User login
Cord blood cell infusions reduce cGVHD incidence
Repeat infusions of mesenchymal stromal stem cells appear to inhibit the development of chronic graft-versus-host disease (cGVHD) in patients who have undergone an allogeneic stem cell transplant.
The 2-year cumulative incidence of cGVHD among those randomized to receive repeated infusions of umbilical cord–derived mesenchymal stromal cells (MSCs) was half that of controls treated with a saline placebo, based on results from a randomized phase II, double blind trial in 124 patients with hematologic malignancies who underwent an HLA-haploidentical allogeneic hematopoietic stem cell transplantation (HSCT).
“Our goal was to minimize the incidence of cGVHD, reduce the severity of cGVHD, and demonstrate the safety of MSC infusions. We performed repeated infusions of MSCs once a month for a total of four rounds for each patient. Over the median 47-month posttransplantation period, the incidence of cGVHD was lower in the MSCs group than in the non-MSCs control group,” Lei Gao, MD, of the Third Military Medical University in Chongqing, China, and colleagues wrote in the Journal of Clinical Oncology (2016 Jul 11. doi: 10.1200/JCO.2015.65.3642).
Although cGVHD is associated with a reduced risk of leukemia relapse, it is still the leading cause of nonrelapse deaths after HSCT. The incidence of cGVHD is higher among recipients of HLA-haploidentical HSCT, in which the donor and recipient have identical HLA alleles on only one copy of chromosome, than among HLA-matched recipients, who have identical alleles on both copies.
The researchers randomly assigned 124 patients who had undergo HLA-haploidentical HSCT to receive either placebo or MSCs at a dose of 3 x 107 cells/100 mL per month for four cycles beginning 4 months after HSCT
Of the 124 randomized patients, 12 discontinued the study due to cGVHD or disease progression.
The 2-year cumulative incidence of cGVHD among patients treated with MSCs was 27%, compared with 49% for placebo-treated controls (P = .021). Seven patients in the control group but none in the MSC-treated group developed typical lung cGVHD (P = .047).
The investigators also observed increases in memory B lymphocytes and regulatory T cells, and in the ratio of type 1 to type 2 T-helper cells, as well as a decrease in natural killer cells.
The finding that the MSC infusions increased the number of regulatory T cells while decreasing the incidence of cGVHD suggests that regulatory T cells play an inhibitory role, the investigators said.
The study was supported by the Chinese Academy of Sciences. Chinese National Natural Science Foundation, and other Chinese government grants. The authors reported having no relationships to disclose.
On the basis of the Gao et al. study, future investigations of cGVHD prophylaxis using MSCs should be explored. Approximately 90% of their population was younger than age 40, however, and it will be interesting to observe if this strategy is effective in older adults. The permutations and combinations for using different cell sources for deriving the MSCs, and in the context of different neoplastic disease, type and stage, conditioning regimen intensity, GVHD prophylaxis, graft and donor source, among other variables, are daunting. Nonetheless, the results of their trial encourage us to further explore this approach.
Hillard M. Lazarus, MD, is with Case Western Reserve University, Cleveland. Steven Z. Pavletic, MD, is with the National Institutes of Health, Bethesda, Md. Their comments were taken from an accompanying editorial (J Clin Oncol. 2016 Jul 11. doi: 10.1200/JCO.2016.67.7344).
On the basis of the Gao et al. study, future investigations of cGVHD prophylaxis using MSCs should be explored. Approximately 90% of their population was younger than age 40, however, and it will be interesting to observe if this strategy is effective in older adults. The permutations and combinations for using different cell sources for deriving the MSCs, and in the context of different neoplastic disease, type and stage, conditioning regimen intensity, GVHD prophylaxis, graft and donor source, among other variables, are daunting. Nonetheless, the results of their trial encourage us to further explore this approach.
Hillard M. Lazarus, MD, is with Case Western Reserve University, Cleveland. Steven Z. Pavletic, MD, is with the National Institutes of Health, Bethesda, Md. Their comments were taken from an accompanying editorial (J Clin Oncol. 2016 Jul 11. doi: 10.1200/JCO.2016.67.7344).
On the basis of the Gao et al. study, future investigations of cGVHD prophylaxis using MSCs should be explored. Approximately 90% of their population was younger than age 40, however, and it will be interesting to observe if this strategy is effective in older adults. The permutations and combinations for using different cell sources for deriving the MSCs, and in the context of different neoplastic disease, type and stage, conditioning regimen intensity, GVHD prophylaxis, graft and donor source, among other variables, are daunting. Nonetheless, the results of their trial encourage us to further explore this approach.
Hillard M. Lazarus, MD, is with Case Western Reserve University, Cleveland. Steven Z. Pavletic, MD, is with the National Institutes of Health, Bethesda, Md. Their comments were taken from an accompanying editorial (J Clin Oncol. 2016 Jul 11. doi: 10.1200/JCO.2016.67.7344).
Repeat infusions of mesenchymal stromal stem cells appear to inhibit the development of chronic graft-versus-host disease (cGVHD) in patients who have undergone an allogeneic stem cell transplant.
The 2-year cumulative incidence of cGVHD among those randomized to receive repeated infusions of umbilical cord–derived mesenchymal stromal cells (MSCs) was half that of controls treated with a saline placebo, based on results from a randomized phase II, double blind trial in 124 patients with hematologic malignancies who underwent an HLA-haploidentical allogeneic hematopoietic stem cell transplantation (HSCT).
“Our goal was to minimize the incidence of cGVHD, reduce the severity of cGVHD, and demonstrate the safety of MSC infusions. We performed repeated infusions of MSCs once a month for a total of four rounds for each patient. Over the median 47-month posttransplantation period, the incidence of cGVHD was lower in the MSCs group than in the non-MSCs control group,” Lei Gao, MD, of the Third Military Medical University in Chongqing, China, and colleagues wrote in the Journal of Clinical Oncology (2016 Jul 11. doi: 10.1200/JCO.2015.65.3642).
Although cGVHD is associated with a reduced risk of leukemia relapse, it is still the leading cause of nonrelapse deaths after HSCT. The incidence of cGVHD is higher among recipients of HLA-haploidentical HSCT, in which the donor and recipient have identical HLA alleles on only one copy of chromosome, than among HLA-matched recipients, who have identical alleles on both copies.
The researchers randomly assigned 124 patients who had undergo HLA-haploidentical HSCT to receive either placebo or MSCs at a dose of 3 x 107 cells/100 mL per month for four cycles beginning 4 months after HSCT
Of the 124 randomized patients, 12 discontinued the study due to cGVHD or disease progression.
The 2-year cumulative incidence of cGVHD among patients treated with MSCs was 27%, compared with 49% for placebo-treated controls (P = .021). Seven patients in the control group but none in the MSC-treated group developed typical lung cGVHD (P = .047).
The investigators also observed increases in memory B lymphocytes and regulatory T cells, and in the ratio of type 1 to type 2 T-helper cells, as well as a decrease in natural killer cells.
The finding that the MSC infusions increased the number of regulatory T cells while decreasing the incidence of cGVHD suggests that regulatory T cells play an inhibitory role, the investigators said.
The study was supported by the Chinese Academy of Sciences. Chinese National Natural Science Foundation, and other Chinese government grants. The authors reported having no relationships to disclose.
Repeat infusions of mesenchymal stromal stem cells appear to inhibit the development of chronic graft-versus-host disease (cGVHD) in patients who have undergone an allogeneic stem cell transplant.
The 2-year cumulative incidence of cGVHD among those randomized to receive repeated infusions of umbilical cord–derived mesenchymal stromal cells (MSCs) was half that of controls treated with a saline placebo, based on results from a randomized phase II, double blind trial in 124 patients with hematologic malignancies who underwent an HLA-haploidentical allogeneic hematopoietic stem cell transplantation (HSCT).
“Our goal was to minimize the incidence of cGVHD, reduce the severity of cGVHD, and demonstrate the safety of MSC infusions. We performed repeated infusions of MSCs once a month for a total of four rounds for each patient. Over the median 47-month posttransplantation period, the incidence of cGVHD was lower in the MSCs group than in the non-MSCs control group,” Lei Gao, MD, of the Third Military Medical University in Chongqing, China, and colleagues wrote in the Journal of Clinical Oncology (2016 Jul 11. doi: 10.1200/JCO.2015.65.3642).
Although cGVHD is associated with a reduced risk of leukemia relapse, it is still the leading cause of nonrelapse deaths after HSCT. The incidence of cGVHD is higher among recipients of HLA-haploidentical HSCT, in which the donor and recipient have identical HLA alleles on only one copy of chromosome, than among HLA-matched recipients, who have identical alleles on both copies.
The researchers randomly assigned 124 patients who had undergo HLA-haploidentical HSCT to receive either placebo or MSCs at a dose of 3 x 107 cells/100 mL per month for four cycles beginning 4 months after HSCT
Of the 124 randomized patients, 12 discontinued the study due to cGVHD or disease progression.
The 2-year cumulative incidence of cGVHD among patients treated with MSCs was 27%, compared with 49% for placebo-treated controls (P = .021). Seven patients in the control group but none in the MSC-treated group developed typical lung cGVHD (P = .047).
The investigators also observed increases in memory B lymphocytes and regulatory T cells, and in the ratio of type 1 to type 2 T-helper cells, as well as a decrease in natural killer cells.
The finding that the MSC infusions increased the number of regulatory T cells while decreasing the incidence of cGVHD suggests that regulatory T cells play an inhibitory role, the investigators said.
The study was supported by the Chinese Academy of Sciences. Chinese National Natural Science Foundation, and other Chinese government grants. The authors reported having no relationships to disclose.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Mesenchymal stromal cell infusions may reduce risk of chronic graft-versus-host disease following allogeneic stem cell transplants.
Major finding: The 2-year cumulative incidence of cGVHD among patients treated with MSCs was 27.4%, compared with 49% for placebo-treated controls.
Data source: Randomized, double-blind, controlled trial in 124 patients following HSCT for hematologic malignancies.
Disclosures: The study was supported by the Chinese Academy of Sciences. Chinese National Natural Science Foundation, and other Chinese government grants. The authors reported having no relationships to disclose.
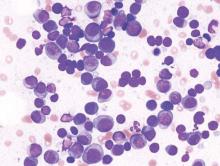
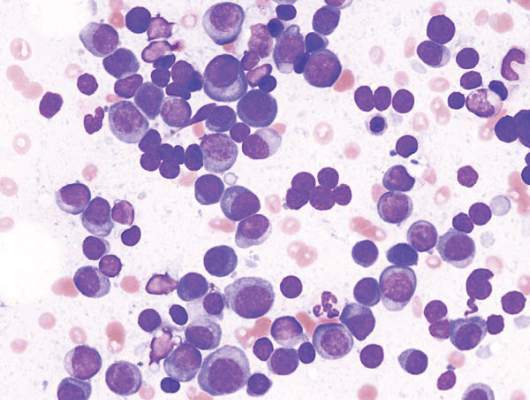
Smoldering multiple myeloma affects 1 in 7 patients
About 1 in 7 cases of multiple myeloma diagnosed in the United States are cases of smoldering disease, according to an analysis of data from the National Cancer Data Base, which represents 70% of cancer cases.
The prevalence of smoldering multiple myeloma varied among various socio- and geodemographic subgroups, but overall survival did not, Aishwarya Ravindran, MBBS, of Mayo Clinic, Rochester, Minn., and colleagues reported at the annual meeting of the American Society of Clinical Oncology. “Our results can be used in the future to study the health care impact of SMM,” the researchers wrote in a poster presentation.
Epidemiologic studies of smoldering multiple myeloma have been limited by the lack of International Classification of Diseases codes specific for smoldering status, the researchers said.
They analyzed 86,327 cases of multiple myeloma, considering socio- and geodemographic subgroups and type of treatment facility. Overall survival was compared for smoldering and active multiple myeloma. The researchers included patients enrolled in the database during 2003-2011; records were examined from the time to initial treatment and they considered reasons for patients not receiving treatment.
Patients who did not require treatment within the first 120 days after diagnosis were considered to have smoldering disease. This group comprised almost 14% of the cases.
The proportion of cases that were smoldering disease did not change significantly during the study period (P = .23 and .34, respectively). Smoldering disease was more likely to be diagnosed among women, black patients, older patients (median age at diagnosis was 67 years), and less educated patients. Smoldering disease was more common in patients with fewer medical comorbidities, those living closer to a treatment facility, and those evaluated for their disease in the Northeast United States. The proportions of cases diagnosed at academic and nonacademic facilities were similar.
The median overall survival for smoldering disease was 63 months; for active disease, 33 months. Overall survival in those with smoldering disease did not differ among the racial groups (P = .27).
The researchers had no financial conflicts.
On Twitter @maryjodales
About 1 in 7 cases of multiple myeloma diagnosed in the United States are cases of smoldering disease, according to an analysis of data from the National Cancer Data Base, which represents 70% of cancer cases.
The prevalence of smoldering multiple myeloma varied among various socio- and geodemographic subgroups, but overall survival did not, Aishwarya Ravindran, MBBS, of Mayo Clinic, Rochester, Minn., and colleagues reported at the annual meeting of the American Society of Clinical Oncology. “Our results can be used in the future to study the health care impact of SMM,” the researchers wrote in a poster presentation.
Epidemiologic studies of smoldering multiple myeloma have been limited by the lack of International Classification of Diseases codes specific for smoldering status, the researchers said.
They analyzed 86,327 cases of multiple myeloma, considering socio- and geodemographic subgroups and type of treatment facility. Overall survival was compared for smoldering and active multiple myeloma. The researchers included patients enrolled in the database during 2003-2011; records were examined from the time to initial treatment and they considered reasons for patients not receiving treatment.
Patients who did not require treatment within the first 120 days after diagnosis were considered to have smoldering disease. This group comprised almost 14% of the cases.
The proportion of cases that were smoldering disease did not change significantly during the study period (P = .23 and .34, respectively). Smoldering disease was more likely to be diagnosed among women, black patients, older patients (median age at diagnosis was 67 years), and less educated patients. Smoldering disease was more common in patients with fewer medical comorbidities, those living closer to a treatment facility, and those evaluated for their disease in the Northeast United States. The proportions of cases diagnosed at academic and nonacademic facilities were similar.
The median overall survival for smoldering disease was 63 months; for active disease, 33 months. Overall survival in those with smoldering disease did not differ among the racial groups (P = .27).
The researchers had no financial conflicts.
On Twitter @maryjodales
About 1 in 7 cases of multiple myeloma diagnosed in the United States are cases of smoldering disease, according to an analysis of data from the National Cancer Data Base, which represents 70% of cancer cases.
The prevalence of smoldering multiple myeloma varied among various socio- and geodemographic subgroups, but overall survival did not, Aishwarya Ravindran, MBBS, of Mayo Clinic, Rochester, Minn., and colleagues reported at the annual meeting of the American Society of Clinical Oncology. “Our results can be used in the future to study the health care impact of SMM,” the researchers wrote in a poster presentation.
Epidemiologic studies of smoldering multiple myeloma have been limited by the lack of International Classification of Diseases codes specific for smoldering status, the researchers said.
They analyzed 86,327 cases of multiple myeloma, considering socio- and geodemographic subgroups and type of treatment facility. Overall survival was compared for smoldering and active multiple myeloma. The researchers included patients enrolled in the database during 2003-2011; records were examined from the time to initial treatment and they considered reasons for patients not receiving treatment.
Patients who did not require treatment within the first 120 days after diagnosis were considered to have smoldering disease. This group comprised almost 14% of the cases.
The proportion of cases that were smoldering disease did not change significantly during the study period (P = .23 and .34, respectively). Smoldering disease was more likely to be diagnosed among women, black patients, older patients (median age at diagnosis was 67 years), and less educated patients. Smoldering disease was more common in patients with fewer medical comorbidities, those living closer to a treatment facility, and those evaluated for their disease in the Northeast United States. The proportions of cases diagnosed at academic and nonacademic facilities were similar.
The median overall survival for smoldering disease was 63 months; for active disease, 33 months. Overall survival in those with smoldering disease did not differ among the racial groups (P = .27).
The researchers had no financial conflicts.
On Twitter @maryjodales
FROM ASCO 2016
Key clinical point: The prevalence of smoldering multiple myeloma varied among various socio- and geodemographic subgroups, but overall survival did not.
Major finding: About 1 in 7 cases of multiple myeloma diagnosed in the United States are cases of smoldering disease.
Data source: At total of 86,327 cases of multiple myeloma from the National Cancer Data Base, which represents 70% of cancer cases.
Disclosures: The researchers had no financial conflicts.
Cancer cell lines predict drug response, study shows

