User login
Application for pegfilgrastim biosimilar withdrawn
Mylan S.A.S. has withdrawn the European marketing authorization application for its pegfilgrastim biosimilar Fulphila, according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
Fulphila was intended to be used to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving cytotoxic therapy for malignancy (except chronic myeloid leukemia and myelodysplastic syndromes).
Fulphila was intended to be highly similar to Neulasta, a solution for injection that contains the active substance pegfilgrastim.
To support the application for Fulphila, Mylan S.A.S. presented results of studies designed to show that Fulphila is highly similar to Neulasta in terms of chemical structure, purity, mechanism, safety, effectiveness, and immunogenicity.
Mylan S.A.S withdrew the application for Fulphila after the CHMP had evaluated the initial documentation the company provided on the drug and formulated a list of questions. The CHMP was assessing the company’s responses to the questions when the application was withdrawn.
At the time of the withdrawal, the CHMP had some concerns and was of the provisional opinion that Fulphila could not have been approved.
One of the CHMP’s main concerns was the lack of a certificate of Good Manufacturing Practice for the manufacturing site of the product. Other concerns related to the description of the manufacturing process, the control of impurities in the active substance, and the sterilization of the final product.
In a letter to the European Medicines Agency, Mylan S.A.S said it withdrew the application for Fulphila because a Good Manufacturing Practice certificate for the manufacturing site could not be obtained in the time available.
The application withdrawal does not impact ongoing clinical trials of Fulphila, and there are no compassionate use programs for the drug.
Mylan S.A.S said it plans to resubmit the application for Fulphila as soon as possible. The company is working to ensure “inspection readiness” at the Fulphila manufacturing site by October 2017. ![]()
Mylan S.A.S. has withdrawn the European marketing authorization application for its pegfilgrastim biosimilar Fulphila, according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
Fulphila was intended to be used to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving cytotoxic therapy for malignancy (except chronic myeloid leukemia and myelodysplastic syndromes).
Fulphila was intended to be highly similar to Neulasta, a solution for injection that contains the active substance pegfilgrastim.
To support the application for Fulphila, Mylan S.A.S. presented results of studies designed to show that Fulphila is highly similar to Neulasta in terms of chemical structure, purity, mechanism, safety, effectiveness, and immunogenicity.
Mylan S.A.S withdrew the application for Fulphila after the CHMP had evaluated the initial documentation the company provided on the drug and formulated a list of questions. The CHMP was assessing the company’s responses to the questions when the application was withdrawn.
At the time of the withdrawal, the CHMP had some concerns and was of the provisional opinion that Fulphila could not have been approved.
One of the CHMP’s main concerns was the lack of a certificate of Good Manufacturing Practice for the manufacturing site of the product. Other concerns related to the description of the manufacturing process, the control of impurities in the active substance, and the sterilization of the final product.
In a letter to the European Medicines Agency, Mylan S.A.S said it withdrew the application for Fulphila because a Good Manufacturing Practice certificate for the manufacturing site could not be obtained in the time available.
The application withdrawal does not impact ongoing clinical trials of Fulphila, and there are no compassionate use programs for the drug.
Mylan S.A.S said it plans to resubmit the application for Fulphila as soon as possible. The company is working to ensure “inspection readiness” at the Fulphila manufacturing site by October 2017. ![]()
Mylan S.A.S. has withdrawn the European marketing authorization application for its pegfilgrastim biosimilar Fulphila, according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
Fulphila was intended to be used to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults receiving cytotoxic therapy for malignancy (except chronic myeloid leukemia and myelodysplastic syndromes).
Fulphila was intended to be highly similar to Neulasta, a solution for injection that contains the active substance pegfilgrastim.
To support the application for Fulphila, Mylan S.A.S. presented results of studies designed to show that Fulphila is highly similar to Neulasta in terms of chemical structure, purity, mechanism, safety, effectiveness, and immunogenicity.
Mylan S.A.S withdrew the application for Fulphila after the CHMP had evaluated the initial documentation the company provided on the drug and formulated a list of questions. The CHMP was assessing the company’s responses to the questions when the application was withdrawn.
At the time of the withdrawal, the CHMP had some concerns and was of the provisional opinion that Fulphila could not have been approved.
One of the CHMP’s main concerns was the lack of a certificate of Good Manufacturing Practice for the manufacturing site of the product. Other concerns related to the description of the manufacturing process, the control of impurities in the active substance, and the sterilization of the final product.
In a letter to the European Medicines Agency, Mylan S.A.S said it withdrew the application for Fulphila because a Good Manufacturing Practice certificate for the manufacturing site could not be obtained in the time available.
The application withdrawal does not impact ongoing clinical trials of Fulphila, and there are no compassionate use programs for the drug.
Mylan S.A.S said it plans to resubmit the application for Fulphila as soon as possible. The company is working to ensure “inspection readiness” at the Fulphila manufacturing site by October 2017. ![]()
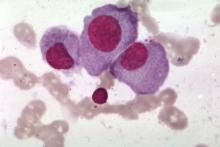
Most daratumumab infusion reactions occur in first infusion
MADRID – The high rate of infusion-related reactions at first daratumumab infusion may be related to treatment duration, based on data from the CASTOR and POLLUX studies presented at the European Society for Medical Oncology Congress.
Infusion-related reactions occur in half of relapsed or refractory multiple myeloma patients who receive daratumumab, but nearly all reactions are grade 2 or less and rarely lead to treatment discontinuation, reported Philippe Moreau, MD, of University Hospital, Nantes, France.
“In the two phase 3 trials, CASTOR and POLLUX, infusion-related reactions occurred in 45% and 48% of patients, respectively. Of these, 98% and 96%, respectively, occurred during the first infusion,” he said. Treatment duration was 7 hours for first infusion vs. 4 hours and 3 hours for the second and third infusions, respectively. Grade 3 infusion-related reactions occurred in 5.3% and 8.6% of patients in CASTOR and POLLUX, respectively. No grade 4 infusion-related reactions were observed in either trial.
(In CASTOR [NCT02136134], daratumumab was combined with bortezomib and dexamethasone. In POLLUX [NCT02076009], it was combined with lenalidomide and dexamethasone. Based on improvements in progression-free survival relative to the background drugs alone, daratumumab was approved for relapsed or refractory multiple myeloma.)
All patients in the trials received some form of preinfusion medications. These included 650-1,000 mg of paracetamol by intravenous or oral administration, 25-50 mg of diphenhydramine, 10 mg of montelukast, and 20 mg of dexamethasone. Patients thought to be at high risk of respiratory complications were candidates for postinfusion medications such as diphenhydramine or a short-acting beta agonist. However, only about 10% of high-risk patients received these therapies, so the impact of this potentially preventive approach is not clear, Dr. Moreau said.
In grade 1 reactions, Dr. Moreau recommended that infusions be paused at the first sign of an infusion-related reaction and then restarted at half the infusion rate when the condition is considered stable. Daratumumab treatment should be withdrawn in grade 2 or higher infusion-related reactions associated with laryngeal edema or grade 2 or higher bronchospasm that does not respond to systemic therapy and resolves within 6 hours of onset.
In grade 3 infusion-related reactions, the recommendation is to stop the daratumumab infusion and closely observe the patient. The infusion should be restarted only if the severity drops to grade 1. Again, the rate of infusion after the interruption should be half the rate provided prior to the infusion-related reaction. Therapy should be withdrawn if the infusion-related reaction recurs for a second time, according to Dr. Moreau.
Infusion-related reactions involving the upper respiratory tract – such as dyspnea, cough, bronchospasm, or throat irritation – may be related to the physiologic function of CD38, Dr. Moreau said. For this reason, grade 3 upper respiratory-related events deserve close attention and persisting symptoms warrant halting treatment.
The evidence is “reassuring” that the majority of infusion-related reactions are confined to the first infusion, said the ESMO-invited discussant, Evangelos Terpos, MD, PhD, of the University of Athens. He noted that the specific treatment recommendations outlined by Dr. Moreau could be helpful for minimizing nuisance infusion-related reactions as well as reducing the risk of more serious infusion-related reactions, particularly those involving respiratory events.
Prophylactic strategies for infusion-related reactions are particularly important in patients with risk factors for respiratory complications, Dr. Terpos added.
MADRID – The high rate of infusion-related reactions at first daratumumab infusion may be related to treatment duration, based on data from the CASTOR and POLLUX studies presented at the European Society for Medical Oncology Congress.
Infusion-related reactions occur in half of relapsed or refractory multiple myeloma patients who receive daratumumab, but nearly all reactions are grade 2 or less and rarely lead to treatment discontinuation, reported Philippe Moreau, MD, of University Hospital, Nantes, France.
“In the two phase 3 trials, CASTOR and POLLUX, infusion-related reactions occurred in 45% and 48% of patients, respectively. Of these, 98% and 96%, respectively, occurred during the first infusion,” he said. Treatment duration was 7 hours for first infusion vs. 4 hours and 3 hours for the second and third infusions, respectively. Grade 3 infusion-related reactions occurred in 5.3% and 8.6% of patients in CASTOR and POLLUX, respectively. No grade 4 infusion-related reactions were observed in either trial.
(In CASTOR [NCT02136134], daratumumab was combined with bortezomib and dexamethasone. In POLLUX [NCT02076009], it was combined with lenalidomide and dexamethasone. Based on improvements in progression-free survival relative to the background drugs alone, daratumumab was approved for relapsed or refractory multiple myeloma.)
