User login
Japan could benefit from hospital medicine expansion, leadership
The need for hospitalists continues to increase in Japan. There are approximately 9,000 hospitals in Japan, and approximately 80% of these hospitals are small- to medium-sized hospitals (<300 beds) where the need for hospital medicine is greatest. Historically, internal medicine subspecialists from nearly all subspecialties served as the primary attending physicians of hospitalized patients because inpatient internal medicine physicians, or hospitalists, did not exist.
Most subspecialists caring for hospitalized patients learned to practice internal medicine “on the fly” because they were not required to complete training in internal medicine before pursuing a subspecialty. After medical school, all graduates are required to complete a 2-year internship known as the National Obligatory Initial Postgraduate Clinical Training Program (NOIPCTP). The level of training during the NOIPCTP is similar to the third and fourth years of medical school in the United States.

The aging population and increasing complexity of hospitalized patients are the two main drivers of hospital medicine in Japan. Recently, the number of patients who have had adverse events because of inpatient medical errors has risen, and the transparency of these adverse events is making the need for hospitalists more apparent. In addition to improving the day-to-day medical management of hospitalized patients, hospitalists are needed to serve as champions of quality improvement, patient safety, and hospital throughput.
Leaders of the Japanese health care system recognize the need to improve the quality of inpatient care. The first step is to establish internal medicine as a specialty with dedicated internal medicine residency training programs. The Japanese Board of Medical Specialties approved establishing standardized, 3-year internal medicine residency training programs starting this spring, but that decision has been met with resistance for various reasons, namely concern for creating a disparity due to the shortage of internists in rural areas. Therefore, launch of this initiative has been postponed until April 2018.
In the meantime, the concept of hospital-based internists has been gradually gaining the support of subspecialists in Japan. Hospitalists are anticipated to work as the primary medical team leaders, directing and coordinating care among subspecialists in the future.
Despite its gradual spread, there are several challenges to growth. First, there are many terms for hospitalists, such as “hospital general practitioners” and “general internal medicine physicians.” A unified term for hospitalists would foster acceptance among Japanese physicians.
Additionally, some physicians, namely subspecialists, still question whether hospitalists are needed in Japan (even though potential loss of clinical revenue is not a significant concern among subspecialists).
Another challenge is lack of standardized training programs that define the skillset of hospitalists. Standardization of internal medicine training will also improve efficiency of communication between hospitalists and subspecialists.
An important milestone in the Japanese hospital medicine movement was the establishment of a society of hospitalists, known as the Japanese Hospitalist Network (JHN). The JHN has a quarterly publication (Hospitalist) targeted at junior faculty and residents that reviews topics in hospital medicine.
The JHN is affiliated with a larger society, the Japanese Society of Hospital General Medicine (JSHGM), which holds meetings twice a year. A unique offering at the next JSHGM meeting in March is a point-of-care ultrasound training workshop. Although this is the first such workshop for hospitalists in Japan, there are many training courses designed for the country’s hospitalists.
The emergence of such courses in Japan has paralleled the increasing need for hospitalists in Japan. We hope these courses for hospitalists will pave the road for the continued growth of hospital medicine in Japan.
Toru Yamada, MD
Dr. Yamada is an internist in the department of general medicine/family and community medicine at Nagoya (Japan) University and practices at Tokyo Bay Urayasu Ichikawa Medical Center in Chiba.
Taro Minami, MD
Dr. Minami is assistant professor of medicine in the division of pulmonary, critical care, and sleep medicine at Brown University in Providence, R.I., and director of ultrasound and simulation training at Memorial Hospital of Rhode Island.
Nilam J. Soni, MD, MS, FHM
Dr. Soni is associate professor of medicine in the division of hospital medicine at the University of Texas, San Antonio, and a hospitalist with the South Texas Veterans Health Care System in San Antonio.
The need for hospitalists continues to increase in Japan. There are approximately 9,000 hospitals in Japan, and approximately 80% of these hospitals are small- to medium-sized hospitals (<300 beds) where the need for hospital medicine is greatest. Historically, internal medicine subspecialists from nearly all subspecialties served as the primary attending physicians of hospitalized patients because inpatient internal medicine physicians, or hospitalists, did not exist.
Most subspecialists caring for hospitalized patients learned to practice internal medicine “on the fly” because they were not required to complete training in internal medicine before pursuing a subspecialty. After medical school, all graduates are required to complete a 2-year internship known as the National Obligatory Initial Postgraduate Clinical Training Program (NOIPCTP). The level of training during the NOIPCTP is similar to the third and fourth years of medical school in the United States.

The aging population and increasing complexity of hospitalized patients are the two main drivers of hospital medicine in Japan. Recently, the number of patients who have had adverse events because of inpatient medical errors has risen, and the transparency of these adverse events is making the need for hospitalists more apparent. In addition to improving the day-to-day medical management of hospitalized patients, hospitalists are needed to serve as champions of quality improvement, patient safety, and hospital throughput.
Leaders of the Japanese health care system recognize the need to improve the quality of inpatient care. The first step is to establish internal medicine as a specialty with dedicated internal medicine residency training programs. The Japanese Board of Medical Specialties approved establishing standardized, 3-year internal medicine residency training programs starting this spring, but that decision has been met with resistance for various reasons, namely concern for creating a disparity due to the shortage of internists in rural areas. Therefore, launch of this initiative has been postponed until April 2018.
In the meantime, the concept of hospital-based internists has been gradually gaining the support of subspecialists in Japan. Hospitalists are anticipated to work as the primary medical team leaders, directing and coordinating care among subspecialists in the future.
Despite its gradual spread, there are several challenges to growth. First, there are many terms for hospitalists, such as “hospital general practitioners” and “general internal medicine physicians.” A unified term for hospitalists would foster acceptance among Japanese physicians.
Additionally, some physicians, namely subspecialists, still question whether hospitalists are needed in Japan (even though potential loss of clinical revenue is not a significant concern among subspecialists).
Another challenge is lack of standardized training programs that define the skillset of hospitalists. Standardization of internal medicine training will also improve efficiency of communication between hospitalists and subspecialists.
An important milestone in the Japanese hospital medicine movement was the establishment of a society of hospitalists, known as the Japanese Hospitalist Network (JHN). The JHN has a quarterly publication (Hospitalist) targeted at junior faculty and residents that reviews topics in hospital medicine.
The JHN is affiliated with a larger society, the Japanese Society of Hospital General Medicine (JSHGM), which holds meetings twice a year. A unique offering at the next JSHGM meeting in March is a point-of-care ultrasound training workshop. Although this is the first such workshop for hospitalists in Japan, there are many training courses designed for the country’s hospitalists.
The emergence of such courses in Japan has paralleled the increasing need for hospitalists in Japan. We hope these courses for hospitalists will pave the road for the continued growth of hospital medicine in Japan.
Toru Yamada, MD
Dr. Yamada is an internist in the department of general medicine/family and community medicine at Nagoya (Japan) University and practices at Tokyo Bay Urayasu Ichikawa Medical Center in Chiba.
Taro Minami, MD
Dr. Minami is assistant professor of medicine in the division of pulmonary, critical care, and sleep medicine at Brown University in Providence, R.I., and director of ultrasound and simulation training at Memorial Hospital of Rhode Island.
Nilam J. Soni, MD, MS, FHM
Dr. Soni is associate professor of medicine in the division of hospital medicine at the University of Texas, San Antonio, and a hospitalist with the South Texas Veterans Health Care System in San Antonio.
The need for hospitalists continues to increase in Japan. There are approximately 9,000 hospitals in Japan, and approximately 80% of these hospitals are small- to medium-sized hospitals (<300 beds) where the need for hospital medicine is greatest. Historically, internal medicine subspecialists from nearly all subspecialties served as the primary attending physicians of hospitalized patients because inpatient internal medicine physicians, or hospitalists, did not exist.
Most subspecialists caring for hospitalized patients learned to practice internal medicine “on the fly” because they were not required to complete training in internal medicine before pursuing a subspecialty. After medical school, all graduates are required to complete a 2-year internship known as the National Obligatory Initial Postgraduate Clinical Training Program (NOIPCTP). The level of training during the NOIPCTP is similar to the third and fourth years of medical school in the United States.

The aging population and increasing complexity of hospitalized patients are the two main drivers of hospital medicine in Japan. Recently, the number of patients who have had adverse events because of inpatient medical errors has risen, and the transparency of these adverse events is making the need for hospitalists more apparent. In addition to improving the day-to-day medical management of hospitalized patients, hospitalists are needed to serve as champions of quality improvement, patient safety, and hospital throughput.
Leaders of the Japanese health care system recognize the need to improve the quality of inpatient care. The first step is to establish internal medicine as a specialty with dedicated internal medicine residency training programs. The Japanese Board of Medical Specialties approved establishing standardized, 3-year internal medicine residency training programs starting this spring, but that decision has been met with resistance for various reasons, namely concern for creating a disparity due to the shortage of internists in rural areas. Therefore, launch of this initiative has been postponed until April 2018.
In the meantime, the concept of hospital-based internists has been gradually gaining the support of subspecialists in Japan. Hospitalists are anticipated to work as the primary medical team leaders, directing and coordinating care among subspecialists in the future.
Despite its gradual spread, there are several challenges to growth. First, there are many terms for hospitalists, such as “hospital general practitioners” and “general internal medicine physicians.” A unified term for hospitalists would foster acceptance among Japanese physicians.
Additionally, some physicians, namely subspecialists, still question whether hospitalists are needed in Japan (even though potential loss of clinical revenue is not a significant concern among subspecialists).
Another challenge is lack of standardized training programs that define the skillset of hospitalists. Standardization of internal medicine training will also improve efficiency of communication between hospitalists and subspecialists.
An important milestone in the Japanese hospital medicine movement was the establishment of a society of hospitalists, known as the Japanese Hospitalist Network (JHN). The JHN has a quarterly publication (Hospitalist) targeted at junior faculty and residents that reviews topics in hospital medicine.
The JHN is affiliated with a larger society, the Japanese Society of Hospital General Medicine (JSHGM), which holds meetings twice a year. A unique offering at the next JSHGM meeting in March is a point-of-care ultrasound training workshop. Although this is the first such workshop for hospitalists in Japan, there are many training courses designed for the country’s hospitalists.
The emergence of such courses in Japan has paralleled the increasing need for hospitalists in Japan. We hope these courses for hospitalists will pave the road for the continued growth of hospital medicine in Japan.
Toru Yamada, MD
Dr. Yamada is an internist in the department of general medicine/family and community medicine at Nagoya (Japan) University and practices at Tokyo Bay Urayasu Ichikawa Medical Center in Chiba.
Taro Minami, MD
Dr. Minami is assistant professor of medicine in the division of pulmonary, critical care, and sleep medicine at Brown University in Providence, R.I., and director of ultrasound and simulation training at Memorial Hospital of Rhode Island.
Nilam J. Soni, MD, MS, FHM
Dr. Soni is associate professor of medicine in the division of hospital medicine at the University of Texas, San Antonio, and a hospitalist with the South Texas Veterans Health Care System in San Antonio.
Scholar grants help future hospitalists explore career pathways
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ernie L. Esquivel, MD, FACP, FHM, the clerkship director, medicine, and assistant professor of clinical medicine in the Division of General Internal Medicine at the Weill Cornell Medical College in New York City. Dr. Esquivel is involved with SHM’s Physicians in Training Committee, and has spearheaded the creation of the Student Hospitalist Scholar Grant program.
What inspired you to become a hospitalist?
I became a hospitalist serendipitously. At a critical juncture in my life about 8 years ago (when a change in career direction became necessary), I chanced upon a locum tenens position in a small community hospital in Lansdale, Pa., as a hospitalist. Having been a primary care track resident who subsequently chose to specialize in nephrology, I rediscovered my generalist inclinations during this job. I fell in love with the fast pace of the hospitalist’s work, the complexity of delivering care and the diversity of diseases, and of personal life stories on the general medicine wards and the ICU.
Subsequently, I worked as an intensivist in Philadelphia for a year before joining the Academic Hospital Medicine Division at Weill Cornell in New York City. At Cornell, I have managed to cultivate my passion for medical education, especially for working with and mentoring students and residents, while continuing to care for patients on the general medicine wards. As the medicine clerkship director, I have had the privilege of creating an innovative curriculum that I hope prepares medical students for the challenges in, and the richness of, encounters in the practice of inpatient medicine.
How and why did you become a member of SHM and the Physicians in Training Committee (PIT)?
I joined SHM 6 years ago as I started to explore my career options more deeply. In 2010, I attended the Academic Hospitalist Academy, and that really offered me a closer look at the different ways in which SHM could help me advance. I went to my first SHM annual meeting 5 years ago; it motivated me to become involved in committee work. Because of my interest in medical education, I volunteered for the PIT Committee and it has given me the opportunity to work closely with other hospitalists around the country, and develop programming specifically targeted toward future hospitalists.
What is the PIT Committee working on?
The committee has continued to find ways for increased engagement of residents and students in SHM. Dr. Brian Kwan, an academic hospitalist at UC San Diego, and I have been developing a travel grant program for resident trainees and hospital medicine fellows to attend the annual meeting. By offering them a stipend to defray the costs of travel if their quality improvement innovation or research project is accepted, we hope that the annual meeting can become a venue for them to highlight their work, while becoming exposed to the many activities and opportunities offered by our society. In addition, it could be a way for them to network with other future hospitalists and established future mentors.
What prompted you to lead the creation of the Student Hospitalist Scholar Grant summer program?
Before I became a hospitalist, I spent about 7 years in research, studying renal genetics. I have always been fascinated by science and asked how I can help to advance our knowledge. As a hospitalist, it became clear to me early on that there are many questions that one can pose about the clinical work we do, the way we practice medicine, or ways to innovate education, and that there are many academic hospitalists who engage in advancing the field. I spearheaded this program because I would like students to see the field of hospital medicine as one in which they can develop a future career in academic medicine, not only by caring for patients, but also by involving themselves in research questions or QI projects.