Image from PNAS
A study published in Cell has shown that patient-derived cancer cell lines harbor most of the same genetic changes found in patients’ tumors and could therefore be used to learn how cancers are likely to respond to new drugs.
Researchers believe this discovery could help advance personalized cancer medicine by leading to results that help doctors predict the best available drugs or the most suitable clinical trials for each individual patient.
“We need better ways to figure out which groups of patients are more likely to respond to a new drug before we run complex and expensive clinical trials,” said study author Ultan McDermott, MD, PhD, of the Wellcome Trust Sanger Institute in Cambridge, UK.
“Our research shows that cancer cell lines do capture the molecular alterations found in tumors and so can be predictive of how a tumor will respond to a drug. This means the cell lines could tell us much more about how a tumor is likely to respond to a new drug before we try to test it in patients. We hope this information will ultimately help in the design of clinical trials that target those patients with the greatest likelihood of benefiting from treatment.”
The researchers said this is the first systematic, large-scale study to combine molecular data from patients, cancer cell lines, and drug sensitivity.
For the study, the team looked at genetic mutations known to cause cancer in more than 11,000 patient samples of 29 different cancer types, including acute lymphoblastic leukemia, acute myeloid leukemia, chronic lymphocytic leukemia, chronic myelogenous leukemia, diffuse large B-cell lymphoma, and multiple myeloma.
The researchers built a catalogue of the genetic changes that cause cancer in patients and mapped these alterations onto 1000 cancer cell lines. Next, they tested the cell lines for sensitivity to 265 different cancer drugs to understand which of these changes affect sensitivity.
This revealed that the majority of molecular abnormalities found in patients’ cancers are also found in cancer cells in the laboratory.
The work also showed that many of the molecular abnormalities detected in the thousands of patient samples can, both individually and in combination, have a strong effect on whether a particular drug affects a cancer cell’s survival.
The results suggest cancer cell lines could be better exploited to learn which drugs offer the most effective treatment to which patients.
“If a cell line has the same genetic features as a patient’s tumor, and that cell line responded to a specific drug, we can focus new research on this finding,” said study author Francesco Iorio, PhD, of the European Bioinformatics Institute in Cambridge, UK.
“This could ultimately help assign cancer patients into more precise groups based on how likely they are to respond to therapy. This resource can really help cancer research. Most importantly, it can be used to create tools for doctors to select a clinical trial which is most promising for their cancer patient. That is still a way off, but we are heading in the right direction.” ![]()

