User login
NK cell product receives orphan designation
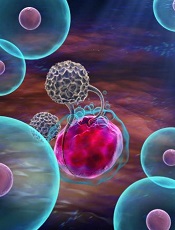
The European Commission has granted orphan designation to a natural killer (NK) cell product for the treatment of multiple myeloma.
The product, called CellProtect, is manufactured from a patient’s own blood.
It consists of NK cells that have been activated and expanded so they can recognize and attack cancer cells.
CellProtect has been studied in a phase 1/2 trial of patients with multiple myeloma.
In this trial, the NK cell product was used as a supplement to autologous stem cell transplant.
CellProtect exhibited a good safety profile and signals of effect in the trial, according to CellProtect Nordic Pharmaceuticals AB, the company developing CellProtect.
Results from the trial are expected to be published in 2018.
“The decision from the commission is based on a recommendation from the European Medicines Agency’s Committee for Orphan Medicinal Products and confirms that a future product is considered to be of significant benefit to those suffering from multiple myeloma,” said Karin Mellström, chief executive officer of CellProtect Nordic Pharmaceuticals AB.
“We can now proceed and plan for additional clinical trials in order to receive approval to market CellProtect.”
Orphan designation from the European Commission provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if a therapy receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. ![]()
The European Commission has granted orphan designation to a natural killer (NK) cell product for the treatment of multiple myeloma.
The product, called CellProtect, is manufactured from a patient’s own blood.
It consists of NK cells that have been activated and expanded so they can recognize and attack cancer cells.
CellProtect has been studied in a phase 1/2 trial of patients with multiple myeloma.
In this trial, the NK cell product was used as a supplement to autologous stem cell transplant.
CellProtect exhibited a good safety profile and signals of effect in the trial, according to CellProtect Nordic Pharmaceuticals AB, the company developing CellProtect.
Results from the trial are expected to be published in 2018.
“The decision from the commission is based on a recommendation from the European Medicines Agency’s Committee for Orphan Medicinal Products and confirms that a future product is considered to be of significant benefit to those suffering from multiple myeloma,” said Karin Mellström, chief executive officer of CellProtect Nordic Pharmaceuticals AB.
“We can now proceed and plan for additional clinical trials in order to receive approval to market CellProtect.”
Orphan designation from the European Commission provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if a therapy receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. ![]()
The European Commission has granted orphan designation to a natural killer (NK) cell product for the treatment of multiple myeloma.
The product, called CellProtect, is manufactured from a patient’s own blood.
It consists of NK cells that have been activated and expanded so they can recognize and attack cancer cells.
CellProtect has been studied in a phase 1/2 trial of patients with multiple myeloma.
In this trial, the NK cell product was used as a supplement to autologous stem cell transplant.
CellProtect exhibited a good safety profile and signals of effect in the trial, according to CellProtect Nordic Pharmaceuticals AB, the company developing CellProtect.
Results from the trial are expected to be published in 2018.
“The decision from the commission is based on a recommendation from the European Medicines Agency’s Committee for Orphan Medicinal Products and confirms that a future product is considered to be of significant benefit to those suffering from multiple myeloma,” said Karin Mellström, chief executive officer of CellProtect Nordic Pharmaceuticals AB.
“We can now proceed and plan for additional clinical trials in order to receive approval to market CellProtect.”
Orphan designation from the European Commission provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if a therapy receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. ![]()
CRB-410 update: Multiple myeloma response rates remain high with bb2121 CAR T-cell therapy
ATLANTA – A novel chimeric antigen receptor (CAR) T-cell therapy that targets B-cell maturation antigen showed promising efficacy with a manageable adverse event profile in heavily pretreated patients with relapsed/refractory multiple myeloma in the CRB-410 multicenter phase 1 dose escalation trial.
The product, known as bb2121, received breakthrough therapy designation from the Food and Drug Administration in November 2017 based on preliminary data from the ongoing trial. Those data showed that as of May 2017, the overall response rate at 1 month in 18 evaluable patients was 89%, whereas the response in those who received active dosing (150 x 106 CAR+ T cells or higher) was 100%.
Multiple myeloma currently is “essentially incurable,” and new treatments are desperately needed; B-cell maturation antigen (BCMA) – which is a member of the tumor necrosis factor superfamily that is expressed primarily by malignant myeloma cells, plasma cells, and some mature B cells – is a promising target, said Dr. Kochenderfer of the National Cancer Institute, Bethesda, Md.
The bb2121 product is a second-generation CAR construct targeting BCMA to redirect T cells to multiple myeloma cells. It was tested at doses of 50, 150, 450, and 800 x 106 CAR+ T cells in patients who first underwent chemotherapy as a conditioning regimen to enhance the activity of the CAR T cells.
A total of 24 patients were enrolled, but three had clinical deterioration and were not dosed. The remaining 21 patients had a median age of 58 years, performance scores of 0 or 1, and a median of 5 years since multiple myeloma diagnosis. A high percentage (43%) had high-risk cytogenetics. The median number of prior lines of therapy was seven, and all patients had undergone prior autologous stem cell transplant.
“Generally, this was a very well tolerated CAR T-cell product, especially in comparison to other protocols that I’ve participated in,” he said, noting that the incidence of adverse events, including dose-limiting toxicities, was the primary outcome measure of this phase of the study.
Cytokine release syndrome occurred in 71% of the 21 patients evaluable for response with a median follow-up of 35 weeks at the Oct. 2, 2017, data cutoff, but was grade 3 or greater in just 10% of those patients. Neurological toxicity occurred in 24% of patients, as well, but no cases were grade 3 or above, he said.
“The neurotoxicity was generally much milder and less prevalent than what I’ve seen in previous anti-CD19 CAR studies,” he said.
Neutropenia, thrombocytopenia, and anemia also occurred, but there were no dose-limiting toxicities observed during dose escalation.
Five deaths occurred. Three were due to disease progression and occurred in patients on the lowest dose (50 x 106 CAR+ T cells), which was deemed inactive. The other deaths occurred in patients receiving higher (active) doses; one was a result of myelodysplastic syndrome, and one from cardiac arrest, he said.
One or more serious adverse events occurred in 14 patients, and in some cases were characterized as such due to strict study protocols, Dr. Kochenderfer said.
Of note, one patient out of 12 in an ongoing dose expansion phase of the study, for which data have not yet been fully reported, experienced a delayed onset reversible grade 4 neurological toxicity associated with tumor lysis syndrome and cytokine release syndrome. The patient, who had the highest disease burden in the trial, completely recovered and has obtained a very good partial response despite low BCMA expression on the myeloma cells, Dr. Kochenderfer said.
In terms of response rates, 17 of 18 patients who received doses above 50 x 106 CAR+ T cells had overall responses, and 10 of the 18 achieved complete remission.
The median time to first response was 1 month, and the times to best response and complete response were 3.74 and 3.84 months, respectively. The rates of progression-free survival were 81% at 6 months, and 71% at 9 months, and responses deepened over time: as of May, the complete response rate was 27%, and as of October, it was 56%.
“Five of these patients so far have met the 1-year progression-free survival standard,” Dr. Kochenderfer said, adding that responses have endured for more than a year in several patients. The longest was 68 weeks at the time of the data presentation, and responses continued to improve as late as 15 months, with very good partial remission to complete remission transitions.
The median progression-free survival had not been reached in the active dose cohorts.
“So, in general, very impressive responses compared to my previous experience treating multiple myeloma,” he said.
The findings support the potential of CAR T therapy with bb2121 as a new treatment paradigm in relapsed/refractory multiple myeloma, he concluded, noting that a global pivotal trial of bb2121 (the phase 2 KarMMa trial) is now enrolling and will dose patients at between 150 and 350 x 106 CAR+ T cells. Under the breakthrough therapy designation granted for bb2121, the product will receive expedited review by the FDA.The CRB-410 trial is sponsored by bluebird bio and Celgene. Dr. Kochenderfer reported receiving research funding from bluebird bio and Kite Pharma, and having multiple patents in the CAR field.
ATLANTA – A novel chimeric antigen receptor (CAR) T-cell therapy that targets B-cell maturation antigen showed promising efficacy with a manageable adverse event profile in heavily pretreated patients with relapsed/refractory multiple myeloma in the CRB-410 multicenter phase 1 dose escalation trial.
The product, known as bb2121, received breakthrough therapy designation from the Food and Drug Administration in November 2017 based on preliminary data from the ongoing trial. Those data showed that as of May 2017, the overall response rate at 1 month in 18 evaluable patients was 89%, whereas the response in those who received active dosing (150 x 106 CAR+ T cells or higher) was 100%.
