User login
Interval cholecystectomy may be a risky business
HOLLYWOOD, FLA – Interval cholecystectomy remains a challenging procedure, with longer operative times and ICU stays, greater blood loss, more biliary and bowel injuries, and even hints of increased mortality, compared with immediate cholecystectomy, according to the findings from a retrospective study of 404 patients.
The staged procedure, completed after antibiotic therapy and percutaneous cholecystostomy, has been increasing in frequency over the past 10 years, but has not been rigorously studied, James Ackerman, MD, said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
“Looking at Medicare data over the past decade, we see a 50% increase in this procedure, which is marked by some striking regional variation,” from 5% of acute cholecystitis cases in the Northeast to less than 1% in some other regions. “This shows that as a group, we really don’t know what to do with this procedure.”
The revised Tokyo Guidelines for the management of acute cholangitis and cholecystitis aren’t hugely helpful either, noted Dr. Ackerman of the University of Pittsburgh Medical Center. While the guidelines are fairly straightforward for patients with grade 1 and grade 3 disease, “there’s a lot of gray area in grade 2.”
Treatment for these patients should include biliary drainage with antibiotics, but, he said, the recommendations for surgery, and whether it should be elective, immediate, or delayed, can be confusing for this group.
Dr. Ackerman’s retrospective analysis comprised 177 patients with acute cholecystitis who underwent an interval cholecystectomy (IC) after percutaneous cholecystostomy, and 227 controls who underwent an immediate cholecystectomy. The analysis spanned 2008-2013 and used data from seven hospitals in one health care system.
Patients who had the IC were older (70 vs. 55 years), had a worse American Society of Anesthesiologists class (3 vs. 2.5), and a worse Tokyo Grade (2 vs. 1).
Most of the IC procedures (119) were laparoscopic. There were 43 conversions to open and 15 were planned open surgeries. Among the immediate cholecystectomies, most (192) were laparoscopic. There were 28 conversions to open and six planned open surgeries.
The conversion rate was significantly higher among the IC group (28% vs.13%). The most common reasons for conversion were hostile abdomen (48% vs. 16%) and hostile right upper quadrant (34% vs. 58%).
Operating time was significantly longer in the IC group (121 vs. 90 minutes). Estimated blood loss was also significantly higher (30 vs. 15 cc). Total hospital stay was significantly longer (7 vs. 5 days), as was ICU stay (1 vs. 0.1 day).
There were no biliary tract injuries in the cholecystectomy group, while 5.7% of IC patients sustained such an injury. Bowel injuries, most often serosal, were also more common in the IC group (6% vs. 0.4%). The IC group had more surgical site infections as well (12% vs. 0.44%).
There was no significant difference in 30-day mortality, but at 1 year, IC patients were significantly more likely to have died (15% vs. 0.44%).
The ongoing CHOCOLATE trial (Acute cholecystitis in high risk surgical patients: percutaneous cholecystostomy versus laparoscopic cholecystectomy) may help clarify the issue further, Dr. Ackerman said. The study being conducted in the Netherlands is randomizing high-risk cholecystitis patients to either laparoscopic cholecystectomy or percutaneous drainage.
Dr. Ackerman had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
HOLLYWOOD, FLA – Interval cholecystectomy remains a challenging procedure, with longer operative times and ICU stays, greater blood loss, more biliary and bowel injuries, and even hints of increased mortality, compared with immediate cholecystectomy, according to the findings from a retrospective study of 404 patients.
The staged procedure, completed after antibiotic therapy and percutaneous cholecystostomy, has been increasing in frequency over the past 10 years, but has not been rigorously studied, James Ackerman, MD, said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
“Looking at Medicare data over the past decade, we see a 50% increase in this procedure, which is marked by some striking regional variation,” from 5% of acute cholecystitis cases in the Northeast to less than 1% in some other regions. “This shows that as a group, we really don’t know what to do with this procedure.”
The revised Tokyo Guidelines for the management of acute cholangitis and cholecystitis aren’t hugely helpful either, noted Dr. Ackerman of the University of Pittsburgh Medical Center. While the guidelines are fairly straightforward for patients with grade 1 and grade 3 disease, “there’s a lot of gray area in grade 2.”
Treatment for these patients should include biliary drainage with antibiotics, but, he said, the recommendations for surgery, and whether it should be elective, immediate, or delayed, can be confusing for this group.
Dr. Ackerman’s retrospective analysis comprised 177 patients with acute cholecystitis who underwent an interval cholecystectomy (IC) after percutaneous cholecystostomy, and 227 controls who underwent an immediate cholecystectomy. The analysis spanned 2008-2013 and used data from seven hospitals in one health care system.
Patients who had the IC were older (70 vs. 55 years), had a worse American Society of Anesthesiologists class (3 vs. 2.5), and a worse Tokyo Grade (2 vs. 1).
Most of the IC procedures (119) were laparoscopic. There were 43 conversions to open and 15 were planned open surgeries. Among the immediate cholecystectomies, most (192) were laparoscopic. There were 28 conversions to open and six planned open surgeries.
The conversion rate was significantly higher among the IC group (28% vs.13%). The most common reasons for conversion were hostile abdomen (48% vs. 16%) and hostile right upper quadrant (34% vs. 58%).
Operating time was significantly longer in the IC group (121 vs. 90 minutes). Estimated blood loss was also significantly higher (30 vs. 15 cc). Total hospital stay was significantly longer (7 vs. 5 days), as was ICU stay (1 vs. 0.1 day).
There were no biliary tract injuries in the cholecystectomy group, while 5.7% of IC patients sustained such an injury. Bowel injuries, most often serosal, were also more common in the IC group (6% vs. 0.4%). The IC group had more surgical site infections as well (12% vs. 0.44%).
There was no significant difference in 30-day mortality, but at 1 year, IC patients were significantly more likely to have died (15% vs. 0.44%).
The ongoing CHOCOLATE trial (Acute cholecystitis in high risk surgical patients: percutaneous cholecystostomy versus laparoscopic cholecystectomy) may help clarify the issue further, Dr. Ackerman said. The study being conducted in the Netherlands is randomizing high-risk cholecystitis patients to either laparoscopic cholecystectomy or percutaneous drainage.
Dr. Ackerman had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
HOLLYWOOD, FLA – Interval cholecystectomy remains a challenging procedure, with longer operative times and ICU stays, greater blood loss, more biliary and bowel injuries, and even hints of increased mortality, compared with immediate cholecystectomy, according to the findings from a retrospective study of 404 patients.
The staged procedure, completed after antibiotic therapy and percutaneous cholecystostomy, has been increasing in frequency over the past 10 years, but has not been rigorously studied, James Ackerman, MD, said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
“Looking at Medicare data over the past decade, we see a 50% increase in this procedure, which is marked by some striking regional variation,” from 5% of acute cholecystitis cases in the Northeast to less than 1% in some other regions. “This shows that as a group, we really don’t know what to do with this procedure.”
The revised Tokyo Guidelines for the management of acute cholangitis and cholecystitis aren’t hugely helpful either, noted Dr. Ackerman of the University of Pittsburgh Medical Center. While the guidelines are fairly straightforward for patients with grade 1 and grade 3 disease, “there’s a lot of gray area in grade 2.”
Treatment for these patients should include biliary drainage with antibiotics, but, he said, the recommendations for surgery, and whether it should be elective, immediate, or delayed, can be confusing for this group.
Dr. Ackerman’s retrospective analysis comprised 177 patients with acute cholecystitis who underwent an interval cholecystectomy (IC) after percutaneous cholecystostomy, and 227 controls who underwent an immediate cholecystectomy. The analysis spanned 2008-2013 and used data from seven hospitals in one health care system.
Patients who had the IC were older (70 vs. 55 years), had a worse American Society of Anesthesiologists class (3 vs. 2.5), and a worse Tokyo Grade (2 vs. 1).
Most of the IC procedures (119) were laparoscopic. There were 43 conversions to open and 15 were planned open surgeries. Among the immediate cholecystectomies, most (192) were laparoscopic. There were 28 conversions to open and six planned open surgeries.
The conversion rate was significantly higher among the IC group (28% vs.13%). The most common reasons for conversion were hostile abdomen (48% vs. 16%) and hostile right upper quadrant (34% vs. 58%).
Operating time was significantly longer in the IC group (121 vs. 90 minutes). Estimated blood loss was also significantly higher (30 vs. 15 cc). Total hospital stay was significantly longer (7 vs. 5 days), as was ICU stay (1 vs. 0.1 day).
There were no biliary tract injuries in the cholecystectomy group, while 5.7% of IC patients sustained such an injury. Bowel injuries, most often serosal, were also more common in the IC group (6% vs. 0.4%). The IC group had more surgical site infections as well (12% vs. 0.44%).
There was no significant difference in 30-day mortality, but at 1 year, IC patients were significantly more likely to have died (15% vs. 0.44%).
The ongoing CHOCOLATE trial (Acute cholecystitis in high risk surgical patients: percutaneous cholecystostomy versus laparoscopic cholecystectomy) may help clarify the issue further, Dr. Ackerman said. The study being conducted in the Netherlands is randomizing high-risk cholecystitis patients to either laparoscopic cholecystectomy or percutaneous drainage.
Dr. Ackerman had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
AT THE EAST ANNUAL SCIENTIFIC ASSEMBLY
Key clinical point:
Major finding: Interval cholecystectomy was associated with greater blood loss, more conversions to open surgery, bowel and biliary injuries, and even higher 1-year mortality (15% vs. 0.44%).
Data source: A retrospective review comparing 177 patients with interval surgery to 227 who had immediate surgery.
Disclosures: Dr. Ackerman had no financial disclosures.
Lysosomal acid lipase replacement corrects rare genetic cause of liver failure, atherosclerosis
BOSTON – Lysosomal acid lipase deficiency (LAL-D), a rare genetic cause of marked dyslipidemia that causes early multisystem organ damage, was effectively treated by a human recombinant enzyme to replace deficient lysosomal acid lipase, and the replacement enzyme was well tolerated over a 76-week trial.
LAL-D, when it begins in infancy, is usually fatal within the first year.
When LAL-D occurs later in life, it’s believed to be an “underappreciated cause of fibrosis, cirrhosis, severe dyslipidemia, and early-onset atherosclerosis,” according to Katryn Furuya, MD, and the coauthors of a poster presentation given at the annual meeting of the American Association for the Study of Liver Diseases.
Supplying the human recombinant lysosomal acid lipase, termed sebelipase alfa (SA), to children and adults with LAL-D over a 76-week period resulted in a reduction in alanine aminotransferase (ALT) for 98% of participants, normalization of ALT for 51% of participants, and normalization of aspartate aminotransferase (AST) levels for 65% of patients. Patients on SA also experienced reductions in serum triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), and liver fat and total liver volume. “We’re basically replacing what they’re missing,” senior author Barbara Burton, MD, said in an interview.
“The target tissues that we want to get to are the liver, primarily, but also the spleen and the endothelial cells,” said Dr. Burton, professor of gastroenterology at Northwestern University, Chicago. “So the enzyme gets in and then it clears the accumulated fat, and that leads to a reduction in inflammation in the liver, because you don’t have these enlarged lysosomes that are irritating to the cells.”
The effects were seen in LAL-D patients participating in an open-label extension of a double-blind placebo-controlled trial of SA. Patients in the placebo arm who began receiving SA “experienced marked and sustained improvements in liver and lipid parameters, mirroring those observed in the SA group during the double-blind period,” wrote Dr. Furuya and her coauthors. Dr. Furuya, currently a pediatric gastroenterologist at the Mayo Clinic in Rochester, Minn., was a fellow at the Alfred I. duPont Hospital for Children, Wilmington, Del., at the time of the study.
The ARISE (Acid Lipase Replacement Investigating Safety and Efficacy) study included patients aged 4 years and older with a confirmed LAL-D diagnosis. They had to have a baseline ALT at least 1.5 times the upper limit of normal, and if taking lipid-lowering medications, they had to have been on a stable dose for at least 6 weeks before starting the study, and remain on the stable dose for at least the first 32 weeks of the study.
Patients with a history of hematopoietic or liver transplantation were excluded, as were those with severe liver dysfunction, indicated by a Child-Pugh score falling into class C.
The study began with 66 patients entering a randomized, double-blind, placebo-controlled study in which patients received an every-other-week intravenous infusion of SA 1 mg/kg (n = 36), or placebo (n = 30). Median age of participants was 13 years (range, 4-58 years).
After 22 weeks, this was followed by an open-label extension period, during which patients in both arms were unblinded and received SA 1 mg/kg for the duration of the study period; 65/66 patients entered this phase. This means that patients who were initially given SA during the blinded phase of the trial received a total of 76 weeks of SA, while patients who first received placebo before entering the open-label extension did not have their data analyzed until they had been on SA for a total of 78 weeks. The extra 2 weeks accounted for a crossover period for the placebo arm to enter the open-label phase.
The protocol allowed dose increases up to 3 mg/kg if patients’ AST, ALT, LDL-C, or TG levels remained elevated, or if patients under the age of 18 continued to have low weight-for-age z scores. For patients who had problems tolerating SA, the dose could be reduced to 0.35 kg/mg.
Efficacy outcome measures included the proportion of patients who achieved AST and ALT normalization, and those whose ALT values were reduced (but not necessarily normalized). Other measures included changes in LDL-C, HDL-C, non-HDL-C, and TG; reductions in hepatic fat content and total liver volume were also tracked.
After 76 weeks, LDL-C levels were reduced by a mean 27.5%, from 199 to 142 mg/dL, and non-HDL-C dropped by a mean 26.6%, from 230 to 166 mg/dL.
Liver volume and fat content was assessed by multiecho gradient echo magnetic resonance imaging (MEGE-MRI) performed at baseline, at week 20, and at study week 52, representing 52 weeks of SA treatment for the intervention arm and 30 weeks for the placebo arm of the initial trial.
After 52 weeks of SA exposure, the mean hepatic fat reduction was 20.5%, with 88% of patients having reduced liver fat. Of those with 30 weeks of SA exposure, 88% also had reduced liver fat, with a mean fat reduction of 28%.
Liver volume also dropped, by a mean of 13.2% for those with 52 weeks of SA exposure, with 90% of patients experiencing reduced liver volume. Patients with 30 weeks of SA treatment saw a mean 11.2% reduction in liver volume; 96% of this patient group saw some decrease in liver volume.
