User login
Opicapone increased on-time without dyskinesia in patients with Parkinson’s disease
PHILADELPHIA -
The 2-hour improvement was considered clinically meaningful, although the average patient in the studies had about 6 hours of off-time, said investigator Peter LeWitt, MD, of Henry Ford Hospital in West Bloomfield, Mich., and the department of neurology at Wayne State University, Detroit. Dr. LeWitt and colleagues will present the data at the annual meeting of the American Academy of Neurology.
“While this is a substantial improvement, it is 2 hours improvement over a total of 6 hours of off-time, which is not perfect,” Dr. LeWitt said in an interview. “So how could we do better is the challenge for all of us who are doing research.”
Opicapone is under development in the United States; it is currently approved in the European Union as adjunctive therapy to preparations of levodopa/DOPA decarboxylase inhibitors for patients with Parkinson’s disease and end-of-dose motor fluctuations.
The ability of opicapone to prolong the clinical actions of levodopa has been evaluated in BIPARK-1 and BIPARK-2. These two international phase 3 studies evaluated the third-generation COMT inhibitor against placebo and, in the case of BIPARK-1, against the COMT inhibitor entacapone as an active control. Each study was 14-15 weeks in duration and included a 1-year open-label phase.
In BIPARK-1, on-time without troublesome dyskinesia was significantly increased for opicapone 50 mg versus placebo, with an absolute increase of 1.9 versus 0.9 hours, respectively, from baseline to week 14 or 15 (P = .002), investigators said. Similarly, BIPARK-2 data showed an increase in this endpoint, at 1.7 versus 0.9 hours for opicapone and placebo, respectively (P = .025).
The 50-mg dose of opicapone was received by 115 patients in BIPARK-1 and 147 patients in BIPARK-2, while placebo was received by 120 and 135 patients in those two studies, respectively.
In the long-term extension studies, the mean change in on-time without dyskinesia from baseline to the end of the open-label endpoint was 2.0 hours for all 494 opicapone-treated patients in BIPARK-1 and 1.8 hours for all 339 opicapone-treated patients in BIPARK-2.
Dyskinesia was reported as a treatment-emergent adverse effect for 17.4% of opicapone-treated patients and 6.2% of placebo-treated patients, according to results of a pooled safety analysis of BIPARK-1 and BIPARK-2. However, only 1.9% of opicapone-treated patients and 0.4% of placebo-treated patients had treatment-emergent dyskinesia leading to discontinuation, and the dyskinesia was considered serious in 0.3% of the opicapone group and 0.0% of the placebo group, investigators added.
Neurocrine Biosciences has announced plans to file a New Drug Application for opicapone for Parkinson’s disease in the United States. That filing is expected to take place in the second quarter of 2019, according to an April 29 press release.
Dr. LeWitt disclosed that he has served as an advisor to Neurocrine Biosciences. He also provided disclosures related to Acadia, Acorda, Adamas, BioElectron Technology, Biotie, Britannia, Intec, Jazz Pharmaceuticals, Lundbeck, the Michael J. Fox Foundation for Parkinson’s Research, Merz, NeuroDerm, the Parkinson Study Group, Pfizer, Prexton, Sage, Scion, Sunovion, SynAgile, and US WorldMeds.
SOURCE: LeWitt P et al. AAN 2019, Abstract S4.003.
PHILADELPHIA -
The 2-hour improvement was considered clinically meaningful, although the average patient in the studies had about 6 hours of off-time, said investigator Peter LeWitt, MD, of Henry Ford Hospital in West Bloomfield, Mich., and the department of neurology at Wayne State University, Detroit. Dr. LeWitt and colleagues will present the data at the annual meeting of the American Academy of Neurology.
“While this is a substantial improvement, it is 2 hours improvement over a total of 6 hours of off-time, which is not perfect,” Dr. LeWitt said in an interview. “So how could we do better is the challenge for all of us who are doing research.”
Opicapone is under development in the United States; it is currently approved in the European Union as adjunctive therapy to preparations of levodopa/DOPA decarboxylase inhibitors for patients with Parkinson’s disease and end-of-dose motor fluctuations.
The ability of opicapone to prolong the clinical actions of levodopa has been evaluated in BIPARK-1 and BIPARK-2. These two international phase 3 studies evaluated the third-generation COMT inhibitor against placebo and, in the case of BIPARK-1, against the COMT inhibitor entacapone as an active control. Each study was 14-15 weeks in duration and included a 1-year open-label phase.
In BIPARK-1, on-time without troublesome dyskinesia was significantly increased for opicapone 50 mg versus placebo, with an absolute increase of 1.9 versus 0.9 hours, respectively, from baseline to week 14 or 15 (P = .002), investigators said. Similarly, BIPARK-2 data showed an increase in this endpoint, at 1.7 versus 0.9 hours for opicapone and placebo, respectively (P = .025).
The 50-mg dose of opicapone was received by 115 patients in BIPARK-1 and 147 patients in BIPARK-2, while placebo was received by 120 and 135 patients in those two studies, respectively.
In the long-term extension studies, the mean change in on-time without dyskinesia from baseline to the end of the open-label endpoint was 2.0 hours for all 494 opicapone-treated patients in BIPARK-1 and 1.8 hours for all 339 opicapone-treated patients in BIPARK-2.
Dyskinesia was reported as a treatment-emergent adverse effect for 17.4% of opicapone-treated patients and 6.2% of placebo-treated patients, according to results of a pooled safety analysis of BIPARK-1 and BIPARK-2. However, only 1.9% of opicapone-treated patients and 0.4% of placebo-treated patients had treatment-emergent dyskinesia leading to discontinuation, and the dyskinesia was considered serious in 0.3% of the opicapone group and 0.0% of the placebo group, investigators added.
Neurocrine Biosciences has announced plans to file a New Drug Application for opicapone for Parkinson’s disease in the United States. That filing is expected to take place in the second quarter of 2019, according to an April 29 press release.
Dr. LeWitt disclosed that he has served as an advisor to Neurocrine Biosciences. He also provided disclosures related to Acadia, Acorda, Adamas, BioElectron Technology, Biotie, Britannia, Intec, Jazz Pharmaceuticals, Lundbeck, the Michael J. Fox Foundation for Parkinson’s Research, Merz, NeuroDerm, the Parkinson Study Group, Pfizer, Prexton, Sage, Scion, Sunovion, SynAgile, and US WorldMeds.
SOURCE: LeWitt P et al. AAN 2019, Abstract S4.003.
PHILADELPHIA -
The 2-hour improvement was considered clinically meaningful, although the average patient in the studies had about 6 hours of off-time, said investigator Peter LeWitt, MD, of Henry Ford Hospital in West Bloomfield, Mich., and the department of neurology at Wayne State University, Detroit. Dr. LeWitt and colleagues will present the data at the annual meeting of the American Academy of Neurology.
“While this is a substantial improvement, it is 2 hours improvement over a total of 6 hours of off-time, which is not perfect,” Dr. LeWitt said in an interview. “So how could we do better is the challenge for all of us who are doing research.”
Opicapone is under development in the United States; it is currently approved in the European Union as adjunctive therapy to preparations of levodopa/DOPA decarboxylase inhibitors for patients with Parkinson’s disease and end-of-dose motor fluctuations.
The ability of opicapone to prolong the clinical actions of levodopa has been evaluated in BIPARK-1 and BIPARK-2. These two international phase 3 studies evaluated the third-generation COMT inhibitor against placebo and, in the case of BIPARK-1, against the COMT inhibitor entacapone as an active control. Each study was 14-15 weeks in duration and included a 1-year open-label phase.
In BIPARK-1, on-time without troublesome dyskinesia was significantly increased for opicapone 50 mg versus placebo, with an absolute increase of 1.9 versus 0.9 hours, respectively, from baseline to week 14 or 15 (P = .002), investigators said. Similarly, BIPARK-2 data showed an increase in this endpoint, at 1.7 versus 0.9 hours for opicapone and placebo, respectively (P = .025).
The 50-mg dose of opicapone was received by 115 patients in BIPARK-1 and 147 patients in BIPARK-2, while placebo was received by 120 and 135 patients in those two studies, respectively.
In the long-term extension studies, the mean change in on-time without dyskinesia from baseline to the end of the open-label endpoint was 2.0 hours for all 494 opicapone-treated patients in BIPARK-1 and 1.8 hours for all 339 opicapone-treated patients in BIPARK-2.
Dyskinesia was reported as a treatment-emergent adverse effect for 17.4% of opicapone-treated patients and 6.2% of placebo-treated patients, according to results of a pooled safety analysis of BIPARK-1 and BIPARK-2. However, only 1.9% of opicapone-treated patients and 0.4% of placebo-treated patients had treatment-emergent dyskinesia leading to discontinuation, and the dyskinesia was considered serious in 0.3% of the opicapone group and 0.0% of the placebo group, investigators added.
Neurocrine Biosciences has announced plans to file a New Drug Application for opicapone for Parkinson’s disease in the United States. That filing is expected to take place in the second quarter of 2019, according to an April 29 press release.
Dr. LeWitt disclosed that he has served as an advisor to Neurocrine Biosciences. He also provided disclosures related to Acadia, Acorda, Adamas, BioElectron Technology, Biotie, Britannia, Intec, Jazz Pharmaceuticals, Lundbeck, the Michael J. Fox Foundation for Parkinson’s Research, Merz, NeuroDerm, the Parkinson Study Group, Pfizer, Prexton, Sage, Scion, Sunovion, SynAgile, and US WorldMeds.
SOURCE: LeWitt P et al. AAN 2019, Abstract S4.003.
FROM AAN 2019
Mindfulness yoga reduced stress and motor symptoms in patients with Parkinson’s disease
Among patients with mild or moderate Parkinson’s disease, mindfulness yoga was as effective as stretching and resistance training in improving motor function and mobility, a randomized trial found.
In addition, mindfulness yoga reduced anxiety and depressive symptoms and increased spiritual well-being and health-related quality of life more than stretching and resistance training, researchers reported in JAMA Neurology.