Multiple myeloma currently is “essentially incurable,” and new treatments are desperately needed; B-cell maturation antigen (BCMA) – which is a member of the tumor necrosis factor superfamily that is expressed primarily by malignant myeloma cells, plasma cells, and some mature B cells – is a promising target, said Dr. Kochenderfer of the National Cancer Institute, Bethesda, Md.
The bb2121 product is a second-generation CAR construct targeting BCMA to redirect T cells to multiple myeloma cells. It was tested at doses of 50, 150, 450, and 800 x 106 CAR+ T cells in patients who first underwent chemotherapy as a conditioning regimen to enhance the activity of the CAR T cells.
A total of 24 patients were enrolled, but three had clinical deterioration and were not dosed. The remaining 21 patients had a median age of 58 years, performance scores of 0 or 1, and a median of 5 years since multiple myeloma diagnosis. A high percentage (43%) had high-risk cytogenetics. The median number of prior lines of therapy was seven, and all patients had undergone prior autologous stem cell transplant.
“Generally, this was a very well tolerated CAR T-cell product, especially in comparison to other protocols that I’ve participated in,” he said, noting that the incidence of adverse events, including dose-limiting toxicities, was the primary outcome measure of this phase of the study.
Cytokine release syndrome occurred in 71% of the 21 patients evaluable for response with a median follow-up of 35 weeks at the Oct. 2, 2017, data cutoff, but was grade 3 or greater in just 10% of those patients. Neurological toxicity occurred in 24% of patients, as well, but no cases were grade 3 or above, he said.
“The neurotoxicity was generally much milder and less prevalent than what I’ve seen in previous anti-CD19 CAR studies,” he said.
Neutropenia, thrombocytopenia, and anemia also occurred, but there were no dose-limiting toxicities observed during dose escalation.
Five deaths occurred. Three were due to disease progression and occurred in patients on the lowest dose (50 x 106 CAR+ T cells), which was deemed inactive. The other deaths occurred in patients receiving higher (active) doses; one was a result of myelodysplastic syndrome, and one from cardiac arrest, he said.
One or more serious adverse events occurred in 14 patients, and in some cases were characterized as such due to strict study protocols, Dr. Kochenderfer said.
Of note, one patient out of 12 in an ongoing dose expansion phase of the study, for which data have not yet been fully reported, experienced a delayed onset reversible grade 4 neurological toxicity associated with tumor lysis syndrome and cytokine release syndrome. The patient, who had the highest disease burden in the trial, completely recovered and has obtained a very good partial response despite low BCMA expression on the myeloma cells, Dr. Kochenderfer said.
In terms of response rates, 17 of 18 patients who received doses above 50 x 106 CAR+ T cells had overall responses, and 10 of the 18 achieved complete remission.
The median time to first response was 1 month, and the times to best response and complete response were 3.74 and 3.84 months, respectively. The rates of progression-free survival were 81% at 6 months, and 71% at 9 months, and responses deepened over time: as of May, the complete response rate was 27%, and as of October, it was 56%.
“Five of these patients so far have met the 1-year progression-free survival standard,” Dr. Kochenderfer said, adding that responses have endured for more than a year in several patients. The longest was 68 weeks at the time of the data presentation, and responses continued to improve as late as 15 months, with very good partial remission to complete remission transitions.
The median progression-free survival had not been reached in the active dose cohorts.
“So, in general, very impressive responses compared to my previous experience treating multiple myeloma,” he said.
The findings support the potential of CAR T therapy with bb2121 as a new treatment paradigm in relapsed/refractory multiple myeloma, he concluded, noting that a global pivotal trial of bb2121 (the phase 2 KarMMa trial) is now enrolling and will dose patients at between 150 and 350 x 106 CAR+ T cells. Under the breakthrough therapy designation granted for bb2121, the product will receive expedited review by the FDA.The CRB-410 trial is sponsored by bluebird bio and Celgene. Dr. Kochenderfer reported receiving research funding from bluebird bio and Kite Pharma, and having multiple patents in the CAR field.
ATLANTA – A novel chimeric antigen receptor (CAR) T-cell therapy that targets B-cell maturation antigen showed promising efficacy with a manageable adverse event profile in heavily pretreated patients with relapsed/refractory multiple myeloma in the CRB-410 multicenter phase 1 dose escalation trial.
The product, known as bb2121, received breakthrough therapy designation from the Food and Drug Administration in November 2017 based on preliminary data from the ongoing trial. Those data showed that as of May 2017, the overall response rate at 1 month in 18 evaluable patients was 89%, whereas the response in those who received active dosing (150 x 106 CAR+ T cells or higher) was 100%.
Multiple myeloma currently is “essentially incurable,” and new treatments are desperately needed; B-cell maturation antigen (BCMA) – which is a member of the tumor necrosis factor superfamily that is expressed primarily by malignant myeloma cells, plasma cells, and some mature B cells – is a promising target, said Dr. Kochenderfer of the National Cancer Institute, Bethesda, Md.
The bb2121 product is a second-generation CAR construct targeting BCMA to redirect T cells to multiple myeloma cells. It was tested at doses of 50, 150, 450, and 800 x 106 CAR+ T cells in patients who first underwent chemotherapy as a conditioning regimen to enhance the activity of the CAR T cells.
A total of 24 patients were enrolled, but three had clinical deterioration and were not dosed. The remaining 21 patients had a median age of 58 years, performance scores of 0 or 1, and a median of 5 years since multiple myeloma diagnosis. A high percentage (43%) had high-risk cytogenetics. The median number of prior lines of therapy was seven, and all patients had undergone prior autologous stem cell transplant.
“Generally, this was a very well tolerated CAR T-cell product, especially in comparison to other protocols that I’ve participated in,” he said, noting that the incidence of adverse events, including dose-limiting toxicities, was the primary outcome measure of this phase of the study.
Cytokine release syndrome occurred in 71% of the 21 patients evaluable for response with a median follow-up of 35 weeks at the Oct. 2, 2017, data cutoff, but was grade 3 or greater in just 10% of those patients. Neurological toxicity occurred in 24% of patients, as well, but no cases were grade 3 or above, he said.
“The neurotoxicity was generally much milder and less prevalent than what I’ve seen in previous anti-CD19 CAR studies,” he said.
Neutropenia, thrombocytopenia, and anemia also occurred, but there were no dose-limiting toxicities observed during dose escalation.
Five deaths occurred. Three were due to disease progression and occurred in patients on the lowest dose (50 x 106 CAR+ T cells), which was deemed inactive. The other deaths occurred in patients receiving higher (active) doses; one was a result of myelodysplastic syndrome, and one from cardiac arrest, he said.
One or more serious adverse events occurred in 14 patients, and in some cases were characterized as such due to strict study protocols, Dr. Kochenderfer said.
Of note, one patient out of 12 in an ongoing dose expansion phase of the study, for which data have not yet been fully reported, experienced a delayed onset reversible grade 4 neurological toxicity associated with tumor lysis syndrome and cytokine release syndrome. The patient, who had the highest disease burden in the trial, completely recovered and has obtained a very good partial response despite low BCMA expression on the myeloma cells, Dr. Kochenderfer said.
In terms of response rates, 17 of 18 patients who received doses above 50 x 106 CAR+ T cells had overall responses, and 10 of the 18 achieved complete remission.
The median time to first response was 1 month, and the times to best response and complete response were 3.74 and 3.84 months, respectively. The rates of progression-free survival were 81% at 6 months, and 71% at 9 months, and responses deepened over time: as of May, the complete response rate was 27%, and as of October, it was 56%.
“Five of these patients so far have met the 1-year progression-free survival standard,” Dr. Kochenderfer said, adding that responses have endured for more than a year in several patients. The longest was 68 weeks at the time of the data presentation, and responses continued to improve as late as 15 months, with very good partial remission to complete remission transitions.
The median progression-free survival had not been reached in the active dose cohorts.
“So, in general, very impressive responses compared to my previous experience treating multiple myeloma,” he said.
The findings support the potential of CAR T therapy with bb2121 as a new treatment paradigm in relapsed/refractory multiple myeloma, he concluded, noting that a global pivotal trial of bb2121 (the phase 2 KarMMa trial) is now enrolling and will dose patients at between 150 and 350 x 106 CAR+ T cells. Under the breakthrough therapy designation granted for bb2121, the product will receive expedited review by the FDA.The CRB-410 trial is sponsored by bluebird bio and Celgene. Dr. Kochenderfer reported receiving research funding from bluebird bio and Kite Pharma, and having multiple patents in the CAR field.
REPORTING FROM ASH 2017
Key clinical point:
Major finding: The overall response rate was 94%.
Study details: An update from the phase 1 CRB-410 dose trial of 21 patients.
Disclosures: The CRB-410 trial is sponsored by bluebird bio and Celgene. Dr. Kochenderfer reported receiving research funding from bluebird bio and Kite Pharma, and having multiple patents in the CAR field.
