User login
Small study advances noninvasive ICP monitoring
A device that noninvasively measures intracranial pressure (ICP) had a sensitivity of 75% and a specificity of 89%, compared with standard invasive monitoring, based on the results of an industry-sponsored study of 14 patients with traumatic brain injury or subarachnoid hemorrhage.
“This study provides the first clinical data on the accuracy of the HS-1000 noninvasive ICP monitor, which uses advanced signal analysis algorithms to evaluate properties of acoustic signals traveling through the brain,” wrote Oliver Ganslandt, MD, of Klinikum Stuttgart (Germany) and his associates. The findings were published online Aug. 8 in the Journal of Neurosurgery.
The noninvasive and invasive measurements produced more than 2,500 parallel ICP data points. Notably, each of the two methods produced the same number of data points. Readings averaged 10 (standard deviation, 6.1) mm Hg with invasive monitoring and 9.5 (SD, 4.7) mm Hg for noninvasive monitoring with the HS-1000. Compared with invasive ICP monitoring, the HS-1000 had a sensitivity of 75% and a specificity of 89% at an arbitrary cutoff of at least 17 mm Hg. Linear regression showed a “strong positive relationship between the [noninvasive and invasive] measurements,” the investigators said. In all, 63% of paired data points fell within 3 mm Hg of each other, and 85% fell within 5 mm Hg of each other. A receiver operating characteristic area under the curve analysis of the two methods generated an area under the curve of almost 90%.
The study did not include children or patients who were pregnant or had ear disease or ear injuries, rhinorrhea or otorrhea, or skull defects, the researchers said. If the HS-1000 holds up in other ongoing studies (NCT02284217, NCT02773901), physicians might be able to use it to decide if patients needs invasive ICP monitoring, they added. Use of the noninvasive method could also help prevent infections and other morbidity associated with invasive ICP monitoring in both neurocritical intensive care units and low-resource settings, they said.
HeadSense Medical sponsored the study. The researchers had no relevant disclosures.
A device that noninvasively measures intracranial pressure (ICP) had a sensitivity of 75% and a specificity of 89%, compared with standard invasive monitoring, based on the results of an industry-sponsored study of 14 patients with traumatic brain injury or subarachnoid hemorrhage.
“This study provides the first clinical data on the accuracy of the HS-1000 noninvasive ICP monitor, which uses advanced signal analysis algorithms to evaluate properties of acoustic signals traveling through the brain,” wrote Oliver Ganslandt, MD, of Klinikum Stuttgart (Germany) and his associates. The findings were published online Aug. 8 in the Journal of Neurosurgery.
The noninvasive and invasive measurements produced more than 2,500 parallel ICP data points. Notably, each of the two methods produced the same number of data points. Readings averaged 10 (standard deviation, 6.1) mm Hg with invasive monitoring and 9.5 (SD, 4.7) mm Hg for noninvasive monitoring with the HS-1000. Compared with invasive ICP monitoring, the HS-1000 had a sensitivity of 75% and a specificity of 89% at an arbitrary cutoff of at least 17 mm Hg. Linear regression showed a “strong positive relationship between the [noninvasive and invasive] measurements,” the investigators said. In all, 63% of paired data points fell within 3 mm Hg of each other, and 85% fell within 5 mm Hg of each other. A receiver operating characteristic area under the curve analysis of the two methods generated an area under the curve of almost 90%.
The study did not include children or patients who were pregnant or had ear disease or ear injuries, rhinorrhea or otorrhea, or skull defects, the researchers said. If the HS-1000 holds up in other ongoing studies (NCT02284217, NCT02773901), physicians might be able to use it to decide if patients needs invasive ICP monitoring, they added. Use of the noninvasive method could also help prevent infections and other morbidity associated with invasive ICP monitoring in both neurocritical intensive care units and low-resource settings, they said.
HeadSense Medical sponsored the study. The researchers had no relevant disclosures.
A device that noninvasively measures intracranial pressure (ICP) had a sensitivity of 75% and a specificity of 89%, compared with standard invasive monitoring, based on the results of an industry-sponsored study of 14 patients with traumatic brain injury or subarachnoid hemorrhage.
“This study provides the first clinical data on the accuracy of the HS-1000 noninvasive ICP monitor, which uses advanced signal analysis algorithms to evaluate properties of acoustic signals traveling through the brain,” wrote Oliver Ganslandt, MD, of Klinikum Stuttgart (Germany) and his associates. The findings were published online Aug. 8 in the Journal of Neurosurgery.
The noninvasive and invasive measurements produced more than 2,500 parallel ICP data points. Notably, each of the two methods produced the same number of data points. Readings averaged 10 (standard deviation, 6.1) mm Hg with invasive monitoring and 9.5 (SD, 4.7) mm Hg for noninvasive monitoring with the HS-1000. Compared with invasive ICP monitoring, the HS-1000 had a sensitivity of 75% and a specificity of 89% at an arbitrary cutoff of at least 17 mm Hg. Linear regression showed a “strong positive relationship between the [noninvasive and invasive] measurements,” the investigators said. In all, 63% of paired data points fell within 3 mm Hg of each other, and 85% fell within 5 mm Hg of each other. A receiver operating characteristic area under the curve analysis of the two methods generated an area under the curve of almost 90%.
The study did not include children or patients who were pregnant or had ear disease or ear injuries, rhinorrhea or otorrhea, or skull defects, the researchers said. If the HS-1000 holds up in other ongoing studies (NCT02284217, NCT02773901), physicians might be able to use it to decide if patients needs invasive ICP monitoring, they added. Use of the noninvasive method could also help prevent infections and other morbidity associated with invasive ICP monitoring in both neurocritical intensive care units and low-resource settings, they said.
HeadSense Medical sponsored the study. The researchers had no relevant disclosures.
FROM THE JOURNAL OF NEUROSURGERY
Key clinical point: A noninvasive device that measures intracranial pressure generated data that was comparable with standard invasive methods.
Major finding: Sensitivity was 75%, and specificity was 89%, compared with standard invasive monitoring at an arbitrary cutoff of at least 17 mm Hg.
Data source: Noninvasive and invasive intracranial pressure monitoring of 14 patients with traumatic brain injury or subarachnoid hemorrhage.
Disclosures: HeadSense Medical sponsored the study. The researchers had no relevant disclosures.
New and Noteworthy Information—August 2017
Brain Training Shows Little Benefit
Commercial brain training with Lumosity has no effect on decision making or cognitive function beyond practice effects on training tasks, according to a study published online ahead of print July 10 in the Journal of Neuroscience. Researchers tested whether training executive cognitive function could influence choice behavior and brain responses. In a randomized controlled trial, 128 young adults (71 male) participated in 10 weeks of training with either a commercial web-based cognitive training program or web-based video games that do not specifically target executive function or adapt the level of difficulty throughout training. The participants also completed a series of cognitive tests that were not part of the training. Although both groups showed improvement, commercial brain training did not lead to more improvement than online video games did.
Kable JW, Caulfield MK, Falcone M, et al. No effect of commercial cognitive training on neural activity during decision-making. J Neurosci. 2017 Jul 10 [Epub ahead of print].
Sense of Purpose Linked to Better Sleep
A higher level of meaning and purpose in life among older adults is associated with better sleep quality and appears to protect against symptoms of sleep apnea and restless legs syndrome (RLS), according to a study published online ahead of print July 10 in Sleep Science and Practice. Included in this study were 825 nondemented older African Americans (n = 428) and whites (n = 397), from the Minority Aging Research Study and the Rush Memory and Aging Project. Participants completed a 32-item questionnaire assessing sleep quality and symptoms of sleep apnea, RLS, and REM sleep behavior disorder. Longitudinal follow-up data indicated that higher levels of purpose in life were associated with lower risk of sleep apnea at baseline, one-year follow-up, and two-year follow-up, and with reduced RLS symptoms at one-year and two-year follow-up.
Turner AD, Smith CE, Ong JC. Is purpose in life associated with less sleep disturbance in older adults? Sleep Sci Pract. 2017 July 10 [Epub ahead of print].
Can Breastfeeding Reduce MS Risk in Mothers?
Mothers who breastfeed longer may be at lower subsequent risk of developing multiple sclerosis (MS), according to a study published online ahead of print July 12 in Neurology. Researchers recruited women with newly diagnosed MS or clinically isolated syndrome (CIS) and matched controls into the MS Sunshine Study from the membership of Kaiser Permanente Southern California. An in-person questionnaire was administered to collect behavioral and biologic factors to calculate ovulatory years. Among women who had live births, a cumulative duration of breastfeeding for 15 months or more was associated with a reduced risk of MS and CIS (adjusted odds ratio, 0.47). Being age 15 or older at menarche also was associated with a lower risk of MS and CIS (adjusted odds ratio, 0.56).
Langer-Gould A, Smith JB, Hellwig K, et al. Breastfeeding, ovulatory years, and risk of multiple sclerosis. Neurology. 2017 July 12 [Epub ahead of print].
Does Added Weight Increase Survival After Stroke?
People who are overweight or mildly obese survive strokes at a higher rate, compared with people of normal body weight, according to a study published June 24 in the Journal of the American Heart Association. Participants from the Framingham Heart Study were followed for as long as 10 years, with BMI measured prior to their strokes. Researchers compared all-cause mortality in participants stratified by prestroke weight. Separate analyses were performed for ischemic stroke and all stroke and for age-, sex-, and BMI category-matched stroke-free controls. There were 782 stroke cases and 2,346 controls. The association of reduced mortality with BMI of 25 or higher, compared with BMI of 18.5 to less than 25, was pronounced among ischemic stroke cases, but diminished with inclusion of hemorrhagic strokes.
Aparicio HJ, Himali JJ, Beiser AS, et al. Overweight, obesity, and survival after stroke in the Framingham Heart Study. J Am Heart Assoc. 2017;6(6).
Poor Sleep Linked to CSF Biomarkers
Self-reported poor sleep is associated with greater Alzheimer’s disease-related pathology in cognitively healthy adults at risk for Alzheimer’s disease, according to a study published online ahead of print July 5 in Neurology. Researchers investigated the relationship between sleep quality and CSF Alzheimer’s disease biomarkers in a cohort enriched for parental history of sporadic Alzheimer’s disease. In all, 101 participants completed sleep assessments and CSF collection and were cognitively normal. CSF was assayed for biomarkers of amyloid metabolism and plaques, tau pathology, neuronal and axonal degeneration, neuroinflammation and astroglial activation, and synaptic dysfunction and degeneration. Worse subjective sleep quality, more sleep problems, and daytime somnolence were associated with greater Alzheimer’s disease pathology, indicated by lower CSF Aβ42/Aβ40 and higher t-tau/Aβ42, p-tau/Aβ42, MCP-1/Aβ42, and YKL-40/Aβ42.
Sprecher KE, Koscik RL, Carlsson CM, et al. Poor sleep is associated with CSF biomarkers of amyloid pathology in cognitively normal adults. Neurology. 2017 Jul 5 [Epub ahead of print].
Is There a Link Between Parkinson’s Disease and Melanoma?
Melanoma and Parkinson’s disease may be associated, according to a study published in the July issue of Mayo Clinic Proceedings. For phase I of the Rochester Epidemiology Project, investigators used records to identify patients with Parkinson’s disease and match three controls per case. During phase II of this study, all Rochester Epidemiology Project cases of melanoma were identified, with one control per case. Investigators used a Cox proportional hazards model to assess the risk of developing Parkinson’s disease after the index date in cases versus controls, and performed Kaplan-Meier analysis to determine the 35-year cumulative risk of Parkinson’s disease. Patients with Parkinson’s disease had a 3.8-fold increased likelihood of having preexisting melanoma, compared with controls. Patients with melanoma had a 4.2-fold increased risk of developing Parkinson’s disease.
Dalvin LA, Damento GM, Yawn BP, et al. Parkinson disease and melanoma: confirming and reexamining an association. Mayo Clin Proc. 2017;92(7):1070-1079.
Zolpidem Treats Various Neurologic Disorders
A systematic review shows that zolpidem can treat various neurologic disorders, most often related to movement disorders and disorders of consciousness, according to a literature review published online ahead of print June 26 in JAMA Neurology. The investigators searched for English-language articles, published by March 20, 2015, that examined the use of zolpidem for noninsomnia neurologic disorders. Searched databases included PubMed, Scopus, Web of Science Core Collection, the Cochrane Library, EMBASE, CENTRAL, and clinicaltrials.gov. In all, 67 articles were eligible for full manuscript review. Thirty-one studies treated movement disorders, 22 treated disorders of consciousness, and 14 treated other neurologic conditions. The effects of zolpidem were wide ranging and generally lasted for one to four hours before the participant returned to baseline. Sedation was the most common adverse effect.
Bomalaski MN, Claflin ES, Townsend W, Peterson MD. Zolpidem for the treatment of neurologic disorders: a systematic review. JAMA Neurol. 2017 Jun 26 [Epub ahead of print].
Colored Light Triggers Responses in Migraineurs
Lights trigger more changes in autonomic functions and negative emotions during migraine than in control subjects, and the association between light and positive emotions is stronger in control subjects than in migraineurs, according to a study published online ahead of print June 26 in the Proceedings of the National Academy of Sciences. Researchers showed different colored lights to 81 migraineurs and 17 people who had never had a migraine. The effects of light and color were tested three times. Investigators found that all colors of light triggered unpleasant physiologic sensations in patients with migraines, during and between attacks. Additionally, migraineurs reported intense emotional responses such as anger, nervousness, hopelessness, sadness, depression, anxiety, and fear when exposed to all light colors except green.
Noseda R, Lee AJ, Nir RR, et al. Neural mechanism for hypothalamic-mediated autonomic responses to light during migraine. Proc Natl Acad Sci. 2017 Jun 26 [Epub ahead of print].
TBI May Not Hasten Cognitive Decline
Having a history of traumatic brain injury (TBI) with loss of consciousness does not affect the rate of cognitive change over time for people with normal cognition or people with Alzheimer’s disease, according to a study published online ahead of print June 22 in the Journal of Alzheimer’s Disease. Researchers compared performance on cognitive tests over time for 432 participants with normal cognition and 274 participants with probable Alzheimer’s disease. They matched participants with a history of TBI with loss of consciousness to an equal number of demographically and clinically similar participants without a history of TBI. Mixed-effects regressions showed that a history of TBI with loss of consciousness did not affect rates of cognitive change in APOE ε4 carriers and noncarriers.
Tripodis Y, Alosco ML, Zirogiannis N, et al. The effect of traumatic brain injury history with loss of consciousness on rate of cognitive decline among older adults with normal cognition and Alzheimer’s disease dementia. J Alzheimers Dis. 2017 Jun 22 [Epub ahead of print].
Visual Changes in Parkinson’s Disease
Visual system alterations can be detected in early stages of Parkinson’s disease, and the entire intracranial visual system can be involved, according to a study published online ahead of print July 11 in Radiology. Twenty patients with newly diagnosed Parkinson’s disease and 20 age-matched control subjects were studied. Researchers used diffusion-weighted imaging to assess white matter changes and voxel-based morphometry (VBM) to investigate concentration changes of gray and white matter. In patients with Parkinson’s disease, significant alterations were found in optic radiation connectivity distribution, with decreased lateral geniculate nucleus V2 density, a significant increase in optic radiation mean diffusivity, and a significant reduction in white matter concentration. VBM analysis also showed a significant reduction in visual cortical volumes.
Arrigo A, Calamuneri A, Milardi D, et al. Visual system involvement in patients with newly diagnosed Parkinson disease. Radiology. 2017 Jul 11 [Epub ahead of print].
—Kimberly Williams
Brain Training Shows Little Benefit
Commercial brain training with Lumosity has no effect on decision making or cognitive function beyond practice effects on training tasks, according to a study published online ahead of print July 10 in the Journal of Neuroscience. Researchers tested whether training executive cognitive function could influence choice behavior and brain responses. In a randomized controlled trial, 128 young adults (71 male) participated in 10 weeks of training with either a commercial web-based cognitive training program or web-based video games that do not specifically target executive function or adapt the level of difficulty throughout training. The participants also completed a series of cognitive tests that were not part of the training. Although both groups showed improvement, commercial brain training did not lead to more improvement than online video games did.
Kable JW, Caulfield MK, Falcone M, et al. No effect of commercial cognitive training on neural activity during decision-making. J Neurosci. 2017 Jul 10 [Epub ahead of print].
Sense of Purpose Linked to Better Sleep
A higher level of meaning and purpose in life among older adults is associated with better sleep quality and appears to protect against symptoms of sleep apnea and restless legs syndrome (RLS), according to a study published online ahead of print July 10 in Sleep Science and Practice. Included in this study were 825 nondemented older African Americans (n = 428) and whites (n = 397), from the Minority Aging Research Study and the Rush Memory and Aging Project. Participants completed a 32-item questionnaire assessing sleep quality and symptoms of sleep apnea, RLS, and REM sleep behavior disorder. Longitudinal follow-up data indicated that higher levels of purpose in life were associated with lower risk of sleep apnea at baseline, one-year follow-up, and two-year follow-up, and with reduced RLS symptoms at one-year and two-year follow-up.
Turner AD, Smith CE, Ong JC. Is purpose in life associated with less sleep disturbance in older adults? Sleep Sci Pract. 2017 July 10 [Epub ahead of print].
Can Breastfeeding Reduce MS Risk in Mothers?
Mothers who breastfeed longer may be at lower subsequent risk of developing multiple sclerosis (MS), according to a study published online ahead of print July 12 in Neurology. Researchers recruited women with newly diagnosed MS or clinically isolated syndrome (CIS) and matched controls into the MS Sunshine Study from the membership of Kaiser Permanente Southern California. An in-person questionnaire was administered to collect behavioral and biologic factors to calculate ovulatory years. Among women who had live births, a cumulative duration of breastfeeding for 15 months or more was associated with a reduced risk of MS and CIS (adjusted odds ratio, 0.47). Being age 15 or older at menarche also was associated with a lower risk of MS and CIS (adjusted odds ratio, 0.56).
Langer-Gould A, Smith JB, Hellwig K, et al. Breastfeeding, ovulatory years, and risk of multiple sclerosis. Neurology. 2017 July 12 [Epub ahead of print].
Does Added Weight Increase Survival After Stroke?
People who are overweight or mildly obese survive strokes at a higher rate, compared with people of normal body weight, according to a study published June 24 in the Journal of the American Heart Association. Participants from the Framingham Heart Study were followed for as long as 10 years, with BMI measured prior to their strokes. Researchers compared all-cause mortality in participants stratified by prestroke weight. Separate analyses were performed for ischemic stroke and all stroke and for age-, sex-, and BMI category-matched stroke-free controls. There were 782 stroke cases and 2,346 controls. The association of reduced mortality with BMI of 25 or higher, compared with BMI of 18.5 to less than 25, was pronounced among ischemic stroke cases, but diminished with inclusion of hemorrhagic strokes.
Aparicio HJ, Himali JJ, Beiser AS, et al. Overweight, obesity, and survival after stroke in the Framingham Heart Study. J Am Heart Assoc. 2017;6(6).
Poor Sleep Linked to CSF Biomarkers
Self-reported poor sleep is associated with greater Alzheimer’s disease-related pathology in cognitively healthy adults at risk for Alzheimer’s disease, according to a study published online ahead of print July 5 in Neurology. Researchers investigated the relationship between sleep quality and CSF Alzheimer’s disease biomarkers in a cohort enriched for parental history of sporadic Alzheimer’s disease. In all, 101 participants completed sleep assessments and CSF collection and were cognitively normal. CSF was assayed for biomarkers of amyloid metabolism and plaques, tau pathology, neuronal and axonal degeneration, neuroinflammation and astroglial activation, and synaptic dysfunction and degeneration. Worse subjective sleep quality, more sleep problems, and daytime somnolence were associated with greater Alzheimer’s disease pathology, indicated by lower CSF Aβ42/Aβ40 and higher t-tau/Aβ42, p-tau/Aβ42, MCP-1/Aβ42, and YKL-40/Aβ42.
Sprecher KE, Koscik RL, Carlsson CM, et al. Poor sleep is associated with CSF biomarkers of amyloid pathology in cognitively normal adults. Neurology. 2017 Jul 5 [Epub ahead of print].
Is There a Link Between Parkinson’s Disease and Melanoma?
Melanoma and Parkinson’s disease may be associated, according to a study published in the July issue of Mayo Clinic Proceedings. For phase I of the Rochester Epidemiology Project, investigators used records to identify patients with Parkinson’s disease and match three controls per case. During phase II of this study, all Rochester Epidemiology Project cases of melanoma were identified, with one control per case. Investigators used a Cox proportional hazards model to assess the risk of developing Parkinson’s disease after the index date in cases versus controls, and performed Kaplan-Meier analysis to determine the 35-year cumulative risk of Parkinson’s disease. Patients with Parkinson’s disease had a 3.8-fold increased likelihood of having preexisting melanoma, compared with controls. Patients with melanoma had a 4.2-fold increased risk of developing Parkinson’s disease.
Dalvin LA, Damento GM, Yawn BP, et al. Parkinson disease and melanoma: confirming and reexamining an association. Mayo Clin Proc. 2017;92(7):1070-1079.
Zolpidem Treats Various Neurologic Disorders
A systematic review shows that zolpidem can treat various neurologic disorders, most often related to movement disorders and disorders of consciousness, according to a literature review published online ahead of print June 26 in JAMA Neurology. The investigators searched for English-language articles, published by March 20, 2015, that examined the use of zolpidem for noninsomnia neurologic disorders. Searched databases included PubMed, Scopus, Web of Science Core Collection, the Cochrane Library, EMBASE, CENTRAL, and clinicaltrials.gov. In all, 67 articles were eligible for full manuscript review. Thirty-one studies treated movement disorders, 22 treated disorders of consciousness, and 14 treated other neurologic conditions. The effects of zolpidem were wide ranging and generally lasted for one to four hours before the participant returned to baseline. Sedation was the most common adverse effect.
Bomalaski MN, Claflin ES, Townsend W, Peterson MD. Zolpidem for the treatment of neurologic disorders: a systematic review. JAMA Neurol. 2017 Jun 26 [Epub ahead of print].
Colored Light Triggers Responses in Migraineurs
Lights trigger more changes in autonomic functions and negative emotions during migraine than in control subjects, and the association between light and positive emotions is stronger in control subjects than in migraineurs, according to a study published online ahead of print June 26 in the Proceedings of the National Academy of Sciences. Researchers showed different colored lights to 81 migraineurs and 17 people who had never had a migraine. The effects of light and color were tested three times. Investigators found that all colors of light triggered unpleasant physiologic sensations in patients with migraines, during and between attacks. Additionally, migraineurs reported intense emotional responses such as anger, nervousness, hopelessness, sadness, depression, anxiety, and fear when exposed to all light colors except green.
Noseda R, Lee AJ, Nir RR, et al. Neural mechanism for hypothalamic-mediated autonomic responses to light during migraine. Proc Natl Acad Sci. 2017 Jun 26 [Epub ahead of print].
TBI May Not Hasten Cognitive Decline
Having a history of traumatic brain injury (TBI) with loss of consciousness does not affect the rate of cognitive change over time for people with normal cognition or people with Alzheimer’s disease, according to a study published online ahead of print June 22 in the Journal of Alzheimer’s Disease. Researchers compared performance on cognitive tests over time for 432 participants with normal cognition and 274 participants with probable Alzheimer’s disease. They matched participants with a history of TBI with loss of consciousness to an equal number of demographically and clinically similar participants without a history of TBI. Mixed-effects regressions showed that a history of TBI with loss of consciousness did not affect rates of cognitive change in APOE ε4 carriers and noncarriers.
Tripodis Y, Alosco ML, Zirogiannis N, et al. The effect of traumatic brain injury history with loss of consciousness on rate of cognitive decline among older adults with normal cognition and Alzheimer’s disease dementia. J Alzheimers Dis. 2017 Jun 22 [Epub ahead of print].