Although guidelines support exercise for patients with Parkinson’s disease, investigators had not examined whether yoga is superior to conventional exercise for stress and symptom management in this patient population. Jojo Y. Y. Kwok, PhD, a research assistant professor of nursing at the University of Hong Kong, and her colleagues conducted an assessor-masked, randomized trial that included 138 adults with idiopathic Parkinson’s disease who were able to stand on their own and walk with or without an assistive device. The trial was conducted at 4 community rehabilitation centers in Hong Kong between December 1, 2016, and May 31, 2017. Participants were randomized to 8 weeks of mindfulness yoga delivered weekly in 90-minute group sessions (71) or stretching and resistance training delivered in weekly 60-minute group sessions (67).
The primary outcomes was psychological distress in terms of anxiety and depressive symptoms assessed with the Hospital Anxiety and Depression Scale (HADS). Secondary outcomes included motor symptom severity, mobility, spiritual well-being in terms of perceived hardship and equanimity, and health-related quality of life. The researchers assessed patients at baseline, 8 weeks, and 20 weeks.
The average age of the participants was 63.7 years; 65 (47.1%) were men. Generalized estimating equation analyses found that patients in the yoga group had significantly better outcomes, including for anxiety (time-by-group interaction, beta, –1.79 at 8 weeks and –2.05 at 20 weeks), and depressive symptoms (beta, –2.75 at 8 weeks and –2.75 at 20 weeks). These improvements were considered “statistically and clinically significant, the authors wrote. There were no significant improvements in anxiety or depressive symptoms in the stretching and resistance training group at the different time points.
Outcomes in the yoga group were also better with regards to disease-specific health-related quality of life (beta, –7.77 at 8 weeks and –7.99 at 20 weeks). Those who were in the mindfulness yoga group also had greater improvements in measures of perceived hardship and equanimity, compared with the stretching and resistance training group.
Referring to the improved psychological outcomes in the yoga group, the authors wrote, “these benefits were remarkable because the participants who received the [mindfulness yoga] intervention attended a mean of only 6 sessions.”
There were significant reductions in motor symptoms in both groups, which were significantly higher among those undergoing stretching, but the differences in the mean scores between the two groups were “clinically insignificant,” they wrote.
Three participants in the yoga group and 2 in the control group reported temporary mild knee pain. No serious adverse events were reported.
Expectation bias, selection bias, and the dropout rates of 15.2% at 8 weeks and 18.8% at 20 weeks are limitations of the study, the authors noted.
“These findings suggest that ,” Dr. Kwok and her colleagues concluded. “Considering that PD is not only a physically limiting condition but also a psychologically distressing life event, health care professionals should adopt a holistic approach in PD rehabilitation. Future rehabilitation programs could consider integrating mindfulness skills into physical therapy to enhance the holistic well-being of people with neurodegenerative conditions.”
The trial was supported by the Professional Development Fund of the Association of Hong Kong Nursing Staff. The authors had no disclosures.
SOURCE: Kwok JYY et al. JAMA Neurol. 2019 Apr 8. doi: 10.1001/jamaneurol.2019.0534.
Among patients with mild or moderate Parkinson’s disease, mindfulness yoga was as effective as stretching and resistance training in improving motor function and mobility, a randomized trial found.
In addition, mindfulness yoga reduced anxiety and depressive symptoms and increased spiritual well-being and health-related quality of life more than stretching and resistance training, researchers reported in JAMA Neurology.
Although guidelines support exercise for patients with Parkinson’s disease, investigators had not examined whether yoga is superior to conventional exercise for stress and symptom management in this patient population. Jojo Y. Y. Kwok, PhD, a research assistant professor of nursing at the University of Hong Kong, and her colleagues conducted an assessor-masked, randomized trial that included 138 adults with idiopathic Parkinson’s disease who were able to stand on their own and walk with or without an assistive device. The trial was conducted at 4 community rehabilitation centers in Hong Kong between December 1, 2016, and May 31, 2017. Participants were randomized to 8 weeks of mindfulness yoga delivered weekly in 90-minute group sessions (71) or stretching and resistance training delivered in weekly 60-minute group sessions (67).
The primary outcomes was psychological distress in terms of anxiety and depressive symptoms assessed with the Hospital Anxiety and Depression Scale (HADS). Secondary outcomes included motor symptom severity, mobility, spiritual well-being in terms of perceived hardship and equanimity, and health-related quality of life. The researchers assessed patients at baseline, 8 weeks, and 20 weeks.
The average age of the participants was 63.7 years; 65 (47.1%) were men. Generalized estimating equation analyses found that patients in the yoga group had significantly better outcomes, including for anxiety (time-by-group interaction, beta, –1.79 at 8 weeks and –2.05 at 20 weeks), and depressive symptoms (beta, –2.75 at 8 weeks and –2.75 at 20 weeks). These improvements were considered “statistically and clinically significant, the authors wrote. There were no significant improvements in anxiety or depressive symptoms in the stretching and resistance training group at the different time points.
Outcomes in the yoga group were also better with regards to disease-specific health-related quality of life (beta, –7.77 at 8 weeks and –7.99 at 20 weeks). Those who were in the mindfulness yoga group also had greater improvements in measures of perceived hardship and equanimity, compared with the stretching and resistance training group.
Referring to the improved psychological outcomes in the yoga group, the authors wrote, “these benefits were remarkable because the participants who received the [mindfulness yoga] intervention attended a mean of only 6 sessions.”
There were significant reductions in motor symptoms in both groups, which were significantly higher among those undergoing stretching, but the differences in the mean scores between the two groups were “clinically insignificant,” they wrote.
Three participants in the yoga group and 2 in the control group reported temporary mild knee pain. No serious adverse events were reported.
Expectation bias, selection bias, and the dropout rates of 15.2% at 8 weeks and 18.8% at 20 weeks are limitations of the study, the authors noted.
“These findings suggest that ,” Dr. Kwok and her colleagues concluded. “Considering that PD is not only a physically limiting condition but also a psychologically distressing life event, health care professionals should adopt a holistic approach in PD rehabilitation. Future rehabilitation programs could consider integrating mindfulness skills into physical therapy to enhance the holistic well-being of people with neurodegenerative conditions.”
The trial was supported by the Professional Development Fund of the Association of Hong Kong Nursing Staff. The authors had no disclosures.
SOURCE: Kwok JYY et al. JAMA Neurol. 2019 Apr 8. doi: 10.1001/jamaneurol.2019.0534.
Among patients with mild or moderate Parkinson’s disease, mindfulness yoga was as effective as stretching and resistance training in improving motor function and mobility, a randomized trial found.
In addition, mindfulness yoga reduced anxiety and depressive symptoms and increased spiritual well-being and health-related quality of life more than stretching and resistance training, researchers reported in JAMA Neurology.
Although guidelines support exercise for patients with Parkinson’s disease, investigators had not examined whether yoga is superior to conventional exercise for stress and symptom management in this patient population. Jojo Y. Y. Kwok, PhD, a research assistant professor of nursing at the University of Hong Kong, and her colleagues conducted an assessor-masked, randomized trial that included 138 adults with idiopathic Parkinson’s disease who were able to stand on their own and walk with or without an assistive device. The trial was conducted at 4 community rehabilitation centers in Hong Kong between December 1, 2016, and May 31, 2017. Participants were randomized to 8 weeks of mindfulness yoga delivered weekly in 90-minute group sessions (71) or stretching and resistance training delivered in weekly 60-minute group sessions (67).
The primary outcomes was psychological distress in terms of anxiety and depressive symptoms assessed with the Hospital Anxiety and Depression Scale (HADS). Secondary outcomes included motor symptom severity, mobility, spiritual well-being in terms of perceived hardship and equanimity, and health-related quality of life. The researchers assessed patients at baseline, 8 weeks, and 20 weeks.
The average age of the participants was 63.7 years; 65 (47.1%) were men. Generalized estimating equation analyses found that patients in the yoga group had significantly better outcomes, including for anxiety (time-by-group interaction, beta, –1.79 at 8 weeks and –2.05 at 20 weeks), and depressive symptoms (beta, –2.75 at 8 weeks and –2.75 at 20 weeks). These improvements were considered “statistically and clinically significant, the authors wrote. There were no significant improvements in anxiety or depressive symptoms in the stretching and resistance training group at the different time points.
Outcomes in the yoga group were also better with regards to disease-specific health-related quality of life (beta, –7.77 at 8 weeks and –7.99 at 20 weeks). Those who were in the mindfulness yoga group also had greater improvements in measures of perceived hardship and equanimity, compared with the stretching and resistance training group.
Referring to the improved psychological outcomes in the yoga group, the authors wrote, “these benefits were remarkable because the participants who received the [mindfulness yoga] intervention attended a mean of only 6 sessions.”
There were significant reductions in motor symptoms in both groups, which were significantly higher among those undergoing stretching, but the differences in the mean scores between the two groups were “clinically insignificant,” they wrote.
Three participants in the yoga group and 2 in the control group reported temporary mild knee pain. No serious adverse events were reported.
Expectation bias, selection bias, and the dropout rates of 15.2% at 8 weeks and 18.8% at 20 weeks are limitations of the study, the authors noted.
“These findings suggest that ,” Dr. Kwok and her colleagues concluded. “Considering that PD is not only a physically limiting condition but also a psychologically distressing life event, health care professionals should adopt a holistic approach in PD rehabilitation. Future rehabilitation programs could consider integrating mindfulness skills into physical therapy to enhance the holistic well-being of people with neurodegenerative conditions.”
The trial was supported by the Professional Development Fund of the Association of Hong Kong Nursing Staff. The authors had no disclosures.
SOURCE: Kwok JYY et al. JAMA Neurol. 2019 Apr 8. doi: 10.1001/jamaneurol.2019.0534.
FROM JAMA NEUROLOGY
Can intraputamenal infusions of GDNF treat Parkinson’s disease?
