User login
Ex–hospital porter a neglected giant of cancer research
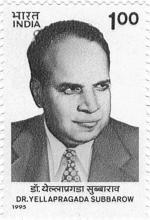
We have a half-forgotten Indian immigrant to thank – a hospital night porter turned biochemist –for revolutionizing treatment of leukemia, the once deadly childhood scourge that is still the most common pediatric cancer.
Dr. Yellapragada SubbaRow has been called the “father of chemotherapy” for developing methotrexate, a powerful, inexpensive therapy for leukemia and other diseases, and he is celebrated for additional scientific achievements. Yet Dr. SubbaRow’s life was marked more by struggle than glory.
Born poor in southeastern India, he nearly succumbed to a tropical disease that killed two older brothers, and he didn’t focus on schoolwork until his father died. Later, prejudice dogged his years as an immigrant to the United States, and a blood clot took his life at the age of 53.
Scientifically, however, Dr. SubbaRow (pronounced sue-buh-rao) triumphed, despite mammoth challenges and a lack of recognition that persists to this day. National Cancer Research Month is a fitting time to look back on his extraordinary life and work and pay tribute to his accomplishments.
‘Yella,’ folic acid, and a paradigm shift
No one appreciates Dr. SubbaRow more than a cadre of Indian-born physicians who have kept his legacy alive in journal articles, presentations, and a Pulitzer Prize-winning book. Among them is author and oncologist Siddhartha Mukherjee, MD, who chronicled Dr. SubbaRow’s achievements in his New York Times No. 1 bestseller, “The Emperor of All Maladies: A Biography of Cancer.”
As Dr. Mukherjee wrote, Dr. SubbaRow was a “pioneer in many ways, a physician turned cellular physiologist, a chemist who had accidentally wandered into biology.” (Per Indian tradition, SubbaRow is the doctor’s first name, and Yellapragada is his surname, but medical literature uses SubbaRow as his cognomen, with some variations in spelling. Dr. Mukherjee wrote that his friends called him “Yella.”)
Dr. SubbaRow came to the United States in 1923, after enduring a difficult childhood and young adulthood. He’d survived bouts of religious fervor, childhood rebellion (including a bid to run away from home and become a banana trader), and a failed arranged marriage. His wife bore him a child who died in infancy. He left it all behind.
In Boston, medical officials rejected his degree. Broke, he worked for a time as a night porter at Brigham and Women’s Hospital in Boston, changing sheets and cleaning urinals. To a poor but proud high-caste Indian Brahmin, the culture shock of carrying out these tasks must have been especially jarring.
Dr. SubbaRow went on to earn a diploma from Harvard Medical School, also in Boston, and became a junior faculty member. As a foreigner, Dr. Mukherjee wrote, Dr. SubbaRow was a “reclusive, nocturnal, heavily accented vegetarian,” so different from his colleagues that advancement seemed impossible. Despite his pioneering biochemistry work, Harvard later declined to offer Dr. SubbaRow a tenured faculty position.
By the early 1940s, he took a job at an upstate New York pharmaceutical company called Lederle Labs (later purchased by Pfizer). At Lederle, Dr. SubbaRow strove to synthesize the vitamin known as folic acid. He ended up creating a kind of antivitamin, a lookalike that acted like folic acid but only succeeded in gumming up the works in receptors. But what good would it do to stop the body from absorbing folic acid? Plenty, it turned out.
Discoveries pile up, but credit and fame prove elusive
Dr. SubbaRow was no stranger to producing landmark biological work. He’d previously codiscovered phosphocreatine and ATP, which are crucial to muscular contractions. However, “in 1935, he had to disown the extent of his role in the discovery of the color test related to phosphorus, instead giving the credit to his co-author, who was being considered for promotion to a full professorship at Harvard,” wrote author Gerald Posner in his 2020 book, “Pharma: Greed, Lies and the Poisoning of America.”
Houston-area oncologist Kirtan Nautiyal, MD, who paid tribute to Dr. SubbaRow in a 2018 article, contended that “with his Indian instinct for self-effacement, he had irreparably sabotaged his own career.”
Dr. SubbaRow and his team also developed “the first effective treatment of filariasis, which causes elephantiasis of the lower limbs and genitals in millions of people, mainly in tropical countries,” Dr. Nautiyal wrote. “Later in the decade, his antibiotic program generated polymyxin, the first effective treatment against the class of bacteria called Gram negatives, and aureomycin, the first “broad-spectrum’ antibiotic.” (Aureomycin is also the first tetracycline antibiotic.)
Dr. SubbaRow’s discovery of a folic acid antagonist would again go largely unheralded. But first came the realization that folic acid made childhood leukemia worse, not better, and the prospect that this process could potentially be reversed.
Rise of methotrexate and fall of leukemia
In Boston, Sidney Farber, MD, a Boston pathologist, was desperate to help Robert Sandler, a 2-year-old leukemia patient. Dr. Farber contacted his ex-colleague Dr. SubbaRow to request a supply of aminopterin, an early version of methotrexate that Dr. SubbaRow and his team had developed. Dr. Farber injected Robert with the substance and within 3 days, the toddler’s white blood count started falling – fast. He stopped bleeding, resumed eating, and once again seemed almost identical to his twin brother, as Dr. Mukherjee wrote in his book.
Leukemia had never gone into remission before. Unfortunately, the treatment only worked temporarily. Robert, like other children treated with the drug, relapsed and died within months. But Dr. Farber “saw a door open” – a chemical, a kind of chemotherapy, that could turn back cancer. In the case of folic acid antagonists, they do so by stopping cancer cells from replicating.
Methotrexate, a related agent synthesized by Dr. SubbaRow, would become a mainstay of leukemia treatment and begin to produce long-term remission from acute lymphoblastic leukemia in 1970, when combination chemotherapy was developed.
Other cancers fell to methotrexate treatment. “Previous assumptions that cancer was nearly always fatal were revised, and the field of medical oncology (treatment of cancer with chemotherapy), which had not previously existed, was formally established in 1971,” according to the National Cancer Institute’s history of methotrexate. This account does not mention Dr. SubbaRow.
Death takes the doctor, but his legacy remains
In biographies, as well as his own words, Dr. SubbaRow comes across as a prickly, hard-driving workaholic who had little interest in intimate human connections. “It is not good to ask in every letter when I will be back,” he wrote to his wife back in India, before cutting off ties completely in the early 1930s. “I will come as early as possible. ... I do not want to write anything more.”
It seems, as his biographer S.P.K. Gupta noted, that “he was quite determined that the time allotted to him on Earth should be completely devoted to finding cures for ailments that plagued mankind.”
Still, Dr. SubbaRow’s research team was devoted to him, and he had plenty of reasons to be bitter, such as the prejudice and isolation he encountered in the United States and earlier, in British-run India. According to Mr. Posner’s book, even as a young medical student, Dr. SubbaRow heeded the call of Indian independence activist Mohandas Gandhi. He “refused the British surgical gown given him at school and instead donned a traditional and simple cotton Khadi. That act of defiance cost SubbaRow the college degree that was necessary for him to get into the State Medical College.”
During the last year of his life, Dr. SubbaRow faced yet another humiliation: In his landmark 1948 study about aminopterin as a treatment for leukemia, his colleague Dr. Farber failed to credit him, an “astonishing omission” as Yaddanapudi Ravindranath, MBBS, a pediatric hematologist/oncologist at Wayne State University, Detroit, put it. “From everything I know, Dr. Farber spent the rest of his career apologizing and trying to make amends for it,” Dr. Ravindranath said in an interview.
A career cut short, and a lasting legacy
In 1948, at the age of 53, Dr. SubbaRow suddenly died. “Many think Dr. SubbaRow would have won [the] Nobel Prize had he lived a few years longer,” said Dr. Ravindranath.
Like Dr. SubbaRow, Dr. Ravindranath was born in Andhra Pradesh state, near the city of Chennai formerly known as Madras. “Being a compatriot, in a way I continue his legacy, and I am obviously proud of him,” said Dr. Ravindranath, who has conducted his own landmark research regarding methotrexate and leukemia.
Nearly 75 years after Dr. SubbaRow’s death, Indian-born physicians like Dr. Ravindranath continue to honor him in print, trying to ensure that he’s not forgotten. Methotrexate remains a crucial treatment for leukemia, along with a long list of other ailments, including psoriasis.
Recognition for “Yella” may have come late and infrequently, but a Lederle Laboratories research library named after him offered Dr. SubbaRow a kind of immortality. A plaque there memorialized him in stone as a scientist, teacher, philosopher, and humanitarian, featuring the quote: “Science simply prolongs life. Religion deepens it.”
By all accounts, Dr. SubbaRow was a man of science and faith who had faith in science.
We have a half-forgotten Indian immigrant to thank – a hospital night porter turned biochemist –for revolutionizing treatment of leukemia, the once deadly childhood scourge that is still the most common pediatric cancer.
Dr. Yellapragada SubbaRow has been called the “father of chemotherapy” for developing methotrexate, a powerful, inexpensive therapy for leukemia and other diseases, and he is celebrated for additional scientific achievements. Yet Dr. SubbaRow’s life was marked more by struggle than glory.
Born poor in southeastern India, he nearly succumbed to a tropical disease that killed two older brothers, and he didn’t focus on schoolwork until his father died. Later, prejudice dogged his years as an immigrant to the United States, and a blood clot took his life at the age of 53.
Scientifically, however, Dr. SubbaRow (pronounced sue-buh-rao) triumphed, despite mammoth challenges and a lack of recognition that persists to this day. National Cancer Research Month is a fitting time to look back on his extraordinary life and work and pay tribute to his accomplishments.
‘Yella,’ folic acid, and a paradigm shift
No one appreciates Dr. SubbaRow more than a cadre of Indian-born physicians who have kept his legacy alive in journal articles, presentations, and a Pulitzer Prize-winning book. Among them is author and oncologist Siddhartha Mukherjee, MD, who chronicled Dr. SubbaRow’s achievements in his New York Times No. 1 bestseller, “The Emperor of All Maladies: A Biography of Cancer.”
As Dr. Mukherjee wrote, Dr. SubbaRow was a “pioneer in many ways, a physician turned cellular physiologist, a chemist who had accidentally wandered into biology.” (Per Indian tradition, SubbaRow is the doctor’s first name, and Yellapragada is his surname, but medical literature uses SubbaRow as his cognomen, with some variations in spelling. Dr. Mukherjee wrote that his friends called him “Yella.”)
Dr. SubbaRow came to the United States in 1923, after enduring a difficult childhood and young adulthood. He’d survived bouts of religious fervor, childhood rebellion (including a bid to run away from home and become a banana trader), and a failed arranged marriage. His wife bore him a child who died in infancy. He left it all behind.
In Boston, medical officials rejected his degree. Broke, he worked for a time as a night porter at Brigham and Women’s Hospital in Boston, changing sheets and cleaning urinals. To a poor but proud high-caste Indian Brahmin, the culture shock of carrying out these tasks must have been especially jarring.
Dr. SubbaRow went on to earn a diploma from Harvard Medical School, also in Boston, and became a junior faculty member. As a foreigner, Dr. Mukherjee wrote, Dr. SubbaRow was a “reclusive, nocturnal, heavily accented vegetarian,” so different from his colleagues that advancement seemed impossible. Despite his pioneering biochemistry work, Harvard later declined to offer Dr. SubbaRow a tenured faculty position.
By the early 1940s, he took a job at an upstate New York pharmaceutical company called Lederle Labs (later purchased by Pfizer). At Lederle, Dr. SubbaRow strove to synthesize the vitamin known as folic acid. He ended up creating a kind of antivitamin, a lookalike that acted like folic acid but only succeeded in gumming up the works in receptors. But what good would it do to stop the body from absorbing folic acid? Plenty, it turned out.
Discoveries pile up, but credit and fame prove elusive
Dr. SubbaRow was no stranger to producing landmark biological work. He’d previously codiscovered phosphocreatine and ATP, which are crucial to muscular contractions. However, “in 1935, he had to disown the extent of his role in the discovery of the color test related to phosphorus, instead giving the credit to his co-author, who was being considered for promotion to a full professorship at Harvard,” wrote author Gerald Posner in his 2020 book, “Pharma: Greed, Lies and the Poisoning of America.”
Houston-area oncologist Kirtan Nautiyal, MD, who paid tribute to Dr. SubbaRow in a 2018 article, contended that “with his Indian instinct for self-effacement, he had irreparably sabotaged his own career.”
Dr. SubbaRow and his team also developed “the first effective treatment of filariasis, which causes elephantiasis of the lower limbs and genitals in millions of people, mainly in tropical countries,” Dr. Nautiyal wrote. “Later in the decade, his antibiotic program generated polymyxin, the first effective treatment against the class of bacteria called Gram negatives, and aureomycin, the first “broad-spectrum’ antibiotic.” (Aureomycin is also the first tetracycline antibiotic.)
Dr. SubbaRow’s discovery of a folic acid antagonist would again go largely unheralded. But first came the realization that folic acid made childhood leukemia worse, not better, and the prospect that this process could potentially be reversed.
Rise of methotrexate and fall of leukemia
In Boston, Sidney Farber, MD, a Boston pathologist, was desperate to help Robert Sandler, a 2-year-old leukemia patient. Dr. Farber contacted his ex-colleague Dr. SubbaRow to request a supply of aminopterin, an early version of methotrexate that Dr. SubbaRow and his team had developed. Dr. Farber injected Robert with the substance and within 3 days, the toddler’s white blood count started falling – fast. He stopped bleeding, resumed eating, and once again seemed almost identical to his twin brother, as Dr. Mukherjee wrote in his book.
Leukemia had never gone into remission before. Unfortunately, the treatment only worked temporarily. Robert, like other children treated with the drug, relapsed and died within months. But Dr. Farber “saw a door open” – a chemical, a kind of chemotherapy, that could turn back cancer. In the case of folic acid antagonists, they do so by stopping cancer cells from replicating.
Methotrexate, a related agent synthesized by Dr. SubbaRow, would become a mainstay of leukemia treatment and begin to produce long-term remission from acute lymphoblastic leukemia in 1970, when combination chemotherapy was developed.
Other cancers fell to methotrexate treatment. “Previous assumptions that cancer was nearly always fatal were revised, and the field of medical oncology (treatment of cancer with chemotherapy), which had not previously existed, was formally established in 1971,” according to the National Cancer Institute’s history of methotrexate. This account does not mention Dr. SubbaRow.
Death takes the doctor, but his legacy remains
In biographies, as well as his own words, Dr. SubbaRow comes across as a prickly, hard-driving workaholic who had little interest in intimate human connections. “It is not good to ask in every letter when I will be back,” he wrote to his wife back in India, before cutting off ties completely in the early 1930s. “I will come as early as possible. ... I do not want to write anything more.”
It seems, as his biographer S.P.K. Gupta noted, that “he was quite determined that the time allotted to him on Earth should be completely devoted to finding cures for ailments that plagued mankind.”
Still, Dr. SubbaRow’s research team was devoted to him, and he had plenty of reasons to be bitter, such as the prejudice and isolation he encountered in the United States and earlier, in British-run India. According to Mr. Posner’s book, even as a young medical student, Dr. SubbaRow heeded the call of Indian independence activist Mohandas Gandhi. He “refused the British surgical gown given him at school and instead donned a traditional and simple cotton Khadi. That act of defiance cost SubbaRow the college degree that was necessary for him to get into the State Medical College.”
During the last year of his life, Dr. SubbaRow faced yet another humiliation: In his landmark 1948 study about aminopterin as a treatment for leukemia, his colleague Dr. Farber failed to credit him, an “astonishing omission” as Yaddanapudi Ravindranath, MBBS, a pediatric hematologist/oncologist at Wayne State University, Detroit, put it. “From everything I know, Dr. Farber spent the rest of his career apologizing and trying to make amends for it,” Dr. Ravindranath said in an interview.
A career cut short, and a lasting legacy
In 1948, at the age of 53, Dr. SubbaRow suddenly died. “Many think Dr. SubbaRow would have won [the] Nobel Prize had he lived a few years longer,” said Dr. Ravindranath.
Like Dr. SubbaRow, Dr. Ravindranath was born in Andhra Pradesh state, near the city of Chennai formerly known as Madras. “Being a compatriot, in a way I continue his legacy, and I am obviously proud of him,” said Dr. Ravindranath, who has conducted his own landmark research regarding methotrexate and leukemia.
Nearly 75 years after Dr. SubbaRow’s death, Indian-born physicians like Dr. Ravindranath continue to honor him in print, trying to ensure that he’s not forgotten. Methotrexate remains a crucial treatment for leukemia, along with a long list of other ailments, including psoriasis.
Recognition for “Yella” may have come late and infrequently, but a Lederle Laboratories research library named after him offered Dr. SubbaRow a kind of immortality. A plaque there memorialized him in stone as a scientist, teacher, philosopher, and humanitarian, featuring the quote: “Science simply prolongs life. Religion deepens it.”
By all accounts, Dr. SubbaRow was a man of science and faith who had faith in science.
We have a half-forgotten Indian immigrant to thank – a hospital night porter turned biochemist –for revolutionizing treatment of leukemia, the once deadly childhood scourge that is still the most common pediatric cancer.
Dr. Yellapragada SubbaRow has been called the “father of chemotherapy” for developing methotrexate, a powerful, inexpensive therapy for leukemia and other diseases, and he is celebrated for additional scientific achievements. Yet Dr. SubbaRow’s life was marked more by struggle than glory.
Born poor in southeastern India, he nearly succumbed to a tropical disease that killed two older brothers, and he didn’t focus on schoolwork until his father died. Later, prejudice dogged his years as an immigrant to the United States, and a blood clot took his life at the age of 53.
Scientifically, however, Dr. SubbaRow (pronounced sue-buh-rao) triumphed, despite mammoth challenges and a lack of recognition that persists to this day. National Cancer Research Month is a fitting time to look back on his extraordinary life and work and pay tribute to his accomplishments.
‘Yella,’ folic acid, and a paradigm shift
No one appreciates Dr. SubbaRow more than a cadre of Indian-born physicians who have kept his legacy alive in journal articles, presentations, and a Pulitzer Prize-winning book. Among them is author and oncologist Siddhartha Mukherjee, MD, who chronicled Dr. SubbaRow’s achievements in his New York Times No. 1 bestseller, “The Emperor of All Maladies: A Biography of Cancer.”
As Dr. Mukherjee wrote, Dr. SubbaRow was a “pioneer in many ways, a physician turned cellular physiologist, a chemist who had accidentally wandered into biology.” (Per Indian tradition, SubbaRow is the doctor’s first name, and Yellapragada is his surname, but medical literature uses SubbaRow as his cognomen, with some variations in spelling. Dr. Mukherjee wrote that his friends called him “Yella.”)
Dr. SubbaRow came to the United States in 1923, after enduring a difficult childhood and young adulthood. He’d survived bouts of religious fervor, childhood rebellion (including a bid to run away from home and become a banana trader), and a failed arranged marriage. His wife bore him a child who died in infancy. He left it all behind.
In Boston, medical officials rejected his degree. Broke, he worked for a time as a night porter at Brigham and Women’s Hospital in Boston, changing sheets and cleaning urinals. To a poor but proud high-caste Indian Brahmin, the culture shock of carrying out these tasks must have been especially jarring.
Dr. SubbaRow went on to earn a diploma from Harvard Medical School, also in Boston, and became a junior faculty member. As a foreigner, Dr. Mukherjee wrote, Dr. SubbaRow was a “reclusive, nocturnal, heavily accented vegetarian,” so different from his colleagues that advancement seemed impossible. Despite his pioneering biochemistry work, Harvard later declined to offer Dr. SubbaRow a tenured faculty position.
By the early 1940s, he took a job at an upstate New York pharmaceutical company called Lederle Labs (later purchased by Pfizer). At Lederle, Dr. SubbaRow strove to synthesize the vitamin known as folic acid. He ended up creating a kind of antivitamin, a lookalike that acted like folic acid but only succeeded in gumming up the works in receptors. But what good would it do to stop the body from absorbing folic acid? Plenty, it turned out.
Discoveries pile up, but credit and fame prove elusive
Dr. SubbaRow was no stranger to producing landmark biological work. He’d previously codiscovered phosphocreatine and ATP, which are crucial to muscular contractions. However, “in 1935, he had to disown the extent of his role in the discovery of the color test related to phosphorus, instead giving the credit to his co-author, who was being considered for promotion to a full professorship at Harvard,” wrote author Gerald Posner in his 2020 book, “Pharma: Greed, Lies and the Poisoning of America.”
Houston-area oncologist Kirtan Nautiyal, MD, who paid tribute to Dr. SubbaRow in a 2018 article, contended that “with his Indian instinct for self-effacement, he had irreparably sabotaged his own career.”
Dr. SubbaRow and his team also developed “the first effective treatment of filariasis, which causes elephantiasis of the lower limbs and genitals in millions of people, mainly in tropical countries,” Dr. Nautiyal wrote. “Later in the decade, his antibiotic program generated polymyxin, the first effective treatment against the class of bacteria called Gram negatives, and aureomycin, the first “broad-spectrum’ antibiotic.” (Aureomycin is also the first tetracycline antibiotic.)
Dr. SubbaRow’s discovery of a folic acid antagonist would again go largely unheralded. But first came the realization that folic acid made childhood leukemia worse, not better, and the prospect that this process could potentially be reversed.
Rise of methotrexate and fall of leukemia
In Boston, Sidney Farber, MD, a Boston pathologist, was desperate to help Robert Sandler, a 2-year-old leukemia patient. Dr. Farber contacted his ex-colleague Dr. SubbaRow to request a supply of aminopterin, an early version of methotrexate that Dr. SubbaRow and his team had developed. Dr. Farber injected Robert with the substance and within 3 days, the toddler’s white blood count started falling – fast. He stopped bleeding, resumed eating, and once again seemed almost identical to his twin brother, as Dr. Mukherjee wrote in his book.
Leukemia had never gone into remission before. Unfortunately, the treatment only worked temporarily. Robert, like other children treated with the drug, relapsed and died within months. But Dr. Farber “saw a door open” – a chemical, a kind of chemotherapy, that could turn back cancer. In the case of folic acid antagonists, they do so by stopping cancer cells from replicating.
Methotrexate, a related agent synthesized by Dr. SubbaRow, would become a mainstay of leukemia treatment and begin to produce long-term remission from acute lymphoblastic leukemia in 1970, when combination chemotherapy was developed.
Other cancers fell to methotrexate treatment. “Previous assumptions that cancer was nearly always fatal were revised, and the field of medical oncology (treatment of cancer with chemotherapy), which had not previously existed, was formally established in 1971,” according to the National Cancer Institute’s history of methotrexate. This account does not mention Dr. SubbaRow.