Safety outcomes included tracking treatment-emergent adverse events (TEAEs), as well as monitoring participants for anti-drug antibodies and for the development of neutralizing antibodies to SA. The safety outcome measures were assessed for patients with longer SA exposure, ranging from 86 to 152 weeks.
There were no patient discontinuations because of TEAEs, and most events were mild or moderate; the only serious adverse event considered related to treatment was an infusion-associated reaction. This patient was able to restart SA therapy after desensitization.
Anti-drug antibodies showed up in 11% of patients (n = 7), and two of these patients had neutralizing antibodies. The safety profile was not different for the group of patients testing positive for anti-drug antibodies, wrote Dr. Furuya and her coauthors.
Replacing LAL-D has promise for a population whose disease may go long undetected. “The patients are not obvious. They are difficult to diagnose,” said Dr. Burton. “They look normal, and they feel normal in many cases, until they have life-threatening disease,” such as end-stage liver disease or cardiovascular complications, she said. Even if elevated transaminases are found in routine screening, physicians are much more likely to think of the more-common nonalcoholic fatty liver disease (NAFLD) than LAL-D, said Dr. Burton, noting that an MRI won’t clarify the diagnosis, though a liver biopsy will show microvesicular rather than macrovesicular fat distribution in LAL-D.
When the clinical picture doesn’t fit with NAFLD, though, LAL-D should be in the differential, she said, adding that she suspects the actual incidence of LAL-D may be higher than has been reported in the literature.
Dr. Burton reported receiving research support, consulting fees, and honoraria from Alexion Pharmaceuticals – the study sponsor and manufacturer of sebelipase alfa. Dr. Furuya reported no disclosures.
[email protected]
On Twitter @karioakes
BOSTON – Lysosomal acid lipase deficiency (LAL-D), a rare genetic cause of marked dyslipidemia that causes early multisystem organ damage, was effectively treated by a human recombinant enzyme to replace deficient lysosomal acid lipase, and the replacement enzyme was well tolerated over a 76-week trial.
LAL-D, when it begins in infancy, is usually fatal within the first year.
When LAL-D occurs later in life, it’s believed to be an “underappreciated cause of fibrosis, cirrhosis, severe dyslipidemia, and early-onset atherosclerosis,” according to Katryn Furuya, MD, and the coauthors of a poster presentation given at the annual meeting of the American Association for the Study of Liver Diseases.
Supplying the human recombinant lysosomal acid lipase, termed sebelipase alfa (SA), to children and adults with LAL-D over a 76-week period resulted in a reduction in alanine aminotransferase (ALT) for 98% of participants, normalization of ALT for 51% of participants, and normalization of aspartate aminotransferase (AST) levels for 65% of patients. Patients on SA also experienced reductions in serum triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), and liver fat and total liver volume. “We’re basically replacing what they’re missing,” senior author Barbara Burton, MD, said in an interview.
“The target tissues that we want to get to are the liver, primarily, but also the spleen and the endothelial cells,” said Dr. Burton, professor of gastroenterology at Northwestern University, Chicago. “So the enzyme gets in and then it clears the accumulated fat, and that leads to a reduction in inflammation in the liver, because you don’t have these enlarged lysosomes that are irritating to the cells.”
The effects were seen in LAL-D patients participating in an open-label extension of a double-blind placebo-controlled trial of SA. Patients in the placebo arm who began receiving SA “experienced marked and sustained improvements in liver and lipid parameters, mirroring those observed in the SA group during the double-blind period,” wrote Dr. Furuya and her coauthors. Dr. Furuya, currently a pediatric gastroenterologist at the Mayo Clinic in Rochester, Minn., was a fellow at the Alfred I. duPont Hospital for Children, Wilmington, Del., at the time of the study.
The ARISE (Acid Lipase Replacement Investigating Safety and Efficacy) study included patients aged 4 years and older with a confirmed LAL-D diagnosis. They had to have a baseline ALT at least 1.5 times the upper limit of normal, and if taking lipid-lowering medications, they had to have been on a stable dose for at least 6 weeks before starting the study, and remain on the stable dose for at least the first 32 weeks of the study.
Patients with a history of hematopoietic or liver transplantation were excluded, as were those with severe liver dysfunction, indicated by a Child-Pugh score falling into class C.
The study began with 66 patients entering a randomized, double-blind, placebo-controlled study in which patients received an every-other-week intravenous infusion of SA 1 mg/kg (n = 36), or placebo (n = 30). Median age of participants was 13 years (range, 4-58 years).
After 22 weeks, this was followed by an open-label extension period, during which patients in both arms were unblinded and received SA 1 mg/kg for the duration of the study period; 65/66 patients entered this phase. This means that patients who were initially given SA during the blinded phase of the trial received a total of 76 weeks of SA, while patients who first received placebo before entering the open-label extension did not have their data analyzed until they had been on SA for a total of 78 weeks. The extra 2 weeks accounted for a crossover period for the placebo arm to enter the open-label phase.
The protocol allowed dose increases up to 3 mg/kg if patients’ AST, ALT, LDL-C, or TG levels remained elevated, or if patients under the age of 18 continued to have low weight-for-age z scores. For patients who had problems tolerating SA, the dose could be reduced to 0.35 kg/mg.
Efficacy outcome measures included the proportion of patients who achieved AST and ALT normalization, and those whose ALT values were reduced (but not necessarily normalized). Other measures included changes in LDL-C, HDL-C, non-HDL-C, and TG; reductions in hepatic fat content and total liver volume were also tracked.
After 76 weeks, LDL-C levels were reduced by a mean 27.5%, from 199 to 142 mg/dL, and non-HDL-C dropped by a mean 26.6%, from 230 to 166 mg/dL.
Liver volume and fat content was assessed by multiecho gradient echo magnetic resonance imaging (MEGE-MRI) performed at baseline, at week 20, and at study week 52, representing 52 weeks of SA treatment for the intervention arm and 30 weeks for the placebo arm of the initial trial.
After 52 weeks of SA exposure, the mean hepatic fat reduction was 20.5%, with 88% of patients having reduced liver fat. Of those with 30 weeks of SA exposure, 88% also had reduced liver fat, with a mean fat reduction of 28%.
Liver volume also dropped, by a mean of 13.2% for those with 52 weeks of SA exposure, with 90% of patients experiencing reduced liver volume. Patients with 30 weeks of SA treatment saw a mean 11.2% reduction in liver volume; 96% of this patient group saw some decrease in liver volume.
Safety outcomes included tracking treatment-emergent adverse events (TEAEs), as well as monitoring participants for anti-drug antibodies and for the development of neutralizing antibodies to SA. The safety outcome measures were assessed for patients with longer SA exposure, ranging from 86 to 152 weeks.
There were no patient discontinuations because of TEAEs, and most events were mild or moderate; the only serious adverse event considered related to treatment was an infusion-associated reaction. This patient was able to restart SA therapy after desensitization.
Anti-drug antibodies showed up in 11% of patients (n = 7), and two of these patients had neutralizing antibodies. The safety profile was not different for the group of patients testing positive for anti-drug antibodies, wrote Dr. Furuya and her coauthors.
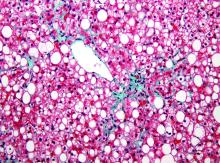
Replacing LAL-D has promise for a population whose disease may go long undetected. “The patients are not obvious. They are difficult to diagnose,” said Dr. Burton. “They look normal, and they feel normal in many cases, until they have life-threatening disease,” such as end-stage liver disease or cardiovascular complications, she said. Even if elevated transaminases are found in routine screening, physicians are much more likely to think of the more-common nonalcoholic fatty liver disease (NAFLD) than LAL-D, said Dr. Burton, noting that an MRI won’t clarify the diagnosis, though a liver biopsy will show microvesicular rather than macrovesicular fat distribution in LAL-D.
When the clinical picture doesn’t fit with NAFLD, though, LAL-D should be in the differential, she said, adding that she suspects the actual incidence of LAL-D may be higher than has been reported in the literature.
Dr. Burton reported receiving research support, consulting fees, and honoraria from Alexion Pharmaceuticals – the study sponsor and manufacturer of sebelipase alfa. Dr. Furuya reported no disclosures.
[email protected]
On Twitter @karioakes
BOSTON – Lysosomal acid lipase deficiency (LAL-D), a rare genetic cause of marked dyslipidemia that causes early multisystem organ damage, was effectively treated by a human recombinant enzyme to replace deficient lysosomal acid lipase, and the replacement enzyme was well tolerated over a 76-week trial.
LAL-D, when it begins in infancy, is usually fatal within the first year.
When LAL-D occurs later in life, it’s believed to be an “underappreciated cause of fibrosis, cirrhosis, severe dyslipidemia, and early-onset atherosclerosis,” according to Katryn Furuya, MD, and the coauthors of a poster presentation given at the annual meeting of the American Association for the Study of Liver Diseases.
Supplying the human recombinant lysosomal acid lipase, termed sebelipase alfa (SA), to children and adults with LAL-D over a 76-week period resulted in a reduction in alanine aminotransferase (ALT) for 98% of participants, normalization of ALT for 51% of participants, and normalization of aspartate aminotransferase (AST) levels for 65% of patients. Patients on SA also experienced reductions in serum triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), and liver fat and total liver volume. “We’re basically replacing what they’re missing,” senior author Barbara Burton, MD, said in an interview.
“The target tissues that we want to get to are the liver, primarily, but also the spleen and the endothelial cells,” said Dr. Burton, professor of gastroenterology at Northwestern University, Chicago. “So the enzyme gets in and then it clears the accumulated fat, and that leads to a reduction in inflammation in the liver, because you don’t have these enlarged lysosomes that are irritating to the cells.”
The effects were seen in LAL-D patients participating in an open-label extension of a double-blind placebo-controlled trial of SA. Patients in the placebo arm who began receiving SA “experienced marked and sustained improvements in liver and lipid parameters, mirroring those observed in the SA group during the double-blind period,” wrote Dr. Furuya and her coauthors. Dr. Furuya, currently a pediatric gastroenterologist at the Mayo Clinic in Rochester, Minn., was a fellow at the Alfred I. duPont Hospital for Children, Wilmington, Del., at the time of the study.
The ARISE (Acid Lipase Replacement Investigating Safety and Efficacy) study included patients aged 4 years and older with a confirmed LAL-D diagnosis. They had to have a baseline ALT at least 1.5 times the upper limit of normal, and if taking lipid-lowering medications, they had to have been on a stable dose for at least 6 weeks before starting the study, and remain on the stable dose for at least the first 32 weeks of the study.
Patients with a history of hematopoietic or liver transplantation were excluded, as were those with severe liver dysfunction, indicated by a Child-Pugh score falling into class C.
The study began with 66 patients entering a randomized, double-blind, placebo-controlled study in which patients received an every-other-week intravenous infusion of SA 1 mg/kg (n = 36), or placebo (n = 30). Median age of participants was 13 years (range, 4-58 years).
After 22 weeks, this was followed by an open-label extension period, during which patients in both arms were unblinded and received SA 1 mg/kg for the duration of the study period; 65/66 patients entered this phase. This means that patients who were initially given SA during the blinded phase of the trial received a total of 76 weeks of SA, while patients who first received placebo before entering the open-label extension did not have their data analyzed until they had been on SA for a total of 78 weeks. The extra 2 weeks accounted for a crossover period for the placebo arm to enter the open-label phase.
The protocol allowed dose increases up to 3 mg/kg if patients’ AST, ALT, LDL-C, or TG levels remained elevated, or if patients under the age of 18 continued to have low weight-for-age z scores. For patients who had problems tolerating SA, the dose could be reduced to 0.35 kg/mg.
Efficacy outcome measures included the proportion of patients who achieved AST and ALT normalization, and those whose ALT values were reduced (but not necessarily normalized). Other measures included changes in LDL-C, HDL-C, non-HDL-C, and TG; reductions in hepatic fat content and total liver volume were also tracked.
After 76 weeks, LDL-C levels were reduced by a mean 27.5%, from 199 to 142 mg/dL, and non-HDL-C dropped by a mean 26.6%, from 230 to 166 mg/dL.
Liver volume and fat content was assessed by multiecho gradient echo magnetic resonance imaging (MEGE-MRI) performed at baseline, at week 20, and at study week 52, representing 52 weeks of SA treatment for the intervention arm and 30 weeks for the placebo arm of the initial trial.
After 52 weeks of SA exposure, the mean hepatic fat reduction was 20.5%, with 88% of patients having reduced liver fat. Of those with 30 weeks of SA exposure, 88% also had reduced liver fat, with a mean fat reduction of 28%.
Liver volume also dropped, by a mean of 13.2% for those with 52 weeks of SA exposure, with 90% of patients experiencing reduced liver volume. Patients with 30 weeks of SA treatment saw a mean 11.2% reduction in liver volume; 96% of this patient group saw some decrease in liver volume.
Safety outcomes included tracking treatment-emergent adverse events (TEAEs), as well as monitoring participants for anti-drug antibodies and for the development of neutralizing antibodies to SA. The safety outcome measures were assessed for patients with longer SA exposure, ranging from 86 to 152 weeks.
There were no patient discontinuations because of TEAEs, and most events were mild or moderate; the only serious adverse event considered related to treatment was an infusion-associated reaction. This patient was able to restart SA therapy after desensitization.
Anti-drug antibodies showed up in 11% of patients (n = 7), and two of these patients had neutralizing antibodies. The safety profile was not different for the group of patients testing positive for anti-drug antibodies, wrote Dr. Furuya and her coauthors.
Replacing LAL-D has promise for a population whose disease may go long undetected. “The patients are not obvious. They are difficult to diagnose,” said Dr. Burton. “They look normal, and they feel normal in many cases, until they have life-threatening disease,” such as end-stage liver disease or cardiovascular complications, she said. Even if elevated transaminases are found in routine screening, physicians are much more likely to think of the more-common nonalcoholic fatty liver disease (NAFLD) than LAL-D, said Dr. Burton, noting that an MRI won’t clarify the diagnosis, though a liver biopsy will show microvesicular rather than macrovesicular fat distribution in LAL-D.
When the clinical picture doesn’t fit with NAFLD, though, LAL-D should be in the differential, she said, adding that she suspects the actual incidence of LAL-D may be higher than has been reported in the literature.
Dr. Burton reported receiving research support, consulting fees, and honoraria from Alexion Pharmaceuticals – the study sponsor and manufacturer of sebelipase alfa. Dr. Furuya reported no disclosures.