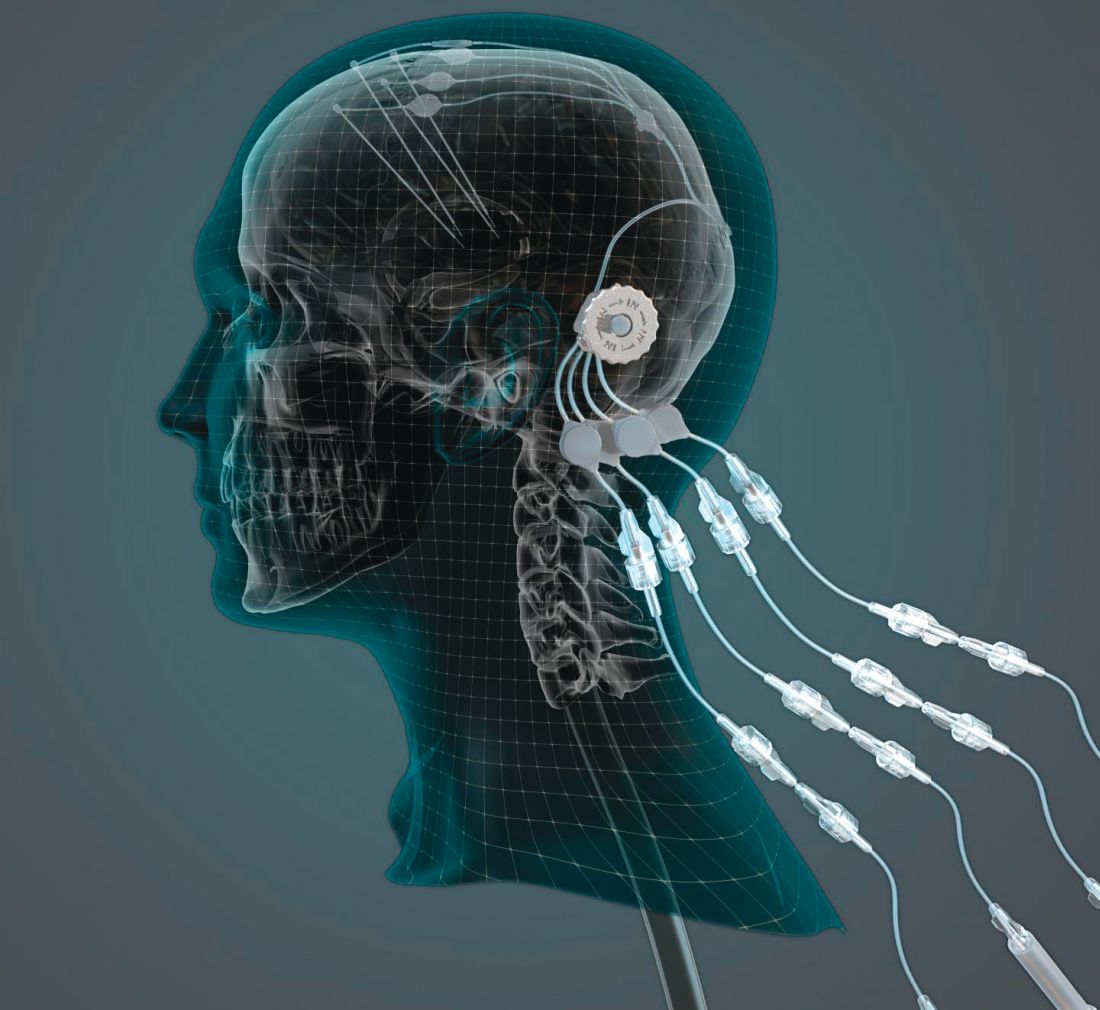
researchers reported. The investigational therapy, delivered through a skull-mounted port, was well tolerated in a 40-week, randomized, controlled trial and a 40-week, open-label extension.
Neither study met its primary endpoint, but post hoc analyses suggest possible clinical benefits. In addition, PET imaging after the 40-week, randomized trial found significantly increased 18F-DOPA uptake in patients who received GDNF. The randomized trial was published in the March 2019 issue of Brain; data from the open-label extension were published online ahead of print Feb. 26, 2019, in the Journal of Parkinson’s Disease.
“The spatial and relative magnitude of the improvement in the brain scans is beyond anything seen previously in trials of surgically delivered growth-factor treatments for Parkinson’s [disease],” said principal investigator Alan L. Whone, MBChB, PhD, of the University of Bristol (England) and North Bristol National Health Service Trust. “This represents some of the most compelling evidence yet that we may have a means to possibly reawaken and restore the dopamine brain cells that are gradually destroyed in Parkinson’s [disease].”
Nevertheless, the trial did not confirm clinical benefits. The hypothesis that growth factors can benefit patients with Parkinson’s disease may be incorrect, the researchers acknowledged. It also is possible that the hypothesis is valid and that a trial with a higher GDNF dose, longer treatment duration, patients with an earlier disease stage, or different outcome measures would yield positive results. GDNF warrants further study, they wrote.
The findings could have implications for other neurologic disorders as well.
“This trial has shown that we can safely and repeatedly infuse drugs directly into patients’ brains over months or years. This is a significant breakthrough in our ability to treat neurologic conditions ... because most drugs that might work cannot cross from the bloodstream into the brain,” said Steven Gill, MB, MS. Mr. Gill, of the North Bristol NHS Trust and the U.K.-based engineering firm Renishaw, designed the convection-enhanced delivery system used in the studies.
A neurotrophic protein
GDNF has neurorestorative and neuroprotective effects in animal models of Parkinson’s disease. In open-label studies, continuous, low-rate intraputamenal administration of GDNF has shown signs of potential efficacy, but a placebo-controlled trial did not replicate clinical benefits. In the present studies, the researchers assessed intermittent GDNF administration using convection-enhanced delivery, which can achieve wider and more even distribution of GDNF, compared with the previous approach.
The researchers conducted a single-center, randomized, double-blind, placebo-controlled trial to study this novel administration approach. Patients were aged 35-75 years, had motor symptoms for at least 5 years, and had moderate disease severity in the off state (that is, Hoehn and Yahr stage 2-3 and Unified Parkinson’s Disease Rating Scale motor score–part III [UPDRS-III] of 25-45).
In a pilot stage of the trial, six patients were randomized 2:1 to receive GDNF (120 mcg per putamen) or placebo. In the primary stage, another 35 patients were randomized 1:1 to GDNF or placebo. The primary outcome was the percentage change from baseline to week 40 in the off-state UPDRS-III among patients from the primary stage of the trial. Further analyses included all 41 patients from the pilot and primary stages.
Patients in the primary analysis had a mean age of 56.4 years and mean disease duration of 10.9 years. About half were female.
Results on primary and secondary clinical endpoints did not significantly differ between the groups. Average off state UPDRS motor score decreased by 17.3 in the active treatment group, compared with 11.8 in the placebo group.
A post hoc analysis, however, found that nine patients (43%) in the active-treatment group had a large, clinically important motor improvement of 10 or more points in the off state, whereas no placebo patients did. These “10-point responders in the GDNF group are a potential focus of interest; however, as this is a post hoc finding we would not wish to overinterpret its meaning,” Dr. Whone and his colleagues wrote. Among patients who received GDNF, PET imaging demonstrated significantly increased 18F-DOPA uptake throughout the putamen, ranging from a 25% increase in the left anterior putamen to a 100% increase in both posterior putamena, whereas patients who received placebo did not have significantly increased uptake.
No drug-related serious adverse events were reported. “The majority of device-related adverse events were port site associated, most commonly local hypertrophic scarring or infections, amenable to antibiotics,” the investigators wrote. “The frequency of these declined during the trial as surgical and device handling experience improved.”
Open-label extension
By week 80, when all participants had received GDNF, both groups showed moderate to large improvement in symptoms, compared with baseline. From baseline to week 80, percentage change in UPDRS motor score in the off state did not significantly differ between patients who received GDNF for 80 weeks and patients who received placebo followed by GDNF (26.7% vs. 27.6%). Secondary endpoints also did not differ between the groups. Treatment compliance was 97.8%; no patients discontinued the study.
The trials were funded by Parkinson’s UK with support from the Cure Parkinson’s Trust and in association with the North Bristol NHS Trust. GDNF and additional resources and funding were provided by MedGenesis Therapeutix, which owns the license for GDNF and received funding from the Michael J. Fox Foundation for Parkinson’s Research. Renishaw manufactured the convection-enhanced delivery device on behalf of North Bristol NHS Trust. The Gatsby Foundation provided a 3T MRI scanner. Some study authors are employed by and have shares or share options with MedGenesis Therapeutix. Other authors are employees of Renishaw. Dr. Gill is Renishaw’s medical director and may have a future royalty share from the drug delivery system that he invented.
SOURCES: Whone AL et al. Brain. 2019 Feb 26. doi: 10.1093/brain/awz023; Whone AL et al. J Parkinsons Dis. 2019 Feb 26. doi: 10.3233/JPD-191576.
researchers reported. The investigational therapy, delivered through a skull-mounted port, was well tolerated in a 40-week, randomized, controlled trial and a 40-week, open-label extension.
Neither study met its primary endpoint, but post hoc analyses suggest possible clinical benefits. In addition, PET imaging after the 40-week, randomized trial found significantly increased 18F-DOPA uptake in patients who received GDNF. The randomized trial was published in the March 2019 issue of Brain; data from the open-label extension were published online ahead of print Feb. 26, 2019, in the Journal of Parkinson’s Disease.
“The spatial and relative magnitude of the improvement in the brain scans is beyond anything seen previously in trials of surgically delivered growth-factor treatments for Parkinson’s [disease],” said principal investigator Alan L. Whone, MBChB, PhD, of the University of Bristol (England) and North Bristol National Health Service Trust. “This represents some of the most compelling evidence yet that we may have a means to possibly reawaken and restore the dopamine brain cells that are gradually destroyed in Parkinson’s [disease].”
Nevertheless, the trial did not confirm clinical benefits. The hypothesis that growth factors can benefit patients with Parkinson’s disease may be incorrect, the researchers acknowledged. It also is possible that the hypothesis is valid and that a trial with a higher GDNF dose, longer treatment duration, patients with an earlier disease stage, or different outcome measures would yield positive results. GDNF warrants further study, they wrote.
The findings could have implications for other neurologic disorders as well.
