User login
Short cervical length more common among black women, and more predictive of preterm birth
DALLAS – Black women are more than twice as likely as nonblacks to have a short cervix in midpregnancy – a finding that may bear some responsibility for their consistently higher rates of spontaneous preterm birth.
A large retrospective study of more than 16,500 women determined that having a cervical length of 20 mm or less was 2.6 times more common among black women than it was among women of other races or ethnicities, Katherine Bligard, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. And no matter what the cervical length cutoff – from 20 mm or less all the way up to 25 mm – having a short cervix conferred a significantly higher risk of spontaneous preterm birth upon black women than it did upon the comparator groups.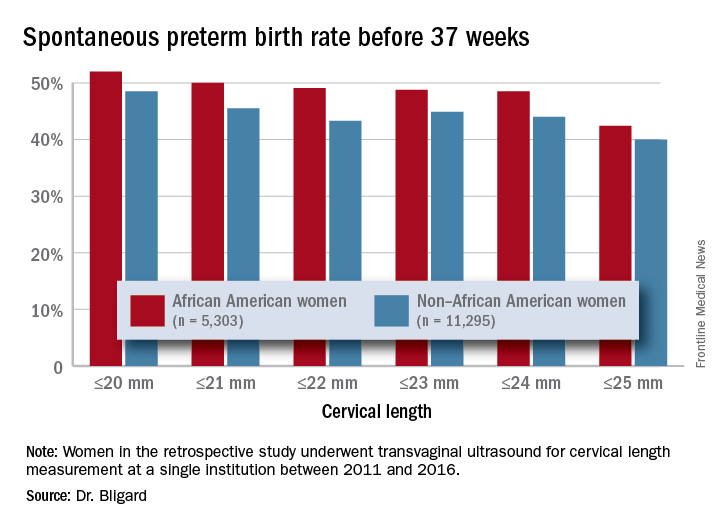
Dr. Bligard and her colleagues retrospectively examined the prevalence of short cervical length in a cohort of 16,598 women who underwent transvaginal ultrasound for cervical length measurement at a single institution between 2011 and 2016. Of these, 5,303 identified as black. These women were significantly younger than were the women who were not black (27 vs. 31 years, respectively) and were seen at a later gestational age (20.2 vs. 19.8 weeks). They were more likely to be smokers (10% vs. 5%), to be obese (40% vs. 25%), to be multiparous (70% vs. 65%), and to have a history of spontaneous preterm birth (6% vs. 3%).
The mean cervical length was significantly shorter in black women (40.3 vs. 41.1 mm). Significantly more had a cervical length of 25 mm or less (3% vs. 1.2%) or 20 mm or less (1.9% vs. 0.6%). After adjusting for gestational age at scan, tobacco use, and history of preterm birth, black women were twice as likely to have a cervical length of 25 mm or less and 2.6 times more likely to have one of 20 mm or less.
An area-under-the-curve analysis showed that shorter cervical length was significantly more predictive of spontaneous preterm birth for black women than it was for nonblack women (AUC, 0.66 vs. 0.62).
Dr. Bligard also looked at sensitivity and specificity for preterm birth at different gestational ages. At a 20 mm or less cutoff, cervical length in black women was just as specific for preterm birth occurring at less than 24 weeks, less than 28 weeks, less than 34 weeks, and less than 37 weeks (98%-99%), but it had a much higher sensitivity (44% vs. 26%, 36% vs. 23%, 26% vs.13%, and 12% vs. 5%, respectively).
The rate of preterm birth was higher for black women at every cervical length cutoff examined, Dr. Bligard noted.
The results should guide current therapy and inform future investigations, she suggested.
“Our data also suggest that race-based cervical length cutoffs may be beneficial in driving treatment, especially in light of the therapies that are available,” Dr. Bligard said. “Future studies should evaluate the efficacy of currently available therapies at a longer cervical length in African American women.”
Washington University sponsored the study, which was also funded by a training grant from the National Institutes of Health. Dr. Bligard had no financial disclosures.
SOURCE: Bligard K et al. Am J Obstet Gynecol. 2018;218:S62-3.
DALLAS – Black women are more than twice as likely as nonblacks to have a short cervix in midpregnancy – a finding that may bear some responsibility for their consistently higher rates of spontaneous preterm birth.
A large retrospective study of more than 16,500 women determined that having a cervical length of 20 mm or less was 2.6 times more common among black women than it was among women of other races or ethnicities, Katherine Bligard, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. And no matter what the cervical length cutoff – from 20 mm or less all the way up to 25 mm – having a short cervix conferred a significantly higher risk of spontaneous preterm birth upon black women than it did upon the comparator groups.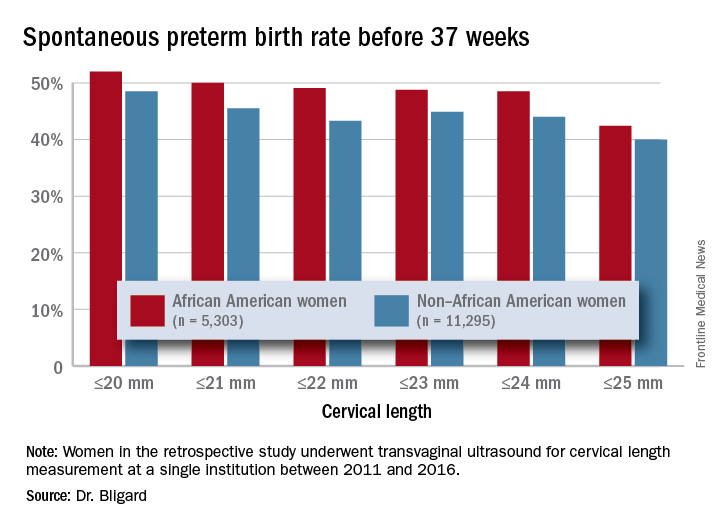
Dr. Bligard and her colleagues retrospectively examined the prevalence of short cervical length in a cohort of 16,598 women who underwent transvaginal ultrasound for cervical length measurement at a single institution between 2011 and 2016. Of these, 5,303 identified as black. These women were significantly younger than were the women who were not black (27 vs. 31 years, respectively) and were seen at a later gestational age (20.2 vs. 19.8 weeks). They were more likely to be smokers (10% vs. 5%), to be obese (40% vs. 25%), to be multiparous (70% vs. 65%), and to have a history of spontaneous preterm birth (6% vs. 3%).
The mean cervical length was significantly shorter in black women (40.3 vs. 41.1 mm). Significantly more had a cervical length of 25 mm or less (3% vs. 1.2%) or 20 mm or less (1.9% vs. 0.6%). After adjusting for gestational age at scan, tobacco use, and history of preterm birth, black women were twice as likely to have a cervical length of 25 mm or less and 2.6 times more likely to have one of 20 mm or less.
An area-under-the-curve analysis showed that shorter cervical length was significantly more predictive of spontaneous preterm birth for black women than it was for nonblack women (AUC, 0.66 vs. 0.62).
Dr. Bligard also looked at sensitivity and specificity for preterm birth at different gestational ages. At a 20 mm or less cutoff, cervical length in black women was just as specific for preterm birth occurring at less than 24 weeks, less than 28 weeks, less than 34 weeks, and less than 37 weeks (98%-99%), but it had a much higher sensitivity (44% vs. 26%, 36% vs. 23%, 26% vs.13%, and 12% vs. 5%, respectively).
The rate of preterm birth was higher for black women at every cervical length cutoff examined, Dr. Bligard noted.
The results should guide current therapy and inform future investigations, she suggested.
“Our data also suggest that race-based cervical length cutoffs may be beneficial in driving treatment, especially in light of the therapies that are available,” Dr. Bligard said. “Future studies should evaluate the efficacy of currently available therapies at a longer cervical length in African American women.”
Washington University sponsored the study, which was also funded by a training grant from the National Institutes of Health. Dr. Bligard had no financial disclosures.
SOURCE: Bligard K et al. Am J Obstet Gynecol. 2018;218:S62-3.
DALLAS – Black women are more than twice as likely as nonblacks to have a short cervix in midpregnancy – a finding that may bear some responsibility for their consistently higher rates of spontaneous preterm birth.
A large retrospective study of more than 16,500 women determined that having a cervical length of 20 mm or less was 2.6 times more common among black women than it was among women of other races or ethnicities, Katherine Bligard, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. And no matter what the cervical length cutoff – from 20 mm or less all the way up to 25 mm – having a short cervix conferred a significantly higher risk of spontaneous preterm birth upon black women than it did upon the comparator groups.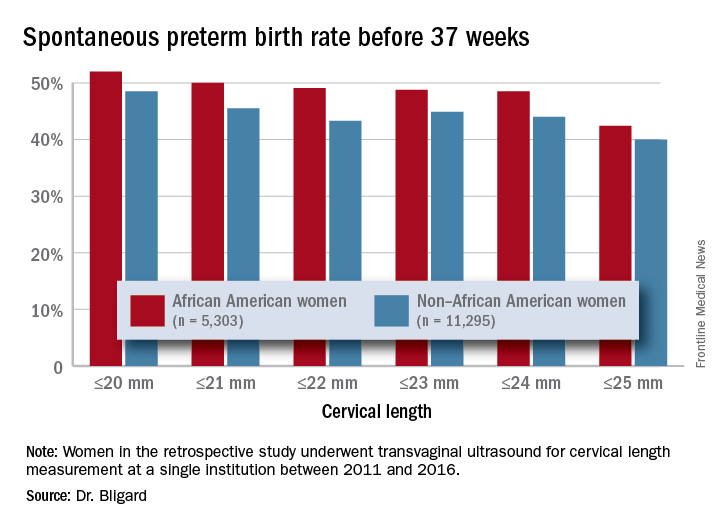
Dr. Bligard and her colleagues retrospectively examined the prevalence of short cervical length in a cohort of 16,598 women who underwent transvaginal ultrasound for cervical length measurement at a single institution between 2011 and 2016. Of these, 5,303 identified as black. These women were significantly younger than were the women who were not black (27 vs. 31 years, respectively) and were seen at a later gestational age (20.2 vs. 19.8 weeks). They were more likely to be smokers (10% vs. 5%), to be obese (40% vs. 25%), to be multiparous (70% vs. 65%), and to have a history of spontaneous preterm birth (6% vs. 3%).
The mean cervical length was significantly shorter in black women (40.3 vs. 41.1 mm). Significantly more had a cervical length of 25 mm or less (3% vs. 1.2%) or 20 mm or less (1.9% vs. 0.6%). After adjusting for gestational age at scan, tobacco use, and history of preterm birth, black women were twice as likely to have a cervical length of 25 mm or less and 2.6 times more likely to have one of 20 mm or less.
An area-under-the-curve analysis showed that shorter cervical length was significantly more predictive of spontaneous preterm birth for black women than it was for nonblack women (AUC, 0.66 vs. 0.62).
Dr. Bligard also looked at sensitivity and specificity for preterm birth at different gestational ages. At a 20 mm or less cutoff, cervical length in black women was just as specific for preterm birth occurring at less than 24 weeks, less than 28 weeks, less than 34 weeks, and less than 37 weeks (98%-99%), but it had a much higher sensitivity (44% vs. 26%, 36% vs. 23%, 26% vs.13%, and 12% vs. 5%, respectively).
The rate of preterm birth was higher for black women at every cervical length cutoff examined, Dr. Bligard noted.
The results should guide current therapy and inform future investigations, she suggested.
“Our data also suggest that race-based cervical length cutoffs may be beneficial in driving treatment, especially in light of the therapies that are available,” Dr. Bligard said. “Future studies should evaluate the efficacy of currently available therapies at a longer cervical length in African American women.”
Washington University sponsored the study, which was also funded by a training grant from the National Institutes of Health. Dr. Bligard had no financial disclosures.
SOURCE: Bligard K et al. Am J Obstet Gynecol. 2018;218:S62-3.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Having a short cervix is more common among black women and more predictive of spontaneous preterm birth.
Major finding: Cervical length of 20 mm or less was 2.6 times more common among black women than it was women of other races or ethnicities.
Study details: The retrospective review comprised more than 16,500 women.
Disclosures: The study was sponsored by Washington University and the National Institutes of Health. Dr. Bligard had no financial disclosures.
Source: Bligard K et al. Am J Obstet Gynecol. 2018;218:S62-3.
Multigene test panel helps diagnose fetal skeletal abnormalities
DALLAS – A multigene skeletal dysplasia panel detected pathogenic variants in 55% of fetal tissue samples with abnormal ultrasound findings and correctly predicted fetal lethality or viability in 75% of these.
The prenatal skeletal dysplasia panel tests 23 genes implicated in 29 different clinical syndromes, Lisa M. Vincent, PhD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. The panel’s performance in a validation cohort of 280 fetal tissue specimens, said Dr. Vincent, “underscores the clinical utility of a comprehensive, multigene sequencing tool that can aid in the diagnosis of prenatal skeletal dysplasias, allowing physicians to better manage these pregnancies.”
