User login
Effects of gluten-free diet on IBS symptoms
Key clinical point: A gluten-free diet influenced bowel habits and had significant positive effects on irritable bowel syndrome (IBS) symptom severity, abdominal pain intensity, and daily life interference.
Major finding: In patients with IBS, the IBS-severity scoring system total score (P = .02), abdominal pain intensity (P = .02), and daily life interference (P = .04) improved significantly after the gluten-free intervention but not after the gluten-containing intervention. Patients with IBS reported fewer loose stools during the gluten-free vs gluten-containing intervention (19.2% vs 27.4%; P = .01).
Study details: The data come from a randomized controlled trial (PROT-IBS) including 20 patients with IBS and 21 healthy control individuals who were challenged with gluten (14 g/day) or rice flour during two 14-day interventions, while adhering to a strict gluten-free diet.
Disclosures: This study was funded by the Swedish Research Council and other sources. Some authors declared receiving consulting fees or research grants or serving on advisory boards for various sources.
Source: Algera JP et al. Randomised controlled trial: Effects of gluten-free diet on symptoms and the gut microenvironment in irritable bowel syndrome. Aliment Pharmacol Ther. 2022;56(9):1318-1327 (Sep 29). Doi: 10.1111/apt.17239
Key clinical point: A gluten-free diet influenced bowel habits and had significant positive effects on irritable bowel syndrome (IBS) symptom severity, abdominal pain intensity, and daily life interference.
Major finding: In patients with IBS, the IBS-severity scoring system total score (P = .02), abdominal pain intensity (P = .02), and daily life interference (P = .04) improved significantly after the gluten-free intervention but not after the gluten-containing intervention. Patients with IBS reported fewer loose stools during the gluten-free vs gluten-containing intervention (19.2% vs 27.4%; P = .01).
Study details: The data come from a randomized controlled trial (PROT-IBS) including 20 patients with IBS and 21 healthy control individuals who were challenged with gluten (14 g/day) or rice flour during two 14-day interventions, while adhering to a strict gluten-free diet.
Disclosures: This study was funded by the Swedish Research Council and other sources. Some authors declared receiving consulting fees or research grants or serving on advisory boards for various sources.
Source: Algera JP et al. Randomised controlled trial: Effects of gluten-free diet on symptoms and the gut microenvironment in irritable bowel syndrome. Aliment Pharmacol Ther. 2022;56(9):1318-1327 (Sep 29). Doi: 10.1111/apt.17239
Key clinical point: A gluten-free diet influenced bowel habits and had significant positive effects on irritable bowel syndrome (IBS) symptom severity, abdominal pain intensity, and daily life interference.
Major finding: In patients with IBS, the IBS-severity scoring system total score (P = .02), abdominal pain intensity (P = .02), and daily life interference (P = .04) improved significantly after the gluten-free intervention but not after the gluten-containing intervention. Patients with IBS reported fewer loose stools during the gluten-free vs gluten-containing intervention (19.2% vs 27.4%; P = .01).
Study details: The data come from a randomized controlled trial (PROT-IBS) including 20 patients with IBS and 21 healthy control individuals who were challenged with gluten (14 g/day) or rice flour during two 14-day interventions, while adhering to a strict gluten-free diet.
Disclosures: This study was funded by the Swedish Research Council and other sources. Some authors declared receiving consulting fees or research grants or serving on advisory boards for various sources.
Source: Algera JP et al. Randomised controlled trial: Effects of gluten-free diet on symptoms and the gut microenvironment in irritable bowel syndrome. Aliment Pharmacol Ther. 2022;56(9):1318-1327 (Sep 29). Doi: 10.1111/apt.17239
Ulcerative colitis: Reassuring findings on long-term tofacitinib reported
Updated long-term safety data suggest that tofacitinib (Xeljanz, Pfizer) is generally safe for long-term use in the treatment of moderate to severe ulcerative colitis (UC), with adverse events (AE) consistent with previous studies and showed stability over time in the incidence of adverse events of special interest.
“Findings from these integrated safety analyses are reassuring for patients with UC. The incidence rates of most key events that led to the black box warning are lower in these cohorts, compared with results observed in the ORAL Surveillance study of older patients with RA [rheumatoid arthritis],” said Siddharth Singh, MD, who was asked to comment on the study.
The results support the current clinical approach, in which tofacitinib is typically employed following infliximab (Remicade, Janssen) failure, though the paradigm may change. “These findings on safety reassure our approach, though there will still be hesitation to use 10-mg twice-daily dosing in older patients. However, with the recent approval of upadacitinib (Rinvoq, AbbVie), a selective JAK1 inhibitor that seems to be more effective than tofacitinib, positioning of tofacitinib may evolve,” said Dr. Singh, who is an associate professor of medicine at University of California, San Diego, and director of the UCSD IBD Center.
There has been evidence to support safety concerns with tofacitinib. The prospective ORAL Surveillance study compared two doses of tofacitinib (5 or 10 mg, twice daily) to tumor necrosis factor (TNF) inhibitors in patients with rheumatoid arthritis. The researchers selected patients aged 50 and older and with at least one additional cardiovascular risk factor. The study found higher rates of major adverse cardiovascular events and malignancies in the tofacitinib groups, as well as higher rates of mortality, serious infection, and venous thromboembolism. The findings prompted a Food and Drug Administration “black box” warning for tofacitinib in July 2019, which was extended to two other JAK inhibitors in September 2021.
However, patients in the UC clinical program are generally younger than participants in the ORAL Surveillance study and were less likely to have a smoking history.
The new study, published in the Journal of Crohn’s and Colitis, represents an update of a pooled analysis from phase 2, phase 3, and open-label extension studies with up to 4.4 years of exposure. Analysis of the earlier cohort showed that tofacitinib had a generally similar safety profile to other UC therapies, with the exception of a higher incidence of herpes zoster infection. Since that publication, the researchers have compiled additional person-years of tofacitinib exposure from the open-label extension OCTAVE Open study and the 6-month interim analysis of the phase 3b/4 RIVETING study.
The new study included 1,157 patients who received at least one dose of tofacitinib. Overall, 35.6% had received treatment for longer than 4 years. The mean age was 41.3 years, 58.7% were male, and 80.1% were White; 64.0% had never smoked, and 30.9% were ex-smokers. The mean disease duration was 8.2 years. In all, 83% of patients were on a 10 mg dose, and 17% were on 5 mg.
In the 2016 analysis, 82.1% of patients had an adverse event and 14.6% had a serious adverse event. In the overall cohort, the percentages were 85.7% and 21%, respectively.
In the updated analysis, 11.6% discontinued medication use because of an adverse event. For all doses, incidence rates (IRs) for adverse events were defined as unique patients with events per 100 person-years of exposure. The IRs for death and adverse events of special interest were similar between the original cohort and the updated cohort. For example, the IR for death was 0.24 for death in the earlier cohort (95% confidence interval, 0.07-0.61) and 0.23 in the combined cohort (95% CI, 0.09-0.46); it was 1.99 for serious infections in the earlier cohort (95% CI 1.37–2.79) and 1.69 in the combined cohort for serious infections (95% CI, 1.26-2.21); it was 4.07 for serious and nonserious herpes zoster infection in the earlier cohort (95% CI, 3.14-5.19), 3.30 for serious and nonserious herpes zoster infection in the combined cohort (95% CI, 2.67-4.04); and it was 1.28 for opportunistic infections in the earlier cohort (95% CI, 0.79-1.96) and 1.03 in the combined cohort for opportunistic infections (95% CI, 0.70-1.46).
The updated cohort included 3.4 more years of observation and an additional 1,386.9 person-years of exposure. That resulted in a final tally of up to 7.8 years of exposure and a combined 2,999.7 person-years of exposure, “thus demonstrating that the safety profile of tofacitinib remained consistent with increased extent and length of exposure,” the authors wrote.
Despite the promising findings, Dr. Singh called for more research. “We need a dedicated safety registry of tofacitinib and other JAK inhibitors in patients with IBD, who do not share the characteristics of those studied in the ORAL Surveillance study,” he said.
The authors disclose ties to various pharmaceutical companies, including Pfizer, which manufactures tofacitinib. Dr. Singh has received personal fees from Pfizer for ad hoc grant review.
Updated long-term safety data suggest that tofacitinib (Xeljanz, Pfizer) is generally safe for long-term use in the treatment of moderate to severe ulcerative colitis (UC), with adverse events (AE) consistent with previous studies and showed stability over time in the incidence of adverse events of special interest.
“Findings from these integrated safety analyses are reassuring for patients with UC. The incidence rates of most key events that led to the black box warning are lower in these cohorts, compared with results observed in the ORAL Surveillance study of older patients with RA [rheumatoid arthritis],” said Siddharth Singh, MD, who was asked to comment on the study.
The results support the current clinical approach, in which tofacitinib is typically employed following infliximab (Remicade, Janssen) failure, though the paradigm may change. “These findings on safety reassure our approach, though there will still be hesitation to use 10-mg twice-daily dosing in older patients. However, with the recent approval of upadacitinib (Rinvoq, AbbVie), a selective JAK1 inhibitor that seems to be more effective than tofacitinib, positioning of tofacitinib may evolve,” said Dr. Singh, who is an associate professor of medicine at University of California, San Diego, and director of the UCSD IBD Center.
There has been evidence to support safety concerns with tofacitinib. The prospective ORAL Surveillance study compared two doses of tofacitinib (5 or 10 mg, twice daily) to tumor necrosis factor (TNF) inhibitors in patients with rheumatoid arthritis. The researchers selected patients aged 50 and older and with at least one additional cardiovascular risk factor. The study found higher rates of major adverse cardiovascular events and malignancies in the tofacitinib groups, as well as higher rates of mortality, serious infection, and venous thromboembolism. The findings prompted a Food and Drug Administration “black box” warning for tofacitinib in July 2019, which was extended to two other JAK inhibitors in September 2021.
However, patients in the UC clinical program are generally younger than participants in the ORAL Surveillance study and were less likely to have a smoking history.
The new study, published in the Journal of Crohn’s and Colitis, represents an update of a pooled analysis from phase 2, phase 3, and open-label extension studies with up to 4.4 years of exposure. Analysis of the earlier cohort showed that tofacitinib had a generally similar safety profile to other UC therapies, with the exception of a higher incidence of herpes zoster infection. Since that publication, the researchers have compiled additional person-years of tofacitinib exposure from the open-label extension OCTAVE Open study and the 6-month interim analysis of the phase 3b/4 RIVETING study.
The new study included 1,157 patients who received at least one dose of tofacitinib. Overall, 35.6% had received treatment for longer than 4 years. The mean age was 41.3 years, 58.7% were male, and 80.1% were White; 64.0% had never smoked, and 30.9% were ex-smokers. The mean disease duration was 8.2 years. In all, 83% of patients were on a 10 mg dose, and 17% were on 5 mg.
In the 2016 analysis, 82.1% of patients had an adverse event and 14.6% had a serious adverse event. In the overall cohort, the percentages were 85.7% and 21%, respectively.
In the updated analysis, 11.6% discontinued medication use because of an adverse event. For all doses, incidence rates (IRs) for adverse events were defined as unique patients with events per 100 person-years of exposure. The IRs for death and adverse events of special interest were similar between the original cohort and the updated cohort. For example, the IR for death was 0.24 for death in the earlier cohort (95% confidence interval, 0.07-0.61) and 0.23 in the combined cohort (95% CI, 0.09-0.46); it was 1.99 for serious infections in the earlier cohort (95% CI 1.37–2.79) and 1.69 in the combined cohort for serious infections (95% CI, 1.26-2.21); it was 4.07 for serious and nonserious herpes zoster infection in the earlier cohort (95% CI, 3.14-5.19), 3.30 for serious and nonserious herpes zoster infection in the combined cohort (95% CI, 2.67-4.04); and it was 1.28 for opportunistic infections in the earlier cohort (95% CI, 0.79-1.96) and 1.03 in the combined cohort for opportunistic infections (95% CI, 0.70-1.46).
The updated cohort included 3.4 more years of observation and an additional 1,386.9 person-years of exposure. That resulted in a final tally of up to 7.8 years of exposure and a combined 2,999.7 person-years of exposure, “thus demonstrating that the safety profile of tofacitinib remained consistent with increased extent and length of exposure,” the authors wrote.
Despite the promising findings, Dr. Singh called for more research. “We need a dedicated safety registry of tofacitinib and other JAK inhibitors in patients with IBD, who do not share the characteristics of those studied in the ORAL Surveillance study,” he said.
The authors disclose ties to various pharmaceutical companies, including Pfizer, which manufactures tofacitinib. Dr. Singh has received personal fees from Pfizer for ad hoc grant review.
Updated long-term safety data suggest that tofacitinib (Xeljanz, Pfizer) is generally safe for long-term use in the treatment of moderate to severe ulcerative colitis (UC), with adverse events (AE) consistent with previous studies and showed stability over time in the incidence of adverse events of special interest.
“Findings from these integrated safety analyses are reassuring for patients with UC. The incidence rates of most key events that led to the black box warning are lower in these cohorts, compared with results observed in the ORAL Surveillance study of older patients with RA [rheumatoid arthritis],” said Siddharth Singh, MD, who was asked to comment on the study.
The results support the current clinical approach, in which tofacitinib is typically employed following infliximab (Remicade, Janssen) failure, though the paradigm may change. “These findings on safety reassure our approach, though there will still be hesitation to use 10-mg twice-daily dosing in older patients. However, with the recent approval of upadacitinib (Rinvoq, AbbVie), a selective JAK1 inhibitor that seems to be more effective than tofacitinib, positioning of tofacitinib may evolve,” said Dr. Singh, who is an associate professor of medicine at University of California, San Diego, and director of the UCSD IBD Center.
There has been evidence to support safety concerns with tofacitinib. The prospective ORAL Surveillance study compared two doses of tofacitinib (5 or 10 mg, twice daily) to tumor necrosis factor (TNF) inhibitors in patients with rheumatoid arthritis. The researchers selected patients aged 50 and older and with at least one additional cardiovascular risk factor. The study found higher rates of major adverse cardiovascular events and malignancies in the tofacitinib groups, as well as higher rates of mortality, serious infection, and venous thromboembolism. The findings prompted a Food and Drug Administration “black box” warning for tofacitinib in July 2019, which was extended to two other JAK inhibitors in September 2021.
However, patients in the UC clinical program are generally younger than participants in the ORAL Surveillance study and were less likely to have a smoking history.
The new study, published in the Journal of Crohn’s and Colitis, represents an update of a pooled analysis from phase 2, phase 3, and open-label extension studies with up to 4.4 years of exposure. Analysis of the earlier cohort showed that tofacitinib had a generally similar safety profile to other UC therapies, with the exception of a higher incidence of herpes zoster infection. Since that publication, the researchers have compiled additional person-years of tofacitinib exposure from the open-label extension OCTAVE Open study and the 6-month interim analysis of the phase 3b/4 RIVETING study.
The new study included 1,157 patients who received at least one dose of tofacitinib. Overall, 35.6% had received treatment for longer than 4 years. The mean age was 41.3 years, 58.7% were male, and 80.1% were White; 64.0% had never smoked, and 30.9% were ex-smokers. The mean disease duration was 8.2 years. In all, 83% of patients were on a 10 mg dose, and 17% were on 5 mg.
In the 2016 analysis, 82.1% of patients had an adverse event and 14.6% had a serious adverse event. In the overall cohort, the percentages were 85.7% and 21%, respectively.
In the updated analysis, 11.6% discontinued medication use because of an adverse event. For all doses, incidence rates (IRs) for adverse events were defined as unique patients with events per 100 person-years of exposure. The IRs for death and adverse events of special interest were similar between the original cohort and the updated cohort. For example, the IR for death was 0.24 for death in the earlier cohort (95% confidence interval, 0.07-0.61) and 0.23 in the combined cohort (95% CI, 0.09-0.46); it was 1.99 for serious infections in the earlier cohort (95% CI 1.37–2.79) and 1.69 in the combined cohort for serious infections (95% CI, 1.26-2.21); it was 4.07 for serious and nonserious herpes zoster infection in the earlier cohort (95% CI, 3.14-5.19), 3.30 for serious and nonserious herpes zoster infection in the combined cohort (95% CI, 2.67-4.04); and it was 1.28 for opportunistic infections in the earlier cohort (95% CI, 0.79-1.96) and 1.03 in the combined cohort for opportunistic infections (95% CI, 0.70-1.46).
The updated cohort included 3.4 more years of observation and an additional 1,386.9 person-years of exposure. That resulted in a final tally of up to 7.8 years of exposure and a combined 2,999.7 person-years of exposure, “thus demonstrating that the safety profile of tofacitinib remained consistent with increased extent and length of exposure,” the authors wrote.
Despite the promising findings, Dr. Singh called for more research. “We need a dedicated safety registry of tofacitinib and other JAK inhibitors in patients with IBD, who do not share the characteristics of those studied in the ORAL Surveillance study,” he said.
The authors disclose ties to various pharmaceutical companies, including Pfizer, which manufactures tofacitinib. Dr. Singh has received personal fees from Pfizer for ad hoc grant review.
FROM JOURNAL OF CROHN’S AND COLITIS
Children with asymptomatic celiac disease may have severe disease histology
Some pediatric patients with celiac disease whose condition is diagnosed after screening because a first-degree relative has the disease may appear asymptomatic but have severe disease histology, according to a new report.
About half of these patients had no symptoms, but disease histology was as severe as among those screened for other reasons, such as having symptomatic disease or high-risk conditions.
“This data supports current recommendations to screen all first-degree relatives of patients with celiac disease, especially pediatric patients in whom the ramifications of untreated disease may be significant,” wrote Michelle Gould, MD, and colleagues at the University of Toronto and McMaster University, Hamilton, Ont.
The study was published online in the Journal of Pediatric Gastroenterology and Nutrition.
Clinical characteristics
The incidence of celiac disease is higher among first-degree relatives of patients with the disease than among the general population, yet the clinical characteristics aren’t well described, the study authors wrote. Determining the clinical, serologic, and histologic phenotype of these patients could help clinicians determine whether continued universal screening of first-degree relatives is appropriate.
Dr. Gould and colleagues conducted a retrospective review of 227 patients diagnosed with celiac disease at McMaster Children’s Hospital between 1996 and 2014. The patients were categorized as being screened for celiac disease because a first-degree relative had the disease or because of other reasons. The other reasons included symptoms consistent with celiac disease or the presence of a high-risk clinical condition for which screening is recommended, such as type 1 diabetes or Down syndrome.
All patients were screened via tissue transglutaminase (tTG-IgA) tests. Positive serology was defined as tTG-IgA greater than the upper limit of normal in the presence of normal IgA immunoglobulin level for age.
The patients who were included in the study had biopsy-proven celiac disease in accordance with the Marsh criteria, which included Marsh III histology, Marsh II histology with positive serology, or Marsh I histology with positive serology and clinical symptoms.
The average age of the patients (144 girls and 83 boys) was 8 years at diagnosis. Among the patients, 49 (21.6%) were screened because a first-degree relative had celiac disease. Of those 49 patients, 24 (49%) were symptomatic, and 25 (51%) were asymptomatic.
By contrast, among the 178 patients who were screened for other reasons, 149 (83.7%) were symptomatic, and 29 (16.3%) were asymptomatic.
There was no significant difference between the patient groups with respect to Marsh score at biopsy and tTG-IgA levels at screening. Among the children who were screened because of family history, Marsh scores were equally severe as among other patients, whether they were symptomatic or not.
In addition, no statistically significant differences were found for other clinical characteristics, including body mass index z-score, weight z-score, height z-score, the presence of anemia, or a low mean corpuscular volume for age.
When comparing the characteristics of those screened because of family history and those screened for other high-risk conditions (type 1 diabetes and Down syndrome), the researchers found that rates of asymptomatic presentation were statistically similar between the groups, as were tissue transglutaminase values, Marsh scores, BMI z-scores, and hemoglobin levels at diagnosis. Although there was a statistical difference between the groups with respect to the mean corpuscular volume values at diagnosis, it was unlikely to be of clinical significance, the authors noted.
At 6 months, 1 year, and 2 years after diagnosis, among patients with repeat tTG-IgA measurements, 93 of 143 patients (65%), 52 of 68 patients (76.5%), and 80 of 90 patients (88.9%) had normal serum tTG-IgA levels, respectively. In comparing the proportion of patients whose tTG-IgA levels were normal, there was no difference between those screened because of family history and those screened for other reasons at any time point after diagnosis.
“This may suggest that the natural history of celiac disease is similar in these two groups following initiation of a gluten-free diet and that there are similar rates of compliance with this therapy regardless of the initial indication for screening,” the study authors wrote.