“This trial has shown that we can safely and repeatedly infuse drugs directly into patients’ brains over months or years. This is a significant breakthrough in our ability to treat neurologic conditions ... because most drugs that might work cannot cross from the bloodstream into the brain,” said Steven Gill, MB, MS. Mr. Gill, of the North Bristol NHS Trust and the U.K.-based engineering firm Renishaw, designed the convection-enhanced delivery system used in the studies.
A neurotrophic protein
GDNF has neurorestorative and neuroprotective effects in animal models of Parkinson’s disease. In open-label studies, continuous, low-rate intraputamenal administration of GDNF has shown signs of potential efficacy, but a placebo-controlled trial did not replicate clinical benefits. In the present studies, the researchers assessed intermittent GDNF administration using convection-enhanced delivery, which can achieve wider and more even distribution of GDNF, compared with the previous approach.
The researchers conducted a single-center, randomized, double-blind, placebo-controlled trial to study this novel administration approach. Patients were aged 35-75 years, had motor symptoms for at least 5 years, and had moderate disease severity in the off state (that is, Hoehn and Yahr stage 2-3 and Unified Parkinson’s Disease Rating Scale motor score–part III [UPDRS-III] of 25-45).
In a pilot stage of the trial, six patients were randomized 2:1 to receive GDNF (120 mcg per putamen) or placebo. In the primary stage, another 35 patients were randomized 1:1 to GDNF or placebo. The primary outcome was the percentage change from baseline to week 40 in the off-state UPDRS-III among patients from the primary stage of the trial. Further analyses included all 41 patients from the pilot and primary stages.
Patients in the primary analysis had a mean age of 56.4 years and mean disease duration of 10.9 years. About half were female.
Results on primary and secondary clinical endpoints did not significantly differ between the groups. Average off state UPDRS motor score decreased by 17.3 in the active treatment group, compared with 11.8 in the placebo group.
A post hoc analysis, however, found that nine patients (43%) in the active-treatment group had a large, clinically important motor improvement of 10 or more points in the off state, whereas no placebo patients did. These “10-point responders in the GDNF group are a potential focus of interest; however, as this is a post hoc finding we would not wish to overinterpret its meaning,” Dr. Whone and his colleagues wrote. Among patients who received GDNF, PET imaging demonstrated significantly increased 18F-DOPA uptake throughout the putamen, ranging from a 25% increase in the left anterior putamen to a 100% increase in both posterior putamena, whereas patients who received placebo did not have significantly increased uptake.
No drug-related serious adverse events were reported. “The majority of device-related adverse events were port site associated, most commonly local hypertrophic scarring or infections, amenable to antibiotics,” the investigators wrote. “The frequency of these declined during the trial as surgical and device handling experience improved.”
Open-label extension
By week 80, when all participants had received GDNF, both groups showed moderate to large improvement in symptoms, compared with baseline. From baseline to week 80, percentage change in UPDRS motor score in the off state did not significantly differ between patients who received GDNF for 80 weeks and patients who received placebo followed by GDNF (26.7% vs. 27.6%). Secondary endpoints also did not differ between the groups. Treatment compliance was 97.8%; no patients discontinued the study.
The trials were funded by Parkinson’s UK with support from the Cure Parkinson’s Trust and in association with the North Bristol NHS Trust. GDNF and additional resources and funding were provided by MedGenesis Therapeutix, which owns the license for GDNF and received funding from the Michael J. Fox Foundation for Parkinson’s Research. Renishaw manufactured the convection-enhanced delivery device on behalf of North Bristol NHS Trust. The Gatsby Foundation provided a 3T MRI scanner. Some study authors are employed by and have shares or share options with MedGenesis Therapeutix. Other authors are employees of Renishaw. Dr. Gill is Renishaw’s medical director and may have a future royalty share from the drug delivery system that he invented.
SOURCES: Whone AL et al. Brain. 2019 Feb 26. doi: 10.1093/brain/awz023; Whone AL et al. J Parkinsons Dis. 2019 Feb 26. doi: 10.3233/JPD-191576.
researchers reported. The investigational therapy, delivered through a skull-mounted port, was well tolerated in a 40-week, randomized, controlled trial and a 40-week, open-label extension.
Neither study met its primary endpoint, but post hoc analyses suggest possible clinical benefits. In addition, PET imaging after the 40-week, randomized trial found significantly increased 18F-DOPA uptake in patients who received GDNF. The randomized trial was published in the March 2019 issue of Brain; data from the open-label extension were published online ahead of print Feb. 26, 2019, in the Journal of Parkinson’s Disease.
“The spatial and relative magnitude of the improvement in the brain scans is beyond anything seen previously in trials of surgically delivered growth-factor treatments for Parkinson’s [disease],” said principal investigator Alan L. Whone, MBChB, PhD, of the University of Bristol (England) and North Bristol National Health Service Trust. “This represents some of the most compelling evidence yet that we may have a means to possibly reawaken and restore the dopamine brain cells that are gradually destroyed in Parkinson’s [disease].”
Nevertheless, the trial did not confirm clinical benefits. The hypothesis that growth factors can benefit patients with Parkinson’s disease may be incorrect, the researchers acknowledged. It also is possible that the hypothesis is valid and that a trial with a higher GDNF dose, longer treatment duration, patients with an earlier disease stage, or different outcome measures would yield positive results. GDNF warrants further study, they wrote.
The findings could have implications for other neurologic disorders as well.
“This trial has shown that we can safely and repeatedly infuse drugs directly into patients’ brains over months or years. This is a significant breakthrough in our ability to treat neurologic conditions ... because most drugs that might work cannot cross from the bloodstream into the brain,” said Steven Gill, MB, MS. Mr. Gill, of the North Bristol NHS Trust and the U.K.-based engineering firm Renishaw, designed the convection-enhanced delivery system used in the studies.
A neurotrophic protein
GDNF has neurorestorative and neuroprotective effects in animal models of Parkinson’s disease. In open-label studies, continuous, low-rate intraputamenal administration of GDNF has shown signs of potential efficacy, but a placebo-controlled trial did not replicate clinical benefits. In the present studies, the researchers assessed intermittent GDNF administration using convection-enhanced delivery, which can achieve wider and more even distribution of GDNF, compared with the previous approach.
The researchers conducted a single-center, randomized, double-blind, placebo-controlled trial to study this novel administration approach. Patients were aged 35-75 years, had motor symptoms for at least 5 years, and had moderate disease severity in the off state (that is, Hoehn and Yahr stage 2-3 and Unified Parkinson’s Disease Rating Scale motor score–part III [UPDRS-III] of 25-45).
In a pilot stage of the trial, six patients were randomized 2:1 to receive GDNF (120 mcg per putamen) or placebo. In the primary stage, another 35 patients were randomized 1:1 to GDNF or placebo. The primary outcome was the percentage change from baseline to week 40 in the off-state UPDRS-III among patients from the primary stage of the trial. Further analyses included all 41 patients from the pilot and primary stages.
Patients in the primary analysis had a mean age of 56.4 years and mean disease duration of 10.9 years. About half were female.
Results on primary and secondary clinical endpoints did not significantly differ between the groups. Average off state UPDRS motor score decreased by 17.3 in the active treatment group, compared with 11.8 in the placebo group.
A post hoc analysis, however, found that nine patients (43%) in the active-treatment group had a large, clinically important motor improvement of 10 or more points in the off state, whereas no placebo patients did. These “10-point responders in the GDNF group are a potential focus of interest; however, as this is a post hoc finding we would not wish to overinterpret its meaning,” Dr. Whone and his colleagues wrote. Among patients who received GDNF, PET imaging demonstrated significantly increased 18F-DOPA uptake throughout the putamen, ranging from a 25% increase in the left anterior putamen to a 100% increase in both posterior putamena, whereas patients who received placebo did not have significantly increased uptake.
No drug-related serious adverse events were reported. “The majority of device-related adverse events were port site associated, most commonly local hypertrophic scarring or infections, amenable to antibiotics,” the investigators wrote. “The frequency of these declined during the trial as surgical and device handling experience improved.”
Open-label extension
By week 80, when all participants had received GDNF, both groups showed moderate to large improvement in symptoms, compared with baseline. From baseline to week 80, percentage change in UPDRS motor score in the off state did not significantly differ between patients who received GDNF for 80 weeks and patients who received placebo followed by GDNF (26.7% vs. 27.6%). Secondary endpoints also did not differ between the groups. Treatment compliance was 97.8%; no patients discontinued the study.
The trials were funded by Parkinson’s UK with support from the Cure Parkinson’s Trust and in association with the North Bristol NHS Trust. GDNF and additional resources and funding were provided by MedGenesis Therapeutix, which owns the license for GDNF and received funding from the Michael J. Fox Foundation for Parkinson’s Research. Renishaw manufactured the convection-enhanced delivery device on behalf of North Bristol NHS Trust. The Gatsby Foundation provided a 3T MRI scanner. Some study authors are employed by and have shares or share options with MedGenesis Therapeutix. Other authors are employees of Renishaw. Dr. Gill is Renishaw’s medical director and may have a future royalty share from the drug delivery system that he invented.
SOURCES: Whone AL et al. Brain. 2019 Feb 26. doi: 10.1093/brain/awz023; Whone AL et al. J Parkinsons Dis. 2019 Feb 26. doi: 10.3233/JPD-191576.
Does adherence to a Mediterranean diet reduce the risk of Parkinson’s disease?
Among older adults, adherence to a Mediterranean diet is associated with lower probability of prodromal Parkinson’s disease, according to research published in Movement Disorders.
“Recommending the Mediterranean diet pattern, either to reduce the risk or lessen the effects ... of prodromal Parkinson’s disease, needs to be considered and further explored,” said lead author Maria I. Maraki, PhD, of the department of nutrition and dietetics at Harokopio University in Athens, Greece, and her research colleagues.
Evidence regarding the effect of a Mediterranean diet on Parkinson’s disease risk remains limited, however, and physicians should be cautious in interpreting the data, researchers noted in accompanying editorials.