Death takes the doctor, but his legacy remains
In biographies, as well as his own words, Dr. SubbaRow comes across as a prickly, hard-driving workaholic who had little interest in intimate human connections. “It is not good to ask in every letter when I will be back,” he wrote to his wife back in India, before cutting off ties completely in the early 1930s. “I will come as early as possible. ... I do not want to write anything more.”
It seems, as his biographer S.P.K. Gupta noted, that “he was quite determined that the time allotted to him on Earth should be completely devoted to finding cures for ailments that plagued mankind.”
Still, Dr. SubbaRow’s research team was devoted to him, and he had plenty of reasons to be bitter, such as the prejudice and isolation he encountered in the United States and earlier, in British-run India. According to Mr. Posner’s book, even as a young medical student, Dr. SubbaRow heeded the call of Indian independence activist Mohandas Gandhi. He “refused the British surgical gown given him at school and instead donned a traditional and simple cotton Khadi. That act of defiance cost SubbaRow the college degree that was necessary for him to get into the State Medical College.”
During the last year of his life, Dr. SubbaRow faced yet another humiliation: In his landmark 1948 study about aminopterin as a treatment for leukemia, his colleague Dr. Farber failed to credit him, an “astonishing omission” as Yaddanapudi Ravindranath, MBBS, a pediatric hematologist/oncologist at Wayne State University, Detroit, put it. “From everything I know, Dr. Farber spent the rest of his career apologizing and trying to make amends for it,” Dr. Ravindranath said in an interview.
A career cut short, and a lasting legacy
In 1948, at the age of 53, Dr. SubbaRow suddenly died. “Many think Dr. SubbaRow would have won [the] Nobel Prize had he lived a few years longer,” said Dr. Ravindranath.
Like Dr. SubbaRow, Dr. Ravindranath was born in Andhra Pradesh state, near the city of Chennai formerly known as Madras. “Being a compatriot, in a way I continue his legacy, and I am obviously proud of him,” said Dr. Ravindranath, who has conducted his own landmark research regarding methotrexate and leukemia.
Nearly 75 years after Dr. SubbaRow’s death, Indian-born physicians like Dr. Ravindranath continue to honor him in print, trying to ensure that he’s not forgotten. Methotrexate remains a crucial treatment for leukemia, along with a long list of other ailments, including psoriasis.
Recognition for “Yella” may have come late and infrequently, but a Lederle Laboratories research library named after him offered Dr. SubbaRow a kind of immortality. A plaque there memorialized him in stone as a scientist, teacher, philosopher, and humanitarian, featuring the quote: “Science simply prolongs life. Religion deepens it.”
By all accounts, Dr. SubbaRow was a man of science and faith who had faith in science.
Obesity increasing the risk for cancer: It’s complicated
The link between obesity and cancer has increasingly been emphasized in public health messages, but is the current message correct?
“Being overweight or having obesity increases your risk of getting cancer,” warns the U.S. Centers for Disease Control and Prevention. It warns that overweight/obesity is “linked with a higher risk of getting 13 types of cancer ... [which] make up 40% of all cancers diagnosed in the United States each year.”
But that message, which is also promulgated by many cancer organizations, is based on data from observational studies, which have many limitations.
In addition, it found an inverse relationship for breast cancer, in which early-life obesity was associated with a reduced risk of breast cancer, and the relationship with obesity was “complicated” for lung and prostate cancer.
The study, headed by Zhe Fang, MBBS, Harvard T. H. Chan School of Public Health, Boston, Mass., was published in the Journal of the National Cancer Institute
“For a seemingly straightforward question of whether excessive body fatness causes cancer, the answer may not be straightforward after all,” writes Song Yao, PhD, professor of oncology, Roswell Park Comprehensive Cancer Center, Buffalo, N.Y., in an accompanying editorial
“How to craft a simple public health message to convey the complexity and nuances of the relationships may be a challenge to be grappled with going forward,” he added.
In an interview, Dr. Yao said that it “really depends on what kind of message you want to get out.”
“If you want to talk about cancer overall, as one disease, we all know that a clear association with obesity does not exist,” he said. “It’s not that simple.”
“You really cannot say that obesity increases cancer risk overall,” he said.
For some cancers included in the study, Dr. Yao continued, it was “very clear that obesity increased the risk ... but for some other cancer types, we either don’t have enough data yet or the association is not as consistent.”
This, he said, is especially the case for prostate and lung cancer.
All of this indicates that there is a complex relationship between obesity and cancer risk, he maintains.
“We always think obesity is bad, not only for cancer but also for more common conditions, like hypertension, diabetes, and cardiovascular disease,” Dr. Yao noted. This points to the link between obesity and chronic inflammation, he added.
However, there are also other hypotheses, including synthesis of estrogen in adipose tissue, which may explain the link between obesity and breast cancer risk in older women.
However, in younger women, obesity protects against breast cancer, and “we really don’t know why,” Dr. Yao said.
The new study used Mendelian randomization to examine these relationships. This is a “new tool that we have developed over the past 20 years or so, largely because there is so much data coming from genome-wide association studies,” Dr. Yao explained.
It has “advantages” over other methods, including observational studies. One of its strengths is that it is “not impacted by reverse causality,” because genetic risk does not change over time.
However, he said, it is “quite straightforward to think that the genetics do not change, but at the same time, the environment we live in throughout our life course changes,” and the impact of genetic variants may be “washed out.”
How genetics influences cancer risk may therefore change over time, and it is a “dynamic process,” Dr. Yao commented.
In addition, this approach has its own limitations, he said, because it depends on how much of the variation in a given measure can be attributed to genetic factors.
New conclusions
In their study, Dr. Fang and colleagues reviewed 204 meta-analyses of 2,179 individual estimates from 507 cohort or case-control studies. They found “strong evidence” that supports the association between obesity and 11 cancers.
These are esophageal adenocarcinoma, multiple myeloma, and cancers of the gastric cardia, colon, rectum, biliary tract system, pancreas, breast, endometrium, ovary, and kidney.
They note, however, that the associations “may be causal for some malignancies” but that the co-occurrence of obesity with various cancer risk factors means that others may be “susceptible to potential confounding bias.”
To overcome some of these limitations, the team looked to Mendelian randomization studies that examined the association between genetic variants linked to body mass index (BMI), indicating lifetime risk of high BMI, and cancer risk for a range of cancer types.
These Mendelian randomization studies were then compared with the results of large-scale conventional observational studies, as well as with evidence in reports from the International Agency for Research on Cancer and the World Cancer Research Fund–American Institute of Cancer Research, which also include experimental studies.
The researchers say that, overall, the Mendelian randomization studies “further establish the causality of obesity” with six cancer types: colorectal, endometrial, ovarian, kidney, and pancreatic cancer, and esophageal adenocarcinoma.
In addition, these studies further establish the inverse relationship of early-life obesity with breast cancer.
However, the approach could not confirm a positive association between obesity and gallbladder and gastric cardia cancer, as well as multiple myeloma.
“This could be due to low power,” the team suggests, “and larger studies are required.”
With respect to lung cancer, the Mendelian randomization identified a positive association with obesity that supports the inverse association identified in observational studies, that is, that obesity may reduce the risk for lung cancer.
The researchers suggest this may reflect reverse causality related to the loss of lean body mass before diagnosis, as well as confounding by smoking.
For prostate cancer, the evidence was “conflicting” and “implies a complicated role of obesity,” Dr. Zhang and colleagues comment.
The link between obesity and lower prostate-specific antigen levels, they suggest, may result in a detection bias by masking the presence of prostate cancer, or it “could be biological” in origin, owing to reduced androgen levels.
For six cancer types for which a causal relationship with obesity could be established, the effect estimates from the Mendelian randomization studies were stronger than those seen in conventional studies, with the magnitude of risk ranging from 1.14-fold for early-life obesity and breast cancer to 1.37-fold for adult obesity and esophageal adenocarcinoma.
In another editorial accompanying the new study, Graham A. Colditz, MD, DrPH, from Washington University School of Medicine, St. Louis, underlined that childhood and adolescent obesity and their contribution to cancer risk need further attention.
“To reap the reward from past research, we must act to implement effective strategies to reduce childhood and adolescent adiposity, reduce excess weight gain in adult years, and maintain a healthy weight,” he writes.
“This will require us to change the way we live, but COVID-19 has shown we can make changes to how we live and work. Let us keep the changes we have already made, or take on new ones, that will cut our collective cancer toll,” he implores.
No funding for the study was described. Dr. Colditz is supported by the Breast Cancer Research Foundation. No other relevant financial relationships were described.
A version of this article first appeared on Medscape.com.
The link between obesity and cancer has increasingly been emphasized in public health messages, but is the current message correct?
“Being overweight or having obesity increases your risk of getting cancer,” warns the U.S. Centers for Disease Control and Prevention. It warns that overweight/obesity is “linked with a higher risk of getting 13 types of cancer ... [which] make up 40% of all cancers diagnosed in the United States each year.”
But that message, which is also promulgated by many cancer organizations, is based on data from observational studies, which have many limitations.
In addition, it found an inverse relationship for breast cancer, in which early-life obesity was associated with a reduced risk of breast cancer, and the relationship with obesity was “complicated” for lung and prostate cancer.
The study, headed by Zhe Fang, MBBS, Harvard T. H. Chan School of Public Health, Boston, Mass., was published in the Journal of the National Cancer Institute
“For a seemingly straightforward question of whether excessive body fatness causes cancer, the answer may not be straightforward after all,” writes Song Yao, PhD, professor of oncology, Roswell Park Comprehensive Cancer Center, Buffalo, N.Y., in an accompanying editorial
“How to craft a simple public health message to convey the complexity and nuances of the relationships may be a challenge to be grappled with going forward,” he added.
In an interview, Dr. Yao said that it “really depends on what kind of message you want to get out.”
“If you want to talk about cancer overall, as one disease, we all know that a clear association with obesity does not exist,” he said. “It’s not that simple.”
“You really cannot say that obesity increases cancer risk overall,” he said.
For some cancers included in the study, Dr. Yao continued, it was “very clear that obesity increased the risk ... but for some other cancer types, we either don’t have enough data yet or the association is not as consistent.”
This, he said, is especially the case for prostate and lung cancer.
All of this indicates that there is a complex relationship between obesity and cancer risk, he maintains.
“We always think obesity is bad, not only for cancer but also for more common conditions, like hypertension, diabetes, and cardiovascular disease,” Dr. Yao noted. This points to the link between obesity and chronic inflammation, he added.
However, there are also other hypotheses, including synthesis of estrogen in adipose tissue, which may explain the link between obesity and breast cancer risk in older women.
However, in younger women, obesity protects against breast cancer, and “we really don’t know why,” Dr. Yao said.
The new study used Mendelian randomization to examine these relationships. This is a “new tool that we have developed over the past 20 years or so, largely because there is so much data coming from genome-wide association studies,” Dr. Yao explained.
It has “advantages” over other methods, including observational studies. One of its strengths is that it is “not impacted by reverse causality,” because genetic risk does not change over time.
However, he said, it is “quite straightforward to think that the genetics do not change, but at the same time, the environment we live in throughout our life course changes,” and the impact of genetic variants may be “washed out.”
How genetics influences cancer risk may therefore change over time, and it is a “dynamic process,” Dr. Yao commented.
In addition, this approach has its own limitations, he said, because it depends on how much of the variation in a given measure can be attributed to genetic factors.
New conclusions
In their study, Dr. Fang and colleagues reviewed 204 meta-analyses of 2,179 individual estimates from 507 cohort or case-control studies. They found “strong evidence” that supports the association between obesity and 11 cancers.
These are esophageal adenocarcinoma, multiple myeloma, and cancers of the gastric cardia, colon, rectum, biliary tract system, pancreas, breast, endometrium, ovary, and kidney.
They note, however, that the associations “may be causal for some malignancies” but that the co-occurrence of obesity with various cancer risk factors means that others may be “susceptible to potential confounding bias.”
To overcome some of these limitations, the team looked to Mendelian randomization studies that examined the association between genetic variants linked to body mass index (BMI), indicating lifetime risk of high BMI, and cancer risk for a range of cancer types.
These Mendelian randomization studies were then compared with the results of large-scale conventional observational studies, as well as with evidence in reports from the International Agency for Research on Cancer and the World Cancer Research Fund–American Institute of Cancer Research, which also include experimental studies.
The researchers say that, overall, the Mendelian randomization studies “further establish the causality of obesity” with six cancer types: colorectal, endometrial, ovarian, kidney, and pancreatic cancer, and esophageal adenocarcinoma.
In addition, these studies further establish the inverse relationship of early-life obesity with breast cancer.
However, the approach could not confirm a positive association between obesity and gallbladder and gastric cardia cancer, as well as multiple myeloma.
“This could be due to low power,” the team suggests, “and larger studies are required.”
With respect to lung cancer, the Mendelian randomization identified a positive association with obesity that supports the inverse association identified in observational studies, that is, that obesity may reduce the risk for lung cancer.
The researchers suggest this may reflect reverse causality related to the loss of lean body mass before diagnosis, as well as confounding by smoking.
For prostate cancer, the evidence was “conflicting” and “implies a complicated role of obesity,” Dr. Zhang and colleagues comment.
The link between obesity and lower prostate-specific antigen levels, they suggest, may result in a detection bias by masking the presence of prostate cancer, or it “could be biological” in origin, owing to reduced androgen levels.
For six cancer types for which a causal relationship with obesity could be established, the effect estimates from the Mendelian randomization studies were stronger than those seen in conventional studies, with the magnitude of risk ranging from 1.14-fold for early-life obesity and breast cancer to 1.37-fold for adult obesity and esophageal adenocarcinoma.
In another editorial accompanying the new study, Graham A. Colditz, MD, DrPH, from Washington University School of Medicine, St. Louis, underlined that childhood and adolescent obesity and their contribution to cancer risk need further attention.
“To reap the reward from past research, we must act to implement effective strategies to reduce childhood and adolescent adiposity, reduce excess weight gain in adult years, and maintain a healthy weight,” he writes.
“This will require us to change the way we live, but COVID-19 has shown we can make changes to how we live and work. Let us keep the changes we have already made, or take on new ones, that will cut our collective cancer toll,” he implores.
No funding for the study was described. Dr. Colditz is supported by the Breast Cancer Research Foundation. No other relevant financial relationships were described.
A version of this article first appeared on Medscape.com.
The link between obesity and cancer has increasingly been emphasized in public health messages, but is the current message correct?
“Being overweight or having obesity increases your risk of getting cancer,” warns the U.S. Centers for Disease Control and Prevention. It warns that overweight/obesity is “linked with a higher risk of getting 13 types of cancer ... [which] make up 40% of all cancers diagnosed in the United States each year.”
But that message, which is also promulgated by many cancer organizations, is based on data from observational studies, which have many limitations.
In addition, it found an inverse relationship for breast cancer, in which early-life obesity was associated with a reduced risk of breast cancer, and the relationship with obesity was “complicated” for lung and prostate cancer.
The study, headed by Zhe Fang, MBBS, Harvard T. H. Chan School of Public Health, Boston, Mass., was published in the Journal of the National Cancer Institute
“For a seemingly straightforward question of whether excessive body fatness causes cancer, the answer may not be straightforward after all,” writes Song Yao, PhD, professor of oncology, Roswell Park Comprehensive Cancer Center, Buffalo, N.Y., in an accompanying editorial
“How to craft a simple public health message to convey the complexity and nuances of the relationships may be a challenge to be grappled with going forward,” he added.
In an interview, Dr. Yao said that it “really depends on what kind of message you want to get out.”
“If you want to talk about cancer overall, as one disease, we all know that a clear association with obesity does not exist,” he said. “It’s not that simple.”
“You really cannot say that obesity increases cancer risk overall,” he said.
For some cancers included in the study, Dr. Yao continued, it was “very clear that obesity increased the risk ... but for some other cancer types, we either don’t have enough data yet or the association is not as consistent.”
This, he said, is especially the case for prostate and lung cancer.
All of this indicates that there is a complex relationship between obesity and cancer risk, he maintains.
“We always think obesity is bad, not only for cancer but also for more common conditions, like hypertension, diabetes, and cardiovascular disease,” Dr. Yao noted. This points to the link between obesity and chronic inflammation, he added.
However, there are also other hypotheses, including synthesis of estrogen in adipose tissue, which may explain the link between obesity and breast cancer risk in older women.
However, in younger women, obesity protects against breast cancer, and “we really don’t know why,” Dr. Yao said.
The new study used Mendelian randomization to examine these relationships. This is a “new tool that we have developed over the past 20 years or so, largely because there is so much data coming from genome-wide association studies,” Dr. Yao explained.
It has “advantages” over other methods, including observational studies. One of its strengths is that it is “not impacted by reverse causality,” because genetic risk does not change over time.
However, he said, it is “quite straightforward to think that the genetics do not change, but at the same time, the environment we live in throughout our life course changes,” and the impact of genetic variants may be “washed out.”
How genetics influences cancer risk may therefore change over time, and it is a “dynamic process,” Dr. Yao commented.
In addition, this approach has its own limitations, he said, because it depends on how much of the variation in a given measure can be attributed to genetic factors.
New conclusions
In their study, Dr. Fang and colleagues reviewed 204 meta-analyses of 2,179 individual estimates from 507 cohort or case-control studies. They found “strong evidence” that supports the association between obesity and 11 cancers.
These are esophageal adenocarcinoma, multiple myeloma, and cancers of the gastric cardia, colon, rectum, biliary tract system, pancreas, breast, endometrium, ovary, and kidney.
They note, however, that the associations “may be causal for some malignancies” but that the co-occurrence of obesity with various cancer risk factors means that others may be “susceptible to potential confounding bias.”
To overcome some of these limitations, the team looked to Mendelian randomization studies that examined the association between genetic variants linked to body mass index (BMI), indicating lifetime risk of high BMI, and cancer risk for a range of cancer types.
These Mendelian randomization studies were then compared with the results of large-scale conventional observational studies, as well as with evidence in reports from the International Agency for Research on Cancer and the World Cancer Research Fund–American Institute of Cancer Research, which also include experimental studies.
The researchers say that, overall, the Mendelian randomization studies “further establish the causality of obesity” with six cancer types: colorectal, endometrial, ovarian, kidney, and pancreatic cancer, and esophageal adenocarcinoma.
In addition, these studies further establish the inverse relationship of early-life obesity with breast cancer.
However, the approach could not confirm a positive association between obesity and gallbladder and gastric cardia cancer, as well as multiple myeloma.
“This could be due to low power,” the team suggests, “and larger studies are required.”
With respect to lung cancer, the Mendelian randomization identified a positive association with obesity that supports the inverse association identified in observational studies, that is, that obesity may reduce the risk for lung cancer.
The researchers suggest this may reflect reverse causality related to the loss of lean body mass before diagnosis, as well as confounding by smoking.
For prostate cancer, the evidence was “conflicting” and “implies a complicated role of obesity,” Dr. Zhang and colleagues comment.
The link between obesity and lower prostate-specific antigen levels, they suggest, may result in a detection bias by masking the presence of prostate cancer, or it “could be biological” in origin, owing to reduced androgen levels.
For six cancer types for which a causal relationship with obesity could be established, the effect estimates from the Mendelian randomization studies were stronger than those seen in conventional studies, with the magnitude of risk ranging from 1.14-fold for early-life obesity and breast cancer to 1.37-fold for adult obesity and esophageal adenocarcinoma.
In another editorial accompanying the new study, Graham A. Colditz, MD, DrPH, from Washington University School of Medicine, St. Louis, underlined that childhood and adolescent obesity and their contribution to cancer risk need further attention.
“To reap the reward from past research, we must act to implement effective strategies to reduce childhood and adolescent adiposity, reduce excess weight gain in adult years, and maintain a healthy weight,” he writes.
“This will require us to change the way we live, but COVID-19 has shown we can make changes to how we live and work. Let us keep the changes we have already made, or take on new ones, that will cut our collective cancer toll,” he implores.
No funding for the study was described. Dr. Colditz is supported by the Breast Cancer Research Foundation. No other relevant financial relationships were described.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE NATIONAL CANCER INSTITUTE
Repurposed drug could revolutionize stem cell transplantation
When the Food and Drug Administration approved abatacept in December 2021 as prophylaxis for acute graft-versus-host disease (aGVHD) in adults and children 2 years and older who are undergoing hematopoietic stem cell transplantation (HSCT), the announcement was notable for couple of key reasons.
Abatacept was approved based on results from the ABA2 trial, which evaluated 142 adults and children with hematologic malignancies who received a four-dose regimen of abatacept in addition to standard of care – a calcineurin inhibitor (CNI) plus methotrexate (MTX) – prior to undergoing an 8/8 HLA-matched, unrelated donor (URD) HSCT, or standard of care alone.
Another arm of the trial examined 43 recipients of a 7/8 HLA-mismatched URD HSCT who received abatacept plus standard of care, compared with a prespecified registry cohort group provided by the Center for International Blood and Marrow Transplant Research, who received CNI and MTX.
Results published in the Journal of Clinical Oncology showed the proportion of patients in the 8/8 group with severe aGVHD in the abatacept group 100 days after HSCT was not significantly lower, compared with the standard of care group (6.8% vs. 14.8%; P = .13), but there was a significant improvement in severe aGVHD–free survival (SGFS) 180 days after HSCT in the abatacept group, compared with the group that received standard of care (93.2% vs. 80%; P = .05).
Among patients in the 7/8 group, there was a significant difference in the proportion of patients with severe aGVHD favoring the abatacept group (2.3% vs. 30.2%; P < .001), and significantly improved SGFS, compared with the CIBMTR registry cohort (97.7% vs. 58.7%; P < .001)
A post hoc analysis of ABA2 published as a research letter in Blood Advances assessed abatacept using real-world data from CIBMTR. Researchers compared the 8/8 group that received standard of care with the 7/8 group that received abatacept plus standard of care and found no significant differences between relapse-free survival and overall survival for patients in the 8/8 group (adjusted hazard ratio, 0.60; 95% confidence interval, 0.28-1.28; P = .19) and 7/8 group (aHR, 0.77; 95% CI, 0.34-1.71; P = .51).
The results suggest “abatacept may eliminate that risk of a mismatched transplant in the setting of that analysis and that small cohort that was assessed there, which is good news for patients that may not have a fully matched donor on the registry,” said Stephen Spellman, vice president at Be The Match Research (operated by the National Marrow Donor Program), and senior scientific director of CIBMTR. The findings from ABA2 “were even more impressive than necessarily expected, especially in the 7/8 arm. This is a truly substantial reduction in acute GVHD risk in that patient population,” he said in an interview.
Could abatacept fuel greater use of mismatched, unrelated donors?
One downside of using an HLA-mismatched donor is the potential risk of developing aGVHD, Doris M. Ponce, MD, a hematologic oncologist with Memorial Sloan Kettering Cancer Center in New York, who was not involved with the research, said in an interview.
