User login
Increasing Birth Weight Impacts Normal Labor Curve
SAN DIEGO – As birth weight increases, progression in labor was slower both in successful trial of labor patients and in patients who ultimately had cesarean deliveries.
The findings come from a retrospective review of electronic data from the Consortium on Safe Labor, an observational study of labor and delivery practices led by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the National Institutes of Health (NIH) that was conducted at 12 clinical centers from 2002 to 2008.
"Since the 1950s, obstetricians have been using the Friedman labor curve in order to assist in interpreting normal and abnormal labor patterns," lead study author Heidi K. Leftwich, D.O., said at the annual meeting of the American College of Obstetricians and Gynecologists.
"However, we have [a] very different patient population these days. There is more obesity, less active management of the second stage of labor, we use more epidurals, and we have an older population, with women waiting later to begin their families."
With the cesarean section rate escalating, she continued, "current research has been focusing on variables which might alter the labor curve, and challenging the notion that one labor curve can apply to all women."
The objective of the current study was to examine data from the Consortium on Safe Labor to determine whether birth weight alters the labor pattern in nulliparas and multiparas. Inclusion criteria consisted of patients with cephalic presentation, singleton gestation, gestational age of 34 weeks or more, who had undergone two or more cervical exams. Those patients with fetal anomalies, elective repeat cesarean section, and lacking birth weight data were excluded from the study.
The researchers created five birth weight categories separated by 500 g increments: less than 2,500 g (category 1), 2,500-2,999 g (category 2), 3,000-3,499 g (category 3), 3,500-3,999 g (category 4), and greater than or equal to 4,000 g (category 5). They used interval-censored regression to estimate the duration of labor, or "traverse times," and repeated measures analysis to construct mean labor curves by parity as well as by birth weight categories.
"The traverse times is more of an approximation of the time it takes for the cervix to dilate a centimeter," explained Dr. Leftwich, a fellow of maternal-fetal medicine in the department of obstetrics and gynecology at the University of Illinois at Chicago. "This is stratified by cervical dilation at admission, as well as exams performed in labor."
A total of 146,904 maternal records met inclusion criteria. Cesarean sections occurred in 21% of group 1, 14% of group 2, 14% of group 3, 17% of group 3, and 25% of group 5. Dr. Leftwich reported that in nulliparas, traverse times increased as birth weight increased, for both vaginal and cesarean deliveries (P less than .001). In multiparas, traverse times increased as birth weight increased from 5-8 cm dilation, for both vaginal and cesarean deliveries (P less than .001). "From 8 cm-10 cm, traverse times still increased by birth weight, but this was not statistically significant secondary to minimal cervical exams," Dr. Leftwich said.
A limitation of the study, she noted, was that "rapid progression of labor in multiparas makes traverse times less accurate for the active phase."
The study was supported by a contract from the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development and an award from the University of Illinois at Chicago Center for Clinical and Translational Science. Dr. Leftwich said that she had no relevant financial disclosures.
SAN DIEGO – As birth weight increases, progression in labor was slower both in successful trial of labor patients and in patients who ultimately had cesarean deliveries.
The findings come from a retrospective review of electronic data from the Consortium on Safe Labor, an observational study of labor and delivery practices led by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the National Institutes of Health (NIH) that was conducted at 12 clinical centers from 2002 to 2008.
"Since the 1950s, obstetricians have been using the Friedman labor curve in order to assist in interpreting normal and abnormal labor patterns," lead study author Heidi K. Leftwich, D.O., said at the annual meeting of the American College of Obstetricians and Gynecologists.
"However, we have [a] very different patient population these days. There is more obesity, less active management of the second stage of labor, we use more epidurals, and we have an older population, with women waiting later to begin their families."
With the cesarean section rate escalating, she continued, "current research has been focusing on variables which might alter the labor curve, and challenging the notion that one labor curve can apply to all women."
The objective of the current study was to examine data from the Consortium on Safe Labor to determine whether birth weight alters the labor pattern in nulliparas and multiparas. Inclusion criteria consisted of patients with cephalic presentation, singleton gestation, gestational age of 34 weeks or more, who had undergone two or more cervical exams. Those patients with fetal anomalies, elective repeat cesarean section, and lacking birth weight data were excluded from the study.
The researchers created five birth weight categories separated by 500 g increments: less than 2,500 g (category 1), 2,500-2,999 g (category 2), 3,000-3,499 g (category 3), 3,500-3,999 g (category 4), and greater than or equal to 4,000 g (category 5). They used interval-censored regression to estimate the duration of labor, or "traverse times," and repeated measures analysis to construct mean labor curves by parity as well as by birth weight categories.
"The traverse times is more of an approximation of the time it takes for the cervix to dilate a centimeter," explained Dr. Leftwich, a fellow of maternal-fetal medicine in the department of obstetrics and gynecology at the University of Illinois at Chicago. "This is stratified by cervical dilation at admission, as well as exams performed in labor."
A total of 146,904 maternal records met inclusion criteria. Cesarean sections occurred in 21% of group 1, 14% of group 2, 14% of group 3, 17% of group 3, and 25% of group 5. Dr. Leftwich reported that in nulliparas, traverse times increased as birth weight increased, for both vaginal and cesarean deliveries (P less than .001). In multiparas, traverse times increased as birth weight increased from 5-8 cm dilation, for both vaginal and cesarean deliveries (P less than .001). "From 8 cm-10 cm, traverse times still increased by birth weight, but this was not statistically significant secondary to minimal cervical exams," Dr. Leftwich said.
A limitation of the study, she noted, was that "rapid progression of labor in multiparas makes traverse times less accurate for the active phase."
The study was supported by a contract from the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development and an award from the University of Illinois at Chicago Center for Clinical and Translational Science. Dr. Leftwich said that she had no relevant financial disclosures.
SAN DIEGO – As birth weight increases, progression in labor was slower both in successful trial of labor patients and in patients who ultimately had cesarean deliveries.
The findings come from a retrospective review of electronic data from the Consortium on Safe Labor, an observational study of labor and delivery practices led by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the National Institutes of Health (NIH) that was conducted at 12 clinical centers from 2002 to 2008.
"Since the 1950s, obstetricians have been using the Friedman labor curve in order to assist in interpreting normal and abnormal labor patterns," lead study author Heidi K. Leftwich, D.O., said at the annual meeting of the American College of Obstetricians and Gynecologists.
"However, we have [a] very different patient population these days. There is more obesity, less active management of the second stage of labor, we use more epidurals, and we have an older population, with women waiting later to begin their families."
With the cesarean section rate escalating, she continued, "current research has been focusing on variables which might alter the labor curve, and challenging the notion that one labor curve can apply to all women."
The objective of the current study was to examine data from the Consortium on Safe Labor to determine whether birth weight alters the labor pattern in nulliparas and multiparas. Inclusion criteria consisted of patients with cephalic presentation, singleton gestation, gestational age of 34 weeks or more, who had undergone two or more cervical exams. Those patients with fetal anomalies, elective repeat cesarean section, and lacking birth weight data were excluded from the study.
The researchers created five birth weight categories separated by 500 g increments: less than 2,500 g (category 1), 2,500-2,999 g (category 2), 3,000-3,499 g (category 3), 3,500-3,999 g (category 4), and greater than or equal to 4,000 g (category 5). They used interval-censored regression to estimate the duration of labor, or "traverse times," and repeated measures analysis to construct mean labor curves by parity as well as by birth weight categories.
"The traverse times is more of an approximation of the time it takes for the cervix to dilate a centimeter," explained Dr. Leftwich, a fellow of maternal-fetal medicine in the department of obstetrics and gynecology at the University of Illinois at Chicago. "This is stratified by cervical dilation at admission, as well as exams performed in labor."
A total of 146,904 maternal records met inclusion criteria. Cesarean sections occurred in 21% of group 1, 14% of group 2, 14% of group 3, 17% of group 3, and 25% of group 5. Dr. Leftwich reported that in nulliparas, traverse times increased as birth weight increased, for both vaginal and cesarean deliveries (P less than .001). In multiparas, traverse times increased as birth weight increased from 5-8 cm dilation, for both vaginal and cesarean deliveries (P less than .001). "From 8 cm-10 cm, traverse times still increased by birth weight, but this was not statistically significant secondary to minimal cervical exams," Dr. Leftwich said.
A limitation of the study, she noted, was that "rapid progression of labor in multiparas makes traverse times less accurate for the active phase."
The study was supported by a contract from the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development and an award from the University of Illinois at Chicago Center for Clinical and Translational Science. Dr. Leftwich said that she had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: In nulliparas, traverse times increased as birth weight increased, for both vaginal and cesarean deliveries (P less than .001). In multiparas, traverse times increased as birth weight increased from 5-8 cm dilation, for both vaginal and cesarean deliveries (P less than .001).
Data Source: Data was from an analysis of 146,904 maternal records from the Consortium on Safe Labor, an observational study of labor and delivery practices conducted from 2002 to 2008.
Disclosures: The study was supported by a contract from the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development and an award from the University of Illinois at Chicago Center for Clinical and Translational Science. Dr. Leftwich said that she had no relevant financial disclosures.
Weight a Factor in Risky Sexual Behaviors of Adolescent Females
SAN DIEGO – The reasons why overweight and obese adolescent females are more likely to engage in risky sexual behaviors compared with their normal weight peers remain unclear, results from a large national study demonstrated.
Although previous studies have shown that overweight and obese adolescent females are more likely than their normal weight peers to have intercourse before age 13, have multiple sexual partners, and are less likely to use contraception, "they only imply association; they do not offer any insight into motivations and the underlying actions," Dr. Erin M. Swanson said at the annual meeting of the American College of Obstetricians and Gynecologists. "Our objective was to examine the association of weight with sexual practices, perceptions of sex, and motivations for contraception among adolescent females."
Dr. Swanson of the department of obstetrics and gynecology at Medical University of South Carolina, Charleston, and her associates performed a cross-sectional analysis of data from wave 1 of the National Longitudinal Study of Adolescent Health, which involved in-home interviews with 3,356 females in grades 7-12 during the 1994-95 school year. The interviews were 1-2 hours long and focused on survey questions regarding sexual perceptions and behaviors in adolescent females.
Dr. Swanson and her associates categorized study participants into three body mass index percentile categories: less than 85% of expected (normal weight), 85%-95% of expected (overweight), and greater than 95% of expected (obese). Self-esteem was divided into two categories: normal or low based on responses to the Rosenberg self-esteem scale, a validated instrument.
At baseline, the mean age of the females was 15 years, 71% were white, 16% were black, and 13% were Hispanic. In addition, 15% were overweight, 8% were obese, 18% met criteria for low self-esteem, and 37% reported having sexual intercourse. Of those who reported having intercourse, 76% reported being over age 13 at the time.
More than one in five overweight females (22%) and 23% of obese females had low self-esteem, compared with 17% of their normal weight peers, a difference that reached statistical significance (P = .03).
Logistic regression analysis revealed that, compared with their normal weight peers, overweight and obese females were more likely to have sexual intercourse before age 13 (odds ratio, 1.3 and OR, 2.1, respectively), become pregnant (OR, 1.8 and OR, 2.3), and less likely to use oral contraception regularly (OR, 0.44 and OR, 0.28).
In addition, obese females were 1.9 times more likely to have been forced to have sex, compared with their normal weight peers.
"Both race and self-esteem were evaluated as possible cofounders and determined to have no effect on the logistic regression model for the reported behaviors," Dr. Swanson said. "Interestingly, the rate of reported gonorrhea and chlamydia did not differ between weight classes."
When asked about their motivations to engage in sex, a significantly higher proportion of overweight and obese females compared with their normal weight peers chose the response option "your friends would respect you more" (P = .01), which suggests a peer influence, Dr. Swanson commented. "Interestingly, when these answers were compared with self-esteem, there was no difference [between weight groups]," she said.
When asked about their motivations to use birth control, a significantly higher proportion of overweight and obese females compared with their normal weight peers chose the response options "birth control is too much of a hassle to use" and "it is hard to get a boy to use birth control with you" (P = .01 for both).
While the motivation for overweight and obese females to engage in risky sexual behaviors remains unclear, "our findings suggest that peer influence may be significant," Dr. Swanson said. "An adolescent’s decision to engage in sex is likely multi-factorial, influenced by more than self-esteem and body image."
She went on to note that overweight and obese adolescent females "should be considered a vulnerable population. Clinicians should identify these patients and spend time exploring their thoughts about themselves, their peers, and their decisions to engage in sexual behaviors. It is our job to give accurate information, screen for and treat sexually transmitted infections, provide contraception, encourage parental involvement and, if needed, give good prenatal care. We as obstetricians and gynecologists have a unique opportunity and responsibility to care for, educate, and give feedback to adolescent girls to improve their overall sexual health."
Dr. Swanson said that she had no relevant financial conflicts to disclose.
SAN DIEGO – The reasons why overweight and obese adolescent females are more likely to engage in risky sexual behaviors compared with their normal weight peers remain unclear, results from a large national study demonstrated.