“There is a puzzling constellation of information and data that cannot be reconciled with a simple model accounting for the role of diet, vascular risk factors, and the neurodegenerative process and mechanisms underlying Parkinson’s disease,” Connie Marras, MD, PhD, and Jose A. Obeso, MD, PhD, said in an editorial. Given Maraki et al.’s findings, “most of us would be glad to accept that such a causal inverse association exists and can therefore be strongly recommended to our patients,” but “further work is needed before definitive conclusions can be reached,” Dr. Marras and Dr. Obeso wrote. Dr. Marras is affiliated with the University Health Network and the University of Toronto. Dr. Obeso is affiliated with University Hospital HM Puerta del Sur, CEU San Pablo University, Móstoles, Spain.
The role of diet
Prior research has suggested that adherence to the Mediterranean diet – characterized by consumption of nonrefined cereals, fruits, vegetables, legumes, potatoes, fish, and olive oil – may be associated with reduced risk of Parkinson’s disease. In addition, studies have found that adherence to the Mediterranean diet may be protective in other diseases, including dementia and cardiovascular disease. Dr. Maraki and her colleagues sought to assess whether adherence to the Mediterranean diet is associated with the likelihood of prodromal Parkinson’s disease or its manifestations. To calculate the probability of prodromal Parkinson’s disease, the investigators used a tool created by the International Parkinson and Movement Disorder Society (MDS) that takes into account baseline risk factors as well as prodromal markers such as constipation and motor slowing.
They analyzed data from 1,731 participants in the population-based Hellenic Longitudinal Investigation of Aging and Diet (HELIAD) cohort in Greece. Participants, 41% of whom were male, were aged 65 years or older and did not have Parkinson’s disease. They completed a detailed food frequency questionnaire, and the researchers calculated how closely each participant’s diet adhered to the Mediterranean diet. Diet adherence scores ranged from 0 to 55, with higher scores indicating greater adherence.
The median probability of prodromal Parkinson’s disease was 1.9% (range, 0.2%-96.7%), and the probability was lower among those with greater adherence to the Mediterranean diet. This difference was “driven mostly by nonmotor markers of prodromal Parkinson’s disease,” including depression, constipation, urinary dysfunction, and daytime somnolence, the researchers said. “Each unit increase in Mediterranean diet score was associated with a 2% decreased probability for prodromal Parkinson’s disease.” Compared with participants in the lowest quartile of Mediterranean diet adherence, those in the highest quartile had an approximately 21% lower probability for prodromal Parkinson’s disease.
Potential confounding
“This study pushes the prodromal criteria into performing a job they were never designed to do,” which presents potential pitfalls, Ronald B. Postuma, MD, of the department of neurology at Montreal General Hospital in Quebec, said in an accompanying editorial.
While the MDS criteria were designed to assess the likelihood that any person over age 50 years is in a state of prodromal Parkinson’s disease, the present study aimed to evaluate whether a single putative risk factor for Parkinson’s disease is associated with the likelihood of its prodromal state.
In addition, the analysis did not include some of the prodromal markers that are part of the MDS criteria, including olfaction, polysomnographic-proven REM sleep behavior disorder, and dopaminergic functional neuroimaging.
“As pointed out by the researchers, many of the risk factors in the prodromal criteria are potentially confounded by factors other than Parkinson’s disease; for example, one could imagine that older people, men, or farmers (with their higher pesticide exposure) are less likely to follow the Mediterranean diet simply because of different cultural lifestyle patterns,” Dr. Postuma said.
It is also possible that the Mediterranean diet affects prodromal markers such as constipation, sleep, or depression without affecting underlying neurodegenerative disease. In any case, the effect sizes observed in the study were small, and there was no evidence that participants who adhered most closely to a Mediterranean diet had less parkinsonism, Dr. Postuma said.
These limitations do not preclude physicians from recommending the diet for other reasons. “Numerous studies, reviews, meta-analyses, and randomized controlled trials consistently rank the Mediterranean diet as among the healthiest diets available,” Dr. Postuma said. “So, one can clearly recommend diets such as these, even if not necessarily for Parkinson’s disease prevention.”
Adding insights
The researchers used a Mediterranean diet score that was developed in a population of adults from metropolitan Athens, “an area not unlike the one in which the score is being applied in the HELIAD study,” Christy C. Tangney, PhD, professor of clinical nutrition and preventive medicine and associate dean for research at Rush University Medical Center, Chicago, said in a separate editorial. As expected, the average Mediterranean diet adherence score in this study was higher than that in the Chicago Health and Aging Project (33.2 vs. 28.2).
“If we can identify differences in diet or lifestyle patterns and risk of this latent phase of Parkinson’s disease neurodegeneration, we may be one step closer to identifying preventive measures,” she said. Follow-up reports from HELIAD and other cohorts may allow researchers to assess how changes in dietary patterns relate to changes in Parkinson’s disease markers, the probability of prodromal Parkinson’s disease, and incident Parkinson’s disease, Dr. Tangney said.
The study authors had no conflicts of interest or financial disclosures. The study was supported by a grant from the Alzheimer’s Association, an ESPA‐EU grant cofunded by the European Social Fund and Greek National resources, and a grant from the Ministry for Health and Social Solidarity (Greece). Dr. Maraki and a coauthor have received financial support from the Greek State Scholarships Foundation. Dr. Tangney and Dr. Postuma had no conflicts of interest.
SOURCE: Maraki MI et al. Mov Disord. 2018 Oct 10. doi: 10.1002/mds.27489.
Among older adults, adherence to a Mediterranean diet is associated with lower probability of prodromal Parkinson’s disease, according to research published in Movement Disorders.
“Recommending the Mediterranean diet pattern, either to reduce the risk or lessen the effects ... of prodromal Parkinson’s disease, needs to be considered and further explored,” said lead author Maria I. Maraki, PhD, of the department of nutrition and dietetics at Harokopio University in Athens, Greece, and her research colleagues.
Evidence regarding the effect of a Mediterranean diet on Parkinson’s disease risk remains limited, however, and physicians should be cautious in interpreting the data, researchers noted in accompanying editorials.
“There is a puzzling constellation of information and data that cannot be reconciled with a simple model accounting for the role of diet, vascular risk factors, and the neurodegenerative process and mechanisms underlying Parkinson’s disease,” Connie Marras, MD, PhD, and Jose A. Obeso, MD, PhD, said in an editorial. Given Maraki et al.’s findings, “most of us would be glad to accept that such a causal inverse association exists and can therefore be strongly recommended to our patients,” but “further work is needed before definitive conclusions can be reached,” Dr. Marras and Dr. Obeso wrote. Dr. Marras is affiliated with the University Health Network and the University of Toronto. Dr. Obeso is affiliated with University Hospital HM Puerta del Sur, CEU San Pablo University, Móstoles, Spain.
The role of diet
Prior research has suggested that adherence to the Mediterranean diet – characterized by consumption of nonrefined cereals, fruits, vegetables, legumes, potatoes, fish, and olive oil – may be associated with reduced risk of Parkinson’s disease. In addition, studies have found that adherence to the Mediterranean diet may be protective in other diseases, including dementia and cardiovascular disease. Dr. Maraki and her colleagues sought to assess whether adherence to the Mediterranean diet is associated with the likelihood of prodromal Parkinson’s disease or its manifestations. To calculate the probability of prodromal Parkinson’s disease, the investigators used a tool created by the International Parkinson and Movement Disorder Society (MDS) that takes into account baseline risk factors as well as prodromal markers such as constipation and motor slowing.
They analyzed data from 1,731 participants in the population-based Hellenic Longitudinal Investigation of Aging and Diet (HELIAD) cohort in Greece. Participants, 41% of whom were male, were aged 65 years or older and did not have Parkinson’s disease. They completed a detailed food frequency questionnaire, and the researchers calculated how closely each participant’s diet adhered to the Mediterranean diet. Diet adherence scores ranged from 0 to 55, with higher scores indicating greater adherence.
The median probability of prodromal Parkinson’s disease was 1.9% (range, 0.2%-96.7%), and the probability was lower among those with greater adherence to the Mediterranean diet. This difference was “driven mostly by nonmotor markers of prodromal Parkinson’s disease,” including depression, constipation, urinary dysfunction, and daytime somnolence, the researchers said. “Each unit increase in Mediterranean diet score was associated with a 2% decreased probability for prodromal Parkinson’s disease.” Compared with participants in the lowest quartile of Mediterranean diet adherence, those in the highest quartile had an approximately 21% lower probability for prodromal Parkinson’s disease.
Potential confounding
“This study pushes the prodromal criteria into performing a job they were never designed to do,” which presents potential pitfalls, Ronald B. Postuma, MD, of the department of neurology at Montreal General Hospital in Quebec, said in an accompanying editorial.
While the MDS criteria were designed to assess the likelihood that any person over age 50 years is in a state of prodromal Parkinson’s disease, the present study aimed to evaluate whether a single putative risk factor for Parkinson’s disease is associated with the likelihood of its prodromal state.
In addition, the analysis did not include some of the prodromal markers that are part of the MDS criteria, including olfaction, polysomnographic-proven REM sleep behavior disorder, and dopaminergic functional neuroimaging.
“As pointed out by the researchers, many of the risk factors in the prodromal criteria are potentially confounded by factors other than Parkinson’s disease; for example, one could imagine that older people, men, or farmers (with their higher pesticide exposure) are less likely to follow the Mediterranean diet simply because of different cultural lifestyle patterns,” Dr. Postuma said.
It is also possible that the Mediterranean diet affects prodromal markers such as constipation, sleep, or depression without affecting underlying neurodegenerative disease. In any case, the effect sizes observed in the study were small, and there was no evidence that participants who adhered most closely to a Mediterranean diet had less parkinsonism, Dr. Postuma said.
These limitations do not preclude physicians from recommending the diet for other reasons. “Numerous studies, reviews, meta-analyses, and randomized controlled trials consistently rank the Mediterranean diet as among the healthiest diets available,” Dr. Postuma said. “So, one can clearly recommend diets such as these, even if not necessarily for Parkinson’s disease prevention.”
Adding insights
The researchers used a Mediterranean diet score that was developed in a population of adults from metropolitan Athens, “an area not unlike the one in which the score is being applied in the HELIAD study,” Christy C. Tangney, PhD, professor of clinical nutrition and preventive medicine and associate dean for research at Rush University Medical Center, Chicago, said in a separate editorial. As expected, the average Mediterranean diet adherence score in this study was higher than that in the Chicago Health and Aging Project (33.2 vs. 28.2).