Do you have any specific advice for students and residents interested in hospital medicine? In what ways can early-career hospitalists utilize SHM resources to leverage their careers?
The decision to pursue a career as a hospitalist will open up many more questions in the future, because there are so many opportunities available. I would suggest that trainees ask in which ways they see themselves growing in the future – clinical research, medical education, QI/patient safety, operations, and hospital leadership are the main avenues. When I interview future faculty, I always pose the same question to each of them: “Every year you are allocated X amount of money that you can use for CME, etc. How are you going to use this money to improve your skills in any particular area?” The ability of candidates to answer this question reflects for me their preparedness to develop themselves as career hospitalists and their willingness to contribute to their group or division in an innovative manner.
The reality is that as one gets older, most will find it difficult to sustain a 26-week/year schedule. So find ways for your energies, in whichever area, to be noticed and developed toward a position of leadership in the hospital or medical school.
As you take care of patients in the hospital or consider your education and training, identify ways in which things can be done better. Invariably, someone in the Society of Hospital Medicine is interested in the same issue(s). Explore your ideas, share them at the meeting, talk to people, go to the SHM website and identify what resources are already available.
If SHM will be your future academic home, volunteer to engage in activities at the chapter or national levels. Our society is really dedicated to identifying ways to welcome you into our exciting and continually evolving field.
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ernie L. Esquivel, MD, FACP, FHM, the clerkship director, medicine, and assistant professor of clinical medicine in the Division of General Internal Medicine at the Weill Cornell Medical College in New York City. Dr. Esquivel is involved with SHM’s Physicians in Training Committee, and has spearheaded the creation of the Student Hospitalist Scholar Grant program.
What inspired you to become a hospitalist?
I became a hospitalist serendipitously. At a critical juncture in my life about 8 years ago (when a change in career direction became necessary), I chanced upon a locum tenens position in a small community hospital in Lansdale, Pa., as a hospitalist. Having been a primary care track resident who subsequently chose to specialize in nephrology, I rediscovered my generalist inclinations during this job. I fell in love with the fast pace of the hospitalist’s work, the complexity of delivering care and the diversity of diseases, and of personal life stories on the general medicine wards and the ICU.
Subsequently, I worked as an intensivist in Philadelphia for a year before joining the Academic Hospital Medicine Division at Weill Cornell in New York City. At Cornell, I have managed to cultivate my passion for medical education, especially for working with and mentoring students and residents, while continuing to care for patients on the general medicine wards. As the medicine clerkship director, I have had the privilege of creating an innovative curriculum that I hope prepares medical students for the challenges in, and the richness of, encounters in the practice of inpatient medicine.
How and why did you become a member of SHM and the Physicians in Training Committee (PIT)?
I joined SHM 6 years ago as I started to explore my career options more deeply. In 2010, I attended the Academic Hospitalist Academy, and that really offered me a closer look at the different ways in which SHM could help me advance. I went to my first SHM annual meeting 5 years ago; it motivated me to become involved in committee work. Because of my interest in medical education, I volunteered for the PIT Committee and it has given me the opportunity to work closely with other hospitalists around the country, and develop programming specifically targeted toward future hospitalists.
What is the PIT Committee working on?
The committee has continued to find ways for increased engagement of residents and students in SHM. Dr. Brian Kwan, an academic hospitalist at UC San Diego, and I have been developing a travel grant program for resident trainees and hospital medicine fellows to attend the annual meeting. By offering them a stipend to defray the costs of travel if their quality improvement innovation or research project is accepted, we hope that the annual meeting can become a venue for them to highlight their work, while becoming exposed to the many activities and opportunities offered by our society. In addition, it could be a way for them to network with other future hospitalists and established future mentors.
What prompted you to lead the creation of the Student Hospitalist Scholar Grant summer program?
Before I became a hospitalist, I spent about 7 years in research, studying renal genetics. I have always been fascinated by science and asked how I can help to advance our knowledge. As a hospitalist, it became clear to me early on that there are many questions that one can pose about the clinical work we do, the way we practice medicine, or ways to innovate education, and that there are many academic hospitalists who engage in advancing the field. I spearheaded this program because I would like students to see the field of hospital medicine as one in which they can develop a future career in academic medicine, not only by caring for patients, but also by involving themselves in research questions or QI projects.
Do you have any specific advice for students and residents interested in hospital medicine? In what ways can early-career hospitalists utilize SHM resources to leverage their careers?
The decision to pursue a career as a hospitalist will open up many more questions in the future, because there are so many opportunities available. I would suggest that trainees ask in which ways they see themselves growing in the future – clinical research, medical education, QI/patient safety, operations, and hospital leadership are the main avenues. When I interview future faculty, I always pose the same question to each of them: “Every year you are allocated X amount of money that you can use for CME, etc. How are you going to use this money to improve your skills in any particular area?” The ability of candidates to answer this question reflects for me their preparedness to develop themselves as career hospitalists and their willingness to contribute to their group or division in an innovative manner.
The reality is that as one gets older, most will find it difficult to sustain a 26-week/year schedule. So find ways for your energies, in whichever area, to be noticed and developed toward a position of leadership in the hospital or medical school.
As you take care of patients in the hospital or consider your education and training, identify ways in which things can be done better. Invariably, someone in the Society of Hospital Medicine is interested in the same issue(s). Explore your ideas, share them at the meeting, talk to people, go to the SHM website and identify what resources are already available.
If SHM will be your future academic home, volunteer to engage in activities at the chapter or national levels. Our society is really dedicated to identifying ways to welcome you into our exciting and continually evolving field.
Felicia Steele is SHM’s communications coordinator.
Editor’s note: Each month, SHM puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Log on to www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Ernie L. Esquivel, MD, FACP, FHM, the clerkship director, medicine, and assistant professor of clinical medicine in the Division of General Internal Medicine at the Weill Cornell Medical College in New York City. Dr. Esquivel is involved with SHM’s Physicians in Training Committee, and has spearheaded the creation of the Student Hospitalist Scholar Grant program.
What inspired you to become a hospitalist?
I became a hospitalist serendipitously. At a critical juncture in my life about 8 years ago (when a change in career direction became necessary), I chanced upon a locum tenens position in a small community hospital in Lansdale, Pa., as a hospitalist. Having been a primary care track resident who subsequently chose to specialize in nephrology, I rediscovered my generalist inclinations during this job. I fell in love with the fast pace of the hospitalist’s work, the complexity of delivering care and the diversity of diseases, and of personal life stories on the general medicine wards and the ICU.
Subsequently, I worked as an intensivist in Philadelphia for a year before joining the Academic Hospital Medicine Division at Weill Cornell in New York City. At Cornell, I have managed to cultivate my passion for medical education, especially for working with and mentoring students and residents, while continuing to care for patients on the general medicine wards. As the medicine clerkship director, I have had the privilege of creating an innovative curriculum that I hope prepares medical students for the challenges in, and the richness of, encounters in the practice of inpatient medicine.
How and why did you become a member of SHM and the Physicians in Training Committee (PIT)?
I joined SHM 6 years ago as I started to explore my career options more deeply. In 2010, I attended the Academic Hospitalist Academy, and that really offered me a closer look at the different ways in which SHM could help me advance. I went to my first SHM annual meeting 5 years ago; it motivated me to become involved in committee work. Because of my interest in medical education, I volunteered for the PIT Committee and it has given me the opportunity to work closely with other hospitalists around the country, and develop programming specifically targeted toward future hospitalists.
What is the PIT Committee working on?
The committee has continued to find ways for increased engagement of residents and students in SHM. Dr. Brian Kwan, an academic hospitalist at UC San Diego, and I have been developing a travel grant program for resident trainees and hospital medicine fellows to attend the annual meeting. By offering them a stipend to defray the costs of travel if their quality improvement innovation or research project is accepted, we hope that the annual meeting can become a venue for them to highlight their work, while becoming exposed to the many activities and opportunities offered by our society. In addition, it could be a way for them to network with other future hospitalists and established future mentors.
What prompted you to lead the creation of the Student Hospitalist Scholar Grant summer program?
Before I became a hospitalist, I spent about 7 years in research, studying renal genetics. I have always been fascinated by science and asked how I can help to advance our knowledge. As a hospitalist, it became clear to me early on that there are many questions that one can pose about the clinical work we do, the way we practice medicine, or ways to innovate education, and that there are many academic hospitalists who engage in advancing the field. I spearheaded this program because I would like students to see the field of hospital medicine as one in which they can develop a future career in academic medicine, not only by caring for patients, but also by involving themselves in research questions or QI projects.
Do you have any specific advice for students and residents interested in hospital medicine? In what ways can early-career hospitalists utilize SHM resources to leverage their careers?
The decision to pursue a career as a hospitalist will open up many more questions in the future, because there are so many opportunities available. I would suggest that trainees ask in which ways they see themselves growing in the future – clinical research, medical education, QI/patient safety, operations, and hospital leadership are the main avenues. When I interview future faculty, I always pose the same question to each of them: “Every year you are allocated X amount of money that you can use for CME, etc. How are you going to use this money to improve your skills in any particular area?” The ability of candidates to answer this question reflects for me their preparedness to develop themselves as career hospitalists and their willingness to contribute to their group or division in an innovative manner.
The reality is that as one gets older, most will find it difficult to sustain a 26-week/year schedule. So find ways for your energies, in whichever area, to be noticed and developed toward a position of leadership in the hospital or medical school.
As you take care of patients in the hospital or consider your education and training, identify ways in which things can be done better. Invariably, someone in the Society of Hospital Medicine is interested in the same issue(s). Explore your ideas, share them at the meeting, talk to people, go to the SHM website and identify what resources are already available.
If SHM will be your future academic home, volunteer to engage in activities at the chapter or national levels. Our society is really dedicated to identifying ways to welcome you into our exciting and continually evolving field.
Felicia Steele is SHM’s communications coordinator.
Trending at SHM
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Top 10 reasons to attend 2017 Quality and Safety Educators Academy
It’s your last chance to register for the 2017 Quality and Safety Educators Academy (QSEA), which will be held Feb. 26-28 in Tempe, Ariz. Looking for some reasons to attend? Here are the top 10:
- Education. Develop and refine your knowledge in quality and patient safety.
- Desert beauty. Enjoy sunny Tempe, or travel to nearby Phoenix or Scottsdale.
- Curriculum development. Return to your institution with a collection of new educational strategies and curriculum development tactics.
- Professional development. Hone your skills and be the best that you can be to meet the increasing demand for medical educators who are well versed in patient safety and quality.
- Relationships. Build your network with faculty mentors and colleagues who have similar career interests.
- Institutional backing. Engage your institutional leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education core competencies and improve patient care.
- Hands-on learning. Engage in an interactive learning environment, with a 10:1 student to faculty ratio, including facilitated large-group sessions, small-group exercises, and panel discussions.
- Variety. Each day has its own topic that breaks down into subtopics, covering the breadth of information you need to know to succeed.
- Faculty. All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Resources. Leave with a toolkit of educational resources and curricular tools for quality and safety education.
Reserve your spot today before the meeting sells out at www.shmqsea.org.
SHM committees address practice management topics
SHM’s Practice Management Committee has been researching, deliberating case studies, and authoring timely content to further define HM’s role in key health care innovations. As the specialty has grown and evolved, so have hospitalists’ involvement in comanagement relationships.
The committee recently released a white paper addressing the evolution of comanagement in hospital medicine. Be on the lookout for that in early 2017.
Similarly, telemedicine is rapidly expanding, and the committee found it imperative to clarify the who, what, when, where, why, and how of telemedicine programs in hospital medicine. You can also expect this white paper in early 2017.
The committee also has created guidelines on how to raise awareness of cultural humility in your HM group. Deemed the “5 R’s of Cultural Humility,” look for a campaign around the guidelines to launch at HM17 in May in Las Vegas.
SHM’s Health Information Technology Committee has been diligently analyzing and reporting on survey results that captured hospitalists’ attitudes toward electronic health records. The purpose of this white paper is to effect change on EHR systems by informing conversations with decision makers, and to provide HM a definitive voice in the landscape of the tumultuous world of EHRs. More information is coming soon.
Make a difference with SHM
Grow professionally, expand your curriculum vitae, and get involved in work you are passionate about with colleagues across the country with SHM’s volunteer experiences. New opportunities are constantly being added that will bolster your strengths, sharpen your professional acumen and enhance your profile in the hospital medicine community at www.hospitalmedicine.org/getinvolved.
Leadership Academy 2017 has a new look
Don’t miss out on the only leadership program designed specifically for hospitalists. SHM Leadership Academy 2017 will be at the JW Marriott Camelback Inn in Scottsdale, Ariz., on Oct. 23-26.
For the first time, the Leadership Academy prerequisite of attendance in the first-level, Foundations course has been removed. Essential Strategies (formerly Leadership Foundations), Influential Management, and Mastering Teamwork courses are available to all attendees, regardless of previous attendance. Prior participants have made recommendations to help interested registrants determine which course fits them best in their leadership journey.
All three courses run concurrently over the span of 4 days. This expanded meeting will provide attendees with world-class networking opportunities, creating opportunities for a more engaging, impactful educational experience.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
Earn dues credits with the Membership Ambassador Program
Help SHM grow its network of hospitalists and continue to provide education, networking, and career advancement for its members. Visit www.hospitalmedicine.org/refer today.
Brett Radler is SHM's communications specialist.
Female physicians, lower mortality, lower readmissions: A case study
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.

My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at [email protected].
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.

My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at [email protected].
Week in, week out for the past 25 years, I have had a front-row seat to the medical practice of a certain female physician: my wife, Heather. We met when we worked together on the wards during residency in 1991; spent a year in rural Montana working together in clinics, ERs, and hospitals; shared the care of one another’s patients as our practices grew in parallel – hers in skilled nursing facilities, mine in the hospital; and reunited in recent years to work together as part of the same practice.