Potential risk factors for aGVHD include “having a female multiparous donor, HLA-mismatched donor, unrelated donor, donor and recipient age (>40 years), [peripheral blood stem cell] stem cell graft, recipient [cytomegalovirus] serostatus (recipient/donor), myeloablative conditioning, [total body irradiation]–based conditioning, [and] gut microbiome dysbiosis,” Dr. Ponce explained.
Abatacept’s approval may have particular relevance for people of color. “It’s been understood for a long time that the likelihood of finding an 8/8 well-matched, volunteer unrelated donor varies by race or ethnicity,” Steven Devine, MD, a board-certified oncologist who is chief medical officer of Be The Match and associate scientific director at CIBMTR, said in an interview.
Mr. Spellman noted that, of the more than 35 million donors on worldwide registries accessible through the National Marrow Donor Program’s Be The Match Registry, “the match rates differ quite substantially by race and ethnicity.” Approximately 29% of African Americans find a full match on the registry, compared with 81% of Whites, 49% of Hispanics, and 47% Asian/Pacific Islanders.
“Being able to utilize a 7/8 match in a safe, effective manner using abatacept, which abatacept has been approved for, does increase those match rates quite substantially,” he explained. Among African Americans, this means the match rate increases to 84%, among Hispanics and Asian/Pacific Islanders to approximately 90%, and among Whites to about 98%.
That kind of improvement in the match rate is “the equivalent of adding more than more than 10 million ethnically diverse donors to the registry in 1 day,” Dr. Devine said. “The availability of abatacept could really level the playing field for patients in need of a lifesaving transplant.”
Further study of abatacept
With abatacept, “I think the results are really encouraging, and I think that further studies [are needed] to better define how the drug would work and whether it can later prevent chronic graft versus host disease,” Dr. Devine said. He said the ABA3 trial has been designed around this question, with the hypothesis that extending abatacept to an eight-dose regimen may help with chronic GVHD.
Although the FDA’s approval of abatacept was recent, Mr. Spellman said, Be The Match has seen early indications that mismatched donors in the registry are being used, which may point to an increased utilization of abatacept. “Through October to December of 2021, there was a pretty substantial increase in the use of mismatched, unrelated donors in that time frame.”
Dr. Devine noted that he is seeing a lot of interest in using abatacept. “I think people are still learning how best to incorporate it into their standard of care right now.”
Meanwhile, Memorial Sloan Kettering Cancer Center is already planning to use abatacept, Dr. Ponce noted. “We have abatacept in our formulary for adult and children, and are planning on using it for patients receiving an unmodified graft from a [matched unrelated donor] or 1-allele [mismatched unrelated donor] using CNI and MTX-based GVHD prophylaxis.”
Dr. Devine and Mr. Spellman are employees of Be The Match and CIBMTR, which provided the registry control group for the ABA2 trial. Dr. Devine also reported that he has been a scientific advisory board member for Bristol-Myers Squibb. Dr. Ponce reports no relevant conflicts of interest.
When the Food and Drug Administration approved abatacept in December 2021 as prophylaxis for acute graft-versus-host disease (aGVHD) in adults and children 2 years and older who are undergoing hematopoietic stem cell transplantation (HSCT), the announcement was notable for couple of key reasons.
Abatacept was approved based on results from the ABA2 trial, which evaluated 142 adults and children with hematologic malignancies who received a four-dose regimen of abatacept in addition to standard of care – a calcineurin inhibitor (CNI) plus methotrexate (MTX) – prior to undergoing an 8/8 HLA-matched, unrelated donor (URD) HSCT, or standard of care alone.
Another arm of the trial examined 43 recipients of a 7/8 HLA-mismatched URD HSCT who received abatacept plus standard of care, compared with a prespecified registry cohort group provided by the Center for International Blood and Marrow Transplant Research, who received CNI and MTX.
Results published in the Journal of Clinical Oncology showed the proportion of patients in the 8/8 group with severe aGVHD in the abatacept group 100 days after HSCT was not significantly lower, compared with the standard of care group (6.8% vs. 14.8%; P = .13), but there was a significant improvement in severe aGVHD–free survival (SGFS) 180 days after HSCT in the abatacept group, compared with the group that received standard of care (93.2% vs. 80%; P = .05).
Among patients in the 7/8 group, there was a significant difference in the proportion of patients with severe aGVHD favoring the abatacept group (2.3% vs. 30.2%; P < .001), and significantly improved SGFS, compared with the CIBMTR registry cohort (97.7% vs. 58.7%; P < .001)
A post hoc analysis of ABA2 published as a research letter in Blood Advances assessed abatacept using real-world data from CIBMTR. Researchers compared the 8/8 group that received standard of care with the 7/8 group that received abatacept plus standard of care and found no significant differences between relapse-free survival and overall survival for patients in the 8/8 group (adjusted hazard ratio, 0.60; 95% confidence interval, 0.28-1.28; P = .19) and 7/8 group (aHR, 0.77; 95% CI, 0.34-1.71; P = .51).
The results suggest “abatacept may eliminate that risk of a mismatched transplant in the setting of that analysis and that small cohort that was assessed there, which is good news for patients that may not have a fully matched donor on the registry,” said Stephen Spellman, vice president at Be The Match Research (operated by the National Marrow Donor Program), and senior scientific director of CIBMTR. The findings from ABA2 “were even more impressive than necessarily expected, especially in the 7/8 arm. This is a truly substantial reduction in acute GVHD risk in that patient population,” he said in an interview.
Could abatacept fuel greater use of mismatched, unrelated donors?
One downside of using an HLA-mismatched donor is the potential risk of developing aGVHD, Doris M. Ponce, MD, a hematologic oncologist with Memorial Sloan Kettering Cancer Center in New York, who was not involved with the research, said in an interview.
Potential risk factors for aGVHD include “having a female multiparous donor, HLA-mismatched donor, unrelated donor, donor and recipient age (>40 years), [peripheral blood stem cell] stem cell graft, recipient [cytomegalovirus] serostatus (recipient/donor), myeloablative conditioning, [total body irradiation]–based conditioning, [and] gut microbiome dysbiosis,” Dr. Ponce explained.
Abatacept’s approval may have particular relevance for people of color. “It’s been understood for a long time that the likelihood of finding an 8/8 well-matched, volunteer unrelated donor varies by race or ethnicity,” Steven Devine, MD, a board-certified oncologist who is chief medical officer of Be The Match and associate scientific director at CIBMTR, said in an interview.
Mr. Spellman noted that, of the more than 35 million donors on worldwide registries accessible through the National Marrow Donor Program’s Be The Match Registry, “the match rates differ quite substantially by race and ethnicity.” Approximately 29% of African Americans find a full match on the registry, compared with 81% of Whites, 49% of Hispanics, and 47% Asian/Pacific Islanders.
“Being able to utilize a 7/8 match in a safe, effective manner using abatacept, which abatacept has been approved for, does increase those match rates quite substantially,” he explained. Among African Americans, this means the match rate increases to 84%, among Hispanics and Asian/Pacific Islanders to approximately 90%, and among Whites to about 98%.
That kind of improvement in the match rate is “the equivalent of adding more than more than 10 million ethnically diverse donors to the registry in 1 day,” Dr. Devine said. “The availability of abatacept could really level the playing field for patients in need of a lifesaving transplant.”
Further study of abatacept
With abatacept, “I think the results are really encouraging, and I think that further studies [are needed] to better define how the drug would work and whether it can later prevent chronic graft versus host disease,” Dr. Devine said. He said the ABA3 trial has been designed around this question, with the hypothesis that extending abatacept to an eight-dose regimen may help with chronic GVHD.
Although the FDA’s approval of abatacept was recent, Mr. Spellman said, Be The Match has seen early indications that mismatched donors in the registry are being used, which may point to an increased utilization of abatacept. “Through October to December of 2021, there was a pretty substantial increase in the use of mismatched, unrelated donors in that time frame.”
Dr. Devine noted that he is seeing a lot of interest in using abatacept. “I think people are still learning how best to incorporate it into their standard of care right now.”
Meanwhile, Memorial Sloan Kettering Cancer Center is already planning to use abatacept, Dr. Ponce noted. “We have abatacept in our formulary for adult and children, and are planning on using it for patients receiving an unmodified graft from a [matched unrelated donor] or 1-allele [mismatched unrelated donor] using CNI and MTX-based GVHD prophylaxis.”
Dr. Devine and Mr. Spellman are employees of Be The Match and CIBMTR, which provided the registry control group for the ABA2 trial. Dr. Devine also reported that he has been a scientific advisory board member for Bristol-Myers Squibb. Dr. Ponce reports no relevant conflicts of interest.
When the Food and Drug Administration approved abatacept in December 2021 as prophylaxis for acute graft-versus-host disease (aGVHD) in adults and children 2 years and older who are undergoing hematopoietic stem cell transplantation (HSCT), the announcement was notable for couple of key reasons.
Abatacept was approved based on results from the ABA2 trial, which evaluated 142 adults and children with hematologic malignancies who received a four-dose regimen of abatacept in addition to standard of care – a calcineurin inhibitor (CNI) plus methotrexate (MTX) – prior to undergoing an 8/8 HLA-matched, unrelated donor (URD) HSCT, or standard of care alone.
Another arm of the trial examined 43 recipients of a 7/8 HLA-mismatched URD HSCT who received abatacept plus standard of care, compared with a prespecified registry cohort group provided by the Center for International Blood and Marrow Transplant Research, who received CNI and MTX.
Results published in the Journal of Clinical Oncology showed the proportion of patients in the 8/8 group with severe aGVHD in the abatacept group 100 days after HSCT was not significantly lower, compared with the standard of care group (6.8% vs. 14.8%; P = .13), but there was a significant improvement in severe aGVHD–free survival (SGFS) 180 days after HSCT in the abatacept group, compared with the group that received standard of care (93.2% vs. 80%; P = .05).
Among patients in the 7/8 group, there was a significant difference in the proportion of patients with severe aGVHD favoring the abatacept group (2.3% vs. 30.2%; P < .001), and significantly improved SGFS, compared with the CIBMTR registry cohort (97.7% vs. 58.7%; P < .001)
A post hoc analysis of ABA2 published as a research letter in Blood Advances assessed abatacept using real-world data from CIBMTR. Researchers compared the 8/8 group that received standard of care with the 7/8 group that received abatacept plus standard of care and found no significant differences between relapse-free survival and overall survival for patients in the 8/8 group (adjusted hazard ratio, 0.60; 95% confidence interval, 0.28-1.28; P = .19) and 7/8 group (aHR, 0.77; 95% CI, 0.34-1.71; P = .51).
The results suggest “abatacept may eliminate that risk of a mismatched transplant in the setting of that analysis and that small cohort that was assessed there, which is good news for patients that may not have a fully matched donor on the registry,” said Stephen Spellman, vice president at Be The Match Research (operated by the National Marrow Donor Program), and senior scientific director of CIBMTR. The findings from ABA2 “were even more impressive than necessarily expected, especially in the 7/8 arm. This is a truly substantial reduction in acute GVHD risk in that patient population,” he said in an interview.
Could abatacept fuel greater use of mismatched, unrelated donors?
One downside of using an HLA-mismatched donor is the potential risk of developing aGVHD, Doris M. Ponce, MD, a hematologic oncologist with Memorial Sloan Kettering Cancer Center in New York, who was not involved with the research, said in an interview.
Potential risk factors for aGVHD include “having a female multiparous donor, HLA-mismatched donor, unrelated donor, donor and recipient age (>40 years), [peripheral blood stem cell] stem cell graft, recipient [cytomegalovirus] serostatus (recipient/donor), myeloablative conditioning, [total body irradiation]–based conditioning, [and] gut microbiome dysbiosis,” Dr. Ponce explained.
Abatacept’s approval may have particular relevance for people of color. “It’s been understood for a long time that the likelihood of finding an 8/8 well-matched, volunteer unrelated donor varies by race or ethnicity,” Steven Devine, MD, a board-certified oncologist who is chief medical officer of Be The Match and associate scientific director at CIBMTR, said in an interview.
Mr. Spellman noted that, of the more than 35 million donors on worldwide registries accessible through the National Marrow Donor Program’s Be The Match Registry, “the match rates differ quite substantially by race and ethnicity.” Approximately 29% of African Americans find a full match on the registry, compared with 81% of Whites, 49% of Hispanics, and 47% Asian/Pacific Islanders.
“Being able to utilize a 7/8 match in a safe, effective manner using abatacept, which abatacept has been approved for, does increase those match rates quite substantially,” he explained. Among African Americans, this means the match rate increases to 84%, among Hispanics and Asian/Pacific Islanders to approximately 90%, and among Whites to about 98%.
That kind of improvement in the match rate is “the equivalent of adding more than more than 10 million ethnically diverse donors to the registry in 1 day,” Dr. Devine said. “The availability of abatacept could really level the playing field for patients in need of a lifesaving transplant.”
Further study of abatacept
With abatacept, “I think the results are really encouraging, and I think that further studies [are needed] to better define how the drug would work and whether it can later prevent chronic graft versus host disease,” Dr. Devine said. He said the ABA3 trial has been designed around this question, with the hypothesis that extending abatacept to an eight-dose regimen may help with chronic GVHD.
Although the FDA’s approval of abatacept was recent, Mr. Spellman said, Be The Match has seen early indications that mismatched donors in the registry are being used, which may point to an increased utilization of abatacept. “Through October to December of 2021, there was a pretty substantial increase in the use of mismatched, unrelated donors in that time frame.”
Dr. Devine noted that he is seeing a lot of interest in using abatacept. “I think people are still learning how best to incorporate it into their standard of care right now.”
Meanwhile, Memorial Sloan Kettering Cancer Center is already planning to use abatacept, Dr. Ponce noted. “We have abatacept in our formulary for adult and children, and are planning on using it for patients receiving an unmodified graft from a [matched unrelated donor] or 1-allele [mismatched unrelated donor] using CNI and MTX-based GVHD prophylaxis.”
Dr. Devine and Mr. Spellman are employees of Be The Match and CIBMTR, which provided the registry control group for the ABA2 trial. Dr. Devine also reported that he has been a scientific advisory board member for Bristol-Myers Squibb. Dr. Ponce reports no relevant conflicts of interest.
FDA approves new CAR T-cell treatment for multiple myeloma
A new treatment option for patients with refractory/relapsed multiple myeloma who have already tried four or more therapies has been approved by the U.S. Food and Drug Administration.
There are already two other therapies on the market that target BCMA – another CAR T cell, idecabtagene vicleucel (Abecma), which was approved by the FDA in March 2021, and a drug conjugate, belantamab mafodotin (Blenrep), which was approved in August 2020.
The approval of cilta-cel was based on clinical data from the CARTITUDE-1 study, which were initially presented in December 2020 at the annual meeting of the American Society of Hematology, as reported at the time by this news organization.
The trial involved 97 patients with relapsed/refractory multiple myeloma who had already received a median of six previous treatments (range, three to 18), including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody.
“The treatment journey for the majority of patients living with multiple myeloma is a relentless cycle of remission and relapse, with fewer patients achieving a deep response as they progress through later lines of therapy,” commented Sundar Jagannath, MBBS, professor of medicine, hematology, and medical oncology at Mount Sinai, who was a principal investigator on the pivotal study.
“That is why I have been really excited about the results from the CARTITUDE-1 study, which has demonstrated that cilta-cel can provide deep and durable responses and long-term treatment-free intervals, even in this heavily pretreated multiple myeloma patient population,” he said.
“Today’s approval of Carvykti helps address a great unmet need for these patients,” he commented in a press release from the manufacturer.
Like other CAR T-cell therapies, ciltacabtagene autoleucel is a one-time treatment. It involves collecting blood from the patient, extracting T cells, genetically engineering them, then transfusing them back to the patient, who in the meantime has undergone conditioning.
The results from CARTITUDE-1 show that this one-time treatment resulted in deep and durable responses.
The overall response rate was 98%, and the majority of patients (78%) achieved a stringent complete response, in which physicians are unable to observe any signs or symptoms of disease via imaging or other tests after treatment.
At a median of 18 months’ follow-up, the median duration of response was 21.8 months.
“The responses in the CARTITUDE-1 study showed durability over time and resulted in the majority of heavily pretreated patients achieving deep responses after 18-month follow-up,” commented Mr. Jagannath.
“The approval of cilta-cel provides physicians an immunotherapy treatment option that offers patients an opportunity to be free from anti-myeloma therapies for a period of time,” he added.
As with other CAR T-cell therapies, there were serious side effects, and these products are available only through restricted programs under a risk evaluation and mitigation strategy.
The product information for Cartykti includes a boxed warning that mentions cytokine release syndrome (CRS), immune effector cell–associated neurotoxicity syndrome, parkinsonism, Guillain-Barré syndrome, hemophagocytic lymphohistiocytosis/macrophage activation syndrome, and prolonged and/or recurrent cytopenias.
The most common adverse reactions (reported in greater than or equal to 20% of patients) are pyrexia, CRS, hypogammaglobulinemia, hypotension, musculoskeletal pain, fatigue, infections–pathogens unspecified, cough, chills, diarrhea, nausea, encephalopathy, decreased appetite, upper respiratory tract infection, headache, tachycardia, dizziness, dyspnea, edema, viral infections, coagulopathy, constipation, and vomiting.
A version of this article first appeared on Medscape.com.
A new treatment option for patients with refractory/relapsed multiple myeloma who have already tried four or more therapies has been approved by the U.S. Food and Drug Administration.
There are already two other therapies on the market that target BCMA – another CAR T cell, idecabtagene vicleucel (Abecma), which was approved by the FDA in March 2021, and a drug conjugate, belantamab mafodotin (Blenrep), which was approved in August 2020.
The approval of cilta-cel was based on clinical data from the CARTITUDE-1 study, which were initially presented in December 2020 at the annual meeting of the American Society of Hematology, as reported at the time by this news organization.
The trial involved 97 patients with relapsed/refractory multiple myeloma who had already received a median of six previous treatments (range, three to 18), including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody.
“The treatment journey for the majority of patients living with multiple myeloma is a relentless cycle of remission and relapse, with fewer patients achieving a deep response as they progress through later lines of therapy,” commented Sundar Jagannath, MBBS, professor of medicine, hematology, and medical oncology at Mount Sinai, who was a principal investigator on the pivotal study.
“That is why I have been really excited about the results from the CARTITUDE-1 study, which has demonstrated that cilta-cel can provide deep and durable responses and long-term treatment-free intervals, even in this heavily pretreated multiple myeloma patient population,” he said.
“Today’s approval of Carvykti helps address a great unmet need for these patients,” he commented in a press release from the manufacturer.
Like other CAR T-cell therapies, ciltacabtagene autoleucel is a one-time treatment. It involves collecting blood from the patient, extracting T cells, genetically engineering them, then transfusing them back to the patient, who in the meantime has undergone conditioning.
The results from CARTITUDE-1 show that this one-time treatment resulted in deep and durable responses.
The overall response rate was 98%, and the majority of patients (78%) achieved a stringent complete response, in which physicians are unable to observe any signs or symptoms of disease via imaging or other tests after treatment.
At a median of 18 months’ follow-up, the median duration of response was 21.8 months.
“The responses in the CARTITUDE-1 study showed durability over time and resulted in the majority of heavily pretreated patients achieving deep responses after 18-month follow-up,” commented Mr. Jagannath.
“The approval of cilta-cel provides physicians an immunotherapy treatment option that offers patients an opportunity to be free from anti-myeloma therapies for a period of time,” he added.
As with other CAR T-cell therapies, there were serious side effects, and these products are available only through restricted programs under a risk evaluation and mitigation strategy.
The product information for Cartykti includes a boxed warning that mentions cytokine release syndrome (CRS), immune effector cell–associated neurotoxicity syndrome, parkinsonism, Guillain-Barré syndrome, hemophagocytic lymphohistiocytosis/macrophage activation syndrome, and prolonged and/or recurrent cytopenias.
The most common adverse reactions (reported in greater than or equal to 20% of patients) are pyrexia, CRS, hypogammaglobulinemia, hypotension, musculoskeletal pain, fatigue, infections–pathogens unspecified, cough, chills, diarrhea, nausea, encephalopathy, decreased appetite, upper respiratory tract infection, headache, tachycardia, dizziness, dyspnea, edema, viral infections, coagulopathy, constipation, and vomiting.
A version of this article first appeared on Medscape.com.
A new treatment option for patients with refractory/relapsed multiple myeloma who have already tried four or more therapies has been approved by the U.S. Food and Drug Administration.
There are already two other therapies on the market that target BCMA – another CAR T cell, idecabtagene vicleucel (Abecma), which was approved by the FDA in March 2021, and a drug conjugate, belantamab mafodotin (Blenrep), which was approved in August 2020.
The approval of cilta-cel was based on clinical data from the CARTITUDE-1 study, which were initially presented in December 2020 at the annual meeting of the American Society of Hematology, as reported at the time by this news organization.
The trial involved 97 patients with relapsed/refractory multiple myeloma who had already received a median of six previous treatments (range, three to 18), including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody.
“The treatment journey for the majority of patients living with multiple myeloma is a relentless cycle of remission and relapse, with fewer patients achieving a deep response as they progress through later lines of therapy,” commented Sundar Jagannath, MBBS, professor of medicine, hematology, and medical oncology at Mount Sinai, who was a principal investigator on the pivotal study.
“That is why I have been really excited about the results from the CARTITUDE-1 study, which has demonstrated that cilta-cel can provide deep and durable responses and long-term treatment-free intervals, even in this heavily pretreated multiple myeloma patient population,” he said.
“Today’s approval of Carvykti helps address a great unmet need for these patients,” he commented in a press release from the manufacturer.
Like other CAR T-cell therapies, ciltacabtagene autoleucel is a one-time treatment. It involves collecting blood from the patient, extracting T cells, genetically engineering them, then transfusing them back to the patient, who in the meantime has undergone conditioning.
The results from CARTITUDE-1 show that this one-time treatment resulted in deep and durable responses.
The overall response rate was 98%, and the majority of patients (78%) achieved a stringent complete response, in which physicians are unable to observe any signs or symptoms of disease via imaging or other tests after treatment.
At a median of 18 months’ follow-up, the median duration of response was 21.8 months.
“The responses in the CARTITUDE-1 study showed durability over time and resulted in the majority of heavily pretreated patients achieving deep responses after 18-month follow-up,” commented Mr. Jagannath.
“The approval of cilta-cel provides physicians an immunotherapy treatment option that offers patients an opportunity to be free from anti-myeloma therapies for a period of time,” he added.
As with other CAR T-cell therapies, there were serious side effects, and these products are available only through restricted programs under a risk evaluation and mitigation strategy.
The product information for Cartykti includes a boxed warning that mentions cytokine release syndrome (CRS), immune effector cell–associated neurotoxicity syndrome, parkinsonism, Guillain-Barré syndrome, hemophagocytic lymphohistiocytosis/macrophage activation syndrome, and prolonged and/or recurrent cytopenias.