“If we can identify differences in diet or lifestyle patterns and risk of this latent phase of Parkinson’s disease neurodegeneration, we may be one step closer to identifying preventive measures,” she said. Follow-up reports from HELIAD and other cohorts may allow researchers to assess how changes in dietary patterns relate to changes in Parkinson’s disease markers, the probability of prodromal Parkinson’s disease, and incident Parkinson’s disease, Dr. Tangney said.
The study authors had no conflicts of interest or financial disclosures. The study was supported by a grant from the Alzheimer’s Association, an ESPA‐EU grant cofunded by the European Social Fund and Greek National resources, and a grant from the Ministry for Health and Social Solidarity (Greece). Dr. Maraki and a coauthor have received financial support from the Greek State Scholarships Foundation. Dr. Tangney and Dr. Postuma had no conflicts of interest.
SOURCE: Maraki MI et al. Mov Disord. 2018 Oct 10. doi: 10.1002/mds.27489.
Among older adults, adherence to a Mediterranean diet is associated with lower probability of prodromal Parkinson’s disease, according to research published in Movement Disorders.
“Recommending the Mediterranean diet pattern, either to reduce the risk or lessen the effects ... of prodromal Parkinson’s disease, needs to be considered and further explored,” said lead author Maria I. Maraki, PhD, of the department of nutrition and dietetics at Harokopio University in Athens, Greece, and her research colleagues.
Evidence regarding the effect of a Mediterranean diet on Parkinson’s disease risk remains limited, however, and physicians should be cautious in interpreting the data, researchers noted in accompanying editorials.
“There is a puzzling constellation of information and data that cannot be reconciled with a simple model accounting for the role of diet, vascular risk factors, and the neurodegenerative process and mechanisms underlying Parkinson’s disease,” Connie Marras, MD, PhD, and Jose A. Obeso, MD, PhD, said in an editorial. Given Maraki et al.’s findings, “most of us would be glad to accept that such a causal inverse association exists and can therefore be strongly recommended to our patients,” but “further work is needed before definitive conclusions can be reached,” Dr. Marras and Dr. Obeso wrote. Dr. Marras is affiliated with the University Health Network and the University of Toronto. Dr. Obeso is affiliated with University Hospital HM Puerta del Sur, CEU San Pablo University, Móstoles, Spain.
The role of diet
Prior research has suggested that adherence to the Mediterranean diet – characterized by consumption of nonrefined cereals, fruits, vegetables, legumes, potatoes, fish, and olive oil – may be associated with reduced risk of Parkinson’s disease. In addition, studies have found that adherence to the Mediterranean diet may be protective in other diseases, including dementia and cardiovascular disease. Dr. Maraki and her colleagues sought to assess whether adherence to the Mediterranean diet is associated with the likelihood of prodromal Parkinson’s disease or its manifestations. To calculate the probability of prodromal Parkinson’s disease, the investigators used a tool created by the International Parkinson and Movement Disorder Society (MDS) that takes into account baseline risk factors as well as prodromal markers such as constipation and motor slowing.
They analyzed data from 1,731 participants in the population-based Hellenic Longitudinal Investigation of Aging and Diet (HELIAD) cohort in Greece. Participants, 41% of whom were male, were aged 65 years or older and did not have Parkinson’s disease. They completed a detailed food frequency questionnaire, and the researchers calculated how closely each participant’s diet adhered to the Mediterranean diet. Diet adherence scores ranged from 0 to 55, with higher scores indicating greater adherence.
The median probability of prodromal Parkinson’s disease was 1.9% (range, 0.2%-96.7%), and the probability was lower among those with greater adherence to the Mediterranean diet. This difference was “driven mostly by nonmotor markers of prodromal Parkinson’s disease,” including depression, constipation, urinary dysfunction, and daytime somnolence, the researchers said. “Each unit increase in Mediterranean diet score was associated with a 2% decreased probability for prodromal Parkinson’s disease.” Compared with participants in the lowest quartile of Mediterranean diet adherence, those in the highest quartile had an approximately 21% lower probability for prodromal Parkinson’s disease.
Potential confounding
“This study pushes the prodromal criteria into performing a job they were never designed to do,” which presents potential pitfalls, Ronald B. Postuma, MD, of the department of neurology at Montreal General Hospital in Quebec, said in an accompanying editorial.
While the MDS criteria were designed to assess the likelihood that any person over age 50 years is in a state of prodromal Parkinson’s disease, the present study aimed to evaluate whether a single putative risk factor for Parkinson’s disease is associated with the likelihood of its prodromal state.
In addition, the analysis did not include some of the prodromal markers that are part of the MDS criteria, including olfaction, polysomnographic-proven REM sleep behavior disorder, and dopaminergic functional neuroimaging.
“As pointed out by the researchers, many of the risk factors in the prodromal criteria are potentially confounded by factors other than Parkinson’s disease; for example, one could imagine that older people, men, or farmers (with their higher pesticide exposure) are less likely to follow the Mediterranean diet simply because of different cultural lifestyle patterns,” Dr. Postuma said.
It is also possible that the Mediterranean diet affects prodromal markers such as constipation, sleep, or depression without affecting underlying neurodegenerative disease. In any case, the effect sizes observed in the study were small, and there was no evidence that participants who adhered most closely to a Mediterranean diet had less parkinsonism, Dr. Postuma said.
These limitations do not preclude physicians from recommending the diet for other reasons. “Numerous studies, reviews, meta-analyses, and randomized controlled trials consistently rank the Mediterranean diet as among the healthiest diets available,” Dr. Postuma said. “So, one can clearly recommend diets such as these, even if not necessarily for Parkinson’s disease prevention.”
Adding insights
The researchers used a Mediterranean diet score that was developed in a population of adults from metropolitan Athens, “an area not unlike the one in which the score is being applied in the HELIAD study,” Christy C. Tangney, PhD, professor of clinical nutrition and preventive medicine and associate dean for research at Rush University Medical Center, Chicago, said in a separate editorial. As expected, the average Mediterranean diet adherence score in this study was higher than that in the Chicago Health and Aging Project (33.2 vs. 28.2).
“If we can identify differences in diet or lifestyle patterns and risk of this latent phase of Parkinson’s disease neurodegeneration, we may be one step closer to identifying preventive measures,” she said. Follow-up reports from HELIAD and other cohorts may allow researchers to assess how changes in dietary patterns relate to changes in Parkinson’s disease markers, the probability of prodromal Parkinson’s disease, and incident Parkinson’s disease, Dr. Tangney said.
The study authors had no conflicts of interest or financial disclosures. The study was supported by a grant from the Alzheimer’s Association, an ESPA‐EU grant cofunded by the European Social Fund and Greek National resources, and a grant from the Ministry for Health and Social Solidarity (Greece). Dr. Maraki and a coauthor have received financial support from the Greek State Scholarships Foundation. Dr. Tangney and Dr. Postuma had no conflicts of interest.
SOURCE: Maraki MI et al. Mov Disord. 2018 Oct 10. doi: 10.1002/mds.27489.
FROM MOVEMENT DISORDERS
Key clinical point: Adherence to a Mediterranean diet is associated with lower probability of prodromal Parkinson’s disease.
Major finding: Each 1-unit increase in Mediterranean diet score was associated with a 2% decreased probability for prodromal Parkinson’s disease.
Study details: A study of 1,731 older adults in the population-based Hellenic Longitudinal Investigation of Aging and Diet (HELIAD) cohort in Greece.
Disclosures: The study authors had no conflicts of interest or financial disclosures. The study was supported by a grant from the Alzheimer’s Association, an ESPA‐EU grant cofunded by the European Social Fund and Greek National resources, and a grant from the Ministry for Health and Social Solidarity (Greece). Dr. Maraki and a coauthor have received financial support from the Greek State Scholarships Foundation.
Source: Maraki MI et al. Mov Disord. 2018 Oct 10. doi:10.1002/mds.27489.
DBS may improve nonmotor symptoms in Parkinson’s disease
LAS VEGAS – , according to a small study presented at the annual meeting of the North American Neuromodulation Society. DBS of the subthalamic nucleus (STN), however, does not significantly improve these symptoms.
“Further work will be needed to confirm whether DBS needs to be bilateral ... and whether demographic differences are significant,” said Michael Gillogly, RN, clinical research nurse in the department of neurosurgery at Albany (New York) Medical Center. “The pilot data suggest that, if all else is equal, and the patient has significant urinary dysfunction as a major complaint, GPI DBS may be preferentially considered.”
The benefits of DBS on motor symptoms in Parkinson’s disease are well documented in the literature, but the technique’s effects on nonmotor symptoms are less clear. Nonmotor symptoms – such as cognitive deficits, gastrointestinal dysfunction, genitourinary dysfunction, and sleep disturbance – are common in all stages of Parkinson’s disease and significantly impair quality of life. Data indicate that speech and neuropsychological symptoms worsen with DBS of the STN, but research into the effect of DBS of the GPI on nonmotor symptoms is limited.
Mr. Gillogly and his colleagues considered all surgical candidates at their facility for enrollment into a study evaluating nonmotor outcomes in Parkinson’s disease at baseline, before implantation, and at 6 months after DBS. Study outcomes were patient perception of urinary, swallowing, and gastrointestinal function at 6 months after DBS of the GPI, compared with DBS of the STN.
The researchers chose two tools each to measure sialorrhea, dysphagia, and genitourinary dysfunction. These tools included the Drooling Severity and Frequency Scale (DSFS), the Swallowing Disturbance Questionnaire, and the International Prostate Symptom Score (IPSS). The investigators also collected demographic information, including sex, age at the time of surgery, duration of illness, neuropsychological profile, and medication inventory.
In all, 34 patients (12 women) were enrolled in the study and completed each outcome measure preoperatively and at 6 months postoperatively. The mean age of our subjects at the time of surgery was 64 years. Eight received DBS of the GPI, and 26 received DBS of the STN. Mr. Gillogly and his colleagues observed a significant 31% improvement in DSFS score and a significant 24% improvement on the IPSS among GPI-targeted patients. They found no significant improvements among patients who had STN targeting. When the investigators compared patients with unilateral lead placement and those with bilateral lead placement, they observed that all of the significant improvement among patients with GPI targeting occurred when treatment was bilateral.
