User login
Hospital at Home: Delivering hospital-level care without the hospital
How to implement a new model of care
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
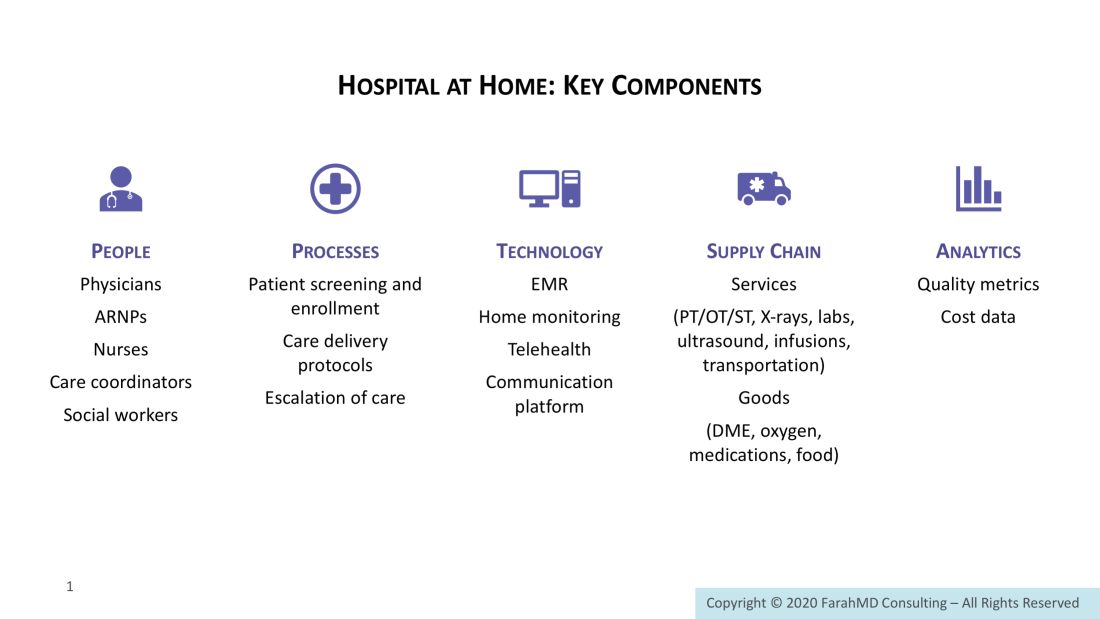
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
How to implement a new model of care
How to implement a new model of care
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
What hospitalists need to know about health care reimbursement and denial prevention
Under a fee-for-service payment model, health care providers get paid by private and public payers for patient services such as physician visits, hospital stays, procedures, and tests. In an ideal world, providers would receive accurate, complete, and timely reimbursements. Unfortunately, the reality is far from ideal, where payment denials and delays are a common occurrence.
According to one study, out of $3 trillion in total claims submitted by health care organizations, an estimated 9% of charges ($262 billion), were initially denied.1 The good news is that 90% of all denials are preventable, and two-thirds of those preventable denials can be successfully appealed.2
Hospitalists are essential in preventing denials for hospital services and should be familiar with the basics of health care reimbursement and common reasons for denials. In this article we will provide an overview of the U.S. health care payment system, revenue cycle management and types of denials, and focus on the role of physician advisors and hospitalists in preventing and combating denials.
Overview of the U.S. health care payment system
In 2018 alone, the U.S. spent $3.6 trillion on health care. Of those dollars, 33% went to payments for hospital care and 20% went to physician and clinical services.3 So where do the nation’s health care dollars come from?
The United States has a complex multiple-payer system that includes private insurance companies and public payers funded by the federal and state governments, such as Medicare and Medicaid. Per the National Association of Insurance Commissioners’ 2018 Market Share Reports, there are 125 private accident and health insurance companies in the U.S., with the top five – UnitedHealth, Kaiser, Anthem, Humana, and CVS – holding a cumulative market share of almost 40%.4
Medicare accounts for 15% of federal budget spending and provides insurance coverage to almost 60 million people who are 65 and older, have end-stage renal disease, or have been approved for Social Security disability insurance benefits.5 Medicare Part A covers hospital, skilled nursing facility, home health, and hospice care. For example, for inpatient stays, Medicare Part A pays hospitals a predetermined rate per discharge according to the Medicare Severity Diagnosis Related Groups (MS-DRGs), which are based on the principal and secondary diagnoses, and performed procedures.6
Medicare Part B covers physician services and outpatient services and supplies, including labs and durable medical equipment, which are paid based on submitted Healthcare Common Procedure Coding System (HCPCS) codes.7 It is important to know that hospital observation stays are considered outpatient services, and are paid by Medicare Part B. Outpatient stays often are reimbursed at a lower rate than inpatient admissions, even in cases with similar utilization of hospital resources.
Medicaid is jointly funded by the states and the federal government and offers insurance coverage to more than 75 million eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. Over 10 million people are dually eligible for both Medicare and Medicaid.5 Increasingly, government payers, both state and federal, are contracting with private insurance companies to deliver Medicare and Medicaid services, also known as Medicare Advantage and Managed Medicaid Plans.
According to the U.S. Department of Treasury, in the 2019 fiscal year (October 2018 to September 2019), 33% of the nation’s health care dollars came from private insurance, 21% from Medicare, 16% from Medicaid, 15% from other government programs (for example, Veteran Affairs), 10% from out-of-pocket, and 4% from other private sources.5
Understanding revenue cycle management and denials
Providers, such as physicians or hospitals, submit claims to insurance companies that include, among other information, patient demographics and insurance, diagnoses, MS-DRGs and/or HCPCS codes, and charges. Revenue cycle management’s goal is to receive accurate, complete, and timely reimbursement for provided patient services, which is a complex and resource-intensive process.
According to the Healthcare Financial Management Association (HFMA), revenue cycle management includes “all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue.” These functions could be broken down into four main categories:
- Claims preparation (for example, patient registration, insurance eligibility, benefit verifications, and preauthorization).
- Claims submission (for example, charge capture, medical coding based on medical record documentation and claims transmission).
- Claims management (for example, payment posting, denial management, and patient collections).
- Reporting and analysis.
Claim denial is “the refusal of an insurance company or carrier to honor a request by an individual (or his or her provider) to pay for health care services obtained from a health care professional.”8 Payers can deny an entire claim or provide only a partial payment. Initial denial rate is tracked at the claim level (number of claims denied/number of claims submitted) and at the dollar level (total dollar amount of claims denied/total dollar amount of claims submitted).
Denials are classified as hard versus soft, and clinical versus technical or administrative:
- Hard denials result in lost revenue unless successfully appealed (for example, lack of medical necessity).
- Soft denials do not require appeal and may be paid if a provider corrects the claim or submits additional information (for example, missing or inaccurate patient information, and missing medical records).
- Clinical denials are based on medical necessity, including level of care determination (for example, inpatient versus outpatient) and length of stay. They can be concurrent and retrospective and typically start as soft denials.
- Technical or administrative denials are based on reasons other than clinical (for example, failure to preauthorize care or lack of benefits).
According to the Advisory Board’s 2017 survey of hospitals and health care systems, 50% of initial denials were technical/demographic errors, 20% medical necessity, 16% eligibility, and 14% authorization. Forty seven percent of those denials came from commercial payers, 33% from Medicare/Medicare Advantage, 17% from Medicaid, and 3% from other payers.9
Determination of medical necessity may vary by payer. As an example, let’s look at inpatient admissions. According to the Medicare Two-Midnight Rule, inpatient admission is appropriate “if the admitting practitioner expects the beneficiary to require medically necessary hospital care spanning two or more midnights, and such reasonable expectation is supported by the medical record documentation.”10
Medicare guidelines acknowledge that a physician’s decision to admit a patient is based on complex medical factors including, but not limited to:
- The beneficiary history and comorbidities, and the severity of signs and symptoms (also known as Severity of Illness or SI).
- Current medical needs (also known as Intensity of Service or IS).
- The risk of an adverse event.
Generally, private payers do not follow the Two-Midnight Rule, and instead utilize evidence-based MCG guidelines,11 InterQual® criteria12 or internal criteria to determine if an inpatient admission is “medically necessary.” Hospital utilization review nurses often use MCG and/or InterQual® to aid admission status decisions and may request secondary review by a physician if medical necessity for an inpatient admission is not clear-cut.
The role of physician advisors
Considering the rising financial pressure and growing complexity of private and public payers’ rules and regulations, many hospitals turned to physician advisors to help prevent and reduce denials. Typically, physician advisors perform concurrent secondary reviews to help determine the most appropriate level of care, participate in peer-to-peer discussions with payers, and write formal appeals to overturn clinical denials.
“Physician advisors are generally not in the business of critiquing clinical practice, instead they review whether the chart documentation supports initial and continued hospitalization,” said Charles Locke, MD, senior physician advisor at the Johns Hopkins Hospital and president of the American College of Physician Advisors (ACPA). “However, physician advisors should seek additional information and provide feedback in those cases where the documentation does not support medical necessity for hospitalization.”
Many physician advisors are current or former hospitalists. Chris Shearer, MD, chief medical officer for remote advisory at Sound Physicians Advisory Services, says that “hospitalists are the natural physician advisors as they have a working knowledge of what patients need to be inpatients and which are less sick and likely to be discharged quickly.”
The role of physician advisors extends beyond reviews to include physician engagement and education. Physician advisors are a critical link between physicians, utilization review nurses, case managers, and clinical documentation integrity (CDI) and revenue cycle teams, and are increasingly involved in hospital-wide denial prevention efforts.
Physician advisors are invaluable in identifying and validating root causes for clinical denials and generating potential solutions, as they bring to the table:
- Clinical expertise.
- Understanding of clinical workflows.
- Knowledge of the most current public and private payers’ regulations.
- Insight into hospital-specific clinical documentation opportunities (for example, by diagnosis, procedure, service line, and provider).
- Understanding of payers’ reasons for clinical denials through peer-to-peer discussions
The role of hospitalists in preventing clinical denials
I asked three experienced physician advisors – Dr. Locke, Dr. Shearer, and Deepak Pahuja, MD, chief medical officer at Aerolib Healthcare Solutions – what hospitalists can do to prevent clinical denials. The experts had the following five recommendations:
1. “THINK IN INK.”
The best tool in combating denials is well-documented clinical judgment that outlines:
- WHY the patient requires hospitalization, based on severity of presenting signs and symptoms, comorbidities, and risk of complications.
- WHAT the plan of care is, including diagnostic tests and/or interventions.
- HOW LONG you anticipate the patient will be in the hospital, including potential implications of social determinants (for example homelessness, active drug use) on discharge planning.
2. MASTER THE TWO-MIDNIGHT RULE.
If you expect that a Medicare Part A patient will require two or more midnights in the hospital, document it in the history and physical along with supporting clinical reasoning and sign an inpatient order. If the patient is discharged prior to the second midnight, document the reason in the progress notes and the discharge summary (for example, death, transfer to another hospital, departure against medical advice, faster than expected clinical improvement, or election of hospice in lieu of continued treatment in the hospital). Remember that Medicare Advantage plans may not follow the Two-Midnight rule and instead may use MCG guidelines, InterQual®, or internal criteria.
3. KNOW “SLAM DUNK” MCG CRITERIA FOR TOP DIAGNOSES.
Most large private payers utilize MCG guidelines to determine medical necessity for hospital admissions. Those guidelines are complex and change every year, and it is not required for hospitalists to know them all. However, it might help to remember a few key inpatient admission criteria for the top 5 to 10 diagnoses, such as:
- First episode of heart failure without prior history.
- Upper gastrointestinal bleeding with liver cirrhosis, syncope, or orthostatic hypotension.
- Pneumonia with documented hypoxia, outpatient treatment failure, pneumonia severity index (PSI) class 4 or 5, or CURB-65 score of 3 or greater.
- Cellulitis with outpatient treatment failure or high-risk comorbid conditions (cirrhosis, symptomatic heart failure, immunosuppression, or HbA1c greater than 10%).
4. EACH DAY, DEFEND WHY THE PATIENT NEEDS TO BE IN THE HOSPITAL.
Don’t let your progress notes be swallowed by a “copy-forward” monster and instead provide daily updates, such as:
- Up-to-date clinical status and response to interventions (for example, oxygenation or pain level).
- Updated plan of care: current interventions, additional diagnostic workup, or changes to the intensity of care (for example, increased intravenous pain medication dose or frequency).
- Why the patient cannot be safely discharged to a lower level of care (for example, a skilled nursing facility or home).
5. WORK WITH YOUR UTILIZATION REVIEW NURSES AND PHYSICIAN ADVISORS.
In the end, the two most powerful tools in combating clinical denials for hospital services are good medicine and clear documentation. Armed with an understanding of health care reimbursement and denial prevention, hospitalists can help their hospitals prevent unnecessary clinical denials and receive the reimbursements they deserve.”
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. LaPointe J. $262B of Total Hospital Charges in 2016 Initially Claim Denials. RevCycle Intelligence. 2017 June 26.
