User login
EC grants ixazomib conditional approval to treat MM
The European Commission (EC) has granted conditional marketing authorization for ixazomib (NinlaroTM) to be used in combination with lenalidomide and dexamethasone to treat adults with multiple myeloma (MM) who have received at least 1 prior therapy.
This decision makes ixazomib the first oral proteasome inhibitor approved to treat MM in the European Economic Area.
“With the approval of Ninlaro by the European Commission, physicians across the region will have the option to prescribe an all-oral triplet regimen to treat patients with multiple myeloma who have received at least 1 prior therapy,” said Philippe Moreau, MD, of the University Hospital of Nantes in France.
Conditional marketing authorization represents an expedited path for approval. The EC grants this type of authorization before pivotal registration studies are completed.
Conditional marketing authorization is granted to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
The conditional authorization for ixazomib means the company developing the drug, Takeda Pharmaceutical Company Limited, is required to provide post-approval updates on safety and efficacy analyses from ongoing studies to demonstrate the long-term effects of ixazomib.
Phase 3 trial
The EC’s decision to grant ixazomib conditional marketing authorization is based on results from the phase 3 TOURMALINE-MM1 trial, which were presented at the 2015 ASH Annual Meeting.
The trial included 722 patients with relapsed or refractory MM. The patients were randomized to receive ixazomib, lenalidomide, and dexamethasone (IRd, n=360) or placebo, lenalidomide, and dexamethasone (Rd, n=362).
Baseline patient characteristics were similar between the treatment arms. Fifty-nine percent of patients in both arms had received 1 prior line of therapy, and 41% in both arms had 2 or 3 prior lines of therapy.
Seventy-eight percent of patients responded to IRd, and 72% responded to Rd (P=0.035). The rates of complete response were 12% and 7%, respectively (P=0.019).
At a median follow-up of about 15 months, the median progression-free survival was 20.6 months in the IRd arm and 14.7 months in the Rd arm. The hazard ratio was 0.742 (P=0.012).
At a median follow-up of about 23 months, the median overall survival had not been reached in either treatment arm. Follow-up analyses for overall survival are planned for 2017.
The incidence of adverse events (AEs) was 98% in the IRd arm and 99% in the Rd arm. The incidence of grade 3 or higher AEs was 74% and 69%, respectively. The incidence of serious AEs was 47% and 49%, respectively.
Common AEs in the IRd and Rd arms, respectively, were diarrhea (45% vs 39%), constipation (35% vs 26%), nausea (29% vs 22%), vomiting (23% vs 12%), rash (36% vs 23%), back pain (24% vs 17%), upper respiratory tract infection (23% vs 19%), thrombocytopenia (31% vs 16%), peripheral neuropathy (27% vs 22%), peripheral edema (28% vs 20%), thromboembolism (8% vs 11%), and neutropenia (33% vs 31%). ![]()
The European Commission (EC) has granted conditional marketing authorization for ixazomib (NinlaroTM) to be used in combination with lenalidomide and dexamethasone to treat adults with multiple myeloma (MM) who have received at least 1 prior therapy.
This decision makes ixazomib the first oral proteasome inhibitor approved to treat MM in the European Economic Area.
“With the approval of Ninlaro by the European Commission, physicians across the region will have the option to prescribe an all-oral triplet regimen to treat patients with multiple myeloma who have received at least 1 prior therapy,” said Philippe Moreau, MD, of the University Hospital of Nantes in France.
Conditional marketing authorization represents an expedited path for approval. The EC grants this type of authorization before pivotal registration studies are completed.
Conditional marketing authorization is granted to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
The conditional authorization for ixazomib means the company developing the drug, Takeda Pharmaceutical Company Limited, is required to provide post-approval updates on safety and efficacy analyses from ongoing studies to demonstrate the long-term effects of ixazomib.
Phase 3 trial
The EC’s decision to grant ixazomib conditional marketing authorization is based on results from the phase 3 TOURMALINE-MM1 trial, which were presented at the 2015 ASH Annual Meeting.
The trial included 722 patients with relapsed or refractory MM. The patients were randomized to receive ixazomib, lenalidomide, and dexamethasone (IRd, n=360) or placebo, lenalidomide, and dexamethasone (Rd, n=362).
Baseline patient characteristics were similar between the treatment arms. Fifty-nine percent of patients in both arms had received 1 prior line of therapy, and 41% in both arms had 2 or 3 prior lines of therapy.
Seventy-eight percent of patients responded to IRd, and 72% responded to Rd (P=0.035). The rates of complete response were 12% and 7%, respectively (P=0.019).
At a median follow-up of about 15 months, the median progression-free survival was 20.6 months in the IRd arm and 14.7 months in the Rd arm. The hazard ratio was 0.742 (P=0.012).
At a median follow-up of about 23 months, the median overall survival had not been reached in either treatment arm. Follow-up analyses for overall survival are planned for 2017.
The incidence of adverse events (AEs) was 98% in the IRd arm and 99% in the Rd arm. The incidence of grade 3 or higher AEs was 74% and 69%, respectively. The incidence of serious AEs was 47% and 49%, respectively.
Common AEs in the IRd and Rd arms, respectively, were diarrhea (45% vs 39%), constipation (35% vs 26%), nausea (29% vs 22%), vomiting (23% vs 12%), rash (36% vs 23%), back pain (24% vs 17%), upper respiratory tract infection (23% vs 19%), thrombocytopenia (31% vs 16%), peripheral neuropathy (27% vs 22%), peripheral edema (28% vs 20%), thromboembolism (8% vs 11%), and neutropenia (33% vs 31%). ![]()
The European Commission (EC) has granted conditional marketing authorization for ixazomib (NinlaroTM) to be used in combination with lenalidomide and dexamethasone to treat adults with multiple myeloma (MM) who have received at least 1 prior therapy.
This decision makes ixazomib the first oral proteasome inhibitor approved to treat MM in the European Economic Area.
“With the approval of Ninlaro by the European Commission, physicians across the region will have the option to prescribe an all-oral triplet regimen to treat patients with multiple myeloma who have received at least 1 prior therapy,” said Philippe Moreau, MD, of the University Hospital of Nantes in France.
Conditional marketing authorization represents an expedited path for approval. The EC grants this type of authorization before pivotal registration studies are completed.
Conditional marketing authorization is granted to products whose benefits are thought to outweigh their risks, products that address unmet needs, and products that are expected to provide a significant public health benefit.
The conditional authorization for ixazomib means the company developing the drug, Takeda Pharmaceutical Company Limited, is required to provide post-approval updates on safety and efficacy analyses from ongoing studies to demonstrate the long-term effects of ixazomib.
Phase 3 trial
The EC’s decision to grant ixazomib conditional marketing authorization is based on results from the phase 3 TOURMALINE-MM1 trial, which were presented at the 2015 ASH Annual Meeting.
The trial included 722 patients with relapsed or refractory MM. The patients were randomized to receive ixazomib, lenalidomide, and dexamethasone (IRd, n=360) or placebo, lenalidomide, and dexamethasone (Rd, n=362).
Baseline patient characteristics were similar between the treatment arms. Fifty-nine percent of patients in both arms had received 1 prior line of therapy, and 41% in both arms had 2 or 3 prior lines of therapy.
Seventy-eight percent of patients responded to IRd, and 72% responded to Rd (P=0.035). The rates of complete response were 12% and 7%, respectively (P=0.019).
At a median follow-up of about 15 months, the median progression-free survival was 20.6 months in the IRd arm and 14.7 months in the Rd arm. The hazard ratio was 0.742 (P=0.012).
At a median follow-up of about 23 months, the median overall survival had not been reached in either treatment arm. Follow-up analyses for overall survival are planned for 2017.
The incidence of adverse events (AEs) was 98% in the IRd arm and 99% in the Rd arm. The incidence of grade 3 or higher AEs was 74% and 69%, respectively. The incidence of serious AEs was 47% and 49%, respectively.
Common AEs in the IRd and Rd arms, respectively, were diarrhea (45% vs 39%), constipation (35% vs 26%), nausea (29% vs 22%), vomiting (23% vs 12%), rash (36% vs 23%), back pain (24% vs 17%), upper respiratory tract infection (23% vs 19%), thrombocytopenia (31% vs 16%), peripheral neuropathy (27% vs 22%), peripheral edema (28% vs 20%), thromboembolism (8% vs 11%), and neutropenia (33% vs 31%). ![]()
FDA approves daratumumab in combination with standard therapy for multiple myeloma
The Food and Drug Administration has approved daratumumab in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, for the treatment of patients with multiple myeloma who have received at least one prior therapy.
The drug was approved last year as monotherapy for patients with multiple myeloma who have received at least three prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or who are double refractory to a proteasome inhibitor and an immunomodulatory agent.
In the POLLUX trial, median PFS had not been reached in the daratumumab plus lenalidomide and dexamethasone arm and was 18.4 months among patients getting lenalidomide and dexamethasone alone (HR=0.37; 95% CI: 0.27, 0.52; P less than.0001).
In the CASTOR trial, which compared the combination of daratumumab, bortezomib, and dexamethasone with bortezomib and dexamethasone, the estimated median PFS had not been reached in the daratumumab arm and was 7.2 months in the control arm (hazard ratio, 0.39; 95% confidence interval, 0.28-0.53; P less than .0001).
Updated results for both trials will be presented at the upcoming annual meeting of the American Society of Hematology (abstract #1150, abstract #1151).
The most frequently reported adverse reactions in POLLUX were infusion reactions, diarrhea, nausea, fatigue, pyrexia, upper respiratory tract infection, muscle spasm, cough, and dyspnea. The most frequently reported adverse reactions in CASTOR were infusion reactions, diarrhea, peripheral edema, upper respiratory tract infection, peripheral sensory neuropathy, cough, and dyspnea.
The recommended dose of daratumumab is 16 mg/kg IV (calculated on actual body weight), the FDA said.
Full prescribing information is available here.
[email protected]
On Twitter @nikolaideslaura
The Food and Drug Administration has approved daratumumab in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, for the treatment of patients with multiple myeloma who have received at least one prior therapy.
The drug was approved last year as monotherapy for patients with multiple myeloma who have received at least three prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or who are double refractory to a proteasome inhibitor and an immunomodulatory agent.
In the POLLUX trial, median PFS had not been reached in the daratumumab plus lenalidomide and dexamethasone arm and was 18.4 months among patients getting lenalidomide and dexamethasone alone (HR=0.37; 95% CI: 0.27, 0.52; P less than.0001).
In the CASTOR trial, which compared the combination of daratumumab, bortezomib, and dexamethasone with bortezomib and dexamethasone, the estimated median PFS had not been reached in the daratumumab arm and was 7.2 months in the control arm (hazard ratio, 0.39; 95% confidence interval, 0.28-0.53; P less than .0001).
Updated results for both trials will be presented at the upcoming annual meeting of the American Society of Hematology (abstract #1150, abstract #1151).
The most frequently reported adverse reactions in POLLUX were infusion reactions, diarrhea, nausea, fatigue, pyrexia, upper respiratory tract infection, muscle spasm, cough, and dyspnea. The most frequently reported adverse reactions in CASTOR were infusion reactions, diarrhea, peripheral edema, upper respiratory tract infection, peripheral sensory neuropathy, cough, and dyspnea.
The recommended dose of daratumumab is 16 mg/kg IV (calculated on actual body weight), the FDA said.
Full prescribing information is available here.
[email protected]
On Twitter @nikolaideslaura
The Food and Drug Administration has approved daratumumab in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, for the treatment of patients with multiple myeloma who have received at least one prior therapy.
The drug was approved last year as monotherapy for patients with multiple myeloma who have received at least three prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or who are double refractory to a proteasome inhibitor and an immunomodulatory agent.
In the POLLUX trial, median PFS had not been reached in the daratumumab plus lenalidomide and dexamethasone arm and was 18.4 months among patients getting lenalidomide and dexamethasone alone (HR=0.37; 95% CI: 0.27, 0.52; P less than.0001).
In the CASTOR trial, which compared the combination of daratumumab, bortezomib, and dexamethasone with bortezomib and dexamethasone, the estimated median PFS had not been reached in the daratumumab arm and was 7.2 months in the control arm (hazard ratio, 0.39; 95% confidence interval, 0.28-0.53; P less than .0001).
Updated results for both trials will be presented at the upcoming annual meeting of the American Society of Hematology (abstract #1150, abstract #1151).
The most frequently reported adverse reactions in POLLUX were infusion reactions, diarrhea, nausea, fatigue, pyrexia, upper respiratory tract infection, muscle spasm, cough, and dyspnea. The most frequently reported adverse reactions in CASTOR were infusion reactions, diarrhea, peripheral edema, upper respiratory tract infection, peripheral sensory neuropathy, cough, and dyspnea.
The recommended dose of daratumumab is 16 mg/kg IV (calculated on actual body weight), the FDA said.
Full prescribing information is available here.
[email protected]
On Twitter @nikolaideslaura
FDA approves new uses for drug in MM