Visual Changes in Parkinson’s Disease
Visual system alterations can be detected in early stages of Parkinson’s disease, and the entire intracranial visual system can be involved, according to a study published online ahead of print July 11 in Radiology. Twenty patients with newly diagnosed Parkinson’s disease and 20 age-matched control subjects were studied. Researchers used diffusion-weighted imaging to assess white matter changes and voxel-based morphometry (VBM) to investigate concentration changes of gray and white matter. In patients with Parkinson’s disease, significant alterations were found in optic radiation connectivity distribution, with decreased lateral geniculate nucleus V2 density, a significant increase in optic radiation mean diffusivity, and a significant reduction in white matter concentration. VBM analysis also showed a significant reduction in visual cortical volumes.
Arrigo A, Calamuneri A, Milardi D, et al. Visual system involvement in patients with newly diagnosed Parkinson disease. Radiology. 2017 Jul 11 [Epub ahead of print].
—Kimberly Williams
Brain Training Shows Little Benefit
Commercial brain training with Lumosity has no effect on decision making or cognitive function beyond practice effects on training tasks, according to a study published online ahead of print July 10 in the Journal of Neuroscience. Researchers tested whether training executive cognitive function could influence choice behavior and brain responses. In a randomized controlled trial, 128 young adults (71 male) participated in 10 weeks of training with either a commercial web-based cognitive training program or web-based video games that do not specifically target executive function or adapt the level of difficulty throughout training. The participants also completed a series of cognitive tests that were not part of the training. Although both groups showed improvement, commercial brain training did not lead to more improvement than online video games did.
Kable JW, Caulfield MK, Falcone M, et al. No effect of commercial cognitive training on neural activity during decision-making. J Neurosci. 2017 Jul 10 [Epub ahead of print].
Sense of Purpose Linked to Better Sleep
A higher level of meaning and purpose in life among older adults is associated with better sleep quality and appears to protect against symptoms of sleep apnea and restless legs syndrome (RLS), according to a study published online ahead of print July 10 in Sleep Science and Practice. Included in this study were 825 nondemented older African Americans (n = 428) and whites (n = 397), from the Minority Aging Research Study and the Rush Memory and Aging Project. Participants completed a 32-item questionnaire assessing sleep quality and symptoms of sleep apnea, RLS, and REM sleep behavior disorder. Longitudinal follow-up data indicated that higher levels of purpose in life were associated with lower risk of sleep apnea at baseline, one-year follow-up, and two-year follow-up, and with reduced RLS symptoms at one-year and two-year follow-up.
Turner AD, Smith CE, Ong JC. Is purpose in life associated with less sleep disturbance in older adults? Sleep Sci Pract. 2017 July 10 [Epub ahead of print].
Can Breastfeeding Reduce MS Risk in Mothers?
Mothers who breastfeed longer may be at lower subsequent risk of developing multiple sclerosis (MS), according to a study published online ahead of print July 12 in Neurology. Researchers recruited women with newly diagnosed MS or clinically isolated syndrome (CIS) and matched controls into the MS Sunshine Study from the membership of Kaiser Permanente Southern California. An in-person questionnaire was administered to collect behavioral and biologic factors to calculate ovulatory years. Among women who had live births, a cumulative duration of breastfeeding for 15 months or more was associated with a reduced risk of MS and CIS (adjusted odds ratio, 0.47). Being age 15 or older at menarche also was associated with a lower risk of MS and CIS (adjusted odds ratio, 0.56).
Langer-Gould A, Smith JB, Hellwig K, et al. Breastfeeding, ovulatory years, and risk of multiple sclerosis. Neurology. 2017 July 12 [Epub ahead of print].
Does Added Weight Increase Survival After Stroke?
People who are overweight or mildly obese survive strokes at a higher rate, compared with people of normal body weight, according to a study published June 24 in the Journal of the American Heart Association. Participants from the Framingham Heart Study were followed for as long as 10 years, with BMI measured prior to their strokes. Researchers compared all-cause mortality in participants stratified by prestroke weight. Separate analyses were performed for ischemic stroke and all stroke and for age-, sex-, and BMI category-matched stroke-free controls. There were 782 stroke cases and 2,346 controls. The association of reduced mortality with BMI of 25 or higher, compared with BMI of 18.5 to less than 25, was pronounced among ischemic stroke cases, but diminished with inclusion of hemorrhagic strokes.
Aparicio HJ, Himali JJ, Beiser AS, et al. Overweight, obesity, and survival after stroke in the Framingham Heart Study. J Am Heart Assoc. 2017;6(6).
Poor Sleep Linked to CSF Biomarkers
Self-reported poor sleep is associated with greater Alzheimer’s disease-related pathology in cognitively healthy adults at risk for Alzheimer’s disease, according to a study published online ahead of print July 5 in Neurology. Researchers investigated the relationship between sleep quality and CSF Alzheimer’s disease biomarkers in a cohort enriched for parental history of sporadic Alzheimer’s disease. In all, 101 participants completed sleep assessments and CSF collection and were cognitively normal. CSF was assayed for biomarkers of amyloid metabolism and plaques, tau pathology, neuronal and axonal degeneration, neuroinflammation and astroglial activation, and synaptic dysfunction and degeneration. Worse subjective sleep quality, more sleep problems, and daytime somnolence were associated with greater Alzheimer’s disease pathology, indicated by lower CSF Aβ42/Aβ40 and higher t-tau/Aβ42, p-tau/Aβ42, MCP-1/Aβ42, and YKL-40/Aβ42.
Sprecher KE, Koscik RL, Carlsson CM, et al. Poor sleep is associated with CSF biomarkers of amyloid pathology in cognitively normal adults. Neurology. 2017 Jul 5 [Epub ahead of print].
Is There a Link Between Parkinson’s Disease and Melanoma?
Melanoma and Parkinson’s disease may be associated, according to a study published in the July issue of Mayo Clinic Proceedings. For phase I of the Rochester Epidemiology Project, investigators used records to identify patients with Parkinson’s disease and match three controls per case. During phase II of this study, all Rochester Epidemiology Project cases of melanoma were identified, with one control per case. Investigators used a Cox proportional hazards model to assess the risk of developing Parkinson’s disease after the index date in cases versus controls, and performed Kaplan-Meier analysis to determine the 35-year cumulative risk of Parkinson’s disease. Patients with Parkinson’s disease had a 3.8-fold increased likelihood of having preexisting melanoma, compared with controls. Patients with melanoma had a 4.2-fold increased risk of developing Parkinson’s disease.
Dalvin LA, Damento GM, Yawn BP, et al. Parkinson disease and melanoma: confirming and reexamining an association. Mayo Clin Proc. 2017;92(7):1070-1079.
Zolpidem Treats Various Neurologic Disorders
A systematic review shows that zolpidem can treat various neurologic disorders, most often related to movement disorders and disorders of consciousness, according to a literature review published online ahead of print June 26 in JAMA Neurology. The investigators searched for English-language articles, published by March 20, 2015, that examined the use of zolpidem for noninsomnia neurologic disorders. Searched databases included PubMed, Scopus, Web of Science Core Collection, the Cochrane Library, EMBASE, CENTRAL, and clinicaltrials.gov. In all, 67 articles were eligible for full manuscript review. Thirty-one studies treated movement disorders, 22 treated disorders of consciousness, and 14 treated other neurologic conditions. The effects of zolpidem were wide ranging and generally lasted for one to four hours before the participant returned to baseline. Sedation was the most common adverse effect.
Bomalaski MN, Claflin ES, Townsend W, Peterson MD. Zolpidem for the treatment of neurologic disorders: a systematic review. JAMA Neurol. 2017 Jun 26 [Epub ahead of print].
Colored Light Triggers Responses in Migraineurs
Lights trigger more changes in autonomic functions and negative emotions during migraine than in control subjects, and the association between light and positive emotions is stronger in control subjects than in migraineurs, according to a study published online ahead of print June 26 in the Proceedings of the National Academy of Sciences. Researchers showed different colored lights to 81 migraineurs and 17 people who had never had a migraine. The effects of light and color were tested three times. Investigators found that all colors of light triggered unpleasant physiologic sensations in patients with migraines, during and between attacks. Additionally, migraineurs reported intense emotional responses such as anger, nervousness, hopelessness, sadness, depression, anxiety, and fear when exposed to all light colors except green.
Noseda R, Lee AJ, Nir RR, et al. Neural mechanism for hypothalamic-mediated autonomic responses to light during migraine. Proc Natl Acad Sci. 2017 Jun 26 [Epub ahead of print].
TBI May Not Hasten Cognitive Decline
Having a history of traumatic brain injury (TBI) with loss of consciousness does not affect the rate of cognitive change over time for people with normal cognition or people with Alzheimer’s disease, according to a study published online ahead of print June 22 in the Journal of Alzheimer’s Disease. Researchers compared performance on cognitive tests over time for 432 participants with normal cognition and 274 participants with probable Alzheimer’s disease. They matched participants with a history of TBI with loss of consciousness to an equal number of demographically and clinically similar participants without a history of TBI. Mixed-effects regressions showed that a history of TBI with loss of consciousness did not affect rates of cognitive change in APOE ε4 carriers and noncarriers.
Tripodis Y, Alosco ML, Zirogiannis N, et al. The effect of traumatic brain injury history with loss of consciousness on rate of cognitive decline among older adults with normal cognition and Alzheimer’s disease dementia. J Alzheimers Dis. 2017 Jun 22 [Epub ahead of print].
Visual Changes in Parkinson’s Disease
Visual system alterations can be detected in early stages of Parkinson’s disease, and the entire intracranial visual system can be involved, according to a study published online ahead of print July 11 in Radiology. Twenty patients with newly diagnosed Parkinson’s disease and 20 age-matched control subjects were studied. Researchers used diffusion-weighted imaging to assess white matter changes and voxel-based morphometry (VBM) to investigate concentration changes of gray and white matter. In patients with Parkinson’s disease, significant alterations were found in optic radiation connectivity distribution, with decreased lateral geniculate nucleus V2 density, a significant increase in optic radiation mean diffusivity, and a significant reduction in white matter concentration. VBM analysis also showed a significant reduction in visual cortical volumes.
Arrigo A, Calamuneri A, Milardi D, et al. Visual system involvement in patients with newly diagnosed Parkinson disease. Radiology. 2017 Jul 11 [Epub ahead of print].
—Kimberly Williams
VIDEO: Further CTE correlation found in deceased American football players
Evidence of a correlation between chronic traumatic encephalopathy (CTE) and playing American football was strengthened in the largest retrospective study cohort to date.
The progressive neurodegenerative disease associated with recurrent head trauma has been linked to football over the past decade. However, this new study took steps to solidify the connection by studying 202 deceased brains, more than double the size of a previous 2013 report.
First author Jesse Mez, MD, of Boston University, and his colleagues examined the brains donated to a brain bank jointly run by the VA Boston Healthcare System, Boston University, and the Concussion Legacy Foundation. They correlated their findings with interviews and questionnaires filled out in 2014 by those close to the donors (JAMA. 2017 Jul 25. doi: 10.1001/jama.2017.8334).
The donors were male, and a majority (79%) were white. The average age at death was 67 years. In the mild cases, there was an average of 13 years of play; in severe cases, the average was 15.8 years.
The researchers found evidence of CTE in 177 (88%) of the 202 brains of football players, with cases found in 3 (21%) who played only in high school, 48 (91%) who played in college, 9 (64%) semiprofessional players, 7 (88%) Canadian Football League players, and 110 (99%) NFL players, according to investigators.
“Nearly all of the former NFL players in this study had CTE pathology, and this pathology was frequently severe,” noted Dr. Mez and his coinvestigators. ”These findings suggest that CTE may be related to prior participation in football and that a high level of play may be related to substantial disease burden.”
Severity of CTE positively correlated with longer playing history and more competitive levels of play. According to the investigators, severe cases of CTE were found in none of the high school players, 27 college players (56%), 5 semiprofessional players (56%), 6 Canadian professional players (86%), and 95 NFL players (86%).
All participants with CTE commonly displayed certain symptoms regardless of severity level.
Impulsiveness occurred in 23 mild cases (89%) and 65 severe cases (80%). Depression was seen in 18 mild cases (67%) and 46 severe cases (56%). A total of 13 players (50%) with mild symptoms showed apathy, compared with 43 with severe symptoms (52%). Anxiety was reported for 14 mild cases (52%) and 41 severe cases (50%). Cognitive symptoms such as problems with memory and attention were also common at both levels of severity, with 19 cases (73%) and 18 cases (69%), respectively, among donors with mild CTE, and 76 (92%) and 67 (81%) among donors with severe CTE.
Those interviewed who were close to the donors also reported other behavior or mood symptoms that the investigators inferred to be related to CTE.
“Many of these participants had a substance use disorder, demonstrated suicidality, or had a family history of psychiatric illness,” the investigators wrote. “Behavior or mood symptoms may be the initial presentation for a subset of individuals with CTE, or alternatively, CTE [phosphorylated tau] pathology may lower the threshold for psychiatric manifestations in susceptible individuals.”
The investigators asserted that the correlation of CTE diagnosis and severity may be more nuanced than just how many times a player is hit.
“Several other football-related factors may influence CTE risk and disease severity, including but not limited to age at first exposure to football, duration of play, player position, cumulative hits, and linear and rotational acceleration of hits,” Dr. Mez and his associates wrote. “Recent work in living former football players has shown that age at first exposure may be related to impaired cognitive performance and altered corpus callosum white matter and that cumulative hits may be related to impairment on self-report and objective measures of cognition, mood, and behavior, although it is unclear if any of these outcomes are related to CTE pathology.”
This study was limited by the potential bias of donors who participated in the program. Researchers acknowledge that public awareness of the issue of CTE and head trauma may have influenced players with symptoms to donate their brains, thereby increasing the CTE frequency in the sample.
In addition, the brain bank where the sample was taken is not representative of the entire population of American football players, as most donors played at the college, semi-professional, and professional level, as opposed to only high school or youth leagues.
The senior author of the study, Ann C. McKee, MD, discussed the study further in a related video interview.
The National Institute of Neurological Disorders and Stroke, the National Institute of Aging, the U.S. Department of Defense, the U.S. Department of Veterans Affairs, the National Operating Committee on Standards for Athletic Equipment, the Alzheimer’s Association, the Concussion Legacy Foundation, the Andlinger Family Foundation, the WWE, and the NFL supported the study. Five authors reported receiving support from relevant sources, including the NFL.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @eaztweets
Traumatic brain injuries (TBIs) are a serious health concern that currently affect 10 million people per year worldwide.
While a majority of TBIs are caused by car crashes, contact sports are estimated to cause between 1.6-3.8 million concussions in the United States every year, making the root of this study – to learn more about CTE among those in contact sports – imperative.
This study used the largest CTE cohort to date, but it is important to read the results, which are concerning, within the context of the study.
Results from the informants who filled out the questionnaires – most commonly friends or family of the deceased – showed cognitive symptoms in 88% of donors and behavioral symptoms in 95%, compared with 5% and 20% prevalence, respectively, among a questionnaire-based study filled out by retired National Football League players. This may mean that rates of symptomatic CTE may be lower outside of a selected cohort of former players.
While early-stage CTE was found in some high school players, most individuals do not play football beyond a high school level, and the link between high school football and future neurological decline was not well established in this study.
This study is a good example of the progress that has been made in TBI research, but there are still many fundamental questions that need to be answered. The next step will be improving disease models and expanding the studies of at-risk populations.
It is of the utmost importance that these improvements are made immediately; increasing our knowledge and public awareness of TBIs is paramount.
Gil Rabinovici, MD, is associate professor of neurology at the University of California–San Francisco, and an associate editor for JAMA Neurology. He receives research support from Avid Radiopharmaceuticals, Eli Lilly, GE Healthcare, and Piramal. He has received consulting or speaking honoraria from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche. These comments were taken from an editorial (JAMA 2017 Jul 25. doi: 10.1001/jama.2017.9353 ).
Traumatic brain injuries (TBIs) are a serious health concern that currently affect 10 million people per year worldwide.
While a majority of TBIs are caused by car crashes, contact sports are estimated to cause between 1.6-3.8 million concussions in the United States every year, making the root of this study – to learn more about CTE among those in contact sports – imperative.
This study used the largest CTE cohort to date, but it is important to read the results, which are concerning, within the context of the study.
Results from the informants who filled out the questionnaires – most commonly friends or family of the deceased – showed cognitive symptoms in 88% of donors and behavioral symptoms in 95%, compared with 5% and 20% prevalence, respectively, among a questionnaire-based study filled out by retired National Football League players. This may mean that rates of symptomatic CTE may be lower outside of a selected cohort of former players.
While early-stage CTE was found in some high school players, most individuals do not play football beyond a high school level, and the link between high school football and future neurological decline was not well established in this study.
This study is a good example of the progress that has been made in TBI research, but there are still many fundamental questions that need to be answered. The next step will be improving disease models and expanding the studies of at-risk populations.
It is of the utmost importance that these improvements are made immediately; increasing our knowledge and public awareness of TBIs is paramount.
Gil Rabinovici, MD, is associate professor of neurology at the University of California–San Francisco, and an associate editor for JAMA Neurology. He receives research support from Avid Radiopharmaceuticals, Eli Lilly, GE Healthcare, and Piramal. He has received consulting or speaking honoraria from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche. These comments were taken from an editorial (JAMA 2017 Jul 25. doi: 10.1001/jama.2017.9353 ).
Traumatic brain injuries (TBIs) are a serious health concern that currently affect 10 million people per year worldwide.
While a majority of TBIs are caused by car crashes, contact sports are estimated to cause between 1.6-3.8 million concussions in the United States every year, making the root of this study – to learn more about CTE among those in contact sports – imperative.
This study used the largest CTE cohort to date, but it is important to read the results, which are concerning, within the context of the study.
Results from the informants who filled out the questionnaires – most commonly friends or family of the deceased – showed cognitive symptoms in 88% of donors and behavioral symptoms in 95%, compared with 5% and 20% prevalence, respectively, among a questionnaire-based study filled out by retired National Football League players. This may mean that rates of symptomatic CTE may be lower outside of a selected cohort of former players.
While early-stage CTE was found in some high school players, most individuals do not play football beyond a high school level, and the link between high school football and future neurological decline was not well established in this study.
This study is a good example of the progress that has been made in TBI research, but there are still many fundamental questions that need to be answered. The next step will be improving disease models and expanding the studies of at-risk populations.
It is of the utmost importance that these improvements are made immediately; increasing our knowledge and public awareness of TBIs is paramount.
Gil Rabinovici, MD, is associate professor of neurology at the University of California–San Francisco, and an associate editor for JAMA Neurology. He receives research support from Avid Radiopharmaceuticals, Eli Lilly, GE Healthcare, and Piramal. He has received consulting or speaking honoraria from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche. These comments were taken from an editorial (JAMA 2017 Jul 25. doi: 10.1001/jama.2017.9353 ).
Evidence of a correlation between chronic traumatic encephalopathy (CTE) and playing American football was strengthened in the largest retrospective study cohort to date.
The progressive neurodegenerative disease associated with recurrent head trauma has been linked to football over the past decade. However, this new study took steps to solidify the connection by studying 202 deceased brains, more than double the size of a previous 2013 report.
First author Jesse Mez, MD, of Boston University, and his colleagues examined the brains donated to a brain bank jointly run by the VA Boston Healthcare System, Boston University, and the Concussion Legacy Foundation. They correlated their findings with interviews and questionnaires filled out in 2014 by those close to the donors (JAMA. 2017 Jul 25. doi: 10.1001/jama.2017.8334).
The donors were male, and a majority (79%) were white. The average age at death was 67 years. In the mild cases, there was an average of 13 years of play; in severe cases, the average was 15.8 years.
The researchers found evidence of CTE in 177 (88%) of the 202 brains of football players, with cases found in 3 (21%) who played only in high school, 48 (91%) who played in college, 9 (64%) semiprofessional players, 7 (88%) Canadian Football League players, and 110 (99%) NFL players, according to investigators.
“Nearly all of the former NFL players in this study had CTE pathology, and this pathology was frequently severe,” noted Dr. Mez and his coinvestigators. ”These findings suggest that CTE may be related to prior participation in football and that a high level of play may be related to substantial disease burden.”
Severity of CTE positively correlated with longer playing history and more competitive levels of play. According to the investigators, severe cases of CTE were found in none of the high school players, 27 college players (56%), 5 semiprofessional players (56%), 6 Canadian professional players (86%), and 95 NFL players (86%).
All participants with CTE commonly displayed certain symptoms regardless of severity level.
Impulsiveness occurred in 23 mild cases (89%) and 65 severe cases (80%). Depression was seen in 18 mild cases (67%) and 46 severe cases (56%). A total of 13 players (50%) with mild symptoms showed apathy, compared with 43 with severe symptoms (52%). Anxiety was reported for 14 mild cases (52%) and 41 severe cases (50%). Cognitive symptoms such as problems with memory and attention were also common at both levels of severity, with 19 cases (73%) and 18 cases (69%), respectively, among donors with mild CTE, and 76 (92%) and 67 (81%) among donors with severe CTE.
Those interviewed who were close to the donors also reported other behavior or mood symptoms that the investigators inferred to be related to CTE.
“Many of these participants had a substance use disorder, demonstrated suicidality, or had a family history of psychiatric illness,” the investigators wrote. “Behavior or mood symptoms may be the initial presentation for a subset of individuals with CTE, or alternatively, CTE [phosphorylated tau] pathology may lower the threshold for psychiatric manifestations in susceptible individuals.”
The investigators asserted that the correlation of CTE diagnosis and severity may be more nuanced than just how many times a player is hit.
“Several other football-related factors may influence CTE risk and disease severity, including but not limited to age at first exposure to football, duration of play, player position, cumulative hits, and linear and rotational acceleration of hits,” Dr. Mez and his associates wrote. “Recent work in living former football players has shown that age at first exposure may be related to impaired cognitive performance and altered corpus callosum white matter and that cumulative hits may be related to impairment on self-report and objective measures of cognition, mood, and behavior, although it is unclear if any of these outcomes are related to CTE pathology.”
This study was limited by the potential bias of donors who participated in the program. Researchers acknowledge that public awareness of the issue of CTE and head trauma may have influenced players with symptoms to donate their brains, thereby increasing the CTE frequency in the sample.
In addition, the brain bank where the sample was taken is not representative of the entire population of American football players, as most donors played at the college, semi-professional, and professional level, as opposed to only high school or youth leagues.
The senior author of the study, Ann C. McKee, MD, discussed the study further in a related video interview.
The National Institute of Neurological Disorders and Stroke, the National Institute of Aging, the U.S. Department of Defense, the U.S. Department of Veterans Affairs, the National Operating Committee on Standards for Athletic Equipment, the Alzheimer’s Association, the Concussion Legacy Foundation, the Andlinger Family Foundation, the WWE, and the NFL supported the study. Five authors reported receiving support from relevant sources, including the NFL.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @eaztweets
Evidence of a correlation between chronic traumatic encephalopathy (CTE) and playing American football was strengthened in the largest retrospective study cohort to date.
The progressive neurodegenerative disease associated with recurrent head trauma has been linked to football over the past decade. However, this new study took steps to solidify the connection by studying 202 deceased brains, more than double the size of a previous 2013 report.
First author Jesse Mez, MD, of Boston University, and his colleagues examined the brains donated to a brain bank jointly run by the VA Boston Healthcare System, Boston University, and the Concussion Legacy Foundation. They correlated their findings with interviews and questionnaires filled out in 2014 by those close to the donors (JAMA. 2017 Jul 25. doi: 10.1001/jama.2017.8334).
The donors were male, and a majority (79%) were white. The average age at death was 67 years. In the mild cases, there was an average of 13 years of play; in severe cases, the average was 15.8 years.
The researchers found evidence of CTE in 177 (88%) of the 202 brains of football players, with cases found in 3 (21%) who played only in high school, 48 (91%) who played in college, 9 (64%) semiprofessional players, 7 (88%) Canadian Football League players, and 110 (99%) NFL players, according to investigators.
“Nearly all of the former NFL players in this study had CTE pathology, and this pathology was frequently severe,” noted Dr. Mez and his coinvestigators. ”These findings suggest that CTE may be related to prior participation in football and that a high level of play may be related to substantial disease burden.”
