might be to examine possible differences between mothers and fathers in the caregiver role, as most of the primary caregivers in this study were mothers.
Additionally, if this intervention is carried into the clinical setting, methods of improving intervention attendance might be considered. Utilizing phone or web-based contact that would allow the parent to remain in the room with the child during hospitalization might help the caregivers more easily access the intervention.
CDC quantifies threat of resistant HAIs in US

in the intensive care unit
New data from the US Centers for Disease Control and Prevention (CDC) suggest the incidence of certain healthcare-associated infections (HAIs) has fallen in recent years, but antibiotic-resistant bacteria remain a threat.
Therefore, the CDC is advising healthcare workers to use a combination of infection control recommendations to better protect patients from these infections.
“New data show that far too many patients are getting infected with dangerous, drug-resistant bacteria in healthcare settings,” said CDC Director Tom Frieden, MD.
The facts and figures are available in the CDC’s latest Vital Signs report and the agency’s annual progress report on HAI prevention.
The data indicate that 1 in 7 catheter- and surgery-related HAIs in acute care hospitals can be caused by 6 types of antibiotic-resistant bacteria. That number increases to 1 in 4 infections in long-term acute care hospitals.
The 6 antibiotic-resistant threats are carbapenem-resistant Enterobacteriaceae (CRE), methicillin-resistant Staphylococcus aureus (MRSA), ESBL-producing Enterobacteriaceae (extended-spectrum β-lactamases), vancomycin-resistant Enterococcus (VRE), multidrug-resistant Pseudomonas aeruginosa, and multidrug-resistant Acinetobacter.
Prevention and resistance
According to the CDC’s data, acute care hospitals saw a 50% decrease in central line-associated bloodstream infections between 2008 and 2014. But 1 in 6 remaining central line-associated bloodstream infections is caused by urgent or serious antibiotic-resistant bacteria.
Between 2008 and 2014, acute care hospitals saw a 17% decrease in surgical site infections related to 10 procedures that were tracked in previous HAI progress reports. One in 7 remaining surgical site infections is caused by urgent or serious antibiotic-resistant bacteria.
Acute care hospitals saw no change in the incidence of catheter-associated urinary tract infections (CAUTIs) between 2009 and 2014. However, there was a reduction in CAUTIs between 2013 and 2014. One in 10 CAUTIs is caused by urgent or serious antibiotic-resistant bacteria.
The Vital Signs report also examines Clostridium difficile, which caused almost half a million infections in the US in 2011 alone. The CDC’s annual progress report shows that hospital-onset C difficile infections decreased by 8% between 2011 and 2014.
In addition to the reports, the CDC has released a web app with interactive data on HAIs caused by antibiotic-resistant bacteria.
The tool, known as the Antibiotic Resistance Patient Safety Atlas, provides national, regional, and state map views of superbug/drug combinations showing percent resistance over time. The Atlas uses data reported to the CDC’s National Healthcare Safety Network from 2011 to 2014 from more than 4000 healthcare facilities.

in the intensive care unit
New data from the US Centers for Disease Control and Prevention (CDC) suggest the incidence of certain healthcare-associated infections (HAIs) has fallen in recent years, but antibiotic-resistant bacteria remain a threat.
Therefore, the CDC is advising healthcare workers to use a combination of infection control recommendations to better protect patients from these infections.
“New data show that far too many patients are getting infected with dangerous, drug-resistant bacteria in healthcare settings,” said CDC Director Tom Frieden, MD.
The facts and figures are available in the CDC’s latest Vital Signs report and the agency’s annual progress report on HAI prevention.
The data indicate that 1 in 7 catheter- and surgery-related HAIs in acute care hospitals can be caused by 6 types of antibiotic-resistant bacteria. That number increases to 1 in 4 infections in long-term acute care hospitals.
The 6 antibiotic-resistant threats are carbapenem-resistant Enterobacteriaceae (CRE), methicillin-resistant Staphylococcus aureus (MRSA), ESBL-producing Enterobacteriaceae (extended-spectrum β-lactamases), vancomycin-resistant Enterococcus (VRE), multidrug-resistant Pseudomonas aeruginosa, and multidrug-resistant Acinetobacter.
Prevention and resistance
According to the CDC’s data, acute care hospitals saw a 50% decrease in central line-associated bloodstream infections between 2008 and 2014. But 1 in 6 remaining central line-associated bloodstream infections is caused by urgent or serious antibiotic-resistant bacteria.
Between 2008 and 2014, acute care hospitals saw a 17% decrease in surgical site infections related to 10 procedures that were tracked in previous HAI progress reports. One in 7 remaining surgical site infections is caused by urgent or serious antibiotic-resistant bacteria.
Acute care hospitals saw no change in the incidence of catheter-associated urinary tract infections (CAUTIs) between 2009 and 2014. However, there was a reduction in CAUTIs between 2013 and 2014. One in 10 CAUTIs is caused by urgent or serious antibiotic-resistant bacteria.
The Vital Signs report also examines Clostridium difficile, which caused almost half a million infections in the US in 2011 alone. The CDC’s annual progress report shows that hospital-onset C difficile infections decreased by 8% between 2011 and 2014.
In addition to the reports, the CDC has released a web app with interactive data on HAIs caused by antibiotic-resistant bacteria.
The tool, known as the Antibiotic Resistance Patient Safety Atlas, provides national, regional, and state map views of superbug/drug combinations showing percent resistance over time. The Atlas uses data reported to the CDC’s National Healthcare Safety Network from 2011 to 2014 from more than 4000 healthcare facilities.