Up to 5 pregnancies per 1,000 are affected by some form of skeletal dysplasia, said Dr. Vincent, a clinical molecular geneticist at GeneDx, which manufactures the test. Early findings are typically picked up on ultrasound; the most frequent include limb shortening, long bone angulation, bowing, or fracture; abnormal bone echogenicity; facial dysmorphism; platyspondyly; chest narrowing and abnormal ribs; and frontal bossing of the fetal skull. However, she noted, it’s not always easy to assign a firm diagnosis based on imaging alone.
“In the prenatal period, clinical diagnosis remains challenging because of lack of availability of high-resolution imaging and lack of experience in interpreting the imaging results. Additionally, these are a genetically heterogeneous group of disorders with overlapping clinical features.”
The testing cohort for this panel comprised 280 specimens. Most (84%) were obtained from amniocentesis; 5% were from chorionic villi sampling, and the remainder were derived from other sources. The median gestational age was 20 weeks and 5 days, but the samples ranged from 5 to 36 weeks’ gestation.
The most common imaging indication for testing was short limbs (87%). Other indications included abnormal ribs or small chest circumference (47%); bowed or fractured bones (28%); leg bowing (27%); upper limb deformity (12%); poly- or syndactyly (5%); and other findings, including facial dysmorphism (23%). About 5% of the samples had a family history of skeletal dysplasia.
The panel returned a positive clinical diagnosis for 55% of the specimens. It could not determine a genetic cause for the observed clinical phenotype in 28%, and the test returned uncertain results in 17%, Dr. Vincent said.
“In these cases, we were uncertain whether the variants we identified caused the clinical features.”
Of the 153 positive cases, 42% were affected by pathogenic variants in the collagen genes of COL1A1, COL1A2, and COL1A3. Variants in the FGFR3 gene (39%) were next most common. FGFR3 is associated with achondroplasia, hypochondroplasia, thanatophoric dysplasia types 1 and 2, SADDAN (severe achondroplasia with developmental delay and acanthosis nigricans), and platyspondylic lethal skeletal dysplasia. Mutations of the SOX-9 gene, responsible for campomelic dysplasia, accounted for 5%. The test also identified nine other genetic variants in small numbers of samples.
“About 90% of the genes were autosomal dominant, indicating they are typically de novo or sporadic,” Dr. Vincent said. “About 10% were autosomal recessive, and just 1% were linked to an X-linked mutation.”
The clinical syndromes identified through these genes included osteogenesis imperfecta and thanatophoric dysplasia (33% each); achondrogenesis and spondyloepiphyseal dysplasia (11%); asphyxiating thoracic dystrophy/short rib polydactyly syndrome and campomelic dysplasia (5% each). The remaining cases were atelosteogenesis, Apert syndrome, Crouzon syndrome, chondrodysplasia punctata, hypochondroplasia, and Ellis-van Creveld syndrome.
The test predicted that 64% of the cases would be lethal. In 26%, viability was uncertain, but 10% – including 5% of the osteogenesis imperfecta cases – could be viable.
“Most lethal cases tended to have several characteristics, including short limbs, abnormal ribs, and bowed or fracture bones,” Dr. Vincent said. “Short limbs were almost five times more common in the lethal cases than in those with variable severity. Abnormal ribs and small chest were five times more frequent in the lethal cases, and bowed or fractured bones were four times more common.”
Among the nonpositive cases, 32% had additional testing. Of these, 8% had cytogenetic or large-array abnormalities, and another 8% were positive for a skeletal dysplasia that was not caused by any of the genes on the test panel.
Dr. Vincent noted that the turnaround time for the test is generally 2-3 weeks.
SOURCE: Vincent L et al. Am J Obstet Gynecol. 2018;18:S57-8.
DALLAS – A multigene skeletal dysplasia panel detected pathogenic variants in 55% of fetal tissue samples with abnormal ultrasound findings and correctly predicted fetal lethality or viability in 75% of these.
The prenatal skeletal dysplasia panel tests 23 genes implicated in 29 different clinical syndromes, Lisa M. Vincent, PhD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. The panel’s performance in a validation cohort of 280 fetal tissue specimens, said Dr. Vincent, “underscores the clinical utility of a comprehensive, multigene sequencing tool that can aid in the diagnosis of prenatal skeletal dysplasias, allowing physicians to better manage these pregnancies.”
Up to 5 pregnancies per 1,000 are affected by some form of skeletal dysplasia, said Dr. Vincent, a clinical molecular geneticist at GeneDx, which manufactures the test. Early findings are typically picked up on ultrasound; the most frequent include limb shortening, long bone angulation, bowing, or fracture; abnormal bone echogenicity; facial dysmorphism; platyspondyly; chest narrowing and abnormal ribs; and frontal bossing of the fetal skull. However, she noted, it’s not always easy to assign a firm diagnosis based on imaging alone.
“In the prenatal period, clinical diagnosis remains challenging because of lack of availability of high-resolution imaging and lack of experience in interpreting the imaging results. Additionally, these are a genetically heterogeneous group of disorders with overlapping clinical features.”
The testing cohort for this panel comprised 280 specimens. Most (84%) were obtained from amniocentesis; 5% were from chorionic villi sampling, and the remainder were derived from other sources. The median gestational age was 20 weeks and 5 days, but the samples ranged from 5 to 36 weeks’ gestation.
The most common imaging indication for testing was short limbs (87%). Other indications included abnormal ribs or small chest circumference (47%); bowed or fractured bones (28%); leg bowing (27%); upper limb deformity (12%); poly- or syndactyly (5%); and other findings, including facial dysmorphism (23%). About 5% of the samples had a family history of skeletal dysplasia.
The panel returned a positive clinical diagnosis for 55% of the specimens. It could not determine a genetic cause for the observed clinical phenotype in 28%, and the test returned uncertain results in 17%, Dr. Vincent said.
“In these cases, we were uncertain whether the variants we identified caused the clinical features.”
Of the 153 positive cases, 42% were affected by pathogenic variants in the collagen genes of COL1A1, COL1A2, and COL1A3. Variants in the FGFR3 gene (39%) were next most common. FGFR3 is associated with achondroplasia, hypochondroplasia, thanatophoric dysplasia types 1 and 2, SADDAN (severe achondroplasia with developmental delay and acanthosis nigricans), and platyspondylic lethal skeletal dysplasia. Mutations of the SOX-9 gene, responsible for campomelic dysplasia, accounted for 5%. The test also identified nine other genetic variants in small numbers of samples.
“About 90% of the genes were autosomal dominant, indicating they are typically de novo or sporadic,” Dr. Vincent said. “About 10% were autosomal recessive, and just 1% were linked to an X-linked mutation.”
The clinical syndromes identified through these genes included osteogenesis imperfecta and thanatophoric dysplasia (33% each); achondrogenesis and spondyloepiphyseal dysplasia (11%); asphyxiating thoracic dystrophy/short rib polydactyly syndrome and campomelic dysplasia (5% each). The remaining cases were atelosteogenesis, Apert syndrome, Crouzon syndrome, chondrodysplasia punctata, hypochondroplasia, and Ellis-van Creveld syndrome.
The test predicted that 64% of the cases would be lethal. In 26%, viability was uncertain, but 10% – including 5% of the osteogenesis imperfecta cases – could be viable.
“Most lethal cases tended to have several characteristics, including short limbs, abnormal ribs, and bowed or fracture bones,” Dr. Vincent said. “Short limbs were almost five times more common in the lethal cases than in those with variable severity. Abnormal ribs and small chest were five times more frequent in the lethal cases, and bowed or fractured bones were four times more common.”
Among the nonpositive cases, 32% had additional testing. Of these, 8% had cytogenetic or large-array abnormalities, and another 8% were positive for a skeletal dysplasia that was not caused by any of the genes on the test panel.
Dr. Vincent noted that the turnaround time for the test is generally 2-3 weeks.
SOURCE: Vincent L et al. Am J Obstet Gynecol. 2018;18:S57-8.
DALLAS – A multigene skeletal dysplasia panel detected pathogenic variants in 55% of fetal tissue samples with abnormal ultrasound findings and correctly predicted fetal lethality or viability in 75% of these.
The prenatal skeletal dysplasia panel tests 23 genes implicated in 29 different clinical syndromes, Lisa M. Vincent, PhD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. The panel’s performance in a validation cohort of 280 fetal tissue specimens, said Dr. Vincent, “underscores the clinical utility of a comprehensive, multigene sequencing tool that can aid in the diagnosis of prenatal skeletal dysplasias, allowing physicians to better manage these pregnancies.”
Up to 5 pregnancies per 1,000 are affected by some form of skeletal dysplasia, said Dr. Vincent, a clinical molecular geneticist at GeneDx, which manufactures the test. Early findings are typically picked up on ultrasound; the most frequent include limb shortening, long bone angulation, bowing, or fracture; abnormal bone echogenicity; facial dysmorphism; platyspondyly; chest narrowing and abnormal ribs; and frontal bossing of the fetal skull. However, she noted, it’s not always easy to assign a firm diagnosis based on imaging alone.
“In the prenatal period, clinical diagnosis remains challenging because of lack of availability of high-resolution imaging and lack of experience in interpreting the imaging results. Additionally, these are a genetically heterogeneous group of disorders with overlapping clinical features.”
The testing cohort for this panel comprised 280 specimens. Most (84%) were obtained from amniocentesis; 5% were from chorionic villi sampling, and the remainder were derived from other sources. The median gestational age was 20 weeks and 5 days, but the samples ranged from 5 to 36 weeks’ gestation.
The most common imaging indication for testing was short limbs (87%). Other indications included abnormal ribs or small chest circumference (47%); bowed or fractured bones (28%); leg bowing (27%); upper limb deformity (12%); poly- or syndactyly (5%); and other findings, including facial dysmorphism (23%). About 5% of the samples had a family history of skeletal dysplasia.
The panel returned a positive clinical diagnosis for 55% of the specimens. It could not determine a genetic cause for the observed clinical phenotype in 28%, and the test returned uncertain results in 17%, Dr. Vincent said.
“In these cases, we were uncertain whether the variants we identified caused the clinical features.”
Of the 153 positive cases, 42% were affected by pathogenic variants in the collagen genes of COL1A1, COL1A2, and COL1A3. Variants in the FGFR3 gene (39%) were next most common. FGFR3 is associated with achondroplasia, hypochondroplasia, thanatophoric dysplasia types 1 and 2, SADDAN (severe achondroplasia with developmental delay and acanthosis nigricans), and platyspondylic lethal skeletal dysplasia. Mutations of the SOX-9 gene, responsible for campomelic dysplasia, accounted for 5%. The test also identified nine other genetic variants in small numbers of samples.
“About 90% of the genes were autosomal dominant, indicating they are typically de novo or sporadic,” Dr. Vincent said. “About 10% were autosomal recessive, and just 1% were linked to an X-linked mutation.”
The clinical syndromes identified through these genes included osteogenesis imperfecta and thanatophoric dysplasia (33% each); achondrogenesis and spondyloepiphyseal dysplasia (11%); asphyxiating thoracic dystrophy/short rib polydactyly syndrome and campomelic dysplasia (5% each). The remaining cases were atelosteogenesis, Apert syndrome, Crouzon syndrome, chondrodysplasia punctata, hypochondroplasia, and Ellis-van Creveld syndrome.
The test predicted that 64% of the cases would be lethal. In 26%, viability was uncertain, but 10% – including 5% of the osteogenesis imperfecta cases – could be viable.
“Most lethal cases tended to have several characteristics, including short limbs, abnormal ribs, and bowed or fracture bones,” Dr. Vincent said. “Short limbs were almost five times more common in the lethal cases than in those with variable severity. Abnormal ribs and small chest were five times more frequent in the lethal cases, and bowed or fractured bones were four times more common.”
Among the nonpositive cases, 32% had additional testing. Of these, 8% had cytogenetic or large-array abnormalities, and another 8% were positive for a skeletal dysplasia that was not caused by any of the genes on the test panel.
Dr. Vincent noted that the turnaround time for the test is generally 2-3 weeks.
SOURCE: Vincent L et al. Am J Obstet Gynecol. 2018;18:S57-8.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: A 23-gene panel can identify 29 fetal skeletal dysplasias.
Major finding: The test identified a clinical diagnosis for 55% of samples and predicted fetal lethality or viability in 75% of these.
Study details: The validation cohort comprised 280 fetal samples.
Disclosures: GeneDx manufactures the test. Dr. Vincent is an employee of the company.
Source: Vincent L et al. Am J Obstet Gynecol. 2018;218:S57-8.
Abdominal CT refines treatment in refractory puerperal fever
DALLAS – Abdominal CT scans changed therapeutic management in 39% of women being unsuccessfully treated for refractory puerperal fever, a retrospective study has determined.