Image from PNAS
A study published in Cell has shown that patient-derived cancer cell lines harbor most of the same genetic changes found in patients’ tumors and could therefore be used to learn how cancers are likely to respond to new drugs.
Researchers believe this discovery could help advance personalized cancer medicine by leading to results that help doctors predict the best available drugs or the most suitable clinical trials for each individual patient.
“We need better ways to figure out which groups of patients are more likely to respond to a new drug before we run complex and expensive clinical trials,” said study author Ultan McDermott, MD, PhD, of the Wellcome Trust Sanger Institute in Cambridge, UK.
“Our research shows that cancer cell lines do capture the molecular alterations found in tumors and so can be predictive of how a tumor will respond to a drug. This means the cell lines could tell us much more about how a tumor is likely to respond to a new drug before we try to test it in patients. We hope this information will ultimately help in the design of clinical trials that target those patients with the greatest likelihood of benefiting from treatment.”
The researchers said this is the first systematic, large-scale study to combine molecular data from patients, cancer cell lines, and drug sensitivity.
For the study, the team looked at genetic mutations known to cause cancer in more than 11,000 patient samples of 29 different cancer types, including acute lymphoblastic leukemia, acute myeloid leukemia, chronic lymphocytic leukemia, chronic myelogenous leukemia, diffuse large B-cell lymphoma, and multiple myeloma.
The researchers built a catalogue of the genetic changes that cause cancer in patients and mapped these alterations onto 1000 cancer cell lines. Next, they tested the cell lines for sensitivity to 265 different cancer drugs to understand which of these changes affect sensitivity.
This revealed that the majority of molecular abnormalities found in patients’ cancers are also found in cancer cells in the laboratory.
The work also showed that many of the molecular abnormalities detected in the thousands of patient samples can, both individually and in combination, have a strong effect on whether a particular drug affects a cancer cell’s survival.
The results suggest cancer cell lines could be better exploited to learn which drugs offer the most effective treatment to which patients.
“If a cell line has the same genetic features as a patient’s tumor, and that cell line responded to a specific drug, we can focus new research on this finding,” said study author Francesco Iorio, PhD, of the European Bioinformatics Institute in Cambridge, UK.
“This could ultimately help assign cancer patients into more precise groups based on how likely they are to respond to therapy. This resource can really help cancer research. Most importantly, it can be used to create tools for doctors to select a clinical trial which is most promising for their cancer patient. That is still a way off, but we are heading in the right direction.” ![]()

Image from PNAS
A study published in Cell has shown that patient-derived cancer cell lines harbor most of the same genetic changes found in patients’ tumors and could therefore be used to learn how cancers are likely to respond to new drugs.
Researchers believe this discovery could help advance personalized cancer medicine by leading to results that help doctors predict the best available drugs or the most suitable clinical trials for each individual patient.
“We need better ways to figure out which groups of patients are more likely to respond to a new drug before we run complex and expensive clinical trials,” said study author Ultan McDermott, MD, PhD, of the Wellcome Trust Sanger Institute in Cambridge, UK.
“Our research shows that cancer cell lines do capture the molecular alterations found in tumors and so can be predictive of how a tumor will respond to a drug. This means the cell lines could tell us much more about how a tumor is likely to respond to a new drug before we try to test it in patients. We hope this information will ultimately help in the design of clinical trials that target those patients with the greatest likelihood of benefiting from treatment.”
The researchers said this is the first systematic, large-scale study to combine molecular data from patients, cancer cell lines, and drug sensitivity.
For the study, the team looked at genetic mutations known to cause cancer in more than 11,000 patient samples of 29 different cancer types, including acute lymphoblastic leukemia, acute myeloid leukemia, chronic lymphocytic leukemia, chronic myelogenous leukemia, diffuse large B-cell lymphoma, and multiple myeloma.
The researchers built a catalogue of the genetic changes that cause cancer in patients and mapped these alterations onto 1000 cancer cell lines. Next, they tested the cell lines for sensitivity to 265 different cancer drugs to understand which of these changes affect sensitivity.
This revealed that the majority of molecular abnormalities found in patients’ cancers are also found in cancer cells in the laboratory.
The work also showed that many of the molecular abnormalities detected in the thousands of patient samples can, both individually and in combination, have a strong effect on whether a particular drug affects a cancer cell’s survival.
The results suggest cancer cell lines could be better exploited to learn which drugs offer the most effective treatment to which patients.
“If a cell line has the same genetic features as a patient’s tumor, and that cell line responded to a specific drug, we can focus new research on this finding,” said study author Francesco Iorio, PhD, of the European Bioinformatics Institute in Cambridge, UK.
“This could ultimately help assign cancer patients into more precise groups based on how likely they are to respond to therapy. This resource can really help cancer research. Most importantly, it can be used to create tools for doctors to select a clinical trial which is most promising for their cancer patient. That is still a way off, but we are heading in the right direction.” ![]()
EC expands approved use of carfilzomib

Photo from Amgen
The European Commission (EC) has expanded the approved use of the proteasome inhibitor carfilzomib (Kyprolis).
The drug is now approved for use in combination with dexamethasone to treat adults with multiple myeloma (MM) who have received at least 1 prior therapy.
Carfilzomib was previously approved by the EC for use in combination with lenalidomide and dexamethasone to treat adult MM patients who have received at least 1 prior therapy.
The EC approved the extended indication for carfilzomib based on data from the phase 3 ENDEAVOR trial.
The trial included 929 MM patients whose disease had relapsed after 1 to 3 prior therapeutic regimens.
The patients received either carfilzomib plus dexamethasone (n=464) or bortezomib plus dexamethasone (n=465) until disease progression.
The primary endpoint was progression-free survival. The median progression-free survival was 18.7 months in the carfilzomib arm and 9.4 months in the bortezomib arm. The hazard ratio was 0.53 (P<0.0001).
Overall survival data were not yet mature at last follow-up.
Treatment discontinuation due to adverse events and on-study deaths were comparable between the 2 treatment arms.
However, a number of known adverse events were reported at a higher rate in the carfilzomib arm than the bortezomib arm, including dyspnea (28% vs 13%), hypertension (25% vs 3%), pyrexia (27% vs 14%), cough (25% vs 15%), cardiac failure (8% vs 3%), and acute renal failure (8% vs 5%).
Carfilzomib is marketed as Kyprolis by Onyx Pharmaceuticals, Inc., a subsidiary of Amgen that holds development and commercialization rights to the drug globally, with the exception of Japan. ![]()

Photo from Amgen
The European Commission (EC) has expanded the approved use of the proteasome inhibitor carfilzomib (Kyprolis).
The drug is now approved for use in combination with dexamethasone to treat adults with multiple myeloma (MM) who have received at least 1 prior therapy.
Carfilzomib was previously approved by the EC for use in combination with lenalidomide and dexamethasone to treat adult MM patients who have received at least 1 prior therapy.
The EC approved the extended indication for carfilzomib based on data from the phase 3 ENDEAVOR trial.
The trial included 929 MM patients whose disease had relapsed after 1 to 3 prior therapeutic regimens.
The patients received either carfilzomib plus dexamethasone (n=464) or bortezomib plus dexamethasone (n=465) until disease progression.
The primary endpoint was progression-free survival. The median progression-free survival was 18.7 months in the carfilzomib arm and 9.4 months in the bortezomib arm. The hazard ratio was 0.53 (P<0.0001).
Overall survival data were not yet mature at last follow-up.
Treatment discontinuation due to adverse events and on-study deaths were comparable between the 2 treatment arms.
However, a number of known adverse events were reported at a higher rate in the carfilzomib arm than the bortezomib arm, including dyspnea (28% vs 13%), hypertension (25% vs 3%), pyrexia (27% vs 14%), cough (25% vs 15%), cardiac failure (8% vs 3%), and acute renal failure (8% vs 5%).
Carfilzomib is marketed as Kyprolis by Onyx Pharmaceuticals, Inc., a subsidiary of Amgen that holds development and commercialization rights to the drug globally, with the exception of Japan. ![]()

Photo from Amgen
The European Commission (EC) has expanded the approved use of the proteasome inhibitor carfilzomib (Kyprolis).
The drug is now approved for use in combination with dexamethasone to treat adults with multiple myeloma (MM) who have received at least 1 prior therapy.
Carfilzomib was previously approved by the EC for use in combination with lenalidomide and dexamethasone to treat adult MM patients who have received at least 1 prior therapy.
The EC approved the extended indication for carfilzomib based on data from the phase 3 ENDEAVOR trial.
The trial included 929 MM patients whose disease had relapsed after 1 to 3 prior therapeutic regimens.
The patients received either carfilzomib plus dexamethasone (n=464) or bortezomib plus dexamethasone (n=465) until disease progression.
The primary endpoint was progression-free survival. The median progression-free survival was 18.7 months in the carfilzomib arm and 9.4 months in the bortezomib arm. The hazard ratio was 0.53 (P<0.0001).
Overall survival data were not yet mature at last follow-up.
Treatment discontinuation due to adverse events and on-study deaths were comparable between the 2 treatment arms.
However, a number of known adverse events were reported at a higher rate in the carfilzomib arm than the bortezomib arm, including dyspnea (28% vs 13%), hypertension (25% vs 3%), pyrexia (27% vs 14%), cough (25% vs 15%), cardiac failure (8% vs 3%), and acute renal failure (8% vs 5%).
Carfilzomib is marketed as Kyprolis by Onyx Pharmaceuticals, Inc., a subsidiary of Amgen that holds development and commercialization rights to the drug globally, with the exception of Japan. ![]()
Study reveals SNPs that may increase risk of MM

