User login
Plerixafor doesn’t overcome HPC failure in R-hyperCVAD for mantle cell lymphoma
A commonly-used intensive induction regimen was associated with higher rates of hematopoietic progenitor cell mobilization failure in patients with mantle cell lymphoma, even when plerixafor rescue was attempted, based on a study by Amandeep Salhotra, MD, and his colleagues at City of Hope, Duarte, Calif.
Patients who received rituximab and hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (R-hyperCVAD) in the era after plerixafor came into use experienced significantly higher rates of peripheral blood stem cell (PBSC) collection failure than did patients receiving other induction regimens (17% vs. 4% failure rate, P = .04).
“Plerixafor does not overcome the negative impact of R-hyperCVAD on PBSC mobilization, and caution is warranted in using R-hyperCVAD in patients with newly diagnosed MCL who are candidates for ASCT (autologous stem cell transplant),” wrote Dr. Salhotra and his colleagues.
The higher rate of hematopoietic progenitor cell collection failure for R-hyperCVAD patients could not be attributed to their age at time of mantle cell lymphoma diagnosis or to the amount of time between diagnosis and collection.
Treatment records for 181 consecutive mantle cell lymphoma patients were examined for a 10 year period in the retrospective single-site study. Plerixafor, a C-X-C chemokine receptor agonist that reduces hematopoietic progenitor cells’ ability to bind to bone marrow stroma, was introduced on August 16, 2009; a total of 71 patients were treated before this point, and 110 were treated afterward.
The R-hyperCVAD regimen was received by 34 pre-plerixafor patients (45%) and by 42 of the post-plerixafor era patients (55%). Other regimens were received by 37 (35%) and 68 (65%) of the pre- and post-plerixafor era patients, respectively.
Before plerixafor came into use, Dr. Salhotra, of City of Hope’s department of hematology and hematopoietic cell transplantation, and his coinvestigators saw no significant difference among their study population in the rates of PBSC collection failure between those receiving R-hyperCVAD (11%) and those receiving other regimens (12%). The findings were reported in Biology of Blood and Marrow Transplantation.
The study was conducted in the context of other recent work that showed higher rates of PBSC collection failure and fewer CD34+ cells collected with the use of an R-hyperCVAD conditioning regimen. The fact that PBSC mobilization rates were significantly lower in R-hyperCVAD patients post-plerixafor surprised the investigators, who had hypothesized that the use of plerixafor would overcome PBSC mobilization failures without regard to the conditioning regimen used.
“It may be worthwhile to consider using a more aggressive strategy for [hematopoetic progenitor cell] mobilization in patients who have received R-hyperCVAD chemotherapy upfront or as salvage for aggressive lymphomas,” the researchers wrote. This might include the use of plerixafor upfront when patients have low CD34 counts before apheresis.
The researchers plan to examine their data to see how the choice of induction regimen and plerixafor usage impact patient survival.
The study authors reported no conflicts of interest.
Source: Amandeep Salhotra, et al. Hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone chemotherapy in mantle cell lymphoma patients is associated with higher rates of hematopoietic progenitor cell mobilization failure despite plerixafor rescue. Biol Blood Marrow Transplant 2017; 23:1264-1268.
SOURCE: Biol Blood Marrow Transplant 2017; 23:1264-1268. http://dx.doi.org/10.1016/j.bbmt.2017.04.011
A commonly-used intensive induction regimen was associated with higher rates of hematopoietic progenitor cell mobilization failure in patients with mantle cell lymphoma, even when plerixafor rescue was attempted, based on a study by Amandeep Salhotra, MD, and his colleagues at City of Hope, Duarte, Calif.
Patients who received rituximab and hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (R-hyperCVAD) in the era after plerixafor came into use experienced significantly higher rates of peripheral blood stem cell (PBSC) collection failure than did patients receiving other induction regimens (17% vs. 4% failure rate, P = .04).
“Plerixafor does not overcome the negative impact of R-hyperCVAD on PBSC mobilization, and caution is warranted in using R-hyperCVAD in patients with newly diagnosed MCL who are candidates for ASCT (autologous stem cell transplant),” wrote Dr. Salhotra and his colleagues.
The higher rate of hematopoietic progenitor cell collection failure for R-hyperCVAD patients could not be attributed to their age at time of mantle cell lymphoma diagnosis or to the amount of time between diagnosis and collection.
Treatment records for 181 consecutive mantle cell lymphoma patients were examined for a 10 year period in the retrospective single-site study. Plerixafor, a C-X-C chemokine receptor agonist that reduces hematopoietic progenitor cells’ ability to bind to bone marrow stroma, was introduced on August 16, 2009; a total of 71 patients were treated before this point, and 110 were treated afterward.
The R-hyperCVAD regimen was received by 34 pre-plerixafor patients (45%) and by 42 of the post-plerixafor era patients (55%). Other regimens were received by 37 (35%) and 68 (65%) of the pre- and post-plerixafor era patients, respectively.
Before plerixafor came into use, Dr. Salhotra, of City of Hope’s department of hematology and hematopoietic cell transplantation, and his coinvestigators saw no significant difference among their study population in the rates of PBSC collection failure between those receiving R-hyperCVAD (11%) and those receiving other regimens (12%). The findings were reported in Biology of Blood and Marrow Transplantation.
The study was conducted in the context of other recent work that showed higher rates of PBSC collection failure and fewer CD34+ cells collected with the use of an R-hyperCVAD conditioning regimen. The fact that PBSC mobilization rates were significantly lower in R-hyperCVAD patients post-plerixafor surprised the investigators, who had hypothesized that the use of plerixafor would overcome PBSC mobilization failures without regard to the conditioning regimen used.
“It may be worthwhile to consider using a more aggressive strategy for [hematopoetic progenitor cell] mobilization in patients who have received R-hyperCVAD chemotherapy upfront or as salvage for aggressive lymphomas,” the researchers wrote. This might include the use of plerixafor upfront when patients have low CD34 counts before apheresis.
The researchers plan to examine their data to see how the choice of induction regimen and plerixafor usage impact patient survival.
The study authors reported no conflicts of interest.
Source: Amandeep Salhotra, et al. Hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone chemotherapy in mantle cell lymphoma patients is associated with higher rates of hematopoietic progenitor cell mobilization failure despite plerixafor rescue. Biol Blood Marrow Transplant 2017; 23:1264-1268.
SOURCE: Biol Blood Marrow Transplant 2017; 23:1264-1268. http://dx.doi.org/10.1016/j.bbmt.2017.04.011
A commonly-used intensive induction regimen was associated with higher rates of hematopoietic progenitor cell mobilization failure in patients with mantle cell lymphoma, even when plerixafor rescue was attempted, based on a study by Amandeep Salhotra, MD, and his colleagues at City of Hope, Duarte, Calif.
Patients who received rituximab and hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (R-hyperCVAD) in the era after plerixafor came into use experienced significantly higher rates of peripheral blood stem cell (PBSC) collection failure than did patients receiving other induction regimens (17% vs. 4% failure rate, P = .04).
“Plerixafor does not overcome the negative impact of R-hyperCVAD on PBSC mobilization, and caution is warranted in using R-hyperCVAD in patients with newly diagnosed MCL who are candidates for ASCT (autologous stem cell transplant),” wrote Dr. Salhotra and his colleagues.
The higher rate of hematopoietic progenitor cell collection failure for R-hyperCVAD patients could not be attributed to their age at time of mantle cell lymphoma diagnosis or to the amount of time between diagnosis and collection.
Treatment records for 181 consecutive mantle cell lymphoma patients were examined for a 10 year period in the retrospective single-site study. Plerixafor, a C-X-C chemokine receptor agonist that reduces hematopoietic progenitor cells’ ability to bind to bone marrow stroma, was introduced on August 16, 2009; a total of 71 patients were treated before this point, and 110 were treated afterward.
The R-hyperCVAD regimen was received by 34 pre-plerixafor patients (45%) and by 42 of the post-plerixafor era patients (55%). Other regimens were received by 37 (35%) and 68 (65%) of the pre- and post-plerixafor era patients, respectively.
Before plerixafor came into use, Dr. Salhotra, of City of Hope’s department of hematology and hematopoietic cell transplantation, and his coinvestigators saw no significant difference among their study population in the rates of PBSC collection failure between those receiving R-hyperCVAD (11%) and those receiving other regimens (12%). The findings were reported in Biology of Blood and Marrow Transplantation.
The study was conducted in the context of other recent work that showed higher rates of PBSC collection failure and fewer CD34+ cells collected with the use of an R-hyperCVAD conditioning regimen. The fact that PBSC mobilization rates were significantly lower in R-hyperCVAD patients post-plerixafor surprised the investigators, who had hypothesized that the use of plerixafor would overcome PBSC mobilization failures without regard to the conditioning regimen used.
“It may be worthwhile to consider using a more aggressive strategy for [hematopoetic progenitor cell] mobilization in patients who have received R-hyperCVAD chemotherapy upfront or as salvage for aggressive lymphomas,” the researchers wrote. This might include the use of plerixafor upfront when patients have low CD34 counts before apheresis.
The researchers plan to examine their data to see how the choice of induction regimen and plerixafor usage impact patient survival.
The study authors reported no conflicts of interest.
Source: Amandeep Salhotra, et al. Hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone chemotherapy in mantle cell lymphoma patients is associated with higher rates of hematopoietic progenitor cell mobilization failure despite plerixafor rescue. Biol Blood Marrow Transplant 2017; 23:1264-1268.
SOURCE: Biol Blood Marrow Transplant 2017; 23:1264-1268. http://dx.doi.org/10.1016/j.bbmt.2017.04.011
FROM BIOLOGY OF BLOOD AND MARROW TRANSPLANTATION
Key clinical point: R-hyperCVAD was associated with increased peripheral blood stem cell (PBSC) collection failure in the post-plerixafor era.
Major finding: Patients receiving R-hyperCVAD in the post-plerixafor era had a 17% PBSC collection failure rate, compared to a 4% rate for those receiving other chemotherapy (P = 0.04).
Study details: Single-center retrospective study of 181 consecutive patients with mantle cell lymphoma over a 10-year period spanning the introduction of plerixafor.
Disclosures: The study was sponsored by City of Hope and the National Cancer Institute; the authors reported no conflicts of interest.
Source: Amandeep Salhotra, et al. Hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone chemotherapy in mantle cell lymphoma patients is associated with higher rates of hematopoietic progenitor cell mobilization failure despite plerixafor rescue. Biol Blood Marrow Transplant 2017; 23:1264-1268.
FDA grants priority review of acalabrutinib for second-line treatment of MCL
The Food and Drug Administration has granted a priority review for acalabrutinib, a Bruton tyrosine kinase inhibitor, for the treatment of patients with mantle cell lymphoma (MCL) who have received at least one prior therapy.
