User login
Study reveals potential treatment avenue for DBA, MDS

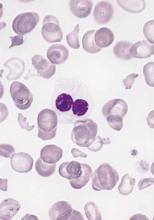
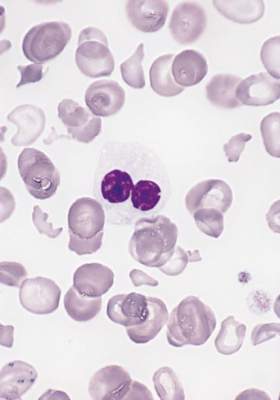
The production of two components of hemoglobin may be out of sync in Diamond Blackfan anemia (DBA) and myelodysplastic syndromes (MDS), according to a new study.
Researchers found that, in samples from patients with DBA or MDS, ribosome dysfunction delayed globin production, while heme synthesis proceeded normally.
This disruption in heme-globin coordination led to a buildup of toxic heme that killed red blood cell (RBC) precursors.
However, treating patient samples with a compound that blocks heme synthesis increased RBC production in both DBA and MDS.
Zhantao Yang, MD, of the University of Washington in Seattle, and his colleagues reported these findings in Science Translational Medicine.
Both DBA and MDS have been linked to defects in ribosome assembly, which is critical to protein production, but how this leads to anemia remains unknown.
To find out, Dr Yang and his colleagues analyzed bone marrow cells from patients with DBA (n=3) or MDS with del(5q) (n=6).
The researchers found that globin translation proceeded slowly in these samples, but heme synthesis proceeded normally.
This resulted in insufficient globin, excess heme, and excess reactive oxygen species in early erythroid precursors and, ultimately, the death of colony-forming unit–erythroid/proerythroblast cells.
The cells that were able to rapidly export heme or slow its synthesis survived and matured into RBCs, but the other colony-forming unit–erythroid cells/early proerythroblasts died.
The researchers noted that it is not clear how excess heme induces cell death in RBC precursors, but they said it likely involves both ferroptosis and apoptosis.
Regardless of the mechanism of cell death, the team found that treating the patients’ cells with succinylacetone (10 mM), a compound that blocks heme synthesis, improved RBC production.
The treatment improved RBC production in DBA and del(5q) MDS marrow cultures by 68% to 95% (P=0.03 to 0.05). In comparison, RBC production in control marrow cultures decreased by 4% to 13%.
The researchers said their experiments revealed additional important findings. First, they found that erythroid differentiation in the marrow cultures “excellently” phenocopied erythroid differentiation in vivo. This suggests these cultures can serve as a reliable platform in preclinical studies.
Second, the team said the fact that epigenetic differences between RBC precursors can lead to their preferential death or survival has broad implications. And querying the cells that preferentially survive could provide important insights. ![]()

The production of two components of hemoglobin may be out of sync in Diamond Blackfan anemia (DBA) and myelodysplastic syndromes (MDS), according to a new study.
Researchers found that, in samples from patients with DBA or MDS, ribosome dysfunction delayed globin production, while heme synthesis proceeded normally.
This disruption in heme-globin coordination led to a buildup of toxic heme that killed red blood cell (RBC) precursors.
However, treating patient samples with a compound that blocks heme synthesis increased RBC production in both DBA and MDS.
Zhantao Yang, MD, of the University of Washington in Seattle, and his colleagues reported these findings in Science Translational Medicine.
Both DBA and MDS have been linked to defects in ribosome assembly, which is critical to protein production, but how this leads to anemia remains unknown.
To find out, Dr Yang and his colleagues analyzed bone marrow cells from patients with DBA (n=3) or MDS with del(5q) (n=6).
The researchers found that globin translation proceeded slowly in these samples, but heme synthesis proceeded normally.
This resulted in insufficient globin, excess heme, and excess reactive oxygen species in early erythroid precursors and, ultimately, the death of colony-forming unit–erythroid/proerythroblast cells.
The cells that were able to rapidly export heme or slow its synthesis survived and matured into RBCs, but the other colony-forming unit–erythroid cells/early proerythroblasts died.
The researchers noted that it is not clear how excess heme induces cell death in RBC precursors, but they said it likely involves both ferroptosis and apoptosis.
Regardless of the mechanism of cell death, the team found that treating the patients’ cells with succinylacetone (10 mM), a compound that blocks heme synthesis, improved RBC production.
The treatment improved RBC production in DBA and del(5q) MDS marrow cultures by 68% to 95% (P=0.03 to 0.05). In comparison, RBC production in control marrow cultures decreased by 4% to 13%.
The researchers said their experiments revealed additional important findings. First, they found that erythroid differentiation in the marrow cultures “excellently” phenocopied erythroid differentiation in vivo. This suggests these cultures can serve as a reliable platform in preclinical studies.
Second, the team said the fact that epigenetic differences between RBC precursors can lead to their preferential death or survival has broad implications. And querying the cells that preferentially survive could provide important insights. ![]()