The most common adverse reactions (reported in greater than or equal to 20% of patients) are pyrexia, CRS, hypogammaglobulinemia, hypotension, musculoskeletal pain, fatigue, infections–pathogens unspecified, cough, chills, diarrhea, nausea, encephalopathy, decreased appetite, upper respiratory tract infection, headache, tachycardia, dizziness, dyspnea, edema, viral infections, coagulopathy, constipation, and vomiting.
A version of this article first appeared on Medscape.com.
100 coauthored papers, 10 years: Cancer transplant pioneers model 'team science'
On July 29, 2021, Sergio Giralt, MD, deputy division head of the division of hematologic malignancies and Miguel-Angel Perales, MD, chief of the adult bone marrow transplant service at MSKCC, published their 100th peer-reviewed paper as coauthors. Listing hundreds of such articles on a CV is standard for top-tier physicians, but the pair had gone one better: 100 publications written together in 10 years.
Their centenary article hit scientific newsstands almost exactly a decade after their first joint paper, which appeared in September 2011, not long after they met.
Born in Cuba, Dr. Giralt grew up in Venezuela. From the age of 14, he knew that medicine was his path, and in 1984 he earned a medical degree from the Universidad Central de Venezuela, Caracas. Next came a research position at Harvard Medical School, a residency at the Good Samaritan Hospital, Cincinnati, and a fellowship at the University of Texas MD Anderson Cancer Center, Houston. Dr. Giralt arrived at MSKCC in 2010 as the new chief of the adult bone marrow transplant service. There he was introduced to a new colleague, Dr. Perales. They soon learned that in addition to expertise in hematology, they had second language in common: Spanish.
Dr. Giralt said: “We both have a Spanish background and in a certain sense, there was an affinity there. ... We both have shared experiences.”
Dr. Perales was brought up in Belgium, a European nation with three official languages: French, Dutch, and German. He speaks five tongues in all and learned Spanish from his father, who came from Spain.
Fluency in Spanish enables both physicians to take care of the many New Yorkers who are more comfortable in that language – especially when navigating cancer treatment. However, both Dr. Giralt and Dr. Perales said that a second language is more than a professional tool. They described the enjoyable change of persona that happens when they switch to Spanish.
“People who are multilingual have different roles [as much as] different languages,” said Dr. Perales. “When I’m in Spanish, part of my brain is [thinking back to] summer vacations and hanging out with my cousins.”
When it comes to clinical science, however, English is the language of choice.
Global leaders in HSCT
Dr. Giralt and Dr. Perales are known worldwide in the field of allogeneic HSCT, a potentially curative treatment for an elongating list of both malignant and nonmalignant diseases.
In 1973, MSKCC conducted the first bone-marrow transplant from an unrelated donor. Fifty years on, medical oncologists in the United States conduct approximately 8,500 allogeneic transplants each year, 72% to treat acute leukemias or myelodysplastic syndrome (MDS).
However, stripping the immune system with intensive chemotherapy ‘conditioning,’ then rebuilding it with non-diseased donor hematopoietic cells is a hazardous undertaking. Older patients are less likely to survive the intensive conditioning, so historically have missed out. Also, even with a good human leukocyte antigen (HLA) match, the recipient needs often brutal immunosuppression.
Since Dr. Giralt and Dr. Perales began their partnership in 2010, the goals of their work have not changed: to develop safer, lower-intensity transplantation suitable for older, more vulnerable patients and reduce fearsome posttransplant sequelae such as graft-versus-host disease (GVHD).
Dr. Giralt’s publication list spans more than 600 peer-reviewed papers, articles and book chapters, almost exclusively on HSCT. Dr. Perales has more than 300 publication credits on the topic.
The two paired up on their first paper just months after Dr. Giralt arrived at MSKCC. That article, published in Biology of Blood and Marrow Transplantation, compared umbilical cord blood for HSCT with donor blood in 367 people with a variety of hematologic malignancies, including acute and chronic leukemias, MDS, and lymphoma.
The MSKCC team found that transplant-related mortality in the first 180 days was higher for the cord blood (21%), but thereafter mortality and relapse were much lower than for donated blood, with the result that 2-year progression-free survival of 55% was similar. Dr. Perales, Dr. Giralt and their coauthors concluded that the data provided “strong support” for further work on cord blood as an alternative stem-cell source.
During their first decade of collaboration, Dr. Giralt and Dr. Perales worked on any promising avenue that could improve outcomes and the experience of HSCT recipients, including reduced-intensity conditioning regimens to allow older adults to benefit from curative HSCT and donor T-cell depletion by CD34 selection, to reduce graft-versus-host disease (GVHD).
The CD34 protein is typically found on the surface of early stage and highly active stem cell types. Selecting these cell types using a range of techniques can eliminate many other potentially interfering or inactive cells. This enriches the transplant population with the most effective cells and can lower the risk of GVHD.
The 100th paper on which Dr. Giralt and Dr. Perales were coauthors was published in Blood Advances on July 27, 2021. The retrospective study examined the fate of 58 MSKCC patients with a rare form of chronic lymphocytic leukemia, CLL with Richter’s transformation (CLL-RT). It was the largest such study to date of this rare disease.
M.D. Anderson Cancer Center had shown in 2006 that, despite chemotherapy, overall survival in patients with CLL-RT was approximately 8 months. HSCT improved survival dramatically (75% at 3 years; n = 7). However, with the advent of novel targeted drugs for CLL such as ibrutinib (Imbruvica), venetoclax (Venclexta), or idelalisib (Zydelig), the MSKCC team asked themselves: What was the role of reduced-intensive conditioning HSCT? Was it even safe? Among other findings, Dr. Giralt and Dr. Perales’ 100th paper showed that reduced-intensity HSCT remained a viable alternative after a CLL-RT patient progressed on a novel agent.
Impact of the pandemic
When COVID-19 hit, the team lost many research staff and developed a huge backlog, said Dr. Giralt. He and Dr. Perales realized that they needed to be “thoughtful and careful” about which studies to continue. “For example, the CD-34 selection trials we did not close because these are our workhorse trials,” Dr. Giralt said. “We have people we need to treat, and some of the patients that we need to treat can only be treated on trial.”
The team was also able to pivot some of their work into COVID 19 itself, and they collected crucial information on HSCT in recovered COVID-19 patients, as an example.
“We were living through a critical time, but that doesn’t mean we [aren’t] obligated to continue our mission, our research mission,” said Dr. Giralt. “It really is team science. The way we look at it ... there’s a common thread: We both like to do allogeneic transplant, and we both believe in trying to make CD-34 selection better. So we’re both very much [working on] how can we improve what we call ‘the Memorial way’ of doing transplants. Where we separate is, Miguel does primarily lymphoma. He doesn’t do myeloma [like me]. So in those two areas, we’re helping develop the junior faculty in a different way.”
Something more in common
Right from the start, Dr. Perales and Dr. Giralt also shared a commitment to mentoring. Since 2010, Dr. Perales has mentored 22 up-and-coming junior faculty, including 10 from Europe (8 from Spain) and 2 from Latin America.
“[It makes] the research enterprise much more productive but [these young scientists] really increase the visibility of the program,” said Dr. Giralt.
He cited Dr. Perales’ track record of mentoring as one of the reasons for his promotion to chief of the adult bone marrow transplant service. In March 2020, Dr. Perales seamlessly stepped into Dr. Giralt’s shoes, while Dr. Giralt moved on to his present role as deputy division head of the division of hematologic malignancies.
Dr. Perales said: “The key aspect [of these promotions] is the fantastic working relationship that we’ve had over the years. ... I consider Sergio my mentor, but also a good friend and colleague. And so I think it’s this ability that we’ve had to work together and that relationship of trust, which has been key.”
“Sergio is somebody who lifts people up,” Dr. Perales added. “Many people will tell you that Sergio has helped them in their career. ... And I think that’s a lesson I’ve learned from him: training the next generation. And [that’s] not just in the U.S., but outside. I think that’s a key role that we have. And our responsibility.”
Asked to comment on their 100th-paper milestone, Dr. Perales firmly turned the spotlight from himself and Dr. Giralt to the junior investigators who have passed through the doors of the bone-marrow transplant program: “This body of work represents not just our collaboration but also the many contributions of our team at MSK ... and beyond MSK.”
This article was updated 1/26/22.
On July 29, 2021, Sergio Giralt, MD, deputy division head of the division of hematologic malignancies and Miguel-Angel Perales, MD, chief of the adult bone marrow transplant service at MSKCC, published their 100th peer-reviewed paper as coauthors. Listing hundreds of such articles on a CV is standard for top-tier physicians, but the pair had gone one better: 100 publications written together in 10 years.
Their centenary article hit scientific newsstands almost exactly a decade after their first joint paper, which appeared in September 2011, not long after they met.
Born in Cuba, Dr. Giralt grew up in Venezuela. From the age of 14, he knew that medicine was his path, and in 1984 he earned a medical degree from the Universidad Central de Venezuela, Caracas. Next came a research position at Harvard Medical School, a residency at the Good Samaritan Hospital, Cincinnati, and a fellowship at the University of Texas MD Anderson Cancer Center, Houston. Dr. Giralt arrived at MSKCC in 2010 as the new chief of the adult bone marrow transplant service. There he was introduced to a new colleague, Dr. Perales. They soon learned that in addition to expertise in hematology, they had second language in common: Spanish.
Dr. Giralt said: “We both have a Spanish background and in a certain sense, there was an affinity there. ... We both have shared experiences.”
Dr. Perales was brought up in Belgium, a European nation with three official languages: French, Dutch, and German. He speaks five tongues in all and learned Spanish from his father, who came from Spain.
Fluency in Spanish enables both physicians to take care of the many New Yorkers who are more comfortable in that language – especially when navigating cancer treatment. However, both Dr. Giralt and Dr. Perales said that a second language is more than a professional tool. They described the enjoyable change of persona that happens when they switch to Spanish.
“People who are multilingual have different roles [as much as] different languages,” said Dr. Perales. “When I’m in Spanish, part of my brain is [thinking back to] summer vacations and hanging out with my cousins.”
When it comes to clinical science, however, English is the language of choice.
Global leaders in HSCT
Dr. Giralt and Dr. Perales are known worldwide in the field of allogeneic HSCT, a potentially curative treatment for an elongating list of both malignant and nonmalignant diseases.
In 1973, MSKCC conducted the first bone-marrow transplant from an unrelated donor. Fifty years on, medical oncologists in the United States conduct approximately 8,500 allogeneic transplants each year, 72% to treat acute leukemias or myelodysplastic syndrome (MDS).
However, stripping the immune system with intensive chemotherapy ‘conditioning,’ then rebuilding it with non-diseased donor hematopoietic cells is a hazardous undertaking. Older patients are less likely to survive the intensive conditioning, so historically have missed out. Also, even with a good human leukocyte antigen (HLA) match, the recipient needs often brutal immunosuppression.
Since Dr. Giralt and Dr. Perales began their partnership in 2010, the goals of their work have not changed: to develop safer, lower-intensity transplantation suitable for older, more vulnerable patients and reduce fearsome posttransplant sequelae such as graft-versus-host disease (GVHD).
Dr. Giralt’s publication list spans more than 600 peer-reviewed papers, articles and book chapters, almost exclusively on HSCT. Dr. Perales has more than 300 publication credits on the topic.
The two paired up on their first paper just months after Dr. Giralt arrived at MSKCC. That article, published in Biology of Blood and Marrow Transplantation, compared umbilical cord blood for HSCT with donor blood in 367 people with a variety of hematologic malignancies, including acute and chronic leukemias, MDS, and lymphoma.
The MSKCC team found that transplant-related mortality in the first 180 days was higher for the cord blood (21%), but thereafter mortality and relapse were much lower than for donated blood, with the result that 2-year progression-free survival of 55% was similar. Dr. Perales, Dr. Giralt and their coauthors concluded that the data provided “strong support” for further work on cord blood as an alternative stem-cell source.
During their first decade of collaboration, Dr. Giralt and Dr. Perales worked on any promising avenue that could improve outcomes and the experience of HSCT recipients, including reduced-intensity conditioning regimens to allow older adults to benefit from curative HSCT and donor T-cell depletion by CD34 selection, to reduce graft-versus-host disease (GVHD).
The CD34 protein is typically found on the surface of early stage and highly active stem cell types. Selecting these cell types using a range of techniques can eliminate many other potentially interfering or inactive cells. This enriches the transplant population with the most effective cells and can lower the risk of GVHD.
The 100th paper on which Dr. Giralt and Dr. Perales were coauthors was published in Blood Advances on July 27, 2021. The retrospective study examined the fate of 58 MSKCC patients with a rare form of chronic lymphocytic leukemia, CLL with Richter’s transformation (CLL-RT). It was the largest such study to date of this rare disease.
M.D. Anderson Cancer Center had shown in 2006 that, despite chemotherapy, overall survival in patients with CLL-RT was approximately 8 months. HSCT improved survival dramatically (75% at 3 years; n = 7). However, with the advent of novel targeted drugs for CLL such as ibrutinib (Imbruvica), venetoclax (Venclexta), or idelalisib (Zydelig), the MSKCC team asked themselves: What was the role of reduced-intensive conditioning HSCT? Was it even safe? Among other findings, Dr. Giralt and Dr. Perales’ 100th paper showed that reduced-intensity HSCT remained a viable alternative after a CLL-RT patient progressed on a novel agent.
Impact of the pandemic
When COVID-19 hit, the team lost many research staff and developed a huge backlog, said Dr. Giralt. He and Dr. Perales realized that they needed to be “thoughtful and careful” about which studies to continue. “For example, the CD-34 selection trials we did not close because these are our workhorse trials,” Dr. Giralt said. “We have people we need to treat, and some of the patients that we need to treat can only be treated on trial.”
The team was also able to pivot some of their work into COVID 19 itself, and they collected crucial information on HSCT in recovered COVID-19 patients, as an example.
“We were living through a critical time, but that doesn’t mean we [aren’t] obligated to continue our mission, our research mission,” said Dr. Giralt. “It really is team science. The way we look at it ... there’s a common thread: We both like to do allogeneic transplant, and we both believe in trying to make CD-34 selection better. So we’re both very much [working on] how can we improve what we call ‘the Memorial way’ of doing transplants. Where we separate is, Miguel does primarily lymphoma. He doesn’t do myeloma [like me]. So in those two areas, we’re helping develop the junior faculty in a different way.”
Something more in common
Right from the start, Dr. Perales and Dr. Giralt also shared a commitment to mentoring. Since 2010, Dr. Perales has mentored 22 up-and-coming junior faculty, including 10 from Europe (8 from Spain) and 2 from Latin America.
“[It makes] the research enterprise much more productive but [these young scientists] really increase the visibility of the program,” said Dr. Giralt.
He cited Dr. Perales’ track record of mentoring as one of the reasons for his promotion to chief of the adult bone marrow transplant service. In March 2020, Dr. Perales seamlessly stepped into Dr. Giralt’s shoes, while Dr. Giralt moved on to his present role as deputy division head of the division of hematologic malignancies.
Dr. Perales said: “The key aspect [of these promotions] is the fantastic working relationship that we’ve had over the years. ... I consider Sergio my mentor, but also a good friend and colleague. And so I think it’s this ability that we’ve had to work together and that relationship of trust, which has been key.”
“Sergio is somebody who lifts people up,” Dr. Perales added. “Many people will tell you that Sergio has helped them in their career. ... And I think that’s a lesson I’ve learned from him: training the next generation. And [that’s] not just in the U.S., but outside. I think that’s a key role that we have. And our responsibility.”
Asked to comment on their 100th-paper milestone, Dr. Perales firmly turned the spotlight from himself and Dr. Giralt to the junior investigators who have passed through the doors of the bone-marrow transplant program: “This body of work represents not just our collaboration but also the many contributions of our team at MSK ... and beyond MSK.”
This article was updated 1/26/22.
On July 29, 2021, Sergio Giralt, MD, deputy division head of the division of hematologic malignancies and Miguel-Angel Perales, MD, chief of the adult bone marrow transplant service at MSKCC, published their 100th peer-reviewed paper as coauthors. Listing hundreds of such articles on a CV is standard for top-tier physicians, but the pair had gone one better: 100 publications written together in 10 years.
Their centenary article hit scientific newsstands almost exactly a decade after their first joint paper, which appeared in September 2011, not long after they met.
Born in Cuba, Dr. Giralt grew up in Venezuela. From the age of 14, he knew that medicine was his path, and in 1984 he earned a medical degree from the Universidad Central de Venezuela, Caracas. Next came a research position at Harvard Medical School, a residency at the Good Samaritan Hospital, Cincinnati, and a fellowship at the University of Texas MD Anderson Cancer Center, Houston. Dr. Giralt arrived at MSKCC in 2010 as the new chief of the adult bone marrow transplant service. There he was introduced to a new colleague, Dr. Perales. They soon learned that in addition to expertise in hematology, they had second language in common: Spanish.
Dr. Giralt said: “We both have a Spanish background and in a certain sense, there was an affinity there. ... We both have shared experiences.”
Dr. Perales was brought up in Belgium, a European nation with three official languages: French, Dutch, and German. He speaks five tongues in all and learned Spanish from his father, who came from Spain.
Fluency in Spanish enables both physicians to take care of the many New Yorkers who are more comfortable in that language – especially when navigating cancer treatment. However, both Dr. Giralt and Dr. Perales said that a second language is more than a professional tool. They described the enjoyable change of persona that happens when they switch to Spanish.
“People who are multilingual have different roles [as much as] different languages,” said Dr. Perales. “When I’m in Spanish, part of my brain is [thinking back to] summer vacations and hanging out with my cousins.”
When it comes to clinical science, however, English is the language of choice.
Global leaders in HSCT
Dr. Giralt and Dr. Perales are known worldwide in the field of allogeneic HSCT, a potentially curative treatment for an elongating list of both malignant and nonmalignant diseases.
In 1973, MSKCC conducted the first bone-marrow transplant from an unrelated donor. Fifty years on, medical oncologists in the United States conduct approximately 8,500 allogeneic transplants each year, 72% to treat acute leukemias or myelodysplastic syndrome (MDS).
However, stripping the immune system with intensive chemotherapy ‘conditioning,’ then rebuilding it with non-diseased donor hematopoietic cells is a hazardous undertaking. Older patients are less likely to survive the intensive conditioning, so historically have missed out. Also, even with a good human leukocyte antigen (HLA) match, the recipient needs often brutal immunosuppression.
Since Dr. Giralt and Dr. Perales began their partnership in 2010, the goals of their work have not changed: to develop safer, lower-intensity transplantation suitable for older, more vulnerable patients and reduce fearsome posttransplant sequelae such as graft-versus-host disease (GVHD).
Dr. Giralt’s publication list spans more than 600 peer-reviewed papers, articles and book chapters, almost exclusively on HSCT. Dr. Perales has more than 300 publication credits on the topic.
The two paired up on their first paper just months after Dr. Giralt arrived at MSKCC. That article, published in Biology of Blood and Marrow Transplantation, compared umbilical cord blood for HSCT with donor blood in 367 people with a variety of hematologic malignancies, including acute and chronic leukemias, MDS, and lymphoma.
The MSKCC team found that transplant-related mortality in the first 180 days was higher for the cord blood (21%), but thereafter mortality and relapse were much lower than for donated blood, with the result that 2-year progression-free survival of 55% was similar. Dr. Perales, Dr. Giralt and their coauthors concluded that the data provided “strong support” for further work on cord blood as an alternative stem-cell source.
During their first decade of collaboration, Dr. Giralt and Dr. Perales worked on any promising avenue that could improve outcomes and the experience of HSCT recipients, including reduced-intensity conditioning regimens to allow older adults to benefit from curative HSCT and donor T-cell depletion by CD34 selection, to reduce graft-versus-host disease (GVHD).
The CD34 protein is typically found on the surface of early stage and highly active stem cell types. Selecting these cell types using a range of techniques can eliminate many other potentially interfering or inactive cells. This enriches the transplant population with the most effective cells and can lower the risk of GVHD.
The 100th paper on which Dr. Giralt and Dr. Perales were coauthors was published in Blood Advances on July 27, 2021. The retrospective study examined the fate of 58 MSKCC patients with a rare form of chronic lymphocytic leukemia, CLL with Richter’s transformation (CLL-RT). It was the largest such study to date of this rare disease.
M.D. Anderson Cancer Center had shown in 2006 that, despite chemotherapy, overall survival in patients with CLL-RT was approximately 8 months. HSCT improved survival dramatically (75% at 3 years; n = 7). However, with the advent of novel targeted drugs for CLL such as ibrutinib (Imbruvica), venetoclax (Venclexta), or idelalisib (Zydelig), the MSKCC team asked themselves: What was the role of reduced-intensive conditioning HSCT? Was it even safe? Among other findings, Dr. Giralt and Dr. Perales’ 100th paper showed that reduced-intensity HSCT remained a viable alternative after a CLL-RT patient progressed on a novel agent.
Impact of the pandemic
When COVID-19 hit, the team lost many research staff and developed a huge backlog, said Dr. Giralt. He and Dr. Perales realized that they needed to be “thoughtful and careful” about which studies to continue. “For example, the CD-34 selection trials we did not close because these are our workhorse trials,” Dr. Giralt said. “We have people we need to treat, and some of the patients that we need to treat can only be treated on trial.”
The team was also able to pivot some of their work into COVID 19 itself, and they collected crucial information on HSCT in recovered COVID-19 patients, as an example.
“We were living through a critical time, but that doesn’t mean we [aren’t] obligated to continue our mission, our research mission,” said Dr. Giralt. “It really is team science. The way we look at it ... there’s a common thread: We both like to do allogeneic transplant, and we both believe in trying to make CD-34 selection better. So we’re both very much [working on] how can we improve what we call ‘the Memorial way’ of doing transplants. Where we separate is, Miguel does primarily lymphoma. He doesn’t do myeloma [like me]. So in those two areas, we’re helping develop the junior faculty in a different way.”
Something more in common
Right from the start, Dr. Perales and Dr. Giralt also shared a commitment to mentoring. Since 2010, Dr. Perales has mentored 22 up-and-coming junior faculty, including 10 from Europe (8 from Spain) and 2 from Latin America.
“[It makes] the research enterprise much more productive but [these young scientists] really increase the visibility of the program,” said Dr. Giralt.
He cited Dr. Perales’ track record of mentoring as one of the reasons for his promotion to chief of the adult bone marrow transplant service. In March 2020, Dr. Perales seamlessly stepped into Dr. Giralt’s shoes, while Dr. Giralt moved on to his present role as deputy division head of the division of hematologic malignancies.