All patients in the trials received some form of preinfusion medications. These included 650-1,000 mg of paracetamol by intravenous or oral administration, 25-50 mg of diphenhydramine, 10 mg of montelukast, and 20 mg of dexamethasone. Patients thought to be at high risk of respiratory complications were candidates for postinfusion medications such as diphenhydramine or a short-acting beta agonist. However, only about 10% of high-risk patients received these therapies, so the impact of this potentially preventive approach is not clear, Dr. Moreau said.
In grade 1 reactions, Dr. Moreau recommended that infusions be paused at the first sign of an infusion-related reaction and then restarted at half the infusion rate when the condition is considered stable. Daratumumab treatment should be withdrawn in grade 2 or higher infusion-related reactions associated with laryngeal edema or grade 2 or higher bronchospasm that does not respond to systemic therapy and resolves within 6 hours of onset.
In grade 3 infusion-related reactions, the recommendation is to stop the daratumumab infusion and closely observe the patient. The infusion should be restarted only if the severity drops to grade 1. Again, the rate of infusion after the interruption should be half the rate provided prior to the infusion-related reaction. Therapy should be withdrawn if the infusion-related reaction recurs for a second time, according to Dr. Moreau.
Infusion-related reactions involving the upper respiratory tract – such as dyspnea, cough, bronchospasm, or throat irritation – may be related to the physiologic function of CD38, Dr. Moreau said. For this reason, grade 3 upper respiratory-related events deserve close attention and persisting symptoms warrant halting treatment.
The evidence is “reassuring” that the majority of infusion-related reactions are confined to the first infusion, said the ESMO-invited discussant, Evangelos Terpos, MD, PhD, of the University of Athens. He noted that the specific treatment recommendations outlined by Dr. Moreau could be helpful for minimizing nuisance infusion-related reactions as well as reducing the risk of more serious infusion-related reactions, particularly those involving respiratory events.
Prophylactic strategies for infusion-related reactions are particularly important in patients with risk factors for respiratory complications, Dr. Terpos added.
MADRID – The high rate of infusion-related reactions at first daratumumab infusion may be related to treatment duration, based on data from the CASTOR and POLLUX studies presented at the European Society for Medical Oncology Congress.
Infusion-related reactions occur in half of relapsed or refractory multiple myeloma patients who receive daratumumab, but nearly all reactions are grade 2 or less and rarely lead to treatment discontinuation, reported Philippe Moreau, MD, of University Hospital, Nantes, France.
“In the two phase 3 trials, CASTOR and POLLUX, infusion-related reactions occurred in 45% and 48% of patients, respectively. Of these, 98% and 96%, respectively, occurred during the first infusion,” he said. Treatment duration was 7 hours for first infusion vs. 4 hours and 3 hours for the second and third infusions, respectively. Grade 3 infusion-related reactions occurred in 5.3% and 8.6% of patients in CASTOR and POLLUX, respectively. No grade 4 infusion-related reactions were observed in either trial.
(In CASTOR [NCT02136134], daratumumab was combined with bortezomib and dexamethasone. In POLLUX [NCT02076009], it was combined with lenalidomide and dexamethasone. Based on improvements in progression-free survival relative to the background drugs alone, daratumumab was approved for relapsed or refractory multiple myeloma.)
All patients in the trials received some form of preinfusion medications. These included 650-1,000 mg of paracetamol by intravenous or oral administration, 25-50 mg of diphenhydramine, 10 mg of montelukast, and 20 mg of dexamethasone. Patients thought to be at high risk of respiratory complications were candidates for postinfusion medications such as diphenhydramine or a short-acting beta agonist. However, only about 10% of high-risk patients received these therapies, so the impact of this potentially preventive approach is not clear, Dr. Moreau said.
In grade 1 reactions, Dr. Moreau recommended that infusions be paused at the first sign of an infusion-related reaction and then restarted at half the infusion rate when the condition is considered stable. Daratumumab treatment should be withdrawn in grade 2 or higher infusion-related reactions associated with laryngeal edema or grade 2 or higher bronchospasm that does not respond to systemic therapy and resolves within 6 hours of onset.
In grade 3 infusion-related reactions, the recommendation is to stop the daratumumab infusion and closely observe the patient. The infusion should be restarted only if the severity drops to grade 1. Again, the rate of infusion after the interruption should be half the rate provided prior to the infusion-related reaction. Therapy should be withdrawn if the infusion-related reaction recurs for a second time, according to Dr. Moreau.
Infusion-related reactions involving the upper respiratory tract – such as dyspnea, cough, bronchospasm, or throat irritation – may be related to the physiologic function of CD38, Dr. Moreau said. For this reason, grade 3 upper respiratory-related events deserve close attention and persisting symptoms warrant halting treatment.
The evidence is “reassuring” that the majority of infusion-related reactions are confined to the first infusion, said the ESMO-invited discussant, Evangelos Terpos, MD, PhD, of the University of Athens. He noted that the specific treatment recommendations outlined by Dr. Moreau could be helpful for minimizing nuisance infusion-related reactions as well as reducing the risk of more serious infusion-related reactions, particularly those involving respiratory events.
Prophylactic strategies for infusion-related reactions are particularly important in patients with risk factors for respiratory complications, Dr. Terpos added.
AT ESMO 2017
Key clinical point: In grade 1 infusion-related reactions, daratumumab infusion should be paused at the first sign of a reaction and then restarted at half the infusion rate when the condition is considered stable.
Major finding:
Data source: Post hoc analysis of the phase 3 trials, CASTOR and POLLUX.
Disclosures: Dr. Moreau reported financial relationships with Amgen, Celgene, Janssen, Novartis, and Takeda.
Report details progress, obstacles in cancer research and care
Deaths from cancer are on the decline in the US, but new cases of cancer are on the rise, according to the 7th annual American Association for Cancer Research (AACR) Cancer Progress Report.
The data suggest the cancer death rate declined by 35% from 1991 to 2014 for children and by 25% for adults, a reduction that translates to 2.1 million cancer deaths avoided.
However, 600,920 people in the US are projected to die from cancer in 2017.
And the number of new cancer cases is predicted to rise from 1.7 million in 2017 to 2.3 million in 2030.
The report also estimates there will be 62,130 new cases of leukemia in 2017 and 24,500 leukemia deaths this year.
This includes:
- 5970 cases of acute lymphocytic leukemia and 1440 deaths
- 20,110 cases of chronic lymphocytic leukemia and 4660 deaths
- 21,380 cases of acute myeloid leukemia (AML) and 10,590 deaths
- 8950 cases of chronic myeloid leukemia and 1080 deaths.
The estimate for lymphomas is 80,500 new cases and 21,210 deaths.
This includes:
- 8260 cases of Hodgkin lymphoma (HL) and 1070 deaths
- 72,240 cases of non-Hodgkin lymphoma and 20,140 deaths.
The estimate for myeloma is 30,280 new cases and 12,590 deaths.
The report says the estimated new cases of cancer are based on cancer incidence rates from 49 states and the District of Columbia from 1995 through 2013, as reported by the North American Association of Central Cancer Registries. This represents about 98% of the US population.
The estimated deaths are based on US mortality data from 1997 through 2013, taken from the National Center for Health Statistics of the Centers for Disease Control and Prevention.
Drug approvals
The AACR report notes that, between August 1, 2016, and July 31, 2017, the US Food and Drug Administration (FDA) approved new uses for 15 anticancer agents, 9 of which had no previous FDA approval.
Five of the agents are immunotherapies, which the report dubs “revolutionary treatments that are increasing survival and improving quality of life for patients.”
Among the recently approved therapies are 3 used for hematology indications:
- Ibrutinib (Imbruvica), approved to treat patients with relapsed/refractory marginal zone lymphoma who require systemic therapy and have received at least 1 prior anti-CD20-based therapy
- Midostaurin (Rydapt), approved as monotherapy for adults with advanced systemic mastocytosis and for use in combination with standard cytarabine and daunorubicin induction, followed by cytarabine consolidation, in adults with newly diagnosed AML who are FLT3 mutation-positive, as detected by an FDA-approved test.
- Pembrolizumab (Keytruda), approved to treat adult and pediatric patients with refractory classical HL or those with classical HL who have relapsed after 3 or more prior lines of therapy.
Disparities and costs
The AACR report points out that advances against cancer have not benefited everyone equally, and cancer health disparities are some of the most pressing challenges.
Among the disparities listed is the fact that adolescents and young adults (ages 15 to 39) with AML have a 5-year relative survival rate that is 22% lower than that of children (ages 1 to 14) with AML.
And Hispanic children are 24% more likely to develop leukemia than non-Hispanic children.
Another concern mentioned in the report is the cost of cancer care. The direct medical costs of cancer care in 2014 were estimated to be nearly $87.6 billion. This number does not include the indirect costs of lost productivity due to cancer-related morbidity and mortality.
With this in mind, the AACR is calling for a $2 billion increase in funding for the National Institutes of Health in fiscal year 2018, for a total funding level of $36.2 billion.
The AACR also recommends an $80 million increase in the FDA budget, bringing it to $2.8 billion for fiscal year 2018. ![]()
Deaths from cancer are on the decline in the US, but new cases of cancer are on the rise, according to the 7th annual American Association for Cancer Research (AACR) Cancer Progress Report.
The data suggest the cancer death rate declined by 35% from 1991 to 2014 for children and by 25% for adults, a reduction that translates to 2.1 million cancer deaths avoided.
However, 600,920 people in the US are projected to die from cancer in 2017.
And the number of new cancer cases is predicted to rise from 1.7 million in 2017 to 2.3 million in 2030.