[email protected]
On Twitter @karioakes
AT THE LIVER MEETING 2016
Key clinical point:
Major finding: Of patients with LAL-D who received sebelipase alfa (recombinant LAL), 51% experienced normalization of ALT, and 65% had normalization of AST.
Data source: Open-label extension of randomized, double-blind, placebo-controlled trial of 66 patients with LAL-D.
Disclosures: Dr. Burton reported receiving research support, consulting fees, and honoraria from Alexion Pharmaceuticals – the study sponsor and manufacturer of sebelipase alfa. Dr. Furuya reported no disclosures.
VIDEO: Protein-rich diet can help manage type 2 diabetes, NAFLD
Patients with type 2 diabetes should be put on diets rich in either animal or plant protein to reduce not only liver fat, but insulin resistance and hepatic necroinflammation markers as well, according to a study published in the February issue of Gastroenterology (doi: 10.1053/j.gastro.2016.10.007).
“High-protein diets have shown variable and sometimes even favorable effects on glucose metabolism and insulin sensitivity in people with type 2 diabetes and it is unclear which metabolic pathways are involved,” wrote the authors of the study, led by Mariya Markova, MD, of the German Institute of Human Nutrition Potsdam-Rehbrücke in Nuthetal, Germany.
SOURCE: American Gastroenterological Association
Obesity and insulin resistance have long been linked to liver fat, with excessive amounts of the latter causing nonalcoholic fatty liver disease (NAFLD), with a significant risk of nonalcoholic steatohepatitis (NASH) developing as well. Compounding this issue, at least in the United States, are widespread dietary and nutritional habits that promote consumption of animal protein, carbohydrates, and saturated fats. This “hypercaloric Western style diet,” as the authors call it, exacerbates the accumulation of fat deposits in the liver and complicates the health of patients across the country, regardless of weight.
“Remarkably, diets restricted in methionine were shown to prevent the development of insulin resistance and of the metabolic syndrome in animal models [so] the type of protein may elicit different metabolic responses depending on the amino acid composition,” Dr. Markova and her coinvestigators noted. “It is therefore hypothesized that high-plant-protein diets exert favorable effects on hepatic fat content and metabolic responses as compared to high intake of animal protein rich in BCAA [branched-chain amino acids] and methionine,” both of which can be found in suitably low levels via plant protein.
Dr. Markova and her team devised a prospective, randomized, open-label clinical trial involving 44 patients with type 2 diabetes and NAFLD, all of whom were recruited at the department of clinical nutrition of the German Institute of Human Nutrition Potsdam-Rehbrücke between June 2013 and March 2015. Subjects were randomized into one of two cohorts, each of which were assigned a diet rich in either animal protein (AP) or plant protein (PP) for a period of 6 weeks. Median body mass index in the AP cohort was 31.0 ± 0.8, and was 29.4 ± 1.0 in the PP cohort.
The AP cohort diet consisted mainly of meat and dairy products, while legumes constituted the bulk of the PP cohort diet. Both diets were isocaloric and had the same macronutrient makeup: 30% protein, 40% carbohydrates, and 30% fat. Seven subjects dropped out prior to completion of the study; of the 37 that remained all the way through – 19 in the AP cohort, 18 in the PP cohort – the age range was 49-78 years. Subjects maintained the same physical exercise regimens throughout the study that they had beforehand, and were asked not to alter them. Hemoglobin A1c levels ranged from 5.8% to 8.8% at baseline, and evaluations were carried out at fasting levels for each subject.
Patients in both cohorts saw significant decreases in intrahepatic fat content by the end of the trial period. Those in the AP cohort saw decreases of 48.0% (P = .0002), while those in the PP cohort saw a decrease of 35.7% (P = .001). Perhaps most importantly, the reductions in both cohorts were not correlated to body weight. In addition, levels of fibroblast growth factor 21 (FGF21), which has been shown to be a predictive marker of NAFLD, decreased by nearly 50% for both AP and PP cohorts (P less than .0002 for both).
“Despite the elevated intake and postprandial uptake of methionine and BCAA in the AP group, there was no indication of negative effects of these components,” the authors stated in the study. “The origin of protein – animal or plant – did not play a major role. Both high-protein diets unexpectedly induced strong reductions of FGF21, which was associated with metabolic improvements and the decrease of IHL.”
Despite these findings, however, the 6-week time span used here is not sufficient to determine just how viable this diet may be in the long term, according to the authors. Further studies will be needed, and will need to take place over longer periods of time, to “show the durability of the responses and eventual adverse effects of the diets.” Furthermore, different age groups must be examined to find out if the benefits observed by Dr. Markova and her coinvestigators were somehow related to the age of these subjects.
The study was funded by grants from German Federal Ministry of Food and Agriculture and German Center for Diabetes Research. Dr. Markova and her coauthors did not report any financial disclosures.
Human studies to assess the effects of isocaloric macronutrient substitution are fraught with difficulty. If one macronutrient is increased, what happens to the others? If you observe an effect, is it the phenomenon you were seeking due to the macronutrient you altered, or an epiphenomenon due to changes in the others?
Markova et al. attempted to study a 6-week “isocaloric” increase of animal vs. plant protein (from 17% to 30% of calories as protein). However, a decrease of percent fat from 41% to 30%, and a reduction in carbohydrate from 42% to 40% occurred commensurately. This brings up three concerns. First, despite the diet’s being “isocaloric,” weight and body mass index decreased by 2 kg and 0.8 kg/m2, respectively. Reductions in intrahepatic, visceral, and subcutaneous fat, and an increase in lean body mass were noted. So was the diet isocaloric? Protein reduces plasma ghrelin levels and is more satiating. Furthermore, metabolism of protein to ATP is inefficient compared to that of carbohydrate or fat. The authors say only that calories were “unrestricted.” These issues do not engender “isocaloric” confidence.
Lastly, the type of carbohydrate was not controlled for. Fructose is significantly more lipogenic than glucose. Yet they were lumped together as “carbohydrate,” and were uncontrolled. So what macronutrient really caused the reduction in liver fat? These methodological issues detract from the author’s message, and this study must be considered preliminary.
Robert H. Lustig, MD, MSL, is in the division of pediatric endocrinology, UCSF Benioff Children’s Hospital, San Francisco; member, UCSF Institute for Health Policy Studies. Dr. Lustig declared no conflicts of interest.
Human studies to assess the effects of isocaloric macronutrient substitution are fraught with difficulty. If one macronutrient is increased, what happens to the others? If you observe an effect, is it the phenomenon you were seeking due to the macronutrient you altered, or an epiphenomenon due to changes in the others?
Markova et al. attempted to study a 6-week “isocaloric” increase of animal vs. plant protein (from 17% to 30% of calories as protein). However, a decrease of percent fat from 41% to 30%, and a reduction in carbohydrate from 42% to 40% occurred commensurately. This brings up three concerns. First, despite the diet’s being “isocaloric,” weight and body mass index decreased by 2 kg and 0.8 kg/m2, respectively. Reductions in intrahepatic, visceral, and subcutaneous fat, and an increase in lean body mass were noted. So was the diet isocaloric? Protein reduces plasma ghrelin levels and is more satiating. Furthermore, metabolism of protein to ATP is inefficient compared to that of carbohydrate or fat. The authors say only that calories were “unrestricted.” These issues do not engender “isocaloric” confidence.
Lastly, the type of carbohydrate was not controlled for. Fructose is significantly more lipogenic than glucose. Yet they were lumped together as “carbohydrate,” and were uncontrolled. So what macronutrient really caused the reduction in liver fat? These methodological issues detract from the author’s message, and this study must be considered preliminary.
Robert H. Lustig, MD, MSL, is in the division of pediatric endocrinology, UCSF Benioff Children’s Hospital, San Francisco; member, UCSF Institute for Health Policy Studies. Dr. Lustig declared no conflicts of interest.
Human studies to assess the effects of isocaloric macronutrient substitution are fraught with difficulty. If one macronutrient is increased, what happens to the others? If you observe an effect, is it the phenomenon you were seeking due to the macronutrient you altered, or an epiphenomenon due to changes in the others?
Markova et al. attempted to study a 6-week “isocaloric” increase of animal vs. plant protein (from 17% to 30% of calories as protein). However, a decrease of percent fat from 41% to 30%, and a reduction in carbohydrate from 42% to 40% occurred commensurately. This brings up three concerns. First, despite the diet’s being “isocaloric,” weight and body mass index decreased by 2 kg and 0.8 kg/m2, respectively. Reductions in intrahepatic, visceral, and subcutaneous fat, and an increase in lean body mass were noted. So was the diet isocaloric? Protein reduces plasma ghrelin levels and is more satiating. Furthermore, metabolism of protein to ATP is inefficient compared to that of carbohydrate or fat. The authors say only that calories were “unrestricted.” These issues do not engender “isocaloric” confidence.
Lastly, the type of carbohydrate was not controlled for. Fructose is significantly more lipogenic than glucose. Yet they were lumped together as “carbohydrate,” and were uncontrolled. So what macronutrient really caused the reduction in liver fat? These methodological issues detract from the author’s message, and this study must be considered preliminary.
Robert H. Lustig, MD, MSL, is in the division of pediatric endocrinology, UCSF Benioff Children’s Hospital, San Francisco; member, UCSF Institute for Health Policy Studies. Dr. Lustig declared no conflicts of interest.
Patients with type 2 diabetes should be put on diets rich in either animal or plant protein to reduce not only liver fat, but insulin resistance and hepatic necroinflammation markers as well, according to a study published in the February issue of Gastroenterology (doi: 10.1053/j.gastro.2016.10.007).
“High-protein diets have shown variable and sometimes even favorable effects on glucose metabolism and insulin sensitivity in people with type 2 diabetes and it is unclear which metabolic pathways are involved,” wrote the authors of the study, led by Mariya Markova, MD, of the German Institute of Human Nutrition Potsdam-Rehbrücke in Nuthetal, Germany.
SOURCE: American Gastroenterological Association
Obesity and insulin resistance have long been linked to liver fat, with excessive amounts of the latter causing nonalcoholic fatty liver disease (NAFLD), with a significant risk of nonalcoholic steatohepatitis (NASH) developing as well. Compounding this issue, at least in the United States, are widespread dietary and nutritional habits that promote consumption of animal protein, carbohydrates, and saturated fats. This “hypercaloric Western style diet,” as the authors call it, exacerbates the accumulation of fat deposits in the liver and complicates the health of patients across the country, regardless of weight.
“Remarkably, diets restricted in methionine were shown to prevent the development of insulin resistance and of the metabolic syndrome in animal models [so] the type of protein may elicit different metabolic responses depending on the amino acid composition,” Dr. Markova and her coinvestigators noted. “It is therefore hypothesized that high-plant-protein diets exert favorable effects on hepatic fat content and metabolic responses as compared to high intake of animal protein rich in BCAA [branched-chain amino acids] and methionine,” both of which can be found in suitably low levels via plant protein.
Dr. Markova and her team devised a prospective, randomized, open-label clinical trial involving 44 patients with type 2 diabetes and NAFLD, all of whom were recruited at the department of clinical nutrition of the German Institute of Human Nutrition Potsdam-Rehbrücke between June 2013 and March 2015. Subjects were randomized into one of two cohorts, each of which were assigned a diet rich in either animal protein (AP) or plant protein (PP) for a period of 6 weeks. Median body mass index in the AP cohort was 31.0 ± 0.8, and was 29.4 ± 1.0 in the PP cohort.
The AP cohort diet consisted mainly of meat and dairy products, while legumes constituted the bulk of the PP cohort diet. Both diets were isocaloric and had the same macronutrient makeup: 30% protein, 40% carbohydrates, and 30% fat. Seven subjects dropped out prior to completion of the study; of the 37 that remained all the way through – 19 in the AP cohort, 18 in the PP cohort – the age range was 49-78 years. Subjects maintained the same physical exercise regimens throughout the study that they had beforehand, and were asked not to alter them. Hemoglobin A1c levels ranged from 5.8% to 8.8% at baseline, and evaluations were carried out at fasting levels for each subject.
Patients in both cohorts saw significant decreases in intrahepatic fat content by the end of the trial period. Those in the AP cohort saw decreases of 48.0% (P = .0002), while those in the PP cohort saw a decrease of 35.7% (P = .001). Perhaps most importantly, the reductions in both cohorts were not correlated to body weight. In addition, levels of fibroblast growth factor 21 (FGF21), which has been shown to be a predictive marker of NAFLD, decreased by nearly 50% for both AP and PP cohorts (P less than .0002 for both).
“Despite the elevated intake and postprandial uptake of methionine and BCAA in the AP group, there was no indication of negative effects of these components,” the authors stated in the study. “The origin of protein – animal or plant – did not play a major role. Both high-protein diets unexpectedly induced strong reductions of FGF21, which was associated with metabolic improvements and the decrease of IHL.”
Despite these findings, however, the 6-week time span used here is not sufficient to determine just how viable this diet may be in the long term, according to the authors. Further studies will be needed, and will need to take place over longer periods of time, to “show the durability of the responses and eventual adverse effects of the diets.” Furthermore, different age groups must be examined to find out if the benefits observed by Dr. Markova and her coinvestigators were somehow related to the age of these subjects.
The study was funded by grants from German Federal Ministry of Food and Agriculture and German Center for Diabetes Research. Dr. Markova and her coauthors did not report any financial disclosures.
Patients with type 2 diabetes should be put on diets rich in either animal or plant protein to reduce not only liver fat, but insulin resistance and hepatic necroinflammation markers as well, according to a study published in the February issue of Gastroenterology (doi: 10.1053/j.gastro.2016.10.007).
“High-protein diets have shown variable and sometimes even favorable effects on glucose metabolism and insulin sensitivity in people with type 2 diabetes and it is unclear which metabolic pathways are involved,” wrote the authors of the study, led by Mariya Markova, MD, of the German Institute of Human Nutrition Potsdam-Rehbrücke in Nuthetal, Germany.
SOURCE: American Gastroenterological Association
Obesity and insulin resistance have long been linked to liver fat, with excessive amounts of the latter causing nonalcoholic fatty liver disease (NAFLD), with a significant risk of nonalcoholic steatohepatitis (NASH) developing as well. Compounding this issue, at least in the United States, are widespread dietary and nutritional habits that promote consumption of animal protein, carbohydrates, and saturated fats. This “hypercaloric Western style diet,” as the authors call it, exacerbates the accumulation of fat deposits in the liver and complicates the health of patients across the country, regardless of weight.