Severity of CTE positively correlated with longer playing history and more competitive levels of play. According to the investigators, severe cases of CTE were found in none of the high school players, 27 college players (56%), 5 semiprofessional players (56%), 6 Canadian professional players (86%), and 95 NFL players (86%).
All participants with CTE commonly displayed certain symptoms regardless of severity level.
Impulsiveness occurred in 23 mild cases (89%) and 65 severe cases (80%). Depression was seen in 18 mild cases (67%) and 46 severe cases (56%). A total of 13 players (50%) with mild symptoms showed apathy, compared with 43 with severe symptoms (52%). Anxiety was reported for 14 mild cases (52%) and 41 severe cases (50%). Cognitive symptoms such as problems with memory and attention were also common at both levels of severity, with 19 cases (73%) and 18 cases (69%), respectively, among donors with mild CTE, and 76 (92%) and 67 (81%) among donors with severe CTE.
Those interviewed who were close to the donors also reported other behavior or mood symptoms that the investigators inferred to be related to CTE.
“Many of these participants had a substance use disorder, demonstrated suicidality, or had a family history of psychiatric illness,” the investigators wrote. “Behavior or mood symptoms may be the initial presentation for a subset of individuals with CTE, or alternatively, CTE [phosphorylated tau] pathology may lower the threshold for psychiatric manifestations in susceptible individuals.”
The investigators asserted that the correlation of CTE diagnosis and severity may be more nuanced than just how many times a player is hit.
“Several other football-related factors may influence CTE risk and disease severity, including but not limited to age at first exposure to football, duration of play, player position, cumulative hits, and linear and rotational acceleration of hits,” Dr. Mez and his associates wrote. “Recent work in living former football players has shown that age at first exposure may be related to impaired cognitive performance and altered corpus callosum white matter and that cumulative hits may be related to impairment on self-report and objective measures of cognition, mood, and behavior, although it is unclear if any of these outcomes are related to CTE pathology.”
This study was limited by the potential bias of donors who participated in the program. Researchers acknowledge that public awareness of the issue of CTE and head trauma may have influenced players with symptoms to donate their brains, thereby increasing the CTE frequency in the sample.
In addition, the brain bank where the sample was taken is not representative of the entire population of American football players, as most donors played at the college, semi-professional, and professional level, as opposed to only high school or youth leagues.
The senior author of the study, Ann C. McKee, MD, discussed the study further in a related video interview.
The National Institute of Neurological Disorders and Stroke, the National Institute of Aging, the U.S. Department of Defense, the U.S. Department of Veterans Affairs, the National Operating Committee on Standards for Athletic Equipment, the Alzheimer’s Association, the Concussion Legacy Foundation, the Andlinger Family Foundation, the WWE, and the NFL supported the study. Five authors reported receiving support from relevant sources, including the NFL.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @eaztweets
FROM JAMA
Key clinical point:
Major finding: Of 202 deceased football players who played at levels ranging from high school to the NFL and who donated their brains, 177 (88%) were diagnosed with CTE.
Data source: A blinded, retrospective study of 202 donated brains, as well as questionnaires and interviews with informants close to the deceased.
Disclosures: The National Institute of Neurological Disorders and Stroke, the National Institute of Aging, U.S. Department of Defense, U.S. Department of Veterans Affairs, the National Operating Committee on Standards for Athletic Equipment, the Alzheimer’s Association, the Concussion Legacy Foundation, the Andlinger Family Foundation, the WWE, and the NFL supported the study. Five authors reported receiving support from relevant sources, including the NFL.
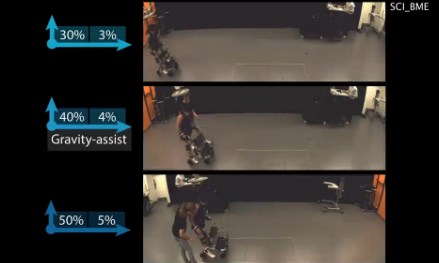
Algorithm-based trunk support system shows potential for recovery of walking ability
A multidirectional gravity-assist device that delivers precise trunk support to stroke and spinal cord injury (SCI) patients via an artificial intelligence algorithm has demonstrated significantly improved locomotor performance beyond treadmill-based systems in a new study.
The harness device used in the study adjusts patients’ balance while they stand still or walk by employing a unique, adaptive multidirectional gravity-assist (MGA) algorithm tailored to the specific needs of the patient, according to Jean-Baptiste Mignardot, PhD, of the Center for Neuroprosthetics and Brain Mind Institute, Swiss Federal Institute of Technology, Lausanne, Switzerland, and fellow investigators.
“The MGA establishes a safe and natural rehabilitation environment wherein individuals with neurological deficits can perform basic and skilled locomotor activities that would not be possible without robotic assistance,” according to the investigators. “The immediate and short-term ameliorations of gait performance during locomotion with MGA illustrate the potential of this environment to augment motor recovery.”
Current gait rehabilitation methods in stroke or SCI patients most commonly involves counterweight mechanisms or force-controlled equipment that apply upward support while walking on a treadmill. However Dr. Mignardot and his colleagues believe these methods are flawed.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Treadmill-restricted environments markedly differ from the rich repertoire of natural locomotor activities underlying daily living,” the investigators wrote. “Vertically restricted trunk support creates undesired forces that impede gait execution.”
To counteract these negative effects, the MGA adjusts both upward and forward forces on the patient’s body, re-creating a more naturally occurring gait posture, which investigators have likened to an inverted pendulum with a natural forward tilt. In order to create the algorithm, investigators ran through a series of procedures, starting with calibrations based on the gait of healthy subjects and adjusting for necessary upward and forward assistance for stroke and SCI patients.
The artificial neural network within the algorithm analyzes patients’ support needs, a job that therapists currently have to do based on visual observations. This opens a window to faster and more accurate estimations, according to the investigators (Sci Transl Med. 2017 Jul 19. doi: 10.1126/scitranslmed.aah3621).
Investigators tested the algorithm on 15 SCI patients and 12 stroke patients. The stroke patients had an average age of 51 years, with length of time after stroke varying from 8 to 235 months. The SCI patients had an average age of 47 years, with a length of time since injury ranging from 12 to 264 months. Most patients in both groups were male.
When tested, the algorithm showed varying success depending on the severity of the injury, according to the researchers.
“For example, the MGA enabled subjects who could not stand independently to walk overground with or without assistive device.” Subjects who were able to move around only with crutches or a walker progressed without the use of assistive devices and exhibited improved spatiotemporal gait features, according to Dr. Mignardot and fellow investigators. “Individuals with stroke exhibited similar or even superior amelioration of locomotor performance and showed that individuals who could only walk with crutches exhibited improved intralimb coordination.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
After initial efficacy tests, the researchers tested the MGA’s effectiveness in five SCI patients immediately after 1 hour of training with the device and found that their gait speed increased during the training. However, the improvements were not evident in a similar test 1 week later. Similar tests using treadmill-restricted step training without the MGA device did not show any improvement during either week of testing.
Although the study’s small sample size limited the conclusions that could be reached, the investigators were encouraged by the overall effects of the algorithm. They noted that further tests are required to test the potential sensitivity and accuracy of the software.
The study was supported by the European Commission’s Seventh Framework Programme, various foundations, and the Swiss National Science Foundation.
Investigators reported holding patents on the step-by-step procedure and use of the MGA algorithm in this study.
[email protected]
On Twitter @eaztweets
A multidirectional gravity-assist device that delivers precise trunk support to stroke and spinal cord injury (SCI) patients via an artificial intelligence algorithm has demonstrated significantly improved locomotor performance beyond treadmill-based systems in a new study.
The harness device used in the study adjusts patients’ balance while they stand still or walk by employing a unique, adaptive multidirectional gravity-assist (MGA) algorithm tailored to the specific needs of the patient, according to Jean-Baptiste Mignardot, PhD, of the Center for Neuroprosthetics and Brain Mind Institute, Swiss Federal Institute of Technology, Lausanne, Switzerland, and fellow investigators.
“The MGA establishes a safe and natural rehabilitation environment wherein individuals with neurological deficits can perform basic and skilled locomotor activities that would not be possible without robotic assistance,” according to the investigators. “The immediate and short-term ameliorations of gait performance during locomotion with MGA illustrate the potential of this environment to augment motor recovery.”
Current gait rehabilitation methods in stroke or SCI patients most commonly involves counterweight mechanisms or force-controlled equipment that apply upward support while walking on a treadmill. However Dr. Mignardot and his colleagues believe these methods are flawed.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Treadmill-restricted environments markedly differ from the rich repertoire of natural locomotor activities underlying daily living,” the investigators wrote. “Vertically restricted trunk support creates undesired forces that impede gait execution.”
To counteract these negative effects, the MGA adjusts both upward and forward forces on the patient’s body, re-creating a more naturally occurring gait posture, which investigators have likened to an inverted pendulum with a natural forward tilt. In order to create the algorithm, investigators ran through a series of procedures, starting with calibrations based on the gait of healthy subjects and adjusting for necessary upward and forward assistance for stroke and SCI patients.
The artificial neural network within the algorithm analyzes patients’ support needs, a job that therapists currently have to do based on visual observations. This opens a window to faster and more accurate estimations, according to the investigators (Sci Transl Med. 2017 Jul 19. doi: 10.1126/scitranslmed.aah3621).
Investigators tested the algorithm on 15 SCI patients and 12 stroke patients. The stroke patients had an average age of 51 years, with length of time after stroke varying from 8 to 235 months. The SCI patients had an average age of 47 years, with a length of time since injury ranging from 12 to 264 months. Most patients in both groups were male.
When tested, the algorithm showed varying success depending on the severity of the injury, according to the researchers.
“For example, the MGA enabled subjects who could not stand independently to walk overground with or without assistive device.” Subjects who were able to move around only with crutches or a walker progressed without the use of assistive devices and exhibited improved spatiotemporal gait features, according to Dr. Mignardot and fellow investigators. “Individuals with stroke exhibited similar or even superior amelioration of locomotor performance and showed that individuals who could only walk with crutches exhibited improved intralimb coordination.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
After initial efficacy tests, the researchers tested the MGA’s effectiveness in five SCI patients immediately after 1 hour of training with the device and found that their gait speed increased during the training. However, the improvements were not evident in a similar test 1 week later. Similar tests using treadmill-restricted step training without the MGA device did not show any improvement during either week of testing.
Although the study’s small sample size limited the conclusions that could be reached, the investigators were encouraged by the overall effects of the algorithm. They noted that further tests are required to test the potential sensitivity and accuracy of the software.
The study was supported by the European Commission’s Seventh Framework Programme, various foundations, and the Swiss National Science Foundation.
Investigators reported holding patents on the step-by-step procedure and use of the MGA algorithm in this study.
[email protected]
On Twitter @eaztweets
A multidirectional gravity-assist device that delivers precise trunk support to stroke and spinal cord injury (SCI) patients via an artificial intelligence algorithm has demonstrated significantly improved locomotor performance beyond treadmill-based systems in a new study.
The harness device used in the study adjusts patients’ balance while they stand still or walk by employing a unique, adaptive multidirectional gravity-assist (MGA) algorithm tailored to the specific needs of the patient, according to Jean-Baptiste Mignardot, PhD, of the Center for Neuroprosthetics and Brain Mind Institute, Swiss Federal Institute of Technology, Lausanne, Switzerland, and fellow investigators.
“The MGA establishes a safe and natural rehabilitation environment wherein individuals with neurological deficits can perform basic and skilled locomotor activities that would not be possible without robotic assistance,” according to the investigators. “The immediate and short-term ameliorations of gait performance during locomotion with MGA illustrate the potential of this environment to augment motor recovery.”
Current gait rehabilitation methods in stroke or SCI patients most commonly involves counterweight mechanisms or force-controlled equipment that apply upward support while walking on a treadmill. However Dr. Mignardot and his colleagues believe these methods are flawed.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
“Treadmill-restricted environments markedly differ from the rich repertoire of natural locomotor activities underlying daily living,” the investigators wrote. “Vertically restricted trunk support creates undesired forces that impede gait execution.”
To counteract these negative effects, the MGA adjusts both upward and forward forces on the patient’s body, re-creating a more naturally occurring gait posture, which investigators have likened to an inverted pendulum with a natural forward tilt. In order to create the algorithm, investigators ran through a series of procedures, starting with calibrations based on the gait of healthy subjects and adjusting for necessary upward and forward assistance for stroke and SCI patients.
The artificial neural network within the algorithm analyzes patients’ support needs, a job that therapists currently have to do based on visual observations. This opens a window to faster and more accurate estimations, according to the investigators (Sci Transl Med. 2017 Jul 19. doi: 10.1126/scitranslmed.aah3621).
Investigators tested the algorithm on 15 SCI patients and 12 stroke patients. The stroke patients had an average age of 51 years, with length of time after stroke varying from 8 to 235 months. The SCI patients had an average age of 47 years, with a length of time since injury ranging from 12 to 264 months. Most patients in both groups were male.
When tested, the algorithm showed varying success depending on the severity of the injury, according to the researchers.
“For example, the MGA enabled subjects who could not stand independently to walk overground with or without assistive device.” Subjects who were able to move around only with crutches or a walker progressed without the use of assistive devices and exhibited improved spatiotemporal gait features, according to Dr. Mignardot and fellow investigators. “Individuals with stroke exhibited similar or even superior amelioration of locomotor performance and showed that individuals who could only walk with crutches exhibited improved intralimb coordination.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
After initial efficacy tests, the researchers tested the MGA’s effectiveness in five SCI patients immediately after 1 hour of training with the device and found that their gait speed increased during the training. However, the improvements were not evident in a similar test 1 week later. Similar tests using treadmill-restricted step training without the MGA device did not show any improvement during either week of testing.
Although the study’s small sample size limited the conclusions that could be reached, the investigators were encouraged by the overall effects of the algorithm. They noted that further tests are required to test the potential sensitivity and accuracy of the software.
The study was supported by the European Commission’s Seventh Framework Programme, various foundations, and the Swiss National Science Foundation.
Investigators reported holding patents on the step-by-step procedure and use of the MGA algorithm in this study.
[email protected]
On Twitter @eaztweets
FROM SCIENCE TRANSLATIONAL MEDICINE
New and Noteworthy Information—July 2017
Device Helps Patients Move Paralyzed Hands After Stroke
Patients with stroke who learn to use their minds to open and close a device fitted over their paralyzed hands gain some control over their hands, according to a study published online ahead of print May 26 in Stroke. Ten survivors of chronic hemiparetic stroke with moderate-to-severe upper-limb motor impairment used a powered exoskeleton that opened and closed the affected hand using spectral power from EEG signals from the unaffected hemisphere associated with imagined hand movements of the paretic limb. At 12 weeks, participants had a statistically significant average increase of 6.2 points in the Action Research Arm Test. This behavioral improvement significantly correlated with improvements in brain–computer interface control. Secondary outcomes of grasp strength, Motricity Index, and the Canadian Occupational Performance Measure also significantly improved.
Bundy DT, Souders L, Baranyai K, et al. Contralesional brain-computer interface control of a powered exoskeleton for motor recovery in chronic stroke survivors. Stroke. 2017 May 26 [Epub ahead of print].
Pyrimethamine Lowers Levels of ALS Biomarker
Pyrimethamine is safe and well tolerated in amyotrophic lateral sclerosis (ALS), according to a study published online ahead of print May 8 in Annals of Neurology. Participants underwent a multicenter, open-label, nine-month dose-ranging study to determine the safety and efficacy of pyrimethamine to lower SOD1 levels in the CSF in patients with SOD1 mutations linked to familial ALS. The study included 32 patients with various SOD1 genetic mutations linked to ALS. Participants had three lumbar punctures, blood studies, and a clinical assessment of strength, motor function, quality of life, and potential adverse effects. A linear mixed effects model showed a significant reduction in CSF SOD1 at visit six, with a mean reduction of 13.5%, and at visit nine, with a mean reduction of 10.5%.
Lange DJ, Shahbazi M, Silani V, et al. Pyrimethamine significantly lowers cerebrospinal fluid Cu/Zn superoxide dismutase in amyotrophic lateral sclerosis patients with SOD1 mutations. Ann Neurol. 2017 May 8 [Epub ahead of print].
Statin Use Linked to Higher Risk of Parkinson’s Disease
Statins, especially lipophilic statins, are associated with higher risk of Parkinson’s disease, according to a study published in the June issue of Movement Disorders. The association is stronger with initial use, which suggests a facilitating effect, said the investigators. Researchers performed a retrospective case–control analysis and identified 2,322 people with incident Parkinson’s disease who had been enrolled in a claims database for at least 2.5 years before diagnosis or prescription of antiparkinson medication. They matched the cases with 2,322 controls by age, gender, and a follow-up window. Statin use was significantly associated with Parkinson’s disease risk. The strongest associations were for lipophilic statins (odds ratio [OR], 1.58) versus hydrophilic statins (OR, 1.19), statins plus nonstatins (OR, 1.95), and for the initial period after starting statins.
Liu G, Sterling NW, Kong L, et al. Statins may facilitate Parkinson’s disease: insight gained from a large, national claims database. Mov Disord. 2017;32(6):913-917.
Is Moderate Drinking Associated With Cognitive Decline?
Moderate alcohol consumption is associated with adverse brain outcomes, including hippocampal atrophy, according to a study published online ahead of print June 6 in BMJ. The study included 550 men and women with a mean age of 43 at study baseline. No patient had alcohol dependence, and all underwent brain MRI at follow-up. Higher alcohol consumption over the 30-year follow-up was associated with increased odds of hippocampal atrophy in a dose-dependent fashion. People consuming more than 30 units/week of alcohol were at the highest risk, compared with abstainers. People who drank moderately had three times the odds of right-sided hippocampal atrophy. There was no protective effect of light drinking over abstinence. Higher alcohol use also was associated with differences in corpus callosum microstructure and faster decline in lexical fluency.
Topiwala A, Allan CL, Valkanova V, et al. Moderate alcohol consumption as risk factor for adverse brain outcomes and cognitive decline: longitudinal cohort study. BMJ. 2017 Jun 6 [Epub ahead of print].
Consuming Low-Fat Dairy May Increase Risk for Parkinson’s Disease
Frequently consuming low-fat dairy products may be associated with an increased risk of Parkinson’s disease, according to a study published online ahead of print June 8 in Neurology. This study is based on data from 80,736 participants in the Nurses’ Health Study and 48,610 participants in the Health Professionals Follow-Up Study, with 26 and 24 years of follow-up, respectively. Both US-based studies were conducted through mailed biennial questionnaires. Dietary intake was assessed with food frequency questionnaires administered repeatedly over the follow-up period. Total dairy intake was not significantly associated with Parkinson’s disease risk, but intake of low-fat dairy foods was associated with Parkinson’s disease risk. This association appeared to result from an increased risk of Parkinson’s disease associated with skim and low-fat milk.
Hughes KC, Gao X, Kim IY, et al. Intake of dairy foods and risk of Parkinson disease. Neurology. 2017 Jun 8 [Epub ahead of print].
Elevated Brain Amyloid Increases Likelihood of Cognitive Decline
Elevated baseline brain amyloid level, compared with normal brain amyloid level, is associated with higher likelihood of cognitive decline, according to a study published June 13 in JAMA. Exploratory analyses were conducted with longitudinal cognitive and biomarker data from 445 cognitively normal people. Participants were classified at baseline as having normal or elevated brain amyloid using PET amyloid imaging or a CSF assay of amyloid β. Outcomes included scores on the Preclinical Alzheimer Cognitive Composite (PACC), Mini-Mental State Examination (MMSE), Clinical Dementia Rating Sum of Boxes (CDR-SOB), and Logical Memory Delayed Recall. Compared with the group with normal amyloid, people with elevated amyloid had worse mean scores at four years on the PACC, MMSE, and CDR-SOB. For Logical Memory Delayed Recall, between-group scores were not significantly different at four years.
Donohue MC, Sperling RA, Petersen R, et al. Association between elevated brain amyloid and subsequent cognitive decline among cognitively normal persons. JAMA. 2017;317(22):2305-2316.
Seven Risk Genes for Insomnia Found
Researchers have found seven risk genes for insomnia, according to a study published online ahead of print June 12 in Nature Genetics. To identify genetic factors for insomnia complaints, investigators performed a genome-wide association study and a genome-wide gene-based association study in 113,006 participants. The authors identified three loci and seven genes, including MEIS1,
Hammerschlag AR, Stringer S, de Leeuw CA, et al. Genome-wide association analysis of insomnia complaints identifies risk genes and genetic overlap with psychiatric and metabolic traits. Nat Genet. 2017 Jun 12 [Epub ahead of print].
Is Telemedicine for Headache as Effective as In-Person Visit?
In people with headache, a video consultation with a neurologist for treatment may be as effective as an in-person visit, according to a study published online ahead of print June 14 in Neurology. Researchers randomized, allocated, and consulted patients with nonacute headache via telemedicine or in a traditional manner in a noninferiority trial. Efficacy end points assessed by questionnaires at three and 12 months included change from baseline in Headache Impact Test-6 (HIT-6) and pain intensity. The primary safety end point was presence of secondary headache within 12 months after consultation. There were no differences between telemedicine and traditional consultations in HIT-6 or pain intensity over three periods. The absolute difference in HIT-6 from baseline was 0.3 at three months and 0.2 at 12 months.
Müller KI, Alstadhaug KB, Bekkelund SI. A randomized trial of telemedicine efficacy and safety for nonacute headaches. Neurology. 2017 Jun 14 [Epub ahead of print].
Minocycline Reduces Risk of Conversion From CIS to MS
The risk of conversion from clinically isolated syndrome (CIS) to multiple sclerosis (MS) is significantly lower with minocycline than with placebo over six months, but not over 24 months, according to a study published June 1 in the New England Journal of Medicine. This study included 142 participants who had had their first demyelinating symptoms within the previous 180 days. At 12 Canadian MS clinics, researchers randomly assigned participants to receive either 100 mg of minocycline, administered orally twice daily, or placebo. Administration of minocycline or placebo was continued until a diagnosis of MS was established or until 24 months after randomization. The unadjusted risk of conversion to MS within six months after randomization was 61.0% in the placebo group and 33.4% in the minocycline group.
Metz LM, Li DKB, Traboulsee AL, et al. Trial of minocycline in a clinically isolated syndrome of multiple sclerosis. N Engl J Med. 2017;376(22):2122-2133.
Can Gene Mutation Speed Memory Loss in Alzheimer’s Disease?
In a middle-aged cohort with Alzheimer’s disease risk, the BDNF Met allele is associated with steeper decline in episodic memory and executive function, according to a study published online ahead of print May 3 in Neurology. One thousand twenty-three adults enrolled in the Wisconsin Registry for Alzheimer’s Prevention underwent BDNF genotyping and cognitive assessment at as many as five time points. A subset of participants underwent Pittsburgh compound B scanning. Compared with BDNF Val/Val homozygotes, Met carriers had steeper decline in verbal learning and memory, and in speed and flexibility. In addition, amyloid β burden moderated the relationship between BDNF and verbal learning and memory, such that Met carriers with greater amyloid β burden showed even steeper cognitive decline.
Boots EA, Schultz SA, Clark LR, et al. BDNF Val66Met predicts cognitive decline in the Wisconsin Registry for Alzheimer’s Prevention. Neurology. 2017 May 3 [Epub ahead of print].
Support From Children Reduces Risk of Dementia
Positive social support from children is associated with reduced risk of dementia, whereas negative social support from children and other immediate family increases the risk, according to a study published in the Journal of Alzheimer’s Disease. Researchers analyzed 10-year follow-up data in 10,055 cognitively normal participants age 50 and older from the English Longitudinal Study of Aging. Incidence of dementia was identified from participant- or informant-reported physician diagnosed dementia or overall score of informant-completed IQCODE questionnaire. Positive social support from children significantly reduced the risk of dementia (hazard ratio, 0.83). Negative support from family and friends was significantly associated with increased risk of dementia. The causal mechanisms that create these associations require further research, said the researchers.
