User login
FDA Panel Rejects Denosumab Against Bone Metastasis in Prostate Cancer
SILVER SPRING, MD. – A Food and Drug Administration advisory panel voted 12 to 1 on Feb. 8 that denosumab did not have a favorable risk-benefit profile as a treatment to reduce the risk of bone metastases in men who are at high risk for developing them with castrate-resistant prostate cancer.
Concern over the possibility of increased toxicity, especially osteonecrosis of the jaw, with longer drug exposure weighed heavily in the Oncologic Drugs Advisory Committee decision (ODAC). The patient representative was the only panelist to vote in favor.
Denosumab (Xgeva) was approved in 2010 for the prevention of skeletal-related events in patients with bone metastases from solid tumors. The new indication, proposed by manufacturer Amgen, would start treatment earlier to avert bone metastases before they develop in men with castrate-resistant prostate cancer (CRPC).
Amgen said that denosumab "prolongs bone metastasis-free survival by reducing the risk of developing bone metastases."
The application is based on the results of a phase III international study of 1,432 men with CRPC at high risk of developing bone metastases (defined as a prostate-specific antigen level of 8.0 ng/mL or higher or a PSA level that had doubled within 10 months or less).
The study found that survival free of bone metastases, the primary end point, was prolonged by a median of about 4 months in patients randomized to denosumab (120 mg subcutaneously every 4 weeks) compared with those on placebo – a statistically significant difference that represented a 15% reduction in risk.
But ODAC was nearly unanimous in finding that this difference in bone metastasis–free survival was modest and did not outweigh the risks of treatment, namely osteonecrosis of the jaw. In the study, almost 5% of those on denosumab developed osteonecrosis of the jaw, a known effect of treatment, compared with none of those on placebo. Panelists were concerned that this risk could increase with longer exposure to the drug.
The panel was not asked specifically whether it recommended approval for this expanded indication. The FDA must make a decision by the Prescription Drug User Fee Act (PDUFA) action date of April 26, 2012.
Amgen issued the following statement after the ODAC vote: "We look forward to further discussions with the FDA as they continue to review our application," it said. "The development of bone metastases in men with castration-resistant prostate cancer is a clinically significant event, and delaying bone metastases in these men is a clear unmet need with no approved therapies."
In the study under consideration, bone metastasis–free survival was determined by time to first occurrence of bone metastasis (symptomatic or asymptomatic at detection) or death, which was a median of 29.5 months among those on denosumab vs. 25.2 months among those on placebo.
There were no significant differences in overall survival, progression-free survival, or patient-reported outcomes between the two groups. In about two-thirds of cases, bone metastases were asymptomatic.
Denosumab, a monoclonal antibody that inhibits the RANK ligand (RANKL), is marketed as Xgeva at the same dose and schedule used in this study for prevention of skeletal events such as fractures from bone metastases. It is not indicated for the prevention of skeletal-related events in patients with multiple myeloma. By binding to RANKL, denosumab "prevents activation of RANK, thereby inhibiting osteoclast formation, activation, and survival," according to Amgen.
Denosumab is also approved as Prolia, at a lower dose administered once a year, to treat postmenopausal women with osteoporosis who are at high risk of fracture; to increase bone mass in men who are at high risk of fracture while receiving androgen deprivation therapy for nonmetastatic prostate cancer; and to increase bone mass in women at high risk of fracture while receiving adjuvant aromatase inhibitor therapy for breast cancer.
If the new indication is granted, Xgeva would be the first treatment approved to prevent or delay bone metastases in men with nonmetastatic CRPC, according to Amgen. But that appears unlikely, since the FDA usually follows the recommendations of its advisory panels.
Panelists were cleared of potential conflicts before voting on denosumab.
SILVER SPRING, MD. – A Food and Drug Administration advisory panel voted 12 to 1 on Feb. 8 that denosumab did not have a favorable risk-benefit profile as a treatment to reduce the risk of bone metastases in men who are at high risk for developing them with castrate-resistant prostate cancer.
Concern over the possibility of increased toxicity, especially osteonecrosis of the jaw, with longer drug exposure weighed heavily in the Oncologic Drugs Advisory Committee decision (ODAC). The patient representative was the only panelist to vote in favor.
Denosumab (Xgeva) was approved in 2010 for the prevention of skeletal-related events in patients with bone metastases from solid tumors. The new indication, proposed by manufacturer Amgen, would start treatment earlier to avert bone metastases before they develop in men with castrate-resistant prostate cancer (CRPC).
Amgen said that denosumab "prolongs bone metastasis-free survival by reducing the risk of developing bone metastases."
The application is based on the results of a phase III international study of 1,432 men with CRPC at high risk of developing bone metastases (defined as a prostate-specific antigen level of 8.0 ng/mL or higher or a PSA level that had doubled within 10 months or less).
The study found that survival free of bone metastases, the primary end point, was prolonged by a median of about 4 months in patients randomized to denosumab (120 mg subcutaneously every 4 weeks) compared with those on placebo – a statistically significant difference that represented a 15% reduction in risk.
But ODAC was nearly unanimous in finding that this difference in bone metastasis–free survival was modest and did not outweigh the risks of treatment, namely osteonecrosis of the jaw. In the study, almost 5% of those on denosumab developed osteonecrosis of the jaw, a known effect of treatment, compared with none of those on placebo. Panelists were concerned that this risk could increase with longer exposure to the drug.
The panel was not asked specifically whether it recommended approval for this expanded indication. The FDA must make a decision by the Prescription Drug User Fee Act (PDUFA) action date of April 26, 2012.
Amgen issued the following statement after the ODAC vote: "We look forward to further discussions with the FDA as they continue to review our application," it said. "The development of bone metastases in men with castration-resistant prostate cancer is a clinically significant event, and delaying bone metastases in these men is a clear unmet need with no approved therapies."
In the study under consideration, bone metastasis–free survival was determined by time to first occurrence of bone metastasis (symptomatic or asymptomatic at detection) or death, which was a median of 29.5 months among those on denosumab vs. 25.2 months among those on placebo.
There were no significant differences in overall survival, progression-free survival, or patient-reported outcomes between the two groups. In about two-thirds of cases, bone metastases were asymptomatic.
Denosumab, a monoclonal antibody that inhibits the RANK ligand (RANKL), is marketed as Xgeva at the same dose and schedule used in this study for prevention of skeletal events such as fractures from bone metastases. It is not indicated for the prevention of skeletal-related events in patients with multiple myeloma. By binding to RANKL, denosumab "prevents activation of RANK, thereby inhibiting osteoclast formation, activation, and survival," according to Amgen.
Denosumab is also approved as Prolia, at a lower dose administered once a year, to treat postmenopausal women with osteoporosis who are at high risk of fracture; to increase bone mass in men who are at high risk of fracture while receiving androgen deprivation therapy for nonmetastatic prostate cancer; and to increase bone mass in women at high risk of fracture while receiving adjuvant aromatase inhibitor therapy for breast cancer.
If the new indication is granted, Xgeva would be the first treatment approved to prevent or delay bone metastases in men with nonmetastatic CRPC, according to Amgen. But that appears unlikely, since the FDA usually follows the recommendations of its advisory panels.
Panelists were cleared of potential conflicts before voting on denosumab.
SILVER SPRING, MD. – A Food and Drug Administration advisory panel voted 12 to 1 on Feb. 8 that denosumab did not have a favorable risk-benefit profile as a treatment to reduce the risk of bone metastases in men who are at high risk for developing them with castrate-resistant prostate cancer.
Concern over the possibility of increased toxicity, especially osteonecrosis of the jaw, with longer drug exposure weighed heavily in the Oncologic Drugs Advisory Committee decision (ODAC). The patient representative was the only panelist to vote in favor.
Denosumab (Xgeva) was approved in 2010 for the prevention of skeletal-related events in patients with bone metastases from solid tumors. The new indication, proposed by manufacturer Amgen, would start treatment earlier to avert bone metastases before they develop in men with castrate-resistant prostate cancer (CRPC).
Amgen said that denosumab "prolongs bone metastasis-free survival by reducing the risk of developing bone metastases."
The application is based on the results of a phase III international study of 1,432 men with CRPC at high risk of developing bone metastases (defined as a prostate-specific antigen level of 8.0 ng/mL or higher or a PSA level that had doubled within 10 months or less).
The study found that survival free of bone metastases, the primary end point, was prolonged by a median of about 4 months in patients randomized to denosumab (120 mg subcutaneously every 4 weeks) compared with those on placebo – a statistically significant difference that represented a 15% reduction in risk.
But ODAC was nearly unanimous in finding that this difference in bone metastasis–free survival was modest and did not outweigh the risks of treatment, namely osteonecrosis of the jaw. In the study, almost 5% of those on denosumab developed osteonecrosis of the jaw, a known effect of treatment, compared with none of those on placebo. Panelists were concerned that this risk could increase with longer exposure to the drug.
The panel was not asked specifically whether it recommended approval for this expanded indication. The FDA must make a decision by the Prescription Drug User Fee Act (PDUFA) action date of April 26, 2012.
Amgen issued the following statement after the ODAC vote: "We look forward to further discussions with the FDA as they continue to review our application," it said. "The development of bone metastases in men with castration-resistant prostate cancer is a clinically significant event, and delaying bone metastases in these men is a clear unmet need with no approved therapies."
In the study under consideration, bone metastasis–free survival was determined by time to first occurrence of bone metastasis (symptomatic or asymptomatic at detection) or death, which was a median of 29.5 months among those on denosumab vs. 25.2 months among those on placebo.
There were no significant differences in overall survival, progression-free survival, or patient-reported outcomes between the two groups. In about two-thirds of cases, bone metastases were asymptomatic.
Denosumab, a monoclonal antibody that inhibits the RANK ligand (RANKL), is marketed as Xgeva at the same dose and schedule used in this study for prevention of skeletal events such as fractures from bone metastases. It is not indicated for the prevention of skeletal-related events in patients with multiple myeloma. By binding to RANKL, denosumab "prevents activation of RANK, thereby inhibiting osteoclast formation, activation, and survival," according to Amgen.
Denosumab is also approved as Prolia, at a lower dose administered once a year, to treat postmenopausal women with osteoporosis who are at high risk of fracture; to increase bone mass in men who are at high risk of fracture while receiving androgen deprivation therapy for nonmetastatic prostate cancer; and to increase bone mass in women at high risk of fracture while receiving adjuvant aromatase inhibitor therapy for breast cancer.