The new drug application is based on results from the phase 2 ACE-LY-004 trial, which evaluated the safety and efficacy of acalabrutinib in patients with relapsed/refractory MCL who had received at least one prior therapy.
[email protected]
On Twitter @NikolaidesLaura
The Food and Drug Administration has granted a priority review for acalabrutinib, a Bruton tyrosine kinase inhibitor, for the treatment of patients with mantle cell lymphoma (MCL) who have received at least one prior therapy.
The new drug application is based on results from the phase 2 ACE-LY-004 trial, which evaluated the safety and efficacy of acalabrutinib in patients with relapsed/refractory MCL who had received at least one prior therapy.
[email protected]
On Twitter @NikolaidesLaura
The Food and Drug Administration has granted a priority review for acalabrutinib, a Bruton tyrosine kinase inhibitor, for the treatment of patients with mantle cell lymphoma (MCL) who have received at least one prior therapy.
The new drug application is based on results from the phase 2 ACE-LY-004 trial, which evaluated the safety and efficacy of acalabrutinib in patients with relapsed/refractory MCL who had received at least one prior therapy.
[email protected]
On Twitter @NikolaidesLaura
IMiD/Anti-CD20 combo induces complete responses in r/r NHL
Lugano, Switzerland – A combination of obinutuzumab (Gazyva) and the experimental immunomodulatory agent CC-122 showed “clinically meaningful” activity against relapsed/refractory diffuse large B cell lymphoma (DLBCL) and indolent non-Hodgkin lymphoma (NHL) in a phase 1b study.
Among 38 patients with heavily pretreated, relapsed/refractory DLBCL, follicular lymphoma (FL), or marginal zone lymphoma (MZL), the overall response rate was 66%, including 12 patients (32%) with a complete response (CR), reported Jean-Marie Michot, MD, from the Goustave-Roussy Cancer Center in Villejuif, France.
CC-122 is a thalidomide analog that shares a molecular target with its cousin lenalidomide (Revlimid). Both molecules bind to the protein cereblon to cause degradation of the lymphoid transcription factors Aiolos and Ikaros.
As a single agent, CC-122 has been shown to have immunomodulatory effects on T-cell and natural killer (NK)–cell functions and has shown clinical activity in heavily pretreated patients with relapsed refractory NHL, including various cell-of-origin–based DLBCL subtypes, Dr, Michot said.
In preclinical studies, the combination of CC-122 and obinutuzumab, an anti-CD20 monoclonal antibody, has shown synergistic effects against FL and greater antilymphoma effects against DLBCL than either agent alone, he added.
In a multicenter, open-label, phase 1b dose-escalation and expansion study, investigators enrolled 19 patients with FL or MZL for whom at least one prior regimen had failed and 19 patients with relapsed/refractory DLBCL following at least two prior regimens and failed autologous stem cell transplant.
The patients received oral CC-122 at different dose levels for 5 of 7 days in each 28 day treatment cycle, plus intravenous obinutuzumab 1000 mg on days 2, 8, and 15 of cycle 1 and day 1 of cycles 2 through 8.
Responses were assessed according to International Working Group 2007 revised response criteria for malignant lymphoma.
Among all 38 patients, 25 (66%) had a response. Responses consisted of 12 CR (3 in patients with DLBCL, and 9 in patients with FL/MZL) and 13 partial responses (six and seven patients, respectively),
The median time to best response was 57 days. Responses were seen in 23 of the 30 patients who received CC-122 at dose level of 3 mg or higher.
“To date, patients receiving CC-122 at a dose of 3 mg and higher have the best and more durable responses to CC-122 plus obinutuzumab,” Dr. Michot said.
Patients generally tolerated the combination well. The most common grade 3 or 4 adverse events were hematologic and included grade 4 febrile neutropenia in two patients. Two patients discontinued treatment because of adverse events.
There was a dose-limiting toxicity, grade 4 neutropenia in one patient who received CC-122 at the 3 mg dose level, and one death from a tumor flare reaction in a patient treated at the 4 mg dose level.
The dose-escalation arm of the study has completed, and investigators are enrolling patients in a dose expansion phase at the 3 mg level.
The study was sponsored by Celgene. Hoffman La-Roche contributed obinutuzumab for the study. Dr. Michot reported serving as an advisor to Bristol-Myers Squibb and receiving travel grants from BMS, Pfizer, and Roche. Seven coauthors are Celgene employees and stockholders.
Lugano, Switzerland – A combination of obinutuzumab (Gazyva) and the experimental immunomodulatory agent CC-122 showed “clinically meaningful” activity against relapsed/refractory diffuse large B cell lymphoma (DLBCL) and indolent non-Hodgkin lymphoma (NHL) in a phase 1b study.
Among 38 patients with heavily pretreated, relapsed/refractory DLBCL, follicular lymphoma (FL), or marginal zone lymphoma (MZL), the overall response rate was 66%, including 12 patients (32%) with a complete response (CR), reported Jean-Marie Michot, MD, from the Goustave-Roussy Cancer Center in Villejuif, France.
CC-122 is a thalidomide analog that shares a molecular target with its cousin lenalidomide (Revlimid). Both molecules bind to the protein cereblon to cause degradation of the lymphoid transcription factors Aiolos and Ikaros.
As a single agent, CC-122 has been shown to have immunomodulatory effects on T-cell and natural killer (NK)–cell functions and has shown clinical activity in heavily pretreated patients with relapsed refractory NHL, including various cell-of-origin–based DLBCL subtypes, Dr, Michot said.
In preclinical studies, the combination of CC-122 and obinutuzumab, an anti-CD20 monoclonal antibody, has shown synergistic effects against FL and greater antilymphoma effects against DLBCL than either agent alone, he added.
In a multicenter, open-label, phase 1b dose-escalation and expansion study, investigators enrolled 19 patients with FL or MZL for whom at least one prior regimen had failed and 19 patients with relapsed/refractory DLBCL following at least two prior regimens and failed autologous stem cell transplant.
The patients received oral CC-122 at different dose levels for 5 of 7 days in each 28 day treatment cycle, plus intravenous obinutuzumab 1000 mg on days 2, 8, and 15 of cycle 1 and day 1 of cycles 2 through 8.
Responses were assessed according to International Working Group 2007 revised response criteria for malignant lymphoma.
Among all 38 patients, 25 (66%) had a response. Responses consisted of 12 CR (3 in patients with DLBCL, and 9 in patients with FL/MZL) and 13 partial responses (six and seven patients, respectively),
The median time to best response was 57 days. Responses were seen in 23 of the 30 patients who received CC-122 at dose level of 3 mg or higher.
“To date, patients receiving CC-122 at a dose of 3 mg and higher have the best and more durable responses to CC-122 plus obinutuzumab,” Dr. Michot said.
Patients generally tolerated the combination well. The most common grade 3 or 4 adverse events were hematologic and included grade 4 febrile neutropenia in two patients. Two patients discontinued treatment because of adverse events.
There was a dose-limiting toxicity, grade 4 neutropenia in one patient who received CC-122 at the 3 mg dose level, and one death from a tumor flare reaction in a patient treated at the 4 mg dose level.
The dose-escalation arm of the study has completed, and investigators are enrolling patients in a dose expansion phase at the 3 mg level.
The study was sponsored by Celgene. Hoffman La-Roche contributed obinutuzumab for the study. Dr. Michot reported serving as an advisor to Bristol-Myers Squibb and receiving travel grants from BMS, Pfizer, and Roche. Seven coauthors are Celgene employees and stockholders.
Lugano, Switzerland – A combination of obinutuzumab (Gazyva) and the experimental immunomodulatory agent CC-122 showed “clinically meaningful” activity against relapsed/refractory diffuse large B cell lymphoma (DLBCL) and indolent non-Hodgkin lymphoma (NHL) in a phase 1b study.
Among 38 patients with heavily pretreated, relapsed/refractory DLBCL, follicular lymphoma (FL), or marginal zone lymphoma (MZL), the overall response rate was 66%, including 12 patients (32%) with a complete response (CR), reported Jean-Marie Michot, MD, from the Goustave-Roussy Cancer Center in Villejuif, France.
CC-122 is a thalidomide analog that shares a molecular target with its cousin lenalidomide (Revlimid). Both molecules bind to the protein cereblon to cause degradation of the lymphoid transcription factors Aiolos and Ikaros.
As a single agent, CC-122 has been shown to have immunomodulatory effects on T-cell and natural killer (NK)–cell functions and has shown clinical activity in heavily pretreated patients with relapsed refractory NHL, including various cell-of-origin–based DLBCL subtypes, Dr, Michot said.
In preclinical studies, the combination of CC-122 and obinutuzumab, an anti-CD20 monoclonal antibody, has shown synergistic effects against FL and greater antilymphoma effects against DLBCL than either agent alone, he added.
In a multicenter, open-label, phase 1b dose-escalation and expansion study, investigators enrolled 19 patients with FL or MZL for whom at least one prior regimen had failed and 19 patients with relapsed/refractory DLBCL following at least two prior regimens and failed autologous stem cell transplant.
The patients received oral CC-122 at different dose levels for 5 of 7 days in each 28 day treatment cycle, plus intravenous obinutuzumab 1000 mg on days 2, 8, and 15 of cycle 1 and day 1 of cycles 2 through 8.
Responses were assessed according to International Working Group 2007 revised response criteria for malignant lymphoma.
Among all 38 patients, 25 (66%) had a response. Responses consisted of 12 CR (3 in patients with DLBCL, and 9 in patients with FL/MZL) and 13 partial responses (six and seven patients, respectively),
The median time to best response was 57 days. Responses were seen in 23 of the 30 patients who received CC-122 at dose level of 3 mg or higher.
“To date, patients receiving CC-122 at a dose of 3 mg and higher have the best and more durable responses to CC-122 plus obinutuzumab,” Dr. Michot said.
Patients generally tolerated the combination well. The most common grade 3 or 4 adverse events were hematologic and included grade 4 febrile neutropenia in two patients. Two patients discontinued treatment because of adverse events.
There was a dose-limiting toxicity, grade 4 neutropenia in one patient who received CC-122 at the 3 mg dose level, and one death from a tumor flare reaction in a patient treated at the 4 mg dose level.
The dose-escalation arm of the study has completed, and investigators are enrolling patients in a dose expansion phase at the 3 mg level.
The study was sponsored by Celgene. Hoffman La-Roche contributed obinutuzumab for the study. Dr. Michot reported serving as an advisor to Bristol-Myers Squibb and receiving travel grants from BMS, Pfizer, and Roche. Seven coauthors are Celgene employees and stockholders.