When I saw the paper by Yusuke Tsugawa, MD, MPH, PhD, and his associates showing lower mortality and readmission rates for female physicians versus their male counterparts, I began to wonder if the case of Heather’s practice style, and my observations of it, could help to interpret the findings of the study (JAMA Intern Med. 2016 Dec 19. doi: 10.1001/jamainternmed.2016.7875). The authors suggested that female physicians may produce better outcomes than male physicians.
The study in question, which analyzed more than 1.5 million hospitalizations, looked at Medicare beneficiaries hospitalized with a medical condition treated by general internists between 2011 and 2014. The authors found that patients treated by female physicians had lower 30-day mortality (adjusted rate, 11.07% vs. 11.49%, P<.001) and readmissions (adjusted rate, 15.02% vs. 15.57%, P<.001) than those treated by male physicians within the same hospital. The differences were “modest but important,” coauthor Ashish K. Jha, MD, MPH, wrote in his blog. Numbers needed to treat to prevent one death and one readmission were 233 and 182, respectively.

My observations of Heather’s practice approach, compared with my own, center around three main themes:
She spends more time considering her approach to a challenging case.
She has less urgency in deciding on a definitive course of action and more patience in sorting things out before proceeding with a diagnostic and therapeutic plan. She is more likely to leave open the possibility of changing her mind; she has less of a tendency to anchor on a particular diagnosis and treatment. Put another way, she is more willing to continue with ambiguous findings without lateralizing to one particular approach.
She brings more work-life balance to her professional responsibilities.
Despite being highly productive at work (and at home), she has worked less than full time throughout her career. This means that, during any given patient encounter, she is more likely to be unburdened by overwork and its negative consequences. It is my sense that many full-time physicians would be happier (and more effective) if they simply worked less. Heather has had the self-knowledge to take on a more manageable workload; the result is that she has remained joyous in practice for more than two decades.
She is less dogmatic and more willing to customize care based on the needs of the individual patient.
Although a good fund of knowledge is essential, if such knowledge obscures the physician’s ability to read the patient, then it is best abandoned, at least temporarily. Heather refers to the body of scientific evidence frequently, but she reserves an equal or greater portion of her cognitive bandwidth for the patient she is caring for at a particular moment.
How might the observations of this case study help to derive meaning from the study by Dr. Tsugawa and his associates, so that all patients may benefit from whatever it is that female physicians do to achieve better outcomes?
First, if physicians – regardless of gender – simply have an awareness of anchoring bias or rushing to land on a diagnosis or treatment, they will be less likely to do so in the future.
Next, we can learn that avoiding overwork can make for more joy in work, and if this is so, our patients may fare better. When I say “avoiding overwork,” that might mean rethinking our assumptions underlying the amount of work we take on.
Finally, while amassing a large fund of knowledge is a good thing, balancing medical knowledge with knowledge of the individual patient is crucial to good medical practice.
Dr. Whitcomb is Chief Medical Officer at Remedy Partners in Darien, CT. He is a cofounder and past president of SHM. Email him at [email protected].
SHM launches Chapter Development Fund to enhance reach, impact of chapters
As hospital medicine continues to experience unparalleled growth, the Society of Hospital Medicine (SHM) seeks to supplement its chapter program via a new $100,000 Chapter Development Fund. The monies will be used to further enhance the reach and impact of SHM’s 50 regional chapters.
Chapters can request up to $5,000 from the fund annually to support projects that promote networking, education, leadership opportunities, and improvements in health care delivery. In addition to growing the chapters, SHM expects that the additional resources will help facilitate relationships with local hospitals and medical schools, and demonstrate the value of membership.
“Chapters that were struggling now feel that they have the support they need to improve, and the ones that have figured out the basics can push their creative limits. That innovation can be passed along and benefit [all chapters],” Dr. Thompson said.
Fund usage already has led to a number of success stories (see Figure 1). During the program’s pilot phase, six chapters – Gulf States, Iowa, Los Angeles, Michigan, New Mexico, and San Francisco – acquired 77 new SHM members through a variety of innovative methods.
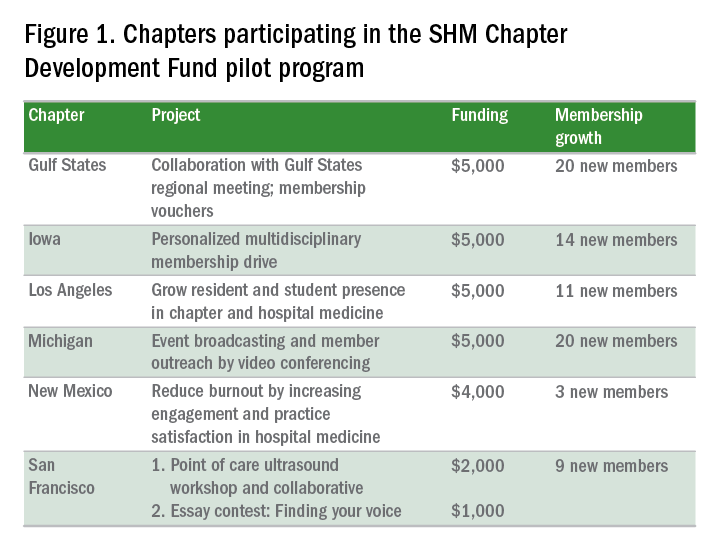
“We were struggling in recruitment, and saw this as an opportunity to attract members,” said chapter leader Venkataraman Palabindala, MD. “We used the funds to create 15 ‘coupons’ for membership. The rest of the money [was used] to start a regional meeting … where chapter leaders were invited to lead talks. [The meeting] really helped us.”
Another example of success comes from the Iowa Chapter, which attracted 14 new members through a multidisciplinary membership drive.
“We … requested funding for a few specific areas. One was marketing, where we had fliers written up to target specific groups, including … students, APPs (advanced practice practitioners), residents, students, and pharmacists, as well as other physicians,” said chapter leader Melinda Johnson, MD, SFHM.
The Iowa Chapter also used funding for SHM-branded “giveaways” (coffee mugs, portable chargers, etc.) to leave behind during meetings with prospective members. Vouchers, offering a 50% discount on a 1-year membership for new members during the pilot program, were especially effective. The combined activities “really increased visibility for SHM within our state and with disciplines besides physicians,” Dr. Johnson said.
Chapters can apply for support on a rolling basis by submitting a proposal to the Chapter Support Committee. For the full details, visit www.hospitalmedicine.org/chapterdevelopment.
When thinking about ideas, Dr. Thompson advises chapters to begin with “a brainstorm of all of the … exciting things that you have wanted to do for your membership. Then think about the ones that are attainable, and map out how to get there. The pilot showed that in a short time, you can reach many people when you plan your project out with timing and specific goals … and let the committee support you.”
In addition to a financial boost, fund recipients enjoy personalized mentorship from the committee, a benefit that both Dr. Johnson and Dr. Palabindala found invaluable. For new and developing chapters, “the support you get, the money, as well as the goal setting and feedback, is amazing,” Dr. Palabindala said.
Chapters, Dr. Johnson said, provide members with networking and leadership opportunities – and ensure that the unique, localized needs of their communities are represented at SHM.
“They become your professional home, providing opportunities,” she said, “that improve personal and professional satisfaction. Anyone is welcome to participate in the conversation.”
For more information on how you can become involved in an SHM chapter, visit www.hospitalmedicine.org/chapters.
Claudia Stahl is a content manager for the Society of Hospital Medicine.
As hospital medicine continues to experience unparalleled growth, the Society of Hospital Medicine (SHM) seeks to supplement its chapter program via a new $100,000 Chapter Development Fund. The monies will be used to further enhance the reach and impact of SHM’s 50 regional chapters.
Chapters can request up to $5,000 from the fund annually to support projects that promote networking, education, leadership opportunities, and improvements in health care delivery. In addition to growing the chapters, SHM expects that the additional resources will help facilitate relationships with local hospitals and medical schools, and demonstrate the value of membership.
“Chapters that were struggling now feel that they have the support they need to improve, and the ones that have figured out the basics can push their creative limits. That innovation can be passed along and benefit [all chapters],” Dr. Thompson said.
Fund usage already has led to a number of success stories (see Figure 1). During the program’s pilot phase, six chapters – Gulf States, Iowa, Los Angeles, Michigan, New Mexico, and San Francisco – acquired 77 new SHM members through a variety of innovative methods.
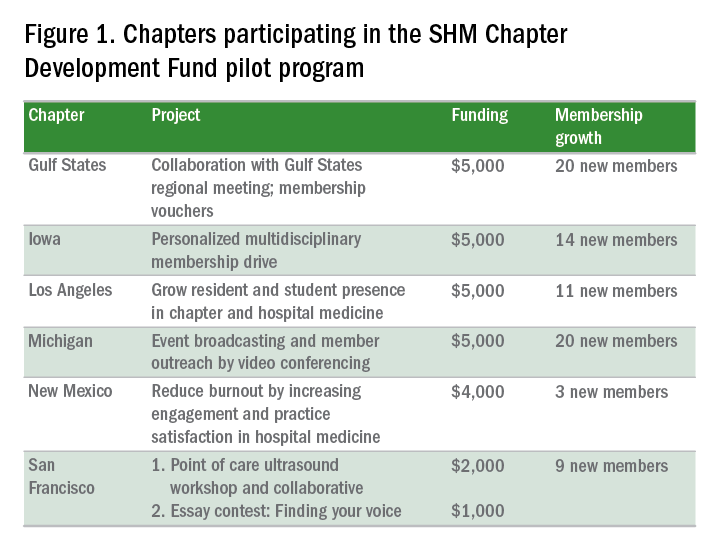
“We were struggling in recruitment, and saw this as an opportunity to attract members,” said chapter leader Venkataraman Palabindala, MD. “We used the funds to create 15 ‘coupons’ for membership. The rest of the money [was used] to start a regional meeting … where chapter leaders were invited to lead talks. [The meeting] really helped us.”
Another example of success comes from the Iowa Chapter, which attracted 14 new members through a multidisciplinary membership drive.
“We … requested funding for a few specific areas. One was marketing, where we had fliers written up to target specific groups, including … students, APPs (advanced practice practitioners), residents, students, and pharmacists, as well as other physicians,” said chapter leader Melinda Johnson, MD, SFHM.
The Iowa Chapter also used funding for SHM-branded “giveaways” (coffee mugs, portable chargers, etc.) to leave behind during meetings with prospective members. Vouchers, offering a 50% discount on a 1-year membership for new members during the pilot program, were especially effective. The combined activities “really increased visibility for SHM within our state and with disciplines besides physicians,” Dr. Johnson said.
Chapters can apply for support on a rolling basis by submitting a proposal to the Chapter Support Committee. For the full details, visit www.hospitalmedicine.org/chapterdevelopment.
When thinking about ideas, Dr. Thompson advises chapters to begin with “a brainstorm of all of the … exciting things that you have wanted to do for your membership. Then think about the ones that are attainable, and map out how to get there. The pilot showed that in a short time, you can reach many people when you plan your project out with timing and specific goals … and let the committee support you.”
In addition to a financial boost, fund recipients enjoy personalized mentorship from the committee, a benefit that both Dr. Johnson and Dr. Palabindala found invaluable. For new and developing chapters, “the support you get, the money, as well as the goal setting and feedback, is amazing,” Dr. Palabindala said.
Chapters, Dr. Johnson said, provide members with networking and leadership opportunities – and ensure that the unique, localized needs of their communities are represented at SHM.
“They become your professional home, providing opportunities,” she said, “that improve personal and professional satisfaction. Anyone is welcome to participate in the conversation.”
For more information on how you can become involved in an SHM chapter, visit www.hospitalmedicine.org/chapters.
Claudia Stahl is a content manager for the Society of Hospital Medicine.
As hospital medicine continues to experience unparalleled growth, the Society of Hospital Medicine (SHM) seeks to supplement its chapter program via a new $100,000 Chapter Development Fund. The monies will be used to further enhance the reach and impact of SHM’s 50 regional chapters.
Chapters can request up to $5,000 from the fund annually to support projects that promote networking, education, leadership opportunities, and improvements in health care delivery. In addition to growing the chapters, SHM expects that the additional resources will help facilitate relationships with local hospitals and medical schools, and demonstrate the value of membership.
“Chapters that were struggling now feel that they have the support they need to improve, and the ones that have figured out the basics can push their creative limits. That innovation can be passed along and benefit [all chapters],” Dr. Thompson said.
Fund usage already has led to a number of success stories (see Figure 1). During the program’s pilot phase, six chapters – Gulf States, Iowa, Los Angeles, Michigan, New Mexico, and San Francisco – acquired 77 new SHM members through a variety of innovative methods.
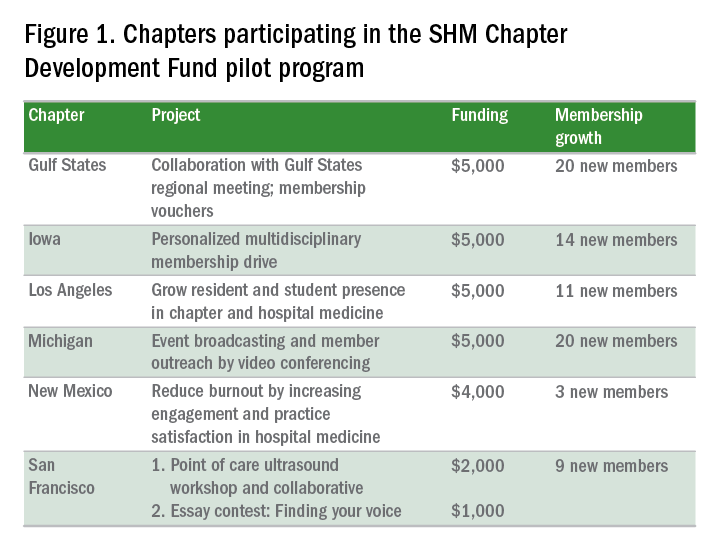
“We were struggling in recruitment, and saw this as an opportunity to attract members,” said chapter leader Venkataraman Palabindala, MD. “We used the funds to create 15 ‘coupons’ for membership. The rest of the money [was used] to start a regional meeting … where chapter leaders were invited to lead talks. [The meeting] really helped us.”