Photo courtesy of Janssen
The US Food and Drug Administration (FDA) has approved new indications for the monoclonal antibody daratumumab (Darzalex®).
The drug is now approved for use in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone to treat patients with multiple myeloma (MM) who have received at least 1 prior therapy.
This approval comes 3 months after a supplemental biologics license application was submitted to the FDA.
The application was granted priority review last month, and the FDA granted daratumumab breakthrough therapy designation in July.
Daratumumab is the first CD38-directed cytolytic antibody approved anywhere in the world.
The drug received accelerated approval from the FDA in November of last year for use as monotherapy in MM patients who have received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or MM patients who are double refractory to a proteasome inhibitor and immunomodulatory agent.
Daratumumab is being developed by Janssen Biotech, Inc. under an exclusive worldwide license from Genmab. For the full prescribing information, visit www.DARZALEX.com.
Phase 3 trials
The FDA’s latest approval of daratumumab was based on data from the phase 3 POLLUX and CASTOR trials.
In the POLLUX trial, researchers compared treatment with lenalidomide and dexamethasone to treatment with daratumumab, lenalidomide, and dexamethasone in patients with relapsed or refractory MM.
Patients who received daratumumab in combination had a significantly higher response rate and longer progression-free survival than patients who received the 2-drug combination.
However, treatment with daratumumab was associated with infusion-related reactions and a higher incidence of neutropenia.
Results from this trial were published in NEJM in October.
In the CASTOR trial, researchers compared treatment with bortezomib and dexamethasone to treatment with daratumumab, bortezomib, and dexamethasone in patients with previously treated MM.
Patients who received the 3-drug combination had a higher response rate, longer progression-free survival, and a higher incidence of grade 3/4 adverse events than those who received the 2-drug combination.
Results from this trial were published in NEJM in August. ![]()

Photo courtesy of Janssen
The US Food and Drug Administration (FDA) has approved new indications for the monoclonal antibody daratumumab (Darzalex®).
The drug is now approved for use in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone to treat patients with multiple myeloma (MM) who have received at least 1 prior therapy.
This approval comes 3 months after a supplemental biologics license application was submitted to the FDA.
The application was granted priority review last month, and the FDA granted daratumumab breakthrough therapy designation in July.
Daratumumab is the first CD38-directed cytolytic antibody approved anywhere in the world.
The drug received accelerated approval from the FDA in November of last year for use as monotherapy in MM patients who have received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or MM patients who are double refractory to a proteasome inhibitor and immunomodulatory agent.
Daratumumab is being developed by Janssen Biotech, Inc. under an exclusive worldwide license from Genmab. For the full prescribing information, visit www.DARZALEX.com.
Phase 3 trials
The FDA’s latest approval of daratumumab was based on data from the phase 3 POLLUX and CASTOR trials.
In the POLLUX trial, researchers compared treatment with lenalidomide and dexamethasone to treatment with daratumumab, lenalidomide, and dexamethasone in patients with relapsed or refractory MM.
Patients who received daratumumab in combination had a significantly higher response rate and longer progression-free survival than patients who received the 2-drug combination.
However, treatment with daratumumab was associated with infusion-related reactions and a higher incidence of neutropenia.
Results from this trial were published in NEJM in October.
In the CASTOR trial, researchers compared treatment with bortezomib and dexamethasone to treatment with daratumumab, bortezomib, and dexamethasone in patients with previously treated MM.
Patients who received the 3-drug combination had a higher response rate, longer progression-free survival, and a higher incidence of grade 3/4 adverse events than those who received the 2-drug combination.
Results from this trial were published in NEJM in August. ![]()

Photo courtesy of Janssen
The US Food and Drug Administration (FDA) has approved new indications for the monoclonal antibody daratumumab (Darzalex®).
The drug is now approved for use in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone to treat patients with multiple myeloma (MM) who have received at least 1 prior therapy.
This approval comes 3 months after a supplemental biologics license application was submitted to the FDA.
The application was granted priority review last month, and the FDA granted daratumumab breakthrough therapy designation in July.
Daratumumab is the first CD38-directed cytolytic antibody approved anywhere in the world.
The drug received accelerated approval from the FDA in November of last year for use as monotherapy in MM patients who have received at least 3 prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or MM patients who are double refractory to a proteasome inhibitor and immunomodulatory agent.
Daratumumab is being developed by Janssen Biotech, Inc. under an exclusive worldwide license from Genmab. For the full prescribing information, visit www.DARZALEX.com.
Phase 3 trials
The FDA’s latest approval of daratumumab was based on data from the phase 3 POLLUX and CASTOR trials.
In the POLLUX trial, researchers compared treatment with lenalidomide and dexamethasone to treatment with daratumumab, lenalidomide, and dexamethasone in patients with relapsed or refractory MM.
Patients who received daratumumab in combination had a significantly higher response rate and longer progression-free survival than patients who received the 2-drug combination.
However, treatment with daratumumab was associated with infusion-related reactions and a higher incidence of neutropenia.
Results from this trial were published in NEJM in October.
In the CASTOR trial, researchers compared treatment with bortezomib and dexamethasone to treatment with daratumumab, bortezomib, and dexamethasone in patients with previously treated MM.
Patients who received the 3-drug combination had a higher response rate, longer progression-free survival, and a higher incidence of grade 3/4 adverse events than those who received the 2-drug combination.
Results from this trial were published in NEJM in August. ![]()
NCCN guidelines on MM now include MRD testing