Although previous studies have shown that overweight and obese adolescent females are more likely than their normal weight peers to have intercourse before age 13, have multiple sexual partners, and are less likely to use contraception, "they only imply association; they do not offer any insight into motivations and the underlying actions," Dr. Erin M. Swanson said at the annual meeting of the American College of Obstetricians and Gynecologists. "Our objective was to examine the association of weight with sexual practices, perceptions of sex, and motivations for contraception among adolescent females."
Dr. Swanson of the department of obstetrics and gynecology at Medical University of South Carolina, Charleston, and her associates performed a cross-sectional analysis of data from wave 1 of the National Longitudinal Study of Adolescent Health, which involved in-home interviews with 3,356 females in grades 7-12 during the 1994-95 school year. The interviews were 1-2 hours long and focused on survey questions regarding sexual perceptions and behaviors in adolescent females.
Dr. Swanson and her associates categorized study participants into three body mass index percentile categories: less than 85% of expected (normal weight), 85%-95% of expected (overweight), and greater than 95% of expected (obese). Self-esteem was divided into two categories: normal or low based on responses to the Rosenberg self-esteem scale, a validated instrument.
At baseline, the mean age of the females was 15 years, 71% were white, 16% were black, and 13% were Hispanic. In addition, 15% were overweight, 8% were obese, 18% met criteria for low self-esteem, and 37% reported having sexual intercourse. Of those who reported having intercourse, 76% reported being over age 13 at the time.
More than one in five overweight females (22%) and 23% of obese females had low self-esteem, compared with 17% of their normal weight peers, a difference that reached statistical significance (P = .03).
Logistic regression analysis revealed that, compared with their normal weight peers, overweight and obese females were more likely to have sexual intercourse before age 13 (odds ratio, 1.3 and OR, 2.1, respectively), become pregnant (OR, 1.8 and OR, 2.3), and less likely to use oral contraception regularly (OR, 0.44 and OR, 0.28).
In addition, obese females were 1.9 times more likely to have been forced to have sex, compared with their normal weight peers.
"Both race and self-esteem were evaluated as possible cofounders and determined to have no effect on the logistic regression model for the reported behaviors," Dr. Swanson said. "Interestingly, the rate of reported gonorrhea and chlamydia did not differ between weight classes."
When asked about their motivations to engage in sex, a significantly higher proportion of overweight and obese females compared with their normal weight peers chose the response option "your friends would respect you more" (P = .01), which suggests a peer influence, Dr. Swanson commented. "Interestingly, when these answers were compared with self-esteem, there was no difference [between weight groups]," she said.
When asked about their motivations to use birth control, a significantly higher proportion of overweight and obese females compared with their normal weight peers chose the response options "birth control is too much of a hassle to use" and "it is hard to get a boy to use birth control with you" (P = .01 for both).
While the motivation for overweight and obese females to engage in risky sexual behaviors remains unclear, "our findings suggest that peer influence may be significant," Dr. Swanson said. "An adolescent’s decision to engage in sex is likely multi-factorial, influenced by more than self-esteem and body image."
She went on to note that overweight and obese adolescent females "should be considered a vulnerable population. Clinicians should identify these patients and spend time exploring their thoughts about themselves, their peers, and their decisions to engage in sexual behaviors. It is our job to give accurate information, screen for and treat sexually transmitted infections, provide contraception, encourage parental involvement and, if needed, give good prenatal care. We as obstetricians and gynecologists have a unique opportunity and responsibility to care for, educate, and give feedback to adolescent girls to improve their overall sexual health."
Dr. Swanson said that she had no relevant financial conflicts to disclose.
SAN DIEGO – The reasons why overweight and obese adolescent females are more likely to engage in risky sexual behaviors compared with their normal weight peers remain unclear, results from a large national study demonstrated.
Although previous studies have shown that overweight and obese adolescent females are more likely than their normal weight peers to have intercourse before age 13, have multiple sexual partners, and are less likely to use contraception, "they only imply association; they do not offer any insight into motivations and the underlying actions," Dr. Erin M. Swanson said at the annual meeting of the American College of Obstetricians and Gynecologists. "Our objective was to examine the association of weight with sexual practices, perceptions of sex, and motivations for contraception among adolescent females."
Dr. Swanson of the department of obstetrics and gynecology at Medical University of South Carolina, Charleston, and her associates performed a cross-sectional analysis of data from wave 1 of the National Longitudinal Study of Adolescent Health, which involved in-home interviews with 3,356 females in grades 7-12 during the 1994-95 school year. The interviews were 1-2 hours long and focused on survey questions regarding sexual perceptions and behaviors in adolescent females.
Dr. Swanson and her associates categorized study participants into three body mass index percentile categories: less than 85% of expected (normal weight), 85%-95% of expected (overweight), and greater than 95% of expected (obese). Self-esteem was divided into two categories: normal or low based on responses to the Rosenberg self-esteem scale, a validated instrument.
At baseline, the mean age of the females was 15 years, 71% were white, 16% were black, and 13% were Hispanic. In addition, 15% were overweight, 8% were obese, 18% met criteria for low self-esteem, and 37% reported having sexual intercourse. Of those who reported having intercourse, 76% reported being over age 13 at the time.
More than one in five overweight females (22%) and 23% of obese females had low self-esteem, compared with 17% of their normal weight peers, a difference that reached statistical significance (P = .03).
Logistic regression analysis revealed that, compared with their normal weight peers, overweight and obese females were more likely to have sexual intercourse before age 13 (odds ratio, 1.3 and OR, 2.1, respectively), become pregnant (OR, 1.8 and OR, 2.3), and less likely to use oral contraception regularly (OR, 0.44 and OR, 0.28).
In addition, obese females were 1.9 times more likely to have been forced to have sex, compared with their normal weight peers.
"Both race and self-esteem were evaluated as possible cofounders and determined to have no effect on the logistic regression model for the reported behaviors," Dr. Swanson said. "Interestingly, the rate of reported gonorrhea and chlamydia did not differ between weight classes."
When asked about their motivations to engage in sex, a significantly higher proportion of overweight and obese females compared with their normal weight peers chose the response option "your friends would respect you more" (P = .01), which suggests a peer influence, Dr. Swanson commented. "Interestingly, when these answers were compared with self-esteem, there was no difference [between weight groups]," she said.
When asked about their motivations to use birth control, a significantly higher proportion of overweight and obese females compared with their normal weight peers chose the response options "birth control is too much of a hassle to use" and "it is hard to get a boy to use birth control with you" (P = .01 for both).
While the motivation for overweight and obese females to engage in risky sexual behaviors remains unclear, "our findings suggest that peer influence may be significant," Dr. Swanson said. "An adolescent’s decision to engage in sex is likely multi-factorial, influenced by more than self-esteem and body image."
She went on to note that overweight and obese adolescent females "should be considered a vulnerable population. Clinicians should identify these patients and spend time exploring their thoughts about themselves, their peers, and their decisions to engage in sexual behaviors. It is our job to give accurate information, screen for and treat sexually transmitted infections, provide contraception, encourage parental involvement and, if needed, give good prenatal care. We as obstetricians and gynecologists have a unique opportunity and responsibility to care for, educate, and give feedback to adolescent girls to improve their overall sexual health."
Dr. Swanson said that she had no relevant financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: Compared with their normal weight peers, overweight and obese adolescent females were more likely to have sexual intercourse before age 13 (odds ratio, 1.3 and OR, 2.1, respectively), become pregnant (OR, 1.8 and OR, 2.3), and less likely to use oral contraception regularly (OR, 0.44 and OR, 0.28).
Data Source: Analysis of data from wave 1 of the National Longitudinal Study of Adolescent Health, which involved in-home interviews with 3,356 females in grades 7-12 during the 1994-1995 school year.
Disclosures: Dr. Swanson said that she had no relevant financial conflicts to disclose.
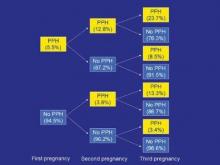
Prior Postpartum Hemorrhage Raises Risk of Another
MONTEREY, CALIF. – Women have a substantially elevated risk of postpartum hemorrhage after a first occurrence, a prospective population-based cohort study has shown.
The study of more than half a million primiparas and roughly 1 million deliveries in Sweden found that women who had postpartum hemorrhage in their first pregnancy were more than three times as likely to have this complication again in their second pregnancy. Risk increased with the severity of hemorrhage in the first pregnancy and with the number of affected pregnancies.
In additional findings, a history of postpartum hemorrhage due to one etiology, for example, uterine atony or retained placenta, increased the risk not only of a recurrence of hemorrhage due to the same etiology but also of occurrence of hemorrhage due to other etiologies.
"The fact that a history of postpartum hemorrhage of one subtype confers risk of other subtypes in a subsequent pregnancy suggests that there are likely shared pathological features across the different etiologies, and I think this is going to be a very interesting area to examine in the future," commented lead investigator Dr. Brian T. Bateman, an anesthesiologist at Harvard Medical School, Boston, at the annual meeting of the Society for Obstetric Anesthesia and Perinatology.
"We could speculate that it might be undiagnosed coagulopathy that explains the shared risk or perhaps characteristics of labor, placentation, or other factors. Given the strong pattern of recurrence, perhaps these are even genetic in nature," he added.
In upcoming research, the investigators will look further into possible explanations. "We are planning to collect a series of women with recurrent hemorrhage, particularly women with hemorrhage from discordant causes, and examine in real granular detail what might be mediating these effects that we are observing at the population level," Dr. Bateman explained. "We are also in the process of conducting familial aggregation studies to determine whether there is a genetic component to postpartum hemorrhage risk."
Session attendee Dr. Richard M. Smiley of Columbia University in New York questioned the reliability of coding of postpartum hemorrhage etiologies in the register used for the study. "It’s really intriguing, the cross-risk, if you will. ... With all due respect to the Swedish database, what’s the chance that that is just miscoded – that a woman bleeds maybe from the same cause, but someone needs to put a cause down on the chart or in the coding system, and they have to pick something, and they pick the wrong thing?" he asked.
"There was a study out of the same database last year looking at the role of obesity as a risk factor for postpartum hemorrhage, and they found when they looked at the risk of postpartum hemorrhage from retained placenta or from laceration, there was no effect of BMI in those categories, but a very, very strong effect on risk of atony, suggesting that there is some specificity in the way that these codes are being applied," Dr. Bateman replied.
Previous research has shown that postpartum hemorrhage is a risk factor for the same complication in subsequent pregnancies, he noted, giving some background to the study. However, "less is known about whether risk accumulates with multiple affected pregnancies and whether the severity of prior postpartum hemorrhage has additional predictive value, and if risk of recurrence varies according to postpartum hemorrhage subtype."
The investigators analyzed data from the Swedish Medical Birth Register. They included 538,332 primiparous women who delivered between 1997 and 2009, and followed this group through 2009, identifying a total of 914,933 subsequent deliveries.
Overall, 5.5% of the women had physician-diagnosed postpartum hemorrhage (an estimated blood loss of greater than 1 L) in their first pregnancy. The rate of this complication in a second pregnancy was higher when the first pregnancy was affected, and the rate was especially high in a third pregnancy when both a first and second pregnancy were affected.
Relative to their counterparts who did not have postpartum hemorrhage in their first pregnancy, women who had postpartum hemorrhage that was not severe, meaning it did not require transfusion, had increased risks of both nonsevere and severe postpartum hemorrhage in a second pregnancy (relative risk, 3.2 and 3.4, respectively).
The respective elevations of risks were even greater in women who had severe postpartum hemorrhage in their first pregnancy (RR, 4.2 and 6.9), "suggesting that severity of hemorrhage does add additional predictive value and can be potentially helpful in triaging high-risk patients," Dr. Bateman said.
Additional analyses showed that postpartum hemorrhage in the first pregnancy due to one etiology increased the risk of postpartum hemorrhage in the second pregnancy due to both that etiology and others. "These findings are really quite surprising and are novel," he commented.
For example, women who had hemorrhage due to uterine atony in their first pregnancy had a 3.9-fold higher risk of hemorrhage due to uterine atony in their second pregnancy. But they also had increased risks of postpartum hemorrhage due to retained placenta (3.1-fold), laceration (1.7-fold), and delayed postpartum hemorrhage (1.8-fold).
When the investigators repeated analyses but excluded women with stable risk factors that might be present across the reproductive years, such as fibroids, inherited coagulopathy, and cesarean delivery, the elevated risks of a recurrence of postpartum hemorrhage were essentially unchanged. "This argues that recurrence is mediated by some other factor," maintained Dr. Bateman.
Dr. Bateman disclosed that he had no conflicts of interest related to the research.
MONTEREY, CALIF. – Women have a substantially elevated risk of postpartum hemorrhage after a first occurrence, a prospective population-based cohort study has shown.
The study of more than half a million primiparas and roughly 1 million deliveries in Sweden found that women who had postpartum hemorrhage in their first pregnancy were more than three times as likely to have this complication again in their second pregnancy. Risk increased with the severity of hemorrhage in the first pregnancy and with the number of affected pregnancies.
In additional findings, a history of postpartum hemorrhage due to one etiology, for example, uterine atony or retained placenta, increased the risk not only of a recurrence of hemorrhage due to the same etiology but also of occurrence of hemorrhage due to other etiologies.
