User login
Replenishing the Primary Care Physician Pipeline
A recent survey of nearly 1,000 students from three medical schools found that just 15% planned to become primary-care physicians, including 11.2% of first-year students.1
That startlingly low number might not be reflective of the whole country, and other national surveys have suggested significantly higher rates. But the responses underscore some important contributors beyond financial concerns that include a more negative overall view of PCPs’ work life compared to that of specialists. “Our data suggest that although medical school does not create these negative views of primary-care work life, it may reinforce them,” the authors write.
Conversely, the results suggest that time spent observing physicians could help break negative stereotypes about the ability to develop good relationships with patients, and that career plans might not be based on perceptions, but rather on values and goals. “The study reinforces the importance of admitting students with primary-care-oriented values and primary-care interest and reinforcing those values over the course of medical school,” the authors conclude.
“Maybe we’re not selecting medical students in the optimal way for what society needs,” says Elbert Huang, MD, associate professor of medicine at the University of Chicago. By emphasizing GPA and test scores, “maybe when you do that, you end with people who don’t want to actually take care of patients in primary care.”
Other studies suggest he’s on to something. Research conducted by the Washington, D.C.-based Robert Graham Center found that students in rural medical schools are significantly more likely to go into rural healthcare and primary care than students in urban medical schools.
“The problem there is that we’ve cut the number of people from rural areas going to medical school by half over the last 20 years,” center director Robert Phillips, MD, MSPH, says. “A lot of students just don’t have the background to make them competitive.” Many students in minority communities face similar challenges.
Ed Salsberg, director of the National Center for Health Workforce Analysis in the Health Resources and Services Administration, says many newer osteopathic schools are positioning themselves in rural communities, helping them attract students who might not have gone to medical school otherwise.
Reaching back even earlier into the pipeline to help mentor elementary and high school students might be another way to help build capacity. Medical organizations also seem to be getting the message. New MCAT recommendations by the Association of American Medical Colleges, for example, place less emphasis on scientific knowledge in favor of a more holistic assessment of critical analysis and reasoning skills. The association also is encouraging medical schools to pay more attention to such personal characteristics as integrity and service orientation.
“That’s more of a long-term strategy, but I think it has an impact on who gets recruited to medical school,” Salsberg says.
Reference
A recent survey of nearly 1,000 students from three medical schools found that just 15% planned to become primary-care physicians, including 11.2% of first-year students.1
That startlingly low number might not be reflective of the whole country, and other national surveys have suggested significantly higher rates. But the responses underscore some important contributors beyond financial concerns that include a more negative overall view of PCPs’ work life compared to that of specialists. “Our data suggest that although medical school does not create these negative views of primary-care work life, it may reinforce them,” the authors write.
Conversely, the results suggest that time spent observing physicians could help break negative stereotypes about the ability to develop good relationships with patients, and that career plans might not be based on perceptions, but rather on values and goals. “The study reinforces the importance of admitting students with primary-care-oriented values and primary-care interest and reinforcing those values over the course of medical school,” the authors conclude.
“Maybe we’re not selecting medical students in the optimal way for what society needs,” says Elbert Huang, MD, associate professor of medicine at the University of Chicago. By emphasizing GPA and test scores, “maybe when you do that, you end with people who don’t want to actually take care of patients in primary care.”
Other studies suggest he’s on to something. Research conducted by the Washington, D.C.-based Robert Graham Center found that students in rural medical schools are significantly more likely to go into rural healthcare and primary care than students in urban medical schools.
“The problem there is that we’ve cut the number of people from rural areas going to medical school by half over the last 20 years,” center director Robert Phillips, MD, MSPH, says. “A lot of students just don’t have the background to make them competitive.” Many students in minority communities face similar challenges.
Ed Salsberg, director of the National Center for Health Workforce Analysis in the Health Resources and Services Administration, says many newer osteopathic schools are positioning themselves in rural communities, helping them attract students who might not have gone to medical school otherwise.
Reaching back even earlier into the pipeline to help mentor elementary and high school students might be another way to help build capacity. Medical organizations also seem to be getting the message. New MCAT recommendations by the Association of American Medical Colleges, for example, place less emphasis on scientific knowledge in favor of a more holistic assessment of critical analysis and reasoning skills. The association also is encouraging medical schools to pay more attention to such personal characteristics as integrity and service orientation.
“That’s more of a long-term strategy, but I think it has an impact on who gets recruited to medical school,” Salsberg says.
Reference
A recent survey of nearly 1,000 students from three medical schools found that just 15% planned to become primary-care physicians, including 11.2% of first-year students.1
That startlingly low number might not be reflective of the whole country, and other national surveys have suggested significantly higher rates. But the responses underscore some important contributors beyond financial concerns that include a more negative overall view of PCPs’ work life compared to that of specialists. “Our data suggest that although medical school does not create these negative views of primary-care work life, it may reinforce them,” the authors write.
Conversely, the results suggest that time spent observing physicians could help break negative stereotypes about the ability to develop good relationships with patients, and that career plans might not be based on perceptions, but rather on values and goals. “The study reinforces the importance of admitting students with primary-care-oriented values and primary-care interest and reinforcing those values over the course of medical school,” the authors conclude.
“Maybe we’re not selecting medical students in the optimal way for what society needs,” says Elbert Huang, MD, associate professor of medicine at the University of Chicago. By emphasizing GPA and test scores, “maybe when you do that, you end with people who don’t want to actually take care of patients in primary care.”
Other studies suggest he’s on to something. Research conducted by the Washington, D.C.-based Robert Graham Center found that students in rural medical schools are significantly more likely to go into rural healthcare and primary care than students in urban medical schools.
“The problem there is that we’ve cut the number of people from rural areas going to medical school by half over the last 20 years,” center director Robert Phillips, MD, MSPH, says. “A lot of students just don’t have the background to make them competitive.” Many students in minority communities face similar challenges.
Ed Salsberg, director of the National Center for Health Workforce Analysis in the Health Resources and Services Administration, says many newer osteopathic schools are positioning themselves in rural communities, helping them attract students who might not have gone to medical school otherwise.
Reaching back even earlier into the pipeline to help mentor elementary and high school students might be another way to help build capacity. Medical organizations also seem to be getting the message. New MCAT recommendations by the Association of American Medical Colleges, for example, place less emphasis on scientific knowledge in favor of a more holistic assessment of critical analysis and reasoning skills. The association also is encouraging medical schools to pay more attention to such personal characteristics as integrity and service orientation.
“That’s more of a long-term strategy, but I think it has an impact on who gets recruited to medical school,” Salsberg says.
Reference
Ready for Recognition?
For hospitalists ready to take the national stage at HM13 next spring in Washington, D.C., it's not too early to be thinking about submissions for SHM's Annual Awards of Excellence and SHM's Research, Innovation, and Clinical Vignettes (RIV) poster competition. In fact, many winners have gone on to become SHM committee chairs, board members, and board presidents.
SHM will begin accepting submissions for both the Awards of Excellence and the RIV poster contest this month. Submissions will be accepted through October.
For more information, visit www.hospitalmedicine.org.
For hospitalists ready to take the national stage at HM13 next spring in Washington, D.C., it's not too early to be thinking about submissions for SHM's Annual Awards of Excellence and SHM's Research, Innovation, and Clinical Vignettes (RIV) poster competition. In fact, many winners have gone on to become SHM committee chairs, board members, and board presidents.
SHM will begin accepting submissions for both the Awards of Excellence and the RIV poster contest this month. Submissions will be accepted through October.
For more information, visit www.hospitalmedicine.org.
For hospitalists ready to take the national stage at HM13 next spring in Washington, D.C., it's not too early to be thinking about submissions for SHM's Annual Awards of Excellence and SHM's Research, Innovation, and Clinical Vignettes (RIV) poster competition. In fact, many winners have gone on to become SHM committee chairs, board members, and board presidents.
SHM will begin accepting submissions for both the Awards of Excellence and the RIV poster contest this month. Submissions will be accepted through October.
For more information, visit www.hospitalmedicine.org.
Training, Leadership, Commitment Integral to HM Improving Stroke Care
Stroke specialists like to say that “time is brain.” With an emphatic focus on those first few critical hours, however, it’s sometimes easy to overlook the vital role that hospitalists play in the days, weeks, and months that follow.
A recent study in The Neurohospitalist suggests that compared to community-based neurologists, practitioners of neurohospital medicine can reduce the length of stay for patients with ischemic stroke.1 A separate study, however, suggests that similar success might have come at a price for their less-specialized hospitalist counterparts.2 Among stroke patients, the latter study found that while the HM model is also associated with a reduced length of stay, it is associated with increased discharges to inpatient rehabilitation centers instead of to home, and higher readmission rates.
In sum, the evidence raises questions about whether rank-and-file hospitalists are adequately equipped to deal with a disease that is a core competency for the profession and ranks among the top sources of adult disability in the United States, at an estimated cost of $34.3 billion in 2008.3
“I think there’s been a mismatch between the training of the average hospitalist and then the expectations for the amount of neurological care they end up delivering once in practice,” says David Likosky, MD, SFHM, director of the stroke program at Evergreen Hospital Medical Center in Kirkland, Wash. “When surveyed, it’s been shown that hospitalists feel that care of stroke is one of the areas with which they’re least comfortable once they get out into practice.” Over the past decade, several studies have reinforced the notion of a training deficit.4,5
Demographic trends suggest that getting up to speed will be imperative, however. “One alarming thing we’re seeing is strokes among individuals that are not in the elderly group, and that group seems to be increasing at an alarming rate,” says Daniel T. Lackland, PhD, professor of epidemiology and neurosciences at the Medical University of South Carolina in Charleston. Hospitals are seeing more ischemic stroke patients in their 40s and 50s, likely a reflection of risk factors such as hypertension, diabetes, and hyperlipidemia that are occurring earlier in life. And because those patients are younger, the aftermath of a stroke could linger for decades.
Although the stroke mortality rate is declining in the U.S., statistics find that about 14% of all patients diagnosed with an initial stroke will have a second one within a year, placing continued strain on a healthcare system already stretched thin.6 Hospitalists, Dr. Lackland says, have an “ideal” opportunity to help build up and improve that system, potentially yielding significant cost savings along with the dramatic improvement in quality of life. Making the most of that opportunity, though, will require a solid understanding of multiple trends that are quickly transforming stroke care delivery.
Time Is of the Essence
Kevin Barrett, MD, MSc, assistant professor of neurology and stroke telemedicine director at the Mayo Clinic in Jacksonville, Fla., says hospitals are focusing more and more on a metric known as “door-to-needle time.” The goal is to treat at least half of incoming ischemic stroke patients with intravenous tissue-type plasminogen activator (IV tPA) within the first 60 minutes after onset of symptoms.
The American Heart Association/American Stroke Association has reinforced the message with its Get With the Guidelines Stroke Program. A recent analysis suggested the program has led to more timely tPA administration and, in turn, better patient outcomes (the program is funded in part through the Bristol-Myers Squib/Sanofi Pharmaceutical Partnership).7
At the same time, clinical research has widened the window for IV tPA delivery from three hours to 4.5 hours for certain patients after the onset of symptoms. Dr. Barrett says “strong evidence” from the European Cooperative Acute Stroke Study III has convinced most clinicians, and the FDA is expected to follow suit in officially approving the extension.8 As more stroke centers become certified, the use of IV tPA has increased accordingly.
Patients who have missed the time window or are not good candidates for IV tPA can still be aided by interarterial tPA at the site of the clot up to six hours after the onset of symptoms. Dr. Likosky says the treatment option should be of particular interest to hospitalists, given that strokes can occur post-operatively and in other patients who cannot receive IV tPA because of bleeding risk.
—Karim Godamunne, MD, MBA, SFHM, medical director, Eagle Hospital Physicians, Roswell, Ga.
For up to eight hours after the onset of symptoms, mechanical clot removal techniques have shown continued efficacy at revascularizing affected areas, with some newer options also offering greater promise of improving patient outcomes. Even with the prospects of declining complication rates, however, “evaluating and initiating treatment in a timely fashion is still going to be one of the most important predictors of outcome,” Dr. Barrett says.
After the initial intervention, hospitalists often are the go-to providers for anticipating and preventing common post-stroke complications, such as aspiration pneumonia, VTE from immobilization, and other infections. The proper use of anti-platelet agents and high-dose statins, also falling solidly within the HM realm, can pay big dividends if used consistently.
Meanwhile, newer studies and clinical observations are widening the scope of considerations that should be on every hospitalist’s radar. Here are a few cited by stroke experts:
Permissive hypertension. After an ischemic stroke, the benefit of permissive hypertension is still widely misunderstood. Perhaps counterintuitively, high blood pressure after a stroke can help protect the area of the brain that is damaged but not yet dead, sometimes called the penumbra. “I highlight this because I think it’s a common mistake, that internists are very used to high blood pressure being a bad thing,” says Andrew Josephson, MD, associate professor of clinical neurology and director of the neurohospitalist program at the University of California at San Francisco (UCSF) Medical Center. “And in general, it is; it’s a cause of stroke. But once somebody has a stroke, in the acute period, it’s important to allow the blood pressure to be high.”
Atrial fibrillation. The accepted role of atrial fibrillation in stroke is evolving. Research suggests that the common but often preventable arrhythmia is an important cause of stroke in about 15% to 20% of cases.9 By the time of hospital discharge, however, Dr. Josephson says physicians haven’t established a cause in about 1 in 4 cases. For these “cryptogenic strokes,” he says, doctors have long suspected that atrial fibrillation not picked up during the initial EKG or by the monitoring with cardiac telemetry could be a major cause.
Recent observations suggest that a longer monitoring period of up to 30 days may uncover atrial fibrillation in a sizable fraction of those patients, highlighting the importance of keeping a close eye on stroke patients both in the hospital and beyond. “It’s very important to identify, because atrial fibrillation changes what we do for folks to prevent a second stroke,” Dr. Josephson explains. Instead of anti-platelet medicine like aspirin, patients with atrial fibrillation often receive anticoagulants like warfarin, or the more recently approved dabigatran and rivaroxaban.
Transient ischemic attack. Improvements in imaging techniques like MRI have likewise begun to shift how stroke patients are treated. For example, Dr. Likosky says, medicine is moving away from a time-based definition of transient ischemic attack (TIA), in which symptoms resolve within 24 hours, to a tissue-based definition. Recent MRI imaging has uncovered evidence of a new infarction in more than half of patients initially diagnosed with TIA.10
“If they do have an infarction on their scan, even if they had symptoms that only lasted for five minutes, that’s a stroke,” Dr. Josephson says. And even a true TIA, he says, represents “a kind of stroke where you got really lucky and you’re not left with deficits, but the risk is still very high.” Accordingly, more patients with TIA are being admitted to the hospital to receive a full workup and preventive treatment. “We think that by evaluating these people urgently, we can reduce the risk of having a stroke by maybe 75% over a three-month time period,” Dr. Josephson says.
Hemorrhagic stroke. To date, the vast majority of patients with hemorrhagic stroke (which accounts for only 13% of all stroke cases) have been managed by neurosurgeons and neurologists. But here, too, Dr. Likosky says the picture could be changing. Recent findings that surgical treatment of intracranial hemorrhaging might not benefit many patients could shift the care paradigm toward a medical management strategy that involves more hospitalists.
Innovations Aplenty
The increasing complexity of stroke care and uneven distribution of resources and expertise have helped fuel several important innovations in delivery, most notably telestroke and neurohospital medicine. Both are being driven, in part, by an increased awareness of time-sensitive interventions and a frequent lack of on-site neurologists at smaller and more rural facilities. If telestroke programs are expanding the reach of neurologists, neurohospitalists are helping to fill the gaps in inpatient stroke care.
Amid the changes, one element is proving a necessary constant: a team approach that relies heavily on the HM emphasis on quality metrics, intensive monitoring, and careful coordination. Who better to lead the charge than hospitalists, says Mary E. Jensen, MD, professor of radiology and neurosurgery at the University of Virginia in Charlottesville. “They’re the ones who are in the hospital, and when these patients go bad, they go bad fast,” she says.
More broadly, Dr. Jensen says, hospitalists should get in on the ground floor when their facility seeks certification as a primary or a comprehensive stroke center. “And they need to make sure that the hospital isn’t just trying to get the sexy elements—the guy with the cath or the gal with the cath who can pull the clot out—but that they have a complete program that involves the care of the patient after they’ve had the procedure done,” she says.
As healthcare reform efforts are making clear, the responsibility doesn’t end after discharge, either. The Affordable Care Act includes a hospital readmission reduction program that will kick in this October, with penalties for hospitals posting unacceptably high 30-day readmission rates. Amy Kind, MD, PhD, assistant professor of medicine in the Division of Geriatrics at the University of Wisconsin School of Medicine and Public Health in Madison, is convinced that a key contributor to high rehospitalization rates among stroke patients may be the woefully incomplete nature of discharge communication.

—Mary E. Jensen, MD, professor of radiology and neurosurgery, University of Virginia, Charlottesville
Dr. Kind, for example, has found a disturbing pattern in communication regarding issues like dysphagia, a common complication among stroke patients and an important risk factor for pneumonia. Countering the risk usually requires such measures as putting patients on a special diet or elevating the head of their bed. “We looked at the quality of the communication of that information in discharge summaries, and it’s just abysmal. It’s absolutely abysmal,” she says. Without clear directives to providers in the next setting of care, such as a skilled-nursing facility, patients could be erroneously put back on a regular diet and aspirate, sending them right back to the hospital.
As one potential solution, Dr. Kind’s team is developing a multidisciplinary stroke discharge summary tool that automatically imports elements like speech-language pathology and dietary recommendations. Although most discharge communication may focus on more visible issues and interventions, Dr. Kind argues that some of the “bread and butter” concerns might ultimately prove just as important for long-term patient outcomes.
Karim Godamunne, MD, MBA, SFHM, vice president of clinical systems integration and medical director of Eagle Hospital Physicians in Atlanta, sees telemedicine as another potential tool to help reach patients after discharge, especially those who haven’t received follow-up care from a primary-care physician (PCP). “We need to be the champions at our hospitals for improving care processes, and we need to work in partnership with the nurses and the other professionals,” Dr. Godamunne says. “As a group, we can really make a difference, and stroke is one of those areas in which we can truly contribute.”
Bryn Nelson is a freelance medical writer in Seattle.
References
- Freeman WD, Dawson SB, Raper C, Thiemann K, et al. Neurohospitalists reduce length of stay for patients with ischemic stroke. The Neurohospitalist. 2011;1(2): 67-70.
- Howrey BT, Kuo Y-F, Goodwin JS. Association of care by hospitalists on discharge destination and 30-day outcomes after acute ischemic stroke. Medical Care. 2011;49(8): 701-707.
- Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2-e220.
- Glasheen JJ, Epstein KR, Siegal E, Kutner JS, Prochazka AV. The spectrum of community-based hospitalist practice: a call to tailor internal medicine residency training. Arch Intern Med. 2007;167(7):727-728.
- Plauth WH, Pantilat SZ, Wachter RM, Fenton CL. Hospitalists’ perceptions of their residency training needs: results of a national survey. Am J Med. 2001; 111(3):247-254.
- Dickerson LM, Carek PJ, Quattlebaum RG. Prevention of recurrent ischemic stroke. Am Fam Physician. 2007; 76(3):382-388.
- Fonarow GC, Smith EE, Saver JL, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123(7):750-758.
- Hacke W, Kaste M, Bluhmki E, Brozman M, et al. Thrombolysis with Alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317-1329.
- Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121:e91.
- Albers GW, Caplan LR, Easton JD, et al. Transient ischemic attack—proposal for a new definition. N Engl J Med. 2002;347(21):1713-1716.
- Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993-1003.
Stroke specialists like to say that “time is brain.” With an emphatic focus on those first few critical hours, however, it’s sometimes easy to overlook the vital role that hospitalists play in the days, weeks, and months that follow.
A recent study in The Neurohospitalist suggests that compared to community-based neurologists, practitioners of neurohospital medicine can reduce the length of stay for patients with ischemic stroke.1 A separate study, however, suggests that similar success might have come at a price for their less-specialized hospitalist counterparts.2 Among stroke patients, the latter study found that while the HM model is also associated with a reduced length of stay, it is associated with increased discharges to inpatient rehabilitation centers instead of to home, and higher readmission rates.
In sum, the evidence raises questions about whether rank-and-file hospitalists are adequately equipped to deal with a disease that is a core competency for the profession and ranks among the top sources of adult disability in the United States, at an estimated cost of $34.3 billion in 2008.3
“I think there’s been a mismatch between the training of the average hospitalist and then the expectations for the amount of neurological care they end up delivering once in practice,” says David Likosky, MD, SFHM, director of the stroke program at Evergreen Hospital Medical Center in Kirkland, Wash. “When surveyed, it’s been shown that hospitalists feel that care of stroke is one of the areas with which they’re least comfortable once they get out into practice.” Over the past decade, several studies have reinforced the notion of a training deficit.4,5
Demographic trends suggest that getting up to speed will be imperative, however. “One alarming thing we’re seeing is strokes among individuals that are not in the elderly group, and that group seems to be increasing at an alarming rate,” says Daniel T. Lackland, PhD, professor of epidemiology and neurosciences at the Medical University of South Carolina in Charleston. Hospitals are seeing more ischemic stroke patients in their 40s and 50s, likely a reflection of risk factors such as hypertension, diabetes, and hyperlipidemia that are occurring earlier in life. And because those patients are younger, the aftermath of a stroke could linger for decades.
Although the stroke mortality rate is declining in the U.S., statistics find that about 14% of all patients diagnosed with an initial stroke will have a second one within a year, placing continued strain on a healthcare system already stretched thin.6 Hospitalists, Dr. Lackland says, have an “ideal” opportunity to help build up and improve that system, potentially yielding significant cost savings along with the dramatic improvement in quality of life. Making the most of that opportunity, though, will require a solid understanding of multiple trends that are quickly transforming stroke care delivery.
Time Is of the Essence
Kevin Barrett, MD, MSc, assistant professor of neurology and stroke telemedicine director at the Mayo Clinic in Jacksonville, Fla., says hospitals are focusing more and more on a metric known as “door-to-needle time.” The goal is to treat at least half of incoming ischemic stroke patients with intravenous tissue-type plasminogen activator (IV tPA) within the first 60 minutes after onset of symptoms.
The American Heart Association/American Stroke Association has reinforced the message with its Get With the Guidelines Stroke Program. A recent analysis suggested the program has led to more timely tPA administration and, in turn, better patient outcomes (the program is funded in part through the Bristol-Myers Squib/Sanofi Pharmaceutical Partnership).7
At the same time, clinical research has widened the window for IV tPA delivery from three hours to 4.5 hours for certain patients after the onset of symptoms. Dr. Barrett says “strong evidence” from the European Cooperative Acute Stroke Study III has convinced most clinicians, and the FDA is expected to follow suit in officially approving the extension.8 As more stroke centers become certified, the use of IV tPA has increased accordingly.
Patients who have missed the time window or are not good candidates for IV tPA can still be aided by interarterial tPA at the site of the clot up to six hours after the onset of symptoms. Dr. Likosky says the treatment option should be of particular interest to hospitalists, given that strokes can occur post-operatively and in other patients who cannot receive IV tPA because of bleeding risk.
—Karim Godamunne, MD, MBA, SFHM, medical director, Eagle Hospital Physicians, Roswell, Ga.
For up to eight hours after the onset of symptoms, mechanical clot removal techniques have shown continued efficacy at revascularizing affected areas, with some newer options also offering greater promise of improving patient outcomes. Even with the prospects of declining complication rates, however, “evaluating and initiating treatment in a timely fashion is still going to be one of the most important predictors of outcome,” Dr. Barrett says.
After the initial intervention, hospitalists often are the go-to providers for anticipating and preventing common post-stroke complications, such as aspiration pneumonia, VTE from immobilization, and other infections. The proper use of anti-platelet agents and high-dose statins, also falling solidly within the HM realm, can pay big dividends if used consistently.
Meanwhile, newer studies and clinical observations are widening the scope of considerations that should be on every hospitalist’s radar. Here are a few cited by stroke experts:
Permissive hypertension. After an ischemic stroke, the benefit of permissive hypertension is still widely misunderstood. Perhaps counterintuitively, high blood pressure after a stroke can help protect the area of the brain that is damaged but not yet dead, sometimes called the penumbra. “I highlight this because I think it’s a common mistake, that internists are very used to high blood pressure being a bad thing,” says Andrew Josephson, MD, associate professor of clinical neurology and director of the neurohospitalist program at the University of California at San Francisco (UCSF) Medical Center. “And in general, it is; it’s a cause of stroke. But once somebody has a stroke, in the acute period, it’s important to allow the blood pressure to be high.”
Atrial fibrillation. The accepted role of atrial fibrillation in stroke is evolving. Research suggests that the common but often preventable arrhythmia is an important cause of stroke in about 15% to 20% of cases.9 By the time of hospital discharge, however, Dr. Josephson says physicians haven’t established a cause in about 1 in 4 cases. For these “cryptogenic strokes,” he says, doctors have long suspected that atrial fibrillation not picked up during the initial EKG or by the monitoring with cardiac telemetry could be a major cause.
Recent observations suggest that a longer monitoring period of up to 30 days may uncover atrial fibrillation in a sizable fraction of those patients, highlighting the importance of keeping a close eye on stroke patients both in the hospital and beyond. “It’s very important to identify, because atrial fibrillation changes what we do for folks to prevent a second stroke,” Dr. Josephson explains. Instead of anti-platelet medicine like aspirin, patients with atrial fibrillation often receive anticoagulants like warfarin, or the more recently approved dabigatran and rivaroxaban.
Transient ischemic attack. Improvements in imaging techniques like MRI have likewise begun to shift how stroke patients are treated. For example, Dr. Likosky says, medicine is moving away from a time-based definition of transient ischemic attack (TIA), in which symptoms resolve within 24 hours, to a tissue-based definition. Recent MRI imaging has uncovered evidence of a new infarction in more than half of patients initially diagnosed with TIA.10
“If they do have an infarction on their scan, even if they had symptoms that only lasted for five minutes, that’s a stroke,” Dr. Josephson says. And even a true TIA, he says, represents “a kind of stroke where you got really lucky and you’re not left with deficits, but the risk is still very high.” Accordingly, more patients with TIA are being admitted to the hospital to receive a full workup and preventive treatment. “We think that by evaluating these people urgently, we can reduce the risk of having a stroke by maybe 75% over a three-month time period,” Dr. Josephson says.
Hemorrhagic stroke. To date, the vast majority of patients with hemorrhagic stroke (which accounts for only 13% of all stroke cases) have been managed by neurosurgeons and neurologists. But here, too, Dr. Likosky says the picture could be changing. Recent findings that surgical treatment of intracranial hemorrhaging might not benefit many patients could shift the care paradigm toward a medical management strategy that involves more hospitalists.
Innovations Aplenty
The increasing complexity of stroke care and uneven distribution of resources and expertise have helped fuel several important innovations in delivery, most notably telestroke and neurohospital medicine. Both are being driven, in part, by an increased awareness of time-sensitive interventions and a frequent lack of on-site neurologists at smaller and more rural facilities. If telestroke programs are expanding the reach of neurologists, neurohospitalists are helping to fill the gaps in inpatient stroke care.
Amid the changes, one element is proving a necessary constant: a team approach that relies heavily on the HM emphasis on quality metrics, intensive monitoring, and careful coordination. Who better to lead the charge than hospitalists, says Mary E. Jensen, MD, professor of radiology and neurosurgery at the University of Virginia in Charlottesville. “They’re the ones who are in the hospital, and when these patients go bad, they go bad fast,” she says.
More broadly, Dr. Jensen says, hospitalists should get in on the ground floor when their facility seeks certification as a primary or a comprehensive stroke center. “And they need to make sure that the hospital isn’t just trying to get the sexy elements—the guy with the cath or the gal with the cath who can pull the clot out—but that they have a complete program that involves the care of the patient after they’ve had the procedure done,” she says.
As healthcare reform efforts are making clear, the responsibility doesn’t end after discharge, either. The Affordable Care Act includes a hospital readmission reduction program that will kick in this October, with penalties for hospitals posting unacceptably high 30-day readmission rates. Amy Kind, MD, PhD, assistant professor of medicine in the Division of Geriatrics at the University of Wisconsin School of Medicine and Public Health in Madison, is convinced that a key contributor to high rehospitalization rates among stroke patients may be the woefully incomplete nature of discharge communication.