A large study has revealed several genetic variations that may increase a person’s risk of developing multiple myeloma (MM).
The findings, published in Nature Communications, build on existing research that suggests MM can run in families.
“Our study expands our understanding of how inherited risk factors can influence the risk of myeloma,” said Richard Houlston, MD, PhD, of The Institute of Cancer Research in London, UK.
“We know that the inherited risk of myeloma does not come from just one or two major risk genes, as can be the case with breast cancer, but from multiple different genetic variants, each with only a small individual effect on risk. Identifying more of these variants gives us new insights into the potential causes of the disease and open up new strategies for prevention.”
For this study, Dr Houlston and his colleagues compared DNA from 9866 MM patients and 239,188 healthy adults.
This confirmed the association between MM and 9 previously reported single nucleotide polymorphisms (SNPs):
- rs6746082 at 2p23.3
- rs1052501 at 3p22.1
- rs4487645 at 7p15.3
- rs10936599 at 3q26.2
- rs2285803 at 6p21.3
- rs4273077 at 17p11.2
- rs877529 at 22q13.1
- rs56219066 at 5q15
- rs138740 at 22q13.
It also revealed 8 new SNPs that may increase the risk of MM:
- rs34229995 at 6p22.3 (P=1.31 × 10−8)
- rs9372120 at 6q21 (P=9.09 × 10−15)
- rs7781265 at 7q36.1 (P=9.71 × 10−9)
- rs1948915 at 8q24.21 (P=4.20 × 10−11)
- rs2811710 at 9p21.3 (P=1.72 × 10−13)
- rs2790457 at 10p12.1 (P=1.77 × 10−8)
- rs7193541 at 16q23.1 (P=5.00 × 10−12)
- rs6066835 at 20q13.13 (P=1.36 × 10−13).
These SNPs are located in regions of the genome involved in regulating genes linked to cell processes known to go wrong in MM development—namely, JARID2, ATG5, SMARCD3, CCAT1, CDKN2A, WAC, RFWD3, and PREX1.
This suggests that subtle effects on the activity of key genes could mean the proper development of plasma cells breaks down, increasing the likelihood of developing MM. However, as the researchers noted, further study is needed to confirm and better understand this phenomenon. ![]()

A large study has revealed several genetic variations that may increase a person’s risk of developing multiple myeloma (MM).
The findings, published in Nature Communications, build on existing research that suggests MM can run in families.
“Our study expands our understanding of how inherited risk factors can influence the risk of myeloma,” said Richard Houlston, MD, PhD, of The Institute of Cancer Research in London, UK.
“We know that the inherited risk of myeloma does not come from just one or two major risk genes, as can be the case with breast cancer, but from multiple different genetic variants, each with only a small individual effect on risk. Identifying more of these variants gives us new insights into the potential causes of the disease and open up new strategies for prevention.”
For this study, Dr Houlston and his colleagues compared DNA from 9866 MM patients and 239,188 healthy adults.
This confirmed the association between MM and 9 previously reported single nucleotide polymorphisms (SNPs):
- rs6746082 at 2p23.3
- rs1052501 at 3p22.1
- rs4487645 at 7p15.3
- rs10936599 at 3q26.2
- rs2285803 at 6p21.3
- rs4273077 at 17p11.2
- rs877529 at 22q13.1
- rs56219066 at 5q15
- rs138740 at 22q13.
It also revealed 8 new SNPs that may increase the risk of MM:
- rs34229995 at 6p22.3 (P=1.31 × 10−8)
- rs9372120 at 6q21 (P=9.09 × 10−15)
- rs7781265 at 7q36.1 (P=9.71 × 10−9)
- rs1948915 at 8q24.21 (P=4.20 × 10−11)
- rs2811710 at 9p21.3 (P=1.72 × 10−13)
- rs2790457 at 10p12.1 (P=1.77 × 10−8)
- rs7193541 at 16q23.1 (P=5.00 × 10−12)
- rs6066835 at 20q13.13 (P=1.36 × 10−13).
These SNPs are located in regions of the genome involved in regulating genes linked to cell processes known to go wrong in MM development—namely, JARID2, ATG5, SMARCD3, CCAT1, CDKN2A, WAC, RFWD3, and PREX1.
This suggests that subtle effects on the activity of key genes could mean the proper development of plasma cells breaks down, increasing the likelihood of developing MM. However, as the researchers noted, further study is needed to confirm and better understand this phenomenon. ![]()

A large study has revealed several genetic variations that may increase a person’s risk of developing multiple myeloma (MM).
The findings, published in Nature Communications, build on existing research that suggests MM can run in families.
“Our study expands our understanding of how inherited risk factors can influence the risk of myeloma,” said Richard Houlston, MD, PhD, of The Institute of Cancer Research in London, UK.
“We know that the inherited risk of myeloma does not come from just one or two major risk genes, as can be the case with breast cancer, but from multiple different genetic variants, each with only a small individual effect on risk. Identifying more of these variants gives us new insights into the potential causes of the disease and open up new strategies for prevention.”
For this study, Dr Houlston and his colleagues compared DNA from 9866 MM patients and 239,188 healthy adults.
This confirmed the association between MM and 9 previously reported single nucleotide polymorphisms (SNPs):
- rs6746082 at 2p23.3
- rs1052501 at 3p22.1
- rs4487645 at 7p15.3
- rs10936599 at 3q26.2
- rs2285803 at 6p21.3
- rs4273077 at 17p11.2
- rs877529 at 22q13.1
- rs56219066 at 5q15
- rs138740 at 22q13.
It also revealed 8 new SNPs that may increase the risk of MM:
- rs34229995 at 6p22.3 (P=1.31 × 10−8)
- rs9372120 at 6q21 (P=9.09 × 10−15)
- rs7781265 at 7q36.1 (P=9.71 × 10−9)
- rs1948915 at 8q24.21 (P=4.20 × 10−11)
- rs2811710 at 9p21.3 (P=1.72 × 10−13)
- rs2790457 at 10p12.1 (P=1.77 × 10−8)
- rs7193541 at 16q23.1 (P=5.00 × 10−12)
- rs6066835 at 20q13.13 (P=1.36 × 10−13).
These SNPs are located in regions of the genome involved in regulating genes linked to cell processes known to go wrong in MM development—namely, JARID2, ATG5, SMARCD3, CCAT1, CDKN2A, WAC, RFWD3, and PREX1.
This suggests that subtle effects on the activity of key genes could mean the proper development of plasma cells breaks down, increasing the likelihood of developing MM. However, as the researchers noted, further study is needed to confirm and better understand this phenomenon. ![]()
New type of CAR T cells can produce responses in NHL

Image courtesy of NIAID
Results of a phase 1 study suggest that chimeric antigen receptor T cells specific for the κ light chain (κ.CAR T cells) can produce responses in patients with relapsed or refractory B-cell malignancies, largely without side effects.
The therapy induced complete and partial responses in some patients with non-Hodgkin lymphoma (NHL), and it allowed other patients with chronic lymphocytic leukemia (CLL) or multiple myeloma (MM) to maintain stable disease.
There was 1 adverse event considered possibly related to the treatment.
The researchers reported these results in The Journal of Clinical Investigation.
The κ.CAR T cells were designed to recognize κ-restricted cells and spare normal B cells expressing the nontargeted λ light chain.
“We reasoned that targeting the light chain expressed by malignant B cells should efficiently kill tumor cells while sparing normal B cells expressing the other type of light chain,” said study author Carlos Ramos, MD, of Baylor College of Medicine in Houston, Texas.
He and his colleagues tested the κ.CAR T cells in 16 patients with relapsed or refractory κ+ NHL (n=7), CLL (n=2), or MM (n=7).
The team isolated T cells from these patients and modified the cells so they could target the κ light chain on the surface of malignant B cells. The modified T cells were infused back into the patients, and each patient was monitored for disease progression and side effects.
Eleven patients stopped receiving other treatments at least 4 weeks prior to T-cell infusion. Six patients without lymphopenia received cyclophosphamide at 12.5 mg/kg 4 days before κ.CAR T-cell infusion (0.2×108 to 2×108 κ.CAR T cells/m2).
“We found the treatment to be feasible and safe at all the dose levels studied,” Dr Ramos said.
One MM patient had grade 3 lymphopenia that was deemed possibly related to treatment, but none of the other adverse events were thought to result from the κ.CAR T cells.
Two patients with NHL achieved a complete response to treatment, 1 lasting more than 32 months and the other lasting 6 weeks. A third NHL patient had a partial response lasting 3 months, and a CLL patient had stable disease lasting 6 weeks.
Five of the 7 MM patients had stable disease, 3 lasting 6 weeks, 1 lasting 17 months, and 1 lasting 24 months.
“Our approach, although we are still optimizing it, offers a new possibility for patients in whom other treatments have not been successful,” Dr Ramos concluded. ![]()

Image courtesy of NIAID
Results of a phase 1 study suggest that chimeric antigen receptor T cells specific for the κ light chain (κ.CAR T cells) can produce responses in patients with relapsed or refractory B-cell malignancies, largely without side effects.
The therapy induced complete and partial responses in some patients with non-Hodgkin lymphoma (NHL), and it allowed other patients with chronic lymphocytic leukemia (CLL) or multiple myeloma (MM) to maintain stable disease.
There was 1 adverse event considered possibly related to the treatment.
The researchers reported these results in The Journal of Clinical Investigation.
The κ.CAR T cells were designed to recognize κ-restricted cells and spare normal B cells expressing the nontargeted λ light chain.
“We reasoned that targeting the light chain expressed by malignant B cells should efficiently kill tumor cells while sparing normal B cells expressing the other type of light chain,” said study author Carlos Ramos, MD, of Baylor College of Medicine in Houston, Texas.
He and his colleagues tested the κ.CAR T cells in 16 patients with relapsed or refractory κ+ NHL (n=7), CLL (n=2), or MM (n=7).
The team isolated T cells from these patients and modified the cells so they could target the κ light chain on the surface of malignant B cells. The modified T cells were infused back into the patients, and each patient was monitored for disease progression and side effects.
Eleven patients stopped receiving other treatments at least 4 weeks prior to T-cell infusion. Six patients without lymphopenia received cyclophosphamide at 12.5 mg/kg 4 days before κ.CAR T-cell infusion (0.2×108 to 2×108 κ.CAR T cells/m2).
“We found the treatment to be feasible and safe at all the dose levels studied,” Dr Ramos said.
One MM patient had grade 3 lymphopenia that was deemed possibly related to treatment, but none of the other adverse events were thought to result from the κ.CAR T cells.
Two patients with NHL achieved a complete response to treatment, 1 lasting more than 32 months and the other lasting 6 weeks. A third NHL patient had a partial response lasting 3 months, and a CLL patient had stable disease lasting 6 weeks.
Five of the 7 MM patients had stable disease, 3 lasting 6 weeks, 1 lasting 17 months, and 1 lasting 24 months.
“Our approach, although we are still optimizing it, offers a new possibility for patients in whom other treatments have not been successful,” Dr Ramos concluded. ![]()