The production of two components of hemoglobin may be out of sync in Diamond Blackfan anemia (DBA) and myelodysplastic syndromes (MDS), according to a new study.
Researchers found that, in samples from patients with DBA or MDS, ribosome dysfunction delayed globin production, while heme synthesis proceeded normally.
This disruption in heme-globin coordination led to a buildup of toxic heme that killed red blood cell (RBC) precursors.
However, treating patient samples with a compound that blocks heme synthesis increased RBC production in both DBA and MDS.
Zhantao Yang, MD, of the University of Washington in Seattle, and his colleagues reported these findings in Science Translational Medicine.
Both DBA and MDS have been linked to defects in ribosome assembly, which is critical to protein production, but how this leads to anemia remains unknown.
To find out, Dr Yang and his colleagues analyzed bone marrow cells from patients with DBA (n=3) or MDS with del(5q) (n=6).
The researchers found that globin translation proceeded slowly in these samples, but heme synthesis proceeded normally.
This resulted in insufficient globin, excess heme, and excess reactive oxygen species in early erythroid precursors and, ultimately, the death of colony-forming unit–erythroid/proerythroblast cells.
The cells that were able to rapidly export heme or slow its synthesis survived and matured into RBCs, but the other colony-forming unit–erythroid cells/early proerythroblasts died.
The researchers noted that it is not clear how excess heme induces cell death in RBC precursors, but they said it likely involves both ferroptosis and apoptosis.
Regardless of the mechanism of cell death, the team found that treating the patients’ cells with succinylacetone (10 mM), a compound that blocks heme synthesis, improved RBC production.
The treatment improved RBC production in DBA and del(5q) MDS marrow cultures by 68% to 95% (P=0.03 to 0.05). In comparison, RBC production in control marrow cultures decreased by 4% to 13%.
The researchers said their experiments revealed additional important findings. First, they found that erythroid differentiation in the marrow cultures “excellently” phenocopied erythroid differentiation in vivo. This suggests these cultures can serve as a reliable platform in preclinical studies.
Second, the team said the fact that epigenetic differences between RBC precursors can lead to their preferential death or survival has broad implications. And querying the cells that preferentially survive could provide important insights. ![]()
Rigosertib falls short for high-risk myelodysplastic syndromes after failure on azacitidine or decitabine
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
THE LANCET ONCOLOGY
Key clinical point: Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
Major finding: Median overall survival was 8.2 months (95% CI, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group.
Data source: An open-label, randomized controlled trial involving 299 patients at 74 medical centers.
Disclosures: The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society..
Rigosertib falls short for high-risk myelodysplastic syndromes after failure on azacitidine or decitabine
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
THE LANCET ONCOLOGY
Key clinical point: Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
Major finding: Median overall survival was 8.2 months (95% CI, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group.
Data source: An open-label, randomized controlled trial involving 299 patients at 74 medical centers.
Disclosures: The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society..
In myelodysplastic syndrome, improved tool for predicting death after HCT
A new risk-stratification tool goes one better than the standard tools used to predict survival in those undergoing allogeneic hematopoietic cell transplantation (allo HCT) for myelodysplastic syndrome, based on a study published online April 4 in the Journal of Clinical Oncology.
The concordance index for the new risk-stratification tool was modestly better at 0.575, compared with 0.538 for the standard International Prognostic Scoring System (IPSS) and 0.554 for the revised IPSS (IPSS-R), according to Dr. Brian C. Shaffer of Memorial Sloan Kettering Cancer Center, New York, and his colleagues who participate in the Center for International Blood and Marrow Transplant Research (CIBMTR) network.
“The proposed system generally agrees with the IPSS-R in the very high–risk subcategory; however, a significant portion of patients in high- and very high–risk IPSS-R groups were represented in the low- and intermediate-risk proposed scoring subcategories. The 3-year survival in patients classified as high risk with the IPSS-R was 75%; it was 57% in those classified as low or intermediate risk with the proposed system,” the researchers wrote.
Further, the “scoring system uses readily available clinical data and can be calculated quickly, facilitating patient consultation with respect to allo HCT, and may also be used to identify high-risk populations where interventions such as post–allo HCT maintenance therapies may be of benefit,” they wrote (J Clin Oncol. 2016 April 4. doi: 10.1200/JCO.2015.65.0515).
The data were obtained from the CIBMTR, a combined research program of the Medical College of Wisconsin and the National Marrow Donor Program. The CIBMTR comprises a voluntary network of more than 450 transplantation centers worldwide that contribute data on consecutive allo and autologous HCTs to a centralized statistical center.
The researchers applied the prognostic tool to 2,133 patients with MDS undergoing HLA-matched (n = 1,728) or -mismatched (n = 405) allo HCT. Factors prognostic of mortality were identified in a training subset (n = 1,151) of the HLA-matched cohort. A weighted score using these factors was then assigned to the validation cohort of 577 remaining patients undergoing HLA-matched allo HCT as well as to patients undergoing HLA-mismatched allo HCT. The training data set was used to develop a prognostic scoring system, and the validation data set was used to assess the prognostic ability of the scoring system, the researchers noted.
In the scoring system, 1 point was assigned for the following factors: Blood blasts greater than 3%, platelet levels of 50 × 109/L or less at transplantation, Karnofsky performance status less than 90%, comprehensive cytogenetic risk score of poor or very poor, and age 30-49 years. Two points were assigned for monosomal karyotype and age 50 years or older.
Based on the scoring system, 3-year overall survival after transplantation was 71% in patients with scores of 1 point, 49% with scores of 2-3, 41% with scores of 4-5, and 25% with scores of 6 or more. Increasing score was predictive of increased relapse and treatment-related mortality in the HLA-matched set and of relapse in the HLA-mismatched cohort.
To develop the scoring system, the researchers used a model that weighed patient age; sex; and Karnofsky performance status; disease stage at transplantation; comprehensive cytogenetic risk status; bone marrow and peripheral blood blast percentages; hemoglobin, neutrophil, and platelet counts at diagnosis and pretransplantation; lactate dehydrogenase at transplantation; pretransplantation therapy (hypomethylating agents, chemotherapy, neither, or both); time from diagnosis to transplantation; year of transplantation; conditioning regimen and regimen intensity (myeloablative v reduced intensity); donor–recipient sex match or mismatch; graft-versus-host disease prophylaxis; graft type (bone marrow vs. peripheral blood); presence of secondary myelodysplastic syndrome; and unrelated donor vs. related donor.
There were no significant differences in overall survival at 1, 3, and 5 years or in the 3-year incidences of relapse and treatment-related mortality in the training subset and the validation cohort.
Data on somatic mutations have become relevant in myelodysplastic syndrome prognostication and were missing from this analysis, the researchers wrote. “The next generation of prognostic tools will need to account for this information.”
Dr. Shaffer had no relevant financial disclosures.
On Twitter @maryjodales
A new risk-stratification tool goes one better than the standard tools used to predict survival in those undergoing allogeneic hematopoietic cell transplantation (allo HCT) for myelodysplastic syndrome, based on a study published online April 4 in the Journal of Clinical Oncology.
The concordance index for the new risk-stratification tool was modestly better at 0.575, compared with 0.538 for the standard International Prognostic Scoring System (IPSS) and 0.554 for the revised IPSS (IPSS-R), according to Dr. Brian C. Shaffer of Memorial Sloan Kettering Cancer Center, New York, and his colleagues who participate in the Center for International Blood and Marrow Transplant Research (CIBMTR) network.
“The proposed system generally agrees with the IPSS-R in the very high–risk subcategory; however, a significant portion of patients in high- and very high–risk IPSS-R groups were represented in the low- and intermediate-risk proposed scoring subcategories. The 3-year survival in patients classified as high risk with the IPSS-R was 75%; it was 57% in those classified as low or intermediate risk with the proposed system,” the researchers wrote.
Further, the “scoring system uses readily available clinical data and can be calculated quickly, facilitating patient consultation with respect to allo HCT, and may also be used to identify high-risk populations where interventions such as post–allo HCT maintenance therapies may be of benefit,” they wrote (J Clin Oncol. 2016 April 4. doi: 10.1200/JCO.2015.65.0515).
The data were obtained from the CIBMTR, a combined research program of the Medical College of Wisconsin and the National Marrow Donor Program. The CIBMTR comprises a voluntary network of more than 450 transplantation centers worldwide that contribute data on consecutive allo and autologous HCTs to a centralized statistical center.
The researchers applied the prognostic tool to 2,133 patients with MDS undergoing HLA-matched (n = 1,728) or -mismatched (n = 405) allo HCT. Factors prognostic of mortality were identified in a training subset (n = 1,151) of the HLA-matched cohort. A weighted score using these factors was then assigned to the validation cohort of 577 remaining patients undergoing HLA-matched allo HCT as well as to patients undergoing HLA-mismatched allo HCT. The training data set was used to develop a prognostic scoring system, and the validation data set was used to assess the prognostic ability of the scoring system, the researchers noted.
In the scoring system, 1 point was assigned for the following factors: Blood blasts greater than 3%, platelet levels of 50 × 109/L or less at transplantation, Karnofsky performance status less than 90%, comprehensive cytogenetic risk score of poor or very poor, and age 30-49 years. Two points were assigned for monosomal karyotype and age 50 years or older.
Based on the scoring system, 3-year overall survival after transplantation was 71% in patients with scores of 1 point, 49% with scores of 2-3, 41% with scores of 4-5, and 25% with scores of 6 or more. Increasing score was predictive of increased relapse and treatment-related mortality in the HLA-matched set and of relapse in the HLA-mismatched cohort.
To develop the scoring system, the researchers used a model that weighed patient age; sex; and Karnofsky performance status; disease stage at transplantation; comprehensive cytogenetic risk status; bone marrow and peripheral blood blast percentages; hemoglobin, neutrophil, and platelet counts at diagnosis and pretransplantation; lactate dehydrogenase at transplantation; pretransplantation therapy (hypomethylating agents, chemotherapy, neither, or both); time from diagnosis to transplantation; year of transplantation; conditioning regimen and regimen intensity (myeloablative v reduced intensity); donor–recipient sex match or mismatch; graft-versus-host disease prophylaxis; graft type (bone marrow vs. peripheral blood); presence of secondary myelodysplastic syndrome; and unrelated donor vs. related donor.
There were no significant differences in overall survival at 1, 3, and 5 years or in the 3-year incidences of relapse and treatment-related mortality in the training subset and the validation cohort.
Data on somatic mutations have become relevant in myelodysplastic syndrome prognostication and were missing from this analysis, the researchers wrote. “The next generation of prognostic tools will need to account for this information.”
Dr. Shaffer had no relevant financial disclosures.
On Twitter @maryjodales
A new risk-stratification tool goes one better than the standard tools used to predict survival in those undergoing allogeneic hematopoietic cell transplantation (allo HCT) for myelodysplastic syndrome, based on a study published online April 4 in the Journal of Clinical Oncology.
The concordance index for the new risk-stratification tool was modestly better at 0.575, compared with 0.538 for the standard International Prognostic Scoring System (IPSS) and 0.554 for the revised IPSS (IPSS-R), according to Dr. Brian C. Shaffer of Memorial Sloan Kettering Cancer Center, New York, and his colleagues who participate in the Center for International Blood and Marrow Transplant Research (CIBMTR) network.
“The proposed system generally agrees with the IPSS-R in the very high–risk subcategory; however, a significant portion of patients in high- and very high–risk IPSS-R groups were represented in the low- and intermediate-risk proposed scoring subcategories. The 3-year survival in patients classified as high risk with the IPSS-R was 75%; it was 57% in those classified as low or intermediate risk with the proposed system,” the researchers wrote.
Further, the “scoring system uses readily available clinical data and can be calculated quickly, facilitating patient consultation with respect to allo HCT, and may also be used to identify high-risk populations where interventions such as post–allo HCT maintenance therapies may be of benefit,” they wrote (J Clin Oncol. 2016 April 4. doi: 10.1200/JCO.2015.65.0515).
The data were obtained from the CIBMTR, a combined research program of the Medical College of Wisconsin and the National Marrow Donor Program. The CIBMTR comprises a voluntary network of more than 450 transplantation centers worldwide that contribute data on consecutive allo and autologous HCTs to a centralized statistical center.
The researchers applied the prognostic tool to 2,133 patients with MDS undergoing HLA-matched (n = 1,728) or -mismatched (n = 405) allo HCT. Factors prognostic of mortality were identified in a training subset (n = 1,151) of the HLA-matched cohort. A weighted score using these factors was then assigned to the validation cohort of 577 remaining patients undergoing HLA-matched allo HCT as well as to patients undergoing HLA-mismatched allo HCT. The training data set was used to develop a prognostic scoring system, and the validation data set was used to assess the prognostic ability of the scoring system, the researchers noted.
In the scoring system, 1 point was assigned for the following factors: Blood blasts greater than 3%, platelet levels of 50 × 109/L or less at transplantation, Karnofsky performance status less than 90%, comprehensive cytogenetic risk score of poor or very poor, and age 30-49 years. Two points were assigned for monosomal karyotype and age 50 years or older.
Based on the scoring system, 3-year overall survival after transplantation was 71% in patients with scores of 1 point, 49% with scores of 2-3, 41% with scores of 4-5, and 25% with scores of 6 or more. Increasing score was predictive of increased relapse and treatment-related mortality in the HLA-matched set and of relapse in the HLA-mismatched cohort.
To develop the scoring system, the researchers used a model that weighed patient age; sex; and Karnofsky performance status; disease stage at transplantation; comprehensive cytogenetic risk status; bone marrow and peripheral blood blast percentages; hemoglobin, neutrophil, and platelet counts at diagnosis and pretransplantation; lactate dehydrogenase at transplantation; pretransplantation therapy (hypomethylating agents, chemotherapy, neither, or both); time from diagnosis to transplantation; year of transplantation; conditioning regimen and regimen intensity (myeloablative v reduced intensity); donor–recipient sex match or mismatch; graft-versus-host disease prophylaxis; graft type (bone marrow vs. peripheral blood); presence of secondary myelodysplastic syndrome; and unrelated donor vs. related donor.
There were no significant differences in overall survival at 1, 3, and 5 years or in the 3-year incidences of relapse and treatment-related mortality in the training subset and the validation cohort.
Data on somatic mutations have become relevant in myelodysplastic syndrome prognostication and were missing from this analysis, the researchers wrote. “The next generation of prognostic tools will need to account for this information.”
Dr. Shaffer had no relevant financial disclosures.
On Twitter @maryjodales
FROM JCO
Key clinical point: A portion of patients with myelodysplastic syndrome in high- and very high–risk groups of the revised International Prognostic Scoring System (IPSS-R) were represented in the low- and intermediate-risk groups of the proposed scoring subcategories.
Major finding: The 3-year survival in patients classified as high risk with the IPSS-R was 75%; it was 57% in those classified as low or intermediate risk with the proposed system.
Data source: The Center for International Blood and Marrow Transplant Research (CIBMTR), a combined research program of the Medical College of Wisconsin and the National Marrow Donor Program. The CIBMTR comprises a voluntary network of more than 450 transplantation centers worldwide that contribute data on consecutive allo and autologous HCTs to a centralized statistical center.
Disclosures: Dr. Shaffer had no relevant financial disclosures.
Drug exhibits preclinical activity against MDS