The scans pinpointed a definite diagnosis in the majority of the cohort, allowing clinicians to reassess their treatment, Michal Fishel-Bartal, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“This study has important clinical implications for women with refractory puerperal fever,” said Dr. Fishel-Bartal of the Chaim Sheba Medical Center, Ramat Gan, Israel. “Our department now recommends that all women with refractory puerperal fever should undergo an assessment for risk factors, including urgent cesarean section, preterm delivery, and general anesthesia, and an evaluation to see if an abdominal CT may be appropriate to investigate the possibility of septic pelvic thrombophlebitis or the need for intra-abdominal drainage.”
She and her colleagues conducted a 10-year retrospective review of refractory puerperal fever cases at Chaim Sheba Medical Center. All of the patients had a CT scan within 7 days of their delivery. A radiologist reviewed each scan, looking for potential causes of the illness, including pelvic collection (a suspected pelvic abscess or collection of 4 cm or more) or signs of septic pelvic thrombophlebitis (enlargement of an involved vein, vessel wall enhancement, or a filling defect).
The primary outcome was a treatment change due to the CT results. These included switching antibiotics, starting therapeutic low-molecular-weight heparin, or a surgical intervention (intra-abdominal drainage or laparotomy).
The cohort comprised 238 women, who were a mean age of 33 years. In comparing them with the hospital’s background population, they were significantly more likely to have delivered at less than 37 weeks (25% vs. 7%), and to have had a cesarean delivery (80% vs. 25%). Dr. Fishel-Bartal also noted that 29% of the patients had experienced general anesthesia.
Most of the scans (144; 60%) were abnormal. Findings included septic pelvic thrombophlebitis (32) and pelvic collections (112). Treatment changed in 93 women (39% of the entire cohort). Changes included adding or switching antibiotics (24), adding low-molecular-weight heparin (28), laparotomy (11), and drainage insertion (30).
The investigators also performed a multivariate analysis to identify any risk factors that significantly predicted the need to change or add treatment. General anesthesia was the only factor significantly more common among those who needed a treatment switch (70% vs. 58%). This could have been a marker for an urgent C-section – something often associated with complications, Dr. Fishel-Bartal noted.
In the discussion period, Dr. Fishel-Bartal fielded a question about whether ultrasound would be a more logical and cost-effective method of assessing these patients.
“We actually do usually start with an ultrasound evaluation in our patients with refractory puerperal fever, and 68% of this group did have one,” Dr. Fishel-Bartal replied. “Findings were positive in 37%. The ultrasound actually was very good at predicting pelvic collections, but it only identified 5 of the 32 with septic thrombophlebitis. So it’s a good modality to start with, but if the patient still has fever or there is a concern for septic pelvic thrombosis, you really still need a CT.”
She had no financial disclosures.
SOURCE: Fishel-Bartal M et al. The Pregnancy Meeting. Am J Obstet Gynecol. 2018;218:S59.
DALLAS – Abdominal CT scans changed therapeutic management in 39% of women being unsuccessfully treated for refractory puerperal fever, a retrospective study has determined.
The scans pinpointed a definite diagnosis in the majority of the cohort, allowing clinicians to reassess their treatment, Michal Fishel-Bartal, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“This study has important clinical implications for women with refractory puerperal fever,” said Dr. Fishel-Bartal of the Chaim Sheba Medical Center, Ramat Gan, Israel. “Our department now recommends that all women with refractory puerperal fever should undergo an assessment for risk factors, including urgent cesarean section, preterm delivery, and general anesthesia, and an evaluation to see if an abdominal CT may be appropriate to investigate the possibility of septic pelvic thrombophlebitis or the need for intra-abdominal drainage.”
She and her colleagues conducted a 10-year retrospective review of refractory puerperal fever cases at Chaim Sheba Medical Center. All of the patients had a CT scan within 7 days of their delivery. A radiologist reviewed each scan, looking for potential causes of the illness, including pelvic collection (a suspected pelvic abscess or collection of 4 cm or more) or signs of septic pelvic thrombophlebitis (enlargement of an involved vein, vessel wall enhancement, or a filling defect).
The primary outcome was a treatment change due to the CT results. These included switching antibiotics, starting therapeutic low-molecular-weight heparin, or a surgical intervention (intra-abdominal drainage or laparotomy).
The cohort comprised 238 women, who were a mean age of 33 years. In comparing them with the hospital’s background population, they were significantly more likely to have delivered at less than 37 weeks (25% vs. 7%), and to have had a cesarean delivery (80% vs. 25%). Dr. Fishel-Bartal also noted that 29% of the patients had experienced general anesthesia.
Most of the scans (144; 60%) were abnormal. Findings included septic pelvic thrombophlebitis (32) and pelvic collections (112). Treatment changed in 93 women (39% of the entire cohort). Changes included adding or switching antibiotics (24), adding low-molecular-weight heparin (28), laparotomy (11), and drainage insertion (30).
The investigators also performed a multivariate analysis to identify any risk factors that significantly predicted the need to change or add treatment. General anesthesia was the only factor significantly more common among those who needed a treatment switch (70% vs. 58%). This could have been a marker for an urgent C-section – something often associated with complications, Dr. Fishel-Bartal noted.
In the discussion period, Dr. Fishel-Bartal fielded a question about whether ultrasound would be a more logical and cost-effective method of assessing these patients.
“We actually do usually start with an ultrasound evaluation in our patients with refractory puerperal fever, and 68% of this group did have one,” Dr. Fishel-Bartal replied. “Findings were positive in 37%. The ultrasound actually was very good at predicting pelvic collections, but it only identified 5 of the 32 with septic thrombophlebitis. So it’s a good modality to start with, but if the patient still has fever or there is a concern for septic pelvic thrombosis, you really still need a CT.”
She had no financial disclosures.
SOURCE: Fishel-Bartal M et al. The Pregnancy Meeting. Am J Obstet Gynecol. 2018;218:S59.
DALLAS – Abdominal CT scans changed therapeutic management in 39% of women being unsuccessfully treated for refractory puerperal fever, a retrospective study has determined.
The scans pinpointed a definite diagnosis in the majority of the cohort, allowing clinicians to reassess their treatment, Michal Fishel-Bartal, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“This study has important clinical implications for women with refractory puerperal fever,” said Dr. Fishel-Bartal of the Chaim Sheba Medical Center, Ramat Gan, Israel. “Our department now recommends that all women with refractory puerperal fever should undergo an assessment for risk factors, including urgent cesarean section, preterm delivery, and general anesthesia, and an evaluation to see if an abdominal CT may be appropriate to investigate the possibility of septic pelvic thrombophlebitis or the need for intra-abdominal drainage.”
She and her colleagues conducted a 10-year retrospective review of refractory puerperal fever cases at Chaim Sheba Medical Center. All of the patients had a CT scan within 7 days of their delivery. A radiologist reviewed each scan, looking for potential causes of the illness, including pelvic collection (a suspected pelvic abscess or collection of 4 cm or more) or signs of septic pelvic thrombophlebitis (enlargement of an involved vein, vessel wall enhancement, or a filling defect).
The primary outcome was a treatment change due to the CT results. These included switching antibiotics, starting therapeutic low-molecular-weight heparin, or a surgical intervention (intra-abdominal drainage or laparotomy).
The cohort comprised 238 women, who were a mean age of 33 years. In comparing them with the hospital’s background population, they were significantly more likely to have delivered at less than 37 weeks (25% vs. 7%), and to have had a cesarean delivery (80% vs. 25%). Dr. Fishel-Bartal also noted that 29% of the patients had experienced general anesthesia.
Most of the scans (144; 60%) were abnormal. Findings included septic pelvic thrombophlebitis (32) and pelvic collections (112). Treatment changed in 93 women (39% of the entire cohort). Changes included adding or switching antibiotics (24), adding low-molecular-weight heparin (28), laparotomy (11), and drainage insertion (30).
The investigators also performed a multivariate analysis to identify any risk factors that significantly predicted the need to change or add treatment. General anesthesia was the only factor significantly more common among those who needed a treatment switch (70% vs. 58%). This could have been a marker for an urgent C-section – something often associated with complications, Dr. Fishel-Bartal noted.
In the discussion period, Dr. Fishel-Bartal fielded a question about whether ultrasound would be a more logical and cost-effective method of assessing these patients.
“We actually do usually start with an ultrasound evaluation in our patients with refractory puerperal fever, and 68% of this group did have one,” Dr. Fishel-Bartal replied. “Findings were positive in 37%. The ultrasound actually was very good at predicting pelvic collections, but it only identified 5 of the 32 with septic thrombophlebitis. So it’s a good modality to start with, but if the patient still has fever or there is a concern for septic pelvic thrombosis, you really still need a CT.”
She had no financial disclosures.
SOURCE: Fishel-Bartal M et al. The Pregnancy Meeting. Am J Obstet Gynecol. 2018;218:S59.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: An abdominal CT was the key to getting treatment right for women with refractory puerperal fever.
Major finding: After the scans, 39% of women got a change in treatment.
Study details: The retrospective review comprised 238 women.
Disclosures: Dr. Fishel-Bartal had no financial disclosures.
Source: Fishel-Bartal M et al. The Pregnancy Meeting. Am J Obstet Gynecol. 2018;218:S59.
Intrapartum maternal oxygen may not be beneficial for resuscitating fetuses with category II heart tracings
DALLAS – Room air was not inferior to maternal oxygen supplementation for the management of category II fetal heart tracings in a clinical trial.
Umbilical cord blood lactate – a marker of fetal acidosis caused by oxygen deprivation – was virtually identical whether the women received oxygen or remained on room air, Nandini Raghuraman, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Other blood gas measures were similar as well, and there were no differences in the number of cesarean sections or operative vaginal deliveries, said Dr. Raghuraman of Washington University, St. Louis.
“Our results suggest that room air is an acceptable alternative. However, we do need further studies, including a superiority trial.”
She noted that three randomized studies have compared oxygen to room air. “None demonstrated benefit to the fetus, and some demonstrated harm, including higher rates of delivery room resuscitation and higher neonatal acidemia. Importantly, all of these studies excluded patients with abnormal fetal heart tracings, which is the primary indication for maternal oxygen during labor and delivery.”
Her study comprised 114 women in active labor with a normal singleton fetus that developed category II heart tracings. Women received either oxygen at 10 L per minute by face mask, or stayed on room air with no face mask. The intervention continued to delivery.
The primary outcome was umbilical artery lactate. Secondary outcomes were umbilical artery blood gases, C-section for nonreassuring fetal heart status, and operative vaginal delivery.
The women were a mean age of 27.5 years; about three-quarters were black. Most (70%) had a labor induction, and 89% had received oxytocin. There were no between-group differences in the need for other fetal resuscitation strategies, including IV fluid bolus, total IV fluids, discontinuation or decrease in oxytocin, maternal repositioning, amnioinfusion, and time from randomization to delivery.
There was no difference in the primary outcome: Lactate levels were 3.4 mmol/L in the oxygen group and 3.5 mmol/L in the room air group.
Dr. Raghuraman also looked at lactate levels among those neonates who had recurrent decelerations and who did not. There was no significant difference in this comparison.
The secondary outcome of umbilical artery blood gases included measures of pH, base excess, partial CO2, and partial oxygen. There were no significant differences in any of these comparisons. Partial O2 was higher (though not significantly so) in the samples that had been exposed to oxygen, as would be expected, Dr. Raghuraman noted.
There were fewer cesarean deliveries among the room air group (4% vs. 12.5%), although this was not statistically significant. Two neonates in the oxygen group were delivered by C-section for nonreassuring fetal heart tracings. There were more operative vaginal deliveries in the room air group (11.8% vs. 2%), but this difference was not statistically significant, with a wide confidence interval (0.71-45.2).
“These results alone are not enough to be practice changing,” Dr. Raghuraman said. “Before we can do that, we need to address efficacy, which this study has called into question. But we also need to explore the results of safety and harm, and until we do so our nurses will likely continue their usual practice of putting these patients on supplement oxygen.”
She had no financial disclosures.
SOURCE: Raghuraman N et al. Am J Obstet Gynecol. 2018 Jan;218:S7.
DALLAS – Room air was not inferior to maternal oxygen supplementation for the management of category II fetal heart tracings in a clinical trial.
Umbilical cord blood lactate – a marker of fetal acidosis caused by oxygen deprivation – was virtually identical whether the women received oxygen or remained on room air, Nandini Raghuraman, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Other blood gas measures were similar as well, and there were no differences in the number of cesarean sections or operative vaginal deliveries, said Dr. Raghuraman of Washington University, St. Louis.
“Our results suggest that room air is an acceptable alternative. However, we do need further studies, including a superiority trial.”
She noted that three randomized studies have compared oxygen to room air. “None demonstrated benefit to the fetus, and some demonstrated harm, including higher rates of delivery room resuscitation and higher neonatal acidemia. Importantly, all of these studies excluded patients with abnormal fetal heart tracings, which is the primary indication for maternal oxygen during labor and delivery.”
Her study comprised 114 women in active labor with a normal singleton fetus that developed category II heart tracings. Women received either oxygen at 10 L per minute by face mask, or stayed on room air with no face mask. The intervention continued to delivery.
The primary outcome was umbilical artery lactate. Secondary outcomes were umbilical artery blood gases, C-section for nonreassuring fetal heart status, and operative vaginal delivery.