2. The Advisory Board. An ounce of prevention pays off: 90% of denials are preventable. 2014 Dec 11. [www.advisory.com/research/revenue-cycle-advancement-center/at-the-margins/2014/12/denials-management]
3. Centers for Medicare & Medicaid Services, Office of the Actuary, National Health Statistics Group. The Nation’s Health Dollar: Where It Came From, Where It Went. [www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf]
4. National Association of Insurance Commissioners. 2018 Market Share Reports. [www.naic.org/prod_serv/MSR-HB-19.pdf]
5. Centers for Medicare & Medicaid Services. Transforming the Healthcare System through Competition and Innovation. 2019 Nov. [www.cms.gov/files/document/cms-financial-report-fiscal-year-2019.pdf]
6. Centers for Medicare & Medicaid Services. MS-DRG Classifications and Software. 2020 Oct. [www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software]
7. Centers for Medicare & Medicaid Services. HCPCS Coding Questions. 2020 Feb. [www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/HCPCS_Coding_Questions]
8. Healthinsurance.org. Health insurance and Obamacare terms. [www.healthinsurance.org/glossary/denial-of-claim/]
9. The Advisory Board. Latest Trends in Hospital Revenue Cycle Performance. 2017. [mahamweb.org/images/meeting/112817/maham_2017__latest_trends_in_hospital_rev_cycle_performance_abc.pdf]
10. Centers for Medicare & Medicaid Services. Medicare Program Integrity Manual. Chapter 6: Medicare Contractor Medical Review Guidelines for Specific Services. 2020 July. [www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/pim83c06.pdf]
11. MCG Health. Industry-Leading Evidence-Based Care Guidelines. [www.mcg.com/care-guidelines/care-guidelines/]
12. Change Healthcare. What Is InterQual? [www.changehealthcare.com/solutions/clinical-decision-support/interqual]
Under a fee-for-service payment model, health care providers get paid by private and public payers for patient services such as physician visits, hospital stays, procedures, and tests. In an ideal world, providers would receive accurate, complete, and timely reimbursements. Unfortunately, the reality is far from ideal, where payment denials and delays are a common occurrence.
According to one study, out of $3 trillion in total claims submitted by health care organizations, an estimated 9% of charges ($262 billion), were initially denied.1 The good news is that 90% of all denials are preventable, and two-thirds of those preventable denials can be successfully appealed.2
Hospitalists are essential in preventing denials for hospital services and should be familiar with the basics of health care reimbursement and common reasons for denials. In this article we will provide an overview of the U.S. health care payment system, revenue cycle management and types of denials, and focus on the role of physician advisors and hospitalists in preventing and combating denials.
Overview of the U.S. health care payment system
In 2018 alone, the U.S. spent $3.6 trillion on health care. Of those dollars, 33% went to payments for hospital care and 20% went to physician and clinical services.3 So where do the nation’s health care dollars come from?
The United States has a complex multiple-payer system that includes private insurance companies and public payers funded by the federal and state governments, such as Medicare and Medicaid. Per the National Association of Insurance Commissioners’ 2018 Market Share Reports, there are 125 private accident and health insurance companies in the U.S., with the top five – UnitedHealth, Kaiser, Anthem, Humana, and CVS – holding a cumulative market share of almost 40%.4
Medicare accounts for 15% of federal budget spending and provides insurance coverage to almost 60 million people who are 65 and older, have end-stage renal disease, or have been approved for Social Security disability insurance benefits.5 Medicare Part A covers hospital, skilled nursing facility, home health, and hospice care. For example, for inpatient stays, Medicare Part A pays hospitals a predetermined rate per discharge according to the Medicare Severity Diagnosis Related Groups (MS-DRGs), which are based on the principal and secondary diagnoses, and performed procedures.6
Medicare Part B covers physician services and outpatient services and supplies, including labs and durable medical equipment, which are paid based on submitted Healthcare Common Procedure Coding System (HCPCS) codes.7 It is important to know that hospital observation stays are considered outpatient services, and are paid by Medicare Part B. Outpatient stays often are reimbursed at a lower rate than inpatient admissions, even in cases with similar utilization of hospital resources.
Medicaid is jointly funded by the states and the federal government and offers insurance coverage to more than 75 million eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. Over 10 million people are dually eligible for both Medicare and Medicaid.5 Increasingly, government payers, both state and federal, are contracting with private insurance companies to deliver Medicare and Medicaid services, also known as Medicare Advantage and Managed Medicaid Plans.
According to the U.S. Department of Treasury, in the 2019 fiscal year (October 2018 to September 2019), 33% of the nation’s health care dollars came from private insurance, 21% from Medicare, 16% from Medicaid, 15% from other government programs (for example, Veteran Affairs), 10% from out-of-pocket, and 4% from other private sources.5
Understanding revenue cycle management and denials
Providers, such as physicians or hospitals, submit claims to insurance companies that include, among other information, patient demographics and insurance, diagnoses, MS-DRGs and/or HCPCS codes, and charges. Revenue cycle management’s goal is to receive accurate, complete, and timely reimbursement for provided patient services, which is a complex and resource-intensive process.
According to the Healthcare Financial Management Association (HFMA), revenue cycle management includes “all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue.” These functions could be broken down into four main categories:
- Claims preparation (for example, patient registration, insurance eligibility, benefit verifications, and preauthorization).
- Claims submission (for example, charge capture, medical coding based on medical record documentation and claims transmission).
- Claims management (for example, payment posting, denial management, and patient collections).
- Reporting and analysis.
Claim denial is “the refusal of an insurance company or carrier to honor a request by an individual (or his or her provider) to pay for health care services obtained from a health care professional.”8 Payers can deny an entire claim or provide only a partial payment. Initial denial rate is tracked at the claim level (number of claims denied/number of claims submitted) and at the dollar level (total dollar amount of claims denied/total dollar amount of claims submitted).
Denials are classified as hard versus soft, and clinical versus technical or administrative:
- Hard denials result in lost revenue unless successfully appealed (for example, lack of medical necessity).
- Soft denials do not require appeal and may be paid if a provider corrects the claim or submits additional information (for example, missing or inaccurate patient information, and missing medical records).
- Clinical denials are based on medical necessity, including level of care determination (for example, inpatient versus outpatient) and length of stay. They can be concurrent and retrospective and typically start as soft denials.
- Technical or administrative denials are based on reasons other than clinical (for example, failure to preauthorize care or lack of benefits).
According to the Advisory Board’s 2017 survey of hospitals and health care systems, 50% of initial denials were technical/demographic errors, 20% medical necessity, 16% eligibility, and 14% authorization. Forty seven percent of those denials came from commercial payers, 33% from Medicare/Medicare Advantage, 17% from Medicaid, and 3% from other payers.9
Determination of medical necessity may vary by payer. As an example, let’s look at inpatient admissions. According to the Medicare Two-Midnight Rule, inpatient admission is appropriate “if the admitting practitioner expects the beneficiary to require medically necessary hospital care spanning two or more midnights, and such reasonable expectation is supported by the medical record documentation.”10
Medicare guidelines acknowledge that a physician’s decision to admit a patient is based on complex medical factors including, but not limited to:
- The beneficiary history and comorbidities, and the severity of signs and symptoms (also known as Severity of Illness or SI).
- Current medical needs (also known as Intensity of Service or IS).
- The risk of an adverse event.
Generally, private payers do not follow the Two-Midnight Rule, and instead utilize evidence-based MCG guidelines,11 InterQual® criteria12 or internal criteria to determine if an inpatient admission is “medically necessary.” Hospital utilization review nurses often use MCG and/or InterQual® to aid admission status decisions and may request secondary review by a physician if medical necessity for an inpatient admission is not clear-cut.
The role of physician advisors
Considering the rising financial pressure and growing complexity of private and public payers’ rules and regulations, many hospitals turned to physician advisors to help prevent and reduce denials. Typically, physician advisors perform concurrent secondary reviews to help determine the most appropriate level of care, participate in peer-to-peer discussions with payers, and write formal appeals to overturn clinical denials.
“Physician advisors are generally not in the business of critiquing clinical practice, instead they review whether the chart documentation supports initial and continued hospitalization,” said Charles Locke, MD, senior physician advisor at the Johns Hopkins Hospital and president of the American College of Physician Advisors (ACPA). “However, physician advisors should seek additional information and provide feedback in those cases where the documentation does not support medical necessity for hospitalization.”
Many physician advisors are current or former hospitalists. Chris Shearer, MD, chief medical officer for remote advisory at Sound Physicians Advisory Services, says that “hospitalists are the natural physician advisors as they have a working knowledge of what patients need to be inpatients and which are less sick and likely to be discharged quickly.”
The role of physician advisors extends beyond reviews to include physician engagement and education. Physician advisors are a critical link between physicians, utilization review nurses, case managers, and clinical documentation integrity (CDI) and revenue cycle teams, and are increasingly involved in hospital-wide denial prevention efforts.
Physician advisors are invaluable in identifying and validating root causes for clinical denials and generating potential solutions, as they bring to the table:
- Clinical expertise.
- Understanding of clinical workflows.
- Knowledge of the most current public and private payers’ regulations.
- Insight into hospital-specific clinical documentation opportunities (for example, by diagnosis, procedure, service line, and provider).
- Understanding of payers’ reasons for clinical denials through peer-to-peer discussions
The role of hospitalists in preventing clinical denials
I asked three experienced physician advisors – Dr. Locke, Dr. Shearer, and Deepak Pahuja, MD, chief medical officer at Aerolib Healthcare Solutions – what hospitalists can do to prevent clinical denials. The experts had the following five recommendations:
1. “THINK IN INK.”
The best tool in combating denials is well-documented clinical judgment that outlines:
- WHY the patient requires hospitalization, based on severity of presenting signs and symptoms, comorbidities, and risk of complications.
- WHAT the plan of care is, including diagnostic tests and/or interventions.
- HOW LONG you anticipate the patient will be in the hospital, including potential implications of social determinants (for example homelessness, active drug use) on discharge planning.
2. MASTER THE TWO-MIDNIGHT RULE.
If you expect that a Medicare Part A patient will require two or more midnights in the hospital, document it in the history and physical along with supporting clinical reasoning and sign an inpatient order. If the patient is discharged prior to the second midnight, document the reason in the progress notes and the discharge summary (for example, death, transfer to another hospital, departure against medical advice, faster than expected clinical improvement, or election of hospice in lieu of continued treatment in the hospital). Remember that Medicare Advantage plans may not follow the Two-Midnight rule and instead may use MCG guidelines, InterQual®, or internal criteria.
3. KNOW “SLAM DUNK” MCG CRITERIA FOR TOP DIAGNOSES.
Most large private payers utilize MCG guidelines to determine medical necessity for hospital admissions. Those guidelines are complex and change every year, and it is not required for hospitalists to know them all. However, it might help to remember a few key inpatient admission criteria for the top 5 to 10 diagnoses, such as:
- First episode of heart failure without prior history.
- Upper gastrointestinal bleeding with liver cirrhosis, syncope, or orthostatic hypotension.
- Pneumonia with documented hypoxia, outpatient treatment failure, pneumonia severity index (PSI) class 4 or 5, or CURB-65 score of 3 or greater.
- Cellulitis with outpatient treatment failure or high-risk comorbid conditions (cirrhosis, symptomatic heart failure, immunosuppression, or HbA1c greater than 10%).
4. EACH DAY, DEFEND WHY THE PATIENT NEEDS TO BE IN THE HOSPITAL.
Don’t let your progress notes be swallowed by a “copy-forward” monster and instead provide daily updates, such as:
- Up-to-date clinical status and response to interventions (for example, oxygenation or pain level).
- Updated plan of care: current interventions, additional diagnostic workup, or changes to the intensity of care (for example, increased intravenous pain medication dose or frequency).
- Why the patient cannot be safely discharged to a lower level of care (for example, a skilled nursing facility or home).
5. WORK WITH YOUR UTILIZATION REVIEW NURSES AND PHYSICIAN ADVISORS.
In the end, the two most powerful tools in combating clinical denials for hospital services are good medicine and clear documentation. Armed with an understanding of health care reimbursement and denial prevention, hospitalists can help their hospitals prevent unnecessary clinical denials and receive the reimbursements they deserve.”
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. LaPointe J. $262B of Total Hospital Charges in 2016 Initially Claim Denials. RevCycle Intelligence. 2017 June 26.
2. The Advisory Board. An ounce of prevention pays off: 90% of denials are preventable. 2014 Dec 11. [www.advisory.com/research/revenue-cycle-advancement-center/at-the-margins/2014/12/denials-management]
3. Centers for Medicare & Medicaid Services, Office of the Actuary, National Health Statistics Group. The Nation’s Health Dollar: Where It Came From, Where It Went. [www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf]
4. National Association of Insurance Commissioners. 2018 Market Share Reports. [www.naic.org/prod_serv/MSR-HB-19.pdf]
5. Centers for Medicare & Medicaid Services. Transforming the Healthcare System through Competition and Innovation. 2019 Nov. [www.cms.gov/files/document/cms-financial-report-fiscal-year-2019.pdf]
6. Centers for Medicare & Medicaid Services. MS-DRG Classifications and Software. 2020 Oct. [www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software]
7. Centers for Medicare & Medicaid Services. HCPCS Coding Questions. 2020 Feb. [www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/HCPCS_Coding_Questions]
8. Healthinsurance.org. Health insurance and Obamacare terms. [www.healthinsurance.org/glossary/denial-of-claim/]
9. The Advisory Board. Latest Trends in Hospital Revenue Cycle Performance. 2017. [mahamweb.org/images/meeting/112817/maham_2017__latest_trends_in_hospital_rev_cycle_performance_abc.pdf]
10. Centers for Medicare & Medicaid Services. Medicare Program Integrity Manual. Chapter 6: Medicare Contractor Medical Review Guidelines for Specific Services. 2020 July. [www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/pim83c06.pdf]
11. MCG Health. Industry-Leading Evidence-Based Care Guidelines. [www.mcg.com/care-guidelines/care-guidelines/]
12. Change Healthcare. What Is InterQual? [www.changehealthcare.com/solutions/clinical-decision-support/interqual]
Under a fee-for-service payment model, health care providers get paid by private and public payers for patient services such as physician visits, hospital stays, procedures, and tests. In an ideal world, providers would receive accurate, complete, and timely reimbursements. Unfortunately, the reality is far from ideal, where payment denials and delays are a common occurrence.