If the new indication is granted, Xgeva would be the first treatment approved to prevent or delay bone metastases in men with nonmetastatic CRPC, according to Amgen. But that appears unlikely, since the FDA usually follows the recommendations of its advisory panels.
Panelists were cleared of potential conflicts before voting on denosumab.
New Antiepileptic No Better for Bones Than Older Drugs
BALTIMORE – Levetiracetam had effects on bone mineral density and markers of bone turnover that were similar to those seen with the older antiepileptic drugs carbamazepine and sodium valproate in a 12-month, randomized, controlled trial of 84 patients with partial epilepsy.
The finding was counter to the expectation that levetiracetam (Keppra) would have neutral or more benign effects on bone health because of its “cleaner pharmacokinetics – no effect on vitamin D metabolism – and a different mechanism of action,” study investigator Dr. Terence J. O'Brien said in an interview.
“Most [experts] thought it would be better for bone health. However, there is a previous study in rats that did show effect on bone. … The clinical message is that neurologists need to monitor bone heath on all their patients chronically treated with AEDs,” he said.
Chronic antiepileptic drug use has been associated with increased risk of both bone disease and fracture, as well as weight gain and insulin resistance. It has been hoped that newer antiepileptic drugs with different mechanisms of action would minimize or eliminate these effects. One of these newer agents, levetiracetam, has a novel mechanism of action, binding to the SV2A receptors that interfere with synaptic vesicle exocytosis. It is not hepatically metabolized, so it does not affect hormonal levels.
“There are plenty of reasons to believe it would have fewer bone and metabolic effects, but this had never been tested before in a randomized, controlled trial,” said Dr. O'Brien, a professor of medicine at the University of Melbourne and head of the department of medicine at the Royal Melbourne Hospital.
Of 84 patients randomized to open-label substitution monotherapy with either levetiracetam or carbamazepine or valproate in the KONQUEST trial, 40 levetiracetam patients and 30 carbamazepine/valproate patients completed an assessment at 15 months. Dosing in the trial was flexible, and was increased or decreased by the treating neurologist according to tolerability and seizure control.
Dual energy X-ray absorptiometry (DXA) measurements of areal bone mineral density (aBMD) in the forearm was significantly lower at 15 months in both the levetiracetam and carbamazepine/valproate groups, compared with measurements taken at 3 months, but more so for levetiracetam, with reductions of 1.4% (P less than .001) and 0.96% (P = .015), respectively. Peripheral quantitative CT measurement of trabecular BMD in the radius was also reduced in both groups, by 2.25% (P = .005) with levetiracetam and by 2.9% (P = .001) for the older AEDs. There were no differences from 3-month assessments in aBMD of the lumbar spine or hip in either treatment group.
Markers of bone formation and resorption were among the secondary end points. The bone resorption marker beta C-terminal telopeptide of type 1 collagen was reduced in both treatment groups, by 12.8% (P = .021) with levetiracetam and by 15.6% (P = .028) with carbamazepine/valproate. However, the bone formation marker procollagen type 1 N-terminal propeptide was reduced only with the older AEDs, by 20.9% (P = .008). There were no differences in vitamin D or other markers of calcium homeostasis, Dr. O'Brien said.
Reduction in serum markers of bone turnover suggests reduced bone remodeling with AEDs, “an atypical mechanism for bone loss which warrants further study,” he said.
In the interview, he added that the lack of effect on markers of bone formation for levetiracetam may indicate some differences in the mechanism of its effect, or may just have been a lack of power.
The exploratory end points of femoral neck aBMD, total bone area (trabecular), trabecular bone mineral content, and total bone area (cortical) were all significantly reduced in both groups. However, the anthropometric exploratory end points of weight and body mass index were increased only with the older AEDs, by 2.0% (P = .039) and 2.15% (P = .044), respectively.
There are no clear guidelines for bone health monitoring in patients on AEDs. “What we recommend is when you start the drug, [get] a baseline, and then [monitor] every 3–5 years. Vitamin D levels should also be checked and supplemented if deficient,” he said in the interview.
A UCB Pharma spokeswoman declined to comment on the findings of KONQUEST.
BALTIMORE – Levetiracetam had effects on bone mineral density and markers of bone turnover that were similar to those seen with the older antiepileptic drugs carbamazepine and sodium valproate in a 12-month, randomized, controlled trial of 84 patients with partial epilepsy.
The finding was counter to the expectation that levetiracetam (Keppra) would have neutral or more benign effects on bone health because of its “cleaner pharmacokinetics – no effect on vitamin D metabolism – and a different mechanism of action,” study investigator Dr. Terence J. O'Brien said in an interview.
“Most [experts] thought it would be better for bone health. However, there is a previous study in rats that did show effect on bone. … The clinical message is that neurologists need to monitor bone heath on all their patients chronically treated with AEDs,” he said.
Chronic antiepileptic drug use has been associated with increased risk of both bone disease and fracture, as well as weight gain and insulin resistance. It has been hoped that newer antiepileptic drugs with different mechanisms of action would minimize or eliminate these effects. One of these newer agents, levetiracetam, has a novel mechanism of action, binding to the SV2A receptors that interfere with synaptic vesicle exocytosis. It is not hepatically metabolized, so it does not affect hormonal levels.
“There are plenty of reasons to believe it would have fewer bone and metabolic effects, but this had never been tested before in a randomized, controlled trial,” said Dr. O'Brien, a professor of medicine at the University of Melbourne and head of the department of medicine at the Royal Melbourne Hospital.
Of 84 patients randomized to open-label substitution monotherapy with either levetiracetam or carbamazepine or valproate in the KONQUEST trial, 40 levetiracetam patients and 30 carbamazepine/valproate patients completed an assessment at 15 months. Dosing in the trial was flexible, and was increased or decreased by the treating neurologist according to tolerability and seizure control.
Dual energy X-ray absorptiometry (DXA) measurements of areal bone mineral density (aBMD) in the forearm was significantly lower at 15 months in both the levetiracetam and carbamazepine/valproate groups, compared with measurements taken at 3 months, but more so for levetiracetam, with reductions of 1.4% (P less than .001) and 0.96% (P = .015), respectively. Peripheral quantitative CT measurement of trabecular BMD in the radius was also reduced in both groups, by 2.25% (P = .005) with levetiracetam and by 2.9% (P = .001) for the older AEDs. There were no differences from 3-month assessments in aBMD of the lumbar spine or hip in either treatment group.
Markers of bone formation and resorption were among the secondary end points. The bone resorption marker beta C-terminal telopeptide of type 1 collagen was reduced in both treatment groups, by 12.8% (P = .021) with levetiracetam and by 15.6% (P = .028) with carbamazepine/valproate. However, the bone formation marker procollagen type 1 N-terminal propeptide was reduced only with the older AEDs, by 20.9% (P = .008). There were no differences in vitamin D or other markers of calcium homeostasis, Dr. O'Brien said.
Reduction in serum markers of bone turnover suggests reduced bone remodeling with AEDs, “an atypical mechanism for bone loss which warrants further study,” he said.
In the interview, he added that the lack of effect on markers of bone formation for levetiracetam may indicate some differences in the mechanism of its effect, or may just have been a lack of power.
The exploratory end points of femoral neck aBMD, total bone area (trabecular), trabecular bone mineral content, and total bone area (cortical) were all significantly reduced in both groups. However, the anthropometric exploratory end points of weight and body mass index were increased only with the older AEDs, by 2.0% (P = .039) and 2.15% (P = .044), respectively.
There are no clear guidelines for bone health monitoring in patients on AEDs. “What we recommend is when you start the drug, [get] a baseline, and then [monitor] every 3–5 years. Vitamin D levels should also be checked and supplemented if deficient,” he said in the interview.
A UCB Pharma spokeswoman declined to comment on the findings of KONQUEST.
BALTIMORE – Levetiracetam had effects on bone mineral density and markers of bone turnover that were similar to those seen with the older antiepileptic drugs carbamazepine and sodium valproate in a 12-month, randomized, controlled trial of 84 patients with partial epilepsy.
The finding was counter to the expectation that levetiracetam (Keppra) would have neutral or more benign effects on bone health because of its “cleaner pharmacokinetics – no effect on vitamin D metabolism – and a different mechanism of action,” study investigator Dr. Terence J. O'Brien said in an interview.
“Most [experts] thought it would be better for bone health. However, there is a previous study in rats that did show effect on bone. … The clinical message is that neurologists need to monitor bone heath on all their patients chronically treated with AEDs,” he said.
Chronic antiepileptic drug use has been associated with increased risk of both bone disease and fracture, as well as weight gain and insulin resistance. It has been hoped that newer antiepileptic drugs with different mechanisms of action would minimize or eliminate these effects. One of these newer agents, levetiracetam, has a novel mechanism of action, binding to the SV2A receptors that interfere with synaptic vesicle exocytosis. It is not hepatically metabolized, so it does not affect hormonal levels.
“There are plenty of reasons to believe it would have fewer bone and metabolic effects, but this had never been tested before in a randomized, controlled trial,” said Dr. O'Brien, a professor of medicine at the University of Melbourne and head of the department of medicine at the Royal Melbourne Hospital.
Of 84 patients randomized to open-label substitution monotherapy with either levetiracetam or carbamazepine or valproate in the KONQUEST trial, 40 levetiracetam patients and 30 carbamazepine/valproate patients completed an assessment at 15 months. Dosing in the trial was flexible, and was increased or decreased by the treating neurologist according to tolerability and seizure control.
Dual energy X-ray absorptiometry (DXA) measurements of areal bone mineral density (aBMD) in the forearm was significantly lower at 15 months in both the levetiracetam and carbamazepine/valproate groups, compared with measurements taken at 3 months, but more so for levetiracetam, with reductions of 1.4% (P less than .001) and 0.96% (P = .015), respectively. Peripheral quantitative CT measurement of trabecular BMD in the radius was also reduced in both groups, by 2.25% (P = .005) with levetiracetam and by 2.9% (P = .001) for the older AEDs. There were no differences from 3-month assessments in aBMD of the lumbar spine or hip in either treatment group.