Image courtesy of NIAID
Results of a phase 1 study suggest that chimeric antigen receptor T cells specific for the κ light chain (κ.CAR T cells) can produce responses in patients with relapsed or refractory B-cell malignancies, largely without side effects.
The therapy induced complete and partial responses in some patients with non-Hodgkin lymphoma (NHL), and it allowed other patients with chronic lymphocytic leukemia (CLL) or multiple myeloma (MM) to maintain stable disease.
There was 1 adverse event considered possibly related to the treatment.
The researchers reported these results in The Journal of Clinical Investigation.
The κ.CAR T cells were designed to recognize κ-restricted cells and spare normal B cells expressing the nontargeted λ light chain.
“We reasoned that targeting the light chain expressed by malignant B cells should efficiently kill tumor cells while sparing normal B cells expressing the other type of light chain,” said study author Carlos Ramos, MD, of Baylor College of Medicine in Houston, Texas.
He and his colleagues tested the κ.CAR T cells in 16 patients with relapsed or refractory κ+ NHL (n=7), CLL (n=2), or MM (n=7).
The team isolated T cells from these patients and modified the cells so they could target the κ light chain on the surface of malignant B cells. The modified T cells were infused back into the patients, and each patient was monitored for disease progression and side effects.
Eleven patients stopped receiving other treatments at least 4 weeks prior to T-cell infusion. Six patients without lymphopenia received cyclophosphamide at 12.5 mg/kg 4 days before κ.CAR T-cell infusion (0.2×108 to 2×108 κ.CAR T cells/m2).
“We found the treatment to be feasible and safe at all the dose levels studied,” Dr Ramos said.
One MM patient had grade 3 lymphopenia that was deemed possibly related to treatment, but none of the other adverse events were thought to result from the κ.CAR T cells.
Two patients with NHL achieved a complete response to treatment, 1 lasting more than 32 months and the other lasting 6 weeks. A third NHL patient had a partial response lasting 3 months, and a CLL patient had stable disease lasting 6 weeks.
Five of the 7 MM patients had stable disease, 3 lasting 6 weeks, 1 lasting 17 months, and 1 lasting 24 months.
“Our approach, although we are still optimizing it, offers a new possibility for patients in whom other treatments have not been successful,” Dr Ramos concluded. ![]()
Health Canada approves mAb for MM

Photo courtesy of Janssen
Health Canada has granted conditional approval, or a Notice of Compliance with Conditions (NOC/c), for daratumumab (Darzalex), a monoclonal antibody (mAb) targeting CD38.
The mAb is now approved to treat patients with multiple myeloma (MM) who have received at least 3 prior lines of therapy, including a proteasome inhibitor (PI) and an immunomodulatory drug (IMiD), or MM patients who are refractory to both a PI and an IMiD.
An NOC/c is authorization to market a drug with the condition that the sponsor—in this case, Janssen Inc.—undertake additional studies to verify a clinical benefit.
The NOC/c policy is designed to provide access to:
- Drugs that can treat serious, life-threatening, or severely debilitating diseases
- Drugs that can treat conditions for which no drug is currently marketed in Canada
- Drugs that provide a significant increase in efficacy or significant decrease in risk when compared to existing drugs marketed in Canada.
Studies of daratumumab
The NOC/c for daratumumab was based on a review of data from the phase 2 SIRIUS study, the phase 1/2 GEN501 study, and additional supportive studies.
The GEN501 study enrolled 102 patients with relapsed MM or relapsed MM that was refractory to 2 or more prior lines of therapy. The patients received daratumumab at a range of doses and on a number of different schedules.
The results suggested daratumumab is most effective at a dose of 16 mg/kg. At this dose, the overall response rate was 36%. Most adverse events in this study were grade 1 or 2, although serious events did occur.
The SIRIUS study enrolled 124 MM patients who had received 3 or more prior lines of therapy. They received daratumumab at different doses and on different schedules, but 106 patients received the drug at 16 mg/kg.
Twenty-nine percent of the 106 patients responded to treatment, and the median duration of response was 7 months. Thirty percent of patients experienced serious adverse events.
Findings from a combined efficacy analysis of the GEN501 and SIRIUS trials demonstrated that, after a mean follow-up of 14.8 months, the estimated median overall survival for patients who received single-agent daratumumab at 16 mg/kg was 20 months.
Five phase 3 clinical studies with daratumumab in MM patients—in relapsed and frontline settings—are ongoing. Additional studies are ongoing or planned to assess the mAb’s potential in other malignant and pre-malignant diseases in which CD38 is expressed.
Janssen has exclusive worldwide rights to the development, manufacturing, and commercialization of daratumumab for all potential indications. The company licensed daratumumab from Genmab A/S in August 2012. ![]()

Photo courtesy of Janssen
Health Canada has granted conditional approval, or a Notice of Compliance with Conditions (NOC/c), for daratumumab (Darzalex), a monoclonal antibody (mAb) targeting CD38.
The mAb is now approved to treat patients with multiple myeloma (MM) who have received at least 3 prior lines of therapy, including a proteasome inhibitor (PI) and an immunomodulatory drug (IMiD), or MM patients who are refractory to both a PI and an IMiD.
An NOC/c is authorization to market a drug with the condition that the sponsor—in this case, Janssen Inc.—undertake additional studies to verify a clinical benefit.
The NOC/c policy is designed to provide access to:
- Drugs that can treat serious, life-threatening, or severely debilitating diseases
- Drugs that can treat conditions for which no drug is currently marketed in Canada
- Drugs that provide a significant increase in efficacy or significant decrease in risk when compared to existing drugs marketed in Canada.
Studies of daratumumab
The NOC/c for daratumumab was based on a review of data from the phase 2 SIRIUS study, the phase 1/2 GEN501 study, and additional supportive studies.
The GEN501 study enrolled 102 patients with relapsed MM or relapsed MM that was refractory to 2 or more prior lines of therapy. The patients received daratumumab at a range of doses and on a number of different schedules.
The results suggested daratumumab is most effective at a dose of 16 mg/kg. At this dose, the overall response rate was 36%. Most adverse events in this study were grade 1 or 2, although serious events did occur.
The SIRIUS study enrolled 124 MM patients who had received 3 or more prior lines of therapy. They received daratumumab at different doses and on different schedules, but 106 patients received the drug at 16 mg/kg.
Twenty-nine percent of the 106 patients responded to treatment, and the median duration of response was 7 months. Thirty percent of patients experienced serious adverse events.
Findings from a combined efficacy analysis of the GEN501 and SIRIUS trials demonstrated that, after a mean follow-up of 14.8 months, the estimated median overall survival for patients who received single-agent daratumumab at 16 mg/kg was 20 months.
Five phase 3 clinical studies with daratumumab in MM patients—in relapsed and frontline settings—are ongoing. Additional studies are ongoing or planned to assess the mAb’s potential in other malignant and pre-malignant diseases in which CD38 is expressed.
Janssen has exclusive worldwide rights to the development, manufacturing, and commercialization of daratumumab for all potential indications. The company licensed daratumumab from Genmab A/S in August 2012. ![]()