“Remarkably, diets restricted in methionine were shown to prevent the development of insulin resistance and of the metabolic syndrome in animal models [so] the type of protein may elicit different metabolic responses depending on the amino acid composition,” Dr. Markova and her coinvestigators noted. “It is therefore hypothesized that high-plant-protein diets exert favorable effects on hepatic fat content and metabolic responses as compared to high intake of animal protein rich in BCAA [branched-chain amino acids] and methionine,” both of which can be found in suitably low levels via plant protein.
Dr. Markova and her team devised a prospective, randomized, open-label clinical trial involving 44 patients with type 2 diabetes and NAFLD, all of whom were recruited at the department of clinical nutrition of the German Institute of Human Nutrition Potsdam-Rehbrücke between June 2013 and March 2015. Subjects were randomized into one of two cohorts, each of which were assigned a diet rich in either animal protein (AP) or plant protein (PP) for a period of 6 weeks. Median body mass index in the AP cohort was 31.0 ± 0.8, and was 29.4 ± 1.0 in the PP cohort.
The AP cohort diet consisted mainly of meat and dairy products, while legumes constituted the bulk of the PP cohort diet. Both diets were isocaloric and had the same macronutrient makeup: 30% protein, 40% carbohydrates, and 30% fat. Seven subjects dropped out prior to completion of the study; of the 37 that remained all the way through – 19 in the AP cohort, 18 in the PP cohort – the age range was 49-78 years. Subjects maintained the same physical exercise regimens throughout the study that they had beforehand, and were asked not to alter them. Hemoglobin A1c levels ranged from 5.8% to 8.8% at baseline, and evaluations were carried out at fasting levels for each subject.
Patients in both cohorts saw significant decreases in intrahepatic fat content by the end of the trial period. Those in the AP cohort saw decreases of 48.0% (P = .0002), while those in the PP cohort saw a decrease of 35.7% (P = .001). Perhaps most importantly, the reductions in both cohorts were not correlated to body weight. In addition, levels of fibroblast growth factor 21 (FGF21), which has been shown to be a predictive marker of NAFLD, decreased by nearly 50% for both AP and PP cohorts (P less than .0002 for both).
“Despite the elevated intake and postprandial uptake of methionine and BCAA in the AP group, there was no indication of negative effects of these components,” the authors stated in the study. “The origin of protein – animal or plant – did not play a major role. Both high-protein diets unexpectedly induced strong reductions of FGF21, which was associated with metabolic improvements and the decrease of IHL.”
Despite these findings, however, the 6-week time span used here is not sufficient to determine just how viable this diet may be in the long term, according to the authors. Further studies will be needed, and will need to take place over longer periods of time, to “show the durability of the responses and eventual adverse effects of the diets.” Furthermore, different age groups must be examined to find out if the benefits observed by Dr. Markova and her coinvestigators were somehow related to the age of these subjects.
The study was funded by grants from German Federal Ministry of Food and Agriculture and German Center for Diabetes Research. Dr. Markova and her coauthors did not report any financial disclosures.
FROM GASTROENTEROLOGY
Key clinical point:
Major finding: Animal- and plant-protein diets reduced liver fat for type 2 diabetes patients by 36%-48% over the course of 6 months (P = .0002 and P = .001, respectively).
Data source: Prospective study of 37 type 2 diabetes patients from June 2013 to March 2015.
Disclosures: The German Federal Ministry of Food and Agriculture and German Center for Diabetes Research supported the study. The authors did not report any financial disclosures.
AGA Clinical Practice Update: Treatment for severe alcohol hepatitis challenging
Acute alcoholic hepatitis carries a high risk of mortality, yet only a minority of patients admitted to the hospital with the condition receive appropriate treatment, said the authors of an expert review.
Writing in the January 2017 issue of Clinical Gastroenterology and Hepatology, Mack C. Mitchell Jr., MD, of the University of Texas Southwestern Medical Center, Dallas, and Craig J. McClain, MD, of the University of Louisville (Ky.), described the challenges associated with treating acute alcoholic hepatitis and its consequences.
Acute alcohol hepatitis develops in heavy drinkers and presents with rapid onset of malaise, anorexia, tender hepatomegaly, and features of the systemic inflammatory response syndrome. Patients with alcoholic hepatitis also are at high risk of nutritional deficiency, infection, acute kidney injury, and multiorgan failure.
The two most widely used therapies are glucocorticoids – generally considered the standard of care for severe alcoholic hepatitis – and the phosphodiesterase inhibitor pentoxifylline (Clin Gastroenterol Hepatol. 2017. doi: 10.1016/j.cgh.2016.08.047).
“Although in its most severe form AH has a high short-term mortality rate if untreated, in 2011, only 28% of more than 1,600 patients admitted to U.S. hospitals were treated with glucocorticoids and 17% with pentoxifylline (PTX), suggesting a lack of widespread confidence in the two most frequently used therapies for AH,” the authors wrote.
Both drugs work by addressing the underlying inflammation that plays a key role in liver injury, but the evidence for both is mixed: A 2008 Cochrane systematic review of 15 trials concluded there was no benefit from glucocorticoids, largely because of substantial variability in bias across the trials, while two meta-analyses of pentoxifylline trials concluded that there were no differences in short-term mortality between those who received it and those who did not.
Some patients are unsuitable for glucocorticoids and others may develop resistance. There is also the possibility that, while glucocorticoids may improve short-term survival, the associated increase in infection risk removes that advantage at 90 days and 1 year after diagnosis. These infections, in turn, often precede the development of acute kidney injury and multiorgan failure.
The authors, however, did suggest that the approach of very high, short-term bursts of glucocorticoids to induce “immune paralysis” – an approach taken for lupus nephritis – might be considered.
They stressed that abstinence was the cornerstone of treatment for acute alcoholic hepatitis, with studies showing that patients with alcoholic hepatitis who resume heavy drinking have significantly worse outcomes than those who don’t.
“Although abstinence is important at all stages, it is particularly important to emphasize abstinence beyond 90 days when many patients are regaining normal functioning,” Dr. Mitchell and Dr. McClain wrote.
Infection, kidney injury, and malnutrition are all significant concerns in patients with acute alcoholic hepatitis.
With respect to infection, the authors said considerable suspicion is required to pick up bacterial and fungal infections, as patients may not always have a fever and an elevated white blood cell count is an unreliable indicator. Infection also can lead to acute kidney injury.
Malnutrition is not only common in patients with alcohol hepatitis, but it has a significant negative impact on recovery. All patients should be encouraged to meet nutritional goals as early as possible, but just how to achieve this is controversial, the authors stressed.
For example, one study suggested that enteral nutrition was as good as glucocorticoids in reducing 28-day mortality, while another found enteral nutrition via nasogastric tube – in addition to glucocorticoids – was no better than glucocorticoids alone. “Whether [nasogastric] tubes should be used to provide enteral nutrition is a subject of controversy,” the authors wrote. “Normal- to high-protein diets are safe and do not increase the risk of encephalopathy in patients with AH.”
No conflicts of interest were declared.
Acute alcoholic hepatitis carries a high risk of mortality, yet only a minority of patients admitted to the hospital with the condition receive appropriate treatment, said the authors of an expert review.
Writing in the January 2017 issue of Clinical Gastroenterology and Hepatology, Mack C. Mitchell Jr., MD, of the University of Texas Southwestern Medical Center, Dallas, and Craig J. McClain, MD, of the University of Louisville (Ky.), described the challenges associated with treating acute alcoholic hepatitis and its consequences.
Acute alcohol hepatitis develops in heavy drinkers and presents with rapid onset of malaise, anorexia, tender hepatomegaly, and features of the systemic inflammatory response syndrome. Patients with alcoholic hepatitis also are at high risk of nutritional deficiency, infection, acute kidney injury, and multiorgan failure.
The two most widely used therapies are glucocorticoids – generally considered the standard of care for severe alcoholic hepatitis – and the phosphodiesterase inhibitor pentoxifylline (Clin Gastroenterol Hepatol. 2017. doi: 10.1016/j.cgh.2016.08.047).
“Although in its most severe form AH has a high short-term mortality rate if untreated, in 2011, only 28% of more than 1,600 patients admitted to U.S. hospitals were treated with glucocorticoids and 17% with pentoxifylline (PTX), suggesting a lack of widespread confidence in the two most frequently used therapies for AH,” the authors wrote.
Both drugs work by addressing the underlying inflammation that plays a key role in liver injury, but the evidence for both is mixed: A 2008 Cochrane systematic review of 15 trials concluded there was no benefit from glucocorticoids, largely because of substantial variability in bias across the trials, while two meta-analyses of pentoxifylline trials concluded that there were no differences in short-term mortality between those who received it and those who did not.
Some patients are unsuitable for glucocorticoids and others may develop resistance. There is also the possibility that, while glucocorticoids may improve short-term survival, the associated increase in infection risk removes that advantage at 90 days and 1 year after diagnosis. These infections, in turn, often precede the development of acute kidney injury and multiorgan failure.
The authors, however, did suggest that the approach of very high, short-term bursts of glucocorticoids to induce “immune paralysis” – an approach taken for lupus nephritis – might be considered.
They stressed that abstinence was the cornerstone of treatment for acute alcoholic hepatitis, with studies showing that patients with alcoholic hepatitis who resume heavy drinking have significantly worse outcomes than those who don’t.
“Although abstinence is important at all stages, it is particularly important to emphasize abstinence beyond 90 days when many patients are regaining normal functioning,” Dr. Mitchell and Dr. McClain wrote.
Infection, kidney injury, and malnutrition are all significant concerns in patients with acute alcoholic hepatitis.
With respect to infection, the authors said considerable suspicion is required to pick up bacterial and fungal infections, as patients may not always have a fever and an elevated white blood cell count is an unreliable indicator. Infection also can lead to acute kidney injury.
Malnutrition is not only common in patients with alcohol hepatitis, but it has a significant negative impact on recovery. All patients should be encouraged to meet nutritional goals as early as possible, but just how to achieve this is controversial, the authors stressed.
For example, one study suggested that enteral nutrition was as good as glucocorticoids in reducing 28-day mortality, while another found enteral nutrition via nasogastric tube – in addition to glucocorticoids – was no better than glucocorticoids alone. “Whether [nasogastric] tubes should be used to provide enteral nutrition is a subject of controversy,” the authors wrote. “Normal- to high-protein diets are safe and do not increase the risk of encephalopathy in patients with AH.”
No conflicts of interest were declared.
Acute alcoholic hepatitis carries a high risk of mortality, yet only a minority of patients admitted to the hospital with the condition receive appropriate treatment, said the authors of an expert review.
Writing in the January 2017 issue of Clinical Gastroenterology and Hepatology, Mack C. Mitchell Jr., MD, of the University of Texas Southwestern Medical Center, Dallas, and Craig J. McClain, MD, of the University of Louisville (Ky.), described the challenges associated with treating acute alcoholic hepatitis and its consequences.
Acute alcohol hepatitis develops in heavy drinkers and presents with rapid onset of malaise, anorexia, tender hepatomegaly, and features of the systemic inflammatory response syndrome. Patients with alcoholic hepatitis also are at high risk of nutritional deficiency, infection, acute kidney injury, and multiorgan failure.
The two most widely used therapies are glucocorticoids – generally considered the standard of care for severe alcoholic hepatitis – and the phosphodiesterase inhibitor pentoxifylline (Clin Gastroenterol Hepatol. 2017. doi: 10.1016/j.cgh.2016.08.047).
“Although in its most severe form AH has a high short-term mortality rate if untreated, in 2011, only 28% of more than 1,600 patients admitted to U.S. hospitals were treated with glucocorticoids and 17% with pentoxifylline (PTX), suggesting a lack of widespread confidence in the two most frequently used therapies for AH,” the authors wrote.
Both drugs work by addressing the underlying inflammation that plays a key role in liver injury, but the evidence for both is mixed: A 2008 Cochrane systematic review of 15 trials concluded there was no benefit from glucocorticoids, largely because of substantial variability in bias across the trials, while two meta-analyses of pentoxifylline trials concluded that there were no differences in short-term mortality between those who received it and those who did not.
Some patients are unsuitable for glucocorticoids and others may develop resistance. There is also the possibility that, while glucocorticoids may improve short-term survival, the associated increase in infection risk removes that advantage at 90 days and 1 year after diagnosis. These infections, in turn, often precede the development of acute kidney injury and multiorgan failure.
The authors, however, did suggest that the approach of very high, short-term bursts of glucocorticoids to induce “immune paralysis” – an approach taken for lupus nephritis – might be considered.
They stressed that abstinence was the cornerstone of treatment for acute alcoholic hepatitis, with studies showing that patients with alcoholic hepatitis who resume heavy drinking have significantly worse outcomes than those who don’t.
“Although abstinence is important at all stages, it is particularly important to emphasize abstinence beyond 90 days when many patients are regaining normal functioning,” Dr. Mitchell and Dr. McClain wrote.
Infection, kidney injury, and malnutrition are all significant concerns in patients with acute alcoholic hepatitis.
With respect to infection, the authors said considerable suspicion is required to pick up bacterial and fungal infections, as patients may not always have a fever and an elevated white blood cell count is an unreliable indicator. Infection also can lead to acute kidney injury.
Malnutrition is not only common in patients with alcohol hepatitis, but it has a significant negative impact on recovery. All patients should be encouraged to meet nutritional goals as early as possible, but just how to achieve this is controversial, the authors stressed.
For example, one study suggested that enteral nutrition was as good as glucocorticoids in reducing 28-day mortality, while another found enteral nutrition via nasogastric tube – in addition to glucocorticoids – was no better than glucocorticoids alone. “Whether [nasogastric] tubes should be used to provide enteral nutrition is a subject of controversy,” the authors wrote. “Normal- to high-protein diets are safe and do not increase the risk of encephalopathy in patients with AH.”
No conflicts of interest were declared.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Covered-stent TIPS tops large-volume paracentesis for cirrhosis survival
One-year survival without liver transplant was far more likely when transjugular intrahepatic portosystemic shunts (TIPS) with covered stents were used to treat cirrhosis with recurrent ascites, instead of ongoing large-volume paracenteses with albumin, in a 62-patient randomized trial from France.
“TIPS with covered stents ... should therefore be preferred to LVP [large-volume paracenteses] with volume expansion... These findings support TIPS as the first-line intervention,” said investigators led by gastroenterologist Christophe Bureau, MD, of Toulouse (France) University in the January issue of Gastroenterology (doi: 10.1053/j.gastro.2016.09.016).