Khondoker M, Rafnsson SB, Morris S, et al. Positive and negative experiences of social support and risk of dementia in later life: an investigation using the English Longitudinal Study of Ageing. J Alzheimers Dis. 2017;58(1):99-108.
—Kimberly Williams
Device Helps Patients Move Paralyzed Hands After Stroke
Patients with stroke who learn to use their minds to open and close a device fitted over their paralyzed hands gain some control over their hands, according to a study published online ahead of print May 26 in Stroke. Ten survivors of chronic hemiparetic stroke with moderate-to-severe upper-limb motor impairment used a powered exoskeleton that opened and closed the affected hand using spectral power from EEG signals from the unaffected hemisphere associated with imagined hand movements of the paretic limb. At 12 weeks, participants had a statistically significant average increase of 6.2 points in the Action Research Arm Test. This behavioral improvement significantly correlated with improvements in brain–computer interface control. Secondary outcomes of grasp strength, Motricity Index, and the Canadian Occupational Performance Measure also significantly improved.
Bundy DT, Souders L, Baranyai K, et al. Contralesional brain-computer interface control of a powered exoskeleton for motor recovery in chronic stroke survivors. Stroke. 2017 May 26 [Epub ahead of print].
Pyrimethamine Lowers Levels of ALS Biomarker
Pyrimethamine is safe and well tolerated in amyotrophic lateral sclerosis (ALS), according to a study published online ahead of print May 8 in Annals of Neurology. Participants underwent a multicenter, open-label, nine-month dose-ranging study to determine the safety and efficacy of pyrimethamine to lower SOD1 levels in the CSF in patients with SOD1 mutations linked to familial ALS. The study included 32 patients with various SOD1 genetic mutations linked to ALS. Participants had three lumbar punctures, blood studies, and a clinical assessment of strength, motor function, quality of life, and potential adverse effects. A linear mixed effects model showed a significant reduction in CSF SOD1 at visit six, with a mean reduction of 13.5%, and at visit nine, with a mean reduction of 10.5%.
Lange DJ, Shahbazi M, Silani V, et al. Pyrimethamine significantly lowers cerebrospinal fluid Cu/Zn superoxide dismutase in amyotrophic lateral sclerosis patients with SOD1 mutations. Ann Neurol. 2017 May 8 [Epub ahead of print].
Statin Use Linked to Higher Risk of Parkinson’s Disease
Statins, especially lipophilic statins, are associated with higher risk of Parkinson’s disease, according to a study published in the June issue of Movement Disorders. The association is stronger with initial use, which suggests a facilitating effect, said the investigators. Researchers performed a retrospective case–control analysis and identified 2,322 people with incident Parkinson’s disease who had been enrolled in a claims database for at least 2.5 years before diagnosis or prescription of antiparkinson medication. They matched the cases with 2,322 controls by age, gender, and a follow-up window. Statin use was significantly associated with Parkinson’s disease risk. The strongest associations were for lipophilic statins (odds ratio [OR], 1.58) versus hydrophilic statins (OR, 1.19), statins plus nonstatins (OR, 1.95), and for the initial period after starting statins.
Liu G, Sterling NW, Kong L, et al. Statins may facilitate Parkinson’s disease: insight gained from a large, national claims database. Mov Disord. 2017;32(6):913-917.
Is Moderate Drinking Associated With Cognitive Decline?
Moderate alcohol consumption is associated with adverse brain outcomes, including hippocampal atrophy, according to a study published online ahead of print June 6 in BMJ. The study included 550 men and women with a mean age of 43 at study baseline. No patient had alcohol dependence, and all underwent brain MRI at follow-up. Higher alcohol consumption over the 30-year follow-up was associated with increased odds of hippocampal atrophy in a dose-dependent fashion. People consuming more than 30 units/week of alcohol were at the highest risk, compared with abstainers. People who drank moderately had three times the odds of right-sided hippocampal atrophy. There was no protective effect of light drinking over abstinence. Higher alcohol use also was associated with differences in corpus callosum microstructure and faster decline in lexical fluency.
Topiwala A, Allan CL, Valkanova V, et al. Moderate alcohol consumption as risk factor for adverse brain outcomes and cognitive decline: longitudinal cohort study. BMJ. 2017 Jun 6 [Epub ahead of print].
Consuming Low-Fat Dairy May Increase Risk for Parkinson’s Disease
Frequently consuming low-fat dairy products may be associated with an increased risk of Parkinson’s disease, according to a study published online ahead of print June 8 in Neurology. This study is based on data from 80,736 participants in the Nurses’ Health Study and 48,610 participants in the Health Professionals Follow-Up Study, with 26 and 24 years of follow-up, respectively. Both US-based studies were conducted through mailed biennial questionnaires. Dietary intake was assessed with food frequency questionnaires administered repeatedly over the follow-up period. Total dairy intake was not significantly associated with Parkinson’s disease risk, but intake of low-fat dairy foods was associated with Parkinson’s disease risk. This association appeared to result from an increased risk of Parkinson’s disease associated with skim and low-fat milk.
Hughes KC, Gao X, Kim IY, et al. Intake of dairy foods and risk of Parkinson disease. Neurology. 2017 Jun 8 [Epub ahead of print].
Elevated Brain Amyloid Increases Likelihood of Cognitive Decline
Elevated baseline brain amyloid level, compared with normal brain amyloid level, is associated with higher likelihood of cognitive decline, according to a study published June 13 in JAMA. Exploratory analyses were conducted with longitudinal cognitive and biomarker data from 445 cognitively normal people. Participants were classified at baseline as having normal or elevated brain amyloid using PET amyloid imaging or a CSF assay of amyloid β. Outcomes included scores on the Preclinical Alzheimer Cognitive Composite (PACC), Mini-Mental State Examination (MMSE), Clinical Dementia Rating Sum of Boxes (CDR-SOB), and Logical Memory Delayed Recall. Compared with the group with normal amyloid, people with elevated amyloid had worse mean scores at four years on the PACC, MMSE, and CDR-SOB. For Logical Memory Delayed Recall, between-group scores were not significantly different at four years.
Donohue MC, Sperling RA, Petersen R, et al. Association between elevated brain amyloid and subsequent cognitive decline among cognitively normal persons. JAMA. 2017;317(22):2305-2316.
Seven Risk Genes for Insomnia Found
Researchers have found seven risk genes for insomnia, according to a study published online ahead of print June 12 in Nature Genetics. To identify genetic factors for insomnia complaints, investigators performed a genome-wide association study and a genome-wide gene-based association study in 113,006 participants. The authors identified three loci and seven genes, including MEIS1,
Hammerschlag AR, Stringer S, de Leeuw CA, et al. Genome-wide association analysis of insomnia complaints identifies risk genes and genetic overlap with psychiatric and metabolic traits. Nat Genet. 2017 Jun 12 [Epub ahead of print].
Is Telemedicine for Headache as Effective as In-Person Visit?
In people with headache, a video consultation with a neurologist for treatment may be as effective as an in-person visit, according to a study published online ahead of print June 14 in Neurology. Researchers randomized, allocated, and consulted patients with nonacute headache via telemedicine or in a traditional manner in a noninferiority trial. Efficacy end points assessed by questionnaires at three and 12 months included change from baseline in Headache Impact Test-6 (HIT-6) and pain intensity. The primary safety end point was presence of secondary headache within 12 months after consultation. There were no differences between telemedicine and traditional consultations in HIT-6 or pain intensity over three periods. The absolute difference in HIT-6 from baseline was 0.3 at three months and 0.2 at 12 months.
Müller KI, Alstadhaug KB, Bekkelund SI. A randomized trial of telemedicine efficacy and safety for nonacute headaches. Neurology. 2017 Jun 14 [Epub ahead of print].
Minocycline Reduces Risk of Conversion From CIS to MS
The risk of conversion from clinically isolated syndrome (CIS) to multiple sclerosis (MS) is significantly lower with minocycline than with placebo over six months, but not over 24 months, according to a study published June 1 in the New England Journal of Medicine. This study included 142 participants who had had their first demyelinating symptoms within the previous 180 days. At 12 Canadian MS clinics, researchers randomly assigned participants to receive either 100 mg of minocycline, administered orally twice daily, or placebo. Administration of minocycline or placebo was continued until a diagnosis of MS was established or until 24 months after randomization. The unadjusted risk of conversion to MS within six months after randomization was 61.0% in the placebo group and 33.4% in the minocycline group.
Metz LM, Li DKB, Traboulsee AL, et al. Trial of minocycline in a clinically isolated syndrome of multiple sclerosis. N Engl J Med. 2017;376(22):2122-2133.
Can Gene Mutation Speed Memory Loss in Alzheimer’s Disease?
In a middle-aged cohort with Alzheimer’s disease risk, the BDNF Met allele is associated with steeper decline in episodic memory and executive function, according to a study published online ahead of print May 3 in Neurology. One thousand twenty-three adults enrolled in the Wisconsin Registry for Alzheimer’s Prevention underwent BDNF genotyping and cognitive assessment at as many as five time points. A subset of participants underwent Pittsburgh compound B scanning. Compared with BDNF Val/Val homozygotes, Met carriers had steeper decline in verbal learning and memory, and in speed and flexibility. In addition, amyloid β burden moderated the relationship between BDNF and verbal learning and memory, such that Met carriers with greater amyloid β burden showed even steeper cognitive decline.
Boots EA, Schultz SA, Clark LR, et al. BDNF Val66Met predicts cognitive decline in the Wisconsin Registry for Alzheimer’s Prevention. Neurology. 2017 May 3 [Epub ahead of print].
Support From Children Reduces Risk of Dementia
Positive social support from children is associated with reduced risk of dementia, whereas negative social support from children and other immediate family increases the risk, according to a study published in the Journal of Alzheimer’s Disease. Researchers analyzed 10-year follow-up data in 10,055 cognitively normal participants age 50 and older from the English Longitudinal Study of Aging. Incidence of dementia was identified from participant- or informant-reported physician diagnosed dementia or overall score of informant-completed IQCODE questionnaire. Positive social support from children significantly reduced the risk of dementia (hazard ratio, 0.83). Negative support from family and friends was significantly associated with increased risk of dementia. The causal mechanisms that create these associations require further research, said the researchers.
Khondoker M, Rafnsson SB, Morris S, et al. Positive and negative experiences of social support and risk of dementia in later life: an investigation using the English Longitudinal Study of Ageing. J Alzheimers Dis. 2017;58(1):99-108.
—Kimberly Williams
Device Helps Patients Move Paralyzed Hands After Stroke
Patients with stroke who learn to use their minds to open and close a device fitted over their paralyzed hands gain some control over their hands, according to a study published online ahead of print May 26 in Stroke. Ten survivors of chronic hemiparetic stroke with moderate-to-severe upper-limb motor impairment used a powered exoskeleton that opened and closed the affected hand using spectral power from EEG signals from the unaffected hemisphere associated with imagined hand movements of the paretic limb. At 12 weeks, participants had a statistically significant average increase of 6.2 points in the Action Research Arm Test. This behavioral improvement significantly correlated with improvements in brain–computer interface control. Secondary outcomes of grasp strength, Motricity Index, and the Canadian Occupational Performance Measure also significantly improved.
Bundy DT, Souders L, Baranyai K, et al. Contralesional brain-computer interface control of a powered exoskeleton for motor recovery in chronic stroke survivors. Stroke. 2017 May 26 [Epub ahead of print].
Pyrimethamine Lowers Levels of ALS Biomarker
Pyrimethamine is safe and well tolerated in amyotrophic lateral sclerosis (ALS), according to a study published online ahead of print May 8 in Annals of Neurology. Participants underwent a multicenter, open-label, nine-month dose-ranging study to determine the safety and efficacy of pyrimethamine to lower SOD1 levels in the CSF in patients with SOD1 mutations linked to familial ALS. The study included 32 patients with various SOD1 genetic mutations linked to ALS. Participants had three lumbar punctures, blood studies, and a clinical assessment of strength, motor function, quality of life, and potential adverse effects. A linear mixed effects model showed a significant reduction in CSF SOD1 at visit six, with a mean reduction of 13.5%, and at visit nine, with a mean reduction of 10.5%.
Lange DJ, Shahbazi M, Silani V, et al. Pyrimethamine significantly lowers cerebrospinal fluid Cu/Zn superoxide dismutase in amyotrophic lateral sclerosis patients with SOD1 mutations. Ann Neurol. 2017 May 8 [Epub ahead of print].
Statin Use Linked to Higher Risk of Parkinson’s Disease
Statins, especially lipophilic statins, are associated with higher risk of Parkinson’s disease, according to a study published in the June issue of Movement Disorders. The association is stronger with initial use, which suggests a facilitating effect, said the investigators. Researchers performed a retrospective case–control analysis and identified 2,322 people with incident Parkinson’s disease who had been enrolled in a claims database for at least 2.5 years before diagnosis or prescription of antiparkinson medication. They matched the cases with 2,322 controls by age, gender, and a follow-up window. Statin use was significantly associated with Parkinson’s disease risk. The strongest associations were for lipophilic statins (odds ratio [OR], 1.58) versus hydrophilic statins (OR, 1.19), statins plus nonstatins (OR, 1.95), and for the initial period after starting statins.
Liu G, Sterling NW, Kong L, et al. Statins may facilitate Parkinson’s disease: insight gained from a large, national claims database. Mov Disord. 2017;32(6):913-917.
Is Moderate Drinking Associated With Cognitive Decline?
Moderate alcohol consumption is associated with adverse brain outcomes, including hippocampal atrophy, according to a study published online ahead of print June 6 in BMJ. The study included 550 men and women with a mean age of 43 at study baseline. No patient had alcohol dependence, and all underwent brain MRI at follow-up. Higher alcohol consumption over the 30-year follow-up was associated with increased odds of hippocampal atrophy in a dose-dependent fashion. People consuming more than 30 units/week of alcohol were at the highest risk, compared with abstainers. People who drank moderately had three times the odds of right-sided hippocampal atrophy. There was no protective effect of light drinking over abstinence. Higher alcohol use also was associated with differences in corpus callosum microstructure and faster decline in lexical fluency.
Topiwala A, Allan CL, Valkanova V, et al. Moderate alcohol consumption as risk factor for adverse brain outcomes and cognitive decline: longitudinal cohort study. BMJ. 2017 Jun 6 [Epub ahead of print].
Consuming Low-Fat Dairy May Increase Risk for Parkinson’s Disease
Frequently consuming low-fat dairy products may be associated with an increased risk of Parkinson’s disease, according to a study published online ahead of print June 8 in Neurology. This study is based on data from 80,736 participants in the Nurses’ Health Study and 48,610 participants in the Health Professionals Follow-Up Study, with 26 and 24 years of follow-up, respectively. Both US-based studies were conducted through mailed biennial questionnaires. Dietary intake was assessed with food frequency questionnaires administered repeatedly over the follow-up period. Total dairy intake was not significantly associated with Parkinson’s disease risk, but intake of low-fat dairy foods was associated with Parkinson’s disease risk. This association appeared to result from an increased risk of Parkinson’s disease associated with skim and low-fat milk.
Hughes KC, Gao X, Kim IY, et al. Intake of dairy foods and risk of Parkinson disease. Neurology. 2017 Jun 8 [Epub ahead of print].
Elevated Brain Amyloid Increases Likelihood of Cognitive Decline
Elevated baseline brain amyloid level, compared with normal brain amyloid level, is associated with higher likelihood of cognitive decline, according to a study published June 13 in JAMA. Exploratory analyses were conducted with longitudinal cognitive and biomarker data from 445 cognitively normal people. Participants were classified at baseline as having normal or elevated brain amyloid using PET amyloid imaging or a CSF assay of amyloid β. Outcomes included scores on the Preclinical Alzheimer Cognitive Composite (PACC), Mini-Mental State Examination (MMSE), Clinical Dementia Rating Sum of Boxes (CDR-SOB), and Logical Memory Delayed Recall. Compared with the group with normal amyloid, people with elevated amyloid had worse mean scores at four years on the PACC, MMSE, and CDR-SOB. For Logical Memory Delayed Recall, between-group scores were not significantly different at four years.
Donohue MC, Sperling RA, Petersen R, et al. Association between elevated brain amyloid and subsequent cognitive decline among cognitively normal persons. JAMA. 2017;317(22):2305-2316.
Seven Risk Genes for Insomnia Found
Researchers have found seven risk genes for insomnia, according to a study published online ahead of print June 12 in Nature Genetics. To identify genetic factors for insomnia complaints, investigators performed a genome-wide association study and a genome-wide gene-based association study in 113,006 participants. The authors identified three loci and seven genes, including MEIS1,
Hammerschlag AR, Stringer S, de Leeuw CA, et al. Genome-wide association analysis of insomnia complaints identifies risk genes and genetic overlap with psychiatric and metabolic traits. Nat Genet. 2017 Jun 12 [Epub ahead of print].
Is Telemedicine for Headache as Effective as In-Person Visit?
In people with headache, a video consultation with a neurologist for treatment may be as effective as an in-person visit, according to a study published online ahead of print June 14 in Neurology. Researchers randomized, allocated, and consulted patients with nonacute headache via telemedicine or in a traditional manner in a noninferiority trial. Efficacy end points assessed by questionnaires at three and 12 months included change from baseline in Headache Impact Test-6 (HIT-6) and pain intensity. The primary safety end point was presence of secondary headache within 12 months after consultation. There were no differences between telemedicine and traditional consultations in HIT-6 or pain intensity over three periods. The absolute difference in HIT-6 from baseline was 0.3 at three months and 0.2 at 12 months.
Müller KI, Alstadhaug KB, Bekkelund SI. A randomized trial of telemedicine efficacy and safety for nonacute headaches. Neurology. 2017 Jun 14 [Epub ahead of print].
Minocycline Reduces Risk of Conversion From CIS to MS
The risk of conversion from clinically isolated syndrome (CIS) to multiple sclerosis (MS) is significantly lower with minocycline than with placebo over six months, but not over 24 months, according to a study published June 1 in the New England Journal of Medicine. This study included 142 participants who had had their first demyelinating symptoms within the previous 180 days. At 12 Canadian MS clinics, researchers randomly assigned participants to receive either 100 mg of minocycline, administered orally twice daily, or placebo. Administration of minocycline or placebo was continued until a diagnosis of MS was established or until 24 months after randomization. The unadjusted risk of conversion to MS within six months after randomization was 61.0% in the placebo group and 33.4% in the minocycline group.
Metz LM, Li DKB, Traboulsee AL, et al. Trial of minocycline in a clinically isolated syndrome of multiple sclerosis. N Engl J Med. 2017;376(22):2122-2133.
Can Gene Mutation Speed Memory Loss in Alzheimer’s Disease?
In a middle-aged cohort with Alzheimer’s disease risk, the BDNF Met allele is associated with steeper decline in episodic memory and executive function, according to a study published online ahead of print May 3 in Neurology. One thousand twenty-three adults enrolled in the Wisconsin Registry for Alzheimer’s Prevention underwent BDNF genotyping and cognitive assessment at as many as five time points. A subset of participants underwent Pittsburgh compound B scanning. Compared with BDNF Val/Val homozygotes, Met carriers had steeper decline in verbal learning and memory, and in speed and flexibility. In addition, amyloid β burden moderated the relationship between BDNF and verbal learning and memory, such that Met carriers with greater amyloid β burden showed even steeper cognitive decline.
Boots EA, Schultz SA, Clark LR, et al. BDNF Val66Met predicts cognitive decline in the Wisconsin Registry for Alzheimer’s Prevention. Neurology. 2017 May 3 [Epub ahead of print].
Support From Children Reduces Risk of Dementia
Positive social support from children is associated with reduced risk of dementia, whereas negative social support from children and other immediate family increases the risk, according to a study published in the Journal of Alzheimer’s Disease. Researchers analyzed 10-year follow-up data in 10,055 cognitively normal participants age 50 and older from the English Longitudinal Study of Aging. Incidence of dementia was identified from participant- or informant-reported physician diagnosed dementia or overall score of informant-completed IQCODE questionnaire. Positive social support from children significantly reduced the risk of dementia (hazard ratio, 0.83). Negative support from family and friends was significantly associated with increased risk of dementia. The causal mechanisms that create these associations require further research, said the researchers.
Khondoker M, Rafnsson SB, Morris S, et al. Positive and negative experiences of social support and risk of dementia in later life: an investigation using the English Longitudinal Study of Ageing. J Alzheimers Dis. 2017;58(1):99-108.
—Kimberly Williams
New approval lights up gliomas to aid resection
The Food and Drug Administration has approved aminolevulinic acid hydrochloride (Gleolan) to help visualize gliomas during surgery and allow for more complete resection.
Aminolevulinic acid hydrochloride lights up the tumor so surgeons can distinguish it from healthy tissue. Patients take the drug orally – 20 mg/kg – approximately 3 hours before anesthesia. Glioma cells take it up and convert it to the fluorescent chemical protoporphyrin IX. When illuminated under blue light, protoporphyrin in the tumor glows an intense red, while normal brain tissue appears blue, enabling “the surgeon to see the tumor more clearly during brain surgery and to remove it more accurately, sparing healthy brain tissue,” according to information from NX Development Corp, which markets Gleolan.
In a phase III trial of 349 patients with suspected malignant glioma amenable to complete resection, a contrast-enhanced tumor was resected in 64% of patients in the aminolevulinic acid (ALA) arm, versus 38 % of patients in the control-group, who had conventional resection under white light (P less than .001); 20.5 % of ALA patients versus 11 % patients in the control arm were alive at 6 months without progression.
FDA officials noted that there’s a risk of false negatives and positives with ALA, and that “an increase in the extent of resection might increase the risk of serious neurologic deficits in the short term.”
Side effects in preapproval studies included fever, hypotension, nausea, and vomiting in more than 1% percent of patients within a week of surgery. Adverse events included chills, abnormal liver function tests, and diarrhea in less than 1% of patients within 6 weeks of surgery.
The Food and Drug Administration has approved aminolevulinic acid hydrochloride (Gleolan) to help visualize gliomas during surgery and allow for more complete resection.
Aminolevulinic acid hydrochloride lights up the tumor so surgeons can distinguish it from healthy tissue. Patients take the drug orally – 20 mg/kg – approximately 3 hours before anesthesia. Glioma cells take it up and convert it to the fluorescent chemical protoporphyrin IX. When illuminated under blue light, protoporphyrin in the tumor glows an intense red, while normal brain tissue appears blue, enabling “the surgeon to see the tumor more clearly during brain surgery and to remove it more accurately, sparing healthy brain tissue,” according to information from NX Development Corp, which markets Gleolan.
In a phase III trial of 349 patients with suspected malignant glioma amenable to complete resection, a contrast-enhanced tumor was resected in 64% of patients in the aminolevulinic acid (ALA) arm, versus 38 % of patients in the control-group, who had conventional resection under white light (P less than .001); 20.5 % of ALA patients versus 11 % patients in the control arm were alive at 6 months without progression.
FDA officials noted that there’s a risk of false negatives and positives with ALA, and that “an increase in the extent of resection might increase the risk of serious neurologic deficits in the short term.”
Side effects in preapproval studies included fever, hypotension, nausea, and vomiting in more than 1% percent of patients within a week of surgery. Adverse events included chills, abnormal liver function tests, and diarrhea in less than 1% of patients within 6 weeks of surgery.
The Food and Drug Administration has approved aminolevulinic acid hydrochloride (Gleolan) to help visualize gliomas during surgery and allow for more complete resection.
Aminolevulinic acid hydrochloride lights up the tumor so surgeons can distinguish it from healthy tissue. Patients take the drug orally – 20 mg/kg – approximately 3 hours before anesthesia. Glioma cells take it up and convert it to the fluorescent chemical protoporphyrin IX. When illuminated under blue light, protoporphyrin in the tumor glows an intense red, while normal brain tissue appears blue, enabling “the surgeon to see the tumor more clearly during brain surgery and to remove it more accurately, sparing healthy brain tissue,” according to information from NX Development Corp, which markets Gleolan.
In a phase III trial of 349 patients with suspected malignant glioma amenable to complete resection, a contrast-enhanced tumor was resected in 64% of patients in the aminolevulinic acid (ALA) arm, versus 38 % of patients in the control-group, who had conventional resection under white light (P less than .001); 20.5 % of ALA patients versus 11 % patients in the control arm were alive at 6 months without progression.