Dr. Perales said: “The key aspect [of these promotions] is the fantastic working relationship that we’ve had over the years. ... I consider Sergio my mentor, but also a good friend and colleague. And so I think it’s this ability that we’ve had to work together and that relationship of trust, which has been key.”
“Sergio is somebody who lifts people up,” Dr. Perales added. “Many people will tell you that Sergio has helped them in their career. ... And I think that’s a lesson I’ve learned from him: training the next generation. And [that’s] not just in the U.S., but outside. I think that’s a key role that we have. And our responsibility.”
Asked to comment on their 100th-paper milestone, Dr. Perales firmly turned the spotlight from himself and Dr. Giralt to the junior investigators who have passed through the doors of the bone-marrow transplant program: “This body of work represents not just our collaboration but also the many contributions of our team at MSK ... and beyond MSK.”
This article was updated 1/26/22.
DKMS: Small nonprofit to world’s largest stem cell donor registry
When Mechtild Harf was diagnosed with acute leukemia in 1990, physicians told her and her husband Peter that a bone marrow transplant was her best hope for survival. Back then, her native Germany had only 3,000 registered donors, and none was a match.
“My dad just went crazy, you know, to save his wife,” recalled Katharina Harf, who was a young teen at the time of her mother’s diagnosis.
In the course of 1 year, the Harfs recruited more than 68,000 potential bone marrow donors, but their heroic efforts couldn’t save Mechtild.
“She unfortunately didn’t make it. She died because of leukemia,” Katharina said.
Although Mechtild Harf did not survive, her legacy lives on in the bone marrow and stem cell donor recruitment organization DKMS (Deutsche Knochenmarkspenderdatei, or German Bone Marrow Donor Center).
In May of 1991, Peter Harf and Gerhard Ehninger, MD, the hematologist who treated Mechtild, founded DKMS with the mission, as its website states, “to provide as many blood cancer patients as possible with a second chance at life.”
From its German roots, the nonprofit organization has extended its mission to the United States (where it was initially known as Delete Blood Cancer DKMS), Poland, the United Kingdom, Chile, and in 2021, to South Africa.
Three decades after her mother’s death, Katharina Harf serves as Executive Chairwoman of DKMS U.S., based in New York.
World’s largest registry
“DKMS has the largest number of unrelated donors of any organization in the world,” noted Richard E. Champlin, MD, chair of the department of stem cell transplantation and cellular therapy at the University of Texas MD Anderson Cancer Center in Houston.
“In a large fraction of our donor searches, we find matches that are in the DKMS registry,” he said in an interview,
Alexander Schmidt, MD, PhD, global chief medical officer for DKMS, said that approximately 25% of all registered donors worldwide were recruited by his organization, and 39% of all unrelated donor transplants are made with peripheral blood stem cell or bone marrow products, donated by volunteers who are recruited by DKMS.
Since its founding, DKMS has registered 7.1 million potential donors in Germany, who made a total of 80,000 stem cell donations. DKMS U.S., which began operations in 2004, has registered 1.1 million donors and enabled 4,700 donations.
Global partners
DKMS partners with donor centers and recruitment organizations in each country where it operates. In the United States, DKMS works with the National Marrow Donor Program (NMDP) and its “Be The Match” donor registry.
“DKMS donors, both those from DKMS in Germany and those from DKMS in the United States are also listed in the NMDP registry, to make it easier for US search coordinators to accept these donors,” Dr. Schmidt explained in an interview.
The international cooperation and coordination makes it possible for a donor in the UK, for example, to save a life of a patient in Germany, the U.S., Chile, India, or many other parts of the world – anywhere that can be reached in time for a patient in need to receive a stem cell donation.
Pandemic affects donations
But, as with just about every aspect of life, the COVID-19 pandemic has created enormous challenges for recruiters, donor centers, and stem cell transplant centers.
Dr. Schmidt said that decline in donations during the pandemic was less severe than initially feared, with a decrease of just 3.5% in 2020, compared with the prepandemic year of 2019. In contrast, though, the average annual growth rate for donations prior to the pandemic was about 4%.
“Nevertheless, at the beginning of the pandemic in March 2020, for a few days things looked quite terrible, because all the borders were closed and flights were canceled, and about 50% of all stem cell products go abroad, and between 20% and 25% go intercontinental,” Dr. Schmidt said.
However, close cooperation and coordination between donor centers and national health authorities soon resolved the problem and helped insure that the flow of life-saving donations could continue with minimal disruption, he noted.
“I don’t think we had any product that could not be delivered at the end of the day, due to the pandemic,” he told this news organization.
Workforce and clinical problems
Although the flow of donations within and between nations has continued, the COVID-19 pandemic has had profound negative effects on transplant centers, particularly during the wave of infections caused by the Omicron variant, according to a transplant expert.
“With this most recent strain and how transmissible it is, what we’re dealing with is mass workforce shortages,” said Yi-Bin Chen, MD, director of the bone marrow transplant program at Massachusetts General Hospital in Boston.
“On top of a short-staffed hospital, you then take a very transmissible variant and deplete it even more due to the need to quarantine,” he said in an interview.
Both Dr. Champlin and Dr. Chen said that on-again, off-again pandemic travel bans and donor illnesses have necessitated first obtaining products and cryopreserving them before starting the recipient on a conditioning regimen for the transplant.
“The problem is that, while you can preserve peripheral blood stem cells pretty reliably, cryopreserving bone marrow is a bit more difficult,” Dr. Chen said.
In addition, evidence from recent studies comparing stem cell sources suggest that outcomes are less good with cryopreserved products than with fresh products, and with peripheral blood stem cells compared with bone marrow.
“But you’ve got to make do. A transplant with a cryopreserved product is better than no transplant,” Dr. Chen said.
To make things even more frustrating, as the pandemic waxed and waned throughout 2020 and 2021, the recommendations from donor centers seesawed between using fresh or cryopreserved product, making it difficult to plan a transplant for an individual patient.
The Omicron wave has also resulted in a much higher rate of donor dropout than anticipated, making it that much harder to schedule a transplant, Dr. Chen noted.
‘Every patient saved’
The pandemic will eventually subside, however, while the need for stem cell transplantation to treat hematologic malignancies will continue.
DKMS recently launched special aid programs to improve access to stem cell transplants in developing nations by offering financial support, free HLA typing, and other services.
In addition to its core mission of recruiting donors, DKMS is dedicated to improving the quality and efficiency of stem cell transplants. For example, in 2017 scientists in DKMS’ Life Science Lab created an antibody test for donor cytomegalovirus (CMV) infection, using a simple buccal swab rather than a more invasive blood sample. CMV infections can compromise the integrity of stem cell grafts and could be fatal to immunocompromised transplant recipients.
The last word goes to Mechtild Harf’s daughter Katharina.
“My big dream is that every patient will be saved from blood cancer,” she said in a video posted on the DKMS website. “When they get sick, we have a solution for them, whether it’s because they need a donor, with research, building hospitals, providing them with the best medical care we can. I will just keep fighting and keep spreading the word, recruiting donors, raising money – all the things that it takes for us to delete blood cancer.”
“I have to believe that this dream will come true because otherwise, why dream, right?” she said.
Dr. Champlin was the recipient of a Mechtild Harf Science Award and is a member of the board of DKMS U.S. Dr. Schmidt is employed by DKMS. Dr. Chen reported having no relevant disclosures.
When Mechtild Harf was diagnosed with acute leukemia in 1990, physicians told her and her husband Peter that a bone marrow transplant was her best hope for survival. Back then, her native Germany had only 3,000 registered donors, and none was a match.
“My dad just went crazy, you know, to save his wife,” recalled Katharina Harf, who was a young teen at the time of her mother’s diagnosis.
In the course of 1 year, the Harfs recruited more than 68,000 potential bone marrow donors, but their heroic efforts couldn’t save Mechtild.
“She unfortunately didn’t make it. She died because of leukemia,” Katharina said.
Although Mechtild Harf did not survive, her legacy lives on in the bone marrow and stem cell donor recruitment organization DKMS (Deutsche Knochenmarkspenderdatei, or German Bone Marrow Donor Center).
In May of 1991, Peter Harf and Gerhard Ehninger, MD, the hematologist who treated Mechtild, founded DKMS with the mission, as its website states, “to provide as many blood cancer patients as possible with a second chance at life.”
From its German roots, the nonprofit organization has extended its mission to the United States (where it was initially known as Delete Blood Cancer DKMS), Poland, the United Kingdom, Chile, and in 2021, to South Africa.
Three decades after her mother’s death, Katharina Harf serves as Executive Chairwoman of DKMS U.S., based in New York.
World’s largest registry
“DKMS has the largest number of unrelated donors of any organization in the world,” noted Richard E. Champlin, MD, chair of the department of stem cell transplantation and cellular therapy at the University of Texas MD Anderson Cancer Center in Houston.
“In a large fraction of our donor searches, we find matches that are in the DKMS registry,” he said in an interview,
Alexander Schmidt, MD, PhD, global chief medical officer for DKMS, said that approximately 25% of all registered donors worldwide were recruited by his organization, and 39% of all unrelated donor transplants are made with peripheral blood stem cell or bone marrow products, donated by volunteers who are recruited by DKMS.
Since its founding, DKMS has registered 7.1 million potential donors in Germany, who made a total of 80,000 stem cell donations. DKMS U.S., which began operations in 2004, has registered 1.1 million donors and enabled 4,700 donations.
Global partners
DKMS partners with donor centers and recruitment organizations in each country where it operates. In the United States, DKMS works with the National Marrow Donor Program (NMDP) and its “Be The Match” donor registry.
“DKMS donors, both those from DKMS in Germany and those from DKMS in the United States are also listed in the NMDP registry, to make it easier for US search coordinators to accept these donors,” Dr. Schmidt explained in an interview.
The international cooperation and coordination makes it possible for a donor in the UK, for example, to save a life of a patient in Germany, the U.S., Chile, India, or many other parts of the world – anywhere that can be reached in time for a patient in need to receive a stem cell donation.
Pandemic affects donations
But, as with just about every aspect of life, the COVID-19 pandemic has created enormous challenges for recruiters, donor centers, and stem cell transplant centers.
Dr. Schmidt said that decline in donations during the pandemic was less severe than initially feared, with a decrease of just 3.5% in 2020, compared with the prepandemic year of 2019. In contrast, though, the average annual growth rate for donations prior to the pandemic was about 4%.
“Nevertheless, at the beginning of the pandemic in March 2020, for a few days things looked quite terrible, because all the borders were closed and flights were canceled, and about 50% of all stem cell products go abroad, and between 20% and 25% go intercontinental,” Dr. Schmidt said.
However, close cooperation and coordination between donor centers and national health authorities soon resolved the problem and helped insure that the flow of life-saving donations could continue with minimal disruption, he noted.
“I don’t think we had any product that could not be delivered at the end of the day, due to the pandemic,” he told this news organization.
Workforce and clinical problems
Although the flow of donations within and between nations has continued, the COVID-19 pandemic has had profound negative effects on transplant centers, particularly during the wave of infections caused by the Omicron variant, according to a transplant expert.
“With this most recent strain and how transmissible it is, what we’re dealing with is mass workforce shortages,” said Yi-Bin Chen, MD, director of the bone marrow transplant program at Massachusetts General Hospital in Boston.
“On top of a short-staffed hospital, you then take a very transmissible variant and deplete it even more due to the need to quarantine,” he said in an interview.
Both Dr. Champlin and Dr. Chen said that on-again, off-again pandemic travel bans and donor illnesses have necessitated first obtaining products and cryopreserving them before starting the recipient on a conditioning regimen for the transplant.
“The problem is that, while you can preserve peripheral blood stem cells pretty reliably, cryopreserving bone marrow is a bit more difficult,” Dr. Chen said.
In addition, evidence from recent studies comparing stem cell sources suggest that outcomes are less good with cryopreserved products than with fresh products, and with peripheral blood stem cells compared with bone marrow.
“But you’ve got to make do. A transplant with a cryopreserved product is better than no transplant,” Dr. Chen said.
To make things even more frustrating, as the pandemic waxed and waned throughout 2020 and 2021, the recommendations from donor centers seesawed between using fresh or cryopreserved product, making it difficult to plan a transplant for an individual patient.
The Omicron wave has also resulted in a much higher rate of donor dropout than anticipated, making it that much harder to schedule a transplant, Dr. Chen noted.
‘Every patient saved’
The pandemic will eventually subside, however, while the need for stem cell transplantation to treat hematologic malignancies will continue.
DKMS recently launched special aid programs to improve access to stem cell transplants in developing nations by offering financial support, free HLA typing, and other services.
In addition to its core mission of recruiting donors, DKMS is dedicated to improving the quality and efficiency of stem cell transplants. For example, in 2017 scientists in DKMS’ Life Science Lab created an antibody test for donor cytomegalovirus (CMV) infection, using a simple buccal swab rather than a more invasive blood sample. CMV infections can compromise the integrity of stem cell grafts and could be fatal to immunocompromised transplant recipients.
The last word goes to Mechtild Harf’s daughter Katharina.
“My big dream is that every patient will be saved from blood cancer,” she said in a video posted on the DKMS website. “When they get sick, we have a solution for them, whether it’s because they need a donor, with research, building hospitals, providing them with the best medical care we can. I will just keep fighting and keep spreading the word, recruiting donors, raising money – all the things that it takes for us to delete blood cancer.”
“I have to believe that this dream will come true because otherwise, why dream, right?” she said.
Dr. Champlin was the recipient of a Mechtild Harf Science Award and is a member of the board of DKMS U.S. Dr. Schmidt is employed by DKMS. Dr. Chen reported having no relevant disclosures.
When Mechtild Harf was diagnosed with acute leukemia in 1990, physicians told her and her husband Peter that a bone marrow transplant was her best hope for survival. Back then, her native Germany had only 3,000 registered donors, and none was a match.
“My dad just went crazy, you know, to save his wife,” recalled Katharina Harf, who was a young teen at the time of her mother’s diagnosis.
In the course of 1 year, the Harfs recruited more than 68,000 potential bone marrow donors, but their heroic efforts couldn’t save Mechtild.
“She unfortunately didn’t make it. She died because of leukemia,” Katharina said.
Although Mechtild Harf did not survive, her legacy lives on in the bone marrow and stem cell donor recruitment organization DKMS (Deutsche Knochenmarkspenderdatei, or German Bone Marrow Donor Center).
In May of 1991, Peter Harf and Gerhard Ehninger, MD, the hematologist who treated Mechtild, founded DKMS with the mission, as its website states, “to provide as many blood cancer patients as possible with a second chance at life.”
From its German roots, the nonprofit organization has extended its mission to the United States (where it was initially known as Delete Blood Cancer DKMS), Poland, the United Kingdom, Chile, and in 2021, to South Africa.
Three decades after her mother’s death, Katharina Harf serves as Executive Chairwoman of DKMS U.S., based in New York.
World’s largest registry
“DKMS has the largest number of unrelated donors of any organization in the world,” noted Richard E. Champlin, MD, chair of the department of stem cell transplantation and cellular therapy at the University of Texas MD Anderson Cancer Center in Houston.
“In a large fraction of our donor searches, we find matches that are in the DKMS registry,” he said in an interview,
Alexander Schmidt, MD, PhD, global chief medical officer for DKMS, said that approximately 25% of all registered donors worldwide were recruited by his organization, and 39% of all unrelated donor transplants are made with peripheral blood stem cell or bone marrow products, donated by volunteers who are recruited by DKMS.
Since its founding, DKMS has registered 7.1 million potential donors in Germany, who made a total of 80,000 stem cell donations. DKMS U.S., which began operations in 2004, has registered 1.1 million donors and enabled 4,700 donations.
Global partners
DKMS partners with donor centers and recruitment organizations in each country where it operates. In the United States, DKMS works with the National Marrow Donor Program (NMDP) and its “Be The Match” donor registry.
“DKMS donors, both those from DKMS in Germany and those from DKMS in the United States are also listed in the NMDP registry, to make it easier for US search coordinators to accept these donors,” Dr. Schmidt explained in an interview.
The international cooperation and coordination makes it possible for a donor in the UK, for example, to save a life of a patient in Germany, the U.S., Chile, India, or many other parts of the world – anywhere that can be reached in time for a patient in need to receive a stem cell donation.
Pandemic affects donations
But, as with just about every aspect of life, the COVID-19 pandemic has created enormous challenges for recruiters, donor centers, and stem cell transplant centers.
Dr. Schmidt said that decline in donations during the pandemic was less severe than initially feared, with a decrease of just 3.5% in 2020, compared with the prepandemic year of 2019. In contrast, though, the average annual growth rate for donations prior to the pandemic was about 4%.
“Nevertheless, at the beginning of the pandemic in March 2020, for a few days things looked quite terrible, because all the borders were closed and flights were canceled, and about 50% of all stem cell products go abroad, and between 20% and 25% go intercontinental,” Dr. Schmidt said.
However, close cooperation and coordination between donor centers and national health authorities soon resolved the problem and helped insure that the flow of life-saving donations could continue with minimal disruption, he noted.
“I don’t think we had any product that could not be delivered at the end of the day, due to the pandemic,” he told this news organization.
Workforce and clinical problems
Although the flow of donations within and between nations has continued, the COVID-19 pandemic has had profound negative effects on transplant centers, particularly during the wave of infections caused by the Omicron variant, according to a transplant expert.
“With this most recent strain and how transmissible it is, what we’re dealing with is mass workforce shortages,” said Yi-Bin Chen, MD, director of the bone marrow transplant program at Massachusetts General Hospital in Boston.
“On top of a short-staffed hospital, you then take a very transmissible variant and deplete it even more due to the need to quarantine,” he said in an interview.
Both Dr. Champlin and Dr. Chen said that on-again, off-again pandemic travel bans and donor illnesses have necessitated first obtaining products and cryopreserving them before starting the recipient on a conditioning regimen for the transplant.
“The problem is that, while you can preserve peripheral blood stem cells pretty reliably, cryopreserving bone marrow is a bit more difficult,” Dr. Chen said.
In addition, evidence from recent studies comparing stem cell sources suggest that outcomes are less good with cryopreserved products than with fresh products, and with peripheral blood stem cells compared with bone marrow.
“But you’ve got to make do. A transplant with a cryopreserved product is better than no transplant,” Dr. Chen said.
To make things even more frustrating, as the pandemic waxed and waned throughout 2020 and 2021, the recommendations from donor centers seesawed between using fresh or cryopreserved product, making it difficult to plan a transplant for an individual patient.
The Omicron wave has also resulted in a much higher rate of donor dropout than anticipated, making it that much harder to schedule a transplant, Dr. Chen noted.
‘Every patient saved’
The pandemic will eventually subside, however, while the need for stem cell transplantation to treat hematologic malignancies will continue.
DKMS recently launched special aid programs to improve access to stem cell transplants in developing nations by offering financial support, free HLA typing, and other services.
In addition to its core mission of recruiting donors, DKMS is dedicated to improving the quality and efficiency of stem cell transplants. For example, in 2017 scientists in DKMS’ Life Science Lab created an antibody test for donor cytomegalovirus (CMV) infection, using a simple buccal swab rather than a more invasive blood sample. CMV infections can compromise the integrity of stem cell grafts and could be fatal to immunocompromised transplant recipients.
The last word goes to Mechtild Harf’s daughter Katharina.
“My big dream is that every patient will be saved from blood cancer,” she said in a video posted on the DKMS website. “When they get sick, we have a solution for them, whether it’s because they need a donor, with research, building hospitals, providing them with the best medical care we can. I will just keep fighting and keep spreading the word, recruiting donors, raising money – all the things that it takes for us to delete blood cancer.”
“I have to believe that this dream will come true because otherwise, why dream, right?” she said.
Dr. Champlin was the recipient of a Mechtild Harf Science Award and is a member of the board of DKMS U.S. Dr. Schmidt is employed by DKMS. Dr. Chen reported having no relevant disclosures.
Meeting the unmet need in multiple myeloma
In multiple myeloma, survival has been very significantly improved by immunomodulatory drugs, proteasome inhibitors, and CD38-targeting antibodies. Despite these advances, multiple myeloma, which is characterized by malignant proliferation of clonal plasma cells in bone marrow, remains an incurable plasma cell disorder with near-certain relapse after successful treatment. Prognosis for patients who develop triple-class refractory disease is poor, with less than 1-year survival. The substantial unmet therapeutic need extends further to other poor survival multiple myeloma populations that include newly diagnosed patients with high cytogenic risk profiles and those with early relapse after first-line therapy. For all of these, interest in drugs with novel mechanisms of action is naturally high.
More specific, less toxic
Post allogeneic hematopoietic stem-cell transplantation and donor lymphocyte infusion sustained remissions reflect a graft-versus-myeloma effect mediated by donor T cells.1 The substantial morbidity and mortality associated with graft-versus-host disease and opportunistic infections, however, have spurred searches for alternative, more specific, and less toxic T-cell therapies with stronger antitumor activity.
Chimeric antigen receptors (CARs)
In CAR T-cell therapies for multiple myeloma, autologous T cells are harvested from the patient and reprogrammed to target multiple myeloma cells through the introduction of genes that encode CARs, which are fusion proteins coupling an antigen-recognition moiety and a transmembrane-spanning element to a T-cell activation domain (typically CD3 zeta [CD247]). The T cells are then expanded and reinfused to the patient following a lymphodepletion regimen. Five strategies using autologous CAR T cells are currently approved for diffuse large B-cell lymphomas, acute lymphoblastic leukemia, multiple myeloma, and other hematologic malignancies. Notably, in patients with heavily pretreated multiple myeloma, CAR T cells have demonstrated impressive activity.
BCMA-targeting CAR T cells
The B-cell maturation antigen (BCMA; TNFRSF17), which plays an important role in the survival of long-lived plasma cells in bone marrow, is an attractive target for CAR T-cell therapy because it is expressed on normal and malignant plasma cell surfaces and by mature B cells. When ligands (TNFSF 13B/TNFSF13) bind to BCMA expressed on multiple myeloma cell surfaces, survival and proliferation pathways and drug resistance are activated.
High-quality responses have been demonstrated in several trials of anti-BCMA CAR T cells, which kill multiple myeloma cell lines and primary multiple myeloma cells through degranulation of T cells and lysis of tumor cells, even those with low BCMA expression. Based on efficacy in triple-class exposed multiple myeloma that compared favorably to conventional care with improved health-related quality of life, the U.S. Food and Drug Administration gave breakthrough designation to ciltacabtagene autoleucel in December 2019 and approval for idecabtagene vicleucel in March 2021.