Photo courtesy of Janssen
Health Canada has granted conditional approval, or a Notice of Compliance with Conditions (NOC/c), for daratumumab (Darzalex), a monoclonal antibody (mAb) targeting CD38.
The mAb is now approved to treat patients with multiple myeloma (MM) who have received at least 3 prior lines of therapy, including a proteasome inhibitor (PI) and an immunomodulatory drug (IMiD), or MM patients who are refractory to both a PI and an IMiD.
An NOC/c is authorization to market a drug with the condition that the sponsor—in this case, Janssen Inc.—undertake additional studies to verify a clinical benefit.
The NOC/c policy is designed to provide access to:
- Drugs that can treat serious, life-threatening, or severely debilitating diseases
- Drugs that can treat conditions for which no drug is currently marketed in Canada
- Drugs that provide a significant increase in efficacy or significant decrease in risk when compared to existing drugs marketed in Canada.
Studies of daratumumab
The NOC/c for daratumumab was based on a review of data from the phase 2 SIRIUS study, the phase 1/2 GEN501 study, and additional supportive studies.
The GEN501 study enrolled 102 patients with relapsed MM or relapsed MM that was refractory to 2 or more prior lines of therapy. The patients received daratumumab at a range of doses and on a number of different schedules.
The results suggested daratumumab is most effective at a dose of 16 mg/kg. At this dose, the overall response rate was 36%. Most adverse events in this study were grade 1 or 2, although serious events did occur.
The SIRIUS study enrolled 124 MM patients who had received 3 or more prior lines of therapy. They received daratumumab at different doses and on different schedules, but 106 patients received the drug at 16 mg/kg.
Twenty-nine percent of the 106 patients responded to treatment, and the median duration of response was 7 months. Thirty percent of patients experienced serious adverse events.
Findings from a combined efficacy analysis of the GEN501 and SIRIUS trials demonstrated that, after a mean follow-up of 14.8 months, the estimated median overall survival for patients who received single-agent daratumumab at 16 mg/kg was 20 months.
Five phase 3 clinical studies with daratumumab in MM patients—in relapsed and frontline settings—are ongoing. Additional studies are ongoing or planned to assess the mAb’s potential in other malignant and pre-malignant diseases in which CD38 is expressed.
Janssen has exclusive worldwide rights to the development, manufacturing, and commercialization of daratumumab for all potential indications. The company licensed daratumumab from Genmab A/S in August 2012. ![]()
Scientists describe mechanism of IMiDs
Researchers say they have identified the molecular mechanism of thalidomide and other immunomodulatory drugs (IMiDs), a finding that is relevant to the treatment of multiple myeloma and other hematologic malignancies.
Previous research showed that cereblon, a cellular protein, plays an important role in the function of IMiDs.
However, the exact details of how cereblon mediates the effects of IMiDs were not clear.
The new study, published in Nature Medicine, provides an explanation.
Researchers found that, inside cells, cereblon usually binds to the proteins CD147 and MCT1. Among other things, these 2 proteins promote proliferation, metabolism, and the formation of new blood vessels. In cancers such as multiple myeloma, tumor cells contain particularly high levels of CD147 and MCT1.
As a protein complex, CD147 and MCT1 always occur as a pair. However, to find their other half and become activated, the proteins require the help of cereblon.
Binding to cereblon promotes development and stability of the complex, which, in return, stimulates cell growth and facilitates the excretion of metabolic products like lactate.
In diseases such as multiple myeloma, an increased abundance of this protein complex enables tumor cells to multiply and spread rapidly.
If such a cancer is treated with IMiDs, the drug virtually displaces the complex from its binding to cereblon. As a result, CD147 and MCT1 can no longer be activated, and they vanish.
“Ultimately, this causes the tumor cells to die,” said study author Ruth Eichner, MD, of Technische Universität München in Munich, Germany.
But the disruption of the protein complex is also responsible for the severe birth defects that can occur in the children of women who take thalidomide and other IMiDs when pregnant.
“The mechanisms are identical,” said study author Florian Bassermann, MD, PhD, of Technische Universität München.
“A specific inactivation of the protein complex resulted in the same developmental defects observed after thalidomide treatment.”
The researchers said this confirms the prevailing hypothesis that the typical IMiD-induced birth defects are related to the reduced and abnormal formation of new blood vessels. That’s because, without CD147 and MCT1, blood vessels cannot develop properly.
The team also said these findings could be used to assess the efficacy of IMiD treatment before actually giving an IMiD to the patient.
“The disappearance of the protein complex could only be observed in patients that had responded well to this type of treatment,” Dr Bassermann explained.
Therefore, he and his colleagues believe this information could be used to assess a patient’s response before starting an IMiD. A sample of the patient’s tumor cells could be cultured and treated with IMiDs. If the cells showed a disruption of the complex, the patient would most likely benefit from IMiD treatment.
The researchers also think the results of this study could lead to the development of new anticancer therapies.
The team said the CD147-MCT1 protein complex is a particularly attractive target for tumor treatment, as it is mainly found on the surface of cells and virtually links the inside to the outside of the cell.
Therefore, inactivation of the complex might be achieved using specifically produced antibodies and other distinctive drugs—a possibility Dr Bassermann and his team are now exploring. ![]()
Researchers say they have identified the molecular mechanism of thalidomide and other immunomodulatory drugs (IMiDs), a finding that is relevant to the treatment of multiple myeloma and other hematologic malignancies.
Previous research showed that cereblon, a cellular protein, plays an important role in the function of IMiDs.
However, the exact details of how cereblon mediates the effects of IMiDs were not clear.
The new study, published in Nature Medicine, provides an explanation.
Researchers found that, inside cells, cereblon usually binds to the proteins CD147 and MCT1. Among other things, these 2 proteins promote proliferation, metabolism, and the formation of new blood vessels. In cancers such as multiple myeloma, tumor cells contain particularly high levels of CD147 and MCT1.
As a protein complex, CD147 and MCT1 always occur as a pair. However, to find their other half and become activated, the proteins require the help of cereblon.
Binding to cereblon promotes development and stability of the complex, which, in return, stimulates cell growth and facilitates the excretion of metabolic products like lactate.
In diseases such as multiple myeloma, an increased abundance of this protein complex enables tumor cells to multiply and spread rapidly.
If such a cancer is treated with IMiDs, the drug virtually displaces the complex from its binding to cereblon. As a result, CD147 and MCT1 can no longer be activated, and they vanish.
“Ultimately, this causes the tumor cells to die,” said study author Ruth Eichner, MD, of Technische Universität München in Munich, Germany.
But the disruption of the protein complex is also responsible for the severe birth defects that can occur in the children of women who take thalidomide and other IMiDs when pregnant.
“The mechanisms are identical,” said study author Florian Bassermann, MD, PhD, of Technische Universität München.
“A specific inactivation of the protein complex resulted in the same developmental defects observed after thalidomide treatment.”
The researchers said this confirms the prevailing hypothesis that the typical IMiD-induced birth defects are related to the reduced and abnormal formation of new blood vessels. That’s because, without CD147 and MCT1, blood vessels cannot develop properly.
The team also said these findings could be used to assess the efficacy of IMiD treatment before actually giving an IMiD to the patient.
“The disappearance of the protein complex could only be observed in patients that had responded well to this type of treatment,” Dr Bassermann explained.
Therefore, he and his colleagues believe this information could be used to assess a patient’s response before starting an IMiD. A sample of the patient’s tumor cells could be cultured and treated with IMiDs. If the cells showed a disruption of the complex, the patient would most likely benefit from IMiD treatment.
The researchers also think the results of this study could lead to the development of new anticancer therapies.
The team said the CD147-MCT1 protein complex is a particularly attractive target for tumor treatment, as it is mainly found on the surface of cells and virtually links the inside to the outside of the cell.
Therefore, inactivation of the complex might be achieved using specifically produced antibodies and other distinctive drugs—a possibility Dr Bassermann and his team are now exploring. ![]()
Researchers say they have identified the molecular mechanism of thalidomide and other immunomodulatory drugs (IMiDs), a finding that is relevant to the treatment of multiple myeloma and other hematologic malignancies.
Previous research showed that cereblon, a cellular protein, plays an important role in the function of IMiDs.
However, the exact details of how cereblon mediates the effects of IMiDs were not clear.
The new study, published in Nature Medicine, provides an explanation.
Researchers found that, inside cells, cereblon usually binds to the proteins CD147 and MCT1. Among other things, these 2 proteins promote proliferation, metabolism, and the formation of new blood vessels. In cancers such as multiple myeloma, tumor cells contain particularly high levels of CD147 and MCT1.
As a protein complex, CD147 and MCT1 always occur as a pair. However, to find their other half and become activated, the proteins require the help of cereblon.
Binding to cereblon promotes development and stability of the complex, which, in return, stimulates cell growth and facilitates the excretion of metabolic products like lactate.
In diseases such as multiple myeloma, an increased abundance of this protein complex enables tumor cells to multiply and spread rapidly.
If such a cancer is treated with IMiDs, the drug virtually displaces the complex from its binding to cereblon. As a result, CD147 and MCT1 can no longer be activated, and they vanish.
“Ultimately, this causes the tumor cells to die,” said study author Ruth Eichner, MD, of Technische Universität München in Munich, Germany.
But the disruption of the protein complex is also responsible for the severe birth defects that can occur in the children of women who take thalidomide and other IMiDs when pregnant.
“The mechanisms are identical,” said study author Florian Bassermann, MD, PhD, of Technische Universität München.
“A specific inactivation of the protein complex resulted in the same developmental defects observed after thalidomide treatment.”
The researchers said this confirms the prevailing hypothesis that the typical IMiD-induced birth defects are related to the reduced and abnormal formation of new blood vessels. That’s because, without CD147 and MCT1, blood vessels cannot develop properly.
The team also said these findings could be used to assess the efficacy of IMiD treatment before actually giving an IMiD to the patient.
“The disappearance of the protein complex could only be observed in patients that had responded well to this type of treatment,” Dr Bassermann explained.
Therefore, he and his colleagues believe this information could be used to assess a patient’s response before starting an IMiD. A sample of the patient’s tumor cells could be cultured and treated with IMiDs. If the cells showed a disruption of the complex, the patient would most likely benefit from IMiD treatment.
The researchers also think the results of this study could lead to the development of new anticancer therapies.
The team said the CD147-MCT1 protein complex is a particularly attractive target for tumor treatment, as it is mainly found on the surface of cells and virtually links the inside to the outside of the cell.
Therefore, inactivation of the complex might be achieved using specifically produced antibodies and other distinctive drugs—a possibility Dr Bassermann and his team are now exploring. ![]()
Continuous Rd again beat MPT for transplant-ineligible multiple myeloma
Individuals with newly diagnosed multiple myeloma who were ineligible for stem cell transplantation were 31% less likely to die or progress on continuous lenalidomide plus low-dose dexamethasone (Rd continuous) than were those on melphalan, prednisone, and thalidomide (MPT), according to an extended follow-up of patients from the FIRST trial.
In addition, Rd continuous was associated with a statistically significant 20% decrease in risk of death or disease progression, compared with MPT among patients older than 75 years, reported Dr. Cyrille Hulin of Bordeaux (France) Hospital University Center and associates. The finding “establishes continuous treatment with Rd until disease progression as a new standard of care for patients with newly diagnosed multiple myeloma who are ineligible for stem cell transplantation, regardless of age. With proper monitoring and dose adjustment, Rd continuous is an effective and tolerable treatment option for even the most elderly patients,” they wrote online June 20 in the Journal of Clinical Oncology.
FIRST (Frontline Investigation of Revlimid Plus Dexamethasone Versus Standard Thalidomide) was an international, randomized, phase III open-label study of patients with untreated symptomatic multiple myeloma enrolled between 2008 and 2011. Patients were randomly assigned to Rd continuous, 72 weeks/18 cycles of Rd (Rd18), or MPT. The primary endpoint was progression-free survival (PFS). In the original analysis, Rd continuous led to a 28% lower risk of progression or death, compared with MPT, for a statistically significant hazard ratio (HR) of 0.72. The current study involved longer follow-up, with an updated data cutoff that was 3 years after the end of recruitment, the researchers said (J Clin Oncol. 2016 Jun 20. doi: 10.1200/JCO.2016.66.7295).
The cohort included 1,623 patients, of whom 567 (35%) were older than 75 years. The intention-to-treat populations included 535 Rd continuous patients, 541 Rd18 patients, and 547 MPT patients. Survivors were followed for a median of 45.5 months. As in the earlier analysis of FIRST data, the PFS was longer with Rd continuous than with MPT. For the overall intention-to-treat group, the median PFS was 26 months with Rd continuous, and 21.9 months with MPT (HR, 0.69; 95% confidence interval, 0.59-0.80). Among patients aged 75 years and younger, the median PFS was 28.1 months and 22.4 months, respectively (HR, 0.64; 95% CI, 0.53-0.77). Among patients over age 75 years, the median PFS was 20.3 months and 19.8 months, respectively (HR, 0.80, 95% CI, 0.62-1.03). In addition, the 4-year PFS “was more than doubled with Rd continuous versus MPT, regardless of age,” the investigators said. In contrast, Rd18 and MPT led to a similar median PFS, regardless of age.
As in the prior FIRST analysis, MPT was more often linked to grade 3 and 4 neutropenia (40% and 47% of older and younger patients, respectively, versus about 28% of Rd continuous patients), while Rd more often led to grade 3 and 4 infections (about 30% of Rd continuous patients, about 22% of Rd18 patients, and 16%-20% of MPT patients).
A total of 40% of younger Rd patients remained at their starting lenalidomide dose at 72 weeks, while only 16% of MPT patients stayed at their starting thalidomide dose. Similarly, 30% of older Rd continuous patients remained on their starting dose at 72 weeks, compared with 19% of older MPT patients.
Older age was associated with International Staging System stage III disease, renal impairment, and more comorbidities, but not with high-risk cytogenetics (that is, del[17p] and t[4;14]). “Although chronologic age is not necessarily an indicator of frailty, FIRST trial results did show greater PFS and OS [overall survival] benefits with Rd continuous versus MPT therapy, regardless of age,” the researchers commented.
The study was funded by Intergroupe Francophone du Myélome and Celgene. Dr. Hulin disclosed honoraria from Celgene, Amgen, Bristol-Myers Squibb, and Novartis.
Individuals with newly diagnosed multiple myeloma who were ineligible for stem cell transplantation were 31% less likely to die or progress on continuous lenalidomide plus low-dose dexamethasone (Rd continuous) than were those on melphalan, prednisone, and thalidomide (MPT), according to an extended follow-up of patients from the FIRST trial.
In addition, Rd continuous was associated with a statistically significant 20% decrease in risk of death or disease progression, compared with MPT among patients older than 75 years, reported Dr. Cyrille Hulin of Bordeaux (France) Hospital University Center and associates. The finding “establishes continuous treatment with Rd until disease progression as a new standard of care for patients with newly diagnosed multiple myeloma who are ineligible for stem cell transplantation, regardless of age. With proper monitoring and dose adjustment, Rd continuous is an effective and tolerable treatment option for even the most elderly patients,” they wrote online June 20 in the Journal of Clinical Oncology.
FIRST (Frontline Investigation of Revlimid Plus Dexamethasone Versus Standard Thalidomide) was an international, randomized, phase III open-label study of patients with untreated symptomatic multiple myeloma enrolled between 2008 and 2011. Patients were randomly assigned to Rd continuous, 72 weeks/18 cycles of Rd (Rd18), or MPT. The primary endpoint was progression-free survival (PFS). In the original analysis, Rd continuous led to a 28% lower risk of progression or death, compared with MPT, for a statistically significant hazard ratio (HR) of 0.72. The current study involved longer follow-up, with an updated data cutoff that was 3 years after the end of recruitment, the researchers said (J Clin Oncol. 2016 Jun 20. doi: 10.1200/JCO.2016.66.7295).
The cohort included 1,623 patients, of whom 567 (35%) were older than 75 years. The intention-to-treat populations included 535 Rd continuous patients, 541 Rd18 patients, and 547 MPT patients. Survivors were followed for a median of 45.5 months. As in the earlier analysis of FIRST data, the PFS was longer with Rd continuous than with MPT. For the overall intention-to-treat group, the median PFS was 26 months with Rd continuous, and 21.9 months with MPT (HR, 0.69; 95% confidence interval, 0.59-0.80). Among patients aged 75 years and younger, the median PFS was 28.1 months and 22.4 months, respectively (HR, 0.64; 95% CI, 0.53-0.77). Among patients over age 75 years, the median PFS was 20.3 months and 19.8 months, respectively (HR, 0.80, 95% CI, 0.62-1.03). In addition, the 4-year PFS “was more than doubled with Rd continuous versus MPT, regardless of age,” the investigators said. In contrast, Rd18 and MPT led to a similar median PFS, regardless of age.
As in the prior FIRST analysis, MPT was more often linked to grade 3 and 4 neutropenia (40% and 47% of older and younger patients, respectively, versus about 28% of Rd continuous patients), while Rd more often led to grade 3 and 4 infections (about 30% of Rd continuous patients, about 22% of Rd18 patients, and 16%-20% of MPT patients).
A total of 40% of younger Rd patients remained at their starting lenalidomide dose at 72 weeks, while only 16% of MPT patients stayed at their starting thalidomide dose. Similarly, 30% of older Rd continuous patients remained on their starting dose at 72 weeks, compared with 19% of older MPT patients.
Older age was associated with International Staging System stage III disease, renal impairment, and more comorbidities, but not with high-risk cytogenetics (that is, del[17p] and t[4;14]). “Although chronologic age is not necessarily an indicator of frailty, FIRST trial results did show greater PFS and OS [overall survival] benefits with Rd continuous versus MPT therapy, regardless of age,” the researchers commented.
The study was funded by Intergroupe Francophone du Myélome and Celgene. Dr. Hulin disclosed honoraria from Celgene, Amgen, Bristol-Myers Squibb, and Novartis.
Individuals with newly diagnosed multiple myeloma who were ineligible for stem cell transplantation were 31% less likely to die or progress on continuous lenalidomide plus low-dose dexamethasone (Rd continuous) than were those on melphalan, prednisone, and thalidomide (MPT), according to an extended follow-up of patients from the FIRST trial.
In addition, Rd continuous was associated with a statistically significant 20% decrease in risk of death or disease progression, compared with MPT among patients older than 75 years, reported Dr. Cyrille Hulin of Bordeaux (France) Hospital University Center and associates. The finding “establishes continuous treatment with Rd until disease progression as a new standard of care for patients with newly diagnosed multiple myeloma who are ineligible for stem cell transplantation, regardless of age. With proper monitoring and dose adjustment, Rd continuous is an effective and tolerable treatment option for even the most elderly patients,” they wrote online June 20 in the Journal of Clinical Oncology.
FIRST (Frontline Investigation of Revlimid Plus Dexamethasone Versus Standard Thalidomide) was an international, randomized, phase III open-label study of patients with untreated symptomatic multiple myeloma enrolled between 2008 and 2011. Patients were randomly assigned to Rd continuous, 72 weeks/18 cycles of Rd (Rd18), or MPT. The primary endpoint was progression-free survival (PFS). In the original analysis, Rd continuous led to a 28% lower risk of progression or death, compared with MPT, for a statistically significant hazard ratio (HR) of 0.72. The current study involved longer follow-up, with an updated data cutoff that was 3 years after the end of recruitment, the researchers said (J Clin Oncol. 2016 Jun 20. doi: 10.1200/JCO.2016.66.7295).
The cohort included 1,623 patients, of whom 567 (35%) were older than 75 years. The intention-to-treat populations included 535 Rd continuous patients, 541 Rd18 patients, and 547 MPT patients. Survivors were followed for a median of 45.5 months. As in the earlier analysis of FIRST data, the PFS was longer with Rd continuous than with MPT. For the overall intention-to-treat group, the median PFS was 26 months with Rd continuous, and 21.9 months with MPT (HR, 0.69; 95% confidence interval, 0.59-0.80). Among patients aged 75 years and younger, the median PFS was 28.1 months and 22.4 months, respectively (HR, 0.64; 95% CI, 0.53-0.77). Among patients over age 75 years, the median PFS was 20.3 months and 19.8 months, respectively (HR, 0.80, 95% CI, 0.62-1.03). In addition, the 4-year PFS “was more than doubled with Rd continuous versus MPT, regardless of age,” the investigators said. In contrast, Rd18 and MPT led to a similar median PFS, regardless of age.
As in the prior FIRST analysis, MPT was more often linked to grade 3 and 4 neutropenia (40% and 47% of older and younger patients, respectively, versus about 28% of Rd continuous patients), while Rd more often led to grade 3 and 4 infections (about 30% of Rd continuous patients, about 22% of Rd18 patients, and 16%-20% of MPT patients).
A total of 40% of younger Rd patients remained at their starting lenalidomide dose at 72 weeks, while only 16% of MPT patients stayed at their starting thalidomide dose. Similarly, 30% of older Rd continuous patients remained on their starting dose at 72 weeks, compared with 19% of older MPT patients.
Older age was associated with International Staging System stage III disease, renal impairment, and more comorbidities, but not with high-risk cytogenetics (that is, del[17p] and t[4;14]). “Although chronologic age is not necessarily an indicator of frailty, FIRST trial results did show greater PFS and OS [overall survival] benefits with Rd continuous versus MPT therapy, regardless of age,” the researchers commented.
The study was funded by Intergroupe Francophone du Myélome and Celgene. Dr. Hulin disclosed honoraria from Celgene, Amgen, Bristol-Myers Squibb, and Novartis.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: For patients with newly diagnosed multiple myeloma who were ineligible for transplant, including older patients, continuous lenalidomide plus low-dose dexamethasone (Rd continuous) was associated with significantly longer progression-free survival than was treatment with melphalan, prednisone, and thalidomide (MPT).
Major finding: Continuous Rd was associated with a 31% lower risk of death or progression in the overall intention-to-treat analysis, a 36% decrease among patients aged 75 years or younger, and a 20% decrease among patients older than 75 years.
Data source: An updated analysis of 1,623 patients from the FIRST trial.
Disclosures: The study was funded by Intergroupe Francophone du Myélome and Celgene. Dr. Hulin disclosed honoraria from Celgene, Amgen, Bristol-Myers Squibb, and Novartis.
Lenalidomide maintenance after transplant improves OS in MM