The National Comprehensive Cancer Network (NCCN) has revised its clinical practice guidelines on multiple myeloma (MM) to include response criteria developed by the International Myeloma Working Group (IMWG) and testing for minimal residual disease (MRD).
The NCCN develops practice guidelines to help physicians in making informed treatment decisions.
Its recommendations can facilitate reimbursement for testing or treatment.
“The NCCN’s action represents a further step toward broad use of MRD testing,” said Brian Durie, MD, chairman of the International Myeloma Foundation (IMF).
The importance of first identifying and then eliminating MRD is the key principle of the IMF’s Black Swan Research Initiative®, a collaborative effort launched in 2012 to cure MM.
“We’ve long believed early intervention with highly effective treatments is the pathway to curing myeloma, and we are currently testing this in clinical trials,” Dr Durie said.
Through the Black Swan Research Initiative, the IMF helped develop next-generation flow cytometry, 1 of 2 tests recommended by the NCCN to assess the presence of MRD in MM patients. The second test is next-generation sequencing.
The new MM response criteria, on which the NCCN based its most recent revision to the guidelines, were developed and agreed upon by the more than 200 members of the IMWG.
The new response criteria spell out exact definitions of “MRD negative” by next-generation flow cytometry or next-generation sequencing.
“We are pleased that the 2016 IMWG response criteria were adopted in full in the new NCCN recommendations,” said Shaji Kumar, MD, of the Mayo Clinic in Rochester, Minnesota.
The 2016 IMWG response criteria were published in The Lancet Oncology in August. ![]()

The National Comprehensive Cancer Network (NCCN) has revised its clinical practice guidelines on multiple myeloma (MM) to include response criteria developed by the International Myeloma Working Group (IMWG) and testing for minimal residual disease (MRD).
The NCCN develops practice guidelines to help physicians in making informed treatment decisions.
Its recommendations can facilitate reimbursement for testing or treatment.
“The NCCN’s action represents a further step toward broad use of MRD testing,” said Brian Durie, MD, chairman of the International Myeloma Foundation (IMF).
The importance of first identifying and then eliminating MRD is the key principle of the IMF’s Black Swan Research Initiative®, a collaborative effort launched in 2012 to cure MM.
“We’ve long believed early intervention with highly effective treatments is the pathway to curing myeloma, and we are currently testing this in clinical trials,” Dr Durie said.
Through the Black Swan Research Initiative, the IMF helped develop next-generation flow cytometry, 1 of 2 tests recommended by the NCCN to assess the presence of MRD in MM patients. The second test is next-generation sequencing.
The new MM response criteria, on which the NCCN based its most recent revision to the guidelines, were developed and agreed upon by the more than 200 members of the IMWG.
The new response criteria spell out exact definitions of “MRD negative” by next-generation flow cytometry or next-generation sequencing.
“We are pleased that the 2016 IMWG response criteria were adopted in full in the new NCCN recommendations,” said Shaji Kumar, MD, of the Mayo Clinic in Rochester, Minnesota.
The 2016 IMWG response criteria were published in The Lancet Oncology in August. ![]()

The National Comprehensive Cancer Network (NCCN) has revised its clinical practice guidelines on multiple myeloma (MM) to include response criteria developed by the International Myeloma Working Group (IMWG) and testing for minimal residual disease (MRD).
The NCCN develops practice guidelines to help physicians in making informed treatment decisions.
Its recommendations can facilitate reimbursement for testing or treatment.
“The NCCN’s action represents a further step toward broad use of MRD testing,” said Brian Durie, MD, chairman of the International Myeloma Foundation (IMF).
The importance of first identifying and then eliminating MRD is the key principle of the IMF’s Black Swan Research Initiative®, a collaborative effort launched in 2012 to cure MM.
“We’ve long believed early intervention with highly effective treatments is the pathway to curing myeloma, and we are currently testing this in clinical trials,” Dr Durie said.
Through the Black Swan Research Initiative, the IMF helped develop next-generation flow cytometry, 1 of 2 tests recommended by the NCCN to assess the presence of MRD in MM patients. The second test is next-generation sequencing.
The new MM response criteria, on which the NCCN based its most recent revision to the guidelines, were developed and agreed upon by the more than 200 members of the IMWG.
The new response criteria spell out exact definitions of “MRD negative” by next-generation flow cytometry or next-generation sequencing.
“We are pleased that the 2016 IMWG response criteria were adopted in full in the new NCCN recommendations,” said Shaji Kumar, MD, of the Mayo Clinic in Rochester, Minnesota.
The 2016 IMWG response criteria were published in The Lancet Oncology in August. ![]()
Tool provides info for cancer patients, survivors

receiving treatment
Photo by Rhoda Baer
The American Cancer Society and National Cancer Institute have launched an online tool for cancer patients and survivors.
The tool, Springboard Beyond Cancer, was designed to help these individuals address medical, psychosocial, and wellness needs during and after treatment.
Springboard Beyond Cancer provides information to help cancer patients and survivors manage ongoing cancer-related symptoms, deal with stress, ensure healthy behavior, communicate better with healthcare teams, and seek support from friends and family.
“With Springboard Beyond Cancer, we want to empower cancer survivors by giving them the information they need to help identify issues, set goals, and create a plan to more smoothly navigate the cancer journey and take control of their health,” said Corinne Leach, PhD, a behavioral scientist and strategic director in the Behavioral Research Center at the American Cancer Society.
“We hope that Springboard Beyond Cancer, along with the close collaboration of their medical team, can help cancer survivors reduce their disease burden and improve their overall wellbeing,” added Erik Augustson, PhD, program director at the National Cancer Institute. ![]()

receiving treatment
Photo by Rhoda Baer
The American Cancer Society and National Cancer Institute have launched an online tool for cancer patients and survivors.
The tool, Springboard Beyond Cancer, was designed to help these individuals address medical, psychosocial, and wellness needs during and after treatment.
Springboard Beyond Cancer provides information to help cancer patients and survivors manage ongoing cancer-related symptoms, deal with stress, ensure healthy behavior, communicate better with healthcare teams, and seek support from friends and family.
“With Springboard Beyond Cancer, we want to empower cancer survivors by giving them the information they need to help identify issues, set goals, and create a plan to more smoothly navigate the cancer journey and take control of their health,” said Corinne Leach, PhD, a behavioral scientist and strategic director in the Behavioral Research Center at the American Cancer Society.
“We hope that Springboard Beyond Cancer, along with the close collaboration of their medical team, can help cancer survivors reduce their disease burden and improve their overall wellbeing,” added Erik Augustson, PhD, program director at the National Cancer Institute. ![]()

receiving treatment
Photo by Rhoda Baer
The American Cancer Society and National Cancer Institute have launched an online tool for cancer patients and survivors.
The tool, Springboard Beyond Cancer, was designed to help these individuals address medical, psychosocial, and wellness needs during and after treatment.
Springboard Beyond Cancer provides information to help cancer patients and survivors manage ongoing cancer-related symptoms, deal with stress, ensure healthy behavior, communicate better with healthcare teams, and seek support from friends and family.
“With Springboard Beyond Cancer, we want to empower cancer survivors by giving them the information they need to help identify issues, set goals, and create a plan to more smoothly navigate the cancer journey and take control of their health,” said Corinne Leach, PhD, a behavioral scientist and strategic director in the Behavioral Research Center at the American Cancer Society.
“We hope that Springboard Beyond Cancer, along with the close collaboration of their medical team, can help cancer survivors reduce their disease burden and improve their overall wellbeing,” added Erik Augustson, PhD, program director at the National Cancer Institute. ![]()
Phase 2 trial of MM drug placed on clinical hold