The report also estimates there will be 62,130 new cases of leukemia in 2017 and 24,500 leukemia deaths this year.
This includes:
- 5970 cases of acute lymphocytic leukemia and 1440 deaths
- 20,110 cases of chronic lymphocytic leukemia and 4660 deaths
- 21,380 cases of acute myeloid leukemia (AML) and 10,590 deaths
- 8950 cases of chronic myeloid leukemia and 1080 deaths.
The estimate for lymphomas is 80,500 new cases and 21,210 deaths.
This includes:
- 8260 cases of Hodgkin lymphoma (HL) and 1070 deaths
- 72,240 cases of non-Hodgkin lymphoma and 20,140 deaths.
The estimate for myeloma is 30,280 new cases and 12,590 deaths.
The report says the estimated new cases of cancer are based on cancer incidence rates from 49 states and the District of Columbia from 1995 through 2013, as reported by the North American Association of Central Cancer Registries. This represents about 98% of the US population.
The estimated deaths are based on US mortality data from 1997 through 2013, taken from the National Center for Health Statistics of the Centers for Disease Control and Prevention.
Drug approvals
The AACR report notes that, between August 1, 2016, and July 31, 2017, the US Food and Drug Administration (FDA) approved new uses for 15 anticancer agents, 9 of which had no previous FDA approval.
Five of the agents are immunotherapies, which the report dubs “revolutionary treatments that are increasing survival and improving quality of life for patients.”
Among the recently approved therapies are 3 used for hematology indications:
- Ibrutinib (Imbruvica), approved to treat patients with relapsed/refractory marginal zone lymphoma who require systemic therapy and have received at least 1 prior anti-CD20-based therapy
- Midostaurin (Rydapt), approved as monotherapy for adults with advanced systemic mastocytosis and for use in combination with standard cytarabine and daunorubicin induction, followed by cytarabine consolidation, in adults with newly diagnosed AML who are FLT3 mutation-positive, as detected by an FDA-approved test.
- Pembrolizumab (Keytruda), approved to treat adult and pediatric patients with refractory classical HL or those with classical HL who have relapsed after 3 or more prior lines of therapy.
Disparities and costs
The AACR report points out that advances against cancer have not benefited everyone equally, and cancer health disparities are some of the most pressing challenges.
Among the disparities listed is the fact that adolescents and young adults (ages 15 to 39) with AML have a 5-year relative survival rate that is 22% lower than that of children (ages 1 to 14) with AML.
And Hispanic children are 24% more likely to develop leukemia than non-Hispanic children.
Another concern mentioned in the report is the cost of cancer care. The direct medical costs of cancer care in 2014 were estimated to be nearly $87.6 billion. This number does not include the indirect costs of lost productivity due to cancer-related morbidity and mortality.
With this in mind, the AACR is calling for a $2 billion increase in funding for the National Institutes of Health in fiscal year 2018, for a total funding level of $36.2 billion.
The AACR also recommends an $80 million increase in the FDA budget, bringing it to $2.8 billion for fiscal year 2018. ![]()
Deaths from cancer are on the decline in the US, but new cases of cancer are on the rise, according to the 7th annual American Association for Cancer Research (AACR) Cancer Progress Report.
The data suggest the cancer death rate declined by 35% from 1991 to 2014 for children and by 25% for adults, a reduction that translates to 2.1 million cancer deaths avoided.
However, 600,920 people in the US are projected to die from cancer in 2017.
And the number of new cancer cases is predicted to rise from 1.7 million in 2017 to 2.3 million in 2030.
The report also estimates there will be 62,130 new cases of leukemia in 2017 and 24,500 leukemia deaths this year.
This includes:
- 5970 cases of acute lymphocytic leukemia and 1440 deaths
- 20,110 cases of chronic lymphocytic leukemia and 4660 deaths
- 21,380 cases of acute myeloid leukemia (AML) and 10,590 deaths
- 8950 cases of chronic myeloid leukemia and 1080 deaths.
The estimate for lymphomas is 80,500 new cases and 21,210 deaths.
This includes:
- 8260 cases of Hodgkin lymphoma (HL) and 1070 deaths
- 72,240 cases of non-Hodgkin lymphoma and 20,140 deaths.
The estimate for myeloma is 30,280 new cases and 12,590 deaths.
The report says the estimated new cases of cancer are based on cancer incidence rates from 49 states and the District of Columbia from 1995 through 2013, as reported by the North American Association of Central Cancer Registries. This represents about 98% of the US population.
The estimated deaths are based on US mortality data from 1997 through 2013, taken from the National Center for Health Statistics of the Centers for Disease Control and Prevention.
Drug approvals
The AACR report notes that, between August 1, 2016, and July 31, 2017, the US Food and Drug Administration (FDA) approved new uses for 15 anticancer agents, 9 of which had no previous FDA approval.
Five of the agents are immunotherapies, which the report dubs “revolutionary treatments that are increasing survival and improving quality of life for patients.”
Among the recently approved therapies are 3 used for hematology indications:
- Ibrutinib (Imbruvica), approved to treat patients with relapsed/refractory marginal zone lymphoma who require systemic therapy and have received at least 1 prior anti-CD20-based therapy
- Midostaurin (Rydapt), approved as monotherapy for adults with advanced systemic mastocytosis and for use in combination with standard cytarabine and daunorubicin induction, followed by cytarabine consolidation, in adults with newly diagnosed AML who are FLT3 mutation-positive, as detected by an FDA-approved test.
- Pembrolizumab (Keytruda), approved to treat adult and pediatric patients with refractory classical HL or those with classical HL who have relapsed after 3 or more prior lines of therapy.
Disparities and costs
The AACR report points out that advances against cancer have not benefited everyone equally, and cancer health disparities are some of the most pressing challenges.
Among the disparities listed is the fact that adolescents and young adults (ages 15 to 39) with AML have a 5-year relative survival rate that is 22% lower than that of children (ages 1 to 14) with AML.
And Hispanic children are 24% more likely to develop leukemia than non-Hispanic children.
Another concern mentioned in the report is the cost of cancer care. The direct medical costs of cancer care in 2014 were estimated to be nearly $87.6 billion. This number does not include the indirect costs of lost productivity due to cancer-related morbidity and mortality.
With this in mind, the AACR is calling for a $2 billion increase in funding for the National Institutes of Health in fiscal year 2018, for a total funding level of $36.2 billion.
The AACR also recommends an $80 million increase in the FDA budget, bringing it to $2.8 billion for fiscal year 2018. ![]()
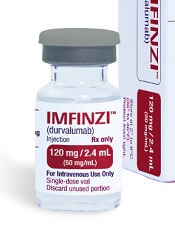
KW-2478 examined as novel add-on therapy for myeloma
Bortezomib and KW-2478, a novel nonansamycin heat shock protein 90 (Hsp90) inhibitor, had modest activity and was well tolerated in an open-label phase 1/2 study of patients with relapsed or refractory multiple myeloma.
The objective response rate in 79 evaluable patients treated with the combination was 39.2%, and the clinical benefit rate was 51.9%. Median progression-free survival was 6.7 months, and median duration of response was 5.5 months, according to a report by Jamie Cavenagh, MD, of St. Bartholomew’s Hospital, West Smithfield, London, and colleagues. The results were published online in the British Journal of Cancer.
KW-2478 showed synergistic antitumor activity with bortezomib in preclinical in vitro and in vivo studies, and the recommended phase 2 intravenous dosage of 175 mg/m2, along with 1.3 mg/m2 of bortezomib on days 1, 4, 8, and 11 of each 21-day cycle (up to eight cycles) in the current study was determined by phase 1 dose escalation; the maximum tolerated dose was not reached.
Although the antimyeloma activity of this novel treatment combination was relatively modest, the tolerability and apparent lack of overlapping toxicity suggest it deserves further exploration, including with alternate dosing schedules and combinations, for the treatment of relapsed/refractory multiple myeloma, the investigators concluded, noting that KW-2478 should also be studied in combination with other antimyeloma agents.
Kyowa Kirin Pharmaceutical Development Inc. funded the study. Dr. Cavenagh reported having no disclosures. Several other authors reported employment by the sponsor or by Kyowa Hakko Kirin Co. Ltd. Another, K. Yong, MD, reported receiving support from the National Institute for Health Research.
Bortezomib and KW-2478, a novel nonansamycin heat shock protein 90 (Hsp90) inhibitor, had modest activity and was well tolerated in an open-label phase 1/2 study of patients with relapsed or refractory multiple myeloma.
The objective response rate in 79 evaluable patients treated with the combination was 39.2%, and the clinical benefit rate was 51.9%. Median progression-free survival was 6.7 months, and median duration of response was 5.5 months, according to a report by Jamie Cavenagh, MD, of St. Bartholomew’s Hospital, West Smithfield, London, and colleagues. The results were published online in the British Journal of Cancer.
KW-2478 showed synergistic antitumor activity with bortezomib in preclinical in vitro and in vivo studies, and the recommended phase 2 intravenous dosage of 175 mg/m2, along with 1.3 mg/m2 of bortezomib on days 1, 4, 8, and 11 of each 21-day cycle (up to eight cycles) in the current study was determined by phase 1 dose escalation; the maximum tolerated dose was not reached.
Although the antimyeloma activity of this novel treatment combination was relatively modest, the tolerability and apparent lack of overlapping toxicity suggest it deserves further exploration, including with alternate dosing schedules and combinations, for the treatment of relapsed/refractory multiple myeloma, the investigators concluded, noting that KW-2478 should also be studied in combination with other antimyeloma agents.