Another example of success comes from the Iowa Chapter, which attracted 14 new members through a multidisciplinary membership drive.
“We … requested funding for a few specific areas. One was marketing, where we had fliers written up to target specific groups, including … students, APPs (advanced practice practitioners), residents, students, and pharmacists, as well as other physicians,” said chapter leader Melinda Johnson, MD, SFHM.
The Iowa Chapter also used funding for SHM-branded “giveaways” (coffee mugs, portable chargers, etc.) to leave behind during meetings with prospective members. Vouchers, offering a 50% discount on a 1-year membership for new members during the pilot program, were especially effective. The combined activities “really increased visibility for SHM within our state and with disciplines besides physicians,” Dr. Johnson said.
Chapters can apply for support on a rolling basis by submitting a proposal to the Chapter Support Committee. For the full details, visit www.hospitalmedicine.org/chapterdevelopment.
When thinking about ideas, Dr. Thompson advises chapters to begin with “a brainstorm of all of the … exciting things that you have wanted to do for your membership. Then think about the ones that are attainable, and map out how to get there. The pilot showed that in a short time, you can reach many people when you plan your project out with timing and specific goals … and let the committee support you.”
In addition to a financial boost, fund recipients enjoy personalized mentorship from the committee, a benefit that both Dr. Johnson and Dr. Palabindala found invaluable. For new and developing chapters, “the support you get, the money, as well as the goal setting and feedback, is amazing,” Dr. Palabindala said.
Chapters, Dr. Johnson said, provide members with networking and leadership opportunities – and ensure that the unique, localized needs of their communities are represented at SHM.
“They become your professional home, providing opportunities,” she said, “that improve personal and professional satisfaction. Anyone is welcome to participate in the conversation.”
For more information on how you can become involved in an SHM chapter, visit www.hospitalmedicine.org/chapters.
Claudia Stahl is a content manager for the Society of Hospital Medicine.
SHM Practice Administrators’ Mentor Program benefits both parties
Editor’s note: Each month, SHM puts the spotlight on our most active members and explores how they are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise and help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Alessandra G. Cornelio, MPH, the acquisition manager at Hartford Healthcare Medical Group in Connecticut. Ms. Cornelio is an active member of SHM’s Practice Administrators Committee. She developed and now directs the Practice Administrators’ Mentor Program.
Answer: I was finishing my internship at the Middlesex Hospital Cancer Center. I was interested in hospital administration and learning more about the inpatient side of health care. I chose to work within hospital medicine because I wanted to help build a team of compassionate doctors who could provide an excellent patient experience while maintaining an environment with safe, high-quality care.
To complement my career goals, SHM helped my professional growth by exposing me to the variety of topics and issues that practice administrators deal with regularly in their practices. I was also able to review and learn from the many resources available on the SHM website, such as white papers and articles, which were extremely useful for a new administrator.
Q: What prompted you to join the Practice Administrators Committee? What are some of the most impactful projects the committee is currently working on?
A: Within my first year of being a practice administrator, I attended a practice administrators’ forum at the SHM annual meeting in Washington. I found that the information was relevant to my daily functions as an administrator, and I was also able to meet and share ideas with other practice administrators from throughout the country. Down the line, I learned that SHM needed new members for the Practice Administrators Committee. I wanted to become more involved in a meaningful way, so I decided to apply.
The Practice Administrators Committee is a hardworking committee that takes on many meaningful projects. Most recently, the team has been working on developing a more user-friendly website for practice administrators, and a subgroup of the committee has cross-referenced “The Key Principles and Characteristics of an Effective Hospital Medicine Group” with existing resources, which will prove valuable to all administrators in the final product.
Q: Can you discuss how you began leading the work group for the Practice Administrators’ Mentor Program and how it has evolved since its inception?
A: As part of the committee’s initiative to help fellow practice administrators, we formed a subcommittee to begin developing a mentor program. (Former SHM staffer) Joseph Miller and I worked together to create an appropriate program model through research and brainstorming. We also utilized the HMX Practice Administrators Community to ask fellow practice administrators what they would expect from a mentor program and if they would participate. There was a strong favorable response rate, and we were able to implement a pilot program.
We implemented two different tracks for the program – the buddy system track and the career development track. The buddy system track is for those of any level of expertise or experience who are more interested in short-term assistance or in need of a sounding board. The career development track is a more traditional approach, matching a seasoned practice administrator with a less experienced practice administrator.
The program was designed to have annual cohorts, with the Practice Administrators Committee members as mentors. There is a detailed application process to ensure that each mentee is matched with an appropriate mentor, based on their interests and needs. We provide an orientation webinar to both parties before kicking off the relationship to present program expectations. The pilot program used this model, and comments from 6-month and annual evaluations showed tremendous satisfaction with the structure and value of this program.
There were approximately 16 pairs during the pilot year, and the following year, we grew to almost 20 pairs. Our goal as a committee is to maintain this program year after year, and in order to expand, we’ll need more than just the committee members to volunteer as mentors. There are so many talented practice administrators, and it would be wonderful to fold them into this gratifying program to pay it forward.
Many mentors, including myself, found value in acting as a mentor. I learned from my mentees as well as made connections and friendships with other professionals in the field.
Q: Given your intimate involvement, how have you seen the Practice Administrators’ Mentor Program benefit both the mentors and the mentees? Can you provide any specific examples?
A: Mentees are able to connect with seasoned mentors and can ask specific questions about career development and any issues they may be experiencing. Mentors are able to share their experiences and pass along important and valuable lessons learned to mentees. I served as a mentor, even though I did not yet consider myself a qualified candidate. However, I found that I was more equipped than I had realized, and I was able to assist my mentee with many aspects of career development (i.e., resume building, discussions with the C-suite, etc.).
My mentee was a practice coordinator who had only been in hospital medicine for 1 year. She had little experience hiring hospitalists, so this was a major area that we worked on together during our yearlong connection. I introduced her to collaborating with her HR department when posting positions, as well as working with permanent placement agencies. Her service was also undergoing a change in leadership, which can be difficult for any service line to experience. We discussed ways in which she could present important information to the new medical director that would produce a meaningful conversation.
In turn, my mentee introduced me to new online resources and was able to connect me with the manager of her practice, who assisted me with streamlining the payroll structure in my practice. I truly enjoyed my experience developing and participating in the program.
Felicia Steele is SHM’s communications coordinator.
Learn more about how you can benefit from the Practice Administrators’ Mentor program via the SHM website.
Editor’s note: Each month, SHM puts the spotlight on our most active members and explores how they are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise and help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Alessandra G. Cornelio, MPH, the acquisition manager at Hartford Healthcare Medical Group in Connecticut. Ms. Cornelio is an active member of SHM’s Practice Administrators Committee. She developed and now directs the Practice Administrators’ Mentor Program.
Answer: I was finishing my internship at the Middlesex Hospital Cancer Center. I was interested in hospital administration and learning more about the inpatient side of health care. I chose to work within hospital medicine because I wanted to help build a team of compassionate doctors who could provide an excellent patient experience while maintaining an environment with safe, high-quality care.
To complement my career goals, SHM helped my professional growth by exposing me to the variety of topics and issues that practice administrators deal with regularly in their practices. I was also able to review and learn from the many resources available on the SHM website, such as white papers and articles, which were extremely useful for a new administrator.
Q: What prompted you to join the Practice Administrators Committee? What are some of the most impactful projects the committee is currently working on?
A: Within my first year of being a practice administrator, I attended a practice administrators’ forum at the SHM annual meeting in Washington. I found that the information was relevant to my daily functions as an administrator, and I was also able to meet and share ideas with other practice administrators from throughout the country. Down the line, I learned that SHM needed new members for the Practice Administrators Committee. I wanted to become more involved in a meaningful way, so I decided to apply.
The Practice Administrators Committee is a hardworking committee that takes on many meaningful projects. Most recently, the team has been working on developing a more user-friendly website for practice administrators, and a subgroup of the committee has cross-referenced “The Key Principles and Characteristics of an Effective Hospital Medicine Group” with existing resources, which will prove valuable to all administrators in the final product.
Q: Can you discuss how you began leading the work group for the Practice Administrators’ Mentor Program and how it has evolved since its inception?
A: As part of the committee’s initiative to help fellow practice administrators, we formed a subcommittee to begin developing a mentor program. (Former SHM staffer) Joseph Miller and I worked together to create an appropriate program model through research and brainstorming. We also utilized the HMX Practice Administrators Community to ask fellow practice administrators what they would expect from a mentor program and if they would participate. There was a strong favorable response rate, and we were able to implement a pilot program.
We implemented two different tracks for the program – the buddy system track and the career development track. The buddy system track is for those of any level of expertise or experience who are more interested in short-term assistance or in need of a sounding board. The career development track is a more traditional approach, matching a seasoned practice administrator with a less experienced practice administrator.
The program was designed to have annual cohorts, with the Practice Administrators Committee members as mentors. There is a detailed application process to ensure that each mentee is matched with an appropriate mentor, based on their interests and needs. We provide an orientation webinar to both parties before kicking off the relationship to present program expectations. The pilot program used this model, and comments from 6-month and annual evaluations showed tremendous satisfaction with the structure and value of this program.
There were approximately 16 pairs during the pilot year, and the following year, we grew to almost 20 pairs. Our goal as a committee is to maintain this program year after year, and in order to expand, we’ll need more than just the committee members to volunteer as mentors. There are so many talented practice administrators, and it would be wonderful to fold them into this gratifying program to pay it forward.
Many mentors, including myself, found value in acting as a mentor. I learned from my mentees as well as made connections and friendships with other professionals in the field.
Q: Given your intimate involvement, how have you seen the Practice Administrators’ Mentor Program benefit both the mentors and the mentees? Can you provide any specific examples?
A: Mentees are able to connect with seasoned mentors and can ask specific questions about career development and any issues they may be experiencing. Mentors are able to share their experiences and pass along important and valuable lessons learned to mentees. I served as a mentor, even though I did not yet consider myself a qualified candidate. However, I found that I was more equipped than I had realized, and I was able to assist my mentee with many aspects of career development (i.e., resume building, discussions with the C-suite, etc.).
My mentee was a practice coordinator who had only been in hospital medicine for 1 year. She had little experience hiring hospitalists, so this was a major area that we worked on together during our yearlong connection. I introduced her to collaborating with her HR department when posting positions, as well as working with permanent placement agencies. Her service was also undergoing a change in leadership, which can be difficult for any service line to experience. We discussed ways in which she could present important information to the new medical director that would produce a meaningful conversation.
In turn, my mentee introduced me to new online resources and was able to connect me with the manager of her practice, who assisted me with streamlining the payroll structure in my practice. I truly enjoyed my experience developing and participating in the program.
Felicia Steele is SHM’s communications coordinator.
Learn more about how you can benefit from the Practice Administrators’ Mentor program via the SHM website.
Editor’s note: Each month, SHM puts the spotlight on our most active members and explores how they are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org/getinvolved for more information on how you can lend your expertise and help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Alessandra G. Cornelio, MPH, the acquisition manager at Hartford Healthcare Medical Group in Connecticut. Ms. Cornelio is an active member of SHM’s Practice Administrators Committee. She developed and now directs the Practice Administrators’ Mentor Program.
Answer: I was finishing my internship at the Middlesex Hospital Cancer Center. I was interested in hospital administration and learning more about the inpatient side of health care. I chose to work within hospital medicine because I wanted to help build a team of compassionate doctors who could provide an excellent patient experience while maintaining an environment with safe, high-quality care.
To complement my career goals, SHM helped my professional growth by exposing me to the variety of topics and issues that practice administrators deal with regularly in their practices. I was also able to review and learn from the many resources available on the SHM website, such as white papers and articles, which were extremely useful for a new administrator.
Q: What prompted you to join the Practice Administrators Committee? What are some of the most impactful projects the committee is currently working on?
A: Within my first year of being a practice administrator, I attended a practice administrators’ forum at the SHM annual meeting in Washington. I found that the information was relevant to my daily functions as an administrator, and I was also able to meet and share ideas with other practice administrators from throughout the country. Down the line, I learned that SHM needed new members for the Practice Administrators Committee. I wanted to become more involved in a meaningful way, so I decided to apply.
The Practice Administrators Committee is a hardworking committee that takes on many meaningful projects. Most recently, the team has been working on developing a more user-friendly website for practice administrators, and a subgroup of the committee has cross-referenced “The Key Principles and Characteristics of an Effective Hospital Medicine Group” with existing resources, which will prove valuable to all administrators in the final product.
Q: Can you discuss how you began leading the work group for the Practice Administrators’ Mentor Program and how it has evolved since its inception?
A: As part of the committee’s initiative to help fellow practice administrators, we formed a subcommittee to begin developing a mentor program. (Former SHM staffer) Joseph Miller and I worked together to create an appropriate program model through research and brainstorming. We also utilized the HMX Practice Administrators Community to ask fellow practice administrators what they would expect from a mentor program and if they would participate. There was a strong favorable response rate, and we were able to implement a pilot program.
We implemented two different tracks for the program – the buddy system track and the career development track. The buddy system track is for those of any level of expertise or experience who are more interested in short-term assistance or in need of a sounding board. The career development track is a more traditional approach, matching a seasoned practice administrator with a less experienced practice administrator.
The program was designed to have annual cohorts, with the Practice Administrators Committee members as mentors. There is a detailed application process to ensure that each mentee is matched with an appropriate mentor, based on their interests and needs. We provide an orientation webinar to both parties before kicking off the relationship to present program expectations. The pilot program used this model, and comments from 6-month and annual evaluations showed tremendous satisfaction with the structure and value of this program.