According to one study, out of $3 trillion in total claims submitted by health care organizations, an estimated 9% of charges ($262 billion), were initially denied.1 The good news is that 90% of all denials are preventable, and two-thirds of those preventable denials can be successfully appealed.2
Hospitalists are essential in preventing denials for hospital services and should be familiar with the basics of health care reimbursement and common reasons for denials. In this article we will provide an overview of the U.S. health care payment system, revenue cycle management and types of denials, and focus on the role of physician advisors and hospitalists in preventing and combating denials.
Overview of the U.S. health care payment system
In 2018 alone, the U.S. spent $3.6 trillion on health care. Of those dollars, 33% went to payments for hospital care and 20% went to physician and clinical services.3 So where do the nation’s health care dollars come from?
The United States has a complex multiple-payer system that includes private insurance companies and public payers funded by the federal and state governments, such as Medicare and Medicaid. Per the National Association of Insurance Commissioners’ 2018 Market Share Reports, there are 125 private accident and health insurance companies in the U.S., with the top five – UnitedHealth, Kaiser, Anthem, Humana, and CVS – holding a cumulative market share of almost 40%.4
Medicare accounts for 15% of federal budget spending and provides insurance coverage to almost 60 million people who are 65 and older, have end-stage renal disease, or have been approved for Social Security disability insurance benefits.5 Medicare Part A covers hospital, skilled nursing facility, home health, and hospice care. For example, for inpatient stays, Medicare Part A pays hospitals a predetermined rate per discharge according to the Medicare Severity Diagnosis Related Groups (MS-DRGs), which are based on the principal and secondary diagnoses, and performed procedures.6
Medicare Part B covers physician services and outpatient services and supplies, including labs and durable medical equipment, which are paid based on submitted Healthcare Common Procedure Coding System (HCPCS) codes.7 It is important to know that hospital observation stays are considered outpatient services, and are paid by Medicare Part B. Outpatient stays often are reimbursed at a lower rate than inpatient admissions, even in cases with similar utilization of hospital resources.
Medicaid is jointly funded by the states and the federal government and offers insurance coverage to more than 75 million eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. Over 10 million people are dually eligible for both Medicare and Medicaid.5 Increasingly, government payers, both state and federal, are contracting with private insurance companies to deliver Medicare and Medicaid services, also known as Medicare Advantage and Managed Medicaid Plans.
According to the U.S. Department of Treasury, in the 2019 fiscal year (October 2018 to September 2019), 33% of the nation’s health care dollars came from private insurance, 21% from Medicare, 16% from Medicaid, 15% from other government programs (for example, Veteran Affairs), 10% from out-of-pocket, and 4% from other private sources.5
Understanding revenue cycle management and denials
Providers, such as physicians or hospitals, submit claims to insurance companies that include, among other information, patient demographics and insurance, diagnoses, MS-DRGs and/or HCPCS codes, and charges. Revenue cycle management’s goal is to receive accurate, complete, and timely reimbursement for provided patient services, which is a complex and resource-intensive process.
According to the Healthcare Financial Management Association (HFMA), revenue cycle management includes “all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue.” These functions could be broken down into four main categories:
- Claims preparation (for example, patient registration, insurance eligibility, benefit verifications, and preauthorization).
- Claims submission (for example, charge capture, medical coding based on medical record documentation and claims transmission).
- Claims management (for example, payment posting, denial management, and patient collections).
- Reporting and analysis.
Claim denial is “the refusal of an insurance company or carrier to honor a request by an individual (or his or her provider) to pay for health care services obtained from a health care professional.”8 Payers can deny an entire claim or provide only a partial payment. Initial denial rate is tracked at the claim level (number of claims denied/number of claims submitted) and at the dollar level (total dollar amount of claims denied/total dollar amount of claims submitted).
Denials are classified as hard versus soft, and clinical versus technical or administrative:
- Hard denials result in lost revenue unless successfully appealed (for example, lack of medical necessity).
- Soft denials do not require appeal and may be paid if a provider corrects the claim or submits additional information (for example, missing or inaccurate patient information, and missing medical records).
- Clinical denials are based on medical necessity, including level of care determination (for example, inpatient versus outpatient) and length of stay. They can be concurrent and retrospective and typically start as soft denials.
- Technical or administrative denials are based on reasons other than clinical (for example, failure to preauthorize care or lack of benefits).
According to the Advisory Board’s 2017 survey of hospitals and health care systems, 50% of initial denials were technical/demographic errors, 20% medical necessity, 16% eligibility, and 14% authorization. Forty seven percent of those denials came from commercial payers, 33% from Medicare/Medicare Advantage, 17% from Medicaid, and 3% from other payers.9
Determination of medical necessity may vary by payer. As an example, let’s look at inpatient admissions. According to the Medicare Two-Midnight Rule, inpatient admission is appropriate “if the admitting practitioner expects the beneficiary to require medically necessary hospital care spanning two or more midnights, and such reasonable expectation is supported by the medical record documentation.”10
Medicare guidelines acknowledge that a physician’s decision to admit a patient is based on complex medical factors including, but not limited to:
- The beneficiary history and comorbidities, and the severity of signs and symptoms (also known as Severity of Illness or SI).
- Current medical needs (also known as Intensity of Service or IS).
- The risk of an adverse event.
Generally, private payers do not follow the Two-Midnight Rule, and instead utilize evidence-based MCG guidelines,11 InterQual® criteria12 or internal criteria to determine if an inpatient admission is “medically necessary.” Hospital utilization review nurses often use MCG and/or InterQual® to aid admission status decisions and may request secondary review by a physician if medical necessity for an inpatient admission is not clear-cut.
The role of physician advisors
Considering the rising financial pressure and growing complexity of private and public payers’ rules and regulations, many hospitals turned to physician advisors to help prevent and reduce denials. Typically, physician advisors perform concurrent secondary reviews to help determine the most appropriate level of care, participate in peer-to-peer discussions with payers, and write formal appeals to overturn clinical denials.
“Physician advisors are generally not in the business of critiquing clinical practice, instead they review whether the chart documentation supports initial and continued hospitalization,” said Charles Locke, MD, senior physician advisor at the Johns Hopkins Hospital and president of the American College of Physician Advisors (ACPA). “However, physician advisors should seek additional information and provide feedback in those cases where the documentation does not support medical necessity for hospitalization.”
Many physician advisors are current or former hospitalists. Chris Shearer, MD, chief medical officer for remote advisory at Sound Physicians Advisory Services, says that “hospitalists are the natural physician advisors as they have a working knowledge of what patients need to be inpatients and which are less sick and likely to be discharged quickly.”
The role of physician advisors extends beyond reviews to include physician engagement and education. Physician advisors are a critical link between physicians, utilization review nurses, case managers, and clinical documentation integrity (CDI) and revenue cycle teams, and are increasingly involved in hospital-wide denial prevention efforts.
Physician advisors are invaluable in identifying and validating root causes for clinical denials and generating potential solutions, as they bring to the table:
- Clinical expertise.
- Understanding of clinical workflows.
- Knowledge of the most current public and private payers’ regulations.
- Insight into hospital-specific clinical documentation opportunities (for example, by diagnosis, procedure, service line, and provider).
- Understanding of payers’ reasons for clinical denials through peer-to-peer discussions
The role of hospitalists in preventing clinical denials
I asked three experienced physician advisors – Dr. Locke, Dr. Shearer, and Deepak Pahuja, MD, chief medical officer at Aerolib Healthcare Solutions – what hospitalists can do to prevent clinical denials. The experts had the following five recommendations:
1. “THINK IN INK.”
The best tool in combating denials is well-documented clinical judgment that outlines:
- WHY the patient requires hospitalization, based on severity of presenting signs and symptoms, comorbidities, and risk of complications.
- WHAT the plan of care is, including diagnostic tests and/or interventions.
- HOW LONG you anticipate the patient will be in the hospital, including potential implications of social determinants (for example homelessness, active drug use) on discharge planning.
2. MASTER THE TWO-MIDNIGHT RULE.
If you expect that a Medicare Part A patient will require two or more midnights in the hospital, document it in the history and physical along with supporting clinical reasoning and sign an inpatient order. If the patient is discharged prior to the second midnight, document the reason in the progress notes and the discharge summary (for example, death, transfer to another hospital, departure against medical advice, faster than expected clinical improvement, or election of hospice in lieu of continued treatment in the hospital). Remember that Medicare Advantage plans may not follow the Two-Midnight rule and instead may use MCG guidelines, InterQual®, or internal criteria.
3. KNOW “SLAM DUNK” MCG CRITERIA FOR TOP DIAGNOSES.
Most large private payers utilize MCG guidelines to determine medical necessity for hospital admissions. Those guidelines are complex and change every year, and it is not required for hospitalists to know them all. However, it might help to remember a few key inpatient admission criteria for the top 5 to 10 diagnoses, such as:
- First episode of heart failure without prior history.
- Upper gastrointestinal bleeding with liver cirrhosis, syncope, or orthostatic hypotension.
- Pneumonia with documented hypoxia, outpatient treatment failure, pneumonia severity index (PSI) class 4 or 5, or CURB-65 score of 3 or greater.
- Cellulitis with outpatient treatment failure or high-risk comorbid conditions (cirrhosis, symptomatic heart failure, immunosuppression, or HbA1c greater than 10%).
4. EACH DAY, DEFEND WHY THE PATIENT NEEDS TO BE IN THE HOSPITAL.
Don’t let your progress notes be swallowed by a “copy-forward” monster and instead provide daily updates, such as:
- Up-to-date clinical status and response to interventions (for example, oxygenation or pain level).
- Updated plan of care: current interventions, additional diagnostic workup, or changes to the intensity of care (for example, increased intravenous pain medication dose or frequency).
- Why the patient cannot be safely discharged to a lower level of care (for example, a skilled nursing facility or home).
5. WORK WITH YOUR UTILIZATION REVIEW NURSES AND PHYSICIAN ADVISORS.
In the end, the two most powerful tools in combating clinical denials for hospital services are good medicine and clear documentation. Armed with an understanding of health care reimbursement and denial prevention, hospitalists can help their hospitals prevent unnecessary clinical denials and receive the reimbursements they deserve.”
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. LaPointe J. $262B of Total Hospital Charges in 2016 Initially Claim Denials. RevCycle Intelligence. 2017 June 26.
2. The Advisory Board. An ounce of prevention pays off: 90% of denials are preventable. 2014 Dec 11. [www.advisory.com/research/revenue-cycle-advancement-center/at-the-margins/2014/12/denials-management]
3. Centers for Medicare & Medicaid Services, Office of the Actuary, National Health Statistics Group. The Nation’s Health Dollar: Where It Came From, Where It Went. [www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf]
4. National Association of Insurance Commissioners. 2018 Market Share Reports. [www.naic.org/prod_serv/MSR-HB-19.pdf]
5. Centers for Medicare & Medicaid Services. Transforming the Healthcare System through Competition and Innovation. 2019 Nov. [www.cms.gov/files/document/cms-financial-report-fiscal-year-2019.pdf]
6. Centers for Medicare & Medicaid Services. MS-DRG Classifications and Software. 2020 Oct. [www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software]
7. Centers for Medicare & Medicaid Services. HCPCS Coding Questions. 2020 Feb. [www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/HCPCS_Coding_Questions]
8. Healthinsurance.org. Health insurance and Obamacare terms. [www.healthinsurance.org/glossary/denial-of-claim/]
9. The Advisory Board. Latest Trends in Hospital Revenue Cycle Performance. 2017. [mahamweb.org/images/meeting/112817/maham_2017__latest_trends_in_hospital_rev_cycle_performance_abc.pdf]
10. Centers for Medicare & Medicaid Services. Medicare Program Integrity Manual. Chapter 6: Medicare Contractor Medical Review Guidelines for Specific Services. 2020 July. [www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/pim83c06.pdf]
11. MCG Health. Industry-Leading Evidence-Based Care Guidelines. [www.mcg.com/care-guidelines/care-guidelines/]
12. Change Healthcare. What Is InterQual? [www.changehealthcare.com/solutions/clinical-decision-support/interqual]
COVID-19: Telehealth at the forefront of the pandemic
On Jan. 20, 2020, the first confirmed case of the 2019 novel coronavirus in the United States was admitted to Providence Regional Medical Center in Everett, Wash. Less than 3 months later, the COVID-19 pandemic has put enormous stress on the U.S. health care system, which is confronting acute resource shortage because of the surge of acute and critically ill patients, health care provider safety and burnout, and an ongoing need for managing vulnerable populations while minimizing the infection spread.