Kyowa Kirin Pharmaceutical Development Inc. funded the study. Dr. Cavenagh reported having no disclosures. Several other authors reported employment by the sponsor or by Kyowa Hakko Kirin Co. Ltd. Another, K. Yong, MD, reported receiving support from the National Institute for Health Research.
Bortezomib and KW-2478, a novel nonansamycin heat shock protein 90 (Hsp90) inhibitor, had modest activity and was well tolerated in an open-label phase 1/2 study of patients with relapsed or refractory multiple myeloma.
The objective response rate in 79 evaluable patients treated with the combination was 39.2%, and the clinical benefit rate was 51.9%. Median progression-free survival was 6.7 months, and median duration of response was 5.5 months, according to a report by Jamie Cavenagh, MD, of St. Bartholomew’s Hospital, West Smithfield, London, and colleagues. The results were published online in the British Journal of Cancer.
KW-2478 showed synergistic antitumor activity with bortezomib in preclinical in vitro and in vivo studies, and the recommended phase 2 intravenous dosage of 175 mg/m2, along with 1.3 mg/m2 of bortezomib on days 1, 4, 8, and 11 of each 21-day cycle (up to eight cycles) in the current study was determined by phase 1 dose escalation; the maximum tolerated dose was not reached.
Although the antimyeloma activity of this novel treatment combination was relatively modest, the tolerability and apparent lack of overlapping toxicity suggest it deserves further exploration, including with alternate dosing schedules and combinations, for the treatment of relapsed/refractory multiple myeloma, the investigators concluded, noting that KW-2478 should also be studied in combination with other antimyeloma agents.
Kyowa Kirin Pharmaceutical Development Inc. funded the study. Dr. Cavenagh reported having no disclosures. Several other authors reported employment by the sponsor or by Kyowa Hakko Kirin Co. Ltd. Another, K. Yong, MD, reported receiving support from the National Institute for Health Research.
FROM THE BRITISH JOURNAL OF CANCER
Key clinical point:
Major finding: The objective response rate was 39.2%, and the clinical benefit rate was 51.9%.
Data source: An open-label phase 1/2 study of 95 patients.
Disclosures: Kyowa Kirin Pharmaceutical Development Inc. funded the study. Dr. Cavenagh reported having no disclosures. Several other authors reported employment by the sponsor or by Kyowa Hakko Kirin Co. Ltd. Another, K. Yong, MD, reported receiving support from the National Institute for Health Research.
Study: Many cancer patients don’t understand clinical trials
MADRID—Results of a nationwide study suggest many cancer patients in Ireland don’t understand key aspects of clinical trial methodology.
Most of the patients surveyed, which included individuals who had participated in a clinical trial, did not understand the concepts of randomization or equipoise.
“Over half of previous medical trial participants and 73% of those who had never been on a cancer clinical trial did not understand that, in a randomized trial, the treatment given was decided by chance,” said study investigator Catherine Kelly, MB BCh, of Mater Misericordiae University Hospital in Dublin, Ireland.
“We also found that most patients did not understand clinical equipoise—the fact that no one knows which treatment is best. Surprisingly, this was more marked in previous clinical trial participants, 60% of whom believed that their doctor would know which study arm was best.”
Dr Kelly and her colleagues presented these findings at the ESMO 2017 Congress (abstract 1465P_PR).
The researchers surveyed 1090 adult cancer patients treated at 1 of 14 participating oncology centers across Ireland.
The patients’ median age was 60 (range, 50-69), 64.4% were female, and 66% were diagnosed between 2014 and 2016. The most common cancer types were breast (31.4%), colorectal (15.6%), hematologic (12.6%), genitourinary (11.6%), and lung (6.8%).
The patients filled out anonymized questionnaires in which they were asked to evaluate statements about clinical trials. The patients had to determine whether a statement is true or false, or they could indicate that they didn’t know an answer.
A majority of the patients (82.3%) said they understood what a medical or cancer clinical trial is. And 27.8% of patients said they had previously participated in a cancer trial.
However, many patients didn’t know when clinical trials may be an option. Twenty-two percent of patients said it is true that “clinical trials are only used when standard treatments have not worked,” and 26.6% said they didn’t know if this statement is true or false.
Roughly a third (33.5%) of patients said it is true that, in a randomized trial, treatment is decided by chance, but 41.4% of patients said this is false, and 25% said they didn’t know.
More than half of patients (56.5%) said their doctor would know which treatment was superior in a clinical trial, and 23.2% of patients said they didn’t know if their doctor would know.
About 61% of all patients said their doctor would make sure they received the superior treatment in a clinical trial. An even greater percentage—63.6%—of patients who had previously participated in a clinical trial said the same.
“To provide informed consent when participating in a trial, patients need to understand these key concepts, and doctors explaining them well is essential to alleviating any fears that might prevent patients from participating,” Dr Kelly said.
“Doctors have a responsibility to properly inform their patients in this regard because they are the ones patients trust the most. As we analyze the data further, we will be able to offer physicians a more detailed picture of the questions patients need answered and the factors that influence their decision-making according to age group, cancer type, educational background, and other demographics.”
Funding for this research was provided to Cancer Trials Ireland by Amgen, Abbvie, Bayor, and Inveva. ![]()
MADRID—Results of a nationwide study suggest many cancer patients in Ireland don’t understand key aspects of clinical trial methodology.
Most of the patients surveyed, which included individuals who had participated in a clinical trial, did not understand the concepts of randomization or equipoise.
“Over half of previous medical trial participants and 73% of those who had never been on a cancer clinical trial did not understand that, in a randomized trial, the treatment given was decided by chance,” said study investigator Catherine Kelly, MB BCh, of Mater Misericordiae University Hospital in Dublin, Ireland.
“We also found that most patients did not understand clinical equipoise—the fact that no one knows which treatment is best. Surprisingly, this was more marked in previous clinical trial participants, 60% of whom believed that their doctor would know which study arm was best.”
Dr Kelly and her colleagues presented these findings at the ESMO 2017 Congress (abstract 1465P_PR).
The researchers surveyed 1090 adult cancer patients treated at 1 of 14 participating oncology centers across Ireland.
The patients’ median age was 60 (range, 50-69), 64.4% were female, and 66% were diagnosed between 2014 and 2016. The most common cancer types were breast (31.4%), colorectal (15.6%), hematologic (12.6%), genitourinary (11.6%), and lung (6.8%).
The patients filled out anonymized questionnaires in which they were asked to evaluate statements about clinical trials. The patients had to determine whether a statement is true or false, or they could indicate that they didn’t know an answer.
A majority of the patients (82.3%) said they understood what a medical or cancer clinical trial is. And 27.8% of patients said they had previously participated in a cancer trial.
However, many patients didn’t know when clinical trials may be an option. Twenty-two percent of patients said it is true that “clinical trials are only used when standard treatments have not worked,” and 26.6% said they didn’t know if this statement is true or false.
Roughly a third (33.5%) of patients said it is true that, in a randomized trial, treatment is decided by chance, but 41.4% of patients said this is false, and 25% said they didn’t know.
More than half of patients (56.5%) said their doctor would know which treatment was superior in a clinical trial, and 23.2% of patients said they didn’t know if their doctor would know.
About 61% of all patients said their doctor would make sure they received the superior treatment in a clinical trial. An even greater percentage—63.6%—of patients who had previously participated in a clinical trial said the same.
“To provide informed consent when participating in a trial, patients need to understand these key concepts, and doctors explaining them well is essential to alleviating any fears that might prevent patients from participating,” Dr Kelly said.
“Doctors have a responsibility to properly inform their patients in this regard because they are the ones patients trust the most. As we analyze the data further, we will be able to offer physicians a more detailed picture of the questions patients need answered and the factors that influence their decision-making according to age group, cancer type, educational background, and other demographics.”
Funding for this research was provided to Cancer Trials Ireland by Amgen, Abbvie, Bayor, and Inveva. ![]()
MADRID—Results of a nationwide study suggest many cancer patients in Ireland don’t understand key aspects of clinical trial methodology.
Most of the patients surveyed, which included individuals who had participated in a clinical trial, did not understand the concepts of randomization or equipoise.
“Over half of previous medical trial participants and 73% of those who had never been on a cancer clinical trial did not understand that, in a randomized trial, the treatment given was decided by chance,” said study investigator Catherine Kelly, MB BCh, of Mater Misericordiae University Hospital in Dublin, Ireland.
“We also found that most patients did not understand clinical equipoise—the fact that no one knows which treatment is best. Surprisingly, this was more marked in previous clinical trial participants, 60% of whom believed that their doctor would know which study arm was best.”
Dr Kelly and her colleagues presented these findings at the ESMO 2017 Congress (abstract 1465P_PR).
The researchers surveyed 1090 adult cancer patients treated at 1 of 14 participating oncology centers across Ireland.
The patients’ median age was 60 (range, 50-69), 64.4% were female, and 66% were diagnosed between 2014 and 2016. The most common cancer types were breast (31.4%), colorectal (15.6%), hematologic (12.6%), genitourinary (11.6%), and lung (6.8%).
The patients filled out anonymized questionnaires in which they were asked to evaluate statements about clinical trials. The patients had to determine whether a statement is true or false, or they could indicate that they didn’t know an answer.
A majority of the patients (82.3%) said they understood what a medical or cancer clinical trial is. And 27.8% of patients said they had previously participated in a cancer trial.