"The fact that a history of postpartum hemorrhage of one subtype confers risk of other subtypes in a subsequent pregnancy suggests that there are likely shared pathological features across the different etiologies, and I think this is going to be a very interesting area to examine in the future," commented lead investigator Dr. Brian T. Bateman, an anesthesiologist at Harvard Medical School, Boston, at the annual meeting of the Society for Obstetric Anesthesia and Perinatology.
"We could speculate that it might be undiagnosed coagulopathy that explains the shared risk or perhaps characteristics of labor, placentation, or other factors. Given the strong pattern of recurrence, perhaps these are even genetic in nature," he added.
In upcoming research, the investigators will look further into possible explanations. "We are planning to collect a series of women with recurrent hemorrhage, particularly women with hemorrhage from discordant causes, and examine in real granular detail what might be mediating these effects that we are observing at the population level," Dr. Bateman explained. "We are also in the process of conducting familial aggregation studies to determine whether there is a genetic component to postpartum hemorrhage risk."
Session attendee Dr. Richard M. Smiley of Columbia University in New York questioned the reliability of coding of postpartum hemorrhage etiologies in the register used for the study. "It’s really intriguing, the cross-risk, if you will. ... With all due respect to the Swedish database, what’s the chance that that is just miscoded – that a woman bleeds maybe from the same cause, but someone needs to put a cause down on the chart or in the coding system, and they have to pick something, and they pick the wrong thing?" he asked.
"There was a study out of the same database last year looking at the role of obesity as a risk factor for postpartum hemorrhage, and they found when they looked at the risk of postpartum hemorrhage from retained placenta or from laceration, there was no effect of BMI in those categories, but a very, very strong effect on risk of atony, suggesting that there is some specificity in the way that these codes are being applied," Dr. Bateman replied.
Previous research has shown that postpartum hemorrhage is a risk factor for the same complication in subsequent pregnancies, he noted, giving some background to the study. However, "less is known about whether risk accumulates with multiple affected pregnancies and whether the severity of prior postpartum hemorrhage has additional predictive value, and if risk of recurrence varies according to postpartum hemorrhage subtype."
The investigators analyzed data from the Swedish Medical Birth Register. They included 538,332 primiparous women who delivered between 1997 and 2009, and followed this group through 2009, identifying a total of 914,933 subsequent deliveries.
Overall, 5.5% of the women had physician-diagnosed postpartum hemorrhage (an estimated blood loss of greater than 1 L) in their first pregnancy. The rate of this complication in a second pregnancy was higher when the first pregnancy was affected, and the rate was especially high in a third pregnancy when both a first and second pregnancy were affected.
Relative to their counterparts who did not have postpartum hemorrhage in their first pregnancy, women who had postpartum hemorrhage that was not severe, meaning it did not require transfusion, had increased risks of both nonsevere and severe postpartum hemorrhage in a second pregnancy (relative risk, 3.2 and 3.4, respectively).
The respective elevations of risks were even greater in women who had severe postpartum hemorrhage in their first pregnancy (RR, 4.2 and 6.9), "suggesting that severity of hemorrhage does add additional predictive value and can be potentially helpful in triaging high-risk patients," Dr. Bateman said.
Additional analyses showed that postpartum hemorrhage in the first pregnancy due to one etiology increased the risk of postpartum hemorrhage in the second pregnancy due to both that etiology and others. "These findings are really quite surprising and are novel," he commented.
For example, women who had hemorrhage due to uterine atony in their first pregnancy had a 3.9-fold higher risk of hemorrhage due to uterine atony in their second pregnancy. But they also had increased risks of postpartum hemorrhage due to retained placenta (3.1-fold), laceration (1.7-fold), and delayed postpartum hemorrhage (1.8-fold).
When the investigators repeated analyses but excluded women with stable risk factors that might be present across the reproductive years, such as fibroids, inherited coagulopathy, and cesarean delivery, the elevated risks of a recurrence of postpartum hemorrhage were essentially unchanged. "This argues that recurrence is mediated by some other factor," maintained Dr. Bateman.
Dr. Bateman disclosed that he had no conflicts of interest related to the research.
MONTEREY, CALIF. – Women have a substantially elevated risk of postpartum hemorrhage after a first occurrence, a prospective population-based cohort study has shown.
The study of more than half a million primiparas and roughly 1 million deliveries in Sweden found that women who had postpartum hemorrhage in their first pregnancy were more than three times as likely to have this complication again in their second pregnancy. Risk increased with the severity of hemorrhage in the first pregnancy and with the number of affected pregnancies.
In additional findings, a history of postpartum hemorrhage due to one etiology, for example, uterine atony or retained placenta, increased the risk not only of a recurrence of hemorrhage due to the same etiology but also of occurrence of hemorrhage due to other etiologies.
"The fact that a history of postpartum hemorrhage of one subtype confers risk of other subtypes in a subsequent pregnancy suggests that there are likely shared pathological features across the different etiologies, and I think this is going to be a very interesting area to examine in the future," commented lead investigator Dr. Brian T. Bateman, an anesthesiologist at Harvard Medical School, Boston, at the annual meeting of the Society for Obstetric Anesthesia and Perinatology.
"We could speculate that it might be undiagnosed coagulopathy that explains the shared risk or perhaps characteristics of labor, placentation, or other factors. Given the strong pattern of recurrence, perhaps these are even genetic in nature," he added.
In upcoming research, the investigators will look further into possible explanations. "We are planning to collect a series of women with recurrent hemorrhage, particularly women with hemorrhage from discordant causes, and examine in real granular detail what might be mediating these effects that we are observing at the population level," Dr. Bateman explained. "We are also in the process of conducting familial aggregation studies to determine whether there is a genetic component to postpartum hemorrhage risk."
Session attendee Dr. Richard M. Smiley of Columbia University in New York questioned the reliability of coding of postpartum hemorrhage etiologies in the register used for the study. "It’s really intriguing, the cross-risk, if you will. ... With all due respect to the Swedish database, what’s the chance that that is just miscoded – that a woman bleeds maybe from the same cause, but someone needs to put a cause down on the chart or in the coding system, and they have to pick something, and they pick the wrong thing?" he asked.
"There was a study out of the same database last year looking at the role of obesity as a risk factor for postpartum hemorrhage, and they found when they looked at the risk of postpartum hemorrhage from retained placenta or from laceration, there was no effect of BMI in those categories, but a very, very strong effect on risk of atony, suggesting that there is some specificity in the way that these codes are being applied," Dr. Bateman replied.
Previous research has shown that postpartum hemorrhage is a risk factor for the same complication in subsequent pregnancies, he noted, giving some background to the study. However, "less is known about whether risk accumulates with multiple affected pregnancies and whether the severity of prior postpartum hemorrhage has additional predictive value, and if risk of recurrence varies according to postpartum hemorrhage subtype."
The investigators analyzed data from the Swedish Medical Birth Register. They included 538,332 primiparous women who delivered between 1997 and 2009, and followed this group through 2009, identifying a total of 914,933 subsequent deliveries.
Overall, 5.5% of the women had physician-diagnosed postpartum hemorrhage (an estimated blood loss of greater than 1 L) in their first pregnancy. The rate of this complication in a second pregnancy was higher when the first pregnancy was affected, and the rate was especially high in a third pregnancy when both a first and second pregnancy were affected.
Relative to their counterparts who did not have postpartum hemorrhage in their first pregnancy, women who had postpartum hemorrhage that was not severe, meaning it did not require transfusion, had increased risks of both nonsevere and severe postpartum hemorrhage in a second pregnancy (relative risk, 3.2 and 3.4, respectively).
The respective elevations of risks were even greater in women who had severe postpartum hemorrhage in their first pregnancy (RR, 4.2 and 6.9), "suggesting that severity of hemorrhage does add additional predictive value and can be potentially helpful in triaging high-risk patients," Dr. Bateman said.
Additional analyses showed that postpartum hemorrhage in the first pregnancy due to one etiology increased the risk of postpartum hemorrhage in the second pregnancy due to both that etiology and others. "These findings are really quite surprising and are novel," he commented.
For example, women who had hemorrhage due to uterine atony in their first pregnancy had a 3.9-fold higher risk of hemorrhage due to uterine atony in their second pregnancy. But they also had increased risks of postpartum hemorrhage due to retained placenta (3.1-fold), laceration (1.7-fold), and delayed postpartum hemorrhage (1.8-fold).
When the investigators repeated analyses but excluded women with stable risk factors that might be present across the reproductive years, such as fibroids, inherited coagulopathy, and cesarean delivery, the elevated risks of a recurrence of postpartum hemorrhage were essentially unchanged. "This argues that recurrence is mediated by some other factor," maintained Dr. Bateman.
Dr. Bateman disclosed that he had no conflicts of interest related to the research.
FROM THE ANNUAL MEETING OF THE SOCIETY FOR OBSTETRIC ANESTHESIA AND PERINATOLOGY
New Model Developed for Identifying Placenta Accreta
MONTEREY, CALIF. – A new model may help take the guesswork out of identifying placenta accreta before cesarean delivery, possibly sparing some women unnecessary interventions such as general anesthesia, placement of large-bore IV lines, and elective hysterectomy.
A study team led by Dr. Carolyn F. Weiniger, an obstetrical anesthesiologist at the Hadassah Hebrew University Medical Center in Jerusalem, reviewed data for 46,623 women who were delivered at the center over a 9-year period.
They identified 92 women with antenatally suspected placenta accreta, of whom only 52 (56%) were confirmed to have had the condition at the time of surgery, she reported at the annual meeting of the Society for Obstetric Anesthesia and Perinatology.
At a maximal-sensitivity cut-off, a predictive model based on just three clinical factors that would be assessed in any woman evaluated for suspected placenta accreta – the presence of placenta previa (yes vs. no), the number of previous cesarean deliveries, and ultrasound suspicion of accreta (high vs. low) – identified 100% of the women who were confirmed to have the condition. The trade-off was a low specificity of 25%.
However, at the optimal cut-off, the model still identified 94% of the women who were confirmed to have placenta accreta, and specificity was better (53%).
The investigators developed a nomogram based on the model that should be easy to apply clinically, according to Dr. Weiniger. "This nomogram could be a laminated card which a physician could sit with at his desk when faced with a suspected placenta accreta patient, to decide whether she is above or below our cut point, whether we think she actually does or does not have placenta accreta," she explained.
Although the study involves one of the largest series of patients with placenta accreta, it still had a fairly small sample size, she acknowledged. "In order to validate such data, a multicenter study would be appropriate."
"Have you changed your practice ... based on your nomogram?" asked Dr. Vilma E. Ortiz, session moderator and an anesthesiologist at the Massachusetts General Hospital in Boston.
"We have just created the nomogram, just finished analyzing the statistics. We haven’t yet had an accreta patient," Dr. Weiniger replied. "But I think as we become much more experienced at managing these patients, in patients who we feel comfortable [that they] have got no risk or low suspicion [of accreta], we will do regional anesthesia."
During the study period, her center’s management in cases of suspected accreta typically included general anesthesia, the booking of an ICU bed, the insertion of two large-bore IVs, and the placement of loops on the internal iliac vessels to aid with hemostasis. It did not include planned cesarean hysterectomy.
"Surgeons were not aware of our primary study outcome [that is, the rate of surgically diagnosed accreta among all cases of antenatally suspected accreta] in order to avoid bias," she noted.
A comparison of the 52 women with and 40 women without surgically confirmed accreta showed that they were statistically indistinguishable with respect to many clinical factors. But they differed significantly on the number of previous cesarean deliveries, the presence of placenta previa, and the presence of ultrasound signs of accreta.
The predictive model based on these three factors had an area under the receiver operating characteristic curve of 0.846, according to Dr. Weiniger. "When we tried to add maternal age and antenatal bleeding, because [these factors have been found to be predictive] in previous studies, it did not improve the area under the curve."
Giving some examples using the new nomogram, she noted that a woman having two previous cesarean deliveries who has placenta previa and a high-suspicion ultrasound would have a probability score approaching 80%, which falls well above cut points based on both 100% and 94% model sensitivity. "So she would be classified as having placenta accreta and would require massive hemorrhage preparation for surgery."
In contrast, a woman having two previous cesarean deliveries who does not have placenta previa and has a low-suspicion ultrasound would have a probability score of almost 0%, which falls well below the cut points, and she would be classified as not having placenta accreta. "So we could manage her with regional anesthesia and maybe not do preparations for massive hemorrhage," Dr. Weiniger commented.
Finally, a woman having two previous cesarean deliveries who has a low-suspicion ultrasound but does have placenta previa would have a probability score of about 20%. This score falls above the cut point corresponding to 100% sensitivity, "so if that was the clinician’s practice, that patient would have massive hemorrhage preparations," she said. "But if we were using the 94% sensitivity, the optimal cut point, she would be right on that, so it would be equivocal as to whether we would classify her as having massive transfusion requirements or not. Possibly, the state of her airway would define how we would manage such a patient."
Dr. Weiniger disclosed no relevant conflicts of interest.