—Mary E. Jensen, MD, professor of radiology and neurosurgery, University of Virginia, Charlottesville
Dr. Kind, for example, has found a disturbing pattern in communication regarding issues like dysphagia, a common complication among stroke patients and an important risk factor for pneumonia. Countering the risk usually requires such measures as putting patients on a special diet or elevating the head of their bed. “We looked at the quality of the communication of that information in discharge summaries, and it’s just abysmal. It’s absolutely abysmal,” she says. Without clear directives to providers in the next setting of care, such as a skilled-nursing facility, patients could be erroneously put back on a regular diet and aspirate, sending them right back to the hospital.
As one potential solution, Dr. Kind’s team is developing a multidisciplinary stroke discharge summary tool that automatically imports elements like speech-language pathology and dietary recommendations. Although most discharge communication may focus on more visible issues and interventions, Dr. Kind argues that some of the “bread and butter” concerns might ultimately prove just as important for long-term patient outcomes.
Karim Godamunne, MD, MBA, SFHM, vice president of clinical systems integration and medical director of Eagle Hospital Physicians in Atlanta, sees telemedicine as another potential tool to help reach patients after discharge, especially those who haven’t received follow-up care from a primary-care physician (PCP). “We need to be the champions at our hospitals for improving care processes, and we need to work in partnership with the nurses and the other professionals,” Dr. Godamunne says. “As a group, we can really make a difference, and stroke is one of those areas in which we can truly contribute.”
Bryn Nelson is a freelance medical writer in Seattle.
References
- Freeman WD, Dawson SB, Raper C, Thiemann K, et al. Neurohospitalists reduce length of stay for patients with ischemic stroke. The Neurohospitalist. 2011;1(2): 67-70.
- Howrey BT, Kuo Y-F, Goodwin JS. Association of care by hospitalists on discharge destination and 30-day outcomes after acute ischemic stroke. Medical Care. 2011;49(8): 701-707.
- Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2-e220.
- Glasheen JJ, Epstein KR, Siegal E, Kutner JS, Prochazka AV. The spectrum of community-based hospitalist practice: a call to tailor internal medicine residency training. Arch Intern Med. 2007;167(7):727-728.
- Plauth WH, Pantilat SZ, Wachter RM, Fenton CL. Hospitalists’ perceptions of their residency training needs: results of a national survey. Am J Med. 2001; 111(3):247-254.
- Dickerson LM, Carek PJ, Quattlebaum RG. Prevention of recurrent ischemic stroke. Am Fam Physician. 2007; 76(3):382-388.
- Fonarow GC, Smith EE, Saver JL, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123(7):750-758.
- Hacke W, Kaste M, Bluhmki E, Brozman M, et al. Thrombolysis with Alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317-1329.
- Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121:e91.
- Albers GW, Caplan LR, Easton JD, et al. Transient ischemic attack—proposal for a new definition. N Engl J Med. 2002;347(21):1713-1716.
- Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993-1003.
Stroke specialists like to say that “time is brain.” With an emphatic focus on those first few critical hours, however, it’s sometimes easy to overlook the vital role that hospitalists play in the days, weeks, and months that follow.
A recent study in The Neurohospitalist suggests that compared to community-based neurologists, practitioners of neurohospital medicine can reduce the length of stay for patients with ischemic stroke.1 A separate study, however, suggests that similar success might have come at a price for their less-specialized hospitalist counterparts.2 Among stroke patients, the latter study found that while the HM model is also associated with a reduced length of stay, it is associated with increased discharges to inpatient rehabilitation centers instead of to home, and higher readmission rates.
In sum, the evidence raises questions about whether rank-and-file hospitalists are adequately equipped to deal with a disease that is a core competency for the profession and ranks among the top sources of adult disability in the United States, at an estimated cost of $34.3 billion in 2008.3
“I think there’s been a mismatch between the training of the average hospitalist and then the expectations for the amount of neurological care they end up delivering once in practice,” says David Likosky, MD, SFHM, director of the stroke program at Evergreen Hospital Medical Center in Kirkland, Wash. “When surveyed, it’s been shown that hospitalists feel that care of stroke is one of the areas with which they’re least comfortable once they get out into practice.” Over the past decade, several studies have reinforced the notion of a training deficit.4,5
Demographic trends suggest that getting up to speed will be imperative, however. “One alarming thing we’re seeing is strokes among individuals that are not in the elderly group, and that group seems to be increasing at an alarming rate,” says Daniel T. Lackland, PhD, professor of epidemiology and neurosciences at the Medical University of South Carolina in Charleston. Hospitals are seeing more ischemic stroke patients in their 40s and 50s, likely a reflection of risk factors such as hypertension, diabetes, and hyperlipidemia that are occurring earlier in life. And because those patients are younger, the aftermath of a stroke could linger for decades.
Although the stroke mortality rate is declining in the U.S., statistics find that about 14% of all patients diagnosed with an initial stroke will have a second one within a year, placing continued strain on a healthcare system already stretched thin.6 Hospitalists, Dr. Lackland says, have an “ideal” opportunity to help build up and improve that system, potentially yielding significant cost savings along with the dramatic improvement in quality of life. Making the most of that opportunity, though, will require a solid understanding of multiple trends that are quickly transforming stroke care delivery.
Time Is of the Essence
Kevin Barrett, MD, MSc, assistant professor of neurology and stroke telemedicine director at the Mayo Clinic in Jacksonville, Fla., says hospitals are focusing more and more on a metric known as “door-to-needle time.” The goal is to treat at least half of incoming ischemic stroke patients with intravenous tissue-type plasminogen activator (IV tPA) within the first 60 minutes after onset of symptoms.
The American Heart Association/American Stroke Association has reinforced the message with its Get With the Guidelines Stroke Program. A recent analysis suggested the program has led to more timely tPA administration and, in turn, better patient outcomes (the program is funded in part through the Bristol-Myers Squib/Sanofi Pharmaceutical Partnership).7
At the same time, clinical research has widened the window for IV tPA delivery from three hours to 4.5 hours for certain patients after the onset of symptoms. Dr. Barrett says “strong evidence” from the European Cooperative Acute Stroke Study III has convinced most clinicians, and the FDA is expected to follow suit in officially approving the extension.8 As more stroke centers become certified, the use of IV tPA has increased accordingly.
Patients who have missed the time window or are not good candidates for IV tPA can still be aided by interarterial tPA at the site of the clot up to six hours after the onset of symptoms. Dr. Likosky says the treatment option should be of particular interest to hospitalists, given that strokes can occur post-operatively and in other patients who cannot receive IV tPA because of bleeding risk.
—Karim Godamunne, MD, MBA, SFHM, medical director, Eagle Hospital Physicians, Roswell, Ga.
For up to eight hours after the onset of symptoms, mechanical clot removal techniques have shown continued efficacy at revascularizing affected areas, with some newer options also offering greater promise of improving patient outcomes. Even with the prospects of declining complication rates, however, “evaluating and initiating treatment in a timely fashion is still going to be one of the most important predictors of outcome,” Dr. Barrett says.
After the initial intervention, hospitalists often are the go-to providers for anticipating and preventing common post-stroke complications, such as aspiration pneumonia, VTE from immobilization, and other infections. The proper use of anti-platelet agents and high-dose statins, also falling solidly within the HM realm, can pay big dividends if used consistently.
Meanwhile, newer studies and clinical observations are widening the scope of considerations that should be on every hospitalist’s radar. Here are a few cited by stroke experts:
Permissive hypertension. After an ischemic stroke, the benefit of permissive hypertension is still widely misunderstood. Perhaps counterintuitively, high blood pressure after a stroke can help protect the area of the brain that is damaged but not yet dead, sometimes called the penumbra. “I highlight this because I think it’s a common mistake, that internists are very used to high blood pressure being a bad thing,” says Andrew Josephson, MD, associate professor of clinical neurology and director of the neurohospitalist program at the University of California at San Francisco (UCSF) Medical Center. “And in general, it is; it’s a cause of stroke. But once somebody has a stroke, in the acute period, it’s important to allow the blood pressure to be high.”
Atrial fibrillation. The accepted role of atrial fibrillation in stroke is evolving. Research suggests that the common but often preventable arrhythmia is an important cause of stroke in about 15% to 20% of cases.9 By the time of hospital discharge, however, Dr. Josephson says physicians haven’t established a cause in about 1 in 4 cases. For these “cryptogenic strokes,” he says, doctors have long suspected that atrial fibrillation not picked up during the initial EKG or by the monitoring with cardiac telemetry could be a major cause.
Recent observations suggest that a longer monitoring period of up to 30 days may uncover atrial fibrillation in a sizable fraction of those patients, highlighting the importance of keeping a close eye on stroke patients both in the hospital and beyond. “It’s very important to identify, because atrial fibrillation changes what we do for folks to prevent a second stroke,” Dr. Josephson explains. Instead of anti-platelet medicine like aspirin, patients with atrial fibrillation often receive anticoagulants like warfarin, or the more recently approved dabigatran and rivaroxaban.
Transient ischemic attack. Improvements in imaging techniques like MRI have likewise begun to shift how stroke patients are treated. For example, Dr. Likosky says, medicine is moving away from a time-based definition of transient ischemic attack (TIA), in which symptoms resolve within 24 hours, to a tissue-based definition. Recent MRI imaging has uncovered evidence of a new infarction in more than half of patients initially diagnosed with TIA.10
“If they do have an infarction on their scan, even if they had symptoms that only lasted for five minutes, that’s a stroke,” Dr. Josephson says. And even a true TIA, he says, represents “a kind of stroke where you got really lucky and you’re not left with deficits, but the risk is still very high.” Accordingly, more patients with TIA are being admitted to the hospital to receive a full workup and preventive treatment. “We think that by evaluating these people urgently, we can reduce the risk of having a stroke by maybe 75% over a three-month time period,” Dr. Josephson says.
Hemorrhagic stroke. To date, the vast majority of patients with hemorrhagic stroke (which accounts for only 13% of all stroke cases) have been managed by neurosurgeons and neurologists. But here, too, Dr. Likosky says the picture could be changing. Recent findings that surgical treatment of intracranial hemorrhaging might not benefit many patients could shift the care paradigm toward a medical management strategy that involves more hospitalists.
Innovations Aplenty
The increasing complexity of stroke care and uneven distribution of resources and expertise have helped fuel several important innovations in delivery, most notably telestroke and neurohospital medicine. Both are being driven, in part, by an increased awareness of time-sensitive interventions and a frequent lack of on-site neurologists at smaller and more rural facilities. If telestroke programs are expanding the reach of neurologists, neurohospitalists are helping to fill the gaps in inpatient stroke care.
Amid the changes, one element is proving a necessary constant: a team approach that relies heavily on the HM emphasis on quality metrics, intensive monitoring, and careful coordination. Who better to lead the charge than hospitalists, says Mary E. Jensen, MD, professor of radiology and neurosurgery at the University of Virginia in Charlottesville. “They’re the ones who are in the hospital, and when these patients go bad, they go bad fast,” she says.
More broadly, Dr. Jensen says, hospitalists should get in on the ground floor when their facility seeks certification as a primary or a comprehensive stroke center. “And they need to make sure that the hospital isn’t just trying to get the sexy elements—the guy with the cath or the gal with the cath who can pull the clot out—but that they have a complete program that involves the care of the patient after they’ve had the procedure done,” she says.
As healthcare reform efforts are making clear, the responsibility doesn’t end after discharge, either. The Affordable Care Act includes a hospital readmission reduction program that will kick in this October, with penalties for hospitals posting unacceptably high 30-day readmission rates. Amy Kind, MD, PhD, assistant professor of medicine in the Division of Geriatrics at the University of Wisconsin School of Medicine and Public Health in Madison, is convinced that a key contributor to high rehospitalization rates among stroke patients may be the woefully incomplete nature of discharge communication.

—Mary E. Jensen, MD, professor of radiology and neurosurgery, University of Virginia, Charlottesville
Dr. Kind, for example, has found a disturbing pattern in communication regarding issues like dysphagia, a common complication among stroke patients and an important risk factor for pneumonia. Countering the risk usually requires such measures as putting patients on a special diet or elevating the head of their bed. “We looked at the quality of the communication of that information in discharge summaries, and it’s just abysmal. It’s absolutely abysmal,” she says. Without clear directives to providers in the next setting of care, such as a skilled-nursing facility, patients could be erroneously put back on a regular diet and aspirate, sending them right back to the hospital.
As one potential solution, Dr. Kind’s team is developing a multidisciplinary stroke discharge summary tool that automatically imports elements like speech-language pathology and dietary recommendations. Although most discharge communication may focus on more visible issues and interventions, Dr. Kind argues that some of the “bread and butter” concerns might ultimately prove just as important for long-term patient outcomes.
Karim Godamunne, MD, MBA, SFHM, vice president of clinical systems integration and medical director of Eagle Hospital Physicians in Atlanta, sees telemedicine as another potential tool to help reach patients after discharge, especially those who haven’t received follow-up care from a primary-care physician (PCP). “We need to be the champions at our hospitals for improving care processes, and we need to work in partnership with the nurses and the other professionals,” Dr. Godamunne says. “As a group, we can really make a difference, and stroke is one of those areas in which we can truly contribute.”
Bryn Nelson is a freelance medical writer in Seattle.
References
- Freeman WD, Dawson SB, Raper C, Thiemann K, et al. Neurohospitalists reduce length of stay for patients with ischemic stroke. The Neurohospitalist. 2011;1(2): 67-70.
- Howrey BT, Kuo Y-F, Goodwin JS. Association of care by hospitalists on discharge destination and 30-day outcomes after acute ischemic stroke. Medical Care. 2011;49(8): 701-707.
- Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2-e220.
- Glasheen JJ, Epstein KR, Siegal E, Kutner JS, Prochazka AV. The spectrum of community-based hospitalist practice: a call to tailor internal medicine residency training. Arch Intern Med. 2007;167(7):727-728.
- Plauth WH, Pantilat SZ, Wachter RM, Fenton CL. Hospitalists’ perceptions of their residency training needs: results of a national survey. Am J Med. 2001; 111(3):247-254.
- Dickerson LM, Carek PJ, Quattlebaum RG. Prevention of recurrent ischemic stroke. Am Fam Physician. 2007; 76(3):382-388.
- Fonarow GC, Smith EE, Saver JL, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123(7):750-758.
- Hacke W, Kaste M, Bluhmki E, Brozman M, et al. Thrombolysis with Alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317-1329.
- Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121:e91.
- Albers GW, Caplan LR, Easton JD, et al. Transient ischemic attack—proposal for a new definition. N Engl J Med. 2002;347(21):1713-1716.
- Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993-1003.
Professional Development Program Advances Hospitalist Leadership Skills
Akin to other doctors, hospitalists seek clinical and nonclinical continuing medical education (CME) opportunities in subjects that they hope will improve their professional skill set. But Emory School of Medicine’s Division of Hospital Medicine has tried to make this training more systematic for its 110 members. Since 2005, competitively awarded grants have supported faculty development training in the areas of administrative leadership, quality improvement and research, and education and training.
According to an abstract presented at HM11, Emory’s faculty development program has helped train 36 HM physicians. The upshot of the program: Thirty-three hospitalists now fill formal leadership positions in six Emory-affiliated hospitals. Examples include hospital chief medical officers, chief quality officers, and medical directors for care coordination.
“Hospital medicine is a young field, and we had a young group of clinicians lacking experience that other physicians might get in the course of a career,” says Daniel Dressler, MD, MSc, SFHM, director of education for the hospital medicine division of the Atlanta-based group. “If we were going to be asked to do things, leadershipwise, in the hospital, we needed to build a program to help individuals get additional training for them.”
The physicians pick courses in areas where they want to better themselves, either local educational offerings or national conferences. A committee applies a structured process for reviewing their applications, with funding coming from the department. “We ask the doctors to come back and report on what they learned,” says Dr. Dressler, an SHM board member.
Akin to other doctors, hospitalists seek clinical and nonclinical continuing medical education (CME) opportunities in subjects that they hope will improve their professional skill set. But Emory School of Medicine’s Division of Hospital Medicine has tried to make this training more systematic for its 110 members. Since 2005, competitively awarded grants have supported faculty development training in the areas of administrative leadership, quality improvement and research, and education and training.
According to an abstract presented at HM11, Emory’s faculty development program has helped train 36 HM physicians. The upshot of the program: Thirty-three hospitalists now fill formal leadership positions in six Emory-affiliated hospitals. Examples include hospital chief medical officers, chief quality officers, and medical directors for care coordination.
“Hospital medicine is a young field, and we had a young group of clinicians lacking experience that other physicians might get in the course of a career,” says Daniel Dressler, MD, MSc, SFHM, director of education for the hospital medicine division of the Atlanta-based group. “If we were going to be asked to do things, leadershipwise, in the hospital, we needed to build a program to help individuals get additional training for them.”
The physicians pick courses in areas where they want to better themselves, either local educational offerings or national conferences. A committee applies a structured process for reviewing their applications, with funding coming from the department. “We ask the doctors to come back and report on what they learned,” says Dr. Dressler, an SHM board member.
Akin to other doctors, hospitalists seek clinical and nonclinical continuing medical education (CME) opportunities in subjects that they hope will improve their professional skill set. But Emory School of Medicine’s Division of Hospital Medicine has tried to make this training more systematic for its 110 members. Since 2005, competitively awarded grants have supported faculty development training in the areas of administrative leadership, quality improvement and research, and education and training.
According to an abstract presented at HM11, Emory’s faculty development program has helped train 36 HM physicians. The upshot of the program: Thirty-three hospitalists now fill formal leadership positions in six Emory-affiliated hospitals. Examples include hospital chief medical officers, chief quality officers, and medical directors for care coordination.
“Hospital medicine is a young field, and we had a young group of clinicians lacking experience that other physicians might get in the course of a career,” says Daniel Dressler, MD, MSc, SFHM, director of education for the hospital medicine division of the Atlanta-based group. “If we were going to be asked to do things, leadershipwise, in the hospital, we needed to build a program to help individuals get additional training for them.”
The physicians pick courses in areas where they want to better themselves, either local educational offerings or national conferences. A committee applies a structured process for reviewing their applications, with funding coming from the department. “We ask the doctors to come back and report on what they learned,” says Dr. Dressler, an SHM board member.
Is a Post-Discharge Clinic in Your Hospital's Future?
The hospitalist concept was established on the foundation of timely, informative handoffs to primary-care physicians (PCPs) once a patient’s hospital stay is complete. With sicker patients and shorter hospital stays, pending test results, and complex post-discharge medication regimens to sort out, this handoff is crucial to successful discharges. But what if a discharged patient can’t get in to see the PCP, or has no established PCP?
Recent research on hospital readmissions by the Dartmouth Atlas Project found that only 42% of hospitalized Medicare patients had any contact with a primary-care clinician within 14 days of discharge.1 For patients with ongoing medical needs, such missed connections are a major contributor to hospital readmissions, and thus a target for hospitals and HM groups wanting to control their readmission rates before Medicare imposes reimbursement penalties starting in October 2012 (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
One proposed solution is the post-discharge clinic, typically located on or near a hospital’s campus and staffed by hospitalists, PCPs, or advanced-practice nurses. The patient can be seen once or a few times in the post-discharge clinic to make sure that health education started in the hospital is understood and followed, and that prescriptions ordered in the hospital are being taken on schedule.
—Lauren Doctoroff, MD, hospitalist, director, post-discharge clinic, Beth Israel Deaconess Medical Center, Boston
Mark V. Williams, MD, FACP, FHM, professor and chief of the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago, describes hospitalist-led post-discharge clinics as “Band-Aids for an inadequate primary-care system.” What would be better, he says, is focusing on the underlying problem and working to improve post-discharge access to primary care. Dr. Williams acknowledges, however, that sometimes a patch is needed to stanch the blood flow—e.g., to better manage care transitions—while waiting on healthcare reform and medical homes to improve care coordination throughout the system.
Working in a post-discharge clinic might seem like “a stretch for many hospitalists, especially those who chose this field because they didn’t want to do outpatient medicine,” says Lauren Doctoroff, MD, a hospitalist who directs a post-discharge clinic at Beth Israel Deaconess Medical Center (BIDMC) in Boston. “But there are times when it may be appropriate for hospital-based doctors to extend their responsibility out of the hospital.”
Dr. Doctoroff also says that working in such a clinic can be practice-changing for hospitalists. “All of a sudden, you have a different view of your hospitalized patients, and you start to ask different questions while they’re in the hospital than you ever did before,” she explains.
What is a Post-Discharge Clinic?
The post-discharge clinic, also known as a transitional-care clinic or after-care clinic, is intended to bridge medical coverage between the hospital and primary care. The clinic at BIDMC is for patients affiliated with its Health Care Associates faculty practice “discharged from either our hospital or another hospital, who need care that their PCP or specialist, because of scheduling conflicts, cannot provide within the needed time frame,” Dr. Doctoroff says.
Four hospitalists from BIDMC’s large HM group were selected to staff the clinic. The hospitalists work in one-month rotations (a total of three months on service per year), and are relieved of other responsibilities during their month in clinic. They provide five half-day clinic sessions per week, with a 40-minute-per-patient visit schedule. Thirty minutes are allotted for patients referred from the hospital’s ED who did not get admitted to the hospital but need clinical follow-up.
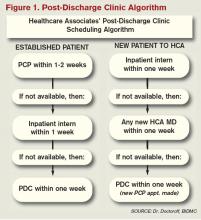
The clinic is based in a BIDMC-affiliated primary-care practice, “which allows us to use its administrative structure and logistical support,” Dr. Doctoroff explains. “A hospital-based administrative service helps set up outpatient visits prior to discharge using computerized physician order entry and a scheduling algorhythm.” (See Figure 1) Patients who can be seen by their PCP in a timely fashion are referred to the PCP office; if not, they are scheduled in the post-discharge clinic. “That helps preserve the PCP relationship, which I think is paramount,” she says.
The first two years were spent getting the clinic established, but in the near future, BIDMC will start measuring such outcomes as access to care and quality. “But not necessarily readmission rates,” Dr. Doctoroff adds. “I know many people think of post-discharge clinics in the context of preventing readmissions, although we don’t have the data yet to fully support that. In fact, some readmissions may result from seeing a doctor. If you get a closer look at some patients after discharge and they are doing badly, they are more likely to be readmitted than if they had just stayed home.” In such cases, readmission could actually be a better outcome for the patient, she notes.
Dr. Doctoroff describes a typical user of her post-discharge clinic as a non-English-speaking patient who was discharged from the hospital with severe back pain from a herniated disk. “He came back to see me 10 days later, still barely able to walk. He hadn’t been able to fill any of the prescriptions from his hospital stay. Within two hours after I saw him, we got his meds filled and outpatient services set up,” she says. “We take care of many patients like him in the hospital with acute pain issues, whom we discharge as soon as they can walk, and later we see them limping into outpatient clinics. It makes me think differently now about how I plan their discharges.”