Markers of bone formation and resorption were among the secondary end points. The bone resorption marker beta C-terminal telopeptide of type 1 collagen was reduced in both treatment groups, by 12.8% (P = .021) with levetiracetam and by 15.6% (P = .028) with carbamazepine/valproate. However, the bone formation marker procollagen type 1 N-terminal propeptide was reduced only with the older AEDs, by 20.9% (P = .008). There were no differences in vitamin D or other markers of calcium homeostasis, Dr. O'Brien said.
Reduction in serum markers of bone turnover suggests reduced bone remodeling with AEDs, “an atypical mechanism for bone loss which warrants further study,” he said.
In the interview, he added that the lack of effect on markers of bone formation for levetiracetam may indicate some differences in the mechanism of its effect, or may just have been a lack of power.
The exploratory end points of femoral neck aBMD, total bone area (trabecular), trabecular bone mineral content, and total bone area (cortical) were all significantly reduced in both groups. However, the anthropometric exploratory end points of weight and body mass index were increased only with the older AEDs, by 2.0% (P = .039) and 2.15% (P = .044), respectively.
There are no clear guidelines for bone health monitoring in patients on AEDs. “What we recommend is when you start the drug, [get] a baseline, and then [monitor] every 3–5 years. Vitamin D levels should also be checked and supplemented if deficient,” he said in the interview.
A UCB Pharma spokeswoman declined to comment on the findings of KONQUEST.
FROM THE ANNUAL MEETING OF THE AMERICAN EPILEPSY SOCIETY
Major Finding: Forearm aBMD was significantly lower at 15
months in both the levetiracetam and carbamazepine/valproate groups, but
more so for levetiracetam, with reductions of 1.4% (P less than .001) and 0.96% (P = .015), respectively.
Data Source: Single-center, open-label, randomized study of 84 epilepsy patients.
Disclosures:
The study was partially funded by UCB Pharma, but it had no role in its
design, data collection, analysis, or interpretation. Dr. O'Brien had
no additional disclosures.
Growth Hormone Builds Bone in Obese Women
CHICAGO – Six months of growth hormone therapy significantly increased bone formation, vitamin D, and thigh muscle mass while decreasing abdominal fat in a study of women with abdominal obesity.
The randomized, double-blind, placebo-controlled trial was the first to explore the relationship between growth hormone levels and bone density in obese but otherwise healthy premenopausal women, Dr. Miriam A. Bredella of Massachusetts General Hospital and Harvard Medical School, Boston, said in at the meeting.
The study builds on work presented by Dr. Bredella at last year's Radiological Society of North America meeting showing an association between abdominal obesity and low bone mineral density in premenopausal women.
That study was the first to implicate abdominal fat as a risk factor for osteoporosis.
The study challenged previous research findings suggesting that increased weight protects against osteoporosis. Those previous studies focused primarily on body mass index (BMI), which incorporates measures of muscle and bone mass and subcutaneous fat as well as visceral fat. Dr. Bredella's work zeroed in on visceral fat.
In the present study, 79 women with low growth hormone levels were randomized to receive low-dose growth hormone replacement therapy or placebo for 6 months. They had a mean age of 36 years and a mean body mass index of 35 kg/m
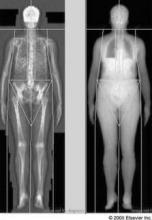
Subjects received MR spectroscopy to measure bone marrow fat and computed tomography to measure subcutaneous and visceral abdominal fat and thigh muscle mass at baseline and 6 months.
The participants were instructed not to change exercise regimens during the study and were monitored for changes in blood glucose.
One of the most surprising and important findings, according to Dr. Bredella, was that 32% of these obese but otherwise healthy young women were already osteopenic (T-score between −2.5 and −1) at baseline and that one had developed osteoporosis (T-score below −2.5).
“It's important that people become aware that obesity doesn't protect against bone loss,” she said.
Growth hormone was associated with increased P1NP (procollagen type 1 amino-terminal propeptide, a marker of bone formation) and CTX (carboxy-terminal collagen crosslinks, a marker of bone resorption), as well as increased vitamin D, thigh muscle mass, and decreased visceral and subcutaneous abdominal fat, compared with placebo, Dr. Bredella said.
Patients with the greatest abdominal fat loss had the greatest increases in bone formation.
Patients with the greatest increases in vitamin D also had the greatest increases in bone formation.
No statistically significant differences were found between the two groups in the more common side effects of growth hormone therapy, including edema of the hands and carpal tunnel syndrome.
“Overall, our patients didn't lose weight, but they had a redistribution of their body fat and muscle mass,” Dr. Bredella noted.
“They lost belly fat but increased their muscle mass, and because muscle is heavier than fat, their overall weight did not change,” she said.
Although the high cost of growth hormone replacement therapy would likely prohibit its widespread use as a treatment for obesity-related bone loss, the results of this study suggest new treatment possibilities.
“It's not going to be the magic therapy for obesity and bone loss, but it could help maybe someone who was unable to lose weight to lower their risk profile for diabetes and cardiovascular disease.”
However, growth hormone therapy “could be used in the aging population because we know as we get older, our growth hormone levels go down,” she added.
CHICAGO – Six months of growth hormone therapy significantly increased bone formation, vitamin D, and thigh muscle mass while decreasing abdominal fat in a study of women with abdominal obesity.
The randomized, double-blind, placebo-controlled trial was the first to explore the relationship between growth hormone levels and bone density in obese but otherwise healthy premenopausal women, Dr. Miriam A. Bredella of Massachusetts General Hospital and Harvard Medical School, Boston, said in at the meeting.
The study builds on work presented by Dr. Bredella at last year's Radiological Society of North America meeting showing an association between abdominal obesity and low bone mineral density in premenopausal women.
That study was the first to implicate abdominal fat as a risk factor for osteoporosis.
The study challenged previous research findings suggesting that increased weight protects against osteoporosis. Those previous studies focused primarily on body mass index (BMI), which incorporates measures of muscle and bone mass and subcutaneous fat as well as visceral fat. Dr. Bredella's work zeroed in on visceral fat.
In the present study, 79 women with low growth hormone levels were randomized to receive low-dose growth hormone replacement therapy or placebo for 6 months. They had a mean age of 36 years and a mean body mass index of 35 kg/m
Subjects received MR spectroscopy to measure bone marrow fat and computed tomography to measure subcutaneous and visceral abdominal fat and thigh muscle mass at baseline and 6 months.
The participants were instructed not to change exercise regimens during the study and were monitored for changes in blood glucose.
One of the most surprising and important findings, according to Dr. Bredella, was that 32% of these obese but otherwise healthy young women were already osteopenic (T-score between −2.5 and −1) at baseline and that one had developed osteoporosis (T-score below −2.5).
“It's important that people become aware that obesity doesn't protect against bone loss,” she said.
Growth hormone was associated with increased P1NP (procollagen type 1 amino-terminal propeptide, a marker of bone formation) and CTX (carboxy-terminal collagen crosslinks, a marker of bone resorption), as well as increased vitamin D, thigh muscle mass, and decreased visceral and subcutaneous abdominal fat, compared with placebo, Dr. Bredella said.
Patients with the greatest abdominal fat loss had the greatest increases in bone formation.
Patients with the greatest increases in vitamin D also had the greatest increases in bone formation.
No statistically significant differences were found between the two groups in the more common side effects of growth hormone therapy, including edema of the hands and carpal tunnel syndrome.
“Overall, our patients didn't lose weight, but they had a redistribution of their body fat and muscle mass,” Dr. Bredella noted.
“They lost belly fat but increased their muscle mass, and because muscle is heavier than fat, their overall weight did not change,” she said.
Although the high cost of growth hormone replacement therapy would likely prohibit its widespread use as a treatment for obesity-related bone loss, the results of this study suggest new treatment possibilities.
“It's not going to be the magic therapy for obesity and bone loss, but it could help maybe someone who was unable to lose weight to lower their risk profile for diabetes and cardiovascular disease.”
However, growth hormone therapy “could be used in the aging population because we know as we get older, our growth hormone levels go down,” she added.
CHICAGO – Six months of growth hormone therapy significantly increased bone formation, vitamin D, and thigh muscle mass while decreasing abdominal fat in a study of women with abdominal obesity.
The randomized, double-blind, placebo-controlled trial was the first to explore the relationship between growth hormone levels and bone density in obese but otherwise healthy premenopausal women, Dr. Miriam A. Bredella of Massachusetts General Hospital and Harvard Medical School, Boston, said in at the meeting.
The study builds on work presented by Dr. Bredella at last year's Radiological Society of North America meeting showing an association between abdominal obesity and low bone mineral density in premenopausal women.
That study was the first to implicate abdominal fat as a risk factor for osteoporosis.
The study challenged previous research findings suggesting that increased weight protects against osteoporosis. Those previous studies focused primarily on body mass index (BMI), which incorporates measures of muscle and bone mass and subcutaneous fat as well as visceral fat. Dr. Bredella's work zeroed in on visceral fat.
In the present study, 79 women with low growth hormone levels were randomized to receive low-dose growth hormone replacement therapy or placebo for 6 months. They had a mean age of 36 years and a mean body mass index of 35 kg/m
Subjects received MR spectroscopy to measure bone marrow fat and computed tomography to measure subcutaneous and visceral abdominal fat and thigh muscle mass at baseline and 6 months.
The participants were instructed not to change exercise regimens during the study and were monitored for changes in blood glucose.
One of the most surprising and important findings, according to Dr. Bredella, was that 32% of these obese but otherwise healthy young women were already osteopenic (T-score between −2.5 and −1) at baseline and that one had developed osteoporosis (T-score below −2.5).
“It's important that people become aware that obesity doesn't protect against bone loss,” she said.
Growth hormone was associated with increased P1NP (procollagen type 1 amino-terminal propeptide, a marker of bone formation) and CTX (carboxy-terminal collagen crosslinks, a marker of bone resorption), as well as increased vitamin D, thigh muscle mass, and decreased visceral and subcutaneous abdominal fat, compared with placebo, Dr. Bredella said.
Patients with the greatest abdominal fat loss had the greatest increases in bone formation.
Patients with the greatest increases in vitamin D also had the greatest increases in bone formation.
No statistically significant differences were found between the two groups in the more common side effects of growth hormone therapy, including edema of the hands and carpal tunnel syndrome.
“Overall, our patients didn't lose weight, but they had a redistribution of their body fat and muscle mass,” Dr. Bredella noted.
“They lost belly fat but increased their muscle mass, and because muscle is heavier than fat, their overall weight did not change,” she said.