MONTEREY, CALIF. – A new model may help take the guesswork out of identifying placenta accreta before cesarean delivery, possibly sparing some women unnecessary interventions such as general anesthesia, placement of large-bore IV lines, and elective hysterectomy.
A study team led by Dr. Carolyn F. Weiniger, an obstetrical anesthesiologist at the Hadassah Hebrew University Medical Center in Jerusalem, reviewed data for 46,623 women who were delivered at the center over a 9-year period.
They identified 92 women with antenatally suspected placenta accreta, of whom only 52 (56%) were confirmed to have had the condition at the time of surgery, she reported at the annual meeting of the Society for Obstetric Anesthesia and Perinatology.
At a maximal-sensitivity cut-off, a predictive model based on just three clinical factors that would be assessed in any woman evaluated for suspected placenta accreta – the presence of placenta previa (yes vs. no), the number of previous cesarean deliveries, and ultrasound suspicion of accreta (high vs. low) – identified 100% of the women who were confirmed to have the condition. The trade-off was a low specificity of 25%.
However, at the optimal cut-off, the model still identified 94% of the women who were confirmed to have placenta accreta, and specificity was better (53%).
The investigators developed a nomogram based on the model that should be easy to apply clinically, according to Dr. Weiniger. "This nomogram could be a laminated card which a physician could sit with at his desk when faced with a suspected placenta accreta patient, to decide whether she is above or below our cut point, whether we think she actually does or does not have placenta accreta," she explained.
Although the study involves one of the largest series of patients with placenta accreta, it still had a fairly small sample size, she acknowledged. "In order to validate such data, a multicenter study would be appropriate."
"Have you changed your practice ... based on your nomogram?" asked Dr. Vilma E. Ortiz, session moderator and an anesthesiologist at the Massachusetts General Hospital in Boston.
"We have just created the nomogram, just finished analyzing the statistics. We haven’t yet had an accreta patient," Dr. Weiniger replied. "But I think as we become much more experienced at managing these patients, in patients who we feel comfortable [that they] have got no risk or low suspicion [of accreta], we will do regional anesthesia."
During the study period, her center’s management in cases of suspected accreta typically included general anesthesia, the booking of an ICU bed, the insertion of two large-bore IVs, and the placement of loops on the internal iliac vessels to aid with hemostasis. It did not include planned cesarean hysterectomy.
"Surgeons were not aware of our primary study outcome [that is, the rate of surgically diagnosed accreta among all cases of antenatally suspected accreta] in order to avoid bias," she noted.
A comparison of the 52 women with and 40 women without surgically confirmed accreta showed that they were statistically indistinguishable with respect to many clinical factors. But they differed significantly on the number of previous cesarean deliveries, the presence of placenta previa, and the presence of ultrasound signs of accreta.
The predictive model based on these three factors had an area under the receiver operating characteristic curve of 0.846, according to Dr. Weiniger. "When we tried to add maternal age and antenatal bleeding, because [these factors have been found to be predictive] in previous studies, it did not improve the area under the curve."
Giving some examples using the new nomogram, she noted that a woman having two previous cesarean deliveries who has placenta previa and a high-suspicion ultrasound would have a probability score approaching 80%, which falls well above cut points based on both 100% and 94% model sensitivity. "So she would be classified as having placenta accreta and would require massive hemorrhage preparation for surgery."
In contrast, a woman having two previous cesarean deliveries who does not have placenta previa and has a low-suspicion ultrasound would have a probability score of almost 0%, which falls well below the cut points, and she would be classified as not having placenta accreta. "So we could manage her with regional anesthesia and maybe not do preparations for massive hemorrhage," Dr. Weiniger commented.
Finally, a woman having two previous cesarean deliveries who has a low-suspicion ultrasound but does have placenta previa would have a probability score of about 20%. This score falls above the cut point corresponding to 100% sensitivity, "so if that was the clinician’s practice, that patient would have massive hemorrhage preparations," she said. "But if we were using the 94% sensitivity, the optimal cut point, she would be right on that, so it would be equivocal as to whether we would classify her as having massive transfusion requirements or not. Possibly, the state of her airway would define how we would manage such a patient."
Dr. Weiniger disclosed no relevant conflicts of interest.
MONTEREY, CALIF. – A new model may help take the guesswork out of identifying placenta accreta before cesarean delivery, possibly sparing some women unnecessary interventions such as general anesthesia, placement of large-bore IV lines, and elective hysterectomy.
A study team led by Dr. Carolyn F. Weiniger, an obstetrical anesthesiologist at the Hadassah Hebrew University Medical Center in Jerusalem, reviewed data for 46,623 women who were delivered at the center over a 9-year period.
They identified 92 women with antenatally suspected placenta accreta, of whom only 52 (56%) were confirmed to have had the condition at the time of surgery, she reported at the annual meeting of the Society for Obstetric Anesthesia and Perinatology.
At a maximal-sensitivity cut-off, a predictive model based on just three clinical factors that would be assessed in any woman evaluated for suspected placenta accreta – the presence of placenta previa (yes vs. no), the number of previous cesarean deliveries, and ultrasound suspicion of accreta (high vs. low) – identified 100% of the women who were confirmed to have the condition. The trade-off was a low specificity of 25%.
However, at the optimal cut-off, the model still identified 94% of the women who were confirmed to have placenta accreta, and specificity was better (53%).
The investigators developed a nomogram based on the model that should be easy to apply clinically, according to Dr. Weiniger. "This nomogram could be a laminated card which a physician could sit with at his desk when faced with a suspected placenta accreta patient, to decide whether she is above or below our cut point, whether we think she actually does or does not have placenta accreta," she explained.
Although the study involves one of the largest series of patients with placenta accreta, it still had a fairly small sample size, she acknowledged. "In order to validate such data, a multicenter study would be appropriate."
"Have you changed your practice ... based on your nomogram?" asked Dr. Vilma E. Ortiz, session moderator and an anesthesiologist at the Massachusetts General Hospital in Boston.
"We have just created the nomogram, just finished analyzing the statistics. We haven’t yet had an accreta patient," Dr. Weiniger replied. "But I think as we become much more experienced at managing these patients, in patients who we feel comfortable [that they] have got no risk or low suspicion [of accreta], we will do regional anesthesia."
During the study period, her center’s management in cases of suspected accreta typically included general anesthesia, the booking of an ICU bed, the insertion of two large-bore IVs, and the placement of loops on the internal iliac vessels to aid with hemostasis. It did not include planned cesarean hysterectomy.
"Surgeons were not aware of our primary study outcome [that is, the rate of surgically diagnosed accreta among all cases of antenatally suspected accreta] in order to avoid bias," she noted.
A comparison of the 52 women with and 40 women without surgically confirmed accreta showed that they were statistically indistinguishable with respect to many clinical factors. But they differed significantly on the number of previous cesarean deliveries, the presence of placenta previa, and the presence of ultrasound signs of accreta.
The predictive model based on these three factors had an area under the receiver operating characteristic curve of 0.846, according to Dr. Weiniger. "When we tried to add maternal age and antenatal bleeding, because [these factors have been found to be predictive] in previous studies, it did not improve the area under the curve."
Giving some examples using the new nomogram, she noted that a woman having two previous cesarean deliveries who has placenta previa and a high-suspicion ultrasound would have a probability score approaching 80%, which falls well above cut points based on both 100% and 94% model sensitivity. "So she would be classified as having placenta accreta and would require massive hemorrhage preparation for surgery."
In contrast, a woman having two previous cesarean deliveries who does not have placenta previa and has a low-suspicion ultrasound would have a probability score of almost 0%, which falls well below the cut points, and she would be classified as not having placenta accreta. "So we could manage her with regional anesthesia and maybe not do preparations for massive hemorrhage," Dr. Weiniger commented.
Finally, a woman having two previous cesarean deliveries who has a low-suspicion ultrasound but does have placenta previa would have a probability score of about 20%. This score falls above the cut point corresponding to 100% sensitivity, "so if that was the clinician’s practice, that patient would have massive hemorrhage preparations," she said. "But if we were using the 94% sensitivity, the optimal cut point, she would be right on that, so it would be equivocal as to whether we would classify her as having massive transfusion requirements or not. Possibly, the state of her airway would define how we would manage such a patient."
Dr. Weiniger disclosed no relevant conflicts of interest.
FROM THE ANNUAL MEETING OF THE SOCIETY FOR OBSTETRIC ANESTHESIA AND PERINATOLOGY
ACR Gives Special Consideration to Pregnancy in Nephritis Guidelines
DESTIN, FLA. – Management of lupus nephritis during pregnancy gets close attention in ACR’s new nephritis guidelines.
No treatment is necessary in pregnant women with prior lupus nephritis who have no current evidence of systemic or renal disease activity, while those with mild systemic activity may be treated with hydroxychloroquine, according to the guidelines, which are published in the June issue of Arthritis Care & Research.
"There are good data suggesting hydroxychloroquine controls lupus in women who are pregnant, resulting in fewer flares" Dr. Bevra H. Hahn said at the Congress of Clinical Rheumatology. Dr. Hahn, professor of medicine and chief of the division of rheumatology at the University of California, Los Angeles, led the ACR core working group that helped with development of the guidelines.
In patients with clinically active nephritis or with substantial extrarenal disease activity, glucocorticoids may be prescribed at doses necessary to control disease activity (Arthritis Care Res. 2012;64:797-08).
"I start at 0.5 mg/kg per day," Dr. Hahn said of glucocorticoids under these circumstances. She noted that only steroids that are metabolized by placental enzymes should be used so that the drug does not reach the fetus.
She and her coauthors cautioned, however, that high-dose glucocorticoid therapy is associated with a high risk of maternal complications – including hypertension and diabetes mellitus – in patients with systemic lupus erythematosus (SLE). They also stress that mycophenolate mofetil, cyclophosphamide, and methotrexate should be avoided in pregnancy, because they are established human teratogens.
Azathioprine, though listed as pregnancy category D indicating teratogenic risk, has been shown in cross-sectional studies to be associated with very low risk of fetal abnormalities and can be added if necessary, according to the task force panel charged with developing the guidelines.
The azathioprine dose, however, should not exceed 2 mg/kg per day in pregnant women, Dr. Hahn said.
The task force has recommended that pregnant patients with a persistently active nephritis and documented or suspected class III or IV disease with crescents may be candidates for delivery after 28 weeks if the fetus is viable. The recommendations with respect to pregnancy were based on level C evidence, indicating they were based on consensus, expert opinion, and case series.
For women with SLE and nephritis who are not pregnant, but who have concerns about fertility preservation, the task force panel recommended that mycophenolate mofetil was preferable to cyclophosphamide for induction therapy, because cyclophosphamide has been shown to cause permanent infertility in both women and men.
For example, one study showed that 6 months of high-dose intravenous cyclophosphamide with a cumulative dose of 4.4 g-10 g was associated with sustained amenorrhea in about 10% of young women, and the risk increased with age.
However, the physician should be certain the patient is not pregnant before prescribing mycophenolate mofetil or mycophenolic acid, and treatment should be stopped for at least 6 weeks before pregnancy is attempted.
The guidelines were sponsored by the American College of Rheumatology via a competitive grant mechanism. Dr. Hahn has received consultant fees, speaking fees, and/or honoraria from UCB and Abbott and has served on the data and safety monitoring board for Anthera. The complete list of disclosures for the guideline authors is available with the full text of the article.
Azathioprine, teratogenic risk,
DESTIN, FLA. – Management of lupus nephritis during pregnancy gets close attention in ACR’s new nephritis guidelines.
No treatment is necessary in pregnant women with prior lupus nephritis who have no current evidence of systemic or renal disease activity, while those with mild systemic activity may be treated with hydroxychloroquine, according to the guidelines, which are published in the June issue of Arthritis Care & Research.
"There are good data suggesting hydroxychloroquine controls lupus in women who are pregnant, resulting in fewer flares" Dr. Bevra H. Hahn said at the Congress of Clinical Rheumatology. Dr. Hahn, professor of medicine and chief of the division of rheumatology at the University of California, Los Angeles, led the ACR core working group that helped with development of the guidelines.
In patients with clinically active nephritis or with substantial extrarenal disease activity, glucocorticoids may be prescribed at doses necessary to control disease activity (Arthritis Care Res. 2012;64:797-08).
"I start at 0.5 mg/kg per day," Dr. Hahn said of glucocorticoids under these circumstances. She noted that only steroids that are metabolized by placental enzymes should be used so that the drug does not reach the fetus.
She and her coauthors cautioned, however, that high-dose glucocorticoid therapy is associated with a high risk of maternal complications – including hypertension and diabetes mellitus – in patients with systemic lupus erythematosus (SLE). They also stress that mycophenolate mofetil, cyclophosphamide, and methotrexate should be avoided in pregnancy, because they are established human teratogens.
Azathioprine, though listed as pregnancy category D indicating teratogenic risk, has been shown in cross-sectional studies to be associated with very low risk of fetal abnormalities and can be added if necessary, according to the task force panel charged with developing the guidelines.
The azathioprine dose, however, should not exceed 2 mg/kg per day in pregnant women, Dr. Hahn said.