Source: Berdeja J et al. ASH 2017 Abstract 740.
CRP drives bone destruction in myeloma, team says
New research suggests that C-reactive protein (CRP) drives multiple myeloma (MM) to destroy bone.
Researchers found that CRP accelerated the onset of bone destruction and made bone damage more severe in mouse models of MM.
The team also observed an association between elevated serum CRP levels and greater degree of bone damage in newly diagnosed MM patients.
The researchers therefore believe that CRP might be targeted to prevent or treat MM-associated bone disease.
Qing Yi, MD, PhD, of the Lerner Research Institute at the Cleveland Clinic in Ohio, and his colleagues conducted this research and reported the results in Science Translational Medicine.
The researchers noted that high levels of circulating CRP have been associated with poor prognosis in many cancers, including MM.
In a previous study, the team found that CRP enhanced MM cell proliferation under stressed conditions and protected MM cells from chemotherapy-induced apoptosis.
Now, the researchers have found that CRP activates MM cells to promote osteoclastogenesis and bone destruction.
In experiments with mouse models, the team found that CRP promoted MM-cell-mediated lytic bone disease. The researchers said CRP enhanced osteoclast differentiation and bone resorption activity.
In vitro experiments showed that CRP stimulates MM cells to produce osteoclast activators such as RANKL, MCP-1, and MIP-1a.
Further investigation revealed that CRP binds to CD32 on MM cells. This activates a pathway mediated by the kinase p38 MAPK and the transcription factor Twist, which increases MM cells’ production of osteolytic cytokines.
Finally, the researchers analyzed samples from newly diagnosed MM patients.
The team found that serum CRP levels “significantly and positively” correlated with the number of bone lesions patients had. And CRP was abundant in lesion biopsies from individuals with severe skeletal disease. ![]()
New research suggests that C-reactive protein (CRP) drives multiple myeloma (MM) to destroy bone.
Researchers found that CRP accelerated the onset of bone destruction and made bone damage more severe in mouse models of MM.
The team also observed an association between elevated serum CRP levels and greater degree of bone damage in newly diagnosed MM patients.
The researchers therefore believe that CRP might be targeted to prevent or treat MM-associated bone disease.
Qing Yi, MD, PhD, of the Lerner Research Institute at the Cleveland Clinic in Ohio, and his colleagues conducted this research and reported the results in Science Translational Medicine.
The researchers noted that high levels of circulating CRP have been associated with poor prognosis in many cancers, including MM.
In a previous study, the team found that CRP enhanced MM cell proliferation under stressed conditions and protected MM cells from chemotherapy-induced apoptosis.
Now, the researchers have found that CRP activates MM cells to promote osteoclastogenesis and bone destruction.
In experiments with mouse models, the team found that CRP promoted MM-cell-mediated lytic bone disease. The researchers said CRP enhanced osteoclast differentiation and bone resorption activity.
In vitro experiments showed that CRP stimulates MM cells to produce osteoclast activators such as RANKL, MCP-1, and MIP-1a.
Further investigation revealed that CRP binds to CD32 on MM cells. This activates a pathway mediated by the kinase p38 MAPK and the transcription factor Twist, which increases MM cells’ production of osteolytic cytokines.
Finally, the researchers analyzed samples from newly diagnosed MM patients.
The team found that serum CRP levels “significantly and positively” correlated with the number of bone lesions patients had. And CRP was abundant in lesion biopsies from individuals with severe skeletal disease. ![]()
New research suggests that C-reactive protein (CRP) drives multiple myeloma (MM) to destroy bone.
Researchers found that CRP accelerated the onset of bone destruction and made bone damage more severe in mouse models of MM.
The team also observed an association between elevated serum CRP levels and greater degree of bone damage in newly diagnosed MM patients.
The researchers therefore believe that CRP might be targeted to prevent or treat MM-associated bone disease.
Qing Yi, MD, PhD, of the Lerner Research Institute at the Cleveland Clinic in Ohio, and his colleagues conducted this research and reported the results in Science Translational Medicine.
The researchers noted that high levels of circulating CRP have been associated with poor prognosis in many cancers, including MM.
In a previous study, the team found that CRP enhanced MM cell proliferation under stressed conditions and protected MM cells from chemotherapy-induced apoptosis.
Now, the researchers have found that CRP activates MM cells to promote osteoclastogenesis and bone destruction.
In experiments with mouse models, the team found that CRP promoted MM-cell-mediated lytic bone disease. The researchers said CRP enhanced osteoclast differentiation and bone resorption activity.
In vitro experiments showed that CRP stimulates MM cells to produce osteoclast activators such as RANKL, MCP-1, and MIP-1a.
Further investigation revealed that CRP binds to CD32 on MM cells. This activates a pathway mediated by the kinase p38 MAPK and the transcription factor Twist, which increases MM cells’ production of osteolytic cytokines.
Finally, the researchers analyzed samples from newly diagnosed MM patients.
The team found that serum CRP levels “significantly and positively” correlated with the number of bone lesions patients had. And CRP was abundant in lesion biopsies from individuals with severe skeletal disease. ![]()
Combo should be standard in MM, doc says
ATLANTA—Study results “strongly support” a new standard of care for transplant-ineligible patients with newly diagnosed multiple myeloma (MM), according to a speaker at the 2017 ASH Annual Meeting.
The study, ALCYONE, suggests treatment with bortezomib, melphalan, and prednisone (VMP) can be improved by the addition of daratumumab (D).
D-VMP produced deeper responses and prolonged progression-free survival (PFS) when compared to VMP.
“In this first phase 3, randomized study with a monoclonal antibody in newly diagnosed multiple myeloma, daratumumab reduced the risk of progression or death by 50%,” said Maria-Victoria Mateos, MD, PhD, of University Hospital of Salamanca in Spain.
“No new safety signals were observed [with D-VMP], except for higher infectious events that resolved. I would say the results of this study strongly support daratumumab in combination with VMP as a standard of care in transplant-ineligible, newly diagnosed multiple myeloma.”
Dr Mateos presented results from ALCYONE as a late-breaking abstract (LBA-4) at the ASH Annual Meeting. The study was simultaneously published in NEJM. The research was supported by Janssen Research and Development.
Patients and treatment
ALCYONE enrolled 706 patients with newly diagnosed MM who were not eligible for high-dose chemotherapy with autologous stem cell transplant.
Patients were randomized to receive VMP or D-VMP. They were stratified by International Staging System (I, II, III), region (Europe vs other), and age (<75 vs ≥75 years).
All patients received up to 9 cycles of VMP:
- Bortezomib at 1.3 mg/m2 twice weekly on weeks 1, 2, 4, and 5 of cycle 1 and once weekly on weeks 1, 2, 4, and 5 of cycles 2 through 9
- Melphalan at 9 mg/m2 once daily on days 1 to 4 of each cycle
- Prednisone at 60 mg/m2 once daily on days 1 to 4 of each cycle.
Patients in the daratumumab arm received the drug at 16 mg/kg once-weekly for the first cycle, every 3 weeks for cycles 2 to 9, and every 4 weeks thereafter, until disease progression. These patients also received dexamethasone (to manage infusion reactions) at 20 mg on the same schedule.
Baseline characteristics were similar between the VMP (n=356) and D-VMP (n=350) arms. The median age was 71 in both arms (range, 50-91 in the VMP arm and 40-93 in the D-VMP arm). Males made up 47% of the VMP arm and 46% of the D-VMP arm.
Forty-nine percent of patients in the VMP arm and 52% in the D-VMP arm had an ECOG performance status of 1. Twenty-eight percent and 22%, respectively, had a status of 0.
The median follow-up was 16.5 months (range, 0.1-28.1). At the clinical cutoff date (June 12, 2017), 5% of patients in the VMP arm were still on study treatment, as were 71% of patients in the D-VMP arm.
Response and survival
“I would like to note that the benefit of the addition of daratumumab was observed since the beginning of the treatment,” Dr Mateos said.
The overall response rate was 74% in the VMP arm and 91% in the D-VMP arm (P<0.0001). The median duration of response was 21.3 months in the VMP arm and was not reached in the D-VMP arm.
The rate of complete response was 24% in the VMP arm and 43% in the D-VMP arm (P<0.0001). Six percent of patients in the VMP arm and 22% in the D-VMP arm were negative for minimal residual disease (P<0.0001).
The hazard ratio for disease progression or death in the D-VMP arm versus the VMP arm was 0.50 (P<0.0001).
The median PFS was 18.1 months in the VMP arm and was not reached in the D-VMP arm. The 12-month PFS was 76% and 87%, respectively. And the 18-month PFS was 50% and 72%, respectively.