Idecabtagene vicleucel
Idecabtagene vicleucel expresses a murine BCMA-targeting single-chain variable fragment with a 4-1BB costimulatory motif. The phase 2 KarMMa study2 evaluated idecabtagene vicleucel (target dose of 450 × 106 CAR T cells; range 150 × 106 to 450 × 106) activity in 128 patients with triple-class exposed multiple myeloma. Partial responses or better were observed in 94 of 128 patients (73%) (95% confidence interval, 66-81); 42 (33%) had a complete response or better (95% CI, 25-41), with a median progression-free survival of 8.8 months (95% CI, 5.6-11.6). Outcomes were improved in the highest fixed-dose group, with partial response or better in 81% (44 of 55), complete response or better in 39% (21), and median overall survival of 12.1 months (95% CI, 8.8-12.3). Patients with high-risk cytogenetic profiles, extramedullary disease, and high tumor burden also had deep and durable responses. Outcomes were less favorable in patients with revised International Staging System stage 3 disease.
Ciltacabtagene autoleucel
Ciltacabtagene autoleucel, a 4-1BB–based CAR T-cell therapy with two BCMA-targeting domains, confers high-avidity binding. In the phase 1b/2 CARTITUDE-1 study, conducted in the United States and Europe, preliminary results in 97 patients showed a 97% response rate with ciltacabtagene autoleucel (target dose 0.75 × 106 CAR T cells per kg), and in 65 patients, a complete response (67%). Progression-free survival at 12 months was 77% (95% CI, 66-84) and overall survival was 89% (95% CI, 80-94).3
In the phase 1 LEGEND-2 study4 that was conducted at four sites in China among less heavily pretreated multiple myeloma patients, while all used the same CAR construct, sites used variable conditioning regimens (split versus single). In the site using cyclophosphamide as the lymphodepletion therapy and three split CAR T-cell infusions, partial response or better was achieved in 50 patients (88%) with a median of three prior therapy lines. The complete response rate was high (74%) and minimal residual disease negativity was reached in 39 patients (68%). Median progression-free survival was 19.9 months (95% CI, 9.6-31.0), but 28.2 months among those with complete responses (95% CI, 19.9-not estimable). Median overall survival was also favorable at 36.1 months (95% CI, 26.4-not estimable); it was 35.0 months-not estimable among patients with complete responses. Results from the other three sites were comparable.
Noteworthy among other BCMA-targeting CAR T-cell products in earlier stages of clinical development is orvacabtagene autoleucel, which has a fully human BCMA-specific binding domain. At higher doses (300 × 106 to 600 × 106 CAR T cells) among 62 patients with triple-class–exposed multiple myeloma in the EVOLVE trial, 92% had a partial or better response, with complete responses or better in 36%, all with an encouraging safety profile.
BCMA-targeting CAR T cell toxicity
While van de Donk, Usmani, and Yong, in their review1 note a lack of evidence of off-target toxicity with BCMA-targeting CAR T-cell therapy in clinical studies so far, they do point to several clinical syndromes (cytokine release syndrome, infections, respiratory failure, neurotoxicity, pulmonary aspergillosis, gastrointestinal hemorrhage) caused by cytokines produced during CAR T-cell expansion and to cytopenias and infections arising from prior treatment, bridging therapy, and lymphodepleting conditioning. Deaths attributed to treatment in the above-mentioned trials underscore the need for careful monitoring and early intervention.
Cytokine release syndrome
In the BCMA-targeting CAR T-cell therapy studies, the frequency of cytokine release syndrome varies widely from 17% to 95% but is generally attributed to CAR T-cell activation and is associated with increased serum ferritin concentrations, high c-reactive proteins, and proinflammatory cytokines. High tumor load, in multiple myeloma patients receiving CD19-targeting CAR T cells, was associated with a higher incidence of severe cytokine release syndrome. In a small number of patients, macrophage activation syndrome and hemophagocytic lymphohistiocytosis, the most aggressive variants of cytokine release syndrome, are caused by severe immune activation and lead to multiorgan dysfunction.
Neurotoxicity
Immune effector cell–-associated neurotoxicity syndrome (ICANS) symptoms, in multiple myeloma patients treated with BCMA-targeting CAR T cells, may include delirium, transient confusion, aphasia, lethargy, tremor, dysgraphia, seizures, cerebral edema, and rarely, posterior reversible encephalopathy syndrome.1 While the pathophysiology of CAR T cell–related neurotoxicity is not well understood, high tumor load, higher peak concentrations of CAR T cells, and more severe cytokine release syndrome are more common in patients with severe neurotoxicity. “The frequency of neurotoxicities,” Dr. Yong noted in an interview, “has been reduced by steps taken to mitigate these risk factors.”
High interest in phase I study
A phase I study presented in Blood has attracted interest because the novel BCMA-targeting CAR agent (CT103A) being tested is fully human.4 In an accompanying editorial, Lee and Yong note that doubt for any real potential for durable CAR T therapy responses in multiple myeloma is raised by the poor persistence of multiple myeloma CAR T cells in multiple myeloma patients.3
In the earliest trials of BCMA CARs, while reported rates of objective antimyeloma responses were in the approximately 33%-88% range among patients with relapsed/refractory multiple myeloma (RRMM), persistence was typically 6 months or less. Lee and Yong point out, however, that while correlation between persistence and duration of response (DOR) has been variable, median persistence was 308 days in the phase I study. Wang and colleagues, the phase I study authors, state that levels of CAR T-cell proliferation and duration of cellular persistence may be determinants of DOR in CAR T therapy for multiple myeloma. They observe that the multiple mechanisms potentially responsible for the inability of some CAR T cells to survive in vivo, may include antigen escape, T-cell intrinsic mechanisms, tumor microenvironment–mediated suppression, and host anti-CAR immunity. CARs with humanized or fully human single-chain variable fragments (scFvs), prior studies suggest, may retain antitumor activity through bypassing potential host anti-CAR immunogenicity.
In the study, CT103A, a fully human scFv, was tested in an open-label, single-arm design for safety and preliminary efficacy in 18 patients (8 female; median age 53.5 years) with RRMM (at least three lines of prior therapies including a proteasome inhibitor and an immunomodulatory agent) who had undergone leukapheresis and had received lymphodepletion chemotherapy with fludarabine and cyclophosphamide. Four patients (22.2%) had been treated previously with murine anti-BCMA CAR T cells. Safety and tolerability (including dose-limiting toxicity) were the primary endpoints, with efficacy and pharmacokinetics secondary.
Rapid responses
Two weeks after infusion, the overall response rate (ORR) was 77.8% (14 of 18) and by 1 month it was 88.9% (16 of 18). Eventually, all responded and 72.2% (13 of 18) achieved a complete response (CR) or stringent complete response (sCR). All 17 patients evaluated for minimum residual disease (MRD) in bone marrow were MRD-negative at 10-4 nucleated cells by flow cytometry within 1 month. Median DOR was 325 days (range, 7-573 days) for all patients and 412 days (range, 213-573 days) for the 13 with CR/sCR. CAR transgenes were detectable at the cutoff date in 77.8% of patients, with a median CAR transgene persistence of 307.5 days.
During follow-up, four deaths were reported, including one patient with persistent sCR (sudden severe infection). Progression-free survival (PFS) and overall survival (OS) rates at 1 year were 58.3% and 75%, respectively. Extramedullary myeloma was associated with a shortened PFS (79.1% versus 20.0%, P = .015), but not OS (79.1% versus 60.0%, P = .328) at 1 year.
All patients experienced grade 3 or higher adverse events, most of which were expected hematologic effects of lymphodepleting chemotherapy and CT103A infusions. Grade 1 and 2 cytokine release syndromes occurred in 70.6% patients (17 of 18), with 1 grade 4 event (5.9%). The patients receiving a dose of up to 3.0 × 106 CAR+ T cells/kg required less treatment of cytokine release syndrome than the patients who received a dose of 6.0 × 106 CAR+ T cells/kg. No immune effector cell–associated neurotoxicity syndrome was observed. Antidrug antibody positivity occurred in only 1 patient.
Two characteristics of CT103A may contribute to its long persistence, stated study senior author Jianfeng Zhou, MD, PhD, chairman and professor of the department of hematology, Tongji Hospital in Wuhan, China. “One is the reduced immunogenicity achieved by the fully human construct; another is the relatively low binding affinity of the CAR binder. Notably, four patients who previously received murine BCMA CAR were included and still benefit from CT103A. It demonstrates the possibility of retreatment with a different CAR.” Dr. Zhou also emphasized that the lack of ICANS in the entire cohort reflects the excellent safety profile of CT103A.
The editorial commentary in Blood by Lydia Sarah Hui Lee, MD, and Kwee L. Yong, PhD, underscored impressive responses to CT103A, specifically to the median time to response of 15 days, the 100% ORR, and the not reached median progression-free survival at 394 days).5 The best results in other published nonhuman BCMA CAR T-cell trials, they note, were about 1 month (time to response), approximately 33%-88% (ORR), and median progression-free survival of 7-15 months.
Immune responses, Dr. Yong said in an interview, can guide subsequent treatment. “For example, if a patient previously exposed to BCMA CAR T cells in which the construct is either chimeric or humanized, but retains some murine elements, and had detectable antimurine antibodies, we may aim for a fully human one if we are considering treating with a different BCMA CAR T-cell product.” She added, “On the other hand, a similar patient whose serum did not contain such antibodies may be a candidate for a humanized product that retained some murine elements.”
Wang and colleagues concluded, “Altogether, CT103A is safe and highly active in patients with relapsed/refractory multiple myeloma and can be developed as a promising therapy for relapsed/refractory multiple myeloma.”4 An ongoing multicenter phase II trial with single-arm design is recruiting 100 patients. The infusion dosage, suggested by the phase I trial, is 1 × 106 cells/kg. Endpoints include efficacy and safety.
Improving CAR T
Optimizing CAR design and adapting manufacturing processes to generate cell products enriched for T-cell subsets, such as early memory cells, are among strategies being explored to improve CAR T effectiveness.1 Also, dual-antigen targeting to interdict antigen escape and rational combination treatments to enhance persistence are under investigation, along with efforts to improve CAR T-cell therapy safety (for example, incorporation of a suicide gene safety system). They note further that several groups are researching use of induced pluripotent stem cells to generate large quantities of off-the-shelf CAR T-cell immunotherapies that would circumvent the complex, costly, and time-consuming process of manufacturing patient-specific autologous CAR T cells.
References
1. van de Donk N et al. Lancet Haematol. 2021 June;8(6):e446-61.
2. Munshi NC et al. N Engl J Med 2021; 384:705-716.
3. Berdeja JG et al. The Lancet. 2021 July; 398:314-24.
4. Wang D et al. Blood. 2021 May;137(21):2890-901.
5. Lee L and Yong K. Blood. 2021 May;137(21):2859-60.
In multiple myeloma, survival has been very significantly improved by immunomodulatory drugs, proteasome inhibitors, and CD38-targeting antibodies. Despite these advances, multiple myeloma, which is characterized by malignant proliferation of clonal plasma cells in bone marrow, remains an incurable plasma cell disorder with near-certain relapse after successful treatment. Prognosis for patients who develop triple-class refractory disease is poor, with less than 1-year survival. The substantial unmet therapeutic need extends further to other poor survival multiple myeloma populations that include newly diagnosed patients with high cytogenic risk profiles and those with early relapse after first-line therapy. For all of these, interest in drugs with novel mechanisms of action is naturally high.
More specific, less toxic
Post allogeneic hematopoietic stem-cell transplantation and donor lymphocyte infusion sustained remissions reflect a graft-versus-myeloma effect mediated by donor T cells.1 The substantial morbidity and mortality associated with graft-versus-host disease and opportunistic infections, however, have spurred searches for alternative, more specific, and less toxic T-cell therapies with stronger antitumor activity.
Chimeric antigen receptors (CARs)
In CAR T-cell therapies for multiple myeloma, autologous T cells are harvested from the patient and reprogrammed to target multiple myeloma cells through the introduction of genes that encode CARs, which are fusion proteins coupling an antigen-recognition moiety and a transmembrane-spanning element to a T-cell activation domain (typically CD3 zeta [CD247]). The T cells are then expanded and reinfused to the patient following a lymphodepletion regimen. Five strategies using autologous CAR T cells are currently approved for diffuse large B-cell lymphomas, acute lymphoblastic leukemia, multiple myeloma, and other hematologic malignancies. Notably, in patients with heavily pretreated multiple myeloma, CAR T cells have demonstrated impressive activity.
BCMA-targeting CAR T cells
The B-cell maturation antigen (BCMA; TNFRSF17), which plays an important role in the survival of long-lived plasma cells in bone marrow, is an attractive target for CAR T-cell therapy because it is expressed on normal and malignant plasma cell surfaces and by mature B cells. When ligands (TNFSF 13B/TNFSF13) bind to BCMA expressed on multiple myeloma cell surfaces, survival and proliferation pathways and drug resistance are activated.
High-quality responses have been demonstrated in several trials of anti-BCMA CAR T cells, which kill multiple myeloma cell lines and primary multiple myeloma cells through degranulation of T cells and lysis of tumor cells, even those with low BCMA expression. Based on efficacy in triple-class exposed multiple myeloma that compared favorably to conventional care with improved health-related quality of life, the U.S. Food and Drug Administration gave breakthrough designation to ciltacabtagene autoleucel in December 2019 and approval for idecabtagene vicleucel in March 2021.
Idecabtagene vicleucel
Idecabtagene vicleucel expresses a murine BCMA-targeting single-chain variable fragment with a 4-1BB costimulatory motif. The phase 2 KarMMa study2 evaluated idecabtagene vicleucel (target dose of 450 × 106 CAR T cells; range 150 × 106 to 450 × 106) activity in 128 patients with triple-class exposed multiple myeloma. Partial responses or better were observed in 94 of 128 patients (73%) (95% confidence interval, 66-81); 42 (33%) had a complete response or better (95% CI, 25-41), with a median progression-free survival of 8.8 months (95% CI, 5.6-11.6). Outcomes were improved in the highest fixed-dose group, with partial response or better in 81% (44 of 55), complete response or better in 39% (21), and median overall survival of 12.1 months (95% CI, 8.8-12.3). Patients with high-risk cytogenetic profiles, extramedullary disease, and high tumor burden also had deep and durable responses. Outcomes were less favorable in patients with revised International Staging System stage 3 disease.
Ciltacabtagene autoleucel
Ciltacabtagene autoleucel, a 4-1BB–based CAR T-cell therapy with two BCMA-targeting domains, confers high-avidity binding. In the phase 1b/2 CARTITUDE-1 study, conducted in the United States and Europe, preliminary results in 97 patients showed a 97% response rate with ciltacabtagene autoleucel (target dose 0.75 × 106 CAR T cells per kg), and in 65 patients, a complete response (67%). Progression-free survival at 12 months was 77% (95% CI, 66-84) and overall survival was 89% (95% CI, 80-94).3
In the phase 1 LEGEND-2 study4 that was conducted at four sites in China among less heavily pretreated multiple myeloma patients, while all used the same CAR construct, sites used variable conditioning regimens (split versus single). In the site using cyclophosphamide as the lymphodepletion therapy and three split CAR T-cell infusions, partial response or better was achieved in 50 patients (88%) with a median of three prior therapy lines. The complete response rate was high (74%) and minimal residual disease negativity was reached in 39 patients (68%). Median progression-free survival was 19.9 months (95% CI, 9.6-31.0), but 28.2 months among those with complete responses (95% CI, 19.9-not estimable). Median overall survival was also favorable at 36.1 months (95% CI, 26.4-not estimable); it was 35.0 months-not estimable among patients with complete responses. Results from the other three sites were comparable.
Noteworthy among other BCMA-targeting CAR T-cell products in earlier stages of clinical development is orvacabtagene autoleucel, which has a fully human BCMA-specific binding domain. At higher doses (300 × 106 to 600 × 106 CAR T cells) among 62 patients with triple-class–exposed multiple myeloma in the EVOLVE trial, 92% had a partial or better response, with complete responses or better in 36%, all with an encouraging safety profile.
BCMA-targeting CAR T cell toxicity
While van de Donk, Usmani, and Yong, in their review1 note a lack of evidence of off-target toxicity with BCMA-targeting CAR T-cell therapy in clinical studies so far, they do point to several clinical syndromes (cytokine release syndrome, infections, respiratory failure, neurotoxicity, pulmonary aspergillosis, gastrointestinal hemorrhage) caused by cytokines produced during CAR T-cell expansion and to cytopenias and infections arising from prior treatment, bridging therapy, and lymphodepleting conditioning. Deaths attributed to treatment in the above-mentioned trials underscore the need for careful monitoring and early intervention.
Cytokine release syndrome
In the BCMA-targeting CAR T-cell therapy studies, the frequency of cytokine release syndrome varies widely from 17% to 95% but is generally attributed to CAR T-cell activation and is associated with increased serum ferritin concentrations, high c-reactive proteins, and proinflammatory cytokines. High tumor load, in multiple myeloma patients receiving CD19-targeting CAR T cells, was associated with a higher incidence of severe cytokine release syndrome. In a small number of patients, macrophage activation syndrome and hemophagocytic lymphohistiocytosis, the most aggressive variants of cytokine release syndrome, are caused by severe immune activation and lead to multiorgan dysfunction.
Neurotoxicity
Immune effector cell–-associated neurotoxicity syndrome (ICANS) symptoms, in multiple myeloma patients treated with BCMA-targeting CAR T cells, may include delirium, transient confusion, aphasia, lethargy, tremor, dysgraphia, seizures, cerebral edema, and rarely, posterior reversible encephalopathy syndrome.1 While the pathophysiology of CAR T cell–related neurotoxicity is not well understood, high tumor load, higher peak concentrations of CAR T cells, and more severe cytokine release syndrome are more common in patients with severe neurotoxicity. “The frequency of neurotoxicities,” Dr. Yong noted in an interview, “has been reduced by steps taken to mitigate these risk factors.”
High interest in phase I study
A phase I study presented in Blood has attracted interest because the novel BCMA-targeting CAR agent (CT103A) being tested is fully human.4 In an accompanying editorial, Lee and Yong note that doubt for any real potential for durable CAR T therapy responses in multiple myeloma is raised by the poor persistence of multiple myeloma CAR T cells in multiple myeloma patients.3
In the earliest trials of BCMA CARs, while reported rates of objective antimyeloma responses were in the approximately 33%-88% range among patients with relapsed/refractory multiple myeloma (RRMM), persistence was typically 6 months or less. Lee and Yong point out, however, that while correlation between persistence and duration of response (DOR) has been variable, median persistence was 308 days in the phase I study. Wang and colleagues, the phase I study authors, state that levels of CAR T-cell proliferation and duration of cellular persistence may be determinants of DOR in CAR T therapy for multiple myeloma. They observe that the multiple mechanisms potentially responsible for the inability of some CAR T cells to survive in vivo, may include antigen escape, T-cell intrinsic mechanisms, tumor microenvironment–mediated suppression, and host anti-CAR immunity. CARs with humanized or fully human single-chain variable fragments (scFvs), prior studies suggest, may retain antitumor activity through bypassing potential host anti-CAR immunogenicity.
In the study, CT103A, a fully human scFv, was tested in an open-label, single-arm design for safety and preliminary efficacy in 18 patients (8 female; median age 53.5 years) with RRMM (at least three lines of prior therapies including a proteasome inhibitor and an immunomodulatory agent) who had undergone leukapheresis and had received lymphodepletion chemotherapy with fludarabine and cyclophosphamide. Four patients (22.2%) had been treated previously with murine anti-BCMA CAR T cells. Safety and tolerability (including dose-limiting toxicity) were the primary endpoints, with efficacy and pharmacokinetics secondary.
Rapid responses
Two weeks after infusion, the overall response rate (ORR) was 77.8% (14 of 18) and by 1 month it was 88.9% (16 of 18). Eventually, all responded and 72.2% (13 of 18) achieved a complete response (CR) or stringent complete response (sCR). All 17 patients evaluated for minimum residual disease (MRD) in bone marrow were MRD-negative at 10-4 nucleated cells by flow cytometry within 1 month. Median DOR was 325 days (range, 7-573 days) for all patients and 412 days (range, 213-573 days) for the 13 with CR/sCR. CAR transgenes were detectable at the cutoff date in 77.8% of patients, with a median CAR transgene persistence of 307.5 days.
During follow-up, four deaths were reported, including one patient with persistent sCR (sudden severe infection). Progression-free survival (PFS) and overall survival (OS) rates at 1 year were 58.3% and 75%, respectively. Extramedullary myeloma was associated with a shortened PFS (79.1% versus 20.0%, P = .015), but not OS (79.1% versus 60.0%, P = .328) at 1 year.
All patients experienced grade 3 or higher adverse events, most of which were expected hematologic effects of lymphodepleting chemotherapy and CT103A infusions. Grade 1 and 2 cytokine release syndromes occurred in 70.6% patients (17 of 18), with 1 grade 4 event (5.9%). The patients receiving a dose of up to 3.0 × 106 CAR+ T cells/kg required less treatment of cytokine release syndrome than the patients who received a dose of 6.0 × 106 CAR+ T cells/kg. No immune effector cell–associated neurotoxicity syndrome was observed. Antidrug antibody positivity occurred in only 1 patient.
Two characteristics of CT103A may contribute to its long persistence, stated study senior author Jianfeng Zhou, MD, PhD, chairman and professor of the department of hematology, Tongji Hospital in Wuhan, China. “One is the reduced immunogenicity achieved by the fully human construct; another is the relatively low binding affinity of the CAR binder. Notably, four patients who previously received murine BCMA CAR were included and still benefit from CT103A. It demonstrates the possibility of retreatment with a different CAR.” Dr. Zhou also emphasized that the lack of ICANS in the entire cohort reflects the excellent safety profile of CT103A.
The editorial commentary in Blood by Lydia Sarah Hui Lee, MD, and Kwee L. Yong, PhD, underscored impressive responses to CT103A, specifically to the median time to response of 15 days, the 100% ORR, and the not reached median progression-free survival at 394 days).5 The best results in other published nonhuman BCMA CAR T-cell trials, they note, were about 1 month (time to response), approximately 33%-88% (ORR), and median progression-free survival of 7-15 months.
Immune responses, Dr. Yong said in an interview, can guide subsequent treatment. “For example, if a patient previously exposed to BCMA CAR T cells in which the construct is either chimeric or humanized, but retains some murine elements, and had detectable antimurine antibodies, we may aim for a fully human one if we are considering treating with a different BCMA CAR T-cell product.” She added, “On the other hand, a similar patient whose serum did not contain such antibodies may be a candidate for a humanized product that retained some murine elements.”
Wang and colleagues concluded, “Altogether, CT103A is safe and highly active in patients with relapsed/refractory multiple myeloma and can be developed as a promising therapy for relapsed/refractory multiple myeloma.”4 An ongoing multicenter phase II trial with single-arm design is recruiting 100 patients. The infusion dosage, suggested by the phase I trial, is 1 × 106 cells/kg. Endpoints include efficacy and safety.