There were approximately 16 pairs during the pilot year, and the following year, we grew to almost 20 pairs. Our goal as a committee is to maintain this program year after year, and in order to expand, we’ll need more than just the committee members to volunteer as mentors. There are so many talented practice administrators, and it would be wonderful to fold them into this gratifying program to pay it forward.
Many mentors, including myself, found value in acting as a mentor. I learned from my mentees as well as made connections and friendships with other professionals in the field.
Q: Given your intimate involvement, how have you seen the Practice Administrators’ Mentor Program benefit both the mentors and the mentees? Can you provide any specific examples?
A: Mentees are able to connect with seasoned mentors and can ask specific questions about career development and any issues they may be experiencing. Mentors are able to share their experiences and pass along important and valuable lessons learned to mentees. I served as a mentor, even though I did not yet consider myself a qualified candidate. However, I found that I was more equipped than I had realized, and I was able to assist my mentee with many aspects of career development (i.e., resume building, discussions with the C-suite, etc.).
My mentee was a practice coordinator who had only been in hospital medicine for 1 year. She had little experience hiring hospitalists, so this was a major area that we worked on together during our yearlong connection. I introduced her to collaborating with her HR department when posting positions, as well as working with permanent placement agencies. Her service was also undergoing a change in leadership, which can be difficult for any service line to experience. We discussed ways in which she could present important information to the new medical director that would produce a meaningful conversation.
In turn, my mentee introduced me to new online resources and was able to connect me with the manager of her practice, who assisted me with streamlining the payroll structure in my practice. I truly enjoyed my experience developing and participating in the program.
Felicia Steele is SHM’s communications coordinator.
Learn more about how you can benefit from the Practice Administrators’ Mentor program via the SHM website.
SHM welcomes its newest members - January 2017
Justin Kimsey, Alabama
Mohammed N.Y. Shah, MD, Alaska
Katharina Beeler, MD, Arizona
Khoi Nguyen, MD, Arizona
Vinay Saini, MD, Arizona
Maria Aceves, PA-C, California
Sarvenaz Alibeigi, California
Peter Cadman, MD, California
Katrina Chapman, DO, MPH, California
Cheryll Gallardo-Villena, MD, California
Sripriya Ganesan, California
Alice Gong, MD, California
Henry Kwang, MD, California
Kevin Li, California
Anthony Murphy, MD, California
Dan Nguyen, California
Daniel Oh, California
Joon Parle, California
Katie Raffel, California
Darshana Sarathchandra, MD, California
Lifang Zhang, California
Jaime Baker, MD, Colorado
Eric Johnson, PA-C, Colorado
Juan Lessing, MD, Colorado
Benjamin Ruckman, DO, Colorado
Rehaan Shaffie, MD, Colorado
Deborah Casey, MD, Connecticut
Daniel Heacock, PA-C, Connecticut
Shabana Ansari, DO, Delaware
Madhu Prattipati, MD, Delaware
Pallavi Aneja, MD, Florida
Satcha Borgella, MD, Florida
Thendrex H. Estrella, MD, Florida
Abid Hussain, MD, Florida
Daphnee Hutchinson, DO, Florida
Muhammad Jaffer, Florida
Sue Lee, ANP, Florida
Melissa Odermann, DO, Florida
Jose Guillermo Revelo Paiz, MD, Florida
Rafael J. Rolon Rivera, MD, Florida
Eleonor Rongo, Florida
Esther Roth, Florida
Shitaye Argaw, MD, Georgia
Taryn DeGrazia, Georgia
Becca Feistritzer, Georgia
Jamal Fitts, Georgia
Kristen Flint, Georgia
Zachary Hermes, Georgia
Mukesh Kumar, Georgia
Kajal Patel, Georgia
Madeline Smith, Georgia
Wade Flowers, PharmD, Idaho
Ajay Bhandare, Illinois
Kimberly Brighton, Illinois
Hristo D. Hristov, MD, Illinois
Sidney Iriana, Illinois
Aurelian Ivan, Illinois
Ming Lee, MD, Illinois
Michelle Lundholm, Illinois
Idrees Mohiuddin, MD, Illinois
Murr Murray, Illinois
Tad Nair, MD, Illinois
Shalini Reddy, MD, Illinois
Richard Rethorst, MD, Illinois
Kelly Robertshaw, Illinois
Gracelene Wegrzyn, Illinois
Evan Yates, Illinois
Lora J. Jones McClure, MD, Indiana
Carleigh Wilson, DO, Indiana
Erin Brown, ARNP, Iowa
Adam Gray, Iowa
Paul Greco, MD, Iowa
Shelly McGurk, ACNP, ARNP, Iowa
Julie Stanik-Hutt, ACNP, CNS, PhD, Iowa
Elizabeth Cozad, DO, Kansas
Roshan Pais, Kentucky
Mark Youssef, MD, Kentucky
Heather Kahn, MD, Louisiana
Danielle Parrott, PA-C, Maine
Erica Lafferty, ACNP, Maryland
Andrea Limpuangthip, Maryland
Steven Schwartz, CCM, MD, Maryland
Eisha Azhar, MBBS, Massachusetts
Badal Kalamkar, MD, MPH, Massachusetts
Bhavya Rajanna, MD, Massachusetts
Sahib Baljinder Singh, MD, Massachusetts
Kathryn Adams, Michigan
Haseeb Aslam, MD, MBBS, Michigan
Hilda Crispin, MD, Michigan
Sharmistha Dev, MD, Michigan
Tristan Feierabend, MD, Michigan
Sonal Kamalia, MD, MBBS, Michigan
Matthew Luzum, MD, Michigan
Daniel Mitzel, MD, Michigan
Richard Raad, Michigan
Mythri Ramegowda, MD, Michigan
Katie Scally, MD, Michigan
Linden Spital, MSN, NP, Michigan
Porama Koy Thanaporn, MD, Michigan
Chanteil Ulatowski, Michigan
Tingting Xiong, MD, Michigan
Adam Zahr, Michigan
Mike Beste, MD, Minnesota
Elise Haupt, PA-C, Minnesota
Lobsang Trasar, MD, Minnesota
Kari Goan, DO, Mississippi
David C. Pierre, Mississippi
Sudheer Tangella, MD, Mississippi
Tahani Atieh, Missouri
Nicholas Arnold, Missouri
Amanda Calhoun, Missouri
Jyotirmoy Das, Missouri
Umber Dube, Missouri
Daniel Gaughan, Missouri
Woojin Joo, Missouri
Khaled Jumean, MBBS, Missouri
Salma Kazmi, MBBS, MD, Missouri
Yoon Kook (Danny) Kim, Missouri
Ryan Kronen, Missouri
Alyssa Kroner, Missouri
Randy Laine, Missouri
Edward Lee, Missouri
Cerena Leung, Missouri
Patricia Lithrow, Missouri
Brandt Lydon, Missouri
Mary Morgan Scott, Missouri
Jay Patel, Missouri
Justin Porter, Missouri
Danelle Reagin, FNP-C, Missouri
Amanda Reis, Missouri
Awik Som, Missouri
Abby Sung, Missouri
Mary Sutherland, Missouri
Maggie Wang, Missouri
Noah Wasserman, Missouri
Alexis Webber, Missouri
Ryan White, Missouri
Amy Xu, Missouri
Ran Xu, Missouri
Michael Yang, Missouri
Christopher Dietrich, MD, Montana
Jason Kunz, DO, Montana
Jodi Cantrell, MD, Nebraska
Steven Hart, MD, Nebraska
Kurt Kapels, MD, Nebraska
Brian Keegan, MD, Nebraska
Shaun Jang, MD, Nevada
Gurpinder Singh, MD, New Hampshire
Pragati Banda, MD, New Jersey
Sahai Donaldson, MBBS, New Jersey
Ashesha Mechineni, MD, New Jersey
Alisa Clark, New Mexico
Prajit Arora, MBBS, New Mexico
Crystal Cardwell, New Mexico
Landon Casaus, New Mexico
Tapuwa Mupfumira, MD, New Mexico
Eric Rightley, New Mexico
David S. Anderson, New York
Joan Bosco, MD, New York
Jessica Caro, New York
Anna Dewan, New York
Amrita Dhillon, MBBS, New York
Julia Frydman, New York
Radhika Gali, MBBS, MDS, New York
Allison Guttmann, MD, New York
Aryles Hedjar, MD, New York
Peter Janes, New York
Nadine Kalavazoff, New York
Jeffrey Lach, DO, New York
Keron Lezama, MD, New York
Yingheng Liu, New York
Taimur Mirza, New York
Cyrus Nensey, MD, New York
Nekee Pandya, MD, New York
Thushara Paul, MD, New York
Yu Sung, New York
Joel Boggan, MD, North Carolina
Angela Fletcher, North Carolina
Rebecca Gimpert, PA-C, North Carolina
Samantha Levering, PA-C, North Carolina
Nancy Martin, North Carolina
Richard Sherwood, North Carolina
Kranthi K. Sitammagari, MD, North Carolina
Aaron Swedberg, MPAS, PA-C, North Carolina
Yih-Cherng Tsai, North Carolina
Richard Bakker, MD, PhD, Ohio
Matthew Broderick, MD, Ohio
Subbaraju Budharaju, MD, MS, Ohio
Steven Bumb, MD, Ohio
Ahmed Eltelbany, MD, Ohio
Tracey Hardin, MS, Ohio
Patricia Hardman, APRN, Ohio
Michael Lewis, MD, Ohio
Volodymyr Manko, Ohio
Rebecca Stone, Ohio
Chaitanya Valluri, Ohio
Holly Wierzbicki, CNP, Ohio
Jamie Yockey, APRN, CNP, Ohio
Mahdi Mussa, MD, Oklahoma
Monica Saemz, DO, Oklahoma
Peter Ganter, MD, Oregon
Bethany Roy, MD, Oregon
Mary Clare Bohnett, Oregon
Molly Rabinowitz, Oregon
Abdullateef Abdulkareem, MD, MPH, Pennsylvania
David Ahamba, MD, MPH, Pennsylvania
David Chin, MD, Pennsylvania
Thomas Conlon, Pennsylvania
Dan Giesler, MD, Pennsylvania
Umair Randhawa, MD, Pennsylvania
Syed Yusuf, MBBS, Pennsylvania
Michael Rigatti, Pennsylvania
Thaylon Barreto, Rhode Island
Jessica Cook, MD, South Carolina
Robin Malik, MD, South Carolina
John Busigin, Tennessee
Shefali Paranjape, MD, Tennessee
Thai Dang, MD, Texas
Matthew Glover, MD, Texas
Snigdha Jain, MD, Texas
David Kellenberger, Texas
Sumeet Kumar, Texas
Kyle McClendon, PA-C, Texas
Sowjanya Mohan, Texas
Akhil D. Vats, MD, Texas
Samatha Vellanki, Texas
Lee-Anna Burgess, MD, Vermont
Rick Hildebrant, MD, Vermont
Matthew Backens, MD, Virginia
Megan Coe, Virginia
Kevin Dehaan, Virginia
Stephen Fox, Virginia
Amber Inofuentes, MD, Virginia
Jessica Keiser, MD, Virginia
Joseph Perez, MD, FAAFP, MBA, Virginia
Kanwapreet S. Saini, MD, Virginia
Erin Vipler, MD, Virginia
Naveen Voore, MBBS, Virginia
Abhishek Agarwal, MD, MBBS, Washington
Robert Cooney, MD, Washington
Cynthia Horton, MD, Washington
Rich A. Kukreja, MD, Washington
Ji Young Nam, MD, Washington
Kai Wilhelm, MD, Washington
In Kyu Yoo, Washington
Temu Brown, Wisconsin
Pablo Colon Nieves, Wisconsin
Christina Evans, PAC, Wisconsin
Swetha Karturi, MBBS, Wisconsin
Mark Babcock, DO, Wyoming
Ahmad Von Schlegell, Canada
Anand Kartha, Japan
Mohamed Sadek, Qatar
Amine Rakab, MD, Qatar
Abazar Saeed, Qatar
Joao Guerra, MD
Justin Kimsey, Alabama
Mohammed N.Y. Shah, MD, Alaska
Katharina Beeler, MD, Arizona
Khoi Nguyen, MD, Arizona
Vinay Saini, MD, Arizona
Maria Aceves, PA-C, California
Sarvenaz Alibeigi, California
Peter Cadman, MD, California
Katrina Chapman, DO, MPH, California
Cheryll Gallardo-Villena, MD, California
Sripriya Ganesan, California
Alice Gong, MD, California
Henry Kwang, MD, California
Kevin Li, California
Anthony Murphy, MD, California
Dan Nguyen, California
Daniel Oh, California
Joon Parle, California
Katie Raffel, California
Darshana Sarathchandra, MD, California
Lifang Zhang, California
Jaime Baker, MD, Colorado
Eric Johnson, PA-C, Colorado
Juan Lessing, MD, Colorado
Benjamin Ruckman, DO, Colorado
Rehaan Shaffie, MD, Colorado
Deborah Casey, MD, Connecticut
Daniel Heacock, PA-C, Connecticut
Shabana Ansari, DO, Delaware
Madhu Prattipati, MD, Delaware
Pallavi Aneja, MD, Florida
Satcha Borgella, MD, Florida
Thendrex H. Estrella, MD, Florida
Abid Hussain, MD, Florida
Daphnee Hutchinson, DO, Florida
Muhammad Jaffer, Florida
Sue Lee, ANP, Florida
Melissa Odermann, DO, Florida
Jose Guillermo Revelo Paiz, MD, Florida
Rafael J. Rolon Rivera, MD, Florida
Eleonor Rongo, Florida
Esther Roth, Florida
Shitaye Argaw, MD, Georgia
Taryn DeGrazia, Georgia
Becca Feistritzer, Georgia
Jamal Fitts, Georgia
Kristen Flint, Georgia
Zachary Hermes, Georgia
Mukesh Kumar, Georgia
Kajal Patel, Georgia
Madeline Smith, Georgia
Wade Flowers, PharmD, Idaho
Ajay Bhandare, Illinois
Kimberly Brighton, Illinois
Hristo D. Hristov, MD, Illinois
Sidney Iriana, Illinois
Aurelian Ivan, Illinois
Ming Lee, MD, Illinois
Michelle Lundholm, Illinois
Idrees Mohiuddin, MD, Illinois
Murr Murray, Illinois
Tad Nair, MD, Illinois
Shalini Reddy, MD, Illinois
Richard Rethorst, MD, Illinois
Kelly Robertshaw, Illinois
Gracelene Wegrzyn, Illinois
Evan Yates, Illinois
Lora J. Jones McClure, MD, Indiana
Carleigh Wilson, DO, Indiana
Erin Brown, ARNP, Iowa
Adam Gray, Iowa
Paul Greco, MD, Iowa
Shelly McGurk, ACNP, ARNP, Iowa
Julie Stanik-Hutt, ACNP, CNS, PhD, Iowa
Elizabeth Cozad, DO, Kansas
Roshan Pais, Kentucky
Mark Youssef, MD, Kentucky
Heather Kahn, MD, Louisiana
Danielle Parrott, PA-C, Maine
Erica Lafferty, ACNP, Maryland