—Shay Martinez, MD, hospitalist, medical director, Harborview Medical Center, Seattle
Who else needs these clinics? Dr. Doctoroff suggests two ways of looking at the question.
“Even for a simple patient admitted to the hospital, that can represent a significant change in the medical picture—a sort of sentinel event. In the discharge clinic, we give them an opportunity to review the hospitalization and answer their questions,” she says. “A lot of information presented to patients in the hospital is not well heard, and the initial visit may be their first time to really talk about what happened.” For other patients with conditions such as congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), or poorly controlled diabetes, treatment guidelines might dictate a pattern for post-discharge follow-up—for example, medical visits in seven or 10 days.
In Seattle, Harborview Medical Center established its After Care Clinic, staffed by hospitalists and nurse practitioners, to provide transitional care for patients discharged from inpatient wards or the ED in need of follow-up, says medical director and hospitalist Shay Martinez, MD. A second priority is to see any CHF patient within 48 hours of discharge.
“We try to limit patients to a maximum of three visits in our clinic,” she says. “At that point, we help them get established in a medical home, either here in one of our primary-care clinics, or in one of the many excellent community clinics in the area.
“This model works well with our patient population. We actually try to do primary care on the inpatient side as well. Our hospitalists are specialized in that approach, given our patient population. We see a lot of immigrants, non-English speakers, people with low health literacy, and the homeless, many of whom lack primary care,” Dr. Martinez says. “We do medication reconciliation, reassessments, and follow-ups with lab tests. We also try to assess who is more likely to be a no-show, and who needs more help with scheduling follow-up appointments.”
Clinical coverage of post-discharge clinics varies by setting, staffing, and scope. If demand is low, hospitalists or ED physicians can be called off the floor to see patients who return to the clinic, or they could staff the clinic after their hospitalist shift ends. Post-discharge clinic staff whose schedules are light can flex into providing primary-care visits in the clinic. Post-discharge can also could be provided in conjunction with—or as an alternative to—physician house calls to patients’ homes. Some post-discharge clinics work with medical call centers or telephonic case managers; some even use telemedicine.
It also could be a growth opportunity for hospitalist practices. “It is an exciting potential role for hospitalists interested in doing a little outpatient care,” Dr. Martinez says. “This is also a good way to be a safety net for your safety-net hospital.”
continued below...
Partner with Community
Tallahassee (Fla.) Memorial Hospital (TMH) in February launched a transitional-care clinic in collaboration with faculty from Florida State University, community-based health providers, and the local Capital Health Plan. Hospitalists don’t staff the clinic, but the HM group is its major source of referrals, says Dean Watson, MD, chief medical officer at TMH. Patients can be followed for up to eight weeks, during which time they get comprehensive assessments, medication review and optimization, and referral by the clinic social worker to a PCP and to available community services.
“Three years ago, we came up with the idea for a patient population we know is at high risk for readmission. Why don’t we partner with organizations in the community, form a clinic, teach students and residents, and learn together?” Dr. Watson says. “In addition to the usual patients, TMH targets those who have been readmitted to the hospital three times or more in the past year.”
The clinic, open five days a week, is staffed by a physician, nurse practitioner, telephonic nurse, and social worker, and also has a geriatric assessment clinic.
“We set up a system to identify patients through our electronic health record, and when they come to the clinic, we focus on their social environment and other non-medical issues that might cause readmissions,” he says. The clinic has a pharmacy and funds to support medications for patients without insurance. “In our first six months, we reduced emergency room visits and readmissions for these patients by 68 percent.”
One key partner, Capital Health Plan, bought and refurbished a building, and made it available for the clinic at no cost. Capital’s motivation, says Tom Glennon, a senior vice president for the plan, is its commitment to the community and to community service.
“We’re a nonprofit HMO. We’re focused on what we can do to serve the community, and we’re looking at this as a way for the hospital to have fewer costly, unreimbursed bouncebacks,” Glennon says. “That’s a win-win for all of us.”
Most of the patients who use the clinic are not members of Capital Health Plan, Glennon adds. “If we see CHP members turning up at the transitions clinic, then we have a problem—a breakdown in our case management,” he explains. “Our goal is to have our members taken care of by primary-care providers.”
Hard Data? Not So Fast
How many post-discharge clinics are in operation today is not known. Fundamental financial data, too, are limited, but some say it is unlikely a post-discharge clinic will cover operating expenses from billing revenues alone.
Thus, such clinics will require funding from the hospital, HM group, health system, or health plans, based on the benefits the clinic provides to discharged patients and the impact on 30-day readmissions (for more about the logistical challenges post-discharge clinics present, see “What Do PCPs Think?”).
Some also suggest that many of the post-discharge clinics now in operation are too new to have demonstrated financial impact or return on investment. “We have not yet been asked to show our financial viability,” Dr. Doctoroff says. “I think the clinic leadership thinks we are fulfilling other goals for now, such as creating easier access for their patients after discharge.”
Amy Boutwell, MD, MPP, a hospitalist at Newton Wellesley Hospital in Massachusetts and founder of Collaborative Healthcare Strategies, is among the post-discharge skeptics. She agrees with Dr. Williams that the post-discharge concept is more of a temporary fix to the long-term issues in primary care. “I think the idea is getting more play than actual activity out there right now,” she says. “We need to find opportunities to manage transitions within our scope today and tomorrow while strategically looking at where we want to be in five years [as hospitals and health systems].”
Dr. Boutwell says she’s experienced the frustration of trying to make follow-up appointments with physicians who don’t have any open slots for hospitalized patients awaiting discharge. “We think of follow up as physician-led, but there are alternatives and physician extenders,” she says. “It is well-documented that our healthcare system underuses home health care and other services that might be helpful. We forget how many other opportunities there are in our communities to get another clinician to touch the patient.”
Hospitalists, as key players in the healthcare system, can speak out in support of strengthening primary-care networks and building more collaborative relationships with PCPs, according to Dr. Williams. “If you’re going to set up an outpatient clinic, ideally, have it staffed by PCPs who can funnel the patients into primary-care networks. If that’s not feasible, then hospitalists should proceed with caution, since this approach begins to take them out of their scope of practice,” he says.
With 13 years of experience in urban hospital settings, Dr. Williams is familiar with the dangers unassigned patients present at discharge. “But I don’t know that we’ve yet optimized the hospital discharge process at any hospital in the United States,” he says.
That said, Dr. Williams knows his hospital in downtown Chicago is now working to establish a post-discharge clinic. It will be staffed by PCPs and will target patients who don’t have a PCP, are on Medicaid, or lack insurance.
“Where it starts to make me uncomfortable,” Dr. Williams says, “is what happens when you follow patients out into the outpatient setting?
It’s hard to do just one visit and draw the line. Yes, you may prevent a readmission, but the patient is still left with chronic illness and the need for primary care.”
Larry Beresford is a freelance writer based in Oakland, Calif.
References
- Goodman, DC, Fisher ES, Chang C. After Hospitalization: A Dartmouth Atlas Report on Post-Acute Care for Medicare Beneficiaries. Dartmouth Atlas website. Available at: www.dartmouthatlas.org/downloads/reports/Post_discharge_events_092811.pdf. Accessed Nov. 3, 2011.
- Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 3-day rehospitalization: A systematic review. Ann Int Med. 2011;155(8): 520-528.
- Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392-397.
- Shu CC, Hsu NC, Lin YF, et al. Integrated post-discharge transitional care in Taiwan. BMC Medicine website. Available at: www.biomedcentral.com/1741-7015/9/96. Accessed Nov. 1, 2011.
The hospitalist concept was established on the foundation of timely, informative handoffs to primary-care physicians (PCPs) once a patient’s hospital stay is complete. With sicker patients and shorter hospital stays, pending test results, and complex post-discharge medication regimens to sort out, this handoff is crucial to successful discharges. But what if a discharged patient can’t get in to see the PCP, or has no established PCP?
Recent research on hospital readmissions by the Dartmouth Atlas Project found that only 42% of hospitalized Medicare patients had any contact with a primary-care clinician within 14 days of discharge.1 For patients with ongoing medical needs, such missed connections are a major contributor to hospital readmissions, and thus a target for hospitals and HM groups wanting to control their readmission rates before Medicare imposes reimbursement penalties starting in October 2012 (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
One proposed solution is the post-discharge clinic, typically located on or near a hospital’s campus and staffed by hospitalists, PCPs, or advanced-practice nurses. The patient can be seen once or a few times in the post-discharge clinic to make sure that health education started in the hospital is understood and followed, and that prescriptions ordered in the hospital are being taken on schedule.
—Lauren Doctoroff, MD, hospitalist, director, post-discharge clinic, Beth Israel Deaconess Medical Center, Boston
Mark V. Williams, MD, FACP, FHM, professor and chief of the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago, describes hospitalist-led post-discharge clinics as “Band-Aids for an inadequate primary-care system.” What would be better, he says, is focusing on the underlying problem and working to improve post-discharge access to primary care. Dr. Williams acknowledges, however, that sometimes a patch is needed to stanch the blood flow—e.g., to better manage care transitions—while waiting on healthcare reform and medical homes to improve care coordination throughout the system.
Working in a post-discharge clinic might seem like “a stretch for many hospitalists, especially those who chose this field because they didn’t want to do outpatient medicine,” says Lauren Doctoroff, MD, a hospitalist who directs a post-discharge clinic at Beth Israel Deaconess Medical Center (BIDMC) in Boston. “But there are times when it may be appropriate for hospital-based doctors to extend their responsibility out of the hospital.”
Dr. Doctoroff also says that working in such a clinic can be practice-changing for hospitalists. “All of a sudden, you have a different view of your hospitalized patients, and you start to ask different questions while they’re in the hospital than you ever did before,” she explains.
What is a Post-Discharge Clinic?
The post-discharge clinic, also known as a transitional-care clinic or after-care clinic, is intended to bridge medical coverage between the hospital and primary care. The clinic at BIDMC is for patients affiliated with its Health Care Associates faculty practice “discharged from either our hospital or another hospital, who need care that their PCP or specialist, because of scheduling conflicts, cannot provide within the needed time frame,” Dr. Doctoroff says.
Four hospitalists from BIDMC’s large HM group were selected to staff the clinic. The hospitalists work in one-month rotations (a total of three months on service per year), and are relieved of other responsibilities during their month in clinic. They provide five half-day clinic sessions per week, with a 40-minute-per-patient visit schedule. Thirty minutes are allotted for patients referred from the hospital’s ED who did not get admitted to the hospital but need clinical follow-up.
The clinic is based in a BIDMC-affiliated primary-care practice, “which allows us to use its administrative structure and logistical support,” Dr. Doctoroff explains. “A hospital-based administrative service helps set up outpatient visits prior to discharge using computerized physician order entry and a scheduling algorhythm.” (See Figure 1) Patients who can be seen by their PCP in a timely fashion are referred to the PCP office; if not, they are scheduled in the post-discharge clinic. “That helps preserve the PCP relationship, which I think is paramount,” she says.
The first two years were spent getting the clinic established, but in the near future, BIDMC will start measuring such outcomes as access to care and quality. “But not necessarily readmission rates,” Dr. Doctoroff adds. “I know many people think of post-discharge clinics in the context of preventing readmissions, although we don’t have the data yet to fully support that. In fact, some readmissions may result from seeing a doctor. If you get a closer look at some patients after discharge and they are doing badly, they are more likely to be readmitted than if they had just stayed home.” In such cases, readmission could actually be a better outcome for the patient, she notes.
Dr. Doctoroff describes a typical user of her post-discharge clinic as a non-English-speaking patient who was discharged from the hospital with severe back pain from a herniated disk. “He came back to see me 10 days later, still barely able to walk. He hadn’t been able to fill any of the prescriptions from his hospital stay. Within two hours after I saw him, we got his meds filled and outpatient services set up,” she says. “We take care of many patients like him in the hospital with acute pain issues, whom we discharge as soon as they can walk, and later we see them limping into outpatient clinics. It makes me think differently now about how I plan their discharges.”

—Shay Martinez, MD, hospitalist, medical director, Harborview Medical Center, Seattle
Who else needs these clinics? Dr. Doctoroff suggests two ways of looking at the question.
“Even for a simple patient admitted to the hospital, that can represent a significant change in the medical picture—a sort of sentinel event. In the discharge clinic, we give them an opportunity to review the hospitalization and answer their questions,” she says. “A lot of information presented to patients in the hospital is not well heard, and the initial visit may be their first time to really talk about what happened.” For other patients with conditions such as congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), or poorly controlled diabetes, treatment guidelines might dictate a pattern for post-discharge follow-up—for example, medical visits in seven or 10 days.
In Seattle, Harborview Medical Center established its After Care Clinic, staffed by hospitalists and nurse practitioners, to provide transitional care for patients discharged from inpatient wards or the ED in need of follow-up, says medical director and hospitalist Shay Martinez, MD. A second priority is to see any CHF patient within 48 hours of discharge.
“We try to limit patients to a maximum of three visits in our clinic,” she says. “At that point, we help them get established in a medical home, either here in one of our primary-care clinics, or in one of the many excellent community clinics in the area.
“This model works well with our patient population. We actually try to do primary care on the inpatient side as well. Our hospitalists are specialized in that approach, given our patient population. We see a lot of immigrants, non-English speakers, people with low health literacy, and the homeless, many of whom lack primary care,” Dr. Martinez says. “We do medication reconciliation, reassessments, and follow-ups with lab tests. We also try to assess who is more likely to be a no-show, and who needs more help with scheduling follow-up appointments.”
Clinical coverage of post-discharge clinics varies by setting, staffing, and scope. If demand is low, hospitalists or ED physicians can be called off the floor to see patients who return to the clinic, or they could staff the clinic after their hospitalist shift ends. Post-discharge clinic staff whose schedules are light can flex into providing primary-care visits in the clinic. Post-discharge can also could be provided in conjunction with—or as an alternative to—physician house calls to patients’ homes. Some post-discharge clinics work with medical call centers or telephonic case managers; some even use telemedicine.
It also could be a growth opportunity for hospitalist practices. “It is an exciting potential role for hospitalists interested in doing a little outpatient care,” Dr. Martinez says. “This is also a good way to be a safety net for your safety-net hospital.”
continued below...
Partner with Community
Tallahassee (Fla.) Memorial Hospital (TMH) in February launched a transitional-care clinic in collaboration with faculty from Florida State University, community-based health providers, and the local Capital Health Plan. Hospitalists don’t staff the clinic, but the HM group is its major source of referrals, says Dean Watson, MD, chief medical officer at TMH. Patients can be followed for up to eight weeks, during which time they get comprehensive assessments, medication review and optimization, and referral by the clinic social worker to a PCP and to available community services.
“Three years ago, we came up with the idea for a patient population we know is at high risk for readmission. Why don’t we partner with organizations in the community, form a clinic, teach students and residents, and learn together?” Dr. Watson says. “In addition to the usual patients, TMH targets those who have been readmitted to the hospital three times or more in the past year.”
The clinic, open five days a week, is staffed by a physician, nurse practitioner, telephonic nurse, and social worker, and also has a geriatric assessment clinic.
“We set up a system to identify patients through our electronic health record, and when they come to the clinic, we focus on their social environment and other non-medical issues that might cause readmissions,” he says. The clinic has a pharmacy and funds to support medications for patients without insurance. “In our first six months, we reduced emergency room visits and readmissions for these patients by 68 percent.”
One key partner, Capital Health Plan, bought and refurbished a building, and made it available for the clinic at no cost. Capital’s motivation, says Tom Glennon, a senior vice president for the plan, is its commitment to the community and to community service.
“We’re a nonprofit HMO. We’re focused on what we can do to serve the community, and we’re looking at this as a way for the hospital to have fewer costly, unreimbursed bouncebacks,” Glennon says. “That’s a win-win for all of us.”
Most of the patients who use the clinic are not members of Capital Health Plan, Glennon adds. “If we see CHP members turning up at the transitions clinic, then we have a problem—a breakdown in our case management,” he explains. “Our goal is to have our members taken care of by primary-care providers.”
Hard Data? Not So Fast
How many post-discharge clinics are in operation today is not known. Fundamental financial data, too, are limited, but some say it is unlikely a post-discharge clinic will cover operating expenses from billing revenues alone.
Thus, such clinics will require funding from the hospital, HM group, health system, or health plans, based on the benefits the clinic provides to discharged patients and the impact on 30-day readmissions (for more about the logistical challenges post-discharge clinics present, see “What Do PCPs Think?”).
Some also suggest that many of the post-discharge clinics now in operation are too new to have demonstrated financial impact or return on investment. “We have not yet been asked to show our financial viability,” Dr. Doctoroff says. “I think the clinic leadership thinks we are fulfilling other goals for now, such as creating easier access for their patients after discharge.”
Amy Boutwell, MD, MPP, a hospitalist at Newton Wellesley Hospital in Massachusetts and founder of Collaborative Healthcare Strategies, is among the post-discharge skeptics. She agrees with Dr. Williams that the post-discharge concept is more of a temporary fix to the long-term issues in primary care. “I think the idea is getting more play than actual activity out there right now,” she says. “We need to find opportunities to manage transitions within our scope today and tomorrow while strategically looking at where we want to be in five years [as hospitals and health systems].”
Dr. Boutwell says she’s experienced the frustration of trying to make follow-up appointments with physicians who don’t have any open slots for hospitalized patients awaiting discharge. “We think of follow up as physician-led, but there are alternatives and physician extenders,” she says. “It is well-documented that our healthcare system underuses home health care and other services that might be helpful. We forget how many other opportunities there are in our communities to get another clinician to touch the patient.”
Hospitalists, as key players in the healthcare system, can speak out in support of strengthening primary-care networks and building more collaborative relationships with PCPs, according to Dr. Williams. “If you’re going to set up an outpatient clinic, ideally, have it staffed by PCPs who can funnel the patients into primary-care networks. If that’s not feasible, then hospitalists should proceed with caution, since this approach begins to take them out of their scope of practice,” he says.
With 13 years of experience in urban hospital settings, Dr. Williams is familiar with the dangers unassigned patients present at discharge. “But I don’t know that we’ve yet optimized the hospital discharge process at any hospital in the United States,” he says.
That said, Dr. Williams knows his hospital in downtown Chicago is now working to establish a post-discharge clinic. It will be staffed by PCPs and will target patients who don’t have a PCP, are on Medicaid, or lack insurance.
“Where it starts to make me uncomfortable,” Dr. Williams says, “is what happens when you follow patients out into the outpatient setting?
It’s hard to do just one visit and draw the line. Yes, you may prevent a readmission, but the patient is still left with chronic illness and the need for primary care.”
Larry Beresford is a freelance writer based in Oakland, Calif.
References
- Goodman, DC, Fisher ES, Chang C. After Hospitalization: A Dartmouth Atlas Report on Post-Acute Care for Medicare Beneficiaries. Dartmouth Atlas website. Available at: www.dartmouthatlas.org/downloads/reports/Post_discharge_events_092811.pdf. Accessed Nov. 3, 2011.
- Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 3-day rehospitalization: A systematic review. Ann Int Med. 2011;155(8): 520-528.
- Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392-397.
- Shu CC, Hsu NC, Lin YF, et al. Integrated post-discharge transitional care in Taiwan. BMC Medicine website. Available at: www.biomedcentral.com/1741-7015/9/96. Accessed Nov. 1, 2011.
The hospitalist concept was established on the foundation of timely, informative handoffs to primary-care physicians (PCPs) once a patient’s hospital stay is complete. With sicker patients and shorter hospital stays, pending test results, and complex post-discharge medication regimens to sort out, this handoff is crucial to successful discharges. But what if a discharged patient can’t get in to see the PCP, or has no established PCP?
Recent research on hospital readmissions by the Dartmouth Atlas Project found that only 42% of hospitalized Medicare patients had any contact with a primary-care clinician within 14 days of discharge.1 For patients with ongoing medical needs, such missed connections are a major contributor to hospital readmissions, and thus a target for hospitals and HM groups wanting to control their readmission rates before Medicare imposes reimbursement penalties starting in October 2012 (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
One proposed solution is the post-discharge clinic, typically located on or near a hospital’s campus and staffed by hospitalists, PCPs, or advanced-practice nurses. The patient can be seen once or a few times in the post-discharge clinic to make sure that health education started in the hospital is understood and followed, and that prescriptions ordered in the hospital are being taken on schedule.
—Lauren Doctoroff, MD, hospitalist, director, post-discharge clinic, Beth Israel Deaconess Medical Center, Boston
Mark V. Williams, MD, FACP, FHM, professor and chief of the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago, describes hospitalist-led post-discharge clinics as “Band-Aids for an inadequate primary-care system.” What would be better, he says, is focusing on the underlying problem and working to improve post-discharge access to primary care. Dr. Williams acknowledges, however, that sometimes a patch is needed to stanch the blood flow—e.g., to better manage care transitions—while waiting on healthcare reform and medical homes to improve care coordination throughout the system.
Working in a post-discharge clinic might seem like “a stretch for many hospitalists, especially those who chose this field because they didn’t want to do outpatient medicine,” says Lauren Doctoroff, MD, a hospitalist who directs a post-discharge clinic at Beth Israel Deaconess Medical Center (BIDMC) in Boston. “But there are times when it may be appropriate for hospital-based doctors to extend their responsibility out of the hospital.”
Dr. Doctoroff also says that working in such a clinic can be practice-changing for hospitalists. “All of a sudden, you have a different view of your hospitalized patients, and you start to ask different questions while they’re in the hospital than you ever did before,” she explains.
What is a Post-Discharge Clinic?
The post-discharge clinic, also known as a transitional-care clinic or after-care clinic, is intended to bridge medical coverage between the hospital and primary care. The clinic at BIDMC is for patients affiliated with its Health Care Associates faculty practice “discharged from either our hospital or another hospital, who need care that their PCP or specialist, because of scheduling conflicts, cannot provide within the needed time frame,” Dr. Doctoroff says.
Four hospitalists from BIDMC’s large HM group were selected to staff the clinic. The hospitalists work in one-month rotations (a total of three months on service per year), and are relieved of other responsibilities during their month in clinic. They provide five half-day clinic sessions per week, with a 40-minute-per-patient visit schedule. Thirty minutes are allotted for patients referred from the hospital’s ED who did not get admitted to the hospital but need clinical follow-up.
The clinic is based in a BIDMC-affiliated primary-care practice, “which allows us to use its administrative structure and logistical support,” Dr. Doctoroff explains. “A hospital-based administrative service helps set up outpatient visits prior to discharge using computerized physician order entry and a scheduling algorhythm.” (See Figure 1) Patients who can be seen by their PCP in a timely fashion are referred to the PCP office; if not, they are scheduled in the post-discharge clinic. “That helps preserve the PCP relationship, which I think is paramount,” she says.
The first two years were spent getting the clinic established, but in the near future, BIDMC will start measuring such outcomes as access to care and quality. “But not necessarily readmission rates,” Dr. Doctoroff adds. “I know many people think of post-discharge clinics in the context of preventing readmissions, although we don’t have the data yet to fully support that. In fact, some readmissions may result from seeing a doctor. If you get a closer look at some patients after discharge and they are doing badly, they are more likely to be readmitted than if they had just stayed home.” In such cases, readmission could actually be a better outcome for the patient, she notes.
Dr. Doctoroff describes a typical user of her post-discharge clinic as a non-English-speaking patient who was discharged from the hospital with severe back pain from a herniated disk. “He came back to see me 10 days later, still barely able to walk. He hadn’t been able to fill any of the prescriptions from his hospital stay. Within two hours after I saw him, we got his meds filled and outpatient services set up,” she says. “We take care of many patients like him in the hospital with acute pain issues, whom we discharge as soon as they can walk, and later we see them limping into outpatient clinics. It makes me think differently now about how I plan their discharges.”