With the onset of these unprecedented challenges, telehealth has emerged as a powerful new resource for health care providers, hospitals, and health care systems across the country. This article offers a summary of government regulations that enabled telehealth expansion, and provides an overview of how two health care organizations, Providence St. Joseph Health and Sound Physicians, are employing telehealth services to combat the COVID-19 health care crisis.
The government response: Telehealth expansion
In response to the pandemic, the Centers for Medicare and Medicaid Services (CMS) have significantly increased access to telehealth services for Medicare and Medicaid beneficiaries. CMS swiftly put measures in place such as:
- Expanding telehealth beyond rural areas.
- Adding 80 services that can be provided in all settings, including patient homes
- Allowing providers to bill for telehealth visits at the same rate as in-person visits.
The U.S. Department of Health and Human Services also aided this effort by:
- Waiving requirements that physicians or other health care professionals must have licenses in the state in which they provide services, if they have an equivalent license from another state.
- Waving penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype
Without prior regulatory and reimbursement restrictions, telehealth rapidly became a powerful tool in helping to solve some of the problems brought about by the COVID-19 pandemic.
Providence Telehealth for COVID-19
Providence St. Joseph Health is a not-for-profit health care system operating 51 hospitals and 1,085 clinics across Alaska, California, Montana, New Mexico, Oregon, Texas, and Washington. Providence has developed an enterprise telemedicine network with more than 100 virtual programs. Several of these services – including Telestroke, Telepsychiatry, TeleICU, and Telehospitalist – have been scaled across several states as a clinical cloud. More than 400 telemedicine endpoints are deployed, such as robotic carts and fixed InTouch TVs. In fact, the first U.S. COVID-19 patient was treated at Providence Regional Medical Center in Everett, Wash., using the telemedical robot Vici from InTouch Health.
According to Todd Czartoski, MD, chief medical technology officer at Providence, “while telehealth has been around for many years, COVID-19 opened a lot of people’s eyes to the value of virtual care delivery.”
Providence’s telehealth response to COVID-19 has encompassed five main areas: COVID-19 home care, COVID-19 acute care, ambulatory virtual visits, behavioral health concierge (BHC) expansion, and additional support for outside partnerships.
COVID-19 Home Care
Providence rapidly deployed home monitoring for nearly 2,000 positive or presumptive COVID-19 patients. Those symptomatic, clinically stable patients are given a thermometer and a pulse oximeter, and are monitored from home by a central team of nurses and physicians using the Xealth and Twistle programs.
Providence is evaluating expansion of home monitoring to other diagnoses, including higher acuity conditions.
COVID-19 Acute Care
TeleTriage expedites the triage of suspected COVID-19 patients and reduces the use of personal protective equipment (PPE) by 50% per patient per day. To date, TeleTriage has resulted in the conservation of more than 90,000 PPE units.
TeleHospitalist services expanded from traditional night coverage to caring for patients in COVID-19 units around the clock. Currently, there are 25 telehospitalists who practice both in-person and virtual medicine.
TeleICU offers remote management of more than 180 ICU beds across 17 hospitals from two central command centers in Washington state and Alaska. The services include night-time intensivist and ICU nurse coverage, including medication and ventilator management, and family conferences. COVID-19 increased the demand for TeleICU, with anticipated expansion to more than 300 beds.
Core TeleSpecialty services include TeleStroke and TelePsychiatry across 135 remote sites.
Ambulatory Virtual Visits
Providence launched the COVID-19 hub microsite to help educate patients by providing accurate and timely information. A chatbot named Grace helps screen patients who are worried about COVID-19. Grace also suggests next steps, such as a video visit with a patient’s primary care provider or a visit using Express Care/Virtual team, a direct-to-consumer service available to patients within and outside of the health care system.
In less than 2 weeks, Providence enabled virtual visits for more than 7,000 outpatient providers, with more than 14,000 alternative visits now occurring daily. This has allowed primary and specialty providers to continue to manage their patient panels remotely. The number of Express Care/Virtual visits increased from 60 to more than 1,000 per day.
BHC Expansion
In the effort to improve care for its caregivers, Providence launched a behavioral health concierge (BHC) service that offers employees and their dependents virtual access to licensed mental health professionals. Over the last half of 2019, BHC provided more than 1,000 phone and virtual visits, depending on the individual preference of patients. Notably, 21% percent of users were physicians; 65% of users were seen the same day and 100% of users were seen within 48 hours.
COVID-19 increased demand for services that initially started in Seattle and rapidly expanded to Montana, Oregon, and California.
Outside Partnerships
Providence has established partnerships with outside facilities by providing services to 135 sites across eight states. COVID-19 accelerated the employment of new services, including TeleICU.
Telemedicine at Sound Physicians
Sound Physicians is a national physician-founded and -led organization that provides emergency medicine, critical care, hospital medicine, population health, and physician advisory services. Five years ago, Sound launched a telemedicine service line. I spoke with Brian Carpenter, MD, national medical director for TeleHospitalist Services at Sound, to learn about his experience implementing Telehospitalist programs across 22 hospitals and 22 skilled nursing facilities.
Prior to COVID-19, Sound offered a spectrum of telemedicine services including night-time telephonic cross coverage, as well as video-assisted admissions, transfers, and rapid responses. In 2019, Sound Telehospitalists received 88,000 connect requests, including 6,400 video-assisted new admissions and 82 rapid responses. Typically, one physician covers four to eight hospitals with back-up available for surges. The team uses a predictive model for staffing and developed an acuity-based algorithm to ensure that patients in distress are evaluated immediately, new stable admissions on average are seen within 12 minutes, and order clarifications are provided within 30 minutes.
The COVID-19 pandemic created an urgent demand for providers to support an overwhelmed health care system. Without the traditional barriers to implementation – such as lack of acceptance by medical staff, nurses and patients, strict state licensing and technology requirements, lack of reimbursement, and delays in hospital credentialing – Sound was able to develop a rapid implementation model for telemedicine services. Currently, four new hospitals are in the active implementation phase, with 40 more hospitals in the pipeline.
Implementing a telemedicine program at your hospital
In order to successfully launch a telemedicine program, Dr. Carpenter outlined the following critical implementation steps:
- In collaboration with local leadership, define the problem you are trying to solve, which helps inform the scope of the telemedicine practice and technology requirements (for example, night-time cross-coverage vs. full telemedicine service).
- Complete a discovery process (for example, existing workflow for patient admission and transfer) with the end-goal of developing a workflow and rules of engagement.
- Obtain hospital credentialing/privileges and EMR access.
- Train end-users, including physicians and nurse telepresenters.
Dr. Carpenter offered this advice to those considering a telemedicine program: “Telemedicine is not just about technology; a true telemedicine program encompasses change management, workflow development, end-user training, compliance, and mechanisms for continuous process improvement. We want to make things better for the physicians, nurses, and patients.”
Telehealth is offering support to health care providers on the front lines, patients in need of care, and health care systems managing the unprecedented surges in volume.
Dr. Farah is a hospitalist, physician adviser, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
On Jan. 20, 2020, the first confirmed case of the 2019 novel coronavirus in the United States was admitted to Providence Regional Medical Center in Everett, Wash. Less than 3 months later, the COVID-19 pandemic has put enormous stress on the U.S. health care system, which is confronting acute resource shortage because of the surge of acute and critically ill patients, health care provider safety and burnout, and an ongoing need for managing vulnerable populations while minimizing the infection spread.
With the onset of these unprecedented challenges, telehealth has emerged as a powerful new resource for health care providers, hospitals, and health care systems across the country. This article offers a summary of government regulations that enabled telehealth expansion, and provides an overview of how two health care organizations, Providence St. Joseph Health and Sound Physicians, are employing telehealth services to combat the COVID-19 health care crisis.
The government response: Telehealth expansion
In response to the pandemic, the Centers for Medicare and Medicaid Services (CMS) have significantly increased access to telehealth services for Medicare and Medicaid beneficiaries. CMS swiftly put measures in place such as:
- Expanding telehealth beyond rural areas.
- Adding 80 services that can be provided in all settings, including patient homes
- Allowing providers to bill for telehealth visits at the same rate as in-person visits.
The U.S. Department of Health and Human Services also aided this effort by:
- Waiving requirements that physicians or other health care professionals must have licenses in the state in which they provide services, if they have an equivalent license from another state.
- Waving penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype
Without prior regulatory and reimbursement restrictions, telehealth rapidly became a powerful tool in helping to solve some of the problems brought about by the COVID-19 pandemic.
Providence Telehealth for COVID-19
Providence St. Joseph Health is a not-for-profit health care system operating 51 hospitals and 1,085 clinics across Alaska, California, Montana, New Mexico, Oregon, Texas, and Washington. Providence has developed an enterprise telemedicine network with more than 100 virtual programs. Several of these services – including Telestroke, Telepsychiatry, TeleICU, and Telehospitalist – have been scaled across several states as a clinical cloud. More than 400 telemedicine endpoints are deployed, such as robotic carts and fixed InTouch TVs. In fact, the first U.S. COVID-19 patient was treated at Providence Regional Medical Center in Everett, Wash., using the telemedical robot Vici from InTouch Health.
According to Todd Czartoski, MD, chief medical technology officer at Providence, “while telehealth has been around for many years, COVID-19 opened a lot of people’s eyes to the value of virtual care delivery.”
Providence’s telehealth response to COVID-19 has encompassed five main areas: COVID-19 home care, COVID-19 acute care, ambulatory virtual visits, behavioral health concierge (BHC) expansion, and additional support for outside partnerships.
COVID-19 Home Care
Providence rapidly deployed home monitoring for nearly 2,000 positive or presumptive COVID-19 patients. Those symptomatic, clinically stable patients are given a thermometer and a pulse oximeter, and are monitored from home by a central team of nurses and physicians using the Xealth and Twistle programs.
Providence is evaluating expansion of home monitoring to other diagnoses, including higher acuity conditions.
COVID-19 Acute Care
TeleTriage expedites the triage of suspected COVID-19 patients and reduces the use of personal protective equipment (PPE) by 50% per patient per day. To date, TeleTriage has resulted in the conservation of more than 90,000 PPE units.
TeleHospitalist services expanded from traditional night coverage to caring for patients in COVID-19 units around the clock. Currently, there are 25 telehospitalists who practice both in-person and virtual medicine.
TeleICU offers remote management of more than 180 ICU beds across 17 hospitals from two central command centers in Washington state and Alaska. The services include night-time intensivist and ICU nurse coverage, including medication and ventilator management, and family conferences. COVID-19 increased the demand for TeleICU, with anticipated expansion to more than 300 beds.
Core TeleSpecialty services include TeleStroke and TelePsychiatry across 135 remote sites.
Ambulatory Virtual Visits
Providence launched the COVID-19 hub microsite to help educate patients by providing accurate and timely information. A chatbot named Grace helps screen patients who are worried about COVID-19. Grace also suggests next steps, such as a video visit with a patient’s primary care provider or a visit using Express Care/Virtual team, a direct-to-consumer service available to patients within and outside of the health care system.
In less than 2 weeks, Providence enabled virtual visits for more than 7,000 outpatient providers, with more than 14,000 alternative visits now occurring daily. This has allowed primary and specialty providers to continue to manage their patient panels remotely. The number of Express Care/Virtual visits increased from 60 to more than 1,000 per day.
BHC Expansion
In the effort to improve care for its caregivers, Providence launched a behavioral health concierge (BHC) service that offers employees and their dependents virtual access to licensed mental health professionals. Over the last half of 2019, BHC provided more than 1,000 phone and virtual visits, depending on the individual preference of patients. Notably, 21% percent of users were physicians; 65% of users were seen the same day and 100% of users were seen within 48 hours.
COVID-19 increased demand for services that initially started in Seattle and rapidly expanded to Montana, Oregon, and California.
Outside Partnerships
Providence has established partnerships with outside facilities by providing services to 135 sites across eight states. COVID-19 accelerated the employment of new services, including TeleICU.
Telemedicine at Sound Physicians
Sound Physicians is a national physician-founded and -led organization that provides emergency medicine, critical care, hospital medicine, population health, and physician advisory services. Five years ago, Sound launched a telemedicine service line. I spoke with Brian Carpenter, MD, national medical director for TeleHospitalist Services at Sound, to learn about his experience implementing Telehospitalist programs across 22 hospitals and 22 skilled nursing facilities.
Prior to COVID-19, Sound offered a spectrum of telemedicine services including night-time telephonic cross coverage, as well as video-assisted admissions, transfers, and rapid responses. In 2019, Sound Telehospitalists received 88,000 connect requests, including 6,400 video-assisted new admissions and 82 rapid responses. Typically, one physician covers four to eight hospitals with back-up available for surges. The team uses a predictive model for staffing and developed an acuity-based algorithm to ensure that patients in distress are evaluated immediately, new stable admissions on average are seen within 12 minutes, and order clarifications are provided within 30 minutes.