Although the high cost of growth hormone replacement therapy would likely prohibit its widespread use as a treatment for obesity-related bone loss, the results of this study suggest new treatment possibilities.
“It's not going to be the magic therapy for obesity and bone loss, but it could help maybe someone who was unable to lose weight to lower their risk profile for diabetes and cardiovascular disease.”
However, growth hormone therapy “could be used in the aging population because we know as we get older, our growth hormone levels go down,” she added.
FROM THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Six months of growth hormone therapy
significantly increased bone formation, vitamin D, and thigh muscle mass
while decreasing abdominal fat in a study of abdominally obese women.
Data Source:
A total of 79 women with low growth hormone levels were randomized to
receive low-dose growth hormone replacement therapy or placebo for 6
months.
Disclosures: Dr. Bredella had no disclosures related to this study.
Evidence Suggests Optimal Intervals for Osteoporosis Screening
Based on available evidence, osteoporosis screening should take place at 15-year intervals for postmenopausal women who have normal bone density or mild osteopenia at their first assessment, at 5-year intervals for those who have moderate osteopenia, and at 1-year intervals for those who have advanced osteopenia, according to a report in the Jan. 19 New England Journal of Medicine.
Screening at shorter intervals is unlikely to improve prediction of the transition to osteoporosis, and thus won’t help clinicians judge when to start osteoporosis therapy so as to avert hip or vertebral fractures, said Dr. Margaret L. Gourlay of the department of family medicine, University of North Carolina, Chapel Hill, and her associates in the Study of Osteoporotic Fractures research group.
Current guidelines do not specify how long to wait between bone mineral density screening with dual-energy x-ray absorptiometry (DEXA), and no U.S. study to date "has addressed this clinical uncertainty," they noted.
"To determine how the BMD testing interval relates to the timing of the transition from normal [bone mineral density] or osteopenia to the development of osteoporosis before a hip or clinical vertebral fracture occurs, we conducted competing-risk analyses of data from 4,957 women, 67 years of age or older, who did not have osteoporosis at baseline and who were followed longitudinally for up to 15 years in the [Study of Osteoporotic Fractures]," the investigators said.
The appropriate screening interval was defined as the estimated time for 10% of the study subjects in each category of osteopenia severity to make the transition from normal BMD or osteopenia to osteoporosis before fractures occurred and before treatment for osteoporosis was initiated. The three categories of severity were normal BMD/mild osteopenia (T score of greater than -1.50) at the initial assessment, moderate osteopenia (T score of -1.50 to -1.99), and advanced osteopenia (T score of -2.00 to -2.49).
This interval was found to be 15 years for normal BMD/mild osteopenia, 5 years for moderate osteopenia, and 1 year for advanced osteopenia, Dr. Gourlay and her colleagues said (N. Engl. J. Med. 2012;366:225-33).
"Recent controversy over the harms of excessive screening for other chronic diseases reinforces the importance of developing a rational screening program for osteoporosis that is based on the best available evidence rather than on health care marketing, advocacy, and public beliefs that have encouraged overtesting and overtreatment in the U.S.," they noted.
"Our estimates for BMD testing proved to be robust after adjustment for major clinical risk factors" such as fracture history, smoking status, use of estrogen, and use of glucocorticoids. "However, clinicians may choose to reevaluate patients before our estimated screening intervals if there is evidence of decreased activity or mobility, weight loss, or other risk factors not considered in our analyses," they said.
This study was supported by the National Institutes of Health. No potential conflicts of interest were reported.
Based on available evidence, osteoporosis screening should take place at 15-year intervals for postmenopausal women who have normal bone density or mild osteopenia at their first assessment, at 5-year intervals for those who have moderate osteopenia, and at 1-year intervals for those who have advanced osteopenia, according to a report in the Jan. 19 New England Journal of Medicine.
Screening at shorter intervals is unlikely to improve prediction of the transition to osteoporosis, and thus won’t help clinicians judge when to start osteoporosis therapy so as to avert hip or vertebral fractures, said Dr. Margaret L. Gourlay of the department of family medicine, University of North Carolina, Chapel Hill, and her associates in the Study of Osteoporotic Fractures research group.
Current guidelines do not specify how long to wait between bone mineral density screening with dual-energy x-ray absorptiometry (DEXA), and no U.S. study to date "has addressed this clinical uncertainty," they noted.
"To determine how the BMD testing interval relates to the timing of the transition from normal [bone mineral density] or osteopenia to the development of osteoporosis before a hip or clinical vertebral fracture occurs, we conducted competing-risk analyses of data from 4,957 women, 67 years of age or older, who did not have osteoporosis at baseline and who were followed longitudinally for up to 15 years in the [Study of Osteoporotic Fractures]," the investigators said.
The appropriate screening interval was defined as the estimated time for 10% of the study subjects in each category of osteopenia severity to make the transition from normal BMD or osteopenia to osteoporosis before fractures occurred and before treatment for osteoporosis was initiated. The three categories of severity were normal BMD/mild osteopenia (T score of greater than -1.50) at the initial assessment, moderate osteopenia (T score of -1.50 to -1.99), and advanced osteopenia (T score of -2.00 to -2.49).
This interval was found to be 15 years for normal BMD/mild osteopenia, 5 years for moderate osteopenia, and 1 year for advanced osteopenia, Dr. Gourlay and her colleagues said (N. Engl. J. Med. 2012;366:225-33).
"Recent controversy over the harms of excessive screening for other chronic diseases reinforces the importance of developing a rational screening program for osteoporosis that is based on the best available evidence rather than on health care marketing, advocacy, and public beliefs that have encouraged overtesting and overtreatment in the U.S.," they noted.
"Our estimates for BMD testing proved to be robust after adjustment for major clinical risk factors" such as fracture history, smoking status, use of estrogen, and use of glucocorticoids. "However, clinicians may choose to reevaluate patients before our estimated screening intervals if there is evidence of decreased activity or mobility, weight loss, or other risk factors not considered in our analyses," they said.
This study was supported by the National Institutes of Health. No potential conflicts of interest were reported.
Based on available evidence, osteoporosis screening should take place at 15-year intervals for postmenopausal women who have normal bone density or mild osteopenia at their first assessment, at 5-year intervals for those who have moderate osteopenia, and at 1-year intervals for those who have advanced osteopenia, according to a report in the Jan. 19 New England Journal of Medicine.
Screening at shorter intervals is unlikely to improve prediction of the transition to osteoporosis, and thus won’t help clinicians judge when to start osteoporosis therapy so as to avert hip or vertebral fractures, said Dr. Margaret L. Gourlay of the department of family medicine, University of North Carolina, Chapel Hill, and her associates in the Study of Osteoporotic Fractures research group.
Current guidelines do not specify how long to wait between bone mineral density screening with dual-energy x-ray absorptiometry (DEXA), and no U.S. study to date "has addressed this clinical uncertainty," they noted.
"To determine how the BMD testing interval relates to the timing of the transition from normal [bone mineral density] or osteopenia to the development of osteoporosis before a hip or clinical vertebral fracture occurs, we conducted competing-risk analyses of data from 4,957 women, 67 years of age or older, who did not have osteoporosis at baseline and who were followed longitudinally for up to 15 years in the [Study of Osteoporotic Fractures]," the investigators said.
The appropriate screening interval was defined as the estimated time for 10% of the study subjects in each category of osteopenia severity to make the transition from normal BMD or osteopenia to osteoporosis before fractures occurred and before treatment for osteoporosis was initiated. The three categories of severity were normal BMD/mild osteopenia (T score of greater than -1.50) at the initial assessment, moderate osteopenia (T score of -1.50 to -1.99), and advanced osteopenia (T score of -2.00 to -2.49).
This interval was found to be 15 years for normal BMD/mild osteopenia, 5 years for moderate osteopenia, and 1 year for advanced osteopenia, Dr. Gourlay and her colleagues said (N. Engl. J. Med. 2012;366:225-33).
"Recent controversy over the harms of excessive screening for other chronic diseases reinforces the importance of developing a rational screening program for osteoporosis that is based on the best available evidence rather than on health care marketing, advocacy, and public beliefs that have encouraged overtesting and overtreatment in the U.S.," they noted.
"Our estimates for BMD testing proved to be robust after adjustment for major clinical risk factors" such as fracture history, smoking status, use of estrogen, and use of glucocorticoids. "However, clinicians may choose to reevaluate patients before our estimated screening intervals if there is evidence of decreased activity or mobility, weight loss, or other risk factors not considered in our analyses," they said.
This study was supported by the National Institutes of Health. No potential conflicts of interest were reported.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: DEXA screening for osteoporosis should be done at 15-year intervals for women with normal BMD or mild osteopenia (T score of greater than -1.50) at their initial screen, at 5-year intervals for those who have moderate osteopenia (T score of -1.50 to -1.99), and at 1-year intervals for those who have advanced osteopenia (T score of -2.00 to -2.49).
Data Source: Analysis of data from the longitudinal Study of Osteoporotic Fractures involving 4,957 postmenopausal women aged 67 years and older at baseline who were followed for 15 years.
Disclosures: This study was supported by the National Institutes of Health. No potential conflicts of interest were reported.
New Anticonvulsants Did Not Impair Bone Density in VA Study
SAN DIEGO – Newer anticonvulsants do not appear to be associated with the reduced bone mineral density seen with traditional anticonvulsants, based on results from a retrospective Veterans Affairs study.
Observational studies have linked traditional anticonvulsants, such as phenytoin, carbamazepine, and valproic acid, to reduced bone mineral density (Neurology 2004;62:2051-7). There are few data on this score regarding the newer anticonvulsants, including gabapentin, levetiracetam, lamotrigine, and topiramate, drugs increasingly prescribed not only for seizure disorders but for mood disorders and neuropathic pain as well.
Dr. Richard Lee and coworkers at Duke University Medical Center, Durham, N.C., performed a retrospective study of 1,799 patients who underwent bone mineral density measurement at the Durham VA Medical Center from 2005 through June 2010. The study population comprised 679 patients on newer anticonvulsants and 382 on traditional antiepileptic drugs.
Bone mineral density in patients on traditional anticonvulsants was progressively lower at the lumbar spine, total hip, and femoral neck with each additional 90-day period on medication during the previous 10 years, based on a multivariate logistic regression analysis.