D-VMP prolonged PFS regardless of patient sex, age, cytogenetic risk, ECOG performance status, baseline renal function, and other factors.
The median overall survival was not reached in either treatment arm. There were 48 deaths in the VMP arm and 45 in the D-VMP arm.
Adverse events
The most common treatment-emergent adverse events (TEAEs; in the D-VMP and VMP arms, respectively) were neutropenia (50% and 53%), thrombocytopenia (49% and 54%), anemia (28% and 38%), peripheral sensory neuropathy (28% and 34%), upper respiratory tract infection (26% and 14%), diarrhea (24% and 25%), pyrexia (23% and 21%), and nausea (21% and 22%).
The most common grade 3/4 TEAEs (in the D-VMP and VMP arms, respectively) were neutropenia (40% and 39%), thrombocytopenia (34% and 38%), and anemia (16% and 20%).
There were 6 deaths due to TEAEs in the D-VMP arm and 5 such deaths in the VMP arm.
The rate of grade 3/4 infections was higher in the D-VMP arm than the VMP arm—23% and 15%, respectively. The most common of these was pneumonia, with rates of 11% and 4%, respectively.
Infections resolved in 88% of cases in the D-VMP arm and 87% of cases in the VMP arm. Rates of treatment discontinuation due to infection were 0.9% and 1.4%, respectively. One patient in each group stopped treatment due to pneumonia.
Twenty-eight percent of patients in the D-VMP arm had infusion-related reactions (15% grade 3 and 2% grade 4). Most of these reactions occurred during the first infusion. Five patients (1.4%) discontinued daratumumab due to infusion-related reactions. ![]()
ATLANTA—Study results “strongly support” a new standard of care for transplant-ineligible patients with newly diagnosed multiple myeloma (MM), according to a speaker at the 2017 ASH Annual Meeting.
The study, ALCYONE, suggests treatment with bortezomib, melphalan, and prednisone (VMP) can be improved by the addition of daratumumab (D).
D-VMP produced deeper responses and prolonged progression-free survival (PFS) when compared to VMP.
“In this first phase 3, randomized study with a monoclonal antibody in newly diagnosed multiple myeloma, daratumumab reduced the risk of progression or death by 50%,” said Maria-Victoria Mateos, MD, PhD, of University Hospital of Salamanca in Spain.
“No new safety signals were observed [with D-VMP], except for higher infectious events that resolved. I would say the results of this study strongly support daratumumab in combination with VMP as a standard of care in transplant-ineligible, newly diagnosed multiple myeloma.”
Dr Mateos presented results from ALCYONE as a late-breaking abstract (LBA-4) at the ASH Annual Meeting. The study was simultaneously published in NEJM. The research was supported by Janssen Research and Development.
Patients and treatment
ALCYONE enrolled 706 patients with newly diagnosed MM who were not eligible for high-dose chemotherapy with autologous stem cell transplant.
Patients were randomized to receive VMP or D-VMP. They were stratified by International Staging System (I, II, III), region (Europe vs other), and age (<75 vs ≥75 years).
All patients received up to 9 cycles of VMP:
- Bortezomib at 1.3 mg/m2 twice weekly on weeks 1, 2, 4, and 5 of cycle 1 and once weekly on weeks 1, 2, 4, and 5 of cycles 2 through 9
- Melphalan at 9 mg/m2 once daily on days 1 to 4 of each cycle
- Prednisone at 60 mg/m2 once daily on days 1 to 4 of each cycle.
Patients in the daratumumab arm received the drug at 16 mg/kg once-weekly for the first cycle, every 3 weeks for cycles 2 to 9, and every 4 weeks thereafter, until disease progression. These patients also received dexamethasone (to manage infusion reactions) at 20 mg on the same schedule.
Baseline characteristics were similar between the VMP (n=356) and D-VMP (n=350) arms. The median age was 71 in both arms (range, 50-91 in the VMP arm and 40-93 in the D-VMP arm). Males made up 47% of the VMP arm and 46% of the D-VMP arm.
Forty-nine percent of patients in the VMP arm and 52% in the D-VMP arm had an ECOG performance status of 1. Twenty-eight percent and 22%, respectively, had a status of 0.
The median follow-up was 16.5 months (range, 0.1-28.1). At the clinical cutoff date (June 12, 2017), 5% of patients in the VMP arm were still on study treatment, as were 71% of patients in the D-VMP arm.
Response and survival
“I would like to note that the benefit of the addition of daratumumab was observed since the beginning of the treatment,” Dr Mateos said.
The overall response rate was 74% in the VMP arm and 91% in the D-VMP arm (P<0.0001). The median duration of response was 21.3 months in the VMP arm and was not reached in the D-VMP arm.
The rate of complete response was 24% in the VMP arm and 43% in the D-VMP arm (P<0.0001). Six percent of patients in the VMP arm and 22% in the D-VMP arm were negative for minimal residual disease (P<0.0001).
The hazard ratio for disease progression or death in the D-VMP arm versus the VMP arm was 0.50 (P<0.0001).
The median PFS was 18.1 months in the VMP arm and was not reached in the D-VMP arm. The 12-month PFS was 76% and 87%, respectively. And the 18-month PFS was 50% and 72%, respectively.
D-VMP prolonged PFS regardless of patient sex, age, cytogenetic risk, ECOG performance status, baseline renal function, and other factors.
The median overall survival was not reached in either treatment arm. There were 48 deaths in the VMP arm and 45 in the D-VMP arm.
Adverse events
The most common treatment-emergent adverse events (TEAEs; in the D-VMP and VMP arms, respectively) were neutropenia (50% and 53%), thrombocytopenia (49% and 54%), anemia (28% and 38%), peripheral sensory neuropathy (28% and 34%), upper respiratory tract infection (26% and 14%), diarrhea (24% and 25%), pyrexia (23% and 21%), and nausea (21% and 22%).
The most common grade 3/4 TEAEs (in the D-VMP and VMP arms, respectively) were neutropenia (40% and 39%), thrombocytopenia (34% and 38%), and anemia (16% and 20%).
There were 6 deaths due to TEAEs in the D-VMP arm and 5 such deaths in the VMP arm.
The rate of grade 3/4 infections was higher in the D-VMP arm than the VMP arm—23% and 15%, respectively. The most common of these was pneumonia, with rates of 11% and 4%, respectively.
Infections resolved in 88% of cases in the D-VMP arm and 87% of cases in the VMP arm. Rates of treatment discontinuation due to infection were 0.9% and 1.4%, respectively. One patient in each group stopped treatment due to pneumonia.
Twenty-eight percent of patients in the D-VMP arm had infusion-related reactions (15% grade 3 and 2% grade 4). Most of these reactions occurred during the first infusion. Five patients (1.4%) discontinued daratumumab due to infusion-related reactions. ![]()
ATLANTA—Study results “strongly support” a new standard of care for transplant-ineligible patients with newly diagnosed multiple myeloma (MM), according to a speaker at the 2017 ASH Annual Meeting.
The study, ALCYONE, suggests treatment with bortezomib, melphalan, and prednisone (VMP) can be improved by the addition of daratumumab (D).
D-VMP produced deeper responses and prolonged progression-free survival (PFS) when compared to VMP.
“In this first phase 3, randomized study with a monoclonal antibody in newly diagnosed multiple myeloma, daratumumab reduced the risk of progression or death by 50%,” said Maria-Victoria Mateos, MD, PhD, of University Hospital of Salamanca in Spain.
“No new safety signals were observed [with D-VMP], except for higher infectious events that resolved. I would say the results of this study strongly support daratumumab in combination with VMP as a standard of care in transplant-ineligible, newly diagnosed multiple myeloma.”
Dr Mateos presented results from ALCYONE as a late-breaking abstract (LBA-4) at the ASH Annual Meeting. The study was simultaneously published in NEJM. The research was supported by Janssen Research and Development.
Patients and treatment
ALCYONE enrolled 706 patients with newly diagnosed MM who were not eligible for high-dose chemotherapy with autologous stem cell transplant.
Patients were randomized to receive VMP or D-VMP. They were stratified by International Staging System (I, II, III), region (Europe vs other), and age (<75 vs ≥75 years).
All patients received up to 9 cycles of VMP:
- Bortezomib at 1.3 mg/m2 twice weekly on weeks 1, 2, 4, and 5 of cycle 1 and once weekly on weeks 1, 2, 4, and 5 of cycles 2 through 9
- Melphalan at 9 mg/m2 once daily on days 1 to 4 of each cycle
- Prednisone at 60 mg/m2 once daily on days 1 to 4 of each cycle.
Patients in the daratumumab arm received the drug at 16 mg/kg once-weekly for the first cycle, every 3 weeks for cycles 2 to 9, and every 4 weeks thereafter, until disease progression. These patients also received dexamethasone (to manage infusion reactions) at 20 mg on the same schedule.