The COVID-19 pandemic created an urgent demand for providers to support an overwhelmed health care system. Without the traditional barriers to implementation – such as lack of acceptance by medical staff, nurses and patients, strict state licensing and technology requirements, lack of reimbursement, and delays in hospital credentialing – Sound was able to develop a rapid implementation model for telemedicine services. Currently, four new hospitals are in the active implementation phase, with 40 more hospitals in the pipeline.
Implementing a telemedicine program at your hospital
In order to successfully launch a telemedicine program, Dr. Carpenter outlined the following critical implementation steps:
- In collaboration with local leadership, define the problem you are trying to solve, which helps inform the scope of the telemedicine practice and technology requirements (for example, night-time cross-coverage vs. full telemedicine service).
- Complete a discovery process (for example, existing workflow for patient admission and transfer) with the end-goal of developing a workflow and rules of engagement.
- Obtain hospital credentialing/privileges and EMR access.
- Train end-users, including physicians and nurse telepresenters.
Dr. Carpenter offered this advice to those considering a telemedicine program: “Telemedicine is not just about technology; a true telemedicine program encompasses change management, workflow development, end-user training, compliance, and mechanisms for continuous process improvement. We want to make things better for the physicians, nurses, and patients.”
Telehealth is offering support to health care providers on the front lines, patients in need of care, and health care systems managing the unprecedented surges in volume.
Dr. Farah is a hospitalist, physician adviser, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
On Jan. 20, 2020, the first confirmed case of the 2019 novel coronavirus in the United States was admitted to Providence Regional Medical Center in Everett, Wash. Less than 3 months later, the COVID-19 pandemic has put enormous stress on the U.S. health care system, which is confronting acute resource shortage because of the surge of acute and critically ill patients, health care provider safety and burnout, and an ongoing need for managing vulnerable populations while minimizing the infection spread.
With the onset of these unprecedented challenges, telehealth has emerged as a powerful new resource for health care providers, hospitals, and health care systems across the country. This article offers a summary of government regulations that enabled telehealth expansion, and provides an overview of how two health care organizations, Providence St. Joseph Health and Sound Physicians, are employing telehealth services to combat the COVID-19 health care crisis.
The government response: Telehealth expansion
In response to the pandemic, the Centers for Medicare and Medicaid Services (CMS) have significantly increased access to telehealth services for Medicare and Medicaid beneficiaries. CMS swiftly put measures in place such as:
- Expanding telehealth beyond rural areas.
- Adding 80 services that can be provided in all settings, including patient homes
- Allowing providers to bill for telehealth visits at the same rate as in-person visits.
The U.S. Department of Health and Human Services also aided this effort by:
- Waiving requirements that physicians or other health care professionals must have licenses in the state in which they provide services, if they have an equivalent license from another state.
- Waving penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype
Without prior regulatory and reimbursement restrictions, telehealth rapidly became a powerful tool in helping to solve some of the problems brought about by the COVID-19 pandemic.
Providence Telehealth for COVID-19
Providence St. Joseph Health is a not-for-profit health care system operating 51 hospitals and 1,085 clinics across Alaska, California, Montana, New Mexico, Oregon, Texas, and Washington. Providence has developed an enterprise telemedicine network with more than 100 virtual programs. Several of these services – including Telestroke, Telepsychiatry, TeleICU, and Telehospitalist – have been scaled across several states as a clinical cloud. More than 400 telemedicine endpoints are deployed, such as robotic carts and fixed InTouch TVs. In fact, the first U.S. COVID-19 patient was treated at Providence Regional Medical Center in Everett, Wash., using the telemedical robot Vici from InTouch Health.
According to Todd Czartoski, MD, chief medical technology officer at Providence, “while telehealth has been around for many years, COVID-19 opened a lot of people’s eyes to the value of virtual care delivery.”
Providence’s telehealth response to COVID-19 has encompassed five main areas: COVID-19 home care, COVID-19 acute care, ambulatory virtual visits, behavioral health concierge (BHC) expansion, and additional support for outside partnerships.
COVID-19 Home Care
Providence rapidly deployed home monitoring for nearly 2,000 positive or presumptive COVID-19 patients. Those symptomatic, clinically stable patients are given a thermometer and a pulse oximeter, and are monitored from home by a central team of nurses and physicians using the Xealth and Twistle programs.
Providence is evaluating expansion of home monitoring to other diagnoses, including higher acuity conditions.
COVID-19 Acute Care
TeleTriage expedites the triage of suspected COVID-19 patients and reduces the use of personal protective equipment (PPE) by 50% per patient per day. To date, TeleTriage has resulted in the conservation of more than 90,000 PPE units.
TeleHospitalist services expanded from traditional night coverage to caring for patients in COVID-19 units around the clock. Currently, there are 25 telehospitalists who practice both in-person and virtual medicine.
TeleICU offers remote management of more than 180 ICU beds across 17 hospitals from two central command centers in Washington state and Alaska. The services include night-time intensivist and ICU nurse coverage, including medication and ventilator management, and family conferences. COVID-19 increased the demand for TeleICU, with anticipated expansion to more than 300 beds.
Core TeleSpecialty services include TeleStroke and TelePsychiatry across 135 remote sites.
Ambulatory Virtual Visits
Providence launched the COVID-19 hub microsite to help educate patients by providing accurate and timely information. A chatbot named Grace helps screen patients who are worried about COVID-19. Grace also suggests next steps, such as a video visit with a patient’s primary care provider or a visit using Express Care/Virtual team, a direct-to-consumer service available to patients within and outside of the health care system.
In less than 2 weeks, Providence enabled virtual visits for more than 7,000 outpatient providers, with more than 14,000 alternative visits now occurring daily. This has allowed primary and specialty providers to continue to manage their patient panels remotely. The number of Express Care/Virtual visits increased from 60 to more than 1,000 per day.
BHC Expansion
In the effort to improve care for its caregivers, Providence launched a behavioral health concierge (BHC) service that offers employees and their dependents virtual access to licensed mental health professionals. Over the last half of 2019, BHC provided more than 1,000 phone and virtual visits, depending on the individual preference of patients. Notably, 21% percent of users were physicians; 65% of users were seen the same day and 100% of users were seen within 48 hours.
COVID-19 increased demand for services that initially started in Seattle and rapidly expanded to Montana, Oregon, and California.
Outside Partnerships
Providence has established partnerships with outside facilities by providing services to 135 sites across eight states. COVID-19 accelerated the employment of new services, including TeleICU.
Telemedicine at Sound Physicians
Sound Physicians is a national physician-founded and -led organization that provides emergency medicine, critical care, hospital medicine, population health, and physician advisory services. Five years ago, Sound launched a telemedicine service line. I spoke with Brian Carpenter, MD, national medical director for TeleHospitalist Services at Sound, to learn about his experience implementing Telehospitalist programs across 22 hospitals and 22 skilled nursing facilities.
Prior to COVID-19, Sound offered a spectrum of telemedicine services including night-time telephonic cross coverage, as well as video-assisted admissions, transfers, and rapid responses. In 2019, Sound Telehospitalists received 88,000 connect requests, including 6,400 video-assisted new admissions and 82 rapid responses. Typically, one physician covers four to eight hospitals with back-up available for surges. The team uses a predictive model for staffing and developed an acuity-based algorithm to ensure that patients in distress are evaluated immediately, new stable admissions on average are seen within 12 minutes, and order clarifications are provided within 30 minutes.
The COVID-19 pandemic created an urgent demand for providers to support an overwhelmed health care system. Without the traditional barriers to implementation – such as lack of acceptance by medical staff, nurses and patients, strict state licensing and technology requirements, lack of reimbursement, and delays in hospital credentialing – Sound was able to develop a rapid implementation model for telemedicine services. Currently, four new hospitals are in the active implementation phase, with 40 more hospitals in the pipeline.
Implementing a telemedicine program at your hospital
In order to successfully launch a telemedicine program, Dr. Carpenter outlined the following critical implementation steps:
- In collaboration with local leadership, define the problem you are trying to solve, which helps inform the scope of the telemedicine practice and technology requirements (for example, night-time cross-coverage vs. full telemedicine service).
- Complete a discovery process (for example, existing workflow for patient admission and transfer) with the end-goal of developing a workflow and rules of engagement.
- Obtain hospital credentialing/privileges and EMR access.
- Train end-users, including physicians and nurse telepresenters.
Dr. Carpenter offered this advice to those considering a telemedicine program: “Telemedicine is not just about technology; a true telemedicine program encompasses change management, workflow development, end-user training, compliance, and mechanisms for continuous process improvement. We want to make things better for the physicians, nurses, and patients.”
Telehealth is offering support to health care providers on the front lines, patients in need of care, and health care systems managing the unprecedented surges in volume.
Dr. Farah is a hospitalist, physician adviser, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
Introduction to population management
Defining the key terms
Traditionally, U.S. health care has operated under a fee-for-service payment model, in which health care providers (such as physicians, hospitals, and health care systems) receive a fee for services such as office visits, hospital stays, procedures, and tests. However, reimbursement discussions are increasingly moving from fee-for-service to value-based, in which payments are tied to managing population health and total cost of care.
Because these changes will impact the entire system all the way down to individual providers, in the upcoming Population Management article series in The Hospitalist, we will discuss the nuances and implications that physicians, executives, and hospitals should be aware of. In this first article, we will examine the impetus for the shift toward population management and introduce common terminology to lay the foundation for the future content.
The traditional model: Fee for service
Under the traditional fee-for-service payment system, health care providers are paid per unit of service. For example, hospitals receive diagnosis-related group (DRG) payments for inpatient stays, and physicians are paid per patient visit. The more services that hospitals or physicians provide, the more money both get paid, without financial consequences for quality outcomes or total cost of care. Total cost of care includes clinic visits, outpatient procedures and tests, hospital and ED visits, home health, skilled nursing facilities, durable medical equipment, and sometimes drugs during an episode of care (for example, a hospital stay plus 90 days after discharge) or over a period of time (for example, a month or a year).
As a result of the fee-for-service payment system, the United States spends more money on health care than other wealthy countries, yet it lags behind other countries on many quality measures, such as disease burden, overall mortality, premature death, and preventable death.1,2
In 2007, the Institute for Healthcare Improvement (IHI) developed the Triple Aim framework that focused on the following:
- Improving the patient experience of care (including quality and satisfaction).
- Improving the health of populations.
- Reducing per capita cost of care.
Both public payers like Medicare and Medicaid, as well as private payers, embraced the Triple Aim to reform how health care is delivered and paid for. As such, health care delivery focus and financial incentives are shifting from managing discrete patient encounters for acute illness to managing population health and total cost of care.
A new approach: Population management
Before diving into population management, it is important to first understand the terms “population” and “population health.” A population can be defined geographically or may include employees of an organization, members of a health plan, or patients receiving care from a specific physician group or health care system. David A. Kindig, MD, PhD, professor emeritus of population health sciences at the University of Wisconsin–Madison, defined population health as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.”3 Dr. Kindig noted that population health outcomes have many determinants, such as the following:4
- Health care (access, cost, quantity, and quality of health care services).
- Individual behavior (including diet, exercise, and substance abuse).
- Genetics.
- The social environment (education, income, occupation, class, and social support).
- Physical environment (air and water quality, lead exposure, and the design of neighborhoods).
IHI operationally defines population health by measures such as life expectancy, mortality rates, health and functional status, the incidence and/or prevalence of chronic disease, and behavioral and physiological factors such as smoking, physical activity, diet, blood pressure, body mass index, and cholesterol.5
On the other hand, population management is primarily concerned with health care determinants of health and, according to IHI, should be clearly distinguished from population health, which focuses on the broader determinants of health.5
According to Ron Greeno, MD, MHM, one of the founding members and a past-president of the Society of Hospital Medicine, population management is a “global approach of caring for an entire patient population to deliver safe and equitable care and to more intelligently allocate resources to keep people well.”
Population management requires understanding the patient population, which includes risk stratification and redesigning and delivering services that are guided by integrated clinical and administrative data and enabled by information technology.
Cost-sharing payment models
The cornerstone of population management is provider accountability for the cost of care, which can be accomplished through shared-risk models or population-based payments. Let’s take a closer look at each.
Under shared-risk models, providers receive payment based on their performance against cost targets. The goal is to generate cost savings by improving care coordination, engaging patients in shared decision making based on their health goals, and reducing utilization of care that provides little to no value for patients (for example, preventable hospital admissions or unnecessary imaging or procedures).
Cost targets and actual spending are reconciled retrospectively. If providers beat cost targets, they are eligible to keep a share of generated savings based on their performance on selected quality measures. However, if providers’ actual spending exceeds cost targets, they will compensate payers for a portion of the losses. Under one-sided risk models, providers are eligible for shared savings but not financially responsible for losses. Under two-sided risk models, providers are accountable for both savings and losses.
With prospective population-based payments, also known as capitation, providers receive in advance a fixed amount of money per patient per unit of time (for example, per month) that creates a budget to cover the cost of agreed-upon health care services. The prospective payments are risk adjusted and typically tied to performance on selected quality, effectiveness, and patient experience measures.
Professional services capitation arrangements between physician groups and payers cover the cost of physician services including primary care, specialty care, and related laboratory and radiology services. Under global capitation or global payment arrangements, health care systems receive payments that cover the total cost of care for the patient population for a defined period.