Researchers have found the fusion protein APG101 can rescue erythropoiesis in bone marrow samples from patients with lower-risk myelodysplastic syndromes (MDS).
Previous research suggested that CD95—a receptor that can induce apoptosis when triggered by the CD95 ligand—is overexpressed in two-thirds of patients with lower-risk MDS, and overexpression of CD95 is predictive of a lower response to erythropoiesis-stimulating agents (ESAs).
APG101, which consists of the extracellular domain of the CD95 receptor and the Fc domain of an IgG antibody, is designed to block the CD95 ligand.
The new study showed that APG101 can inhibit apoptosis in erythrocyte precursor cells and improve their overall proliferation rate. The drug increased the number of burst-forming unit-erythroid (BFU-E) progenitors in samples from MDS patients with low BFU-E numbers at baseline.
“APG101 added to cellular assays efficiently rescued the growth of erythroid progenitors in MDS patients harboring a profound defect of erythropoiesis, independent of the expression level of CD95 or CD95 ligand,” said Michaela Fontenay, MD, PhD, of the Institut Cochin in Paris, France.
Dr Fontenay and her colleagues described these results in Oncotarget. The research was funded by Apogenix, the company developing APG101.
By comparing bone marrow samples from MDS patients and healthy control subjects, the researchers found that CD95, but not CD95 ligand, was overexpressed in patients with lower-risk MDS.
Further analysis revealed that a patient’s CD95 expression level at diagnosis could predict response to an ESA. Specifically, CD95 overexpression was predictive of a lower response rate to ESAs in patients with low- or intermediate-1-risk MDS.
Next, the researchers tested bone marrow erythroid progenitors from 3 control subjects and 5 patients with MDS and found that CD95 expression increased during MDS erythroid progenitor amplification but remained lower in control cultures.
On day 5 of culture, the mean number of BFU-Es was significantly lower in MDS patient samples than in controls. And treatment with APG101 prompted a dose-dependent increase in BFU-E growth in MDS samples but not in controls.
When the researchers added APG101 (at 10 μg/mL) to the cultures over 7 days, they observed an improvement in the proliferation of erythroblasts but no significant effect on the kinetics of differentiation.
They also found that APG101 reduced apoptosis in immature precursors by 30% but had no effect on apoptosis in mature precursors.
Baseline BFU-E number affects response
The researchers then assessed the effects of APG101 in samples from 5 control subjects and 20 MDS patients with varying responses to ESAs and varying baseline levels of BFU-Es.
Fifteen of the MDS patients had a significantly lower number of baseline BFU-Es than controls (P=0.005), but 5 MDS patients had a mean number of BFU-Es that was comparable to controls (P=0.429). There was no significant difference in WHO classification or CD95 expression between the 2 groups of MDS patients (P=0.612).
However, 11 of the 15 patients with low erythropoiesis had received an ESA, and all of them were resistant to this treatment. In all, 15 of the MDS patients had received an ESA, and 14 were resistant to it (6 primary and 8 secondary).
The researchers found that APG101 induced a dose-dependent increase of BFU-Es in samples from the 15 MDS patients with low erythropoiesis but not in samples from the 5 patients with normal erythropoiesis or in the control samples (P<0.001).
The team said that a low BFU-E number at baseline was significantly associated with in vitro response to APG101 among the 20 MDS patients (P=0.031) and the 14 ESA-resistant patients (P=0.027).
Further investigation confirmed that a low clonogenic progenitor number at baseline, but not the level of CD95 or CD95 ligand expression, was predictive of the response to APG101.
“This study provides a rationale for further clinical investigation of this potential new therapeutic option in patients with severely impaired erythropoiesis who are resistant to erythropoiesis-stimulating agents,” Dr Fontenay said.
Apogenix has conducted a phase 1 trial of APG101 in transfusion-dependent patients with low- to intermediate-1-risk MDS. The company expects the results of this trial will be available in the coming months. ![]()

Researchers have found the fusion protein APG101 can rescue erythropoiesis in bone marrow samples from patients with lower-risk myelodysplastic syndromes (MDS).
Previous research suggested that CD95—a receptor that can induce apoptosis when triggered by the CD95 ligand—is overexpressed in two-thirds of patients with lower-risk MDS, and overexpression of CD95 is predictive of a lower response to erythropoiesis-stimulating agents (ESAs).
APG101, which consists of the extracellular domain of the CD95 receptor and the Fc domain of an IgG antibody, is designed to block the CD95 ligand.
The new study showed that APG101 can inhibit apoptosis in erythrocyte precursor cells and improve their overall proliferation rate. The drug increased the number of burst-forming unit-erythroid (BFU-E) progenitors in samples from MDS patients with low BFU-E numbers at baseline.
“APG101 added to cellular assays efficiently rescued the growth of erythroid progenitors in MDS patients harboring a profound defect of erythropoiesis, independent of the expression level of CD95 or CD95 ligand,” said Michaela Fontenay, MD, PhD, of the Institut Cochin in Paris, France.
Dr Fontenay and her colleagues described these results in Oncotarget. The research was funded by Apogenix, the company developing APG101.
By comparing bone marrow samples from MDS patients and healthy control subjects, the researchers found that CD95, but not CD95 ligand, was overexpressed in patients with lower-risk MDS.
Further analysis revealed that a patient’s CD95 expression level at diagnosis could predict response to an ESA. Specifically, CD95 overexpression was predictive of a lower response rate to ESAs in patients with low- or intermediate-1-risk MDS.
Next, the researchers tested bone marrow erythroid progenitors from 3 control subjects and 5 patients with MDS and found that CD95 expression increased during MDS erythroid progenitor amplification but remained lower in control cultures.
On day 5 of culture, the mean number of BFU-Es was significantly lower in MDS patient samples than in controls. And treatment with APG101 prompted a dose-dependent increase in BFU-E growth in MDS samples but not in controls.
When the researchers added APG101 (at 10 μg/mL) to the cultures over 7 days, they observed an improvement in the proliferation of erythroblasts but no significant effect on the kinetics of differentiation.
They also found that APG101 reduced apoptosis in immature precursors by 30% but had no effect on apoptosis in mature precursors.
Baseline BFU-E number affects response
The researchers then assessed the effects of APG101 in samples from 5 control subjects and 20 MDS patients with varying responses to ESAs and varying baseline levels of BFU-Es.
Fifteen of the MDS patients had a significantly lower number of baseline BFU-Es than controls (P=0.005), but 5 MDS patients had a mean number of BFU-Es that was comparable to controls (P=0.429). There was no significant difference in WHO classification or CD95 expression between the 2 groups of MDS patients (P=0.612).
However, 11 of the 15 patients with low erythropoiesis had received an ESA, and all of them were resistant to this treatment. In all, 15 of the MDS patients had received an ESA, and 14 were resistant to it (6 primary and 8 secondary).
The researchers found that APG101 induced a dose-dependent increase of BFU-Es in samples from the 15 MDS patients with low erythropoiesis but not in samples from the 5 patients with normal erythropoiesis or in the control samples (P<0.001).
The team said that a low BFU-E number at baseline was significantly associated with in vitro response to APG101 among the 20 MDS patients (P=0.031) and the 14 ESA-resistant patients (P=0.027).
Further investigation confirmed that a low clonogenic progenitor number at baseline, but not the level of CD95 or CD95 ligand expression, was predictive of the response to APG101.
“This study provides a rationale for further clinical investigation of this potential new therapeutic option in patients with severely impaired erythropoiesis who are resistant to erythropoiesis-stimulating agents,” Dr Fontenay said.
Apogenix has conducted a phase 1 trial of APG101 in transfusion-dependent patients with low- to intermediate-1-risk MDS. The company expects the results of this trial will be available in the coming months. ![]()