AT 14-ICML
Key clinical point: A combination of the experimental immunomodulator CC-122 and obinutuzumab showed significant activity against relapsed/refractory non-Hodgkin lymphoma.
Major finding: The overall response rate was 66%, including 32% complete responses.
Data source: A multicenter open-label phase 1b dose-escalation study in 19 patients with DLBCL and 19 with follicular lymphoma or marginal zone lymphoma.
Disclosures: The study was sponsored by Celgene. Hoffman La-Roche contributed obinutuzumab for the study. Dr. Michot reported serving as an advisor to Bristol-Myers Squibb and receiving travel grants from BMS, Pfizer, and Roche. Seven coauthors are Celgene employees and stockholders.
Chemo-free induction in MCL keeps getting better
Lugano, Switzerland – It’s not the end of chemotherapy for young patients with newly diagnosed mantle cell lymphoma (MCL), but it’s a start.
For these patients, induction with a combination of ibrutinib and rituximab, followed by shorter cycles of chemoimmunotherapy, was associated in an early study with an objective response rate of 100%, including 90% complete responses (CR), reported Michael Wang, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“This is the first time for a chemo-free therapy – ibrutinib/rituximab – to achieve an overall response rate of 100%. This has an unprecedented efficacy in the frontline in young patients with mantle-cell lymphoma,” he said at the 14th International Congress on Malignant Lymphoma.
In patients with relapsed or refractory MCL, the combination of ibrutinib and rituximab has been associated with durable responses in 88% of patients. The success of the combination suggests that fit patients younger than age 65 years with newly diagnosed MCL might benefit from a chemotherapy-free induction regimen with ibrutinib and rituximab, followed by consolidation with a short but intense course of chemoimmunotherapy, Dr. Wang said.
He presented updated results from the phase II Window I study, first results of which were reported at the 2016 meeting of the American Society of Hematology.
“Frontline therapy is the most important therapy for mantle cell lymphoma, because mantle cell lymphoma cells are most vulnerable to frontline attack. If the frontline therapy is good enough, it could kill all the mantle cell lymphoma cells, therefore leaving no chance for secondary resistance, and thereby (resulting in) long-term survival. And it is really my belief that if we ideally optimized the frontline therapy, that would be a shortcut to a cure,” he said.
To test this idea, Dr. Wang and MD Anderson colleagues initiated a phase II trial at their institution with 50 patients age 65 years or under with newly diagnosed, CD20-positive and Cyclin D1-positive MCL.
A total of 50 patients age 65 years or younger (median age 54) with newly diagnosed, untreated MCL underwent induction with continuous daily ibrutinib 560 mg, plus rituximab 375 mg/m2 administered weekly for 4 weeks during cycle 1 and on day 1 of cycles 3-12. Consolidation consisted of rituximab plus hyper-CVAD (hyper-fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone), alternating every 28 days with rituximab plus high-dose methotrexate–cytarabine.
Patients who had complete responses to induction received four cycles of chemoimmunotherapy, while those who experienced disease progression and those who had partial responses received chemoimmunotherapy for two cycles beyond the point of complete remissions.
At the time of the presentation, all 50 patients were evaluable for the induction phase (part 2), and 47 were evaluable for both induction and consolidation (part 2) .Of the evaluable patients, the overall response rate (ORR) to chemotherapy-free induction therapy alone (Part 1 ) was 100% (50), with CR in 90% of patients and partial responses (PR) in 10%. Of the 47 patients evaluable for part 2 (chemoimmunotherapy), all had CRs, for an ORR of 100%.
Dr. Wang noted that one patient had a dramatic radiographic reduction in spleen size following just two cycles of chemotherapy-free induction, and two other patients had similar reductions after four and six cycles, respectively.
After a median follow-up of 15.9 months, neither the median duration of response, progression-free survival, nor overall survival have been reached. There have been no deaths and only one case of disease progression after one year of therapy.
The patients generally tolerated the regimen very well, Dr. Wang said. There were no cases of lymphocytosis, bleeding, or atrial fibrillation after 332 combined cycles.
Nonhematological adverse events were primarily grade 1 or 2. Grade 3 fatigue was reported in approximately 10% of patients. There were no grade 4 adverse events.
“This study may provide a window of opportunity to reduce the frontline therapies and reduce the long-term toxicities such as secondary malignancies.” Dr. Wang said.
He acknowledged that four cycles of intensive chemotherapy is still toxic and that further efforts to reduce these toxicities are needed. The investigators are currently planning the Window II study, in which a fraction of patients will be treated with no chemotherapy at all, he said.
The study was supported by Pharmacyclics and Janssen. Dr. Wang disclosed receiving research grants and honoraria and serving as a consultant for the companies.
Lugano, Switzerland – It’s not the end of chemotherapy for young patients with newly diagnosed mantle cell lymphoma (MCL), but it’s a start.
For these patients, induction with a combination of ibrutinib and rituximab, followed by shorter cycles of chemoimmunotherapy, was associated in an early study with an objective response rate of 100%, including 90% complete responses (CR), reported Michael Wang, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“This is the first time for a chemo-free therapy – ibrutinib/rituximab – to achieve an overall response rate of 100%. This has an unprecedented efficacy in the frontline in young patients with mantle-cell lymphoma,” he said at the 14th International Congress on Malignant Lymphoma.
In patients with relapsed or refractory MCL, the combination of ibrutinib and rituximab has been associated with durable responses in 88% of patients. The success of the combination suggests that fit patients younger than age 65 years with newly diagnosed MCL might benefit from a chemotherapy-free induction regimen with ibrutinib and rituximab, followed by consolidation with a short but intense course of chemoimmunotherapy, Dr. Wang said.
He presented updated results from the phase II Window I study, first results of which were reported at the 2016 meeting of the American Society of Hematology.
“Frontline therapy is the most important therapy for mantle cell lymphoma, because mantle cell lymphoma cells are most vulnerable to frontline attack. If the frontline therapy is good enough, it could kill all the mantle cell lymphoma cells, therefore leaving no chance for secondary resistance, and thereby (resulting in) long-term survival. And it is really my belief that if we ideally optimized the frontline therapy, that would be a shortcut to a cure,” he said.
To test this idea, Dr. Wang and MD Anderson colleagues initiated a phase II trial at their institution with 50 patients age 65 years or under with newly diagnosed, CD20-positive and Cyclin D1-positive MCL.
A total of 50 patients age 65 years or younger (median age 54) with newly diagnosed, untreated MCL underwent induction with continuous daily ibrutinib 560 mg, plus rituximab 375 mg/m2 administered weekly for 4 weeks during cycle 1 and on day 1 of cycles 3-12. Consolidation consisted of rituximab plus hyper-CVAD (hyper-fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone), alternating every 28 days with rituximab plus high-dose methotrexate–cytarabine.
Patients who had complete responses to induction received four cycles of chemoimmunotherapy, while those who experienced disease progression and those who had partial responses received chemoimmunotherapy for two cycles beyond the point of complete remissions.
At the time of the presentation, all 50 patients were evaluable for the induction phase (part 2), and 47 were evaluable for both induction and consolidation (part 2) .Of the evaluable patients, the overall response rate (ORR) to chemotherapy-free induction therapy alone (Part 1 ) was 100% (50), with CR in 90% of patients and partial responses (PR) in 10%. Of the 47 patients evaluable for part 2 (chemoimmunotherapy), all had CRs, for an ORR of 100%.
Dr. Wang noted that one patient had a dramatic radiographic reduction in spleen size following just two cycles of chemotherapy-free induction, and two other patients had similar reductions after four and six cycles, respectively.
After a median follow-up of 15.9 months, neither the median duration of response, progression-free survival, nor overall survival have been reached. There have been no deaths and only one case of disease progression after one year of therapy.
The patients generally tolerated the regimen very well, Dr. Wang said. There were no cases of lymphocytosis, bleeding, or atrial fibrillation after 332 combined cycles.
Nonhematological adverse events were primarily grade 1 or 2. Grade 3 fatigue was reported in approximately 10% of patients. There were no grade 4 adverse events.
“This study may provide a window of opportunity to reduce the frontline therapies and reduce the long-term toxicities such as secondary malignancies.” Dr. Wang said.
He acknowledged that four cycles of intensive chemotherapy is still toxic and that further efforts to reduce these toxicities are needed. The investigators are currently planning the Window II study, in which a fraction of patients will be treated with no chemotherapy at all, he said.
The study was supported by Pharmacyclics and Janssen. Dr. Wang disclosed receiving research grants and honoraria and serving as a consultant for the companies.
Lugano, Switzerland – It’s not the end of chemotherapy for young patients with newly diagnosed mantle cell lymphoma (MCL), but it’s a start.
For these patients, induction with a combination of ibrutinib and rituximab, followed by shorter cycles of chemoimmunotherapy, was associated in an early study with an objective response rate of 100%, including 90% complete responses (CR), reported Michael Wang, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“This is the first time for a chemo-free therapy – ibrutinib/rituximab – to achieve an overall response rate of 100%. This has an unprecedented efficacy in the frontline in young patients with mantle-cell lymphoma,” he said at the 14th International Congress on Malignant Lymphoma.
In patients with relapsed or refractory MCL, the combination of ibrutinib and rituximab has been associated with durable responses in 88% of patients. The success of the combination suggests that fit patients younger than age 65 years with newly diagnosed MCL might benefit from a chemotherapy-free induction regimen with ibrutinib and rituximab, followed by consolidation with a short but intense course of chemoimmunotherapy, Dr. Wang said.
He presented updated results from the phase II Window I study, first results of which were reported at the 2016 meeting of the American Society of Hematology.
“Frontline therapy is the most important therapy for mantle cell lymphoma, because mantle cell lymphoma cells are most vulnerable to frontline attack. If the frontline therapy is good enough, it could kill all the mantle cell lymphoma cells, therefore leaving no chance for secondary resistance, and thereby (resulting in) long-term survival. And it is really my belief that if we ideally optimized the frontline therapy, that would be a shortcut to a cure,” he said.
To test this idea, Dr. Wang and MD Anderson colleagues initiated a phase II trial at their institution with 50 patients age 65 years or under with newly diagnosed, CD20-positive and Cyclin D1-positive MCL.
A total of 50 patients age 65 years or younger (median age 54) with newly diagnosed, untreated MCL underwent induction with continuous daily ibrutinib 560 mg, plus rituximab 375 mg/m2 administered weekly for 4 weeks during cycle 1 and on day 1 of cycles 3-12. Consolidation consisted of rituximab plus hyper-CVAD (hyper-fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone), alternating every 28 days with rituximab plus high-dose methotrexate–cytarabine.