However, many patients didn’t know when clinical trials may be an option. Twenty-two percent of patients said it is true that “clinical trials are only used when standard treatments have not worked,” and 26.6% said they didn’t know if this statement is true or false.
Roughly a third (33.5%) of patients said it is true that, in a randomized trial, treatment is decided by chance, but 41.4% of patients said this is false, and 25% said they didn’t know.
More than half of patients (56.5%) said their doctor would know which treatment was superior in a clinical trial, and 23.2% of patients said they didn’t know if their doctor would know.
About 61% of all patients said their doctor would make sure they received the superior treatment in a clinical trial. An even greater percentage—63.6%—of patients who had previously participated in a clinical trial said the same.
“To provide informed consent when participating in a trial, patients need to understand these key concepts, and doctors explaining them well is essential to alleviating any fears that might prevent patients from participating,” Dr Kelly said.
“Doctors have a responsibility to properly inform their patients in this regard because they are the ones patients trust the most. As we analyze the data further, we will be able to offer physicians a more detailed picture of the questions patients need answered and the factors that influence their decision-making according to age group, cancer type, educational background, and other demographics.”
Funding for this research was provided to Cancer Trials Ireland by Amgen, Abbvie, Bayor, and Inveva. ![]()
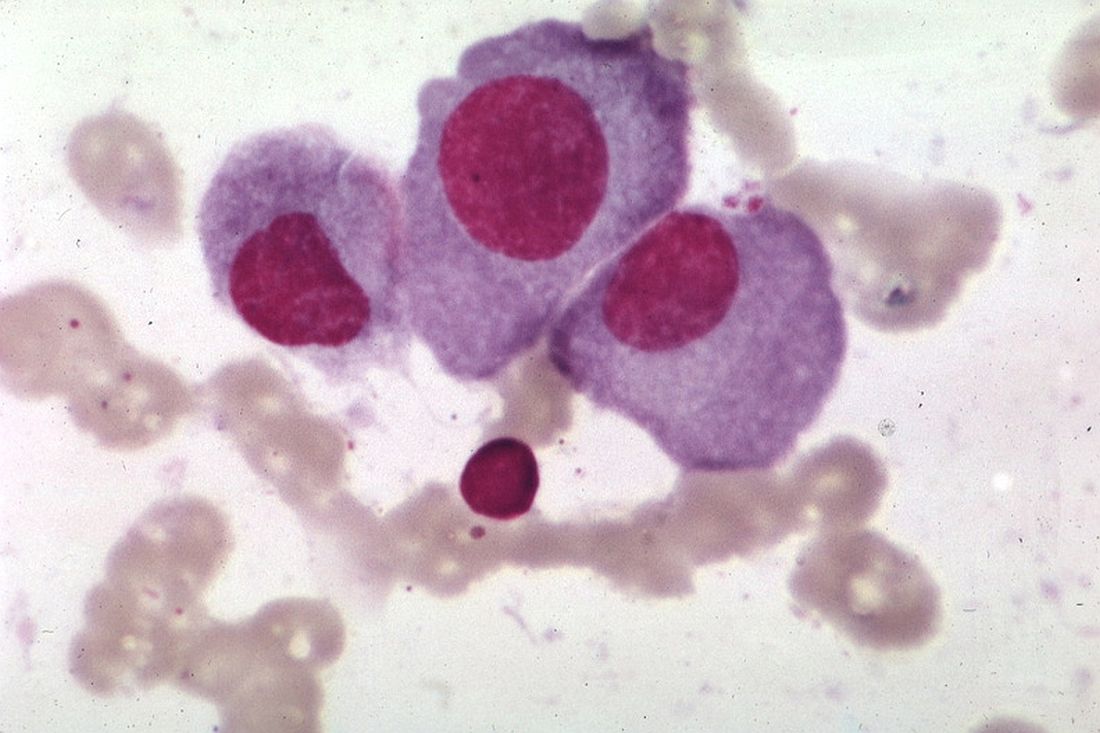
FDA places full, partial holds on durvalumab trials
The US Food and Drug Administration (FDA) has placed a partial clinical hold on 5 trials and a full clinical hold on 1 trial of the anti-PD-L1 antibody durvalumab (Imfinzi™).
In these trials, researchers are testing durvalumab in combination with immunomodulatory and chemotherapy agents in patients with multiple myeloma (MM) and lymphomas.
At present, no new patients can be enrolled in any of the 6 trials.
Patients enrolled in the trials on partial clinical hold can remain on treatment if they are receiving clinical benefit.
Patients enrolled in the trial on full clinical hold will discontinue the study treatment.
The FDA’s decision to place these trials on hold is related to risks identified in trials studying another anti-PD-1 agent, pembrolizumab, in MM patients.
Data from the pembrolizumab trials indicate the risks outweigh the benefits when PD-1/PD-L1 treatment is given to MM patients in combination with dexamethasone and pomalidomide or lenalidomide.
In addition, there may be an unfavorable risk-benefit ratio for MM patients receiving PD-1/PD-L1 treatments alone or in other combinations.
With this in mind, the FDA placed the MEDI4736-MM-002 trial on full clinical hold.
MEDI4736-MM-002 is a phase 1b study designed to determine the recommended dose and regimen of durvalumab in combination with lenalidomide, with and without low-dose dexamethasone, in patients with newly diagnosed MM.
The FDA also placed the following trials on partial clinical hold:
- MEDI4736-MM-001: A phase 1b study to determine the recommended dose and regimen of durvalumab either as monotherapy or in combination with pomalidomide, with or without low-dose dexamethasone, in patients with relapsed and refractory MM
- MEDI4736-MM-003: A phase 2 study to determine the safety and efficacy of the combination of durvalumab and daratumumab in patients with relapsed and refractory MM
- MEDI4736-MM-005: A phase 2 study to determine the efficacy of the combination of durvalumab plus daratumumab in patients with relapsed and refractory MM who have progressed while on a current treatment regimen containing daratumumab
- MEDI4736-NHL-001: A phase 1/2 study to assess the safety and tolerability of durvalumab as monotherapy and in combination therapy in patients with lymphomas, including chronic lymphocytic leukemia. The only arm in this trial for which enrollment is suspended is the arm with the durvalumab, lenalidomide, and rituximab combination.
- MEDI4736-DLBCL-001: A phase 2 study to evaluate the safety and clinical activity of durvalumab in combination with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) or with lenalidomide plus R-CHOP in patients with previously untreated, high-risk diffuse large B-cell lymphoma.
The trials that will continue to enroll are:
- MEDI4736-MDS-001: A phase 2 study evaluating the efficacy and safety of subcutaneous azacitidine in combination with durvalumab in previously untreated patients with higher-risk myelodysplastic syndromes or in elderly (≥65 years) acute myeloid leukemia patients not eligible for hematopoietic stem cell transplant
- CC-486-MDS-006: A phase 2 study to evaluate the efficacy and safety of CC-486 alone or in combination with durvalumab in patients with myelodysplastic syndromes who fail to achieve an objective response to treatment with azacitidine for injection or decitabine.
Durvalumab is being developed by Celgene Corporation and MedImmune, the global biologics research and development arm of AstraZeneca.
The use of durvalumab in combination with other agents for the treatment of patients with hematologic malignancies is not approved by the FDA, and the safety and efficacy of those combinations has not been established.
Durvalumab has accelerated approval from the FDA to treat patients with locally advanced or metastatic urothelial carcinoma. ![]()
The US Food and Drug Administration (FDA) has placed a partial clinical hold on 5 trials and a full clinical hold on 1 trial of the anti-PD-L1 antibody durvalumab (Imfinzi™).
In these trials, researchers are testing durvalumab in combination with immunomodulatory and chemotherapy agents in patients with multiple myeloma (MM) and lymphomas.
At present, no new patients can be enrolled in any of the 6 trials.
Patients enrolled in the trials on partial clinical hold can remain on treatment if they are receiving clinical benefit.
Patients enrolled in the trial on full clinical hold will discontinue the study treatment.
The FDA’s decision to place these trials on hold is related to risks identified in trials studying another anti-PD-1 agent, pembrolizumab, in MM patients.
Data from the pembrolizumab trials indicate the risks outweigh the benefits when PD-1/PD-L1 treatment is given to MM patients in combination with dexamethasone and pomalidomide or lenalidomide.
In addition, there may be an unfavorable risk-benefit ratio for MM patients receiving PD-1/PD-L1 treatments alone or in other combinations.
With this in mind, the FDA placed the MEDI4736-MM-002 trial on full clinical hold.
MEDI4736-MM-002 is a phase 1b study designed to determine the recommended dose and regimen of durvalumab in combination with lenalidomide, with and without low-dose dexamethasone, in patients with newly diagnosed MM.
The FDA also placed the following trials on partial clinical hold:
- MEDI4736-MM-001: A phase 1b study to determine the recommended dose and regimen of durvalumab either as monotherapy or in combination with pomalidomide, with or without low-dose dexamethasone, in patients with relapsed and refractory MM
- MEDI4736-MM-003: A phase 2 study to determine the safety and efficacy of the combination of durvalumab and daratumumab in patients with relapsed and refractory MM
- MEDI4736-MM-005: A phase 2 study to determine the efficacy of the combination of durvalumab plus daratumumab in patients with relapsed and refractory MM who have progressed while on a current treatment regimen containing daratumumab
- MEDI4736-NHL-001: A phase 1/2 study to assess the safety and tolerability of durvalumab as monotherapy and in combination therapy in patients with lymphomas, including chronic lymphocytic leukemia. The only arm in this trial for which enrollment is suspended is the arm with the durvalumab, lenalidomide, and rituximab combination.