A phase 2 study of the antibody BI-505 in patients with multiple myeloma (MM) has been placed on full clinical hold.
BioInvent International, the company developing BI-505, said it has received verbal notice of the clinical hold from the US Food and Drug Administration (FDA).
The clinical hold means no new subjects can be enrolled on the trial, and there can be no further dosing of subjects who are already enrolled.
BioInvent International said it has yet to receive written notice of the clinical hold from the FDA. However, based on verbal communications, the clinical hold is due to an adverse cardiopulmonary event.
The study (NCT02756728) is being conducted by BioInvent International in collaboration with investigators at the University of Pennsylvania.
The goal of the study is to determine if BI-505 can deepen therapeutic response and thereby prevent or delay relapse in MM patients undergoing autologous stem cell transplant with high-dose melphalan.
BioInvent International said it will analyze the possibility to obtain release of the clinical hold and will provide updates when there is further information to report.
About BI-505
BI-505 is a human antibody targeting ICAM-1, a protein that is elevated in MM cells. BI-505 has been shown to attack MM in 2 ways—by inducing apoptosis in MM cells and by engaging macrophages to attack and kill MM cells.
According to BioInvent International, the development strategy for BI-505 is focused on eliminating residual disease by combining the antibody with modern standard-of-care drugs used to treat MM.
The company said BI-505 proved safe in a phase 1 trial of patients with relapsed/refractory MM, as well as demonstrating “signs of a positive effect against the disease.” This study was published in Clinical Cancer Research in June 2015.
BI-505 has received orphan drug designation as a treatment for MM from both the FDA and the European Medicines Agency. ![]()

A phase 2 study of the antibody BI-505 in patients with multiple myeloma (MM) has been placed on full clinical hold.
BioInvent International, the company developing BI-505, said it has received verbal notice of the clinical hold from the US Food and Drug Administration (FDA).
The clinical hold means no new subjects can be enrolled on the trial, and there can be no further dosing of subjects who are already enrolled.
BioInvent International said it has yet to receive written notice of the clinical hold from the FDA. However, based on verbal communications, the clinical hold is due to an adverse cardiopulmonary event.
The study (NCT02756728) is being conducted by BioInvent International in collaboration with investigators at the University of Pennsylvania.
The goal of the study is to determine if BI-505 can deepen therapeutic response and thereby prevent or delay relapse in MM patients undergoing autologous stem cell transplant with high-dose melphalan.
BioInvent International said it will analyze the possibility to obtain release of the clinical hold and will provide updates when there is further information to report.
About BI-505
BI-505 is a human antibody targeting ICAM-1, a protein that is elevated in MM cells. BI-505 has been shown to attack MM in 2 ways—by inducing apoptosis in MM cells and by engaging macrophages to attack and kill MM cells.
According to BioInvent International, the development strategy for BI-505 is focused on eliminating residual disease by combining the antibody with modern standard-of-care drugs used to treat MM.
The company said BI-505 proved safe in a phase 1 trial of patients with relapsed/refractory MM, as well as demonstrating “signs of a positive effect against the disease.” This study was published in Clinical Cancer Research in June 2015.
BI-505 has received orphan drug designation as a treatment for MM from both the FDA and the European Medicines Agency. ![]()

A phase 2 study of the antibody BI-505 in patients with multiple myeloma (MM) has been placed on full clinical hold.
BioInvent International, the company developing BI-505, said it has received verbal notice of the clinical hold from the US Food and Drug Administration (FDA).
The clinical hold means no new subjects can be enrolled on the trial, and there can be no further dosing of subjects who are already enrolled.
BioInvent International said it has yet to receive written notice of the clinical hold from the FDA. However, based on verbal communications, the clinical hold is due to an adverse cardiopulmonary event.
The study (NCT02756728) is being conducted by BioInvent International in collaboration with investigators at the University of Pennsylvania.
The goal of the study is to determine if BI-505 can deepen therapeutic response and thereby prevent or delay relapse in MM patients undergoing autologous stem cell transplant with high-dose melphalan.
BioInvent International said it will analyze the possibility to obtain release of the clinical hold and will provide updates when there is further information to report.
About BI-505
BI-505 is a human antibody targeting ICAM-1, a protein that is elevated in MM cells. BI-505 has been shown to attack MM in 2 ways—by inducing apoptosis in MM cells and by engaging macrophages to attack and kill MM cells.
According to BioInvent International, the development strategy for BI-505 is focused on eliminating residual disease by combining the antibody with modern standard-of-care drugs used to treat MM.
The company said BI-505 proved safe in a phase 1 trial of patients with relapsed/refractory MM, as well as demonstrating “signs of a positive effect against the disease.” This study was published in Clinical Cancer Research in June 2015.
BI-505 has received orphan drug designation as a treatment for MM from both the FDA and the European Medicines Agency. ![]()
CTC analysis as good as BM biopsy in MM, team says

Photo by Juan D. Alfonso
Analysis of circulating tumor cells (CTCs) can provide at least as much genetic information about multiple myeloma (MM) as a bone marrow (BM) biopsy, according to a new study.
Researchers found evidence to suggest that analyzing CTCs isolated from the peripheral blood of MM patients could help physicians monitor disease progression over time, track the emergence of drug resistance, and tailor therapies to individual patients.
Jens Lohr, MD, PhD, of the Broad Institute of MIT and Harvard in Cambridge, Massachusetts, and colleagues conducted this research and detailed their findings in Science Translational Medicine.
The researchers said they devised a method that was “highly sensitive” in detecting and sequencing single CTCs, even from patients with low tumor burden.
Specifically, the team found they could isolate CTCs from, and detect mutations in, blood samples from an MM patient who had achieved a very good partial response to treatment and a patient with monoclonal gammopathy of undetermined significance.
Overall, the researchers found that CTCs could be used to identify mutations relevant for prognosis, and some of these mutations were more abundant in CTCs than in BM samples.
For example, the team detected somatic mutations in the KRAS, BRAF, IRF4, and TP53 genes in single CTCs from 3 MM patients. And the same mutations were present in single BM-derived MM cells.
In another 3 patients, the proportion of CTCs harboring TP53 R273C, BRAF G469A, and NRAS G13D mutations was higher than that observed in BM-derived cells. In 2 of the patients, the mutations weren’t detectable in BM cells because of insufficient sample material.
The researchers also found that CTCs could reveal patients with an overabundance of molecules expressed by MM cells—such as CD38 and SLAMF7—that can be targeted by therapies currently approved to treat MM—such as daratumumab and elotuzumab.
The team therefore believes that, with further development, CTC analysis could be a valuable tool for advancing precision medicine in MM. ![]()

Photo by Juan D. Alfonso
Analysis of circulating tumor cells (CTCs) can provide at least as much genetic information about multiple myeloma (MM) as a bone marrow (BM) biopsy, according to a new study.
Researchers found evidence to suggest that analyzing CTCs isolated from the peripheral blood of MM patients could help physicians monitor disease progression over time, track the emergence of drug resistance, and tailor therapies to individual patients.
Jens Lohr, MD, PhD, of the Broad Institute of MIT and Harvard in Cambridge, Massachusetts, and colleagues conducted this research and detailed their findings in Science Translational Medicine.
The researchers said they devised a method that was “highly sensitive” in detecting and sequencing single CTCs, even from patients with low tumor burden.
Specifically, the team found they could isolate CTCs from, and detect mutations in, blood samples from an MM patient who had achieved a very good partial response to treatment and a patient with monoclonal gammopathy of undetermined significance.
Overall, the researchers found that CTCs could be used to identify mutations relevant for prognosis, and some of these mutations were more abundant in CTCs than in BM samples.
For example, the team detected somatic mutations in the KRAS, BRAF, IRF4, and TP53 genes in single CTCs from 3 MM patients. And the same mutations were present in single BM-derived MM cells.
In another 3 patients, the proportion of CTCs harboring TP53 R273C, BRAF G469A, and NRAS G13D mutations was higher than that observed in BM-derived cells. In 2 of the patients, the mutations weren’t detectable in BM cells because of insufficient sample material.
The researchers also found that CTCs could reveal patients with an overabundance of molecules expressed by MM cells—such as CD38 and SLAMF7—that can be targeted by therapies currently approved to treat MM—such as daratumumab and elotuzumab.
The team therefore believes that, with further development, CTC analysis could be a valuable tool for advancing precision medicine in MM. ![]()