The task force has recommended that pregnant patients with a persistently active nephritis and documented or suspected class III or IV disease with crescents may be candidates for delivery after 28 weeks if the fetus is viable. The recommendations with respect to pregnancy were based on level C evidence, indicating they were based on consensus, expert opinion, and case series.
For women with SLE and nephritis who are not pregnant, but who have concerns about fertility preservation, the task force panel recommended that mycophenolate mofetil was preferable to cyclophosphamide for induction therapy, because cyclophosphamide has been shown to cause permanent infertility in both women and men.
For example, one study showed that 6 months of high-dose intravenous cyclophosphamide with a cumulative dose of 4.4 g-10 g was associated with sustained amenorrhea in about 10% of young women, and the risk increased with age.
However, the physician should be certain the patient is not pregnant before prescribing mycophenolate mofetil or mycophenolic acid, and treatment should be stopped for at least 6 weeks before pregnancy is attempted.
The guidelines were sponsored by the American College of Rheumatology via a competitive grant mechanism. Dr. Hahn has received consultant fees, speaking fees, and/or honoraria from UCB and Abbott and has served on the data and safety monitoring board for Anthera. The complete list of disclosures for the guideline authors is available with the full text of the article.
DESTIN, FLA. – Management of lupus nephritis during pregnancy gets close attention in ACR’s new nephritis guidelines.
No treatment is necessary in pregnant women with prior lupus nephritis who have no current evidence of systemic or renal disease activity, while those with mild systemic activity may be treated with hydroxychloroquine, according to the guidelines, which are published in the June issue of Arthritis Care & Research.
"There are good data suggesting hydroxychloroquine controls lupus in women who are pregnant, resulting in fewer flares" Dr. Bevra H. Hahn said at the Congress of Clinical Rheumatology. Dr. Hahn, professor of medicine and chief of the division of rheumatology at the University of California, Los Angeles, led the ACR core working group that helped with development of the guidelines.
In patients with clinically active nephritis or with substantial extrarenal disease activity, glucocorticoids may be prescribed at doses necessary to control disease activity (Arthritis Care Res. 2012;64:797-08).
"I start at 0.5 mg/kg per day," Dr. Hahn said of glucocorticoids under these circumstances. She noted that only steroids that are metabolized by placental enzymes should be used so that the drug does not reach the fetus.
She and her coauthors cautioned, however, that high-dose glucocorticoid therapy is associated with a high risk of maternal complications – including hypertension and diabetes mellitus – in patients with systemic lupus erythematosus (SLE). They also stress that mycophenolate mofetil, cyclophosphamide, and methotrexate should be avoided in pregnancy, because they are established human teratogens.
Azathioprine, though listed as pregnancy category D indicating teratogenic risk, has been shown in cross-sectional studies to be associated with very low risk of fetal abnormalities and can be added if necessary, according to the task force panel charged with developing the guidelines.
The azathioprine dose, however, should not exceed 2 mg/kg per day in pregnant women, Dr. Hahn said.
The task force has recommended that pregnant patients with a persistently active nephritis and documented or suspected class III or IV disease with crescents may be candidates for delivery after 28 weeks if the fetus is viable. The recommendations with respect to pregnancy were based on level C evidence, indicating they were based on consensus, expert opinion, and case series.
For women with SLE and nephritis who are not pregnant, but who have concerns about fertility preservation, the task force panel recommended that mycophenolate mofetil was preferable to cyclophosphamide for induction therapy, because cyclophosphamide has been shown to cause permanent infertility in both women and men.
For example, one study showed that 6 months of high-dose intravenous cyclophosphamide with a cumulative dose of 4.4 g-10 g was associated with sustained amenorrhea in about 10% of young women, and the risk increased with age.
However, the physician should be certain the patient is not pregnant before prescribing mycophenolate mofetil or mycophenolic acid, and treatment should be stopped for at least 6 weeks before pregnancy is attempted.
The guidelines were sponsored by the American College of Rheumatology via a competitive grant mechanism. Dr. Hahn has received consultant fees, speaking fees, and/or honoraria from UCB and Abbott and has served on the data and safety monitoring board for Anthera. The complete list of disclosures for the guideline authors is available with the full text of the article.
Azathioprine, teratogenic risk,
Azathioprine, teratogenic risk,
FROM THE CONGRESS OF CLINICAL RHEUMATOLOGY
Large Database Links Adolescent Pregnancy to More Adverse Events
MIAMI BEACH – A study of more than 150,000 pregnancies indicates adolescents and their newborns run an increased risk for complications.
Dr. Kathy Wilson and her colleagues at Washington Hospital Center and Georgetown University Hospital, in Washington, compared peripartum outcomes among 1,312 teens aged 15 years and younger; 19,403 teens aged 16 to 19 years; and 130,453 adults aged 20-34 years. Each had a singleton pregnancy of at least 24 weeks’ gestation between 2002 and 2008.
Adolescent mothers had higher rates of complications, including anemia, preterm premature rupture of membranes (PPROM), chorioamnionitis, and eclampsia, compared with adults.
Anemia affected 9.4% of the teens under age 16 years and 10.2% of the older teenagers. These rates were significantly higher than was the 8.2% rate in adults.
PPROM was noted in the records of 2.1% of younger teens, 2.5% of older teens, and 1.9% of adults. Chorioamnionitis occurred in 8.8% of young adolescents, 8.0% of older adolescents, and 4.8% of adults. Rates of both complications were significantly different between adolescents and adults.
Other researchers have researched risks in adolescent pregnancy, but most of these studies have been small, Dr. Wilson said at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology. Clinical and demographic data for the 151,476 women in this study come from the Consortium on Safe Labor, which includes electronic medical records from 19 hospitals in the United States. The consortium is sponsored by the National Institute of Child Health and Human Development.
The researchers found a nonsignificant trend for higher prevalence of eclampsia in the adolescent mothers as well – 0.25% of the younger teenagers and 0.12% of the older teenagers vs. 0.008% among adult mothers.
Neonates born to adolescent mothers were more likely to be delivered preterm, to be low birth weight or very low birth weight, to have lower APGAR scores, and to have higher rates of admission to a neonatal intensive care unit.
Preterm births occurred in 21.1% of the teens under age 16 years, 18.3% of teens aged 16-19 years, and 16% of adults.
Low birth weight infants were born to 13.1% of the younger teen mothers, 12% of the older teen mothers, and 7.8% of adult mothers. Very low birth weight infants were born to 2.7% of the young teens, 2.5% of the older teens, and 1.7% of the adults. All differences between infants born to adolescents and adults were statistically significant.
Other findings include a higher percentage of 5-minute APGAR scores below 7 for neonates of younger teen mothers, 2.8%, compared with 2.3% for older teens and 2% for adult mothers. Neonatal ICU admission rates were 14.8% for the newborns of young teens, 14% for those born to older teens, and 11.8% for those born to adults.
Cesarean section rate was one factor that was significantly lower among the younger adolescent mothers. Their c-section rate was 15.9%, compared with 21.1% for the older teenagers and 24.8% for the adults.
Young adolescents were more likely to have public health insurance, 70.3%, compared with 66.6% of older adolescents and 39.1% of adult mothers.
Dr. Wilson had no relevant financial disclosures.
MIAMI BEACH – A study of more than 150,000 pregnancies indicates adolescents and their newborns run an increased risk for complications.
Dr. Kathy Wilson and her colleagues at Washington Hospital Center and Georgetown University Hospital, in Washington, compared peripartum outcomes among 1,312 teens aged 15 years and younger; 19,403 teens aged 16 to 19 years; and 130,453 adults aged 20-34 years. Each had a singleton pregnancy of at least 24 weeks’ gestation between 2002 and 2008.
Adolescent mothers had higher rates of complications, including anemia, preterm premature rupture of membranes (PPROM), chorioamnionitis, and eclampsia, compared with adults.
Anemia affected 9.4% of the teens under age 16 years and 10.2% of the older teenagers. These rates were significantly higher than was the 8.2% rate in adults.
PPROM was noted in the records of 2.1% of younger teens, 2.5% of older teens, and 1.9% of adults. Chorioamnionitis occurred in 8.8% of young adolescents, 8.0% of older adolescents, and 4.8% of adults. Rates of both complications were significantly different between adolescents and adults.
Other researchers have researched risks in adolescent pregnancy, but most of these studies have been small, Dr. Wilson said at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology. Clinical and demographic data for the 151,476 women in this study come from the Consortium on Safe Labor, which includes electronic medical records from 19 hospitals in the United States. The consortium is sponsored by the National Institute of Child Health and Human Development.
The researchers found a nonsignificant trend for higher prevalence of eclampsia in the adolescent mothers as well – 0.25% of the younger teenagers and 0.12% of the older teenagers vs. 0.008% among adult mothers.
Neonates born to adolescent mothers were more likely to be delivered preterm, to be low birth weight or very low birth weight, to have lower APGAR scores, and to have higher rates of admission to a neonatal intensive care unit.
Preterm births occurred in 21.1% of the teens under age 16 years, 18.3% of teens aged 16-19 years, and 16% of adults.
Low birth weight infants were born to 13.1% of the younger teen mothers, 12% of the older teen mothers, and 7.8% of adult mothers. Very low birth weight infants were born to 2.7% of the young teens, 2.5% of the older teens, and 1.7% of the adults. All differences between infants born to adolescents and adults were statistically significant.
Other findings include a higher percentage of 5-minute APGAR scores below 7 for neonates of younger teen mothers, 2.8%, compared with 2.3% for older teens and 2% for adult mothers. Neonatal ICU admission rates were 14.8% for the newborns of young teens, 14% for those born to older teens, and 11.8% for those born to adults.
Cesarean section rate was one factor that was significantly lower among the younger adolescent mothers. Their c-section rate was 15.9%, compared with 21.1% for the older teenagers and 24.8% for the adults.
Young adolescents were more likely to have public health insurance, 70.3%, compared with 66.6% of older adolescents and 39.1% of adult mothers.
Dr. Wilson had no relevant financial disclosures.
MIAMI BEACH – A study of more than 150,000 pregnancies indicates adolescents and their newborns run an increased risk for complications.
Dr. Kathy Wilson and her colleagues at Washington Hospital Center and Georgetown University Hospital, in Washington, compared peripartum outcomes among 1,312 teens aged 15 years and younger; 19,403 teens aged 16 to 19 years; and 130,453 adults aged 20-34 years. Each had a singleton pregnancy of at least 24 weeks’ gestation between 2002 and 2008.
Adolescent mothers had higher rates of complications, including anemia, preterm premature rupture of membranes (PPROM), chorioamnionitis, and eclampsia, compared with adults.
Anemia affected 9.4% of the teens under age 16 years and 10.2% of the older teenagers. These rates were significantly higher than was the 8.2% rate in adults.
PPROM was noted in the records of 2.1% of younger teens, 2.5% of older teens, and 1.9% of adults. Chorioamnionitis occurred in 8.8% of young adolescents, 8.0% of older adolescents, and 4.8% of adults. Rates of both complications were significantly different between adolescents and adults.
Other researchers have researched risks in adolescent pregnancy, but most of these studies have been small, Dr. Wilson said at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology. Clinical and demographic data for the 151,476 women in this study come from the Consortium on Safe Labor, which includes electronic medical records from 19 hospitals in the United States. The consortium is sponsored by the National Institute of Child Health and Human Development.
The researchers found a nonsignificant trend for higher prevalence of eclampsia in the adolescent mothers as well – 0.25% of the younger teenagers and 0.12% of the older teenagers vs. 0.008% among adult mothers.
Neonates born to adolescent mothers were more likely to be delivered preterm, to be low birth weight or very low birth weight, to have lower APGAR scores, and to have higher rates of admission to a neonatal intensive care unit.
Preterm births occurred in 21.1% of the teens under age 16 years, 18.3% of teens aged 16-19 years, and 16% of adults.
Low birth weight infants were born to 13.1% of the younger teen mothers, 12% of the older teen mothers, and 7.8% of adult mothers. Very low birth weight infants were born to 2.7% of the young teens, 2.5% of the older teens, and 1.7% of the adults. All differences between infants born to adolescents and adults were statistically significant.
Other findings include a higher percentage of 5-minute APGAR scores below 7 for neonates of younger teen mothers, 2.8%, compared with 2.3% for older teens and 2% for adult mothers. Neonatal ICU admission rates were 14.8% for the newborns of young teens, 14% for those born to older teens, and 11.8% for those born to adults.
Cesarean section rate was one factor that was significantly lower among the younger adolescent mothers. Their c-section rate was 15.9%, compared with 21.1% for the older teenagers and 24.8% for the adults.
Young adolescents were more likely to have public health insurance, 70.3%, compared with 66.6% of older adolescents and 39.1% of adult mothers.
Dr. Wilson had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE NORTH AMERICAN SOCIETY FOR PEDIATRIC AND ADOLESCENT GYNECOLOGY
Major Finding: Chorioamnionitis rates were significantly higher in pregnant teens than in pregnant adults: 8.8% of teens under age 16 years, 8.0% of teens aged16-19 years, and 4.8% of adults.