FDA officials noted that there’s a risk of false negatives and positives with ALA, and that “an increase in the extent of resection might increase the risk of serious neurologic deficits in the short term.”
Side effects in preapproval studies included fever, hypotension, nausea, and vomiting in more than 1% percent of patients within a week of surgery. Adverse events included chills, abnormal liver function tests, and diarrhea in less than 1% of patients within 6 weeks of surgery.
New and Noteworthy Information—June 2017
Can Biomarkers Predict Cognitive Deficits in Parkinson’s Disease?
Biomarkers may predict which patients with Parkinson’s disease will have significant cognitive deficits within the first three years after diagnosis, according to a study published May 17 in PLOS One. Researchers conducted an international, prospective study of 423 newly diagnosed and untreated patients with Parkinson’s disease with no signs of cognitive impairment at the time of enrollment in 2010. Investigators conducted brain scans, genetic tests, and analyses of CSF at baseline and during follow-up. At three years, between 15% and 38% of participants had developed cognitive impairment. Brain scans identified dopamine deficiency and decreased brain volume as predictors of cognitive decline. Low CSF beta-amyloid level and single-nucleotide polymorphisms (SNPs) in COMT and BDNF also predicted cognitive decline. These SNPs previously had been associated with cognitive impairment.
Caspell-Garcia C, Simuni T, Tosun-Turgut D, et al. Multiple modality biomarker prediction of cognitive impairment in prospectively followed de novo Parkinson disease. PLoS One. 2017 May 17;12(5):e0175674.
Service Members With Concussive Blast TBI Have Worsening Outcomes
Military service members with concussive blast traumatic brain injury (TBI) have considerable decline in clinical outcomes over five years, according to a study published online ahead of print May 1 in JAMA Neurology. This prospective longitudinal study enrolled active-duty US military after concussive blast injury in the acute to subacute stage and combat-deployed control individuals in Afghanistan or after medical evacuation to Germany from November 1, 2008, through July 1, 2013. Physicians in the United States performed one- and five-year clinical evaluations. Among the 94 participants, global disability, satisfaction with life, neurobehavioral symptom severity, psychiatric symptom severity, and sleep impairment were significantly worse in patients with concussive blast TBI, compared with combat-deployed controls, whereas performance on cognitive measures was no different between groups at the five-year evaluation.
Mac Donald CL, Barber J, Jordan M, et al. Early clinical predictors of 5-year outcome after concussive blast traumatic brain injury. JAMA Neurol. 2017 May 1 [Epub ahead of print].
Biomarker Linked to Increased Risk of Ischemic Stroke in Women
High levels of β2-microglobulin are associated with an increased risk of ischemic stroke among women, according to a study published online ahead of print May 10 in Neurology. Researchers performed a nested case–control study among women enrolled in the Nurses’ Health Study who provided blood samples between 1989 and 1990 and were free of prior stroke and cancer. Investigators measured β2-microglobulin levels in 473 ischemic stroke cases and 473 controls matched on age, race, and other variables. Median levels of β2-microglobulin were 1.86 mg/L in cases and 1.80 mg/L in controls. Women in the highest β2-microglobulin quartile had a multivariable-adjusted increased risk of ischemic stroke, compared with women in the lowest quartile (odds ratio, 1.56). Results were similar when restricted to those without chronic kidney disease.
Rist PM, Jiménez MC, Rexrode KM. Prospective association between β2-microglobulin levels and ischemic stroke risk among women. Neurology. 2017 May 10 [Epub ahead of print].
Female Hormones May Cause Headache in Girls With Migraine
Age and pubertal development could moderate the effect of ovarian hormones on days of headache onset in girls with migraine, according to a study published online ahead of print May 8 in Cephalalgia. The study included 34 girls with migraine grouped into three age strata (ie, prepubertal, pubertal, and postpubertal). Participants collected daily urine samples and recorded the occurrence and severity of headache in a daily diary. Urine samples were assayed for estrone glucuronide and pregnandiol glucuronide, and the daily change in each was calculated. The primary outcome measures were headache onset days and headache severity. Models of headache onset days demonstrated a significant interaction between age and pregnandiol glucuronide. Change in pregnandiol glucuronide was associated with headache severity.
Martin VT, Allen JR, Houle TT, et al. Ovarian hormones, age and pubertal development and their association with days of headache onset in girls with migraine: an observational cohort study. Cephalalgia. 2017 Jan 1 [Epub ahead of print].
PTSD Is Associated With Risk for Dementia Diagnosis
Posttraumatic stress disorder (PTSD) diagnosis is associated with an increased risk for dementia diagnosis that varies with psychotropic medication, according to a study published in the May issue of the Journal of the American Geriatrics Society. Researchers examined information from 417,172 veterans age 56 and older without dementia or mild cognitive impairment. During the study’s nine-year follow-up period, participants had a clinical encounter every two years. PTSD diagnosis significantly increased the risk for dementia diagnosis. The hazard ratio for dementia diagnosis among veterans diagnosed with PTSD who did not use psychotropic medications was 1.55. Among veterans diagnosed with PTSD and prescribed psychotropic medication, the hazard ratio for dementia diagnosis ranged from 1.99 for SSRIs to 4.21 for atypical antipsychotics.
Mawanda F, Wallace RB, McCoy K, Abrams TE. PTSD, psychotropic medication use, and the risk of dementia among US veterans: a retrospective cohort study. J Am Geriatr Soc. 2017;65(5):1043-1050.
Screening for Atrial Fibrillation Recommended
Screening for asymptomatic atrial fibrillation in people age 65 and older and treating it with anticoagulant medications could greatly reduce the risk of stroke and premature death, according to the AF-SCREEN International Collaboration report published May 9 in Circulation. In 2016, 60 members of the collaboration, including physicians, nurses, allied health professionals, health economists, and patient advocates, were invited to prepare a draft document. They concluded that screen-detected atrial fibrillation found at a single timepoint or by intermittent ECG recordings over two weeks is not a benign condition and, with additional stroke factors, carries sufficient risk of stroke to justify consideration of anticoagulation. Handheld ECG devices are preferred as screening tools because they provide a verifiable ECG trace that guidelines require for diagnosis, said the authors.
Freedman B, Camm J, Calkins H, et al. Screening for atrial fibrillation: a report of the AF-SCREEN international collaboration. Circulation. 2017;135(19):1851-1867.
Can Music Reduce Depressive Symptoms in Dementia?
Providing people with dementia with at least five sessions of a music-based therapeutic intervention probably reduces depressive symptoms, but has little or no effect on agitation or aggression, according to a study published online ahead of print May 2 in the Cochrane Database of Systematic Reviews. Researchers searched ALOIS on April 14, 2010, using the terms “music therapy,” “music,” “singing,” “sing,” and “auditory stimulation.” Sixteen studies with a total of 620 participants contributed data to meta-analyses. Participants in the studies had dementia of varying severity. The investigators found that music-based therapeutic interventions may have little or no effect on emotional well-being and quality of life, overall behavior problems, and cognition. Study authors also found moderate-quality evidence that these interventions reduce depressive symptoms, but do not decrease agitation or aggression.
van der Steen JT, van Soest-Poortvliet MC, van der Wouden JC, et al. Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev. 2017 May 2 [Epub ahead of print].
FDA Approves Radicava for Treatment of ALS
The FDA has approved Radicava (edaravone) as an IV treatment for amyotrophic lateral sclerosis (ALS). A phase III study evaluated the efficacy and safety of Radicava, compared with placebo, in 137 people with ALS. After a 12-week preobservation period, eligible patients were randomized 1:1 to receive 60 mg of Radicava in an IV for 60 minutes or placebo during a six-month double-blind phase. People given Radicava showed significantly less decline in physical function, compared with controls, as measured by the ALS Functional Rating Scale-Revised. The most common adverse reactions that occurred in greater than 10% of patients and greater than placebo were bruising, walking difficulties, and headache. Radicava is administered in 28-day cycles. MT Pharma America, headquartered in Jersey City, New Jersey, markets Radicava.
Can Cooling the Body Reduce Brain Injury?
Cooling the body may reduce brain injury for people in a coma after being revived from cardiac arrest, according to a guideline published online ahead of print May 10 in Neurology. Researchers reviewed evidence from studies of methods to reduce brain injury in people who are comatose after resuscitation from cardiac arrest. The guideline found that for patients who are treated with electric shocks to the heart after out-of-hospital cardiac arrest and who are in a coma, cooling the body to 89.6 to 93.2 °F for 24 hours effectively improves the chance of recovering brain function. The authors also found that keeping the body cooled to 96.8 °F for 24 hours, followed by rewarming to 99.5 °F over eight hours, effectively reduces brain injury after cardiac arrest.
Geocadin RG, Wijdicks E, Armstrong MJ, et al. Practice guideline summary: reducing brain injury following cardiopulmonary resuscitation: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2017 May 10 [Epub ahead of print].
Granger Causality Analysis Can Localize Ictal Networks
Granger causality analysis has the potential to help localize ictal networks from interictal data, according to a study published online ahead of print May 2 in Neurosurgery. For this study, 20-minute interictal baselines were obtained from 25 patients with hard-to-treat epilepsy who previously had had long-term EEG monitoring. The Granger causality maps were quantitatively compared with conventionally constructed surgical plans by using rank order and Cartesian distance statistics. In 16 of 25 participants, the interictal Granger causality rankings of the electrodes in the ictally active electrode set were lower than predicted by chance. The Granger causality maps thus likely correlated with ictal networks. The distance from the highest Granger causality electrode to the ictally active electrode set and to the resection averaged 6 and 4 mm, respectively.
Park EH, Madsen JR. Granger causality analysis of interictal iEEG predicts seizure focus and ultimate resection. Neurosurgery. 2017 May 2 [Epub ahead of print].
Tourette Disorder Risk Genes Identified
Researchers have identified the first risk gene for Tourette disorder and three other probable risk genes, according to a study published May 3 in Neuron. Researchers analyzed genomic data from 311 trios of children with Tourette disorder and their parents. Data were collected by the Tourette International Collaborative Genetics group. The authors found strong evidence that variants of WWC1 can play a significant role in triggering the disorder. Investigators conducted a replication study in 173 trios and found the same results. Extrapolating from the number of de novo variants, investigators estimated that approximately 12% of Tourette disorder cases are likely to involve de novo variants. The genes CELSR3, NIPBL, and FN1 were identified as having at least 70% probability of contributing to Tourette disorder.
Willsey AJ, Fernandez TV, Yu D, et al. De novo coding variants are strongly associated with Tourette disorder. Neuron. 2017;94(3):486-499.
—Kimberly Williams
Can Biomarkers Predict Cognitive Deficits in Parkinson’s Disease?
Biomarkers may predict which patients with Parkinson’s disease will have significant cognitive deficits within the first three years after diagnosis, according to a study published May 17 in PLOS One. Researchers conducted an international, prospective study of 423 newly diagnosed and untreated patients with Parkinson’s disease with no signs of cognitive impairment at the time of enrollment in 2010. Investigators conducted brain scans, genetic tests, and analyses of CSF at baseline and during follow-up. At three years, between 15% and 38% of participants had developed cognitive impairment. Brain scans identified dopamine deficiency and decreased brain volume as predictors of cognitive decline. Low CSF beta-amyloid level and single-nucleotide polymorphisms (SNPs) in COMT and BDNF also predicted cognitive decline. These SNPs previously had been associated with cognitive impairment.
Caspell-Garcia C, Simuni T, Tosun-Turgut D, et al. Multiple modality biomarker prediction of cognitive impairment in prospectively followed de novo Parkinson disease. PLoS One. 2017 May 17;12(5):e0175674.
Service Members With Concussive Blast TBI Have Worsening Outcomes
Military service members with concussive blast traumatic brain injury (TBI) have considerable decline in clinical outcomes over five years, according to a study published online ahead of print May 1 in JAMA Neurology. This prospective longitudinal study enrolled active-duty US military after concussive blast injury in the acute to subacute stage and combat-deployed control individuals in Afghanistan or after medical evacuation to Germany from November 1, 2008, through July 1, 2013. Physicians in the United States performed one- and five-year clinical evaluations. Among the 94 participants, global disability, satisfaction with life, neurobehavioral symptom severity, psychiatric symptom severity, and sleep impairment were significantly worse in patients with concussive blast TBI, compared with combat-deployed controls, whereas performance on cognitive measures was no different between groups at the five-year evaluation.
Mac Donald CL, Barber J, Jordan M, et al. Early clinical predictors of 5-year outcome after concussive blast traumatic brain injury. JAMA Neurol. 2017 May 1 [Epub ahead of print].
Biomarker Linked to Increased Risk of Ischemic Stroke in Women
High levels of β2-microglobulin are associated with an increased risk of ischemic stroke among women, according to a study published online ahead of print May 10 in Neurology. Researchers performed a nested case–control study among women enrolled in the Nurses’ Health Study who provided blood samples between 1989 and 1990 and were free of prior stroke and cancer. Investigators measured β2-microglobulin levels in 473 ischemic stroke cases and 473 controls matched on age, race, and other variables. Median levels of β2-microglobulin were 1.86 mg/L in cases and 1.80 mg/L in controls. Women in the highest β2-microglobulin quartile had a multivariable-adjusted increased risk of ischemic stroke, compared with women in the lowest quartile (odds ratio, 1.56). Results were similar when restricted to those without chronic kidney disease.
Rist PM, Jiménez MC, Rexrode KM. Prospective association between β2-microglobulin levels and ischemic stroke risk among women. Neurology. 2017 May 10 [Epub ahead of print].
Female Hormones May Cause Headache in Girls With Migraine
Age and pubertal development could moderate the effect of ovarian hormones on days of headache onset in girls with migraine, according to a study published online ahead of print May 8 in Cephalalgia. The study included 34 girls with migraine grouped into three age strata (ie, prepubertal, pubertal, and postpubertal). Participants collected daily urine samples and recorded the occurrence and severity of headache in a daily diary. Urine samples were assayed for estrone glucuronide and pregnandiol glucuronide, and the daily change in each was calculated. The primary outcome measures were headache onset days and headache severity. Models of headache onset days demonstrated a significant interaction between age and pregnandiol glucuronide. Change in pregnandiol glucuronide was associated with headache severity.
Martin VT, Allen JR, Houle TT, et al. Ovarian hormones, age and pubertal development and their association with days of headache onset in girls with migraine: an observational cohort study. Cephalalgia. 2017 Jan 1 [Epub ahead of print].
PTSD Is Associated With Risk for Dementia Diagnosis
Posttraumatic stress disorder (PTSD) diagnosis is associated with an increased risk for dementia diagnosis that varies with psychotropic medication, according to a study published in the May issue of the Journal of the American Geriatrics Society. Researchers examined information from 417,172 veterans age 56 and older without dementia or mild cognitive impairment. During the study’s nine-year follow-up period, participants had a clinical encounter every two years. PTSD diagnosis significantly increased the risk for dementia diagnosis. The hazard ratio for dementia diagnosis among veterans diagnosed with PTSD who did not use psychotropic medications was 1.55. Among veterans diagnosed with PTSD and prescribed psychotropic medication, the hazard ratio for dementia diagnosis ranged from 1.99 for SSRIs to 4.21 for atypical antipsychotics.
Mawanda F, Wallace RB, McCoy K, Abrams TE. PTSD, psychotropic medication use, and the risk of dementia among US veterans: a retrospective cohort study. J Am Geriatr Soc. 2017;65(5):1043-1050.
Screening for Atrial Fibrillation Recommended
Screening for asymptomatic atrial fibrillation in people age 65 and older and treating it with anticoagulant medications could greatly reduce the risk of stroke and premature death, according to the AF-SCREEN International Collaboration report published May 9 in Circulation. In 2016, 60 members of the collaboration, including physicians, nurses, allied health professionals, health economists, and patient advocates, were invited to prepare a draft document. They concluded that screen-detected atrial fibrillation found at a single timepoint or by intermittent ECG recordings over two weeks is not a benign condition and, with additional stroke factors, carries sufficient risk of stroke to justify consideration of anticoagulation. Handheld ECG devices are preferred as screening tools because they provide a verifiable ECG trace that guidelines require for diagnosis, said the authors.
Freedman B, Camm J, Calkins H, et al. Screening for atrial fibrillation: a report of the AF-SCREEN international collaboration. Circulation. 2017;135(19):1851-1867.
Can Music Reduce Depressive Symptoms in Dementia?
Providing people with dementia with at least five sessions of a music-based therapeutic intervention probably reduces depressive symptoms, but has little or no effect on agitation or aggression, according to a study published online ahead of print May 2 in the Cochrane Database of Systematic Reviews. Researchers searched ALOIS on April 14, 2010, using the terms “music therapy,” “music,” “singing,” “sing,” and “auditory stimulation.” Sixteen studies with a total of 620 participants contributed data to meta-analyses. Participants in the studies had dementia of varying severity. The investigators found that music-based therapeutic interventions may have little or no effect on emotional well-being and quality of life, overall behavior problems, and cognition. Study authors also found moderate-quality evidence that these interventions reduce depressive symptoms, but do not decrease agitation or aggression.
van der Steen JT, van Soest-Poortvliet MC, van der Wouden JC, et al. Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev. 2017 May 2 [Epub ahead of print].
FDA Approves Radicava for Treatment of ALS
The FDA has approved Radicava (edaravone) as an IV treatment for amyotrophic lateral sclerosis (ALS). A phase III study evaluated the efficacy and safety of Radicava, compared with placebo, in 137 people with ALS. After a 12-week preobservation period, eligible patients were randomized 1:1 to receive 60 mg of Radicava in an IV for 60 minutes or placebo during a six-month double-blind phase. People given Radicava showed significantly less decline in physical function, compared with controls, as measured by the ALS Functional Rating Scale-Revised. The most common adverse reactions that occurred in greater than 10% of patients and greater than placebo were bruising, walking difficulties, and headache. Radicava is administered in 28-day cycles. MT Pharma America, headquartered in Jersey City, New Jersey, markets Radicava.
Can Cooling the Body Reduce Brain Injury?
Cooling the body may reduce brain injury for people in a coma after being revived from cardiac arrest, according to a guideline published online ahead of print May 10 in Neurology. Researchers reviewed evidence from studies of methods to reduce brain injury in people who are comatose after resuscitation from cardiac arrest. The guideline found that for patients who are treated with electric shocks to the heart after out-of-hospital cardiac arrest and who are in a coma, cooling the body to 89.6 to 93.2 °F for 24 hours effectively improves the chance of recovering brain function. The authors also found that keeping the body cooled to 96.8 °F for 24 hours, followed by rewarming to 99.5 °F over eight hours, effectively reduces brain injury after cardiac arrest.
Geocadin RG, Wijdicks E, Armstrong MJ, et al. Practice guideline summary: reducing brain injury following cardiopulmonary resuscitation: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2017 May 10 [Epub ahead of print].
Granger Causality Analysis Can Localize Ictal Networks
Granger causality analysis has the potential to help localize ictal networks from interictal data, according to a study published online ahead of print May 2 in Neurosurgery. For this study, 20-minute interictal baselines were obtained from 25 patients with hard-to-treat epilepsy who previously had had long-term EEG monitoring. The Granger causality maps were quantitatively compared with conventionally constructed surgical plans by using rank order and Cartesian distance statistics. In 16 of 25 participants, the interictal Granger causality rankings of the electrodes in the ictally active electrode set were lower than predicted by chance. The Granger causality maps thus likely correlated with ictal networks. The distance from the highest Granger causality electrode to the ictally active electrode set and to the resection averaged 6 and 4 mm, respectively.
Park EH, Madsen JR. Granger causality analysis of interictal iEEG predicts seizure focus and ultimate resection. Neurosurgery. 2017 May 2 [Epub ahead of print].
Tourette Disorder Risk Genes Identified
Researchers have identified the first risk gene for Tourette disorder and three other probable risk genes, according to a study published May 3 in Neuron. Researchers analyzed genomic data from 311 trios of children with Tourette disorder and their parents. Data were collected by the Tourette International Collaborative Genetics group. The authors found strong evidence that variants of WWC1 can play a significant role in triggering the disorder. Investigators conducted a replication study in 173 trios and found the same results. Extrapolating from the number of de novo variants, investigators estimated that approximately 12% of Tourette disorder cases are likely to involve de novo variants. The genes CELSR3, NIPBL, and FN1 were identified as having at least 70% probability of contributing to Tourette disorder.
Willsey AJ, Fernandez TV, Yu D, et al. De novo coding variants are strongly associated with Tourette disorder. Neuron. 2017;94(3):486-499.
—Kimberly Williams
Can Biomarkers Predict Cognitive Deficits in Parkinson’s Disease?
Biomarkers may predict which patients with Parkinson’s disease will have significant cognitive deficits within the first three years after diagnosis, according to a study published May 17 in PLOS One. Researchers conducted an international, prospective study of 423 newly diagnosed and untreated patients with Parkinson’s disease with no signs of cognitive impairment at the time of enrollment in 2010. Investigators conducted brain scans, genetic tests, and analyses of CSF at baseline and during follow-up. At three years, between 15% and 38% of participants had developed cognitive impairment. Brain scans identified dopamine deficiency and decreased brain volume as predictors of cognitive decline. Low CSF beta-amyloid level and single-nucleotide polymorphisms (SNPs) in COMT and BDNF also predicted cognitive decline. These SNPs previously had been associated with cognitive impairment.
Caspell-Garcia C, Simuni T, Tosun-Turgut D, et al. Multiple modality biomarker prediction of cognitive impairment in prospectively followed de novo Parkinson disease. PLoS One. 2017 May 17;12(5):e0175674.
Service Members With Concussive Blast TBI Have Worsening Outcomes
Military service members with concussive blast traumatic brain injury (TBI) have considerable decline in clinical outcomes over five years, according to a study published online ahead of print May 1 in JAMA Neurology. This prospective longitudinal study enrolled active-duty US military after concussive blast injury in the acute to subacute stage and combat-deployed control individuals in Afghanistan or after medical evacuation to Germany from November 1, 2008, through July 1, 2013. Physicians in the United States performed one- and five-year clinical evaluations. Among the 94 participants, global disability, satisfaction with life, neurobehavioral symptom severity, psychiatric symptom severity, and sleep impairment were significantly worse in patients with concussive blast TBI, compared with combat-deployed controls, whereas performance on cognitive measures was no different between groups at the five-year evaluation.
Mac Donald CL, Barber J, Jordan M, et al. Early clinical predictors of 5-year outcome after concussive blast traumatic brain injury. JAMA Neurol. 2017 May 1 [Epub ahead of print].
Biomarker Linked to Increased Risk of Ischemic Stroke in Women
High levels of β2-microglobulin are associated with an increased risk of ischemic stroke among women, according to a study published online ahead of print May 10 in Neurology. Researchers performed a nested case–control study among women enrolled in the Nurses’ Health Study who provided blood samples between 1989 and 1990 and were free of prior stroke and cancer. Investigators measured β2-microglobulin levels in 473 ischemic stroke cases and 473 controls matched on age, race, and other variables. Median levels of β2-microglobulin were 1.86 mg/L in cases and 1.80 mg/L in controls. Women in the highest β2-microglobulin quartile had a multivariable-adjusted increased risk of ischemic stroke, compared with women in the lowest quartile (odds ratio, 1.56). Results were similar when restricted to those without chronic kidney disease.
Rist PM, Jiménez MC, Rexrode KM. Prospective association between β2-microglobulin levels and ischemic stroke risk among women. Neurology. 2017 May 10 [Epub ahead of print].
Female Hormones May Cause Headache in Girls With Migraine
Age and pubertal development could moderate the effect of ovarian hormones on days of headache onset in girls with migraine, according to a study published online ahead of print May 8 in Cephalalgia. The study included 34 girls with migraine grouped into three age strata (ie, prepubertal, pubertal, and postpubertal). Participants collected daily urine samples and recorded the occurrence and severity of headache in a daily diary. Urine samples were assayed for estrone glucuronide and pregnandiol glucuronide, and the daily change in each was calculated. The primary outcome measures were headache onset days and headache severity. Models of headache onset days demonstrated a significant interaction between age and pregnandiol glucuronide. Change in pregnandiol glucuronide was associated with headache severity.