Baseline characteristics were similar between the VMP (n=356) and D-VMP (n=350) arms. The median age was 71 in both arms (range, 50-91 in the VMP arm and 40-93 in the D-VMP arm). Males made up 47% of the VMP arm and 46% of the D-VMP arm.
Forty-nine percent of patients in the VMP arm and 52% in the D-VMP arm had an ECOG performance status of 1. Twenty-eight percent and 22%, respectively, had a status of 0.
The median follow-up was 16.5 months (range, 0.1-28.1). At the clinical cutoff date (June 12, 2017), 5% of patients in the VMP arm were still on study treatment, as were 71% of patients in the D-VMP arm.
Response and survival
“I would like to note that the benefit of the addition of daratumumab was observed since the beginning of the treatment,” Dr Mateos said.
The overall response rate was 74% in the VMP arm and 91% in the D-VMP arm (P<0.0001). The median duration of response was 21.3 months in the VMP arm and was not reached in the D-VMP arm.
The rate of complete response was 24% in the VMP arm and 43% in the D-VMP arm (P<0.0001). Six percent of patients in the VMP arm and 22% in the D-VMP arm were negative for minimal residual disease (P<0.0001).
The hazard ratio for disease progression or death in the D-VMP arm versus the VMP arm was 0.50 (P<0.0001).
The median PFS was 18.1 months in the VMP arm and was not reached in the D-VMP arm. The 12-month PFS was 76% and 87%, respectively. And the 18-month PFS was 50% and 72%, respectively.
D-VMP prolonged PFS regardless of patient sex, age, cytogenetic risk, ECOG performance status, baseline renal function, and other factors.
The median overall survival was not reached in either treatment arm. There were 48 deaths in the VMP arm and 45 in the D-VMP arm.
Adverse events
The most common treatment-emergent adverse events (TEAEs; in the D-VMP and VMP arms, respectively) were neutropenia (50% and 53%), thrombocytopenia (49% and 54%), anemia (28% and 38%), peripheral sensory neuropathy (28% and 34%), upper respiratory tract infection (26% and 14%), diarrhea (24% and 25%), pyrexia (23% and 21%), and nausea (21% and 22%).
The most common grade 3/4 TEAEs (in the D-VMP and VMP arms, respectively) were neutropenia (40% and 39%), thrombocytopenia (34% and 38%), and anemia (16% and 20%).
There were 6 deaths due to TEAEs in the D-VMP arm and 5 such deaths in the VMP arm.
The rate of grade 3/4 infections was higher in the D-VMP arm than the VMP arm—23% and 15%, respectively. The most common of these was pneumonia, with rates of 11% and 4%, respectively.
Infections resolved in 88% of cases in the D-VMP arm and 87% of cases in the VMP arm. Rates of treatment discontinuation due to infection were 0.9% and 1.4%, respectively. One patient in each group stopped treatment due to pneumonia.
Twenty-eight percent of patients in the D-VMP arm had infusion-related reactions (15% grade 3 and 2% grade 4). Most of these reactions occurred during the first infusion. Five patients (1.4%) discontinued daratumumab due to infusion-related reactions. ![]()
VIDEO: Daratumumab gives kick to standard first-line myeloma therapy
ATLANTA – The VMP regimen, consisting of bortezomib, melphalan, and prednisone, is a standard of care in Europe for frontline therapy for patients with multiple myeloma who, for reasons of age or infirmity, are not good candidates for autologous stem cell transplant.
In this video interview at the annual meeting of the American Society of Hematology, Jesus San-Miguel, MD, of the Clinical University of Navarra in Pamplona, Spain, discusses the results of the phase 3 international ALCYONE trial, comparing VMP with the same regimen plus the addition of the anti-CD38 monoclonal antibody daratumumab (Darzalex).
Adding daratumumab to VMP regimen as first-line therapy for 706 patients with multiple myeloma cut in half the risk of disease progression or death and substantially improved the rate of minimal residual disease negativity, Dr. San-Miguel reported. There were no new safety signals from adding the monoclonal antibody to VMP.
The ALCYONE study was supported by Janssen Research & Development. Dr. San-Miguel reported serving as an adviser to the company and several others.
ATLANTA – The VMP regimen, consisting of bortezomib, melphalan, and prednisone, is a standard of care in Europe for frontline therapy for patients with multiple myeloma who, for reasons of age or infirmity, are not good candidates for autologous stem cell transplant.
In this video interview at the annual meeting of the American Society of Hematology, Jesus San-Miguel, MD, of the Clinical University of Navarra in Pamplona, Spain, discusses the results of the phase 3 international ALCYONE trial, comparing VMP with the same regimen plus the addition of the anti-CD38 monoclonal antibody daratumumab (Darzalex).
Adding daratumumab to VMP regimen as first-line therapy for 706 patients with multiple myeloma cut in half the risk of disease progression or death and substantially improved the rate of minimal residual disease negativity, Dr. San-Miguel reported. There were no new safety signals from adding the monoclonal antibody to VMP.
The ALCYONE study was supported by Janssen Research & Development. Dr. San-Miguel reported serving as an adviser to the company and several others.
ATLANTA – The VMP regimen, consisting of bortezomib, melphalan, and prednisone, is a standard of care in Europe for frontline therapy for patients with multiple myeloma who, for reasons of age or infirmity, are not good candidates for autologous stem cell transplant.
In this video interview at the annual meeting of the American Society of Hematology, Jesus San-Miguel, MD, of the Clinical University of Navarra in Pamplona, Spain, discusses the results of the phase 3 international ALCYONE trial, comparing VMP with the same regimen plus the addition of the anti-CD38 monoclonal antibody daratumumab (Darzalex).
Adding daratumumab to VMP regimen as first-line therapy for 706 patients with multiple myeloma cut in half the risk of disease progression or death and substantially improved the rate of minimal residual disease negativity, Dr. San-Miguel reported. There were no new safety signals from adding the monoclonal antibody to VMP.
The ALCYONE study was supported by Janssen Research & Development. Dr. San-Miguel reported serving as an adviser to the company and several others.
REPORTING FROM ASH 2017
Daratumumab plus VMP boosts PFS, MRD-negativity in de novo myeloma
ATLANTA – Adding the anti-CD38 monoclonal antibody daratumumab (Darzalex) to the standard VMP regimen as first-line therapy for patients with multiple myeloma cut in half the risk of disease progression or death and substantially improved the rate of minimal residual disease (MRD) negativity, investigators in the ALCYONE trial reported.
This difference translated into a hazard ratio for progression or death with D-VMP of 0.50 (P less than .0001), said Jesus San-Miguel, MD, from the Clinical University of Navarra in Pamplona, Spain.
“This result clearly indicated for the first time that, in a phase 3 randomized study conducted with a monoclonal antibody in newly diagnosed myeloma patients, the addition of daratumumab to the standard of care reduced the risk of progression or death by 50%, and this is associated with significantly deeper responses, including a threefold higher MRD negativity rate,” he said at a media briefing prior to presentation of the data in a late-breaking abstract session at the annual meeting of the American Society of Hematology.
The VMP regimen is used more commonly in Europe than the United States as first-line therapy for patients with previously untreated multiple myeloma who are aged 65 years or older or are otherwise not suitable candidates for autologous stem cell transplants (ASCT).
In the ALCYONE trial, patients who met this definition were enrolled and stratified by International Staging System scores, region, and age (younger or older than 75 years) and were then randomized to 6-week cycles of VMP, with or without daratumumab. In the experimental arm, daratumumab was given at 16 mg/kg IV weekly for cycle 1, every 3 weeks for cycles 2-9, and every 4 weeks for cycles 10 and beyond (post VMP-treatment phase) until disease progression.
As noted before, the primary endpoint of investigator-assessed PFS significantly favored the addition of daratumumab. Dr. San-Miguel attributed this difference to the overall response rates, which were 91%, including 43% complete responses with daratumumab, vs. 74% ORR with 24% CR, without the monoclonal antibody.
The rate of MRD negativity, measured with a threshold sensitivity of 10–5, was also significantly higher with daratumumab at 22% vs. 6% (P less than .0001).
Among all patients who achieved MRD negativity, regardless of treatment, there was a lower risk of progression or death, Dr. San-Miguel said.
The rate of treatment discontinuation because of infection was higher with VMP (1.4%) than with D-VMP (0.9%). One patient in each trial arm discontinued therapy because of pneumonia. Rates of any serious adverse event were higher with D-VMP (42%, compared with 33%). Infusion-related reactions occurred in 27.7% of patients assigned to daratumumab.