Data Source: This is a retrospective study of 151,476 adolescent and adult women aged 34 years and younger who had a singleton delivery after at least 24 weeks’ gestation recorded in the Consortium on Safe Labor database.
Disclosures: Dr. Wilson had no relevant financial disclosures.
Prenatal Screen Predicts Maternal Risk of Traumatic Death
BOSTON – A screening tool designed to identify medical and psychosocial risk factors associated with poor pregnancy outcomes also seems to predict maternal traumatic pregnancy–associated death, according to Dr. Nancy S. Hardt.
The Florida Healthy Start Prenatal Risk Screen has been validated for the identification of women who are at risk for preterm delivery or for delivering a low-birth-weight infant. Even low levels of risk on the screening test, which has been offered to all pregnant women in Florida at their first prenatal visit as per state legislative statute since 1991, appear to be associated with an increased likelihood of traumatic maternal death, Dr. Hardt said at the annual meeting of the Pediatric Academic Societies.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death," she said. "It doesn’t take a whole lot of practice change to address some of the factors that might be putting the moms at risk, such as dispelling the myth that pregnant women shouldn’t wear seatbelts, asking patients if they feel safe in their homes, and stressing the dangers of substance use and abuse, including prescription drug use."
Dr. Hardt and her colleagues reviewed 600,000 Healthy Start screens from 1999 to 2005, as well as linked data for the concurrent period from Florida’s Enhanced Maternal Mortality Reporting Database. Of the women who died during the period of study, 144 experienced traumatic deaths. These included accidents, homicides, suicides, and drug overdoses, she said, noting that the top four causes of maternal deaths were trauma related.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death."
Specifically, the causes of death that had the greatest maternal mortality ratios were transport accidents (13.3), homicide (5.5), accidental poisoning (3.3), and suicide (2.9).
"We have to go through quite a few categories of traumatic deaths before we get to the obstetric-related deaths," such as hypertension disorders (2.7), hemorrhage (2.2), thrombotic embolism (2.2), and infection (2.0), observed Dr. Hardt, professor of pathology and ob.gyn. at the University of Florida in Gainesville.
To evaluate the predictive value of the Healthy Start screen for identifying risk of traumatic death, the investigators used the same screening threshold as that used for identifying women at risk for poor pregnancy outcomes, Dr. Hardt said. "A score of 4 or higher on the [15-item] weighted measure, which includes demographic as well as environmental and social factors, indicates a positive screen for risk of preterm or low-birth-weight delivery and triggers referral to Healthy Start services," Dr. Hardt explained. "We hypothesized that the risk factors for these infant problems would be the same as for maternal death, and as such the screening instruments would work for identifying at-risk moms."
An analysis of the data showed that as a woman’s risk score increased, the probability of traumatic death also increased. In fact, "a woman with a risk score of 4 had nearly 12 times the risk of traumatic death compared to a women with a risk score of zero, and a woman with a risk score of 9 had 52 times the risk of traumatic death compared to one who scored zero," Dr. Hardt said. "What we observed is that with each increase in score of 1, the relative risk of death increased 1.5 to 2 times."
What this means, in terms of a prediction tool, "is that for every 100,000 women with a score of 4, expect nearly 48 traumatic maternal deaths, and for every one with a score of 9, expect 215 traumatic deaths," according to Dr. Hardt.
Many of the specific risk determinants associated with poor pregnancy outcomes are likely the same as those that are predictive of maternal traumatic death, including mental health, substance use, domestic violence, education, and employment/family income status, Dr. Hardt said.
Dr. Hardt said she had no relevant financial disclosures.
BOSTON – A screening tool designed to identify medical and psychosocial risk factors associated with poor pregnancy outcomes also seems to predict maternal traumatic pregnancy–associated death, according to Dr. Nancy S. Hardt.
The Florida Healthy Start Prenatal Risk Screen has been validated for the identification of women who are at risk for preterm delivery or for delivering a low-birth-weight infant. Even low levels of risk on the screening test, which has been offered to all pregnant women in Florida at their first prenatal visit as per state legislative statute since 1991, appear to be associated with an increased likelihood of traumatic maternal death, Dr. Hardt said at the annual meeting of the Pediatric Academic Societies.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death," she said. "It doesn’t take a whole lot of practice change to address some of the factors that might be putting the moms at risk, such as dispelling the myth that pregnant women shouldn’t wear seatbelts, asking patients if they feel safe in their homes, and stressing the dangers of substance use and abuse, including prescription drug use."
Dr. Hardt and her colleagues reviewed 600,000 Healthy Start screens from 1999 to 2005, as well as linked data for the concurrent period from Florida’s Enhanced Maternal Mortality Reporting Database. Of the women who died during the period of study, 144 experienced traumatic deaths. These included accidents, homicides, suicides, and drug overdoses, she said, noting that the top four causes of maternal deaths were trauma related.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death."
Specifically, the causes of death that had the greatest maternal mortality ratios were transport accidents (13.3), homicide (5.5), accidental poisoning (3.3), and suicide (2.9).
"We have to go through quite a few categories of traumatic deaths before we get to the obstetric-related deaths," such as hypertension disorders (2.7), hemorrhage (2.2), thrombotic embolism (2.2), and infection (2.0), observed Dr. Hardt, professor of pathology and ob.gyn. at the University of Florida in Gainesville.
To evaluate the predictive value of the Healthy Start screen for identifying risk of traumatic death, the investigators used the same screening threshold as that used for identifying women at risk for poor pregnancy outcomes, Dr. Hardt said. "A score of 4 or higher on the [15-item] weighted measure, which includes demographic as well as environmental and social factors, indicates a positive screen for risk of preterm or low-birth-weight delivery and triggers referral to Healthy Start services," Dr. Hardt explained. "We hypothesized that the risk factors for these infant problems would be the same as for maternal death, and as such the screening instruments would work for identifying at-risk moms."
An analysis of the data showed that as a woman’s risk score increased, the probability of traumatic death also increased. In fact, "a woman with a risk score of 4 had nearly 12 times the risk of traumatic death compared to a women with a risk score of zero, and a woman with a risk score of 9 had 52 times the risk of traumatic death compared to one who scored zero," Dr. Hardt said. "What we observed is that with each increase in score of 1, the relative risk of death increased 1.5 to 2 times."
What this means, in terms of a prediction tool, "is that for every 100,000 women with a score of 4, expect nearly 48 traumatic maternal deaths, and for every one with a score of 9, expect 215 traumatic deaths," according to Dr. Hardt.
Many of the specific risk determinants associated with poor pregnancy outcomes are likely the same as those that are predictive of maternal traumatic death, including mental health, substance use, domestic violence, education, and employment/family income status, Dr. Hardt said.
Dr. Hardt said she had no relevant financial disclosures.
BOSTON – A screening tool designed to identify medical and psychosocial risk factors associated with poor pregnancy outcomes also seems to predict maternal traumatic pregnancy–associated death, according to Dr. Nancy S. Hardt.
The Florida Healthy Start Prenatal Risk Screen has been validated for the identification of women who are at risk for preterm delivery or for delivering a low-birth-weight infant. Even low levels of risk on the screening test, which has been offered to all pregnant women in Florida at their first prenatal visit as per state legislative statute since 1991, appear to be associated with an increased likelihood of traumatic maternal death, Dr. Hardt said at the annual meeting of the Pediatric Academic Societies.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death," she said. "It doesn’t take a whole lot of practice change to address some of the factors that might be putting the moms at risk, such as dispelling the myth that pregnant women shouldn’t wear seatbelts, asking patients if they feel safe in their homes, and stressing the dangers of substance use and abuse, including prescription drug use."
Dr. Hardt and her colleagues reviewed 600,000 Healthy Start screens from 1999 to 2005, as well as linked data for the concurrent period from Florida’s Enhanced Maternal Mortality Reporting Database. Of the women who died during the period of study, 144 experienced traumatic deaths. These included accidents, homicides, suicides, and drug overdoses, she said, noting that the top four causes of maternal deaths were trauma related.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death."
Specifically, the causes of death that had the greatest maternal mortality ratios were transport accidents (13.3), homicide (5.5), accidental poisoning (3.3), and suicide (2.9).
"We have to go through quite a few categories of traumatic deaths before we get to the obstetric-related deaths," such as hypertension disorders (2.7), hemorrhage (2.2), thrombotic embolism (2.2), and infection (2.0), observed Dr. Hardt, professor of pathology and ob.gyn. at the University of Florida in Gainesville.
To evaluate the predictive value of the Healthy Start screen for identifying risk of traumatic death, the investigators used the same screening threshold as that used for identifying women at risk for poor pregnancy outcomes, Dr. Hardt said. "A score of 4 or higher on the [15-item] weighted measure, which includes demographic as well as environmental and social factors, indicates a positive screen for risk of preterm or low-birth-weight delivery and triggers referral to Healthy Start services," Dr. Hardt explained. "We hypothesized that the risk factors for these infant problems would be the same as for maternal death, and as such the screening instruments would work for identifying at-risk moms."
An analysis of the data showed that as a woman’s risk score increased, the probability of traumatic death also increased. In fact, "a woman with a risk score of 4 had nearly 12 times the risk of traumatic death compared to a women with a risk score of zero, and a woman with a risk score of 9 had 52 times the risk of traumatic death compared to one who scored zero," Dr. Hardt said. "What we observed is that with each increase in score of 1, the relative risk of death increased 1.5 to 2 times."
What this means, in terms of a prediction tool, "is that for every 100,000 women with a score of 4, expect nearly 48 traumatic maternal deaths, and for every one with a score of 9, expect 215 traumatic deaths," according to Dr. Hardt.
Many of the specific risk determinants associated with poor pregnancy outcomes are likely the same as those that are predictive of maternal traumatic death, including mental health, substance use, domestic violence, education, and employment/family income status, Dr. Hardt said.
Dr. Hardt said she had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Coronary Dissection Drives MI Rates in Pregnancy
CHICAGO – Coronary dissection, a rare and sometimes fatal condition, surpassed atherosclerosis as the most common cause of pregnancy-associated acute myocardial infarction in a retrospective analysis of 150 women.
Pregnant women also appear to be at increased risk of coronary dissection during coronary angiography and percutaneous coronary intervention, leading to death in one patient, coronary artery bypass grafting in four, and multiple stenting in two.
Moreover, standard treatment with thrombolytic agents may actually increase the risk of hemorrhage and further progression of the dissection in pregnant patients, Dr. Uri Elkayam explained at the annual meeting of the American College of Cardiology.
"Because of this, we are ready now to come up with some strong recommendations that we hope will be reflected in the guidelines that the approach to heart attack in pregnancy should be different than that recommended in the general population," said Dr. Elkayam, professor of medicine in the cardiovascular medicine division at the University of Southern California in Los Angeles and director of the Heart Failure Program at USC Medical Center and University Hospital.
Although the European Society of Cardiology recently published guidelines for the management of cardiovascular diseases during pregnancy (Eur. Heart J. 2011;32:3147-97), neither the American College of Cardiology nor the American Heart Association has specific guidelines.
The analysis included 150 cases of myocardial infarction during pregnancy or the 12 weeks after delivery that were identified in the literature, consulted on, or cared for by the research team since 2005. The women’s average age was 34 years, and 75% were at least 30 years old.
The cause of acute MI was coronary dissection in 56 of the 129 women who had angiography, with 10 dissections occurring in the third trimester and 41 postpartum. Atherosclerotic coronary artery disease, the most common cause of acute MI in the general population, was identified in only 35 women, followed by intracoronary thrombus without evidence of atherosclerosis in 22, normal coronary anatomy with possible spasm in 16, documented spasm in 3, and takotsubo cardiomyopathy in 1. Four of the 22 patients with intracoronary thrombus did not undergo an angiogram.
Coronary dissection, which is thought to occur during pregnancy because of hormonally mediated weakening of the walls of coronary arteries, was managed with bypass surgery in 41.5% of patients, stenting in 38%, medication without coronary intervention in 22%, and a Bentall procedure in 1%.
Percutaneous coronary intervention (PCI) was performed in 40% of all patients and coronary angiography in 79%.
The use of thrombolytic therapy is relatively contraindicated in pregnancy due to the risk of bleeding. In addition, thrombolytic therapy may not be effective in women with normal coronaries, spasm, or coronary dissection, and in the last group it can even be detrimental, Dr. Elkayam observed.
"Thrombolytic therapy should therefore be considered second choice to primary PCI in patients with ST-segment elevation MI during pregnancy, especially during the third trimester, [in] the peripartum and early postpartum periods when the incidence of dissection is high," he suggested.
The use of angiography to determine the cause of the MI and guide therapy is recommended in pregnant women with ST-segment elevation MI and in other high-risk MI patients, but because of the increased risk of iatrogenic coronary dissection, stable and low-risk non-STEMI patients should be treated noninvasively during pregnancy and postpartum, Dr. Elkayam recommended.
Most women in the current analysis did not present with traditional cardiovascular risk factors. Only 9% had diabetes, 15% had hypertension, and 20% had hyperlipidemia, although one-fourth were smokers.