Photo by Juan D. Alfonso
Analysis of circulating tumor cells (CTCs) can provide at least as much genetic information about multiple myeloma (MM) as a bone marrow (BM) biopsy, according to a new study.
Researchers found evidence to suggest that analyzing CTCs isolated from the peripheral blood of MM patients could help physicians monitor disease progression over time, track the emergence of drug resistance, and tailor therapies to individual patients.
Jens Lohr, MD, PhD, of the Broad Institute of MIT and Harvard in Cambridge, Massachusetts, and colleagues conducted this research and detailed their findings in Science Translational Medicine.
The researchers said they devised a method that was “highly sensitive” in detecting and sequencing single CTCs, even from patients with low tumor burden.
Specifically, the team found they could isolate CTCs from, and detect mutations in, blood samples from an MM patient who had achieved a very good partial response to treatment and a patient with monoclonal gammopathy of undetermined significance.
Overall, the researchers found that CTCs could be used to identify mutations relevant for prognosis, and some of these mutations were more abundant in CTCs than in BM samples.
For example, the team detected somatic mutations in the KRAS, BRAF, IRF4, and TP53 genes in single CTCs from 3 MM patients. And the same mutations were present in single BM-derived MM cells.
In another 3 patients, the proportion of CTCs harboring TP53 R273C, BRAF G469A, and NRAS G13D mutations was higher than that observed in BM-derived cells. In 2 of the patients, the mutations weren’t detectable in BM cells because of insufficient sample material.
The researchers also found that CTCs could reveal patients with an overabundance of molecules expressed by MM cells—such as CD38 and SLAMF7—that can be targeted by therapies currently approved to treat MM—such as daratumumab and elotuzumab.
The team therefore believes that, with further development, CTC analysis could be a valuable tool for advancing precision medicine in MM. ![]()
Continuous Rd should be standard of care, group says

Photo courtesy of Celgene
Updated trial results support continuous treatment with lenalidomide and low-dose dexamethasone (Rd) as a standard of care for patients of all ages who have newly diagnosed multiple myeloma (MM) and are ineligible for stem cell transplant, according to researchers.
In this phase 3 trial, patients who received continuous Rd (until disease progression) had better progression-free survival (PFS) and overall survival (OS) than patients who received 18 cycles of Rd (Rd18) or a combination of melphalan, prednisone, and thalidomide (MPT).
Updated results from this study, known as the FIRST trial, were published in the Journal of Clinical Oncology.
Results were previously published in NEJM in 2014. The study was supported by Intergroupe Francophone du Myélome and Celgene Corporation, the makers of lenalidomide.
Thierry Facon, MD, of Centre Hospitalier Regional Universitaire de Lille in France, and his colleagues enrolled 1623 patients on this trial. They were newly diagnosed with MM and not eligible for stem cell transplant.
Patients were randomized to receive Rd in 28-day cycles until disease progression (n=535), Rd18 for 72 weeks (n=541), or MPT for 72 weeks (n=547).
Response
In the intent-to-treat population, the overall response rate was 81% for the continuous Rd group, 79% for the Rd18 group, and 67% in the MPT group. The complete response rates were 21%, 20%, and 12%, respectively.
The median duration of response was 32 months (range, 26-37) in the continuous Rd group, 22 months (range, 19-23) in the Rd18 group, and 22 months (range, 20-25) in the MPT group.
PFS and OS
The median PFS was 26.0 months in the continuous Rd group, 21.0 months in the Rd18 group, and 21.9 months in the MPT group. At 4 years, the PFS rate was 33%, 14%, and 13%, respectively.
The hazard ratio (HR) for continuous Rd vs MPT was 0.69. The HR for continuous Rd vs Rd18 was 0.71. And the HR for Rd18 vs MPT was 0.99.
The median OS was 58.9 months in the continuous Rd group, 56.7 months in the Rd18 group, and 48.5 months in the MPT group. At 4 years, the OS rate was 60%, 57%, and 51%, respectively.
The HR for continuous Rd vs MPT was 0.75. The HR for continuous Rd vs Rd18 was 0.91. And the HR for Rd18 vs MPT was 0.83.
Safety
The most frequent grade 3/4 hematologic treatment-emergent adverse events were neutropenia and anemia. The rate of grade 3/4 neutropenia was higher in the MPT group than the continuous Rd or Rd18 groups.
Infections were the most common grade 3/4 non-hematologic treatment-emergent adverse events. The rate of grade 3/4 infections was higher in the Rd groups than the MPT group.
Grade 3/4 peripheral sensory neuropathy was less frequent in the continuous Rd and Rd18 groups than the MPT group.
The incidence of invasive second primary malignancy was 4% in the continuous Rd group, 6% in the Rd18 group, and 6% in the MPT group. ![]()

Photo courtesy of Celgene
Updated trial results support continuous treatment with lenalidomide and low-dose dexamethasone (Rd) as a standard of care for patients of all ages who have newly diagnosed multiple myeloma (MM) and are ineligible for stem cell transplant, according to researchers.
In this phase 3 trial, patients who received continuous Rd (until disease progression) had better progression-free survival (PFS) and overall survival (OS) than patients who received 18 cycles of Rd (Rd18) or a combination of melphalan, prednisone, and thalidomide (MPT).
Updated results from this study, known as the FIRST trial, were published in the Journal of Clinical Oncology.
Results were previously published in NEJM in 2014. The study was supported by Intergroupe Francophone du Myélome and Celgene Corporation, the makers of lenalidomide.
Thierry Facon, MD, of Centre Hospitalier Regional Universitaire de Lille in France, and his colleagues enrolled 1623 patients on this trial. They were newly diagnosed with MM and not eligible for stem cell transplant.
Patients were randomized to receive Rd in 28-day cycles until disease progression (n=535), Rd18 for 72 weeks (n=541), or MPT for 72 weeks (n=547).
Response
In the intent-to-treat population, the overall response rate was 81% for the continuous Rd group, 79% for the Rd18 group, and 67% in the MPT group. The complete response rates were 21%, 20%, and 12%, respectively.
The median duration of response was 32 months (range, 26-37) in the continuous Rd group, 22 months (range, 19-23) in the Rd18 group, and 22 months (range, 20-25) in the MPT group.
PFS and OS
The median PFS was 26.0 months in the continuous Rd group, 21.0 months in the Rd18 group, and 21.9 months in the MPT group. At 4 years, the PFS rate was 33%, 14%, and 13%, respectively.
The hazard ratio (HR) for continuous Rd vs MPT was 0.69. The HR for continuous Rd vs Rd18 was 0.71. And the HR for Rd18 vs MPT was 0.99.
The median OS was 58.9 months in the continuous Rd group, 56.7 months in the Rd18 group, and 48.5 months in the MPT group. At 4 years, the OS rate was 60%, 57%, and 51%, respectively.
The HR for continuous Rd vs MPT was 0.75. The HR for continuous Rd vs Rd18 was 0.91. And the HR for Rd18 vs MPT was 0.83.
Safety
The most frequent grade 3/4 hematologic treatment-emergent adverse events were neutropenia and anemia. The rate of grade 3/4 neutropenia was higher in the MPT group than the continuous Rd or Rd18 groups.
Infections were the most common grade 3/4 non-hematologic treatment-emergent adverse events. The rate of grade 3/4 infections was higher in the Rd groups than the MPT group.
Grade 3/4 peripheral sensory neuropathy was less frequent in the continuous Rd and Rd18 groups than the MPT group.
The incidence of invasive second primary malignancy was 4% in the continuous Rd group, 6% in the Rd18 group, and 6% in the MPT group. ![]()