Rates of grade 3 or 4 hematologic and nonhematologic toxicities were generally similar between the treatment arms, and there were no new safety signals with daratumumab, Dr. San-Miguel said.
The ALCYONE trial is one of several ongoing studies looking at the addition of daratumumab to standard therapies in the frontline, including the phase 3 MAIA trial (with daratumumab added to lenalidomide and dexamethasone), the phase 3 CASSIOPEIA trial (with the antibody added to bortezomib, thalidomide, and dexamethasone), the phase 2 GRIFFIN trial (with daratumumab plus lenalidomide, bortezomib, and dexamethasone), and the phase 2 LYRA trial (with the antibody added to cyclophosphamide, bortezomib, and dexamethasone).
The ALCYONE study was supported by Janssen Research & Development. Dr. San-Miguel reported serving as an adviser to the company and several others. Multiple coauthors disclosed similar relationships.
SOURCE: Mateos MV et al. ASH Abstract LBA-4.
ATLANTA – Adding the anti-CD38 monoclonal antibody daratumumab (Darzalex) to the standard VMP regimen as first-line therapy for patients with multiple myeloma cut in half the risk of disease progression or death and substantially improved the rate of minimal residual disease (MRD) negativity, investigators in the ALCYONE trial reported.
This difference translated into a hazard ratio for progression or death with D-VMP of 0.50 (P less than .0001), said Jesus San-Miguel, MD, from the Clinical University of Navarra in Pamplona, Spain.
“This result clearly indicated for the first time that, in a phase 3 randomized study conducted with a monoclonal antibody in newly diagnosed myeloma patients, the addition of daratumumab to the standard of care reduced the risk of progression or death by 50%, and this is associated with significantly deeper responses, including a threefold higher MRD negativity rate,” he said at a media briefing prior to presentation of the data in a late-breaking abstract session at the annual meeting of the American Society of Hematology.
The VMP regimen is used more commonly in Europe than the United States as first-line therapy for patients with previously untreated multiple myeloma who are aged 65 years or older or are otherwise not suitable candidates for autologous stem cell transplants (ASCT).
In the ALCYONE trial, patients who met this definition were enrolled and stratified by International Staging System scores, region, and age (younger or older than 75 years) and were then randomized to 6-week cycles of VMP, with or without daratumumab. In the experimental arm, daratumumab was given at 16 mg/kg IV weekly for cycle 1, every 3 weeks for cycles 2-9, and every 4 weeks for cycles 10 and beyond (post VMP-treatment phase) until disease progression.
As noted before, the primary endpoint of investigator-assessed PFS significantly favored the addition of daratumumab. Dr. San-Miguel attributed this difference to the overall response rates, which were 91%, including 43% complete responses with daratumumab, vs. 74% ORR with 24% CR, without the monoclonal antibody.
The rate of MRD negativity, measured with a threshold sensitivity of 10–5, was also significantly higher with daratumumab at 22% vs. 6% (P less than .0001).
Among all patients who achieved MRD negativity, regardless of treatment, there was a lower risk of progression or death, Dr. San-Miguel said.
The rate of treatment discontinuation because of infection was higher with VMP (1.4%) than with D-VMP (0.9%). One patient in each trial arm discontinued therapy because of pneumonia. Rates of any serious adverse event were higher with D-VMP (42%, compared with 33%). Infusion-related reactions occurred in 27.7% of patients assigned to daratumumab.
Rates of grade 3 or 4 hematologic and nonhematologic toxicities were generally similar between the treatment arms, and there were no new safety signals with daratumumab, Dr. San-Miguel said.
The ALCYONE trial is one of several ongoing studies looking at the addition of daratumumab to standard therapies in the frontline, including the phase 3 MAIA trial (with daratumumab added to lenalidomide and dexamethasone), the phase 3 CASSIOPEIA trial (with the antibody added to bortezomib, thalidomide, and dexamethasone), the phase 2 GRIFFIN trial (with daratumumab plus lenalidomide, bortezomib, and dexamethasone), and the phase 2 LYRA trial (with the antibody added to cyclophosphamide, bortezomib, and dexamethasone).
The ALCYONE study was supported by Janssen Research & Development. Dr. San-Miguel reported serving as an adviser to the company and several others. Multiple coauthors disclosed similar relationships.
SOURCE: Mateos MV et al. ASH Abstract LBA-4.
ATLANTA – Adding the anti-CD38 monoclonal antibody daratumumab (Darzalex) to the standard VMP regimen as first-line therapy for patients with multiple myeloma cut in half the risk of disease progression or death and substantially improved the rate of minimal residual disease (MRD) negativity, investigators in the ALCYONE trial reported.
This difference translated into a hazard ratio for progression or death with D-VMP of 0.50 (P less than .0001), said Jesus San-Miguel, MD, from the Clinical University of Navarra in Pamplona, Spain.
“This result clearly indicated for the first time that, in a phase 3 randomized study conducted with a monoclonal antibody in newly diagnosed myeloma patients, the addition of daratumumab to the standard of care reduced the risk of progression or death by 50%, and this is associated with significantly deeper responses, including a threefold higher MRD negativity rate,” he said at a media briefing prior to presentation of the data in a late-breaking abstract session at the annual meeting of the American Society of Hematology.
The VMP regimen is used more commonly in Europe than the United States as first-line therapy for patients with previously untreated multiple myeloma who are aged 65 years or older or are otherwise not suitable candidates for autologous stem cell transplants (ASCT).
In the ALCYONE trial, patients who met this definition were enrolled and stratified by International Staging System scores, region, and age (younger or older than 75 years) and were then randomized to 6-week cycles of VMP, with or without daratumumab. In the experimental arm, daratumumab was given at 16 mg/kg IV weekly for cycle 1, every 3 weeks for cycles 2-9, and every 4 weeks for cycles 10 and beyond (post VMP-treatment phase) until disease progression.
As noted before, the primary endpoint of investigator-assessed PFS significantly favored the addition of daratumumab. Dr. San-Miguel attributed this difference to the overall response rates, which were 91%, including 43% complete responses with daratumumab, vs. 74% ORR with 24% CR, without the monoclonal antibody.
The rate of MRD negativity, measured with a threshold sensitivity of 10–5, was also significantly higher with daratumumab at 22% vs. 6% (P less than .0001).
Among all patients who achieved MRD negativity, regardless of treatment, there was a lower risk of progression or death, Dr. San-Miguel said.
The rate of treatment discontinuation because of infection was higher with VMP (1.4%) than with D-VMP (0.9%). One patient in each trial arm discontinued therapy because of pneumonia. Rates of any serious adverse event were higher with D-VMP (42%, compared with 33%). Infusion-related reactions occurred in 27.7% of patients assigned to daratumumab.
Rates of grade 3 or 4 hematologic and nonhematologic toxicities were generally similar between the treatment arms, and there were no new safety signals with daratumumab, Dr. San-Miguel said.
The ALCYONE trial is one of several ongoing studies looking at the addition of daratumumab to standard therapies in the frontline, including the phase 3 MAIA trial (with daratumumab added to lenalidomide and dexamethasone), the phase 3 CASSIOPEIA trial (with the antibody added to bortezomib, thalidomide, and dexamethasone), the phase 2 GRIFFIN trial (with daratumumab plus lenalidomide, bortezomib, and dexamethasone), and the phase 2 LYRA trial (with the antibody added to cyclophosphamide, bortezomib, and dexamethasone).
The ALCYONE study was supported by Janssen Research & Development. Dr. San-Miguel reported serving as an adviser to the company and several others. Multiple coauthors disclosed similar relationships.
SOURCE: Mateos MV et al. ASH Abstract LBA-4.
REPORTING FROM ASH 2017
Key clinical point:
Major finding: The hazard ratio for progression or death with daratumumab plus VMP was 0.50 (P less than .0001).
Study details: Randomized phase 3 trial in 706 patients with multiple myeloma who were ineligible for transplant.
Disclosures: The ALCYONE study was supported by Janssen Research & Development. Dr. San-Miguel reported serving as an adviser to the company and several others. Multiple coauthors disclosed similar relationships.
Source: Mateos MV et al. ASH Abstract LBA-4.
Activating the Immune System to Treat Multiple Myeloma
Sagar Lonial, MD
Chief Medical Officer, Winship Cancer Institute of Emory University
Chair, Dept. of Hematology and Medical Oncology, Emory School of Medicine
Faculty/Faculty Disclosure
Dr. Lonial reports that he is a compensated consultant for Bristol-Myers Squibb; Celgene Corporation; Janssen Pharmaceuticals, Inc.; Merck & Co., Inc.; Millennium Pharmaceuticals, Inc.; Novartis Pharmaceuticals Corporation; and Onyx Pharmaceuticals, Inc.