In contrast, bone density increased at the lumbar spine and total hip with exposure to the newer nonenzyme-inducing anticonvulsants. There was a nonsignificant trend for increasing bone density at the femoral neck with greater exposure to these agents. For every 90 days on one of the newer nonenzyme-inducing anticonvulsants (lamotrigine, gabapentin, levetiracetam, pregabalin), dual-energy x-ray absorptiometry T scores increased significantly by 0.13 at the lumbar spine and by 0.087 at the total hip.
Topiramate, unlike the other newer anticonvulsants, is enzyme inducing, yet it also showed favorable bone-boosting trends that did not reach statistical significance.
The analysis was adjusted for age, race, body mass index, alcohol and tobacco use, prior fractures, and medical comorbidities. Dr. Lee said he had no disclosures.
SAN DIEGO – Newer anticonvulsants do not appear to be associated with the reduced bone mineral density seen with traditional anticonvulsants, based on results from a retrospective Veterans Affairs study.
Observational studies have linked traditional anticonvulsants, such as phenytoin, carbamazepine, and valproic acid, to reduced bone mineral density (Neurology 2004;62:2051-7). There are few data on this score regarding the newer anticonvulsants, including gabapentin, levetiracetam, lamotrigine, and topiramate, drugs increasingly prescribed not only for seizure disorders but for mood disorders and neuropathic pain as well.
Dr. Richard Lee and coworkers at Duke University Medical Center, Durham, N.C., performed a retrospective study of 1,799 patients who underwent bone mineral density measurement at the Durham VA Medical Center from 2005 through June 2010. The study population comprised 679 patients on newer anticonvulsants and 382 on traditional antiepileptic drugs.
Bone mineral density in patients on traditional anticonvulsants was progressively lower at the lumbar spine, total hip, and femoral neck with each additional 90-day period on medication during the previous 10 years, based on a multivariate logistic regression analysis.
In contrast, bone density increased at the lumbar spine and total hip with exposure to the newer nonenzyme-inducing anticonvulsants. There was a nonsignificant trend for increasing bone density at the femoral neck with greater exposure to these agents. For every 90 days on one of the newer nonenzyme-inducing anticonvulsants (lamotrigine, gabapentin, levetiracetam, pregabalin), dual-energy x-ray absorptiometry T scores increased significantly by 0.13 at the lumbar spine and by 0.087 at the total hip.
Topiramate, unlike the other newer anticonvulsants, is enzyme inducing, yet it also showed favorable bone-boosting trends that did not reach statistical significance.
The analysis was adjusted for age, race, body mass index, alcohol and tobacco use, prior fractures, and medical comorbidities. Dr. Lee said he had no disclosures.
SAN DIEGO – Newer anticonvulsants do not appear to be associated with the reduced bone mineral density seen with traditional anticonvulsants, based on results from a retrospective Veterans Affairs study.
Observational studies have linked traditional anticonvulsants, such as phenytoin, carbamazepine, and valproic acid, to reduced bone mineral density (Neurology 2004;62:2051-7). There are few data on this score regarding the newer anticonvulsants, including gabapentin, levetiracetam, lamotrigine, and topiramate, drugs increasingly prescribed not only for seizure disorders but for mood disorders and neuropathic pain as well.
Dr. Richard Lee and coworkers at Duke University Medical Center, Durham, N.C., performed a retrospective study of 1,799 patients who underwent bone mineral density measurement at the Durham VA Medical Center from 2005 through June 2010. The study population comprised 679 patients on newer anticonvulsants and 382 on traditional antiepileptic drugs.
Bone mineral density in patients on traditional anticonvulsants was progressively lower at the lumbar spine, total hip, and femoral neck with each additional 90-day period on medication during the previous 10 years, based on a multivariate logistic regression analysis.
In contrast, bone density increased at the lumbar spine and total hip with exposure to the newer nonenzyme-inducing anticonvulsants. There was a nonsignificant trend for increasing bone density at the femoral neck with greater exposure to these agents. For every 90 days on one of the newer nonenzyme-inducing anticonvulsants (lamotrigine, gabapentin, levetiracetam, pregabalin), dual-energy x-ray absorptiometry T scores increased significantly by 0.13 at the lumbar spine and by 0.087 at the total hip.
Topiramate, unlike the other newer anticonvulsants, is enzyme inducing, yet it also showed favorable bone-boosting trends that did not reach statistical significance.
The analysis was adjusted for age, race, body mass index, alcohol and tobacco use, prior fractures, and medical comorbidities. Dr. Lee said he had no disclosures.
From the Annual Meeting of the American Society for Bone and Mineral Research
Low Vitamin D Levels Tied to Psychotic Symptoms in Teens
TORONTO – Low vitamin D levels were linked with more psychotic features in mentally ill adolescents, in a small study.
Studies have linked vitamin D deficiency with seasonal affective disorder, schizophrenia, and depression, Dr. Barbara L. Gracious of Ohio State University, Columbus, said at the meeting. She and her colleagues studied 104 consecutive teens seen for acute or partial hospital stays for psychiatric symptoms over an 18-month period. Patients' average age was 15, 27% were male, and 73% were white. Overall, 72% had low vitamin D levels (25-OHD levels less than 30 ng/mL), and 34% were vitamin D deficient (25-OHD levels less than 20 ng/mL). By comparison, 9% of a cohort of teens from the NHANES (National Health and Nutrition Survey) were vitamin D deficient, the researchers noted.
Psychotic features were seen in 40% of the teens with low vitamin D levels and 16% of those with normal levels, a statistically significant difference. Black ethnicity was linked with vitamin D deficiency, but vitamin D–deficient black teens were not significantly more likely than were vitamin D–deficient white teens to exhibit psychotic features.
No studies indicate that vitamin D deficiency is a causative factor in psychosis.
Dr. Gracious is a consultant for Johnson & Johnson. None of her coauthors reported conflicts. The study was supported by the National Institutes of Health, Ohio State University, and the University of Rochester (N.Y.).
TORONTO – Low vitamin D levels were linked with more psychotic features in mentally ill adolescents, in a small study.
Studies have linked vitamin D deficiency with seasonal affective disorder, schizophrenia, and depression, Dr. Barbara L. Gracious of Ohio State University, Columbus, said at the meeting. She and her colleagues studied 104 consecutive teens seen for acute or partial hospital stays for psychiatric symptoms over an 18-month period. Patients' average age was 15, 27% were male, and 73% were white. Overall, 72% had low vitamin D levels (25-OHD levels less than 30 ng/mL), and 34% were vitamin D deficient (25-OHD levels less than 20 ng/mL). By comparison, 9% of a cohort of teens from the NHANES (National Health and Nutrition Survey) were vitamin D deficient, the researchers noted.
Psychotic features were seen in 40% of the teens with low vitamin D levels and 16% of those with normal levels, a statistically significant difference. Black ethnicity was linked with vitamin D deficiency, but vitamin D–deficient black teens were not significantly more likely than were vitamin D–deficient white teens to exhibit psychotic features.
No studies indicate that vitamin D deficiency is a causative factor in psychosis.
Dr. Gracious is a consultant for Johnson & Johnson. None of her coauthors reported conflicts. The study was supported by the National Institutes of Health, Ohio State University, and the University of Rochester (N.Y.).
TORONTO – Low vitamin D levels were linked with more psychotic features in mentally ill adolescents, in a small study.
Studies have linked vitamin D deficiency with seasonal affective disorder, schizophrenia, and depression, Dr. Barbara L. Gracious of Ohio State University, Columbus, said at the meeting. She and her colleagues studied 104 consecutive teens seen for acute or partial hospital stays for psychiatric symptoms over an 18-month period. Patients' average age was 15, 27% were male, and 73% were white. Overall, 72% had low vitamin D levels (25-OHD levels less than 30 ng/mL), and 34% were vitamin D deficient (25-OHD levels less than 20 ng/mL). By comparison, 9% of a cohort of teens from the NHANES (National Health and Nutrition Survey) were vitamin D deficient, the researchers noted.
Psychotic features were seen in 40% of the teens with low vitamin D levels and 16% of those with normal levels, a statistically significant difference. Black ethnicity was linked with vitamin D deficiency, but vitamin D–deficient black teens were not significantly more likely than were vitamin D–deficient white teens to exhibit psychotic features.
No studies indicate that vitamin D deficiency is a causative factor in psychosis.
Dr. Gracious is a consultant for Johnson & Johnson. None of her coauthors reported conflicts. The study was supported by the National Institutes of Health, Ohio State University, and the University of Rochester (N.Y.).
From the Annual Meeting of the American Academy of Child and Adolescent Psychiatry
Analysis Challenges Link Between Vitamin D Deficiency and Cancer
SAN ANTONIO – A new meta-analysis of 16 studies challenges the notion that breast cancer risk is inversely related to serum vitamin D level.
In 10 studies, vitamin D was measured before diagnosis of breast cancer; in the other 6 studies, blood samples were gathered for vitamin D measurement only after the diagnosis.
When data from all 16 studies were pooled, lower vitamin D levels were linked with a significant 1.5-fold increased rate of breast cancer (P less than .001). Thus, low vitamin D might be causally related to breast cancer, and, by extension, vitamin D supplementation might be an effective option for breast cancer prevention. But a major difficulty with this line of thinking arose when the two groups of studies were analyzed separately, Dr. Eitan Amir said at the meeting.
Only 1 of the 10 studies in which vitamin D was measured before diagnosis of breast cancer showed a significant relationship between low levels of vitamin D and subsequent increased likelihood of the malignancy. But all six studies in which serum vitamin D was measured after the diagnosis showed a significant inverse relationship. In the pooled analysis of these six studies, lower serum vitamin D was associated with a highly significant, 2.63-fold increased likelihood of breast cancer (P less than .001), said Dr. Amir of the University of Toronto.
Breast cancer cells have been shown to express vitamin D catalytic enzymes that may interfere with accurate measurement of serum levels of the vitamin, added Dr. Amir, who said he had no disclosures.
SAN ANTONIO – A new meta-analysis of 16 studies challenges the notion that breast cancer risk is inversely related to serum vitamin D level.
In 10 studies, vitamin D was measured before diagnosis of breast cancer; in the other 6 studies, blood samples were gathered for vitamin D measurement only after the diagnosis.
When data from all 16 studies were pooled, lower vitamin D levels were linked with a significant 1.5-fold increased rate of breast cancer (P less than .001). Thus, low vitamin D might be causally related to breast cancer, and, by extension, vitamin D supplementation might be an effective option for breast cancer prevention. But a major difficulty with this line of thinking arose when the two groups of studies were analyzed separately, Dr. Eitan Amir said at the meeting.