Photo courtesy of Celgene
Updated trial results support continuous treatment with lenalidomide and low-dose dexamethasone (Rd) as a standard of care for patients of all ages who have newly diagnosed multiple myeloma (MM) and are ineligible for stem cell transplant, according to researchers.
In this phase 3 trial, patients who received continuous Rd (until disease progression) had better progression-free survival (PFS) and overall survival (OS) than patients who received 18 cycles of Rd (Rd18) or a combination of melphalan, prednisone, and thalidomide (MPT).
Updated results from this study, known as the FIRST trial, were published in the Journal of Clinical Oncology.
Results were previously published in NEJM in 2014. The study was supported by Intergroupe Francophone du Myélome and Celgene Corporation, the makers of lenalidomide.
Thierry Facon, MD, of Centre Hospitalier Regional Universitaire de Lille in France, and his colleagues enrolled 1623 patients on this trial. They were newly diagnosed with MM and not eligible for stem cell transplant.
Patients were randomized to receive Rd in 28-day cycles until disease progression (n=535), Rd18 for 72 weeks (n=541), or MPT for 72 weeks (n=547).
Response
In the intent-to-treat population, the overall response rate was 81% for the continuous Rd group, 79% for the Rd18 group, and 67% in the MPT group. The complete response rates were 21%, 20%, and 12%, respectively.
The median duration of response was 32 months (range, 26-37) in the continuous Rd group, 22 months (range, 19-23) in the Rd18 group, and 22 months (range, 20-25) in the MPT group.
PFS and OS
The median PFS was 26.0 months in the continuous Rd group, 21.0 months in the Rd18 group, and 21.9 months in the MPT group. At 4 years, the PFS rate was 33%, 14%, and 13%, respectively.
The hazard ratio (HR) for continuous Rd vs MPT was 0.69. The HR for continuous Rd vs Rd18 was 0.71. And the HR for Rd18 vs MPT was 0.99.
The median OS was 58.9 months in the continuous Rd group, 56.7 months in the Rd18 group, and 48.5 months in the MPT group. At 4 years, the OS rate was 60%, 57%, and 51%, respectively.
The HR for continuous Rd vs MPT was 0.75. The HR for continuous Rd vs Rd18 was 0.91. And the HR for Rd18 vs MPT was 0.83.
Safety
The most frequent grade 3/4 hematologic treatment-emergent adverse events were neutropenia and anemia. The rate of grade 3/4 neutropenia was higher in the MPT group than the continuous Rd or Rd18 groups.
Infections were the most common grade 3/4 non-hematologic treatment-emergent adverse events. The rate of grade 3/4 infections was higher in the Rd groups than the MPT group.
Grade 3/4 peripheral sensory neuropathy was less frequent in the continuous Rd and Rd18 groups than the MPT group.
The incidence of invasive second primary malignancy was 4% in the continuous Rd group, 6% in the Rd18 group, and 6% in the MPT group.
Rethinking testing in multiple myeloma
NEW YORK—As the number of therapeutic options for multiple myeloma (MM) increases, so too does the need to reassess prognostic markers for the disease, according to a speaker at Lymphoma & Myeloma 2016.
“A good prognosticator for one patient may have little meaning for another patient,” said Scott Ely, MD, of Weill Cornell Medicine in New York, New York.
“It’s really important before doing any testing to ask, ‘Will the result of this test affect patient care?’”
To answer this question, Dr Ely reviewed the different testing methods used in MM patients and explained the advantages of each.
“[I]t’s really important to understand that a lot of methods are really great for research but don’t work or are not feasible for real-life diagnostic purposes,” he added.
Dr Ely also said it’s important to consider who wants the data, how much the test costs, and who will pay for it, keeping in mind that, these days, the patient’s share of the bill is increasing.
Dr Ely stressed that, until more precise targets or a better understanding of drug mechanisms exist, clinical features—patient age, performance status or frailty, renal function, and disease stage—remain the most important prognosticators.
“But still, 2 patients in the same box based on clinical features will often have very different outcomes,” he said. “So in addition to clinical factors, we need prognosticators for tumor cell behavior. We need to know how fast they are growing and how they will respond to treatment.”
Methods to assess myeloma cell proliferation
Cytogenetics (FISH), gene array technology, and genomics using next-generation sequencing can provide some information, but they are not necessarily good methods to assess proliferation, Dr Ely explained.
To determine the proliferation rate of a patient’s cancer, you can look at tens of thousands of genes by gene array, he said, “or you can just look at one thing, which is Ki67.”
If the cell has Ki67, it’s proliferating, and if it doesn’t have Ki67, it’s not.
“Often, looking at all the other upstream molecules can be confusing and even misleading,” he noted. “So Ki67 is the best way to look for proliferation when it comes to myeloma.”
Other methods include the plasma cell labeling index (PCLI), gene expression profiling, flow cytometry, and multiplex immunohistochemistry (mIHC).
Dr Ely, as a hematopathologist, has found IHC to be the best method to determine proliferation, most likely because the other methods use bone marrow aspirate and IHC uses core biopsy of histologic sections.
It’s the gold standard, he said, for determining the percentage of plasma cells because core biopsy takes a “complete, intact piece of marrow that’s truly representative of what’s going on in the patient.”
In a study of more than 350 bone marrow samples comparing core biopsy with aspirate smears, plasma cells were under-represented in approximately half the aspirate specimens by about 20%.
In addition, Dr Ely noted that myeloma cells die very quickly once they are removed from the stroma.
“So if you take myeloma cells out as an aspirate,” he said, “myeloma cells die and others survive.”
And if the aspirate is sent overnight to the lab, the number of plasma cells in the specimen will already be reduced when the lab gets it.
Aspirates are best for leukemia and myelodysplastic syndromes, Dr Ely said, while core biopsies are best for lymphoma and myeloma.
Plasma cell proliferation indices
Proliferation is a myeloma-defining criterion, Dr Ely said. It predicts an 80% probability of progression in 2 years.
And PCLI has shown conclusively that plasma cell proliferation is a good prognosticator in all types of myeloma patients. However, it is not really feasible to use or easy to perform.
On the other hand, core biopsy combined with IHC is a feasible way of measuring plasma cell proliferation for routine clinical use.
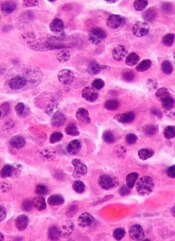
Using standard IHC, it’s difficult to distinguish proliferating from non-proliferating cells, Dr Ely said.
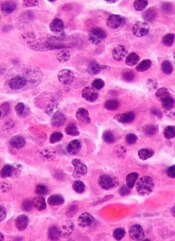
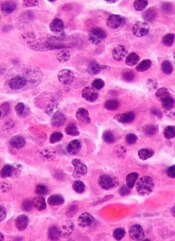
“The solution to this problem is multiplex IHC,” he said, using 3 stains—red for CD138 (the plasma cell marker), brown for Ki67 (the proliferation marker), and blue as a negative nuclear counter stain.
A red membrane around the stained cell indicates a myeloma cell. Non-proliferating MM cells have blue nuclei, and proliferating MM cells have brown nuclei.
This assay is called the plasma cell proliferation index (PCPI).
“[A]ny lab that can do standard IHC can do multiplex IHC,” Dr Ely added.
It uses the same machines, the same reagents, the same expertise, and it’s easy to set up.
Validation studies
Dr Ely and his colleagues performed extensive laboratory validation to make sure the new PCPI correlated with the old PCLI.
They also performed 3 clinical validation studies, the first in bone marrow transplant patients. The investigators followed the patients for 12 years and found the PCPI correlated with survival.
The investigators performed a second clinical validation in 151 newly diagnosed patients. On multivariate analysis, the team found PCPI to be an independent prognostic indicator.
Each 1% increase in PCPI was associated with a 3% increased risk of disease progression (hazard ratio=1.03, 95% CI, 1.01-1.05, P=0.02).
The third clinical validation the investigators conducted was a retrospective cohort study in which they evaluated the effect of rising PCPI at relapse in 37 patients. The team defined rising PCPI as a 5% or greater increase in plasma cells.
Nineteen patients had a rising PCPI, and 17 patients had stable or decreased PCPI.
Patients with a rising PCPI at relapse had a shorter median overall survival than patients with stable or decreased PCPI—72 months and not reached, respectively (P=0.0069).
Patients with a rising PCPI also had a shorter median progression-free survival on first post-relapse treatment compared to patients with stable or decreased PCPI—25 months and 47 months, respectively (P=0.036).
“It’s also important to note that if you’re getting high-risk by PCPI plus β2-microglobulin albumin, I’d advise that, for all high-risk patients, getting the cytogenetics doesn’t really help,” Dr Ely said
Three patients considered high-risk by cytogenetics were standard-risk by PCPI plus β2 microglobulin.
“So we found that cytogenetics isn’t really adding anything except the cost,” Dr Ely asserted.
Other labs are now using PCPI for prognostication, he noted, adding, “We hope PCPI will be incorporated into the International Myeloma Working Group diagnosis of MM.”
NEW YORK—As the number of therapeutic options for multiple myeloma (MM) increases, so too does the need to reassess prognostic markers for the disease, according to a speaker at Lymphoma & Myeloma 2016.
“A good prognosticator for one patient may have little meaning for another patient,” said Scott Ely, MD, of Weill Cornell Medicine in New York, New York.
“It’s really important before doing any testing to ask, ‘Will the result of this test affect patient care?’”
To answer this question, Dr Ely reviewed the different testing methods used in MM patients and explained the advantages of each.
“[I]t’s really important to understand that a lot of methods are really great for research but don’t work or are not feasible for real-life diagnostic purposes,” he added.
Dr Ely also said it’s important to consider who wants the data, how much the test costs, and who will pay for it, keeping in mind that, these days, the patient’s share of the bill is increasing.
Dr Ely stressed that, until more precise targets or a better understanding of drug mechanisms exist, clinical features—patient age, performance status or frailty, renal function, and disease stage—remain the most important prognosticators.
“But still, 2 patients in the same box based on clinical features will often have very different outcomes,” he said. “So in addition to clinical factors, we need prognosticators for tumor cell behavior. We need to know how fast they are growing and how they will respond to treatment.”
Methods to assess myeloma cell proliferation
Cytogenetics (FISH), gene array technology, and genomics using next-generation sequencing can provide some information, but they are not necessarily good methods to assess proliferation, Dr Ely explained.
To determine the proliferation rate of a patient’s cancer, you can look at tens of thousands of genes by gene array, he said, “or you can just look at one thing, which is Ki67.”
If the cell has Ki67, it’s proliferating, and if it doesn’t have Ki67, it’s not.
“Often, looking at all the other upstream molecules can be confusing and even misleading,” he noted. “So Ki67 is the best way to look for proliferation when it comes to myeloma.”
Other methods include the plasma cell labeling index (PCLI), gene expression profiling, flow cytometry, and multiplex immunohistochemistry (mIHC).
Dr Ely, as a hematopathologist, has found IHC to be the best method to determine proliferation, most likely because the other methods use bone marrow aspirate and IHC uses core biopsy of histologic sections.
It’s the gold standard, he said, for determining the percentage of plasma cells because core biopsy takes a “complete, intact piece of marrow that’s truly representative of what’s going on in the patient.”
In a study of more than 350 bone marrow samples comparing core biopsy with aspirate smears, plasma cells were under-represented in approximately half the aspirate specimens by about 20%.
In addition, Dr Ely noted that myeloma cells die very quickly once they are removed from the stroma.
“So if you take myeloma cells out as an aspirate,” he said, “myeloma cells die and others survive.”
And if the aspirate is sent overnight to the lab, the number of plasma cells in the specimen will already be reduced when the lab gets it.
Aspirates are best for leukemia and myelodysplastic syndromes, Dr Ely said, while core biopsies are best for lymphoma and myeloma.
Plasma cell proliferation indices
Proliferation is a myeloma-defining criterion, Dr Ely said. It predicts an 80% probability of progression in 2 years.
And PCLI has shown conclusively that plasma cell proliferation is a good prognosticator in all types of myeloma patients. However, it is not really feasible to use or easy to perform.
On the other hand, core biopsy combined with IHC is a feasible way of measuring plasma cell proliferation for routine clinical use.
Using standard IHC, it’s difficult to distinguish proliferating from non-proliferating cells, Dr Ely said.
“The solution to this problem is multiplex IHC,” he said, using 3 stains—red for CD138 (the plasma cell marker), brown for Ki67 (the proliferation marker), and blue as a negative nuclear counter stain.
A red membrane around the stained cell indicates a myeloma cell. Non-proliferating MM cells have blue nuclei, and proliferating MM cells have brown nuclei.
This assay is called the plasma cell proliferation index (PCPI).
“[A]ny lab that can do standard IHC can do multiplex IHC,” Dr Ely added.
It uses the same machines, the same reagents, the same expertise, and it’s easy to set up.
Validation studies
Dr Ely and his colleagues performed extensive laboratory validation to make sure the new PCPI correlated with the old PCLI.
They also performed 3 clinical validation studies, the first in bone marrow transplant patients. The investigators followed the patients for 12 years and found the PCPI correlated with survival.
The investigators performed a second clinical validation in 151 newly diagnosed patients. On multivariate analysis, the team found PCPI to be an independent prognostic indicator.
Each 1% increase in PCPI was associated with a 3% increased risk of disease progression (hazard ratio=1.03, 95% CI, 1.01-1.05, P=0.02).
The third clinical validation the investigators conducted was a retrospective cohort study in which they evaluated the effect of rising PCPI at relapse in 37 patients. The team defined rising PCPI as a 5% or greater increase in plasma cells.
Nineteen patients had a rising PCPI, and 17 patients had stable or decreased PCPI.
Patients with a rising PCPI at relapse had a shorter median overall survival than patients with stable or decreased PCPI—72 months and not reached, respectively (P=0.0069).
Patients with a rising PCPI also had a shorter median progression-free survival on first post-relapse treatment compared to patients with stable or decreased PCPI—25 months and 47 months, respectively (P=0.036).
“It’s also important to note that if you’re getting high-risk by PCPI plus β2-microglobulin albumin, I’d advise that, for all high-risk patients, getting the cytogenetics doesn’t really help,” Dr Ely said
Three patients considered high-risk by cytogenetics were standard-risk by PCPI plus β2 microglobulin.
“So we found that cytogenetics isn’t really adding anything except the cost,” Dr Ely asserted.
Other labs are now using PCPI for prognostication, he noted, adding, “We hope PCPI will be incorporated into the International Myeloma Working Group diagnosis of MM.”
NEW YORK—As the number of therapeutic options for multiple myeloma (MM) increases, so too does the need to reassess prognostic markers for the disease, according to a speaker at Lymphoma & Myeloma 2016.
“A good prognosticator for one patient may have little meaning for another patient,” said Scott Ely, MD, of Weill Cornell Medicine in New York, New York.
“It’s really important before doing any testing to ask, ‘Will the result of this test affect patient care?’”
To answer this question, Dr Ely reviewed the different testing methods used in MM patients and explained the advantages of each.
“[I]t’s really important to understand that a lot of methods are really great for research but don’t work or are not feasible for real-life diagnostic purposes,” he added.
Dr Ely also said it’s important to consider who wants the data, how much the test costs, and who will pay for it, keeping in mind that, these days, the patient’s share of the bill is increasing.
Dr Ely stressed that, until more precise targets or a better understanding of drug mechanisms exist, clinical features—patient age, performance status or frailty, renal function, and disease stage—remain the most important prognosticators.
“But still, 2 patients in the same box based on clinical features will often have very different outcomes,” he said. “So in addition to clinical factors, we need prognosticators for tumor cell behavior. We need to know how fast they are growing and how they will respond to treatment.”
Methods to assess myeloma cell proliferation
Cytogenetics (FISH), gene array technology, and genomics using next-generation sequencing can provide some information, but they are not necessarily good methods to assess proliferation, Dr Ely explained.
To determine the proliferation rate of a patient’s cancer, you can look at tens of thousands of genes by gene array, he said, “or you can just look at one thing, which is Ki67.”
If the cell has Ki67, it’s proliferating, and if it doesn’t have Ki67, it’s not.
“Often, looking at all the other upstream molecules can be confusing and even misleading,” he noted. “So Ki67 is the best way to look for proliferation when it comes to myeloma.”
Other methods include the plasma cell labeling index (PCLI), gene expression profiling, flow cytometry, and multiplex immunohistochemistry (mIHC).
Dr Ely, as a hematopathologist, has found IHC to be the best method to determine proliferation, most likely because the other methods use bone marrow aspirate and IHC uses core biopsy of histologic sections.
It’s the gold standard, he said, for determining the percentage of plasma cells because core biopsy takes a “complete, intact piece of marrow that’s truly representative of what’s going on in the patient.”
In a study of more than 350 bone marrow samples comparing core biopsy with aspirate smears, plasma cells were under-represented in approximately half the aspirate specimens by about 20%.
In addition, Dr Ely noted that myeloma cells die very quickly once they are removed from the stroma.
“So if you take myeloma cells out as an aspirate,” he said, “myeloma cells die and others survive.”
And if the aspirate is sent overnight to the lab, the number of plasma cells in the specimen will already be reduced when the lab gets it.
Aspirates are best for leukemia and myelodysplastic syndromes, Dr Ely said, while core biopsies are best for lymphoma and myeloma.
Plasma cell proliferation indices
Proliferation is a myeloma-defining criterion, Dr Ely said. It predicts an 80% probability of progression in 2 years.
And PCLI has shown conclusively that plasma cell proliferation is a good prognosticator in all types of myeloma patients. However, it is not really feasible to use or easy to perform.
On the other hand, core biopsy combined with IHC is a feasible way of measuring plasma cell proliferation for routine clinical use.
Using standard IHC, it’s difficult to distinguish proliferating from non-proliferating cells, Dr Ely said.
“The solution to this problem is multiplex IHC,” he said, using 3 stains—red for CD138 (the plasma cell marker), brown for Ki67 (the proliferation marker), and blue as a negative nuclear counter stain.
A red membrane around the stained cell indicates a myeloma cell. Non-proliferating MM cells have blue nuclei, and proliferating MM cells have brown nuclei.
This assay is called the plasma cell proliferation index (PCPI).
“[A]ny lab that can do standard IHC can do multiplex IHC,” Dr Ely added.
It uses the same machines, the same reagents, the same expertise, and it’s easy to set up.
Validation studies
Dr Ely and his colleagues performed extensive laboratory validation to make sure the new PCPI correlated with the old PCLI.
They also performed 3 clinical validation studies, the first in bone marrow transplant patients. The investigators followed the patients for 12 years and found the PCPI correlated with survival.
The investigators performed a second clinical validation in 151 newly diagnosed patients. On multivariate analysis, the team found PCPI to be an independent prognostic indicator.
Each 1% increase in PCPI was associated with a 3% increased risk of disease progression (hazard ratio=1.03, 95% CI, 1.01-1.05, P=0.02).
The third clinical validation the investigators conducted was a retrospective cohort study in which they evaluated the effect of rising PCPI at relapse in 37 patients. The team defined rising PCPI as a 5% or greater increase in plasma cells.
Nineteen patients had a rising PCPI, and 17 patients had stable or decreased PCPI.
Patients with a rising PCPI at relapse had a shorter median overall survival than patients with stable or decreased PCPI—72 months and not reached, respectively (P=0.0069).
Patients with a rising PCPI also had a shorter median progression-free survival on first post-relapse treatment compared to patients with stable or decreased PCPI—25 months and 47 months, respectively (P=0.036).
“It’s also important to note that if you’re getting high-risk by PCPI plus β2-microglobulin albumin, I’d advise that, for all high-risk patients, getting the cytogenetics doesn’t really help,” Dr Ely said
Three patients considered high-risk by cytogenetics were standard-risk by PCPI plus β2 microglobulin.
“So we found that cytogenetics isn’t really adding anything except the cost,” Dr Ely asserted.
Other labs are now using PCPI for prognostication, he noted, adding, “We hope PCPI will be incorporated into the International Myeloma Working Group diagnosis of MM.”
Treatment facility volume linked to survival in MM