in the intensive care unit
New data from the US Centers for Disease Control and Prevention (CDC) suggest the incidence of certain healthcare-associated infections (HAIs) has fallen in recent years, but antibiotic-resistant bacteria remain a threat.
Therefore, the CDC is advising healthcare workers to use a combination of infection control recommendations to better protect patients from these infections.
“New data show that far too many patients are getting infected with dangerous, drug-resistant bacteria in healthcare settings,” said CDC Director Tom Frieden, MD.
The facts and figures are available in the CDC’s latest Vital Signs report and the agency’s annual progress report on HAI prevention.
The data indicate that 1 in 7 catheter- and surgery-related HAIs in acute care hospitals can be caused by 6 types of antibiotic-resistant bacteria. That number increases to 1 in 4 infections in long-term acute care hospitals.
The 6 antibiotic-resistant threats are carbapenem-resistant Enterobacteriaceae (CRE), methicillin-resistant Staphylococcus aureus (MRSA), ESBL-producing Enterobacteriaceae (extended-spectrum β-lactamases), vancomycin-resistant Enterococcus (VRE), multidrug-resistant Pseudomonas aeruginosa, and multidrug-resistant Acinetobacter.
Prevention and resistance
According to the CDC’s data, acute care hospitals saw a 50% decrease in central line-associated bloodstream infections between 2008 and 2014. But 1 in 6 remaining central line-associated bloodstream infections is caused by urgent or serious antibiotic-resistant bacteria.
Between 2008 and 2014, acute care hospitals saw a 17% decrease in surgical site infections related to 10 procedures that were tracked in previous HAI progress reports. One in 7 remaining surgical site infections is caused by urgent or serious antibiotic-resistant bacteria.
Acute care hospitals saw no change in the incidence of catheter-associated urinary tract infections (CAUTIs) between 2009 and 2014. However, there was a reduction in CAUTIs between 2013 and 2014. One in 10 CAUTIs is caused by urgent or serious antibiotic-resistant bacteria.
The Vital Signs report also examines Clostridium difficile, which caused almost half a million infections in the US in 2011 alone. The CDC’s annual progress report shows that hospital-onset C difficile infections decreased by 8% between 2011 and 2014.
In addition to the reports, the CDC has released a web app with interactive data on HAIs caused by antibiotic-resistant bacteria.
The tool, known as the Antibiotic Resistance Patient Safety Atlas, provides national, regional, and state map views of superbug/drug combinations showing percent resistance over time. The Atlas uses data reported to the CDC’s National Healthcare Safety Network from 2011 to 2014 from more than 4000 healthcare facilities.
Bundle can decrease CLABSI incidence