Only 1 of the 10 studies in which vitamin D was measured before diagnosis of breast cancer showed a significant relationship between low levels of vitamin D and subsequent increased likelihood of the malignancy. But all six studies in which serum vitamin D was measured after the diagnosis showed a significant inverse relationship. In the pooled analysis of these six studies, lower serum vitamin D was associated with a highly significant, 2.63-fold increased likelihood of breast cancer (P less than .001), said Dr. Amir of the University of Toronto.
Breast cancer cells have been shown to express vitamin D catalytic enzymes that may interfere with accurate measurement of serum levels of the vitamin, added Dr. Amir, who said he had no disclosures.
SAN ANTONIO – A new meta-analysis of 16 studies challenges the notion that breast cancer risk is inversely related to serum vitamin D level.
In 10 studies, vitamin D was measured before diagnosis of breast cancer; in the other 6 studies, blood samples were gathered for vitamin D measurement only after the diagnosis.
When data from all 16 studies were pooled, lower vitamin D levels were linked with a significant 1.5-fold increased rate of breast cancer (P less than .001). Thus, low vitamin D might be causally related to breast cancer, and, by extension, vitamin D supplementation might be an effective option for breast cancer prevention. But a major difficulty with this line of thinking arose when the two groups of studies were analyzed separately, Dr. Eitan Amir said at the meeting.
Only 1 of the 10 studies in which vitamin D was measured before diagnosis of breast cancer showed a significant relationship between low levels of vitamin D and subsequent increased likelihood of the malignancy. But all six studies in which serum vitamin D was measured after the diagnosis showed a significant inverse relationship. In the pooled analysis of these six studies, lower serum vitamin D was associated with a highly significant, 2.63-fold increased likelihood of breast cancer (P less than .001), said Dr. Amir of the University of Toronto.
Breast cancer cells have been shown to express vitamin D catalytic enzymes that may interfere with accurate measurement of serum levels of the vitamin, added Dr. Amir, who said he had no disclosures.
From the San Antonio Breast Cancer Symposium
Early Oophorectomy Linked to Osteoporosis and Arthritis
SAN ANTONIO – Bilateral oophorectomy in women younger than age 45 is associated with a subsequent doubled prevalence of osteoporosis and a similarly elevated rate of arthritis, compared with women with intact ovaries.
The findings from a new analysis of the Third National Health and Nutrition Examination Survey (NHANES III) had a further twist: The likelihood of having low bone mineral density and/or arthritis was even greater in the subgroup of women not on hormone replacement therapy following their surgically-induced abrupt menopause, Anne Marie McCarthy said at the symposium.
“The implication of our findings is that women who've had their ovaries removed at a young age can now be informed about their risk for bone loss over the long term. However, additional studies are needed to determine the frequency of monitoring for osteoporosis and the appropriateness of various preventive strategies in women who've had their ovaries removed,” said Ms. McCarthy, a doctoral candidate in epidemiology at Johns Hopkins University, Baltimore.
The bone mineral density analysis included 3,660 women who underwent femoral neck bone density measurement by dual energy x-ray as part of their participation in NHANES III, which was conducted in a U.S. nationally representative sample in 1988-1994.
The age-standardized mean femoral neck bone density was significantly lower in women with oophorectomy before age 45 than in those with intact ovaries: 0.711 compared with 0.743 g/m
The Johns Hopkins researchers are doing a study in which they're measuring bone mineral density before and after prophylactic oophorectomy in women who carry high-risk BRCA mutations.
The arthritis analysis included 4,039 women. Those who had undergone oophorectomy were significantly more likely to report having been informed by a physician that they have arthritis, by a margin of 45.4% to 32.1% (P less than .001). In the subset of women with oophorectomy before age 45, the prevalence of arthritis was higher at 47.7%. In a multivariate analysis, women with oophorectomy before age 45 had a 1.78-fold increased odds of arthritis compared with those with intact ovaries. If they didn't use hormone therapy, however, those odds rose to 1.99-fold.
The researchers did not study the NHANES III subjects' medical records, so they were unable to say which forms of arthritis were more prevalent in the early oophorectomy group. Ms. McCarthy said the oophorectomy-arthritis association needs confirmation by other studies. There are animal data supporting such a link, she noted.
“We think estrogen is important for the health of cartilage, so losing estrogen can lead to inflammation and damage of cartilage, perhaps,” Ms. McCarthy said.
Prophylactic bilateral oophorectomy is a widely accepted procedure to reduce the risks of breast and ovarian cancer in BRCA mutation carriers. But this indication accounts for only a small fraction of oophorectomies performed in this country. About 600,000 women per year undergo hysterectomy for indications such as fibroids, abnormal bleeding, endometriosis, and uterine prolapse, according to the Centers for Disease Control and Prevention, and about half of them have both ovaries removed at that time to prevent ovarian cancer.
NHANES III was conducted by the CDC. Ms. McCarthy said she had no relevant financial disclosures.
'Women who've had their ovaries removed at a young age can now be informed about their risk for bone loss.'
Source DR. McCARTHY
SAN ANTONIO – Bilateral oophorectomy in women younger than age 45 is associated with a subsequent doubled prevalence of osteoporosis and a similarly elevated rate of arthritis, compared with women with intact ovaries.
The findings from a new analysis of the Third National Health and Nutrition Examination Survey (NHANES III) had a further twist: The likelihood of having low bone mineral density and/or arthritis was even greater in the subgroup of women not on hormone replacement therapy following their surgically-induced abrupt menopause, Anne Marie McCarthy said at the symposium.
“The implication of our findings is that women who've had their ovaries removed at a young age can now be informed about their risk for bone loss over the long term. However, additional studies are needed to determine the frequency of monitoring for osteoporosis and the appropriateness of various preventive strategies in women who've had their ovaries removed,” said Ms. McCarthy, a doctoral candidate in epidemiology at Johns Hopkins University, Baltimore.
The bone mineral density analysis included 3,660 women who underwent femoral neck bone density measurement by dual energy x-ray as part of their participation in NHANES III, which was conducted in a U.S. nationally representative sample in 1988-1994.
The age-standardized mean femoral neck bone density was significantly lower in women with oophorectomy before age 45 than in those with intact ovaries: 0.711 compared with 0.743 g/m
The Johns Hopkins researchers are doing a study in which they're measuring bone mineral density before and after prophylactic oophorectomy in women who carry high-risk BRCA mutations.
The arthritis analysis included 4,039 women. Those who had undergone oophorectomy were significantly more likely to report having been informed by a physician that they have arthritis, by a margin of 45.4% to 32.1% (P less than .001). In the subset of women with oophorectomy before age 45, the prevalence of arthritis was higher at 47.7%. In a multivariate analysis, women with oophorectomy before age 45 had a 1.78-fold increased odds of arthritis compared with those with intact ovaries. If they didn't use hormone therapy, however, those odds rose to 1.99-fold.
The researchers did not study the NHANES III subjects' medical records, so they were unable to say which forms of arthritis were more prevalent in the early oophorectomy group. Ms. McCarthy said the oophorectomy-arthritis association needs confirmation by other studies. There are animal data supporting such a link, she noted.
“We think estrogen is important for the health of cartilage, so losing estrogen can lead to inflammation and damage of cartilage, perhaps,” Ms. McCarthy said.
Prophylactic bilateral oophorectomy is a widely accepted procedure to reduce the risks of breast and ovarian cancer in BRCA mutation carriers. But this indication accounts for only a small fraction of oophorectomies performed in this country. About 600,000 women per year undergo hysterectomy for indications such as fibroids, abnormal bleeding, endometriosis, and uterine prolapse, according to the Centers for Disease Control and Prevention, and about half of them have both ovaries removed at that time to prevent ovarian cancer.
NHANES III was conducted by the CDC. Ms. McCarthy said she had no relevant financial disclosures.
'Women who've had their ovaries removed at a young age can now be informed about their risk for bone loss.'
Source DR. McCARTHY
SAN ANTONIO – Bilateral oophorectomy in women younger than age 45 is associated with a subsequent doubled prevalence of osteoporosis and a similarly elevated rate of arthritis, compared with women with intact ovaries.
The findings from a new analysis of the Third National Health and Nutrition Examination Survey (NHANES III) had a further twist: The likelihood of having low bone mineral density and/or arthritis was even greater in the subgroup of women not on hormone replacement therapy following their surgically-induced abrupt menopause, Anne Marie McCarthy said at the symposium.
“The implication of our findings is that women who've had their ovaries removed at a young age can now be informed about their risk for bone loss over the long term. However, additional studies are needed to determine the frequency of monitoring for osteoporosis and the appropriateness of various preventive strategies in women who've had their ovaries removed,” said Ms. McCarthy, a doctoral candidate in epidemiology at Johns Hopkins University, Baltimore.
The bone mineral density analysis included 3,660 women who underwent femoral neck bone density measurement by dual energy x-ray as part of their participation in NHANES III, which was conducted in a U.S. nationally representative sample in 1988-1994.
The age-standardized mean femoral neck bone density was significantly lower in women with oophorectomy before age 45 than in those with intact ovaries: 0.711 compared with 0.743 g/m
The Johns Hopkins researchers are doing a study in which they're measuring bone mineral density before and after prophylactic oophorectomy in women who carry high-risk BRCA mutations.
The arthritis analysis included 4,039 women. Those who had undergone oophorectomy were significantly more likely to report having been informed by a physician that they have arthritis, by a margin of 45.4% to 32.1% (P less than .001). In the subset of women with oophorectomy before age 45, the prevalence of arthritis was higher at 47.7%. In a multivariate analysis, women with oophorectomy before age 45 had a 1.78-fold increased odds of arthritis compared with those with intact ovaries. If they didn't use hormone therapy, however, those odds rose to 1.99-fold.
The researchers did not study the NHANES III subjects' medical records, so they were unable to say which forms of arthritis were more prevalent in the early oophorectomy group. Ms. McCarthy said the oophorectomy-arthritis association needs confirmation by other studies. There are animal data supporting such a link, she noted.
“We think estrogen is important for the health of cartilage, so losing estrogen can lead to inflammation and damage of cartilage, perhaps,” Ms. McCarthy said.