The women were a mean age of 27.5 years; about three-quarters were black. Most (70%) had a labor induction, and 89% had received oxytocin. There were no between-group differences in the need for other fetal resuscitation strategies, including IV fluid bolus, total IV fluids, discontinuation or decrease in oxytocin, maternal repositioning, amnioinfusion, and time from randomization to delivery.
There was no difference in the primary outcome: Lactate levels were 3.4 mmol/L in the oxygen group and 3.5 mmol/L in the room air group.
Dr. Raghuraman also looked at lactate levels among those neonates who had recurrent decelerations and who did not. There was no significant difference in this comparison.
The secondary outcome of umbilical artery blood gases included measures of pH, base excess, partial CO2, and partial oxygen. There were no significant differences in any of these comparisons. Partial O2 was higher (though not significantly so) in the samples that had been exposed to oxygen, as would be expected, Dr. Raghuraman noted.
There were fewer cesarean deliveries among the room air group (4% vs. 12.5%), although this was not statistically significant. Two neonates in the oxygen group were delivered by C-section for nonreassuring fetal heart tracings. There were more operative vaginal deliveries in the room air group (11.8% vs. 2%), but this difference was not statistically significant, with a wide confidence interval (0.71-45.2).
“These results alone are not enough to be practice changing,” Dr. Raghuraman said. “Before we can do that, we need to address efficacy, which this study has called into question. But we also need to explore the results of safety and harm, and until we do so our nurses will likely continue their usual practice of putting these patients on supplement oxygen.”
She had no financial disclosures.
SOURCE: Raghuraman N et al. Am J Obstet Gynecol. 2018 Jan;218:S7.
DALLAS – Room air was not inferior to maternal oxygen supplementation for the management of category II fetal heart tracings in a clinical trial.
Umbilical cord blood lactate – a marker of fetal acidosis caused by oxygen deprivation – was virtually identical whether the women received oxygen or remained on room air, Nandini Raghuraman, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Other blood gas measures were similar as well, and there were no differences in the number of cesarean sections or operative vaginal deliveries, said Dr. Raghuraman of Washington University, St. Louis.
“Our results suggest that room air is an acceptable alternative. However, we do need further studies, including a superiority trial.”
She noted that three randomized studies have compared oxygen to room air. “None demonstrated benefit to the fetus, and some demonstrated harm, including higher rates of delivery room resuscitation and higher neonatal acidemia. Importantly, all of these studies excluded patients with abnormal fetal heart tracings, which is the primary indication for maternal oxygen during labor and delivery.”
Her study comprised 114 women in active labor with a normal singleton fetus that developed category II heart tracings. Women received either oxygen at 10 L per minute by face mask, or stayed on room air with no face mask. The intervention continued to delivery.
The primary outcome was umbilical artery lactate. Secondary outcomes were umbilical artery blood gases, C-section for nonreassuring fetal heart status, and operative vaginal delivery.
The women were a mean age of 27.5 years; about three-quarters were black. Most (70%) had a labor induction, and 89% had received oxytocin. There were no between-group differences in the need for other fetal resuscitation strategies, including IV fluid bolus, total IV fluids, discontinuation or decrease in oxytocin, maternal repositioning, amnioinfusion, and time from randomization to delivery.
There was no difference in the primary outcome: Lactate levels were 3.4 mmol/L in the oxygen group and 3.5 mmol/L in the room air group.
Dr. Raghuraman also looked at lactate levels among those neonates who had recurrent decelerations and who did not. There was no significant difference in this comparison.
The secondary outcome of umbilical artery blood gases included measures of pH, base excess, partial CO2, and partial oxygen. There were no significant differences in any of these comparisons. Partial O2 was higher (though not significantly so) in the samples that had been exposed to oxygen, as would be expected, Dr. Raghuraman noted.
There were fewer cesarean deliveries among the room air group (4% vs. 12.5%), although this was not statistically significant. Two neonates in the oxygen group were delivered by C-section for nonreassuring fetal heart tracings. There were more operative vaginal deliveries in the room air group (11.8% vs. 2%), but this difference was not statistically significant, with a wide confidence interval (0.71-45.2).
“These results alone are not enough to be practice changing,” Dr. Raghuraman said. “Before we can do that, we need to address efficacy, which this study has called into question. But we also need to explore the results of safety and harm, and until we do so our nurses will likely continue their usual practice of putting these patients on supplement oxygen.”
She had no financial disclosures.
SOURCE: Raghuraman N et al. Am J Obstet Gynecol. 2018 Jan;218:S7.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Room air was not inferior to maternal oxygen for the resuscitation of a fetus who developed category II heart rhythms.
Major finding: Umbilical artery lactate was 3.4 mmol/L in the oxygen group and 3.5 mmol/L in the room air group.
Study details: The trial randomized 114 women.
Disclosures: The study was sponsored by the Washington University School of Medicine. Dr. Raghuraman had no financial disclosures.
Source: Raghuraman N et al. Am J Obstet Gynecol. 2018 Jan;218:S7.
Monthly vs. biweekly ultrasounds to ID fetal growth and amniotic fluid abnormalities
DALLAS – Monthly ultrasound scans in the last trimester pick up just as many fetal growth and amniotic fluid problems as do scans done every 2 weeks, Suneet P. Chauhan, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“We found that about one in three of these high-risk pregnancies was complicated by an abnormality of fetal growth or amniotic fluid,” said Dr. Chauhan of the department of obstetrics, gynecology, and reproductive sciences at the University of Texas, Houston. “But more frequent scans did not increase the frequency of identifying these abnormalities. And since there are approximately 1.7 million such high-risk pregnancies each year, these findings have significant implications on personal, departmental, and societal levels.”
However, he added, the SUN trial, which randomized women to monthly or biweekly scans, wasn’t large enough to definitively determine the optimal timing of ultrasounds in this population. “We need larger trials to determine this.”
The trial results, published in the American Journal of Obstetrics & Gynecology, comprised 228 women with singleton pregnancies complicated by medical comorbidities, putting the fetus at risk of problems with growth or amniotic fluid volume. They were randomized to ultrasound scans every 2 weeks or every 4 weeks during the last trimester. The primary outcome was identification of four pregnancy complications: fetal growth restriction, large for gestational age, oligohydramnios, or polyhydramnios.
There were also secondary outcomes of composite maternal morbidity (chorioamnionitis, wound infection, transfusion, diabetic ketoacidosis, venous thromboembolism, ICU admission, and death) and neonatal morbidity (Apgar score of less than 5 at 5 minutes, umbilical artery pH less than 7, hyperbilirubinemia, intubation, high-grade intraventricular hemorrhage, necrotizing enterocolitis, and death).
Women were eligible for the study if they had autoimmune disease, a body mass index of 40 kg/m2 or higher, a history of delivering a small for gestational age or macrosomic infant, hypertensive disease, substance abuse, or sickle cell disease.
About half had multiple risk factors, the three most common being high body mass index, diabetes (either gestational or insulin-dependent), and hypertensive disease. Their gestational age at randomization was a mean of 23 weeks. The first scan was conducted at a mean of 29 weeks.
There were 28% more scans in the 2-week group than in the 4-week group (492 vs. 382). There were also more exams for potentially concerning findings, including more scans looking at growth (359 vs. 278), biophysical profiles (99 vs. 79), and umbilical artery Dopplers (34 vs. 27). Despite the increased scans and investigations, the primary outcome was detected at similar points (31.7 vs. 32.2 weeks).
A primary outcome finding was detected in 38% of the 2-week group and 32% of the 4-week group – not significantly different. There were no significant differences in the proportion of outcomes detected in each group, including fetal growth restriction (19% vs. 16%), large for gestational age (14% each group), oligohydramnios (4% each group) and polyhydramnios (9% each group).
Infants in each group were born at about the same time – 13.5 weeks after randomization. The mean gestational age in both groups was 37 weeks, with about 28.5% less than 37 weeks at birth. There were no significant differences in the rate of cesarean deliveries, or small or large for gestational age births.
The composite maternal morbidity outcome was similar in the 2-week and 4-week groups (26% vs. 22%). There were no significant differences in any of the individual components of the outcome. No mother died.
The composite neonatal outcome was also similar between the groups (14% vs. 12%). There were no significant differences in any of the individual components. No infant died.
The study was sponsored by the University of Texas Health Science Center, Houston. Dr. Chauhan had no financial disclosures.
SOURCE: Roberts RP et al. Am J Obstet Gynecol. 2018;218:S3.
DALLAS – Monthly ultrasound scans in the last trimester pick up just as many fetal growth and amniotic fluid problems as do scans done every 2 weeks, Suneet P. Chauhan, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“We found that about one in three of these high-risk pregnancies was complicated by an abnormality of fetal growth or amniotic fluid,” said Dr. Chauhan of the department of obstetrics, gynecology, and reproductive sciences at the University of Texas, Houston. “But more frequent scans did not increase the frequency of identifying these abnormalities. And since there are approximately 1.7 million such high-risk pregnancies each year, these findings have significant implications on personal, departmental, and societal levels.”
However, he added, the SUN trial, which randomized women to monthly or biweekly scans, wasn’t large enough to definitively determine the optimal timing of ultrasounds in this population. “We need larger trials to determine this.”
The trial results, published in the American Journal of Obstetrics & Gynecology, comprised 228 women with singleton pregnancies complicated by medical comorbidities, putting the fetus at risk of problems with growth or amniotic fluid volume. They were randomized to ultrasound scans every 2 weeks or every 4 weeks during the last trimester. The primary outcome was identification of four pregnancy complications: fetal growth restriction, large for gestational age, oligohydramnios, or polyhydramnios.
There were also secondary outcomes of composite maternal morbidity (chorioamnionitis, wound infection, transfusion, diabetic ketoacidosis, venous thromboembolism, ICU admission, and death) and neonatal morbidity (Apgar score of less than 5 at 5 minutes, umbilical artery pH less than 7, hyperbilirubinemia, intubation, high-grade intraventricular hemorrhage, necrotizing enterocolitis, and death).
Women were eligible for the study if they had autoimmune disease, a body mass index of 40 kg/m2 or higher, a history of delivering a small for gestational age or macrosomic infant, hypertensive disease, substance abuse, or sickle cell disease.
About half had multiple risk factors, the three most common being high body mass index, diabetes (either gestational or insulin-dependent), and hypertensive disease. Their gestational age at randomization was a mean of 23 weeks. The first scan was conducted at a mean of 29 weeks.
There were 28% more scans in the 2-week group than in the 4-week group (492 vs. 382). There were also more exams for potentially concerning findings, including more scans looking at growth (359 vs. 278), biophysical profiles (99 vs. 79), and umbilical artery Dopplers (34 vs. 27). Despite the increased scans and investigations, the primary outcome was detected at similar points (31.7 vs. 32.2 weeks).
A primary outcome finding was detected in 38% of the 2-week group and 32% of the 4-week group – not significantly different. There were no significant differences in the proportion of outcomes detected in each group, including fetal growth restriction (19% vs. 16%), large for gestational age (14% each group), oligohydramnios (4% each group) and polyhydramnios (9% each group).
Infants in each group were born at about the same time – 13.5 weeks after randomization. The mean gestational age in both groups was 37 weeks, with about 28.5% less than 37 weeks at birth. There were no significant differences in the rate of cesarean deliveries, or small or large for gestational age births.
The composite maternal morbidity outcome was similar in the 2-week and 4-week groups (26% vs. 22%). There were no significant differences in any of the individual components of the outcome. No mother died.
The composite neonatal outcome was also similar between the groups (14% vs. 12%). There were no significant differences in any of the individual components. No infant died.
The study was sponsored by the University of Texas Health Science Center, Houston. Dr. Chauhan had no financial disclosures.
SOURCE: Roberts RP et al. Am J Obstet Gynecol. 2018;218:S3.
DALLAS – Monthly ultrasound scans in the last trimester pick up just as many fetal growth and amniotic fluid problems as do scans done every 2 weeks, Suneet P. Chauhan, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“We found that about one in three of these high-risk pregnancies was complicated by an abnormality of fetal growth or amniotic fluid,” said Dr. Chauhan of the department of obstetrics, gynecology, and reproductive sciences at the University of Texas, Houston. “But more frequent scans did not increase the frequency of identifying these abnormalities. And since there are approximately 1.7 million such high-risk pregnancies each year, these findings have significant implications on personal, departmental, and societal levels.”
However, he added, the SUN trial, which randomized women to monthly or biweekly scans, wasn’t large enough to definitively determine the optimal timing of ultrasounds in this population. “We need larger trials to determine this.”
The trial results, published in the American Journal of Obstetrics & Gynecology, comprised 228 women with singleton pregnancies complicated by medical comorbidities, putting the fetus at risk of problems with growth or amniotic fluid volume. They were randomized to ultrasound scans every 2 weeks or every 4 weeks during the last trimester. The primary outcome was identification of four pregnancy complications: fetal growth restriction, large for gestational age, oligohydramnios, or polyhydramnios.