Sagar Lonial, MD
Chief Medical Officer, Winship Cancer Institute of Emory University
Chair, Dept. of Hematology and Medical Oncology, Emory School of Medicine
Faculty/Faculty Disclosure
Dr. Lonial reports that he is a compensated consultant for Bristol-Myers Squibb; Celgene Corporation; Janssen Pharmaceuticals, Inc.; Merck & Co., Inc.; Millennium Pharmaceuticals, Inc.; Novartis Pharmaceuticals Corporation; and Onyx Pharmaceuticals, Inc.
Sagar Lonial, MD
Chief Medical Officer, Winship Cancer Institute of Emory University
Chair, Dept. of Hematology and Medical Oncology, Emory School of Medicine
Faculty/Faculty Disclosure
Dr. Lonial reports that he is a compensated consultant for Bristol-Myers Squibb; Celgene Corporation; Janssen Pharmaceuticals, Inc.; Merck & Co., Inc.; Millennium Pharmaceuticals, Inc.; Novartis Pharmaceuticals Corporation; and Onyx Pharmaceuticals, Inc.
FDA lifts partial hold on nivolumab trials
The US Food and Drug Administration (FDA) has lifted the partial clinical hold placed on 2 trials of the PD-1 immune checkpoint inhibitor nivolumab (Opdivo).
In these trials, CheckMate-039 (CA209 -039) and CA204142, researchers are investigating nivolumab-based combinations in patients with relapsed or refractory multiple myeloma (MM).
The partial clinical hold on these trials was a result of risks identified in studies involving another anti-PD-1 agent, pembrolizumab.
Data from the pembrolizumab trials suggested that risks outweigh benefits when PD-1/PD-L1 treatment is given to MM patients in combination with dexamethasone and pomalidomide or lenalidomide.
In addition, there could be an unfavorable risk-benefit ratio for MM patients receiving PD-1/PD-L1 treatments alone or in other combinations.
Therefore, the FDA placed a partial hold on the following nivolumab trials:
- CheckMate-602: A randomized, phase 3 trial of combinations of nivolumab, elotuzumab, pomalidomide, and dexamethasone in relapsed and refractory MM
- CheckMate-039: A phase 1 study intended to establish the tolerability of nivolumab and the combination of nivolumab and daratumumab, with or without pomalidomide and dexamethasone, in patients with relapsed or refractory MM
- CA204142: A phase 2 study of elotuzumab in combination with pomalidomide and low-dose dexamethasone, and in combination with nivolumab, in patients with MM who relapsed after or were refractory to prior treatment with lenalidomide.
After consulting with Bristol-Myers Squibb, the FDA decided to lift the hold on CheckMate-039 (CA209 -039) and CA204142. These trials will continue with amended protocols.
The third trial, CheckMate-602, remains on partial clinical hold. Bristol-Myers Squibb said it is continuing to work with the FDA to determine next steps for this trial.
CheckMate-602 is not enrolling new patients. However, patients who are experiencing clinical benefit are continuing to receive treatment. ![]()
The US Food and Drug Administration (FDA) has lifted the partial clinical hold placed on 2 trials of the PD-1 immune checkpoint inhibitor nivolumab (Opdivo).
In these trials, CheckMate-039 (CA209 -039) and CA204142, researchers are investigating nivolumab-based combinations in patients with relapsed or refractory multiple myeloma (MM).
The partial clinical hold on these trials was a result of risks identified in studies involving another anti-PD-1 agent, pembrolizumab.
Data from the pembrolizumab trials suggested that risks outweigh benefits when PD-1/PD-L1 treatment is given to MM patients in combination with dexamethasone and pomalidomide or lenalidomide.
In addition, there could be an unfavorable risk-benefit ratio for MM patients receiving PD-1/PD-L1 treatments alone or in other combinations.
Therefore, the FDA placed a partial hold on the following nivolumab trials:
- CheckMate-602: A randomized, phase 3 trial of combinations of nivolumab, elotuzumab, pomalidomide, and dexamethasone in relapsed and refractory MM
- CheckMate-039: A phase 1 study intended to establish the tolerability of nivolumab and the combination of nivolumab and daratumumab, with or without pomalidomide and dexamethasone, in patients with relapsed or refractory MM
- CA204142: A phase 2 study of elotuzumab in combination with pomalidomide and low-dose dexamethasone, and in combination with nivolumab, in patients with MM who relapsed after or were refractory to prior treatment with lenalidomide.
After consulting with Bristol-Myers Squibb, the FDA decided to lift the hold on CheckMate-039 (CA209 -039) and CA204142. These trials will continue with amended protocols.
The third trial, CheckMate-602, remains on partial clinical hold. Bristol-Myers Squibb said it is continuing to work with the FDA to determine next steps for this trial.
CheckMate-602 is not enrolling new patients. However, patients who are experiencing clinical benefit are continuing to receive treatment. ![]()
The US Food and Drug Administration (FDA) has lifted the partial clinical hold placed on 2 trials of the PD-1 immune checkpoint inhibitor nivolumab (Opdivo).
In these trials, CheckMate-039 (CA209 -039) and CA204142, researchers are investigating nivolumab-based combinations in patients with relapsed or refractory multiple myeloma (MM).
The partial clinical hold on these trials was a result of risks identified in studies involving another anti-PD-1 agent, pembrolizumab.
Data from the pembrolizumab trials suggested that risks outweigh benefits when PD-1/PD-L1 treatment is given to MM patients in combination with dexamethasone and pomalidomide or lenalidomide.
In addition, there could be an unfavorable risk-benefit ratio for MM patients receiving PD-1/PD-L1 treatments alone or in other combinations.
Therefore, the FDA placed a partial hold on the following nivolumab trials:
- CheckMate-602: A randomized, phase 3 trial of combinations of nivolumab, elotuzumab, pomalidomide, and dexamethasone in relapsed and refractory MM
- CheckMate-039: A phase 1 study intended to establish the tolerability of nivolumab and the combination of nivolumab and daratumumab, with or without pomalidomide and dexamethasone, in patients with relapsed or refractory MM
- CA204142: A phase 2 study of elotuzumab in combination with pomalidomide and low-dose dexamethasone, and in combination with nivolumab, in patients with MM who relapsed after or were refractory to prior treatment with lenalidomide.
After consulting with Bristol-Myers Squibb, the FDA decided to lift the hold on CheckMate-039 (CA209 -039) and CA204142. These trials will continue with amended protocols.
The third trial, CheckMate-602, remains on partial clinical hold. Bristol-Myers Squibb said it is continuing to work with the FDA to determine next steps for this trial.
CheckMate-602 is not enrolling new patients. However, patients who are experiencing clinical benefit are continuing to receive treatment. ![]()
Anti-BCMA CAR T-cell therapy being fast tracked at FDA
The Food and Drug Administration has granted breakthrough therapy designation to bb2121, a chimeric antigen receptor T-cell (CAR T) therapy that targets b-cell maturation antigen (BCMA) in patients with relapsed/refractory multiple myeloma.
The therapy, being developed jointly by Celgene and bluebird bio, will be given expedited review by the FDA under the program. Meanwhile, European drug officials have granted it Priority Medicines eligibility, which also provides accelerated review.
The decision to fast track the review of bb2121 is based on preliminary data from the ongoing phase I CRB-401 trial. As of May 2017, there was 1-month clinical response data from 18 patients with multiple myeloma who were infused with bb2121. The overall response rate was 89%, but was 100% for patients who had been treated with doses of 150 × 106 CAR+ T cells or higher, according to an abstract from the annual meeting of the American Society of Hematology. Five months of follow-up data on these patients, plus initial data on additional patients, will be presented at ASH 2017 on Dec. 11.
The Food and Drug Administration has granted breakthrough therapy designation to bb2121, a chimeric antigen receptor T-cell (CAR T) therapy that targets b-cell maturation antigen (BCMA) in patients with relapsed/refractory multiple myeloma.
The therapy, being developed jointly by Celgene and bluebird bio, will be given expedited review by the FDA under the program. Meanwhile, European drug officials have granted it Priority Medicines eligibility, which also provides accelerated review.
The decision to fast track the review of bb2121 is based on preliminary data from the ongoing phase I CRB-401 trial. As of May 2017, there was 1-month clinical response data from 18 patients with multiple myeloma who were infused with bb2121. The overall response rate was 89%, but was 100% for patients who had been treated with doses of 150 × 106 CAR+ T cells or higher, according to an abstract from the annual meeting of the American Society of Hematology. Five months of follow-up data on these patients, plus initial data on additional patients, will be presented at ASH 2017 on Dec. 11.
The Food and Drug Administration has granted breakthrough therapy designation to bb2121, a chimeric antigen receptor T-cell (CAR T) therapy that targets b-cell maturation antigen (BCMA) in patients with relapsed/refractory multiple myeloma.