—Shay Martinez, MD, hospitalist, medical director, Harborview Medical Center, Seattle
Who else needs these clinics? Dr. Doctoroff suggests two ways of looking at the question.
“Even for a simple patient admitted to the hospital, that can represent a significant change in the medical picture—a sort of sentinel event. In the discharge clinic, we give them an opportunity to review the hospitalization and answer their questions,” she says. “A lot of information presented to patients in the hospital is not well heard, and the initial visit may be their first time to really talk about what happened.” For other patients with conditions such as congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), or poorly controlled diabetes, treatment guidelines might dictate a pattern for post-discharge follow-up—for example, medical visits in seven or 10 days.
In Seattle, Harborview Medical Center established its After Care Clinic, staffed by hospitalists and nurse practitioners, to provide transitional care for patients discharged from inpatient wards or the ED in need of follow-up, says medical director and hospitalist Shay Martinez, MD. A second priority is to see any CHF patient within 48 hours of discharge.
“We try to limit patients to a maximum of three visits in our clinic,” she says. “At that point, we help them get established in a medical home, either here in one of our primary-care clinics, or in one of the many excellent community clinics in the area.
“This model works well with our patient population. We actually try to do primary care on the inpatient side as well. Our hospitalists are specialized in that approach, given our patient population. We see a lot of immigrants, non-English speakers, people with low health literacy, and the homeless, many of whom lack primary care,” Dr. Martinez says. “We do medication reconciliation, reassessments, and follow-ups with lab tests. We also try to assess who is more likely to be a no-show, and who needs more help with scheduling follow-up appointments.”
Clinical coverage of post-discharge clinics varies by setting, staffing, and scope. If demand is low, hospitalists or ED physicians can be called off the floor to see patients who return to the clinic, or they could staff the clinic after their hospitalist shift ends. Post-discharge clinic staff whose schedules are light can flex into providing primary-care visits in the clinic. Post-discharge can also could be provided in conjunction with—or as an alternative to—physician house calls to patients’ homes. Some post-discharge clinics work with medical call centers or telephonic case managers; some even use telemedicine.
It also could be a growth opportunity for hospitalist practices. “It is an exciting potential role for hospitalists interested in doing a little outpatient care,” Dr. Martinez says. “This is also a good way to be a safety net for your safety-net hospital.”
continued below...
Partner with Community
Tallahassee (Fla.) Memorial Hospital (TMH) in February launched a transitional-care clinic in collaboration with faculty from Florida State University, community-based health providers, and the local Capital Health Plan. Hospitalists don’t staff the clinic, but the HM group is its major source of referrals, says Dean Watson, MD, chief medical officer at TMH. Patients can be followed for up to eight weeks, during which time they get comprehensive assessments, medication review and optimization, and referral by the clinic social worker to a PCP and to available community services.
“Three years ago, we came up with the idea for a patient population we know is at high risk for readmission. Why don’t we partner with organizations in the community, form a clinic, teach students and residents, and learn together?” Dr. Watson says. “In addition to the usual patients, TMH targets those who have been readmitted to the hospital three times or more in the past year.”
The clinic, open five days a week, is staffed by a physician, nurse practitioner, telephonic nurse, and social worker, and also has a geriatric assessment clinic.
“We set up a system to identify patients through our electronic health record, and when they come to the clinic, we focus on their social environment and other non-medical issues that might cause readmissions,” he says. The clinic has a pharmacy and funds to support medications for patients without insurance. “In our first six months, we reduced emergency room visits and readmissions for these patients by 68 percent.”
One key partner, Capital Health Plan, bought and refurbished a building, and made it available for the clinic at no cost. Capital’s motivation, says Tom Glennon, a senior vice president for the plan, is its commitment to the community and to community service.
“We’re a nonprofit HMO. We’re focused on what we can do to serve the community, and we’re looking at this as a way for the hospital to have fewer costly, unreimbursed bouncebacks,” Glennon says. “That’s a win-win for all of us.”
Most of the patients who use the clinic are not members of Capital Health Plan, Glennon adds. “If we see CHP members turning up at the transitions clinic, then we have a problem—a breakdown in our case management,” he explains. “Our goal is to have our members taken care of by primary-care providers.”
Hard Data? Not So Fast
How many post-discharge clinics are in operation today is not known. Fundamental financial data, too, are limited, but some say it is unlikely a post-discharge clinic will cover operating expenses from billing revenues alone.
Thus, such clinics will require funding from the hospital, HM group, health system, or health plans, based on the benefits the clinic provides to discharged patients and the impact on 30-day readmissions (for more about the logistical challenges post-discharge clinics present, see “What Do PCPs Think?”).
Some also suggest that many of the post-discharge clinics now in operation are too new to have demonstrated financial impact or return on investment. “We have not yet been asked to show our financial viability,” Dr. Doctoroff says. “I think the clinic leadership thinks we are fulfilling other goals for now, such as creating easier access for their patients after discharge.”
Amy Boutwell, MD, MPP, a hospitalist at Newton Wellesley Hospital in Massachusetts and founder of Collaborative Healthcare Strategies, is among the post-discharge skeptics. She agrees with Dr. Williams that the post-discharge concept is more of a temporary fix to the long-term issues in primary care. “I think the idea is getting more play than actual activity out there right now,” she says. “We need to find opportunities to manage transitions within our scope today and tomorrow while strategically looking at where we want to be in five years [as hospitals and health systems].”
Dr. Boutwell says she’s experienced the frustration of trying to make follow-up appointments with physicians who don’t have any open slots for hospitalized patients awaiting discharge. “We think of follow up as physician-led, but there are alternatives and physician extenders,” she says. “It is well-documented that our healthcare system underuses home health care and other services that might be helpful. We forget how many other opportunities there are in our communities to get another clinician to touch the patient.”
Hospitalists, as key players in the healthcare system, can speak out in support of strengthening primary-care networks and building more collaborative relationships with PCPs, according to Dr. Williams. “If you’re going to set up an outpatient clinic, ideally, have it staffed by PCPs who can funnel the patients into primary-care networks. If that’s not feasible, then hospitalists should proceed with caution, since this approach begins to take them out of their scope of practice,” he says.
With 13 years of experience in urban hospital settings, Dr. Williams is familiar with the dangers unassigned patients present at discharge. “But I don’t know that we’ve yet optimized the hospital discharge process at any hospital in the United States,” he says.
That said, Dr. Williams knows his hospital in downtown Chicago is now working to establish a post-discharge clinic. It will be staffed by PCPs and will target patients who don’t have a PCP, are on Medicaid, or lack insurance.
“Where it starts to make me uncomfortable,” Dr. Williams says, “is what happens when you follow patients out into the outpatient setting?
It’s hard to do just one visit and draw the line. Yes, you may prevent a readmission, but the patient is still left with chronic illness and the need for primary care.”
Larry Beresford is a freelance writer based in Oakland, Calif.
References
- Goodman, DC, Fisher ES, Chang C. After Hospitalization: A Dartmouth Atlas Report on Post-Acute Care for Medicare Beneficiaries. Dartmouth Atlas website. Available at: www.dartmouthatlas.org/downloads/reports/Post_discharge_events_092811.pdf. Accessed Nov. 3, 2011.
- Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 3-day rehospitalization: A systematic review. Ann Int Med. 2011;155(8): 520-528.
- Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392-397.
- Shu CC, Hsu NC, Lin YF, et al. Integrated post-discharge transitional care in Taiwan. BMC Medicine website. Available at: www.biomedcentral.com/1741-7015/9/96. Accessed Nov. 1, 2011.
HM@15 - Are You Living Up to High Expectations of Efficiency?
In 2002, a summary article in the Journal of the American Medical Association helped put the relatively small but rapidly growing HM profession on the map. Reviewing the available data, Robert Wachter, MD, MHM, and Lee Goldman, MD, MPH, of the University of California at San Francisco (UCSF) concluded that implementing a hospitalist program yielded an average savings of 13.4% in hospital costs and a 16.6% reduction in the length of stay (LOS).1
A decade later, the idea of efficiency has become so intertwined with hospitalists that SHM has included the concept in its definition of a profession that now comprises more than 30,000 doctors, nurses, and other care providers. HM practitioners work to enhance hospital and healthcare performance, in part, through “efficient use of hospital and healthcare resources,” according to SHM.
The growth of any profession can create exceptions and outliers, and observers point out that HM programs have become as varied as the hospitals in which they reside, complicating any attempt at broad generalizations. As a core part of the job description, though, efficiency and its implied benefit on costs have been widely promoted as arguments for expanding HM’s reach.
So are hospitalists meeting the lofty expectations?
A Look at the Evidence
A large retrospective study that examined outcomes of care for nearly 77,000 patients in 45 hospitals found that those cared for by hospitalists had a “modestly shorter” stay (by 0.4 days) in the hospital than those cared for by either general internists or family physicians.2 Hospitalists saved about $270 per hospitalization compared with general internists but only about $125 per stay compared with family physicians, the latter of which was not deemed statistically significant.
A more recent review of 33 studies found general agreement that hospitalist care led to reduced costs and length of stay but revealed less uniformity in the impacts on quality and patient outcomes.3
A more dramatic—albeit smaller—affirmation of HM as an efficient force has come from a study of patients admitted to 200-bed Olive View-UCLA Medical Center in Sylmar, Calif. The study, led by assistant medical director Scott Lundberg, MD, concluded that the arrival of an academic hospitalist program led to a one-year increase of $2.3 million in reimbursements from Medi-Cal, California’s Medicaid program.4
“Most other places that have demonstrated the cost-effectiveness of hospitalists generally point to reducing length of stay, which therefore reduces the costs,” Dr. Lundberg says. Under Medicare’s diagnosis-based reimbursement (DRG) system, hospitals could get paid the same amount whether the patient stays one day or five.
Medi-Cal, however, uses a straight-up per diem reimbursement system. “So reducing someone’s length of stay is not necessarily desirable if Medi-Cal would have paid you for all of those days,” Dr. Lundberg says. The state’s Medicare program also can deny coverage for days deemed medically unnecessary after a review of patient charts.
Hospitalists, he says, helped boost revenue in two ways. First, the program helped the hospital avoid denied coverage days by ensuring that patients stayed only as long as necessary. Average LOS, in fact, dropped to 1.92 days from 2.48 days, decreasing the Medi-Cal denial rate to 31.8% (from 43.8%) and bumping up the average reimbursement per inpatient day to $955 from $787.
Hospitalists also helped alleviate the work-hour limits for residents imposed by the Accreditation Council for Graduate Medical Education (ACGME), which had effectively capped the number of inpatients the center could admit. Because Olive View-UCLA receives per diem payments from Medi-Cal, making room to accept more patients into the hospital has meant increased revenues. Among the other benefits, the program has improved patient satisfaction and relieved some of the pressure on teaching teams.
With $310,000 for salary outlay in the hospitalist program’s first year, the study found a net cost benefit of $2 million. “One of the real challenges in getting this hospitalist thing going was getting our administrators to shell out the money for the salaries,” Dr. Lundberg says. The study demonstrated that a hospitalist program not only pays for itself, but also can substantially ramp up revenue. “I’m guessing that others, especially at public hospitals, face the same challenges,” he says. “I’m hoping they can point to this analysis and say, ‘Look, here’s what L.A. County did. They were able to show a net increase in revenue from this hospitalist service.’ ”
On the opposite side of the country, hospitalists are pointing to a success story in pediatric care. At the 120-bed Children’s Hospital at Montefiore at Albert Einstein College of Medicine in the Bronx, N.Y., a recent study concluded that establishing a pediatric HM program led to a significant reduction in LOS for patients with asthma or bronchiolitis.5 Nora Esteban-Cruciani, MD, MS, assistant director of pediatric hospital medicine and lead author of the report, which was presented at HM11, says it’s the first study to demonstrate such an effect for asthma in an inner-city academic setting.
Compared to a traditional resident-attending team, care administered by a resident-physician’s assistant-hospitalist team reduced LOS for bronchiolitis by 15.5% and asthma by 11.8%. With the 378 hospital-bed days saved annually, Children’s Hospital at Montefiore achieved an estimated savings of about $944,000 before taking salaries into account. “We anticipate seeing similar benefits in other groups of patients, and the total savings will far exceed the hospitalist salaries,” Dr. Esteban-Cruciani says.
After the pediatric HM program launched, her study also documented a 17% to 25% decrease in rehospitalizations among asthmatic children at four, six, and 12 months after their initial hospital discharge. As a result of the demonstrated value, Dr. Esteban-Cruciani says, the children’s hospital is expanding its HM program and hiring another 4.5 full-time equivalents.
So how did hospitalists achieve the positive results?
“Knowing the most up-to-date and evidence-based treatment plans, understanding how to use the hospital systems in the most efficient manner, being on the ward for eight to 12 hours per day to respond to issues that arise, as well as 24-hour availability by phone for the residents,” she says. “The day-to-day continuity, as well as the ability to consistently improve systems of care, are distinctive advantages to hospital medicine.”
The case for HM as a model of efficiency comes with a major caveat, however. David Meltzer, MD, PhD, FHM, chief of the section of hospital medicine and an economist and public-policy expert at the University of Chicago, points out that healthcare costs don’t end with a patient’s hospital discharge. Could savings achieved during inpatient care be offset by greater costs afterward?
A new study in the Annals of Internal Medicine by researchers at the University of Texas Medical Branch in Galveston has sharpened that question with the suggestion that, at least in some cases, hospitalist-procured savings might not last.6 When compared to care delivered by primary-care physicians (PCPs), the researchers found that hospitalist care yielded an average inpatient savings of $282 per Medicare beneficiary. But that reduction was wiped out by an extra $332 average cost in the month after discharge, due to higher readmissions, more emergency department visits, and more patients sent to nursing facilities instead of to their own homes. An accompanying editorial raises the uncomfortable question: “Are hospitalists discharging their patients more quickly but less appropriately, such that some of their patients bounce back?”7

—David Meltzer, MD, PhD, FHM, chief, section of hospital medicine, economist, University of Chicago
The study itself has its own share of caveats: Data were collected only until 2006, before reducing 30-day readmissions became a widespread focal point. The editorial also highlights the possibility that hospitalists might care for patients whose weaker relationships with outpatient providers could be the true driver of increased readmissions. In a statement, SHM President Joe Li, MD, SFHM, adds that constructive talks about healthcare costs must include the notion of quality, something the organization has worked to improve with interventions like Project BOOST.
At the very least, the new research highlights the importance of context when considering HM impacts on cost and quality. Separate studies, meanwhile, suggest that the jury is still out on whether other hospitalist-led models can consistently improve outcomes and costs. At academic centers, for instance, work-hour limits for medical residents have provided a strong impetus for joint-care arrangements, such as comanagement systems. A 2004 study found that an orthopedics-hospitalist comanagement structure led to a modest reduction in complications after elective hip and knee surgery. But the report documented no difference in costs or actual length of stay.8
More recently, a study of nearly 7,600 patients at UCSF Medical Center found that an HM-neurosurgery comanagement model had no significant impact on the center’s patient mortality, readmissions, LOS, or patient satisfaction. The comanagement system, however, yielded an average savings of $1,439 per hospitalization and boosted physicians’ perceptions of quality and safety.9
Andrew Auerbach, MD, MPH, SFHM, associate professor of medicine at UCSF Medical Center, says the savings, while not dramatic, nevertheless can add up when applied to the thousands of patients seen by the service every year. “That’s compelling because I think one of the things that you’re arguing when you’re doing these services is what the return on investment is going to be,” he says. “Traditionally, these have been implemented without any specific financial return on investment being applied, but the large expectation that clinical improvement is going to happen.”
His study at UCSF found just the opposite: no clinical improvement but a net cost benefit. “We were a little disappointed in some ways, but in other ways not surprised because there are very few data out in the community that suggest comanagement improves any outcomes,” Dr. Auerbach says. Among complicated neurosurgery patients, the strongest determinants of outcome might be beyond the scope of hospitalist-aided medical care.
With hospitals nervously eyeing their bottom lines, however, any financial improvement that does not adversely affect quality can still be seen as a positive development, and Dr. Auerbach says his study was the first to demonstrate that benefit. At UCSF Medical Center, at least, comanagement has proven compelling enough to spur plans for extending the service to orthopedic surgery patients.
Regardless of the care model, other studies suggest that specific interventions at key moments can yield substantial savings. A small, randomized controlled study led by hospitalists at Johns Hopkins University in Baltimore, for example, supports the idea that “simply showing providers the cost of some diagnostic tests at the time of order entry can affect behavior.”10 Although the study didn’t focus exclusively on hospitalists, experts say they’re in the best position to take the lead in curbing unnecessary costs.
“Hospitalists, I think, have a better understanding of the impact of resource utilization on the total cost of care and can be more prudent in the use of technologies,” says Kenneth Epstein, MD, MBA, FHM, FACP, chief medical officer for Traverse City, Mich.-based Hospitalist Consultants Inc. One reason is that hospitalists aren’t beholden to any specific technology, whether endoscopies or cardiac catheterization.

—Scott Lundberg, MD, assistant medical director, Olive View-UCLA Medical Center, Sylmar, Calif.
Mark Graban, author of the book “Lean Hospitals: Improving Quality, Patient Safety, and Employee Satisfaction,” says hospitalists can play another critical role in controlling costs by mapping out and simplifying the discharge processes. He recalls how hospitalists helped coordinate the effort by one of his hospital clients to prevent discharge delays that would have unnecessarily kept patients in the hospital for an additional night or two.
“That length-of-stay reduction, especially in a fixed-reimbursement setting, can have a huge financial impact,” Graban says. “And, inarguably, it’s the right thing to do for the patient, because it’s patients that are medically ready to be discharged. It gets them home and it reduces their increased risk of picking up infections or being involved in hospital errors.”
Focusing on patient safety could translate into big cost savings under the new Medicare system that penalizes providers for certain hospital-acquired conditions, such as skin ulcers and urinary tract infections, Dr. Epstein says. “There’s an emphasis by hospitalists in understanding the system and being willing to put energy into things like documenting ‘present on admission,’ which then has a huge impact on the hospital,” he says. Close monitoring of patients and developing standardization of care can likewise minimize the risk of conditions, such as catheter-associated infections, from cropping up in the hospital.
Dr. Meltzer says his own research suggests that experienced hospitalists are most effective at controlling costs. “So a program that is structured in such a way as to hire or retain experienced hospitalists is likely to have a higher cost savings than one that doesn’t,” he says.
In a broader sense, the maturation of the HM model and more widespread adoption of effective methods by practitioners might be boosting the overall impact of hospitalist care. A study that examined nearly 2 million Medicare admissions over six years found that the effects of the hospitalist care model on LOS became progressively more pronounced over time, from an average reduction of only 0.02 inpatient days in 2001-2002 to a decrease of 0.35 days by 2005-2006.11
Interestingly, the study’s authors suggest that effects attributable to hospitalists were most pronounced among older, complicated, nonsurgical patients cared for at nonprofit community hospitals.
The Verdict
Despite the variable design and scope of individual programs, experts say, HM’s overall net positive on the efficiency of inpatient care is fairly well documented. Future considerations of hospitalists’ true effects on costs, however, will demand an accounting of healthcare across an entire system, where the HM impact is decidedly less certain. “The right comparison in some sense is, What are the total costs of care for a patient cared for in a system that uses hospitalists versus the totals costs of similar patients cared for in a system that doesn’t use hospitalists?” Dr. Meltzer says.
David Mitchell, MD, PhD, a hospitalist at Sibley Memorial Hospital in Washington, D.C., and a member of SHM’s Performance Standards Committee, is among those with an additional concern: Providers may not be taking full advantage of their position to control costs.
“The reason is primarily that the reimbursement structure is not set up to incentivize us to cut costs,” he says. Dr. Mitchell, who has worked in 12 hospitals in six states, argues that hospitalists still are too detached from the true price of ordered tests. “That’s what I fear in hospital medicine, that we just become robots: chest pain means CT scan without thinking,” he says. “This just doesn’t make sense.” Dr. Mitchell also contends that the focus of some HM programs on seeing as many patients as possible to maximize reimbursements is leading to less efficiency. At HM11 in May, he met another hospitalist who said he regularly saw 40 to 45 patients every day. “I know there’s absolutely no way you can see that many patients and do an efficient job,” Dr. Mitchell says.
If one of the clearest areas of success for hospitalists has been in reducing length of stay within a hospital, experts acknowledge that it may no longer be enough. “In the new payment model, success is going to be defined differently, and it will be in terms of reducing the total cost of care,” Dr. Meltzer says.
Over the next decade, hospitalists will need to respond to new set of incentives. “And I think one of the really interesting questions will be how hospitalists can best do that, and the extent to which it causes them to rethink the ways in which they organize their practice,” he says.
Bryn Nelson is a freelance medical writer based in Seattle.
References
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287(4):487-494.
- Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007;357:2589-2600.
- Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3): 248-254.
- Lundberg S, Balingit P, Wali S, Cope D. Cost-effectiveness of a hospitalist service in a public teaching hospital. Acad Med. 2010;85(8):1312-1315.
- Esteban-Cruciani N, Montejo J, Azzarone G, Douglas L, et al. Impact of a pediatric hospital medicine program on resource utilization for children with respiratory disorders. J Hosp Med. 2011;6(4)Supp 2:S27.
- Kuo Y-F, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155(3): 152-159.
- Chen LM, Saint S. Moments in time. Ann Intern Med. 2011;155(3):194-195.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38.
- Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22): 2004-2010.
- Feldman L, Thiemann D, Brotman D. Financial impact of presenting lab cost data to providers at the time of order entry: a randomized controlled clinical trial. J Hosp Med. 2011;6(4)Supp 2:S93.
- Kuo Y-F, Goodwin JS. Effect of hospitalists on length of stay in the Medicare population: variation according to hospital and patient characteristics. J Am Geriatr Soc. 2010;58:1649-1657.
- Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-8.
- Chandra S, Howell E, Wright S. CICLE: Creating incentives and continuity leading to efficiency. J Hosp Med. 2011;6(4)Supp 2:S17
In 2002, a summary article in the Journal of the American Medical Association helped put the relatively small but rapidly growing HM profession on the map. Reviewing the available data, Robert Wachter, MD, MHM, and Lee Goldman, MD, MPH, of the University of California at San Francisco (UCSF) concluded that implementing a hospitalist program yielded an average savings of 13.4% in hospital costs and a 16.6% reduction in the length of stay (LOS).1
A decade later, the idea of efficiency has become so intertwined with hospitalists that SHM has included the concept in its definition of a profession that now comprises more than 30,000 doctors, nurses, and other care providers. HM practitioners work to enhance hospital and healthcare performance, in part, through “efficient use of hospital and healthcare resources,” according to SHM.
The growth of any profession can create exceptions and outliers, and observers point out that HM programs have become as varied as the hospitals in which they reside, complicating any attempt at broad generalizations. As a core part of the job description, though, efficiency and its implied benefit on costs have been widely promoted as arguments for expanding HM’s reach.
So are hospitalists meeting the lofty expectations?
A Look at the Evidence
A large retrospective study that examined outcomes of care for nearly 77,000 patients in 45 hospitals found that those cared for by hospitalists had a “modestly shorter” stay (by 0.4 days) in the hospital than those cared for by either general internists or family physicians.2 Hospitalists saved about $270 per hospitalization compared with general internists but only about $125 per stay compared with family physicians, the latter of which was not deemed statistically significant.
A more recent review of 33 studies found general agreement that hospitalist care led to reduced costs and length of stay but revealed less uniformity in the impacts on quality and patient outcomes.3
A more dramatic—albeit smaller—affirmation of HM as an efficient force has come from a study of patients admitted to 200-bed Olive View-UCLA Medical Center in Sylmar, Calif. The study, led by assistant medical director Scott Lundberg, MD, concluded that the arrival of an academic hospitalist program led to a one-year increase of $2.3 million in reimbursements from Medi-Cal, California’s Medicaid program.4
“Most other places that have demonstrated the cost-effectiveness of hospitalists generally point to reducing length of stay, which therefore reduces the costs,” Dr. Lundberg says. Under Medicare’s diagnosis-based reimbursement (DRG) system, hospitals could get paid the same amount whether the patient stays one day or five.
Medi-Cal, however, uses a straight-up per diem reimbursement system. “So reducing someone’s length of stay is not necessarily desirable if Medi-Cal would have paid you for all of those days,” Dr. Lundberg says. The state’s Medicare program also can deny coverage for days deemed medically unnecessary after a review of patient charts.
Hospitalists, he says, helped boost revenue in two ways. First, the program helped the hospital avoid denied coverage days by ensuring that patients stayed only as long as necessary. Average LOS, in fact, dropped to 1.92 days from 2.48 days, decreasing the Medi-Cal denial rate to 31.8% (from 43.8%) and bumping up the average reimbursement per inpatient day to $955 from $787.
Hospitalists also helped alleviate the work-hour limits for residents imposed by the Accreditation Council for Graduate Medical Education (ACGME), which had effectively capped the number of inpatients the center could admit. Because Olive View-UCLA receives per diem payments from Medi-Cal, making room to accept more patients into the hospital has meant increased revenues. Among the other benefits, the program has improved patient satisfaction and relieved some of the pressure on teaching teams.
With $310,000 for salary outlay in the hospitalist program’s first year, the study found a net cost benefit of $2 million. “One of the real challenges in getting this hospitalist thing going was getting our administrators to shell out the money for the salaries,” Dr. Lundberg says. The study demonstrated that a hospitalist program not only pays for itself, but also can substantially ramp up revenue. “I’m guessing that others, especially at public hospitals, face the same challenges,” he says. “I’m hoping they can point to this analysis and say, ‘Look, here’s what L.A. County did. They were able to show a net increase in revenue from this hospitalist service.’ ”
On the opposite side of the country, hospitalists are pointing to a success story in pediatric care. At the 120-bed Children’s Hospital at Montefiore at Albert Einstein College of Medicine in the Bronx, N.Y., a recent study concluded that establishing a pediatric HM program led to a significant reduction in LOS for patients with asthma or bronchiolitis.5 Nora Esteban-Cruciani, MD, MS, assistant director of pediatric hospital medicine and lead author of the report, which was presented at HM11, says it’s the first study to demonstrate such an effect for asthma in an inner-city academic setting.
Compared to a traditional resident-attending team, care administered by a resident-physician’s assistant-hospitalist team reduced LOS for bronchiolitis by 15.5% and asthma by 11.8%. With the 378 hospital-bed days saved annually, Children’s Hospital at Montefiore achieved an estimated savings of about $944,000 before taking salaries into account. “We anticipate seeing similar benefits in other groups of patients, and the total savings will far exceed the hospitalist salaries,” Dr. Esteban-Cruciani says.
After the pediatric HM program launched, her study also documented a 17% to 25% decrease in rehospitalizations among asthmatic children at four, six, and 12 months after their initial hospital discharge. As a result of the demonstrated value, Dr. Esteban-Cruciani says, the children’s hospital is expanding its HM program and hiring another 4.5 full-time equivalents.
So how did hospitalists achieve the positive results?
“Knowing the most up-to-date and evidence-based treatment plans, understanding how to use the hospital systems in the most efficient manner, being on the ward for eight to 12 hours per day to respond to issues that arise, as well as 24-hour availability by phone for the residents,” she says. “The day-to-day continuity, as well as the ability to consistently improve systems of care, are distinctive advantages to hospital medicine.”
The case for HM as a model of efficiency comes with a major caveat, however. David Meltzer, MD, PhD, FHM, chief of the section of hospital medicine and an economist and public-policy expert at the University of Chicago, points out that healthcare costs don’t end with a patient’s hospital discharge. Could savings achieved during inpatient care be offset by greater costs afterward?
A new study in the Annals of Internal Medicine by researchers at the University of Texas Medical Branch in Galveston has sharpened that question with the suggestion that, at least in some cases, hospitalist-procured savings might not last.6 When compared to care delivered by primary-care physicians (PCPs), the researchers found that hospitalist care yielded an average inpatient savings of $282 per Medicare beneficiary. But that reduction was wiped out by an extra $332 average cost in the month after discharge, due to higher readmissions, more emergency department visits, and more patients sent to nursing facilities instead of to their own homes. An accompanying editorial raises the uncomfortable question: “Are hospitalists discharging their patients more quickly but less appropriately, such that some of their patients bounce back?”7