All 62 patients had at least two LVPs prior to the study; 29 were then randomized to covered transjugular intrahepatic portosystemic shunt (TIPS), and 33 to LVP and albumin as needed. All the patients were on a low-salt diet.
Twenty-seven TIPS patients (93%) were alive without a liver transplant at 1 year, versus 17 (52%) in the LVP group (P = .003). TIPS patients had a total of 32 paracenteses in the first year, versus 320 in the LVP group. Six paracentesis patients (18%) had portal hypertension–related bleeding, and six had hernia-related complications; none of the TIPS patients had either. LVP patients spent a mean of 35 days in the hospital, versus 17 days for the TIPS group (P = .04). The probability of remaining free of encephalopathy at 1 year was the same in both groups, at 65%.
It has been shown before that TIPS has the edge on LVP for reducing recurrence of tense ascites. However, early studies used uncovered stents and, due to their almost 80% risk of dysfunction, they did not show a significant benefit for survival. As a result, repeated paracenteses have been recommended as first-line treatment, with TIPS held in reserve for patients who need very frequent LVP.
Polytetrafluoroethylene-covered stents appear to have changed the equation, “owing to a substantial decrease in the rate of shunt dysfunction,” the investigators said.
The French results are a bit better than previous reports of covered TIPS. “This could be related to greater experience with the TIPS procedure;” there were no technical failures. The study also mostly included patients younger than 65 years with Child-Pugh class B disease and no prior encephalopathy – favorable factors that also may have contributed to the results. However, “we believe that the use of covered stents was the main determinant of the observed improvement in outcomes... TIPS with uncovered stent[s] should not be considered effective or recommended any longer for the long-term treatment of” portal hypertension, they said.
Cirrhosis in the trial was due almost entirely to alcohol abuse. About three-quarters of both groups reported abstinence while enrolled. The mean age was 56 years, and the majority of subjects were men.
The work was funded by the French Ministry of Health and supported by Gore, maker of the covered stent used in the study. Dr. Bureau and another author are Gore consultants.
One-year survival without liver transplant was far more likely when transjugular intrahepatic portosystemic shunts (TIPS) with covered stents were used to treat cirrhosis with recurrent ascites, instead of ongoing large-volume paracenteses with albumin, in a 62-patient randomized trial from France.
“TIPS with covered stents ... should therefore be preferred to LVP [large-volume paracenteses] with volume expansion... These findings support TIPS as the first-line intervention,” said investigators led by gastroenterologist Christophe Bureau, MD, of Toulouse (France) University in the January issue of Gastroenterology (doi: 10.1053/j.gastro.2016.09.016).
All 62 patients had at least two LVPs prior to the study; 29 were then randomized to covered transjugular intrahepatic portosystemic shunt (TIPS), and 33 to LVP and albumin as needed. All the patients were on a low-salt diet.
Twenty-seven TIPS patients (93%) were alive without a liver transplant at 1 year, versus 17 (52%) in the LVP group (P = .003). TIPS patients had a total of 32 paracenteses in the first year, versus 320 in the LVP group. Six paracentesis patients (18%) had portal hypertension–related bleeding, and six had hernia-related complications; none of the TIPS patients had either. LVP patients spent a mean of 35 days in the hospital, versus 17 days for the TIPS group (P = .04). The probability of remaining free of encephalopathy at 1 year was the same in both groups, at 65%.
It has been shown before that TIPS has the edge on LVP for reducing recurrence of tense ascites. However, early studies used uncovered stents and, due to their almost 80% risk of dysfunction, they did not show a significant benefit for survival. As a result, repeated paracenteses have been recommended as first-line treatment, with TIPS held in reserve for patients who need very frequent LVP.
Polytetrafluoroethylene-covered stents appear to have changed the equation, “owing to a substantial decrease in the rate of shunt dysfunction,” the investigators said.
The French results are a bit better than previous reports of covered TIPS. “This could be related to greater experience with the TIPS procedure;” there were no technical failures. The study also mostly included patients younger than 65 years with Child-Pugh class B disease and no prior encephalopathy – favorable factors that also may have contributed to the results. However, “we believe that the use of covered stents was the main determinant of the observed improvement in outcomes... TIPS with uncovered stent[s] should not be considered effective or recommended any longer for the long-term treatment of” portal hypertension, they said.
Cirrhosis in the trial was due almost entirely to alcohol abuse. About three-quarters of both groups reported abstinence while enrolled. The mean age was 56 years, and the majority of subjects were men.
The work was funded by the French Ministry of Health and supported by Gore, maker of the covered stent used in the study. Dr. Bureau and another author are Gore consultants.
One-year survival without liver transplant was far more likely when transjugular intrahepatic portosystemic shunts (TIPS) with covered stents were used to treat cirrhosis with recurrent ascites, instead of ongoing large-volume paracenteses with albumin, in a 62-patient randomized trial from France.
“TIPS with covered stents ... should therefore be preferred to LVP [large-volume paracenteses] with volume expansion... These findings support TIPS as the first-line intervention,” said investigators led by gastroenterologist Christophe Bureau, MD, of Toulouse (France) University in the January issue of Gastroenterology (doi: 10.1053/j.gastro.2016.09.016).
All 62 patients had at least two LVPs prior to the study; 29 were then randomized to covered transjugular intrahepatic portosystemic shunt (TIPS), and 33 to LVP and albumin as needed. All the patients were on a low-salt diet.
Twenty-seven TIPS patients (93%) were alive without a liver transplant at 1 year, versus 17 (52%) in the LVP group (P = .003). TIPS patients had a total of 32 paracenteses in the first year, versus 320 in the LVP group. Six paracentesis patients (18%) had portal hypertension–related bleeding, and six had hernia-related complications; none of the TIPS patients had either. LVP patients spent a mean of 35 days in the hospital, versus 17 days for the TIPS group (P = .04). The probability of remaining free of encephalopathy at 1 year was the same in both groups, at 65%.
It has been shown before that TIPS has the edge on LVP for reducing recurrence of tense ascites. However, early studies used uncovered stents and, due to their almost 80% risk of dysfunction, they did not show a significant benefit for survival. As a result, repeated paracenteses have been recommended as first-line treatment, with TIPS held in reserve for patients who need very frequent LVP.
Polytetrafluoroethylene-covered stents appear to have changed the equation, “owing to a substantial decrease in the rate of shunt dysfunction,” the investigators said.
The French results are a bit better than previous reports of covered TIPS. “This could be related to greater experience with the TIPS procedure;” there were no technical failures. The study also mostly included patients younger than 65 years with Child-Pugh class B disease and no prior encephalopathy – favorable factors that also may have contributed to the results. However, “we believe that the use of covered stents was the main determinant of the observed improvement in outcomes... TIPS with uncovered stent[s] should not be considered effective or recommended any longer for the long-term treatment of” portal hypertension, they said.
Cirrhosis in the trial was due almost entirely to alcohol abuse. About three-quarters of both groups reported abstinence while enrolled. The mean age was 56 years, and the majority of subjects were men.
The work was funded by the French Ministry of Health and supported by Gore, maker of the covered stent used in the study. Dr. Bureau and another author are Gore consultants.
FROM GASTROENTEROLOGY
Key clinical point:
Major finding: Twenty-seven TIPS patients (93%) were alive without a liver transplant at 1 year, versus 17 (52%) in the LVP group (P = .003).
Data source: Randomized trial with 62 patients.
Disclosures: The work was funded by the French Ministry of Health and supported by Gore, maker of the covered stent used in the study. The lead and one other investigator are Gore consultants.
Hepatitis Outlook: November 2016
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
The introduction of universal mass vaccination against hepatitis A in countries with intermediate endemicity for HAV infection led to a considerable decrease in the incidence of HAV in vaccinated and in nonvaccinated age groups alike.
Mortality was high among chronic hepatitis C patients, with and without cirrhosis, compared with the general population, a Danish cohort study found. Curing CHC was associated with reduced mortality among cirrhotic patients but remained higher than the general population.
A hepatitis C outbreak in a North Dakota skilled nursing facility highlights the importance of prompt reporting and investigation of incident HCV infection, and the need for adherence to basic infection control procedures by health care personnel.
A recent study identified a novel hepatitis B virus subgenotype D10 circulating in Ethiopia, underlining the high genetic variability of HBV strains in Africa.
A study in the Journal of Viral Hepatitis found that baseline hepatitis B core antibody predicts treatment response in chronic hepatitis B patients receiving long-term entecavir.
A novel quantitative microarray antibody capture assay was able to identify extremely high hepatitis delta virus prevalence amongst hepatitis B virus–infected Mongolians.
The albumin-bilirubin (ALBI) score was effective in predicting the long-term prognosis for patients with hepatitis B virus–related cirrhosis and was more accurate than Child-Pugh and Model for End-Stage Liver Disease (MELD) scores.
A study in Hepatology found that proanthocyanidin (PAC) and its analogs present a new class of anti–hepatitis B virus agents that directly target the preS1 region of the HBV large surface protein and could contribute to the development of a potent, well-tolerated, and broadly active inhibitor of HBV infection.
A hepatitis C virus core antigen (HCV-Ag) assay proved to be useful in monitoring treatment of HCV-infected patients with sustained viral response and in patients who experienced treatment failures, according to a study in Diagnostic Microbiology and Infectious Disease.
The introduction of a managed care network for patients infected with hepatitis C virus increased access to care and reduced all-cause mortality, according to a recent study.
A study in South Korea found that hepatitis B infection was associated with an increased incidence of thrombocytopenia in healthy adults without cirrhosis.
A proof-of-concept study demonstrated that peritransplant immunoprophylaxis combined with a single oral direct-acting antiviral in the immediate post-transplant period can prevent HCV recurrence.
A study in the Journal of Viral Hepatitis established the baseline mortality and hepatocellular carcinoma progression rates in decompensated cirrhosis patients against which the impact of new antiviral therapies could be measured.
Genetic distance-based network analyses can be used to identify characteristics associated with hepatitis C virus transmission, informing targeted prevention and treatment strategies, according to a recent study.
According to a new study, primary T-cell immunodeficiency is associated with a lower spontaneous clearance of hepatitis C virus, while female sex and coinfection with hepatitis B virus are associated with a higher spontaneous clearance.
A study in the Journal of Viral Hepatitis found that the induction of humoral and cellular immune response to hepatitis B virus vaccine can be upregulated by CpG oligonucleotides complexed with Dectin-1 ligand.
[email protected]
On Twitter @richpizzi
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
The introduction of universal mass vaccination against hepatitis A in countries with intermediate endemicity for HAV infection led to a considerable decrease in the incidence of HAV in vaccinated and in nonvaccinated age groups alike.
Mortality was high among chronic hepatitis C patients, with and without cirrhosis, compared with the general population, a Danish cohort study found. Curing CHC was associated with reduced mortality among cirrhotic patients but remained higher than the general population.
A hepatitis C outbreak in a North Dakota skilled nursing facility highlights the importance of prompt reporting and investigation of incident HCV infection, and the need for adherence to basic infection control procedures by health care personnel.
A recent study identified a novel hepatitis B virus subgenotype D10 circulating in Ethiopia, underlining the high genetic variability of HBV strains in Africa.
A study in the Journal of Viral Hepatitis found that baseline hepatitis B core antibody predicts treatment response in chronic hepatitis B patients receiving long-term entecavir.
A novel quantitative microarray antibody capture assay was able to identify extremely high hepatitis delta virus prevalence amongst hepatitis B virus–infected Mongolians.
The albumin-bilirubin (ALBI) score was effective in predicting the long-term prognosis for patients with hepatitis B virus–related cirrhosis and was more accurate than Child-Pugh and Model for End-Stage Liver Disease (MELD) scores.
A study in Hepatology found that proanthocyanidin (PAC) and its analogs present a new class of anti–hepatitis B virus agents that directly target the preS1 region of the HBV large surface protein and could contribute to the development of a potent, well-tolerated, and broadly active inhibitor of HBV infection.
A hepatitis C virus core antigen (HCV-Ag) assay proved to be useful in monitoring treatment of HCV-infected patients with sustained viral response and in patients who experienced treatment failures, according to a study in Diagnostic Microbiology and Infectious Disease.
The introduction of a managed care network for patients infected with hepatitis C virus increased access to care and reduced all-cause mortality, according to a recent study.
A study in South Korea found that hepatitis B infection was associated with an increased incidence of thrombocytopenia in healthy adults without cirrhosis.
A proof-of-concept study demonstrated that peritransplant immunoprophylaxis combined with a single oral direct-acting antiviral in the immediate post-transplant period can prevent HCV recurrence.
A study in the Journal of Viral Hepatitis established the baseline mortality and hepatocellular carcinoma progression rates in decompensated cirrhosis patients against which the impact of new antiviral therapies could be measured.
Genetic distance-based network analyses can be used to identify characteristics associated with hepatitis C virus transmission, informing targeted prevention and treatment strategies, according to a recent study.
According to a new study, primary T-cell immunodeficiency is associated with a lower spontaneous clearance of hepatitis C virus, while female sex and coinfection with hepatitis B virus are associated with a higher spontaneous clearance.
A study in the Journal of Viral Hepatitis found that the induction of humoral and cellular immune response to hepatitis B virus vaccine can be upregulated by CpG oligonucleotides complexed with Dectin-1 ligand.
[email protected]
On Twitter @richpizzi
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
The introduction of universal mass vaccination against hepatitis A in countries with intermediate endemicity for HAV infection led to a considerable decrease in the incidence of HAV in vaccinated and in nonvaccinated age groups alike.
Mortality was high among chronic hepatitis C patients, with and without cirrhosis, compared with the general population, a Danish cohort study found. Curing CHC was associated with reduced mortality among cirrhotic patients but remained higher than the general population.
A hepatitis C outbreak in a North Dakota skilled nursing facility highlights the importance of prompt reporting and investigation of incident HCV infection, and the need for adherence to basic infection control procedures by health care personnel.
A recent study identified a novel hepatitis B virus subgenotype D10 circulating in Ethiopia, underlining the high genetic variability of HBV strains in Africa.
A study in the Journal of Viral Hepatitis found that baseline hepatitis B core antibody predicts treatment response in chronic hepatitis B patients receiving long-term entecavir.
A novel quantitative microarray antibody capture assay was able to identify extremely high hepatitis delta virus prevalence amongst hepatitis B virus–infected Mongolians.
The albumin-bilirubin (ALBI) score was effective in predicting the long-term prognosis for patients with hepatitis B virus–related cirrhosis and was more accurate than Child-Pugh and Model for End-Stage Liver Disease (MELD) scores.