Maternal mortality was 7%, down from 20% during 1922-1995 and 11% during 1996-2005, as previously reported by the researchers (Ann. Intern. Med. 1996;125:751-62; J. Am. Coll. Cardiol. 2008;52:171-80). In spite of the decreased rate of maternal death, women who experience a pregnancy-related MI are three to five times more likely to die than nonpregnant women of comparable age, he said.
Fetal deaths, driven largely by maternal mortality, were also lower at 5%, compared with 12% and 9% in the previous analyses.
Still, Dr. Elkayam stressed that women should not avoid becoming pregnant because of fears of an MI, as the incidence is extremely low, at one in 16,000 deliveries. Although maternal and fetal mortality have been decreasing, the number of women with cardiac problems in pregnancy is rising due to older maternal age at first pregnancy; a spike in age-related cardiovascular risk factors such as diabetes, obesity, and hypertension; and mostly, improved treatment of congenital heart disease, allowing more women to reach childbearing age.
"In general, most patients with mild and even moderate cardiac problems can become pregnant and have children safely," he said in an interview. "Patients are often getting information that is not realistic, usually exaggerating the risk. The reality is such that most physicians are not interested in really managing this problem, and so oftentimes women with heart disease will get advice not to become pregnant."
Dr. Elkayam said women with heart disease should be treated by a cardiologist and obstetrician experienced in managing cardiac problems in pregnancy, and that high-risk patients should managed by an expert multidisciplinary team in a specialist center. He also called for a national registry, similar to the registry established in Europe, to better track outcomes of pregnancy-related heart disease in general, including MI.
Dr. Elkayam reported no conflicts of interest.
CHICAGO – Coronary dissection, a rare and sometimes fatal condition, surpassed atherosclerosis as the most common cause of pregnancy-associated acute myocardial infarction in a retrospective analysis of 150 women.
Pregnant women also appear to be at increased risk of coronary dissection during coronary angiography and percutaneous coronary intervention, leading to death in one patient, coronary artery bypass grafting in four, and multiple stenting in two.
Moreover, standard treatment with thrombolytic agents may actually increase the risk of hemorrhage and further progression of the dissection in pregnant patients, Dr. Uri Elkayam explained at the annual meeting of the American College of Cardiology.
"Because of this, we are ready now to come up with some strong recommendations that we hope will be reflected in the guidelines that the approach to heart attack in pregnancy should be different than that recommended in the general population," said Dr. Elkayam, professor of medicine in the cardiovascular medicine division at the University of Southern California in Los Angeles and director of the Heart Failure Program at USC Medical Center and University Hospital.
Although the European Society of Cardiology recently published guidelines for the management of cardiovascular diseases during pregnancy (Eur. Heart J. 2011;32:3147-97), neither the American College of Cardiology nor the American Heart Association has specific guidelines.
The analysis included 150 cases of myocardial infarction during pregnancy or the 12 weeks after delivery that were identified in the literature, consulted on, or cared for by the research team since 2005. The women’s average age was 34 years, and 75% were at least 30 years old.
The cause of acute MI was coronary dissection in 56 of the 129 women who had angiography, with 10 dissections occurring in the third trimester and 41 postpartum. Atherosclerotic coronary artery disease, the most common cause of acute MI in the general population, was identified in only 35 women, followed by intracoronary thrombus without evidence of atherosclerosis in 22, normal coronary anatomy with possible spasm in 16, documented spasm in 3, and takotsubo cardiomyopathy in 1. Four of the 22 patients with intracoronary thrombus did not undergo an angiogram.
Coronary dissection, which is thought to occur during pregnancy because of hormonally mediated weakening of the walls of coronary arteries, was managed with bypass surgery in 41.5% of patients, stenting in 38%, medication without coronary intervention in 22%, and a Bentall procedure in 1%.
Percutaneous coronary intervention (PCI) was performed in 40% of all patients and coronary angiography in 79%.
The use of thrombolytic therapy is relatively contraindicated in pregnancy due to the risk of bleeding. In addition, thrombolytic therapy may not be effective in women with normal coronaries, spasm, or coronary dissection, and in the last group it can even be detrimental, Dr. Elkayam observed.
"Thrombolytic therapy should therefore be considered second choice to primary PCI in patients with ST-segment elevation MI during pregnancy, especially during the third trimester, [in] the peripartum and early postpartum periods when the incidence of dissection is high," he suggested.
The use of angiography to determine the cause of the MI and guide therapy is recommended in pregnant women with ST-segment elevation MI and in other high-risk MI patients, but because of the increased risk of iatrogenic coronary dissection, stable and low-risk non-STEMI patients should be treated noninvasively during pregnancy and postpartum, Dr. Elkayam recommended.
Most women in the current analysis did not present with traditional cardiovascular risk factors. Only 9% had diabetes, 15% had hypertension, and 20% had hyperlipidemia, although one-fourth were smokers.
Maternal mortality was 7%, down from 20% during 1922-1995 and 11% during 1996-2005, as previously reported by the researchers (Ann. Intern. Med. 1996;125:751-62; J. Am. Coll. Cardiol. 2008;52:171-80). In spite of the decreased rate of maternal death, women who experience a pregnancy-related MI are three to five times more likely to die than nonpregnant women of comparable age, he said.
Fetal deaths, driven largely by maternal mortality, were also lower at 5%, compared with 12% and 9% in the previous analyses.
Still, Dr. Elkayam stressed that women should not avoid becoming pregnant because of fears of an MI, as the incidence is extremely low, at one in 16,000 deliveries. Although maternal and fetal mortality have been decreasing, the number of women with cardiac problems in pregnancy is rising due to older maternal age at first pregnancy; a spike in age-related cardiovascular risk factors such as diabetes, obesity, and hypertension; and mostly, improved treatment of congenital heart disease, allowing more women to reach childbearing age.
"In general, most patients with mild and even moderate cardiac problems can become pregnant and have children safely," he said in an interview. "Patients are often getting information that is not realistic, usually exaggerating the risk. The reality is such that most physicians are not interested in really managing this problem, and so oftentimes women with heart disease will get advice not to become pregnant."
Dr. Elkayam said women with heart disease should be treated by a cardiologist and obstetrician experienced in managing cardiac problems in pregnancy, and that high-risk patients should managed by an expert multidisciplinary team in a specialist center. He also called for a national registry, similar to the registry established in Europe, to better track outcomes of pregnancy-related heart disease in general, including MI.
Dr. Elkayam reported no conflicts of interest.
CHICAGO – Coronary dissection, a rare and sometimes fatal condition, surpassed atherosclerosis as the most common cause of pregnancy-associated acute myocardial infarction in a retrospective analysis of 150 women.
Pregnant women also appear to be at increased risk of coronary dissection during coronary angiography and percutaneous coronary intervention, leading to death in one patient, coronary artery bypass grafting in four, and multiple stenting in two.
Moreover, standard treatment with thrombolytic agents may actually increase the risk of hemorrhage and further progression of the dissection in pregnant patients, Dr. Uri Elkayam explained at the annual meeting of the American College of Cardiology.
"Because of this, we are ready now to come up with some strong recommendations that we hope will be reflected in the guidelines that the approach to heart attack in pregnancy should be different than that recommended in the general population," said Dr. Elkayam, professor of medicine in the cardiovascular medicine division at the University of Southern California in Los Angeles and director of the Heart Failure Program at USC Medical Center and University Hospital.
Although the European Society of Cardiology recently published guidelines for the management of cardiovascular diseases during pregnancy (Eur. Heart J. 2011;32:3147-97), neither the American College of Cardiology nor the American Heart Association has specific guidelines.
The analysis included 150 cases of myocardial infarction during pregnancy or the 12 weeks after delivery that were identified in the literature, consulted on, or cared for by the research team since 2005. The women’s average age was 34 years, and 75% were at least 30 years old.
The cause of acute MI was coronary dissection in 56 of the 129 women who had angiography, with 10 dissections occurring in the third trimester and 41 postpartum. Atherosclerotic coronary artery disease, the most common cause of acute MI in the general population, was identified in only 35 women, followed by intracoronary thrombus without evidence of atherosclerosis in 22, normal coronary anatomy with possible spasm in 16, documented spasm in 3, and takotsubo cardiomyopathy in 1. Four of the 22 patients with intracoronary thrombus did not undergo an angiogram.
Coronary dissection, which is thought to occur during pregnancy because of hormonally mediated weakening of the walls of coronary arteries, was managed with bypass surgery in 41.5% of patients, stenting in 38%, medication without coronary intervention in 22%, and a Bentall procedure in 1%.
Percutaneous coronary intervention (PCI) was performed in 40% of all patients and coronary angiography in 79%.
The use of thrombolytic therapy is relatively contraindicated in pregnancy due to the risk of bleeding. In addition, thrombolytic therapy may not be effective in women with normal coronaries, spasm, or coronary dissection, and in the last group it can even be detrimental, Dr. Elkayam observed.
"Thrombolytic therapy should therefore be considered second choice to primary PCI in patients with ST-segment elevation MI during pregnancy, especially during the third trimester, [in] the peripartum and early postpartum periods when the incidence of dissection is high," he suggested.
The use of angiography to determine the cause of the MI and guide therapy is recommended in pregnant women with ST-segment elevation MI and in other high-risk MI patients, but because of the increased risk of iatrogenic coronary dissection, stable and low-risk non-STEMI patients should be treated noninvasively during pregnancy and postpartum, Dr. Elkayam recommended.
Most women in the current analysis did not present with traditional cardiovascular risk factors. Only 9% had diabetes, 15% had hypertension, and 20% had hyperlipidemia, although one-fourth were smokers.
Maternal mortality was 7%, down from 20% during 1922-1995 and 11% during 1996-2005, as previously reported by the researchers (Ann. Intern. Med. 1996;125:751-62; J. Am. Coll. Cardiol. 2008;52:171-80). In spite of the decreased rate of maternal death, women who experience a pregnancy-related MI are three to five times more likely to die than nonpregnant women of comparable age, he said.
Fetal deaths, driven largely by maternal mortality, were also lower at 5%, compared with 12% and 9% in the previous analyses.
Still, Dr. Elkayam stressed that women should not avoid becoming pregnant because of fears of an MI, as the incidence is extremely low, at one in 16,000 deliveries. Although maternal and fetal mortality have been decreasing, the number of women with cardiac problems in pregnancy is rising due to older maternal age at first pregnancy; a spike in age-related cardiovascular risk factors such as diabetes, obesity, and hypertension; and mostly, improved treatment of congenital heart disease, allowing more women to reach childbearing age.
"In general, most patients with mild and even moderate cardiac problems can become pregnant and have children safely," he said in an interview. "Patients are often getting information that is not realistic, usually exaggerating the risk. The reality is such that most physicians are not interested in really managing this problem, and so oftentimes women with heart disease will get advice not to become pregnant."
Dr. Elkayam said women with heart disease should be treated by a cardiologist and obstetrician experienced in managing cardiac problems in pregnancy, and that high-risk patients should managed by an expert multidisciplinary team in a specialist center. He also called for a national registry, similar to the registry established in Europe, to better track outcomes of pregnancy-related heart disease in general, including MI.
Dr. Elkayam reported no conflicts of interest.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF CARDIOLOGY
BMI Linked to Success of Arrest of Dilatation Treatment
SAN DIEGO – Women with a body mass index of 35 kg/m2 or greater responded poorly to oxytocin treatment for arrest of dilatation, compared with leaner subjects, results from a single study showed.
"Maternal obesity is increasingly prevalent and is associated with high rates of dysfunctional labor and cesarean delivery, outcomes that are not completely attributable to high fetal weight," researchers led by Dr. Shelly Soni wrote in a poster presented during the annual meeting of the American College of Obstetricians and Gynecologists. "Obesity may inhibit uterine contractility and labor progress."
To test their hypothesis that oxytocin administered to treat arrest of dilatation is less effective in obese women, compared with lean women, Dr. Soni and her associates reviewed an electronic database for women with singleton term pregnancies in cephalic presentation who labored and delivered at Flushing (N.Y.) Hospital Medical Center between July 2004 and August 2011. After excluding patients with medical complications or prior cesarean delivery, the researchers identified 118 consecutive cases diagnosed with arrest of dilatation and grouped them into one of four body mass index (BMI) classifications: BMI of less than 25 kg/m2 (group A; n = 30); BMI of 25-29.9 kg/m2 (group B; n = 33); BMI of 30-34.9 kg/m2 (group C; n = 32), and BMI of 35 kg/m2 or greater (group D; n =23).
An investigator blinded to the patients and to the groups constructed labor curves for each patient. Successful treatment of an arrest of dilatation was defined as attainment of full dilatation.
Dr. Soni, a third-year resident in the department of obstetrics and gynecology at the center, reported that none of the four groups differed significantly in birth weight, gestational age, parity, or maternal age. However, successful treatment of the arrest disorder was achieved in 90% of women in groups A and B, 72% of women in group C, and just 39% of women in group D.
"The amount of oxytocin used as well as time to delivery or cesarean decision after starting oxytocin was significantly higher in group D (P = .001) [and] the cesarean delivery rate was directly related to maternal BMI across the cohort (P = .001)," the researchers noted. "Among patients who had further dilatation after beginning oxytocin, the frequency with which the post-arrest slope was equal to or greater than the pre-arrest slope was inversely related to maternal BMI."