Clinical implications
Dr. Gould and colleagues noted that celiac disease was considered histologically severe – with a Marsh III score or higher – among nearly all patients whose condition was diagnosed because of family history. Histology was equally severe regardless of whether the patients were symptomatic or asymptomatic at screening – 100% of symptomatic patients had a high score, and 96% of asymptomatic patients had a high score.
“This emphasizes the importance of celiac screening in all patients with first-degree relatives with celiac disease, as symptom status does not predict diagnosis or severity of disease,” they wrote.
Previous studies have indicated that the prevalence of celiac disease is highest among siblings of patients with celiac disease, compared with other types of first-degree relatives, the authors wrote. However, they lacked this information in their records, which would be valuable for analysis in future studies.
In addition, ongoing research should investigate the optimal frequency of screening for first-degree relatives, they noted.
“One study suggests that individuals screened before 10 years of age should have repeat screening in their second decade for a small increased pick-up of diagnoses,” they wrote.
No funding for the study has been reported. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Some pediatric patients with celiac disease whose condition is diagnosed after screening because a first-degree relative has the disease may appear asymptomatic but have severe disease histology, according to a new report.
About half of these patients had no symptoms, but disease histology was as severe as among those screened for other reasons, such as having symptomatic disease or high-risk conditions.
“This data supports current recommendations to screen all first-degree relatives of patients with celiac disease, especially pediatric patients in whom the ramifications of untreated disease may be significant,” wrote Michelle Gould, MD, and colleagues at the University of Toronto and McMaster University, Hamilton, Ont.
The study was published online in the Journal of Pediatric Gastroenterology and Nutrition.
Clinical characteristics
The incidence of celiac disease is higher among first-degree relatives of patients with the disease than among the general population, yet the clinical characteristics aren’t well described, the study authors wrote. Determining the clinical, serologic, and histologic phenotype of these patients could help clinicians determine whether continued universal screening of first-degree relatives is appropriate.
Dr. Gould and colleagues conducted a retrospective review of 227 patients diagnosed with celiac disease at McMaster Children’s Hospital between 1996 and 2014. The patients were categorized as being screened for celiac disease because a first-degree relative had the disease or because of other reasons. The other reasons included symptoms consistent with celiac disease or the presence of a high-risk clinical condition for which screening is recommended, such as type 1 diabetes or Down syndrome.
All patients were screened via tissue transglutaminase (tTG-IgA) tests. Positive serology was defined as tTG-IgA greater than the upper limit of normal in the presence of normal IgA immunoglobulin level for age.
The patients who were included in the study had biopsy-proven celiac disease in accordance with the Marsh criteria, which included Marsh III histology, Marsh II histology with positive serology, or Marsh I histology with positive serology and clinical symptoms.
The average age of the patients (144 girls and 83 boys) was 8 years at diagnosis. Among the patients, 49 (21.6%) were screened because a first-degree relative had celiac disease. Of those 49 patients, 24 (49%) were symptomatic, and 25 (51%) were asymptomatic.
By contrast, among the 178 patients who were screened for other reasons, 149 (83.7%) were symptomatic, and 29 (16.3%) were asymptomatic.
There was no significant difference between the patient groups with respect to Marsh score at biopsy and tTG-IgA levels at screening. Among the children who were screened because of family history, Marsh scores were equally severe as among other patients, whether they were symptomatic or not.
In addition, no statistically significant differences were found for other clinical characteristics, including body mass index z-score, weight z-score, height z-score, the presence of anemia, or a low mean corpuscular volume for age.
When comparing the characteristics of those screened because of family history and those screened for other high-risk conditions (type 1 diabetes and Down syndrome), the researchers found that rates of asymptomatic presentation were statistically similar between the groups, as were tissue transglutaminase values, Marsh scores, BMI z-scores, and hemoglobin levels at diagnosis. Although there was a statistical difference between the groups with respect to the mean corpuscular volume values at diagnosis, it was unlikely to be of clinical significance, the authors noted.
At 6 months, 1 year, and 2 years after diagnosis, among patients with repeat tTG-IgA measurements, 93 of 143 patients (65%), 52 of 68 patients (76.5%), and 80 of 90 patients (88.9%) had normal serum tTG-IgA levels, respectively. In comparing the proportion of patients whose tTG-IgA levels were normal, there was no difference between those screened because of family history and those screened for other reasons at any time point after diagnosis.
“This may suggest that the natural history of celiac disease is similar in these two groups following initiation of a gluten-free diet and that there are similar rates of compliance with this therapy regardless of the initial indication for screening,” the study authors wrote.
Clinical implications
Dr. Gould and colleagues noted that celiac disease was considered histologically severe – with a Marsh III score or higher – among nearly all patients whose condition was diagnosed because of family history. Histology was equally severe regardless of whether the patients were symptomatic or asymptomatic at screening – 100% of symptomatic patients had a high score, and 96% of asymptomatic patients had a high score.
“This emphasizes the importance of celiac screening in all patients with first-degree relatives with celiac disease, as symptom status does not predict diagnosis or severity of disease,” they wrote.
Previous studies have indicated that the prevalence of celiac disease is highest among siblings of patients with celiac disease, compared with other types of first-degree relatives, the authors wrote. However, they lacked this information in their records, which would be valuable for analysis in future studies.
In addition, ongoing research should investigate the optimal frequency of screening for first-degree relatives, they noted.
“One study suggests that individuals screened before 10 years of age should have repeat screening in their second decade for a small increased pick-up of diagnoses,” they wrote.
No funding for the study has been reported. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Some pediatric patients with celiac disease whose condition is diagnosed after screening because a first-degree relative has the disease may appear asymptomatic but have severe disease histology, according to a new report.
About half of these patients had no symptoms, but disease histology was as severe as among those screened for other reasons, such as having symptomatic disease or high-risk conditions.
“This data supports current recommendations to screen all first-degree relatives of patients with celiac disease, especially pediatric patients in whom the ramifications of untreated disease may be significant,” wrote Michelle Gould, MD, and colleagues at the University of Toronto and McMaster University, Hamilton, Ont.
The study was published online in the Journal of Pediatric Gastroenterology and Nutrition.
Clinical characteristics
The incidence of celiac disease is higher among first-degree relatives of patients with the disease than among the general population, yet the clinical characteristics aren’t well described, the study authors wrote. Determining the clinical, serologic, and histologic phenotype of these patients could help clinicians determine whether continued universal screening of first-degree relatives is appropriate.
Dr. Gould and colleagues conducted a retrospective review of 227 patients diagnosed with celiac disease at McMaster Children’s Hospital between 1996 and 2014. The patients were categorized as being screened for celiac disease because a first-degree relative had the disease or because of other reasons. The other reasons included symptoms consistent with celiac disease or the presence of a high-risk clinical condition for which screening is recommended, such as type 1 diabetes or Down syndrome.
All patients were screened via tissue transglutaminase (tTG-IgA) tests. Positive serology was defined as tTG-IgA greater than the upper limit of normal in the presence of normal IgA immunoglobulin level for age.
The patients who were included in the study had biopsy-proven celiac disease in accordance with the Marsh criteria, which included Marsh III histology, Marsh II histology with positive serology, or Marsh I histology with positive serology and clinical symptoms.
The average age of the patients (144 girls and 83 boys) was 8 years at diagnosis. Among the patients, 49 (21.6%) were screened because a first-degree relative had celiac disease. Of those 49 patients, 24 (49%) were symptomatic, and 25 (51%) were asymptomatic.
By contrast, among the 178 patients who were screened for other reasons, 149 (83.7%) were symptomatic, and 29 (16.3%) were asymptomatic.
There was no significant difference between the patient groups with respect to Marsh score at biopsy and tTG-IgA levels at screening. Among the children who were screened because of family history, Marsh scores were equally severe as among other patients, whether they were symptomatic or not.
In addition, no statistically significant differences were found for other clinical characteristics, including body mass index z-score, weight z-score, height z-score, the presence of anemia, or a low mean corpuscular volume for age.
When comparing the characteristics of those screened because of family history and those screened for other high-risk conditions (type 1 diabetes and Down syndrome), the researchers found that rates of asymptomatic presentation were statistically similar between the groups, as were tissue transglutaminase values, Marsh scores, BMI z-scores, and hemoglobin levels at diagnosis. Although there was a statistical difference between the groups with respect to the mean corpuscular volume values at diagnosis, it was unlikely to be of clinical significance, the authors noted.
At 6 months, 1 year, and 2 years after diagnosis, among patients with repeat tTG-IgA measurements, 93 of 143 patients (65%), 52 of 68 patients (76.5%), and 80 of 90 patients (88.9%) had normal serum tTG-IgA levels, respectively. In comparing the proportion of patients whose tTG-IgA levels were normal, there was no difference between those screened because of family history and those screened for other reasons at any time point after diagnosis.
“This may suggest that the natural history of celiac disease is similar in these two groups following initiation of a gluten-free diet and that there are similar rates of compliance with this therapy regardless of the initial indication for screening,” the study authors wrote.
Clinical implications
Dr. Gould and colleagues noted that celiac disease was considered histologically severe – with a Marsh III score or higher – among nearly all patients whose condition was diagnosed because of family history. Histology was equally severe regardless of whether the patients were symptomatic or asymptomatic at screening – 100% of symptomatic patients had a high score, and 96% of asymptomatic patients had a high score.
“This emphasizes the importance of celiac screening in all patients with first-degree relatives with celiac disease, as symptom status does not predict diagnosis or severity of disease,” they wrote.
Previous studies have indicated that the prevalence of celiac disease is highest among siblings of patients with celiac disease, compared with other types of first-degree relatives, the authors wrote. However, they lacked this information in their records, which would be valuable for analysis in future studies.
In addition, ongoing research should investigate the optimal frequency of screening for first-degree relatives, they noted.
“One study suggests that individuals screened before 10 years of age should have repeat screening in their second decade for a small increased pick-up of diagnoses,” they wrote.
No funding for the study has been reported. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF PEDIATRIC GASTROENTEROLOGY AND NUTRITION
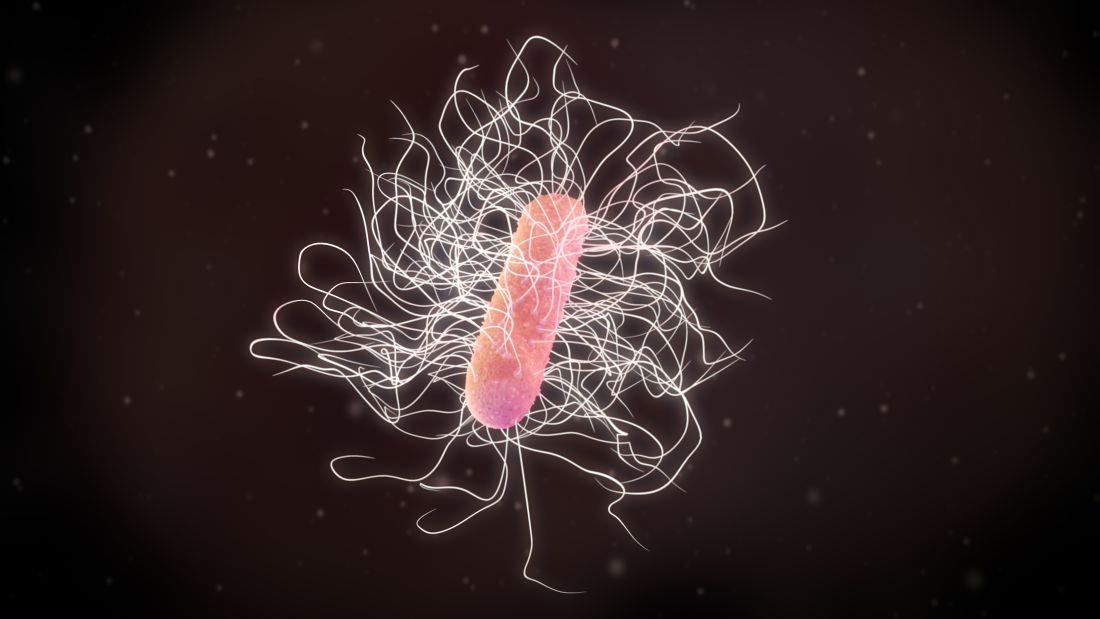
FMT in IBS: ‘We’ve been targeting the wrong part of the intestine’
VIENNA – , vs. it being administered into the large intestine, according to a new study.
Patients also reported an improvement in symptoms and quality of life with repeated doses of FMT (two doses, given 1 week apart), compared with a single dose in the small intestine, although statistical significance was not met.
“Administering a fecal transplant to the small intestine leads to long-term – up to 1 year in this analysis – colonization of beneficial bacteria, whereas administrating the fecal transplant to the large intestine results in the effect only lasting for the first 3 months,” said Magdy El-Salhy, MD, from the University of Bergen, Norway.
Dr. El-Salhy presented the results at the annual United European Gastroenterology Week meeting.
“It seems that bacteria in the small intestine play a more central role in IBS, as well as its associated fatigue, than bacteria in the large intestine,” Dr. El-Salhy said in an interview.
“Until now, we’ve been targeting the wrong part of the intestine,” he said.
The findings are the first to show that the small intestine is a more effective location for administering FMT than the large intestine for IBS. “It would be worthwhile doing similar [studies] in other diseases, especially in inflammatory bowel diseases,” said Dr. El-Salhy.
Researchers also didn’t expect the repeated dose to improve symptoms for a longer duration. “It really was revolutionary to see,” he added.
Some of Dr. El-Salhy’s patients have had up to 5 years of follow-up, although these results were not presented at this year’s UEG, he said.
“Around 75% of my patients have shown duration of response up to 3 years, and a few up to 5 years, on a 60-g dose from an earlier study group,” he said. “It’s an incredible result after a 10-minute treatment.”
In Dr. El-Salhy’s previous work, he found that increasing the dose from 30 g to 60 g increased the response from about 75% to about 90%. However, in this study presented, he found that increasing the dose to 90 g did not further increase the response. He also noted that while repeating the FMT dose improved symptoms and quality of life more than a single transplantation, it did not increase the response.
Targeting the small intestine
FMT has been widely investigated for the treatment of such conditions as psoriatic arthritis, Clostridioides difficile infection, and ulcerative colitis.
In this study, Dr. El-Salhy built on prior work (seven randomized controlled studies with varied outcomes) by asking whether the transplant dose increases FMT efficacy, which route of administration is more effective, and whether repeating FMT increases efficacy in patients with IBS.
A total of 186 patients were randomized to one of three groups: 90 g of frozen transplant into the large intestine (n = 62), 90 g of frozen transplant into the small intestine (n = 62), or 90 g of frozen transplant into the small intestine twice (with a 1-week interval; n = 62). FMT was administered via nasoduodenal tube and colonoscopy into the small and large intestines, respectively.
Outcomes were measured at 3, 6, and 12 months. The 12-month analysis of outcomes via patient questionnaire included 60, 61, and 60 patients, respectively.
The patient questionnaires included in the study were the IBS-SSS (a composite score of abdominal pain, duration of abdominal pain, bloating/distention, satisfaction with bowel habits, and IBS-related quality of life), the Birmingham IBS Symptom questionnaire, the Fatigue Assessment Scale questionnaire, the IBS-Quality of Life assessment, and the Short-Form Nepean Dyspepsia Index.
Fecal samples were taken and tested for bacterial loads. The bacterial profile and dysbiosis index were determined using the 16S rRNA gene.
At 3 months, patients had similar response rates, around 80%, across single dose in large intestine, single dose in small intestine, and repeat doses in small intestine.
At 6 months, the differences in response rates started to become noticeable, with 67.9% for single dose in large intestine, 71.4% for single dose in small intestine, and 86% for repeat doses in small intestine.
By 12 months, the difference in response rate between the single dose in the large and small intestines was statistically significant at 51.9% and 75.5%, respectively. The response rate to the repeat doses in the small intestine at 12 months (80.9%) was similar to that at 3 months (80.8%).
Side effects, including mild abdominal pain, diarrhea, and constipation, after FMT were seen for the first 5 days after treatment. “People who generally suffer from constipation get diarrhea after FMT and vice versa,” Dr. El-Salhy reported.
“Long-term side effects, as monitored up to 3 years, were not observed,” he added.
Treatment reduced IBS symptoms in all patient groups as measured by IBS-SSS scores. By 12 months, the score fell from around 350 to around 220 in patients who received a single dose in the large intestine, from around 300 to around 200 in patients who received a single dose in the small intestine, and from around 350 to around 170 in patients who received repeat doses in the small intestine.
Quality of life showed a statistically significant difference at 3 months between single and repeated doses in the small intestine and similarly at 6 and 12 months.
Chronic fatigue, experienced by many patients with IBS, was substantially reduced after FMT, Dr. El-Salhy noted. “This surge in energy is often more important to them than the gastrointestinal symptoms.”
Location affects bacterial success
Certain beneficial bacteria were found to thrive more when the donor transplant was administered to the small intestine than to the large intestine.
Of note, Lactobacillus species and Holdemanella biformis grew and then dropped off sharply after 3 months in patients who received a single-dose fecal transplant in the large intestine, while they grew after 3 months and continued to grow after 6 and 12 months in the groups who received a fecal transplant in the small intestine.
“We think bacteria in the small intestine have different characteristics to those in the large intestine,” Dr. El-Salhy said. “This is relatively new, because many years ago it was thought that bile acids prevented bacterial survival. Now we know lots can thrive in the small intestine.”
“It might be viral or some other component that is most effective here. We don’t know yet, but so far we have identified 11 bacteria of interest,” he added.
Broader questions
“Rather than focusing on a specific, single strain microbe as a predictor of success in a disease, the global equilibrium of microbiota is more important, and microbial ecology parameters would be interesting to assess,” remarked Gianluca Ianiro, MD, from the Università Cattolica del Sacro Cuore, Rome, who comoderated the session. “Selected survival of some bacteria through the gut may be the response.”
FMT emerged in response to the challenges posed by recurrent C. difficile infections, noted Alexander Khoruts, MD, a professor of medicine in the division of gastroenterology, hepatology, and nutrition at the University of Minnesota, Minneapolis, who was not involved in the research.
“It is much harder to achieve remodeling of the gut microbiome in non–C. difficile conditions where there is an intact and resilient indigenous microbiota,” he said in an interview. “Therefore, regimens using antibiotic preconditioning and repeated administrations of microbiota are generally more efficacious in achieving this objective.”
The specificity of the bacteria according to disease type targeted was important, said Dr. Khoruts, who has a special interest in gut microbiota.
“The big question in non–C. difficile indications is the composition of donor microbiota. It is critical that we understand the mechanisms involved in each target disease to design appropriate microbiota-based therapeutics,” he said.
Dr. Khoruts sounded a note of caution with respect to establishing the pharmacokinetic and dynamic data related to FMT, which is classified as a drug in the United States.
“It’s imperative that we develop the pharmacology discipline appropriate for this class of therapeutics, including their pharmacokinetics and pharmacodynamics, and an understanding of their potential toxicity and drug-drug interactions,” he said.
Drug distribution data are needed to determine host-microbiota interactions.
“This includes the small bowel microbiome, which continues to be woefully understudied,” Dr. Khoruts said.
Dr. El-Salhy reports no relevant financial relationships. Dr. Ianiro reports receiving personal fees for acting as speaker for Biocodex, Sofar, Malesci, and Tillotts Pharma, and for acting as consultant/advisor for Ferring Therapeutics, Biocodex, Tillotts Pharma, and Zambon. Dr. Khoruts reports he has patents pertaining to fecal microbiota separation from stool and their cryopreservation and lyopreservation.
Through the AGA Center for Gut Microbiome Research and Education, AGA is committed to keeping you up-to-speed on the latest news, research and policy updates related to the gut microbiome: www.gastro.org/microbiome.
A version of this article first appeared on Medscape.com.
VIENNA – , vs. it being administered into the large intestine, according to a new study.
Patients also reported an improvement in symptoms and quality of life with repeated doses of FMT (two doses, given 1 week apart), compared with a single dose in the small intestine, although statistical significance was not met.
“Administering a fecal transplant to the small intestine leads to long-term – up to 1 year in this analysis – colonization of beneficial bacteria, whereas administrating the fecal transplant to the large intestine results in the effect only lasting for the first 3 months,” said Magdy El-Salhy, MD, from the University of Bergen, Norway.
Dr. El-Salhy presented the results at the annual United European Gastroenterology Week meeting.
“It seems that bacteria in the small intestine play a more central role in IBS, as well as its associated fatigue, than bacteria in the large intestine,” Dr. El-Salhy said in an interview.
“Until now, we’ve been targeting the wrong part of the intestine,” he said.
The findings are the first to show that the small intestine is a more effective location for administering FMT than the large intestine for IBS. “It would be worthwhile doing similar [studies] in other diseases, especially in inflammatory bowel diseases,” said Dr. El-Salhy.