The small sample size is a notable limitation of the study, and subset analyses were limited, said Mr. Gillogly. In addition, it was difficult to determine whether the symptoms studied were directly related to Parkinson’s disease, because they often arise as part of the natural aging process. “Other limitations of the study include lack of objective measurements, as these are all patient perception, and the innate limitations of self-reported questionnaires,” said Mr. Gillogly.
Two of the researchers reported having consulted for Medtronic, which markets a DBS system. One author received grant funding and consulting fees from Boston Scientific, Medtronic, and Abbott, all of which make DBS devices.
LAS VEGAS – , according to a small study presented at the annual meeting of the North American Neuromodulation Society. DBS of the subthalamic nucleus (STN), however, does not significantly improve these symptoms.
“Further work will be needed to confirm whether DBS needs to be bilateral ... and whether demographic differences are significant,” said Michael Gillogly, RN, clinical research nurse in the department of neurosurgery at Albany (New York) Medical Center. “The pilot data suggest that, if all else is equal, and the patient has significant urinary dysfunction as a major complaint, GPI DBS may be preferentially considered.”
The benefits of DBS on motor symptoms in Parkinson’s disease are well documented in the literature, but the technique’s effects on nonmotor symptoms are less clear. Nonmotor symptoms – such as cognitive deficits, gastrointestinal dysfunction, genitourinary dysfunction, and sleep disturbance – are common in all stages of Parkinson’s disease and significantly impair quality of life. Data indicate that speech and neuropsychological symptoms worsen with DBS of the STN, but research into the effect of DBS of the GPI on nonmotor symptoms is limited.
Mr. Gillogly and his colleagues considered all surgical candidates at their facility for enrollment into a study evaluating nonmotor outcomes in Parkinson’s disease at baseline, before implantation, and at 6 months after DBS. Study outcomes were patient perception of urinary, swallowing, and gastrointestinal function at 6 months after DBS of the GPI, compared with DBS of the STN.
The researchers chose two tools each to measure sialorrhea, dysphagia, and genitourinary dysfunction. These tools included the Drooling Severity and Frequency Scale (DSFS), the Swallowing Disturbance Questionnaire, and the International Prostate Symptom Score (IPSS). The investigators also collected demographic information, including sex, age at the time of surgery, duration of illness, neuropsychological profile, and medication inventory.
In all, 34 patients (12 women) were enrolled in the study and completed each outcome measure preoperatively and at 6 months postoperatively. The mean age of our subjects at the time of surgery was 64 years. Eight received DBS of the GPI, and 26 received DBS of the STN. Mr. Gillogly and his colleagues observed a significant 31% improvement in DSFS score and a significant 24% improvement on the IPSS among GPI-targeted patients. They found no significant improvements among patients who had STN targeting. When the investigators compared patients with unilateral lead placement and those with bilateral lead placement, they observed that all of the significant improvement among patients with GPI targeting occurred when treatment was bilateral.
The small sample size is a notable limitation of the study, and subset analyses were limited, said Mr. Gillogly. In addition, it was difficult to determine whether the symptoms studied were directly related to Parkinson’s disease, because they often arise as part of the natural aging process. “Other limitations of the study include lack of objective measurements, as these are all patient perception, and the innate limitations of self-reported questionnaires,” said Mr. Gillogly.
Two of the researchers reported having consulted for Medtronic, which markets a DBS system. One author received grant funding and consulting fees from Boston Scientific, Medtronic, and Abbott, all of which make DBS devices.
LAS VEGAS – , according to a small study presented at the annual meeting of the North American Neuromodulation Society. DBS of the subthalamic nucleus (STN), however, does not significantly improve these symptoms.
“Further work will be needed to confirm whether DBS needs to be bilateral ... and whether demographic differences are significant,” said Michael Gillogly, RN, clinical research nurse in the department of neurosurgery at Albany (New York) Medical Center. “The pilot data suggest that, if all else is equal, and the patient has significant urinary dysfunction as a major complaint, GPI DBS may be preferentially considered.”
The benefits of DBS on motor symptoms in Parkinson’s disease are well documented in the literature, but the technique’s effects on nonmotor symptoms are less clear. Nonmotor symptoms – such as cognitive deficits, gastrointestinal dysfunction, genitourinary dysfunction, and sleep disturbance – are common in all stages of Parkinson’s disease and significantly impair quality of life. Data indicate that speech and neuropsychological symptoms worsen with DBS of the STN, but research into the effect of DBS of the GPI on nonmotor symptoms is limited.
Mr. Gillogly and his colleagues considered all surgical candidates at their facility for enrollment into a study evaluating nonmotor outcomes in Parkinson’s disease at baseline, before implantation, and at 6 months after DBS. Study outcomes were patient perception of urinary, swallowing, and gastrointestinal function at 6 months after DBS of the GPI, compared with DBS of the STN.
The researchers chose two tools each to measure sialorrhea, dysphagia, and genitourinary dysfunction. These tools included the Drooling Severity and Frequency Scale (DSFS), the Swallowing Disturbance Questionnaire, and the International Prostate Symptom Score (IPSS). The investigators also collected demographic information, including sex, age at the time of surgery, duration of illness, neuropsychological profile, and medication inventory.
In all, 34 patients (12 women) were enrolled in the study and completed each outcome measure preoperatively and at 6 months postoperatively. The mean age of our subjects at the time of surgery was 64 years. Eight received DBS of the GPI, and 26 received DBS of the STN. Mr. Gillogly and his colleagues observed a significant 31% improvement in DSFS score and a significant 24% improvement on the IPSS among GPI-targeted patients. They found no significant improvements among patients who had STN targeting. When the investigators compared patients with unilateral lead placement and those with bilateral lead placement, they observed that all of the significant improvement among patients with GPI targeting occurred when treatment was bilateral.
The small sample size is a notable limitation of the study, and subset analyses were limited, said Mr. Gillogly. In addition, it was difficult to determine whether the symptoms studied were directly related to Parkinson’s disease, because they often arise as part of the natural aging process. “Other limitations of the study include lack of objective measurements, as these are all patient perception, and the innate limitations of self-reported questionnaires,” said Mr. Gillogly.
Two of the researchers reported having consulted for Medtronic, which markets a DBS system. One author received grant funding and consulting fees from Boston Scientific, Medtronic, and Abbott, all of which make DBS devices.
REPORTING FROM NANS 2019
Key clinical point: Bilateral stimulation of the globus pallidus internus reduces sialorrhea and improves genitourinary symptoms.
Major finding: Patients reported 31% improvement in sialorrhea and 24% improvement in urinary function.
Study details: A prospective study of 34 patients receiving DBS of the STN or GPI.
Disclosures: No funding was reported.
DBS provides long-term benefits for patients with Parkinson’s disease
LAS VEGAS – , according to a large-scale collection of outcome data. The treatment improves motor function and quality of life and has an acceptable safety profile. The analysis was presented at the annual meeting of the North American Neuromodulation Society.
Research by Okun et al. in 2012 and Schuepbach et al. in 2013 demonstrated that DBS effectively reduces the motor complications of Parkinson’s disease. To monitor the treatment’s efficacy and safety on a large scale, investigators established a prospective registry of patients with levodopa-responsive Parkinson’s disease who underwent DBS implantation. An aim of the registry is to improve understanding of the clinical use and outcomes of DBS in this population. As many as 1,000 patients have been implanted with Vercise DBS systems at 70 international sites. These systems enable multiple independent current source control.
Participants presented for clinical visits at 3 months, 6 months, 1 year, 2 years, and 3 years after surgery. Jan Vesper, MD, PhD, professor of neurosurgery at Heinrich Heine University in Düsseldorf, Germany, and his colleagues analyzed patient outcomes, including the Parkinson’s Disease Questionnaire (PDQ-39), Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), Clinical Global Impression of Change (as assessed by the patient, caregiver, and clinician), and the Schwab and England (SE) scale. The researchers also reported adverse events.
As of November 2018, 403 participants had been enrolled in the registry, and 359 had undergone DBS implantation. At baseline, mean age was 59.6 years, and approximately 70% of participants were male. Mean disease duration was 10.4 years. Without medication, mean MDS-UPDRS III score was 44.8, and mean PDQ-39 Summary Index score was 28.8.
At 1 year, participants’ mean off-medication MDS-UPDRS III score was 29.7. This result represented a significant 34% improvement in motor performance.
PDQ-39 Summary Index score was improved by 6.7 points at 6 months, 4.7 points at 1 year, and 3.0 points at 2 years, which represented a sustained benefit for participants’ quality of life. Improvements in activities of daily living were sustained throughout the 2-year period. Cognition was improved at 6 months, but not at subsequent visits. Mobility, stigma, and bodily discomfort were improved at 6 months and 1 year, but not at 2 years. Furthermore, more than 80% of patients, caregivers, and clinicians observed improvements in Parkinson’s disease symptoms at all time points.
The investigators did not find any unanticipated adverse events. In all, 217 serious adverse events occurred in 121 participants. Of these events, 60 were related to stimulation. No lead fractures or breakages occurred.
“This registry represents the first large-scale collection of outcomes using a DBS system capable of multiple independent current source control,” said Dr. Vesper and colleagues.
The investigators did not report any conflicts of interest.
LAS VEGAS – , according to a large-scale collection of outcome data. The treatment improves motor function and quality of life and has an acceptable safety profile. The analysis was presented at the annual meeting of the North American Neuromodulation Society.
Research by Okun et al. in 2012 and Schuepbach et al. in 2013 demonstrated that DBS effectively reduces the motor complications of Parkinson’s disease. To monitor the treatment’s efficacy and safety on a large scale, investigators established a prospective registry of patients with levodopa-responsive Parkinson’s disease who underwent DBS implantation. An aim of the registry is to improve understanding of the clinical use and outcomes of DBS in this population. As many as 1,000 patients have been implanted with Vercise DBS systems at 70 international sites. These systems enable multiple independent current source control.