The therapy, being developed jointly by Celgene and bluebird bio, will be given expedited review by the FDA under the program. Meanwhile, European drug officials have granted it Priority Medicines eligibility, which also provides accelerated review.
The decision to fast track the review of bb2121 is based on preliminary data from the ongoing phase I CRB-401 trial. As of May 2017, there was 1-month clinical response data from 18 patients with multiple myeloma who were infused with bb2121. The overall response rate was 89%, but was 100% for patients who had been treated with doses of 150 × 106 CAR+ T cells or higher, according to an abstract from the annual meeting of the American Society of Hematology. Five months of follow-up data on these patients, plus initial data on additional patients, will be presented at ASH 2017 on Dec. 11.
Enzyme may be target for MM treatment
The enzyme ADAR1 may be a therapeutic target for multiple myeloma (MM), according to research published in Nature Communications.
Investigators found that high ADAR1 levels correlate with reduced survival rates in MM patients.
The team also discovered that blocking ADAR1 reduced regeneration of high-risk MM in serially transplantable patient-derived xenografts.
The investigators believe that JAK2 inhibitors could be used to dampen ADAR1 activity and ultimately prevent progression or relapse in patients with MM.
“Despite new therapies, it’s virtually inevitable that a patient with multiple myeloma will experience relapse of the disease at some point,” said study author Catriona Jamieson, MD, PhD, of University of California, San Diego, in La Jolla.
“That’s why it’s exciting that this discovery may allow us to detect the disease earlier and address the root cause.”
Dr Jamieson and her colleagues knew that ADAR1 is normally expressed during fetal development to help blood cells form. The enzyme edits the sequence of RNA and is known to promote cancer progression and resistance to therapy.
With previous work, Dr Jamieson’s team described ADAR1’s contributions to chronic myeloid leukemia (CML). The enzyme’s RNA-editing activity boosts leukemic stem cells, giving rise to CML, increasing disease recurrence, and allowing CML to resist treatment.
For their current study, Dr Jamieson and her colleagues investigated ADAR1’s role in MM, first analyzing a database of nearly 800 MM patient samples.
The investigators found that patients with low ADAR1 levels in their tumor cells survived longer than patients with high ADAR1 levels.
While more than 90% of patients with low ADAR1 levels survived longer than 2 years after their initial diagnosis, fewer than 70% of patients with high ADAR1 levels did the same.
The investigators also created a humanized mouse model of MM and found that silencing the ADAR1 gene reduced the engraftment of MM.
“This is a difficult disease to model in animals; there isn’t a single gene we can manipulate to mimic multiple myeloma,” said study author Leslie A. Crews, PhD, of University of California, San Diego.
“This study is important, in part because we now have a new xenograft model that will, for the first time, allow us to apply new biomarkers to better predict disease progression and test new therapeutics.”
To advance their findings from this study, the investigators are exploring ways to leverage ADAR1 to detect MM progression as early as possible.
They are also testing inhibitors of JAK2, a molecule that influences ADAR1 activity, for their ability to eliminate cancer stem cells in MM models.
“Several major advances in recent years have been good news for multiple myeloma patients, but those new drugs only target terminally differentiated cancer cells and, thus, can only reduce the bulk of the tumor,” Dr Jamieson said.
“They don’t get to the root cause of disease development, progression, and relapse—cancer stem cells—the way inhibiting ADAR1 does. I like to call our approach ‘precision regenerative medicine.’” ![]()
The enzyme ADAR1 may be a therapeutic target for multiple myeloma (MM), according to research published in Nature Communications.
Investigators found that high ADAR1 levels correlate with reduced survival rates in MM patients.
The team also discovered that blocking ADAR1 reduced regeneration of high-risk MM in serially transplantable patient-derived xenografts.
The investigators believe that JAK2 inhibitors could be used to dampen ADAR1 activity and ultimately prevent progression or relapse in patients with MM.
“Despite new therapies, it’s virtually inevitable that a patient with multiple myeloma will experience relapse of the disease at some point,” said study author Catriona Jamieson, MD, PhD, of University of California, San Diego, in La Jolla.
“That’s why it’s exciting that this discovery may allow us to detect the disease earlier and address the root cause.”
Dr Jamieson and her colleagues knew that ADAR1 is normally expressed during fetal development to help blood cells form. The enzyme edits the sequence of RNA and is known to promote cancer progression and resistance to therapy.
With previous work, Dr Jamieson’s team described ADAR1’s contributions to chronic myeloid leukemia (CML). The enzyme’s RNA-editing activity boosts leukemic stem cells, giving rise to CML, increasing disease recurrence, and allowing CML to resist treatment.
For their current study, Dr Jamieson and her colleagues investigated ADAR1’s role in MM, first analyzing a database of nearly 800 MM patient samples.
The investigators found that patients with low ADAR1 levels in their tumor cells survived longer than patients with high ADAR1 levels.
While more than 90% of patients with low ADAR1 levels survived longer than 2 years after their initial diagnosis, fewer than 70% of patients with high ADAR1 levels did the same.
The investigators also created a humanized mouse model of MM and found that silencing the ADAR1 gene reduced the engraftment of MM.
“This is a difficult disease to model in animals; there isn’t a single gene we can manipulate to mimic multiple myeloma,” said study author Leslie A. Crews, PhD, of University of California, San Diego.
“This study is important, in part because we now have a new xenograft model that will, for the first time, allow us to apply new biomarkers to better predict disease progression and test new therapeutics.”
To advance their findings from this study, the investigators are exploring ways to leverage ADAR1 to detect MM progression as early as possible.
They are also testing inhibitors of JAK2, a molecule that influences ADAR1 activity, for their ability to eliminate cancer stem cells in MM models.
“Several major advances in recent years have been good news for multiple myeloma patients, but those new drugs only target terminally differentiated cancer cells and, thus, can only reduce the bulk of the tumor,” Dr Jamieson said.
“They don’t get to the root cause of disease development, progression, and relapse—cancer stem cells—the way inhibiting ADAR1 does. I like to call our approach ‘precision regenerative medicine.’” ![]()
The enzyme ADAR1 may be a therapeutic target for multiple myeloma (MM), according to research published in Nature Communications.
Investigators found that high ADAR1 levels correlate with reduced survival rates in MM patients.
The team also discovered that blocking ADAR1 reduced regeneration of high-risk MM in serially transplantable patient-derived xenografts.
The investigators believe that JAK2 inhibitors could be used to dampen ADAR1 activity and ultimately prevent progression or relapse in patients with MM.
“Despite new therapies, it’s virtually inevitable that a patient with multiple myeloma will experience relapse of the disease at some point,” said study author Catriona Jamieson, MD, PhD, of University of California, San Diego, in La Jolla.
“That’s why it’s exciting that this discovery may allow us to detect the disease earlier and address the root cause.”
Dr Jamieson and her colleagues knew that ADAR1 is normally expressed during fetal development to help blood cells form. The enzyme edits the sequence of RNA and is known to promote cancer progression and resistance to therapy.
With previous work, Dr Jamieson’s team described ADAR1’s contributions to chronic myeloid leukemia (CML). The enzyme’s RNA-editing activity boosts leukemic stem cells, giving rise to CML, increasing disease recurrence, and allowing CML to resist treatment.
For their current study, Dr Jamieson and her colleagues investigated ADAR1’s role in MM, first analyzing a database of nearly 800 MM patient samples.
The investigators found that patients with low ADAR1 levels in their tumor cells survived longer than patients with high ADAR1 levels.
While more than 90% of patients with low ADAR1 levels survived longer than 2 years after their initial diagnosis, fewer than 70% of patients with high ADAR1 levels did the same.
The investigators also created a humanized mouse model of MM and found that silencing the ADAR1 gene reduced the engraftment of MM.
“This is a difficult disease to model in animals; there isn’t a single gene we can manipulate to mimic multiple myeloma,” said study author Leslie A. Crews, PhD, of University of California, San Diego.
“This study is important, in part because we now have a new xenograft model that will, for the first time, allow us to apply new biomarkers to better predict disease progression and test new therapeutics.”
To advance their findings from this study, the investigators are exploring ways to leverage ADAR1 to detect MM progression as early as possible.
They are also testing inhibitors of JAK2, a molecule that influences ADAR1 activity, for their ability to eliminate cancer stem cells in MM models.
“Several major advances in recent years have been good news for multiple myeloma patients, but those new drugs only target terminally differentiated cancer cells and, thus, can only reduce the bulk of the tumor,” Dr Jamieson said.
“They don’t get to the root cause of disease development, progression, and relapse—cancer stem cells—the way inhibiting ADAR1 does. I like to call our approach ‘precision regenerative medicine.’” ![]()