Patients who had complete responses to induction received four cycles of chemoimmunotherapy, while those who experienced disease progression and those who had partial responses received chemoimmunotherapy for two cycles beyond the point of complete remissions.
At the time of the presentation, all 50 patients were evaluable for the induction phase (part 2), and 47 were evaluable for both induction and consolidation (part 2) .Of the evaluable patients, the overall response rate (ORR) to chemotherapy-free induction therapy alone (Part 1 ) was 100% (50), with CR in 90% of patients and partial responses (PR) in 10%. Of the 47 patients evaluable for part 2 (chemoimmunotherapy), all had CRs, for an ORR of 100%.
Dr. Wang noted that one patient had a dramatic radiographic reduction in spleen size following just two cycles of chemotherapy-free induction, and two other patients had similar reductions after four and six cycles, respectively.
After a median follow-up of 15.9 months, neither the median duration of response, progression-free survival, nor overall survival have been reached. There have been no deaths and only one case of disease progression after one year of therapy.
The patients generally tolerated the regimen very well, Dr. Wang said. There were no cases of lymphocytosis, bleeding, or atrial fibrillation after 332 combined cycles.
Nonhematological adverse events were primarily grade 1 or 2. Grade 3 fatigue was reported in approximately 10% of patients. There were no grade 4 adverse events.
“This study may provide a window of opportunity to reduce the frontline therapies and reduce the long-term toxicities such as secondary malignancies.” Dr. Wang said.
He acknowledged that four cycles of intensive chemotherapy is still toxic and that further efforts to reduce these toxicities are needed. The investigators are currently planning the Window II study, in which a fraction of patients will be treated with no chemotherapy at all, he said.
The study was supported by Pharmacyclics and Janssen. Dr. Wang disclosed receiving research grants and honoraria and serving as a consultant for the companies.
AT14-ICML
Key clinical point: A chemotherapy-free induction regimen with ibrutinib and rituximab was associated with high response rates in patients with newly diagnosed mantle cell lymphoma (MCL).
Major finding: The overall response rate after induction was 100%, including 90% complete responses.
Data source: Update results from phase II investigator-initiated study in 50 patients aged 65 years and younger with MCL.
Disclosures: The study was supported by Pharmacyclics and Janssen. Dr. Wang disclosed receiving research grants and honoraria and serving as a consultant for the companies.
Bendamustine plus rituximab may have edge for treating indolent NHL, MCL
CHICAGO – Overall survival was comparable at 5 years of follow up for three regimens in treatment-naive patients with indolent non-Hodgkin lymphoma (NHL) or mantle cell lymphoma (MCL), based on long-term results from the BRIGHT study.
While progression-free survival, event-free survival, and duration of response were significantly better with bendamustine plus rituximab (BR), overall survival at 5 years did not significantly differ in patients given this regimen and compared to patients given rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) or rituximab with cyclophosphamide, vincristine and prednisone (R-CVP), Ian Flinn, MD, of Tennessee Oncology, Nashville, reported at the annual meeting of the American Society of Clinical Oncology.
Quality of life was somewhat better for the patients given BR, but those patients were also at higher risk for secondary malignancies (42 vs. 24), most of which were squamous cell carcinomas, observed Dr. Kahl, professor of medicine at Washington University, St. Louis.
In BRIGHT, 224 treatment-naive patients with indolent NHL or MCL were randomized to receive BR and were compared to 223 similar patients who received either R-CHOP (104 patients) or R-CVP (119 patients). At least six cycles of therapy were completed by 203 patients in the BR group and by 196 in the R-CHOP/R-CVP group. Rituximab maintenance therapy was given to 43% of the BR group and to 45% of the R-CHOP/R-CVP group.
For BR and R-CHOP/R-CVP, the 5-year progression-free survival rate was 65.5% (95% CI, 58.5-71.6) and 55.8% (95% CI, 48.4-62.5), respectively. The overall survival rate for the entire patient group was 81.7% (75.7-86.3) and 85% (79.3-89.3) respectively. Comparing BR and R-CHOP/R-CVP, the hazard ratio (95% CI) for progression-free survival was 0.61 (0.45-0.85; P = .0025), the HR for event-free survival was 0.63 (0.46-0.84; P = .0020), the HR for duration of response was 0.66 (0.47-0.92; P = .0134), and the HR for overall survival was 1.15 (0.72-1.84; P = .5461).
Similar results were found in indolent NHL (progression-free survival 0.70 [0.49-1.01; P = .0582]) and MCL (progression-free survival 0.40 [0.21-0.75; P = .0035]), with the strongest effect in MCL, Dr. Flinn said.
Dr. Kahl noted that the advantages for the BR regimen include that it is not associated with alopecia, neuropathy, or steroid issues, and that it may extend progression-free survival and time to next treatment. On the other hand, R-CHOP is associated with less GI toxicity, rash, opportunistic infections, and prolonged cytopenia. Also, the BR regimen was associated with a higher risk of secondary cancers, primarily squamous cell carcinomas.
There were 42 secondary malignancies in the BR group and 24 in the R-CHOP/R-CVP group, Dr. Flinn reported.
It is theoretically possible that BR equals R-CHOP plus maintenance therapy from an efficacy perspective, Dr. Kahl said.
As virtually all excess adverse event fatalities occurred during maintenance therapy, it is possible that maintenance therapy after BR “does more harm than good.” This high priority issue “should be evaluated in the BRIGHT data set,” Dr. Kahl recommended.
Teva Branded Pharmaceutical Products R&D sponsored the study. Dr. Flinn had no relationships to disclose; two of his fellow researchers are Teva employees. Dr. Kahl disclosed serving as an adviser or consultant to Abbvie, Acerta Pharma, Celgene, Cell Therapeutics, Genentech/Roche, Incyte, Infinity Pharmaceuticals, Juno Therapeutics, Millennium, Pharmacyclics, Sandoz, and Seattle Genetics.
[email protected]
On Twitter @maryjodales
CHICAGO – Overall survival was comparable at 5 years of follow up for three regimens in treatment-naive patients with indolent non-Hodgkin lymphoma (NHL) or mantle cell lymphoma (MCL), based on long-term results from the BRIGHT study.
While progression-free survival, event-free survival, and duration of response were significantly better with bendamustine plus rituximab (BR), overall survival at 5 years did not significantly differ in patients given this regimen and compared to patients given rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) or rituximab with cyclophosphamide, vincristine and prednisone (R-CVP), Ian Flinn, MD, of Tennessee Oncology, Nashville, reported at the annual meeting of the American Society of Clinical Oncology.
Quality of life was somewhat better for the patients given BR, but those patients were also at higher risk for secondary malignancies (42 vs. 24), most of which were squamous cell carcinomas, observed Dr. Kahl, professor of medicine at Washington University, St. Louis.
In BRIGHT, 224 treatment-naive patients with indolent NHL or MCL were randomized to receive BR and were compared to 223 similar patients who received either R-CHOP (104 patients) or R-CVP (119 patients). At least six cycles of therapy were completed by 203 patients in the BR group and by 196 in the R-CHOP/R-CVP group. Rituximab maintenance therapy was given to 43% of the BR group and to 45% of the R-CHOP/R-CVP group.
For BR and R-CHOP/R-CVP, the 5-year progression-free survival rate was 65.5% (95% CI, 58.5-71.6) and 55.8% (95% CI, 48.4-62.5), respectively. The overall survival rate for the entire patient group was 81.7% (75.7-86.3) and 85% (79.3-89.3) respectively. Comparing BR and R-CHOP/R-CVP, the hazard ratio (95% CI) for progression-free survival was 0.61 (0.45-0.85; P = .0025), the HR for event-free survival was 0.63 (0.46-0.84; P = .0020), the HR for duration of response was 0.66 (0.47-0.92; P = .0134), and the HR for overall survival was 1.15 (0.72-1.84; P = .5461).
Similar results were found in indolent NHL (progression-free survival 0.70 [0.49-1.01; P = .0582]) and MCL (progression-free survival 0.40 [0.21-0.75; P = .0035]), with the strongest effect in MCL, Dr. Flinn said.
Dr. Kahl noted that the advantages for the BR regimen include that it is not associated with alopecia, neuropathy, or steroid issues, and that it may extend progression-free survival and time to next treatment. On the other hand, R-CHOP is associated with less GI toxicity, rash, opportunistic infections, and prolonged cytopenia. Also, the BR regimen was associated with a higher risk of secondary cancers, primarily squamous cell carcinomas.
There were 42 secondary malignancies in the BR group and 24 in the R-CHOP/R-CVP group, Dr. Flinn reported.
It is theoretically possible that BR equals R-CHOP plus maintenance therapy from an efficacy perspective, Dr. Kahl said.
As virtually all excess adverse event fatalities occurred during maintenance therapy, it is possible that maintenance therapy after BR “does more harm than good.” This high priority issue “should be evaluated in the BRIGHT data set,” Dr. Kahl recommended.
Teva Branded Pharmaceutical Products R&D sponsored the study. Dr. Flinn had no relationships to disclose; two of his fellow researchers are Teva employees. Dr. Kahl disclosed serving as an adviser or consultant to Abbvie, Acerta Pharma, Celgene, Cell Therapeutics, Genentech/Roche, Incyte, Infinity Pharmaceuticals, Juno Therapeutics, Millennium, Pharmacyclics, Sandoz, and Seattle Genetics.
[email protected]
On Twitter @maryjodales
CHICAGO – Overall survival was comparable at 5 years of follow up for three regimens in treatment-naive patients with indolent non-Hodgkin lymphoma (NHL) or mantle cell lymphoma (MCL), based on long-term results from the BRIGHT study.
While progression-free survival, event-free survival, and duration of response were significantly better with bendamustine plus rituximab (BR), overall survival at 5 years did not significantly differ in patients given this regimen and compared to patients given rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) or rituximab with cyclophosphamide, vincristine and prednisone (R-CVP), Ian Flinn, MD, of Tennessee Oncology, Nashville, reported at the annual meeting of the American Society of Clinical Oncology.
Quality of life was somewhat better for the patients given BR, but those patients were also at higher risk for secondary malignancies (42 vs. 24), most of which were squamous cell carcinomas, observed Dr. Kahl, professor of medicine at Washington University, St. Louis.
In BRIGHT, 224 treatment-naive patients with indolent NHL or MCL were randomized to receive BR and were compared to 223 similar patients who received either R-CHOP (104 patients) or R-CVP (119 patients). At least six cycles of therapy were completed by 203 patients in the BR group and by 196 in the R-CHOP/R-CVP group. Rituximab maintenance therapy was given to 43% of the BR group and to 45% of the R-CHOP/R-CVP group.