Photo courtesy of the CDC
Patients with multiple myeloma (MM) are more likely to live longer if they are treated at a medical center where the staff has more experience with the disease, according to research published in the Journal of Clinical Oncology.
The study showed that patients treated at medical centers seeing 10 new MM patients per year had a 20% higher risk of death than patients treated at centers seeing 40 new MM patients per year.
Most cancer treatment centers in the US see fewer than 10 new MM patients per year.
“It is very difficult to be proficient when doctors are seeing only 1 or 2 new cases of multiple myeloma per year,” said study author Ronald Go, MD, of the Mayo Clinic in Rochester, Minnesota.
“Studies on cancer surgery have shown the more experience the center or practitioner has, the better the outcome. We wanted to see if volume matters when it comes to nonsurgical treatment of rare cancers such as multiple myeloma.”
To investigate, Dr Go and his colleagues used the National Cancer Database, examining outcomes for 94,722 newly diagnosed MM patients treated at 1333 facilities between 2003 and 2011.
The researchers grouped the facilities into quartiles according to the volume of MM patients treated there each year.
The mean number of MM patients treated per year was:
- Less than 3.6 for quartile 1 (Q1)
- 3.6 to 6.1 for Q2
- 6.1 to 10.3 for Q3
- More than 10.3 for Q4.
The majority of patients (60.3%) were treated in Q4 facilities. For all facilities, the median number of new MM patients per year was 6.1 (range, 3.6 to 10.3). The mean was 8.8 ± 9.9.
The researchers calculated the relationship between MM patient volume at these facilities and patient mortality, adjusting for demographic characteristics, socioeconomic factors, geographic factors, comorbidities, and year of diagnosis.
Outcomes
The unadjusted median overall survival was 26.9 months for patients treated at Q1 facilities, 29.1 months for Q2, 31.9 months for Q3, and 49.1 months for Q4 (P<0.001).
The 1-year mortality rate was 33.5% for patients treated at Q1 facilities, 32.3% for Q2, 30.7% for Q3, and 21.9% for Q4.
The researchers’ multivariable analysis showed that facility volume was independently associated with all-cause mortality.
Patients treated at the lower-quartile facilities had a higher risk of death than patients treated at Q4 facilities. The hazard ratios were 1.12 for patients at Q3 facilities, 1.12 for Q2, and 1.22 for Q1.
The researchers performed another analysis in which volume was treated as a continuous variable, and they compared various volume sizes to a reference volume of 10 patients per year.
Compared with facilities treating 10 new MM patients per year, facilities treating 20 MM patients per year had roughly 10% lower overall mortality rates.
Facilities treating 30 MM patients per year had about 15% lower mortality rates. And facilities treating 40 MM patients per year had 20% lower overall mortality rates.