Researchers have found the fusion protein APG101 can rescue erythropoiesis in bone marrow samples from patients with lower-risk myelodysplastic syndromes (MDS).
Previous research suggested that CD95—a receptor that can induce apoptosis when triggered by the CD95 ligand—is overexpressed in two-thirds of patients with lower-risk MDS, and overexpression of CD95 is predictive of a lower response to erythropoiesis-stimulating agents (ESAs).
APG101, which consists of the extracellular domain of the CD95 receptor and the Fc domain of an IgG antibody, is designed to block the CD95 ligand.
The new study showed that APG101 can inhibit apoptosis in erythrocyte precursor cells and improve their overall proliferation rate. The drug increased the number of burst-forming unit-erythroid (BFU-E) progenitors in samples from MDS patients with low BFU-E numbers at baseline.
“APG101 added to cellular assays efficiently rescued the growth of erythroid progenitors in MDS patients harboring a profound defect of erythropoiesis, independent of the expression level of CD95 or CD95 ligand,” said Michaela Fontenay, MD, PhD, of the Institut Cochin in Paris, France.
Dr Fontenay and her colleagues described these results in Oncotarget. The research was funded by Apogenix, the company developing APG101.
By comparing bone marrow samples from MDS patients and healthy control subjects, the researchers found that CD95, but not CD95 ligand, was overexpressed in patients with lower-risk MDS.
Further analysis revealed that a patient’s CD95 expression level at diagnosis could predict response to an ESA. Specifically, CD95 overexpression was predictive of a lower response rate to ESAs in patients with low- or intermediate-1-risk MDS.
Next, the researchers tested bone marrow erythroid progenitors from 3 control subjects and 5 patients with MDS and found that CD95 expression increased during MDS erythroid progenitor amplification but remained lower in control cultures.
On day 5 of culture, the mean number of BFU-Es was significantly lower in MDS patient samples than in controls. And treatment with APG101 prompted a dose-dependent increase in BFU-E growth in MDS samples but not in controls.
When the researchers added APG101 (at 10 μg/mL) to the cultures over 7 days, they observed an improvement in the proliferation of erythroblasts but no significant effect on the kinetics of differentiation.
They also found that APG101 reduced apoptosis in immature precursors by 30% but had no effect on apoptosis in mature precursors.
Baseline BFU-E number affects response
The researchers then assessed the effects of APG101 in samples from 5 control subjects and 20 MDS patients with varying responses to ESAs and varying baseline levels of BFU-Es.
Fifteen of the MDS patients had a significantly lower number of baseline BFU-Es than controls (P=0.005), but 5 MDS patients had a mean number of BFU-Es that was comparable to controls (P=0.429). There was no significant difference in WHO classification or CD95 expression between the 2 groups of MDS patients (P=0.612).
However, 11 of the 15 patients with low erythropoiesis had received an ESA, and all of them were resistant to this treatment. In all, 15 of the MDS patients had received an ESA, and 14 were resistant to it (6 primary and 8 secondary).
The researchers found that APG101 induced a dose-dependent increase of BFU-Es in samples from the 15 MDS patients with low erythropoiesis but not in samples from the 5 patients with normal erythropoiesis or in the control samples (P<0.001).
The team said that a low BFU-E number at baseline was significantly associated with in vitro response to APG101 among the 20 MDS patients (P=0.031) and the 14 ESA-resistant patients (P=0.027).
Further investigation confirmed that a low clonogenic progenitor number at baseline, but not the level of CD95 or CD95 ligand expression, was predictive of the response to APG101.
“This study provides a rationale for further clinical investigation of this potential new therapeutic option in patients with severely impaired erythropoiesis who are resistant to erythropoiesis-stimulating agents,” Dr Fontenay said.
Apogenix has conducted a phase 1 trial of APG101 in transfusion-dependent patients with low- to intermediate-1-risk MDS. The company expects the results of this trial will be available in the coming months. ![]()
Drug may best BSC in some high-risk MDS patients

Results of a phase 3 trial suggest the small-molecule inhibitor rigosertib may improve overall survival (OS) in some patients with higher-risk myelodysplastic syndromes (HR-MDS).
Overall, researchers found no significant difference in OS between patients who received rigosertib and those who received best supportive care (BSC).
However, the data indicate that rigosertib can confer a survival benefit in certain subgroups of HR-MDS patients.
The results of this trial, known as ONTIME, were published in The Lancet Oncology. The trial was sponsored by Onconova Therapeutics, Inc., the company developing rigosertib.
The trial enrolled 299 HR-MDS patients. They had refractory anemia with excess blasts (RAEB)-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia based on local site assessment. They had all failed treatment with a hypomethylating agent (HMA) in the past 2 years.
The patients were randomized (2:1) to receive rigosertib at 1800 mg per 24 hours via 72-hour continuous intravenous (IV) infusion, administered every other week (n=199), or BSC with or without low-dose cytarabine (n=100).
At a median follow-up of 19.5 months, there was no significant difference in OS between the treatment arms. The median OS was 8.2 months in the rigosertib arm and 5.9 months in the BSC arm. The hazard ratio (HR) was 0.87 (P=0.33).
However, the researchers said that subgroup analyses suggested rigosertib may provide a survival benefit over BSC in some HR-MDS patients. This includes:
- Patients younger than 75 years of age (HR=0.55, P=0.0010)
- Patients who received HMA therapy for 9 months or fewer (HR=0.54, P=0.0016)
- Patients with primary, rather than secondary, HMA failure (HR=0.72, P=0.060)
- Patients who were classified as “very high risk” according to the Revised International Prognostic Scoring System (HR=0.61, P=0.015)
- Patients with monosomy 7 (HR=0.26, P=0.0041)
- Patients with trisomy 8 (HR=0.28, P=0.0083).
The most common grade 3 or higher adverse events—in the rigosertib and BSC arms, respectively—were anemia (18% vs 8%), thrombocytopenia (19% vs 7%), neutropenia (17% vs 8%), febrile neutropenia (12% vs 11%), and pneumonia (12% vs 11%).
Twenty-two percent of patients in the rigosertib arm and 33% in the BSC arm died due to adverse events. Three deaths were attributed to rigosertib.
“Rigosertib was well-tolerated in patients with a high unmet medical need who have no approved therapeutic options,” said study author Guillermo Garcia-Manero, MD, of The University of Texas MD Anderson Cancer Center in Houston.
“We are impressed by the trend to notable efficacy in well-defined, well-balanced subgroups of HR-MDS patients with very poor prognosis. Based on these findings, we have designed the new phase 3 INSPIRE study with IV rigosertib, which is currently enrolling patients.”
INSPIRE is a randomized, controlled study designed to assess the efficacy and safety of IV rigosertib in HR-MDS patients under 80 years of age who had progressed on, failed to respond to, or relapsed after previous treatment with an HMA within the first 9 months of HMA treatment initiation.
The trial is expected to enroll approximately 225 patients, who will be randomized at a 2:1 ratio into 2 treatment arms: IV rigosertib plus BSC versus physician’s choice plus BSC. The primary endpoint is OS. Full details on the trial can be found on clinicaltrials.gov (NCT02562443). ![]()