A study in Hepatology found that proanthocyanidin (PAC) and its analogs present a new class of anti–hepatitis B virus agents that directly target the preS1 region of the HBV large surface protein and could contribute to the development of a potent, well-tolerated, and broadly active inhibitor of HBV infection.
A hepatitis C virus core antigen (HCV-Ag) assay proved to be useful in monitoring treatment of HCV-infected patients with sustained viral response and in patients who experienced treatment failures, according to a study in Diagnostic Microbiology and Infectious Disease.
The introduction of a managed care network for patients infected with hepatitis C virus increased access to care and reduced all-cause mortality, according to a recent study.
A study in South Korea found that hepatitis B infection was associated with an increased incidence of thrombocytopenia in healthy adults without cirrhosis.
A proof-of-concept study demonstrated that peritransplant immunoprophylaxis combined with a single oral direct-acting antiviral in the immediate post-transplant period can prevent HCV recurrence.
A study in the Journal of Viral Hepatitis established the baseline mortality and hepatocellular carcinoma progression rates in decompensated cirrhosis patients against which the impact of new antiviral therapies could be measured.
Genetic distance-based network analyses can be used to identify characteristics associated with hepatitis C virus transmission, informing targeted prevention and treatment strategies, according to a recent study.
According to a new study, primary T-cell immunodeficiency is associated with a lower spontaneous clearance of hepatitis C virus, while female sex and coinfection with hepatitis B virus are associated with a higher spontaneous clearance.
A study in the Journal of Viral Hepatitis found that the induction of humoral and cellular immune response to hepatitis B virus vaccine can be upregulated by CpG oligonucleotides complexed with Dectin-1 ligand.
[email protected]
On Twitter @richpizzi
VIDEO: Angiogenesis has a role to play in NASH and NAFLD
BOSTON – A multimodal research process has provided clues to the role of angiogenesis in nonalcoholic fatty liver disease (NAFLD) and its more serious cousin, nonalcoholic steatohepatitis (NASH).
In constructing a protocol that began with patients, moved on to bioinformatics and then performed final validation in the petri dish, Savneet Kaur, PhD, and her colleagues were able to identify several angiogenesis genes likely to contribute to the development of NAFLD and NASH.
“We have seen angiogenic mechanisms and angiogenic genes in the pathophysiology of nonalcoholic fatty liver disease,” said Dr. Kaur, professor of biotechnology at Gautam Buddha Medical School, Greater Noida, India, in a video interview at the annual meeting of the American Association for the Study of Liver Diseases.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Kaur said that she and her coinvestigators began with a small group of eight patients with NASH, and seven patients with NAFLD, and also with seven healthy control participants. Genetic analysis and comparison of these patients yielded differential expression of certain genes already known to be associated with angiogenesis in the NASH and NAFLD, but not the healthy control participants.
“We did a microarray analysis, a high throughput gene expression study, and then we selected around 25 to 26 genes which were associated with oxidative stress and angiogenesis,” said Dr. Kaur.
For validation of these genes, Dr. Kaur and her associates used a larger study group of about 150 participants, again approximately evenly divided between those with mild NAFLD, those with more severe steatohepatitis, and healthy controls. “We validated the angiogenic genes in the subject group, and found that around 13 genes are preferentially expressed.”
“About 13 genes including VEGFR1, PIK3CA, CXCL8, NOS3, EREG, CCL2, PRKCE, PPar-gamma, PROK2, RUNX1, SIRT1, HMOX1 and CXCR4 showed significantly different gene expression in the [reverse transcription–polymerase chain reaction] analysis in Gr3 as compared to Gr1 (P less than .05 for each), whereas genes such as PIK3CA, CXCL8, NOS3, CCL2, PROK2, RUNX1, and HMOX1 were differentially expressed in Gr3 in comparison to Gr2 (P less than .05 each). A few genes, PPar-gamma, SIRT1, VEGFR1, HMOX1, PIK3CA, CXCR4, PROK2, and CCL2, showed correlations with fibrosis scores, angiogenesis scores, and NAFLD activity scores of the patients,” wrote Dr. Kaur and her colleagues in the abstract accompanying the poster presentation.
Taking these candidate genes, Dr. Kaur and her colleagues conducted a bioinformatics analysis to determine which transcription factors were controlling the genes. “We wanted to study the pathway – the mechanisms – to determine the upregulation and downregulation of these genes,” said Dr. Kaur.
Finally, Dr. Kaur and her associates took an in vitro approach, using human steatotic hepatocytes and endothelial cells, since “angiogenesis is a property of endothelial cells.” The two types of cells were cultured together, and angiogenic function and gene expression were examined, and checked against the genes and pathways identified in the first two steps. They again saw expression of the angiogenic pathways in the cell culture model. This was consistent with what is seen in patients with NAFLD and NASH: “Definitely, there’s an increase in angiogenesis. There’s an increase in the endothelial cell proliferation, with more fat, more steatosis in the patients,” said Dr. Kaur. Some genes, said Dr. Kaur, are “really important” to this process. Her group is now investigating how the genes are regulated, in order to understand better the precise role of angiogenesis in steatohepatitis.
The study was part of a joint Indo-German project, and sponsored by the Indian Council for Medical Research and the German Federal Ministry of Education and Research. Dr. Kaur reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
BOSTON – A multimodal research process has provided clues to the role of angiogenesis in nonalcoholic fatty liver disease (NAFLD) and its more serious cousin, nonalcoholic steatohepatitis (NASH).
In constructing a protocol that began with patients, moved on to bioinformatics and then performed final validation in the petri dish, Savneet Kaur, PhD, and her colleagues were able to identify several angiogenesis genes likely to contribute to the development of NAFLD and NASH.
“We have seen angiogenic mechanisms and angiogenic genes in the pathophysiology of nonalcoholic fatty liver disease,” said Dr. Kaur, professor of biotechnology at Gautam Buddha Medical School, Greater Noida, India, in a video interview at the annual meeting of the American Association for the Study of Liver Diseases.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Kaur said that she and her coinvestigators began with a small group of eight patients with NASH, and seven patients with NAFLD, and also with seven healthy control participants. Genetic analysis and comparison of these patients yielded differential expression of certain genes already known to be associated with angiogenesis in the NASH and NAFLD, but not the healthy control participants.
“We did a microarray analysis, a high throughput gene expression study, and then we selected around 25 to 26 genes which were associated with oxidative stress and angiogenesis,” said Dr. Kaur.
For validation of these genes, Dr. Kaur and her associates used a larger study group of about 150 participants, again approximately evenly divided between those with mild NAFLD, those with more severe steatohepatitis, and healthy controls. “We validated the angiogenic genes in the subject group, and found that around 13 genes are preferentially expressed.”
“About 13 genes including VEGFR1, PIK3CA, CXCL8, NOS3, EREG, CCL2, PRKCE, PPar-gamma, PROK2, RUNX1, SIRT1, HMOX1 and CXCR4 showed significantly different gene expression in the [reverse transcription–polymerase chain reaction] analysis in Gr3 as compared to Gr1 (P less than .05 for each), whereas genes such as PIK3CA, CXCL8, NOS3, CCL2, PROK2, RUNX1, and HMOX1 were differentially expressed in Gr3 in comparison to Gr2 (P less than .05 each). A few genes, PPar-gamma, SIRT1, VEGFR1, HMOX1, PIK3CA, CXCR4, PROK2, and CCL2, showed correlations with fibrosis scores, angiogenesis scores, and NAFLD activity scores of the patients,” wrote Dr. Kaur and her colleagues in the abstract accompanying the poster presentation.
Taking these candidate genes, Dr. Kaur and her colleagues conducted a bioinformatics analysis to determine which transcription factors were controlling the genes. “We wanted to study the pathway – the mechanisms – to determine the upregulation and downregulation of these genes,” said Dr. Kaur.
Finally, Dr. Kaur and her associates took an in vitro approach, using human steatotic hepatocytes and endothelial cells, since “angiogenesis is a property of endothelial cells.” The two types of cells were cultured together, and angiogenic function and gene expression were examined, and checked against the genes and pathways identified in the first two steps. They again saw expression of the angiogenic pathways in the cell culture model. This was consistent with what is seen in patients with NAFLD and NASH: “Definitely, there’s an increase in angiogenesis. There’s an increase in the endothelial cell proliferation, with more fat, more steatosis in the patients,” said Dr. Kaur. Some genes, said Dr. Kaur, are “really important” to this process. Her group is now investigating how the genes are regulated, in order to understand better the precise role of angiogenesis in steatohepatitis.
The study was part of a joint Indo-German project, and sponsored by the Indian Council for Medical Research and the German Federal Ministry of Education and Research. Dr. Kaur reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
BOSTON – A multimodal research process has provided clues to the role of angiogenesis in nonalcoholic fatty liver disease (NAFLD) and its more serious cousin, nonalcoholic steatohepatitis (NASH).
In constructing a protocol that began with patients, moved on to bioinformatics and then performed final validation in the petri dish, Savneet Kaur, PhD, and her colleagues were able to identify several angiogenesis genes likely to contribute to the development of NAFLD and NASH.
“We have seen angiogenic mechanisms and angiogenic genes in the pathophysiology of nonalcoholic fatty liver disease,” said Dr. Kaur, professor of biotechnology at Gautam Buddha Medical School, Greater Noida, India, in a video interview at the annual meeting of the American Association for the Study of Liver Diseases.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Kaur said that she and her coinvestigators began with a small group of eight patients with NASH, and seven patients with NAFLD, and also with seven healthy control participants. Genetic analysis and comparison of these patients yielded differential expression of certain genes already known to be associated with angiogenesis in the NASH and NAFLD, but not the healthy control participants.
“We did a microarray analysis, a high throughput gene expression study, and then we selected around 25 to 26 genes which were associated with oxidative stress and angiogenesis,” said Dr. Kaur.
For validation of these genes, Dr. Kaur and her associates used a larger study group of about 150 participants, again approximately evenly divided between those with mild NAFLD, those with more severe steatohepatitis, and healthy controls. “We validated the angiogenic genes in the subject group, and found that around 13 genes are preferentially expressed.”
“About 13 genes including VEGFR1, PIK3CA, CXCL8, NOS3, EREG, CCL2, PRKCE, PPar-gamma, PROK2, RUNX1, SIRT1, HMOX1 and CXCR4 showed significantly different gene expression in the [reverse transcription–polymerase chain reaction] analysis in Gr3 as compared to Gr1 (P less than .05 for each), whereas genes such as PIK3CA, CXCL8, NOS3, CCL2, PROK2, RUNX1, and HMOX1 were differentially expressed in Gr3 in comparison to Gr2 (P less than .05 each). A few genes, PPar-gamma, SIRT1, VEGFR1, HMOX1, PIK3CA, CXCR4, PROK2, and CCL2, showed correlations with fibrosis scores, angiogenesis scores, and NAFLD activity scores of the patients,” wrote Dr. Kaur and her colleagues in the abstract accompanying the poster presentation.
Taking these candidate genes, Dr. Kaur and her colleagues conducted a bioinformatics analysis to determine which transcription factors were controlling the genes. “We wanted to study the pathway – the mechanisms – to determine the upregulation and downregulation of these genes,” said Dr. Kaur.
Finally, Dr. Kaur and her associates took an in vitro approach, using human steatotic hepatocytes and endothelial cells, since “angiogenesis is a property of endothelial cells.” The two types of cells were cultured together, and angiogenic function and gene expression were examined, and checked against the genes and pathways identified in the first two steps. They again saw expression of the angiogenic pathways in the cell culture model. This was consistent with what is seen in patients with NAFLD and NASH: “Definitely, there’s an increase in angiogenesis. There’s an increase in the endothelial cell proliferation, with more fat, more steatosis in the patients,” said Dr. Kaur. Some genes, said Dr. Kaur, are “really important” to this process. Her group is now investigating how the genes are regulated, in order to understand better the precise role of angiogenesis in steatohepatitis.
The study was part of a joint Indo-German project, and sponsored by the Indian Council for Medical Research and the German Federal Ministry of Education and Research. Dr. Kaur reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
AT THE LIVER MEETING 2016
Key clinical point:
Major finding: PPar-gamma, SIRT1, VEGFR1, and other genes are associated with fibrosis, angiogenesis, and steatosis.
Data source: Human bioinformatics–in vitro exploration of genetic pathways associated with angiogenesis in NASH and nonalcoholic fatty liver disease (NAFLD).
Disclosures: The study was part of a joint Indo-German project, and funded by the Indian Council for Medical Research and the German Federal Ministry of Education and Research. Dr. Kaur reported no relevant financial disclosures.
Nonalcoholic fatty liver disease accelerates brain aging
TORONTO – Nonalcoholic fatty liver disease seems to accelerate physical brain aging by up to 7 years, according to a new subanalysis of the ongoing Framingham Heart Study.
However, while finding that the liver disorder directly endangers brains, the study also offers hope, Galit Weinstein, PhD, said at the Alzheimer’s Association International Conference 2016. “If indeed nonalcoholic fatty liver disease is a risk factor for brain aging and subsequent dementia, then it is a modifiable one,” said Dr. Weinstein of Boston University. “We have reason to hope that NAFLD remission could possibly improve cognitive outcomes” as patients age.
For this study, the researchers assessed the presence of NAFLD by abdominal CT scans and white-matter hyperintensities and brain volume (total, frontal, and hippocampal) by MRI. The resulting associations were then adjusted for age, sex, alcohol consumption, visceral adipose tissue, body mass index, menopausal status, systolic blood pressure, current smoking, diabetes, history of cardiovascular disease, physical activity, insulin resistance, and C-reactive protein.
There were no significant associations with white-matter hyperintensities or with hippocampal volume, but the researches did find a significant association with total brain volume: Even after adjustment for all of the covariates, patients with NAFLD had smaller-than-normal brains for their age. This can be seen as a pathologic acceleration of the brain aging process, Dr. Weinstein said.
The finding was most striking among the youngest subjects, she said, accounting for about a 7-year advance in brain aging for those younger than 60 years. Older patients with NAFLD showed about a 2-year advance in brain aging.
The effect is probably mediated by the liver’s complex interplay in metabolism and vascular functions, Dr. Weinstein said.
She had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
TORONTO – Nonalcoholic fatty liver disease seems to accelerate physical brain aging by up to 7 years, according to a new subanalysis of the ongoing Framingham Heart Study.