Researchers also didn’t expect the repeated dose to improve symptoms for a longer duration. “It really was revolutionary to see,” he added.
Some of Dr. El-Salhy’s patients have had up to 5 years of follow-up, although these results were not presented at this year’s UEG, he said.
“Around 75% of my patients have shown duration of response up to 3 years, and a few up to 5 years, on a 60-g dose from an earlier study group,” he said. “It’s an incredible result after a 10-minute treatment.”
In Dr. El-Salhy’s previous work, he found that increasing the dose from 30 g to 60 g increased the response from about 75% to about 90%. However, in this study presented, he found that increasing the dose to 90 g did not further increase the response. He also noted that while repeating the FMT dose improved symptoms and quality of life more than a single transplantation, it did not increase the response.
Targeting the small intestine
FMT has been widely investigated for the treatment of such conditions as psoriatic arthritis, Clostridioides difficile infection, and ulcerative colitis.
In this study, Dr. El-Salhy built on prior work (seven randomized controlled studies with varied outcomes) by asking whether the transplant dose increases FMT efficacy, which route of administration is more effective, and whether repeating FMT increases efficacy in patients with IBS.
A total of 186 patients were randomized to one of three groups: 90 g of frozen transplant into the large intestine (n = 62), 90 g of frozen transplant into the small intestine (n = 62), or 90 g of frozen transplant into the small intestine twice (with a 1-week interval; n = 62). FMT was administered via nasoduodenal tube and colonoscopy into the small and large intestines, respectively.
Outcomes were measured at 3, 6, and 12 months. The 12-month analysis of outcomes via patient questionnaire included 60, 61, and 60 patients, respectively.
The patient questionnaires included in the study were the IBS-SSS (a composite score of abdominal pain, duration of abdominal pain, bloating/distention, satisfaction with bowel habits, and IBS-related quality of life), the Birmingham IBS Symptom questionnaire, the Fatigue Assessment Scale questionnaire, the IBS-Quality of Life assessment, and the Short-Form Nepean Dyspepsia Index.
Fecal samples were taken and tested for bacterial loads. The bacterial profile and dysbiosis index were determined using the 16S rRNA gene.
At 3 months, patients had similar response rates, around 80%, across single dose in large intestine, single dose in small intestine, and repeat doses in small intestine.
At 6 months, the differences in response rates started to become noticeable, with 67.9% for single dose in large intestine, 71.4% for single dose in small intestine, and 86% for repeat doses in small intestine.
By 12 months, the difference in response rate between the single dose in the large and small intestines was statistically significant at 51.9% and 75.5%, respectively. The response rate to the repeat doses in the small intestine at 12 months (80.9%) was similar to that at 3 months (80.8%).
Side effects, including mild abdominal pain, diarrhea, and constipation, after FMT were seen for the first 5 days after treatment. “People who generally suffer from constipation get diarrhea after FMT and vice versa,” Dr. El-Salhy reported.
“Long-term side effects, as monitored up to 3 years, were not observed,” he added.
Treatment reduced IBS symptoms in all patient groups as measured by IBS-SSS scores. By 12 months, the score fell from around 350 to around 220 in patients who received a single dose in the large intestine, from around 300 to around 200 in patients who received a single dose in the small intestine, and from around 350 to around 170 in patients who received repeat doses in the small intestine.
Quality of life showed a statistically significant difference at 3 months between single and repeated doses in the small intestine and similarly at 6 and 12 months.
Chronic fatigue, experienced by many patients with IBS, was substantially reduced after FMT, Dr. El-Salhy noted. “This surge in energy is often more important to them than the gastrointestinal symptoms.”
Location affects bacterial success
Certain beneficial bacteria were found to thrive more when the donor transplant was administered to the small intestine than to the large intestine.
Of note, Lactobacillus species and Holdemanella biformis grew and then dropped off sharply after 3 months in patients who received a single-dose fecal transplant in the large intestine, while they grew after 3 months and continued to grow after 6 and 12 months in the groups who received a fecal transplant in the small intestine.
“We think bacteria in the small intestine have different characteristics to those in the large intestine,” Dr. El-Salhy said. “This is relatively new, because many years ago it was thought that bile acids prevented bacterial survival. Now we know lots can thrive in the small intestine.”
“It might be viral or some other component that is most effective here. We don’t know yet, but so far we have identified 11 bacteria of interest,” he added.
Broader questions
“Rather than focusing on a specific, single strain microbe as a predictor of success in a disease, the global equilibrium of microbiota is more important, and microbial ecology parameters would be interesting to assess,” remarked Gianluca Ianiro, MD, from the Università Cattolica del Sacro Cuore, Rome, who comoderated the session. “Selected survival of some bacteria through the gut may be the response.”
FMT emerged in response to the challenges posed by recurrent C. difficile infections, noted Alexander Khoruts, MD, a professor of medicine in the division of gastroenterology, hepatology, and nutrition at the University of Minnesota, Minneapolis, who was not involved in the research.
“It is much harder to achieve remodeling of the gut microbiome in non–C. difficile conditions where there is an intact and resilient indigenous microbiota,” he said in an interview. “Therefore, regimens using antibiotic preconditioning and repeated administrations of microbiota are generally more efficacious in achieving this objective.”
The specificity of the bacteria according to disease type targeted was important, said Dr. Khoruts, who has a special interest in gut microbiota.
“The big question in non–C. difficile indications is the composition of donor microbiota. It is critical that we understand the mechanisms involved in each target disease to design appropriate microbiota-based therapeutics,” he said.
Dr. Khoruts sounded a note of caution with respect to establishing the pharmacokinetic and dynamic data related to FMT, which is classified as a drug in the United States.
“It’s imperative that we develop the pharmacology discipline appropriate for this class of therapeutics, including their pharmacokinetics and pharmacodynamics, and an understanding of their potential toxicity and drug-drug interactions,” he said.
Drug distribution data are needed to determine host-microbiota interactions.
“This includes the small bowel microbiome, which continues to be woefully understudied,” Dr. Khoruts said.
Dr. El-Salhy reports no relevant financial relationships. Dr. Ianiro reports receiving personal fees for acting as speaker for Biocodex, Sofar, Malesci, and Tillotts Pharma, and for acting as consultant/advisor for Ferring Therapeutics, Biocodex, Tillotts Pharma, and Zambon. Dr. Khoruts reports he has patents pertaining to fecal microbiota separation from stool and their cryopreservation and lyopreservation.
Through the AGA Center for Gut Microbiome Research and Education, AGA is committed to keeping you up-to-speed on the latest news, research and policy updates related to the gut microbiome: www.gastro.org/microbiome.
A version of this article first appeared on Medscape.com.
VIENNA – , vs. it being administered into the large intestine, according to a new study.
Patients also reported an improvement in symptoms and quality of life with repeated doses of FMT (two doses, given 1 week apart), compared with a single dose in the small intestine, although statistical significance was not met.
“Administering a fecal transplant to the small intestine leads to long-term – up to 1 year in this analysis – colonization of beneficial bacteria, whereas administrating the fecal transplant to the large intestine results in the effect only lasting for the first 3 months,” said Magdy El-Salhy, MD, from the University of Bergen, Norway.
Dr. El-Salhy presented the results at the annual United European Gastroenterology Week meeting.
“It seems that bacteria in the small intestine play a more central role in IBS, as well as its associated fatigue, than bacteria in the large intestine,” Dr. El-Salhy said in an interview.
“Until now, we’ve been targeting the wrong part of the intestine,” he said.
The findings are the first to show that the small intestine is a more effective location for administering FMT than the large intestine for IBS. “It would be worthwhile doing similar [studies] in other diseases, especially in inflammatory bowel diseases,” said Dr. El-Salhy.
Researchers also didn’t expect the repeated dose to improve symptoms for a longer duration. “It really was revolutionary to see,” he added.
Some of Dr. El-Salhy’s patients have had up to 5 years of follow-up, although these results were not presented at this year’s UEG, he said.
“Around 75% of my patients have shown duration of response up to 3 years, and a few up to 5 years, on a 60-g dose from an earlier study group,” he said. “It’s an incredible result after a 10-minute treatment.”
In Dr. El-Salhy’s previous work, he found that increasing the dose from 30 g to 60 g increased the response from about 75% to about 90%. However, in this study presented, he found that increasing the dose to 90 g did not further increase the response. He also noted that while repeating the FMT dose improved symptoms and quality of life more than a single transplantation, it did not increase the response.
Targeting the small intestine
FMT has been widely investigated for the treatment of such conditions as psoriatic arthritis, Clostridioides difficile infection, and ulcerative colitis.
In this study, Dr. El-Salhy built on prior work (seven randomized controlled studies with varied outcomes) by asking whether the transplant dose increases FMT efficacy, which route of administration is more effective, and whether repeating FMT increases efficacy in patients with IBS.
A total of 186 patients were randomized to one of three groups: 90 g of frozen transplant into the large intestine (n = 62), 90 g of frozen transplant into the small intestine (n = 62), or 90 g of frozen transplant into the small intestine twice (with a 1-week interval; n = 62). FMT was administered via nasoduodenal tube and colonoscopy into the small and large intestines, respectively.
Outcomes were measured at 3, 6, and 12 months. The 12-month analysis of outcomes via patient questionnaire included 60, 61, and 60 patients, respectively.
The patient questionnaires included in the study were the IBS-SSS (a composite score of abdominal pain, duration of abdominal pain, bloating/distention, satisfaction with bowel habits, and IBS-related quality of life), the Birmingham IBS Symptom questionnaire, the Fatigue Assessment Scale questionnaire, the IBS-Quality of Life assessment, and the Short-Form Nepean Dyspepsia Index.
Fecal samples were taken and tested for bacterial loads. The bacterial profile and dysbiosis index were determined using the 16S rRNA gene.
At 3 months, patients had similar response rates, around 80%, across single dose in large intestine, single dose in small intestine, and repeat doses in small intestine.
At 6 months, the differences in response rates started to become noticeable, with 67.9% for single dose in large intestine, 71.4% for single dose in small intestine, and 86% for repeat doses in small intestine.
By 12 months, the difference in response rate between the single dose in the large and small intestines was statistically significant at 51.9% and 75.5%, respectively. The response rate to the repeat doses in the small intestine at 12 months (80.9%) was similar to that at 3 months (80.8%).
Side effects, including mild abdominal pain, diarrhea, and constipation, after FMT were seen for the first 5 days after treatment. “People who generally suffer from constipation get diarrhea after FMT and vice versa,” Dr. El-Salhy reported.
“Long-term side effects, as monitored up to 3 years, were not observed,” he added.
Treatment reduced IBS symptoms in all patient groups as measured by IBS-SSS scores. By 12 months, the score fell from around 350 to around 220 in patients who received a single dose in the large intestine, from around 300 to around 200 in patients who received a single dose in the small intestine, and from around 350 to around 170 in patients who received repeat doses in the small intestine.
Quality of life showed a statistically significant difference at 3 months between single and repeated doses in the small intestine and similarly at 6 and 12 months.
Chronic fatigue, experienced by many patients with IBS, was substantially reduced after FMT, Dr. El-Salhy noted. “This surge in energy is often more important to them than the gastrointestinal symptoms.”
Location affects bacterial success
Certain beneficial bacteria were found to thrive more when the donor transplant was administered to the small intestine than to the large intestine.
Of note, Lactobacillus species and Holdemanella biformis grew and then dropped off sharply after 3 months in patients who received a single-dose fecal transplant in the large intestine, while they grew after 3 months and continued to grow after 6 and 12 months in the groups who received a fecal transplant in the small intestine.
“We think bacteria in the small intestine have different characteristics to those in the large intestine,” Dr. El-Salhy said. “This is relatively new, because many years ago it was thought that bile acids prevented bacterial survival. Now we know lots can thrive in the small intestine.”
“It might be viral or some other component that is most effective here. We don’t know yet, but so far we have identified 11 bacteria of interest,” he added.
Broader questions
“Rather than focusing on a specific, single strain microbe as a predictor of success in a disease, the global equilibrium of microbiota is more important, and microbial ecology parameters would be interesting to assess,” remarked Gianluca Ianiro, MD, from the Università Cattolica del Sacro Cuore, Rome, who comoderated the session. “Selected survival of some bacteria through the gut may be the response.”
FMT emerged in response to the challenges posed by recurrent C. difficile infections, noted Alexander Khoruts, MD, a professor of medicine in the division of gastroenterology, hepatology, and nutrition at the University of Minnesota, Minneapolis, who was not involved in the research.
“It is much harder to achieve remodeling of the gut microbiome in non–C. difficile conditions where there is an intact and resilient indigenous microbiota,” he said in an interview. “Therefore, regimens using antibiotic preconditioning and repeated administrations of microbiota are generally more efficacious in achieving this objective.”
The specificity of the bacteria according to disease type targeted was important, said Dr. Khoruts, who has a special interest in gut microbiota.
“The big question in non–C. difficile indications is the composition of donor microbiota. It is critical that we understand the mechanisms involved in each target disease to design appropriate microbiota-based therapeutics,” he said.
Dr. Khoruts sounded a note of caution with respect to establishing the pharmacokinetic and dynamic data related to FMT, which is classified as a drug in the United States.
“It’s imperative that we develop the pharmacology discipline appropriate for this class of therapeutics, including their pharmacokinetics and pharmacodynamics, and an understanding of their potential toxicity and drug-drug interactions,” he said.
Drug distribution data are needed to determine host-microbiota interactions.
“This includes the small bowel microbiome, which continues to be woefully understudied,” Dr. Khoruts said.
Dr. El-Salhy reports no relevant financial relationships. Dr. Ianiro reports receiving personal fees for acting as speaker for Biocodex, Sofar, Malesci, and Tillotts Pharma, and for acting as consultant/advisor for Ferring Therapeutics, Biocodex, Tillotts Pharma, and Zambon. Dr. Khoruts reports he has patents pertaining to fecal microbiota separation from stool and their cryopreservation and lyopreservation.
Through the AGA Center for Gut Microbiome Research and Education, AGA is committed to keeping you up-to-speed on the latest news, research and policy updates related to the gut microbiome: www.gastro.org/microbiome.
A version of this article first appeared on Medscape.com.
Vedolizumab linked to increased treatment failure in older patients with Crohn’s
Findings indicate that vedolizumab is associated with an increased risk for treatment failure in older patients with inflammatory bowel disease (IBD), as compared with tumor necrosis factor (TNF) antagonists, according to a new study published in JAMA Network Open.
Although the incidence and prevalence of IBD among older adults are rapidly increasing, there is a lack of evidence-based treatment guidance for these patients, who represent less than 5% of participants in IBD-related clinical trials, wrote Siddharth Singh, MD, a gastroenterologist and assistant professor of medicine at the University of California, San Diego, and colleagues.
“Older patients are frequently undertreated and mismanaged with long-term corticosteroid use and limited use of steroid-sparing therapies owing to patients’ and clinicians’ concerns about the safety of immunosuppressive therapy,” the authors wrote. “There is considerable need for evidence-based treatment guidance for older patients with IBD.”
The researchers undertook an observational study of the comparative effectiveness of vedolizumab versus TNF antagonists (namely infliximab, adalimumab, and golimumab) among older patients with IBD in Denmark. Using the Danish National Patient Register, the authors included 754 patients aged 50 years and older who received treatment between 2005 and 2018.
The primary effectiveness outcome was treatment failure, defined as the composite 1-year risk of IBD-related hospitalization, IBD-related surgery, or a new corticosteroid prescription more than 6 weeks after initiation of treatment with a biologic. Secondary effectiveness outcomes included time to each component included in the composite score.
The primary safety outcome was the risk of serious infections, defined as those that required hospitalization. Secondary safety outcomes were risk of cancer and major adverse cardiovascular or venous thromboembolic events.
The researchers conducted a 1:1 propensity score-matched analysis, accounting for patient, disease, and treatment factors. The 754 patients included 377 incident users of vedolizumab, including 177 with Crohn’s disease; and 377 incident users of TNF antagonists, including 182 with Crohn’s disease. The average follow-up after treatment initiation occurred between 32 and 40 weeks.
Notably, patients treated with vedolizumab were more likely than those treated with TNF antagonists to have multimorbidity, at 16.2% versus 14.1%, and a higher burden of frailty, at 2.7% versus 1.9%. No significant differences were observed in the proportion of patients with recent immunomodulator and corticosteroid exposure.
Overall, vedolizumab was associated with a 31% increased risk of treatment failure (45.4%), compared with TNF antagonists (34.7%). This included an increased risk of IBD-related hospitalization (27.8% versus 16.3%) and IBD-related major abdominal surgery (21.3% versus 8%).
Among patients with Crohn’s disease, vedolizumab was associated with a 77% increased risk of treatment failure, as well as a greater need for corticosteroids. There was no significant difference in the risk of treatment failure or need for corticosteroids in patients with ulcerative colitis
No significant differences were seen in the risk of serious infections between patients treated with vedolizumab or TNF antagonists, at 8.2% versus 8.7%. This didn’t change by IBD phenotype, age at time of biologic therapy initiation, or treatment with biologic monotherapy versus combination therapy with immunomodulators.
The overall incidence of major adverse cardiovascular or venous thromboembolic events was similar among the groups. Rates of new malignant neoplasms were low, with fewer than five events.
In a subgroup analysis based on the Charlson Comorbidity Index, vedolizumab was associated with a 63% increased risk of treatment failure for patients without comorbidities but not for patients with comorbidities.
“This study adds to the body of literature comparing vedolizumab and anti-TNF in older adults. The findings have been mixed, in some part due to differences in study designs,” said Ashwin N. Ananthakrishnan, MBBS, MPH, associate professor of medicine at Harvard Medical School and a gastroenterologist at Massachusetts General Hospital, both in Boston.
Dr. Ananthakrishnan, who wasn’t involved with this study, has previously researched the two treatments and found that they are comparably safe in older adults. In fact, among patients with significant comorbidity, vedolizumab may be safer. However, the Danish study wasn’t powered to describe that, he said. Moreover, patient characteristics and treatment approaches likely differ between the United States and Denmark.
“Overall, the findings are reassuring. Often when we treat older adults, the emphasis is on safety,” he said. “But by highlighting the difference in clinical response rates – their findings being consistent with a study we published a few years ago – it highlights the importance of also considering efficacy and onset of action for specific disease phenotypes in treatment selection.”
Dr. Ananthakrishnan and colleagues are currently developing clinical tools for risk stratification and prognostication in older adults with IBD, including functional and frailty assessments. “Biologically, older adults may be particularly vulnerable to specific treatment risks such as infections and cancer, but they are also vulnerable to the consequences of untreated disease, including loss of functional independence and frailty,” he explained. “Thus, arriving at the right risk to benefit balance is critically important when making treatment decisions for older adults.”
The study by Dr. Singh and colleagues was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases and the Danish National Research Foundation. Dr. Singh reported receiving grants from pharmaceutical companies unrelated to the study, as well as support from the International Organization for the Study of Inflammatory Bowel Disease Operating Grant and Litwin Pioneers in IBD. No other disclosures were reported. Dr. Ananthakrishnan reported no relevant disclosures.
Findings indicate that vedolizumab is associated with an increased risk for treatment failure in older patients with inflammatory bowel disease (IBD), as compared with tumor necrosis factor (TNF) antagonists, according to a new study published in JAMA Network Open.
Although the incidence and prevalence of IBD among older adults are rapidly increasing, there is a lack of evidence-based treatment guidance for these patients, who represent less than 5% of participants in IBD-related clinical trials, wrote Siddharth Singh, MD, a gastroenterologist and assistant professor of medicine at the University of California, San Diego, and colleagues.
“Older patients are frequently undertreated and mismanaged with long-term corticosteroid use and limited use of steroid-sparing therapies owing to patients’ and clinicians’ concerns about the safety of immunosuppressive therapy,” the authors wrote. “There is considerable need for evidence-based treatment guidance for older patients with IBD.”
The researchers undertook an observational study of the comparative effectiveness of vedolizumab versus TNF antagonists (namely infliximab, adalimumab, and golimumab) among older patients with IBD in Denmark. Using the Danish National Patient Register, the authors included 754 patients aged 50 years and older who received treatment between 2005 and 2018.
The primary effectiveness outcome was treatment failure, defined as the composite 1-year risk of IBD-related hospitalization, IBD-related surgery, or a new corticosteroid prescription more than 6 weeks after initiation of treatment with a biologic. Secondary effectiveness outcomes included time to each component included in the composite score.
The primary safety outcome was the risk of serious infections, defined as those that required hospitalization. Secondary safety outcomes were risk of cancer and major adverse cardiovascular or venous thromboembolic events.
The researchers conducted a 1:1 propensity score-matched analysis, accounting for patient, disease, and treatment factors. The 754 patients included 377 incident users of vedolizumab, including 177 with Crohn’s disease; and 377 incident users of TNF antagonists, including 182 with Crohn’s disease. The average follow-up after treatment initiation occurred between 32 and 40 weeks.