- MEDI4736-DLBCL-001: A phase 2 study to evaluate the safety and clinical activity of durvalumab in combination with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) or with lenalidomide plus R-CHOP in patients with previously untreated, high-risk diffuse large B-cell lymphoma.
The trials that will continue to enroll are:
- MEDI4736-MDS-001: A phase 2 study evaluating the efficacy and safety of subcutaneous azacitidine in combination with durvalumab in previously untreated patients with higher-risk myelodysplastic syndromes or in elderly (≥65 years) acute myeloid leukemia patients not eligible for hematopoietic stem cell transplant
- CC-486-MDS-006: A phase 2 study to evaluate the efficacy and safety of CC-486 alone or in combination with durvalumab in patients with myelodysplastic syndromes who fail to achieve an objective response to treatment with azacitidine for injection or decitabine.
Durvalumab is being developed by Celgene Corporation and MedImmune, the global biologics research and development arm of AstraZeneca.
The use of durvalumab in combination with other agents for the treatment of patients with hematologic malignancies is not approved by the FDA, and the safety and efficacy of those combinations has not been established.
Durvalumab has accelerated approval from the FDA to treat patients with locally advanced or metastatic urothelial carcinoma. ![]()
The US Food and Drug Administration (FDA) has placed a partial clinical hold on 5 trials and a full clinical hold on 1 trial of the anti-PD-L1 antibody durvalumab (Imfinzi™).
In these trials, researchers are testing durvalumab in combination with immunomodulatory and chemotherapy agents in patients with multiple myeloma (MM) and lymphomas.
At present, no new patients can be enrolled in any of the 6 trials.
Patients enrolled in the trials on partial clinical hold can remain on treatment if they are receiving clinical benefit.
Patients enrolled in the trial on full clinical hold will discontinue the study treatment.
The FDA’s decision to place these trials on hold is related to risks identified in trials studying another anti-PD-1 agent, pembrolizumab, in MM patients.
Data from the pembrolizumab trials indicate the risks outweigh the benefits when PD-1/PD-L1 treatment is given to MM patients in combination with dexamethasone and pomalidomide or lenalidomide.
In addition, there may be an unfavorable risk-benefit ratio for MM patients receiving PD-1/PD-L1 treatments alone or in other combinations.
With this in mind, the FDA placed the MEDI4736-MM-002 trial on full clinical hold.
MEDI4736-MM-002 is a phase 1b study designed to determine the recommended dose and regimen of durvalumab in combination with lenalidomide, with and without low-dose dexamethasone, in patients with newly diagnosed MM.
The FDA also placed the following trials on partial clinical hold:
- MEDI4736-MM-001: A phase 1b study to determine the recommended dose and regimen of durvalumab either as monotherapy or in combination with pomalidomide, with or without low-dose dexamethasone, in patients with relapsed and refractory MM
- MEDI4736-MM-003: A phase 2 study to determine the safety and efficacy of the combination of durvalumab and daratumumab in patients with relapsed and refractory MM
- MEDI4736-MM-005: A phase 2 study to determine the efficacy of the combination of durvalumab plus daratumumab in patients with relapsed and refractory MM who have progressed while on a current treatment regimen containing daratumumab
- MEDI4736-NHL-001: A phase 1/2 study to assess the safety and tolerability of durvalumab as monotherapy and in combination therapy in patients with lymphomas, including chronic lymphocytic leukemia. The only arm in this trial for which enrollment is suspended is the arm with the durvalumab, lenalidomide, and rituximab combination.
- MEDI4736-DLBCL-001: A phase 2 study to evaluate the safety and clinical activity of durvalumab in combination with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) or with lenalidomide plus R-CHOP in patients with previously untreated, high-risk diffuse large B-cell lymphoma.
The trials that will continue to enroll are:
- MEDI4736-MDS-001: A phase 2 study evaluating the efficacy and safety of subcutaneous azacitidine in combination with durvalumab in previously untreated patients with higher-risk myelodysplastic syndromes or in elderly (≥65 years) acute myeloid leukemia patients not eligible for hematopoietic stem cell transplant
- CC-486-MDS-006: A phase 2 study to evaluate the efficacy and safety of CC-486 alone or in combination with durvalumab in patients with myelodysplastic syndromes who fail to achieve an objective response to treatment with azacitidine for injection or decitabine.
Durvalumab is being developed by Celgene Corporation and MedImmune, the global biologics research and development arm of AstraZeneca.
The use of durvalumab in combination with other agents for the treatment of patients with hematologic malignancies is not approved by the FDA, and the safety and efficacy of those combinations has not been established.
Durvalumab has accelerated approval from the FDA to treat patients with locally advanced or metastatic urothelial carcinoma. ![]()
FDA places partial hold on trials of nivolumab in MM
The US Food and Drug Administration (FDA) has placed a partial clinical hold on 3 trials of the PD-1 immune checkpoint inhibitor nivolumab (Opdivo).
The trials were designed to investigate nivolumab-based combination regimens in patients with relapsed or refractory multiple myeloma (MM).
The partial clinical hold means patients currently enrolled in these 3 trials can continue treatment if they are experiencing clinical benefit. However, no new patients can be enrolled at this time.
The partial clinical hold is related to risks identified in trials studying another anti-PD-1 agent, pembrolizumab, in MM patients.
Data from the pembrolizumab trials indicate the risks outweigh the benefits when PD-1/PD-L1 treatment is given to MM patients in combination with dexamethasone and pomalidomide or lenalidomide.
In addition, there may be an unfavorable risk-benefit ratio for MM patients receiving PD-1/PD-L1 treatments alone or in other combinations.
With this in mind, the FDA placed the partial hold on the following nivolumab trials:
- CheckMate-602: A randomized, phase 3 trial of combinations of nivolumab, elotuzumab, pomalidomide, and dexamethasone in relapsed and refractory MM
- CheckMate-039: A phase 1 study intended to establish the tolerability of nivolumab and the combination of nivolumab and daratumumab, with or without pomalidomide and dexamethasone, in patients with relapsed or refractory MM
- CA204142: A phase 2 study of elotuzumab in combination with pomalidomide and low-dose dexamethasone, and in combination with nivolumab, in patients with MM who relapsed after or were refractory to prior treatment with lenalidomide.
Other studies of nivolumab will continue as planned.
Bristol-Myers Squibb, the company developing and marketing nivolumab, said it remains steadfast in its commitment to improve outcomes for MM patients and will work closely with the FDA to address concerns.
Nivolumab is currently FDA-approved to treat:
- Adults with classical Hodgkin lymphoma that has relapsed or progressed after autologous hematopoietic stem cell transplant and brentuximab vedotin or after 3 or more lines of therapy, including autologous transplant
- Patients with previously treated metastatic non-small cell lung cancer
- Metastatic melanoma patients
- Advanced renal cell carcinoma patients who received prior anti-angiogenic therapy
- Patients with recurrent or metastatic squamous cell carcinoma of the head and neck on or after platinum-based therapy
- Patients with previously treated locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-based chemotherapy
- Patients (≥12 years) with microsatellite instability high or mismatch repair-deficient metastatic colorectal cancer that has progressed following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.

The US Food and Drug Administration (FDA) has placed a partial clinical hold on 3 trials of the PD-1 immune checkpoint inhibitor nivolumab (Opdivo).
The trials were designed to investigate nivolumab-based combination regimens in patients with relapsed or refractory multiple myeloma (MM).
The partial clinical hold means patients currently enrolled in these 3 trials can continue treatment if they are experiencing clinical benefit. However, no new patients can be enrolled at this time.
The partial clinical hold is related to risks identified in trials studying another anti-PD-1 agent, pembrolizumab, in MM patients.
Data from the pembrolizumab trials indicate the risks outweigh the benefits when PD-1/PD-L1 treatment is given to MM patients in combination with dexamethasone and pomalidomide or lenalidomide.
In addition, there may be an unfavorable risk-benefit ratio for MM patients receiving PD-1/PD-L1 treatments alone or in other combinations.
With this in mind, the FDA placed the partial hold on the following nivolumab trials:
- CheckMate-602: A randomized, phase 3 trial of combinations of nivolumab, elotuzumab, pomalidomide, and dexamethasone in relapsed and refractory MM
- CheckMate-039: A phase 1 study intended to establish the tolerability of nivolumab and the combination of nivolumab and daratumumab, with or without pomalidomide and dexamethasone, in patients with relapsed or refractory MM
- CA204142: A phase 2 study of elotuzumab in combination with pomalidomide and low-dose dexamethasone, and in combination with nivolumab, in patients with MM who relapsed after or were refractory to prior treatment with lenalidomide.
Other studies of nivolumab will continue as planned.
Bristol-Myers Squibb, the company developing and marketing nivolumab, said it remains steadfast in its commitment to improve outcomes for MM patients and will work closely with the FDA to address concerns.
Nivolumab is currently FDA-approved to treat:
- Adults with classical Hodgkin lymphoma that has relapsed or progressed after autologous hematopoietic stem cell transplant and brentuximab vedotin or after 3 or more lines of therapy, including autologous transplant
- Patients with previously treated metastatic non-small cell lung cancer
- Metastatic melanoma patients
- Advanced renal cell carcinoma patients who received prior anti-angiogenic therapy
- Patients with recurrent or metastatic squamous cell carcinoma of the head and neck on or after platinum-based therapy
- Patients with previously treated locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-based chemotherapy
- Patients (≥12 years) with microsatellite instability high or mismatch repair-deficient metastatic colorectal cancer that has progressed following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.