Results of a phase 3 trial suggest the small-molecule inhibitor rigosertib may improve overall survival (OS) in some patients with higher-risk myelodysplastic syndromes (HR-MDS).
Overall, researchers found no significant difference in OS between patients who received rigosertib and those who received best supportive care (BSC).
However, the data indicate that rigosertib can confer a survival benefit in certain subgroups of HR-MDS patients.
The results of this trial, known as ONTIME, were published in The Lancet Oncology. The trial was sponsored by Onconova Therapeutics, Inc., the company developing rigosertib.
The trial enrolled 299 HR-MDS patients. They had refractory anemia with excess blasts (RAEB)-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia based on local site assessment. They had all failed treatment with a hypomethylating agent (HMA) in the past 2 years.
The patients were randomized (2:1) to receive rigosertib at 1800 mg per 24 hours via 72-hour continuous intravenous (IV) infusion, administered every other week (n=199), or BSC with or without low-dose cytarabine (n=100).
At a median follow-up of 19.5 months, there was no significant difference in OS between the treatment arms. The median OS was 8.2 months in the rigosertib arm and 5.9 months in the BSC arm. The hazard ratio (HR) was 0.87 (P=0.33).
However, the researchers said that subgroup analyses suggested rigosertib may provide a survival benefit over BSC in some HR-MDS patients. This includes:
- Patients younger than 75 years of age (HR=0.55, P=0.0010)
- Patients who received HMA therapy for 9 months or fewer (HR=0.54, P=0.0016)
- Patients with primary, rather than secondary, HMA failure (HR=0.72, P=0.060)
- Patients who were classified as “very high risk” according to the Revised International Prognostic Scoring System (HR=0.61, P=0.015)
- Patients with monosomy 7 (HR=0.26, P=0.0041)
- Patients with trisomy 8 (HR=0.28, P=0.0083).
The most common grade 3 or higher adverse events—in the rigosertib and BSC arms, respectively—were anemia (18% vs 8%), thrombocytopenia (19% vs 7%), neutropenia (17% vs 8%), febrile neutropenia (12% vs 11%), and pneumonia (12% vs 11%).
Twenty-two percent of patients in the rigosertib arm and 33% in the BSC arm died due to adverse events. Three deaths were attributed to rigosertib.
“Rigosertib was well-tolerated in patients with a high unmet medical need who have no approved therapeutic options,” said study author Guillermo Garcia-Manero, MD, of The University of Texas MD Anderson Cancer Center in Houston.
“We are impressed by the trend to notable efficacy in well-defined, well-balanced subgroups of HR-MDS patients with very poor prognosis. Based on these findings, we have designed the new phase 3 INSPIRE study with IV rigosertib, which is currently enrolling patients.”
INSPIRE is a randomized, controlled study designed to assess the efficacy and safety of IV rigosertib in HR-MDS patients under 80 years of age who had progressed on, failed to respond to, or relapsed after previous treatment with an HMA within the first 9 months of HMA treatment initiation.
The trial is expected to enroll approximately 225 patients, who will be randomized at a 2:1 ratio into 2 treatment arms: IV rigosertib plus BSC versus physician’s choice plus BSC. The primary endpoint is OS. Full details on the trial can be found on clinicaltrials.gov (NCT02562443). ![]()

Results of a phase 3 trial suggest the small-molecule inhibitor rigosertib may improve overall survival (OS) in some patients with higher-risk myelodysplastic syndromes (HR-MDS).
Overall, researchers found no significant difference in OS between patients who received rigosertib and those who received best supportive care (BSC).
However, the data indicate that rigosertib can confer a survival benefit in certain subgroups of HR-MDS patients.
The results of this trial, known as ONTIME, were published in The Lancet Oncology. The trial was sponsored by Onconova Therapeutics, Inc., the company developing rigosertib.
The trial enrolled 299 HR-MDS patients. They had refractory anemia with excess blasts (RAEB)-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia based on local site assessment. They had all failed treatment with a hypomethylating agent (HMA) in the past 2 years.
The patients were randomized (2:1) to receive rigosertib at 1800 mg per 24 hours via 72-hour continuous intravenous (IV) infusion, administered every other week (n=199), or BSC with or without low-dose cytarabine (n=100).
At a median follow-up of 19.5 months, there was no significant difference in OS between the treatment arms. The median OS was 8.2 months in the rigosertib arm and 5.9 months in the BSC arm. The hazard ratio (HR) was 0.87 (P=0.33).
However, the researchers said that subgroup analyses suggested rigosertib may provide a survival benefit over BSC in some HR-MDS patients. This includes:
- Patients younger than 75 years of age (HR=0.55, P=0.0010)
- Patients who received HMA therapy for 9 months or fewer (HR=0.54, P=0.0016)
- Patients with primary, rather than secondary, HMA failure (HR=0.72, P=0.060)
- Patients who were classified as “very high risk” according to the Revised International Prognostic Scoring System (HR=0.61, P=0.015)
- Patients with monosomy 7 (HR=0.26, P=0.0041)
- Patients with trisomy 8 (HR=0.28, P=0.0083).
The most common grade 3 or higher adverse events—in the rigosertib and BSC arms, respectively—were anemia (18% vs 8%), thrombocytopenia (19% vs 7%), neutropenia (17% vs 8%), febrile neutropenia (12% vs 11%), and pneumonia (12% vs 11%).
Twenty-two percent of patients in the rigosertib arm and 33% in the BSC arm died due to adverse events. Three deaths were attributed to rigosertib.
“Rigosertib was well-tolerated in patients with a high unmet medical need who have no approved therapeutic options,” said study author Guillermo Garcia-Manero, MD, of The University of Texas MD Anderson Cancer Center in Houston.
“We are impressed by the trend to notable efficacy in well-defined, well-balanced subgroups of HR-MDS patients with very poor prognosis. Based on these findings, we have designed the new phase 3 INSPIRE study with IV rigosertib, which is currently enrolling patients.”
INSPIRE is a randomized, controlled study designed to assess the efficacy and safety of IV rigosertib in HR-MDS patients under 80 years of age who had progressed on, failed to respond to, or relapsed after previous treatment with an HMA within the first 9 months of HMA treatment initiation.
The trial is expected to enroll approximately 225 patients, who will be randomized at a 2:1 ratio into 2 treatment arms: IV rigosertib plus BSC versus physician’s choice plus BSC. The primary endpoint is OS. Full details on the trial can be found on clinicaltrials.gov (NCT02562443). ![]()
Germline mutations linked to hematologic malignancies

A new study suggests mutations in the gene DDX41 occur in families where hematologic malignancies are common.
Previous research showed that both germline and acquired DDX41 mutations occur in families with multiple cases of late-onset myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML).
The new study, published in Blood, has linked germline mutations in DDX41 to chronic myeloid leukemia and lymphomas as well.
“This is the first gene identified in families with lymphoma and represents a major breakthrough for the field,” said study author Hamish Scott, PhD, of the University of Adelaide in South Australia.
“Researchers are recognizing now that genetic predisposition to blood cancer is more common than previously thought, and our study shows the importance of taking a thorough family history at diagnosis.”
To conduct this study, Dr Scott and his colleagues screened 2 cohorts of families with a range of hematologic disorders (malignant and non-malignant). One cohort included 240 individuals from 93 families in Australia. The other included 246 individuals from 198 families in the US.
In all, 9 of the families (3%) had germline DDX41 mutations.
Three families carried the recurrent p.D140Gfs*2 mutation, which was linked to AML.
One family carried a germline mutation—p.R525H, c.1574G.A—that was previously described only as a somatic mutation at the time of progression to MDS or AML. In the current study, the mutation was again linked to MDS and AML.
Five families carried novel DDX41 mutations.
One of these mutations was a germline substitution—c.435-2_435-1delAGinsCA—that was linked to MDS in 1 family.
Two families had a missense start-loss substitution—c.3G.A, p.M1I—that was linked to MDS, AML, chronic myeloid leukemia, and non-Hodgkin lymphoma.
One family had a DDX41 missense variant—c.490C.T, p.R164W. This was linked to Hodgkin and non-Hodgkin lymphoma (including 3 cases of follicular lymphoma). There was a possible link to multiple myeloma as well, but the diagnosis could not be confirmed.
And 1 family had a missense mutation in the helicase domain—p.G530D—that was linked to AML.
“DDX41 is a new type of cancer predisposition gene, and we are still investigating its function,” Dr Scott noted.
“But it appears to have dual roles in regulating the correct expression of genes in the cell and also enabling the immune system to respond to threats such as bacteria and viruses, as well as the development of cancer cells. Immunotherapy is a promising approach for cancer treatment, and our research to understand the function of DDX41 will help design better therapies.” ![]()