Prophylactic bilateral oophorectomy is a widely accepted procedure to reduce the risks of breast and ovarian cancer in BRCA mutation carriers. But this indication accounts for only a small fraction of oophorectomies performed in this country. About 600,000 women per year undergo hysterectomy for indications such as fibroids, abnormal bleeding, endometriosis, and uterine prolapse, according to the Centers for Disease Control and Prevention, and about half of them have both ovaries removed at that time to prevent ovarian cancer.
NHANES III was conducted by the CDC. Ms. McCarthy said she had no relevant financial disclosures.
'Women who've had their ovaries removed at a young age can now be informed about their risk for bone loss.'
Source DR. McCARTHY
From the San Antonio Breast Cancer Symposium
Early Oophorectomy Linked to Osteoporosis, Arthritis
SAN ANTONIO – Bilateral oophorectomy in women younger than age 45 is associated with a subsequent doubled prevalence of osteoporosis and a similarly elevated rate of arthritis, compared with women with intact ovaries.
These findings from a new analysis of the Third National Health and Nutrition Examination Survey (NHANES III) had a further twist: The likelihood of having low bone mineral density and/or arthritis was even greater in the subgroup of women not on hormone replacement therapy following their surgically-induced abrupt menopause, Anne Marie McCarthy said at the San Antonio Breast Cancer Symposium.
"The implication of our findings is that women who’ve had their ovaries removed at a young age can now be informed about their risk for bone loss over the long term. However, additional studies are needed to determine the frequency of monitoring for osteoporosis and the appropriateness of various preventive strategies in women who’ve had their ovaries removed," according to Ms. McCarthy, a doctoral candidate in epidemiology at Johns Hopkins University, Baltimore.
The bone mineral density analysis included 3,660 women who underwent femoral neck bone density measurement by dual energy x-ray as part of their participation in NHANES III, which was conducted in a U.S. nationally representative sample in 1988-1994.
The age-standardized mean femoral neck bone density was significantly lower in women with oophorectomy before age 45 than in those with intact ovaries: 0.711 compared with 0.743 g/m2 (P = .017). Moreover, in a multivariate logistic regression analysis, women with early oophorectomy had an adjusted 1.78-fold increased likelihood of having osteoporosis, compared with women with intact ovaries. Upon exclusion of hormone replacement therapy users, the odds climbed even higher so that oophorectomy before age 45 was associated with a 2.92-fold increased likelihood of osteoporosis, she reported.
The Johns Hopkins investigators are now in the midst of a study in which they’re measuring bone mineral density before and after prophylactic oophorectomy in women who carry high-risk BRCA mutations.
The arthritis analysis included 4,039 women. Those who had undergone oophorectomy were significantly more likely to report having been informed by a physician that they have arthritis, by a margin of 45.4% to 32.1% (P less than .001). Among the subset of women with oophorectomy before age 45, the prevalence of arthritis was even higher at 47.7%. In a multivariate analysis, women with oophorectomy when they were younger than 45 had a 1.78-fold increased odds of arthritis compared with those with intact ovaries. If they didn’t use hormone replacement therapy, however, those odds rose to 1.99-fold.
Because the investigators didn’t study the NHANES III participants’ actual medical records, they were unable to say what specific forms of arthritis were more prevalent in the early oophorectomy group. Also, since to Ms. McCarthy’s knowledge this is the first-ever study linking oophorectomy to arthritis, this association needs confirmation by others. There are animal data supporting such a link, she noted.
"One possible mechanism is that we think estrogen is important for the health of cartilage, so losing estrogen can lead to inflammation and damage of cartilage, perhaps," Ms. McCarthy speculated.
Prophylactic bilateral oophorectomy is a widely accepted procedure to reduce the risks of breast and ovarian cancer in BRCA mutation carriers. But this indication actually accounts for only a small fraction of oophorectomies performed in this country. About 600,000 women per year undergo hysterectomy for indications including fibroids, abnormal bleeding, endometriosis, and uterine prolapse, according to the Centers for Disease Control and Prevention, and about half of them have both ovaries removed at that time to prevent ovarian cancer.
NHANES III was conducted by the CDC. Ms. McCarthy said she had no relevant financial disclosures.
SAN ANTONIO – Bilateral oophorectomy in women younger than age 45 is associated with a subsequent doubled prevalence of osteoporosis and a similarly elevated rate of arthritis, compared with women with intact ovaries.
These findings from a new analysis of the Third National Health and Nutrition Examination Survey (NHANES III) had a further twist: The likelihood of having low bone mineral density and/or arthritis was even greater in the subgroup of women not on hormone replacement therapy following their surgically-induced abrupt menopause, Anne Marie McCarthy said at the San Antonio Breast Cancer Symposium.
"The implication of our findings is that women who’ve had their ovaries removed at a young age can now be informed about their risk for bone loss over the long term. However, additional studies are needed to determine the frequency of monitoring for osteoporosis and the appropriateness of various preventive strategies in women who’ve had their ovaries removed," according to Ms. McCarthy, a doctoral candidate in epidemiology at Johns Hopkins University, Baltimore.
The bone mineral density analysis included 3,660 women who underwent femoral neck bone density measurement by dual energy x-ray as part of their participation in NHANES III, which was conducted in a U.S. nationally representative sample in 1988-1994.
The age-standardized mean femoral neck bone density was significantly lower in women with oophorectomy before age 45 than in those with intact ovaries: 0.711 compared with 0.743 g/m2 (P = .017). Moreover, in a multivariate logistic regression analysis, women with early oophorectomy had an adjusted 1.78-fold increased likelihood of having osteoporosis, compared with women with intact ovaries. Upon exclusion of hormone replacement therapy users, the odds climbed even higher so that oophorectomy before age 45 was associated with a 2.92-fold increased likelihood of osteoporosis, she reported.
The Johns Hopkins investigators are now in the midst of a study in which they’re measuring bone mineral density before and after prophylactic oophorectomy in women who carry high-risk BRCA mutations.
The arthritis analysis included 4,039 women. Those who had undergone oophorectomy were significantly more likely to report having been informed by a physician that they have arthritis, by a margin of 45.4% to 32.1% (P less than .001). Among the subset of women with oophorectomy before age 45, the prevalence of arthritis was even higher at 47.7%. In a multivariate analysis, women with oophorectomy when they were younger than 45 had a 1.78-fold increased odds of arthritis compared with those with intact ovaries. If they didn’t use hormone replacement therapy, however, those odds rose to 1.99-fold.
Because the investigators didn’t study the NHANES III participants’ actual medical records, they were unable to say what specific forms of arthritis were more prevalent in the early oophorectomy group. Also, since to Ms. McCarthy’s knowledge this is the first-ever study linking oophorectomy to arthritis, this association needs confirmation by others. There are animal data supporting such a link, she noted.
"One possible mechanism is that we think estrogen is important for the health of cartilage, so losing estrogen can lead to inflammation and damage of cartilage, perhaps," Ms. McCarthy speculated.
Prophylactic bilateral oophorectomy is a widely accepted procedure to reduce the risks of breast and ovarian cancer in BRCA mutation carriers. But this indication actually accounts for only a small fraction of oophorectomies performed in this country. About 600,000 women per year undergo hysterectomy for indications including fibroids, abnormal bleeding, endometriosis, and uterine prolapse, according to the Centers for Disease Control and Prevention, and about half of them have both ovaries removed at that time to prevent ovarian cancer.
NHANES III was conducted by the CDC. Ms. McCarthy said she had no relevant financial disclosures.
SAN ANTONIO – Bilateral oophorectomy in women younger than age 45 is associated with a subsequent doubled prevalence of osteoporosis and a similarly elevated rate of arthritis, compared with women with intact ovaries.
These findings from a new analysis of the Third National Health and Nutrition Examination Survey (NHANES III) had a further twist: The likelihood of having low bone mineral density and/or arthritis was even greater in the subgroup of women not on hormone replacement therapy following their surgically-induced abrupt menopause, Anne Marie McCarthy said at the San Antonio Breast Cancer Symposium.
"The implication of our findings is that women who’ve had their ovaries removed at a young age can now be informed about their risk for bone loss over the long term. However, additional studies are needed to determine the frequency of monitoring for osteoporosis and the appropriateness of various preventive strategies in women who’ve had their ovaries removed," according to Ms. McCarthy, a doctoral candidate in epidemiology at Johns Hopkins University, Baltimore.
The bone mineral density analysis included 3,660 women who underwent femoral neck bone density measurement by dual energy x-ray as part of their participation in NHANES III, which was conducted in a U.S. nationally representative sample in 1988-1994.
The age-standardized mean femoral neck bone density was significantly lower in women with oophorectomy before age 45 than in those with intact ovaries: 0.711 compared with 0.743 g/m2 (P = .017). Moreover, in a multivariate logistic regression analysis, women with early oophorectomy had an adjusted 1.78-fold increased likelihood of having osteoporosis, compared with women with intact ovaries. Upon exclusion of hormone replacement therapy users, the odds climbed even higher so that oophorectomy before age 45 was associated with a 2.92-fold increased likelihood of osteoporosis, she reported.
The Johns Hopkins investigators are now in the midst of a study in which they’re measuring bone mineral density before and after prophylactic oophorectomy in women who carry high-risk BRCA mutations.
The arthritis analysis included 4,039 women. Those who had undergone oophorectomy were significantly more likely to report having been informed by a physician that they have arthritis, by a margin of 45.4% to 32.1% (P less than .001). Among the subset of women with oophorectomy before age 45, the prevalence of arthritis was even higher at 47.7%. In a multivariate analysis, women with oophorectomy when they were younger than 45 had a 1.78-fold increased odds of arthritis compared with those with intact ovaries. If they didn’t use hormone replacement therapy, however, those odds rose to 1.99-fold.
Because the investigators didn’t study the NHANES III participants’ actual medical records, they were unable to say what specific forms of arthritis were more prevalent in the early oophorectomy group. Also, since to Ms. McCarthy’s knowledge this is the first-ever study linking oophorectomy to arthritis, this association needs confirmation by others. There are animal data supporting such a link, she noted.
"One possible mechanism is that we think estrogen is important for the health of cartilage, so losing estrogen can lead to inflammation and damage of cartilage, perhaps," Ms. McCarthy speculated.
Prophylactic bilateral oophorectomy is a widely accepted procedure to reduce the risks of breast and ovarian cancer in BRCA mutation carriers. But this indication actually accounts for only a small fraction of oophorectomies performed in this country. About 600,000 women per year undergo hysterectomy for indications including fibroids, abnormal bleeding, endometriosis, and uterine prolapse, according to the Centers for Disease Control and Prevention, and about half of them have both ovaries removed at that time to prevent ovarian cancer.