Notably, patients treated with vedolizumab were more likely than those treated with TNF antagonists to have multimorbidity, at 16.2% versus 14.1%, and a higher burden of frailty, at 2.7% versus 1.9%. No significant differences were observed in the proportion of patients with recent immunomodulator and corticosteroid exposure.
Overall, vedolizumab was associated with a 31% increased risk of treatment failure (45.4%), compared with TNF antagonists (34.7%). This included an increased risk of IBD-related hospitalization (27.8% versus 16.3%) and IBD-related major abdominal surgery (21.3% versus 8%).
Among patients with Crohn’s disease, vedolizumab was associated with a 77% increased risk of treatment failure, as well as a greater need for corticosteroids. There was no significant difference in the risk of treatment failure or need for corticosteroids in patients with ulcerative colitis
No significant differences were seen in the risk of serious infections between patients treated with vedolizumab or TNF antagonists, at 8.2% versus 8.7%. This didn’t change by IBD phenotype, age at time of biologic therapy initiation, or treatment with biologic monotherapy versus combination therapy with immunomodulators.
The overall incidence of major adverse cardiovascular or venous thromboembolic events was similar among the groups. Rates of new malignant neoplasms were low, with fewer than five events.
In a subgroup analysis based on the Charlson Comorbidity Index, vedolizumab was associated with a 63% increased risk of treatment failure for patients without comorbidities but not for patients with comorbidities.
“This study adds to the body of literature comparing vedolizumab and anti-TNF in older adults. The findings have been mixed, in some part due to differences in study designs,” said Ashwin N. Ananthakrishnan, MBBS, MPH, associate professor of medicine at Harvard Medical School and a gastroenterologist at Massachusetts General Hospital, both in Boston.
Dr. Ananthakrishnan, who wasn’t involved with this study, has previously researched the two treatments and found that they are comparably safe in older adults. In fact, among patients with significant comorbidity, vedolizumab may be safer. However, the Danish study wasn’t powered to describe that, he said. Moreover, patient characteristics and treatment approaches likely differ between the United States and Denmark.
“Overall, the findings are reassuring. Often when we treat older adults, the emphasis is on safety,” he said. “But by highlighting the difference in clinical response rates – their findings being consistent with a study we published a few years ago – it highlights the importance of also considering efficacy and onset of action for specific disease phenotypes in treatment selection.”
Dr. Ananthakrishnan and colleagues are currently developing clinical tools for risk stratification and prognostication in older adults with IBD, including functional and frailty assessments. “Biologically, older adults may be particularly vulnerable to specific treatment risks such as infections and cancer, but they are also vulnerable to the consequences of untreated disease, including loss of functional independence and frailty,” he explained. “Thus, arriving at the right risk to benefit balance is critically important when making treatment decisions for older adults.”
The study by Dr. Singh and colleagues was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases and the Danish National Research Foundation. Dr. Singh reported receiving grants from pharmaceutical companies unrelated to the study, as well as support from the International Organization for the Study of Inflammatory Bowel Disease Operating Grant and Litwin Pioneers in IBD. No other disclosures were reported. Dr. Ananthakrishnan reported no relevant disclosures.
Findings indicate that vedolizumab is associated with an increased risk for treatment failure in older patients with inflammatory bowel disease (IBD), as compared with tumor necrosis factor (TNF) antagonists, according to a new study published in JAMA Network Open.
Although the incidence and prevalence of IBD among older adults are rapidly increasing, there is a lack of evidence-based treatment guidance for these patients, who represent less than 5% of participants in IBD-related clinical trials, wrote Siddharth Singh, MD, a gastroenterologist and assistant professor of medicine at the University of California, San Diego, and colleagues.
“Older patients are frequently undertreated and mismanaged with long-term corticosteroid use and limited use of steroid-sparing therapies owing to patients’ and clinicians’ concerns about the safety of immunosuppressive therapy,” the authors wrote. “There is considerable need for evidence-based treatment guidance for older patients with IBD.”
The researchers undertook an observational study of the comparative effectiveness of vedolizumab versus TNF antagonists (namely infliximab, adalimumab, and golimumab) among older patients with IBD in Denmark. Using the Danish National Patient Register, the authors included 754 patients aged 50 years and older who received treatment between 2005 and 2018.
The primary effectiveness outcome was treatment failure, defined as the composite 1-year risk of IBD-related hospitalization, IBD-related surgery, or a new corticosteroid prescription more than 6 weeks after initiation of treatment with a biologic. Secondary effectiveness outcomes included time to each component included in the composite score.
The primary safety outcome was the risk of serious infections, defined as those that required hospitalization. Secondary safety outcomes were risk of cancer and major adverse cardiovascular or venous thromboembolic events.
The researchers conducted a 1:1 propensity score-matched analysis, accounting for patient, disease, and treatment factors. The 754 patients included 377 incident users of vedolizumab, including 177 with Crohn’s disease; and 377 incident users of TNF antagonists, including 182 with Crohn’s disease. The average follow-up after treatment initiation occurred between 32 and 40 weeks.
Notably, patients treated with vedolizumab were more likely than those treated with TNF antagonists to have multimorbidity, at 16.2% versus 14.1%, and a higher burden of frailty, at 2.7% versus 1.9%. No significant differences were observed in the proportion of patients with recent immunomodulator and corticosteroid exposure.
Overall, vedolizumab was associated with a 31% increased risk of treatment failure (45.4%), compared with TNF antagonists (34.7%). This included an increased risk of IBD-related hospitalization (27.8% versus 16.3%) and IBD-related major abdominal surgery (21.3% versus 8%).
Among patients with Crohn’s disease, vedolizumab was associated with a 77% increased risk of treatment failure, as well as a greater need for corticosteroids. There was no significant difference in the risk of treatment failure or need for corticosteroids in patients with ulcerative colitis
No significant differences were seen in the risk of serious infections between patients treated with vedolizumab or TNF antagonists, at 8.2% versus 8.7%. This didn’t change by IBD phenotype, age at time of biologic therapy initiation, or treatment with biologic monotherapy versus combination therapy with immunomodulators.
The overall incidence of major adverse cardiovascular or venous thromboembolic events was similar among the groups. Rates of new malignant neoplasms were low, with fewer than five events.
In a subgroup analysis based on the Charlson Comorbidity Index, vedolizumab was associated with a 63% increased risk of treatment failure for patients without comorbidities but not for patients with comorbidities.
“This study adds to the body of literature comparing vedolizumab and anti-TNF in older adults. The findings have been mixed, in some part due to differences in study designs,” said Ashwin N. Ananthakrishnan, MBBS, MPH, associate professor of medicine at Harvard Medical School and a gastroenterologist at Massachusetts General Hospital, both in Boston.
Dr. Ananthakrishnan, who wasn’t involved with this study, has previously researched the two treatments and found that they are comparably safe in older adults. In fact, among patients with significant comorbidity, vedolizumab may be safer. However, the Danish study wasn’t powered to describe that, he said. Moreover, patient characteristics and treatment approaches likely differ between the United States and Denmark.
“Overall, the findings are reassuring. Often when we treat older adults, the emphasis is on safety,” he said. “But by highlighting the difference in clinical response rates – their findings being consistent with a study we published a few years ago – it highlights the importance of also considering efficacy and onset of action for specific disease phenotypes in treatment selection.”
Dr. Ananthakrishnan and colleagues are currently developing clinical tools for risk stratification and prognostication in older adults with IBD, including functional and frailty assessments. “Biologically, older adults may be particularly vulnerable to specific treatment risks such as infections and cancer, but they are also vulnerable to the consequences of untreated disease, including loss of functional independence and frailty,” he explained. “Thus, arriving at the right risk to benefit balance is critically important when making treatment decisions for older adults.”
The study by Dr. Singh and colleagues was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases and the Danish National Research Foundation. Dr. Singh reported receiving grants from pharmaceutical companies unrelated to the study, as well as support from the International Organization for the Study of Inflammatory Bowel Disease Operating Grant and Litwin Pioneers in IBD. No other disclosures were reported. Dr. Ananthakrishnan reported no relevant disclosures.
FROM JAMA NETWORK OPEN
Patients differ with providers on definitions for IBD remission
Patients’ reports of remission from inflammatory bowel disease (IBD) don’t always line up with remission as defined by patient-reported outcomes (PROs) or physician global assessment (PGA), according to a study published in Inflammatory Bowel Diseases.
Patients have various definitions of remission, which may focus on symptom improvement and the impact on daily activities, while physicians tend to focus on test results. “Examining patient-reported remission may be a valuable approach to better understand remission from the perspective of patients and can assist in aligning shared decision-making between patients and health care providers,” wrote Kendra Kamp, PhD, assistant professor of biobehavioral nursing and health informatics at the University of Washington, and colleagues, on behalf of the IBD Qorus.
In a retrospective study, Dr. Kamp and colleagues analyzed 3,257 deidentified surveys from 2,004 patients who participated in the Crohn’s and Colitis Foundation’s IBD Qorus Learning Health System between September 2019 and February 2021. Adults with IBD who participated in the IBD Qorus received an email before their gastroenterology clinical appointment with a link to a survey that asked questions about primary concerns or goals, symptoms, well-being, recent health care utilization, and medication use.
The researchers looked at the clinical and demographic factors associated with discordance among patient-defined remission, PROs, and PGAs. Patient-defined remission was captured as a yes/no response to the question: “Do you feel your disease is currently in remission (by remission we mean a complete absence of IBD-related symptoms)?”
PROs for ulcerative colitis were measured through stool frequency and rectal bleeding, with remission defined as no blood in the stool and a normal (or fewer than normal) number of stools. For Crohn’s disease, PROs were measured through the average number of liquid stools, abdominal pain, and general well-being, with remission defined as two or fewer loose stools, no or mild abdominal pain, and feeling generally well or slightly under par.
For PGAs, clinicians selected whether the patient had normal, mild, moderate, or severe disease activity. The values were included in the analysis if the clinicians completed the assessment within 14 days of the patient’s survey.
Among the 2,004 patients, 806 had ulcerative colitis and 1,198 had Crohn’s disease. Patients with ulcerative colitis as well as those with Crohn’s disease were aged 44 years on average. Most of the patients were women: 58% with ulcerative colitis and 56% with Crohn’s disease.
Among the 1,316 visits for ulcerative colitis, 668 patients (51%) self-reported to be in remission, compared with 55% in remission based on PROs. Of the people in PRO–defined remission, 77% reported being in remission, and 23% reported active disease. Of the people with PRO–defined active disease, 81% reported active disease and 19% reported remission. Overall concordance was 79% between patient self-reported and PRO–defined remission.
Discordance in patient-defined remission for ulcerative colitis was primarily influenced by tolerance of an increased stool frequency. About 25% of patients with one or two stools more than normal reported being in remission.
A subset of 397 ulcerative colitis visits had an associated PGA score. Among patients in PGA-defined remission, 53% reported being in remission. Of those with PGA-defined active disease, 60% reported active disease. Overall, concordance was 49% between patient self-reported and PGA-defined remission.
Among the 1,947 visits for Crohn’s disease, 929 patients (48%) self-reported to be in remission, compared with 63% in remission based on PRO. Of the people in PRO-defined remission, 63% reported being in remission, although 37% reported active disease. Of the people with PRO-defined active disease, 79% reported active disease and 21% reported remission. Overall concordance was 69% between patient self-reported and patient-reported outcomes–defined remission.
Discordance in patient-defined remission for Crohn’s disease was primarily influenced by patients with a tolerance of mild to moderate symptoms.
A subset of 575 Crohn’s disease visits had an associated PGA score. Among patients in PGA-defined remission, 52% reported being in remission. Of those with PGA-defined active disease, 57% reported active disease. Overall concordance was 54% between patient self-reported and PGA-defined remission.
Several factors were associated with discordance in remission definitions. Among patients in PRO-defined remission, those who had a diagnosis of IBD for fewer than 5 years were more likely to report having active disease compared with those who had received a diagnosis more than 15 years before.
Patients with high health confidence in managing their condition were less likely to report having active disease. In addition, patients with Crohn’s disease were more likely to report having active disease if they were using prednisone or opioids or if they had an IBD-related emergency department visit in the past 6 months.
“Studies that address the discordance between patient-reported outcomes and clinician assessment in inflammatory bowel disease are important to develop a patient-centered model of practice,” said Sadeea Abbasi, MD, PhD, a gastroenterologist and IBD specialist at Cedars-Sinai Gastroenterology in Santa Monica, Calif.
Dr. Abbasi, who wasn’t involved with this study, has promoted patient advocacy in IBD management.
“Measurable objective data are not the only parameter to measure disease outcomes or individualize treatment protocols. In fact, outcomes can dramatically change if the patient’s experience is not taken into account. Studies that address this reality are crucial for physicians to be able to advocate for their patients,” she said. “The empowered physician-patient relationship is one of strength and trust and tends to be associated with the best overall outcomes.”
IBD Qorus is an initiative of the Crohn’s and Colitis Foundation and is supported by numerous pharmaceutical companies. Supporters had no involvement in the study and didn’t provide direct funding for any aspect of the study. The authors have received funding from the Crohn’s and Colitis Foundation, National Institutes of Health, and various foundations and pharmaceutical companies. Dr. Abbasi reported no relevant disclosures.
Patients’ reports of remission from inflammatory bowel disease (IBD) don’t always line up with remission as defined by patient-reported outcomes (PROs) or physician global assessment (PGA), according to a study published in Inflammatory Bowel Diseases.
Patients have various definitions of remission, which may focus on symptom improvement and the impact on daily activities, while physicians tend to focus on test results. “Examining patient-reported remission may be a valuable approach to better understand remission from the perspective of patients and can assist in aligning shared decision-making between patients and health care providers,” wrote Kendra Kamp, PhD, assistant professor of biobehavioral nursing and health informatics at the University of Washington, and colleagues, on behalf of the IBD Qorus.
In a retrospective study, Dr. Kamp and colleagues analyzed 3,257 deidentified surveys from 2,004 patients who participated in the Crohn’s and Colitis Foundation’s IBD Qorus Learning Health System between September 2019 and February 2021. Adults with IBD who participated in the IBD Qorus received an email before their gastroenterology clinical appointment with a link to a survey that asked questions about primary concerns or goals, symptoms, well-being, recent health care utilization, and medication use.
The researchers looked at the clinical and demographic factors associated with discordance among patient-defined remission, PROs, and PGAs. Patient-defined remission was captured as a yes/no response to the question: “Do you feel your disease is currently in remission (by remission we mean a complete absence of IBD-related symptoms)?”
PROs for ulcerative colitis were measured through stool frequency and rectal bleeding, with remission defined as no blood in the stool and a normal (or fewer than normal) number of stools. For Crohn’s disease, PROs were measured through the average number of liquid stools, abdominal pain, and general well-being, with remission defined as two or fewer loose stools, no or mild abdominal pain, and feeling generally well or slightly under par.
For PGAs, clinicians selected whether the patient had normal, mild, moderate, or severe disease activity. The values were included in the analysis if the clinicians completed the assessment within 14 days of the patient’s survey.
Among the 2,004 patients, 806 had ulcerative colitis and 1,198 had Crohn’s disease. Patients with ulcerative colitis as well as those with Crohn’s disease were aged 44 years on average. Most of the patients were women: 58% with ulcerative colitis and 56% with Crohn’s disease.
Among the 1,316 visits for ulcerative colitis, 668 patients (51%) self-reported to be in remission, compared with 55% in remission based on PROs. Of the people in PRO–defined remission, 77% reported being in remission, and 23% reported active disease. Of the people with PRO–defined active disease, 81% reported active disease and 19% reported remission. Overall concordance was 79% between patient self-reported and PRO–defined remission.
Discordance in patient-defined remission for ulcerative colitis was primarily influenced by tolerance of an increased stool frequency. About 25% of patients with one or two stools more than normal reported being in remission.
A subset of 397 ulcerative colitis visits had an associated PGA score. Among patients in PGA-defined remission, 53% reported being in remission. Of those with PGA-defined active disease, 60% reported active disease. Overall, concordance was 49% between patient self-reported and PGA-defined remission.
Among the 1,947 visits for Crohn’s disease, 929 patients (48%) self-reported to be in remission, compared with 63% in remission based on PRO. Of the people in PRO-defined remission, 63% reported being in remission, although 37% reported active disease. Of the people with PRO-defined active disease, 79% reported active disease and 21% reported remission. Overall concordance was 69% between patient self-reported and patient-reported outcomes–defined remission.
Discordance in patient-defined remission for Crohn’s disease was primarily influenced by patients with a tolerance of mild to moderate symptoms.
A subset of 575 Crohn’s disease visits had an associated PGA score. Among patients in PGA-defined remission, 52% reported being in remission. Of those with PGA-defined active disease, 57% reported active disease. Overall concordance was 54% between patient self-reported and PGA-defined remission.
Several factors were associated with discordance in remission definitions. Among patients in PRO-defined remission, those who had a diagnosis of IBD for fewer than 5 years were more likely to report having active disease compared with those who had received a diagnosis more than 15 years before.
Patients with high health confidence in managing their condition were less likely to report having active disease. In addition, patients with Crohn’s disease were more likely to report having active disease if they were using prednisone or opioids or if they had an IBD-related emergency department visit in the past 6 months.
“Studies that address the discordance between patient-reported outcomes and clinician assessment in inflammatory bowel disease are important to develop a patient-centered model of practice,” said Sadeea Abbasi, MD, PhD, a gastroenterologist and IBD specialist at Cedars-Sinai Gastroenterology in Santa Monica, Calif.
Dr. Abbasi, who wasn’t involved with this study, has promoted patient advocacy in IBD management.
“Measurable objective data are not the only parameter to measure disease outcomes or individualize treatment protocols. In fact, outcomes can dramatically change if the patient’s experience is not taken into account. Studies that address this reality are crucial for physicians to be able to advocate for their patients,” she said. “The empowered physician-patient relationship is one of strength and trust and tends to be associated with the best overall outcomes.”
IBD Qorus is an initiative of the Crohn’s and Colitis Foundation and is supported by numerous pharmaceutical companies. Supporters had no involvement in the study and didn’t provide direct funding for any aspect of the study. The authors have received funding from the Crohn’s and Colitis Foundation, National Institutes of Health, and various foundations and pharmaceutical companies. Dr. Abbasi reported no relevant disclosures.
Patients’ reports of remission from inflammatory bowel disease (IBD) don’t always line up with remission as defined by patient-reported outcomes (PROs) or physician global assessment (PGA), according to a study published in Inflammatory Bowel Diseases.
Patients have various definitions of remission, which may focus on symptom improvement and the impact on daily activities, while physicians tend to focus on test results. “Examining patient-reported remission may be a valuable approach to better understand remission from the perspective of patients and can assist in aligning shared decision-making between patients and health care providers,” wrote Kendra Kamp, PhD, assistant professor of biobehavioral nursing and health informatics at the University of Washington, and colleagues, on behalf of the IBD Qorus.
In a retrospective study, Dr. Kamp and colleagues analyzed 3,257 deidentified surveys from 2,004 patients who participated in the Crohn’s and Colitis Foundation’s IBD Qorus Learning Health System between September 2019 and February 2021. Adults with IBD who participated in the IBD Qorus received an email before their gastroenterology clinical appointment with a link to a survey that asked questions about primary concerns or goals, symptoms, well-being, recent health care utilization, and medication use.
The researchers looked at the clinical and demographic factors associated with discordance among patient-defined remission, PROs, and PGAs. Patient-defined remission was captured as a yes/no response to the question: “Do you feel your disease is currently in remission (by remission we mean a complete absence of IBD-related symptoms)?”
PROs for ulcerative colitis were measured through stool frequency and rectal bleeding, with remission defined as no blood in the stool and a normal (or fewer than normal) number of stools. For Crohn’s disease, PROs were measured through the average number of liquid stools, abdominal pain, and general well-being, with remission defined as two or fewer loose stools, no or mild abdominal pain, and feeling generally well or slightly under par.
For PGAs, clinicians selected whether the patient had normal, mild, moderate, or severe disease activity. The values were included in the analysis if the clinicians completed the assessment within 14 days of the patient’s survey.
Among the 2,004 patients, 806 had ulcerative colitis and 1,198 had Crohn’s disease. Patients with ulcerative colitis as well as those with Crohn’s disease were aged 44 years on average. Most of the patients were women: 58% with ulcerative colitis and 56% with Crohn’s disease.
Among the 1,316 visits for ulcerative colitis, 668 patients (51%) self-reported to be in remission, compared with 55% in remission based on PROs. Of the people in PRO–defined remission, 77% reported being in remission, and 23% reported active disease. Of the people with PRO–defined active disease, 81% reported active disease and 19% reported remission. Overall concordance was 79% between patient self-reported and PRO–defined remission.