Staphylococcus infection
Photo by Bill Branson
A central catheter maintenance bundle can decrease the incidence of central line-associated bloodstream infections (CLABSIs), according to a study published in the American Journal of Critical Care.
A team from the healthcare company Select Medical developed and implemented the bundle at 30 long-term acute care hospitals.
The team used infection prevention guidelines from the Centers for Disease Control and Prevention as the core of the bundle, with mandatory use of alcohol-based central catheter caps and chlorhexidine gluconate dressings.
Ongoing education of clinical staff about the protocol and a checklist to track compliance were also key elements of the initiative.
At each hospital, staff nurses who demonstrated competency in the care of central catheters monitored implementation of the bundle for the initial 6 months of the study.
Researchers reviewed the medical records of 6660 patients discharged during the 14 months prior to the study and 6559 patients discharged after implementation of the bundle. Patient days and central catheter days before and after the bundle was implemented were comparable.
Six months after the bundle was implemented, the CLABSI standardized infection rate had dropped 29%. The rate was 1.28 in the 6 months before the bundle was implemented and 0.96 six months after implementation.
There was a mean reduction of 4.5 CLABSIs per hospital for 14 months after the bundle was implemented.
“Our results encourage the development and implementation of similar bundles as effective infection reduction strategies in [long-term acute care hospitals],” said study author Antony Grigonis, PhD, vice-president of quality and healthcare analytics at Select Medical.
“Preventing these infections can help reduce complications and the length of stay for other patients. This infection reduction could also translate to a savings of approximately $3.7 million annually for the 30 long-term acute care hospitals studied.”
Select Medical, which is based in Mechanicsburg, Pennsylvania, owns long-term acute care and inpatient rehabilitation hospitals, as well as occupational health and physical therapy clinics.

Staphylococcus infection
Photo by Bill Branson
A central catheter maintenance bundle can decrease the incidence of central line-associated bloodstream infections (CLABSIs), according to a study published in the American Journal of Critical Care.
A team from the healthcare company Select Medical developed and implemented the bundle at 30 long-term acute care hospitals.
The team used infection prevention guidelines from the Centers for Disease Control and Prevention as the core of the bundle, with mandatory use of alcohol-based central catheter caps and chlorhexidine gluconate dressings.
Ongoing education of clinical staff about the protocol and a checklist to track compliance were also key elements of the initiative.
At each hospital, staff nurses who demonstrated competency in the care of central catheters monitored implementation of the bundle for the initial 6 months of the study.
Researchers reviewed the medical records of 6660 patients discharged during the 14 months prior to the study and 6559 patients discharged after implementation of the bundle. Patient days and central catheter days before and after the bundle was implemented were comparable.
Six months after the bundle was implemented, the CLABSI standardized infection rate had dropped 29%. The rate was 1.28 in the 6 months before the bundle was implemented and 0.96 six months after implementation.
There was a mean reduction of 4.5 CLABSIs per hospital for 14 months after the bundle was implemented.
“Our results encourage the development and implementation of similar bundles as effective infection reduction strategies in [long-term acute care hospitals],” said study author Antony Grigonis, PhD, vice-president of quality and healthcare analytics at Select Medical.
“Preventing these infections can help reduce complications and the length of stay for other patients. This infection reduction could also translate to a savings of approximately $3.7 million annually for the 30 long-term acute care hospitals studied.”
Select Medical, which is based in Mechanicsburg, Pennsylvania, owns long-term acute care and inpatient rehabilitation hospitals, as well as occupational health and physical therapy clinics.

Staphylococcus infection
Photo by Bill Branson
A central catheter maintenance bundle can decrease the incidence of central line-associated bloodstream infections (CLABSIs), according to a study published in the American Journal of Critical Care.
A team from the healthcare company Select Medical developed and implemented the bundle at 30 long-term acute care hospitals.
The team used infection prevention guidelines from the Centers for Disease Control and Prevention as the core of the bundle, with mandatory use of alcohol-based central catheter caps and chlorhexidine gluconate dressings.
Ongoing education of clinical staff about the protocol and a checklist to track compliance were also key elements of the initiative.
At each hospital, staff nurses who demonstrated competency in the care of central catheters monitored implementation of the bundle for the initial 6 months of the study.
Researchers reviewed the medical records of 6660 patients discharged during the 14 months prior to the study and 6559 patients discharged after implementation of the bundle. Patient days and central catheter days before and after the bundle was implemented were comparable.
Six months after the bundle was implemented, the CLABSI standardized infection rate had dropped 29%. The rate was 1.28 in the 6 months before the bundle was implemented and 0.96 six months after implementation.
There was a mean reduction of 4.5 CLABSIs per hospital for 14 months after the bundle was implemented.
“Our results encourage the development and implementation of similar bundles as effective infection reduction strategies in [long-term acute care hospitals],” said study author Antony Grigonis, PhD, vice-president of quality and healthcare analytics at Select Medical.
“Preventing these infections can help reduce complications and the length of stay for other patients. This infection reduction could also translate to a savings of approximately $3.7 million annually for the 30 long-term acute care hospitals studied.”
Select Medical, which is based in Mechanicsburg, Pennsylvania, owns long-term acute care and inpatient rehabilitation hospitals, as well as occupational health and physical therapy clinics.