Population-based payments create incentives to provide high-quality and efficient care within a set budget.6 If actual cost of delivering services to the defined patient population comes under the budget, the providers will realize savings, but otherwise will encounter losses.
What is next?
Now that we have explained the impetus for population management and the terminology, in the next article in this series we will discuss the current state of population management. We will also delve into a hospitalist’s role and participation so you can be aware of impending changes and ensure you are set up for success, no matter how the payment models evolve.
Dr. Farah is a hospitalist, physician adviser, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. Source: https://www.healthsystemtracker.org/chart-collection/health-spending-u-s-compare-countries/#item-start
2. Source: https://www.healthsystemtracker.org/brief/on-several-indicators-of-healthcare-quality the-u-s-falls-short/
3. Kindig D, Asada Y, Booske B. (2008). A Population Health Framework for Setting National and State Health Goals. JAMA, 299, 2081-2083.
4. Source: https://improvingpopulationhealth.typepad.com/blog/what-are-health-factorsdeterminants.html
5. Source: http://www.ihi.org/communities/blogs/population-health-population-management-terminology-in-us-health-care
6. Source: http://hcp-lan.org/workproducts/apm-refresh-whitepaper-final.pdf
Defining the key terms
Defining the key terms
Traditionally, U.S. health care has operated under a fee-for-service payment model, in which health care providers (such as physicians, hospitals, and health care systems) receive a fee for services such as office visits, hospital stays, procedures, and tests. However, reimbursement discussions are increasingly moving from fee-for-service to value-based, in which payments are tied to managing population health and total cost of care.
Because these changes will impact the entire system all the way down to individual providers, in the upcoming Population Management article series in The Hospitalist, we will discuss the nuances and implications that physicians, executives, and hospitals should be aware of. In this first article, we will examine the impetus for the shift toward population management and introduce common terminology to lay the foundation for the future content.
The traditional model: Fee for service
Under the traditional fee-for-service payment system, health care providers are paid per unit of service. For example, hospitals receive diagnosis-related group (DRG) payments for inpatient stays, and physicians are paid per patient visit. The more services that hospitals or physicians provide, the more money both get paid, without financial consequences for quality outcomes or total cost of care. Total cost of care includes clinic visits, outpatient procedures and tests, hospital and ED visits, home health, skilled nursing facilities, durable medical equipment, and sometimes drugs during an episode of care (for example, a hospital stay plus 90 days after discharge) or over a period of time (for example, a month or a year).
As a result of the fee-for-service payment system, the United States spends more money on health care than other wealthy countries, yet it lags behind other countries on many quality measures, such as disease burden, overall mortality, premature death, and preventable death.1,2
In 2007, the Institute for Healthcare Improvement (IHI) developed the Triple Aim framework that focused on the following:
- Improving the patient experience of care (including quality and satisfaction).
- Improving the health of populations.
- Reducing per capita cost of care.
Both public payers like Medicare and Medicaid, as well as private payers, embraced the Triple Aim to reform how health care is delivered and paid for. As such, health care delivery focus and financial incentives are shifting from managing discrete patient encounters for acute illness to managing population health and total cost of care.
A new approach: Population management
Before diving into population management, it is important to first understand the terms “population” and “population health.” A population can be defined geographically or may include employees of an organization, members of a health plan, or patients receiving care from a specific physician group or health care system. David A. Kindig, MD, PhD, professor emeritus of population health sciences at the University of Wisconsin–Madison, defined population health as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.”3 Dr. Kindig noted that population health outcomes have many determinants, such as the following:4
- Health care (access, cost, quantity, and quality of health care services).
- Individual behavior (including diet, exercise, and substance abuse).
- Genetics.
- The social environment (education, income, occupation, class, and social support).
- Physical environment (air and water quality, lead exposure, and the design of neighborhoods).
IHI operationally defines population health by measures such as life expectancy, mortality rates, health and functional status, the incidence and/or prevalence of chronic disease, and behavioral and physiological factors such as smoking, physical activity, diet, blood pressure, body mass index, and cholesterol.5
On the other hand, population management is primarily concerned with health care determinants of health and, according to IHI, should be clearly distinguished from population health, which focuses on the broader determinants of health.5
According to Ron Greeno, MD, MHM, one of the founding members and a past-president of the Society of Hospital Medicine, population management is a “global approach of caring for an entire patient population to deliver safe and equitable care and to more intelligently allocate resources to keep people well.”
Population management requires understanding the patient population, which includes risk stratification and redesigning and delivering services that are guided by integrated clinical and administrative data and enabled by information technology.
Cost-sharing payment models
The cornerstone of population management is provider accountability for the cost of care, which can be accomplished through shared-risk models or population-based payments. Let’s take a closer look at each.
Under shared-risk models, providers receive payment based on their performance against cost targets. The goal is to generate cost savings by improving care coordination, engaging patients in shared decision making based on their health goals, and reducing utilization of care that provides little to no value for patients (for example, preventable hospital admissions or unnecessary imaging or procedures).
Cost targets and actual spending are reconciled retrospectively. If providers beat cost targets, they are eligible to keep a share of generated savings based on their performance on selected quality measures. However, if providers’ actual spending exceeds cost targets, they will compensate payers for a portion of the losses. Under one-sided risk models, providers are eligible for shared savings but not financially responsible for losses. Under two-sided risk models, providers are accountable for both savings and losses.
With prospective population-based payments, also known as capitation, providers receive in advance a fixed amount of money per patient per unit of time (for example, per month) that creates a budget to cover the cost of agreed-upon health care services. The prospective payments are risk adjusted and typically tied to performance on selected quality, effectiveness, and patient experience measures.
Professional services capitation arrangements between physician groups and payers cover the cost of physician services including primary care, specialty care, and related laboratory and radiology services. Under global capitation or global payment arrangements, health care systems receive payments that cover the total cost of care for the patient population for a defined period.
Population-based payments create incentives to provide high-quality and efficient care within a set budget.6 If actual cost of delivering services to the defined patient population comes under the budget, the providers will realize savings, but otherwise will encounter losses.
What is next?
Now that we have explained the impetus for population management and the terminology, in the next article in this series we will discuss the current state of population management. We will also delve into a hospitalist’s role and participation so you can be aware of impending changes and ensure you are set up for success, no matter how the payment models evolve.
Dr. Farah is a hospitalist, physician adviser, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. Source: https://www.healthsystemtracker.org/chart-collection/health-spending-u-s-compare-countries/#item-start
2. Source: https://www.healthsystemtracker.org/brief/on-several-indicators-of-healthcare-quality the-u-s-falls-short/
3. Kindig D, Asada Y, Booske B. (2008). A Population Health Framework for Setting National and State Health Goals. JAMA, 299, 2081-2083.
4. Source: https://improvingpopulationhealth.typepad.com/blog/what-are-health-factorsdeterminants.html
5. Source: http://www.ihi.org/communities/blogs/population-health-population-management-terminology-in-us-health-care
6. Source: http://hcp-lan.org/workproducts/apm-refresh-whitepaper-final.pdf
Traditionally, U.S. health care has operated under a fee-for-service payment model, in which health care providers (such as physicians, hospitals, and health care systems) receive a fee for services such as office visits, hospital stays, procedures, and tests. However, reimbursement discussions are increasingly moving from fee-for-service to value-based, in which payments are tied to managing population health and total cost of care.
Because these changes will impact the entire system all the way down to individual providers, in the upcoming Population Management article series in The Hospitalist, we will discuss the nuances and implications that physicians, executives, and hospitals should be aware of. In this first article, we will examine the impetus for the shift toward population management and introduce common terminology to lay the foundation for the future content.
The traditional model: Fee for service
Under the traditional fee-for-service payment system, health care providers are paid per unit of service. For example, hospitals receive diagnosis-related group (DRG) payments for inpatient stays, and physicians are paid per patient visit. The more services that hospitals or physicians provide, the more money both get paid, without financial consequences for quality outcomes or total cost of care. Total cost of care includes clinic visits, outpatient procedures and tests, hospital and ED visits, home health, skilled nursing facilities, durable medical equipment, and sometimes drugs during an episode of care (for example, a hospital stay plus 90 days after discharge) or over a period of time (for example, a month or a year).
As a result of the fee-for-service payment system, the United States spends more money on health care than other wealthy countries, yet it lags behind other countries on many quality measures, such as disease burden, overall mortality, premature death, and preventable death.1,2
In 2007, the Institute for Healthcare Improvement (IHI) developed the Triple Aim framework that focused on the following:
- Improving the patient experience of care (including quality and satisfaction).
- Improving the health of populations.
- Reducing per capita cost of care.
Both public payers like Medicare and Medicaid, as well as private payers, embraced the Triple Aim to reform how health care is delivered and paid for. As such, health care delivery focus and financial incentives are shifting from managing discrete patient encounters for acute illness to managing population health and total cost of care.
A new approach: Population management
Before diving into population management, it is important to first understand the terms “population” and “population health.” A population can be defined geographically or may include employees of an organization, members of a health plan, or patients receiving care from a specific physician group or health care system. David A. Kindig, MD, PhD, professor emeritus of population health sciences at the University of Wisconsin–Madison, defined population health as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.”3 Dr. Kindig noted that population health outcomes have many determinants, such as the following:4
- Health care (access, cost, quantity, and quality of health care services).
- Individual behavior (including diet, exercise, and substance abuse).
- Genetics.
- The social environment (education, income, occupation, class, and social support).
- Physical environment (air and water quality, lead exposure, and the design of neighborhoods).
IHI operationally defines population health by measures such as life expectancy, mortality rates, health and functional status, the incidence and/or prevalence of chronic disease, and behavioral and physiological factors such as smoking, physical activity, diet, blood pressure, body mass index, and cholesterol.5
On the other hand, population management is primarily concerned with health care determinants of health and, according to IHI, should be clearly distinguished from population health, which focuses on the broader determinants of health.5
According to Ron Greeno, MD, MHM, one of the founding members and a past-president of the Society of Hospital Medicine, population management is a “global approach of caring for an entire patient population to deliver safe and equitable care and to more intelligently allocate resources to keep people well.”
Population management requires understanding the patient population, which includes risk stratification and redesigning and delivering services that are guided by integrated clinical and administrative data and enabled by information technology.
Cost-sharing payment models
The cornerstone of population management is provider accountability for the cost of care, which can be accomplished through shared-risk models or population-based payments. Let’s take a closer look at each.
Under shared-risk models, providers receive payment based on their performance against cost targets. The goal is to generate cost savings by improving care coordination, engaging patients in shared decision making based on their health goals, and reducing utilization of care that provides little to no value for patients (for example, preventable hospital admissions or unnecessary imaging or procedures).
Cost targets and actual spending are reconciled retrospectively. If providers beat cost targets, they are eligible to keep a share of generated savings based on their performance on selected quality measures. However, if providers’ actual spending exceeds cost targets, they will compensate payers for a portion of the losses. Under one-sided risk models, providers are eligible for shared savings but not financially responsible for losses. Under two-sided risk models, providers are accountable for both savings and losses.
With prospective population-based payments, also known as capitation, providers receive in advance a fixed amount of money per patient per unit of time (for example, per month) that creates a budget to cover the cost of agreed-upon health care services. The prospective payments are risk adjusted and typically tied to performance on selected quality, effectiveness, and patient experience measures.
Professional services capitation arrangements between physician groups and payers cover the cost of physician services including primary care, specialty care, and related laboratory and radiology services. Under global capitation or global payment arrangements, health care systems receive payments that cover the total cost of care for the patient population for a defined period.
Population-based payments create incentives to provide high-quality and efficient care within a set budget.6 If actual cost of delivering services to the defined patient population comes under the budget, the providers will realize savings, but otherwise will encounter losses.
What is next?
Now that we have explained the impetus for population management and the terminology, in the next article in this series we will discuss the current state of population management. We will also delve into a hospitalist’s role and participation so you can be aware of impending changes and ensure you are set up for success, no matter how the payment models evolve.
Dr. Farah is a hospitalist, physician adviser, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. Source: https://www.healthsystemtracker.org/chart-collection/health-spending-u-s-compare-countries/#item-start
2. Source: https://www.healthsystemtracker.org/brief/on-several-indicators-of-healthcare-quality the-u-s-falls-short/
3. Kindig D, Asada Y, Booske B. (2008). A Population Health Framework for Setting National and State Health Goals. JAMA, 299, 2081-2083.
4. Source: https://improvingpopulationhealth.typepad.com/blog/what-are-health-factorsdeterminants.html
5. Source: http://www.ihi.org/communities/blogs/population-health-population-management-terminology-in-us-health-care
6. Source: http://hcp-lan.org/workproducts/apm-refresh-whitepaper-final.pdf
In search of high-value care
Six steps that can help your team
U.S. spending on health care is growing rapidly and expected to reach 19.7% of gross domestic product by 2026.1 In response, the Centers for Medicare and Medicaid Services and national organizations such as the American Board of Internal Medicine (ABIM) and the American College of Physicians (ACP) have launched initiatives to ensure that the value being delivered to patients is on par with the escalating cost of care.
Over the past 10 years, I have led and advised hundreds of small- and large-scale projects that focused on improving patient care quality and cost. Below, I share what I, along with other leaders in high-value care, have observed that it takes to implement successful and lasting improvements – for the benefit of patients and hospitals.