Photo courtesy of the CDC
Patients with multiple myeloma (MM) are more likely to live longer if they are treated at a medical center where the staff has more experience with the disease, according to research published in the Journal of Clinical Oncology.
The study showed that patients treated at medical centers seeing 10 new MM patients per year had a 20% higher risk of death than patients treated at centers seeing 40 new MM patients per year.
Most cancer treatment centers in the US see fewer than 10 new MM patients per year.
“It is very difficult to be proficient when doctors are seeing only 1 or 2 new cases of multiple myeloma per year,” said study author Ronald Go, MD, of the Mayo Clinic in Rochester, Minnesota.
“Studies on cancer surgery have shown the more experience the center or practitioner has, the better the outcome. We wanted to see if volume matters when it comes to nonsurgical treatment of rare cancers such as multiple myeloma.”
To investigate, Dr Go and his colleagues used the National Cancer Database, examining outcomes for 94,722 newly diagnosed MM patients treated at 1333 facilities between 2003 and 2011.
The researchers grouped the facilities into quartiles according to the volume of MM patients treated there each year.
The mean number of MM patients treated per year was:
- Less than 3.6 for quartile 1 (Q1)
- 3.6 to 6.1 for Q2
- 6.1 to 10.3 for Q3
- More than 10.3 for Q4.
The majority of patients (60.3%) were treated in Q4 facilities. For all facilities, the median number of new MM patients per year was 6.1 (range, 3.6 to 10.3). The mean was 8.8 ± 9.9.
The researchers calculated the relationship between MM patient volume at these facilities and patient mortality, adjusting for demographic characteristics, socioeconomic factors, geographic factors, comorbidities, and year of diagnosis.
Outcomes
The unadjusted median overall survival was 26.9 months for patients treated at Q1 facilities, 29.1 months for Q2, 31.9 months for Q3, and 49.1 months for Q4 (P<0.001).
The 1-year mortality rate was 33.5% for patients treated at Q1 facilities, 32.3% for Q2, 30.7% for Q3, and 21.9% for Q4.
The researchers’ multivariable analysis showed that facility volume was independently associated with all-cause mortality.
Patients treated at the lower-quartile facilities had a higher risk of death than patients treated at Q4 facilities. The hazard ratios were 1.12 for patients at Q3 facilities, 1.12 for Q2, and 1.22 for Q1.
The researchers performed another analysis in which volume was treated as a continuous variable, and they compared various volume sizes to a reference volume of 10 patients per year.
Compared with facilities treating 10 new MM patients per year, facilities treating 20 MM patients per year had roughly 10% lower overall mortality rates.
Facilities treating 30 MM patients per year had about 15% lower mortality rates. And facilities treating 40 MM patients per year had 20% lower overall mortality rates.

Photo courtesy of the CDC
Patients with multiple myeloma (MM) are more likely to live longer if they are treated at a medical center where the staff has more experience with the disease, according to research published in the Journal of Clinical Oncology.
The study showed that patients treated at medical centers seeing 10 new MM patients per year had a 20% higher risk of death than patients treated at centers seeing 40 new MM patients per year.
Most cancer treatment centers in the US see fewer than 10 new MM patients per year.
“It is very difficult to be proficient when doctors are seeing only 1 or 2 new cases of multiple myeloma per year,” said study author Ronald Go, MD, of the Mayo Clinic in Rochester, Minnesota.
“Studies on cancer surgery have shown the more experience the center or practitioner has, the better the outcome. We wanted to see if volume matters when it comes to nonsurgical treatment of rare cancers such as multiple myeloma.”
To investigate, Dr Go and his colleagues used the National Cancer Database, examining outcomes for 94,722 newly diagnosed MM patients treated at 1333 facilities between 2003 and 2011.
The researchers grouped the facilities into quartiles according to the volume of MM patients treated there each year.
The mean number of MM patients treated per year was:
- Less than 3.6 for quartile 1 (Q1)
- 3.6 to 6.1 for Q2
- 6.1 to 10.3 for Q3
- More than 10.3 for Q4.
The majority of patients (60.3%) were treated in Q4 facilities. For all facilities, the median number of new MM patients per year was 6.1 (range, 3.6 to 10.3). The mean was 8.8 ± 9.9.
The researchers calculated the relationship between MM patient volume at these facilities and patient mortality, adjusting for demographic characteristics, socioeconomic factors, geographic factors, comorbidities, and year of diagnosis.
Outcomes
The unadjusted median overall survival was 26.9 months for patients treated at Q1 facilities, 29.1 months for Q2, 31.9 months for Q3, and 49.1 months for Q4 (P<0.001).
The 1-year mortality rate was 33.5% for patients treated at Q1 facilities, 32.3% for Q2, 30.7% for Q3, and 21.9% for Q4.
The researchers’ multivariable analysis showed that facility volume was independently associated with all-cause mortality.
Patients treated at the lower-quartile facilities had a higher risk of death than patients treated at Q4 facilities. The hazard ratios were 1.12 for patients at Q3 facilities, 1.12 for Q2, and 1.22 for Q1.
The researchers performed another analysis in which volume was treated as a continuous variable, and they compared various volume sizes to a reference volume of 10 patients per year.
Compared with facilities treating 10 new MM patients per year, facilities treating 20 MM patients per year had roughly 10% lower overall mortality rates.
Facilities treating 30 MM patients per year had about 15% lower mortality rates. And facilities treating 40 MM patients per year had 20% lower overall mortality rates.