Improving CAR T
Optimizing CAR design and adapting manufacturing processes to generate cell products enriched for T-cell subsets, such as early memory cells, are among strategies being explored to improve CAR T effectiveness.1 Also, dual-antigen targeting to interdict antigen escape and rational combination treatments to enhance persistence are under investigation, along with efforts to improve CAR T-cell therapy safety (for example, incorporation of a suicide gene safety system). They note further that several groups are researching use of induced pluripotent stem cells to generate large quantities of off-the-shelf CAR T-cell immunotherapies that would circumvent the complex, costly, and time-consuming process of manufacturing patient-specific autologous CAR T cells.
References
1. van de Donk N et al. Lancet Haematol. 2021 June;8(6):e446-61.
2. Munshi NC et al. N Engl J Med 2021; 384:705-716.
3. Berdeja JG et al. The Lancet. 2021 July; 398:314-24.
4. Wang D et al. Blood. 2021 May;137(21):2890-901.
5. Lee L and Yong K. Blood. 2021 May;137(21):2859-60.
In multiple myeloma, survival has been very significantly improved by immunomodulatory drugs, proteasome inhibitors, and CD38-targeting antibodies. Despite these advances, multiple myeloma, which is characterized by malignant proliferation of clonal plasma cells in bone marrow, remains an incurable plasma cell disorder with near-certain relapse after successful treatment. Prognosis for patients who develop triple-class refractory disease is poor, with less than 1-year survival. The substantial unmet therapeutic need extends further to other poor survival multiple myeloma populations that include newly diagnosed patients with high cytogenic risk profiles and those with early relapse after first-line therapy. For all of these, interest in drugs with novel mechanisms of action is naturally high.
More specific, less toxic
Post allogeneic hematopoietic stem-cell transplantation and donor lymphocyte infusion sustained remissions reflect a graft-versus-myeloma effect mediated by donor T cells.1 The substantial morbidity and mortality associated with graft-versus-host disease and opportunistic infections, however, have spurred searches for alternative, more specific, and less toxic T-cell therapies with stronger antitumor activity.
Chimeric antigen receptors (CARs)
In CAR T-cell therapies for multiple myeloma, autologous T cells are harvested from the patient and reprogrammed to target multiple myeloma cells through the introduction of genes that encode CARs, which are fusion proteins coupling an antigen-recognition moiety and a transmembrane-spanning element to a T-cell activation domain (typically CD3 zeta [CD247]). The T cells are then expanded and reinfused to the patient following a lymphodepletion regimen. Five strategies using autologous CAR T cells are currently approved for diffuse large B-cell lymphomas, acute lymphoblastic leukemia, multiple myeloma, and other hematologic malignancies. Notably, in patients with heavily pretreated multiple myeloma, CAR T cells have demonstrated impressive activity.
BCMA-targeting CAR T cells
The B-cell maturation antigen (BCMA; TNFRSF17), which plays an important role in the survival of long-lived plasma cells in bone marrow, is an attractive target for CAR T-cell therapy because it is expressed on normal and malignant plasma cell surfaces and by mature B cells. When ligands (TNFSF 13B/TNFSF13) bind to BCMA expressed on multiple myeloma cell surfaces, survival and proliferation pathways and drug resistance are activated.
High-quality responses have been demonstrated in several trials of anti-BCMA CAR T cells, which kill multiple myeloma cell lines and primary multiple myeloma cells through degranulation of T cells and lysis of tumor cells, even those with low BCMA expression. Based on efficacy in triple-class exposed multiple myeloma that compared favorably to conventional care with improved health-related quality of life, the U.S. Food and Drug Administration gave breakthrough designation to ciltacabtagene autoleucel in December 2019 and approval for idecabtagene vicleucel in March 2021.
Idecabtagene vicleucel
Idecabtagene vicleucel expresses a murine BCMA-targeting single-chain variable fragment with a 4-1BB costimulatory motif. The phase 2 KarMMa study2 evaluated idecabtagene vicleucel (target dose of 450 × 106 CAR T cells; range 150 × 106 to 450 × 106) activity in 128 patients with triple-class exposed multiple myeloma. Partial responses or better were observed in 94 of 128 patients (73%) (95% confidence interval, 66-81); 42 (33%) had a complete response or better (95% CI, 25-41), with a median progression-free survival of 8.8 months (95% CI, 5.6-11.6). Outcomes were improved in the highest fixed-dose group, with partial response or better in 81% (44 of 55), complete response or better in 39% (21), and median overall survival of 12.1 months (95% CI, 8.8-12.3). Patients with high-risk cytogenetic profiles, extramedullary disease, and high tumor burden also had deep and durable responses. Outcomes were less favorable in patients with revised International Staging System stage 3 disease.
Ciltacabtagene autoleucel
Ciltacabtagene autoleucel, a 4-1BB–based CAR T-cell therapy with two BCMA-targeting domains, confers high-avidity binding. In the phase 1b/2 CARTITUDE-1 study, conducted in the United States and Europe, preliminary results in 97 patients showed a 97% response rate with ciltacabtagene autoleucel (target dose 0.75 × 106 CAR T cells per kg), and in 65 patients, a complete response (67%). Progression-free survival at 12 months was 77% (95% CI, 66-84) and overall survival was 89% (95% CI, 80-94).3
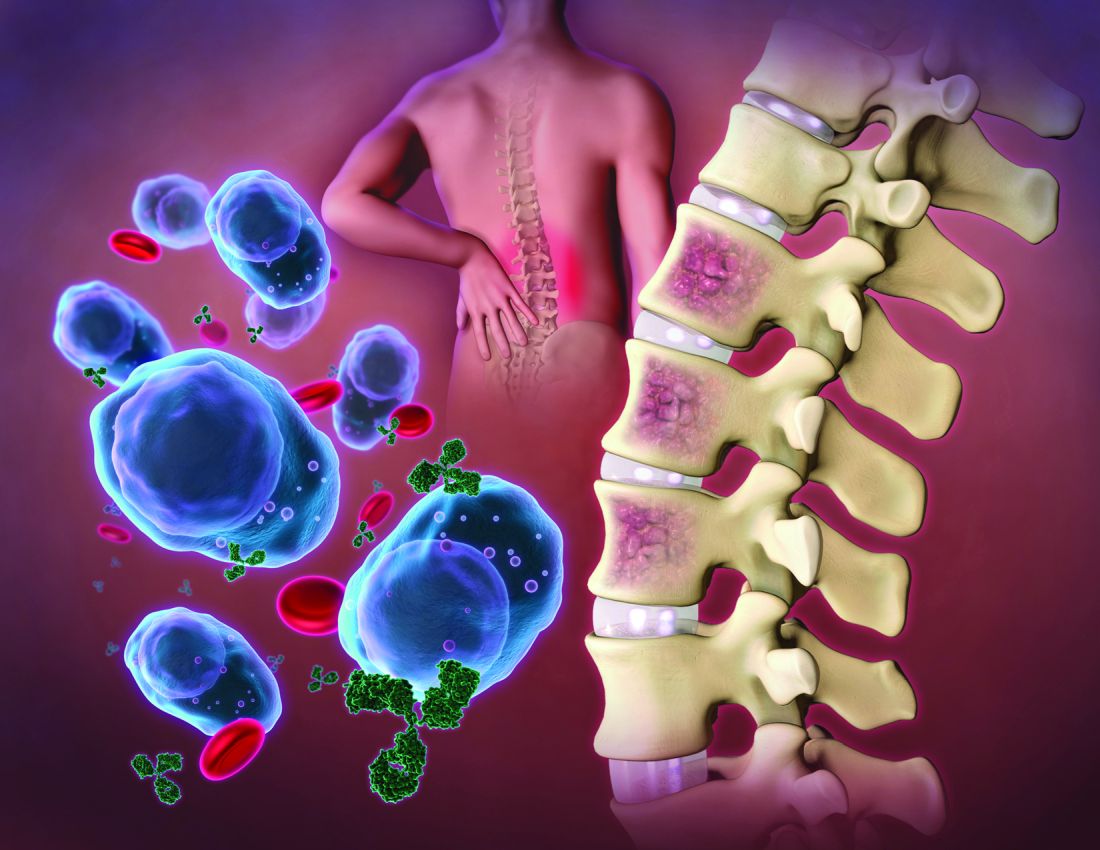
In the phase 1 LEGEND-2 study4 that was conducted at four sites in China among less heavily pretreated multiple myeloma patients, while all used the same CAR construct, sites used variable conditioning regimens (split versus single). In the site using cyclophosphamide as the lymphodepletion therapy and three split CAR T-cell infusions, partial response or better was achieved in 50 patients (88%) with a median of three prior therapy lines. The complete response rate was high (74%) and minimal residual disease negativity was reached in 39 patients (68%). Median progression-free survival was 19.9 months (95% CI, 9.6-31.0), but 28.2 months among those with complete responses (95% CI, 19.9-not estimable). Median overall survival was also favorable at 36.1 months (95% CI, 26.4-not estimable); it was 35.0 months-not estimable among patients with complete responses. Results from the other three sites were comparable.
Noteworthy among other BCMA-targeting CAR T-cell products in earlier stages of clinical development is orvacabtagene autoleucel, which has a fully human BCMA-specific binding domain. At higher doses (300 × 106 to 600 × 106 CAR T cells) among 62 patients with triple-class–exposed multiple myeloma in the EVOLVE trial, 92% had a partial or better response, with complete responses or better in 36%, all with an encouraging safety profile.
BCMA-targeting CAR T cell toxicity
While van de Donk, Usmani, and Yong, in their review1 note a lack of evidence of off-target toxicity with BCMA-targeting CAR T-cell therapy in clinical studies so far, they do point to several clinical syndromes (cytokine release syndrome, infections, respiratory failure, neurotoxicity, pulmonary aspergillosis, gastrointestinal hemorrhage) caused by cytokines produced during CAR T-cell expansion and to cytopenias and infections arising from prior treatment, bridging therapy, and lymphodepleting conditioning. Deaths attributed to treatment in the above-mentioned trials underscore the need for careful monitoring and early intervention.
Cytokine release syndrome
In the BCMA-targeting CAR T-cell therapy studies, the frequency of cytokine release syndrome varies widely from 17% to 95% but is generally attributed to CAR T-cell activation and is associated with increased serum ferritin concentrations, high c-reactive proteins, and proinflammatory cytokines. High tumor load, in multiple myeloma patients receiving CD19-targeting CAR T cells, was associated with a higher incidence of severe cytokine release syndrome. In a small number of patients, macrophage activation syndrome and hemophagocytic lymphohistiocytosis, the most aggressive variants of cytokine release syndrome, are caused by severe immune activation and lead to multiorgan dysfunction.
Neurotoxicity
Immune effector cell–-associated neurotoxicity syndrome (ICANS) symptoms, in multiple myeloma patients treated with BCMA-targeting CAR T cells, may include delirium, transient confusion, aphasia, lethargy, tremor, dysgraphia, seizures, cerebral edema, and rarely, posterior reversible encephalopathy syndrome.1 While the pathophysiology of CAR T cell–related neurotoxicity is not well understood, high tumor load, higher peak concentrations of CAR T cells, and more severe cytokine release syndrome are more common in patients with severe neurotoxicity. “The frequency of neurotoxicities,” Dr. Yong noted in an interview, “has been reduced by steps taken to mitigate these risk factors.”
High interest in phase I study
A phase I study presented in Blood has attracted interest because the novel BCMA-targeting CAR agent (CT103A) being tested is fully human.4 In an accompanying editorial, Lee and Yong note that doubt for any real potential for durable CAR T therapy responses in multiple myeloma is raised by the poor persistence of multiple myeloma CAR T cells in multiple myeloma patients.3
In the earliest trials of BCMA CARs, while reported rates of objective antimyeloma responses were in the approximately 33%-88% range among patients with relapsed/refractory multiple myeloma (RRMM), persistence was typically 6 months or less. Lee and Yong point out, however, that while correlation between persistence and duration of response (DOR) has been variable, median persistence was 308 days in the phase I study. Wang and colleagues, the phase I study authors, state that levels of CAR T-cell proliferation and duration of cellular persistence may be determinants of DOR in CAR T therapy for multiple myeloma. They observe that the multiple mechanisms potentially responsible for the inability of some CAR T cells to survive in vivo, may include antigen escape, T-cell intrinsic mechanisms, tumor microenvironment–mediated suppression, and host anti-CAR immunity. CARs with humanized or fully human single-chain variable fragments (scFvs), prior studies suggest, may retain antitumor activity through bypassing potential host anti-CAR immunogenicity.
In the study, CT103A, a fully human scFv, was tested in an open-label, single-arm design for safety and preliminary efficacy in 18 patients (8 female; median age 53.5 years) with RRMM (at least three lines of prior therapies including a proteasome inhibitor and an immunomodulatory agent) who had undergone leukapheresis and had received lymphodepletion chemotherapy with fludarabine and cyclophosphamide. Four patients (22.2%) had been treated previously with murine anti-BCMA CAR T cells. Safety and tolerability (including dose-limiting toxicity) were the primary endpoints, with efficacy and pharmacokinetics secondary.
Rapid responses
Two weeks after infusion, the overall response rate (ORR) was 77.8% (14 of 18) and by 1 month it was 88.9% (16 of 18). Eventually, all responded and 72.2% (13 of 18) achieved a complete response (CR) or stringent complete response (sCR). All 17 patients evaluated for minimum residual disease (MRD) in bone marrow were MRD-negative at 10-4 nucleated cells by flow cytometry within 1 month. Median DOR was 325 days (range, 7-573 days) for all patients and 412 days (range, 213-573 days) for the 13 with CR/sCR. CAR transgenes were detectable at the cutoff date in 77.8% of patients, with a median CAR transgene persistence of 307.5 days.
During follow-up, four deaths were reported, including one patient with persistent sCR (sudden severe infection). Progression-free survival (PFS) and overall survival (OS) rates at 1 year were 58.3% and 75%, respectively. Extramedullary myeloma was associated with a shortened PFS (79.1% versus 20.0%, P = .015), but not OS (79.1% versus 60.0%, P = .328) at 1 year.
All patients experienced grade 3 or higher adverse events, most of which were expected hematologic effects of lymphodepleting chemotherapy and CT103A infusions. Grade 1 and 2 cytokine release syndromes occurred in 70.6% patients (17 of 18), with 1 grade 4 event (5.9%). The patients receiving a dose of up to 3.0 × 106 CAR+ T cells/kg required less treatment of cytokine release syndrome than the patients who received a dose of 6.0 × 106 CAR+ T cells/kg. No immune effector cell–associated neurotoxicity syndrome was observed. Antidrug antibody positivity occurred in only 1 patient.
Two characteristics of CT103A may contribute to its long persistence, stated study senior author Jianfeng Zhou, MD, PhD, chairman and professor of the department of hematology, Tongji Hospital in Wuhan, China. “One is the reduced immunogenicity achieved by the fully human construct; another is the relatively low binding affinity of the CAR binder. Notably, four patients who previously received murine BCMA CAR were included and still benefit from CT103A. It demonstrates the possibility of retreatment with a different CAR.” Dr. Zhou also emphasized that the lack of ICANS in the entire cohort reflects the excellent safety profile of CT103A.
The editorial commentary in Blood by Lydia Sarah Hui Lee, MD, and Kwee L. Yong, PhD, underscored impressive responses to CT103A, specifically to the median time to response of 15 days, the 100% ORR, and the not reached median progression-free survival at 394 days).5 The best results in other published nonhuman BCMA CAR T-cell trials, they note, were about 1 month (time to response), approximately 33%-88% (ORR), and median progression-free survival of 7-15 months.
Immune responses, Dr. Yong said in an interview, can guide subsequent treatment. “For example, if a patient previously exposed to BCMA CAR T cells in which the construct is either chimeric or humanized, but retains some murine elements, and had detectable antimurine antibodies, we may aim for a fully human one if we are considering treating with a different BCMA CAR T-cell product.” She added, “On the other hand, a similar patient whose serum did not contain such antibodies may be a candidate for a humanized product that retained some murine elements.”
Wang and colleagues concluded, “Altogether, CT103A is safe and highly active in patients with relapsed/refractory multiple myeloma and can be developed as a promising therapy for relapsed/refractory multiple myeloma.”4 An ongoing multicenter phase II trial with single-arm design is recruiting 100 patients. The infusion dosage, suggested by the phase I trial, is 1 × 106 cells/kg. Endpoints include efficacy and safety.
Improving CAR T
Optimizing CAR design and adapting manufacturing processes to generate cell products enriched for T-cell subsets, such as early memory cells, are among strategies being explored to improve CAR T effectiveness.1 Also, dual-antigen targeting to interdict antigen escape and rational combination treatments to enhance persistence are under investigation, along with efforts to improve CAR T-cell therapy safety (for example, incorporation of a suicide gene safety system). They note further that several groups are researching use of induced pluripotent stem cells to generate large quantities of off-the-shelf CAR T-cell immunotherapies that would circumvent the complex, costly, and time-consuming process of manufacturing patient-specific autologous CAR T cells.
References
1. van de Donk N et al. Lancet Haematol. 2021 June;8(6):e446-61.
2. Munshi NC et al. N Engl J Med 2021; 384:705-716.
3. Berdeja JG et al. The Lancet. 2021 July; 398:314-24.
4. Wang D et al. Blood. 2021 May;137(21):2890-901.
5. Lee L and Yong K. Blood. 2021 May;137(21):2859-60.
Isatuximab added to RVd boosts response in new myeloma
ATLANTA -
The drug is isatuximab (Sarclisa, Sanofi), an anti-CD38 antibody that was approved last year for use in patients with advanced disease.
Now it has shown benefit in patients who have been newly diagnosed with the disease. When isatuximab was added onto a usual triplet therapy for myeloma, it increased the likelihood that patients would be negative for minimal residual disease (MRD) at the end of the induction phase of treatment, thereby increasing their chances for a successful autologous stem cell transplant (ASCT).
The new results come from the GMMG-HD7 trial, in which all patients were treated with the triplet combination of lenalidomide (Revlimid), bortezomib (Velcade), and dexamethasone (RVd).
Some patients, after randomization, also received isatuximab, and in this group, the MRD-negativity rate was 50.1% at the end of induction therapy compared with 35.6% for patients treated with RVd alone.
Patients who are MRD-negative at the time of ASCT have significantly better outcomes than patients who remain MRD-positive.
“Isa-RVd is the first regimen to demonstrate significant MRD-negativity benefit at the end of induction versus RVd in a phase 3 trial,” reported Hartmut Goldschmidt, MD, from University Hospital Heidelberg, Germany.
“The benefits of the addition of Isa to RVd versus RVd regarding MRD negativity after induction therapy was consistent in all subgroups,” he added.
Dr. Goldschmidt spoke at a press briefing prior to his presentation of the data here at the annual meeting of the American Society of Hematology (ASH).
“I think that these data are encouraging, but they are preliminary, and we need mature data to be absolutely certain about whether this presents a major advance in treatment,” commented Ravi Vij, MD, from the Siteman Cancer Center and Washington University School of Medicine in St. Louis. Dr. Vij was not involved in the study.
“We know that for transplant-eligible patients, for whom this trial was conducted, the field is moving toward giving four drugs for induction,” he said in an interview with this news organization.
He noted that the combination of RVd with the other currently available anti-CD38 antibody, daratumumab (Darzalex), was approved for this indication in the United States in Jan. 2021.
Dr. Vij said that isatuximab has been slow to catch on in the United States both because it was approved after clinicians had already become familiar with daratumumab and because it is given intravenously, compared with subcutaneous administration of the latest formulation of daratumumab.
“Whereas isatuximab can take an hour-and-a-half with each infusion, daratumumab takes 5 minutes for an injection and the patient is out of there, so it is convenient both for the patient and the treating institution,” he said.
MRD vs. CR?
Dr. Goldschmidt was asked during the briefing about whether MRD-negativity or complete response rates are better predictors of progression-free survival (PFS). He replied that with current standardized sequencing techniques and sensitivity down to 10-6, “it’s a big benefit to analyze MRD negativity, and there is ongoing discussion between colleagues from the myeloma group with the Food and Drug Administration about how we can merge the data and predict PFS and overall survival.”
Laurie Sehn, MD, MPH, from the BC Cancer Centre for Lymphoid Cancer, Vancouver, who moderated the briefing, commented that “we’re desperately looking for surrogate markers to speed up answers to clinical trials, and I think MRD in myeloma is quickly becoming a very important surrogate marker.”
GMMG-7 results
For their trial, Dr. Goldschmidt and colleagues enrolled 662 patients with newly diagnosed multiple myeloma who were candidates for high-dose therapy and ASCT and after stratification by revised International Staging System (r-ISS) criteria, randomly assigned them six three-week cycles of induction therapy with Isa-RVd or RVd alone.
Following ASCT, patients were again randomized to maintenance with either isatuximab plus lenalidomide or lenalidomide alone.
As noted before, MRD rates at the end of induction were 50.1% with Isa-RVd versus 35.6% with RVd alone, translating to a hazard ratio favoring the four-drug combination of 1.83 (P < .001).
Treatment with Isa-RVd was the only significant predictor for the likelihood of MRD negativity in a multivariate analysis controlling for treatment group, r-ISS status, performance status, renal impairment, age, and sex.
Although the rate of complete responses at the end of induction was similar between the treatment groups, the rate of very good partial response or better was higher with the isatuximab-containing combination (77.3% vs. 60.5%; P < .001).
The respective rates of disease progression at the end of induction in the Isa-RVd and RVd groups were 1.5% versus 4.0%.
The rates of adverse events were generally similar between the groups, except a higher proportion of patients had leukocytopenia or neutropenia in the Isa-RVd than the RVdgroup (26.4% vs. 9.1%). There were four deaths in the Isa-RVd group and eight in the RVd group. Most of the deaths were attributable to disease progression or COVID-19, said Dr. Goldschmidt.
The study was funded by Sanofi. Dr. Goldschmidt has disclosed honoraria and research grants from Sanofi and others. Dr. Vij has disclosed honoraria or advisory board activities from various companies, including Sanofi. Dr. Sehn is a consultant for and has received honoraria from various companies, not including Sanofi.
A version of this article first appeared on Medscape.com.
ATLANTA -
The drug is isatuximab (Sarclisa, Sanofi), an anti-CD38 antibody that was approved last year for use in patients with advanced disease.
Now it has shown benefit in patients who have been newly diagnosed with the disease. When isatuximab was added onto a usual triplet therapy for myeloma, it increased the likelihood that patients would be negative for minimal residual disease (MRD) at the end of the induction phase of treatment, thereby increasing their chances for a successful autologous stem cell transplant (ASCT).
The new results come from the GMMG-HD7 trial, in which all patients were treated with the triplet combination of lenalidomide (Revlimid), bortezomib (Velcade), and dexamethasone (RVd).
Some patients, after randomization, also received isatuximab, and in this group, the MRD-negativity rate was 50.1% at the end of induction therapy compared with 35.6% for patients treated with RVd alone.