the ASCO Annual Meeting
© ASCO/Todd Buchanan
CHICAGO—Lenalidomide maintenance after high-dose melphalan and autologous stem cell transplant (ASCT) should be considered the standard of care in
newly diagnosed multiple myeloma (MM) patients, according to a meta-analysis presented at the 2016 ASCO Annual Meeting.
Lenalidomide maintenance increased overall survival (OS), with a 26% reduction in the risk of death, representing an estimated 2.5-year increase in median survival.
Several studies have demonstrated that lenalidomide maintenance post-ASCT reduces the risk of disease progression or death in patients with MM by about 50%.
However, these studies were not powered for OS, said Philip McCarthy, MD, of Roswell Park Cancer Institute in Buffalo, New York.
With this in mind, Dr McCarthy and his colleagues conducted a meta-analysis to assess the effect of post-ASCT lenalidomide maintenance on OS using a pooled analysis of primary source patient data. A search revealed 17 randomized, controlled trials using lenalidomide post-ASCT.
Three trials met pre-specified inclusion criteria and had sufficient OS events to test a treatment effect. The studies intended for lenalidomide maintenance to be given until progression.
In these trials, 1209 MM patients, with a median age of 58, were randomized from 2005 to 2009 to receive lenalidomide (605 patients) at 10 mg/day on days 1-21/28 or days 1-28/28. The remaining 604 patients served as controls. Baseline characteristics were generally balanced between the 2 groups.
With a median follow-up of 6.6 years, 491 patients (41%) had died.
After induction and single (82%) or tandem (18%) ASCT, 55% of patients achieved a complete response (CR) or very good partial response.
The median OS has not been reached in the lenalidomide arm but was 86 months for the control arm.
“There is a 26% reduction in the risk of death, representing an estimated 2.5-year increase in median survival,” Dr McCarthy said.
The OS benefit favoring lenalidomide was generally consistent across the majority of subgroup analyses, including age, sex, ISS stage, response after ASCT, and prior induction therapy.
All studies contributed to the positive results of the meta-analysis. Heterogeneity tests showed significant differences across trials, mainly because of a difference in the magnitude of treatment effect, Dr McCarthy said.
The mean treatment duration of maintenance was 25 to 30 months in the lenalidomide group and 13 to 20 months in controls. About one-third to more than half of the patients received therapy for 3 or more years, Dr McCarthy said.
Lenalidomide led to an increased risk in the cumulative incidence of hematologic and solid tumor second primary malignancies. However, Dr McCarthy said the OS benefit of lenalidomide maintenance outweighs the risk of developing second primary malignancy.
“This large meta-analysis demonstrates that lenalidomide maintenance significantly prolonged OS post-ASCT, including in patients who achieved CR, demonstrating benefit in patients in all response categories,” Dr McCarthy said.
“Lenalidomide maintenance after ASCT can be considered a standard of care for newly diagnosed multiple myeloma patients. However, we have more to learn. Understanding the role of minimal residual disease detection and immune reconstitution after transplant should allow us to further improve OS. Critically, developing early endpoints as surrogates for long-term outcome and OS is important for the future. Otherwise, trials may continue for 10 years or longer.”
Dr McCarthy presented these findings as abstract 8001. ![]()