A new study suggests mutations in the gene DDX41 occur in families where hematologic malignancies are common.
Previous research showed that both germline and acquired DDX41 mutations occur in families with multiple cases of late-onset myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML).
The new study, published in Blood, has linked germline mutations in DDX41 to chronic myeloid leukemia and lymphomas as well.
“This is the first gene identified in families with lymphoma and represents a major breakthrough for the field,” said study author Hamish Scott, PhD, of the University of Adelaide in South Australia.
“Researchers are recognizing now that genetic predisposition to blood cancer is more common than previously thought, and our study shows the importance of taking a thorough family history at diagnosis.”
To conduct this study, Dr Scott and his colleagues screened 2 cohorts of families with a range of hematologic disorders (malignant and non-malignant). One cohort included 240 individuals from 93 families in Australia. The other included 246 individuals from 198 families in the US.
In all, 9 of the families (3%) had germline DDX41 mutations.
Three families carried the recurrent p.D140Gfs*2 mutation, which was linked to AML.
One family carried a germline mutation—p.R525H, c.1574G.A—that was previously described only as a somatic mutation at the time of progression to MDS or AML. In the current study, the mutation was again linked to MDS and AML.
Five families carried novel DDX41 mutations.
One of these mutations was a germline substitution—c.435-2_435-1delAGinsCA—that was linked to MDS in 1 family.
Two families had a missense start-loss substitution—c.3G.A, p.M1I—that was linked to MDS, AML, chronic myeloid leukemia, and non-Hodgkin lymphoma.
One family had a DDX41 missense variant—c.490C.T, p.R164W. This was linked to Hodgkin and non-Hodgkin lymphoma (including 3 cases of follicular lymphoma). There was a possible link to multiple myeloma as well, but the diagnosis could not be confirmed.
And 1 family had a missense mutation in the helicase domain—p.G530D—that was linked to AML.
“DDX41 is a new type of cancer predisposition gene, and we are still investigating its function,” Dr Scott noted.
“But it appears to have dual roles in regulating the correct expression of genes in the cell and also enabling the immune system to respond to threats such as bacteria and viruses, as well as the development of cancer cells. Immunotherapy is a promising approach for cancer treatment, and our research to understand the function of DDX41 will help design better therapies.” ![]()

A new study suggests mutations in the gene DDX41 occur in families where hematologic malignancies are common.
Previous research showed that both germline and acquired DDX41 mutations occur in families with multiple cases of late-onset myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML).
The new study, published in Blood, has linked germline mutations in DDX41 to chronic myeloid leukemia and lymphomas as well.
“This is the first gene identified in families with lymphoma and represents a major breakthrough for the field,” said study author Hamish Scott, PhD, of the University of Adelaide in South Australia.
“Researchers are recognizing now that genetic predisposition to blood cancer is more common than previously thought, and our study shows the importance of taking a thorough family history at diagnosis.”
To conduct this study, Dr Scott and his colleagues screened 2 cohorts of families with a range of hematologic disorders (malignant and non-malignant). One cohort included 240 individuals from 93 families in Australia. The other included 246 individuals from 198 families in the US.
In all, 9 of the families (3%) had germline DDX41 mutations.
Three families carried the recurrent p.D140Gfs*2 mutation, which was linked to AML.
One family carried a germline mutation—p.R525H, c.1574G.A—that was previously described only as a somatic mutation at the time of progression to MDS or AML. In the current study, the mutation was again linked to MDS and AML.
Five families carried novel DDX41 mutations.
One of these mutations was a germline substitution—c.435-2_435-1delAGinsCA—that was linked to MDS in 1 family.
Two families had a missense start-loss substitution—c.3G.A, p.M1I—that was linked to MDS, AML, chronic myeloid leukemia, and non-Hodgkin lymphoma.
One family had a DDX41 missense variant—c.490C.T, p.R164W. This was linked to Hodgkin and non-Hodgkin lymphoma (including 3 cases of follicular lymphoma). There was a possible link to multiple myeloma as well, but the diagnosis could not be confirmed.
And 1 family had a missense mutation in the helicase domain—p.G530D—that was linked to AML.
“DDX41 is a new type of cancer predisposition gene, and we are still investigating its function,” Dr Scott noted.
“But it appears to have dual roles in regulating the correct expression of genes in the cell and also enabling the immune system to respond to threats such as bacteria and viruses, as well as the development of cancer cells. Immunotherapy is a promising approach for cancer treatment, and our research to understand the function of DDX41 will help design better therapies.” ![]()
Generic imatinib launched with savings program

Photo by Rhoda Baer
Sun Pharma has announced the US launch of imatinib mesylate tablets, which are a generic version of Novartis’s Gleevec, for indications approved by the US Food and Drug Administration (FDA).
As part of this launch, Sun Pharma has rolled out a savings card program. The goal is to provide greater access to imatinib mesylate tablets for patients who have commercial insurance, but their out-of-pocket cost may exceed an affordable amount.
Sun Pharma’s Imatinib Mesylate Savings Card will reduce patient’s co-payment to $10. The card will also offer patients an additional savings benefit of up to $700 for a 30-day fill to offset any additional out-of-pocket cost should they be required to meet their deductible or co-insurance.
Participating pharmacies across the US can use the patient’s card as part of this program.
Eligible patients can participate in Sun Pharma’s Imatinib Mesylate Savings Card program by registering at www.imatinibrx.com or by requesting a savings card from their oncologist. Sun Pharma will be supplying its Imatinib Mesylate Savings Cards to more than 4500 oncologists.
Sun Pharma has established a Hub service so patients can call and speak with a trained healthcare professional about imatinib mesylate. The number is 1-844-502-5950.
In addition, qualifying patients can receive Sun Pharma’s imatinib mesylate at no cost. Based on qualifications for applying and including a doctor’s prescription, the Hub service will determine if a patient is qualified to receive imatinib mesylate for free. Upon acceptance, the prescription will be processed and delivered to the qualifying patient at no cost.
Sun Pharma’s imatinib mesylate was approved by the FDA in December 2015 and was granted 180 days of marketing exclusivity from the time of its launch. The drug is available in 100 mg and 400 mg tablets.
It is approved to treat:
- Newly diagnosed adult and pediatric patients with Philadelphia-chromosome-positive chronic myeloid leukemia (Ph+ CML) in chronic phase
- Patients with Ph+ CML in blast crisis, accelerated phase, or in chronic phase after failure of interferon-alpha therapy
- Adults with relapsed or refractory Ph+ acute lymphoblastic leukemia
- Adults with myelodysplastic/myeloproliferative diseases associated with PDGFR gene re-arrangements
- Adults with aggressive systemic mastocytosis without the D816V c-Kit mutation or with c-Kit mutational status unknown
- Adults with hypereosinophilic syndrome and/or chronic eosinophilic leukemia, including those who have the FIP1L1-PDGFRα fusion kinase
- Adult patients with unresectable, recurrent, and/or metastatic dermatofibrosarcoma protuberans.
Sun Pharma’s imatinib mesylate is not approved to treat patients with KIT (CD117)-positive unresectable and/or metastatic malignant gastrointestinal stromal tumors. ![]()

Photo by Rhoda Baer
Sun Pharma has announced the US launch of imatinib mesylate tablets, which are a generic version of Novartis’s Gleevec, for indications approved by the US Food and Drug Administration (FDA).
As part of this launch, Sun Pharma has rolled out a savings card program. The goal is to provide greater access to imatinib mesylate tablets for patients who have commercial insurance, but their out-of-pocket cost may exceed an affordable amount.
Sun Pharma’s Imatinib Mesylate Savings Card will reduce patient’s co-payment to $10. The card will also offer patients an additional savings benefit of up to $700 for a 30-day fill to offset any additional out-of-pocket cost should they be required to meet their deductible or co-insurance.
Participating pharmacies across the US can use the patient’s card as part of this program.
Eligible patients can participate in Sun Pharma’s Imatinib Mesylate Savings Card program by registering at www.imatinibrx.com or by requesting a savings card from their oncologist. Sun Pharma will be supplying its Imatinib Mesylate Savings Cards to more than 4500 oncologists.
Sun Pharma has established a Hub service so patients can call and speak with a trained healthcare professional about imatinib mesylate. The number is 1-844-502-5950.
In addition, qualifying patients can receive Sun Pharma’s imatinib mesylate at no cost. Based on qualifications for applying and including a doctor’s prescription, the Hub service will determine if a patient is qualified to receive imatinib mesylate for free. Upon acceptance, the prescription will be processed and delivered to the qualifying patient at no cost.
Sun Pharma’s imatinib mesylate was approved by the FDA in December 2015 and was granted 180 days of marketing exclusivity from the time of its launch. The drug is available in 100 mg and 400 mg tablets.
It is approved to treat:
- Newly diagnosed adult and pediatric patients with Philadelphia-chromosome-positive chronic myeloid leukemia (Ph+ CML) in chronic phase
- Patients with Ph+ CML in blast crisis, accelerated phase, or in chronic phase after failure of interferon-alpha therapy
- Adults with relapsed or refractory Ph+ acute lymphoblastic leukemia
- Adults with myelodysplastic/myeloproliferative diseases associated with PDGFR gene re-arrangements
- Adults with aggressive systemic mastocytosis without the D816V c-Kit mutation or with c-Kit mutational status unknown
- Adults with hypereosinophilic syndrome and/or chronic eosinophilic leukemia, including those who have the FIP1L1-PDGFRα fusion kinase
- Adult patients with unresectable, recurrent, and/or metastatic dermatofibrosarcoma protuberans.
Sun Pharma’s imatinib mesylate is not approved to treat patients with KIT (CD117)-positive unresectable and/or metastatic malignant gastrointestinal stromal tumors. ![]()