Andrea Limpuangthip, Maryland
Steven Schwartz, CCM, MD, Maryland
Eisha Azhar, MBBS, Massachusetts
Badal Kalamkar, MD, MPH, Massachusetts
Bhavya Rajanna, MD, Massachusetts
Sahib Baljinder Singh, MD, Massachusetts
Kathryn Adams, Michigan
Haseeb Aslam, MD, MBBS, Michigan
Hilda Crispin, MD, Michigan
Sharmistha Dev, MD, Michigan
Tristan Feierabend, MD, Michigan
Sonal Kamalia, MD, MBBS, Michigan
Matthew Luzum, MD, Michigan
Daniel Mitzel, MD, Michigan
Richard Raad, Michigan
Mythri Ramegowda, MD, Michigan
Katie Scally, MD, Michigan
Linden Spital, MSN, NP, Michigan
Porama Koy Thanaporn, MD, Michigan
Chanteil Ulatowski, Michigan
Tingting Xiong, MD, Michigan
Adam Zahr, Michigan
Mike Beste, MD, Minnesota
Elise Haupt, PA-C, Minnesota
Lobsang Trasar, MD, Minnesota
Kari Goan, DO, Mississippi
David C. Pierre, Mississippi
Sudheer Tangella, MD, Mississippi
Tahani Atieh, Missouri
Nicholas Arnold, Missouri
Amanda Calhoun, Missouri
Jyotirmoy Das, Missouri
Umber Dube, Missouri
Daniel Gaughan, Missouri
Woojin Joo, Missouri
Khaled Jumean, MBBS, Missouri
Salma Kazmi, MBBS, MD, Missouri
Yoon Kook (Danny) Kim, Missouri
Ryan Kronen, Missouri
Alyssa Kroner, Missouri
Randy Laine, Missouri
Edward Lee, Missouri
Cerena Leung, Missouri
Patricia Lithrow, Missouri
Brandt Lydon, Missouri
Mary Morgan Scott, Missouri
Jay Patel, Missouri
Justin Porter, Missouri
Danelle Reagin, FNP-C, Missouri
Amanda Reis, Missouri
Awik Som, Missouri
Abby Sung, Missouri
Mary Sutherland, Missouri
Maggie Wang, Missouri
Noah Wasserman, Missouri
Alexis Webber, Missouri
Ryan White, Missouri
Amy Xu, Missouri
Ran Xu, Missouri
Michael Yang, Missouri
Christopher Dietrich, MD, Montana
Jason Kunz, DO, Montana
Jodi Cantrell, MD, Nebraska
Steven Hart, MD, Nebraska
Kurt Kapels, MD, Nebraska
Brian Keegan, MD, Nebraska
Shaun Jang, MD, Nevada
Gurpinder Singh, MD, New Hampshire
Pragati Banda, MD, New Jersey
Sahai Donaldson, MBBS, New Jersey
Ashesha Mechineni, MD, New Jersey
Alisa Clark, New Mexico
Prajit Arora, MBBS, New Mexico
Crystal Cardwell, New Mexico
Landon Casaus, New Mexico
Tapuwa Mupfumira, MD, New Mexico
Eric Rightley, New Mexico
David S. Anderson, New York
Joan Bosco, MD, New York
Jessica Caro, New York
Anna Dewan, New York
Amrita Dhillon, MBBS, New York
Julia Frydman, New York
Radhika Gali, MBBS, MDS, New York
Allison Guttmann, MD, New York
Aryles Hedjar, MD, New York
Peter Janes, New York
Nadine Kalavazoff, New York
Jeffrey Lach, DO, New York
Keron Lezama, MD, New York
Yingheng Liu, New York
Taimur Mirza, New York
Cyrus Nensey, MD, New York
Nekee Pandya, MD, New York
Thushara Paul, MD, New York
Yu Sung, New York
Joel Boggan, MD, North Carolina
Angela Fletcher, North Carolina
Rebecca Gimpert, PA-C, North Carolina
Samantha Levering, PA-C, North Carolina
Nancy Martin, North Carolina
Richard Sherwood, North Carolina
Kranthi K. Sitammagari, MD, North Carolina
Aaron Swedberg, MPAS, PA-C, North Carolina
Yih-Cherng Tsai, North Carolina
Richard Bakker, MD, PhD, Ohio
Matthew Broderick, MD, Ohio
Subbaraju Budharaju, MD, MS, Ohio
Steven Bumb, MD, Ohio
Ahmed Eltelbany, MD, Ohio
Tracey Hardin, MS, Ohio
Patricia Hardman, APRN, Ohio
Michael Lewis, MD, Ohio
Volodymyr Manko, Ohio
Rebecca Stone, Ohio
Chaitanya Valluri, Ohio
Holly Wierzbicki, CNP, Ohio
Jamie Yockey, APRN, CNP, Ohio
Mahdi Mussa, MD, Oklahoma
Monica Saemz, DO, Oklahoma
Peter Ganter, MD, Oregon
Bethany Roy, MD, Oregon
Mary Clare Bohnett, Oregon
Molly Rabinowitz, Oregon
Abdullateef Abdulkareem, MD, MPH, Pennsylvania
David Ahamba, MD, MPH, Pennsylvania
David Chin, MD, Pennsylvania
Thomas Conlon, Pennsylvania
Dan Giesler, MD, Pennsylvania
Umair Randhawa, MD, Pennsylvania
Syed Yusuf, MBBS, Pennsylvania
Michael Rigatti, Pennsylvania
Thaylon Barreto, Rhode Island
Jessica Cook, MD, South Carolina
Robin Malik, MD, South Carolina
John Busigin, Tennessee
Shefali Paranjape, MD, Tennessee
Thai Dang, MD, Texas
Matthew Glover, MD, Texas
Snigdha Jain, MD, Texas
David Kellenberger, Texas
Sumeet Kumar, Texas
Kyle McClendon, PA-C, Texas
Sowjanya Mohan, Texas
Akhil D. Vats, MD, Texas
Samatha Vellanki, Texas
Lee-Anna Burgess, MD, Vermont
Rick Hildebrant, MD, Vermont
Matthew Backens, MD, Virginia
Megan Coe, Virginia
Kevin Dehaan, Virginia
Stephen Fox, Virginia
Amber Inofuentes, MD, Virginia
Jessica Keiser, MD, Virginia
Joseph Perez, MD, FAAFP, MBA, Virginia
Kanwapreet S. Saini, MD, Virginia
Erin Vipler, MD, Virginia
Naveen Voore, MBBS, Virginia
Abhishek Agarwal, MD, MBBS, Washington
Robert Cooney, MD, Washington
Cynthia Horton, MD, Washington
Rich A. Kukreja, MD, Washington
Ji Young Nam, MD, Washington
Kai Wilhelm, MD, Washington
In Kyu Yoo, Washington
Temu Brown, Wisconsin
Pablo Colon Nieves, Wisconsin
Christina Evans, PAC, Wisconsin
Swetha Karturi, MBBS, Wisconsin
Mark Babcock, DO, Wyoming
Ahmad Von Schlegell, Canada
Anand Kartha, Japan
Mohamed Sadek, Qatar
Amine Rakab, MD, Qatar
Abazar Saeed, Qatar
Joao Guerra, MD
Justin Kimsey, Alabama
Mohammed N.Y. Shah, MD, Alaska
Katharina Beeler, MD, Arizona
Khoi Nguyen, MD, Arizona
Vinay Saini, MD, Arizona
Maria Aceves, PA-C, California
Sarvenaz Alibeigi, California
Peter Cadman, MD, California
Katrina Chapman, DO, MPH, California
Cheryll Gallardo-Villena, MD, California
Sripriya Ganesan, California
Alice Gong, MD, California
Henry Kwang, MD, California
Kevin Li, California
Anthony Murphy, MD, California
Dan Nguyen, California
Daniel Oh, California
Joon Parle, California
Katie Raffel, California
Darshana Sarathchandra, MD, California
Lifang Zhang, California
Jaime Baker, MD, Colorado
Eric Johnson, PA-C, Colorado
Juan Lessing, MD, Colorado
Benjamin Ruckman, DO, Colorado
Rehaan Shaffie, MD, Colorado
Deborah Casey, MD, Connecticut
Daniel Heacock, PA-C, Connecticut
Shabana Ansari, DO, Delaware
Madhu Prattipati, MD, Delaware
Pallavi Aneja, MD, Florida
Satcha Borgella, MD, Florida
Thendrex H. Estrella, MD, Florida
Abid Hussain, MD, Florida
Daphnee Hutchinson, DO, Florida
Muhammad Jaffer, Florida
Sue Lee, ANP, Florida
Melissa Odermann, DO, Florida
Jose Guillermo Revelo Paiz, MD, Florida
Rafael J. Rolon Rivera, MD, Florida
Eleonor Rongo, Florida
Esther Roth, Florida
Shitaye Argaw, MD, Georgia
Taryn DeGrazia, Georgia
Becca Feistritzer, Georgia
Jamal Fitts, Georgia
Kristen Flint, Georgia
Zachary Hermes, Georgia
Mukesh Kumar, Georgia
Kajal Patel, Georgia
Madeline Smith, Georgia
Wade Flowers, PharmD, Idaho
Ajay Bhandare, Illinois
Kimberly Brighton, Illinois
Hristo D. Hristov, MD, Illinois
Sidney Iriana, Illinois
Aurelian Ivan, Illinois
Ming Lee, MD, Illinois
Michelle Lundholm, Illinois
Idrees Mohiuddin, MD, Illinois
Murr Murray, Illinois
Tad Nair, MD, Illinois
Shalini Reddy, MD, Illinois
Richard Rethorst, MD, Illinois
Kelly Robertshaw, Illinois
Gracelene Wegrzyn, Illinois
Evan Yates, Illinois
Lora J. Jones McClure, MD, Indiana
Carleigh Wilson, DO, Indiana
Erin Brown, ARNP, Iowa
Adam Gray, Iowa
Paul Greco, MD, Iowa
Shelly McGurk, ACNP, ARNP, Iowa
Julie Stanik-Hutt, ACNP, CNS, PhD, Iowa
Elizabeth Cozad, DO, Kansas
Roshan Pais, Kentucky
Mark Youssef, MD, Kentucky
Heather Kahn, MD, Louisiana
Danielle Parrott, PA-C, Maine
Erica Lafferty, ACNP, Maryland
Andrea Limpuangthip, Maryland
Steven Schwartz, CCM, MD, Maryland
Eisha Azhar, MBBS, Massachusetts
Badal Kalamkar, MD, MPH, Massachusetts
Bhavya Rajanna, MD, Massachusetts
Sahib Baljinder Singh, MD, Massachusetts
Kathryn Adams, Michigan
Haseeb Aslam, MD, MBBS, Michigan
Hilda Crispin, MD, Michigan
Sharmistha Dev, MD, Michigan
Tristan Feierabend, MD, Michigan
Sonal Kamalia, MD, MBBS, Michigan
Matthew Luzum, MD, Michigan
Daniel Mitzel, MD, Michigan
Richard Raad, Michigan
Mythri Ramegowda, MD, Michigan
Katie Scally, MD, Michigan
Linden Spital, MSN, NP, Michigan
Porama Koy Thanaporn, MD, Michigan
Chanteil Ulatowski, Michigan
Tingting Xiong, MD, Michigan
Adam Zahr, Michigan
Mike Beste, MD, Minnesota
Elise Haupt, PA-C, Minnesota
Lobsang Trasar, MD, Minnesota
Kari Goan, DO, Mississippi
David C. Pierre, Mississippi
Sudheer Tangella, MD, Mississippi
Tahani Atieh, Missouri
Nicholas Arnold, Missouri
Amanda Calhoun, Missouri
Jyotirmoy Das, Missouri
Umber Dube, Missouri
Daniel Gaughan, Missouri
Woojin Joo, Missouri
Khaled Jumean, MBBS, Missouri
Salma Kazmi, MBBS, MD, Missouri
Yoon Kook (Danny) Kim, Missouri
Ryan Kronen, Missouri
Alyssa Kroner, Missouri
Randy Laine, Missouri
Edward Lee, Missouri
Cerena Leung, Missouri
Patricia Lithrow, Missouri
Brandt Lydon, Missouri
Mary Morgan Scott, Missouri
Jay Patel, Missouri
Justin Porter, Missouri
Danelle Reagin, FNP-C, Missouri
Amanda Reis, Missouri
Awik Som, Missouri
Abby Sung, Missouri
Mary Sutherland, Missouri
Maggie Wang, Missouri
Noah Wasserman, Missouri
Alexis Webber, Missouri
Ryan White, Missouri
Amy Xu, Missouri
Ran Xu, Missouri
Michael Yang, Missouri
Christopher Dietrich, MD, Montana
Jason Kunz, DO, Montana
Jodi Cantrell, MD, Nebraska
Steven Hart, MD, Nebraska
Kurt Kapels, MD, Nebraska
Brian Keegan, MD, Nebraska
Shaun Jang, MD, Nevada
Gurpinder Singh, MD, New Hampshire
Pragati Banda, MD, New Jersey
Sahai Donaldson, MBBS, New Jersey
Ashesha Mechineni, MD, New Jersey
Alisa Clark, New Mexico
Prajit Arora, MBBS, New Mexico
Crystal Cardwell, New Mexico
Landon Casaus, New Mexico
Tapuwa Mupfumira, MD, New Mexico
Eric Rightley, New Mexico
David S. Anderson, New York
Joan Bosco, MD, New York
Jessica Caro, New York
Anna Dewan, New York
Amrita Dhillon, MBBS, New York
Julia Frydman, New York
Radhika Gali, MBBS, MDS, New York
Allison Guttmann, MD, New York
Aryles Hedjar, MD, New York
Peter Janes, New York
Nadine Kalavazoff, New York
Jeffrey Lach, DO, New York
Keron Lezama, MD, New York
Yingheng Liu, New York
Taimur Mirza, New York
Cyrus Nensey, MD, New York
Nekee Pandya, MD, New York
Thushara Paul, MD, New York
Yu Sung, New York
Joel Boggan, MD, North Carolina
Angela Fletcher, North Carolina
Rebecca Gimpert, PA-C, North Carolina
Samantha Levering, PA-C, North Carolina
Nancy Martin, North Carolina
Richard Sherwood, North Carolina
Kranthi K. Sitammagari, MD, North Carolina
Aaron Swedberg, MPAS, PA-C, North Carolina
Yih-Cherng Tsai, North Carolina
Richard Bakker, MD, PhD, Ohio
Matthew Broderick, MD, Ohio
Subbaraju Budharaju, MD, MS, Ohio
Steven Bumb, MD, Ohio
Ahmed Eltelbany, MD, Ohio
Tracey Hardin, MS, Ohio
Patricia Hardman, APRN, Ohio
Michael Lewis, MD, Ohio
Volodymyr Manko, Ohio
Rebecca Stone, Ohio
Chaitanya Valluri, Ohio
Holly Wierzbicki, CNP, Ohio
Jamie Yockey, APRN, CNP, Ohio
Mahdi Mussa, MD, Oklahoma
Monica Saemz, DO, Oklahoma
Peter Ganter, MD, Oregon
Bethany Roy, MD, Oregon
Mary Clare Bohnett, Oregon
Molly Rabinowitz, Oregon
Abdullateef Abdulkareem, MD, MPH, Pennsylvania
David Ahamba, MD, MPH, Pennsylvania
David Chin, MD, Pennsylvania
Thomas Conlon, Pennsylvania
Dan Giesler, MD, Pennsylvania
Umair Randhawa, MD, Pennsylvania
Syed Yusuf, MBBS, Pennsylvania
Michael Rigatti, Pennsylvania
Thaylon Barreto, Rhode Island
Jessica Cook, MD, South Carolina
Robin Malik, MD, South Carolina
John Busigin, Tennessee
Shefali Paranjape, MD, Tennessee
Thai Dang, MD, Texas
Matthew Glover, MD, Texas
Snigdha Jain, MD, Texas
David Kellenberger, Texas
Sumeet Kumar, Texas
Kyle McClendon, PA-C, Texas
Sowjanya Mohan, Texas
Akhil D. Vats, MD, Texas
Samatha Vellanki, Texas
Lee-Anna Burgess, MD, Vermont
Rick Hildebrant, MD, Vermont
Matthew Backens, MD, Virginia
Megan Coe, Virginia
Kevin Dehaan, Virginia
Stephen Fox, Virginia
Amber Inofuentes, MD, Virginia
Jessica Keiser, MD, Virginia
Joseph Perez, MD, FAAFP, MBA, Virginia
Kanwapreet S. Saini, MD, Virginia
Erin Vipler, MD, Virginia
Naveen Voore, MBBS, Virginia
Abhishek Agarwal, MD, MBBS, Washington
Robert Cooney, MD, Washington
Cynthia Horton, MD, Washington
Rich A. Kukreja, MD, Washington
Ji Young Nam, MD, Washington
Kai Wilhelm, MD, Washington