—David Meltzer, MD, PhD, FHM, chief, section of hospital medicine, economist, University of Chicago
The study itself has its own share of caveats: Data were collected only until 2006, before reducing 30-day readmissions became a widespread focal point. The editorial also highlights the possibility that hospitalists might care for patients whose weaker relationships with outpatient providers could be the true driver of increased readmissions. In a statement, SHM President Joe Li, MD, SFHM, adds that constructive talks about healthcare costs must include the notion of quality, something the organization has worked to improve with interventions like Project BOOST.
At the very least, the new research highlights the importance of context when considering HM impacts on cost and quality. Separate studies, meanwhile, suggest that the jury is still out on whether other hospitalist-led models can consistently improve outcomes and costs. At academic centers, for instance, work-hour limits for medical residents have provided a strong impetus for joint-care arrangements, such as comanagement systems. A 2004 study found that an orthopedics-hospitalist comanagement structure led to a modest reduction in complications after elective hip and knee surgery. But the report documented no difference in costs or actual length of stay.8
More recently, a study of nearly 7,600 patients at UCSF Medical Center found that an HM-neurosurgery comanagement model had no significant impact on the center’s patient mortality, readmissions, LOS, or patient satisfaction. The comanagement system, however, yielded an average savings of $1,439 per hospitalization and boosted physicians’ perceptions of quality and safety.9
Andrew Auerbach, MD, MPH, SFHM, associate professor of medicine at UCSF Medical Center, says the savings, while not dramatic, nevertheless can add up when applied to the thousands of patients seen by the service every year. “That’s compelling because I think one of the things that you’re arguing when you’re doing these services is what the return on investment is going to be,” he says. “Traditionally, these have been implemented without any specific financial return on investment being applied, but the large expectation that clinical improvement is going to happen.”
His study at UCSF found just the opposite: no clinical improvement but a net cost benefit. “We were a little disappointed in some ways, but in other ways not surprised because there are very few data out in the community that suggest comanagement improves any outcomes,” Dr. Auerbach says. Among complicated neurosurgery patients, the strongest determinants of outcome might be beyond the scope of hospitalist-aided medical care.
With hospitals nervously eyeing their bottom lines, however, any financial improvement that does not adversely affect quality can still be seen as a positive development, and Dr. Auerbach says his study was the first to demonstrate that benefit. At UCSF Medical Center, at least, comanagement has proven compelling enough to spur plans for extending the service to orthopedic surgery patients.
Regardless of the care model, other studies suggest that specific interventions at key moments can yield substantial savings. A small, randomized controlled study led by hospitalists at Johns Hopkins University in Baltimore, for example, supports the idea that “simply showing providers the cost of some diagnostic tests at the time of order entry can affect behavior.”10 Although the study didn’t focus exclusively on hospitalists, experts say they’re in the best position to take the lead in curbing unnecessary costs.
“Hospitalists, I think, have a better understanding of the impact of resource utilization on the total cost of care and can be more prudent in the use of technologies,” says Kenneth Epstein, MD, MBA, FHM, FACP, chief medical officer for Traverse City, Mich.-based Hospitalist Consultants Inc. One reason is that hospitalists aren’t beholden to any specific technology, whether endoscopies or cardiac catheterization.

—Scott Lundberg, MD, assistant medical director, Olive View-UCLA Medical Center, Sylmar, Calif.
Mark Graban, author of the book “Lean Hospitals: Improving Quality, Patient Safety, and Employee Satisfaction,” says hospitalists can play another critical role in controlling costs by mapping out and simplifying the discharge processes. He recalls how hospitalists helped coordinate the effort by one of his hospital clients to prevent discharge delays that would have unnecessarily kept patients in the hospital for an additional night or two.
“That length-of-stay reduction, especially in a fixed-reimbursement setting, can have a huge financial impact,” Graban says. “And, inarguably, it’s the right thing to do for the patient, because it’s patients that are medically ready to be discharged. It gets them home and it reduces their increased risk of picking up infections or being involved in hospital errors.”
Focusing on patient safety could translate into big cost savings under the new Medicare system that penalizes providers for certain hospital-acquired conditions, such as skin ulcers and urinary tract infections, Dr. Epstein says. “There’s an emphasis by hospitalists in understanding the system and being willing to put energy into things like documenting ‘present on admission,’ which then has a huge impact on the hospital,” he says. Close monitoring of patients and developing standardization of care can likewise minimize the risk of conditions, such as catheter-associated infections, from cropping up in the hospital.
Dr. Meltzer says his own research suggests that experienced hospitalists are most effective at controlling costs. “So a program that is structured in such a way as to hire or retain experienced hospitalists is likely to have a higher cost savings than one that doesn’t,” he says.
In a broader sense, the maturation of the HM model and more widespread adoption of effective methods by practitioners might be boosting the overall impact of hospitalist care. A study that examined nearly 2 million Medicare admissions over six years found that the effects of the hospitalist care model on LOS became progressively more pronounced over time, from an average reduction of only 0.02 inpatient days in 2001-2002 to a decrease of 0.35 days by 2005-2006.11
Interestingly, the study’s authors suggest that effects attributable to hospitalists were most pronounced among older, complicated, nonsurgical patients cared for at nonprofit community hospitals.
The Verdict
Despite the variable design and scope of individual programs, experts say, HM’s overall net positive on the efficiency of inpatient care is fairly well documented. Future considerations of hospitalists’ true effects on costs, however, will demand an accounting of healthcare across an entire system, where the HM impact is decidedly less certain. “The right comparison in some sense is, What are the total costs of care for a patient cared for in a system that uses hospitalists versus the totals costs of similar patients cared for in a system that doesn’t use hospitalists?” Dr. Meltzer says.
David Mitchell, MD, PhD, a hospitalist at Sibley Memorial Hospital in Washington, D.C., and a member of SHM’s Performance Standards Committee, is among those with an additional concern: Providers may not be taking full advantage of their position to control costs.
“The reason is primarily that the reimbursement structure is not set up to incentivize us to cut costs,” he says. Dr. Mitchell, who has worked in 12 hospitals in six states, argues that hospitalists still are too detached from the true price of ordered tests. “That’s what I fear in hospital medicine, that we just become robots: chest pain means CT scan without thinking,” he says. “This just doesn’t make sense.” Dr. Mitchell also contends that the focus of some HM programs on seeing as many patients as possible to maximize reimbursements is leading to less efficiency. At HM11 in May, he met another hospitalist who said he regularly saw 40 to 45 patients every day. “I know there’s absolutely no way you can see that many patients and do an efficient job,” Dr. Mitchell says.
If one of the clearest areas of success for hospitalists has been in reducing length of stay within a hospital, experts acknowledge that it may no longer be enough. “In the new payment model, success is going to be defined differently, and it will be in terms of reducing the total cost of care,” Dr. Meltzer says.
Over the next decade, hospitalists will need to respond to new set of incentives. “And I think one of the really interesting questions will be how hospitalists can best do that, and the extent to which it causes them to rethink the ways in which they organize their practice,” he says.
Bryn Nelson is a freelance medical writer based in Seattle.
References
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287(4):487-494.
- Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007;357:2589-2600.
- Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3): 248-254.
- Lundberg S, Balingit P, Wali S, Cope D. Cost-effectiveness of a hospitalist service in a public teaching hospital. Acad Med. 2010;85(8):1312-1315.
- Esteban-Cruciani N, Montejo J, Azzarone G, Douglas L, et al. Impact of a pediatric hospital medicine program on resource utilization for children with respiratory disorders. J Hosp Med. 2011;6(4)Supp 2:S27.
- Kuo Y-F, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155(3): 152-159.
- Chen LM, Saint S. Moments in time. Ann Intern Med. 2011;155(3):194-195.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38.
- Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22): 2004-2010.
- Feldman L, Thiemann D, Brotman D. Financial impact of presenting lab cost data to providers at the time of order entry: a randomized controlled clinical trial. J Hosp Med. 2011;6(4)Supp 2:S93.
- Kuo Y-F, Goodwin JS. Effect of hospitalists on length of stay in the Medicare population: variation according to hospital and patient characteristics. J Am Geriatr Soc. 2010;58:1649-1657.
- Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-8.
- Chandra S, Howell E, Wright S. CICLE: Creating incentives and continuity leading to efficiency. J Hosp Med. 2011;6(4)Supp 2:S17
In 2002, a summary article in the Journal of the American Medical Association helped put the relatively small but rapidly growing HM profession on the map. Reviewing the available data, Robert Wachter, MD, MHM, and Lee Goldman, MD, MPH, of the University of California at San Francisco (UCSF) concluded that implementing a hospitalist program yielded an average savings of 13.4% in hospital costs and a 16.6% reduction in the length of stay (LOS).1
A decade later, the idea of efficiency has become so intertwined with hospitalists that SHM has included the concept in its definition of a profession that now comprises more than 30,000 doctors, nurses, and other care providers. HM practitioners work to enhance hospital and healthcare performance, in part, through “efficient use of hospital and healthcare resources,” according to SHM.
The growth of any profession can create exceptions and outliers, and observers point out that HM programs have become as varied as the hospitals in which they reside, complicating any attempt at broad generalizations. As a core part of the job description, though, efficiency and its implied benefit on costs have been widely promoted as arguments for expanding HM’s reach.
So are hospitalists meeting the lofty expectations?
A Look at the Evidence
A large retrospective study that examined outcomes of care for nearly 77,000 patients in 45 hospitals found that those cared for by hospitalists had a “modestly shorter” stay (by 0.4 days) in the hospital than those cared for by either general internists or family physicians.2 Hospitalists saved about $270 per hospitalization compared with general internists but only about $125 per stay compared with family physicians, the latter of which was not deemed statistically significant.
A more recent review of 33 studies found general agreement that hospitalist care led to reduced costs and length of stay but revealed less uniformity in the impacts on quality and patient outcomes.3
A more dramatic—albeit smaller—affirmation of HM as an efficient force has come from a study of patients admitted to 200-bed Olive View-UCLA Medical Center in Sylmar, Calif. The study, led by assistant medical director Scott Lundberg, MD, concluded that the arrival of an academic hospitalist program led to a one-year increase of $2.3 million in reimbursements from Medi-Cal, California’s Medicaid program.4
“Most other places that have demonstrated the cost-effectiveness of hospitalists generally point to reducing length of stay, which therefore reduces the costs,” Dr. Lundberg says. Under Medicare’s diagnosis-based reimbursement (DRG) system, hospitals could get paid the same amount whether the patient stays one day or five.
Medi-Cal, however, uses a straight-up per diem reimbursement system. “So reducing someone’s length of stay is not necessarily desirable if Medi-Cal would have paid you for all of those days,” Dr. Lundberg says. The state’s Medicare program also can deny coverage for days deemed medically unnecessary after a review of patient charts.
Hospitalists, he says, helped boost revenue in two ways. First, the program helped the hospital avoid denied coverage days by ensuring that patients stayed only as long as necessary. Average LOS, in fact, dropped to 1.92 days from 2.48 days, decreasing the Medi-Cal denial rate to 31.8% (from 43.8%) and bumping up the average reimbursement per inpatient day to $955 from $787.
Hospitalists also helped alleviate the work-hour limits for residents imposed by the Accreditation Council for Graduate Medical Education (ACGME), which had effectively capped the number of inpatients the center could admit. Because Olive View-UCLA receives per diem payments from Medi-Cal, making room to accept more patients into the hospital has meant increased revenues. Among the other benefits, the program has improved patient satisfaction and relieved some of the pressure on teaching teams.
With $310,000 for salary outlay in the hospitalist program’s first year, the study found a net cost benefit of $2 million. “One of the real challenges in getting this hospitalist thing going was getting our administrators to shell out the money for the salaries,” Dr. Lundberg says. The study demonstrated that a hospitalist program not only pays for itself, but also can substantially ramp up revenue. “I’m guessing that others, especially at public hospitals, face the same challenges,” he says. “I’m hoping they can point to this analysis and say, ‘Look, here’s what L.A. County did. They were able to show a net increase in revenue from this hospitalist service.’ ”
On the opposite side of the country, hospitalists are pointing to a success story in pediatric care. At the 120-bed Children’s Hospital at Montefiore at Albert Einstein College of Medicine in the Bronx, N.Y., a recent study concluded that establishing a pediatric HM program led to a significant reduction in LOS for patients with asthma or bronchiolitis.5 Nora Esteban-Cruciani, MD, MS, assistant director of pediatric hospital medicine and lead author of the report, which was presented at HM11, says it’s the first study to demonstrate such an effect for asthma in an inner-city academic setting.
Compared to a traditional resident-attending team, care administered by a resident-physician’s assistant-hospitalist team reduced LOS for bronchiolitis by 15.5% and asthma by 11.8%. With the 378 hospital-bed days saved annually, Children’s Hospital at Montefiore achieved an estimated savings of about $944,000 before taking salaries into account. “We anticipate seeing similar benefits in other groups of patients, and the total savings will far exceed the hospitalist salaries,” Dr. Esteban-Cruciani says.
After the pediatric HM program launched, her study also documented a 17% to 25% decrease in rehospitalizations among asthmatic children at four, six, and 12 months after their initial hospital discharge. As a result of the demonstrated value, Dr. Esteban-Cruciani says, the children’s hospital is expanding its HM program and hiring another 4.5 full-time equivalents.
So how did hospitalists achieve the positive results?
“Knowing the most up-to-date and evidence-based treatment plans, understanding how to use the hospital systems in the most efficient manner, being on the ward for eight to 12 hours per day to respond to issues that arise, as well as 24-hour availability by phone for the residents,” she says. “The day-to-day continuity, as well as the ability to consistently improve systems of care, are distinctive advantages to hospital medicine.”
The case for HM as a model of efficiency comes with a major caveat, however. David Meltzer, MD, PhD, FHM, chief of the section of hospital medicine and an economist and public-policy expert at the University of Chicago, points out that healthcare costs don’t end with a patient’s hospital discharge. Could savings achieved during inpatient care be offset by greater costs afterward?
A new study in the Annals of Internal Medicine by researchers at the University of Texas Medical Branch in Galveston has sharpened that question with the suggestion that, at least in some cases, hospitalist-procured savings might not last.6 When compared to care delivered by primary-care physicians (PCPs), the researchers found that hospitalist care yielded an average inpatient savings of $282 per Medicare beneficiary. But that reduction was wiped out by an extra $332 average cost in the month after discharge, due to higher readmissions, more emergency department visits, and more patients sent to nursing facilities instead of to their own homes. An accompanying editorial raises the uncomfortable question: “Are hospitalists discharging their patients more quickly but less appropriately, such that some of their patients bounce back?”7

—David Meltzer, MD, PhD, FHM, chief, section of hospital medicine, economist, University of Chicago
The study itself has its own share of caveats: Data were collected only until 2006, before reducing 30-day readmissions became a widespread focal point. The editorial also highlights the possibility that hospitalists might care for patients whose weaker relationships with outpatient providers could be the true driver of increased readmissions. In a statement, SHM President Joe Li, MD, SFHM, adds that constructive talks about healthcare costs must include the notion of quality, something the organization has worked to improve with interventions like Project BOOST.
At the very least, the new research highlights the importance of context when considering HM impacts on cost and quality. Separate studies, meanwhile, suggest that the jury is still out on whether other hospitalist-led models can consistently improve outcomes and costs. At academic centers, for instance, work-hour limits for medical residents have provided a strong impetus for joint-care arrangements, such as comanagement systems. A 2004 study found that an orthopedics-hospitalist comanagement structure led to a modest reduction in complications after elective hip and knee surgery. But the report documented no difference in costs or actual length of stay.8
More recently, a study of nearly 7,600 patients at UCSF Medical Center found that an HM-neurosurgery comanagement model had no significant impact on the center’s patient mortality, readmissions, LOS, or patient satisfaction. The comanagement system, however, yielded an average savings of $1,439 per hospitalization and boosted physicians’ perceptions of quality and safety.9
Andrew Auerbach, MD, MPH, SFHM, associate professor of medicine at UCSF Medical Center, says the savings, while not dramatic, nevertheless can add up when applied to the thousands of patients seen by the service every year. “That’s compelling because I think one of the things that you’re arguing when you’re doing these services is what the return on investment is going to be,” he says. “Traditionally, these have been implemented without any specific financial return on investment being applied, but the large expectation that clinical improvement is going to happen.”
His study at UCSF found just the opposite: no clinical improvement but a net cost benefit. “We were a little disappointed in some ways, but in other ways not surprised because there are very few data out in the community that suggest comanagement improves any outcomes,” Dr. Auerbach says. Among complicated neurosurgery patients, the strongest determinants of outcome might be beyond the scope of hospitalist-aided medical care.
With hospitals nervously eyeing their bottom lines, however, any financial improvement that does not adversely affect quality can still be seen as a positive development, and Dr. Auerbach says his study was the first to demonstrate that benefit. At UCSF Medical Center, at least, comanagement has proven compelling enough to spur plans for extending the service to orthopedic surgery patients.
Regardless of the care model, other studies suggest that specific interventions at key moments can yield substantial savings. A small, randomized controlled study led by hospitalists at Johns Hopkins University in Baltimore, for example, supports the idea that “simply showing providers the cost of some diagnostic tests at the time of order entry can affect behavior.”10 Although the study didn’t focus exclusively on hospitalists, experts say they’re in the best position to take the lead in curbing unnecessary costs.
“Hospitalists, I think, have a better understanding of the impact of resource utilization on the total cost of care and can be more prudent in the use of technologies,” says Kenneth Epstein, MD, MBA, FHM, FACP, chief medical officer for Traverse City, Mich.-based Hospitalist Consultants Inc. One reason is that hospitalists aren’t beholden to any specific technology, whether endoscopies or cardiac catheterization.