For BR and R-CHOP/R-CVP, the 5-year progression-free survival rate was 65.5% (95% CI, 58.5-71.6) and 55.8% (95% CI, 48.4-62.5), respectively. The overall survival rate for the entire patient group was 81.7% (75.7-86.3) and 85% (79.3-89.3) respectively. Comparing BR and R-CHOP/R-CVP, the hazard ratio (95% CI) for progression-free survival was 0.61 (0.45-0.85; P = .0025), the HR for event-free survival was 0.63 (0.46-0.84; P = .0020), the HR for duration of response was 0.66 (0.47-0.92; P = .0134), and the HR for overall survival was 1.15 (0.72-1.84; P = .5461).
Similar results were found in indolent NHL (progression-free survival 0.70 [0.49-1.01; P = .0582]) and MCL (progression-free survival 0.40 [0.21-0.75; P = .0035]), with the strongest effect in MCL, Dr. Flinn said.
Dr. Kahl noted that the advantages for the BR regimen include that it is not associated with alopecia, neuropathy, or steroid issues, and that it may extend progression-free survival and time to next treatment. On the other hand, R-CHOP is associated with less GI toxicity, rash, opportunistic infections, and prolonged cytopenia. Also, the BR regimen was associated with a higher risk of secondary cancers, primarily squamous cell carcinomas.
There were 42 secondary malignancies in the BR group and 24 in the R-CHOP/R-CVP group, Dr. Flinn reported.
It is theoretically possible that BR equals R-CHOP plus maintenance therapy from an efficacy perspective, Dr. Kahl said.
As virtually all excess adverse event fatalities occurred during maintenance therapy, it is possible that maintenance therapy after BR “does more harm than good.” This high priority issue “should be evaluated in the BRIGHT data set,” Dr. Kahl recommended.
Teva Branded Pharmaceutical Products R&D sponsored the study. Dr. Flinn had no relationships to disclose; two of his fellow researchers are Teva employees. Dr. Kahl disclosed serving as an adviser or consultant to Abbvie, Acerta Pharma, Celgene, Cell Therapeutics, Genentech/Roche, Incyte, Infinity Pharmaceuticals, Juno Therapeutics, Millennium, Pharmacyclics, Sandoz, and Seattle Genetics.
[email protected]
On Twitter @maryjodales
AT ASCO 2017
Key clinical point:
Major finding: For BR and R-CHOP/R-CVP, the 5-year progression-free survival rate was 65.5% (95% CI, 58.5-71.6) and 55.8% (95% CI, 48.4-62.5), respectively.
Data source: In BRIGHT, 224 treatment-naive patients with indolent non-Hodgkin lymphoma or mantle cell lymphoma were randomized to receive BR and were compared to 223 similar patients who received either R-CHOP (104 patients) or R-CVP (119 patients).
Disclosures: Teva Branded Pharmaceutical Products R&D sponsored the study. Dr. Flinn had no relationships to disclose; two of his fellow researchers are Teva employees. Dr. Kahl disclosed serving as an adviser or consultant to Abbvie, Acerta Pharma, Celgene, Cell Therapeutics, Genentech/Roche, Incyte, Infinity Pharmaceuticals, Juno Therapeutics, Millennium, Pharmacyclics, Sandoz, and Seattle Genetics.
Hitting BTK, PI3K pays off in B-cell malignancies
LUGANO, SWITZERLAND – A combination of ibrutinib and umbralisib, an investigational inhibitor of phosphatidylinostiol 3-kinase (PI3K), induced high response rates in patients with relapsed/refractory B-cell malignancies, with no dose-limiting toxicities, based on updated early efficacy results from a phase I/IB dose-escalation study.
One-year progression-free survival (PFS) was 88% for patients with chronic lymphocytic leukemia (CLL), and 1-year overall survival (OS) was 94%, reported Matthew S. Davids, MD, MMSc, of the Dana-Farber Cancer Institute in Boston.
Single-agent ibrutinib (Imbruvica), an inhibitor of Bruton’s tyrosine kinase, is effective in patients with high-risk CLL or MCL, but the depth and durability of response are limited, he said. Umbralisib (TGR-1202) is a second-generation PI3K inhibitor with a high degree of specificity for the delta isoform of the kinase. It was designed to have a better safety profile than the first-in-class agent idelalisib (Zydelig).
“We hypothesized that inhibiting multiple BCR [B-cell receptor] pathways with kinase inhibitors may both deepen and prolong response and potentially overcome resistance mutations,” he said at the International Conference on Malignant Lymphoma.
In an ongoing, investigator-initiated phase I/IB trial, Dr. Davids and his colleagues enrolled 14 patients with MCL and 18 with CLL into parallel dose-escalation arms. Data were insufficient for the preliminary efficacy analysis.
Among patients with CLL, the objective response rate was 94% (16 of 17 patients). Of the 17 patients, 15 had a partial response or a partial response with lymphocytosis. One patient had a complete response, and three had radiographic complete responses, but these were not included in the objective response rate.
All three patients who had prior exposure to a PI3K inhibitor had responses, as did one of two patients with prior ibrutinib exposure.
For the patients with MCL, the objective response rate was 79% (11 of 14 patients); 10 had a partial response and 1 had a complete response. One other patient with a radiographic complete response was not included in the objective response rate.
Median follow-up among survivors was 14 months. As noted, the 1-year PFS and OS for patients with CLL were 88% and 94%, and the median PFS and OS for patients with MCL were 8.4 and 11.6 months.
One patient with CLL and five with MCL died of disease progression. A sixth patient with MCL did not have an adequate response to ibrutinib/umbralisib and died of toxicities related to the next line of therapy.
The safety analysis showed no dose-limiting toxicities, and the maximum tolerated dose was not identified with umbralisib at doses of 400 mg, 600 mg, or 800 mg daily in patients with either CLL or MCL.
The most common hematologic adverse events were grade 3/4 neutropenia in approximately 37% of patients in each arm, thrombocytopenia in 11% of CLL patients and 36% of MCL patients, and anemia in 15% and 29%, respectively.
The MCL arm of the study is still accruing patients, and correlative studies are in progress, Dr. Davids said.
The study is supported by TG Therapeutics, BCRP/LLS TAP, and grants from ASCO and the National Institutes of Health. Dr. Davids disclosed honoraria from Janssen and research funding to his institution from Phamarcyclics.
LUGANO, SWITZERLAND – A combination of ibrutinib and umbralisib, an investigational inhibitor of phosphatidylinostiol 3-kinase (PI3K), induced high response rates in patients with relapsed/refractory B-cell malignancies, with no dose-limiting toxicities, based on updated early efficacy results from a phase I/IB dose-escalation study.
One-year progression-free survival (PFS) was 88% for patients with chronic lymphocytic leukemia (CLL), and 1-year overall survival (OS) was 94%, reported Matthew S. Davids, MD, MMSc, of the Dana-Farber Cancer Institute in Boston.
Single-agent ibrutinib (Imbruvica), an inhibitor of Bruton’s tyrosine kinase, is effective in patients with high-risk CLL or MCL, but the depth and durability of response are limited, he said. Umbralisib (TGR-1202) is a second-generation PI3K inhibitor with a high degree of specificity for the delta isoform of the kinase. It was designed to have a better safety profile than the first-in-class agent idelalisib (Zydelig).
“We hypothesized that inhibiting multiple BCR [B-cell receptor] pathways with kinase inhibitors may both deepen and prolong response and potentially overcome resistance mutations,” he said at the International Conference on Malignant Lymphoma.
In an ongoing, investigator-initiated phase I/IB trial, Dr. Davids and his colleagues enrolled 14 patients with MCL and 18 with CLL into parallel dose-escalation arms. Data were insufficient for the preliminary efficacy analysis.
Among patients with CLL, the objective response rate was 94% (16 of 17 patients). Of the 17 patients, 15 had a partial response or a partial response with lymphocytosis. One patient had a complete response, and three had radiographic complete responses, but these were not included in the objective response rate.
All three patients who had prior exposure to a PI3K inhibitor had responses, as did one of two patients with prior ibrutinib exposure.
For the patients with MCL, the objective response rate was 79% (11 of 14 patients); 10 had a partial response and 1 had a complete response. One other patient with a radiographic complete response was not included in the objective response rate.
Median follow-up among survivors was 14 months. As noted, the 1-year PFS and OS for patients with CLL were 88% and 94%, and the median PFS and OS for patients with MCL were 8.4 and 11.6 months.
One patient with CLL and five with MCL died of disease progression. A sixth patient with MCL did not have an adequate response to ibrutinib/umbralisib and died of toxicities related to the next line of therapy.
The safety analysis showed no dose-limiting toxicities, and the maximum tolerated dose was not identified with umbralisib at doses of 400 mg, 600 mg, or 800 mg daily in patients with either CLL or MCL.
The most common hematologic adverse events were grade 3/4 neutropenia in approximately 37% of patients in each arm, thrombocytopenia in 11% of CLL patients and 36% of MCL patients, and anemia in 15% and 29%, respectively.
The MCL arm of the study is still accruing patients, and correlative studies are in progress, Dr. Davids said.
The study is supported by TG Therapeutics, BCRP/LLS TAP, and grants from ASCO and the National Institutes of Health. Dr. Davids disclosed honoraria from Janssen and research funding to his institution from Phamarcyclics.
LUGANO, SWITZERLAND – A combination of ibrutinib and umbralisib, an investigational inhibitor of phosphatidylinostiol 3-kinase (PI3K), induced high response rates in patients with relapsed/refractory B-cell malignancies, with no dose-limiting toxicities, based on updated early efficacy results from a phase I/IB dose-escalation study.
One-year progression-free survival (PFS) was 88% for patients with chronic lymphocytic leukemia (CLL), and 1-year overall survival (OS) was 94%, reported Matthew S. Davids, MD, MMSc, of the Dana-Farber Cancer Institute in Boston.
Single-agent ibrutinib (Imbruvica), an inhibitor of Bruton’s tyrosine kinase, is effective in patients with high-risk CLL or MCL, but the depth and durability of response are limited, he said. Umbralisib (TGR-1202) is a second-generation PI3K inhibitor with a high degree of specificity for the delta isoform of the kinase. It was designed to have a better safety profile than the first-in-class agent idelalisib (Zydelig).
“We hypothesized that inhibiting multiple BCR [B-cell receptor] pathways with kinase inhibitors may both deepen and prolong response and potentially overcome resistance mutations,” he said at the International Conference on Malignant Lymphoma.
In an ongoing, investigator-initiated phase I/IB trial, Dr. Davids and his colleagues enrolled 14 patients with MCL and 18 with CLL into parallel dose-escalation arms. Data were insufficient for the preliminary efficacy analysis.