Martin VT, Allen JR, Houle TT, et al. Ovarian hormones, age and pubertal development and their association with days of headache onset in girls with migraine: an observational cohort study. Cephalalgia. 2017 Jan 1 [Epub ahead of print].
PTSD Is Associated With Risk for Dementia Diagnosis
Posttraumatic stress disorder (PTSD) diagnosis is associated with an increased risk for dementia diagnosis that varies with psychotropic medication, according to a study published in the May issue of the Journal of the American Geriatrics Society. Researchers examined information from 417,172 veterans age 56 and older without dementia or mild cognitive impairment. During the study’s nine-year follow-up period, participants had a clinical encounter every two years. PTSD diagnosis significantly increased the risk for dementia diagnosis. The hazard ratio for dementia diagnosis among veterans diagnosed with PTSD who did not use psychotropic medications was 1.55. Among veterans diagnosed with PTSD and prescribed psychotropic medication, the hazard ratio for dementia diagnosis ranged from 1.99 for SSRIs to 4.21 for atypical antipsychotics.
Mawanda F, Wallace RB, McCoy K, Abrams TE. PTSD, psychotropic medication use, and the risk of dementia among US veterans: a retrospective cohort study. J Am Geriatr Soc. 2017;65(5):1043-1050.
Screening for Atrial Fibrillation Recommended
Screening for asymptomatic atrial fibrillation in people age 65 and older and treating it with anticoagulant medications could greatly reduce the risk of stroke and premature death, according to the AF-SCREEN International Collaboration report published May 9 in Circulation. In 2016, 60 members of the collaboration, including physicians, nurses, allied health professionals, health economists, and patient advocates, were invited to prepare a draft document. They concluded that screen-detected atrial fibrillation found at a single timepoint or by intermittent ECG recordings over two weeks is not a benign condition and, with additional stroke factors, carries sufficient risk of stroke to justify consideration of anticoagulation. Handheld ECG devices are preferred as screening tools because they provide a verifiable ECG trace that guidelines require for diagnosis, said the authors.
Freedman B, Camm J, Calkins H, et al. Screening for atrial fibrillation: a report of the AF-SCREEN international collaboration. Circulation. 2017;135(19):1851-1867.
Can Music Reduce Depressive Symptoms in Dementia?
Providing people with dementia with at least five sessions of a music-based therapeutic intervention probably reduces depressive symptoms, but has little or no effect on agitation or aggression, according to a study published online ahead of print May 2 in the Cochrane Database of Systematic Reviews. Researchers searched ALOIS on April 14, 2010, using the terms “music therapy,” “music,” “singing,” “sing,” and “auditory stimulation.” Sixteen studies with a total of 620 participants contributed data to meta-analyses. Participants in the studies had dementia of varying severity. The investigators found that music-based therapeutic interventions may have little or no effect on emotional well-being and quality of life, overall behavior problems, and cognition. Study authors also found moderate-quality evidence that these interventions reduce depressive symptoms, but do not decrease agitation or aggression.
van der Steen JT, van Soest-Poortvliet MC, van der Wouden JC, et al. Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev. 2017 May 2 [Epub ahead of print].
FDA Approves Radicava for Treatment of ALS
The FDA has approved Radicava (edaravone) as an IV treatment for amyotrophic lateral sclerosis (ALS). A phase III study evaluated the efficacy and safety of Radicava, compared with placebo, in 137 people with ALS. After a 12-week preobservation period, eligible patients were randomized 1:1 to receive 60 mg of Radicava in an IV for 60 minutes or placebo during a six-month double-blind phase. People given Radicava showed significantly less decline in physical function, compared with controls, as measured by the ALS Functional Rating Scale-Revised. The most common adverse reactions that occurred in greater than 10% of patients and greater than placebo were bruising, walking difficulties, and headache. Radicava is administered in 28-day cycles. MT Pharma America, headquartered in Jersey City, New Jersey, markets Radicava.
Can Cooling the Body Reduce Brain Injury?
Cooling the body may reduce brain injury for people in a coma after being revived from cardiac arrest, according to a guideline published online ahead of print May 10 in Neurology. Researchers reviewed evidence from studies of methods to reduce brain injury in people who are comatose after resuscitation from cardiac arrest. The guideline found that for patients who are treated with electric shocks to the heart after out-of-hospital cardiac arrest and who are in a coma, cooling the body to 89.6 to 93.2 °F for 24 hours effectively improves the chance of recovering brain function. The authors also found that keeping the body cooled to 96.8 °F for 24 hours, followed by rewarming to 99.5 °F over eight hours, effectively reduces brain injury after cardiac arrest.
Geocadin RG, Wijdicks E, Armstrong MJ, et al. Practice guideline summary: reducing brain injury following cardiopulmonary resuscitation: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2017 May 10 [Epub ahead of print].
Granger Causality Analysis Can Localize Ictal Networks
Granger causality analysis has the potential to help localize ictal networks from interictal data, according to a study published online ahead of print May 2 in Neurosurgery. For this study, 20-minute interictal baselines were obtained from 25 patients with hard-to-treat epilepsy who previously had had long-term EEG monitoring. The Granger causality maps were quantitatively compared with conventionally constructed surgical plans by using rank order and Cartesian distance statistics. In 16 of 25 participants, the interictal Granger causality rankings of the electrodes in the ictally active electrode set were lower than predicted by chance. The Granger causality maps thus likely correlated with ictal networks. The distance from the highest Granger causality electrode to the ictally active electrode set and to the resection averaged 6 and 4 mm, respectively.
Park EH, Madsen JR. Granger causality analysis of interictal iEEG predicts seizure focus and ultimate resection. Neurosurgery. 2017 May 2 [Epub ahead of print].
Tourette Disorder Risk Genes Identified
Researchers have identified the first risk gene for Tourette disorder and three other probable risk genes, according to a study published May 3 in Neuron. Researchers analyzed genomic data from 311 trios of children with Tourette disorder and their parents. Data were collected by the Tourette International Collaborative Genetics group. The authors found strong evidence that variants of WWC1 can play a significant role in triggering the disorder. Investigators conducted a replication study in 173 trios and found the same results. Extrapolating from the number of de novo variants, investigators estimated that approximately 12% of Tourette disorder cases are likely to involve de novo variants. The genes CELSR3, NIPBL, and FN1 were identified as having at least 70% probability of contributing to Tourette disorder.
Willsey AJ, Fernandez TV, Yu D, et al. De novo coding variants are strongly associated with Tourette disorder. Neuron. 2017;94(3):486-499.
—Kimberly Williams
New and Noteworthy Information—May 2017
The Biomarkers for Infant Brain Injury Score can identify infants with acute intracranial hemorrhage, according to a study published online ahead of print April 10 in JAMA Pediatrics. Binary logistic regression was used to develop a multivariable model incorporating three serum biomarkers and one clinical variable (total hemoglobin). The Biomarkers for Infant Brain Injury Score was applied to 599 infants (mean age, 4.7 months) at increased risk for abusive head trauma. Fifty-two percent were boys, 78% were white, and 8% were Hispanic. At a cutoff of 0.182, the model was 89.3% sensitive and 48.0% specific for acute intracranial hemorrhage. Positive and negative predictive values were 21.3% and 95.6%, respectively. The model was neither sensitive nor specific for atraumatic brain abnormalities, isolated skull fractures, or chronic intracranial hemorrhage.
The FDA has approved Ocrevus (ocrelizumab), an IV infusion, to treat adults with relapsing forms of multiple sclerosis (MS) and primary progressive MS. This drug is the first to be approved by the FDA for primary progressive MS. The efficacy of Ocrevus for the treatment of relapsing-remitting MS was shown in two clinical trials including 1,656 participants treated for 96 weeks. In both studies, patients receiving Ocrevus had reduced relapse rates and reduced worsening of disability, compared with patients receiving interferon beta-1a. In a study of 732 participants with primary progressive MS treated for at least 120 weeks, participants receiving Ocrevus had a longer time to the worsening of disability, compared with participants receiving placebo. Common side effects include infusion-related reactions and upper respiratory tract infection. Genentech markets Ocrevus.
Unemployed men and women and reemployed men have an increased risk of hemorrhagic and ischemic stroke and mortality, according to a study published online ahead of print April 6 in Stroke. This prospective study included 21,902 men and 19,826 women, ages 40 to 59, from nine public health centers across Japan. Participants were followed up from 1990–1993 to the end of 2009–2014. During the follow-up period, 973 incident strokes and 275 deaths from stroke occurred in men, as well as 460 strokes and 131 deaths from stroke in women. Compared with continuously employed subjects, the multivariable hazard ratio (HR) for total stroke incidence was 1.58 in unemployed men and 1.51 in unemployed women. HR for total stroke mortality was 2.22 in men and 2.48 in women.
In people with uncomplicated childhood-onset epilepsy and five-year terminal remission, young adult social outcomes are comparable to those of sibling controls, according to a study published online ahead of print April 4 in Epilepsia. Long-term social outcomes were assessed at the 15-year follow-up of the Connecticut Study of Epilepsy, which included 361 individuals with epilepsy and 173 controls. Social outcomes for cases with uncomplicated epilepsy with five or more years’ terminal remission were comparable to those of controls. Cases with uncomplicated epilepsy and less than five years of seizure freedom were more likely to be less productive and not to have a driver’s license. Complicated cases with epilepsy and less than five years of seizure freedom had worse outcomes across multiple domains, including not graduating high school.
Deep brain stimulation of the ventralis oralis internus and centromedian-parafascicular thalamus is an effective and relatively safe treatment for severe, refractory Tourette syndrome, according to a study published online ahead of print April 7 in the Journal of Neurosurgery. Researchers retrospectively reviewed outcomes in 13 patients with refractory Tourette syndrome who underwent medial thalamic deep brain stimulation for seven years. Patients were evaluated by a multidisciplinary team, and preoperative objective assessments were performed using the Yale Global Tic Severity Scale and Yale-Brown Obsessive Compulsive Scale. Patients showed an average decrease of 37% in total tic severity at their first postoperative visit. During their most recent visit, patient scores decreased from preoperative scores by an average of 50%, which was statistically significant. Device-related complications occurred in two patients, necessitating additional surgeries.
The FDA has approved Ingrezza (valbenazine) capsules for the treatment of adults with tardive dyskinesia. Ingrezza is a selective vesicular monoamine transporter 2 inhibitor. The approval of Ingrezza was based on data from the Kinect 3 study, a phase III, randomized, double-blind, placebo-controlled, parallel-group, fixed-dose study comparing once-daily Ingrezza (80 mg and 40 mg) to placebo over six weeks in patients with schizophrenia, schizoaffective disorder, or mood disorder. The mean change from baseline to week six in the AIMS dyskinesia total score was –3.2 for patients receiving 80 mg/day of Ingrezza, compared with –0.1 for controls. Ingrezza also was generally well tolerated, with somnolence as the only adverse event occurring at a rate of 5% or greater and twice the rate associated with placebo. Neurocrine Biosciences markets Ingrezza.
Benzodiazepine use is associated with an increased risk of pneumonia among patients with Alzheimer’s disease, according to a study published April 10 in CMAJ. Researchers obtained data on all community-dwelling adults with a recent diagnosis of Alzheimer disease in Finland between 2005 and 2011 from the Medication use and Alzheimer’s disease cohort. Incident users of benzodiazepines and nonbenzodiazepines were identified using a one-year washout period and matched with nonusers through propensity scores. Among 49,484 eligible participants with Alzheimer’s disease, 5,232 taking benzodiazepines and 3,269 taking nonbenzodiazepines were matched 1:1 with people not taking these drugs. Benzodiazepine and nonbenzodiazepine use was associated with a 22% increased risk of pneumonia. When analyzed separately, benzodiazepine use was significantly associated with a 28% increased risk of pneumonia, but nonbenzodiazepine use was not.
Hospitalization rates for acute ischemic stroke in young adults are increasing, along with the prevalence of traditional stroke risk factors, according to a study published online ahead of print April 10 in JAMA Neurology. Hospitalization data from the National Inpatient Sample from 1995 through 2012 were used to analyze acute stroke hospitalization rates among people ages 18 to 64. The 2003–2004 set included 362,339 hospitalizations, and the 2011–2012 set included 421,815 hospitalizations. Acute ischemic stroke hospitalization rates increased significantly for men and women, and for certain racial and ethnic groups, among younger adults ages 18 to 54. The prevalence of stroke risk factors among people hospitalized for acute ischemic stroke continued to increase from 2003–2004 through 2011–2012 for men and women ages 18 to 64.
A polygenic hazard score may help quantify individual differences in age-specific genetic risk for Alzheimer’s disease, according to a study published March 21 in PLOS Medicine. The investigators reviewed single-nucleotide polymorphisms associated with Alzheimer’s disease risk. Using a Cox proportional hazard model, they calculated polygenic hazard scores for participants in the Alzheimer’s Disease Genetics Consortium and tested them in two independent cohorts. People in the top polygenic hazard score quartile developed Alzheimer’s disease at a considerably lower age and had the highest yearly Alzheimer’s disease incidence rate. Among people who did not have the APOE ε3 allele, polygenic hazard score modified the age of expected onset by more than 10 years between the lowest and highest deciles. In independent cohorts, the polygenic hazard score strongly predicted age of Alzheimer’s disease onset.
Generalized anxiety disorder (GAD) is associated with migraine, according to a study published in the March issue of Headache. Researchers performed a secondary data analysis of the 2012 Canadian Community Health Survey-Mental Health. The first subsample included people with and without migraine. The second subsample was restricted to people with migraine. Six percent of people with migraine had had GAD in the previous year, compared with 2.1% of people without migraine. The adjusted odds of previous year GAD were 2.5 times higher among people with migraine than among people without. In the sample containing only migraineurs, the factors associated with higher odds of 12-month GAD included having a university degree, having low income, being without a confidant, and being male.
The rates of childhood epilepsy increase with maternal overweight or obesity in a dose-response manner, according to a study published online ahead of print April 3 in JAMA Neurology. Researchers conducted a population-based cohort study of 1,441,623 live single births at 22 or more gestational weeks in Sweden from January 1, 1997, to December 31, 2011. The risk of childhood epilepsy increased by maternal BMI from 6.30 per 10,000 child-years among normal-weight women to 12.4 per 10,000 child-years among women with grade III obesity. Risk of epilepsy increased by 11% in children of overweight mothers, compared with children of normal-weight mothers. Grade I obesity was associated with a 20% increased risk, grade II obesity was associated with a 30% increased risk, and grade III obesity was associated with an 82% increased risk.
The FDA has approved a label expansion for Trokendi XR (topiramate) to include migraine prophylaxis in adults and adolescents age 12 and older. Trokendi XR is a once-daily extended release formulation. The drug previously was approved as initial monotherapy and adjunctive therapy in patients age 6 and older with partial onset or primary generalized tonic-clonic seizures and as adjunctive therapy in patients age 6 and older with seizures associated with Lennox-Gastaut syndrome. Trokendi XR is available in 25-mg, 50-mg, 100-mg, and 200-mg capsules. The drug may cause sudden decrease in vision, secondary angle closure glaucoma, or decreased sweating. Approximately one in 500 people who take Trokendi XR may have suicidal thoughts. Supernus Pharmaceuticals markets Trokendi XR.
The FDA has approved Austedo (deutetrabenazine) tablets for the treatment of chorea associated with Huntington’s disease. Austedo was previously referred to by the name SD-809 and was granted Orphan Drug Designation by the FDA. Austedo is the second product approved for Huntington’s disease. The approval was based on phase III results in a randomized, double-blind, placebo-controlled, multicenter trial conducted in 90 ambulatory patients with manifest chorea associated with Huntington’s disease. Total Maximal Chorea Scores for patients receiving Austedo improved by approximately 4.4 units from baseline to the maintenance period, compared with approximately 1.9 units in the placebo group. At the week 13 follow-up visit (one week after discontinuation of the study drug), the Total Maximal Chorea Scores of patients who had received Austedo returned to baseline levels. Teva Pharmaceutical Industries markets Austedo.
—Kimberly Williams
The Biomarkers for Infant Brain Injury Score can identify infants with acute intracranial hemorrhage, according to a study published online ahead of print April 10 in JAMA Pediatrics. Binary logistic regression was used to develop a multivariable model incorporating three serum biomarkers and one clinical variable (total hemoglobin). The Biomarkers for Infant Brain Injury Score was applied to 599 infants (mean age, 4.7 months) at increased risk for abusive head trauma. Fifty-two percent were boys, 78% were white, and 8% were Hispanic. At a cutoff of 0.182, the model was 89.3% sensitive and 48.0% specific for acute intracranial hemorrhage. Positive and negative predictive values were 21.3% and 95.6%, respectively. The model was neither sensitive nor specific for atraumatic brain abnormalities, isolated skull fractures, or chronic intracranial hemorrhage.
The FDA has approved Ocrevus (ocrelizumab), an IV infusion, to treat adults with relapsing forms of multiple sclerosis (MS) and primary progressive MS. This drug is the first to be approved by the FDA for primary progressive MS. The efficacy of Ocrevus for the treatment of relapsing-remitting MS was shown in two clinical trials including 1,656 participants treated for 96 weeks. In both studies, patients receiving Ocrevus had reduced relapse rates and reduced worsening of disability, compared with patients receiving interferon beta-1a. In a study of 732 participants with primary progressive MS treated for at least 120 weeks, participants receiving Ocrevus had a longer time to the worsening of disability, compared with participants receiving placebo. Common side effects include infusion-related reactions and upper respiratory tract infection. Genentech markets Ocrevus.
Unemployed men and women and reemployed men have an increased risk of hemorrhagic and ischemic stroke and mortality, according to a study published online ahead of print April 6 in Stroke. This prospective study included 21,902 men and 19,826 women, ages 40 to 59, from nine public health centers across Japan. Participants were followed up from 1990–1993 to the end of 2009–2014. During the follow-up period, 973 incident strokes and 275 deaths from stroke occurred in men, as well as 460 strokes and 131 deaths from stroke in women. Compared with continuously employed subjects, the multivariable hazard ratio (HR) for total stroke incidence was 1.58 in unemployed men and 1.51 in unemployed women. HR for total stroke mortality was 2.22 in men and 2.48 in women.
In people with uncomplicated childhood-onset epilepsy and five-year terminal remission, young adult social outcomes are comparable to those of sibling controls, according to a study published online ahead of print April 4 in Epilepsia. Long-term social outcomes were assessed at the 15-year follow-up of the Connecticut Study of Epilepsy, which included 361 individuals with epilepsy and 173 controls. Social outcomes for cases with uncomplicated epilepsy with five or more years’ terminal remission were comparable to those of controls. Cases with uncomplicated epilepsy and less than five years of seizure freedom were more likely to be less productive and not to have a driver’s license. Complicated cases with epilepsy and less than five years of seizure freedom had worse outcomes across multiple domains, including not graduating high school.
Deep brain stimulation of the ventralis oralis internus and centromedian-parafascicular thalamus is an effective and relatively safe treatment for severe, refractory Tourette syndrome, according to a study published online ahead of print April 7 in the Journal of Neurosurgery. Researchers retrospectively reviewed outcomes in 13 patients with refractory Tourette syndrome who underwent medial thalamic deep brain stimulation for seven years. Patients were evaluated by a multidisciplinary team, and preoperative objective assessments were performed using the Yale Global Tic Severity Scale and Yale-Brown Obsessive Compulsive Scale. Patients showed an average decrease of 37% in total tic severity at their first postoperative visit. During their most recent visit, patient scores decreased from preoperative scores by an average of 50%, which was statistically significant. Device-related complications occurred in two patients, necessitating additional surgeries.
The FDA has approved Ingrezza (valbenazine) capsules for the treatment of adults with tardive dyskinesia. Ingrezza is a selective vesicular monoamine transporter 2 inhibitor. The approval of Ingrezza was based on data from the Kinect 3 study, a phase III, randomized, double-blind, placebo-controlled, parallel-group, fixed-dose study comparing once-daily Ingrezza (80 mg and 40 mg) to placebo over six weeks in patients with schizophrenia, schizoaffective disorder, or mood disorder. The mean change from baseline to week six in the AIMS dyskinesia total score was –3.2 for patients receiving 80 mg/day of Ingrezza, compared with –0.1 for controls. Ingrezza also was generally well tolerated, with somnolence as the only adverse event occurring at a rate of 5% or greater and twice the rate associated with placebo. Neurocrine Biosciences markets Ingrezza.
Benzodiazepine use is associated with an increased risk of pneumonia among patients with Alzheimer’s disease, according to a study published April 10 in CMAJ. Researchers obtained data on all community-dwelling adults with a recent diagnosis of Alzheimer disease in Finland between 2005 and 2011 from the Medication use and Alzheimer’s disease cohort. Incident users of benzodiazepines and nonbenzodiazepines were identified using a one-year washout period and matched with nonusers through propensity scores. Among 49,484 eligible participants with Alzheimer’s disease, 5,232 taking benzodiazepines and 3,269 taking nonbenzodiazepines were matched 1:1 with people not taking these drugs. Benzodiazepine and nonbenzodiazepine use was associated with a 22% increased risk of pneumonia. When analyzed separately, benzodiazepine use was significantly associated with a 28% increased risk of pneumonia, but nonbenzodiazepine use was not.
Hospitalization rates for acute ischemic stroke in young adults are increasing, along with the prevalence of traditional stroke risk factors, according to a study published online ahead of print April 10 in JAMA Neurology. Hospitalization data from the National Inpatient Sample from 1995 through 2012 were used to analyze acute stroke hospitalization rates among people ages 18 to 64. The 2003–2004 set included 362,339 hospitalizations, and the 2011–2012 set included 421,815 hospitalizations. Acute ischemic stroke hospitalization rates increased significantly for men and women, and for certain racial and ethnic groups, among younger adults ages 18 to 54. The prevalence of stroke risk factors among people hospitalized for acute ischemic stroke continued to increase from 2003–2004 through 2011–2012 for men and women ages 18 to 64.
A polygenic hazard score may help quantify individual differences in age-specific genetic risk for Alzheimer’s disease, according to a study published March 21 in PLOS Medicine. The investigators reviewed single-nucleotide polymorphisms associated with Alzheimer’s disease risk. Using a Cox proportional hazard model, they calculated polygenic hazard scores for participants in the Alzheimer’s Disease Genetics Consortium and tested them in two independent cohorts. People in the top polygenic hazard score quartile developed Alzheimer’s disease at a considerably lower age and had the highest yearly Alzheimer’s disease incidence rate. Among people who did not have the APOE ε3 allele, polygenic hazard score modified the age of expected onset by more than 10 years between the lowest and highest deciles. In independent cohorts, the polygenic hazard score strongly predicted age of Alzheimer’s disease onset.
Generalized anxiety disorder (GAD) is associated with migraine, according to a study published in the March issue of Headache. Researchers performed a secondary data analysis of the 2012 Canadian Community Health Survey-Mental Health. The first subsample included people with and without migraine. The second subsample was restricted to people with migraine. Six percent of people with migraine had had GAD in the previous year, compared with 2.1% of people without migraine. The adjusted odds of previous year GAD were 2.5 times higher among people with migraine than among people without. In the sample containing only migraineurs, the factors associated with higher odds of 12-month GAD included having a university degree, having low income, being without a confidant, and being male.
The rates of childhood epilepsy increase with maternal overweight or obesity in a dose-response manner, according to a study published online ahead of print April 3 in JAMA Neurology. Researchers conducted a population-based cohort study of 1,441,623 live single births at 22 or more gestational weeks in Sweden from January 1, 1997, to December 31, 2011. The risk of childhood epilepsy increased by maternal BMI from 6.30 per 10,000 child-years among normal-weight women to 12.4 per 10,000 child-years among women with grade III obesity. Risk of epilepsy increased by 11% in children of overweight mothers, compared with children of normal-weight mothers. Grade I obesity was associated with a 20% increased risk, grade II obesity was associated with a 30% increased risk, and grade III obesity was associated with an 82% increased risk.