—Scott Lundberg, MD, assistant medical director, Olive View-UCLA Medical Center, Sylmar, Calif.
Mark Graban, author of the book “Lean Hospitals: Improving Quality, Patient Safety, and Employee Satisfaction,” says hospitalists can play another critical role in controlling costs by mapping out and simplifying the discharge processes. He recalls how hospitalists helped coordinate the effort by one of his hospital clients to prevent discharge delays that would have unnecessarily kept patients in the hospital for an additional night or two.
“That length-of-stay reduction, especially in a fixed-reimbursement setting, can have a huge financial impact,” Graban says. “And, inarguably, it’s the right thing to do for the patient, because it’s patients that are medically ready to be discharged. It gets them home and it reduces their increased risk of picking up infections or being involved in hospital errors.”
Focusing on patient safety could translate into big cost savings under the new Medicare system that penalizes providers for certain hospital-acquired conditions, such as skin ulcers and urinary tract infections, Dr. Epstein says. “There’s an emphasis by hospitalists in understanding the system and being willing to put energy into things like documenting ‘present on admission,’ which then has a huge impact on the hospital,” he says. Close monitoring of patients and developing standardization of care can likewise minimize the risk of conditions, such as catheter-associated infections, from cropping up in the hospital.
Dr. Meltzer says his own research suggests that experienced hospitalists are most effective at controlling costs. “So a program that is structured in such a way as to hire or retain experienced hospitalists is likely to have a higher cost savings than one that doesn’t,” he says.
In a broader sense, the maturation of the HM model and more widespread adoption of effective methods by practitioners might be boosting the overall impact of hospitalist care. A study that examined nearly 2 million Medicare admissions over six years found that the effects of the hospitalist care model on LOS became progressively more pronounced over time, from an average reduction of only 0.02 inpatient days in 2001-2002 to a decrease of 0.35 days by 2005-2006.11
Interestingly, the study’s authors suggest that effects attributable to hospitalists were most pronounced among older, complicated, nonsurgical patients cared for at nonprofit community hospitals.
The Verdict
Despite the variable design and scope of individual programs, experts say, HM’s overall net positive on the efficiency of inpatient care is fairly well documented. Future considerations of hospitalists’ true effects on costs, however, will demand an accounting of healthcare across an entire system, where the HM impact is decidedly less certain. “The right comparison in some sense is, What are the total costs of care for a patient cared for in a system that uses hospitalists versus the totals costs of similar patients cared for in a system that doesn’t use hospitalists?” Dr. Meltzer says.
David Mitchell, MD, PhD, a hospitalist at Sibley Memorial Hospital in Washington, D.C., and a member of SHM’s Performance Standards Committee, is among those with an additional concern: Providers may not be taking full advantage of their position to control costs.
“The reason is primarily that the reimbursement structure is not set up to incentivize us to cut costs,” he says. Dr. Mitchell, who has worked in 12 hospitals in six states, argues that hospitalists still are too detached from the true price of ordered tests. “That’s what I fear in hospital medicine, that we just become robots: chest pain means CT scan without thinking,” he says. “This just doesn’t make sense.” Dr. Mitchell also contends that the focus of some HM programs on seeing as many patients as possible to maximize reimbursements is leading to less efficiency. At HM11 in May, he met another hospitalist who said he regularly saw 40 to 45 patients every day. “I know there’s absolutely no way you can see that many patients and do an efficient job,” Dr. Mitchell says.
If one of the clearest areas of success for hospitalists has been in reducing length of stay within a hospital, experts acknowledge that it may no longer be enough. “In the new payment model, success is going to be defined differently, and it will be in terms of reducing the total cost of care,” Dr. Meltzer says.
Over the next decade, hospitalists will need to respond to new set of incentives. “And I think one of the really interesting questions will be how hospitalists can best do that, and the extent to which it causes them to rethink the ways in which they organize their practice,” he says.
Bryn Nelson is a freelance medical writer based in Seattle.
References
- Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002;287(4):487-494.
- Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007;357:2589-2600.
- Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3): 248-254.
- Lundberg S, Balingit P, Wali S, Cope D. Cost-effectiveness of a hospitalist service in a public teaching hospital. Acad Med. 2010;85(8):1312-1315.
- Esteban-Cruciani N, Montejo J, Azzarone G, Douglas L, et al. Impact of a pediatric hospital medicine program on resource utilization for children with respiratory disorders. J Hosp Med. 2011;6(4)Supp 2:S27.
- Kuo Y-F, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155(3): 152-159.
- Chen LM, Saint S. Moments in time. Ann Intern Med. 2011;155(3):194-195.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141(1):28-38.
- Auerbach AD, Wachter RM, Cheng HQ, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170(22): 2004-2010.
- Feldman L, Thiemann D, Brotman D. Financial impact of presenting lab cost data to providers at the time of order entry: a randomized controlled clinical trial. J Hosp Med. 2011;6(4)Supp 2:S93.
- Kuo Y-F, Goodwin JS. Effect of hospitalists on length of stay in the Medicare population: variation according to hospital and patient characteristics. J Am Geriatr Soc. 2010;58:1649-1657.
- Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-8.
- Chandra S, Howell E, Wright S. CICLE: Creating incentives and continuity leading to efficiency. J Hosp Med. 2011;6(4)Supp 2:S17
Find Your Niche
“You must define yourself as a hospitalist.” I smiled uncomfortably at my colleagues across the table as I pondered how best to respond to this statement. This seemingly innocuous comment had me perplexed, despite the fact that I aced the “What I want to be when I grow up” question as a fifth-grader. What had changed in all these years?
It was my first job as a hospitalist. I was two months out of residency and had accepted a position at the large academic hospital where I’d spent the previous three years of my life. The comfort was alluring and the transition appeared mundane. However, I naively did not realize that the difference between residency and the launch of a professional career was far greater than a miraculous transformation of paychecks.
Don’t get me wrong—throughout residency, I knew that I had a wealth of untapped energy and ideas; I was just too exhausted from patient-care duties to put action and plans into place. But as I vaulted into my career, I realized I now had the opportunity to act on these ideas and transcend the physician-in-training stereotype.
And so here I was, sitting with colleagues, attempting to define what would occupy the nonclinical portion of my upcoming career.
You might be wondering, “Isn’t great patient care enough for me as a hospitalist?” Indeed, in residency, we are praised, ranked, and valued almost solely on clinical acuity. As a hospitalist, however, we have the unique opportunity of defining ourselves in ways beyond bedside skills. While we are all astute clinicians, an important secret was kept from you during residency: You can choose another hat to wear and—unlike during your training years—you will have the time to do so.
Not buying it? It’s true. Simply pause and reflect on the hospitalists or general internal-medicine physicians you once admired; odds are they weren’t just clinicians, but they were also clinician-educators, clinician-researchers, clinician-administrators, clinician-fill-in-the-blank. In essence, they found a niche, a path that defined their careers.
And now, it’s time you did the same. But how, you ask? Here are a few pointers to get you started:
No. 1: Take Your Time
Before you go off trying to find your claim to fame, keep in mind that the first few years out of residency are a time of transition. Simply put, taking on too much, too early, could capsize your vessel. Learning to become an attending comes with a myriad of diverse responsibilities and a slow march to confidence in your clinical skills. This is a full-time position and one that requires diligence, both to ensure that you gain a strong clinical footing and fully understand the dimensions and nuances of potential “niches.” Get secure in your new role before beginning the search for your new calling. Once you feel comfortable with the resident-to-attending transition, you might find yourself itching to take on that new role in the hospital.
No. 2: Identify Your Passion
My mentor in residency was Dr. M, an all-star attending who had the energy to inspire by building an effortless bridge over the intern-resident-attending communication gap. As I studied her actions during my intern year, I found myself asking, “Could I ever be that successful in my career?”
As we shared experiences, I realized Dr. M genuinely was happy and passionate about her job every day. Her ability to effectively communicate to residents, nurses, and patients was a simple segue to her niche. So what is her niche? Dr. M is a clinician-communicator. Whether it is blogging about a recent patient experience on the wards or appearing as a physician correspondent for an Atlanta news affiliate, Dr. M’s strength is effective communication. Despite being a great clinician, it was her drive outside the wards that helped me understand she had found, and was living, her passion.
During residency, every physician had that one thing that continued to drive us when the going got tough. For some, it was the eager medical student who deserved to learn about that critical aortic stenosis murmur, even if you were 28 hours into your shift. For others, it was quality-improvement (QI) projects that arose from experiencing firsthand the effects of haphazard care transitions. Still others became passionate about patient advocacy after watching patients struggle to understand complex diseases.
Why are these examples relevant? Because each example represents a pathway to your niche. The first person might find a niche as a clinician-educator, exploring opportunities with the medical school during their first year. The second might align themselves with like-minded colleagues in QI and begin projects that will solve frustrations or improve physician efficiency. The third might get involved with local health fairs or local news stations to promote health awareness. The common link between all of these examples is that a clinician’s niche is based on their passion.
No. 3: Stay in Your Own Orbit
We’ve all been go-getters. We’re used to stretching ourselves thin to show what efficient, all-around superdocs we are. And this drive to say yes to your boss, that clinical nurse specialist, and to your colleague who schedules medical student clinical exams will lead to fruitful clinical ventures. Ultimately, however, this approach will leave you exhausted and will leave your colleagues wondering what it is that you actually do with your nonclinical time.
The solution? Learn to invest yourself, and your time, wisely.
During the first week of my new career (when I was asked that fateful question to define myself), I received the best advice. Dr. S (yes, another mentor—it’s OK to have multiple mentors) drew a series of random dots on a sheet of paper. Each of these dots represented opportunities that would arise during my first year. Circling a dot in the middle of the page, Dr. S looked at me and said, “One of these dots represents your passion. The remaining dots are where others’ interests lie. Pick one of these and work in its orbit only. Sure, you may jump up to another dot for a project, but the more you stay within the orbit of your passion, the happier and more productive you’ll be.”
In your first few years on the job, do say yes to joining committees, taking on projects, and collaborating with colleagues. But as you do, ensure that each of these decisions is within your orbit. Saying yes is easy, but saying yes and making it count twice is a skill that you will develop as your career progresses.
Not sure what your orbit is? I encourage you to refer back to tip No. 2 and start seeking out opportunities that center around your passion, not someone else’s.
No. 4: Master the Network
Networking is an art in which our business-minded friends from college excel. Unfortunately, studying for exams and resting after a 30-hour MICU call is a solo venture that leaves little room to hone networking skills. But now, the onlooker must become the master … of networking.
Networking is an important skill to develop, and you start the very first day of your career. The relationships you forge with successful colleagues and superiors will provide you with opportunities beyond the clinical arena (see “Simple Strategies to Expand Your HM Network,” below).
Not sure where to start? A mentor can help. Look at the well-respected leaders in your department and institution, and take note of how each of these people always talk about their mentors and the role they played in crystallizing their career paths. Good mentors steer you toward other like-minded professionals. They help you navigate the complex relationships that are at the base of a successful networking strategy. A wise strategy is to find multiple mentors who serve different purposes in your career; this usually leads to untold opportunities.
Can’t find a suitable mentor at the workplace? Fear not. Consider networking at local, regional, and national society meetings (www.hospitalmedicine.org/events). When the opportunity arises, do more than just attend the clinical sessions during these meetings. Learn which committees are available through the various societies and contact their leaders to express interest in joining next year’s group. Your fellow committee members will be a natural place to practice your networking skills. High-quality relationships made during this time have the potential to grow, and they could lead to more opportunities as your career progresses.
No. 5: Take Calculated Risks
This might sound simple enough, but it is not easy. It is uncomfortable to make mistakes in front of a public audience (and believe me, we all make mistakes). But you will be successful, too, and you must learn how to promote yourself during these times.
Challenge yourself by attending SHM’s Academic Hospitalist Academy (www.academichospitalist.org), or by taking on that project discussed at the last committee meeting. Say yes to your mentor when they learn your passion is QI and appropriately volunteer you to lead a resident research project. Submit your most recent project to an abstract competition, such as SHM’s Research, Innovation, and Clinical Vignettes (RIV) competition. Before you go, research others in your field with similar interests and seek them out during the meeting to share your experiences. Be ready to explain your pitfalls as well, and use this as an opportunity to learn from experienced colleagues.
Whether it is speaking in front of a group of strangers at the academy, giving a presentation to your colleagues, or meeting HM leaders at the national meeting, opportunities abound and often pay off in the long run.
No. 6: Ready For Change
Wait, change? Back up to tip No. 2. I know you’re saying, “But I’m following my passion.” Remember that, fresh out of residency, your interests likely are somewhat different than those of your future self. Thus, as the saying goes, the only thing that is certain is change.
Through networking and putting yourself in new positions, you will discover a world that was never revealed to you in residency. Case in point: my friend and colleague Dr. H. As a chief resident, Dr. H was exposed to a year of educational opportunities before she embarked on a hospitalist career. Education seemed like a natural fit in her first year as a hospitalist. In fact, she never imagined that it would be her experience with the inner workings of her hospital’s electronic medical record (EMR) during her chief year that would catapult her career as the physician director for information services. Yes, she is now a hospitalist-administrator. The bottom line: Remain resilient and ready to take up that next interesting opportunity.
Residency provides you with the skills to be a confident and effective clinician. But as residency comes to a close, think about what really drives you. Where do you see yourself in five years? How about 10 years?
Plot your course to live your passion at work every day; as you start your new job, find, refine, and define your niche.
Dr. Payne is a hospitalist in the Department of Internal Medicine at Emory University Hospital in Atlanta, and a clinical instructor of medicine at Emory University School of Medicine.
“You must define yourself as a hospitalist.” I smiled uncomfortably at my colleagues across the table as I pondered how best to respond to this statement. This seemingly innocuous comment had me perplexed, despite the fact that I aced the “What I want to be when I grow up” question as a fifth-grader. What had changed in all these years?
It was my first job as a hospitalist. I was two months out of residency and had accepted a position at the large academic hospital where I’d spent the previous three years of my life. The comfort was alluring and the transition appeared mundane. However, I naively did not realize that the difference between residency and the launch of a professional career was far greater than a miraculous transformation of paychecks.
Don’t get me wrong—throughout residency, I knew that I had a wealth of untapped energy and ideas; I was just too exhausted from patient-care duties to put action and plans into place. But as I vaulted into my career, I realized I now had the opportunity to act on these ideas and transcend the physician-in-training stereotype.
And so here I was, sitting with colleagues, attempting to define what would occupy the nonclinical portion of my upcoming career.
You might be wondering, “Isn’t great patient care enough for me as a hospitalist?” Indeed, in residency, we are praised, ranked, and valued almost solely on clinical acuity. As a hospitalist, however, we have the unique opportunity of defining ourselves in ways beyond bedside skills. While we are all astute clinicians, an important secret was kept from you during residency: You can choose another hat to wear and—unlike during your training years—you will have the time to do so.
Not buying it? It’s true. Simply pause and reflect on the hospitalists or general internal-medicine physicians you once admired; odds are they weren’t just clinicians, but they were also clinician-educators, clinician-researchers, clinician-administrators, clinician-fill-in-the-blank. In essence, they found a niche, a path that defined their careers.
And now, it’s time you did the same. But how, you ask? Here are a few pointers to get you started:
No. 1: Take Your Time
Before you go off trying to find your claim to fame, keep in mind that the first few years out of residency are a time of transition. Simply put, taking on too much, too early, could capsize your vessel. Learning to become an attending comes with a myriad of diverse responsibilities and a slow march to confidence in your clinical skills. This is a full-time position and one that requires diligence, both to ensure that you gain a strong clinical footing and fully understand the dimensions and nuances of potential “niches.” Get secure in your new role before beginning the search for your new calling. Once you feel comfortable with the resident-to-attending transition, you might find yourself itching to take on that new role in the hospital.
No. 2: Identify Your Passion
My mentor in residency was Dr. M, an all-star attending who had the energy to inspire by building an effortless bridge over the intern-resident-attending communication gap. As I studied her actions during my intern year, I found myself asking, “Could I ever be that successful in my career?”
As we shared experiences, I realized Dr. M genuinely was happy and passionate about her job every day. Her ability to effectively communicate to residents, nurses, and patients was a simple segue to her niche. So what is her niche? Dr. M is a clinician-communicator. Whether it is blogging about a recent patient experience on the wards or appearing as a physician correspondent for an Atlanta news affiliate, Dr. M’s strength is effective communication. Despite being a great clinician, it was her drive outside the wards that helped me understand she had found, and was living, her passion.
During residency, every physician had that one thing that continued to drive us when the going got tough. For some, it was the eager medical student who deserved to learn about that critical aortic stenosis murmur, even if you were 28 hours into your shift. For others, it was quality-improvement (QI) projects that arose from experiencing firsthand the effects of haphazard care transitions. Still others became passionate about patient advocacy after watching patients struggle to understand complex diseases.
Why are these examples relevant? Because each example represents a pathway to your niche. The first person might find a niche as a clinician-educator, exploring opportunities with the medical school during their first year. The second might align themselves with like-minded colleagues in QI and begin projects that will solve frustrations or improve physician efficiency. The third might get involved with local health fairs or local news stations to promote health awareness. The common link between all of these examples is that a clinician’s niche is based on their passion.
No. 3: Stay in Your Own Orbit
We’ve all been go-getters. We’re used to stretching ourselves thin to show what efficient, all-around superdocs we are. And this drive to say yes to your boss, that clinical nurse specialist, and to your colleague who schedules medical student clinical exams will lead to fruitful clinical ventures. Ultimately, however, this approach will leave you exhausted and will leave your colleagues wondering what it is that you actually do with your nonclinical time.
The solution? Learn to invest yourself, and your time, wisely.
During the first week of my new career (when I was asked that fateful question to define myself), I received the best advice. Dr. S (yes, another mentor—it’s OK to have multiple mentors) drew a series of random dots on a sheet of paper. Each of these dots represented opportunities that would arise during my first year. Circling a dot in the middle of the page, Dr. S looked at me and said, “One of these dots represents your passion. The remaining dots are where others’ interests lie. Pick one of these and work in its orbit only. Sure, you may jump up to another dot for a project, but the more you stay within the orbit of your passion, the happier and more productive you’ll be.”
In your first few years on the job, do say yes to joining committees, taking on projects, and collaborating with colleagues. But as you do, ensure that each of these decisions is within your orbit. Saying yes is easy, but saying yes and making it count twice is a skill that you will develop as your career progresses.
Not sure what your orbit is? I encourage you to refer back to tip No. 2 and start seeking out opportunities that center around your passion, not someone else’s.
No. 4: Master the Network
Networking is an art in which our business-minded friends from college excel. Unfortunately, studying for exams and resting after a 30-hour MICU call is a solo venture that leaves little room to hone networking skills. But now, the onlooker must become the master … of networking.
Networking is an important skill to develop, and you start the very first day of your career. The relationships you forge with successful colleagues and superiors will provide you with opportunities beyond the clinical arena (see “Simple Strategies to Expand Your HM Network,” below).
Not sure where to start? A mentor can help. Look at the well-respected leaders in your department and institution, and take note of how each of these people always talk about their mentors and the role they played in crystallizing their career paths. Good mentors steer you toward other like-minded professionals. They help you navigate the complex relationships that are at the base of a successful networking strategy. A wise strategy is to find multiple mentors who serve different purposes in your career; this usually leads to untold opportunities.
Can’t find a suitable mentor at the workplace? Fear not. Consider networking at local, regional, and national society meetings (www.hospitalmedicine.org/events). When the opportunity arises, do more than just attend the clinical sessions during these meetings. Learn which committees are available through the various societies and contact their leaders to express interest in joining next year’s group. Your fellow committee members will be a natural place to practice your networking skills. High-quality relationships made during this time have the potential to grow, and they could lead to more opportunities as your career progresses.
No. 5: Take Calculated Risks
This might sound simple enough, but it is not easy. It is uncomfortable to make mistakes in front of a public audience (and believe me, we all make mistakes). But you will be successful, too, and you must learn how to promote yourself during these times.
Challenge yourself by attending SHM’s Academic Hospitalist Academy (www.academichospitalist.org), or by taking on that project discussed at the last committee meeting. Say yes to your mentor when they learn your passion is QI and appropriately volunteer you to lead a resident research project. Submit your most recent project to an abstract competition, such as SHM’s Research, Innovation, and Clinical Vignettes (RIV) competition. Before you go, research others in your field with similar interests and seek them out during the meeting to share your experiences. Be ready to explain your pitfalls as well, and use this as an opportunity to learn from experienced colleagues.
Whether it is speaking in front of a group of strangers at the academy, giving a presentation to your colleagues, or meeting HM leaders at the national meeting, opportunities abound and often pay off in the long run.
No. 6: Ready For Change
Wait, change? Back up to tip No. 2. I know you’re saying, “But I’m following my passion.” Remember that, fresh out of residency, your interests likely are somewhat different than those of your future self. Thus, as the saying goes, the only thing that is certain is change.
Through networking and putting yourself in new positions, you will discover a world that was never revealed to you in residency. Case in point: my friend and colleague Dr. H. As a chief resident, Dr. H was exposed to a year of educational opportunities before she embarked on a hospitalist career. Education seemed like a natural fit in her first year as a hospitalist. In fact, she never imagined that it would be her experience with the inner workings of her hospital’s electronic medical record (EMR) during her chief year that would catapult her career as the physician director for information services. Yes, she is now a hospitalist-administrator. The bottom line: Remain resilient and ready to take up that next interesting opportunity.
Residency provides you with the skills to be a confident and effective clinician. But as residency comes to a close, think about what really drives you. Where do you see yourself in five years? How about 10 years?
Plot your course to live your passion at work every day; as you start your new job, find, refine, and define your niche.
Dr. Payne is a hospitalist in the Department of Internal Medicine at Emory University Hospital in Atlanta, and a clinical instructor of medicine at Emory University School of Medicine.
“You must define yourself as a hospitalist.” I smiled uncomfortably at my colleagues across the table as I pondered how best to respond to this statement. This seemingly innocuous comment had me perplexed, despite the fact that I aced the “What I want to be when I grow up” question as a fifth-grader. What had changed in all these years?
It was my first job as a hospitalist. I was two months out of residency and had accepted a position at the large academic hospital where I’d spent the previous three years of my life. The comfort was alluring and the transition appeared mundane. However, I naively did not realize that the difference between residency and the launch of a professional career was far greater than a miraculous transformation of paychecks.
Don’t get me wrong—throughout residency, I knew that I had a wealth of untapped energy and ideas; I was just too exhausted from patient-care duties to put action and plans into place. But as I vaulted into my career, I realized I now had the opportunity to act on these ideas and transcend the physician-in-training stereotype.
And so here I was, sitting with colleagues, attempting to define what would occupy the nonclinical portion of my upcoming career.
You might be wondering, “Isn’t great patient care enough for me as a hospitalist?” Indeed, in residency, we are praised, ranked, and valued almost solely on clinical acuity. As a hospitalist, however, we have the unique opportunity of defining ourselves in ways beyond bedside skills. While we are all astute clinicians, an important secret was kept from you during residency: You can choose another hat to wear and—unlike during your training years—you will have the time to do so.
Not buying it? It’s true. Simply pause and reflect on the hospitalists or general internal-medicine physicians you once admired; odds are they weren’t just clinicians, but they were also clinician-educators, clinician-researchers, clinician-administrators, clinician-fill-in-the-blank. In essence, they found a niche, a path that defined their careers.
And now, it’s time you did the same. But how, you ask? Here are a few pointers to get you started:
No. 1: Take Your Time
Before you go off trying to find your claim to fame, keep in mind that the first few years out of residency are a time of transition. Simply put, taking on too much, too early, could capsize your vessel. Learning to become an attending comes with a myriad of diverse responsibilities and a slow march to confidence in your clinical skills. This is a full-time position and one that requires diligence, both to ensure that you gain a strong clinical footing and fully understand the dimensions and nuances of potential “niches.” Get secure in your new role before beginning the search for your new calling. Once you feel comfortable with the resident-to-attending transition, you might find yourself itching to take on that new role in the hospital.
No. 2: Identify Your Passion
My mentor in residency was Dr. M, an all-star attending who had the energy to inspire by building an effortless bridge over the intern-resident-attending communication gap. As I studied her actions during my intern year, I found myself asking, “Could I ever be that successful in my career?”
As we shared experiences, I realized Dr. M genuinely was happy and passionate about her job every day. Her ability to effectively communicate to residents, nurses, and patients was a simple segue to her niche. So what is her niche? Dr. M is a clinician-communicator. Whether it is blogging about a recent patient experience on the wards or appearing as a physician correspondent for an Atlanta news affiliate, Dr. M’s strength is effective communication. Despite being a great clinician, it was her drive outside the wards that helped me understand she had found, and was living, her passion.
During residency, every physician had that one thing that continued to drive us when the going got tough. For some, it was the eager medical student who deserved to learn about that critical aortic stenosis murmur, even if you were 28 hours into your shift. For others, it was quality-improvement (QI) projects that arose from experiencing firsthand the effects of haphazard care transitions. Still others became passionate about patient advocacy after watching patients struggle to understand complex diseases.
Why are these examples relevant? Because each example represents a pathway to your niche. The first person might find a niche as a clinician-educator, exploring opportunities with the medical school during their first year. The second might align themselves with like-minded colleagues in QI and begin projects that will solve frustrations or improve physician efficiency. The third might get involved with local health fairs or local news stations to promote health awareness. The common link between all of these examples is that a clinician’s niche is based on their passion.
No. 3: Stay in Your Own Orbit
We’ve all been go-getters. We’re used to stretching ourselves thin to show what efficient, all-around superdocs we are. And this drive to say yes to your boss, that clinical nurse specialist, and to your colleague who schedules medical student clinical exams will lead to fruitful clinical ventures. Ultimately, however, this approach will leave you exhausted and will leave your colleagues wondering what it is that you actually do with your nonclinical time.
The solution? Learn to invest yourself, and your time, wisely.
During the first week of my new career (when I was asked that fateful question to define myself), I received the best advice. Dr. S (yes, another mentor—it’s OK to have multiple mentors) drew a series of random dots on a sheet of paper. Each of these dots represented opportunities that would arise during my first year. Circling a dot in the middle of the page, Dr. S looked at me and said, “One of these dots represents your passion. The remaining dots are where others’ interests lie. Pick one of these and work in its orbit only. Sure, you may jump up to another dot for a project, but the more you stay within the orbit of your passion, the happier and more productive you’ll be.”
In your first few years on the job, do say yes to joining committees, taking on projects, and collaborating with colleagues. But as you do, ensure that each of these decisions is within your orbit. Saying yes is easy, but saying yes and making it count twice is a skill that you will develop as your career progresses.
Not sure what your orbit is? I encourage you to refer back to tip No. 2 and start seeking out opportunities that center around your passion, not someone else’s.
No. 4: Master the Network
Networking is an art in which our business-minded friends from college excel. Unfortunately, studying for exams and resting after a 30-hour MICU call is a solo venture that leaves little room to hone networking skills. But now, the onlooker must become the master … of networking.
Networking is an important skill to develop, and you start the very first day of your career. The relationships you forge with successful colleagues and superiors will provide you with opportunities beyond the clinical arena (see “Simple Strategies to Expand Your HM Network,” below).
Not sure where to start? A mentor can help. Look at the well-respected leaders in your department and institution, and take note of how each of these people always talk about their mentors and the role they played in crystallizing their career paths. Good mentors steer you toward other like-minded professionals. They help you navigate the complex relationships that are at the base of a successful networking strategy. A wise strategy is to find multiple mentors who serve different purposes in your career; this usually leads to untold opportunities.
Can’t find a suitable mentor at the workplace? Fear not. Consider networking at local, regional, and national society meetings (www.hospitalmedicine.org/events). When the opportunity arises, do more than just attend the clinical sessions during these meetings. Learn which committees are available through the various societies and contact their leaders to express interest in joining next year’s group. Your fellow committee members will be a natural place to practice your networking skills. High-quality relationships made during this time have the potential to grow, and they could lead to more opportunities as your career progresses.
No. 5: Take Calculated Risks
This might sound simple enough, but it is not easy. It is uncomfortable to make mistakes in front of a public audience (and believe me, we all make mistakes). But you will be successful, too, and you must learn how to promote yourself during these times.
Challenge yourself by attending SHM’s Academic Hospitalist Academy (www.academichospitalist.org), or by taking on that project discussed at the last committee meeting. Say yes to your mentor when they learn your passion is QI and appropriately volunteer you to lead a resident research project. Submit your most recent project to an abstract competition, such as SHM’s Research, Innovation, and Clinical Vignettes (RIV) competition. Before you go, research others in your field with similar interests and seek them out during the meeting to share your experiences. Be ready to explain your pitfalls as well, and use this as an opportunity to learn from experienced colleagues.
Whether it is speaking in front of a group of strangers at the academy, giving a presentation to your colleagues, or meeting HM leaders at the national meeting, opportunities abound and often pay off in the long run.
No. 6: Ready For Change
Wait, change? Back up to tip No. 2. I know you’re saying, “But I’m following my passion.” Remember that, fresh out of residency, your interests likely are somewhat different than those of your future self. Thus, as the saying goes, the only thing that is certain is change.
Through networking and putting yourself in new positions, you will discover a world that was never revealed to you in residency. Case in point: my friend and colleague Dr. H. As a chief resident, Dr. H was exposed to a year of educational opportunities before she embarked on a hospitalist career. Education seemed like a natural fit in her first year as a hospitalist. In fact, she never imagined that it would be her experience with the inner workings of her hospital’s electronic medical record (EMR) during her chief year that would catapult her career as the physician director for information services. Yes, she is now a hospitalist-administrator. The bottom line: Remain resilient and ready to take up that next interesting opportunity.
Residency provides you with the skills to be a confident and effective clinician. But as residency comes to a close, think about what really drives you. Where do you see yourself in five years? How about 10 years?
Plot your course to live your passion at work every day; as you start your new job, find, refine, and define your niche.
Dr. Payne is a hospitalist in the Department of Internal Medicine at Emory University Hospital in Atlanta, and a clinical instructor of medicine at Emory University School of Medicine.
Dr. Optimization
Like many physicians, Larry Holder, MD, FACP, FHM, entered the medical profession with the desire to make a difference. After completing a fellowship in hematology and oncology in 1988, he joined Cancer Care Specialists of Central Illinois, a community oncology practice based in Decatur, and anticipated a lengthy career in which he would contribute to significant breakthroughs in cancer treatment.
After 12 years, however, he changed direction.
“I had become a bit disillusioned and realized we weren’t making big impacts, especially on the more common cancers,” he says. “I also got very attached to my patients, and in oncology, that’s not always a good thing. It became very trying emotionally.”
Dr. Holder spent the next five years practicing internal medicine at Community Health Improvement Center in Decatur. In 2005, he joined the hospitalist program at Decatur Memorial Hospital. Last year, he became medical director of hospitalist services, chief medical informatics officer (CMIO), and medical director of information systems.
Although he has found a new niche, his philosophy remains the same.
“Everything I do comes down to the fact I still love taking care of patients,” says Dr. Holder, one of six new members of Team Hospitalist. “That’s why I became a doctor. It’s very rewarding, and I never want to give that up.”