There were also secondary outcomes of composite maternal morbidity (chorioamnionitis, wound infection, transfusion, diabetic ketoacidosis, venous thromboembolism, ICU admission, and death) and neonatal morbidity (Apgar score of less than 5 at 5 minutes, umbilical artery pH less than 7, hyperbilirubinemia, intubation, high-grade intraventricular hemorrhage, necrotizing enterocolitis, and death).
Women were eligible for the study if they had autoimmune disease, a body mass index of 40 kg/m2 or higher, a history of delivering a small for gestational age or macrosomic infant, hypertensive disease, substance abuse, or sickle cell disease.
About half had multiple risk factors, the three most common being high body mass index, diabetes (either gestational or insulin-dependent), and hypertensive disease. Their gestational age at randomization was a mean of 23 weeks. The first scan was conducted at a mean of 29 weeks.
There were 28% more scans in the 2-week group than in the 4-week group (492 vs. 382). There were also more exams for potentially concerning findings, including more scans looking at growth (359 vs. 278), biophysical profiles (99 vs. 79), and umbilical artery Dopplers (34 vs. 27). Despite the increased scans and investigations, the primary outcome was detected at similar points (31.7 vs. 32.2 weeks).
A primary outcome finding was detected in 38% of the 2-week group and 32% of the 4-week group – not significantly different. There were no significant differences in the proportion of outcomes detected in each group, including fetal growth restriction (19% vs. 16%), large for gestational age (14% each group), oligohydramnios (4% each group) and polyhydramnios (9% each group).
Infants in each group were born at about the same time – 13.5 weeks after randomization. The mean gestational age in both groups was 37 weeks, with about 28.5% less than 37 weeks at birth. There were no significant differences in the rate of cesarean deliveries, or small or large for gestational age births.
The composite maternal morbidity outcome was similar in the 2-week and 4-week groups (26% vs. 22%). There were no significant differences in any of the individual components of the outcome. No mother died.
The composite neonatal outcome was also similar between the groups (14% vs. 12%). There were no significant differences in any of the individual components. No infant died.
The study was sponsored by the University of Texas Health Science Center, Houston. Dr. Chauhan had no financial disclosures.
SOURCE: Roberts RP et al. Am J Obstet Gynecol. 2018;218:S3.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Ultrasound scans every 4 weeks identify just as many fetal growth of amniotic fluid problems as more frequent scans.
Major finding: A fetal or fluid abnormality was detected in 38% of the 2-week group and 32% of the 4-week group – not significantly different.
Study details: The randomized prospective trial comprised 228 women.
Disclosures: The University of Texas Medical Center, Houston, sponsored the study. Dr. Chauhan had no financial disclosures.
Source: Roberts RP et al. Am J Obstet Gynecol. 2018;218:S3.
TRAAP trial looks at tranexamic acid to prevent postpartum hemorrhage after vaginal delivery
DALLAS – An intravenous drug administered to women along with oxytocin after vaginal delivery did not reduce the risk of a large-volume hemorrhage, but it did significantly affect some other markers of postpartum blood loss.
The TRAAP trial failed to achieve its primary endpoint – reduction of postpartum hemorrhage of at least 500 ml, Loïc Sentilhes, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. But tranexamic acid’s success in the prespecified secondary endpoints suggests there still may be a place for the drug in obstetrics, said Dr. Sentilhes of the University Hospital of Bordeaux, France.
TRAAP randomized 4,079 women in labor for a planned vaginal birth to either 1 g of tranexamic acid or placebo. The interventions were added to existing IV fluids within 2 minutes after vaginal birth, after the women had also received routine oxytocin.
The study’s primary outcome was the incidence of postpartum hemorrhage, defined as a blood loss of 500 ml or more. There were a number of prespecified secondary outcomes, including clinically significant blood loss, need for additional uterotonics, severe hemorrhage (more than 1,000 mL), estimated total blood loss, transfusion, and changes in hemoglobin and hematocrit.
The study also looked at these outcomes in prespecified subgroups: women who had an episiotomy, who had an operative delivery, and who had a history of prior postpartum hemorrhage.
Women in the study were a mean age of 30 years; about half were primiparous, and 5% were attempting a vaginal birth after cesarean section. Of the women, 4% had experienced a prior postpartum hemorrhage. Labor was induced in 20%, and about 60% needed labor augmentation.
An operative vaginal delivery was necessary for 17%. Forms of assistance included forceps (55%) and vacuum extraction (45%). About a quarter had an episiotomy, and 8% had a macrosomic neonate of more than 4,000 g.
The primary endpoint of at least 500 ml blood loss occurred in 8.1% of the active group and 9.8% of the placebo group – a nonsignificant difference (relative risk, 0.83; P = .07).
Of the secondary endpoints, only two – clinically significant bleeding and need for additional uterotonics – were significantly better in the tranexamic acid group. The drug reduced the risk of clinically significant bleeding by 26% (RR, 0.74; P = .004) and the need for additional uterotonics by 25% (RR, 0.75; P = .006).
While the primary endpoint was not realized in the overall patient group, tranexamic acid achieved barely significant risk reductions of 34% in the risk of hemorrhage among women who had an operative delivery (RR, 0.66; P = .0498) and 27% among those who had an episiotomy (RR, 0.73; P = .049).
It was no better than placebo in women with a history of postpartum hemorrhage.
Those who received the drug were twice as likely to experience nausea and vomiting after delivery as did those who received placebo. But tranexamic acid exerted no lingering prothrombotic effects at 3 months after delivery, with no signals in deep vein thrombosis, no pulmonary embolism, and no clots in the ovarian or superficial veins.
The TRAAP trial was funded by the French Ministry of Health under its clinical research hospital program. Dr. Sentilhes had no financial disclosures.
SOURCE: Sentilhes L et al. Am J Obstet Gynecol. 2018;218:S1.
DALLAS – An intravenous drug administered to women along with oxytocin after vaginal delivery did not reduce the risk of a large-volume hemorrhage, but it did significantly affect some other markers of postpartum blood loss.
The TRAAP trial failed to achieve its primary endpoint – reduction of postpartum hemorrhage of at least 500 ml, Loïc Sentilhes, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. But tranexamic acid’s success in the prespecified secondary endpoints suggests there still may be a place for the drug in obstetrics, said Dr. Sentilhes of the University Hospital of Bordeaux, France.
TRAAP randomized 4,079 women in labor for a planned vaginal birth to either 1 g of tranexamic acid or placebo. The interventions were added to existing IV fluids within 2 minutes after vaginal birth, after the women had also received routine oxytocin.
The study’s primary outcome was the incidence of postpartum hemorrhage, defined as a blood loss of 500 ml or more. There were a number of prespecified secondary outcomes, including clinically significant blood loss, need for additional uterotonics, severe hemorrhage (more than 1,000 mL), estimated total blood loss, transfusion, and changes in hemoglobin and hematocrit.
The study also looked at these outcomes in prespecified subgroups: women who had an episiotomy, who had an operative delivery, and who had a history of prior postpartum hemorrhage.
Women in the study were a mean age of 30 years; about half were primiparous, and 5% were attempting a vaginal birth after cesarean section. Of the women, 4% had experienced a prior postpartum hemorrhage. Labor was induced in 20%, and about 60% needed labor augmentation.
An operative vaginal delivery was necessary for 17%. Forms of assistance included forceps (55%) and vacuum extraction (45%). About a quarter had an episiotomy, and 8% had a macrosomic neonate of more than 4,000 g.
The primary endpoint of at least 500 ml blood loss occurred in 8.1% of the active group and 9.8% of the placebo group – a nonsignificant difference (relative risk, 0.83; P = .07).
Of the secondary endpoints, only two – clinically significant bleeding and need for additional uterotonics – were significantly better in the tranexamic acid group. The drug reduced the risk of clinically significant bleeding by 26% (RR, 0.74; P = .004) and the need for additional uterotonics by 25% (RR, 0.75; P = .006).
While the primary endpoint was not realized in the overall patient group, tranexamic acid achieved barely significant risk reductions of 34% in the risk of hemorrhage among women who had an operative delivery (RR, 0.66; P = .0498) and 27% among those who had an episiotomy (RR, 0.73; P = .049).
It was no better than placebo in women with a history of postpartum hemorrhage.
Those who received the drug were twice as likely to experience nausea and vomiting after delivery as did those who received placebo. But tranexamic acid exerted no lingering prothrombotic effects at 3 months after delivery, with no signals in deep vein thrombosis, no pulmonary embolism, and no clots in the ovarian or superficial veins.
The TRAAP trial was funded by the French Ministry of Health under its clinical research hospital program. Dr. Sentilhes had no financial disclosures.
SOURCE: Sentilhes L et al. Am J Obstet Gynecol. 2018;218:S1.
DALLAS – An intravenous drug administered to women along with oxytocin after vaginal delivery did not reduce the risk of a large-volume hemorrhage, but it did significantly affect some other markers of postpartum blood loss.
The TRAAP trial failed to achieve its primary endpoint – reduction of postpartum hemorrhage of at least 500 ml, Loïc Sentilhes, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. But tranexamic acid’s success in the prespecified secondary endpoints suggests there still may be a place for the drug in obstetrics, said Dr. Sentilhes of the University Hospital of Bordeaux, France.
TRAAP randomized 4,079 women in labor for a planned vaginal birth to either 1 g of tranexamic acid or placebo. The interventions were added to existing IV fluids within 2 minutes after vaginal birth, after the women had also received routine oxytocin.
The study’s primary outcome was the incidence of postpartum hemorrhage, defined as a blood loss of 500 ml or more. There were a number of prespecified secondary outcomes, including clinically significant blood loss, need for additional uterotonics, severe hemorrhage (more than 1,000 mL), estimated total blood loss, transfusion, and changes in hemoglobin and hematocrit.
The study also looked at these outcomes in prespecified subgroups: women who had an episiotomy, who had an operative delivery, and who had a history of prior postpartum hemorrhage.
Women in the study were a mean age of 30 years; about half were primiparous, and 5% were attempting a vaginal birth after cesarean section. Of the women, 4% had experienced a prior postpartum hemorrhage. Labor was induced in 20%, and about 60% needed labor augmentation.
An operative vaginal delivery was necessary for 17%. Forms of assistance included forceps (55%) and vacuum extraction (45%). About a quarter had an episiotomy, and 8% had a macrosomic neonate of more than 4,000 g.
The primary endpoint of at least 500 ml blood loss occurred in 8.1% of the active group and 9.8% of the placebo group – a nonsignificant difference (relative risk, 0.83; P = .07).
Of the secondary endpoints, only two – clinically significant bleeding and need for additional uterotonics – were significantly better in the tranexamic acid group. The drug reduced the risk of clinically significant bleeding by 26% (RR, 0.74; P = .004) and the need for additional uterotonics by 25% (RR, 0.75; P = .006).
While the primary endpoint was not realized in the overall patient group, tranexamic acid achieved barely significant risk reductions of 34% in the risk of hemorrhage among women who had an operative delivery (RR, 0.66; P = .0498) and 27% among those who had an episiotomy (RR, 0.73; P = .049).
It was no better than placebo in women with a history of postpartum hemorrhage.
Those who received the drug were twice as likely to experience nausea and vomiting after delivery as did those who received placebo. But tranexamic acid exerted no lingering prothrombotic effects at 3 months after delivery, with no signals in deep vein thrombosis, no pulmonary embolism, and no clots in the ovarian or superficial veins.
The TRAAP trial was funded by the French Ministry of Health under its clinical research hospital program. Dr. Sentilhes had no financial disclosures.
SOURCE: Sentilhes L et al. Am J Obstet Gynecol. 2018;218:S1.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Tranexamic acid didn’t significantly reduce the risk of a postpartum hemorrhage of 500 ml or more.
Major finding: Hemorrhage occurred in 8.1% of the active group and 9.8% of the placebo group – a nonsignificant difference (relative risk, 0.83; P = .07).
Study details: The randomized, placebo-controlled study comprised 4,079 women.
Disclosures: The TRAAP trial was funded by the French Ministry of Health under its clinical research hospital program. Dr. Sentilhes had no financial disclosures.
Source: Sentilhes L et al. Am J Obstet Gynecol. 2018;218:S1.
Status asthmaticus risk upped fourfold with IV labetalol for preeclampsia
DALLAS – A maternal death occurred at Columbia University Medical Center after a patient with asthma was given intravenous labetalol, prompting a study that found an elevated risk of status asthmaticus associated with intravenous (IV) labetalol administration but not with the uterotonic carboprost.
“Overall, 71.4% of status asthmaticus cases occurred among women receiving IV labetalol,” said Whitney A. Booker, MD, speaking about the findings at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The risk of status asthmaticus didn’t reach statistical significance when women with asthma who experienced postpartum hemorrhage were given carboprost, compared with other uterotonics (3.1 vs. 1.0 per 1,000 patients; P = .56).
“Some regularly used medications in obstetrics can trigger bronchospasm,” said Dr. Booker; the American College of Obstetricians and Gynecologists lists both carboprost and labetalol as contraindicated for use in patients with asthma because of the potential for bronchospasm with each medication.