The US Food and Drug Administration (FDA) has placed a partial clinical hold on 3 trials of the PD-1 immune checkpoint inhibitor nivolumab (Opdivo).
The trials were designed to investigate nivolumab-based combination regimens in patients with relapsed or refractory multiple myeloma (MM).
The partial clinical hold means patients currently enrolled in these 3 trials can continue treatment if they are experiencing clinical benefit. However, no new patients can be enrolled at this time.
The partial clinical hold is related to risks identified in trials studying another anti-PD-1 agent, pembrolizumab, in MM patients.
Data from the pembrolizumab trials indicate the risks outweigh the benefits when PD-1/PD-L1 treatment is given to MM patients in combination with dexamethasone and pomalidomide or lenalidomide.
In addition, there may be an unfavorable risk-benefit ratio for MM patients receiving PD-1/PD-L1 treatments alone or in other combinations.
With this in mind, the FDA placed the partial hold on the following nivolumab trials:
- CheckMate-602: A randomized, phase 3 trial of combinations of nivolumab, elotuzumab, pomalidomide, and dexamethasone in relapsed and refractory MM
- CheckMate-039: A phase 1 study intended to establish the tolerability of nivolumab and the combination of nivolumab and daratumumab, with or without pomalidomide and dexamethasone, in patients with relapsed or refractory MM
- CA204142: A phase 2 study of elotuzumab in combination with pomalidomide and low-dose dexamethasone, and in combination with nivolumab, in patients with MM who relapsed after or were refractory to prior treatment with lenalidomide.
Other studies of nivolumab will continue as planned.
Bristol-Myers Squibb, the company developing and marketing nivolumab, said it remains steadfast in its commitment to improve outcomes for MM patients and will work closely with the FDA to address concerns.
Nivolumab is currently FDA-approved to treat:
- Adults with classical Hodgkin lymphoma that has relapsed or progressed after autologous hematopoietic stem cell transplant and brentuximab vedotin or after 3 or more lines of therapy, including autologous transplant
- Patients with previously treated metastatic non-small cell lung cancer
- Metastatic melanoma patients
- Advanced renal cell carcinoma patients who received prior anti-angiogenic therapy
- Patients with recurrent or metastatic squamous cell carcinoma of the head and neck on or after platinum-based therapy
- Patients with previously treated locally advanced or metastatic urothelial carcinoma who have disease progression during or following platinum-based chemotherapy
- Patients (≥12 years) with microsatellite instability high or mismatch repair-deficient metastatic colorectal cancer that has progressed following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.

FDA grants orphan designation to product for CMV
The US Food and Drug Administration (FDA) has granted orphan drug designation to ATA230 for the treatment of cytomegalovirus (CMV) viremia and disease in immunocompromised patients.
ATA230 is an allogeneic, cytotoxic T-lymphocyte (CTL) product targeting antigens expressed by CMV.
The product is under investigation in phase 2 trials of patients with CMV viremia and disease who are refractory or resistant to antiviral treatment.
Atara Biotherapeutics, Inc., the company developing ATA230, said it will evaluate development plans for this therapy with the FDA and other global health authorities after beginning phase 3 studies of another product, ATA129.
The company said it decided to prioritize ATA129, which is being developed to treat patients with Epstein-Barr-virus-associated post-transplant lymphoproliferative disorder.
Phase 2 trial of ATA230
Researchers reported phase 2 results with ATA230 at the 2016 ASH Annual Meeting.
The data encompassed 15 patients with documented CMV mutations conferring resistance to antiviral therapies. The patients had received a median of 3 prior therapies.
Eleven of the 15 patients (73.3%) responded to ATA230, 6 with complete responses and 5 with partial responses.
At 6 months, the overall survival was 72.7% in responders and 25% in non-responders.
Within the 6 months of follow-up, 1 of the 11 responders died of CMV, and 3 of the 4 non-responders died of CMV.
Adverse events occurred in 6 patients. One grade 3 event and 1 grade 4 event were considered possibly related to ATA230.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to ATA230 for the treatment of cytomegalovirus (CMV) viremia and disease in immunocompromised patients.
ATA230 is an allogeneic, cytotoxic T-lymphocyte (CTL) product targeting antigens expressed by CMV.
The product is under investigation in phase 2 trials of patients with CMV viremia and disease who are refractory or resistant to antiviral treatment.
Atara Biotherapeutics, Inc., the company developing ATA230, said it will evaluate development plans for this therapy with the FDA and other global health authorities after beginning phase 3 studies of another product, ATA129.
The company said it decided to prioritize ATA129, which is being developed to treat patients with Epstein-Barr-virus-associated post-transplant lymphoproliferative disorder.
Phase 2 trial of ATA230
Researchers reported phase 2 results with ATA230 at the 2016 ASH Annual Meeting.
The data encompassed 15 patients with documented CMV mutations conferring resistance to antiviral therapies. The patients had received a median of 3 prior therapies.
Eleven of the 15 patients (73.3%) responded to ATA230, 6 with complete responses and 5 with partial responses.
At 6 months, the overall survival was 72.7% in responders and 25% in non-responders.
Within the 6 months of follow-up, 1 of the 11 responders died of CMV, and 3 of the 4 non-responders died of CMV.
Adverse events occurred in 6 patients. One grade 3 event and 1 grade 4 event were considered possibly related to ATA230.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to ATA230 for the treatment of cytomegalovirus (CMV) viremia and disease in immunocompromised patients.
ATA230 is an allogeneic, cytotoxic T-lymphocyte (CTL) product targeting antigens expressed by CMV.
The product is under investigation in phase 2 trials of patients with CMV viremia and disease who are refractory or resistant to antiviral treatment.
Atara Biotherapeutics, Inc., the company developing ATA230, said it will evaluate development plans for this therapy with the FDA and other global health authorities after beginning phase 3 studies of another product, ATA129.
The company said it decided to prioritize ATA129, which is being developed to treat patients with Epstein-Barr-virus-associated post-transplant lymphoproliferative disorder.
Phase 2 trial of ATA230
Researchers reported phase 2 results with ATA230 at the 2016 ASH Annual Meeting.
The data encompassed 15 patients with documented CMV mutations conferring resistance to antiviral therapies. The patients had received a median of 3 prior therapies.
Eleven of the 15 patients (73.3%) responded to ATA230, 6 with complete responses and 5 with partial responses.
At 6 months, the overall survival was 72.7% in responders and 25% in non-responders.
Within the 6 months of follow-up, 1 of the 11 responders died of CMV, and 3 of the 4 non-responders died of CMV.
Adverse events occurred in 6 patients. One grade 3 event and 1 grade 4 event were considered possibly related to ATA230.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
FDA grants orphan designation to product for GVHD
The US Food and Drug Administration (FDA) has granted orphan drug designation to ApoGraft™ as prophylaxis for acute and chronic graft-versus-host disease (GVHD) in transplant recipients.
ApoGraft is a mobilized peripheral blood cell product collected via apheresis from a matched, related donor. The product is exposed to the apoptotic mediator Fas ligand prior to transplantation.
ApoGraft was designed to eliminate immune responses after transplantation of foreign cells and tissues.
ApoGraft is being developed by Cellect Biotechnology Ltd.
The company is testing ApoGraft as acute GVHD prophylaxis in a phase 1/2 trial.
The trial is currently enrolling patients with hemato-oncology disorders who are eligible for allogeneic, HLA-matched hematopoietic stem cell transplant (HSCT).
The study is expected to have 4 cohorts, each consisting of 3 patients.
The difference between the cohorts is the amount of apoptotic mediator Fas ligand (APO010) to which the graft is exposed during incubation prior to ApoGraft transplantation and HSCT:
- 10 ng/mL APO010 in Cohort 1
- 25 ng/mL APO010 in Cohort 2
- 50 ng/mL APO010 in Cohort 3
- 100 ng/mL APO010 in Cohort 4.
The study is expected to progress from one cohort to the next based on an independent data safety monitoring board review and analysis of safety data.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to ApoGraft™ as prophylaxis for acute and chronic graft-versus-host disease (GVHD) in transplant recipients.
ApoGraft is a mobilized peripheral blood cell product collected via apheresis from a matched, related donor. The product is exposed to the apoptotic mediator Fas ligand prior to transplantation.
ApoGraft was designed to eliminate immune responses after transplantation of foreign cells and tissues.
ApoGraft is being developed by Cellect Biotechnology Ltd.
The company is testing ApoGraft as acute GVHD prophylaxis in a phase 1/2 trial.
The trial is currently enrolling patients with hemato-oncology disorders who are eligible for allogeneic, HLA-matched hematopoietic stem cell transplant (HSCT).
The study is expected to have 4 cohorts, each consisting of 3 patients.
The difference between the cohorts is the amount of apoptotic mediator Fas ligand (APO010) to which the graft is exposed during incubation prior to ApoGraft transplantation and HSCT:
- 10 ng/mL APO010 in Cohort 1
- 25 ng/mL APO010 in Cohort 2
- 50 ng/mL APO010 in Cohort 3
- 100 ng/mL APO010 in Cohort 4.
The study is expected to progress from one cohort to the next based on an independent data safety monitoring board review and analysis of safety data.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to ApoGraft™ as prophylaxis for acute and chronic graft-versus-host disease (GVHD) in transplant recipients.
ApoGraft is a mobilized peripheral blood cell product collected via apheresis from a matched, related donor. The product is exposed to the apoptotic mediator Fas ligand prior to transplantation.