Question: You left oncology partly because you became attached to your patients. Does that approach help you as a hospitalist?
Answer: Definitely. I try to teach younger hospitalists the value of developing a rapport with patients. I enjoy building that emotional or intellectual attachment. I’m a big believer in the human aspect of what we do, and it’s one of the aspects of my job I love the most.
Q: Did you join Decatur Memorial with aspirations of leading its hospitalist program?
A: No. My plan was to focus on giving good patient care, get involved on the quality side, and become the CMIO for the hospital. When the medical director role opened up, it seemed to be sitting there waiting to be filled. I structured it so I could continue to see patients and split my administrative time between being the medical director of the hospitalists and being the CMIO.
Q: Why is it so important for you to still see patients?
A: As a physician, I still find it extremely rewarding. As medical director, I need to be in the trenches to know what the hospitalists are going through and what problems they are having. As CMIO, it’s very important that I use the system I’m in charge of trying to optimize.
Q: What advice would you give to a physician who is about to become leader of a program?
A: You need to anticipate growth. I was caught off guard by how fast our program continued to grow, and how quickly we reached the point where we needed more hospitalists. In retrospect, I should have immediately started looking to recruit. I also was not prepared for the financial aspect. If you don’t have a financial background, I would very quickly get training in that area.
Q: What is your biggest challenge as medical director?
A: Getting others in the hospital to accept change, even when all indications are it’s for the better.
Q: Have you identified a strategy that helps make that process easier?
A: The first step is to establish a sense of urgency. Then I try to get people who will be involved in the process or people who don’t oppose change to help set up a vision for the project and communicate that vision. Once you get empowerment to do the project, go for a short, early win that shows the concept is viable and can make it.
Q: How did you develop your interest in information systems?
A: I’ve always been interested in computers and how we can use computerization and informatic systems to improve patient care. When I became a hospitalist, I got much more involved. Decatur Memorial implemented computer physician order entry (CPOE). I became the physician champion for that, and my interest grew from there. I’m fortunate our administration is very good at pushing to improve our information systems.
Q: Does that interest fit with your approach toward medicine?
A: Absolutely. I’m a big believer in evidenced-based medicine. I think computer systems complement that very well.
Q: You were a finalist for McKesson’s Distinguished Achieve-ment Award and received an award this year from the Association of Medical Directors of Information Systems. What were those honors for?
A: We did a complete cultural change with nurses and physicians in terms of how they deal with diabetes. As part of that project, I developed a CPOE order set that automatically calculated the basal, nutritional, and correctional insulin dosage for the physician based on the patient’s weight and height. It made the right thing to do the easy thing to do. The concept involved the use of evidence-based medicine, project improvement with the Six Sigma process, and the high-level use of informatics.
Q: Has that improved patient care?
A: I was able to demonstrate a statistically significant improvement in glucose control without a change in hypoglycemia, so I did demonstrate an improved clinical outcome.
Q: What’s next for you professionally?
A: I have no intention of changing jobs, but I will continue to be very involved in quality projects. The biggest long-term project is developing more patient- and family-centered care at our hospital. I went to a national conference in February, and a big component was patient-centered care. I was very intrigued by it and brought the vision back to our hospital.
Q: Where does the effort stand?
A: I thought our hospitalist group would be a good group to do an initial component of the project. It went over really well, and people started asking me to present it to others. It took on a life of its own, and I wound up on a bit of a lecture series. It has since become an official Six Sigma project. We got the charter for it and it’s going in the hospital’s strategic plan, which I’m very pleased about.
Q: You earned FHM designation earlier this year. What does that mean to you?
A: It means a great deal. It’s tremendous recognition for the work I’ve done, the quality improvement projects I’ve been involved with, and the leadership roles I’ve taken on. At the same time, when you are able to show a national society views your work as important, I think it gives me even more credibility with the administration and the support staff.
Mark Leiser is a freelance writer based in New Jersey.
Like many physicians, Larry Holder, MD, FACP, FHM, entered the medical profession with the desire to make a difference. After completing a fellowship in hematology and oncology in 1988, he joined Cancer Care Specialists of Central Illinois, a community oncology practice based in Decatur, and anticipated a lengthy career in which he would contribute to significant breakthroughs in cancer treatment.
After 12 years, however, he changed direction.
“I had become a bit disillusioned and realized we weren’t making big impacts, especially on the more common cancers,” he says. “I also got very attached to my patients, and in oncology, that’s not always a good thing. It became very trying emotionally.”
Dr. Holder spent the next five years practicing internal medicine at Community Health Improvement Center in Decatur. In 2005, he joined the hospitalist program at Decatur Memorial Hospital. Last year, he became medical director of hospitalist services, chief medical informatics officer (CMIO), and medical director of information systems.
Although he has found a new niche, his philosophy remains the same.
“Everything I do comes down to the fact I still love taking care of patients,” says Dr. Holder, one of six new members of Team Hospitalist. “That’s why I became a doctor. It’s very rewarding, and I never want to give that up.”

Question: You left oncology partly because you became attached to your patients. Does that approach help you as a hospitalist?
Answer: Definitely. I try to teach younger hospitalists the value of developing a rapport with patients. I enjoy building that emotional or intellectual attachment. I’m a big believer in the human aspect of what we do, and it’s one of the aspects of my job I love the most.
Q: Did you join Decatur Memorial with aspirations of leading its hospitalist program?
A: No. My plan was to focus on giving good patient care, get involved on the quality side, and become the CMIO for the hospital. When the medical director role opened up, it seemed to be sitting there waiting to be filled. I structured it so I could continue to see patients and split my administrative time between being the medical director of the hospitalists and being the CMIO.
Q: Why is it so important for you to still see patients?
A: As a physician, I still find it extremely rewarding. As medical director, I need to be in the trenches to know what the hospitalists are going through and what problems they are having. As CMIO, it’s very important that I use the system I’m in charge of trying to optimize.
Q: What advice would you give to a physician who is about to become leader of a program?
A: You need to anticipate growth. I was caught off guard by how fast our program continued to grow, and how quickly we reached the point where we needed more hospitalists. In retrospect, I should have immediately started looking to recruit. I also was not prepared for the financial aspect. If you don’t have a financial background, I would very quickly get training in that area.
Q: What is your biggest challenge as medical director?
A: Getting others in the hospital to accept change, even when all indications are it’s for the better.
Q: Have you identified a strategy that helps make that process easier?
A: The first step is to establish a sense of urgency. Then I try to get people who will be involved in the process or people who don’t oppose change to help set up a vision for the project and communicate that vision. Once you get empowerment to do the project, go for a short, early win that shows the concept is viable and can make it.
Q: How did you develop your interest in information systems?
A: I’ve always been interested in computers and how we can use computerization and informatic systems to improve patient care. When I became a hospitalist, I got much more involved. Decatur Memorial implemented computer physician order entry (CPOE). I became the physician champion for that, and my interest grew from there. I’m fortunate our administration is very good at pushing to improve our information systems.
Q: Does that interest fit with your approach toward medicine?
A: Absolutely. I’m a big believer in evidenced-based medicine. I think computer systems complement that very well.
Q: You were a finalist for McKesson’s Distinguished Achieve-ment Award and received an award this year from the Association of Medical Directors of Information Systems. What were those honors for?
A: We did a complete cultural change with nurses and physicians in terms of how they deal with diabetes. As part of that project, I developed a CPOE order set that automatically calculated the basal, nutritional, and correctional insulin dosage for the physician based on the patient’s weight and height. It made the right thing to do the easy thing to do. The concept involved the use of evidence-based medicine, project improvement with the Six Sigma process, and the high-level use of informatics.
Q: Has that improved patient care?
A: I was able to demonstrate a statistically significant improvement in glucose control without a change in hypoglycemia, so I did demonstrate an improved clinical outcome.
Q: What’s next for you professionally?
A: I have no intention of changing jobs, but I will continue to be very involved in quality projects. The biggest long-term project is developing more patient- and family-centered care at our hospital. I went to a national conference in February, and a big component was patient-centered care. I was very intrigued by it and brought the vision back to our hospital.
Q: Where does the effort stand?
A: I thought our hospitalist group would be a good group to do an initial component of the project. It went over really well, and people started asking me to present it to others. It took on a life of its own, and I wound up on a bit of a lecture series. It has since become an official Six Sigma project. We got the charter for it and it’s going in the hospital’s strategic plan, which I’m very pleased about.
Q: You earned FHM designation earlier this year. What does that mean to you?
A: It means a great deal. It’s tremendous recognition for the work I’ve done, the quality improvement projects I’ve been involved with, and the leadership roles I’ve taken on. At the same time, when you are able to show a national society views your work as important, I think it gives me even more credibility with the administration and the support staff.
Mark Leiser is a freelance writer based in New Jersey.
Like many physicians, Larry Holder, MD, FACP, FHM, entered the medical profession with the desire to make a difference. After completing a fellowship in hematology and oncology in 1988, he joined Cancer Care Specialists of Central Illinois, a community oncology practice based in Decatur, and anticipated a lengthy career in which he would contribute to significant breakthroughs in cancer treatment.
After 12 years, however, he changed direction.
“I had become a bit disillusioned and realized we weren’t making big impacts, especially on the more common cancers,” he says. “I also got very attached to my patients, and in oncology, that’s not always a good thing. It became very trying emotionally.”
Dr. Holder spent the next five years practicing internal medicine at Community Health Improvement Center in Decatur. In 2005, he joined the hospitalist program at Decatur Memorial Hospital. Last year, he became medical director of hospitalist services, chief medical informatics officer (CMIO), and medical director of information systems.
Although he has found a new niche, his philosophy remains the same.
“Everything I do comes down to the fact I still love taking care of patients,” says Dr. Holder, one of six new members of Team Hospitalist. “That’s why I became a doctor. It’s very rewarding, and I never want to give that up.”

Question: You left oncology partly because you became attached to your patients. Does that approach help you as a hospitalist?
Answer: Definitely. I try to teach younger hospitalists the value of developing a rapport with patients. I enjoy building that emotional or intellectual attachment. I’m a big believer in the human aspect of what we do, and it’s one of the aspects of my job I love the most.
Q: Did you join Decatur Memorial with aspirations of leading its hospitalist program?
A: No. My plan was to focus on giving good patient care, get involved on the quality side, and become the CMIO for the hospital. When the medical director role opened up, it seemed to be sitting there waiting to be filled. I structured it so I could continue to see patients and split my administrative time between being the medical director of the hospitalists and being the CMIO.
Q: Why is it so important for you to still see patients?
A: As a physician, I still find it extremely rewarding. As medical director, I need to be in the trenches to know what the hospitalists are going through and what problems they are having. As CMIO, it’s very important that I use the system I’m in charge of trying to optimize.
Q: What advice would you give to a physician who is about to become leader of a program?
A: You need to anticipate growth. I was caught off guard by how fast our program continued to grow, and how quickly we reached the point where we needed more hospitalists. In retrospect, I should have immediately started looking to recruit. I also was not prepared for the financial aspect. If you don’t have a financial background, I would very quickly get training in that area.
Q: What is your biggest challenge as medical director?
A: Getting others in the hospital to accept change, even when all indications are it’s for the better.
Q: Have you identified a strategy that helps make that process easier?
A: The first step is to establish a sense of urgency. Then I try to get people who will be involved in the process or people who don’t oppose change to help set up a vision for the project and communicate that vision. Once you get empowerment to do the project, go for a short, early win that shows the concept is viable and can make it.
Q: How did you develop your interest in information systems?
A: I’ve always been interested in computers and how we can use computerization and informatic systems to improve patient care. When I became a hospitalist, I got much more involved. Decatur Memorial implemented computer physician order entry (CPOE). I became the physician champion for that, and my interest grew from there. I’m fortunate our administration is very good at pushing to improve our information systems.
Q: Does that interest fit with your approach toward medicine?
A: Absolutely. I’m a big believer in evidenced-based medicine. I think computer systems complement that very well.
Q: You were a finalist for McKesson’s Distinguished Achieve-ment Award and received an award this year from the Association of Medical Directors of Information Systems. What were those honors for?
A: We did a complete cultural change with nurses and physicians in terms of how they deal with diabetes. As part of that project, I developed a CPOE order set that automatically calculated the basal, nutritional, and correctional insulin dosage for the physician based on the patient’s weight and height. It made the right thing to do the easy thing to do. The concept involved the use of evidence-based medicine, project improvement with the Six Sigma process, and the high-level use of informatics.
Q: Has that improved patient care?
A: I was able to demonstrate a statistically significant improvement in glucose control without a change in hypoglycemia, so I did demonstrate an improved clinical outcome.
Q: What’s next for you professionally?
A: I have no intention of changing jobs, but I will continue to be very involved in quality projects. The biggest long-term project is developing more patient- and family-centered care at our hospital. I went to a national conference in February, and a big component was patient-centered care. I was very intrigued by it and brought the vision back to our hospital.
Q: Where does the effort stand?
A: I thought our hospitalist group would be a good group to do an initial component of the project. It went over really well, and people started asking me to present it to others. It took on a life of its own, and I wound up on a bit of a lecture series. It has since become an official Six Sigma project. We got the charter for it and it’s going in the hospital’s strategic plan, which I’m very pleased about.
Q: You earned FHM designation earlier this year. What does that mean to you?
A: It means a great deal. It’s tremendous recognition for the work I’ve done, the quality improvement projects I’ve been involved with, and the leadership roles I’ve taken on. At the same time, when you are able to show a national society views your work as important, I think it gives me even more credibility with the administration and the support staff.
Mark Leiser is a freelance writer based in New Jersey.
A Critical First Step
For those of you who were kind enough to catch my column in last month’s issue of The Hospitalist (see “What Is Your Value,” p. 56), you spent a few minutes reading my thoughts on the value of hospitalists. I mentioned the fact that the U.S. is moving rapidly toward a value-based system of purchasing healthcare, and that all healthcare providers, including hospitalists, increasingly will be judged on the value of care they deliver to their patients and the healthcare system. (Remember, value=quality/cost.)
Hospitalists, like all other healthcare providers, can increase their “value” by improving the quality of care they provide and decreasing the cost of healthcare delivery. Seems simple enough, right? Take better care of patients and do so while minimizing unnecessary costs. (If you have figured out how to do this, I want to learn from you!)
As a doctor and as the leader of the hospitalist group at Beth Israel Deaconess Medical Center in Boston, I have given this topic considerable thought. How do I become a “high value” provider? How do I help my hospitalist colleagues become “high value” hospitalists? Another persistent thought that has crossed my mind is: “How do I know that I am not already a high-value hospitalist?”
Maybe all of my hospitalist colleagues at Beth Israel Deaconess Medical Center are high-value providers. Seems fair enough, right? Maybe each of us is providing “high quality” care and doing so while minimizing unnecessary costs.
I mean, who really wants to think of themselves as low-quality doctors spending a considerable amount of unnecessary resources?
Like many of you, it became evident to me that the first step to improving quality and/or decreasing cost is to define “quality” and “cost.”
The First Step
Although it might seem difficult for the individual hospitalist to know the cost of a patient’s hospitalization, such information is available, and your hospital administrator might be willing to share such information with you and your group. But when it comes to quality of care, I think most patients would expect that doctors should understand the definition of “high-quality care.”
So, what is the definition of “high-quality care?” Try asking this question of patients and doctors, and you are likely to get very different answers. Not surprised? Try asking this question just to doctors, and you are likely to get some different answers. (For fun, you could try this exercise with your hospitalist colleagues; I have.)
Honestly, none of us should be alarmed if a group of doctors cannot easily define “high-quality care.” Not being able to do so does not mean these are “bad” doctors. While it may not be easy to define high-quality care, I suspect most of us recognize it when we see it.
The process of defining the quality of care involves capturing the essence of what we see. For example, can we agree that prescribing aspirin for patients with acute coronary syndrome is optimal care? If so, it stands to reason that a patient with acute coronary syndrome who did not receive aspirin received suboptimal care.
This is how a group of hospitalists can go about creating a quality standard. If you are a hospitalist or HM group leader who is interested in improving the quality of care you and your colleagues are providing to your patients, defining a quality standard is the critical first step to process improvement. Do not limit yourself to clinical processes. Although clinical processes are important, so are communication and documentation processes.
For example, most of us, as hospitalists, believe that communication with outpatient providers is important to the provision of high-quality inpatient care. How often do your hospitalists communicate with patients’ primary-care providers? Is this a quality standard for your hospitalist group? What about the documentation of a patient’s code status at the time of admission or documentation of a patient’s functional status in the discharge summary?
If you believe these are important, your group should include these as quality standards. You should be measuring them and reporting the results to individual providers.
Start with Definition
At this point, some of us might be tempted to get ahead of ourselves and worry about what standards we can or cannot measure, but I urge you to complete this first step of defining “high-quality care” before worrying about anything else. (In other words, don’t start running before you can walk.)
Another suggestion: Please don’t try to do too much all at once. Nobody is going to argue that patients with acute coronary syndrome should not receive aspirin. Reaching consensus on other quality standards might not be as easy. But do not get bogged down trying to create too many quality standards all at once. Start with a few and get yourself and your colleagues accustomed to the process.
Remember, when it comes to doctors, we have centuries of history of not knowing exactly what we are doing. I hope it won’t take centuries to fix this problem, but I also know we are not going to fix this in a few days or weeks. Small victories along the way are important if we hope to succeed.
Once you and your hospitalist colleagues arrive at a mutually agreed upon quality standard, the next step is performance measurement. I honestly believe performance measurement is easy when we spend the time understanding and agreeing to the most appropriate quality standards for our hospitalist groups.
I am interested in learning about your efforts to define the quality standards for your hospitalist group. Feel free to email me at [email protected].
Dr. Li is president of SHM.
For those of you who were kind enough to catch my column in last month’s issue of The Hospitalist (see “What Is Your Value,” p. 56), you spent a few minutes reading my thoughts on the value of hospitalists. I mentioned the fact that the U.S. is moving rapidly toward a value-based system of purchasing healthcare, and that all healthcare providers, including hospitalists, increasingly will be judged on the value of care they deliver to their patients and the healthcare system. (Remember, value=quality/cost.)
Hospitalists, like all other healthcare providers, can increase their “value” by improving the quality of care they provide and decreasing the cost of healthcare delivery. Seems simple enough, right? Take better care of patients and do so while minimizing unnecessary costs. (If you have figured out how to do this, I want to learn from you!)
As a doctor and as the leader of the hospitalist group at Beth Israel Deaconess Medical Center in Boston, I have given this topic considerable thought. How do I become a “high value” provider? How do I help my hospitalist colleagues become “high value” hospitalists? Another persistent thought that has crossed my mind is: “How do I know that I am not already a high-value hospitalist?”
Maybe all of my hospitalist colleagues at Beth Israel Deaconess Medical Center are high-value providers. Seems fair enough, right? Maybe each of us is providing “high quality” care and doing so while minimizing unnecessary costs.
I mean, who really wants to think of themselves as low-quality doctors spending a considerable amount of unnecessary resources?
Like many of you, it became evident to me that the first step to improving quality and/or decreasing cost is to define “quality” and “cost.”
The First Step
Although it might seem difficult for the individual hospitalist to know the cost of a patient’s hospitalization, such information is available, and your hospital administrator might be willing to share such information with you and your group. But when it comes to quality of care, I think most patients would expect that doctors should understand the definition of “high-quality care.”
So, what is the definition of “high-quality care?” Try asking this question of patients and doctors, and you are likely to get very different answers. Not surprised? Try asking this question just to doctors, and you are likely to get some different answers. (For fun, you could try this exercise with your hospitalist colleagues; I have.)
Honestly, none of us should be alarmed if a group of doctors cannot easily define “high-quality care.” Not being able to do so does not mean these are “bad” doctors. While it may not be easy to define high-quality care, I suspect most of us recognize it when we see it.
The process of defining the quality of care involves capturing the essence of what we see. For example, can we agree that prescribing aspirin for patients with acute coronary syndrome is optimal care? If so, it stands to reason that a patient with acute coronary syndrome who did not receive aspirin received suboptimal care.
This is how a group of hospitalists can go about creating a quality standard. If you are a hospitalist or HM group leader who is interested in improving the quality of care you and your colleagues are providing to your patients, defining a quality standard is the critical first step to process improvement. Do not limit yourself to clinical processes. Although clinical processes are important, so are communication and documentation processes.
For example, most of us, as hospitalists, believe that communication with outpatient providers is important to the provision of high-quality inpatient care. How often do your hospitalists communicate with patients’ primary-care providers? Is this a quality standard for your hospitalist group? What about the documentation of a patient’s code status at the time of admission or documentation of a patient’s functional status in the discharge summary?
If you believe these are important, your group should include these as quality standards. You should be measuring them and reporting the results to individual providers.
Start with Definition
At this point, some of us might be tempted to get ahead of ourselves and worry about what standards we can or cannot measure, but I urge you to complete this first step of defining “high-quality care” before worrying about anything else. (In other words, don’t start running before you can walk.)
Another suggestion: Please don’t try to do too much all at once. Nobody is going to argue that patients with acute coronary syndrome should not receive aspirin. Reaching consensus on other quality standards might not be as easy. But do not get bogged down trying to create too many quality standards all at once. Start with a few and get yourself and your colleagues accustomed to the process.
Remember, when it comes to doctors, we have centuries of history of not knowing exactly what we are doing. I hope it won’t take centuries to fix this problem, but I also know we are not going to fix this in a few days or weeks. Small victories along the way are important if we hope to succeed.
Once you and your hospitalist colleagues arrive at a mutually agreed upon quality standard, the next step is performance measurement. I honestly believe performance measurement is easy when we spend the time understanding and agreeing to the most appropriate quality standards for our hospitalist groups.
I am interested in learning about your efforts to define the quality standards for your hospitalist group. Feel free to email me at [email protected].
Dr. Li is president of SHM.
For those of you who were kind enough to catch my column in last month’s issue of The Hospitalist (see “What Is Your Value,” p. 56), you spent a few minutes reading my thoughts on the value of hospitalists. I mentioned the fact that the U.S. is moving rapidly toward a value-based system of purchasing healthcare, and that all healthcare providers, including hospitalists, increasingly will be judged on the value of care they deliver to their patients and the healthcare system. (Remember, value=quality/cost.)
Hospitalists, like all other healthcare providers, can increase their “value” by improving the quality of care they provide and decreasing the cost of healthcare delivery. Seems simple enough, right? Take better care of patients and do so while minimizing unnecessary costs. (If you have figured out how to do this, I want to learn from you!)
As a doctor and as the leader of the hospitalist group at Beth Israel Deaconess Medical Center in Boston, I have given this topic considerable thought. How do I become a “high value” provider? How do I help my hospitalist colleagues become “high value” hospitalists? Another persistent thought that has crossed my mind is: “How do I know that I am not already a high-value hospitalist?”
Maybe all of my hospitalist colleagues at Beth Israel Deaconess Medical Center are high-value providers. Seems fair enough, right? Maybe each of us is providing “high quality” care and doing so while minimizing unnecessary costs.
I mean, who really wants to think of themselves as low-quality doctors spending a considerable amount of unnecessary resources?
Like many of you, it became evident to me that the first step to improving quality and/or decreasing cost is to define “quality” and “cost.”
The First Step
Although it might seem difficult for the individual hospitalist to know the cost of a patient’s hospitalization, such information is available, and your hospital administrator might be willing to share such information with you and your group. But when it comes to quality of care, I think most patients would expect that doctors should understand the definition of “high-quality care.”
So, what is the definition of “high-quality care?” Try asking this question of patients and doctors, and you are likely to get very different answers. Not surprised? Try asking this question just to doctors, and you are likely to get some different answers. (For fun, you could try this exercise with your hospitalist colleagues; I have.)
Honestly, none of us should be alarmed if a group of doctors cannot easily define “high-quality care.” Not being able to do so does not mean these are “bad” doctors. While it may not be easy to define high-quality care, I suspect most of us recognize it when we see it.
The process of defining the quality of care involves capturing the essence of what we see. For example, can we agree that prescribing aspirin for patients with acute coronary syndrome is optimal care? If so, it stands to reason that a patient with acute coronary syndrome who did not receive aspirin received suboptimal care.
This is how a group of hospitalists can go about creating a quality standard. If you are a hospitalist or HM group leader who is interested in improving the quality of care you and your colleagues are providing to your patients, defining a quality standard is the critical first step to process improvement. Do not limit yourself to clinical processes. Although clinical processes are important, so are communication and documentation processes.
For example, most of us, as hospitalists, believe that communication with outpatient providers is important to the provision of high-quality inpatient care. How often do your hospitalists communicate with patients’ primary-care providers? Is this a quality standard for your hospitalist group? What about the documentation of a patient’s code status at the time of admission or documentation of a patient’s functional status in the discharge summary?
If you believe these are important, your group should include these as quality standards. You should be measuring them and reporting the results to individual providers.
Start with Definition
At this point, some of us might be tempted to get ahead of ourselves and worry about what standards we can or cannot measure, but I urge you to complete this first step of defining “high-quality care” before worrying about anything else. (In other words, don’t start running before you can walk.)
Another suggestion: Please don’t try to do too much all at once. Nobody is going to argue that patients with acute coronary syndrome should not receive aspirin. Reaching consensus on other quality standards might not be as easy. But do not get bogged down trying to create too many quality standards all at once. Start with a few and get yourself and your colleagues accustomed to the process.
Remember, when it comes to doctors, we have centuries of history of not knowing exactly what we are doing. I hope it won’t take centuries to fix this problem, but I also know we are not going to fix this in a few days or weeks. Small victories along the way are important if we hope to succeed.
Once you and your hospitalist colleagues arrive at a mutually agreed upon quality standard, the next step is performance measurement. I honestly believe performance measurement is easy when we spend the time understanding and agreeing to the most appropriate quality standards for our hospitalist groups.
I am interested in learning about your efforts to define the quality standards for your hospitalist group. Feel free to email me at [email protected].
Dr. Li is president of SHM.
Discharge improvement
If you’re a hospitalist interested in reducing readmissions in your hospital, the time to act is now.
Project BOOST (Better Outcomes for Older Adults through Safe Transitions), SHM’s groundbreaking program designed to help hospitals reduce unplanned readmissions, is now accepting applications for two new cohorts: one national and another specific to California. The deadline for applications is August 1.
Now with 85 sites as part of the national community, Project BOOST will introduce new sites across the country in the fall. In addition to the national cohort, Project BOOST will also establish a new cohort in California, with discounted tuition through grants from three healthcare groups in the state.
“It’s a great time to apply,” says Stephanie Rennke, MD, assistant clinical professor of medicine at the University of California San Francisco Medical Center. “We are at the cusp of a lot of big changes in health reform. The time to address readmissions is now. Hospitals will have to address this, and BOOST is one way to do that.”