Photo by Rhoda Baer
Sun Pharma has announced the US launch of imatinib mesylate tablets, which are a generic version of Novartis’s Gleevec, for indications approved by the US Food and Drug Administration (FDA).
As part of this launch, Sun Pharma has rolled out a savings card program. The goal is to provide greater access to imatinib mesylate tablets for patients who have commercial insurance, but their out-of-pocket cost may exceed an affordable amount.
Sun Pharma’s Imatinib Mesylate Savings Card will reduce patient’s co-payment to $10. The card will also offer patients an additional savings benefit of up to $700 for a 30-day fill to offset any additional out-of-pocket cost should they be required to meet their deductible or co-insurance.
Participating pharmacies across the US can use the patient’s card as part of this program.
Eligible patients can participate in Sun Pharma’s Imatinib Mesylate Savings Card program by registering at www.imatinibrx.com or by requesting a savings card from their oncologist. Sun Pharma will be supplying its Imatinib Mesylate Savings Cards to more than 4500 oncologists.
Sun Pharma has established a Hub service so patients can call and speak with a trained healthcare professional about imatinib mesylate. The number is 1-844-502-5950.
In addition, qualifying patients can receive Sun Pharma’s imatinib mesylate at no cost. Based on qualifications for applying and including a doctor’s prescription, the Hub service will determine if a patient is qualified to receive imatinib mesylate for free. Upon acceptance, the prescription will be processed and delivered to the qualifying patient at no cost.
Sun Pharma’s imatinib mesylate was approved by the FDA in December 2015 and was granted 180 days of marketing exclusivity from the time of its launch. The drug is available in 100 mg and 400 mg tablets.
It is approved to treat:
- Newly diagnosed adult and pediatric patients with Philadelphia-chromosome-positive chronic myeloid leukemia (Ph+ CML) in chronic phase
- Patients with Ph+ CML in blast crisis, accelerated phase, or in chronic phase after failure of interferon-alpha therapy
- Adults with relapsed or refractory Ph+ acute lymphoblastic leukemia
- Adults with myelodysplastic/myeloproliferative diseases associated with PDGFR gene re-arrangements
- Adults with aggressive systemic mastocytosis without the D816V c-Kit mutation or with c-Kit mutational status unknown
- Adults with hypereosinophilic syndrome and/or chronic eosinophilic leukemia, including those who have the FIP1L1-PDGFRα fusion kinase
- Adult patients with unresectable, recurrent, and/or metastatic dermatofibrosarcoma protuberans.
Sun Pharma’s imatinib mesylate is not approved to treat patients with KIT (CD117)-positive unresectable and/or metastatic malignant gastrointestinal stromal tumors. ![]()
Medicare to cover HSCT in approved clinical trials for myeloma, myelofibrosis, sickle cell disease
Medicare will cover allogeneic hematopoietic stem cell transplantation (HSCT) for beneficiaries with multiple myeloma, myelofibrosis, or sickle cell disease in the context of approved, prospective clinical trials, the Centers for Medicare & Medicaid Services announced in a final decision memo Jan. 27.
Approvable studies must examine whether Medicare beneficiaries who receive allogeneic HSCT have improved outcomes, compared with patients who do not receive allogeneic HSCT as measured by graft vs. host disease, other transplant-related adverse events, overall survival, and, optionally, quality of life measures.
In multiple myeloma, allogeneic HSCT will be covered only for Medicare beneficiaries who have Durie-Salmon Stage II or III multiple myeloma, or International Staging System (ISS) Stage II or Stage III multiple myeloma, and are participating in an approved prospective clinical study. Such studies must control for selection bias and potential confounding by age, duration of diagnosis, disease classification, International Myeloma Working Group (IMWG) classification, ISS staging, Durie-Salmon staging, comorbid conditions, type of preparative/conditioning regimen, graft vs. host disease (GVHD) prophylaxis, donor type, and cell source, the CMS said in its memo.
In myelofibrosis, allogeneic HSCT will be covered by Medicare in an approved prospective study only for beneficiaries with Dynamic International Prognostic Scoring System (DIPSS plus) intermediate-2 or high primary or secondary myelofibrosis. Studies must be controlled for selection bias and potential confounding by age, duration of diagnosis, disease classification, DIPSS plus score, comorbid conditions, type of preparative/conditioning regimen, GVHD prophylaxis, donor type, and cell source.
In sickle cell disease, allogeneic HSCT will be covered by Medicare only for beneficiaries who have severe, symptomatic disease. Approvable studies must control for selection bias and potential confounding by age, duration of diagnosis, comorbid conditions, type of preparative/conditioning regimen, GVHD prophylaxis, donor type, and cell source.
On Twitter @maryjodales
Dr. Navneet Majhail comments: I welcome the decision by CMS [the Centers for Medicare & Medicaid Services] to cover allogeneic hematopoietic stem cell transplantation (HSCT) for multiple myeloma, myelofibrosis, and sickle cell disease under the coverage with evidence development (CED) mechanism. This action will allow us to provide transplant as a treatment option for older patients with myeloma and myelofibrosis and for Medicare beneficiaries with sickle cell disease: Lack of coverage is a real challenge at present for this population and prevents us from offering a potentially curative treatment option to these high-risk patients.

|
Dr. Navneet Majhail |
The decision is the result of collective advocacy efforts of our transplant community, patients, and patient advocacy organizations, Be the Match, and the American Society for Blood and Marrow Transplantation.
The CED asks for a prospective clinical trial that mandates the presence of a control arm of comparable patients who do not receive allogeneic transplantation. I completely support provision of transplantation on a clinical trial for CED purposes; however, I believe it would have been better to allow hematology and transplant experts to determine the appropriate study design in consultation with CMS to fulfill the CED requirements. For example, on the basis of available evidence, it will be challenging to enroll patients with high-risk myelofibrosis to a nontransplant arm. Irrespective, this is a big win for patients with these life-threatening diseases and for physicians who treat them.
Dr. Navneet Majhail is the director of the Cleveland Clinic’s Blood & Marrow Transplant Program. He serves as a staff physician at the Taussig Cancer Institute and is a professor of medicine with the Cleveland Clinic Lerner College of Medicine.
Dr. Navneet Majhail comments: I welcome the decision by CMS [the Centers for Medicare & Medicaid Services] to cover allogeneic hematopoietic stem cell transplantation (HSCT) for multiple myeloma, myelofibrosis, and sickle cell disease under the coverage with evidence development (CED) mechanism. This action will allow us to provide transplant as a treatment option for older patients with myeloma and myelofibrosis and for Medicare beneficiaries with sickle cell disease: Lack of coverage is a real challenge at present for this population and prevents us from offering a potentially curative treatment option to these high-risk patients.

|
Dr. Navneet Majhail |
The decision is the result of collective advocacy efforts of our transplant community, patients, and patient advocacy organizations, Be the Match, and the American Society for Blood and Marrow Transplantation.
The CED asks for a prospective clinical trial that mandates the presence of a control arm of comparable patients who do not receive allogeneic transplantation. I completely support provision of transplantation on a clinical trial for CED purposes; however, I believe it would have been better to allow hematology and transplant experts to determine the appropriate study design in consultation with CMS to fulfill the CED requirements. For example, on the basis of available evidence, it will be challenging to enroll patients with high-risk myelofibrosis to a nontransplant arm. Irrespective, this is a big win for patients with these life-threatening diseases and for physicians who treat them.
Dr. Navneet Majhail is the director of the Cleveland Clinic’s Blood & Marrow Transplant Program. He serves as a staff physician at the Taussig Cancer Institute and is a professor of medicine with the Cleveland Clinic Lerner College of Medicine.
Dr. Navneet Majhail comments: I welcome the decision by CMS [the Centers for Medicare & Medicaid Services] to cover allogeneic hematopoietic stem cell transplantation (HSCT) for multiple myeloma, myelofibrosis, and sickle cell disease under the coverage with evidence development (CED) mechanism. This action will allow us to provide transplant as a treatment option for older patients with myeloma and myelofibrosis and for Medicare beneficiaries with sickle cell disease: Lack of coverage is a real challenge at present for this population and prevents us from offering a potentially curative treatment option to these high-risk patients.