Among patients with CLL, the objective response rate was 94% (16 of 17 patients). Of the 17 patients, 15 had a partial response or a partial response with lymphocytosis. One patient had a complete response, and three had radiographic complete responses, but these were not included in the objective response rate.
All three patients who had prior exposure to a PI3K inhibitor had responses, as did one of two patients with prior ibrutinib exposure.
For the patients with MCL, the objective response rate was 79% (11 of 14 patients); 10 had a partial response and 1 had a complete response. One other patient with a radiographic complete response was not included in the objective response rate.
Median follow-up among survivors was 14 months. As noted, the 1-year PFS and OS for patients with CLL were 88% and 94%, and the median PFS and OS for patients with MCL were 8.4 and 11.6 months.
One patient with CLL and five with MCL died of disease progression. A sixth patient with MCL did not have an adequate response to ibrutinib/umbralisib and died of toxicities related to the next line of therapy.
The safety analysis showed no dose-limiting toxicities, and the maximum tolerated dose was not identified with umbralisib at doses of 400 mg, 600 mg, or 800 mg daily in patients with either CLL or MCL.
The most common hematologic adverse events were grade 3/4 neutropenia in approximately 37% of patients in each arm, thrombocytopenia in 11% of CLL patients and 36% of MCL patients, and anemia in 15% and 29%, respectively.
The MCL arm of the study is still accruing patients, and correlative studies are in progress, Dr. Davids said.
The study is supported by TG Therapeutics, BCRP/LLS TAP, and grants from ASCO and the National Institutes of Health. Dr. Davids disclosed honoraria from Janssen and research funding to his institution from Phamarcyclics.
AT 14-ICML
Key clinical point:
Major finding: The objective response rate to the combination was 94% in 18 patients with chronic lymphocytic leukemia and 79% in 14 patients with mantle cell lymphoma.
Data source: A phase I/IB dose-escalation study.
Disclosures: The study is supported by TG Therapeutics, BCRP/LLS TAP, and grants from ASCO and the National Institutes of Health. Dr. Davids disclosed honoraria from Janssen and research funding to his institution from Phamarcyclics.
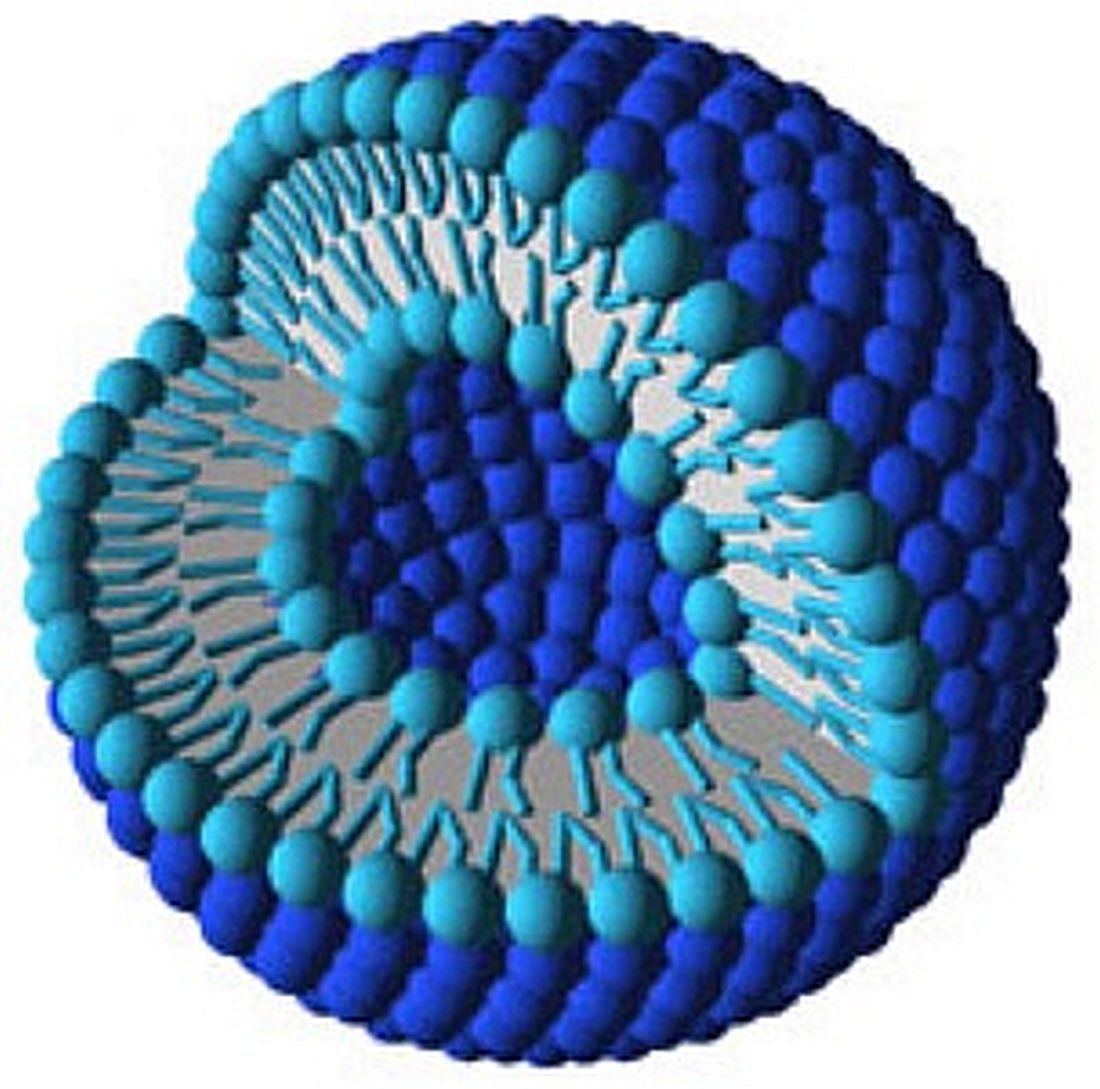
Liposomes boost bortezomib efficacy
Bortezomib treatment using liposome nanocarriers leads to decreased cell viability and greater apoptosis in vitro, compared with treatment with free bortezomib, according to a study in the Journal of Pharmaceutical Sciences and Pharmacology.
Liposomes are lipid sacs with a watery compartment, which can be used to encapsulate and deliver a therapeutic cargo. The delivery method has been found to have improved efficacy with lesser side effects.
Ceramide liposomes are an attractive drug-delivery vehicle, the researchers said, because of their cell-permeability and because they’ve been found, on their own, to mediate apoptosis. Researchers said they believed this was the first time results have been reported on combining ceramide liposomes with an anticancer drug such as bortezomib. Cationic liposomes were picked because they’re known to destabilize cell membranes, helping with intracellular delivery of the drug.
Free bortezomib and bortezomib loaded into liposomes were tested for efficacy on mouse preosteoclast calvaria MC3T3 cells, mouse macrophage-like RAW 264.7 cells, and human osteosarcoma U2OS cells.
On the RAW 264.7 cells, researchers found a significant difference in cell viability between free bortezomib and ceramide liposomes after 24 hours (P less than .01) and 48 hours (P less than .05) and between free bortezomib and cationic liposomes at 24 hours (P less than .01). They also reported a significant difference with cationic liposomes on MC3T3 cells and U2OS cells at 48 hours (both P less than .01).
One nanomolar (nM) of ceramide-loaded bortezomib induced significantly more apoptosis than did 1 nM of free bortezomib (P less than .01), and 10 nM of ceramide-loaded bortezomib brought about more cell death and apoptosis than did 10 nM of free bortezomib (P less than .05). These effects were likely the result of increased expression of proteins involved in apoptosis.
Liposomes might be able to boost the efficacy of bortezomib, according to the researchers, who are now studying the localization of these liposomes with confocal microscopes to better understand the mechanism of action.
“Such improvements,” they wrote, “offer the potential to reduce side effects known to occur with this chemotherapy, such as peripheral neuropathy, as well as to target Bort-resistant cancers.”
Bortezomib treatment using liposome nanocarriers leads to decreased cell viability and greater apoptosis in vitro, compared with treatment with free bortezomib, according to a study in the Journal of Pharmaceutical Sciences and Pharmacology.
Liposomes are lipid sacs with a watery compartment, which can be used to encapsulate and deliver a therapeutic cargo. The delivery method has been found to have improved efficacy with lesser side effects.
Ceramide liposomes are an attractive drug-delivery vehicle, the researchers said, because of their cell-permeability and because they’ve been found, on their own, to mediate apoptosis. Researchers said they believed this was the first time results have been reported on combining ceramide liposomes with an anticancer drug such as bortezomib. Cationic liposomes were picked because they’re known to destabilize cell membranes, helping with intracellular delivery of the drug.
Free bortezomib and bortezomib loaded into liposomes were tested for efficacy on mouse preosteoclast calvaria MC3T3 cells, mouse macrophage-like RAW 264.7 cells, and human osteosarcoma U2OS cells.
On the RAW 264.7 cells, researchers found a significant difference in cell viability between free bortezomib and ceramide liposomes after 24 hours (P less than .01) and 48 hours (P less than .05) and between free bortezomib and cationic liposomes at 24 hours (P less than .01). They also reported a significant difference with cationic liposomes on MC3T3 cells and U2OS cells at 48 hours (both P less than .01).
One nanomolar (nM) of ceramide-loaded bortezomib induced significantly more apoptosis than did 1 nM of free bortezomib (P less than .01), and 10 nM of ceramide-loaded bortezomib brought about more cell death and apoptosis than did 10 nM of free bortezomib (P less than .05). These effects were likely the result of increased expression of proteins involved in apoptosis.
Liposomes might be able to boost the efficacy of bortezomib, according to the researchers, who are now studying the localization of these liposomes with confocal microscopes to better understand the mechanism of action.
“Such improvements,” they wrote, “offer the potential to reduce side effects known to occur with this chemotherapy, such as peripheral neuropathy, as well as to target Bort-resistant cancers.”
Bortezomib treatment using liposome nanocarriers leads to decreased cell viability and greater apoptosis in vitro, compared with treatment with free bortezomib, according to a study in the Journal of Pharmaceutical Sciences and Pharmacology.
Liposomes are lipid sacs with a watery compartment, which can be used to encapsulate and deliver a therapeutic cargo. The delivery method has been found to have improved efficacy with lesser side effects.
Ceramide liposomes are an attractive drug-delivery vehicle, the researchers said, because of their cell-permeability and because they’ve been found, on their own, to mediate apoptosis. Researchers said they believed this was the first time results have been reported on combining ceramide liposomes with an anticancer drug such as bortezomib. Cationic liposomes were picked because they’re known to destabilize cell membranes, helping with intracellular delivery of the drug.