A brief history of high-value care
When compared to other wealthy countries, the United States spends disproportionately more money on health care. In 2016, U.S. health care spending was $3.3 trillion1, or $10,348 per person.2 Hospital care alone was responsible for a third of health spending and amounted to $1.1 trillion in 20161. By 2026, national health spending is projected to reach $5.7 trillion1.
In response to escalating health care costs, CMS and other payers have shifted toward value-based reimbursements that tie payments to health care facilities and clinicians to their performance on selected quality, cost, and efficiency measures. For example, under the CMS Merit-based Incentive Payment System (MIPS), 5% of clinicians’ revenue in 2020 is tied to their 2018 performance in four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The percentage of revenue at risk will increase to 9% in 2022, based on 2020 performance.
Rising health care costs put a burden not just on the federal and state budgets, but on individual and family budgets as well. Out-of-pocket spending grew 3.9% in 2016 to $352.5 billion1 and is expected to increase in the future. High health care costs rightfully bring into question the value individual consumers of health care services are getting in return. If value is defined as the level of benefit achieved for a given cost, what is high-value care? The 2013 Institute of Medicine report3 defined high-value care as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.” It goes beyond a set of quality and cost measures used by payers to affect provider reimbursement and is driven by day-to-day individual providers’ decisions that affect individual patients’ outcomes and their cost of care.
High-value care has been embraced by national organizations. In 2012, the ABIM Foundation launched the Choosing Wisely initiative to support and promote conversations between clinicians and patients in choosing care that is truly necessary, supported by evidence, and free from harm. The result was an evidence-based list of recommendations from 540 specialty societies, including the Society of Hospital Medicine. The SHM – Adult Hospital Medicine list4 features the following “Five things physicians and patients should question”:
- Don’t place, or leave in place, urinary catheters for incontinence or convenience or monitoring of output for non–critically ill patients.
- Don’t prescribe medications for stress ulcer prophylaxis to medical inpatients unless at high risk for GI complications.
- Avoid transfusions of red blood cells for arbitrary hemoglobin or hematocrit thresholds and in the absence of symptoms of active coronary disease, heart failure, or stroke.
- Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.
- Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability.
The ACP launched a high-value care initiative that offers learning resources for clinicians and medical educators, clinical guidelines, and best practice advice. In 2012, a workgroup of internists convened by ACP developed a list of 37 clinical situations in which medical tests are commonly used but do not provide high value.5 Seven of those situations are applicable to adult hospital medicine.
High-value care today: What the experts say
More than 5 years later, what progress have hospitalists made in adopting high-value care practices? To answer this and other questions, I reached out to three national experts in high-value care in hospital medicine: Amit Pahwa, MD, assistant professor of medicine and pediatrics at Johns Hopkins University, Baltimore, and a course director of “Topics in interdisciplinary medicine: High-value health care”; Christopher Petrilli, MD, clinical assistant professor in the department of medicine at New York University Langone Health and clinical lead, Manhattan campus, value-based management; and Charlie Wray, DO, MS, assistant professor of medicine at the University of California in San Francisco and a coauthor of an article on high-value care in hospital medicine published recently in the Journal of General Internal Medicine6.
The experts agree that awareness of high-value care among practicing physicians and medical trainees has increased in the last few years. Major professional publications have highlighted the topic, including The Journal of Hospital Medicine’s “Things We Do For No Reason” series, JAMA’s “Teachable Moments,” and the American Journal of Medicine’s recurring column dedicated to high-value care practice. Leading teaching institutions have built high-value care curricula as a part of their medical student and resident training. However, widespread adoption has been slow and sometimes difficult.
The barriers to adoption of high-value practices among hospitalists are numerous and deep rooted in historical practices and culture. As Dr. Petrilli said, the “culture of overordering [diagnostic tests] is hard to break.” Hospitalists may not have well-developed relationships with patients, or time to explain why some tests or treatments are unnecessary. There is a lack of cost transparency, including the cost of the tests themselves and the downstream costs of additional tests and follow-ups. The best intended interventions fail to produce durable change unless they are seamlessly integrated into a hospitalist’s daily workflow.
Six steps to implementing a successful high-value care initiative
What can hospitalists do to improve the value of care they provide to their patients and hospital partners?
1. Identify high-value care opportunities at your hospital.
Dr. Wray pointed out that “all high-value care is local.” Start by looking at the national guidelines and talking to your senior clinical leaders and colleagues. Review your hospital data to identify opportunities and understand the root causes, including variability among providers.
If you choose to analyze and present provider-specific data, first be transparent on why you are doing that. Your goal is not to tell physicians how to practice or to score them, but instead, to promote adoption of evidence-based high-value care by identifying and discussing provider practice variations, and to generate possible solutions. Second, make sure that the data you present is credible and trustworthy by clearly outlining the data source, time frame, sample size per provider, any inclusion and exclusion criteria, attribution logic, and severity adjustment methodology. Third, expect initial pushback as transparency and change can be scary. But most doctors are inherently competitive and will want to be the best at caring for their patients.
2. Assemble the team.
Identify an executive sponsor – a senior clinical executive (for example, the chief medical officer or vice president of medical affairs) whose role is to help engage stakeholders, secure resources, and remove barriers. When assembling the rest of the team, include a representative from each major stakeholder group, but keep the team small enough to be effective. For example, if your project focuses on improving telemetry utilization, seek representation from hospitalists, cardiologists, nurses, utilization managers, and possibly IT. Look for people with the relevant knowledge and experience who are respected by their peers and can influence opinion.
3. Design a sustainable solution.
To be sustainable, a solution must be evidence based, well integrated in provider workflow, and have acceptable impact on daily workload (e.g., additional time per patient). If an estimated impact is significant, you need to discuss adding resources or negotiating trade-offs.
A great example of a sustainable solution, aimed to control overutilization of telemetry and urinary catheters, is the one implemented by Dr. Wray and his team.7 They designed an EHR-based “silent” indicator that clearly signaled an active telemetry or urinary catheter order for each patient. Clicking on the indicator directed a provider to a “manage order” screen where she could cancel the order, if necessary.
4. Engage providers.
You may design the best solution, but it will not succeed unless it is embraced by others. To engage providers, you must clearly communicate why the change is urgently needed for the benefit of their patients, hospital, or community, and appeal to their minds, hearts, and competitive nature.
For example, if you are focusing on overutilization of urinary catheters, you may share your hospital’s urinary catheter device utilization ratio (# of indwelling catheter days/# patient days) against national benchmarks, or the impact on hospital catheter–associated urinary tract infections (CAUTI) rates to appeal to the physicians’ minds. Often, data alone are not enough to move people to action. You must appeal to their hearts by sharing stories of real patients whose lives were affected by preventable CAUTI. Leverage physicians’ competitive nature by using provider-specific data to compare against their peers to spark a discussion.
5. Evaluate impact.
Even before you implement a solution, select metrics to measure impact and set SMART (specific, measurable, achievable, relevant, and time-bound) goals. As your implementation moves forward, do not let up or give up – continue to evaluate impact, remove barriers, refine your solution to get back on track if needed, and constantly communicate to share ongoing project results and lessons learned.
6. Sustain improvements.
Sustainable improvements require well-designed solutions integrated into provider workflow, but that is just the first step. Once you demonstrate the impact, consider including the metric (e.g., telemetry or urinary catheter utilization) in your team and/or individual provider performance dashboard, regularly reviewing and discussing performance during your team meetings to maintain engagement, and if needed, making improvements to get back on track.
Successful adoption of high-value care practices requires a disciplined approach to design and implement solutions that are patient-centric, evidence-based, data-driven and integrated in provider workflow.
Dr. Farah is a hospitalist, Physician Advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. From the Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2018-2027.
2. Peterson-Kaiser Health System Tracker: How does health spending in the U.S. compare to other countries?
3. Creating a new culture of care, in “Best care at lower cost: The path to continuously learning health care in America.” (Washington: National Academies Press, 2013, pp. 255-80).
4. Choosing Wisely: SHM – Adult Hospital Medicine; Five things physicians and patients should question.
5. Qaseem A et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012 Jan 17;156(2):147-9.
6. Cho HJ et al. Right care in hospital medicine: Co-creation of ten opportunities in overuse and underuse for improving value in hospital medicine. J Gen Intern Med. 2018 Jun;33(6):804-6.
7. Wray CM et al. Improving value by reducing unnecessary telemetry and urinary catheter utilization in hospitalized patients. Am J Med. 2017 Sep;130(9):1037-41.
Six steps that can help your team
Six steps that can help your team
U.S. spending on health care is growing rapidly and expected to reach 19.7% of gross domestic product by 2026.1 In response, the Centers for Medicare and Medicaid Services and national organizations such as the American Board of Internal Medicine (ABIM) and the American College of Physicians (ACP) have launched initiatives to ensure that the value being delivered to patients is on par with the escalating cost of care.
Over the past 10 years, I have led and advised hundreds of small- and large-scale projects that focused on improving patient care quality and cost. Below, I share what I, along with other leaders in high-value care, have observed that it takes to implement successful and lasting improvements – for the benefit of patients and hospitals.
A brief history of high-value care
When compared to other wealthy countries, the United States spends disproportionately more money on health care. In 2016, U.S. health care spending was $3.3 trillion1, or $10,348 per person.2 Hospital care alone was responsible for a third of health spending and amounted to $1.1 trillion in 20161. By 2026, national health spending is projected to reach $5.7 trillion1.
In response to escalating health care costs, CMS and other payers have shifted toward value-based reimbursements that tie payments to health care facilities and clinicians to their performance on selected quality, cost, and efficiency measures. For example, under the CMS Merit-based Incentive Payment System (MIPS), 5% of clinicians’ revenue in 2020 is tied to their 2018 performance in four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The percentage of revenue at risk will increase to 9% in 2022, based on 2020 performance.
Rising health care costs put a burden not just on the federal and state budgets, but on individual and family budgets as well. Out-of-pocket spending grew 3.9% in 2016 to $352.5 billion1 and is expected to increase in the future. High health care costs rightfully bring into question the value individual consumers of health care services are getting in return. If value is defined as the level of benefit achieved for a given cost, what is high-value care? The 2013 Institute of Medicine report3 defined high-value care as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.” It goes beyond a set of quality and cost measures used by payers to affect provider reimbursement and is driven by day-to-day individual providers’ decisions that affect individual patients’ outcomes and their cost of care.
High-value care has been embraced by national organizations. In 2012, the ABIM Foundation launched the Choosing Wisely initiative to support and promote conversations between clinicians and patients in choosing care that is truly necessary, supported by evidence, and free from harm. The result was an evidence-based list of recommendations from 540 specialty societies, including the Society of Hospital Medicine. The SHM – Adult Hospital Medicine list4 features the following “Five things physicians and patients should question”:
- Don’t place, or leave in place, urinary catheters for incontinence or convenience or monitoring of output for non–critically ill patients.
- Don’t prescribe medications for stress ulcer prophylaxis to medical inpatients unless at high risk for GI complications.
- Avoid transfusions of red blood cells for arbitrary hemoglobin or hematocrit thresholds and in the absence of symptoms of active coronary disease, heart failure, or stroke.
- Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.
- Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability.
The ACP launched a high-value care initiative that offers learning resources for clinicians and medical educators, clinical guidelines, and best practice advice. In 2012, a workgroup of internists convened by ACP developed a list of 37 clinical situations in which medical tests are commonly used but do not provide high value.5 Seven of those situations are applicable to adult hospital medicine.
High-value care today: What the experts say
More than 5 years later, what progress have hospitalists made in adopting high-value care practices? To answer this and other questions, I reached out to three national experts in high-value care in hospital medicine: Amit Pahwa, MD, assistant professor of medicine and pediatrics at Johns Hopkins University, Baltimore, and a course director of “Topics in interdisciplinary medicine: High-value health care”; Christopher Petrilli, MD, clinical assistant professor in the department of medicine at New York University Langone Health and clinical lead, Manhattan campus, value-based management; and Charlie Wray, DO, MS, assistant professor of medicine at the University of California in San Francisco and a coauthor of an article on high-value care in hospital medicine published recently in the Journal of General Internal Medicine6.
The experts agree that awareness of high-value care among practicing physicians and medical trainees has increased in the last few years. Major professional publications have highlighted the topic, including The Journal of Hospital Medicine’s “Things We Do For No Reason” series, JAMA’s “Teachable Moments,” and the American Journal of Medicine’s recurring column dedicated to high-value care practice. Leading teaching institutions have built high-value care curricula as a part of their medical student and resident training. However, widespread adoption has been slow and sometimes difficult.
The barriers to adoption of high-value practices among hospitalists are numerous and deep rooted in historical practices and culture. As Dr. Petrilli said, the “culture of overordering [diagnostic tests] is hard to break.” Hospitalists may not have well-developed relationships with patients, or time to explain why some tests or treatments are unnecessary. There is a lack of cost transparency, including the cost of the tests themselves and the downstream costs of additional tests and follow-ups. The best intended interventions fail to produce durable change unless they are seamlessly integrated into a hospitalist’s daily workflow.
Six steps to implementing a successful high-value care initiative
What can hospitalists do to improve the value of care they provide to their patients and hospital partners?