They went on to speculate that obesity "may inhibit uterine contractility and the uterine response to oxytocin, which in turn may explain our results, and the high rates of dysfunctional labor and cesarean delivery among obese women."
In an interview, Dr. Soni noted that one limitation of the analysis was that "it was not designed to see if a higher dose of oxytocin would be effective in obese women."
Dr. Soni said she had no relevant financial conflicts to disclose.
SAN DIEGO – Women with a body mass index of 35 kg/m2 or greater responded poorly to oxytocin treatment for arrest of dilatation, compared with leaner subjects, results from a single study showed.
"Maternal obesity is increasingly prevalent and is associated with high rates of dysfunctional labor and cesarean delivery, outcomes that are not completely attributable to high fetal weight," researchers led by Dr. Shelly Soni wrote in a poster presented during the annual meeting of the American College of Obstetricians and Gynecologists. "Obesity may inhibit uterine contractility and labor progress."
To test their hypothesis that oxytocin administered to treat arrest of dilatation is less effective in obese women, compared with lean women, Dr. Soni and her associates reviewed an electronic database for women with singleton term pregnancies in cephalic presentation who labored and delivered at Flushing (N.Y.) Hospital Medical Center between July 2004 and August 2011. After excluding patients with medical complications or prior cesarean delivery, the researchers identified 118 consecutive cases diagnosed with arrest of dilatation and grouped them into one of four body mass index (BMI) classifications: BMI of less than 25 kg/m2 (group A; n = 30); BMI of 25-29.9 kg/m2 (group B; n = 33); BMI of 30-34.9 kg/m2 (group C; n = 32), and BMI of 35 kg/m2 or greater (group D; n =23).
An investigator blinded to the patients and to the groups constructed labor curves for each patient. Successful treatment of an arrest of dilatation was defined as attainment of full dilatation.
Dr. Soni, a third-year resident in the department of obstetrics and gynecology at the center, reported that none of the four groups differed significantly in birth weight, gestational age, parity, or maternal age. However, successful treatment of the arrest disorder was achieved in 90% of women in groups A and B, 72% of women in group C, and just 39% of women in group D.
"The amount of oxytocin used as well as time to delivery or cesarean decision after starting oxytocin was significantly higher in group D (P = .001) [and] the cesarean delivery rate was directly related to maternal BMI across the cohort (P = .001)," the researchers noted. "Among patients who had further dilatation after beginning oxytocin, the frequency with which the post-arrest slope was equal to or greater than the pre-arrest slope was inversely related to maternal BMI."
They went on to speculate that obesity "may inhibit uterine contractility and the uterine response to oxytocin, which in turn may explain our results, and the high rates of dysfunctional labor and cesarean delivery among obese women."
In an interview, Dr. Soni noted that one limitation of the analysis was that "it was not designed to see if a higher dose of oxytocin would be effective in obese women."
Dr. Soni said she had no relevant financial conflicts to disclose.
SAN DIEGO – Women with a body mass index of 35 kg/m2 or greater responded poorly to oxytocin treatment for arrest of dilatation, compared with leaner subjects, results from a single study showed.
"Maternal obesity is increasingly prevalent and is associated with high rates of dysfunctional labor and cesarean delivery, outcomes that are not completely attributable to high fetal weight," researchers led by Dr. Shelly Soni wrote in a poster presented during the annual meeting of the American College of Obstetricians and Gynecologists. "Obesity may inhibit uterine contractility and labor progress."
To test their hypothesis that oxytocin administered to treat arrest of dilatation is less effective in obese women, compared with lean women, Dr. Soni and her associates reviewed an electronic database for women with singleton term pregnancies in cephalic presentation who labored and delivered at Flushing (N.Y.) Hospital Medical Center between July 2004 and August 2011. After excluding patients with medical complications or prior cesarean delivery, the researchers identified 118 consecutive cases diagnosed with arrest of dilatation and grouped them into one of four body mass index (BMI) classifications: BMI of less than 25 kg/m2 (group A; n = 30); BMI of 25-29.9 kg/m2 (group B; n = 33); BMI of 30-34.9 kg/m2 (group C; n = 32), and BMI of 35 kg/m2 or greater (group D; n =23).
An investigator blinded to the patients and to the groups constructed labor curves for each patient. Successful treatment of an arrest of dilatation was defined as attainment of full dilatation.
Dr. Soni, a third-year resident in the department of obstetrics and gynecology at the center, reported that none of the four groups differed significantly in birth weight, gestational age, parity, or maternal age. However, successful treatment of the arrest disorder was achieved in 90% of women in groups A and B, 72% of women in group C, and just 39% of women in group D.
"The amount of oxytocin used as well as time to delivery or cesarean decision after starting oxytocin was significantly higher in group D (P = .001) [and] the cesarean delivery rate was directly related to maternal BMI across the cohort (P = .001)," the researchers noted. "Among patients who had further dilatation after beginning oxytocin, the frequency with which the post-arrest slope was equal to or greater than the pre-arrest slope was inversely related to maternal BMI."
They went on to speculate that obesity "may inhibit uterine contractility and the uterine response to oxytocin, which in turn may explain our results, and the high rates of dysfunctional labor and cesarean delivery among obese women."
In an interview, Dr. Soni noted that one limitation of the analysis was that "it was not designed to see if a higher dose of oxytocin would be effective in obese women."
Dr. Soni said she had no relevant financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: Successful treatment of arrest of dilatation with oxytocin was achieved in 90% of women with body mass indexes of less than 25 kg/m2 and 25-29.9 kg/m2, 72% in women with a BMI of 30-34.9 kg/m2, and 39% in women with a BMI of 35 kg/m2 or greater.
Data Source: A review of 118 women with singleton pregnancies who labored and delivered at Flushing (N.Y.) Hospital Medical Center between July 2004 and August 2011.
Disclosures: Dr. Soni said she had no relevant financial conflicts to disclose.
Abnormal Placenta Linked to Increased Postcesarean Hemorrhage Risk
SAN DIEGO – Three of the main risk factors for severe hemorrhage following a cesarean are abnormal placenta, uterine rupture or incision extension, and labor prior to cesarean, results from a large single-center study demonstrated.
For the study, Steven Kyle Thompson, D.O., and his associates at the University of Kansas, Wichita, reviewed the medical records of 3,677 cesarean deliveries performed at Wesley Medical Center, a large hospital in Wichita affiliated with the university, from Jan. 1, 2009 through Oct. 31, 2010. Hemorrhage was defined as having at least 1,000 mL of estimated blood loss (EBL) after the procedure.
Hemorrhage occurred in 303 of the deliveries (8.2%), and there were no maternal or fetal deaths. The researchers observed that the median EBL was greater in cases that involved administration of misoprostol, methylergonovine, or carboprost tromethamine vs. nothing (1,400 mL vs. 1,200 mL, P less than .001), as well as with the use of a Bakri balloon, B-Lynch suture, or cesarean hysterectomy vs. nothing (3,000 mL vs. 1,200 mL, P less .001). Median EBL also was greater in cases that required blood transfusion (2,500 mL vs. 1,200 mL, P less .001) and use of an intensive care unit (2,000 mL vs. 1,200 mL, P less .001).
Dr. Thompson and his associates also observed that a hemoglobin decrease by at least 30% of the preoperative value was significantly associated with abnormal placenta (odds ratio [OR], 5.38), uterine rupture or incision extension (OR, 2.81), labor prior to cesarean (OR, 2.78), and EBL of at least 1,500 mL (OR, 2.44).
Adjusted independent risk factors that were significantly associated with a postoperative decrease in hemoglobin below 7 g/dL were abnormal placenta (OR, 5.50), delivery between 2 a.m. and 7 a.m. (OR, 4.85), preoperative hemoglobin less than 11 g/dL (OR, 4.03), labor before cesarean (OR, 2.61), and EBL of at least 1,500 mL (OR, 2.31), they reported in a poster session at the annual meeting of the American College of Obstetricians and Gynecologists.
"Plan ahead of time if you have an individual who falls into a high-risk category," Dr. Thompson, a fourth-year ob.gyn. resident at the university, advised in an interview.
The researchers are currently replicating the study for vaginal deliveries.
Dr. Thompson said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Three of the main risk factors for severe hemorrhage following a cesarean are abnormal placenta, uterine rupture or incision extension, and labor prior to cesarean, results from a large single-center study demonstrated.
For the study, Steven Kyle Thompson, D.O., and his associates at the University of Kansas, Wichita, reviewed the medical records of 3,677 cesarean deliveries performed at Wesley Medical Center, a large hospital in Wichita affiliated with the university, from Jan. 1, 2009 through Oct. 31, 2010. Hemorrhage was defined as having at least 1,000 mL of estimated blood loss (EBL) after the procedure.
Hemorrhage occurred in 303 of the deliveries (8.2%), and there were no maternal or fetal deaths. The researchers observed that the median EBL was greater in cases that involved administration of misoprostol, methylergonovine, or carboprost tromethamine vs. nothing (1,400 mL vs. 1,200 mL, P less than .001), as well as with the use of a Bakri balloon, B-Lynch suture, or cesarean hysterectomy vs. nothing (3,000 mL vs. 1,200 mL, P less .001). Median EBL also was greater in cases that required blood transfusion (2,500 mL vs. 1,200 mL, P less .001) and use of an intensive care unit (2,000 mL vs. 1,200 mL, P less .001).
Dr. Thompson and his associates also observed that a hemoglobin decrease by at least 30% of the preoperative value was significantly associated with abnormal placenta (odds ratio [OR], 5.38), uterine rupture or incision extension (OR, 2.81), labor prior to cesarean (OR, 2.78), and EBL of at least 1,500 mL (OR, 2.44).
Adjusted independent risk factors that were significantly associated with a postoperative decrease in hemoglobin below 7 g/dL were abnormal placenta (OR, 5.50), delivery between 2 a.m. and 7 a.m. (OR, 4.85), preoperative hemoglobin less than 11 g/dL (OR, 4.03), labor before cesarean (OR, 2.61), and EBL of at least 1,500 mL (OR, 2.31), they reported in a poster session at the annual meeting of the American College of Obstetricians and Gynecologists.
"Plan ahead of time if you have an individual who falls into a high-risk category," Dr. Thompson, a fourth-year ob.gyn. resident at the university, advised in an interview.
The researchers are currently replicating the study for vaginal deliveries.
Dr. Thompson said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Three of the main risk factors for severe hemorrhage following a cesarean are abnormal placenta, uterine rupture or incision extension, and labor prior to cesarean, results from a large single-center study demonstrated.
For the study, Steven Kyle Thompson, D.O., and his associates at the University of Kansas, Wichita, reviewed the medical records of 3,677 cesarean deliveries performed at Wesley Medical Center, a large hospital in Wichita affiliated with the university, from Jan. 1, 2009 through Oct. 31, 2010. Hemorrhage was defined as having at least 1,000 mL of estimated blood loss (EBL) after the procedure.
Hemorrhage occurred in 303 of the deliveries (8.2%), and there were no maternal or fetal deaths. The researchers observed that the median EBL was greater in cases that involved administration of misoprostol, methylergonovine, or carboprost tromethamine vs. nothing (1,400 mL vs. 1,200 mL, P less than .001), as well as with the use of a Bakri balloon, B-Lynch suture, or cesarean hysterectomy vs. nothing (3,000 mL vs. 1,200 mL, P less .001). Median EBL also was greater in cases that required blood transfusion (2,500 mL vs. 1,200 mL, P less .001) and use of an intensive care unit (2,000 mL vs. 1,200 mL, P less .001).
Dr. Thompson and his associates also observed that a hemoglobin decrease by at least 30% of the preoperative value was significantly associated with abnormal placenta (odds ratio [OR], 5.38), uterine rupture or incision extension (OR, 2.81), labor prior to cesarean (OR, 2.78), and EBL of at least 1,500 mL (OR, 2.44).
Adjusted independent risk factors that were significantly associated with a postoperative decrease in hemoglobin below 7 g/dL were abnormal placenta (OR, 5.50), delivery between 2 a.m. and 7 a.m. (OR, 4.85), preoperative hemoglobin less than 11 g/dL (OR, 4.03), labor before cesarean (OR, 2.61), and EBL of at least 1,500 mL (OR, 2.31), they reported in a poster session at the annual meeting of the American College of Obstetricians and Gynecologists.
"Plan ahead of time if you have an individual who falls into a high-risk category," Dr. Thompson, a fourth-year ob.gyn. resident at the university, advised in an interview.
The researchers are currently replicating the study for vaginal deliveries.
Dr. Thompson said that he had no relevant financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: A hemoglobin decrease of at least 30% from the preoperative value was significantly associated with abnormal placenta (OR, 5.38), incision extension or uterine rupture (OR, 2.81), and labor (OR, 2.78).
Data Source: This review involved 3,677 cesarean deliveries performed at a large hospital between Jan. 1, 2009 and Oct. 31, 2010.
Disclosures: Dr. Thompson said that he had no relevant financial conflicts to disclose.