However, while finding that the liver disorder directly endangers brains, the study also offers hope, Galit Weinstein, PhD, said at the Alzheimer’s Association International Conference 2016. “If indeed nonalcoholic fatty liver disease is a risk factor for brain aging and subsequent dementia, then it is a modifiable one,” said Dr. Weinstein of Boston University. “We have reason to hope that NAFLD remission could possibly improve cognitive outcomes” as patients age.
For this study, the researchers assessed the presence of NAFLD by abdominal CT scans and white-matter hyperintensities and brain volume (total, frontal, and hippocampal) by MRI. The resulting associations were then adjusted for age, sex, alcohol consumption, visceral adipose tissue, body mass index, menopausal status, systolic blood pressure, current smoking, diabetes, history of cardiovascular disease, physical activity, insulin resistance, and C-reactive protein.
There were no significant associations with white-matter hyperintensities or with hippocampal volume, but the researches did find a significant association with total brain volume: Even after adjustment for all of the covariates, patients with NAFLD had smaller-than-normal brains for their age. This can be seen as a pathologic acceleration of the brain aging process, Dr. Weinstein said.
The finding was most striking among the youngest subjects, she said, accounting for about a 7-year advance in brain aging for those younger than 60 years. Older patients with NAFLD showed about a 2-year advance in brain aging.
The effect is probably mediated by the liver’s complex interplay in metabolism and vascular functions, Dr. Weinstein said.
She had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
TORONTO – Nonalcoholic fatty liver disease seems to accelerate physical brain aging by up to 7 years, according to a new subanalysis of the ongoing Framingham Heart Study.
However, while finding that the liver disorder directly endangers brains, the study also offers hope, Galit Weinstein, PhD, said at the Alzheimer’s Association International Conference 2016. “If indeed nonalcoholic fatty liver disease is a risk factor for brain aging and subsequent dementia, then it is a modifiable one,” said Dr. Weinstein of Boston University. “We have reason to hope that NAFLD remission could possibly improve cognitive outcomes” as patients age.
For this study, the researchers assessed the presence of NAFLD by abdominal CT scans and white-matter hyperintensities and brain volume (total, frontal, and hippocampal) by MRI. The resulting associations were then adjusted for age, sex, alcohol consumption, visceral adipose tissue, body mass index, menopausal status, systolic blood pressure, current smoking, diabetes, history of cardiovascular disease, physical activity, insulin resistance, and C-reactive protein.
There were no significant associations with white-matter hyperintensities or with hippocampal volume, but the researches did find a significant association with total brain volume: Even after adjustment for all of the covariates, patients with NAFLD had smaller-than-normal brains for their age. This can be seen as a pathologic acceleration of the brain aging process, Dr. Weinstein said.
The finding was most striking among the youngest subjects, she said, accounting for about a 7-year advance in brain aging for those younger than 60 years. Older patients with NAFLD showed about a 2-year advance in brain aging.
The effect is probably mediated by the liver’s complex interplay in metabolism and vascular functions, Dr. Weinstein said.
She had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
AT AAIC 2016
Key clinical point:
Major finding: NAFLD was associated with a 7-year advance in brain aging in people younger than 60 years.
Data source: An analysis of 906 members of the Framingham Offspring Cohort.
Disclosures: Dr. Weinstein had no financial declarations.
The Liver Meeting 2016 debrief – key abstracts
BOSTON – Amid a plethora of quality research, several abstracts stood out at the annual meeting of the American Association for the Study of Liver Diseases, Arun J. Sanyal, MD, said during the final debrief.
He focused first on nonalcoholic fatty liver disease (NAFLD), which has lacked rigorous studies of disease evolution. Consequently, “current therapeutic development is based on small retrospective data sets with heterogenous populations,” Dr. Sanyal said. Therefore, he and his associates correlated serial biopsies with clinical data (abstract 37). The results confirmed the waxing and waning nature of NAFLD and linked regressing or progressive fibrosis to several factors, including NAFLD Disease Activity score (NAS). NAFLD and nonalcoholic steatohepatitis (NASH) are “not two different diseases, it’s the same disease,” Dr. Sanyal said. “Establishing disease activity as a driver of disease progression is highly relevant for development of noninvasive biomarkers, and also gives us a foundation for the development of clinical trials in this space.”
Several studies of NASH biomarkers yielded notable results at the meeting. In the largest study to date of circulating microRNAs as markers of NASH, (LB2) the miRNAs 34a, 122a, and 200a distinguished patients with and without NAS scores of at least 4 and at least stage 2 fibrosis with areas under the receiver operating characteristic curve (AUROC) between 0.59 and 0.80. “MicroRNAs appear promising, but likely need to be combined with additional biomarkers,” Dr. Sanyal said.
He also noted a study (abstract 40) in which metabolomics of liquid biopsies comprehensively evaluated NAFLD, including fibrosis stage, with AUROCs up to 0.95. Metabolomics “holds promise as a diagnostic tool that can be operationalized for point-of-care testing,” he said.
When it comes to NAFLD, hepatologists “often struggle with what to tell our patients about alcohol,” Dr. Sanyal said. To help clarify the issue, abstract 31 compared NAFLD patients who did or did not report habitually consuming up to two drinks a day in formal prospective questionnaires. After adjustment for baseline histology, abstainers and modest drinkers did not differ on any measure of histologic change, except that abstainers had a greater decrease in steatosis on follow-up biopsy. These findings negate several retrospective studies by suggesting that alcohol consumption does not positively affect the trajectory of NAFLD, Dr. Sanyal concluded.
Many new compounds for treating NASH are in early development, he noted. Among those further along the pipeline, the immunomodulator and CCR2/CCR5 inhibitor cenicriviroc (CVC) missed its primary endpoint (improved NAS and no worsening of fibrosis) but was associated with significantly improved fibrosis without worsening of NASH in the phase 2b CENTAUR study (LB1).
“We also saw highly promising evidence for the effects of ASK1 [apoptosis signal regulating kinase] inhibition on hepatic fibrosis and disease activity in NASH,” Dr. Sanyal added. In a randomized phase II trial (LB3), the ASK1 inhibitor GS-4997 was associated with significant improvement in fibrosis without worsening of NASH when given in combination with simtuzumab, and also improved liver stiffness and magnetic resonance imaging–estimated proton density fat fraction (MRI-PDFF). “These very promising and exciting results need confirmation in more advanced, placebo-controlled trials,” Dr. Sanyal said.
Studies of alcohol use disorders of the liver confirmed that prednisolone has marginal benefits, that the benefits of steroids in general are offset by sepsis, and that pentoxifylline produced no mortality benefit, Dr. Sanyal noted. In studies of primary biliary cirrhosis, the farnesoid-X receptor agonist obeticholic acid (OCA), which was approved by the Food and Drug Administration in 2016, was associated with significantly improved AST to Platelet Ratio Index (APRI) and liver stiffness measures by transient elastography at doses of 10 mg or titrated from 5 mg to 10 mg, with or without ursodeoxycholic acid (abstract 209). In another study, patients with PBC who received norUDCA, a side chain–shortened version of UDCA, experienced decreases in serum ALP levels that were dose dependent and differed significantly from trends in the placebo group (abstract 210).
In another study, the investigational ileal bile acid transporter inhibitor GSK2330672 was associated with significant reductions in itch, compared with placebo, and with lower serum bile acids among pruritic PBC patients (abstract 205). Treatment was associated with diarrhea, but it was usually mild and transient.
Dr. Sanyal concluded by reviewing several studies of cirrhosis and hepatic encephalopathy. In a prospective randomized controlled trial (abstract 247), lactulose with albumin significantly outperformed lactulose monotherapy for reversing hepatic encephalopathy, reducing hospital stays, and preventing mortality, especially sepsis-related death.
In another multicenter, 24-week, phase IV open-label study (abstract 248), 25% of patients experienced breakthrough hepatic encephalopathy when treated with rifaximin monotherapy, compared with only 14% of patients who received both rifaximin and lactulose.
Finally, in a phase II trial (abstract 2064), rifaximin immediate-release (40 mg) significantly outperformed placebo in terms of cirrhosis-related mortality, hospitalizations for cirrhosis, and breakthrough hepatic encephalopathy. The takeaways? “Use albumin with lactulose for acute hepatic encephalopathy,” Dr. Sanyal said. “Rifaximin with lactulose is better than rifaximin alone for secondary prophylaxis, and rifaximin immediate-release may decrease the need for hospitalization and the first bout of hepatic encephalopathy.”
The Liver Meeting next convenes October 20-24, 2017, in Washington, D.C.
Dr. Sanyal disclosed ties to Genfit, NewCo, Akarna, Elsevier, UptoDate, Novartis, Pfizer, Lilly, Astra Zeneca, and a number of other companies.
BOSTON – Amid a plethora of quality research, several abstracts stood out at the annual meeting of the American Association for the Study of Liver Diseases, Arun J. Sanyal, MD, said during the final debrief.
He focused first on nonalcoholic fatty liver disease (NAFLD), which has lacked rigorous studies of disease evolution. Consequently, “current therapeutic development is based on small retrospective data sets with heterogenous populations,” Dr. Sanyal said. Therefore, he and his associates correlated serial biopsies with clinical data (abstract 37). The results confirmed the waxing and waning nature of NAFLD and linked regressing or progressive fibrosis to several factors, including NAFLD Disease Activity score (NAS). NAFLD and nonalcoholic steatohepatitis (NASH) are “not two different diseases, it’s the same disease,” Dr. Sanyal said. “Establishing disease activity as a driver of disease progression is highly relevant for development of noninvasive biomarkers, and also gives us a foundation for the development of clinical trials in this space.”
Several studies of NASH biomarkers yielded notable results at the meeting. In the largest study to date of circulating microRNAs as markers of NASH, (LB2) the miRNAs 34a, 122a, and 200a distinguished patients with and without NAS scores of at least 4 and at least stage 2 fibrosis with areas under the receiver operating characteristic curve (AUROC) between 0.59 and 0.80. “MicroRNAs appear promising, but likely need to be combined with additional biomarkers,” Dr. Sanyal said.
He also noted a study (abstract 40) in which metabolomics of liquid biopsies comprehensively evaluated NAFLD, including fibrosis stage, with AUROCs up to 0.95. Metabolomics “holds promise as a diagnostic tool that can be operationalized for point-of-care testing,” he said.
When it comes to NAFLD, hepatologists “often struggle with what to tell our patients about alcohol,” Dr. Sanyal said. To help clarify the issue, abstract 31 compared NAFLD patients who did or did not report habitually consuming up to two drinks a day in formal prospective questionnaires. After adjustment for baseline histology, abstainers and modest drinkers did not differ on any measure of histologic change, except that abstainers had a greater decrease in steatosis on follow-up biopsy. These findings negate several retrospective studies by suggesting that alcohol consumption does not positively affect the trajectory of NAFLD, Dr. Sanyal concluded.
Many new compounds for treating NASH are in early development, he noted. Among those further along the pipeline, the immunomodulator and CCR2/CCR5 inhibitor cenicriviroc (CVC) missed its primary endpoint (improved NAS and no worsening of fibrosis) but was associated with significantly improved fibrosis without worsening of NASH in the phase 2b CENTAUR study (LB1).
“We also saw highly promising evidence for the effects of ASK1 [apoptosis signal regulating kinase] inhibition on hepatic fibrosis and disease activity in NASH,” Dr. Sanyal added. In a randomized phase II trial (LB3), the ASK1 inhibitor GS-4997 was associated with significant improvement in fibrosis without worsening of NASH when given in combination with simtuzumab, and also improved liver stiffness and magnetic resonance imaging–estimated proton density fat fraction (MRI-PDFF). “These very promising and exciting results need confirmation in more advanced, placebo-controlled trials,” Dr. Sanyal said.
Studies of alcohol use disorders of the liver confirmed that prednisolone has marginal benefits, that the benefits of steroids in general are offset by sepsis, and that pentoxifylline produced no mortality benefit, Dr. Sanyal noted. In studies of primary biliary cirrhosis, the farnesoid-X receptor agonist obeticholic acid (OCA), which was approved by the Food and Drug Administration in 2016, was associated with significantly improved AST to Platelet Ratio Index (APRI) and liver stiffness measures by transient elastography at doses of 10 mg or titrated from 5 mg to 10 mg, with or without ursodeoxycholic acid (abstract 209). In another study, patients with PBC who received norUDCA, a side chain–shortened version of UDCA, experienced decreases in serum ALP levels that were dose dependent and differed significantly from trends in the placebo group (abstract 210).
In another study, the investigational ileal bile acid transporter inhibitor GSK2330672 was associated with significant reductions in itch, compared with placebo, and with lower serum bile acids among pruritic PBC patients (abstract 205). Treatment was associated with diarrhea, but it was usually mild and transient.
Dr. Sanyal concluded by reviewing several studies of cirrhosis and hepatic encephalopathy. In a prospective randomized controlled trial (abstract 247), lactulose with albumin significantly outperformed lactulose monotherapy for reversing hepatic encephalopathy, reducing hospital stays, and preventing mortality, especially sepsis-related death.
In another multicenter, 24-week, phase IV open-label study (abstract 248), 25% of patients experienced breakthrough hepatic encephalopathy when treated with rifaximin monotherapy, compared with only 14% of patients who received both rifaximin and lactulose.
Finally, in a phase II trial (abstract 2064), rifaximin immediate-release (40 mg) significantly outperformed placebo in terms of cirrhosis-related mortality, hospitalizations for cirrhosis, and breakthrough hepatic encephalopathy. The takeaways? “Use albumin with lactulose for acute hepatic encephalopathy,” Dr. Sanyal said. “Rifaximin with lactulose is better than rifaximin alone for secondary prophylaxis, and rifaximin immediate-release may decrease the need for hospitalization and the first bout of hepatic encephalopathy.”
The Liver Meeting next convenes October 20-24, 2017, in Washington, D.C.
Dr. Sanyal disclosed ties to Genfit, NewCo, Akarna, Elsevier, UptoDate, Novartis, Pfizer, Lilly, Astra Zeneca, and a number of other companies.
BOSTON – Amid a plethora of quality research, several abstracts stood out at the annual meeting of the American Association for the Study of Liver Diseases, Arun J. Sanyal, MD, said during the final debrief.