1. Identify high-value care opportunities at your hospital.
Dr. Wray pointed out that “all high-value care is local.” Start by looking at the national guidelines and talking to your senior clinical leaders and colleagues. Review your hospital data to identify opportunities and understand the root causes, including variability among providers.
If you choose to analyze and present provider-specific data, first be transparent on why you are doing that. Your goal is not to tell physicians how to practice or to score them, but instead, to promote adoption of evidence-based high-value care by identifying and discussing provider practice variations, and to generate possible solutions. Second, make sure that the data you present is credible and trustworthy by clearly outlining the data source, time frame, sample size per provider, any inclusion and exclusion criteria, attribution logic, and severity adjustment methodology. Third, expect initial pushback as transparency and change can be scary. But most doctors are inherently competitive and will want to be the best at caring for their patients.
2. Assemble the team.
Identify an executive sponsor – a senior clinical executive (for example, the chief medical officer or vice president of medical affairs) whose role is to help engage stakeholders, secure resources, and remove barriers. When assembling the rest of the team, include a representative from each major stakeholder group, but keep the team small enough to be effective. For example, if your project focuses on improving telemetry utilization, seek representation from hospitalists, cardiologists, nurses, utilization managers, and possibly IT. Look for people with the relevant knowledge and experience who are respected by their peers and can influence opinion.
3. Design a sustainable solution.
To be sustainable, a solution must be evidence based, well integrated in provider workflow, and have acceptable impact on daily workload (e.g., additional time per patient). If an estimated impact is significant, you need to discuss adding resources or negotiating trade-offs.
A great example of a sustainable solution, aimed to control overutilization of telemetry and urinary catheters, is the one implemented by Dr. Wray and his team.7 They designed an EHR-based “silent” indicator that clearly signaled an active telemetry or urinary catheter order for each patient. Clicking on the indicator directed a provider to a “manage order” screen where she could cancel the order, if necessary.
4. Engage providers.
You may design the best solution, but it will not succeed unless it is embraced by others. To engage providers, you must clearly communicate why the change is urgently needed for the benefit of their patients, hospital, or community, and appeal to their minds, hearts, and competitive nature.
For example, if you are focusing on overutilization of urinary catheters, you may share your hospital’s urinary catheter device utilization ratio (# of indwelling catheter days/# patient days) against national benchmarks, or the impact on hospital catheter–associated urinary tract infections (CAUTI) rates to appeal to the physicians’ minds. Often, data alone are not enough to move people to action. You must appeal to their hearts by sharing stories of real patients whose lives were affected by preventable CAUTI. Leverage physicians’ competitive nature by using provider-specific data to compare against their peers to spark a discussion.
5. Evaluate impact.
Even before you implement a solution, select metrics to measure impact and set SMART (specific, measurable, achievable, relevant, and time-bound) goals. As your implementation moves forward, do not let up or give up – continue to evaluate impact, remove barriers, refine your solution to get back on track if needed, and constantly communicate to share ongoing project results and lessons learned.
6. Sustain improvements.
Sustainable improvements require well-designed solutions integrated into provider workflow, but that is just the first step. Once you demonstrate the impact, consider including the metric (e.g., telemetry or urinary catheter utilization) in your team and/or individual provider performance dashboard, regularly reviewing and discussing performance during your team meetings to maintain engagement, and if needed, making improvements to get back on track.
Successful adoption of high-value care practices requires a disciplined approach to design and implement solutions that are patient-centric, evidence-based, data-driven and integrated in provider workflow.
Dr. Farah is a hospitalist, Physician Advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. From the Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2018-2027.
2. Peterson-Kaiser Health System Tracker: How does health spending in the U.S. compare to other countries?
3. Creating a new culture of care, in “Best care at lower cost: The path to continuously learning health care in America.” (Washington: National Academies Press, 2013, pp. 255-80).
4. Choosing Wisely: SHM – Adult Hospital Medicine; Five things physicians and patients should question.
5. Qaseem A et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012 Jan 17;156(2):147-9.
6. Cho HJ et al. Right care in hospital medicine: Co-creation of ten opportunities in overuse and underuse for improving value in hospital medicine. J Gen Intern Med. 2018 Jun;33(6):804-6.
7. Wray CM et al. Improving value by reducing unnecessary telemetry and urinary catheter utilization in hospitalized patients. Am J Med. 2017 Sep;130(9):1037-41.
U.S. spending on health care is growing rapidly and expected to reach 19.7% of gross domestic product by 2026.1 In response, the Centers for Medicare and Medicaid Services and national organizations such as the American Board of Internal Medicine (ABIM) and the American College of Physicians (ACP) have launched initiatives to ensure that the value being delivered to patients is on par with the escalating cost of care.
Over the past 10 years, I have led and advised hundreds of small- and large-scale projects that focused on improving patient care quality and cost. Below, I share what I, along with other leaders in high-value care, have observed that it takes to implement successful and lasting improvements – for the benefit of patients and hospitals.
A brief history of high-value care
When compared to other wealthy countries, the United States spends disproportionately more money on health care. In 2016, U.S. health care spending was $3.3 trillion1, or $10,348 per person.2 Hospital care alone was responsible for a third of health spending and amounted to $1.1 trillion in 20161. By 2026, national health spending is projected to reach $5.7 trillion1.
In response to escalating health care costs, CMS and other payers have shifted toward value-based reimbursements that tie payments to health care facilities and clinicians to their performance on selected quality, cost, and efficiency measures. For example, under the CMS Merit-based Incentive Payment System (MIPS), 5% of clinicians’ revenue in 2020 is tied to their 2018 performance in four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The percentage of revenue at risk will increase to 9% in 2022, based on 2020 performance.
Rising health care costs put a burden not just on the federal and state budgets, but on individual and family budgets as well. Out-of-pocket spending grew 3.9% in 2016 to $352.5 billion1 and is expected to increase in the future. High health care costs rightfully bring into question the value individual consumers of health care services are getting in return. If value is defined as the level of benefit achieved for a given cost, what is high-value care? The 2013 Institute of Medicine report3 defined high-value care as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.” It goes beyond a set of quality and cost measures used by payers to affect provider reimbursement and is driven by day-to-day individual providers’ decisions that affect individual patients’ outcomes and their cost of care.
High-value care has been embraced by national organizations. In 2012, the ABIM Foundation launched the Choosing Wisely initiative to support and promote conversations between clinicians and patients in choosing care that is truly necessary, supported by evidence, and free from harm. The result was an evidence-based list of recommendations from 540 specialty societies, including the Society of Hospital Medicine. The SHM – Adult Hospital Medicine list4 features the following “Five things physicians and patients should question”:
- Don’t place, or leave in place, urinary catheters for incontinence or convenience or monitoring of output for non–critically ill patients.
- Don’t prescribe medications for stress ulcer prophylaxis to medical inpatients unless at high risk for GI complications.
- Avoid transfusions of red blood cells for arbitrary hemoglobin or hematocrit thresholds and in the absence of symptoms of active coronary disease, heart failure, or stroke.
- Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.
- Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability.
The ACP launched a high-value care initiative that offers learning resources for clinicians and medical educators, clinical guidelines, and best practice advice. In 2012, a workgroup of internists convened by ACP developed a list of 37 clinical situations in which medical tests are commonly used but do not provide high value.5 Seven of those situations are applicable to adult hospital medicine.
High-value care today: What the experts say
More than 5 years later, what progress have hospitalists made in adopting high-value care practices? To answer this and other questions, I reached out to three national experts in high-value care in hospital medicine: Amit Pahwa, MD, assistant professor of medicine and pediatrics at Johns Hopkins University, Baltimore, and a course director of “Topics in interdisciplinary medicine: High-value health care”; Christopher Petrilli, MD, clinical assistant professor in the department of medicine at New York University Langone Health and clinical lead, Manhattan campus, value-based management; and Charlie Wray, DO, MS, assistant professor of medicine at the University of California in San Francisco and a coauthor of an article on high-value care in hospital medicine published recently in the Journal of General Internal Medicine6.
The experts agree that awareness of high-value care among practicing physicians and medical trainees has increased in the last few years. Major professional publications have highlighted the topic, including The Journal of Hospital Medicine’s “Things We Do For No Reason” series, JAMA’s “Teachable Moments,” and the American Journal of Medicine’s recurring column dedicated to high-value care practice. Leading teaching institutions have built high-value care curricula as a part of their medical student and resident training. However, widespread adoption has been slow and sometimes difficult.
The barriers to adoption of high-value practices among hospitalists are numerous and deep rooted in historical practices and culture. As Dr. Petrilli said, the “culture of overordering [diagnostic tests] is hard to break.” Hospitalists may not have well-developed relationships with patients, or time to explain why some tests or treatments are unnecessary. There is a lack of cost transparency, including the cost of the tests themselves and the downstream costs of additional tests and follow-ups. The best intended interventions fail to produce durable change unless they are seamlessly integrated into a hospitalist’s daily workflow.
Six steps to implementing a successful high-value care initiative
What can hospitalists do to improve the value of care they provide to their patients and hospital partners?
1. Identify high-value care opportunities at your hospital.
Dr. Wray pointed out that “all high-value care is local.” Start by looking at the national guidelines and talking to your senior clinical leaders and colleagues. Review your hospital data to identify opportunities and understand the root causes, including variability among providers.
If you choose to analyze and present provider-specific data, first be transparent on why you are doing that. Your goal is not to tell physicians how to practice or to score them, but instead, to promote adoption of evidence-based high-value care by identifying and discussing provider practice variations, and to generate possible solutions. Second, make sure that the data you present is credible and trustworthy by clearly outlining the data source, time frame, sample size per provider, any inclusion and exclusion criteria, attribution logic, and severity adjustment methodology. Third, expect initial pushback as transparency and change can be scary. But most doctors are inherently competitive and will want to be the best at caring for their patients.
2. Assemble the team.
Identify an executive sponsor – a senior clinical executive (for example, the chief medical officer or vice president of medical affairs) whose role is to help engage stakeholders, secure resources, and remove barriers. When assembling the rest of the team, include a representative from each major stakeholder group, but keep the team small enough to be effective. For example, if your project focuses on improving telemetry utilization, seek representation from hospitalists, cardiologists, nurses, utilization managers, and possibly IT. Look for people with the relevant knowledge and experience who are respected by their peers and can influence opinion.
3. Design a sustainable solution.
To be sustainable, a solution must be evidence based, well integrated in provider workflow, and have acceptable impact on daily workload (e.g., additional time per patient). If an estimated impact is significant, you need to discuss adding resources or negotiating trade-offs.
A great example of a sustainable solution, aimed to control overutilization of telemetry and urinary catheters, is the one implemented by Dr. Wray and his team.7 They designed an EHR-based “silent” indicator that clearly signaled an active telemetry or urinary catheter order for each patient. Clicking on the indicator directed a provider to a “manage order” screen where she could cancel the order, if necessary.
4. Engage providers.
You may design the best solution, but it will not succeed unless it is embraced by others. To engage providers, you must clearly communicate why the change is urgently needed for the benefit of their patients, hospital, or community, and appeal to their minds, hearts, and competitive nature.
For example, if you are focusing on overutilization of urinary catheters, you may share your hospital’s urinary catheter device utilization ratio (# of indwelling catheter days/# patient days) against national benchmarks, or the impact on hospital catheter–associated urinary tract infections (CAUTI) rates to appeal to the physicians’ minds. Often, data alone are not enough to move people to action. You must appeal to their hearts by sharing stories of real patients whose lives were affected by preventable CAUTI. Leverage physicians’ competitive nature by using provider-specific data to compare against their peers to spark a discussion.
5. Evaluate impact.
Even before you implement a solution, select metrics to measure impact and set SMART (specific, measurable, achievable, relevant, and time-bound) goals. As your implementation moves forward, do not let up or give up – continue to evaluate impact, remove barriers, refine your solution to get back on track if needed, and constantly communicate to share ongoing project results and lessons learned.
6. Sustain improvements.
Sustainable improvements require well-designed solutions integrated into provider workflow, but that is just the first step. Once you demonstrate the impact, consider including the metric (e.g., telemetry or urinary catheter utilization) in your team and/or individual provider performance dashboard, regularly reviewing and discussing performance during your team meetings to maintain engagement, and if needed, making improvements to get back on track.
Successful adoption of high-value care practices requires a disciplined approach to design and implement solutions that are patient-centric, evidence-based, data-driven and integrated in provider workflow.
Dr. Farah is a hospitalist, Physician Advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. From the Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2018-2027.
2. Peterson-Kaiser Health System Tracker: How does health spending in the U.S. compare to other countries?
3. Creating a new culture of care, in “Best care at lower cost: The path to continuously learning health care in America.” (Washington: National Academies Press, 2013, pp. 255-80).
4. Choosing Wisely: SHM – Adult Hospital Medicine; Five things physicians and patients should question.
5. Qaseem A et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012 Jan 17;156(2):147-9.
6. Cho HJ et al. Right care in hospital medicine: Co-creation of ten opportunities in overuse and underuse for improving value in hospital medicine. J Gen Intern Med. 2018 Jun;33(6):804-6.
7. Wray CM et al. Improving value by reducing unnecessary telemetry and urinary catheter utilization in hospitalized patients. Am J Med. 2017 Sep;130(9):1037-41.