The FDA has approved a label expansion for Trokendi XR (topiramate) to include migraine prophylaxis in adults and adolescents age 12 and older. Trokendi XR is a once-daily extended release formulation. The drug previously was approved as initial monotherapy and adjunctive therapy in patients age 6 and older with partial onset or primary generalized tonic-clonic seizures and as adjunctive therapy in patients age 6 and older with seizures associated with Lennox-Gastaut syndrome. Trokendi XR is available in 25-mg, 50-mg, 100-mg, and 200-mg capsules. The drug may cause sudden decrease in vision, secondary angle closure glaucoma, or decreased sweating. Approximately one in 500 people who take Trokendi XR may have suicidal thoughts. Supernus Pharmaceuticals markets Trokendi XR.
The FDA has approved Austedo (deutetrabenazine) tablets for the treatment of chorea associated with Huntington’s disease. Austedo was previously referred to by the name SD-809 and was granted Orphan Drug Designation by the FDA. Austedo is the second product approved for Huntington’s disease. The approval was based on phase III results in a randomized, double-blind, placebo-controlled, multicenter trial conducted in 90 ambulatory patients with manifest chorea associated with Huntington’s disease. Total Maximal Chorea Scores for patients receiving Austedo improved by approximately 4.4 units from baseline to the maintenance period, compared with approximately 1.9 units in the placebo group. At the week 13 follow-up visit (one week after discontinuation of the study drug), the Total Maximal Chorea Scores of patients who had received Austedo returned to baseline levels. Teva Pharmaceutical Industries markets Austedo.
—Kimberly Williams
The Biomarkers for Infant Brain Injury Score can identify infants with acute intracranial hemorrhage, according to a study published online ahead of print April 10 in JAMA Pediatrics. Binary logistic regression was used to develop a multivariable model incorporating three serum biomarkers and one clinical variable (total hemoglobin). The Biomarkers for Infant Brain Injury Score was applied to 599 infants (mean age, 4.7 months) at increased risk for abusive head trauma. Fifty-two percent were boys, 78% were white, and 8% were Hispanic. At a cutoff of 0.182, the model was 89.3% sensitive and 48.0% specific for acute intracranial hemorrhage. Positive and negative predictive values were 21.3% and 95.6%, respectively. The model was neither sensitive nor specific for atraumatic brain abnormalities, isolated skull fractures, or chronic intracranial hemorrhage.
The FDA has approved Ocrevus (ocrelizumab), an IV infusion, to treat adults with relapsing forms of multiple sclerosis (MS) and primary progressive MS. This drug is the first to be approved by the FDA for primary progressive MS. The efficacy of Ocrevus for the treatment of relapsing-remitting MS was shown in two clinical trials including 1,656 participants treated for 96 weeks. In both studies, patients receiving Ocrevus had reduced relapse rates and reduced worsening of disability, compared with patients receiving interferon beta-1a. In a study of 732 participants with primary progressive MS treated for at least 120 weeks, participants receiving Ocrevus had a longer time to the worsening of disability, compared with participants receiving placebo. Common side effects include infusion-related reactions and upper respiratory tract infection. Genentech markets Ocrevus.
Unemployed men and women and reemployed men have an increased risk of hemorrhagic and ischemic stroke and mortality, according to a study published online ahead of print April 6 in Stroke. This prospective study included 21,902 men and 19,826 women, ages 40 to 59, from nine public health centers across Japan. Participants were followed up from 1990–1993 to the end of 2009–2014. During the follow-up period, 973 incident strokes and 275 deaths from stroke occurred in men, as well as 460 strokes and 131 deaths from stroke in women. Compared with continuously employed subjects, the multivariable hazard ratio (HR) for total stroke incidence was 1.58 in unemployed men and 1.51 in unemployed women. HR for total stroke mortality was 2.22 in men and 2.48 in women.
In people with uncomplicated childhood-onset epilepsy and five-year terminal remission, young adult social outcomes are comparable to those of sibling controls, according to a study published online ahead of print April 4 in Epilepsia. Long-term social outcomes were assessed at the 15-year follow-up of the Connecticut Study of Epilepsy, which included 361 individuals with epilepsy and 173 controls. Social outcomes for cases with uncomplicated epilepsy with five or more years’ terminal remission were comparable to those of controls. Cases with uncomplicated epilepsy and less than five years of seizure freedom were more likely to be less productive and not to have a driver’s license. Complicated cases with epilepsy and less than five years of seizure freedom had worse outcomes across multiple domains, including not graduating high school.
Deep brain stimulation of the ventralis oralis internus and centromedian-parafascicular thalamus is an effective and relatively safe treatment for severe, refractory Tourette syndrome, according to a study published online ahead of print April 7 in the Journal of Neurosurgery. Researchers retrospectively reviewed outcomes in 13 patients with refractory Tourette syndrome who underwent medial thalamic deep brain stimulation for seven years. Patients were evaluated by a multidisciplinary team, and preoperative objective assessments were performed using the Yale Global Tic Severity Scale and Yale-Brown Obsessive Compulsive Scale. Patients showed an average decrease of 37% in total tic severity at their first postoperative visit. During their most recent visit, patient scores decreased from preoperative scores by an average of 50%, which was statistically significant. Device-related complications occurred in two patients, necessitating additional surgeries.
The FDA has approved Ingrezza (valbenazine) capsules for the treatment of adults with tardive dyskinesia. Ingrezza is a selective vesicular monoamine transporter 2 inhibitor. The approval of Ingrezza was based on data from the Kinect 3 study, a phase III, randomized, double-blind, placebo-controlled, parallel-group, fixed-dose study comparing once-daily Ingrezza (80 mg and 40 mg) to placebo over six weeks in patients with schizophrenia, schizoaffective disorder, or mood disorder. The mean change from baseline to week six in the AIMS dyskinesia total score was –3.2 for patients receiving 80 mg/day of Ingrezza, compared with –0.1 for controls. Ingrezza also was generally well tolerated, with somnolence as the only adverse event occurring at a rate of 5% or greater and twice the rate associated with placebo. Neurocrine Biosciences markets Ingrezza.
Benzodiazepine use is associated with an increased risk of pneumonia among patients with Alzheimer’s disease, according to a study published April 10 in CMAJ. Researchers obtained data on all community-dwelling adults with a recent diagnosis of Alzheimer disease in Finland between 2005 and 2011 from the Medication use and Alzheimer’s disease cohort. Incident users of benzodiazepines and nonbenzodiazepines were identified using a one-year washout period and matched with nonusers through propensity scores. Among 49,484 eligible participants with Alzheimer’s disease, 5,232 taking benzodiazepines and 3,269 taking nonbenzodiazepines were matched 1:1 with people not taking these drugs. Benzodiazepine and nonbenzodiazepine use was associated with a 22% increased risk of pneumonia. When analyzed separately, benzodiazepine use was significantly associated with a 28% increased risk of pneumonia, but nonbenzodiazepine use was not.
Hospitalization rates for acute ischemic stroke in young adults are increasing, along with the prevalence of traditional stroke risk factors, according to a study published online ahead of print April 10 in JAMA Neurology. Hospitalization data from the National Inpatient Sample from 1995 through 2012 were used to analyze acute stroke hospitalization rates among people ages 18 to 64. The 2003–2004 set included 362,339 hospitalizations, and the 2011–2012 set included 421,815 hospitalizations. Acute ischemic stroke hospitalization rates increased significantly for men and women, and for certain racial and ethnic groups, among younger adults ages 18 to 54. The prevalence of stroke risk factors among people hospitalized for acute ischemic stroke continued to increase from 2003–2004 through 2011–2012 for men and women ages 18 to 64.
A polygenic hazard score may help quantify individual differences in age-specific genetic risk for Alzheimer’s disease, according to a study published March 21 in PLOS Medicine. The investigators reviewed single-nucleotide polymorphisms associated with Alzheimer’s disease risk. Using a Cox proportional hazard model, they calculated polygenic hazard scores for participants in the Alzheimer’s Disease Genetics Consortium and tested them in two independent cohorts. People in the top polygenic hazard score quartile developed Alzheimer’s disease at a considerably lower age and had the highest yearly Alzheimer’s disease incidence rate. Among people who did not have the APOE ε3 allele, polygenic hazard score modified the age of expected onset by more than 10 years between the lowest and highest deciles. In independent cohorts, the polygenic hazard score strongly predicted age of Alzheimer’s disease onset.
Generalized anxiety disorder (GAD) is associated with migraine, according to a study published in the March issue of Headache. Researchers performed a secondary data analysis of the 2012 Canadian Community Health Survey-Mental Health. The first subsample included people with and without migraine. The second subsample was restricted to people with migraine. Six percent of people with migraine had had GAD in the previous year, compared with 2.1% of people without migraine. The adjusted odds of previous year GAD were 2.5 times higher among people with migraine than among people without. In the sample containing only migraineurs, the factors associated with higher odds of 12-month GAD included having a university degree, having low income, being without a confidant, and being male.
The rates of childhood epilepsy increase with maternal overweight or obesity in a dose-response manner, according to a study published online ahead of print April 3 in JAMA Neurology. Researchers conducted a population-based cohort study of 1,441,623 live single births at 22 or more gestational weeks in Sweden from January 1, 1997, to December 31, 2011. The risk of childhood epilepsy increased by maternal BMI from 6.30 per 10,000 child-years among normal-weight women to 12.4 per 10,000 child-years among women with grade III obesity. Risk of epilepsy increased by 11% in children of overweight mothers, compared with children of normal-weight mothers. Grade I obesity was associated with a 20% increased risk, grade II obesity was associated with a 30% increased risk, and grade III obesity was associated with an 82% increased risk.
The FDA has approved a label expansion for Trokendi XR (topiramate) to include migraine prophylaxis in adults and adolescents age 12 and older. Trokendi XR is a once-daily extended release formulation. The drug previously was approved as initial monotherapy and adjunctive therapy in patients age 6 and older with partial onset or primary generalized tonic-clonic seizures and as adjunctive therapy in patients age 6 and older with seizures associated with Lennox-Gastaut syndrome. Trokendi XR is available in 25-mg, 50-mg, 100-mg, and 200-mg capsules. The drug may cause sudden decrease in vision, secondary angle closure glaucoma, or decreased sweating. Approximately one in 500 people who take Trokendi XR may have suicidal thoughts. Supernus Pharmaceuticals markets Trokendi XR.
The FDA has approved Austedo (deutetrabenazine) tablets for the treatment of chorea associated with Huntington’s disease. Austedo was previously referred to by the name SD-809 and was granted Orphan Drug Designation by the FDA. Austedo is the second product approved for Huntington’s disease. The approval was based on phase III results in a randomized, double-blind, placebo-controlled, multicenter trial conducted in 90 ambulatory patients with manifest chorea associated with Huntington’s disease. Total Maximal Chorea Scores for patients receiving Austedo improved by approximately 4.4 units from baseline to the maintenance period, compared with approximately 1.9 units in the placebo group. At the week 13 follow-up visit (one week after discontinuation of the study drug), the Total Maximal Chorea Scores of patients who had received Austedo returned to baseline levels. Teva Pharmaceutical Industries markets Austedo.
—Kimberly Williams
New and Noteworthy Information—April 2017
More than 80% of patients with stroke and a history of atrial fibrillation received inadequate or no anticoagulation therapy before the stroke, despite the drugs’ proven record of reducing stroke risk, according to a study published March 14 in JAMA. This retrospective observational study included 94,474 patients with acute ischemic stroke and a known history of atrial fibrillation enrolled in the Get With the Guidelines-Stroke program registry. Approximately 16% of patients with atrial fibrillation had received the recommended anticoagulation medication prior to having a stroke. In addition, 84% of patients were not treated according to the guidelines prior to stroke. Thirty percent of patients were not taking any antithrombotic treatment, 40% were taking an antiplatelet drug, and 13.5% of patients were taking a subtherapeutic dose of warfarin.
Microwave measurements can enable rapid detection of intracranial bleeding in traumatic brain injuries, according to a study published online ahead of print March 13 in the Journal of Neurotrauma. The study compared 20 patients hospitalized for surgery of chronic subdural hematoma with 20 healthy volunteers. The patients were examined with microwave measurements that were compared with CT scans. The researchers assessed whether these measurements, together with a diagnostic algorithm, could distinguish between groups. The accuracy of the diagnostic algorithm was assessed using a leave-one-out analysis. At 100% sensitivity, the algorithm’s specificity was 75%. “The result indicates that the microwave measurements can be useful in ambulances and in other care settings,” said the researchers. Further studies of patients with acute head injury are ongoing.
People with epilepsy use cannabis products when antiepileptic drug side-effects are intolerable and their epilepsy is uncontrolled, according to Australian survey results published online ahead of print February 24 in Epilepsy & Behavior. The Epilepsy Action Australia survey consisted of 39 questions assessing demographics; clinical factors, including diagnosis and seizure types; and experiences with and opinions of cannabis use in epilepsy. In all, 976 responses met the inclusion criteria. Approximately 15% of adults with epilepsy and 13% of parents and guardians of children with epilepsy were currently using or had previously used cannabis products to treat epilepsy. Of those with a history of cannabis product use, 90% of adults and 71% of parents reported success in reducing seizure frequency after using cannabis products.
Interhemispheric transfer time may help predict which children will take longer to recover from a traumatic brain injury (TBI), according to a study published online ahead of print March 15 in Neurology. Researchers studied 21 children with moderate to severe TBI at two to five months post injury and at 13 to 19 months post injury. Twenty well-matched healthy control children also were studied. Investigators assessed corpus callosum function through interhemispheric transfer time, and related it to diffusion-weighted MRI measures of white matter microstructure. Children with TBI and normal interhemispheric transfer time did not differ significantly from healthy controls in white matter organization in the chronic phase or between the two evaluations. Children with TBI and slow interhemispheric transfer time had low and progressively declining white matter organization, compared with controls.
Dietary factors are associated with approximately half of deaths from heart disease, stroke, and type 2 diabetes, according to a study published March 7 in JAMA. Researchers used data from the National Health and Nutrition Examination Surveys, estimated associations of diet and disease from studies and clinical trials, and estimated disease-specific national mortality from the National Center for Health Statistics. The authors focused on the consumption of 10 foods and nutrients associated with cardiometabolic diseases. The largest numbers of estimated diet-related cardiometabolic deaths were related to high sodium intake, low nut and seed intake, high processed meat intake, low seafood omega-3 fat intake, low vegetable intake, low fruit intake, and high sugar-sweetened beverage intake. Declines in cardiometabolic deaths were associated with increased consumption of polyunsaturated fats.
Monoamine oxidase type B (MAO-B) inhibitors may reduce clinical decline in Parkinson’s disease, according to a study published March 6 in the Journal of Parkinson’s Disease. Researchers performed a secondary analysis of the NET-PD LS1 trial. They used a linear mixed model to explore the association between the cumulative duration of MAO-B inhibitor exposure and the Global Outcome, which included five clinical measures. The investigators found a significant association between longer duration of MAO-B inhibitor exposure and slower clinical decline. Each additional year of MAO-B inhibitor exposure reduced the annual clinical decline by approximately 20%. Significant associations between duration of MAO-B inhibitor exposure and less progression were observed for the Activities of Daily Living scale, ambulatory capacity, and the modified Rankin scale.
Topological data analysis has identified a multivariate phenotype associated with unfavorable outcome at three and six months after mild traumatic brain injury (TBI), according to a study published online ahead of print March 3 in PLOS ONE. The Transforming Research and Clinical Knowledge in TBI Pilot multicenter study included 586 patients with acute TBI and collected diverse common data elements from them. Researchers applied topology-based data-driven discovery to identify subgroups of patients. The analysis identified a multivariate phenotype with high rates of posttraumatic stress disorder that was enriched for PARP1, ANKK1, and COMT. Machine learning methods such as topological data analysis may provide a robust method for patient stratification and treatment planning that targets identified biomarkers in future clinical trials in patients with TBI, said the investigators.
In patients ages 18 to 45 with ischemic stroke, migraine, especially migraine without aura, is consistently associated with cervical artery dissection (CEAD), according to a study published online ahead of print March 6 in JAMA Neurology. In all, 2,485 patients enrolled in the multicenter Italian Project on Stroke in Young Adults study that was conducted between January 1, 2000, and June 30, 2015. Of the people included in the study, 13.4% had CEAD ischemic stroke and 86.6% had non-CEAD ischemic stroke. Migraine was more common in the CEAD ischemic stroke group, mainly because of migraine without aura. Compared with migraine with aura, migraine without aura was independently associated with CEAD ischemic stroke. The strength of this association was higher in men and in patients age 39 or younger.
Data are insufficient to support a recommendation of cognitive training in the treatment of patients with dementia, according to a study published in the Journal of Alzheimer’s Disease. Researchers systematically reviewed the current evidence from randomized controlled trials to determine whether cognitive training improves or stabilizes cognition or everyday functioning in patients with mild and moderate Alzheimer’s disease. The investigators examined 31 randomized controlled trials with cognitive training as either the primary intervention or part of a broader cognitive or multicomponent intervention. A positive effect was reported in 24 trials, mainly on global cognition and training-specific tasks. The trials yielded little evidence of improved everyday functioning, however. Future randomized controlled trials with appropriate classification and specification of cognitive interventions are needed to confirm the latter’s benefit, said the authors.
Patients who infer a correlation between data collected on wearable sleep-tracking devices and daytime fatigue may begin a perfectionistic quest for ideal sleep to optimize daytime function, according to a case series published February 15 in the Journal of Clinical Sleep Medicine. Many patients believe that the devices are more reliable than they are. A male patient went to bed feeling the pressure of ensuring that the tracker would display eight hours of sleep the next day. He thus had self-induced anxiety that made achieving sound sleep more difficult. A female patient complained about feeling unrefreshed when awakening after what she perceived had been a poor night’s sleep. Polysomnography revealed that the woman had had deep sleep, but the woman dismissed the finding in favor of her device’s data.
Changes in brain connectivity at the time of mild traumatic brain injury (mTBI) may predict cognitive and behavioral performance at six months, according to a study published online ahead of print January 13 in the Journal of Neurotrauma. Seventy-five patients with mTBI were recruited into a pilot study and compared with 47 matched healthy subjects. Resting-state functional MRI data were acquired and processed using probabilistic independent component analysis. The investigators found alterations in the spatial maps of the resting-state networks between patients with mTBI and healthy controls in networks involved in behavioral and cognition processes. These alterations predicted outcomes at six months post injury in patients with mTBI. Compared with controls, patients with mTBI and lesions and those with mTBI without lesions had different patterns of reduced network interactions.
Patients with the BChE-K genotype who receive donepezil for mild cognitive impairment (MCI) may have faster cognitive decline, according to a study published in the January issue of the Journal of Alzheimer’s Disease. Researchers examined the association between BChE-K genotype and changes in cognitive function using data collected during a study of people with amnestic MCI who were treated with vitamin E, donepezil, or placebo. They found significant interactions between BChE-K genotype and the duration of donepezil treatment, with increased changes in Mini-Mental State Examination (MMSE) and Clinical Dementia Rating Scale Sum of Boxes (CDR-SB) scores, compared with the common allele. BChE-K homozygous people treated with donepezil had faster decline on MMSE score and faster rise in CDR-SB score, compared with untreated BChE-K homozygous individuals.
The FDA has approved Xadago (safinamide) tablets as an add-on treatment for patients with Parkinson’s disease who are taking levodopa–carbidopa and experiencing off episodes. In a clinical trial of 645 participants with Parkinson’s disease taking levodopa and experiencing off time, participants who received Xadago had more on time without troublesome dyskinesia, compared with controls. The increase in on time was accompanied by a reduction in off time and better scores on a measure of motor function assessed during on time. Patients with severe liver problems and those who take dextromethorphan should not take Xadago. Patients who take a monoamine oxidase inhibitor or St. John’s wort also should not take Xadago. The most common adverse reactions observed in patients taking Xadago were uncontrolled involuntary movement, falls, nausea, and insomnia.
—Kimberly Williams
More than 80% of patients with stroke and a history of atrial fibrillation received inadequate or no anticoagulation therapy before the stroke, despite the drugs’ proven record of reducing stroke risk, according to a study published March 14 in JAMA. This retrospective observational study included 94,474 patients with acute ischemic stroke and a known history of atrial fibrillation enrolled in the Get With the Guidelines-Stroke program registry. Approximately 16% of patients with atrial fibrillation had received the recommended anticoagulation medication prior to having a stroke. In addition, 84% of patients were not treated according to the guidelines prior to stroke. Thirty percent of patients were not taking any antithrombotic treatment, 40% were taking an antiplatelet drug, and 13.5% of patients were taking a subtherapeutic dose of warfarin.
Microwave measurements can enable rapid detection of intracranial bleeding in traumatic brain injuries, according to a study published online ahead of print March 13 in the Journal of Neurotrauma. The study compared 20 patients hospitalized for surgery of chronic subdural hematoma with 20 healthy volunteers. The patients were examined with microwave measurements that were compared with CT scans. The researchers assessed whether these measurements, together with a diagnostic algorithm, could distinguish between groups. The accuracy of the diagnostic algorithm was assessed using a leave-one-out analysis. At 100% sensitivity, the algorithm’s specificity was 75%. “The result indicates that the microwave measurements can be useful in ambulances and in other care settings,” said the researchers. Further studies of patients with acute head injury are ongoing.
People with epilepsy use cannabis products when antiepileptic drug side-effects are intolerable and their epilepsy is uncontrolled, according to Australian survey results published online ahead of print February 24 in Epilepsy & Behavior. The Epilepsy Action Australia survey consisted of 39 questions assessing demographics; clinical factors, including diagnosis and seizure types; and experiences with and opinions of cannabis use in epilepsy. In all, 976 responses met the inclusion criteria. Approximately 15% of adults with epilepsy and 13% of parents and guardians of children with epilepsy were currently using or had previously used cannabis products to treat epilepsy. Of those with a history of cannabis product use, 90% of adults and 71% of parents reported success in reducing seizure frequency after using cannabis products.
Interhemispheric transfer time may help predict which children will take longer to recover from a traumatic brain injury (TBI), according to a study published online ahead of print March 15 in Neurology. Researchers studied 21 children with moderate to severe TBI at two to five months post injury and at 13 to 19 months post injury. Twenty well-matched healthy control children also were studied. Investigators assessed corpus callosum function through interhemispheric transfer time, and related it to diffusion-weighted MRI measures of white matter microstructure. Children with TBI and normal interhemispheric transfer time did not differ significantly from healthy controls in white matter organization in the chronic phase or between the two evaluations. Children with TBI and slow interhemispheric transfer time had low and progressively declining white matter organization, compared with controls.
Dietary factors are associated with approximately half of deaths from heart disease, stroke, and type 2 diabetes, according to a study published March 7 in JAMA. Researchers used data from the National Health and Nutrition Examination Surveys, estimated associations of diet and disease from studies and clinical trials, and estimated disease-specific national mortality from the National Center for Health Statistics. The authors focused on the consumption of 10 foods and nutrients associated with cardiometabolic diseases. The largest numbers of estimated diet-related cardiometabolic deaths were related to high sodium intake, low nut and seed intake, high processed meat intake, low seafood omega-3 fat intake, low vegetable intake, low fruit intake, and high sugar-sweetened beverage intake. Declines in cardiometabolic deaths were associated with increased consumption of polyunsaturated fats.
Monoamine oxidase type B (MAO-B) inhibitors may reduce clinical decline in Parkinson’s disease, according to a study published March 6 in the Journal of Parkinson’s Disease. Researchers performed a secondary analysis of the NET-PD LS1 trial. They used a linear mixed model to explore the association between the cumulative duration of MAO-B inhibitor exposure and the Global Outcome, which included five clinical measures. The investigators found a significant association between longer duration of MAO-B inhibitor exposure and slower clinical decline. Each additional year of MAO-B inhibitor exposure reduced the annual clinical decline by approximately 20%. Significant associations between duration of MAO-B inhibitor exposure and less progression were observed for the Activities of Daily Living scale, ambulatory capacity, and the modified Rankin scale.