Free bortezomib and bortezomib loaded into liposomes were tested for efficacy on mouse preosteoclast calvaria MC3T3 cells, mouse macrophage-like RAW 264.7 cells, and human osteosarcoma U2OS cells.
On the RAW 264.7 cells, researchers found a significant difference in cell viability between free bortezomib and ceramide liposomes after 24 hours (P less than .01) and 48 hours (P less than .05) and between free bortezomib and cationic liposomes at 24 hours (P less than .01). They also reported a significant difference with cationic liposomes on MC3T3 cells and U2OS cells at 48 hours (both P less than .01).
One nanomolar (nM) of ceramide-loaded bortezomib induced significantly more apoptosis than did 1 nM of free bortezomib (P less than .01), and 10 nM of ceramide-loaded bortezomib brought about more cell death and apoptosis than did 10 nM of free bortezomib (P less than .05). These effects were likely the result of increased expression of proteins involved in apoptosis.
Liposomes might be able to boost the efficacy of bortezomib, according to the researchers, who are now studying the localization of these liposomes with confocal microscopes to better understand the mechanism of action.
“Such improvements,” they wrote, “offer the potential to reduce side effects known to occur with this chemotherapy, such as peripheral neuropathy, as well as to target Bort-resistant cancers.”
FROM THE JOURNAL OF PHARMACEUTICAL SCIENCES AND PHARMACOLOGY
Key clinical point: Ceramide and cationic liposomes loaded with bortezomib decreased cell viability and increased apoptosis in vitro, compared with bortezomib alone.
Major finding: One nanomolar (nM) of ceramide-loaded bortezomib induced significantly more apoptosis than did 1 nM of free bortezomib (P less than .01), and 10 nM of ceramide-loaded bortezomib brought about more cell death and apoptosis than did 10 nM of free bortezomib (P less than .05).
Data source: An in vitro study conducted at Midwestern University.
Disclosures: Researchers reported no conflicts of interest.
Early allo SCT advised for high-risk mantle cell lymphoma
High-risk patients with mantle cell lymphoma who have a matched related donor have a better chance for survival if they don’t delay allogeneic hematopoietic stem cell transplantation (allo SCT), based on a small single-center study reported by Daniel Allen Kobrinski, DO, and his colleagues at Loyola University, Chicago.
They based the recommendation on the outcomes of 29 mantle cell lymphoma patients who underwent allo SCT at Loyola University Medical Center between Jan. 1, 1999 and Jan. 1, 2016. Before having allo SCT, 23 of 29 patients had three or more lines of treatment. Six had myeloablative conditioning and 23 had reduced-intensity conditioning; 15 had a related donor, 6 had a matched unrelated donor, and 8 had an unmatched cord blood donor.
Probability estimates for overall survival and non–relapse mortality at 5 years were calculated from the date of allo SCT to the date of patient death or last known follow-up. The 5-year rate of overall survival was 42% and the rate of non–relapse mortality was 53%. Based on a univariate analysis, the risk of death was lower in patients who received total body irradiation-based conditioning (hazard ratio, 0.19; 95% confidence interval, 0.04-0.81; P = .03), and in those who had HLA-matched, related donor transplants (HR, 0.29; 95% CI, 0.11-0.79; P = .02).
Patients who received more than three lines of prior treatment had a higher risk of death (HR, 2.77; 95% CI, 1.05-7.34; P = .04).
Four of the patients had grade III/IV acute graft-versus-host disease (GVHD) and four relapsed. Two patients died from acute GVHD, and most of the other deaths were from treatment-related toxicities.
Dr. Kobrinski had no relationships to disclose.
Allogeneic hematopoietic stem cell transplantation for mantle cell lymphoma in a heavily pretreated patient population. 2017 ASCO Annual Meeting Abstract No: 7558
[email protected]
On Twitter @maryjodales
High-risk patients with mantle cell lymphoma who have a matched related donor have a better chance for survival if they don’t delay allogeneic hematopoietic stem cell transplantation (allo SCT), based on a small single-center study reported by Daniel Allen Kobrinski, DO, and his colleagues at Loyola University, Chicago.
They based the recommendation on the outcomes of 29 mantle cell lymphoma patients who underwent allo SCT at Loyola University Medical Center between Jan. 1, 1999 and Jan. 1, 2016. Before having allo SCT, 23 of 29 patients had three or more lines of treatment. Six had myeloablative conditioning and 23 had reduced-intensity conditioning; 15 had a related donor, 6 had a matched unrelated donor, and 8 had an unmatched cord blood donor.
Probability estimates for overall survival and non–relapse mortality at 5 years were calculated from the date of allo SCT to the date of patient death or last known follow-up. The 5-year rate of overall survival was 42% and the rate of non–relapse mortality was 53%. Based on a univariate analysis, the risk of death was lower in patients who received total body irradiation-based conditioning (hazard ratio, 0.19; 95% confidence interval, 0.04-0.81; P = .03), and in those who had HLA-matched, related donor transplants (HR, 0.29; 95% CI, 0.11-0.79; P = .02).
Patients who received more than three lines of prior treatment had a higher risk of death (HR, 2.77; 95% CI, 1.05-7.34; P = .04).
Four of the patients had grade III/IV acute graft-versus-host disease (GVHD) and four relapsed. Two patients died from acute GVHD, and most of the other deaths were from treatment-related toxicities.
Dr. Kobrinski had no relationships to disclose.
Allogeneic hematopoietic stem cell transplantation for mantle cell lymphoma in a heavily pretreated patient population. 2017 ASCO Annual Meeting Abstract No: 7558
[email protected]
On Twitter @maryjodales
High-risk patients with mantle cell lymphoma who have a matched related donor have a better chance for survival if they don’t delay allogeneic hematopoietic stem cell transplantation (allo SCT), based on a small single-center study reported by Daniel Allen Kobrinski, DO, and his colleagues at Loyola University, Chicago.
They based the recommendation on the outcomes of 29 mantle cell lymphoma patients who underwent allo SCT at Loyola University Medical Center between Jan. 1, 1999 and Jan. 1, 2016. Before having allo SCT, 23 of 29 patients had three or more lines of treatment. Six had myeloablative conditioning and 23 had reduced-intensity conditioning; 15 had a related donor, 6 had a matched unrelated donor, and 8 had an unmatched cord blood donor.
Probability estimates for overall survival and non–relapse mortality at 5 years were calculated from the date of allo SCT to the date of patient death or last known follow-up. The 5-year rate of overall survival was 42% and the rate of non–relapse mortality was 53%. Based on a univariate analysis, the risk of death was lower in patients who received total body irradiation-based conditioning (hazard ratio, 0.19; 95% confidence interval, 0.04-0.81; P = .03), and in those who had HLA-matched, related donor transplants (HR, 0.29; 95% CI, 0.11-0.79; P = .02).
Patients who received more than three lines of prior treatment had a higher risk of death (HR, 2.77; 95% CI, 1.05-7.34; P = .04).
Four of the patients had grade III/IV acute graft-versus-host disease (GVHD) and four relapsed. Two patients died from acute GVHD, and most of the other deaths were from treatment-related toxicities.
Dr. Kobrinski had no relationships to disclose.
Allogeneic hematopoietic stem cell transplantation for mantle cell lymphoma in a heavily pretreated patient population. 2017 ASCO Annual Meeting Abstract No: 7558
[email protected]
On Twitter @maryjodales
FROM ASCO 2017 ANNUAL MEETING
Key clinical point:
Major finding: Based on a univariate analysis, the risk of death was lower in patients who received total body irradiation-based conditioning (HR, 0.1; 95% CI, 0.04-0.81; P = .03), and in those who had HLA-matched, related donor transplants (HR, 0.29; 95% CI, 0.11-0.79; P = .02).
Data source: A retrospective study of all 29 patients who were treated with an allo stem cell transplant for mantle cell lymphoma at Loyola University Medical Center between Jan. 1, 1999 and Jan. 1, 2016.
Disclosures: Dr. Kobrinski had no relationships to disclose.
Citation: Allogeneic hematopoietic stem cell transplantation for mantle cell lymphoma in a heavily pretreated patient population. 2017 ASCO Annual Meeting Abstract No: 7558.
ALC/AMC prognostic in mantle cell lymphoma
The peripheral blood absolute lymphocyte-to-monocyte ratio (ALC/AMC) was prognostic for overall survival in mantle cell lymphoma patients who have undergone induction therapy, based on a retrospective review study of 96 patients by Andre Goy, MD, of John Theurer Cancer Center, Hackensack (NJ) University, and his colleagues.
Overall survival was better when ALC/AMC was 2 or greater following induction therapy, the researchers wrote in an abstract published in conjunction with the annual meeting of the American Society of Clinical Oncology.
The finding indicates that novel maintenance programs, including targeting the microenvironment or immune response, might be appropriate when patients with mantle cell lymphoma have low ALC/AMC.
The researchers examined data for 96 consecutive mantle cell lymphoma patients. The ALC/AMC was determined from peripheral blood counts obtained approximately 30 days following completion of initial therapy or immediately prior to stem cell mobilization in patients who had first line stem cell transplants.
The ALC/AMC was less than 2 in 67 patients and was 2 or greater in 29 patients. The two patient cohorts were similar in median age, ethnicities, stage distributions, elevated beta-2-microglobulin, elevated lactate dehydrogenate, and Mantle Cell Lymphoma International Prognostic Index scores.
ALC/AMC was less than 2 in 10 of 13 transplanted patients and in 57 of 83 patients who did not undergo transplants. At a median follow-up of 43 months, the median overall survival has not been reached in either cohort.
The 5-year survival rate was 90% among patients with an ALC/AMC of 2 or greater and 68% in those with an ALC/AMC less than 2 (log-rank P less than .05).
Similar ALC/AMC 5-year survival trends were noted when subsetting to the 25 patients with high risk Mantle Cell Lymphoma International Prognostic Index scores (72% vs. 45%; P = .07).
Dr. Goy disclosed honoraria from Acerta Pharma, Celgene, Pharmacyclics, and Takeda; a consulting or advisory role with Acerta Pharma, Celgene, Infinity Pharmaceuticals, Pharmacyclics, and Takeda; and speakers’ bureaus participation for Pharmacyclics and Takeda.
Prognostic value of the absolute lymphocyte-to-monocyte (ALC/AMC) ratio on overall survival among patients with mantle cell lymphoma. Published in conjunction with the 2017 ASCO Annual Meeting. Abstract No: e19030.
[email protected]
On Twitter @maryjodales
The peripheral blood absolute lymphocyte-to-monocyte ratio (ALC/AMC) was prognostic for overall survival in mantle cell lymphoma patients who have undergone induction therapy, based on a retrospective review study of 96 patients by Andre Goy, MD, of John Theurer Cancer Center, Hackensack (NJ) University, and his colleagues.