He focused first on nonalcoholic fatty liver disease (NAFLD), which has lacked rigorous studies of disease evolution. Consequently, “current therapeutic development is based on small retrospective data sets with heterogenous populations,” Dr. Sanyal said. Therefore, he and his associates correlated serial biopsies with clinical data (abstract 37). The results confirmed the waxing and waning nature of NAFLD and linked regressing or progressive fibrosis to several factors, including NAFLD Disease Activity score (NAS). NAFLD and nonalcoholic steatohepatitis (NASH) are “not two different diseases, it’s the same disease,” Dr. Sanyal said. “Establishing disease activity as a driver of disease progression is highly relevant for development of noninvasive biomarkers, and also gives us a foundation for the development of clinical trials in this space.”
Several studies of NASH biomarkers yielded notable results at the meeting. In the largest study to date of circulating microRNAs as markers of NASH, (LB2) the miRNAs 34a, 122a, and 200a distinguished patients with and without NAS scores of at least 4 and at least stage 2 fibrosis with areas under the receiver operating characteristic curve (AUROC) between 0.59 and 0.80. “MicroRNAs appear promising, but likely need to be combined with additional biomarkers,” Dr. Sanyal said.
He also noted a study (abstract 40) in which metabolomics of liquid biopsies comprehensively evaluated NAFLD, including fibrosis stage, with AUROCs up to 0.95. Metabolomics “holds promise as a diagnostic tool that can be operationalized for point-of-care testing,” he said.
When it comes to NAFLD, hepatologists “often struggle with what to tell our patients about alcohol,” Dr. Sanyal said. To help clarify the issue, abstract 31 compared NAFLD patients who did or did not report habitually consuming up to two drinks a day in formal prospective questionnaires. After adjustment for baseline histology, abstainers and modest drinkers did not differ on any measure of histologic change, except that abstainers had a greater decrease in steatosis on follow-up biopsy. These findings negate several retrospective studies by suggesting that alcohol consumption does not positively affect the trajectory of NAFLD, Dr. Sanyal concluded.
Many new compounds for treating NASH are in early development, he noted. Among those further along the pipeline, the immunomodulator and CCR2/CCR5 inhibitor cenicriviroc (CVC) missed its primary endpoint (improved NAS and no worsening of fibrosis) but was associated with significantly improved fibrosis without worsening of NASH in the phase 2b CENTAUR study (LB1).
“We also saw highly promising evidence for the effects of ASK1 [apoptosis signal regulating kinase] inhibition on hepatic fibrosis and disease activity in NASH,” Dr. Sanyal added. In a randomized phase II trial (LB3), the ASK1 inhibitor GS-4997 was associated with significant improvement in fibrosis without worsening of NASH when given in combination with simtuzumab, and also improved liver stiffness and magnetic resonance imaging–estimated proton density fat fraction (MRI-PDFF). “These very promising and exciting results need confirmation in more advanced, placebo-controlled trials,” Dr. Sanyal said.
Studies of alcohol use disorders of the liver confirmed that prednisolone has marginal benefits, that the benefits of steroids in general are offset by sepsis, and that pentoxifylline produced no mortality benefit, Dr. Sanyal noted. In studies of primary biliary cirrhosis, the farnesoid-X receptor agonist obeticholic acid (OCA), which was approved by the Food and Drug Administration in 2016, was associated with significantly improved AST to Platelet Ratio Index (APRI) and liver stiffness measures by transient elastography at doses of 10 mg or titrated from 5 mg to 10 mg, with or without ursodeoxycholic acid (abstract 209). In another study, patients with PBC who received norUDCA, a side chain–shortened version of UDCA, experienced decreases in serum ALP levels that were dose dependent and differed significantly from trends in the placebo group (abstract 210).
In another study, the investigational ileal bile acid transporter inhibitor GSK2330672 was associated with significant reductions in itch, compared with placebo, and with lower serum bile acids among pruritic PBC patients (abstract 205). Treatment was associated with diarrhea, but it was usually mild and transient.
Dr. Sanyal concluded by reviewing several studies of cirrhosis and hepatic encephalopathy. In a prospective randomized controlled trial (abstract 247), lactulose with albumin significantly outperformed lactulose monotherapy for reversing hepatic encephalopathy, reducing hospital stays, and preventing mortality, especially sepsis-related death.
In another multicenter, 24-week, phase IV open-label study (abstract 248), 25% of patients experienced breakthrough hepatic encephalopathy when treated with rifaximin monotherapy, compared with only 14% of patients who received both rifaximin and lactulose.
Finally, in a phase II trial (abstract 2064), rifaximin immediate-release (40 mg) significantly outperformed placebo in terms of cirrhosis-related mortality, hospitalizations for cirrhosis, and breakthrough hepatic encephalopathy. The takeaways? “Use albumin with lactulose for acute hepatic encephalopathy,” Dr. Sanyal said. “Rifaximin with lactulose is better than rifaximin alone for secondary prophylaxis, and rifaximin immediate-release may decrease the need for hospitalization and the first bout of hepatic encephalopathy.”
The Liver Meeting next convenes October 20-24, 2017, in Washington, D.C.
Dr. Sanyal disclosed ties to Genfit, NewCo, Akarna, Elsevier, UptoDate, Novartis, Pfizer, Lilly, Astra Zeneca, and a number of other companies.
AT THE LIVER MEETING 2016
VIDEO: Hepato-adrenal syndrome is an under-recognized source of ICU morbidity
BOSTON – Patients with serious liver disease who also had hepato-adrenal syndrome had significantly longer hospital stays; these patients had significantly longer ICU courses as well.
According to a recent study of this under-recognized syndrome, patients with cirrhosis, acute liver failure, or acute liver injury who also had clinically significant adrenocortical dysfunction had longer hospital stays when compared to patients without hepato-adrenal syndrome (HAS).
Presenting the study findings at a poster session at the annual meeting of the American Association for the Study of Liver Disease, Christina Lindenmeyer, MD, and her associates noted that the longer stays for HAS patients with serious liver disease held true even after adjustment for gender, blood glucose levels, and Child-Pugh score (median 29 days, HAS; 17 days, non-HAS; P = .001).
Further, the patients with HAS were more likely to have a prolonged ICU stay, after multivariable analysis adjusted for a variety of factors including the need for mechanical ventilation, age, bilirubin level, Model for End-stage Liver Disease (MELD) score, and severity of encephalopathy (13.5 vs. 4.9 days; P = .002).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Patients with cirrhosis commonly have hypotension, and I think it’s underrecognized that the elevated levels of endotoxin and the low levels of lipoprotein circulating in patients with cirrhosis can lead to adrenocortical dysfunction,” Dr. Lindenmeyer said in a video interview.
The single-center study enrolled ICU patients with cirrhosis, acute liver injury, and/or acute liver failure who had random cortisol or adrenocorticotropin-releasing hormone (ACTH) stimulation test results. From 2008 to 2014, the tertiary care center saw 69 patients meeting these criteria; 32 patients (46%) had HAS. The mean age was 57.4 years, and 63.8% of enrolled patients were male. There were no significant differences in these demographics between the groups. Serum bicarbonate was higher in patients with HAS (21.4 vs. 17.5 mEq/L; P = .020); other blood chemistries, mean arterial pressures, and the MELD and Child-Pugh scores did not differ significantly between groups.
Dr. Lindenmeyer, a fellow in the Cleveland Clinic’s department of gastroenterology and hepatology, said that the accepted definition of HAS is a random cortisol level of less than 15 mcg/dL in “patients who were highly stressed in the ICU, typically with respiratory failure or hypotension,” she said. For non-ICU patients, the random cortisol level should be less than 20 mcg/dL. An alternative criterion is a post-ACTH stimulation test cortisol level of less than 20 mcg/dL.
Though there was no statistically significant difference between in-hospital mortality for those patients meeting HAS criteria, the trend was actually for those patients to have lower in-hospital mortality (44% vs. 51%; P = .53). This was true even after correction for MELD scores and serum potassium levels. Dr. Lindenmeyer said these results were “a little surprising,” and noted that the study didn’t examine 90-day or 1-year mortality. “That would be something interesting to look at,” she said.
“Early recognition and treatment of HAS may improve judicious allocation of critical care and hospital resources,” wrote Dr. Lindenmeyer and her colleagues.
Dr. Lindenmeyer reported no conflicts of interest, and there were no outside sources of funding reported.
[email protected]
On Twitter @karioakes
BOSTON – Patients with serious liver disease who also had hepato-adrenal syndrome had significantly longer hospital stays; these patients had significantly longer ICU courses as well.
According to a recent study of this under-recognized syndrome, patients with cirrhosis, acute liver failure, or acute liver injury who also had clinically significant adrenocortical dysfunction had longer hospital stays when compared to patients without hepato-adrenal syndrome (HAS).
Presenting the study findings at a poster session at the annual meeting of the American Association for the Study of Liver Disease, Christina Lindenmeyer, MD, and her associates noted that the longer stays for HAS patients with serious liver disease held true even after adjustment for gender, blood glucose levels, and Child-Pugh score (median 29 days, HAS; 17 days, non-HAS; P = .001).
Further, the patients with HAS were more likely to have a prolonged ICU stay, after multivariable analysis adjusted for a variety of factors including the need for mechanical ventilation, age, bilirubin level, Model for End-stage Liver Disease (MELD) score, and severity of encephalopathy (13.5 vs. 4.9 days; P = .002).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Patients with cirrhosis commonly have hypotension, and I think it’s underrecognized that the elevated levels of endotoxin and the low levels of lipoprotein circulating in patients with cirrhosis can lead to adrenocortical dysfunction,” Dr. Lindenmeyer said in a video interview.
The single-center study enrolled ICU patients with cirrhosis, acute liver injury, and/or acute liver failure who had random cortisol or adrenocorticotropin-releasing hormone (ACTH) stimulation test results. From 2008 to 2014, the tertiary care center saw 69 patients meeting these criteria; 32 patients (46%) had HAS. The mean age was 57.4 years, and 63.8% of enrolled patients were male. There were no significant differences in these demographics between the groups. Serum bicarbonate was higher in patients with HAS (21.4 vs. 17.5 mEq/L; P = .020); other blood chemistries, mean arterial pressures, and the MELD and Child-Pugh scores did not differ significantly between groups.
Dr. Lindenmeyer, a fellow in the Cleveland Clinic’s department of gastroenterology and hepatology, said that the accepted definition of HAS is a random cortisol level of less than 15 mcg/dL in “patients who were highly stressed in the ICU, typically with respiratory failure or hypotension,” she said. For non-ICU patients, the random cortisol level should be less than 20 mcg/dL. An alternative criterion is a post-ACTH stimulation test cortisol level of less than 20 mcg/dL.
Though there was no statistically significant difference between in-hospital mortality for those patients meeting HAS criteria, the trend was actually for those patients to have lower in-hospital mortality (44% vs. 51%; P = .53). This was true even after correction for MELD scores and serum potassium levels. Dr. Lindenmeyer said these results were “a little surprising,” and noted that the study didn’t examine 90-day or 1-year mortality. “That would be something interesting to look at,” she said.
“Early recognition and treatment of HAS may improve judicious allocation of critical care and hospital resources,” wrote Dr. Lindenmeyer and her colleagues.
Dr. Lindenmeyer reported no conflicts of interest, and there were no outside sources of funding reported.
[email protected]
On Twitter @karioakes
BOSTON – Patients with serious liver disease who also had hepato-adrenal syndrome had significantly longer hospital stays; these patients had significantly longer ICU courses as well.
According to a recent study of this under-recognized syndrome, patients with cirrhosis, acute liver failure, or acute liver injury who also had clinically significant adrenocortical dysfunction had longer hospital stays when compared to patients without hepato-adrenal syndrome (HAS).
Presenting the study findings at a poster session at the annual meeting of the American Association for the Study of Liver Disease, Christina Lindenmeyer, MD, and her associates noted that the longer stays for HAS patients with serious liver disease held true even after adjustment for gender, blood glucose levels, and Child-Pugh score (median 29 days, HAS; 17 days, non-HAS; P = .001).
Further, the patients with HAS were more likely to have a prolonged ICU stay, after multivariable analysis adjusted for a variety of factors including the need for mechanical ventilation, age, bilirubin level, Model for End-stage Liver Disease (MELD) score, and severity of encephalopathy (13.5 vs. 4.9 days; P = .002).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Patients with cirrhosis commonly have hypotension, and I think it’s underrecognized that the elevated levels of endotoxin and the low levels of lipoprotein circulating in patients with cirrhosis can lead to adrenocortical dysfunction,” Dr. Lindenmeyer said in a video interview.
The single-center study enrolled ICU patients with cirrhosis, acute liver injury, and/or acute liver failure who had random cortisol or adrenocorticotropin-releasing hormone (ACTH) stimulation test results. From 2008 to 2014, the tertiary care center saw 69 patients meeting these criteria; 32 patients (46%) had HAS. The mean age was 57.4 years, and 63.8% of enrolled patients were male. There were no significant differences in these demographics between the groups. Serum bicarbonate was higher in patients with HAS (21.4 vs. 17.5 mEq/L; P = .020); other blood chemistries, mean arterial pressures, and the MELD and Child-Pugh scores did not differ significantly between groups.
Dr. Lindenmeyer, a fellow in the Cleveland Clinic’s department of gastroenterology and hepatology, said that the accepted definition of HAS is a random cortisol level of less than 15 mcg/dL in “patients who were highly stressed in the ICU, typically with respiratory failure or hypotension,” she said. For non-ICU patients, the random cortisol level should be less than 20 mcg/dL. An alternative criterion is a post-ACTH stimulation test cortisol level of less than 20 mcg/dL.
Though there was no statistically significant difference between in-hospital mortality for those patients meeting HAS criteria, the trend was actually for those patients to have lower in-hospital mortality (44% vs. 51%; P = .53). This was true even after correction for MELD scores and serum potassium levels. Dr. Lindenmeyer said these results were “a little surprising,” and noted that the study didn’t examine 90-day or 1-year mortality. “That would be something interesting to look at,” she said.
“Early recognition and treatment of HAS may improve judicious allocation of critical care and hospital resources,” wrote Dr. Lindenmeyer and her colleagues.
Dr. Lindenmeyer reported no conflicts of interest, and there were no outside sources of funding reported.
[email protected]
On Twitter @karioakes
AT THE LIVER MEETING 2016
Key clinical point:
Major finding: Patients with HAS had a longer length of hospital stay (median 29 days, HAS; 17 days, non-HAS; P = .001)
Data source: Single-center study of 69 consecutively enrolled ICU patients with serious liver disease and random cortisol or adrenocorticotropin-releasing hormone results.
Disclosures: The study investigators reported no disclosures, and no external sources of funding.