In Kyu Yoo, Washington
Temu Brown, Wisconsin
Pablo Colon Nieves, Wisconsin
Christina Evans, PAC, Wisconsin
Swetha Karturi, MBBS, Wisconsin
Mark Babcock, DO, Wyoming
Ahmad Von Schlegell, Canada
Anand Kartha, Japan
Mohamed Sadek, Qatar
Amine Rakab, MD, Qatar
Abazar Saeed, Qatar
Joao Guerra, MD
Trending at SHM
Unveiling the hospitalist specialty code
The Centers for Medicare & Medicaid Services announced in November the official implementation date for the Medicare physician specialty code for hospitalists. On April 3, “hospitalist” will be an official specialty designation under Medicare; the code will be C6. Starting on that date, hospitalists can change their specialty designation on the Medicare enrollment application (Form CMS-855I) or through CMS’ online portal (Provider Enrollment, Chain, and Ownership System, or PECOS).
Appropriate use of specialty codes helps distinguish differences among providers and improves the quality of utilization data. SHM applied for a specialty code for hospitalists nearly 3 years ago, and CMS approved the application in February 2016.
Stand with your fellow hospitalists and make sure to declare, “I’m a C6.”
Develop curricula to educate, engage medical students and residents
The ACGME requirements for training in quality and safety are changing – it is no longer an elective. As sponsoring institutions’ residency and fellowship programs mobilize to meet these requirements, leaders may find few faculty members are comfortable enough with the material to teach and create educational content for trainees. These faculty need further development.
Sponsored by SHM, the Quality and Safety Educators Academy (QSEA) responds to that demand by providing medical educators with the knowledge and tools to integrate quality improvement and safety concepts into their curricula. The 2017 meeting is Feb. 26-28 at the Tempe Mission Palms Hotel in Arizona.
This 2½ day meeting aims to fill the current gaps for faculty by offering basic concepts and educational tools in quality improvement and patient safety. Material is presented in an interactive way, providing guidance on career and curriculum development and establishing a national network of quality and safety educators.
For more information and to register, visit www.shmqsea.org.
EHRs: blessing or curse?
SHM’s Health Information Technology (HIT) Committee invited you to participate in a brief survey to inform your experiences with inpatient electronic health record (EHR) systems. The results will serve as a foundation for a white paper to be written by the HIT Committee addressing hospitalists’ attitudes toward EHR systems. It will be released next month, so stay tuned then to view the final paper.
SHM chapters: Your connection to local education, networking, leadership opportunities
SHM offers various opportunities to grow professionally, expand your CV, and engage with other hospitalists. With more than 50 chapters across the country, you can network, learn, teach, and continue to improve patient care at a local level. Find a chapter in your area or start a chapter today by visiting www.hospitalmedicine.org/chapters.
Enhance opioid safety for inpatients
SHM enrolled 10 hospitals into a second mentored implementation cohort around Reducing Adverse Drug Events Related to Opioids (RADEO). The program is now in its second month as the sites work with their mentors to enhance safety for patients in the hospital who are prescribed opioid medications by:
- Developing a needs assessment.
- Putting in place formal selections of data collection measures.
- Beginning to take outcomes and process data collection on intervention units.
- Starting to design and implement key interventions.
Even if you’re not in this mentored implementation cohort, visit www.hospitalmedicine.org/RADEO and view the online toolkit or download the implementation guide.
Earn recognition for your research with SHM’s Junior Investigator Award
The SHM Junior Investigator Award was created for junior/early-stage investigators, defined as faculty in the first 5 years of their most recent position/appointment. Applicants must be a hospitalist or clinician-investigators whose research interests focus on the care of hospitalized patients, the organization of hospitals, or the practice of hospitalists. Applicants must be members of SHM in good standing. Nominations from mentors and self-nominations are both welcome.
The winner will be invited to receive the award during SHM’s annual meeting, HM17, May 1-4, at Mandalay Bay Resort and Casino in Las Vegas. The winner will receive complimentary registration for this meeting as well as a complimentary 1-year membership to SHM.
For more information on the application process, visit www.hospitalmedicine.org/juniorinvestigator.
Unveiling the hospitalist specialty code
The Centers for Medicare & Medicaid Services announced in November the official implementation date for the Medicare physician specialty code for hospitalists. On April 3, “hospitalist” will be an official specialty designation under Medicare; the code will be C6. Starting on that date, hospitalists can change their specialty designation on the Medicare enrollment application (Form CMS-855I) or through CMS’ online portal (Provider Enrollment, Chain, and Ownership System, or PECOS).
Appropriate use of specialty codes helps distinguish differences among providers and improves the quality of utilization data. SHM applied for a specialty code for hospitalists nearly 3 years ago, and CMS approved the application in February 2016.
Stand with your fellow hospitalists and make sure to declare, “I’m a C6.”
Develop curricula to educate, engage medical students and residents
The ACGME requirements for training in quality and safety are changing – it is no longer an elective. As sponsoring institutions’ residency and fellowship programs mobilize to meet these requirements, leaders may find few faculty members are comfortable enough with the material to teach and create educational content for trainees. These faculty need further development.
Sponsored by SHM, the Quality and Safety Educators Academy (QSEA) responds to that demand by providing medical educators with the knowledge and tools to integrate quality improvement and safety concepts into their curricula. The 2017 meeting is Feb. 26-28 at the Tempe Mission Palms Hotel in Arizona.
This 2½ day meeting aims to fill the current gaps for faculty by offering basic concepts and educational tools in quality improvement and patient safety. Material is presented in an interactive way, providing guidance on career and curriculum development and establishing a national network of quality and safety educators.
For more information and to register, visit www.shmqsea.org.
EHRs: blessing or curse?
SHM’s Health Information Technology (HIT) Committee invited you to participate in a brief survey to inform your experiences with inpatient electronic health record (EHR) systems. The results will serve as a foundation for a white paper to be written by the HIT Committee addressing hospitalists’ attitudes toward EHR systems. It will be released next month, so stay tuned then to view the final paper.
SHM chapters: Your connection to local education, networking, leadership opportunities
SHM offers various opportunities to grow professionally, expand your CV, and engage with other hospitalists. With more than 50 chapters across the country, you can network, learn, teach, and continue to improve patient care at a local level. Find a chapter in your area or start a chapter today by visiting www.hospitalmedicine.org/chapters.
Enhance opioid safety for inpatients
SHM enrolled 10 hospitals into a second mentored implementation cohort around Reducing Adverse Drug Events Related to Opioids (RADEO). The program is now in its second month as the sites work with their mentors to enhance safety for patients in the hospital who are prescribed opioid medications by:
- Developing a needs assessment.
- Putting in place formal selections of data collection measures.
- Beginning to take outcomes and process data collection on intervention units.
- Starting to design and implement key interventions.
Even if you’re not in this mentored implementation cohort, visit www.hospitalmedicine.org/RADEO and view the online toolkit or download the implementation guide.
Earn recognition for your research with SHM’s Junior Investigator Award
The SHM Junior Investigator Award was created for junior/early-stage investigators, defined as faculty in the first 5 years of their most recent position/appointment. Applicants must be a hospitalist or clinician-investigators whose research interests focus on the care of hospitalized patients, the organization of hospitals, or the practice of hospitalists. Applicants must be members of SHM in good standing. Nominations from mentors and self-nominations are both welcome.
The winner will be invited to receive the award during SHM’s annual meeting, HM17, May 1-4, at Mandalay Bay Resort and Casino in Las Vegas. The winner will receive complimentary registration for this meeting as well as a complimentary 1-year membership to SHM.
For more information on the application process, visit www.hospitalmedicine.org/juniorinvestigator.
Unveiling the hospitalist specialty code
The Centers for Medicare & Medicaid Services announced in November the official implementation date for the Medicare physician specialty code for hospitalists. On April 3, “hospitalist” will be an official specialty designation under Medicare; the code will be C6. Starting on that date, hospitalists can change their specialty designation on the Medicare enrollment application (Form CMS-855I) or through CMS’ online portal (Provider Enrollment, Chain, and Ownership System, or PECOS).
Appropriate use of specialty codes helps distinguish differences among providers and improves the quality of utilization data. SHM applied for a specialty code for hospitalists nearly 3 years ago, and CMS approved the application in February 2016.
Stand with your fellow hospitalists and make sure to declare, “I’m a C6.”
Develop curricula to educate, engage medical students and residents
The ACGME requirements for training in quality and safety are changing – it is no longer an elective. As sponsoring institutions’ residency and fellowship programs mobilize to meet these requirements, leaders may find few faculty members are comfortable enough with the material to teach and create educational content for trainees. These faculty need further development.
Sponsored by SHM, the Quality and Safety Educators Academy (QSEA) responds to that demand by providing medical educators with the knowledge and tools to integrate quality improvement and safety concepts into their curricula. The 2017 meeting is Feb. 26-28 at the Tempe Mission Palms Hotel in Arizona.
This 2½ day meeting aims to fill the current gaps for faculty by offering basic concepts and educational tools in quality improvement and patient safety. Material is presented in an interactive way, providing guidance on career and curriculum development and establishing a national network of quality and safety educators.
For more information and to register, visit www.shmqsea.org.
EHRs: blessing or curse?
SHM’s Health Information Technology (HIT) Committee invited you to participate in a brief survey to inform your experiences with inpatient electronic health record (EHR) systems. The results will serve as a foundation for a white paper to be written by the HIT Committee addressing hospitalists’ attitudes toward EHR systems. It will be released next month, so stay tuned then to view the final paper.