Discordance in patient-defined remission for ulcerative colitis was primarily influenced by tolerance of an increased stool frequency. About 25% of patients with one or two stools more than normal reported being in remission.
A subset of 397 ulcerative colitis visits had an associated PGA score. Among patients in PGA-defined remission, 53% reported being in remission. Of those with PGA-defined active disease, 60% reported active disease. Overall, concordance was 49% between patient self-reported and PGA-defined remission.
Among the 1,947 visits for Crohn’s disease, 929 patients (48%) self-reported to be in remission, compared with 63% in remission based on PRO. Of the people in PRO-defined remission, 63% reported being in remission, although 37% reported active disease. Of the people with PRO-defined active disease, 79% reported active disease and 21% reported remission. Overall concordance was 69% between patient self-reported and patient-reported outcomes–defined remission.
Discordance in patient-defined remission for Crohn’s disease was primarily influenced by patients with a tolerance of mild to moderate symptoms.
A subset of 575 Crohn’s disease visits had an associated PGA score. Among patients in PGA-defined remission, 52% reported being in remission. Of those with PGA-defined active disease, 57% reported active disease. Overall concordance was 54% between patient self-reported and PGA-defined remission.
Several factors were associated with discordance in remission definitions. Among patients in PRO-defined remission, those who had a diagnosis of IBD for fewer than 5 years were more likely to report having active disease compared with those who had received a diagnosis more than 15 years before.
Patients with high health confidence in managing their condition were less likely to report having active disease. In addition, patients with Crohn’s disease were more likely to report having active disease if they were using prednisone or opioids or if they had an IBD-related emergency department visit in the past 6 months.
“Studies that address the discordance between patient-reported outcomes and clinician assessment in inflammatory bowel disease are important to develop a patient-centered model of practice,” said Sadeea Abbasi, MD, PhD, a gastroenterologist and IBD specialist at Cedars-Sinai Gastroenterology in Santa Monica, Calif.
Dr. Abbasi, who wasn’t involved with this study, has promoted patient advocacy in IBD management.
“Measurable objective data are not the only parameter to measure disease outcomes or individualize treatment protocols. In fact, outcomes can dramatically change if the patient’s experience is not taken into account. Studies that address this reality are crucial for physicians to be able to advocate for their patients,” she said. “The empowered physician-patient relationship is one of strength and trust and tends to be associated with the best overall outcomes.”
IBD Qorus is an initiative of the Crohn’s and Colitis Foundation and is supported by numerous pharmaceutical companies. Supporters had no involvement in the study and didn’t provide direct funding for any aspect of the study. The authors have received funding from the Crohn’s and Colitis Foundation, National Institutes of Health, and various foundations and pharmaceutical companies. Dr. Abbasi reported no relevant disclosures.
FROM INFLAMMATORY BOWEL DISEASES
UC reaches remission with FMT plus anti-inflammatory diet: Study
The combination of fecal microbiota transplantation (FMT) and an anti-inflammatory diet (AID) successfully induced and sustained remission of ulcerative colitis (UC) more effectively than optimizing medications for the condition did, according to a randomized controlled trial published in the journal Gut.
”Deep remission at 48 weeks was also significantly better in the FMT-AID arm, suggesting that the anti-inflammatory diet could sustain the FMT-AID–induced endoscopic and clinical remission,” wrote Saurabh Kedia, MD, of the All India Institute of Medical Sciences in New Delhi, and colleagues. “The adherence to modified diet was maintained until 48 weeks, suggesting the acceptability of this approach to patients.”
The open-label trial involved 66 patients with mild to moderate UC, based on a Simple Clinical Colitis Activity Index (SCCAI) score in the range of 3-9 and a score above 1 on the Ulcerative Colitis Endoscopic Index of Severity (UCEIS). Their average age was 35, and 34.8% of the participants had pancolitis. Their median SCCAI score was 6 (interquartile range, 5-7), and their median UCEIS score was 4 (IQR, 3-5) at enrollment.
The control group of 31 patients received standard medical therapy, which meant continuing on their baseline medications along with optimization of their therapy. The optimization involved increasing 5-aminosalicylic acid and/or adding topical therapy (topical 5-ASA or topical steroids in those already on topical 5-ASA); steroid dose was increased in patients already on topical steroids and 5-ASA.
The 35 patients randomized to the FMT-AID arm received seven weekly colonoscopic infusions of FMT from multiple donors, drawn from healthy rural adults aged 18-45, and were instructed to follow an anti-inflammatory diet. The anti-inflammatory diet was “rich in dietary constituents that expand T-regulatory cells, promote healthy microbiota, and improve the intestinal barrier, and poor in dietary constituents that cause dysbiosis or have negative effect on intestinal barrier,” the authors wrote. Foods to avoid included gluten-based grains, dairy products, processed and red meat, food additives, and refined sugars. Participants were encouraged to increase their intake of fresh fruit and vegetables, fermented foods, cruciferous vegetables, and polyphenols. The patients received a diet chart to follow, and a dietitian called every 2 weeks during the first 2 months to assess diet compliance.
The patients’ outcomes were assessed at 8 weeks with blood and stool samples and endoscopy, scored by an assignment-blinded physician. The primary outcome consisted of both clinical remission (SCCAI score of 2 or less) and endoscopic remission (UCEIS score of 1 or less), which the investigators considered deep remission. They also looked at those who clinically responded – a decline in SCCAI of at least 3 points – even if they didn’t reach remission. The researchers defined treatment failure as either an increase in SCCAI of at least 3 points with a rectal bleeding score of at least 1, or a need for oral steroids without improvement of at least 3 points in their SCCAI score.
At 8 weeks, patients in the FMT-AID arm were more than three times more likely to achieve remission or clinically respond than those receiving standard medical therapy. Two-thirds of those in the FMT-AID arm (65.7%) clinically responded, compared with 35.5% of those receiving standard therapy (odds ratio, 3.5; 95% confidence interval, 1.3-9.6). Clinical remission occurred in 60% of those in the FMT-AID arm, compared with 32.3% of the standard therapy arm (OR, 3.2; 95% CI, 1.1-8.7). Just over half the FMT-AID arm participants (51.5%) showed endoscopic response, compared with 17.4% of those with standard therapy (OR, 5.0; 95% CI, 1.4-18.1). Endoscopic remission was also greater in the FMT-AID group (36.4%) than the standard therapy group (17.4%) but without statistical significance (P = .15). Finally, about a third of the FMT-AID arm experienced deep remission (36.4%), compared with 8.7% of the standard therapy arm (OR, 6.0; 95% CI, 1.2-30.2). Those in the FMT-AID arm with milder disease or left-sided colitis were significantly more likely to reach clinical remission, and all the patients who hadn’t taken steroids had remission.
Those with clinical response or remission at 8 weeks – 23 people in the FMT-AID arm and 11 in the standard therapy arm – were then followed for the next 40 weeks. During that period, participants in the FMT-AID arm continued their anti-inflammatory diet and medications while the standard medical care group took only their medications.
At 48 weeks, half the original cohort of FMT-AID patients had maintained clinical remission or response, compared with a third of the standard care group, but the difference between the groups didn’t reach significance. However, a quarter of FMT-AID participants (25%) had maintained endoscopic remission, compared with none in the standard therapy arm (P = .007), and the same was true for deep remission (25% vs. 0%; P = .007).
Adverse events were similar in the FMT-AID (74%) and standard care (87%) arms and mild or moderate, mainly abdominal pain, bloating, gas, diarrhea, and worsened disease activity.
A substantial challenge in the trial came from interruptions because of the COVID-19 pandemic. Among the 66 trial participants, 52 were recruited between September 2019 and March 2020, when the pandemic prevented further recruitment. The remaining 14 participants were recruited between August and November 2021.
“The major strength of our study was a unique protocol combining two microbiome manipulation strategies: FMT and diet,” the authors wrote. “While both were used for induction of remission, the effect was maintained only with diet, which adds novelty to the study design.”
Vineet Ahuja, MD, DM, the paper’s senior author and a professor of gastroenterology at the All India Institute of Medical Sciences, said there likely wasn’t any major impact from the pandemic on participants’ ability to follow the diet given that none mentioned it during the dietitian calls.
”There are less possible chances of recall bias since we had a dedicated IBD dietician who would contact patients regularly for recalling the diet,” Dr. Ahuja said in an interview. “We also have created a diet app, IBD Nutricare, in which real-time recording of daily diet can be done by the patient and the input is analyzable at the web end.”
Most in the FMT-AID arm (84.6%) were qualitatively highly adherent to the diet at 8 weeks, with the other 15.4% moderately adherent. The highly adherent rate fell to 66.7% at 48 weeks, with the other third remaining moderately adherent. No patients were poorly or nonadherent during the study. At 8 weeks, 92.3% of patients were avoiding prohibited foods, which fell to 71.4% at 48 weeks.
Ashwin Ananthakrishnan, MBBS, MPH, an associate professor of medicine at Massachusetts General Hospital and director of the MGH Crohn’s and Colitis center in Boston, found the study design “intriguing and practical.”
”Prior studies of FMT in UC examined UC alone – they required fairly high intensity of FMT treatment for the entire duration of the trial – consequently they may not be sustainable in real world practice,” Dr. Ananthakrishnan said in an interview. “This is a more practically applicable study where the dietary intervention could be continued for a longer period of time. So in all, it’s a very promising study and provides a lot of guidance into how to practically position these treatments.”
The authors similarly noted that the two-intervention approach is ”practical for patients as they can practice the modified diet at home and avoid hospital visits for repeat FMTs.” The authors also noted that their study “provides a low-cost, safe alternative for IBD physicians in resource-limited settings.”
That said, Dr. Ananthakrishnan drew attention to the small size of the study as a limitation.
”To what degree the sustained benefit was due to AID vs. FMT cannot be established,” Dr. Ananthakrishnan said. “The optimized standard medical therapy arm had patients with mild disease who had only minor adjustments to their baseline treatment. Whether they would have had similar benefit if they had been treated with a short course of systemic steroids and continued their optimized treatment is unclear.”
The research was funded by a grant from the Indian Council of Medical Research. The authors and Dr. Ananthakrishnan reported no conflicts of interest.
The combination of fecal microbiota transplantation (FMT) and an anti-inflammatory diet (AID) successfully induced and sustained remission of ulcerative colitis (UC) more effectively than optimizing medications for the condition did, according to a randomized controlled trial published in the journal Gut.
”Deep remission at 48 weeks was also significantly better in the FMT-AID arm, suggesting that the anti-inflammatory diet could sustain the FMT-AID–induced endoscopic and clinical remission,” wrote Saurabh Kedia, MD, of the All India Institute of Medical Sciences in New Delhi, and colleagues. “The adherence to modified diet was maintained until 48 weeks, suggesting the acceptability of this approach to patients.”
The open-label trial involved 66 patients with mild to moderate UC, based on a Simple Clinical Colitis Activity Index (SCCAI) score in the range of 3-9 and a score above 1 on the Ulcerative Colitis Endoscopic Index of Severity (UCEIS). Their average age was 35, and 34.8% of the participants had pancolitis. Their median SCCAI score was 6 (interquartile range, 5-7), and their median UCEIS score was 4 (IQR, 3-5) at enrollment.
The control group of 31 patients received standard medical therapy, which meant continuing on their baseline medications along with optimization of their therapy. The optimization involved increasing 5-aminosalicylic acid and/or adding topical therapy (topical 5-ASA or topical steroids in those already on topical 5-ASA); steroid dose was increased in patients already on topical steroids and 5-ASA.
The 35 patients randomized to the FMT-AID arm received seven weekly colonoscopic infusions of FMT from multiple donors, drawn from healthy rural adults aged 18-45, and were instructed to follow an anti-inflammatory diet. The anti-inflammatory diet was “rich in dietary constituents that expand T-regulatory cells, promote healthy microbiota, and improve the intestinal barrier, and poor in dietary constituents that cause dysbiosis or have negative effect on intestinal barrier,” the authors wrote. Foods to avoid included gluten-based grains, dairy products, processed and red meat, food additives, and refined sugars. Participants were encouraged to increase their intake of fresh fruit and vegetables, fermented foods, cruciferous vegetables, and polyphenols. The patients received a diet chart to follow, and a dietitian called every 2 weeks during the first 2 months to assess diet compliance.
The patients’ outcomes were assessed at 8 weeks with blood and stool samples and endoscopy, scored by an assignment-blinded physician. The primary outcome consisted of both clinical remission (SCCAI score of 2 or less) and endoscopic remission (UCEIS score of 1 or less), which the investigators considered deep remission. They also looked at those who clinically responded – a decline in SCCAI of at least 3 points – even if they didn’t reach remission. The researchers defined treatment failure as either an increase in SCCAI of at least 3 points with a rectal bleeding score of at least 1, or a need for oral steroids without improvement of at least 3 points in their SCCAI score.
At 8 weeks, patients in the FMT-AID arm were more than three times more likely to achieve remission or clinically respond than those receiving standard medical therapy. Two-thirds of those in the FMT-AID arm (65.7%) clinically responded, compared with 35.5% of those receiving standard therapy (odds ratio, 3.5; 95% confidence interval, 1.3-9.6). Clinical remission occurred in 60% of those in the FMT-AID arm, compared with 32.3% of the standard therapy arm (OR, 3.2; 95% CI, 1.1-8.7). Just over half the FMT-AID arm participants (51.5%) showed endoscopic response, compared with 17.4% of those with standard therapy (OR, 5.0; 95% CI, 1.4-18.1). Endoscopic remission was also greater in the FMT-AID group (36.4%) than the standard therapy group (17.4%) but without statistical significance (P = .15). Finally, about a third of the FMT-AID arm experienced deep remission (36.4%), compared with 8.7% of the standard therapy arm (OR, 6.0; 95% CI, 1.2-30.2). Those in the FMT-AID arm with milder disease or left-sided colitis were significantly more likely to reach clinical remission, and all the patients who hadn’t taken steroids had remission.
Those with clinical response or remission at 8 weeks – 23 people in the FMT-AID arm and 11 in the standard therapy arm – were then followed for the next 40 weeks. During that period, participants in the FMT-AID arm continued their anti-inflammatory diet and medications while the standard medical care group took only their medications.
At 48 weeks, half the original cohort of FMT-AID patients had maintained clinical remission or response, compared with a third of the standard care group, but the difference between the groups didn’t reach significance. However, a quarter of FMT-AID participants (25%) had maintained endoscopic remission, compared with none in the standard therapy arm (P = .007), and the same was true for deep remission (25% vs. 0%; P = .007).
Adverse events were similar in the FMT-AID (74%) and standard care (87%) arms and mild or moderate, mainly abdominal pain, bloating, gas, diarrhea, and worsened disease activity.
A substantial challenge in the trial came from interruptions because of the COVID-19 pandemic. Among the 66 trial participants, 52 were recruited between September 2019 and March 2020, when the pandemic prevented further recruitment. The remaining 14 participants were recruited between August and November 2021.
“The major strength of our study was a unique protocol combining two microbiome manipulation strategies: FMT and diet,” the authors wrote. “While both were used for induction of remission, the effect was maintained only with diet, which adds novelty to the study design.”
Vineet Ahuja, MD, DM, the paper’s senior author and a professor of gastroenterology at the All India Institute of Medical Sciences, said there likely wasn’t any major impact from the pandemic on participants’ ability to follow the diet given that none mentioned it during the dietitian calls.
”There are less possible chances of recall bias since we had a dedicated IBD dietician who would contact patients regularly for recalling the diet,” Dr. Ahuja said in an interview. “We also have created a diet app, IBD Nutricare, in which real-time recording of daily diet can be done by the patient and the input is analyzable at the web end.”
Most in the FMT-AID arm (84.6%) were qualitatively highly adherent to the diet at 8 weeks, with the other 15.4% moderately adherent. The highly adherent rate fell to 66.7% at 48 weeks, with the other third remaining moderately adherent. No patients were poorly or nonadherent during the study. At 8 weeks, 92.3% of patients were avoiding prohibited foods, which fell to 71.4% at 48 weeks.
Ashwin Ananthakrishnan, MBBS, MPH, an associate professor of medicine at Massachusetts General Hospital and director of the MGH Crohn’s and Colitis center in Boston, found the study design “intriguing and practical.”
”Prior studies of FMT in UC examined UC alone – they required fairly high intensity of FMT treatment for the entire duration of the trial – consequently they may not be sustainable in real world practice,” Dr. Ananthakrishnan said in an interview. “This is a more practically applicable study where the dietary intervention could be continued for a longer period of time. So in all, it’s a very promising study and provides a lot of guidance into how to practically position these treatments.”
The authors similarly noted that the two-intervention approach is ”practical for patients as they can practice the modified diet at home and avoid hospital visits for repeat FMTs.” The authors also noted that their study “provides a low-cost, safe alternative for IBD physicians in resource-limited settings.”
That said, Dr. Ananthakrishnan drew attention to the small size of the study as a limitation.
”To what degree the sustained benefit was due to AID vs. FMT cannot be established,” Dr. Ananthakrishnan said. “The optimized standard medical therapy arm had patients with mild disease who had only minor adjustments to their baseline treatment. Whether they would have had similar benefit if they had been treated with a short course of systemic steroids and continued their optimized treatment is unclear.”
The research was funded by a grant from the Indian Council of Medical Research. The authors and Dr. Ananthakrishnan reported no conflicts of interest.
The combination of fecal microbiota transplantation (FMT) and an anti-inflammatory diet (AID) successfully induced and sustained remission of ulcerative colitis (UC) more effectively than optimizing medications for the condition did, according to a randomized controlled trial published in the journal Gut.
”Deep remission at 48 weeks was also significantly better in the FMT-AID arm, suggesting that the anti-inflammatory diet could sustain the FMT-AID–induced endoscopic and clinical remission,” wrote Saurabh Kedia, MD, of the All India Institute of Medical Sciences in New Delhi, and colleagues. “The adherence to modified diet was maintained until 48 weeks, suggesting the acceptability of this approach to patients.”
The open-label trial involved 66 patients with mild to moderate UC, based on a Simple Clinical Colitis Activity Index (SCCAI) score in the range of 3-9 and a score above 1 on the Ulcerative Colitis Endoscopic Index of Severity (UCEIS). Their average age was 35, and 34.8% of the participants had pancolitis. Their median SCCAI score was 6 (interquartile range, 5-7), and their median UCEIS score was 4 (IQR, 3-5) at enrollment.
The control group of 31 patients received standard medical therapy, which meant continuing on their baseline medications along with optimization of their therapy. The optimization involved increasing 5-aminosalicylic acid and/or adding topical therapy (topical 5-ASA or topical steroids in those already on topical 5-ASA); steroid dose was increased in patients already on topical steroids and 5-ASA.
The 35 patients randomized to the FMT-AID arm received seven weekly colonoscopic infusions of FMT from multiple donors, drawn from healthy rural adults aged 18-45, and were instructed to follow an anti-inflammatory diet. The anti-inflammatory diet was “rich in dietary constituents that expand T-regulatory cells, promote healthy microbiota, and improve the intestinal barrier, and poor in dietary constituents that cause dysbiosis or have negative effect on intestinal barrier,” the authors wrote. Foods to avoid included gluten-based grains, dairy products, processed and red meat, food additives, and refined sugars. Participants were encouraged to increase their intake of fresh fruit and vegetables, fermented foods, cruciferous vegetables, and polyphenols. The patients received a diet chart to follow, and a dietitian called every 2 weeks during the first 2 months to assess diet compliance.
The patients’ outcomes were assessed at 8 weeks with blood and stool samples and endoscopy, scored by an assignment-blinded physician. The primary outcome consisted of both clinical remission (SCCAI score of 2 or less) and endoscopic remission (UCEIS score of 1 or less), which the investigators considered deep remission. They also looked at those who clinically responded – a decline in SCCAI of at least 3 points – even if they didn’t reach remission. The researchers defined treatment failure as either an increase in SCCAI of at least 3 points with a rectal bleeding score of at least 1, or a need for oral steroids without improvement of at least 3 points in their SCCAI score.
At 8 weeks, patients in the FMT-AID arm were more than three times more likely to achieve remission or clinically respond than those receiving standard medical therapy. Two-thirds of those in the FMT-AID arm (65.7%) clinically responded, compared with 35.5% of those receiving standard therapy (odds ratio, 3.5; 95% confidence interval, 1.3-9.6). Clinical remission occurred in 60% of those in the FMT-AID arm, compared with 32.3% of the standard therapy arm (OR, 3.2; 95% CI, 1.1-8.7). Just over half the FMT-AID arm participants (51.5%) showed endoscopic response, compared with 17.4% of those with standard therapy (OR, 5.0; 95% CI, 1.4-18.1). Endoscopic remission was also greater in the FMT-AID group (36.4%) than the standard therapy group (17.4%) but without statistical significance (P = .15). Finally, about a third of the FMT-AID arm experienced deep remission (36.4%), compared with 8.7% of the standard therapy arm (OR, 6.0; 95% CI, 1.2-30.2). Those in the FMT-AID arm with milder disease or left-sided colitis were significantly more likely to reach clinical remission, and all the patients who hadn’t taken steroids had remission.