|
Dr. Navneet Majhail |
The decision is the result of collective advocacy efforts of our transplant community, patients, and patient advocacy organizations, Be the Match, and the American Society for Blood and Marrow Transplantation.
The CED asks for a prospective clinical trial that mandates the presence of a control arm of comparable patients who do not receive allogeneic transplantation. I completely support provision of transplantation on a clinical trial for CED purposes; however, I believe it would have been better to allow hematology and transplant experts to determine the appropriate study design in consultation with CMS to fulfill the CED requirements. For example, on the basis of available evidence, it will be challenging to enroll patients with high-risk myelofibrosis to a nontransplant arm. Irrespective, this is a big win for patients with these life-threatening diseases and for physicians who treat them.
Dr. Navneet Majhail is the director of the Cleveland Clinic’s Blood & Marrow Transplant Program. He serves as a staff physician at the Taussig Cancer Institute and is a professor of medicine with the Cleveland Clinic Lerner College of Medicine.
Medicare will cover allogeneic hematopoietic stem cell transplantation (HSCT) for beneficiaries with multiple myeloma, myelofibrosis, or sickle cell disease in the context of approved, prospective clinical trials, the Centers for Medicare & Medicaid Services announced in a final decision memo Jan. 27.
Approvable studies must examine whether Medicare beneficiaries who receive allogeneic HSCT have improved outcomes, compared with patients who do not receive allogeneic HSCT as measured by graft vs. host disease, other transplant-related adverse events, overall survival, and, optionally, quality of life measures.
In multiple myeloma, allogeneic HSCT will be covered only for Medicare beneficiaries who have Durie-Salmon Stage II or III multiple myeloma, or International Staging System (ISS) Stage II or Stage III multiple myeloma, and are participating in an approved prospective clinical study. Such studies must control for selection bias and potential confounding by age, duration of diagnosis, disease classification, International Myeloma Working Group (IMWG) classification, ISS staging, Durie-Salmon staging, comorbid conditions, type of preparative/conditioning regimen, graft vs. host disease (GVHD) prophylaxis, donor type, and cell source, the CMS said in its memo.
In myelofibrosis, allogeneic HSCT will be covered by Medicare in an approved prospective study only for beneficiaries with Dynamic International Prognostic Scoring System (DIPSS plus) intermediate-2 or high primary or secondary myelofibrosis. Studies must be controlled for selection bias and potential confounding by age, duration of diagnosis, disease classification, DIPSS plus score, comorbid conditions, type of preparative/conditioning regimen, GVHD prophylaxis, donor type, and cell source.
In sickle cell disease, allogeneic HSCT will be covered by Medicare only for beneficiaries who have severe, symptomatic disease. Approvable studies must control for selection bias and potential confounding by age, duration of diagnosis, comorbid conditions, type of preparative/conditioning regimen, GVHD prophylaxis, donor type, and cell source.
On Twitter @maryjodales
Medicare will cover allogeneic hematopoietic stem cell transplantation (HSCT) for beneficiaries with multiple myeloma, myelofibrosis, or sickle cell disease in the context of approved, prospective clinical trials, the Centers for Medicare & Medicaid Services announced in a final decision memo Jan. 27.
Approvable studies must examine whether Medicare beneficiaries who receive allogeneic HSCT have improved outcomes, compared with patients who do not receive allogeneic HSCT as measured by graft vs. host disease, other transplant-related adverse events, overall survival, and, optionally, quality of life measures.
In multiple myeloma, allogeneic HSCT will be covered only for Medicare beneficiaries who have Durie-Salmon Stage II or III multiple myeloma, or International Staging System (ISS) Stage II or Stage III multiple myeloma, and are participating in an approved prospective clinical study. Such studies must control for selection bias and potential confounding by age, duration of diagnosis, disease classification, International Myeloma Working Group (IMWG) classification, ISS staging, Durie-Salmon staging, comorbid conditions, type of preparative/conditioning regimen, graft vs. host disease (GVHD) prophylaxis, donor type, and cell source, the CMS said in its memo.
In myelofibrosis, allogeneic HSCT will be covered by Medicare in an approved prospective study only for beneficiaries with Dynamic International Prognostic Scoring System (DIPSS plus) intermediate-2 or high primary or secondary myelofibrosis. Studies must be controlled for selection bias and potential confounding by age, duration of diagnosis, disease classification, DIPSS plus score, comorbid conditions, type of preparative/conditioning regimen, GVHD prophylaxis, donor type, and cell source.
In sickle cell disease, allogeneic HSCT will be covered by Medicare only for beneficiaries who have severe, symptomatic disease. Approvable studies must control for selection bias and potential confounding by age, duration of diagnosis, comorbid conditions, type of preparative/conditioning regimen, GVHD prophylaxis, donor type, and cell source.
On Twitter @maryjodales
Predicting transformation from MDS to AML

Photo courtesy of
McMaster University
Research published in Cancer Cell suggests a molecular signature can be used to predict which patients with myelodysplastic syndromes (MDS) will develop acute myeloid leukemia (AML).
Investigators found that progressive removal of glycogen synthase kinase-3 (GSK-3) signaling via GSK-3β deletion in hematopoietic stem cells (HSCs) results in an MDS-like state.
And when both GSK-3β and GSK-3α are deleted, AML develops.
“We’ve found that the transition from healthy to cancerous blood stem cells happens in clear, compartmentalized steps,” said study author Mick Bhatia, PhD, of McMaster University in Hamilton, Ontario, Canada. “We’ve identified 2 steps in that staircase.”
Specifically, the investigators found that deleting GSK-3β in HSCs led to the generation of self-renewing cells dubbed MDS-initiating cells. These cells proved capable of sustaining MDS in vivo.
Next, the team found that GSK-3β deletion drives Wnt/Akt/mTOR signaling and can induce AML in the absence of GSK-3α.
They noted that GSK-3α has no biological impact on hematopoiesis, but GSK-3α deletion is necessary for the evolution of MDS to AML that occurs in the absence of GSK-3β.
The investigators then defined a molecular signature of GSK-3β-deficient HSCs that could predict transformation to AML in patients with MDS.
The team tested the utility of this 63-gene signature using blood samples that were previously collected from patients with MDS, some of whom ultimately developed AML. The results showed the signature could accurately predict which patients would develop AML and which would not.
“[O]ur next step is to go beyond better predictive measures for the development of a blood cancer and use this predictive gene expression as a target for drugs to prevent AML from developing altogether,” Dr Bhatia said. “This will be part of a new era of genetic-based drug discovery.” ![]()

Photo courtesy of
McMaster University
Research published in Cancer Cell suggests a molecular signature can be used to predict which patients with myelodysplastic syndromes (MDS) will develop acute myeloid leukemia (AML).
Investigators found that progressive removal of glycogen synthase kinase-3 (GSK-3) signaling via GSK-3β deletion in hematopoietic stem cells (HSCs) results in an MDS-like state.
And when both GSK-3β and GSK-3α are deleted, AML develops.
“We’ve found that the transition from healthy to cancerous blood stem cells happens in clear, compartmentalized steps,” said study author Mick Bhatia, PhD, of McMaster University in Hamilton, Ontario, Canada. “We’ve identified 2 steps in that staircase.”
Specifically, the investigators found that deleting GSK-3β in HSCs led to the generation of self-renewing cells dubbed MDS-initiating cells. These cells proved capable of sustaining MDS in vivo.
Next, the team found that GSK-3β deletion drives Wnt/Akt/mTOR signaling and can induce AML in the absence of GSK-3α.
They noted that GSK-3α has no biological impact on hematopoiesis, but GSK-3α deletion is necessary for the evolution of MDS to AML that occurs in the absence of GSK-3β.
The investigators then defined a molecular signature of GSK-3β-deficient HSCs that could predict transformation to AML in patients with MDS.
The team tested the utility of this 63-gene signature using blood samples that were previously collected from patients with MDS, some of whom ultimately developed AML. The results showed the signature could accurately predict which patients would develop AML and which would not.
“[O]ur next step is to go beyond better predictive measures for the development of a blood cancer and use this predictive gene expression as a target for drugs to prevent AML from developing altogether,” Dr Bhatia said. “This will be part of a new era of genetic-based drug discovery.” ![]()

Photo courtesy of
McMaster University
Research published in Cancer Cell suggests a molecular signature can be used to predict which patients with myelodysplastic syndromes (MDS) will develop acute myeloid leukemia (AML).
Investigators found that progressive removal of glycogen synthase kinase-3 (GSK-3) signaling via GSK-3β deletion in hematopoietic stem cells (HSCs) results in an MDS-like state.
And when both GSK-3β and GSK-3α are deleted, AML develops.
“We’ve found that the transition from healthy to cancerous blood stem cells happens in clear, compartmentalized steps,” said study author Mick Bhatia, PhD, of McMaster University in Hamilton, Ontario, Canada. “We’ve identified 2 steps in that staircase.”
Specifically, the investigators found that deleting GSK-3β in HSCs led to the generation of self-renewing cells dubbed MDS-initiating cells. These cells proved capable of sustaining MDS in vivo.
Next, the team found that GSK-3β deletion drives Wnt/Akt/mTOR signaling and can induce AML in the absence of GSK-3α.
They noted that GSK-3α has no biological impact on hematopoiesis, but GSK-3α deletion is necessary for the evolution of MDS to AML that occurs in the absence of GSK-3β.
The investigators then defined a molecular signature of GSK-3β-deficient HSCs that could predict transformation to AML in patients with MDS.
The team tested the utility of this 63-gene signature using blood samples that were previously collected from patients with MDS, some of whom ultimately developed AML. The results showed the signature could accurately predict which patients would develop AML and which would not.
“[O]ur next step is to go beyond better predictive measures for the development of a blood cancer and use this predictive gene expression as a target for drugs to prevent AML from developing altogether,” Dr Bhatia said. “This will be part of a new era of genetic-based drug discovery.” ![]()