NHANES III was conducted by the CDC. Ms. McCarthy said she had no relevant financial disclosures.
FROM THE SAN ANTONIO BREAST CANCER SYMPOSIUM
Major Finding: The age-standardized mean femoral neck bone density was significantly lower in women with oophorectomy before age 45 than in those with intact ovaries: 0.711 compared with 0.743 g/m2 (P = .017). In a multivariate logistic regression analysis, women with early oophorectomy had an adjusted 1.78-fold increased likelihood of having osteoporosis, compared with women with intact ovaries.
Data Source: The Third National Health and Nutrition Examination Survey (NHANES III), conducted in a nationally representative sample of the U.S. population. The bone mineral density analysis included 3,660 women, and the arthritis analysis included 4,039 women.
Disclosures: NHANES III was conducted by the Centers for Disease Control and Prevention. Ms. McCarthy said she had no relevant financial disclosures.
Bisphosphonates Reduced Bone-Metastasis Risk
SAN DIEGO – Bisphosphonate use to treat osteoporosis was associated with a lower risk for bone metastases in women who later were diagnosed with breast cancer and continued on bisphosphonate therapy, according to findings from a retrospective cohort study.
This protective effect of bisphosphonates against bone metastases was independent of the stage of breast cancer at the time of diagnosis, Dr. Richard Kremer reported at the meeting.
Surprisingly, the 2% of study participants who stopped bisphosphonate therapy when diagnosed with breast cancer actually had a higher rate of developing bone metastases than did never-users of the medication, added Dr. Kremer of McGill University, Montreal.
The findings were gleaned from an administrative database that included 16,669 women diagnosed with local breast cancer and 4,850 diagnosed with regional disease during 1998-2005 and followed for a median of 5 years.
Ongoing randomized, double-blind, placebo-controlled clinical trials, such as the National Surgical Adjuvant Breast and Bowel Project B-34, are expected to provide definitive answers as to whether prescribing bisphosphonates protects against bone metastases. At present, the approved indication for bisphosphonates in the setting of cancer is for pain relief and prevention of fractures in patients with known bone metastases.
Among the 2,221 women who used a bisphosphonate in the 2-year period prior to diagnosis of their malignancy, 4% developed bone metastases. Of the other 19,298 women, 6.5% developed bone metastases.
Upon adjustment for breast cancer stage, comorbid conditions, age, and socioeconomic status, using a bisphosphonate prior to diagnosis of malignancy was associated with a 22% reduction in the risk of developing bone metastases. A definite dose-response effect was evident; the longer a woman was on a bisphosphonate, the greater her reduction in risk of bone metastases.
“Our study suggests that bisphosphonate therapy for treatment of osteoporosis produces significant additional benefit in preventing an important complication of breast cancer,” he said.
There is, however, a catch: The great majority of women who took a bisphosphonate during the 2 years prior to diagnosis of breast cancer continued to do so afterwards. Roughly 10% of breast cancer patients in the study were on a bisphosphonate both before and after diagnosis of their malignancy, 20% went on a bisphosphonate only upon being diagnosed with breast cancer, and just 2% of women took a bisphosphonate only prior to their breast cancer diagnosis. Nearly 70% of subjects were never on a bisphosphonate.
Women with localized breast cancer and a documented lack of lymph node involvement had a 27% reduction in their risk of developing bone metastases if they received a bisphosphonate both before and after diagnosis of their cancer, a 45% risk reduction if they went on the medication only following diagnosis of breast cancer, and a paradoxical twofold increased risk if they were on a bisphosphonate during the 2 years prior to diagnosis and then stopped.
Women with regional breast cancer who stopped taking a bisphosphonate within 2 years prior to diagnosis had a nonsignificant 19% increased risk of bone metastases compared with women never on the medication.
In contrast, they had a 49% reduction in risk if they received a bisphosphonate both before and after their diagnosis, and the same magnitude of risk reduction if they went on the drug only after their breast cancer was detected.
Dr. Kremer disclosed that he serves on the speakers bureaus of Merck Frosst Canada and Sanofi-Aventis.
SAN DIEGO – Bisphosphonate use to treat osteoporosis was associated with a lower risk for bone metastases in women who later were diagnosed with breast cancer and continued on bisphosphonate therapy, according to findings from a retrospective cohort study.
This protective effect of bisphosphonates against bone metastases was independent of the stage of breast cancer at the time of diagnosis, Dr. Richard Kremer reported at the meeting.
Surprisingly, the 2% of study participants who stopped bisphosphonate therapy when diagnosed with breast cancer actually had a higher rate of developing bone metastases than did never-users of the medication, added Dr. Kremer of McGill University, Montreal.
The findings were gleaned from an administrative database that included 16,669 women diagnosed with local breast cancer and 4,850 diagnosed with regional disease during 1998-2005 and followed for a median of 5 years.
Ongoing randomized, double-blind, placebo-controlled clinical trials, such as the National Surgical Adjuvant Breast and Bowel Project B-34, are expected to provide definitive answers as to whether prescribing bisphosphonates protects against bone metastases. At present, the approved indication for bisphosphonates in the setting of cancer is for pain relief and prevention of fractures in patients with known bone metastases.
Among the 2,221 women who used a bisphosphonate in the 2-year period prior to diagnosis of their malignancy, 4% developed bone metastases. Of the other 19,298 women, 6.5% developed bone metastases.
Upon adjustment for breast cancer stage, comorbid conditions, age, and socioeconomic status, using a bisphosphonate prior to diagnosis of malignancy was associated with a 22% reduction in the risk of developing bone metastases. A definite dose-response effect was evident; the longer a woman was on a bisphosphonate, the greater her reduction in risk of bone metastases.
“Our study suggests that bisphosphonate therapy for treatment of osteoporosis produces significant additional benefit in preventing an important complication of breast cancer,” he said.
There is, however, a catch: The great majority of women who took a bisphosphonate during the 2 years prior to diagnosis of breast cancer continued to do so afterwards. Roughly 10% of breast cancer patients in the study were on a bisphosphonate both before and after diagnosis of their malignancy, 20% went on a bisphosphonate only upon being diagnosed with breast cancer, and just 2% of women took a bisphosphonate only prior to their breast cancer diagnosis. Nearly 70% of subjects were never on a bisphosphonate.
Women with localized breast cancer and a documented lack of lymph node involvement had a 27% reduction in their risk of developing bone metastases if they received a bisphosphonate both before and after diagnosis of their cancer, a 45% risk reduction if they went on the medication only following diagnosis of breast cancer, and a paradoxical twofold increased risk if they were on a bisphosphonate during the 2 years prior to diagnosis and then stopped.
Women with regional breast cancer who stopped taking a bisphosphonate within 2 years prior to diagnosis had a nonsignificant 19% increased risk of bone metastases compared with women never on the medication.
In contrast, they had a 49% reduction in risk if they received a bisphosphonate both before and after their diagnosis, and the same magnitude of risk reduction if they went on the drug only after their breast cancer was detected.
Dr. Kremer disclosed that he serves on the speakers bureaus of Merck Frosst Canada and Sanofi-Aventis.
SAN DIEGO – Bisphosphonate use to treat osteoporosis was associated with a lower risk for bone metastases in women who later were diagnosed with breast cancer and continued on bisphosphonate therapy, according to findings from a retrospective cohort study.
This protective effect of bisphosphonates against bone metastases was independent of the stage of breast cancer at the time of diagnosis, Dr. Richard Kremer reported at the meeting.
Surprisingly, the 2% of study participants who stopped bisphosphonate therapy when diagnosed with breast cancer actually had a higher rate of developing bone metastases than did never-users of the medication, added Dr. Kremer of McGill University, Montreal.
The findings were gleaned from an administrative database that included 16,669 women diagnosed with local breast cancer and 4,850 diagnosed with regional disease during 1998-2005 and followed for a median of 5 years.
Ongoing randomized, double-blind, placebo-controlled clinical trials, such as the National Surgical Adjuvant Breast and Bowel Project B-34, are expected to provide definitive answers as to whether prescribing bisphosphonates protects against bone metastases. At present, the approved indication for bisphosphonates in the setting of cancer is for pain relief and prevention of fractures in patients with known bone metastases.
Among the 2,221 women who used a bisphosphonate in the 2-year period prior to diagnosis of their malignancy, 4% developed bone metastases. Of the other 19,298 women, 6.5% developed bone metastases.
Upon adjustment for breast cancer stage, comorbid conditions, age, and socioeconomic status, using a bisphosphonate prior to diagnosis of malignancy was associated with a 22% reduction in the risk of developing bone metastases. A definite dose-response effect was evident; the longer a woman was on a bisphosphonate, the greater her reduction in risk of bone metastases.
“Our study suggests that bisphosphonate therapy for treatment of osteoporosis produces significant additional benefit in preventing an important complication of breast cancer,” he said.
There is, however, a catch: The great majority of women who took a bisphosphonate during the 2 years prior to diagnosis of breast cancer continued to do so afterwards. Roughly 10% of breast cancer patients in the study were on a bisphosphonate both before and after diagnosis of their malignancy, 20% went on a bisphosphonate only upon being diagnosed with breast cancer, and just 2% of women took a bisphosphonate only prior to their breast cancer diagnosis. Nearly 70% of subjects were never on a bisphosphonate.
Women with localized breast cancer and a documented lack of lymph node involvement had a 27% reduction in their risk of developing bone metastases if they received a bisphosphonate both before and after diagnosis of their cancer, a 45% risk reduction if they went on the medication only following diagnosis of breast cancer, and a paradoxical twofold increased risk if they were on a bisphosphonate during the 2 years prior to diagnosis and then stopped.
Women with regional breast cancer who stopped taking a bisphosphonate within 2 years prior to diagnosis had a nonsignificant 19% increased risk of bone metastases compared with women never on the medication.
In contrast, they had a 49% reduction in risk if they received a bisphosphonate both before and after their diagnosis, and the same magnitude of risk reduction if they went on the drug only after their breast cancer was detected.
Dr. Kremer disclosed that he serves on the speakers bureaus of Merck Frosst Canada and Sanofi-Aventis.
From the Annual Meeting of the American Society for Bone and Mineral Research