Those with clinical response or remission at 8 weeks – 23 people in the FMT-AID arm and 11 in the standard therapy arm – were then followed for the next 40 weeks. During that period, participants in the FMT-AID arm continued their anti-inflammatory diet and medications while the standard medical care group took only their medications.
At 48 weeks, half the original cohort of FMT-AID patients had maintained clinical remission or response, compared with a third of the standard care group, but the difference between the groups didn’t reach significance. However, a quarter of FMT-AID participants (25%) had maintained endoscopic remission, compared with none in the standard therapy arm (P = .007), and the same was true for deep remission (25% vs. 0%; P = .007).
Adverse events were similar in the FMT-AID (74%) and standard care (87%) arms and mild or moderate, mainly abdominal pain, bloating, gas, diarrhea, and worsened disease activity.
A substantial challenge in the trial came from interruptions because of the COVID-19 pandemic. Among the 66 trial participants, 52 were recruited between September 2019 and March 2020, when the pandemic prevented further recruitment. The remaining 14 participants were recruited between August and November 2021.
“The major strength of our study was a unique protocol combining two microbiome manipulation strategies: FMT and diet,” the authors wrote. “While both were used for induction of remission, the effect was maintained only with diet, which adds novelty to the study design.”
Vineet Ahuja, MD, DM, the paper’s senior author and a professor of gastroenterology at the All India Institute of Medical Sciences, said there likely wasn’t any major impact from the pandemic on participants’ ability to follow the diet given that none mentioned it during the dietitian calls.
”There are less possible chances of recall bias since we had a dedicated IBD dietician who would contact patients regularly for recalling the diet,” Dr. Ahuja said in an interview. “We also have created a diet app, IBD Nutricare, in which real-time recording of daily diet can be done by the patient and the input is analyzable at the web end.”
Most in the FMT-AID arm (84.6%) were qualitatively highly adherent to the diet at 8 weeks, with the other 15.4% moderately adherent. The highly adherent rate fell to 66.7% at 48 weeks, with the other third remaining moderately adherent. No patients were poorly or nonadherent during the study. At 8 weeks, 92.3% of patients were avoiding prohibited foods, which fell to 71.4% at 48 weeks.
Ashwin Ananthakrishnan, MBBS, MPH, an associate professor of medicine at Massachusetts General Hospital and director of the MGH Crohn’s and Colitis center in Boston, found the study design “intriguing and practical.”
”Prior studies of FMT in UC examined UC alone – they required fairly high intensity of FMT treatment for the entire duration of the trial – consequently they may not be sustainable in real world practice,” Dr. Ananthakrishnan said in an interview. “This is a more practically applicable study where the dietary intervention could be continued for a longer period of time. So in all, it’s a very promising study and provides a lot of guidance into how to practically position these treatments.”
The authors similarly noted that the two-intervention approach is ”practical for patients as they can practice the modified diet at home and avoid hospital visits for repeat FMTs.” The authors also noted that their study “provides a low-cost, safe alternative for IBD physicians in resource-limited settings.”
That said, Dr. Ananthakrishnan drew attention to the small size of the study as a limitation.
”To what degree the sustained benefit was due to AID vs. FMT cannot be established,” Dr. Ananthakrishnan said. “The optimized standard medical therapy arm had patients with mild disease who had only minor adjustments to their baseline treatment. Whether they would have had similar benefit if they had been treated with a short course of systemic steroids and continued their optimized treatment is unclear.”
The research was funded by a grant from the Indian Council of Medical Research. The authors and Dr. Ananthakrishnan reported no conflicts of interest.
FROM GUT
Early FMT shows promise for preventing recurrent C. difficile
Fecal microbiota transplantation (FMT) is safe and highly effective as first-line therapy for patients with first or second Clostridioides difficile infection, according to the first randomized, double-blind, placebo-controlled trial of its kind.
Study enrollment was halted after an interim analysis revealed significantly better outcomes among patients who received vancomycin plus FMT versus vancomycin alone, reported lead author Simon Mark Dahl Baunwall, MD, of Aarhus (Denmark) University Hospital and colleagues in The Lancet Gastroenterology & Hepatology.
The investigators noted that the participants represented a real-world patient population, so the data support FMT “as a necessary, effective first-line option” in routine management of C. difficile infection.
“Previous studies have demonstrated clinical cure rates [with FMT] of up to 92%,” Dr. Baunwall and colleagues wrote. “Early use of FMT for first or second C. difficile infection has therapeutic potential, but no formal randomized trials to support use of the approach as a first-line therapy have been done.”
The present trial, conducted at a university hospital in Denmark, involved 42 adult patients with first or second C. difficile infection. Patients were randomized in a 1:1 ratio to receive either vancomycin alone or vancomycin plus FMT. All patients received 125 mg oral vancomycin four times daily for a minimum of 10 days after diagnosis. On day 1 after completion of vancomycin therapy and again between day 3 and 7, patients received either oral FMT or matching placebo, depending on their group. After completing the protocol, patients were followed for 8 weeks or C. difficile recurrence to evaluate resolution of C. difficile–associated diarrhea.
“In this trial, patients were treated with two sequential FMT procedures on separate days,” the investigators noted. “This practice might have overtreated some patients and differs from previous trials. It remains unknown whether optimal effect is achieved by one or two treatments.”
The trial design called for 84 patients, but enrollment was halted after an interim analysis of the above cohort of 42 patients because of significantly lower rate resolution in the placebo group. At the 2-month mark, 90% (95% confidence interval, 70%-99%) of patients in the FMT group had resolution, compared with only 33% (95% CI, 15%-57%) of patients in the placebo group (P = .0003), constituting a 57% (95% CI, 33%-81%) absolute risk reduction.
Most patients experienced adverse events, including 20 in the FMT group and all 21 in the placebo group, although most were transient and nonserious. The most common adverse events were diarrhea, which occurred more frequently in the FMT group (23 vs. 14 events), followed by abdominal pain(14 vs. 11 events) and nausea (12 vs. 5 events).
One limitation of the study was its single-center design with regional uptake; the authors noted that, despite having high statistical power for the clinical effect, the study’s premature termination and low patient number prevent inferences regarding mortality, time to effect, and cost.
“The results of this trial highlight how the use of fecal microbiota transplantation as a first-line treatment can effectively prevent C. difficile recurrence and suggests that microbiota restoration might be necessary to obtain sustained resolution,” the investigators wrote. “At present, only 10% of patients with multiple, recurrent C. difficile infection and indication for FMT receive it. International initiatives address the unmet need, but logistic and regulatory obstacles remain unsolved.”
Encouraging findings, lingering concerns
Nicholas Turner, MD, assistant professor in the division of infectious diseases at Duke University, Durham, N.C., praised the study for “pushing the boundaries for FMT,” and noted that the methodology appeared sound. Results in the placebo group, however, cast doubt on the generalizability of the findings, he said.
“If you look at the group that received vancomycin plus placebo, their failure rate was really astoundingly high,” Dr. Turner said in an interview, referring to the 67% failure rate in the control group; he noted previous studies had reported failure rates closer to 10%. “I think that just calls into question just a little bit what happened with that control group.”
Dr. Turner said his confidence would go “way, way up” if the findings were reproduced in a larger study. Ideally, these future trials would use fidaxomicin, he added, which is becoming the preferred option over vancomycin for treating C. difficile.
John Y. Kao, MD, professor of medicine and codirector of the FMT program at University of Michigan Medicine, Ann Arbor, offered a different perspective, suggesting that the control group findings shouldn’t overshadow the efficacy of FMT.
“I agree that historical data would tell us that the placebo population should see a much higher response,” Dr. Kao said in an interview. “In my mind though, the success rate of FMT over placebo is what I would expect. The message of the study should be upheld: that FMT is an effective therapy whether it’s given early or, as the way we give it now, as a sort of rescue therapy.”
Despite this confidence in FMT as an efficacious first-line option, Dr. Kao said it is unlikely to be routinely used in this way anytime soon, even if a larger trial echoes the present results.
“We don’t know the long-term risks of FMT therapy, although we’ve been doing this now probably close to 20 years,” Dr. Kao said.
Specifically, Dr. Kao was most concerned about the long-term risk of colon cancer, as mouse models suggest that microbiome characteristics may affect risk level, and risk may vary based on host-microbiome relationships. In other words, an organism may pose no risk in the gut of the donor, but the same may not be true for the recipient.
While increased rates of colon cancer or other serious illnesses have not been detected in humans who have undergone FMT over the past 2 decades, Dr. Kao said that these findings cannot be extrapolated over a patient’s entire lifetime, especially for younger individuals.
“In a patient that’s 80, you would say, yeah, let’s go ahead and treat you [with FMT] as first-line therapy, whereas someone who’s 20, and has maybe another 50 or 60 years longevity, you may not want to give FMT as first-line therapy,” Dr. Kao said.
This study was supported by Innovation Fund Denmark. The investigators disclosed no competing interests. Dr. Turner previously performed statistical analyses for a Merck study comparing vancomycin, fidaxomicin, and metronidazole for C. difficile infection. Dr. Kao disclosed no relevant conflicts of interest.
Help your patients understand their C. difficile diagnosis by sharing patient education from the AGA GI Patient Center (www.gastro.org/Cdiff).
Fecal microbiota transplantation (FMT) is safe and highly effective as first-line therapy for patients with first or second Clostridioides difficile infection, according to the first randomized, double-blind, placebo-controlled trial of its kind.
Study enrollment was halted after an interim analysis revealed significantly better outcomes among patients who received vancomycin plus FMT versus vancomycin alone, reported lead author Simon Mark Dahl Baunwall, MD, of Aarhus (Denmark) University Hospital and colleagues in The Lancet Gastroenterology & Hepatology.
The investigators noted that the participants represented a real-world patient population, so the data support FMT “as a necessary, effective first-line option” in routine management of C. difficile infection.
“Previous studies have demonstrated clinical cure rates [with FMT] of up to 92%,” Dr. Baunwall and colleagues wrote. “Early use of FMT for first or second C. difficile infection has therapeutic potential, but no formal randomized trials to support use of the approach as a first-line therapy have been done.”
The present trial, conducted at a university hospital in Denmark, involved 42 adult patients with first or second C. difficile infection. Patients were randomized in a 1:1 ratio to receive either vancomycin alone or vancomycin plus FMT. All patients received 125 mg oral vancomycin four times daily for a minimum of 10 days after diagnosis. On day 1 after completion of vancomycin therapy and again between day 3 and 7, patients received either oral FMT or matching placebo, depending on their group. After completing the protocol, patients were followed for 8 weeks or C. difficile recurrence to evaluate resolution of C. difficile–associated diarrhea.
“In this trial, patients were treated with two sequential FMT procedures on separate days,” the investigators noted. “This practice might have overtreated some patients and differs from previous trials. It remains unknown whether optimal effect is achieved by one or two treatments.”
The trial design called for 84 patients, but enrollment was halted after an interim analysis of the above cohort of 42 patients because of significantly lower rate resolution in the placebo group. At the 2-month mark, 90% (95% confidence interval, 70%-99%) of patients in the FMT group had resolution, compared with only 33% (95% CI, 15%-57%) of patients in the placebo group (P = .0003), constituting a 57% (95% CI, 33%-81%) absolute risk reduction.
Most patients experienced adverse events, including 20 in the FMT group and all 21 in the placebo group, although most were transient and nonserious. The most common adverse events were diarrhea, which occurred more frequently in the FMT group (23 vs. 14 events), followed by abdominal pain(14 vs. 11 events) and nausea (12 vs. 5 events).
One limitation of the study was its single-center design with regional uptake; the authors noted that, despite having high statistical power for the clinical effect, the study’s premature termination and low patient number prevent inferences regarding mortality, time to effect, and cost.
“The results of this trial highlight how the use of fecal microbiota transplantation as a first-line treatment can effectively prevent C. difficile recurrence and suggests that microbiota restoration might be necessary to obtain sustained resolution,” the investigators wrote. “At present, only 10% of patients with multiple, recurrent C. difficile infection and indication for FMT receive it. International initiatives address the unmet need, but logistic and regulatory obstacles remain unsolved.”
Encouraging findings, lingering concerns
Nicholas Turner, MD, assistant professor in the division of infectious diseases at Duke University, Durham, N.C., praised the study for “pushing the boundaries for FMT,” and noted that the methodology appeared sound. Results in the placebo group, however, cast doubt on the generalizability of the findings, he said.
“If you look at the group that received vancomycin plus placebo, their failure rate was really astoundingly high,” Dr. Turner said in an interview, referring to the 67% failure rate in the control group; he noted previous studies had reported failure rates closer to 10%. “I think that just calls into question just a little bit what happened with that control group.”
Dr. Turner said his confidence would go “way, way up” if the findings were reproduced in a larger study. Ideally, these future trials would use fidaxomicin, he added, which is becoming the preferred option over vancomycin for treating C. difficile.
John Y. Kao, MD, professor of medicine and codirector of the FMT program at University of Michigan Medicine, Ann Arbor, offered a different perspective, suggesting that the control group findings shouldn’t overshadow the efficacy of FMT.
“I agree that historical data would tell us that the placebo population should see a much higher response,” Dr. Kao said in an interview. “In my mind though, the success rate of FMT over placebo is what I would expect. The message of the study should be upheld: that FMT is an effective therapy whether it’s given early or, as the way we give it now, as a sort of rescue therapy.”
Despite this confidence in FMT as an efficacious first-line option, Dr. Kao said it is unlikely to be routinely used in this way anytime soon, even if a larger trial echoes the present results.
“We don’t know the long-term risks of FMT therapy, although we’ve been doing this now probably close to 20 years,” Dr. Kao said.
Specifically, Dr. Kao was most concerned about the long-term risk of colon cancer, as mouse models suggest that microbiome characteristics may affect risk level, and risk may vary based on host-microbiome relationships. In other words, an organism may pose no risk in the gut of the donor, but the same may not be true for the recipient.
While increased rates of colon cancer or other serious illnesses have not been detected in humans who have undergone FMT over the past 2 decades, Dr. Kao said that these findings cannot be extrapolated over a patient’s entire lifetime, especially for younger individuals.
“In a patient that’s 80, you would say, yeah, let’s go ahead and treat you [with FMT] as first-line therapy, whereas someone who’s 20, and has maybe another 50 or 60 years longevity, you may not want to give FMT as first-line therapy,” Dr. Kao said.
This study was supported by Innovation Fund Denmark. The investigators disclosed no competing interests. Dr. Turner previously performed statistical analyses for a Merck study comparing vancomycin, fidaxomicin, and metronidazole for C. difficile infection. Dr. Kao disclosed no relevant conflicts of interest.
Help your patients understand their C. difficile diagnosis by sharing patient education from the AGA GI Patient Center (www.gastro.org/Cdiff).
Fecal microbiota transplantation (FMT) is safe and highly effective as first-line therapy for patients with first or second Clostridioides difficile infection, according to the first randomized, double-blind, placebo-controlled trial of its kind.
Study enrollment was halted after an interim analysis revealed significantly better outcomes among patients who received vancomycin plus FMT versus vancomycin alone, reported lead author Simon Mark Dahl Baunwall, MD, of Aarhus (Denmark) University Hospital and colleagues in The Lancet Gastroenterology & Hepatology.
The investigators noted that the participants represented a real-world patient population, so the data support FMT “as a necessary, effective first-line option” in routine management of C. difficile infection.
“Previous studies have demonstrated clinical cure rates [with FMT] of up to 92%,” Dr. Baunwall and colleagues wrote. “Early use of FMT for first or second C. difficile infection has therapeutic potential, but no formal randomized trials to support use of the approach as a first-line therapy have been done.”
The present trial, conducted at a university hospital in Denmark, involved 42 adult patients with first or second C. difficile infection. Patients were randomized in a 1:1 ratio to receive either vancomycin alone or vancomycin plus FMT. All patients received 125 mg oral vancomycin four times daily for a minimum of 10 days after diagnosis. On day 1 after completion of vancomycin therapy and again between day 3 and 7, patients received either oral FMT or matching placebo, depending on their group. After completing the protocol, patients were followed for 8 weeks or C. difficile recurrence to evaluate resolution of C. difficile–associated diarrhea.
“In this trial, patients were treated with two sequential FMT procedures on separate days,” the investigators noted. “This practice might have overtreated some patients and differs from previous trials. It remains unknown whether optimal effect is achieved by one or two treatments.”
The trial design called for 84 patients, but enrollment was halted after an interim analysis of the above cohort of 42 patients because of significantly lower rate resolution in the placebo group. At the 2-month mark, 90% (95% confidence interval, 70%-99%) of patients in the FMT group had resolution, compared with only 33% (95% CI, 15%-57%) of patients in the placebo group (P = .0003), constituting a 57% (95% CI, 33%-81%) absolute risk reduction.
Most patients experienced adverse events, including 20 in the FMT group and all 21 in the placebo group, although most were transient and nonserious. The most common adverse events were diarrhea, which occurred more frequently in the FMT group (23 vs. 14 events), followed by abdominal pain(14 vs. 11 events) and nausea (12 vs. 5 events).
One limitation of the study was its single-center design with regional uptake; the authors noted that, despite having high statistical power for the clinical effect, the study’s premature termination and low patient number prevent inferences regarding mortality, time to effect, and cost.
“The results of this trial highlight how the use of fecal microbiota transplantation as a first-line treatment can effectively prevent C. difficile recurrence and suggests that microbiota restoration might be necessary to obtain sustained resolution,” the investigators wrote. “At present, only 10% of patients with multiple, recurrent C. difficile infection and indication for FMT receive it. International initiatives address the unmet need, but logistic and regulatory obstacles remain unsolved.”
Encouraging findings, lingering concerns
Nicholas Turner, MD, assistant professor in the division of infectious diseases at Duke University, Durham, N.C., praised the study for “pushing the boundaries for FMT,” and noted that the methodology appeared sound. Results in the placebo group, however, cast doubt on the generalizability of the findings, he said.
“If you look at the group that received vancomycin plus placebo, their failure rate was really astoundingly high,” Dr. Turner said in an interview, referring to the 67% failure rate in the control group; he noted previous studies had reported failure rates closer to 10%. “I think that just calls into question just a little bit what happened with that control group.”
Dr. Turner said his confidence would go “way, way up” if the findings were reproduced in a larger study. Ideally, these future trials would use fidaxomicin, he added, which is becoming the preferred option over vancomycin for treating C. difficile.
John Y. Kao, MD, professor of medicine and codirector of the FMT program at University of Michigan Medicine, Ann Arbor, offered a different perspective, suggesting that the control group findings shouldn’t overshadow the efficacy of FMT.
“I agree that historical data would tell us that the placebo population should see a much higher response,” Dr. Kao said in an interview. “In my mind though, the success rate of FMT over placebo is what I would expect. The message of the study should be upheld: that FMT is an effective therapy whether it’s given early or, as the way we give it now, as a sort of rescue therapy.”
Despite this confidence in FMT as an efficacious first-line option, Dr. Kao said it is unlikely to be routinely used in this way anytime soon, even if a larger trial echoes the present results.
“We don’t know the long-term risks of FMT therapy, although we’ve been doing this now probably close to 20 years,” Dr. Kao said.
Specifically, Dr. Kao was most concerned about the long-term risk of colon cancer, as mouse models suggest that microbiome characteristics may affect risk level, and risk may vary based on host-microbiome relationships. In other words, an organism may pose no risk in the gut of the donor, but the same may not be true for the recipient.
While increased rates of colon cancer or other serious illnesses have not been detected in humans who have undergone FMT over the past 2 decades, Dr. Kao said that these findings cannot be extrapolated over a patient’s entire lifetime, especially for younger individuals.
“In a patient that’s 80, you would say, yeah, let’s go ahead and treat you [with FMT] as first-line therapy, whereas someone who’s 20, and has maybe another 50 or 60 years longevity, you may not want to give FMT as first-line therapy,” Dr. Kao said.
This study was supported by Innovation Fund Denmark. The investigators disclosed no competing interests. Dr. Turner previously performed statistical analyses for a Merck study comparing vancomycin, fidaxomicin, and metronidazole for C. difficile infection. Dr. Kao disclosed no relevant conflicts of interest.
Help your patients understand their C. difficile diagnosis by sharing patient education from the AGA GI Patient Center (www.gastro.org/Cdiff).