However, she said, data on the actual risk of bronchospasm when these medications are used in obstetric patients is limited.
The retrospective cohort study constructed by Dr. Booker and her colleagues at Columbia University Medical Center’s department of obstetrics and gynecology tapped 10 years’ worth of data from a large inpatient drug utilization database.
Dr. Booker, a maternal-fetal medicine fellow, said that patients were included if they were admitted for delivery and had a diagnosis of preeclampsia or postpartum hemorrhage. Of the 5.7 million hospitalizations from 2006 to 2015, 2.5% were for postpartum hemorrhage, and 4.2% for preeclampsia.
Of the patients with hemorrhage, 5,633 had a prior history of asthma, as did 12,486 of the patients with preeclampsia. In both groups, a little more than a third of patients were younger than 25 years, and about a quarter were black. Half were on Medicaid, and most were in urban areas and cared for in a teaching hospital.
The first outcome that Dr. Booker and her colleagues looked at was how practice patterns for postpartum hemorrhage varied according to whether patients had asthma; to do so, they looked at receipt of carboprost, misoprostol, and methylergonovine. A similar analysis was performed for the second outcome addressing patients with preeclampsia, in which investigators examined the use of both IV and oral labetalol, hydralazine, and nifedipine. For this and the hemorrhage outcome, the investigators performed multivariable analysis, with receipt of carboprost and IV labetalol as the outcomes of interest.
Finally, the investigators assessed the risk of status asthmaticus by comparing receipt of either carboprost (for postpartum hemorrhage) or IV labetalol (for preeclampsia) with receipt of the other medications to treat these conditions.
They found that overall, 11.4% of patients with asthma and 18% of patients without asthma received carboprost to treat postpartum hemorrhage, which makes for an adjusted risk model of 0.68 (95% confidence interval, 0.62-0.74) for receipt of carboprost for patients with asthma versus those without.
However, the pattern was different for IV labetalol: 18.5% of patients with asthma and preeclampsia received labetalol, compared with 16.7% of those without asthma. After statistical adjustment, patients with asthma had a risk ratio of 0.93 (95% CI, 0.90-0.97) for receiving IV labetalol for preeclampsia.
The analysis showed that pregnant patients with asthma were less likely to be given carboprost than labetalol, although the actual risk of status asthmaticus was higher when patients with asthma received labetalol than when they received carboprost.
“Given similar theoretical risks, obstetric providers currently administer carboprost differently than labetalol. ... Obstetricians should proceed with caution prior to giving labetalol to patients with underlying asthma,” said Dr. Booker.
During the discussion after the presentation, one attendee suggested that a next step might be to examine claims databases in conjunction with the findings of Dr. Booker’s current work in order to see whether there’s an association between asthma medication prescription fills – a surrogate for disease severity – and the risk of bronchospasm. Dr. Booker agreed that this might be a promising line of inquiry.
Dr. Booker and her colleagues reported that they had no conflicts of interest. The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
SOURCE: Booker W et al. Am J Obstet Gynecol. 2018 Jan;218:S51.
I teach my residents and fellows the “rule of thirds”: One-third of asthma patients get worse during pregnancy; one-third get better; one-third stay the same.” Asthma during pregnancy remains a challenging problem, with physicians striving to treat two complicated patients (mother and child) safely and effectively. We learn now that the use of labetalol, a beta-blocker, to treat preeclampsia in pregnant asthma patients may be associated with an increased incidence of status asthmaticus. Until we learn more about these occurrences, we should use great caution in treating pregnant asthma patients with labetalol and other beta-blockers
I teach my residents and fellows the “rule of thirds”: One-third of asthma patients get worse during pregnancy; one-third get better; one-third stay the same.” Asthma during pregnancy remains a challenging problem, with physicians striving to treat two complicated patients (mother and child) safely and effectively. We learn now that the use of labetalol, a beta-blocker, to treat preeclampsia in pregnant asthma patients may be associated with an increased incidence of status asthmaticus. Until we learn more about these occurrences, we should use great caution in treating pregnant asthma patients with labetalol and other beta-blockers
I teach my residents and fellows the “rule of thirds”: One-third of asthma patients get worse during pregnancy; one-third get better; one-third stay the same.” Asthma during pregnancy remains a challenging problem, with physicians striving to treat two complicated patients (mother and child) safely and effectively. We learn now that the use of labetalol, a beta-blocker, to treat preeclampsia in pregnant asthma patients may be associated with an increased incidence of status asthmaticus. Until we learn more about these occurrences, we should use great caution in treating pregnant asthma patients with labetalol and other beta-blockers
DALLAS – A maternal death occurred at Columbia University Medical Center after a patient with asthma was given intravenous labetalol, prompting a study that found an elevated risk of status asthmaticus associated with intravenous (IV) labetalol administration but not with the uterotonic carboprost.
“Overall, 71.4% of status asthmaticus cases occurred among women receiving IV labetalol,” said Whitney A. Booker, MD, speaking about the findings at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The risk of status asthmaticus didn’t reach statistical significance when women with asthma who experienced postpartum hemorrhage were given carboprost, compared with other uterotonics (3.1 vs. 1.0 per 1,000 patients; P = .56).
“Some regularly used medications in obstetrics can trigger bronchospasm,” said Dr. Booker; the American College of Obstetricians and Gynecologists lists both carboprost and labetalol as contraindicated for use in patients with asthma because of the potential for bronchospasm with each medication.
However, she said, data on the actual risk of bronchospasm when these medications are used in obstetric patients is limited.
The retrospective cohort study constructed by Dr. Booker and her colleagues at Columbia University Medical Center’s department of obstetrics and gynecology tapped 10 years’ worth of data from a large inpatient drug utilization database.
Dr. Booker, a maternal-fetal medicine fellow, said that patients were included if they were admitted for delivery and had a diagnosis of preeclampsia or postpartum hemorrhage. Of the 5.7 million hospitalizations from 2006 to 2015, 2.5% were for postpartum hemorrhage, and 4.2% for preeclampsia.
Of the patients with hemorrhage, 5,633 had a prior history of asthma, as did 12,486 of the patients with preeclampsia. In both groups, a little more than a third of patients were younger than 25 years, and about a quarter were black. Half were on Medicaid, and most were in urban areas and cared for in a teaching hospital.
The first outcome that Dr. Booker and her colleagues looked at was how practice patterns for postpartum hemorrhage varied according to whether patients had asthma; to do so, they looked at receipt of carboprost, misoprostol, and methylergonovine. A similar analysis was performed for the second outcome addressing patients with preeclampsia, in which investigators examined the use of both IV and oral labetalol, hydralazine, and nifedipine. For this and the hemorrhage outcome, the investigators performed multivariable analysis, with receipt of carboprost and IV labetalol as the outcomes of interest.
Finally, the investigators assessed the risk of status asthmaticus by comparing receipt of either carboprost (for postpartum hemorrhage) or IV labetalol (for preeclampsia) with receipt of the other medications to treat these conditions.
They found that overall, 11.4% of patients with asthma and 18% of patients without asthma received carboprost to treat postpartum hemorrhage, which makes for an adjusted risk model of 0.68 (95% confidence interval, 0.62-0.74) for receipt of carboprost for patients with asthma versus those without.
However, the pattern was different for IV labetalol: 18.5% of patients with asthma and preeclampsia received labetalol, compared with 16.7% of those without asthma. After statistical adjustment, patients with asthma had a risk ratio of 0.93 (95% CI, 0.90-0.97) for receiving IV labetalol for preeclampsia.
The analysis showed that pregnant patients with asthma were less likely to be given carboprost than labetalol, although the actual risk of status asthmaticus was higher when patients with asthma received labetalol than when they received carboprost.
“Given similar theoretical risks, obstetric providers currently administer carboprost differently than labetalol. ... Obstetricians should proceed with caution prior to giving labetalol to patients with underlying asthma,” said Dr. Booker.
During the discussion after the presentation, one attendee suggested that a next step might be to examine claims databases in conjunction with the findings of Dr. Booker’s current work in order to see whether there’s an association between asthma medication prescription fills – a surrogate for disease severity – and the risk of bronchospasm. Dr. Booker agreed that this might be a promising line of inquiry.
Dr. Booker and her colleagues reported that they had no conflicts of interest. The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
SOURCE: Booker W et al. Am J Obstet Gynecol. 2018 Jan;218:S51.
DALLAS – A maternal death occurred at Columbia University Medical Center after a patient with asthma was given intravenous labetalol, prompting a study that found an elevated risk of status asthmaticus associated with intravenous (IV) labetalol administration but not with the uterotonic carboprost.
“Overall, 71.4% of status asthmaticus cases occurred among women receiving IV labetalol,” said Whitney A. Booker, MD, speaking about the findings at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The risk of status asthmaticus didn’t reach statistical significance when women with asthma who experienced postpartum hemorrhage were given carboprost, compared with other uterotonics (3.1 vs. 1.0 per 1,000 patients; P = .56).
“Some regularly used medications in obstetrics can trigger bronchospasm,” said Dr. Booker; the American College of Obstetricians and Gynecologists lists both carboprost and labetalol as contraindicated for use in patients with asthma because of the potential for bronchospasm with each medication.
However, she said, data on the actual risk of bronchospasm when these medications are used in obstetric patients is limited.
The retrospective cohort study constructed by Dr. Booker and her colleagues at Columbia University Medical Center’s department of obstetrics and gynecology tapped 10 years’ worth of data from a large inpatient drug utilization database.
Dr. Booker, a maternal-fetal medicine fellow, said that patients were included if they were admitted for delivery and had a diagnosis of preeclampsia or postpartum hemorrhage. Of the 5.7 million hospitalizations from 2006 to 2015, 2.5% were for postpartum hemorrhage, and 4.2% for preeclampsia.
Of the patients with hemorrhage, 5,633 had a prior history of asthma, as did 12,486 of the patients with preeclampsia. In both groups, a little more than a third of patients were younger than 25 years, and about a quarter were black. Half were on Medicaid, and most were in urban areas and cared for in a teaching hospital.
The first outcome that Dr. Booker and her colleagues looked at was how practice patterns for postpartum hemorrhage varied according to whether patients had asthma; to do so, they looked at receipt of carboprost, misoprostol, and methylergonovine. A similar analysis was performed for the second outcome addressing patients with preeclampsia, in which investigators examined the use of both IV and oral labetalol, hydralazine, and nifedipine. For this and the hemorrhage outcome, the investigators performed multivariable analysis, with receipt of carboprost and IV labetalol as the outcomes of interest.
Finally, the investigators assessed the risk of status asthmaticus by comparing receipt of either carboprost (for postpartum hemorrhage) or IV labetalol (for preeclampsia) with receipt of the other medications to treat these conditions.
They found that overall, 11.4% of patients with asthma and 18% of patients without asthma received carboprost to treat postpartum hemorrhage, which makes for an adjusted risk model of 0.68 (95% confidence interval, 0.62-0.74) for receipt of carboprost for patients with asthma versus those without.
However, the pattern was different for IV labetalol: 18.5% of patients with asthma and preeclampsia received labetalol, compared with 16.7% of those without asthma. After statistical adjustment, patients with asthma had a risk ratio of 0.93 (95% CI, 0.90-0.97) for receiving IV labetalol for preeclampsia.
The analysis showed that pregnant patients with asthma were less likely to be given carboprost than labetalol, although the actual risk of status asthmaticus was higher when patients with asthma received labetalol than when they received carboprost.
“Given similar theoretical risks, obstetric providers currently administer carboprost differently than labetalol. ... Obstetricians should proceed with caution prior to giving labetalol to patients with underlying asthma,” said Dr. Booker.
During the discussion after the presentation, one attendee suggested that a next step might be to examine claims databases in conjunction with the findings of Dr. Booker’s current work in order to see whether there’s an association between asthma medication prescription fills – a surrogate for disease severity – and the risk of bronchospasm. Dr. Booker agreed that this might be a promising line of inquiry.
Dr. Booker and her colleagues reported that they had no conflicts of interest. The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
SOURCE: Booker W et al. Am J Obstet Gynecol. 2018 Jan;218:S51.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: IV labetalol receipt meant a fourfold increase in risk of status asthmaticus for women with preeclampsia and asthma.
Major finding: Status asthmaticus occurred in 6.5 per 1,000 patients given IV labetalol, and 1.7 per 1,000 given a different antihypertensive.
Study details: Retrospective review of 10 years’ data from a national inpatient database, which gathered data on 18,149 women with asthma and either preeclampsia or postpartum hemorrhage.
Disclosures: The study was sponsored by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The study authors had no conflicts of interest.
Source: Booker W et al. Am J Obstet Gynecol. 2018 Jan;218:S51.
Patients want information on religious hospitals’ restrictions
A majority of women want to know about restrictions on care imposed by some religious hospitals, based on data from a survey of 1,430 women.
The survey results, published in the American Journal of Obstetrics and Gynecology, showed that 35% of women thought knowing a hospital’s religion was important when choosing care, but many more – 81% – said that knowing a hospital’s religious restrictions on care was important.