Topological data analysis has identified a multivariate phenotype associated with unfavorable outcome at three and six months after mild traumatic brain injury (TBI), according to a study published online ahead of print March 3 in PLOS ONE. The Transforming Research and Clinical Knowledge in TBI Pilot multicenter study included 586 patients with acute TBI and collected diverse common data elements from them. Researchers applied topology-based data-driven discovery to identify subgroups of patients. The analysis identified a multivariate phenotype with high rates of posttraumatic stress disorder that was enriched for PARP1, ANKK1, and COMT. Machine learning methods such as topological data analysis may provide a robust method for patient stratification and treatment planning that targets identified biomarkers in future clinical trials in patients with TBI, said the investigators.
In patients ages 18 to 45 with ischemic stroke, migraine, especially migraine without aura, is consistently associated with cervical artery dissection (CEAD), according to a study published online ahead of print March 6 in JAMA Neurology. In all, 2,485 patients enrolled in the multicenter Italian Project on Stroke in Young Adults study that was conducted between January 1, 2000, and June 30, 2015. Of the people included in the study, 13.4% had CEAD ischemic stroke and 86.6% had non-CEAD ischemic stroke. Migraine was more common in the CEAD ischemic stroke group, mainly because of migraine without aura. Compared with migraine with aura, migraine without aura was independently associated with CEAD ischemic stroke. The strength of this association was higher in men and in patients age 39 or younger.
Data are insufficient to support a recommendation of cognitive training in the treatment of patients with dementia, according to a study published in the Journal of Alzheimer’s Disease. Researchers systematically reviewed the current evidence from randomized controlled trials to determine whether cognitive training improves or stabilizes cognition or everyday functioning in patients with mild and moderate Alzheimer’s disease. The investigators examined 31 randomized controlled trials with cognitive training as either the primary intervention or part of a broader cognitive or multicomponent intervention. A positive effect was reported in 24 trials, mainly on global cognition and training-specific tasks. The trials yielded little evidence of improved everyday functioning, however. Future randomized controlled trials with appropriate classification and specification of cognitive interventions are needed to confirm the latter’s benefit, said the authors.
Patients who infer a correlation between data collected on wearable sleep-tracking devices and daytime fatigue may begin a perfectionistic quest for ideal sleep to optimize daytime function, according to a case series published February 15 in the Journal of Clinical Sleep Medicine. Many patients believe that the devices are more reliable than they are. A male patient went to bed feeling the pressure of ensuring that the tracker would display eight hours of sleep the next day. He thus had self-induced anxiety that made achieving sound sleep more difficult. A female patient complained about feeling unrefreshed when awakening after what she perceived had been a poor night’s sleep. Polysomnography revealed that the woman had had deep sleep, but the woman dismissed the finding in favor of her device’s data.
Changes in brain connectivity at the time of mild traumatic brain injury (mTBI) may predict cognitive and behavioral performance at six months, according to a study published online ahead of print January 13 in the Journal of Neurotrauma. Seventy-five patients with mTBI were recruited into a pilot study and compared with 47 matched healthy subjects. Resting-state functional MRI data were acquired and processed using probabilistic independent component analysis. The investigators found alterations in the spatial maps of the resting-state networks between patients with mTBI and healthy controls in networks involved in behavioral and cognition processes. These alterations predicted outcomes at six months post injury in patients with mTBI. Compared with controls, patients with mTBI and lesions and those with mTBI without lesions had different patterns of reduced network interactions.
Patients with the BChE-K genotype who receive donepezil for mild cognitive impairment (MCI) may have faster cognitive decline, according to a study published in the January issue of the Journal of Alzheimer’s Disease. Researchers examined the association between BChE-K genotype and changes in cognitive function using data collected during a study of people with amnestic MCI who were treated with vitamin E, donepezil, or placebo. They found significant interactions between BChE-K genotype and the duration of donepezil treatment, with increased changes in Mini-Mental State Examination (MMSE) and Clinical Dementia Rating Scale Sum of Boxes (CDR-SB) scores, compared with the common allele. BChE-K homozygous people treated with donepezil had faster decline on MMSE score and faster rise in CDR-SB score, compared with untreated BChE-K homozygous individuals.
The FDA has approved Xadago (safinamide) tablets as an add-on treatment for patients with Parkinson’s disease who are taking levodopa–carbidopa and experiencing off episodes. In a clinical trial of 645 participants with Parkinson’s disease taking levodopa and experiencing off time, participants who received Xadago had more on time without troublesome dyskinesia, compared with controls. The increase in on time was accompanied by a reduction in off time and better scores on a measure of motor function assessed during on time. Patients with severe liver problems and those who take dextromethorphan should not take Xadago. Patients who take a monoamine oxidase inhibitor or St. John’s wort also should not take Xadago. The most common adverse reactions observed in patients taking Xadago were uncontrolled involuntary movement, falls, nausea, and insomnia.
—Kimberly Williams
More than 80% of patients with stroke and a history of atrial fibrillation received inadequate or no anticoagulation therapy before the stroke, despite the drugs’ proven record of reducing stroke risk, according to a study published March 14 in JAMA. This retrospective observational study included 94,474 patients with acute ischemic stroke and a known history of atrial fibrillation enrolled in the Get With the Guidelines-Stroke program registry. Approximately 16% of patients with atrial fibrillation had received the recommended anticoagulation medication prior to having a stroke. In addition, 84% of patients were not treated according to the guidelines prior to stroke. Thirty percent of patients were not taking any antithrombotic treatment, 40% were taking an antiplatelet drug, and 13.5% of patients were taking a subtherapeutic dose of warfarin.
Microwave measurements can enable rapid detection of intracranial bleeding in traumatic brain injuries, according to a study published online ahead of print March 13 in the Journal of Neurotrauma. The study compared 20 patients hospitalized for surgery of chronic subdural hematoma with 20 healthy volunteers. The patients were examined with microwave measurements that were compared with CT scans. The researchers assessed whether these measurements, together with a diagnostic algorithm, could distinguish between groups. The accuracy of the diagnostic algorithm was assessed using a leave-one-out analysis. At 100% sensitivity, the algorithm’s specificity was 75%. “The result indicates that the microwave measurements can be useful in ambulances and in other care settings,” said the researchers. Further studies of patients with acute head injury are ongoing.
People with epilepsy use cannabis products when antiepileptic drug side-effects are intolerable and their epilepsy is uncontrolled, according to Australian survey results published online ahead of print February 24 in Epilepsy & Behavior. The Epilepsy Action Australia survey consisted of 39 questions assessing demographics; clinical factors, including diagnosis and seizure types; and experiences with and opinions of cannabis use in epilepsy. In all, 976 responses met the inclusion criteria. Approximately 15% of adults with epilepsy and 13% of parents and guardians of children with epilepsy were currently using or had previously used cannabis products to treat epilepsy. Of those with a history of cannabis product use, 90% of adults and 71% of parents reported success in reducing seizure frequency after using cannabis products.
Interhemispheric transfer time may help predict which children will take longer to recover from a traumatic brain injury (TBI), according to a study published online ahead of print March 15 in Neurology. Researchers studied 21 children with moderate to severe TBI at two to five months post injury and at 13 to 19 months post injury. Twenty well-matched healthy control children also were studied. Investigators assessed corpus callosum function through interhemispheric transfer time, and related it to diffusion-weighted MRI measures of white matter microstructure. Children with TBI and normal interhemispheric transfer time did not differ significantly from healthy controls in white matter organization in the chronic phase or between the two evaluations. Children with TBI and slow interhemispheric transfer time had low and progressively declining white matter organization, compared with controls.
Dietary factors are associated with approximately half of deaths from heart disease, stroke, and type 2 diabetes, according to a study published March 7 in JAMA. Researchers used data from the National Health and Nutrition Examination Surveys, estimated associations of diet and disease from studies and clinical trials, and estimated disease-specific national mortality from the National Center for Health Statistics. The authors focused on the consumption of 10 foods and nutrients associated with cardiometabolic diseases. The largest numbers of estimated diet-related cardiometabolic deaths were related to high sodium intake, low nut and seed intake, high processed meat intake, low seafood omega-3 fat intake, low vegetable intake, low fruit intake, and high sugar-sweetened beverage intake. Declines in cardiometabolic deaths were associated with increased consumption of polyunsaturated fats.
Monoamine oxidase type B (MAO-B) inhibitors may reduce clinical decline in Parkinson’s disease, according to a study published March 6 in the Journal of Parkinson’s Disease. Researchers performed a secondary analysis of the NET-PD LS1 trial. They used a linear mixed model to explore the association between the cumulative duration of MAO-B inhibitor exposure and the Global Outcome, which included five clinical measures. The investigators found a significant association between longer duration of MAO-B inhibitor exposure and slower clinical decline. Each additional year of MAO-B inhibitor exposure reduced the annual clinical decline by approximately 20%. Significant associations between duration of MAO-B inhibitor exposure and less progression were observed for the Activities of Daily Living scale, ambulatory capacity, and the modified Rankin scale.
Topological data analysis has identified a multivariate phenotype associated with unfavorable outcome at three and six months after mild traumatic brain injury (TBI), according to a study published online ahead of print March 3 in PLOS ONE. The Transforming Research and Clinical Knowledge in TBI Pilot multicenter study included 586 patients with acute TBI and collected diverse common data elements from them. Researchers applied topology-based data-driven discovery to identify subgroups of patients. The analysis identified a multivariate phenotype with high rates of posttraumatic stress disorder that was enriched for PARP1, ANKK1, and COMT. Machine learning methods such as topological data analysis may provide a robust method for patient stratification and treatment planning that targets identified biomarkers in future clinical trials in patients with TBI, said the investigators.
In patients ages 18 to 45 with ischemic stroke, migraine, especially migraine without aura, is consistently associated with cervical artery dissection (CEAD), according to a study published online ahead of print March 6 in JAMA Neurology. In all, 2,485 patients enrolled in the multicenter Italian Project on Stroke in Young Adults study that was conducted between January 1, 2000, and June 30, 2015. Of the people included in the study, 13.4% had CEAD ischemic stroke and 86.6% had non-CEAD ischemic stroke. Migraine was more common in the CEAD ischemic stroke group, mainly because of migraine without aura. Compared with migraine with aura, migraine without aura was independently associated with CEAD ischemic stroke. The strength of this association was higher in men and in patients age 39 or younger.
Data are insufficient to support a recommendation of cognitive training in the treatment of patients with dementia, according to a study published in the Journal of Alzheimer’s Disease. Researchers systematically reviewed the current evidence from randomized controlled trials to determine whether cognitive training improves or stabilizes cognition or everyday functioning in patients with mild and moderate Alzheimer’s disease. The investigators examined 31 randomized controlled trials with cognitive training as either the primary intervention or part of a broader cognitive or multicomponent intervention. A positive effect was reported in 24 trials, mainly on global cognition and training-specific tasks. The trials yielded little evidence of improved everyday functioning, however. Future randomized controlled trials with appropriate classification and specification of cognitive interventions are needed to confirm the latter’s benefit, said the authors.
Patients who infer a correlation between data collected on wearable sleep-tracking devices and daytime fatigue may begin a perfectionistic quest for ideal sleep to optimize daytime function, according to a case series published February 15 in the Journal of Clinical Sleep Medicine. Many patients believe that the devices are more reliable than they are. A male patient went to bed feeling the pressure of ensuring that the tracker would display eight hours of sleep the next day. He thus had self-induced anxiety that made achieving sound sleep more difficult. A female patient complained about feeling unrefreshed when awakening after what she perceived had been a poor night’s sleep. Polysomnography revealed that the woman had had deep sleep, but the woman dismissed the finding in favor of her device’s data.
Changes in brain connectivity at the time of mild traumatic brain injury (mTBI) may predict cognitive and behavioral performance at six months, according to a study published online ahead of print January 13 in the Journal of Neurotrauma. Seventy-five patients with mTBI were recruited into a pilot study and compared with 47 matched healthy subjects. Resting-state functional MRI data were acquired and processed using probabilistic independent component analysis. The investigators found alterations in the spatial maps of the resting-state networks between patients with mTBI and healthy controls in networks involved in behavioral and cognition processes. These alterations predicted outcomes at six months post injury in patients with mTBI. Compared with controls, patients with mTBI and lesions and those with mTBI without lesions had different patterns of reduced network interactions.
Patients with the BChE-K genotype who receive donepezil for mild cognitive impairment (MCI) may have faster cognitive decline, according to a study published in the January issue of the Journal of Alzheimer’s Disease. Researchers examined the association between BChE-K genotype and changes in cognitive function using data collected during a study of people with amnestic MCI who were treated with vitamin E, donepezil, or placebo. They found significant interactions between BChE-K genotype and the duration of donepezil treatment, with increased changes in Mini-Mental State Examination (MMSE) and Clinical Dementia Rating Scale Sum of Boxes (CDR-SB) scores, compared with the common allele. BChE-K homozygous people treated with donepezil had faster decline on MMSE score and faster rise in CDR-SB score, compared with untreated BChE-K homozygous individuals.
The FDA has approved Xadago (safinamide) tablets as an add-on treatment for patients with Parkinson’s disease who are taking levodopa–carbidopa and experiencing off episodes. In a clinical trial of 645 participants with Parkinson’s disease taking levodopa and experiencing off time, participants who received Xadago had more on time without troublesome dyskinesia, compared with controls. The increase in on time was accompanied by a reduction in off time and better scores on a measure of motor function assessed during on time. Patients with severe liver problems and those who take dextromethorphan should not take Xadago. Patients who take a monoamine oxidase inhibitor or St. John’s wort also should not take Xadago. The most common adverse reactions observed in patients taking Xadago were uncontrolled involuntary movement, falls, nausea, and insomnia.
—Kimberly Williams
VIDEO: Stroke thrombectomy count jumps after 2015 landmark reports
HOUSTON – Use of endovascular mechanical thrombectomy for treating selected patients with acute ischemic stroke surged in U.S. practice following publication of several studies in early 2015 that documented the treatment’s efficacy, in data collected by a large U.S. hospital registry.
During April-June 2016, 3.5% of all acute ischemic stroke patients seen at the nearly 2,000 U.S. hospitals enrolled in the Get With the Guidelines-Stroke program underwent treatment with endovascular thrombectomy, up from the 2% rate at the end of 2014,The new data he reported also showed substantial increases for other measures of thrombectomy use during a roughly 18-month period that followed a flurry of reports in late 2014 and early 2015 that presented clear evidence of the safety and efficacy of thrombectomy for selected ischemic stroke patients. The percentage of hospitals participating in the Get With the Guidelines-Stroke program that performed thrombectomies increased from about a quarter of enrolled hospitals at the end of 2014 to almost a third by mid 2016, and the average quarterly number of endovascular thrombectomy cases at hospitals offering the procedure rose from about 7 during the final 3 months of 2014 to about 12 during July-September 2016, reported Dr. Smith, a neurologist and medical director of the Cognitive Neurosciences Clinic at the University of Calgary (Alta.).
“Before 2015, we saw a slow increase in the use of intra-arterial therapy, but after studies showed it was effective, there was an acceleration in the proportion of hospitals providing this therapy, the number of cases treated at each hospital, and the number of ischemic stroke patients treated,” Dr. Smith said in a video interview. “This shows rapid uptake of endovascular thrombectomy, but we still have a ways to go.”
He estimated that roughly 10%-15% of all U.S. acute ischemic stroke patients are eligible for endovascular thrombectomy based on location of the occluding clot in a large cerebral artery and the time frame when patients appear at a thrombectomy hospital relative to their stroke onset. This suggests that by mid-2016, roughly 20%-33% of U.S. ischemic stroke patients eligible for thrombectomy actually received the treatment.
“I don’t think we should be satisfied until we treat every eligible patient as quickly as we can. We need to move toward 100%,” he said.
The analyses he reported came from data collected on more than 2.4 million ischemic stroke patients treated at more than 2,200 U.S. hospitals participating in the Get With the Guidelines-Stroke program during 2003-2016.
The 2016 data also showed that, while the median thrombectomy annual case volume from mid-2015 to mid-2016 was 32 patients per year at thrombectomy hospitals, about 5% of these centers performed 100 or more cases during this 1-year period, and about 10% performed 10 or fewer thrombectomy cases. “There may be a relationship between case volume and the skill of performing the procedure, and a potential need for a volume minimum for thrombectomy certification to ensure that centers and operators maintain their skills,” Dr. Smith said.
He contrasted the recent pace of thrombectomy uptake with the first few years of routine thrombolytic treatment for the same disease during the mid-1990s, when little uptake occurred. Dr. Smith attributed the more robust penetration of thrombectomy to several factors: the impressive benefit of the treatment, the concurrent reporting of several confirmatory studies, and the stronger acute stroke–care infrastructure now in place, compared with what was available to stroke patients a generation ago.
“It’s encouraging to see such early growth in thrombectomy when thrombolysis lagged for so many years,” Dr. Smith said.
Dr. Smith had no disclosures. Get With the Guidelines-Stroke is a program of the American Heart Association and American Stroke Association using funding provided by several drug companies.
Eric E. Smith, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
HOUSTON – Use of endovascular mechanical thrombectomy for treating selected patients with acute ischemic stroke surged in U.S. practice following publication of several studies in early 2015 that documented the treatment’s efficacy, in data collected by a large U.S. hospital registry.
During April-June 2016, 3.5% of all acute ischemic stroke patients seen at the nearly 2,000 U.S. hospitals enrolled in the Get With the Guidelines-Stroke program underwent treatment with endovascular thrombectomy, up from the 2% rate at the end of 2014,The new data he reported also showed substantial increases for other measures of thrombectomy use during a roughly 18-month period that followed a flurry of reports in late 2014 and early 2015 that presented clear evidence of the safety and efficacy of thrombectomy for selected ischemic stroke patients. The percentage of hospitals participating in the Get With the Guidelines-Stroke program that performed thrombectomies increased from about a quarter of enrolled hospitals at the end of 2014 to almost a third by mid 2016, and the average quarterly number of endovascular thrombectomy cases at hospitals offering the procedure rose from about 7 during the final 3 months of 2014 to about 12 during July-September 2016, reported Dr. Smith, a neurologist and medical director of the Cognitive Neurosciences Clinic at the University of Calgary (Alta.).
“Before 2015, we saw a slow increase in the use of intra-arterial therapy, but after studies showed it was effective, there was an acceleration in the proportion of hospitals providing this therapy, the number of cases treated at each hospital, and the number of ischemic stroke patients treated,” Dr. Smith said in a video interview. “This shows rapid uptake of endovascular thrombectomy, but we still have a ways to go.”
He estimated that roughly 10%-15% of all U.S. acute ischemic stroke patients are eligible for endovascular thrombectomy based on location of the occluding clot in a large cerebral artery and the time frame when patients appear at a thrombectomy hospital relative to their stroke onset. This suggests that by mid-2016, roughly 20%-33% of U.S. ischemic stroke patients eligible for thrombectomy actually received the treatment.
“I don’t think we should be satisfied until we treat every eligible patient as quickly as we can. We need to move toward 100%,” he said.
The analyses he reported came from data collected on more than 2.4 million ischemic stroke patients treated at more than 2,200 U.S. hospitals participating in the Get With the Guidelines-Stroke program during 2003-2016.
The 2016 data also showed that, while the median thrombectomy annual case volume from mid-2015 to mid-2016 was 32 patients per year at thrombectomy hospitals, about 5% of these centers performed 100 or more cases during this 1-year period, and about 10% performed 10 or fewer thrombectomy cases. “There may be a relationship between case volume and the skill of performing the procedure, and a potential need for a volume minimum for thrombectomy certification to ensure that centers and operators maintain their skills,” Dr. Smith said.
He contrasted the recent pace of thrombectomy uptake with the first few years of routine thrombolytic treatment for the same disease during the mid-1990s, when little uptake occurred. Dr. Smith attributed the more robust penetration of thrombectomy to several factors: the impressive benefit of the treatment, the concurrent reporting of several confirmatory studies, and the stronger acute stroke–care infrastructure now in place, compared with what was available to stroke patients a generation ago.
“It’s encouraging to see such early growth in thrombectomy when thrombolysis lagged for so many years,” Dr. Smith said.
Dr. Smith had no disclosures. Get With the Guidelines-Stroke is a program of the American Heart Association and American Stroke Association using funding provided by several drug companies.
Eric E. Smith, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
HOUSTON – Use of endovascular mechanical thrombectomy for treating selected patients with acute ischemic stroke surged in U.S. practice following publication of several studies in early 2015 that documented the treatment’s efficacy, in data collected by a large U.S. hospital registry.
During April-June 2016, 3.5% of all acute ischemic stroke patients seen at the nearly 2,000 U.S. hospitals enrolled in the Get With the Guidelines-Stroke program underwent treatment with endovascular thrombectomy, up from the 2% rate at the end of 2014,The new data he reported also showed substantial increases for other measures of thrombectomy use during a roughly 18-month period that followed a flurry of reports in late 2014 and early 2015 that presented clear evidence of the safety and efficacy of thrombectomy for selected ischemic stroke patients. The percentage of hospitals participating in the Get With the Guidelines-Stroke program that performed thrombectomies increased from about a quarter of enrolled hospitals at the end of 2014 to almost a third by mid 2016, and the average quarterly number of endovascular thrombectomy cases at hospitals offering the procedure rose from about 7 during the final 3 months of 2014 to about 12 during July-September 2016, reported Dr. Smith, a neurologist and medical director of the Cognitive Neurosciences Clinic at the University of Calgary (Alta.).
“Before 2015, we saw a slow increase in the use of intra-arterial therapy, but after studies showed it was effective, there was an acceleration in the proportion of hospitals providing this therapy, the number of cases treated at each hospital, and the number of ischemic stroke patients treated,” Dr. Smith said in a video interview. “This shows rapid uptake of endovascular thrombectomy, but we still have a ways to go.”
He estimated that roughly 10%-15% of all U.S. acute ischemic stroke patients are eligible for endovascular thrombectomy based on location of the occluding clot in a large cerebral artery and the time frame when patients appear at a thrombectomy hospital relative to their stroke onset. This suggests that by mid-2016, roughly 20%-33% of U.S. ischemic stroke patients eligible for thrombectomy actually received the treatment.
“I don’t think we should be satisfied until we treat every eligible patient as quickly as we can. We need to move toward 100%,” he said.
The analyses he reported came from data collected on more than 2.4 million ischemic stroke patients treated at more than 2,200 U.S. hospitals participating in the Get With the Guidelines-Stroke program during 2003-2016.
The 2016 data also showed that, while the median thrombectomy annual case volume from mid-2015 to mid-2016 was 32 patients per year at thrombectomy hospitals, about 5% of these centers performed 100 or more cases during this 1-year period, and about 10% performed 10 or fewer thrombectomy cases. “There may be a relationship between case volume and the skill of performing the procedure, and a potential need for a volume minimum for thrombectomy certification to ensure that centers and operators maintain their skills,” Dr. Smith said.
He contrasted the recent pace of thrombectomy uptake with the first few years of routine thrombolytic treatment for the same disease during the mid-1990s, when little uptake occurred. Dr. Smith attributed the more robust penetration of thrombectomy to several factors: the impressive benefit of the treatment, the concurrent reporting of several confirmatory studies, and the stronger acute stroke–care infrastructure now in place, compared with what was available to stroke patients a generation ago.
“It’s encouraging to see such early growth in thrombectomy when thrombolysis lagged for so many years,” Dr. Smith said.
Dr. Smith had no disclosures. Get With the Guidelines-Stroke is a program of the American Heart Association and American Stroke Association using funding provided by several drug companies.
Eric E. Smith, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point:
Major finding: U.S. thrombectomy treatment jumped from 2% of all acute ischemic stroke patients in late 2014 to 3.5% in mid-2016.
Data source: Hospitalization records for more than 2.4 million ischemic stroke patients treated at more than 2,200 U.S. hospitals participating in the Get With the Guidelines-Stroke program during 2003-2016.
Disclosures: Dr. Smith had no disclosures. Get With the Guidelines-Stroke is a program of the American Heart Association and American Stroke Association using funding provided by several drug companies.