FROM THE LANCET GASTROENTEROLOGY & HEPATOLOGY
Air pollution linked to increased IBS incidence
Increased levels of air pollution were linked to a slight uptick in new diagnoses of irritable bowel syndrome (IBS) in California residents, according to an ecologic study published in Clinical Gastroenterology and Hepatology.
“These data provide support for the role of environmental pollutants, especially air pollutants, in the development of IBS,” Philip N. Okafor, MD, MPH, of Stanford (Calif.) University, and colleagues wrote. “In contrast, we found no significant relationships between the seven environmental exposures and the ZIP-code level incidence of functional dyspepsia, ulcerative colitis, Crohn’s disease, and eosinophilic esophagitis.”
John I. Allen MD, MBA, a retired clinical professor medicine at the University of Michigan, Ann Arbor, said the findings were somewhat surprising, but he was impressed with the “fascinating and well-constructed” study.
“The differentiation between GI disorders that are linked to environmental pollutants [such as IBS] and those that are not [such as inflammatory bowel disease and eosinophilic esophagitis] is quite interesting and lends further credibility to the conclusions,” Dr. Allen said in an interview. “While definitive causal conclusions cannot rest on retrospective, population-level, studies alone, this extraordinarily detailed analysis should prompt further studies investigating root causes for these correlations,” such as gut epithelial changes secondary to ingested pollutants, for example.
The researchers noted that an “epidemiological shift in gastrointestinal diseases is underway,” with increasing incidence of inflammatory bowel disease (IBD), eosinophilic esophagitis (EoE), and disorders related to gut-brain interaction.
“While the underlying causes of this shift remain unclear, the association with industrialization suggests that environmental triggers may play a role in disease pathogenesis,” the authors wrote. Data to support that possibility, however, are lacking, Dr. Okafor said in an interview.
One potential mechanism to explain such an association could be local or systemic inflammation resulting from pollution exposure and leading to tissue injury. Others could include alterations in the gut microbiome or direct damage to the mucosal epithelial barrier from pollutants, which then results in epithelial cell death and subsequently increased intestinal permeability.
To explore whether any such associations exist, the researchers analyzed the incidence of IBS, functional dyspepsia, ulcerative colitis, Crohn’s disease, and eosinophilic esophagitis in different California ZIP codes with regard to each area’s levels of seven different pollutant markers. They used claims data for patients with Optum insurance to identify new diagnoses by ZIP code for nearly 2.9 million adult patients between 2009 and 2014 (ICD-9 era) and nearly 2.5 million patients between 2016 and 2019 (ICD-10 era). Preexisting diagnoses were excluded. The analysis included 1,365 different ZIP codes.
The measures of pollutants they assessed included the following: ozone, particulate matter less than 2.5 mcm (PM2.5), diesel emissions, drinking water contaminants, pesticides, toxic releases from industrial facilities, and traffic density. They used shoulder dislocations as a negative control in comparing incidence, and they adjusted the analysis to account for socioeconomic markers, patient-level sampling estimates, and county-level fixed effects.
Socioeconomic markers included not only income and race/ethnicity but also health insurance status, educational level, proportion of owner-occupied homes, median house prices, and the proportion of households receiving food stamps or meeting criteria for food insecurity. Given the number of potential confounders, the authors also made statistical adjustment (Bonferroni correction) to account for many multiple comparisons and reduce the likelihood of inflated statistical significance for any one finding.
The researchers found that the incidence of IBS per ZIP code was associated with the levels of PM2.5 and industrial airborne toxic releases during both time periods. An increase of 1 mcg/m3 of PM2.5 or additional 1% in toxic releases correlated with an additional 0.02 cases of IBS per 100 person-years (adjusted incidence rate ratios approximately 1.03 for IBS associated with both pollutants during both time periods).
”These associations were maintained across extensive adjustment for residual confounding and sensitivity analyses,” the authors added.
That increase in the total incidence of IBS in this study is very minor, but it’s not known how high environmental toxin levels may become in the future, Rishi D. Naik, MD, MSCI, assistant professor of medicine at Vanderbilt University Medical Center’s Esophageal Center in Nashville, Tenn., said in an interview.
“Though the increase on an absolute number currently is trivial, the percent increase if toxin releases dramatically increased can have an impact on our patients,” Dr. Naik said. “Public health policies should be in place to monitor these changes and future studies should be done prospectively to understand if this relationship is linear or has upper limits for absolute increases of incidence of IBS.”
Like the authors, however, Dr. Naik cautioned that these findings do not show causation and require further investigation. At least one potential confounder not considered in the study, Dr. Naik said, is that an increase in pharmacological therapy for IBS – which requires proper coding for insurance approval – increased during the time period as well.
Unlike EoE and IBD, IBS lacks objective pathological biomarkers for diagnosis that allow verification that “these patients truly had the disease versus were labeled with the diagnosis based on symptoms and need to obtain therapy,” Dr. Naik said. “Adjusting for prescription use and separating based on IBS-diarrhea and IBS-constipation would also help with the etiologies.”
Although the researchers also identified an association between IBS incidence and both traffic density and drinking water contaminants, these did not reach statistical significance after adjustment for multiple comparisons. Similarly, diesel particulate matter emissions were associated with functional dyspepsia and IBS until the statistical correction for multiple comparisons. None of the other conditions’ incidence was associated with any pollutant measured included in the study.
“It is important to highlight that our findings are not proof that environmental pollution causes irritable bowel syndrome but provide evidence to support further research on this topic,” Dr. Okafor said. “Our results are hypothesis generating. It would be helpful to better collect environmental hazards at a population level in a more systematic, reproducible manner so better ecological studies can be performed in the future to close knowledge gaps and improve our understanding of these diseases.”
Dr. Okafor said it would be valuable to explore potential associations between GI diseases and environmental pollutants in other states, but it would depend on how thorough data collection of pollutants is in other states. “Our study is the first step to exploring these interactions,” he noted.
“Though interesting data, the lack of patient-level data, dose response, treatment with an intervention, and the use of claims data prevent generalizability to larger populations both from a geographic perspective and also from ones based on gender, ethnicity, or socioeconomic factors,” Dr. Naik said. “Prospective studies showing incidence changes and interventions based on pollution control would help support their findings.”
Future studies could also further break down IBS incidence into IBS-diarrhea versus IBS-constipation and consider antibiotic exposure, treatment for symptoms, and symptom resolution, Dr. Naik said. “To support their association, patient-level trafficking of those who move to low and high rates of PM2.5 would help determine if individual symptoms improve with the sole intervention of geographic location,” he added.
Though it would be premature for the study to prompt any clinical changes in practice, Dr. Allen pointed out that the findings should raise clinicians’ awareness about the value of considering patients’ living areas and pollution exposure when evaluating GI symptoms.
“These data would lend support to the inclusive approach to an IBS diagnosis as opposed to a ‘rule-out’ diagnosis,” Dr. Allen said. “Additionally, we should investigate possible behavioral changes for patients exposed to environmental pollutants.”
He emphasized the importance of asking patients about their socioeconomic and environmental factors while helping them deal with GI disorders.
“These are complex and difficult histories to elicit during brief clinic encounters,” Dr. Allen said. “We need better ways to help patients understand their GI disorders in the context of their specific life stresses and avoid ordering multiple diagnostic tests when a different approach is needed to solve patients’ issues.”
The study’s biggest limitation is its ecologic design, which cannot link individual people’s exposures to their specific diagnosis. They also could not consider seasonal changes in pollutant levels or the possible interaction or cumulative effects of different pollutants. The authors also noted a number of other pollution exposures that they did not measure at all in this study, such as nitrogen dioxide, sulfur dioxide, heavy metals, or bacteria.
“Ecologic studies using claims data without a prespecified singular outcome, even when corrected for multiple comparisons, is at risk of confounding and bias,” Dr. Naik said. “This study will hopefully help with future environmental studies to understand the role of the environment and GI health.”
Dr. Okafor further cautioned that it’s likely premature to advocate for policy change right now based on these findings.
“We will need better temporal data to associate exposure to airborne pollutants and GI disease incidence and even severity,” Dr. Okafor said. “If it is possible to demonstrate this reliably, it may impact our ability to provide better care for our patients.”
As more research like this is conducted, however, it has the potential to improve how clinicians care for patients, Dr. Allen suggested.
“As we begin to understand the complex interactions of environment, social determinants of health, individual life stresses, and a person’s unique reaction to stress, we will be much better at helping patients live with GI symptoms and disorders,” Dr. Allen said. “We also can assign accountability for the externalities [costs] that environmental pollution causes.”
Dr. Allen, Dr. Naik, and the authors reported no conflicts of interest. The research was funded by the National Institutes of Health and Stanford University.
Increased levels of air pollution were linked to a slight uptick in new diagnoses of irritable bowel syndrome (IBS) in California residents, according to an ecologic study published in Clinical Gastroenterology and Hepatology.
“These data provide support for the role of environmental pollutants, especially air pollutants, in the development of IBS,” Philip N. Okafor, MD, MPH, of Stanford (Calif.) University, and colleagues wrote. “In contrast, we found no significant relationships between the seven environmental exposures and the ZIP-code level incidence of functional dyspepsia, ulcerative colitis, Crohn’s disease, and eosinophilic esophagitis.”
John I. Allen MD, MBA, a retired clinical professor medicine at the University of Michigan, Ann Arbor, said the findings were somewhat surprising, but he was impressed with the “fascinating and well-constructed” study.
“The differentiation between GI disorders that are linked to environmental pollutants [such as IBS] and those that are not [such as inflammatory bowel disease and eosinophilic esophagitis] is quite interesting and lends further credibility to the conclusions,” Dr. Allen said in an interview. “While definitive causal conclusions cannot rest on retrospective, population-level, studies alone, this extraordinarily detailed analysis should prompt further studies investigating root causes for these correlations,” such as gut epithelial changes secondary to ingested pollutants, for example.
The researchers noted that an “epidemiological shift in gastrointestinal diseases is underway,” with increasing incidence of inflammatory bowel disease (IBD), eosinophilic esophagitis (EoE), and disorders related to gut-brain interaction.
“While the underlying causes of this shift remain unclear, the association with industrialization suggests that environmental triggers may play a role in disease pathogenesis,” the authors wrote. Data to support that possibility, however, are lacking, Dr. Okafor said in an interview.
One potential mechanism to explain such an association could be local or systemic inflammation resulting from pollution exposure and leading to tissue injury. Others could include alterations in the gut microbiome or direct damage to the mucosal epithelial barrier from pollutants, which then results in epithelial cell death and subsequently increased intestinal permeability.
To explore whether any such associations exist, the researchers analyzed the incidence of IBS, functional dyspepsia, ulcerative colitis, Crohn’s disease, and eosinophilic esophagitis in different California ZIP codes with regard to each area’s levels of seven different pollutant markers. They used claims data for patients with Optum insurance to identify new diagnoses by ZIP code for nearly 2.9 million adult patients between 2009 and 2014 (ICD-9 era) and nearly 2.5 million patients between 2016 and 2019 (ICD-10 era). Preexisting diagnoses were excluded. The analysis included 1,365 different ZIP codes.
The measures of pollutants they assessed included the following: ozone, particulate matter less than 2.5 mcm (PM2.5), diesel emissions, drinking water contaminants, pesticides, toxic releases from industrial facilities, and traffic density. They used shoulder dislocations as a negative control in comparing incidence, and they adjusted the analysis to account for socioeconomic markers, patient-level sampling estimates, and county-level fixed effects.
Socioeconomic markers included not only income and race/ethnicity but also health insurance status, educational level, proportion of owner-occupied homes, median house prices, and the proportion of households receiving food stamps or meeting criteria for food insecurity. Given the number of potential confounders, the authors also made statistical adjustment (Bonferroni correction) to account for many multiple comparisons and reduce the likelihood of inflated statistical significance for any one finding.
The researchers found that the incidence of IBS per ZIP code was associated with the levels of PM2.5 and industrial airborne toxic releases during both time periods. An increase of 1 mcg/m3 of PM2.5 or additional 1% in toxic releases correlated with an additional 0.02 cases of IBS per 100 person-years (adjusted incidence rate ratios approximately 1.03 for IBS associated with both pollutants during both time periods).
”These associations were maintained across extensive adjustment for residual confounding and sensitivity analyses,” the authors added.
That increase in the total incidence of IBS in this study is very minor, but it’s not known how high environmental toxin levels may become in the future, Rishi D. Naik, MD, MSCI, assistant professor of medicine at Vanderbilt University Medical Center’s Esophageal Center in Nashville, Tenn., said in an interview.
“Though the increase on an absolute number currently is trivial, the percent increase if toxin releases dramatically increased can have an impact on our patients,” Dr. Naik said. “Public health policies should be in place to monitor these changes and future studies should be done prospectively to understand if this relationship is linear or has upper limits for absolute increases of incidence of IBS.”
Like the authors, however, Dr. Naik cautioned that these findings do not show causation and require further investigation. At least one potential confounder not considered in the study, Dr. Naik said, is that an increase in pharmacological therapy for IBS – which requires proper coding for insurance approval – increased during the time period as well.
Unlike EoE and IBD, IBS lacks objective pathological biomarkers for diagnosis that allow verification that “these patients truly had the disease versus were labeled with the diagnosis based on symptoms and need to obtain therapy,” Dr. Naik said. “Adjusting for prescription use and separating based on IBS-diarrhea and IBS-constipation would also help with the etiologies.”
Although the researchers also identified an association between IBS incidence and both traffic density and drinking water contaminants, these did not reach statistical significance after adjustment for multiple comparisons. Similarly, diesel particulate matter emissions were associated with functional dyspepsia and IBS until the statistical correction for multiple comparisons. None of the other conditions’ incidence was associated with any pollutant measured included in the study.
“It is important to highlight that our findings are not proof that environmental pollution causes irritable bowel syndrome but provide evidence to support further research on this topic,” Dr. Okafor said. “Our results are hypothesis generating. It would be helpful to better collect environmental hazards at a population level in a more systematic, reproducible manner so better ecological studies can be performed in the future to close knowledge gaps and improve our understanding of these diseases.”
Dr. Okafor said it would be valuable to explore potential associations between GI diseases and environmental pollutants in other states, but it would depend on how thorough data collection of pollutants is in other states. “Our study is the first step to exploring these interactions,” he noted.
“Though interesting data, the lack of patient-level data, dose response, treatment with an intervention, and the use of claims data prevent generalizability to larger populations both from a geographic perspective and also from ones based on gender, ethnicity, or socioeconomic factors,” Dr. Naik said. “Prospective studies showing incidence changes and interventions based on pollution control would help support their findings.”
Future studies could also further break down IBS incidence into IBS-diarrhea versus IBS-constipation and consider antibiotic exposure, treatment for symptoms, and symptom resolution, Dr. Naik said. “To support their association, patient-level trafficking of those who move to low and high rates of PM2.5 would help determine if individual symptoms improve with the sole intervention of geographic location,” he added.
Though it would be premature for the study to prompt any clinical changes in practice, Dr. Allen pointed out that the findings should raise clinicians’ awareness about the value of considering patients’ living areas and pollution exposure when evaluating GI symptoms.
“These data would lend support to the inclusive approach to an IBS diagnosis as opposed to a ‘rule-out’ diagnosis,” Dr. Allen said. “Additionally, we should investigate possible behavioral changes for patients exposed to environmental pollutants.”
He emphasized the importance of asking patients about their socioeconomic and environmental factors while helping them deal with GI disorders.
“These are complex and difficult histories to elicit during brief clinic encounters,” Dr. Allen said. “We need better ways to help patients understand their GI disorders in the context of their specific life stresses and avoid ordering multiple diagnostic tests when a different approach is needed to solve patients’ issues.”
The study’s biggest limitation is its ecologic design, which cannot link individual people’s exposures to their specific diagnosis. They also could not consider seasonal changes in pollutant levels or the possible interaction or cumulative effects of different pollutants. The authors also noted a number of other pollution exposures that they did not measure at all in this study, such as nitrogen dioxide, sulfur dioxide, heavy metals, or bacteria.
“Ecologic studies using claims data without a prespecified singular outcome, even when corrected for multiple comparisons, is at risk of confounding and bias,” Dr. Naik said. “This study will hopefully help with future environmental studies to understand the role of the environment and GI health.”
Dr. Okafor further cautioned that it’s likely premature to advocate for policy change right now based on these findings.
“We will need better temporal data to associate exposure to airborne pollutants and GI disease incidence and even severity,” Dr. Okafor said. “If it is possible to demonstrate this reliably, it may impact our ability to provide better care for our patients.”
As more research like this is conducted, however, it has the potential to improve how clinicians care for patients, Dr. Allen suggested.
“As we begin to understand the complex interactions of environment, social determinants of health, individual life stresses, and a person’s unique reaction to stress, we will be much better at helping patients live with GI symptoms and disorders,” Dr. Allen said. “We also can assign accountability for the externalities [costs] that environmental pollution causes.”
Dr. Allen, Dr. Naik, and the authors reported no conflicts of interest. The research was funded by the National Institutes of Health and Stanford University.
Increased levels of air pollution were linked to a slight uptick in new diagnoses of irritable bowel syndrome (IBS) in California residents, according to an ecologic study published in Clinical Gastroenterology and Hepatology.
“These data provide support for the role of environmental pollutants, especially air pollutants, in the development of IBS,” Philip N. Okafor, MD, MPH, of Stanford (Calif.) University, and colleagues wrote. “In contrast, we found no significant relationships between the seven environmental exposures and the ZIP-code level incidence of functional dyspepsia, ulcerative colitis, Crohn’s disease, and eosinophilic esophagitis.”
John I. Allen MD, MBA, a retired clinical professor medicine at the University of Michigan, Ann Arbor, said the findings were somewhat surprising, but he was impressed with the “fascinating and well-constructed” study.
“The differentiation between GI disorders that are linked to environmental pollutants [such as IBS] and those that are not [such as inflammatory bowel disease and eosinophilic esophagitis] is quite interesting and lends further credibility to the conclusions,” Dr. Allen said in an interview. “While definitive causal conclusions cannot rest on retrospective, population-level, studies alone, this extraordinarily detailed analysis should prompt further studies investigating root causes for these correlations,” such as gut epithelial changes secondary to ingested pollutants, for example.
The researchers noted that an “epidemiological shift in gastrointestinal diseases is underway,” with increasing incidence of inflammatory bowel disease (IBD), eosinophilic esophagitis (EoE), and disorders related to gut-brain interaction.
“While the underlying causes of this shift remain unclear, the association with industrialization suggests that environmental triggers may play a role in disease pathogenesis,” the authors wrote. Data to support that possibility, however, are lacking, Dr. Okafor said in an interview.
One potential mechanism to explain such an association could be local or systemic inflammation resulting from pollution exposure and leading to tissue injury. Others could include alterations in the gut microbiome or direct damage to the mucosal epithelial barrier from pollutants, which then results in epithelial cell death and subsequently increased intestinal permeability.
To explore whether any such associations exist, the researchers analyzed the incidence of IBS, functional dyspepsia, ulcerative colitis, Crohn’s disease, and eosinophilic esophagitis in different California ZIP codes with regard to each area’s levels of seven different pollutant markers. They used claims data for patients with Optum insurance to identify new diagnoses by ZIP code for nearly 2.9 million adult patients between 2009 and 2014 (ICD-9 era) and nearly 2.5 million patients between 2016 and 2019 (ICD-10 era). Preexisting diagnoses were excluded. The analysis included 1,365 different ZIP codes.
The measures of pollutants they assessed included the following: ozone, particulate matter less than 2.5 mcm (PM2.5), diesel emissions, drinking water contaminants, pesticides, toxic releases from industrial facilities, and traffic density. They used shoulder dislocations as a negative control in comparing incidence, and they adjusted the analysis to account for socioeconomic markers, patient-level sampling estimates, and county-level fixed effects.
Socioeconomic markers included not only income and race/ethnicity but also health insurance status, educational level, proportion of owner-occupied homes, median house prices, and the proportion of households receiving food stamps or meeting criteria for food insecurity. Given the number of potential confounders, the authors also made statistical adjustment (Bonferroni correction) to account for many multiple comparisons and reduce the likelihood of inflated statistical significance for any one finding.
The researchers found that the incidence of IBS per ZIP code was associated with the levels of PM2.5 and industrial airborne toxic releases during both time periods. An increase of 1 mcg/m3 of PM2.5 or additional 1% in toxic releases correlated with an additional 0.02 cases of IBS per 100 person-years (adjusted incidence rate ratios approximately 1.03 for IBS associated with both pollutants during both time periods).
”These associations were maintained across extensive adjustment for residual confounding and sensitivity analyses,” the authors added.