The discrepancy between respondents’ desire to know a hospital’s religious orientation and to know any religious restrictions suggests that many women may have been unaware of restrictions before taking the survey, wrote Lori R. Freedman, PhD, of the University of California, San Francisco, and her colleagues.
Religious hospitals in the United States, 70% of which are Catholic, are a growing part of the health care system, but “no prior studies have asked women from across the United States what information they have and want to have before deciding where to seek care for a miscarriage or other reproductive condition that may be affected by the hospital’s religion,” the researchers said.
The researchers conducted an online survey of women aged 18-45 years who were part of the AmeriSpeak panel, a national database that includes civilian, noninstitutionalized adults. Approximately one-quarter (24%) of the women reported attending a weekly religious service.
Overall, Catholic women were no more likely than non-Catholic women to state that knowing a hospital’s religion or religious-based care restrictions was important. For example, 71% of the participants overall said an acceptable option was to admit a patient, inform her of all treatment options for miscarriage, and refer her elsewhere if she chose an option not available on religious grounds.
“ACOG recommends that institutions make information about all reproductive options available to patients and safeguard patients’ rights to access care consistent with the patient’s own values; however, Catholic hospitals may lack financial, legal, and ideological incentives to voluntarily comply with ACOG’s recommendations,” the researchers noted.
The study findings were limited by several factors, including the use of a panel-based sample and a response rate of approximately 50%. The results, however, suggest that patients need more complete information before choosing a hospital, the researchers said.
The researchers had no financial conflicts to disclose. Dr. Freedman was supported by the Greenwall Foundation. The study was supported by the Society for Family Planning.
SOURCE: Freedman LR et al. Am J Obstet Gynecol. 2018;218:251.e1-9.
A majority of women want to know about restrictions on care imposed by some religious hospitals, based on data from a survey of 1,430 women.
The survey results, published in the American Journal of Obstetrics and Gynecology, showed that 35% of women thought knowing a hospital’s religion was important when choosing care, but many more – 81% – said that knowing a hospital’s religious restrictions on care was important.
The discrepancy between respondents’ desire to know a hospital’s religious orientation and to know any religious restrictions suggests that many women may have been unaware of restrictions before taking the survey, wrote Lori R. Freedman, PhD, of the University of California, San Francisco, and her colleagues.
Religious hospitals in the United States, 70% of which are Catholic, are a growing part of the health care system, but “no prior studies have asked women from across the United States what information they have and want to have before deciding where to seek care for a miscarriage or other reproductive condition that may be affected by the hospital’s religion,” the researchers said.
The researchers conducted an online survey of women aged 18-45 years who were part of the AmeriSpeak panel, a national database that includes civilian, noninstitutionalized adults. Approximately one-quarter (24%) of the women reported attending a weekly religious service.
Overall, Catholic women were no more likely than non-Catholic women to state that knowing a hospital’s religion or religious-based care restrictions was important. For example, 71% of the participants overall said an acceptable option was to admit a patient, inform her of all treatment options for miscarriage, and refer her elsewhere if she chose an option not available on religious grounds.
“ACOG recommends that institutions make information about all reproductive options available to patients and safeguard patients’ rights to access care consistent with the patient’s own values; however, Catholic hospitals may lack financial, legal, and ideological incentives to voluntarily comply with ACOG’s recommendations,” the researchers noted.
The study findings were limited by several factors, including the use of a panel-based sample and a response rate of approximately 50%. The results, however, suggest that patients need more complete information before choosing a hospital, the researchers said.
The researchers had no financial conflicts to disclose. Dr. Freedman was supported by the Greenwall Foundation. The study was supported by the Society for Family Planning.
SOURCE: Freedman LR et al. Am J Obstet Gynecol. 2018;218:251.e1-9.
A majority of women want to know about restrictions on care imposed by some religious hospitals, based on data from a survey of 1,430 women.
The survey results, published in the American Journal of Obstetrics and Gynecology, showed that 35% of women thought knowing a hospital’s religion was important when choosing care, but many more – 81% – said that knowing a hospital’s religious restrictions on care was important.
The discrepancy between respondents’ desire to know a hospital’s religious orientation and to know any religious restrictions suggests that many women may have been unaware of restrictions before taking the survey, wrote Lori R. Freedman, PhD, of the University of California, San Francisco, and her colleagues.
Religious hospitals in the United States, 70% of which are Catholic, are a growing part of the health care system, but “no prior studies have asked women from across the United States what information they have and want to have before deciding where to seek care for a miscarriage or other reproductive condition that may be affected by the hospital’s religion,” the researchers said.
The researchers conducted an online survey of women aged 18-45 years who were part of the AmeriSpeak panel, a national database that includes civilian, noninstitutionalized adults. Approximately one-quarter (24%) of the women reported attending a weekly religious service.
Overall, Catholic women were no more likely than non-Catholic women to state that knowing a hospital’s religion or religious-based care restrictions was important. For example, 71% of the participants overall said an acceptable option was to admit a patient, inform her of all treatment options for miscarriage, and refer her elsewhere if she chose an option not available on religious grounds.
“ACOG recommends that institutions make information about all reproductive options available to patients and safeguard patients’ rights to access care consistent with the patient’s own values; however, Catholic hospitals may lack financial, legal, and ideological incentives to voluntarily comply with ACOG’s recommendations,” the researchers noted.
The study findings were limited by several factors, including the use of a panel-based sample and a response rate of approximately 50%. The results, however, suggest that patients need more complete information before choosing a hospital, the researchers said.
The researchers had no financial conflicts to disclose. Dr. Freedman was supported by the Greenwall Foundation. The study was supported by the Society for Family Planning.
SOURCE: Freedman LR et al. Am J Obstet Gynecol. 2018;218:251.e1-9.
FROM AMERICAN JOURNAL OF OBSTETRICS & GYNECOLOGY
Key clinical point: Many patients receiving care at religious hospitals are unaware of restrictions on treatment.
Major finding: Approximately 81% of women said it was important to know a hospital’s religious restrictions on care.
Study details: Survey of 1,430 women aged 18-45 years.
Disclosures: The researchers had no financial conflicts to disclose. Dr. Freedman was supported by the Greenwall Foundation. The study was supported by the Society for Family Planning.
Source: Freedman LR et al. Am J Obstet Gynecol. 2018;218:251.e1-9.
Prenatal betamethasone could save millions in care costs for women at risk of late preterm delivery
DALLAS – If betamethasone became a routine part of managing women at risk for late preterm birth, the U.S. health care system could save up to $200 million in direct costs every year.
A significant decrease in the cost of managing newborn respiratory morbidity would account for most of the savings, Cynthia Gyamfi-Bannerman, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Not only was betamethasone treatment cost effective at its base price, but treatment retained economic dominance over no treatment even when its cost was inflated up to 500%.
She presented a cost analysis of the 2016 PARENT trial. PARENT randomized 2,831 women at risk of late preterm delivery to two injections of betamethasone or matching placebo 24 hours apart. Infants exposed to betamethasone were 20% less likely to experience the primary endpoint – a composite of the need for continuous positive airway pressure or high-flow nasal cannula, supplemental oxygen, extracorporeal membrane oxygenation, or mechanical ventilation. They were also significantly less likely to be stillborn or to die within 72 hours of delivery.
“We found that antenatal betamethasone significantly decreased perinatal morbidity and mortality,” she said. “However, the costs of this intervention were unknown. Therefore, we compared the cost-effectiveness of treatment with no treatment in these women.”
Dr. Gyamfi-Bannerman described the study as a cost-minimization analysis. “The analysis took a third-party payer approach with a time horizon to first hospital discharge to home.”
Maternal costs were based on Medicaid rates. These included the cost of the betamethasone, and any out- or inpatient visits necessary to administer the drug. The neonatal costs included all direct medical costs for the newborn, including neonatal ICU admissions and any respiratory therapy the infant required.
The analysis included all mother-infant pairs in PARENT who had at least one dose of their assigned study drug and full follow-up. This comprised 1,425 pairs who received betamethasone and 1,396 who received placebo. The total mean cost of maternal/newborn care in the betamethasone group was $4,774, compared with $5,473 in the placebo group – a significant difference.
The cost-effectiveness analysis, with effectiveness defined as the proportion not reaching the primary outcome, significantly favored betamethasone as well (88.4% vs. 85.5%).
Dr. Gyamfi-Bannerman also examined cost-effectiveness in a variety of pricing scenarios, from looking at betamethasone at its base cost with hospital and physician services priced at 50% of the current level, to betamethasone inflated by 500% and other costs by 200%.
“In almost every estimate, betamethasone remained the cost-effective management option,” she said. “ and was cost effective across most of our variable estimate.”
She had no financial disclosures.
SOURCE: Gyamfi-Bannerman C et al. Am J Obstet Gynecol. 2018;218:S14.
DALLAS – If betamethasone became a routine part of managing women at risk for late preterm birth, the U.S. health care system could save up to $200 million in direct costs every year.
A significant decrease in the cost of managing newborn respiratory morbidity would account for most of the savings, Cynthia Gyamfi-Bannerman, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Not only was betamethasone treatment cost effective at its base price, but treatment retained economic dominance over no treatment even when its cost was inflated up to 500%.
She presented a cost analysis of the 2016 PARENT trial. PARENT randomized 2,831 women at risk of late preterm delivery to two injections of betamethasone or matching placebo 24 hours apart. Infants exposed to betamethasone were 20% less likely to experience the primary endpoint – a composite of the need for continuous positive airway pressure or high-flow nasal cannula, supplemental oxygen, extracorporeal membrane oxygenation, or mechanical ventilation. They were also significantly less likely to be stillborn or to die within 72 hours of delivery.
“We found that antenatal betamethasone significantly decreased perinatal morbidity and mortality,” she said. “However, the costs of this intervention were unknown. Therefore, we compared the cost-effectiveness of treatment with no treatment in these women.”
Dr. Gyamfi-Bannerman described the study as a cost-minimization analysis. “The analysis took a third-party payer approach with a time horizon to first hospital discharge to home.”
Maternal costs were based on Medicaid rates. These included the cost of the betamethasone, and any out- or inpatient visits necessary to administer the drug. The neonatal costs included all direct medical costs for the newborn, including neonatal ICU admissions and any respiratory therapy the infant required.
The analysis included all mother-infant pairs in PARENT who had at least one dose of their assigned study drug and full follow-up. This comprised 1,425 pairs who received betamethasone and 1,396 who received placebo. The total mean cost of maternal/newborn care in the betamethasone group was $4,774, compared with $5,473 in the placebo group – a significant difference.
The cost-effectiveness analysis, with effectiveness defined as the proportion not reaching the primary outcome, significantly favored betamethasone as well (88.4% vs. 85.5%).
Dr. Gyamfi-Bannerman also examined cost-effectiveness in a variety of pricing scenarios, from looking at betamethasone at its base cost with hospital and physician services priced at 50% of the current level, to betamethasone inflated by 500% and other costs by 200%.
“In almost every estimate, betamethasone remained the cost-effective management option,” she said. “ and was cost effective across most of our variable estimate.”
She had no financial disclosures.
SOURCE: Gyamfi-Bannerman C et al. Am J Obstet Gynecol. 2018;218:S14.
DALLAS – If betamethasone became a routine part of managing women at risk for late preterm birth, the U.S. health care system could save up to $200 million in direct costs every year.
A significant decrease in the cost of managing newborn respiratory morbidity would account for most of the savings, Cynthia Gyamfi-Bannerman, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Not only was betamethasone treatment cost effective at its base price, but treatment retained economic dominance over no treatment even when its cost was inflated up to 500%.
She presented a cost analysis of the 2016 PARENT trial. PARENT randomized 2,831 women at risk of late preterm delivery to two injections of betamethasone or matching placebo 24 hours apart. Infants exposed to betamethasone were 20% less likely to experience the primary endpoint – a composite of the need for continuous positive airway pressure or high-flow nasal cannula, supplemental oxygen, extracorporeal membrane oxygenation, or mechanical ventilation. They were also significantly less likely to be stillborn or to die within 72 hours of delivery.
“We found that antenatal betamethasone significantly decreased perinatal morbidity and mortality,” she said. “However, the costs of this intervention were unknown. Therefore, we compared the cost-effectiveness of treatment with no treatment in these women.”
Dr. Gyamfi-Bannerman described the study as a cost-minimization analysis. “The analysis took a third-party payer approach with a time horizon to first hospital discharge to home.”
Maternal costs were based on Medicaid rates. These included the cost of the betamethasone, and any out- or inpatient visits necessary to administer the drug. The neonatal costs included all direct medical costs for the newborn, including neonatal ICU admissions and any respiratory therapy the infant required.
The analysis included all mother-infant pairs in PARENT who had at least one dose of their assigned study drug and full follow-up. This comprised 1,425 pairs who received betamethasone and 1,396 who received placebo. The total mean cost of maternal/newborn care in the betamethasone group was $4,774, compared with $5,473 in the placebo group – a significant difference.