ApoGraft was designed to eliminate immune responses after transplantation of foreign cells and tissues.
ApoGraft is being developed by Cellect Biotechnology Ltd.
The company is testing ApoGraft as acute GVHD prophylaxis in a phase 1/2 trial.
The trial is currently enrolling patients with hemato-oncology disorders who are eligible for allogeneic, HLA-matched hematopoietic stem cell transplant (HSCT).
The study is expected to have 4 cohorts, each consisting of 3 patients.
The difference between the cohorts is the amount of apoptotic mediator Fas ligand (APO010) to which the graft is exposed during incubation prior to ApoGraft transplantation and HSCT:
- 10 ng/mL APO010 in Cohort 1
- 25 ng/mL APO010 in Cohort 2
- 50 ng/mL APO010 in Cohort 3
- 100 ng/mL APO010 in Cohort 4.
The study is expected to progress from one cohort to the next based on an independent data safety monitoring board review and analysis of safety data.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
FDA warns about risk of death with pembrolizumab in MM
The US Food and Drug Administration (FDA) has issued a statement warning about an increased risk of death associated with an unapproved use of pembrolizumab (Keytruda).
Results from 2 clinical trials have shown that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with multiple myeloma (MM).
The FDA issued its statement to remind doctors and patients that pembrolizumab is not approved to treat MM and should not be given in combination with immunomodulatory agents to treat MM.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, and microsatellite instability-high cancer.
The FDA believes the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks, according to Janet Woodcock, director of the FDA’s Center for Drug Evaluation and Research.
However, the FDA is investigating trials of pembrolizumab as well as trials of other PD-1/PD-L1 inhibitors.
Pembrolizumab in MM
The FDA’s warning is based on a review of data from 2 clinical trials—KEYNOTE-183 and KEYNOTE-185. The FDA placed a clinical hold on these trials—as well as KEYNOTE-023—in July.
KEYNOTE-183 is a phase 3 study of pomalidomide and low-dose dexamethasone, given with or without pembrolizumab, to patients with refractory or relapsed and refractory MM.
KEYNOTE-185 is a phase 3 study of lenalidomide and low-dose dexamethasone, given with or without pembrolizumab, to patients with newly diagnosed and treatment-naïve MM.
KEYNOTE-023 is a phase 1 trial of pembrolizumab in combination with backbone treatments. Cohort 1 of this trial was designed to evaluate pembrolizumab in combination with lenalidomide and dexamethasone in MM patients who received prior treatment with an immunomodulatory agent (lenalidomide, pomalidomide, or thalidomide).
Interim results from KEYNOTE-183 and KEYNOTE-185 revealed an increased risk of death for patients receiving pembrolizumab, when compared to patients receiving the control therapies.
Merck & Co., Inc., the company developing pembrolizumab, was informed of this risk by an external data monitoring committee. The company suspended enrollment in the trials and notified the FDA of the issue in June.
The following month, the FDA announced that all patients enrolled in KEYNOTE-183 and KEYNOTE-185, as well as patients in the pembrolizumab/lenalidomide/dexamethasone cohort of KEYNOTE-023, would discontinue investigational treatment with pembrolizumab.
FDA investigation
The FDA is examining data from the pembrolizumab trials and working with Merck to better understand the cause of the safety concerns, according to Woodcock.
The agency is also working with sponsors of other PD-1/PD-L1 inhibitors to examine other trials in which these drugs are being studied in combination with immunomodulatory agents and trials in which the inhibitors are being studied in combination with other classes of drugs in patients with hematologic malignancies.
Woodcock said the FDA will take appropriate action as warranted to ensure patients enrolled in these trials are protected and that doctors and researchers understand the risks associated with this investigational use.
The agency is also encouraging healthcare professionals and consumers to report any adverse events or side effects related to the use of pembrolizumab and other PD-1/PD-L1 inhibitors to FDA’s MedWatch Adverse Event Reporting Program.
The US Food and Drug Administration (FDA) has issued a statement warning about an increased risk of death associated with an unapproved use of pembrolizumab (Keytruda).
Results from 2 clinical trials have shown that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with multiple myeloma (MM).
The FDA issued its statement to remind doctors and patients that pembrolizumab is not approved to treat MM and should not be given in combination with immunomodulatory agents to treat MM.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, and microsatellite instability-high cancer.
The FDA believes the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks, according to Janet Woodcock, director of the FDA’s Center for Drug Evaluation and Research.
However, the FDA is investigating trials of pembrolizumab as well as trials of other PD-1/PD-L1 inhibitors.
Pembrolizumab in MM
The FDA’s warning is based on a review of data from 2 clinical trials—KEYNOTE-183 and KEYNOTE-185. The FDA placed a clinical hold on these trials—as well as KEYNOTE-023—in July.
KEYNOTE-183 is a phase 3 study of pomalidomide and low-dose dexamethasone, given with or without pembrolizumab, to patients with refractory or relapsed and refractory MM.
KEYNOTE-185 is a phase 3 study of lenalidomide and low-dose dexamethasone, given with or without pembrolizumab, to patients with newly diagnosed and treatment-naïve MM.
KEYNOTE-023 is a phase 1 trial of pembrolizumab in combination with backbone treatments. Cohort 1 of this trial was designed to evaluate pembrolizumab in combination with lenalidomide and dexamethasone in MM patients who received prior treatment with an immunomodulatory agent (lenalidomide, pomalidomide, or thalidomide).
Interim results from KEYNOTE-183 and KEYNOTE-185 revealed an increased risk of death for patients receiving pembrolizumab, when compared to patients receiving the control therapies.
Merck & Co., Inc., the company developing pembrolizumab, was informed of this risk by an external data monitoring committee. The company suspended enrollment in the trials and notified the FDA of the issue in June.
The following month, the FDA announced that all patients enrolled in KEYNOTE-183 and KEYNOTE-185, as well as patients in the pembrolizumab/lenalidomide/dexamethasone cohort of KEYNOTE-023, would discontinue investigational treatment with pembrolizumab.
FDA investigation
The FDA is examining data from the pembrolizumab trials and working with Merck to better understand the cause of the safety concerns, according to Woodcock.
The agency is also working with sponsors of other PD-1/PD-L1 inhibitors to examine other trials in which these drugs are being studied in combination with immunomodulatory agents and trials in which the inhibitors are being studied in combination with other classes of drugs in patients with hematologic malignancies.
Woodcock said the FDA will take appropriate action as warranted to ensure patients enrolled in these trials are protected and that doctors and researchers understand the risks associated with this investigational use.
The agency is also encouraging healthcare professionals and consumers to report any adverse events or side effects related to the use of pembrolizumab and other PD-1/PD-L1 inhibitors to FDA’s MedWatch Adverse Event Reporting Program.
The US Food and Drug Administration (FDA) has issued a statement warning about an increased risk of death associated with an unapproved use of pembrolizumab (Keytruda).
Results from 2 clinical trials have shown that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with multiple myeloma (MM).
The FDA issued its statement to remind doctors and patients that pembrolizumab is not approved to treat MM and should not be given in combination with immunomodulatory agents to treat MM.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, and microsatellite instability-high cancer.
The FDA believes the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks, according to Janet Woodcock, director of the FDA’s Center for Drug Evaluation and Research.
However, the FDA is investigating trials of pembrolizumab as well as trials of other PD-1/PD-L1 inhibitors.
Pembrolizumab in MM
The FDA’s warning is based on a review of data from 2 clinical trials—KEYNOTE-183 and KEYNOTE-185. The FDA placed a clinical hold on these trials—as well as KEYNOTE-023—in July.
KEYNOTE-183 is a phase 3 study of pomalidomide and low-dose dexamethasone, given with or without pembrolizumab, to patients with refractory or relapsed and refractory MM.
KEYNOTE-185 is a phase 3 study of lenalidomide and low-dose dexamethasone, given with or without pembrolizumab, to patients with newly diagnosed and treatment-naïve MM.
KEYNOTE-023 is a phase 1 trial of pembrolizumab in combination with backbone treatments. Cohort 1 of this trial was designed to evaluate pembrolizumab in combination with lenalidomide and dexamethasone in MM patients who received prior treatment with an immunomodulatory agent (lenalidomide, pomalidomide, or thalidomide).
Interim results from KEYNOTE-183 and KEYNOTE-185 revealed an increased risk of death for patients receiving pembrolizumab, when compared to patients receiving the control therapies.
Merck & Co., Inc., the company developing pembrolizumab, was informed of this risk by an external data monitoring committee. The company suspended enrollment in the trials and notified the FDA of the issue in June.
The following month, the FDA announced that all patients enrolled in KEYNOTE-183 and KEYNOTE-185, as well as patients in the pembrolizumab/lenalidomide/dexamethasone cohort of KEYNOTE-023, would discontinue investigational treatment with pembrolizumab.
FDA investigation
The FDA is examining data from the pembrolizumab trials and working with Merck to better understand the cause of the safety concerns, according to Woodcock.
The agency is also working with sponsors of other PD-1/PD-L1 inhibitors to examine other trials in which these drugs are being studied in combination with immunomodulatory agents and trials in which the inhibitors are being studied in combination with other classes of drugs in patients with hematologic malignancies.
Woodcock said the FDA will take appropriate action as warranted to ensure patients enrolled in these trials are protected and that doctors and researchers understand the risks associated with this investigational use.
The agency is also encouraging healthcare professionals and consumers to report any adverse events or side effects related to the use of pembrolizumab and other PD-1/PD-L1 inhibitors to FDA’s MedWatch Adverse Event Reporting Program.