That increase in the total incidence of IBS in this study is very minor, but it’s not known how high environmental toxin levels may become in the future, Rishi D. Naik, MD, MSCI, assistant professor of medicine at Vanderbilt University Medical Center’s Esophageal Center in Nashville, Tenn., said in an interview.
“Though the increase on an absolute number currently is trivial, the percent increase if toxin releases dramatically increased can have an impact on our patients,” Dr. Naik said. “Public health policies should be in place to monitor these changes and future studies should be done prospectively to understand if this relationship is linear or has upper limits for absolute increases of incidence of IBS.”
Like the authors, however, Dr. Naik cautioned that these findings do not show causation and require further investigation. At least one potential confounder not considered in the study, Dr. Naik said, is that an increase in pharmacological therapy for IBS – which requires proper coding for insurance approval – increased during the time period as well.
Unlike EoE and IBD, IBS lacks objective pathological biomarkers for diagnosis that allow verification that “these patients truly had the disease versus were labeled with the diagnosis based on symptoms and need to obtain therapy,” Dr. Naik said. “Adjusting for prescription use and separating based on IBS-diarrhea and IBS-constipation would also help with the etiologies.”
Although the researchers also identified an association between IBS incidence and both traffic density and drinking water contaminants, these did not reach statistical significance after adjustment for multiple comparisons. Similarly, diesel particulate matter emissions were associated with functional dyspepsia and IBS until the statistical correction for multiple comparisons. None of the other conditions’ incidence was associated with any pollutant measured included in the study.
“It is important to highlight that our findings are not proof that environmental pollution causes irritable bowel syndrome but provide evidence to support further research on this topic,” Dr. Okafor said. “Our results are hypothesis generating. It would be helpful to better collect environmental hazards at a population level in a more systematic, reproducible manner so better ecological studies can be performed in the future to close knowledge gaps and improve our understanding of these diseases.”
Dr. Okafor said it would be valuable to explore potential associations between GI diseases and environmental pollutants in other states, but it would depend on how thorough data collection of pollutants is in other states. “Our study is the first step to exploring these interactions,” he noted.
“Though interesting data, the lack of patient-level data, dose response, treatment with an intervention, and the use of claims data prevent generalizability to larger populations both from a geographic perspective and also from ones based on gender, ethnicity, or socioeconomic factors,” Dr. Naik said. “Prospective studies showing incidence changes and interventions based on pollution control would help support their findings.”
Future studies could also further break down IBS incidence into IBS-diarrhea versus IBS-constipation and consider antibiotic exposure, treatment for symptoms, and symptom resolution, Dr. Naik said. “To support their association, patient-level trafficking of those who move to low and high rates of PM2.5 would help determine if individual symptoms improve with the sole intervention of geographic location,” he added.
Though it would be premature for the study to prompt any clinical changes in practice, Dr. Allen pointed out that the findings should raise clinicians’ awareness about the value of considering patients’ living areas and pollution exposure when evaluating GI symptoms.
“These data would lend support to the inclusive approach to an IBS diagnosis as opposed to a ‘rule-out’ diagnosis,” Dr. Allen said. “Additionally, we should investigate possible behavioral changes for patients exposed to environmental pollutants.”
He emphasized the importance of asking patients about their socioeconomic and environmental factors while helping them deal with GI disorders.
“These are complex and difficult histories to elicit during brief clinic encounters,” Dr. Allen said. “We need better ways to help patients understand their GI disorders in the context of their specific life stresses and avoid ordering multiple diagnostic tests when a different approach is needed to solve patients’ issues.”
The study’s biggest limitation is its ecologic design, which cannot link individual people’s exposures to their specific diagnosis. They also could not consider seasonal changes in pollutant levels or the possible interaction or cumulative effects of different pollutants. The authors also noted a number of other pollution exposures that they did not measure at all in this study, such as nitrogen dioxide, sulfur dioxide, heavy metals, or bacteria.
“Ecologic studies using claims data without a prespecified singular outcome, even when corrected for multiple comparisons, is at risk of confounding and bias,” Dr. Naik said. “This study will hopefully help with future environmental studies to understand the role of the environment and GI health.”
Dr. Okafor further cautioned that it’s likely premature to advocate for policy change right now based on these findings.
“We will need better temporal data to associate exposure to airborne pollutants and GI disease incidence and even severity,” Dr. Okafor said. “If it is possible to demonstrate this reliably, it may impact our ability to provide better care for our patients.”
As more research like this is conducted, however, it has the potential to improve how clinicians care for patients, Dr. Allen suggested.
“As we begin to understand the complex interactions of environment, social determinants of health, individual life stresses, and a person’s unique reaction to stress, we will be much better at helping patients live with GI symptoms and disorders,” Dr. Allen said. “We also can assign accountability for the externalities [costs] that environmental pollution causes.”
Dr. Allen, Dr. Naik, and the authors reported no conflicts of interest. The research was funded by the National Institutes of Health and Stanford University.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
AGA Clinical Practice Update: Expert review of management of refractory celiac disease
The diagnosis and management of refractory celiac disease remains challenging, but ongoing studies can provide the proper diagnostic criteria and identify the optimal management strategies, according to a new American Gastroenterological Association expert review published in Gastroenterology.
Celiac disease is present in about 1% of the U.S. population and can cause various symptoms, wrote Peter H. R. Green, MD, director of the Celiac Disease Center at Columbia University, New York, and colleagues. Adhering to a strict gluten-free diet can improve symptoms, normalize serum antibody levels, and reverse small bowel villous atrophy. However, persistent or recurrent symptoms and elevated celiac antibodies can persist in some patients after a year of trying a gluten-free diet, a condition called nonresponsive celiac disease. In some patients, this raises concern for refractory celiac disease, or RCD.
“RCD is believed to occur in only approximately 1% of patients with celiac disease, although this may be an overestimate, as data are obtained from referral centers,” the authors wrote.
RCD can be classified into two subtypes with different diagnostic criteria, prognoses, and therapy responses. The first, called RCD1, is characterized by villous atrophy but has intraepithelial lymphocytes similar to conventional celiac disease. The other, called RCD2, is characterized by aberrant clonal T-cell expansion in the intestinal tract and other organs, has a poorer prognosis than RCD1, and has a risk of developing ulcerative jejunoileitis or enteropathy-associated T-cell lymphoma.
The experts developed 10 clinical practice advice statements based on a review of the published literature and expert opinion.
First, in patients who have persistent or recurring symptoms, an initial celiac disease diagnosis should be confirmed through review of prior diagnostic testing, including serologies, endoscopies, and histologic findings. Celiac disease can overlap with other gastrointestinal conditions, and some pathologic findings aren’t specific to celiac disease. Results of serologic testing with tissue transglutaminase immunoglobulin A, deamidated gliadin peptide IgA and IgG, and endomysial antibodies should be reviewed or obtained if not previously performed.
Next, in those with confirmed but nonresponsive celiac disease, ongoing gluten ingestion should be excluded as a cause of symptoms with serologic testing, dietitian review, and potentially detection of immunogenic peptides in stool or urine samples. The authors noted that persistent gluten ingestion, whether intentional or inadvertent, accounts for 40%-50% of patients with nonresponsive celiac disease. In these cases, esophagogastroduodenoscopy and small bowel biopsies should be performed to look for persistent villous atrophy, which can also be caused by common variable immunodeficiency, autoimmune enteropathy, tropical sprue, and medication-induced enteropathy. Patients with villous atrophy due to other causes won’t respond to a gluten-free diet.
After excluding gluten, clinicians should perform a systematic evaluation for other potential causes of symptoms, including functional bowel disorders, lactose or fructose intolerance, microscopic colitis, pancreatic insufficiency, inflammatory bowel disease, and small intestinal bacterial growth. Irritable bowel syndrome, for instance, may contribute to persistent symptoms and respond to fermentable oligo-, di-, and monosaccharides and polyols (FODMAP) restriction. RCD should be strongly considered in patients with persistent symptoms or signs of malabsorption after the exclusion of the other causes.
To distinguish between the two subtypes of RCD and exclude enteropathy-associated T-cell lymphoma, clinicians should use flow cytometry, immunohistochemistry, and T-cell receptor rearrangement studies. RCD1 has a normal intraepithelial lymphocyte population, and RCD2 has an aberrant, clonal intraepithelial lymphocyte population. Consulting with a hematopathologist may be necessary to interpret these studies.
After RCD2 is diagnosed, complications such as enteropathy-associated T-cell lymphoma and ulcerative jejunoileitis should be excluded through small bowel imaging with capsule endoscopy and either computed tomography (CT) or magnetic resonance enterography. In general, the extent and severity of villous atrophy is greater in patients with RCD2, compared with RCD1.
In patients diagnosed with RCD, clinicians should complete a detailed nutritional assessment with investigation of micronutrient and macronutrient deficiencies. Check albumin as an independent prognostic factor. Then, try to correct deficiencies with oral supplements. Malnourished patients may need enteral support, and those with severe malnutrition due to malabsorption may need parenteral support.
So far, RCD management suggestions are based on small retrospective studies and expert opinion, with minimal prospective data and no Food and Drug Administration–approved therapies. The goals should be to improve symptoms and duodenal mucosal abnormalities, manage malnutrition, and prevent lymphoma. Glucocorticoids are considered first-line therapy, typically open-capsule budesonide given as 3 mg three times daily. Prednisone serves as an alternative with proven efficacy but a higher risk for adverse effects.
The optimal choice for second-line therapy is unknown, but the addition of an immunosuppressant agent to steroids appears to be effective in RCD1, including azathioprine, mercaptopurine, and tioguanine. The best treatment for RCD2 is unknown, though clinical response has been reported with steroids, and cladribine has been well tolerated in some patients.
Patients with RCD who don’t respond to steroids may benefit from referral to a center with expertise for management or evaluation for inclusion in clinical trials. Frequent medical visits are advised until the disease is well controlled, with regular follow-up after that.
Ultimately, “patients with RCD benefit from evaluation and regular follow-up by a multidisciplinary team, including gastroenterologists and dietitians, to assess clinical and histologic response to therapy,” the authors wrote. “Identify local experts with expertise in celiac disease to assist with management.”
The authors reported no grant support or funding sources for this study. One author has received research report from Freenome, and another is on the celiac disease advisory board for Takeda. The remaining authors disclosed no conflicts.
The diagnosis and management of refractory celiac disease remains challenging, but ongoing studies can provide the proper diagnostic criteria and identify the optimal management strategies, according to a new American Gastroenterological Association expert review published in Gastroenterology.
Celiac disease is present in about 1% of the U.S. population and can cause various symptoms, wrote Peter H. R. Green, MD, director of the Celiac Disease Center at Columbia University, New York, and colleagues. Adhering to a strict gluten-free diet can improve symptoms, normalize serum antibody levels, and reverse small bowel villous atrophy. However, persistent or recurrent symptoms and elevated celiac antibodies can persist in some patients after a year of trying a gluten-free diet, a condition called nonresponsive celiac disease. In some patients, this raises concern for refractory celiac disease, or RCD.
“RCD is believed to occur in only approximately 1% of patients with celiac disease, although this may be an overestimate, as data are obtained from referral centers,” the authors wrote.
RCD can be classified into two subtypes with different diagnostic criteria, prognoses, and therapy responses. The first, called RCD1, is characterized by villous atrophy but has intraepithelial lymphocytes similar to conventional celiac disease. The other, called RCD2, is characterized by aberrant clonal T-cell expansion in the intestinal tract and other organs, has a poorer prognosis than RCD1, and has a risk of developing ulcerative jejunoileitis or enteropathy-associated T-cell lymphoma.
The experts developed 10 clinical practice advice statements based on a review of the published literature and expert opinion.
First, in patients who have persistent or recurring symptoms, an initial celiac disease diagnosis should be confirmed through review of prior diagnostic testing, including serologies, endoscopies, and histologic findings. Celiac disease can overlap with other gastrointestinal conditions, and some pathologic findings aren’t specific to celiac disease. Results of serologic testing with tissue transglutaminase immunoglobulin A, deamidated gliadin peptide IgA and IgG, and endomysial antibodies should be reviewed or obtained if not previously performed.
Next, in those with confirmed but nonresponsive celiac disease, ongoing gluten ingestion should be excluded as a cause of symptoms with serologic testing, dietitian review, and potentially detection of immunogenic peptides in stool or urine samples. The authors noted that persistent gluten ingestion, whether intentional or inadvertent, accounts for 40%-50% of patients with nonresponsive celiac disease. In these cases, esophagogastroduodenoscopy and small bowel biopsies should be performed to look for persistent villous atrophy, which can also be caused by common variable immunodeficiency, autoimmune enteropathy, tropical sprue, and medication-induced enteropathy. Patients with villous atrophy due to other causes won’t respond to a gluten-free diet.
After excluding gluten, clinicians should perform a systematic evaluation for other potential causes of symptoms, including functional bowel disorders, lactose or fructose intolerance, microscopic colitis, pancreatic insufficiency, inflammatory bowel disease, and small intestinal bacterial growth. Irritable bowel syndrome, for instance, may contribute to persistent symptoms and respond to fermentable oligo-, di-, and monosaccharides and polyols (FODMAP) restriction. RCD should be strongly considered in patients with persistent symptoms or signs of malabsorption after the exclusion of the other causes.
To distinguish between the two subtypes of RCD and exclude enteropathy-associated T-cell lymphoma, clinicians should use flow cytometry, immunohistochemistry, and T-cell receptor rearrangement studies. RCD1 has a normal intraepithelial lymphocyte population, and RCD2 has an aberrant, clonal intraepithelial lymphocyte population. Consulting with a hematopathologist may be necessary to interpret these studies.
After RCD2 is diagnosed, complications such as enteropathy-associated T-cell lymphoma and ulcerative jejunoileitis should be excluded through small bowel imaging with capsule endoscopy and either computed tomography (CT) or magnetic resonance enterography. In general, the extent and severity of villous atrophy is greater in patients with RCD2, compared with RCD1.
In patients diagnosed with RCD, clinicians should complete a detailed nutritional assessment with investigation of micronutrient and macronutrient deficiencies. Check albumin as an independent prognostic factor. Then, try to correct deficiencies with oral supplements. Malnourished patients may need enteral support, and those with severe malnutrition due to malabsorption may need parenteral support.
So far, RCD management suggestions are based on small retrospective studies and expert opinion, with minimal prospective data and no Food and Drug Administration–approved therapies. The goals should be to improve symptoms and duodenal mucosal abnormalities, manage malnutrition, and prevent lymphoma. Glucocorticoids are considered first-line therapy, typically open-capsule budesonide given as 3 mg three times daily. Prednisone serves as an alternative with proven efficacy but a higher risk for adverse effects.
The optimal choice for second-line therapy is unknown, but the addition of an immunosuppressant agent to steroids appears to be effective in RCD1, including azathioprine, mercaptopurine, and tioguanine. The best treatment for RCD2 is unknown, though clinical response has been reported with steroids, and cladribine has been well tolerated in some patients.
Patients with RCD who don’t respond to steroids may benefit from referral to a center with expertise for management or evaluation for inclusion in clinical trials. Frequent medical visits are advised until the disease is well controlled, with regular follow-up after that.
Ultimately, “patients with RCD benefit from evaluation and regular follow-up by a multidisciplinary team, including gastroenterologists and dietitians, to assess clinical and histologic response to therapy,” the authors wrote. “Identify local experts with expertise in celiac disease to assist with management.”
The authors reported no grant support or funding sources for this study. One author has received research report from Freenome, and another is on the celiac disease advisory board for Takeda. The remaining authors disclosed no conflicts.
The diagnosis and management of refractory celiac disease remains challenging, but ongoing studies can provide the proper diagnostic criteria and identify the optimal management strategies, according to a new American Gastroenterological Association expert review published in Gastroenterology.
Celiac disease is present in about 1% of the U.S. population and can cause various symptoms, wrote Peter H. R. Green, MD, director of the Celiac Disease Center at Columbia University, New York, and colleagues. Adhering to a strict gluten-free diet can improve symptoms, normalize serum antibody levels, and reverse small bowel villous atrophy. However, persistent or recurrent symptoms and elevated celiac antibodies can persist in some patients after a year of trying a gluten-free diet, a condition called nonresponsive celiac disease. In some patients, this raises concern for refractory celiac disease, or RCD.
“RCD is believed to occur in only approximately 1% of patients with celiac disease, although this may be an overestimate, as data are obtained from referral centers,” the authors wrote.
RCD can be classified into two subtypes with different diagnostic criteria, prognoses, and therapy responses. The first, called RCD1, is characterized by villous atrophy but has intraepithelial lymphocytes similar to conventional celiac disease. The other, called RCD2, is characterized by aberrant clonal T-cell expansion in the intestinal tract and other organs, has a poorer prognosis than RCD1, and has a risk of developing ulcerative jejunoileitis or enteropathy-associated T-cell lymphoma.
The experts developed 10 clinical practice advice statements based on a review of the published literature and expert opinion.
First, in patients who have persistent or recurring symptoms, an initial celiac disease diagnosis should be confirmed through review of prior diagnostic testing, including serologies, endoscopies, and histologic findings. Celiac disease can overlap with other gastrointestinal conditions, and some pathologic findings aren’t specific to celiac disease. Results of serologic testing with tissue transglutaminase immunoglobulin A, deamidated gliadin peptide IgA and IgG, and endomysial antibodies should be reviewed or obtained if not previously performed.
Next, in those with confirmed but nonresponsive celiac disease, ongoing gluten ingestion should be excluded as a cause of symptoms with serologic testing, dietitian review, and potentially detection of immunogenic peptides in stool or urine samples. The authors noted that persistent gluten ingestion, whether intentional or inadvertent, accounts for 40%-50% of patients with nonresponsive celiac disease. In these cases, esophagogastroduodenoscopy and small bowel biopsies should be performed to look for persistent villous atrophy, which can also be caused by common variable immunodeficiency, autoimmune enteropathy, tropical sprue, and medication-induced enteropathy. Patients with villous atrophy due to other causes won’t respond to a gluten-free diet.
After excluding gluten, clinicians should perform a systematic evaluation for other potential causes of symptoms, including functional bowel disorders, lactose or fructose intolerance, microscopic colitis, pancreatic insufficiency, inflammatory bowel disease, and small intestinal bacterial growth. Irritable bowel syndrome, for instance, may contribute to persistent symptoms and respond to fermentable oligo-, di-, and monosaccharides and polyols (FODMAP) restriction. RCD should be strongly considered in patients with persistent symptoms or signs of malabsorption after the exclusion of the other causes.
To distinguish between the two subtypes of RCD and exclude enteropathy-associated T-cell lymphoma, clinicians should use flow cytometry, immunohistochemistry, and T-cell receptor rearrangement studies. RCD1 has a normal intraepithelial lymphocyte population, and RCD2 has an aberrant, clonal intraepithelial lymphocyte population. Consulting with a hematopathologist may be necessary to interpret these studies.
After RCD2 is diagnosed, complications such as enteropathy-associated T-cell lymphoma and ulcerative jejunoileitis should be excluded through small bowel imaging with capsule endoscopy and either computed tomography (CT) or magnetic resonance enterography. In general, the extent and severity of villous atrophy is greater in patients with RCD2, compared with RCD1.
In patients diagnosed with RCD, clinicians should complete a detailed nutritional assessment with investigation of micronutrient and macronutrient deficiencies. Check albumin as an independent prognostic factor. Then, try to correct deficiencies with oral supplements. Malnourished patients may need enteral support, and those with severe malnutrition due to malabsorption may need parenteral support.
So far, RCD management suggestions are based on small retrospective studies and expert opinion, with minimal prospective data and no Food and Drug Administration–approved therapies. The goals should be to improve symptoms and duodenal mucosal abnormalities, manage malnutrition, and prevent lymphoma. Glucocorticoids are considered first-line therapy, typically open-capsule budesonide given as 3 mg three times daily. Prednisone serves as an alternative with proven efficacy but a higher risk for adverse effects.
The optimal choice for second-line therapy is unknown, but the addition of an immunosuppressant agent to steroids appears to be effective in RCD1, including azathioprine, mercaptopurine, and tioguanine. The best treatment for RCD2 is unknown, though clinical response has been reported with steroids, and cladribine has been well tolerated in some patients.
Patients with RCD who don’t respond to steroids may benefit from referral to a center with expertise for management or evaluation for inclusion in clinical trials. Frequent medical visits are advised until the disease is well controlled, with regular follow-up after that.
Ultimately, “patients with RCD benefit from evaluation and regular follow-up by a multidisciplinary team, including gastroenterologists and dietitians, to assess clinical and histologic response to therapy,” the authors wrote. “Identify local experts with expertise in celiac disease to assist with management.”
The authors reported no grant support or funding sources for this study. One author has received research report from Freenome, and another is on the celiac disease advisory board for Takeda. The remaining authors disclosed no conflicts.
FROM GASTROENTEROLOGY