SHM chapters: Your connection to local education, networking, leadership opportunities
SHM offers various opportunities to grow professionally, expand your CV, and engage with other hospitalists. With more than 50 chapters across the country, you can network, learn, teach, and continue to improve patient care at a local level. Find a chapter in your area or start a chapter today by visiting www.hospitalmedicine.org/chapters.
Enhance opioid safety for inpatients
SHM enrolled 10 hospitals into a second mentored implementation cohort around Reducing Adverse Drug Events Related to Opioids (RADEO). The program is now in its second month as the sites work with their mentors to enhance safety for patients in the hospital who are prescribed opioid medications by:
- Developing a needs assessment.
- Putting in place formal selections of data collection measures.
- Beginning to take outcomes and process data collection on intervention units.
- Starting to design and implement key interventions.
Even if you’re not in this mentored implementation cohort, visit www.hospitalmedicine.org/RADEO and view the online toolkit or download the implementation guide.
Earn recognition for your research with SHM’s Junior Investigator Award
The SHM Junior Investigator Award was created for junior/early-stage investigators, defined as faculty in the first 5 years of their most recent position/appointment. Applicants must be a hospitalist or clinician-investigators whose research interests focus on the care of hospitalized patients, the organization of hospitals, or the practice of hospitalists. Applicants must be members of SHM in good standing. Nominations from mentors and self-nominations are both welcome.
The winner will be invited to receive the award during SHM’s annual meeting, HM17, May 1-4, at Mandalay Bay Resort and Casino in Las Vegas. The winner will receive complimentary registration for this meeting as well as a complimentary 1-year membership to SHM.
For more information on the application process, visit www.hospitalmedicine.org/juniorinvestigator.
Promoting the Health of Healthcare Employees
Provisions in the Affordable Care Act (ACA) encourage hospitals to work with their communities to improve population health. Like so many things, these efforts can and should begin at home—in this case, the hospital itself. Health and wellness programs for healthcare workers need to be emphasized, according to “Health and Wellness Programs for Hospital Employees: Results from a 2015 American Hospital Association Survey.”1
Such efforts allow healthcare workers to lead by example.
“To help create a culture of health, hospitals and health systems can provide leadership, and hospital employees can be role models, for health and wellness in their communities,” according to the report. “Developing health and wellness strategies and programs at hospitals will help establish an environment that provides the support, resources, and incentives for hospital employees to serve as such role models.”
Developing health and wellness programs can also help hospitals achieve the public health goals of the Healthy People 2020 initiative from the Office of Disease Prevention and Health Promotion.
To find out how hospitals are doing in this work, the 26-question survey was done in 2010 and again in 2015 and sent to approximately 6,000 hospitals in the United States. Response rate was 15% in 2010 and 18% in 2015. Some of the findings include:
- About the same number of hospitals have a health and wellness program or other initiative(s) for employees (86% in 2010 and 87% in 2015); however, the types of health and wellness programs and benefits that hospitals offer to their employees increased.
- The number of hospitals with 70% to 90% or more of employees participating in health and wellness programs increased from 19% in 2010 to 31% in 2015.
- The number of hospitals offering health and wellness programs to people in the community increased from 19% in 2010 to 66% in 2015.
- The number of hospitals offering incentives for participating in health and wellness programs increased as did the value of incentives, with more hospitals giving $500 or more to employees (7% in 2010 and 29% in 2015).
Reference
- Health Research & Educational Trust. Health and wellness programs for hospital employees: results from a 2015 American Hospital Association survey. Hospitals in Pursuit of Excellence website.
Provisions in the Affordable Care Act (ACA) encourage hospitals to work with their communities to improve population health. Like so many things, these efforts can and should begin at home—in this case, the hospital itself. Health and wellness programs for healthcare workers need to be emphasized, according to “Health and Wellness Programs for Hospital Employees: Results from a 2015 American Hospital Association Survey.”1
Such efforts allow healthcare workers to lead by example.
“To help create a culture of health, hospitals and health systems can provide leadership, and hospital employees can be role models, for health and wellness in their communities,” according to the report. “Developing health and wellness strategies and programs at hospitals will help establish an environment that provides the support, resources, and incentives for hospital employees to serve as such role models.”
Developing health and wellness programs can also help hospitals achieve the public health goals of the Healthy People 2020 initiative from the Office of Disease Prevention and Health Promotion.
To find out how hospitals are doing in this work, the 26-question survey was done in 2010 and again in 2015 and sent to approximately 6,000 hospitals in the United States. Response rate was 15% in 2010 and 18% in 2015. Some of the findings include:
- About the same number of hospitals have a health and wellness program or other initiative(s) for employees (86% in 2010 and 87% in 2015); however, the types of health and wellness programs and benefits that hospitals offer to their employees increased.
- The number of hospitals with 70% to 90% or more of employees participating in health and wellness programs increased from 19% in 2010 to 31% in 2015.
- The number of hospitals offering health and wellness programs to people in the community increased from 19% in 2010 to 66% in 2015.
- The number of hospitals offering incentives for participating in health and wellness programs increased as did the value of incentives, with more hospitals giving $500 or more to employees (7% in 2010 and 29% in 2015).
Reference
- Health Research & Educational Trust. Health and wellness programs for hospital employees: results from a 2015 American Hospital Association survey. Hospitals in Pursuit of Excellence website.
Provisions in the Affordable Care Act (ACA) encourage hospitals to work with their communities to improve population health. Like so many things, these efforts can and should begin at home—in this case, the hospital itself. Health and wellness programs for healthcare workers need to be emphasized, according to “Health and Wellness Programs for Hospital Employees: Results from a 2015 American Hospital Association Survey.”1
Such efforts allow healthcare workers to lead by example.
“To help create a culture of health, hospitals and health systems can provide leadership, and hospital employees can be role models, for health and wellness in their communities,” according to the report. “Developing health and wellness strategies and programs at hospitals will help establish an environment that provides the support, resources, and incentives for hospital employees to serve as such role models.”
Developing health and wellness programs can also help hospitals achieve the public health goals of the Healthy People 2020 initiative from the Office of Disease Prevention and Health Promotion.
To find out how hospitals are doing in this work, the 26-question survey was done in 2010 and again in 2015 and sent to approximately 6,000 hospitals in the United States. Response rate was 15% in 2010 and 18% in 2015. Some of the findings include:
- About the same number of hospitals have a health and wellness program or other initiative(s) for employees (86% in 2010 and 87% in 2015); however, the types of health and wellness programs and benefits that hospitals offer to their employees increased.
- The number of hospitals with 70% to 90% or more of employees participating in health and wellness programs increased from 19% in 2010 to 31% in 2015.
- The number of hospitals offering health and wellness programs to people in the community increased from 19% in 2010 to 66% in 2015.
- The number of hospitals offering incentives for participating in health and wellness programs increased as did the value of incentives, with more hospitals giving $500 or more to employees (7% in 2010 and 29% in 2015).
Reference
- Health Research & Educational Trust. Health and wellness programs for hospital employees: results from a 2015 American Hospital Association survey. Hospitals in Pursuit of Excellence website.
SHM Rolls Out New Structure for Leadership Academy 2017
For years, SHM’s Leadership Academy courses have been selling out. To meet and exceed the demand and expectations of attendees, SHM is rolling out a new structure designed to provide more opportunities for those who seek to advance their careers and expand their leadership skills.
New for Leadership Academy 2017, Strategic Essentials (formerly Leadership Foundations), Influential Management, and Mastering Teamwork will be available to all attendees regardless of previous attendance. SHM provides recommendations for interested registrants to allow them to determine which course fits them best in their leadership journey.
The 2017 Leadership Academy will be held October 23–26, 2017, at the JW Marriott Scottsdale Camelback Inn Resort & Spa in Arizona. The revised course structure includes:
Strategic Essentials
Learn how to evaluate personal leadership strengths and weaknesses, create and execute a communication strategy for key team members, understand key hospital finances and drivers, examine how hospital metrics are derived, and more in this four-day hands-on educational course covering various hospital medicine–focused leadership skills.
Attendees are grouped at tables of 10, each with a skilled facilitator to ensure meaningful, relevant application of concepts to hands-on activities.
The Strategic Essentials course is recommended for residents, early-career hospitalists, first-time hospitalist leaders, and hospitalist leaders wishing to strengthen their leadership skills set and advance their careers.
Influential Management
The Influential Management course provides leadership skills specific to the incorporation of meta-leadership styles, driving culture change through specific leadership behaviors and actions, financial storytelling, effective professional negotiation with proven techniques, and more.
Participants engage in several tabletop exercises throughout the four-day course, encouraging an interactive learning environment with world-renowned faculty.
The Influential Management course is recommended for early-career hospitalists to midlevel-career hospitalists and hospitalist leaders desiring to enhance their leadership skills set in specific areas.
Mastering Teamwork
Find out how to critically assess program growth opportunities and develop operational plans; utilize the principles of SWARM intelligence; lead, manage, and motivate teams in complex hospital environments; and communicate effectively in the Mastering Teamwork course.
Prominent faculty deep-dive into many of leadership skills and practices in this session to provide participants with a better understanding of team and organizational dynamics and how their personal leadership skills can strengthen teams and improve organizational growth and success.
Mastering Teamwork is recommended for hospitalists with three or more years of experience as well as hospitalist leaders looking to advance their career to the organizational strategy level.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
For years, SHM’s Leadership Academy courses have been selling out. To meet and exceed the demand and expectations of attendees, SHM is rolling out a new structure designed to provide more opportunities for those who seek to advance their careers and expand their leadership skills.
New for Leadership Academy 2017, Strategic Essentials (formerly Leadership Foundations), Influential Management, and Mastering Teamwork will be available to all attendees regardless of previous attendance. SHM provides recommendations for interested registrants to allow them to determine which course fits them best in their leadership journey.
The 2017 Leadership Academy will be held October 23–26, 2017, at the JW Marriott Scottsdale Camelback Inn Resort & Spa in Arizona. The revised course structure includes:
Strategic Essentials
Learn how to evaluate personal leadership strengths and weaknesses, create and execute a communication strategy for key team members, understand key hospital finances and drivers, examine how hospital metrics are derived, and more in this four-day hands-on educational course covering various hospital medicine–focused leadership skills.
Attendees are grouped at tables of 10, each with a skilled facilitator to ensure meaningful, relevant application of concepts to hands-on activities.
The Strategic Essentials course is recommended for residents, early-career hospitalists, first-time hospitalist leaders, and hospitalist leaders wishing to strengthen their leadership skills set and advance their careers.
Influential Management
The Influential Management course provides leadership skills specific to the incorporation of meta-leadership styles, driving culture change through specific leadership behaviors and actions, financial storytelling, effective professional negotiation with proven techniques, and more.
Participants engage in several tabletop exercises throughout the four-day course, encouraging an interactive learning environment with world-renowned faculty.
The Influential Management course is recommended for early-career hospitalists to midlevel-career hospitalists and hospitalist leaders desiring to enhance their leadership skills set in specific areas.
Mastering Teamwork
Find out how to critically assess program growth opportunities and develop operational plans; utilize the principles of SWARM intelligence; lead, manage, and motivate teams in complex hospital environments; and communicate effectively in the Mastering Teamwork course.
Prominent faculty deep-dive into many of leadership skills and practices in this session to provide participants with a better understanding of team and organizational dynamics and how their personal leadership skills can strengthen teams and improve organizational growth and success.
Mastering Teamwork is recommended for hospitalists with three or more years of experience as well as hospitalist leaders looking to advance their career to the organizational strategy level.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.
For years, SHM’s Leadership Academy courses have been selling out. To meet and exceed the demand and expectations of attendees, SHM is rolling out a new structure designed to provide more opportunities for those who seek to advance their careers and expand their leadership skills.
New for Leadership Academy 2017, Strategic Essentials (formerly Leadership Foundations), Influential Management, and Mastering Teamwork will be available to all attendees regardless of previous attendance. SHM provides recommendations for interested registrants to allow them to determine which course fits them best in their leadership journey.
The 2017 Leadership Academy will be held October 23–26, 2017, at the JW Marriott Scottsdale Camelback Inn Resort & Spa in Arizona. The revised course structure includes:
Strategic Essentials
Learn how to evaluate personal leadership strengths and weaknesses, create and execute a communication strategy for key team members, understand key hospital finances and drivers, examine how hospital metrics are derived, and more in this four-day hands-on educational course covering various hospital medicine–focused leadership skills.
Attendees are grouped at tables of 10, each with a skilled facilitator to ensure meaningful, relevant application of concepts to hands-on activities.
The Strategic Essentials course is recommended for residents, early-career hospitalists, first-time hospitalist leaders, and hospitalist leaders wishing to strengthen their leadership skills set and advance their careers.
Influential Management
The Influential Management course provides leadership skills specific to the incorporation of meta-leadership styles, driving culture change through specific leadership behaviors and actions, financial storytelling, effective professional negotiation with proven techniques, and more.
Participants engage in several tabletop exercises throughout the four-day course, encouraging an interactive learning environment with world-renowned faculty.
The Influential Management course is recommended for early-career hospitalists to midlevel-career hospitalists and hospitalist leaders desiring to enhance their leadership skills set in specific areas.
Mastering Teamwork
Find out how to critically assess program growth opportunities and develop operational plans; utilize the principles of SWARM intelligence; lead, manage, and motivate teams in complex hospital environments; and communicate effectively in the Mastering Teamwork course.
Prominent faculty deep-dive into many of leadership skills and practices in this session to provide participants with a better understanding of team and organizational dynamics and how their personal leadership skills can strengthen teams and improve organizational growth and success.
Mastering Teamwork is recommended for hospitalists with three or more years of experience as well as hospitalist leaders looking to advance their career to the organizational strategy level.
Learn more about SHM’s Leadership Academy at www.shmleadershipacademy.org.