Overall survival was better when ALC/AMC was 2 or greater following induction therapy, the researchers wrote in an abstract published in conjunction with the annual meeting of the American Society of Clinical Oncology.
The finding indicates that novel maintenance programs, including targeting the microenvironment or immune response, might be appropriate when patients with mantle cell lymphoma have low ALC/AMC.
The researchers examined data for 96 consecutive mantle cell lymphoma patients. The ALC/AMC was determined from peripheral blood counts obtained approximately 30 days following completion of initial therapy or immediately prior to stem cell mobilization in patients who had first line stem cell transplants.
The ALC/AMC was less than 2 in 67 patients and was 2 or greater in 29 patients. The two patient cohorts were similar in median age, ethnicities, stage distributions, elevated beta-2-microglobulin, elevated lactate dehydrogenate, and Mantle Cell Lymphoma International Prognostic Index scores.
ALC/AMC was less than 2 in 10 of 13 transplanted patients and in 57 of 83 patients who did not undergo transplants. At a median follow-up of 43 months, the median overall survival has not been reached in either cohort.
The 5-year survival rate was 90% among patients with an ALC/AMC of 2 or greater and 68% in those with an ALC/AMC less than 2 (log-rank P less than .05).
Similar ALC/AMC 5-year survival trends were noted when subsetting to the 25 patients with high risk Mantle Cell Lymphoma International Prognostic Index scores (72% vs. 45%; P = .07).
Dr. Goy disclosed honoraria from Acerta Pharma, Celgene, Pharmacyclics, and Takeda; a consulting or advisory role with Acerta Pharma, Celgene, Infinity Pharmaceuticals, Pharmacyclics, and Takeda; and speakers’ bureaus participation for Pharmacyclics and Takeda.
Prognostic value of the absolute lymphocyte-to-monocyte (ALC/AMC) ratio on overall survival among patients with mantle cell lymphoma. Published in conjunction with the 2017 ASCO Annual Meeting. Abstract No: e19030.
[email protected]
On Twitter @maryjodales
The peripheral blood absolute lymphocyte-to-monocyte ratio (ALC/AMC) was prognostic for overall survival in mantle cell lymphoma patients who have undergone induction therapy, based on a retrospective review study of 96 patients by Andre Goy, MD, of John Theurer Cancer Center, Hackensack (NJ) University, and his colleagues.
Overall survival was better when ALC/AMC was 2 or greater following induction therapy, the researchers wrote in an abstract published in conjunction with the annual meeting of the American Society of Clinical Oncology.
The finding indicates that novel maintenance programs, including targeting the microenvironment or immune response, might be appropriate when patients with mantle cell lymphoma have low ALC/AMC.
The researchers examined data for 96 consecutive mantle cell lymphoma patients. The ALC/AMC was determined from peripheral blood counts obtained approximately 30 days following completion of initial therapy or immediately prior to stem cell mobilization in patients who had first line stem cell transplants.
The ALC/AMC was less than 2 in 67 patients and was 2 or greater in 29 patients. The two patient cohorts were similar in median age, ethnicities, stage distributions, elevated beta-2-microglobulin, elevated lactate dehydrogenate, and Mantle Cell Lymphoma International Prognostic Index scores.
ALC/AMC was less than 2 in 10 of 13 transplanted patients and in 57 of 83 patients who did not undergo transplants. At a median follow-up of 43 months, the median overall survival has not been reached in either cohort.
The 5-year survival rate was 90% among patients with an ALC/AMC of 2 or greater and 68% in those with an ALC/AMC less than 2 (log-rank P less than .05).
Similar ALC/AMC 5-year survival trends were noted when subsetting to the 25 patients with high risk Mantle Cell Lymphoma International Prognostic Index scores (72% vs. 45%; P = .07).
Dr. Goy disclosed honoraria from Acerta Pharma, Celgene, Pharmacyclics, and Takeda; a consulting or advisory role with Acerta Pharma, Celgene, Infinity Pharmaceuticals, Pharmacyclics, and Takeda; and speakers’ bureaus participation for Pharmacyclics and Takeda.
Prognostic value of the absolute lymphocyte-to-monocyte (ALC/AMC) ratio on overall survival among patients with mantle cell lymphoma. Published in conjunction with the 2017 ASCO Annual Meeting. Abstract No: e19030.
[email protected]
On Twitter @maryjodales
IN CONJUNCTION WITH ASCO 2017
Key clinical point:
Major finding: The 5-year survival rate was 90% among patients with an ALC/AMC of 2 or greater and 68% in those with an ALC/AMC less than 2 (log-rank P less than .05).
Data source: A retrospective review study of 96 patients.
Disclosures: Dr. Goy disclosed honoraria from Acerta Pharma, Celgene, Pharmacyclics, and Takeda; a consulting or advisory role with Acerta Pharma, Celgene, Infinity Pharmaceuticals, Pharmacyclics, and Takeda; and speakers’ bureaus participation for Pharmacyclics and Takeda.
Citation: Prognostic value of the absolute lymphocyte-to-monocyte (ALC/AMC) ratio on overall survival among patients with mantle cell lymphoma. Published in conjunction with the 2017 ASCO Annual Meeting. Abstract No: e19030.
CAR T-cell data expected soon in mantle cell lymphoma
Final data collection for primary outcome measures is anticipated in September for ZUMA-2, a Phase II multicenter study of the chimeric antigen receptor (CAR) T-cell product KTE-C19 in patients with relapsed/refractory mantle cell lymphoma.
ZUMA-2 (NCT02601313), with a planned enrollment of 70 patients, is expected to release the overall response rate at 12 months. Secondary outcome measures include duration of response, best objective response, and progression-free survival.
Subjects can have up to five prior regimens, which must include anthracycline or bendamustine-containing chemotherapy, anti-CD20 monoclonal antibody therapy, and ibrutinib. Study subjects cannot have received allogeneic stem cell transplantation, prior CD19 targeted therapy, or prior CAR or other genetically modified T cell therapy.
Trial participants must be adults with an Eastern cooperative oncology group (ECOG) performance status of 0 or 1, an absolute neutrophil count of at least 1000/µL, and a platelet count of at least 50,000/µL. All need to have adequate renal function, defined as a serum creatinine of 1.5 mg/dL or less; adequate hepatic function, defined as a serum ALT/AST of 2.5 the upper limit of normal or less; and a total bilirubin of 1.5 mg/dL or less (except in subjects with Gilbert’s syndrome), and adequate cardiac function, defined as a cardiac ejection fraction of 50% or more with no evidence of pericardial effusion.
Exclusion criteria include a history of another cancer other than nonmelanomatous skin cancer or carcinoma in situ (for example, cervix, bladder, breast) unless disease free for at least 3 years, known infection with HIV or hepatitis B or C virus, metastases in cerebrospinal fluid or brain, and a history of a seizure disorder, cerebrovascular ischemia/hemorrhage, dementia, cerebellar disease, or any autoimmune disease with CNS involvement.
The study is sponsored by Kite Pharma, the makers of KTE-C19.
Final data collection for primary outcome measures is anticipated in September for ZUMA-2, a Phase II multicenter study of the chimeric antigen receptor (CAR) T-cell product KTE-C19 in patients with relapsed/refractory mantle cell lymphoma.
ZUMA-2 (NCT02601313), with a planned enrollment of 70 patients, is expected to release the overall response rate at 12 months. Secondary outcome measures include duration of response, best objective response, and progression-free survival.
Subjects can have up to five prior regimens, which must include anthracycline or bendamustine-containing chemotherapy, anti-CD20 monoclonal antibody therapy, and ibrutinib. Study subjects cannot have received allogeneic stem cell transplantation, prior CD19 targeted therapy, or prior CAR or other genetically modified T cell therapy.
Trial participants must be adults with an Eastern cooperative oncology group (ECOG) performance status of 0 or 1, an absolute neutrophil count of at least 1000/µL, and a platelet count of at least 50,000/µL. All need to have adequate renal function, defined as a serum creatinine of 1.5 mg/dL or less; adequate hepatic function, defined as a serum ALT/AST of 2.5 the upper limit of normal or less; and a total bilirubin of 1.5 mg/dL or less (except in subjects with Gilbert’s syndrome), and adequate cardiac function, defined as a cardiac ejection fraction of 50% or more with no evidence of pericardial effusion.
Exclusion criteria include a history of another cancer other than nonmelanomatous skin cancer or carcinoma in situ (for example, cervix, bladder, breast) unless disease free for at least 3 years, known infection with HIV or hepatitis B or C virus, metastases in cerebrospinal fluid or brain, and a history of a seizure disorder, cerebrovascular ischemia/hemorrhage, dementia, cerebellar disease, or any autoimmune disease with CNS involvement.
The study is sponsored by Kite Pharma, the makers of KTE-C19.
Final data collection for primary outcome measures is anticipated in September for ZUMA-2, a Phase II multicenter study of the chimeric antigen receptor (CAR) T-cell product KTE-C19 in patients with relapsed/refractory mantle cell lymphoma.
ZUMA-2 (NCT02601313), with a planned enrollment of 70 patients, is expected to release the overall response rate at 12 months. Secondary outcome measures include duration of response, best objective response, and progression-free survival.
Subjects can have up to five prior regimens, which must include anthracycline or bendamustine-containing chemotherapy, anti-CD20 monoclonal antibody therapy, and ibrutinib. Study subjects cannot have received allogeneic stem cell transplantation, prior CD19 targeted therapy, or prior CAR or other genetically modified T cell therapy.
Trial participants must be adults with an Eastern cooperative oncology group (ECOG) performance status of 0 or 1, an absolute neutrophil count of at least 1000/µL, and a platelet count of at least 50,000/µL. All need to have adequate renal function, defined as a serum creatinine of 1.5 mg/dL or less; adequate hepatic function, defined as a serum ALT/AST of 2.5 the upper limit of normal or less; and a total bilirubin of 1.5 mg/dL or less (except in subjects with Gilbert’s syndrome), and adequate cardiac function, defined as a cardiac ejection fraction of 50% or more with no evidence of pericardial effusion.
Exclusion criteria include a history of another cancer other than nonmelanomatous skin cancer or carcinoma in situ (for example, cervix, bladder, breast) unless disease free for at least 3 years, known infection with HIV or hepatitis B or C virus, metastases in cerebrospinal fluid or brain, and a history of a seizure disorder, cerebrovascular ischemia/hemorrhage, dementia, cerebellar disease, or any autoimmune disease with CNS involvement.
The study is sponsored by Kite Pharma, the makers of KTE-C19.
SUMMARY FROM CLINICALTRIALS.GOV