the ASCO Annual Meeting
© ASCO/Todd Buchanan
CHICAGO—Lenalidomide maintenance after high-dose melphalan and autologous stem cell transplant (ASCT) should be considered the standard of care in
newly diagnosed multiple myeloma (MM) patients, according to a meta-analysis presented at the 2016 ASCO Annual Meeting.
Lenalidomide maintenance increased overall survival (OS), with a 26% reduction in the risk of death, representing an estimated 2.5-year increase in median survival.
Several studies have demonstrated that lenalidomide maintenance post-ASCT reduces the risk of disease progression or death in patients with MM by about 50%.
However, these studies were not powered for OS, said Philip McCarthy, MD, of Roswell Park Cancer Institute in Buffalo, New York.
With this in mind, Dr McCarthy and his colleagues conducted a meta-analysis to assess the effect of post-ASCT lenalidomide maintenance on OS using a pooled analysis of primary source patient data. A search revealed 17 randomized, controlled trials using lenalidomide post-ASCT.
Three trials met pre-specified inclusion criteria and had sufficient OS events to test a treatment effect. The studies intended for lenalidomide maintenance to be given until progression.
In these trials, 1209 MM patients, with a median age of 58, were randomized from 2005 to 2009 to receive lenalidomide (605 patients) at 10 mg/day on days 1-21/28 or days 1-28/28. The remaining 604 patients served as controls. Baseline characteristics were generally balanced between the 2 groups.
With a median follow-up of 6.6 years, 491 patients (41%) had died.
After induction and single (82%) or tandem (18%) ASCT, 55% of patients achieved a complete response (CR) or very good partial response.
The median OS has not been reached in the lenalidomide arm but was 86 months for the control arm.
“There is a 26% reduction in the risk of death, representing an estimated 2.5-year increase in median survival,” Dr McCarthy said.
The OS benefit favoring lenalidomide was generally consistent across the majority of subgroup analyses, including age, sex, ISS stage, response after ASCT, and prior induction therapy.
All studies contributed to the positive results of the meta-analysis. Heterogeneity tests showed significant differences across trials, mainly because of a difference in the magnitude of treatment effect, Dr McCarthy said.
The mean treatment duration of maintenance was 25 to 30 months in the lenalidomide group and 13 to 20 months in controls. About one-third to more than half of the patients received therapy for 3 or more years, Dr McCarthy said.
Lenalidomide led to an increased risk in the cumulative incidence of hematologic and solid tumor second primary malignancies. However, Dr McCarthy said the OS benefit of lenalidomide maintenance outweighs the risk of developing second primary malignancy.
“This large meta-analysis demonstrates that lenalidomide maintenance significantly prolonged OS post-ASCT, including in patients who achieved CR, demonstrating benefit in patients in all response categories,” Dr McCarthy said.
“Lenalidomide maintenance after ASCT can be considered a standard of care for newly diagnosed multiple myeloma patients. However, we have more to learn. Understanding the role of minimal residual disease detection and immune reconstitution after transplant should allow us to further improve OS. Critically, developing early endpoints as surrogates for long-term outcome and OS is important for the future. Otherwise, trials may continue for 10 years or longer.”
Dr McCarthy presented these findings as abstract 8001. ![]()

the ASCO Annual Meeting
© ASCO/Todd Buchanan
CHICAGO—Lenalidomide maintenance after high-dose melphalan and autologous stem cell transplant (ASCT) should be considered the standard of care in
newly diagnosed multiple myeloma (MM) patients, according to a meta-analysis presented at the 2016 ASCO Annual Meeting.
Lenalidomide maintenance increased overall survival (OS), with a 26% reduction in the risk of death, representing an estimated 2.5-year increase in median survival.
Several studies have demonstrated that lenalidomide maintenance post-ASCT reduces the risk of disease progression or death in patients with MM by about 50%.
However, these studies were not powered for OS, said Philip McCarthy, MD, of Roswell Park Cancer Institute in Buffalo, New York.
With this in mind, Dr McCarthy and his colleagues conducted a meta-analysis to assess the effect of post-ASCT lenalidomide maintenance on OS using a pooled analysis of primary source patient data. A search revealed 17 randomized, controlled trials using lenalidomide post-ASCT.
Three trials met pre-specified inclusion criteria and had sufficient OS events to test a treatment effect. The studies intended for lenalidomide maintenance to be given until progression.
In these trials, 1209 MM patients, with a median age of 58, were randomized from 2005 to 2009 to receive lenalidomide (605 patients) at 10 mg/day on days 1-21/28 or days 1-28/28. The remaining 604 patients served as controls. Baseline characteristics were generally balanced between the 2 groups.
With a median follow-up of 6.6 years, 491 patients (41%) had died.
After induction and single (82%) or tandem (18%) ASCT, 55% of patients achieved a complete response (CR) or very good partial response.
The median OS has not been reached in the lenalidomide arm but was 86 months for the control arm.
“There is a 26% reduction in the risk of death, representing an estimated 2.5-year increase in median survival,” Dr McCarthy said.
The OS benefit favoring lenalidomide was generally consistent across the majority of subgroup analyses, including age, sex, ISS stage, response after ASCT, and prior induction therapy.
All studies contributed to the positive results of the meta-analysis. Heterogeneity tests showed significant differences across trials, mainly because of a difference in the magnitude of treatment effect, Dr McCarthy said.
The mean treatment duration of maintenance was 25 to 30 months in the lenalidomide group and 13 to 20 months in controls. About one-third to more than half of the patients received therapy for 3 or more years, Dr McCarthy said.
Lenalidomide led to an increased risk in the cumulative incidence of hematologic and solid tumor second primary malignancies. However, Dr McCarthy said the OS benefit of lenalidomide maintenance outweighs the risk of developing second primary malignancy.
“This large meta-analysis demonstrates that lenalidomide maintenance significantly prolonged OS post-ASCT, including in patients who achieved CR, demonstrating benefit in patients in all response categories,” Dr McCarthy said.
“Lenalidomide maintenance after ASCT can be considered a standard of care for newly diagnosed multiple myeloma patients. However, we have more to learn. Understanding the role of minimal residual disease detection and immune reconstitution after transplant should allow us to further improve OS. Critically, developing early endpoints as surrogates for long-term outcome and OS is important for the future. Otherwise, trials may continue for 10 years or longer.”
Dr McCarthy presented these findings as abstract 8001.