Patients who are MRD-negative at the time of ASCT have significantly better outcomes than patients who remain MRD-positive.
“Isa-RVd is the first regimen to demonstrate significant MRD-negativity benefit at the end of induction versus RVd in a phase 3 trial,” reported Hartmut Goldschmidt, MD, from University Hospital Heidelberg, Germany.
“The benefits of the addition of Isa to RVd versus RVd regarding MRD negativity after induction therapy was consistent in all subgroups,” he added.
Dr. Goldschmidt spoke at a press briefing prior to his presentation of the data here at the annual meeting of the American Society of Hematology (ASH).
“I think that these data are encouraging, but they are preliminary, and we need mature data to be absolutely certain about whether this presents a major advance in treatment,” commented Ravi Vij, MD, from the Siteman Cancer Center and Washington University School of Medicine in St. Louis. Dr. Vij was not involved in the study.
“We know that for transplant-eligible patients, for whom this trial was conducted, the field is moving toward giving four drugs for induction,” he said in an interview with this news organization.
He noted that the combination of RVd with the other currently available anti-CD38 antibody, daratumumab (Darzalex), was approved for this indication in the United States in Jan. 2021.
Dr. Vij said that isatuximab has been slow to catch on in the United States both because it was approved after clinicians had already become familiar with daratumumab and because it is given intravenously, compared with subcutaneous administration of the latest formulation of daratumumab.
“Whereas isatuximab can take an hour-and-a-half with each infusion, daratumumab takes 5 minutes for an injection and the patient is out of there, so it is convenient both for the patient and the treating institution,” he said.
MRD vs. CR?
Dr. Goldschmidt was asked during the briefing about whether MRD-negativity or complete response rates are better predictors of progression-free survival (PFS). He replied that with current standardized sequencing techniques and sensitivity down to 10-6, “it’s a big benefit to analyze MRD negativity, and there is ongoing discussion between colleagues from the myeloma group with the Food and Drug Administration about how we can merge the data and predict PFS and overall survival.”
Laurie Sehn, MD, MPH, from the BC Cancer Centre for Lymphoid Cancer, Vancouver, who moderated the briefing, commented that “we’re desperately looking for surrogate markers to speed up answers to clinical trials, and I think MRD in myeloma is quickly becoming a very important surrogate marker.”
GMMG-7 results
For their trial, Dr. Goldschmidt and colleagues enrolled 662 patients with newly diagnosed multiple myeloma who were candidates for high-dose therapy and ASCT and after stratification by revised International Staging System (r-ISS) criteria, randomly assigned them six three-week cycles of induction therapy with Isa-RVd or RVd alone.
Following ASCT, patients were again randomized to maintenance with either isatuximab plus lenalidomide or lenalidomide alone.
As noted before, MRD rates at the end of induction were 50.1% with Isa-RVd versus 35.6% with RVd alone, translating to a hazard ratio favoring the four-drug combination of 1.83 (P < .001).
Treatment with Isa-RVd was the only significant predictor for the likelihood of MRD negativity in a multivariate analysis controlling for treatment group, r-ISS status, performance status, renal impairment, age, and sex.
Although the rate of complete responses at the end of induction was similar between the treatment groups, the rate of very good partial response or better was higher with the isatuximab-containing combination (77.3% vs. 60.5%; P < .001).
The respective rates of disease progression at the end of induction in the Isa-RVd and RVd groups were 1.5% versus 4.0%.
The rates of adverse events were generally similar between the groups, except a higher proportion of patients had leukocytopenia or neutropenia in the Isa-RVd than the RVdgroup (26.4% vs. 9.1%). There were four deaths in the Isa-RVd group and eight in the RVd group. Most of the deaths were attributable to disease progression or COVID-19, said Dr. Goldschmidt.
The study was funded by Sanofi. Dr. Goldschmidt has disclosed honoraria and research grants from Sanofi and others. Dr. Vij has disclosed honoraria or advisory board activities from various companies, including Sanofi. Dr. Sehn is a consultant for and has received honoraria from various companies, not including Sanofi.
A version of this article first appeared on Medscape.com.
ATLANTA -
The drug is isatuximab (Sarclisa, Sanofi), an anti-CD38 antibody that was approved last year for use in patients with advanced disease.
Now it has shown benefit in patients who have been newly diagnosed with the disease. When isatuximab was added onto a usual triplet therapy for myeloma, it increased the likelihood that patients would be negative for minimal residual disease (MRD) at the end of the induction phase of treatment, thereby increasing their chances for a successful autologous stem cell transplant (ASCT).
The new results come from the GMMG-HD7 trial, in which all patients were treated with the triplet combination of lenalidomide (Revlimid), bortezomib (Velcade), and dexamethasone (RVd).
Some patients, after randomization, also received isatuximab, and in this group, the MRD-negativity rate was 50.1% at the end of induction therapy compared with 35.6% for patients treated with RVd alone.
Patients who are MRD-negative at the time of ASCT have significantly better outcomes than patients who remain MRD-positive.
“Isa-RVd is the first regimen to demonstrate significant MRD-negativity benefit at the end of induction versus RVd in a phase 3 trial,” reported Hartmut Goldschmidt, MD, from University Hospital Heidelberg, Germany.
“The benefits of the addition of Isa to RVd versus RVd regarding MRD negativity after induction therapy was consistent in all subgroups,” he added.
Dr. Goldschmidt spoke at a press briefing prior to his presentation of the data here at the annual meeting of the American Society of Hematology (ASH).
“I think that these data are encouraging, but they are preliminary, and we need mature data to be absolutely certain about whether this presents a major advance in treatment,” commented Ravi Vij, MD, from the Siteman Cancer Center and Washington University School of Medicine in St. Louis. Dr. Vij was not involved in the study.
“We know that for transplant-eligible patients, for whom this trial was conducted, the field is moving toward giving four drugs for induction,” he said in an interview with this news organization.
He noted that the combination of RVd with the other currently available anti-CD38 antibody, daratumumab (Darzalex), was approved for this indication in the United States in Jan. 2021.
Dr. Vij said that isatuximab has been slow to catch on in the United States both because it was approved after clinicians had already become familiar with daratumumab and because it is given intravenously, compared with subcutaneous administration of the latest formulation of daratumumab.
“Whereas isatuximab can take an hour-and-a-half with each infusion, daratumumab takes 5 minutes for an injection and the patient is out of there, so it is convenient both for the patient and the treating institution,” he said.
MRD vs. CR?
Dr. Goldschmidt was asked during the briefing about whether MRD-negativity or complete response rates are better predictors of progression-free survival (PFS). He replied that with current standardized sequencing techniques and sensitivity down to 10-6, “it’s a big benefit to analyze MRD negativity, and there is ongoing discussion between colleagues from the myeloma group with the Food and Drug Administration about how we can merge the data and predict PFS and overall survival.”
Laurie Sehn, MD, MPH, from the BC Cancer Centre for Lymphoid Cancer, Vancouver, who moderated the briefing, commented that “we’re desperately looking for surrogate markers to speed up answers to clinical trials, and I think MRD in myeloma is quickly becoming a very important surrogate marker.”
GMMG-7 results
For their trial, Dr. Goldschmidt and colleagues enrolled 662 patients with newly diagnosed multiple myeloma who were candidates for high-dose therapy and ASCT and after stratification by revised International Staging System (r-ISS) criteria, randomly assigned them six three-week cycles of induction therapy with Isa-RVd or RVd alone.
Following ASCT, patients were again randomized to maintenance with either isatuximab plus lenalidomide or lenalidomide alone.
As noted before, MRD rates at the end of induction were 50.1% with Isa-RVd versus 35.6% with RVd alone, translating to a hazard ratio favoring the four-drug combination of 1.83 (P < .001).
Treatment with Isa-RVd was the only significant predictor for the likelihood of MRD negativity in a multivariate analysis controlling for treatment group, r-ISS status, performance status, renal impairment, age, and sex.
Although the rate of complete responses at the end of induction was similar between the treatment groups, the rate of very good partial response or better was higher with the isatuximab-containing combination (77.3% vs. 60.5%; P < .001).
The respective rates of disease progression at the end of induction in the Isa-RVd and RVd groups were 1.5% versus 4.0%.
The rates of adverse events were generally similar between the groups, except a higher proportion of patients had leukocytopenia or neutropenia in the Isa-RVd than the RVdgroup (26.4% vs. 9.1%). There were four deaths in the Isa-RVd group and eight in the RVd group. Most of the deaths were attributable to disease progression or COVID-19, said Dr. Goldschmidt.
The study was funded by Sanofi. Dr. Goldschmidt has disclosed honoraria and research grants from Sanofi and others. Dr. Vij has disclosed honoraria or advisory board activities from various companies, including Sanofi. Dr. Sehn is a consultant for and has received honoraria from various companies, not including Sanofi.
A version of this article first appeared on Medscape.com.
AT ASH 2021
FDA approves time-saving combo for r/r multiple myeloma
The U.S. Food and Drug Administration who have had one to three prior lines of therapy.
Using the newly approved combination in this setting is a time-saver for patients and clinics, observed an investigator.
“The approval of subcutaneous daratumumab in combination with Kd will help clinicians address unmet patient needs by reducing the administration time from hours to just minutes and reducing the frequency of infusion-related reactions, as compared to the intravenous daratumumab formulation in combination with Kd,” said Ajai Chari, MD, of Mount Sinai Cancer Clinical Trials Office in New York City in a Janssen press statement.
Efficacy data for the new approval come from a single-arm cohort of PLEIADES, a multicohort, open-label trial. The cohort included 66 patients with relapsed or refractory multiple myeloma who had received one or more prior lines of therapy. Patients received daratumumab + hyaluronidase-fihj subcutaneously in combination with carfilzomib and dexamethasone.
The main efficacy outcome measure was overall response rate, which was 84.8%. At a median follow-up of 9.2 months, the median duration of response had not been reached.
The response rate with the new combination, which features a subcutaneous injection, was akin to those with the older combination, which features the more time-consuming IV administration and was FDA approved, according to the company press release.
The most common adverse reactions (≥20%) occurring in patients treated with Darzalex Faspro, Kyprolis, and dexamethasone were upper respiratory tract infections, fatigue, insomnia, hypertension, diarrhea, cough, dyspnea, headache, pyrexia, nausea, and edema peripheral.
A version of this article first appeared on Medscape.com .
The U.S. Food and Drug Administration who have had one to three prior lines of therapy.
Using the newly approved combination in this setting is a time-saver for patients and clinics, observed an investigator.
“The approval of subcutaneous daratumumab in combination with Kd will help clinicians address unmet patient needs by reducing the administration time from hours to just minutes and reducing the frequency of infusion-related reactions, as compared to the intravenous daratumumab formulation in combination with Kd,” said Ajai Chari, MD, of Mount Sinai Cancer Clinical Trials Office in New York City in a Janssen press statement.
Efficacy data for the new approval come from a single-arm cohort of PLEIADES, a multicohort, open-label trial. The cohort included 66 patients with relapsed or refractory multiple myeloma who had received one or more prior lines of therapy. Patients received daratumumab + hyaluronidase-fihj subcutaneously in combination with carfilzomib and dexamethasone.
The main efficacy outcome measure was overall response rate, which was 84.8%. At a median follow-up of 9.2 months, the median duration of response had not been reached.
The response rate with the new combination, which features a subcutaneous injection, was akin to those with the older combination, which features the more time-consuming IV administration and was FDA approved, according to the company press release.
The most common adverse reactions (≥20%) occurring in patients treated with Darzalex Faspro, Kyprolis, and dexamethasone were upper respiratory tract infections, fatigue, insomnia, hypertension, diarrhea, cough, dyspnea, headache, pyrexia, nausea, and edema peripheral.
A version of this article first appeared on Medscape.com .
The U.S. Food and Drug Administration who have had one to three prior lines of therapy.
Using the newly approved combination in this setting is a time-saver for patients and clinics, observed an investigator.
“The approval of subcutaneous daratumumab in combination with Kd will help clinicians address unmet patient needs by reducing the administration time from hours to just minutes and reducing the frequency of infusion-related reactions, as compared to the intravenous daratumumab formulation in combination with Kd,” said Ajai Chari, MD, of Mount Sinai Cancer Clinical Trials Office in New York City in a Janssen press statement.
Efficacy data for the new approval come from a single-arm cohort of PLEIADES, a multicohort, open-label trial. The cohort included 66 patients with relapsed or refractory multiple myeloma who had received one or more prior lines of therapy. Patients received daratumumab + hyaluronidase-fihj subcutaneously in combination with carfilzomib and dexamethasone.
The main efficacy outcome measure was overall response rate, which was 84.8%. At a median follow-up of 9.2 months, the median duration of response had not been reached.
The response rate with the new combination, which features a subcutaneous injection, was akin to those with the older combination, which features the more time-consuming IV administration and was FDA approved, according to the company press release.
The most common adverse reactions (≥20%) occurring in patients treated with Darzalex Faspro, Kyprolis, and dexamethasone were upper respiratory tract infections, fatigue, insomnia, hypertension, diarrhea, cough, dyspnea, headache, pyrexia, nausea, and edema peripheral.
A version of this article first appeared on Medscape.com .
Severe COVID two times higher for cancer patients
A new systematic review and meta-analysis finds that unvaccinated cancer patients who contracted COVID-19 last year, were more than two times more likely – than people without cancer – to develop a case of COVID-19 so severe it required hospitalization in an intensive care unit.
“Our study provides the most precise measure to date of the effect of COVID-19 in cancer patients,” wrote researchers who were led by Paolo Boffetta, MD, MPH, a specialist in population science with the Stony Brook Cancer Center in New York.
Dr. Boffetta and colleagues also found that patients with hematologic neoplasms had a higher mortality rate from COVID-19 comparable to that of all cancers combined.
Cancer patients have long been considered to be among those patients who are at high risk of developing COVID-19, and if they contract the disease, they are at high risk of having poor outcomes. Other high-risk patients include those with hypertension, diabetes, chronic kidney disease, or COPD, or the elderly. But how high the risk of developing severe COVID-19 disease is for cancer patients hasn’t yet been documented on a wide scale.
The study, which was made available as a preprint on medRxiv on Oct. 23, is based on an analysis of COVID-19 cases that were documented in 35 reviews, meta-analyses, case reports, and studies indexed in PubMed from authors in North America, Europe, and Asia.
In this study, the pooled odds ratio for mortality for all patients with any cancer was 2.32 (95% confidence interval, 1.82-2.94; 24 studies). For ICU admission, the odds ratio was 2.39 (95% CI, 1.90-3.02; I2 0.0%; 5 studies). And, for disease severity or hospitalization, it was 2.08 (95% CI, 1.60-2.72; I2 92.1%; 15 studies). The pooled mortality odds ratio for hematologic neoplasms was 2.14 (95% CI, 1.87-2.44; I2 20.8%; 8 studies).
Their findings, which have not yet been peer reviewed, confirmed the results of a similar analysis from China published as a preprint in May 2020. The analysis included 181,323 patients (23,736 cancer patients) from 26 studies reported an odds ratio of 2.54 (95% CI, 1.47-4.42). “Cancer patients with COVID-19 have an increased likelihood of death compared to non-cancer COVID-19 patients,” Venkatesulu et al. wrote. And a systematic review and meta-analysis of five studies of 2,619 patients published in October 2020 in Medicine also found a significantly higher risk of death from COVID-19 among cancer patients (odds ratio, 2.63; 95% confidence interval, 1.14-6.06; P = .023; I2 = 26.4%).
Fakih et al., writing in the journal Hematology/Oncology and Stem Cell Therapy conducted a meta-analysis early last year finding a threefold increase for admission to the intensive care unit, an almost fourfold increase for a severe SARS-CoV-2 infection, and a fivefold increase for being intubated.
The three studies show that mortality rates were higher early in the pandemic “when diagnosis and treatment for SARS-CoV-2 might have been delayed, resulting in higher death rate,” Boffetta et al. wrote, adding that their analysis showed only a twofold increase most likely because it was a year-long analysis.
“Future studies will be able to better analyze this association for the different subtypes of cancer. Furthermore, they will eventually be able to evaluate whether the difference among vaccinated population is reduced,” Boffetta et al. wrote.
The authors noted several limitations for the study, including the fact that many of the studies included in the analysis did not include sex, age, comorbidities, and therapy. Nor were the authors able to analyze specific cancers other than hematologic neoplasms.
The authors declared no conflicts of interest.
A new systematic review and meta-analysis finds that unvaccinated cancer patients who contracted COVID-19 last year, were more than two times more likely – than people without cancer – to develop a case of COVID-19 so severe it required hospitalization in an intensive care unit.
“Our study provides the most precise measure to date of the effect of COVID-19 in cancer patients,” wrote researchers who were led by Paolo Boffetta, MD, MPH, a specialist in population science with the Stony Brook Cancer Center in New York.
Dr. Boffetta and colleagues also found that patients with hematologic neoplasms had a higher mortality rate from COVID-19 comparable to that of all cancers combined.
Cancer patients have long been considered to be among those patients who are at high risk of developing COVID-19, and if they contract the disease, they are at high risk of having poor outcomes. Other high-risk patients include those with hypertension, diabetes, chronic kidney disease, or COPD, or the elderly. But how high the risk of developing severe COVID-19 disease is for cancer patients hasn’t yet been documented on a wide scale.
The study, which was made available as a preprint on medRxiv on Oct. 23, is based on an analysis of COVID-19 cases that were documented in 35 reviews, meta-analyses, case reports, and studies indexed in PubMed from authors in North America, Europe, and Asia.
In this study, the pooled odds ratio for mortality for all patients with any cancer was 2.32 (95% confidence interval, 1.82-2.94; 24 studies). For ICU admission, the odds ratio was 2.39 (95% CI, 1.90-3.02; I2 0.0%; 5 studies). And, for disease severity or hospitalization, it was 2.08 (95% CI, 1.60-2.72; I2 92.1%; 15 studies). The pooled mortality odds ratio for hematologic neoplasms was 2.14 (95% CI, 1.87-2.44; I2 20.8%; 8 studies).
Their findings, which have not yet been peer reviewed, confirmed the results of a similar analysis from China published as a preprint in May 2020. The analysis included 181,323 patients (23,736 cancer patients) from 26 studies reported an odds ratio of 2.54 (95% CI, 1.47-4.42). “Cancer patients with COVID-19 have an increased likelihood of death compared to non-cancer COVID-19 patients,” Venkatesulu et al. wrote. And a systematic review and meta-analysis of five studies of 2,619 patients published in October 2020 in Medicine also found a significantly higher risk of death from COVID-19 among cancer patients (odds ratio, 2.63; 95% confidence interval, 1.14-6.06; P = .023; I2 = 26.4%).
Fakih et al., writing in the journal Hematology/Oncology and Stem Cell Therapy conducted a meta-analysis early last year finding a threefold increase for admission to the intensive care unit, an almost fourfold increase for a severe SARS-CoV-2 infection, and a fivefold increase for being intubated.
The three studies show that mortality rates were higher early in the pandemic “when diagnosis and treatment for SARS-CoV-2 might have been delayed, resulting in higher death rate,” Boffetta et al. wrote, adding that their analysis showed only a twofold increase most likely because it was a year-long analysis.
“Future studies will be able to better analyze this association for the different subtypes of cancer. Furthermore, they will eventually be able to evaluate whether the difference among vaccinated population is reduced,” Boffetta et al. wrote.
The authors noted several limitations for the study, including the fact that many of the studies included in the analysis did not include sex, age, comorbidities, and therapy. Nor were the authors able to analyze specific cancers other than hematologic neoplasms.
The authors declared no conflicts of interest.
A new systematic review and meta-analysis finds that unvaccinated cancer patients who contracted COVID-19 last year, were more than two times more likely – than people without cancer – to develop a case of COVID-19 so severe it required hospitalization in an intensive care unit.
“Our study provides the most precise measure to date of the effect of COVID-19 in cancer patients,” wrote researchers who were led by Paolo Boffetta, MD, MPH, a specialist in population science with the Stony Brook Cancer Center in New York.
Dr. Boffetta and colleagues also found that patients with hematologic neoplasms had a higher mortality rate from COVID-19 comparable to that of all cancers combined.
Cancer patients have long been considered to be among those patients who are at high risk of developing COVID-19, and if they contract the disease, they are at high risk of having poor outcomes. Other high-risk patients include those with hypertension, diabetes, chronic kidney disease, or COPD, or the elderly. But how high the risk of developing severe COVID-19 disease is for cancer patients hasn’t yet been documented on a wide scale.
The study, which was made available as a preprint on medRxiv on Oct. 23, is based on an analysis of COVID-19 cases that were documented in 35 reviews, meta-analyses, case reports, and studies indexed in PubMed from authors in North America, Europe, and Asia.
In this study, the pooled odds ratio for mortality for all patients with any cancer was 2.32 (95% confidence interval, 1.82-2.94; 24 studies). For ICU admission, the odds ratio was 2.39 (95% CI, 1.90-3.02; I2 0.0%; 5 studies). And, for disease severity or hospitalization, it was 2.08 (95% CI, 1.60-2.72; I2 92.1%; 15 studies). The pooled mortality odds ratio for hematologic neoplasms was 2.14 (95% CI, 1.87-2.44; I2 20.8%; 8 studies).
Their findings, which have not yet been peer reviewed, confirmed the results of a similar analysis from China published as a preprint in May 2020. The analysis included 181,323 patients (23,736 cancer patients) from 26 studies reported an odds ratio of 2.54 (95% CI, 1.47-4.42). “Cancer patients with COVID-19 have an increased likelihood of death compared to non-cancer COVID-19 patients,” Venkatesulu et al. wrote. And a systematic review and meta-analysis of five studies of 2,619 patients published in October 2020 in Medicine also found a significantly higher risk of death from COVID-19 among cancer patients (odds ratio, 2.63; 95% confidence interval, 1.14-6.06; P = .023; I2 = 26.4%).
Fakih et al., writing in the journal Hematology/Oncology and Stem Cell Therapy conducted a meta-analysis early last year finding a threefold increase for admission to the intensive care unit, an almost fourfold increase for a severe SARS-CoV-2 infection, and a fivefold increase for being intubated.
The three studies show that mortality rates were higher early in the pandemic “when diagnosis and treatment for SARS-CoV-2 might have been delayed, resulting in higher death rate,” Boffetta et al. wrote, adding that their analysis showed only a twofold increase most likely because it was a year-long analysis.
“Future studies will be able to better analyze this association for the different subtypes of cancer. Furthermore, they will eventually be able to evaluate whether the difference among vaccinated population is reduced,” Boffetta et al. wrote.
The authors noted several limitations for the study, including the fact that many of the studies included in the analysis did not include sex, age, comorbidities, and therapy. Nor were the authors able to analyze specific cancers other than hematologic neoplasms.
The authors declared no conflicts of interest.
FROM MEDRXIV