The cost-effectiveness analysis, with effectiveness defined as the proportion not reaching the primary outcome, significantly favored betamethasone as well (88.4% vs. 85.5%).
Dr. Gyamfi-Bannerman also examined cost-effectiveness in a variety of pricing scenarios, from looking at betamethasone at its base cost with hospital and physician services priced at 50% of the current level, to betamethasone inflated by 500% and other costs by 200%.
“In almost every estimate, betamethasone remained the cost-effective management option,” she said. “ and was cost effective across most of our variable estimate.”
She had no financial disclosures.
SOURCE: Gyamfi-Bannerman C et al. Am J Obstet Gynecol. 2018;218:S14.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: If widely adopted, prenatal betamethasone could save up to $200 million per year by preventing neonatal respiratory morbidity.
Major finding: The total mean maternal/newborn care cost was $4,774 in the betamethasone group and $5,473 in the placebo group.
Study details: The cost analysis of the PARENT trial comprised 2,821 mother/infant pairs.
Disclosures: Dr. Gyamfi-Bannerman had no financial disclosures.
Source: Gyamfi-Bannerman C et al. Am J Obstet Gynecol. 2018;218:S14.
Cerclage plus progesterone for preventing preterm births
DALLAS – Placing a cerclage conferred additional benefit over vaginal progesterone alone for women with extreme short cervixes and singleton pregnancies, in a recent study. Those who received rescue cerclage in addition to vaginal progesterone had a 92% overall reduction in spontaneous preterm birth rates, and infants had fewer neonatal ICU admissions and neonatal complications.
The single-center retrospective cohort study of 75 women with cervical length less than 10 cm who were receiving vaginal progesterone was presented by Christopher Enakpene, MD, at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Women who received rescue cerclage in addition to progesterone delivered at a mean 34.3 weeks gestational age, compared with 27.5 weeks for those receiving progesterone alone (P less than .001).
There were 13 neonatal ICU admissions for infants born to the 36 patients in the cerclage group, compared with 23 for the 39 women receiving progesterone alone (P = .009). And there were seven perinatal or neonatal deaths among the group who did not receive cerclage; no deaths occurred in the cerclage group.
“Premature cervical ripening plays a significant role in spontaneous preterm birth,” said Dr. Enakpene. “And studies have shown that, the shorter the cervix, the higher the risk of spontaneous preterm birth.”
Preterm birth, said Dr. Enakpene, is the top cause of neonatal morbidity and mortality both in the United States and worldwide; it is associated with 70% of neonatal deaths and half of all neurodevelopmental delay, he said.
At the University of Illinois at Chicago, where Dr. Enakpene is a maternal-fetal medicine fellow in the department of obstetrics and gynecology, all pregnant women are screened for cervical length by transvaginal ultrasound during their second trimester.
If screening reveals cervical length of less than 20 mm, the patient receives vaginal progesterone, “the current standard of care in singleton pregnancy with incidental short cervix,” said Dr. Enakpene. Vaginal progesterone can reduce the risk of spontaneous preterm birth by about half, he said.
At his facility, women with a short cervix then receive serial cervical length assessments every week or 2 until 24 weeks’ gestation, to identify women whose cervixes continue to shorten. For these women, it’s usually physician preference that determines whether cerclage is placed to reinforce the progressively shortening cervix, said Dr. Enakpene.
There had been previous retrospective work showing that cerclage was more effective at preventing spontaneous preterm birth than was doing nothing when a woman with a singleton pregnancy had a short cervix. However, Dr. Enakpene said that vaginal progesterone alone had not been compared with continuing progesterone and adding a cerclage.
During the study period, 310 women with cervical length of less than 20 mm were placed on progesterone. These women were included in the study cohort if, over the course of at least two cervical length measurements, their cervix shortened to less than 10 mm while they were on vaginal progesterone. They could not have indications that delivery was imminent when the 10 mm threshold was met, said Dr. Enakpene.
Women with known intrauterine fetal death, an undesired pregnancy, or any sign of intra-amniotic infection or fetal anomalies were excluded from the study.
A total of 75 women met final inclusion criteria, and received cerclage (n = 36), or not (n = 39) according to physician judgment. Demographic and pregnancy-specific characteristics were generally similar between the two groups.
In their statistical analysis, Dr. Enakpene and his colleagues used Kaplan-Meier survival analysis to look at pregnancy latency over time for women who did – or didn’t – receive a cerclage. There were significantly fewer spontaneous preterm births before 24, 28, and 34 weeks gestational age in the cerclage group (P less than .001 for all).
Dr. Enakpene acknowledged the study’s limitations, including its retrospective nature, the small sample size, and the fact that cerclage placement was done by the preference of the attending physician. However, this study was the first to examine rescue cerclage as add-on to vaginal progesterone, he said, adding, “Following this study, we are designing a prospective randomized interventional study to address this important topic.”
Dr. Enakpene reported that he had no conflicts of interest, and reported no outside sources of funding.
SOURCE: Enakpene C et al. Am J Obstet Gynecol. 2018 Jan;218:S72-S73.
DALLAS – Placing a cerclage conferred additional benefit over vaginal progesterone alone for women with extreme short cervixes and singleton pregnancies, in a recent study. Those who received rescue cerclage in addition to vaginal progesterone had a 92% overall reduction in spontaneous preterm birth rates, and infants had fewer neonatal ICU admissions and neonatal complications.
The single-center retrospective cohort study of 75 women with cervical length less than 10 cm who were receiving vaginal progesterone was presented by Christopher Enakpene, MD, at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Women who received rescue cerclage in addition to progesterone delivered at a mean 34.3 weeks gestational age, compared with 27.5 weeks for those receiving progesterone alone (P less than .001).
There were 13 neonatal ICU admissions for infants born to the 36 patients in the cerclage group, compared with 23 for the 39 women receiving progesterone alone (P = .009). And there were seven perinatal or neonatal deaths among the group who did not receive cerclage; no deaths occurred in the cerclage group.
“Premature cervical ripening plays a significant role in spontaneous preterm birth,” said Dr. Enakpene. “And studies have shown that, the shorter the cervix, the higher the risk of spontaneous preterm birth.”
Preterm birth, said Dr. Enakpene, is the top cause of neonatal morbidity and mortality both in the United States and worldwide; it is associated with 70% of neonatal deaths and half of all neurodevelopmental delay, he said.
At the University of Illinois at Chicago, where Dr. Enakpene is a maternal-fetal medicine fellow in the department of obstetrics and gynecology, all pregnant women are screened for cervical length by transvaginal ultrasound during their second trimester.
If screening reveals cervical length of less than 20 mm, the patient receives vaginal progesterone, “the current standard of care in singleton pregnancy with incidental short cervix,” said Dr. Enakpene. Vaginal progesterone can reduce the risk of spontaneous preterm birth by about half, he said.
At his facility, women with a short cervix then receive serial cervical length assessments every week or 2 until 24 weeks’ gestation, to identify women whose cervixes continue to shorten. For these women, it’s usually physician preference that determines whether cerclage is placed to reinforce the progressively shortening cervix, said Dr. Enakpene.
There had been previous retrospective work showing that cerclage was more effective at preventing spontaneous preterm birth than was doing nothing when a woman with a singleton pregnancy had a short cervix. However, Dr. Enakpene said that vaginal progesterone alone had not been compared with continuing progesterone and adding a cerclage.
During the study period, 310 women with cervical length of less than 20 mm were placed on progesterone. These women were included in the study cohort if, over the course of at least two cervical length measurements, their cervix shortened to less than 10 mm while they were on vaginal progesterone. They could not have indications that delivery was imminent when the 10 mm threshold was met, said Dr. Enakpene.
Women with known intrauterine fetal death, an undesired pregnancy, or any sign of intra-amniotic infection or fetal anomalies were excluded from the study.
A total of 75 women met final inclusion criteria, and received cerclage (n = 36), or not (n = 39) according to physician judgment. Demographic and pregnancy-specific characteristics were generally similar between the two groups.
In their statistical analysis, Dr. Enakpene and his colleagues used Kaplan-Meier survival analysis to look at pregnancy latency over time for women who did – or didn’t – receive a cerclage. There were significantly fewer spontaneous preterm births before 24, 28, and 34 weeks gestational age in the cerclage group (P less than .001 for all).
Dr. Enakpene acknowledged the study’s limitations, including its retrospective nature, the small sample size, and the fact that cerclage placement was done by the preference of the attending physician. However, this study was the first to examine rescue cerclage as add-on to vaginal progesterone, he said, adding, “Following this study, we are designing a prospective randomized interventional study to address this important topic.”
Dr. Enakpene reported that he had no conflicts of interest, and reported no outside sources of funding.
SOURCE: Enakpene C et al. Am J Obstet Gynecol. 2018 Jan;218:S72-S73.
DALLAS – Placing a cerclage conferred additional benefit over vaginal progesterone alone for women with extreme short cervixes and singleton pregnancies, in a recent study. Those who received rescue cerclage in addition to vaginal progesterone had a 92% overall reduction in spontaneous preterm birth rates, and infants had fewer neonatal ICU admissions and neonatal complications.
The single-center retrospective cohort study of 75 women with cervical length less than 10 cm who were receiving vaginal progesterone was presented by Christopher Enakpene, MD, at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Women who received rescue cerclage in addition to progesterone delivered at a mean 34.3 weeks gestational age, compared with 27.5 weeks for those receiving progesterone alone (P less than .001).
There were 13 neonatal ICU admissions for infants born to the 36 patients in the cerclage group, compared with 23 for the 39 women receiving progesterone alone (P = .009). And there were seven perinatal or neonatal deaths among the group who did not receive cerclage; no deaths occurred in the cerclage group.
“Premature cervical ripening plays a significant role in spontaneous preterm birth,” said Dr. Enakpene. “And studies have shown that, the shorter the cervix, the higher the risk of spontaneous preterm birth.”
Preterm birth, said Dr. Enakpene, is the top cause of neonatal morbidity and mortality both in the United States and worldwide; it is associated with 70% of neonatal deaths and half of all neurodevelopmental delay, he said.
At the University of Illinois at Chicago, where Dr. Enakpene is a maternal-fetal medicine fellow in the department of obstetrics and gynecology, all pregnant women are screened for cervical length by transvaginal ultrasound during their second trimester.
If screening reveals cervical length of less than 20 mm, the patient receives vaginal progesterone, “the current standard of care in singleton pregnancy with incidental short cervix,” said Dr. Enakpene. Vaginal progesterone can reduce the risk of spontaneous preterm birth by about half, he said.
At his facility, women with a short cervix then receive serial cervical length assessments every week or 2 until 24 weeks’ gestation, to identify women whose cervixes continue to shorten. For these women, it’s usually physician preference that determines whether cerclage is placed to reinforce the progressively shortening cervix, said Dr. Enakpene.
There had been previous retrospective work showing that cerclage was more effective at preventing spontaneous preterm birth than was doing nothing when a woman with a singleton pregnancy had a short cervix. However, Dr. Enakpene said that vaginal progesterone alone had not been compared with continuing progesterone and adding a cerclage.
During the study period, 310 women with cervical length of less than 20 mm were placed on progesterone. These women were included in the study cohort if, over the course of at least two cervical length measurements, their cervix shortened to less than 10 mm while they were on vaginal progesterone. They could not have indications that delivery was imminent when the 10 mm threshold was met, said Dr. Enakpene.
Women with known intrauterine fetal death, an undesired pregnancy, or any sign of intra-amniotic infection or fetal anomalies were excluded from the study.
A total of 75 women met final inclusion criteria, and received cerclage (n = 36), or not (n = 39) according to physician judgment. Demographic and pregnancy-specific characteristics were generally similar between the two groups.
In their statistical analysis, Dr. Enakpene and his colleagues used Kaplan-Meier survival analysis to look at pregnancy latency over time for women who did – or didn’t – receive a cerclage. There were significantly fewer spontaneous preterm births before 24, 28, and 34 weeks gestational age in the cerclage group (P less than .001 for all).
Dr. Enakpene acknowledged the study’s limitations, including its retrospective nature, the small sample size, and the fact that cerclage placement was done by the preference of the attending physician. However, this study was the first to examine rescue cerclage as add-on to vaginal progesterone, he said, adding, “Following this study, we are designing a prospective randomized interventional study to address this important topic.”
Dr. Enakpene reported that he had no conflicts of interest, and reported no outside sources of funding.
SOURCE: Enakpene C et al. Am J Obstet Gynecol. 2018 Jan;218:S72-S73.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Women receiving rescue cerclage plus progesterone had fewer spontaneous preterm births.
Major finding: Those who also received cerclage delivered at 34.3 weeks gestational age, compared with 27.5 weeks for those on progesterone alone (P less than .001).
Study details: Retrospective cohort study of 75 women with singleton pregnancies and very short cervixes.
Disclosures: Dr. Enakpene reported no outside sources of funding and had no conflicts of interest.
Source: Enakpene C et al. Am J Obstet Gynecol. 2018 Jan;218:S72-S73.