—Stephanie Rennke, MD, assistant clinical professor of medicine, University of California San Francisco Medical Center
Applications are submitted online (www.hospitalmedicine.org/boost) and evaluated based on whether improving discharge and care transitions is a high priority at the institution. Applications must be accompanied by a letter of support from an executive sponsor within the applicant’s hospital.
Once accepted into the program, BOOST participants pay a tuition fee of $28,000. Thanks to the support of the California HealthCare Foundation, the L.A. Care Health Plan, and the Hospital Association of Southern California, sites in California are eligible for reduced tuition based on site location and availability of funds.
For Dr. Rennke, the link between healthcare reform and readmissions is clear, along with the repercussions for hospitals. Most notably, the discharge process affects multiple quality issues, including “patient satisfaction, provider satisfaction and improving communication from hospital to home.”
“Hospitals need to realize healthcare reform is coming,” says Dr. Rennke, who previously served as a Project BOOST site team member and now works as a BOOST mentor. “Not only is reducing readmissions the right thing to do, it will also have a financial impact for hospitals that don’t address it. … It’s going to be of paramount importance to address the discharge process.”
National Growth
Since it was initially developed through a grant from the John A. Hartford Foundation, Project BOOST has spread to hospitals across the country and received widespread attention throughout the healthcare community.
At the time of Project BOOST’s inception in 2008, readmissions already were an intractable and costly issue for hospitals. The next year, research coauthored by Project BOOST principal investigator Mark V. Williams, MD, FHM, and published in the New England Journal of Medicine revealed that unplanned readmissions cost Medicare $17.4 billion annually.
Project BOOST’s pilot cohort consisted of six hospital sites. The program’s growth accelerated quickly, and it soon added another 24 sites and, later, two statewide programs in Michigan and Illinois.
The popularity of Project BOOST among hospitals has captured the attention of media and other organizations as well:
- This year, Kaiser Health News featured the work of Atlanta’s Piedmont Hospital to reduce readmissions using Project BOOST in an article focusing on the impact of healthcare reform laws on hospital readmissions.
- The Bassett Healthcare Network, a Project BOOST site in upstate New York, has earned the Hospital Association of New York State’s prestigious 2011 HANYS Pinnacle Award for Quality and Safety for the group’s care-transition work. The award was presented to Bassett Healthcare Network chief executives in June.
- In California, the Kaiser Permanente West LA BOOST Team was recognized with an award from Dr. Benjamin Chu, president of Southern California Kaiser Foundation Health Plan.
- In December 2010, Dr. Williams and hospitalist Matthew Schreiber, CMO of Piedmont Hospital, shared their experiences with Project BOOST at a national conference hosted by the Centers for Medicare & Medicaid Services (CMS).
The Project BOOST Process
Once a site is accepted as a Project BOOST site, the site leader receives an information package and access to the Project BOOST online repository for recording and uploading readmission data. Then, each Project BOOST cohort performs an in-person conference. Networking and personal interaction are an important part of sharing challenges and successes in reducing readmissions. The conference also includes training on root-cause analysis and process mapping, a required step for application of the new Community Based Care Transitions Program (CCTP), part of the Affordable Care Act.
Each site leader is assigned a Project BOOST mentor, a national expert on reducing readmissions to the hospital. The mentor conducts a site visit to the hospital to meet the entire team in person and better understand the discharge challenges first-hand.
Over the course of the year, through regularly scheduled telephone calls, the mentor works with the Project BOOST team to best apply the program to the needs of the specific hospital. Mentors also help answer questions related to project planning, toolkit materials, data collection, implementation, and analysis.
In Dr. Rennke’s case, the process helped augment and guide UCSF’s current discharge program. Having multiple team members from different disciplines made distributing the work and implementation easier.
“Overall, we knew this was going to be doable because we incorporated Project BOOST into an already existing discharge process,” Dr. Rennke says.
Readmissions in the Crosshairs
The impacts of preventable readmissions on patient safety and efficiency of care in the hospital have made the issue a heated one in public policy. Earlier this year, the U.S. Department of Health and Human Services announced the creation of Partnership for Patients, a $1 billion initiative to address “quality, safety, and affordability of healthcare for all Americans.” SHM was one of the first medical societies to sign on to the “Partnership for Patients Pledge.”
One of the partnership’s two major goals is to reduce hospital readmissions by 20%. According to the Partnership for Patients website, “achieving this goal would mean more than 1.6 million patients would recover from illness without suffering a preventable complication requiring rehospitalization within 30 days of discharge.”
The government is backing up this goal with funding for hospitals with concrete plans to reduce readmissions. Under the Affordable Care Act of 2010—commonly known as the healthcare reform law—Medicare created the five-year CCTP earlier this year. The program provides $500 million to collaborative partnerships between hospitals and community-based organizations to implement care-transition services for Medicare beneficiaries, many of whom are at high risk of readmission.
To Dr. Rennke, the attention to reducing readmissions is an extension of her responsibility as a caregiver. “Our responsibility doesn’t end when the patient leaves the hospital,” she says. TH
Brendon Shank is SHM’s assistant vice president of communications.
If you’re a hospitalist interested in reducing readmissions in your hospital, the time to act is now.
Project BOOST (Better Outcomes for Older Adults through Safe Transitions), SHM’s groundbreaking program designed to help hospitals reduce unplanned readmissions, is now accepting applications for two new cohorts: one national and another specific to California. The deadline for applications is August 1.
Now with 85 sites as part of the national community, Project BOOST will introduce new sites across the country in the fall. In addition to the national cohort, Project BOOST will also establish a new cohort in California, with discounted tuition through grants from three healthcare groups in the state.
“It’s a great time to apply,” says Stephanie Rennke, MD, assistant clinical professor of medicine at the University of California San Francisco Medical Center. “We are at the cusp of a lot of big changes in health reform. The time to address readmissions is now. Hospitals will have to address this, and BOOST is one way to do that.”

—Stephanie Rennke, MD, assistant clinical professor of medicine, University of California San Francisco Medical Center
Applications are submitted online (www.hospitalmedicine.org/boost) and evaluated based on whether improving discharge and care transitions is a high priority at the institution. Applications must be accompanied by a letter of support from an executive sponsor within the applicant’s hospital.
Once accepted into the program, BOOST participants pay a tuition fee of $28,000. Thanks to the support of the California HealthCare Foundation, the L.A. Care Health Plan, and the Hospital Association of Southern California, sites in California are eligible for reduced tuition based on site location and availability of funds.
For Dr. Rennke, the link between healthcare reform and readmissions is clear, along with the repercussions for hospitals. Most notably, the discharge process affects multiple quality issues, including “patient satisfaction, provider satisfaction and improving communication from hospital to home.”
“Hospitals need to realize healthcare reform is coming,” says Dr. Rennke, who previously served as a Project BOOST site team member and now works as a BOOST mentor. “Not only is reducing readmissions the right thing to do, it will also have a financial impact for hospitals that don’t address it. … It’s going to be of paramount importance to address the discharge process.”
National Growth
Since it was initially developed through a grant from the John A. Hartford Foundation, Project BOOST has spread to hospitals across the country and received widespread attention throughout the healthcare community.
At the time of Project BOOST’s inception in 2008, readmissions already were an intractable and costly issue for hospitals. The next year, research coauthored by Project BOOST principal investigator Mark V. Williams, MD, FHM, and published in the New England Journal of Medicine revealed that unplanned readmissions cost Medicare $17.4 billion annually.
Project BOOST’s pilot cohort consisted of six hospital sites. The program’s growth accelerated quickly, and it soon added another 24 sites and, later, two statewide programs in Michigan and Illinois.
The popularity of Project BOOST among hospitals has captured the attention of media and other organizations as well:
- This year, Kaiser Health News featured the work of Atlanta’s Piedmont Hospital to reduce readmissions using Project BOOST in an article focusing on the impact of healthcare reform laws on hospital readmissions.
- The Bassett Healthcare Network, a Project BOOST site in upstate New York, has earned the Hospital Association of New York State’s prestigious 2011 HANYS Pinnacle Award for Quality and Safety for the group’s care-transition work. The award was presented to Bassett Healthcare Network chief executives in June.
- In California, the Kaiser Permanente West LA BOOST Team was recognized with an award from Dr. Benjamin Chu, president of Southern California Kaiser Foundation Health Plan.
- In December 2010, Dr. Williams and hospitalist Matthew Schreiber, CMO of Piedmont Hospital, shared their experiences with Project BOOST at a national conference hosted by the Centers for Medicare & Medicaid Services (CMS).
The Project BOOST Process
Once a site is accepted as a Project BOOST site, the site leader receives an information package and access to the Project BOOST online repository for recording and uploading readmission data. Then, each Project BOOST cohort performs an in-person conference. Networking and personal interaction are an important part of sharing challenges and successes in reducing readmissions. The conference also includes training on root-cause analysis and process mapping, a required step for application of the new Community Based Care Transitions Program (CCTP), part of the Affordable Care Act.
Each site leader is assigned a Project BOOST mentor, a national expert on reducing readmissions to the hospital. The mentor conducts a site visit to the hospital to meet the entire team in person and better understand the discharge challenges first-hand.
Over the course of the year, through regularly scheduled telephone calls, the mentor works with the Project BOOST team to best apply the program to the needs of the specific hospital. Mentors also help answer questions related to project planning, toolkit materials, data collection, implementation, and analysis.
In Dr. Rennke’s case, the process helped augment and guide UCSF’s current discharge program. Having multiple team members from different disciplines made distributing the work and implementation easier.
“Overall, we knew this was going to be doable because we incorporated Project BOOST into an already existing discharge process,” Dr. Rennke says.
Readmissions in the Crosshairs
The impacts of preventable readmissions on patient safety and efficiency of care in the hospital have made the issue a heated one in public policy. Earlier this year, the U.S. Department of Health and Human Services announced the creation of Partnership for Patients, a $1 billion initiative to address “quality, safety, and affordability of healthcare for all Americans.” SHM was one of the first medical societies to sign on to the “Partnership for Patients Pledge.”
One of the partnership’s two major goals is to reduce hospital readmissions by 20%. According to the Partnership for Patients website, “achieving this goal would mean more than 1.6 million patients would recover from illness without suffering a preventable complication requiring rehospitalization within 30 days of discharge.”
The government is backing up this goal with funding for hospitals with concrete plans to reduce readmissions. Under the Affordable Care Act of 2010—commonly known as the healthcare reform law—Medicare created the five-year CCTP earlier this year. The program provides $500 million to collaborative partnerships between hospitals and community-based organizations to implement care-transition services for Medicare beneficiaries, many of whom are at high risk of readmission.
To Dr. Rennke, the attention to reducing readmissions is an extension of her responsibility as a caregiver. “Our responsibility doesn’t end when the patient leaves the hospital,” she says. TH
Brendon Shank is SHM’s assistant vice president of communications.
If you’re a hospitalist interested in reducing readmissions in your hospital, the time to act is now.
Project BOOST (Better Outcomes for Older Adults through Safe Transitions), SHM’s groundbreaking program designed to help hospitals reduce unplanned readmissions, is now accepting applications for two new cohorts: one national and another specific to California. The deadline for applications is August 1.
Now with 85 sites as part of the national community, Project BOOST will introduce new sites across the country in the fall. In addition to the national cohort, Project BOOST will also establish a new cohort in California, with discounted tuition through grants from three healthcare groups in the state.
“It’s a great time to apply,” says Stephanie Rennke, MD, assistant clinical professor of medicine at the University of California San Francisco Medical Center. “We are at the cusp of a lot of big changes in health reform. The time to address readmissions is now. Hospitals will have to address this, and BOOST is one way to do that.”

—Stephanie Rennke, MD, assistant clinical professor of medicine, University of California San Francisco Medical Center
Applications are submitted online (www.hospitalmedicine.org/boost) and evaluated based on whether improving discharge and care transitions is a high priority at the institution. Applications must be accompanied by a letter of support from an executive sponsor within the applicant’s hospital.
Once accepted into the program, BOOST participants pay a tuition fee of $28,000. Thanks to the support of the California HealthCare Foundation, the L.A. Care Health Plan, and the Hospital Association of Southern California, sites in California are eligible for reduced tuition based on site location and availability of funds.
For Dr. Rennke, the link between healthcare reform and readmissions is clear, along with the repercussions for hospitals. Most notably, the discharge process affects multiple quality issues, including “patient satisfaction, provider satisfaction and improving communication from hospital to home.”
“Hospitals need to realize healthcare reform is coming,” says Dr. Rennke, who previously served as a Project BOOST site team member and now works as a BOOST mentor. “Not only is reducing readmissions the right thing to do, it will also have a financial impact for hospitals that don’t address it. … It’s going to be of paramount importance to address the discharge process.”
National Growth
Since it was initially developed through a grant from the John A. Hartford Foundation, Project BOOST has spread to hospitals across the country and received widespread attention throughout the healthcare community.
At the time of Project BOOST’s inception in 2008, readmissions already were an intractable and costly issue for hospitals. The next year, research coauthored by Project BOOST principal investigator Mark V. Williams, MD, FHM, and published in the New England Journal of Medicine revealed that unplanned readmissions cost Medicare $17.4 billion annually.
Project BOOST’s pilot cohort consisted of six hospital sites. The program’s growth accelerated quickly, and it soon added another 24 sites and, later, two statewide programs in Michigan and Illinois.
The popularity of Project BOOST among hospitals has captured the attention of media and other organizations as well:
- This year, Kaiser Health News featured the work of Atlanta’s Piedmont Hospital to reduce readmissions using Project BOOST in an article focusing on the impact of healthcare reform laws on hospital readmissions.
- The Bassett Healthcare Network, a Project BOOST site in upstate New York, has earned the Hospital Association of New York State’s prestigious 2011 HANYS Pinnacle Award for Quality and Safety for the group’s care-transition work. The award was presented to Bassett Healthcare Network chief executives in June.
- In California, the Kaiser Permanente West LA BOOST Team was recognized with an award from Dr. Benjamin Chu, president of Southern California Kaiser Foundation Health Plan.
- In December 2010, Dr. Williams and hospitalist Matthew Schreiber, CMO of Piedmont Hospital, shared their experiences with Project BOOST at a national conference hosted by the Centers for Medicare & Medicaid Services (CMS).
The Project BOOST Process
Once a site is accepted as a Project BOOST site, the site leader receives an information package and access to the Project BOOST online repository for recording and uploading readmission data. Then, each Project BOOST cohort performs an in-person conference. Networking and personal interaction are an important part of sharing challenges and successes in reducing readmissions. The conference also includes training on root-cause analysis and process mapping, a required step for application of the new Community Based Care Transitions Program (CCTP), part of the Affordable Care Act.
Each site leader is assigned a Project BOOST mentor, a national expert on reducing readmissions to the hospital. The mentor conducts a site visit to the hospital to meet the entire team in person and better understand the discharge challenges first-hand.
Over the course of the year, through regularly scheduled telephone calls, the mentor works with the Project BOOST team to best apply the program to the needs of the specific hospital. Mentors also help answer questions related to project planning, toolkit materials, data collection, implementation, and analysis.
In Dr. Rennke’s case, the process helped augment and guide UCSF’s current discharge program. Having multiple team members from different disciplines made distributing the work and implementation easier.
“Overall, we knew this was going to be doable because we incorporated Project BOOST into an already existing discharge process,” Dr. Rennke says.
Readmissions in the Crosshairs
The impacts of preventable readmissions on patient safety and efficiency of care in the hospital have made the issue a heated one in public policy. Earlier this year, the U.S. Department of Health and Human Services announced the creation of Partnership for Patients, a $1 billion initiative to address “quality, safety, and affordability of healthcare for all Americans.” SHM was one of the first medical societies to sign on to the “Partnership for Patients Pledge.”
One of the partnership’s two major goals is to reduce hospital readmissions by 20%. According to the Partnership for Patients website, “achieving this goal would mean more than 1.6 million patients would recover from illness without suffering a preventable complication requiring rehospitalization within 30 days of discharge.”
The government is backing up this goal with funding for hospitals with concrete plans to reduce readmissions. Under the Affordable Care Act of 2010—commonly known as the healthcare reform law—Medicare created the five-year CCTP earlier this year. The program provides $500 million to collaborative partnerships between hospitals and community-based organizations to implement care-transition services for Medicare beneficiaries, many of whom are at high risk of readmission.
To Dr. Rennke, the attention to reducing readmissions is an extension of her responsibility as a caregiver. “Our responsibility doesn’t end when the patient leaves the hospital,” she says. TH
Brendon Shank is SHM’s assistant vice president of communications.