Participants presented for clinical visits at 3 months, 6 months, 1 year, 2 years, and 3 years after surgery. Jan Vesper, MD, PhD, professor of neurosurgery at Heinrich Heine University in Düsseldorf, Germany, and his colleagues analyzed patient outcomes, including the Parkinson’s Disease Questionnaire (PDQ-39), Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), Clinical Global Impression of Change (as assessed by the patient, caregiver, and clinician), and the Schwab and England (SE) scale. The researchers also reported adverse events.
As of November 2018, 403 participants had been enrolled in the registry, and 359 had undergone DBS implantation. At baseline, mean age was 59.6 years, and approximately 70% of participants were male. Mean disease duration was 10.4 years. Without medication, mean MDS-UPDRS III score was 44.8, and mean PDQ-39 Summary Index score was 28.8.
At 1 year, participants’ mean off-medication MDS-UPDRS III score was 29.7. This result represented a significant 34% improvement in motor performance.
PDQ-39 Summary Index score was improved by 6.7 points at 6 months, 4.7 points at 1 year, and 3.0 points at 2 years, which represented a sustained benefit for participants’ quality of life. Improvements in activities of daily living were sustained throughout the 2-year period. Cognition was improved at 6 months, but not at subsequent visits. Mobility, stigma, and bodily discomfort were improved at 6 months and 1 year, but not at 2 years. Furthermore, more than 80% of patients, caregivers, and clinicians observed improvements in Parkinson’s disease symptoms at all time points.
The investigators did not find any unanticipated adverse events. In all, 217 serious adverse events occurred in 121 participants. Of these events, 60 were related to stimulation. No lead fractures or breakages occurred.
“This registry represents the first large-scale collection of outcomes using a DBS system capable of multiple independent current source control,” said Dr. Vesper and colleagues.
The investigators did not report any conflicts of interest.
LAS VEGAS – , according to a large-scale collection of outcome data. The treatment improves motor function and quality of life and has an acceptable safety profile. The analysis was presented at the annual meeting of the North American Neuromodulation Society.
Research by Okun et al. in 2012 and Schuepbach et al. in 2013 demonstrated that DBS effectively reduces the motor complications of Parkinson’s disease. To monitor the treatment’s efficacy and safety on a large scale, investigators established a prospective registry of patients with levodopa-responsive Parkinson’s disease who underwent DBS implantation. An aim of the registry is to improve understanding of the clinical use and outcomes of DBS in this population. As many as 1,000 patients have been implanted with Vercise DBS systems at 70 international sites. These systems enable multiple independent current source control.
Participants presented for clinical visits at 3 months, 6 months, 1 year, 2 years, and 3 years after surgery. Jan Vesper, MD, PhD, professor of neurosurgery at Heinrich Heine University in Düsseldorf, Germany, and his colleagues analyzed patient outcomes, including the Parkinson’s Disease Questionnaire (PDQ-39), Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), Clinical Global Impression of Change (as assessed by the patient, caregiver, and clinician), and the Schwab and England (SE) scale. The researchers also reported adverse events.
As of November 2018, 403 participants had been enrolled in the registry, and 359 had undergone DBS implantation. At baseline, mean age was 59.6 years, and approximately 70% of participants were male. Mean disease duration was 10.4 years. Without medication, mean MDS-UPDRS III score was 44.8, and mean PDQ-39 Summary Index score was 28.8.
At 1 year, participants’ mean off-medication MDS-UPDRS III score was 29.7. This result represented a significant 34% improvement in motor performance.
PDQ-39 Summary Index score was improved by 6.7 points at 6 months, 4.7 points at 1 year, and 3.0 points at 2 years, which represented a sustained benefit for participants’ quality of life. Improvements in activities of daily living were sustained throughout the 2-year period. Cognition was improved at 6 months, but not at subsequent visits. Mobility, stigma, and bodily discomfort were improved at 6 months and 1 year, but not at 2 years. Furthermore, more than 80% of patients, caregivers, and clinicians observed improvements in Parkinson’s disease symptoms at all time points.
The investigators did not find any unanticipated adverse events. In all, 217 serious adverse events occurred in 121 participants. Of these events, 60 were related to stimulation. No lead fractures or breakages occurred.
“This registry represents the first large-scale collection of outcomes using a DBS system capable of multiple independent current source control,” said Dr. Vesper and colleagues.
The investigators did not report any conflicts of interest.
REPORTING FROM NANS 2019
Key clinical point: DBS provides sustained improvements in motor and nonmotor symptoms over 2 years.
Major finding: At 1 year, DBS had significantly improved motor scores by 34%.
Study details: An analysis of prospective registry data for 359 patients with Parkinson’s disease who underwent DBS implantation.
Disclosures: The authors reported no study funding or conflicts of interest.
No evidence for disease-modifying effect of levodopa in Parkinson’s disease
investigators reported. The disease course was not significantly different for patients who had a full 80 weeks of levodopa/carbodopa therapy, compared with that seen with those who started treatment after a 40-week delay, according to the investigators.
“These findings imply that levodopa had no disease-modifying effect on Parkinson’s disease over the period of the trial,” wrote investigator Rob M. A. de Bie, MD, PhD, professor of movement disorders at the University of Amsterdam, and his colleagues in the New England Journal of Medicine.
By contrast, results of an earlier randomized, placebo-controlled trial suggested that levodopa had disease-modifying effects, though the findings of that study were inconclusive, according to authors of an editorial (see Views on the News).
In the current multicenter trial, known as LEAP (Levodopa in Early Parkinson’s Disease) a total of 445 patients with early Parkinson’s disease were randomized to either 80 weeks of levodopa and carbodopa or to 40 weeks of placebo followed by 40 weeks of levodopa/carbodopa.
Levodopa was dosed at 100 mg three times per day, and carbodopa at 25 mg three times per day, according to the report.
There was no significant difference between the early and delayed treatment groups for primary outcome of the trial, which was change in the Unified Parkinson’s Disease Rating Scale (UPDRS) from baseline to week 80.
The mean change in UPDRS was –1.0 in the group of patients who had the full 80 weeks of levodopa/carbodopa and –2.0 for those who had delayed therapy, for a difference of 1 point (P = .44). Higher scores on the UPDRS signify worse disease.
At week 40, there was a change in UPDRS favoring the early-initiation strategy, which reflected the effects of levodopa on disease symptoms, investigators added.
Nausea was more common in the early-start group during the first 40 weeks of the trial. However, there were no differences between groups in other adverse events of particular interest, including dyskinesias and motor fluctuations related to levodopa, Dr. de Bie and his colleagues reported.
Taken together, these results suggest no beneficial or detrimental disease-modifying effect for an early treatment strategy, although further trials are warranted to evaluate other strategies, such as higher levodopa doses, longer administration, or starting the drug at later stages of disease, they wrote.
Dr. de Bie reported grants from ZonMw, Parkinson Vereniging, and Stichting Parkinsonfonds during the conduct of the study, as well as grants from GE Health and Medtronic outside the submitted work. Study authors provided disclosures related to Netherlands Organization for Scientific Research, Michael J. Fox Foundation, UCB, AbbVie, Boston Scientific, Biogen, Merck, and others.
SOURCE: Verschuur CVM et al. N Engl J Med. 2019;380:315-24.
This trial supports current clinical practice in two ways, according to Susan Bressman, MD, and Rachel Saunders‑Pullman, MD, MPH. On one hand, the study provides no evidence to suggest that levodopa slows Parkinson’s disease progression, Dr. Bressman and Dr. Saunders-Pullman wrote in an editorial accompanying the study. On the other hand, they added, it provides no evidence that clinicians should delay therapy when it is clinically indicated.
The LEAP trial (Levodopa in Early Parkinson’s Disease) was designed to resolve uncertainty over the potential effects of levodopa on disease progression, they noted. This was necessary because of the results of the placebo-controlled ELLDOPA trial, which was published about 14 years ago and suggested that patients randomized to 40 weeks of levodopa did not deteriorate clinically to the degree that was observed in patients randomized to placebo.
The primary end point of that trial was Unified Parkinson’s Disease Rating Scale (UPDRS) scores after a 2-week washout period.
While one interpretation of the UPDRS results from ELLDOPA was that levodopa slowed disease progression, another was that the 2-week washout period was too short, allowing for residual effects of levodopa on symptoms, suggested Dr. Bressman and Dr. Saunders-Pullman.
The randomized LEAP study now shows not only that there were no differences in UPDRS scores when using a delayed start trial design – which implies that there was no disease-modifying effect – but also that starting levodopa early did not have negative effects, the editorial authors wrote.
In particular, the researchers showed no differences in rates of dyskinesia or levodopa-related fluctuations in those started early versus those started later.
“The results of the current trial, taken together with those of other trials, support treatment that is guided by clinical need and that uses the lowest dose that provides a satisfactory clinical effect,” wrote the editorial’s authors.
Dr. Bressman and Dr. Saunders‑Pullman are with the Icahn School of Medicine at Mt. Sinai, New York. Their editorial appears in the New England Journal of Medicine (2019;380:389-90). Dr. Bressman reported disclosures related to Denali Therapeutics, the Michael J. Fox Foundation, and Prevail Therapeutics, while Dr. Saunders-Pullman reported disclosures with Denali Therapeutics, the National Institutes of Health, Genzyme Sanofi, and the Bigglesworth Family Foundation.
This trial supports current clinical practice in two ways, according to Susan Bressman, MD, and Rachel Saunders‑Pullman, MD, MPH. On one hand, the study provides no evidence to suggest that levodopa slows Parkinson’s disease progression, Dr. Bressman and Dr. Saunders-Pullman wrote in an editorial accompanying the study. On the other hand, they added, it provides no evidence that clinicians should delay therapy when it is clinically indicated.
The LEAP trial (Levodopa in Early Parkinson’s Disease) was designed to resolve uncertainty over the potential effects of levodopa on disease progression, they noted. This was necessary because of the results of the placebo-controlled ELLDOPA trial, which was published about 14 years ago and suggested that patients randomized to 40 weeks of levodopa did not deteriorate clinically to the degree that was observed in patients randomized to placebo.
The primary end point of that trial was Unified Parkinson’s Disease Rating Scale (UPDRS) scores after a 2-week washout period.
While one interpretation of the UPDRS results from ELLDOPA was that levodopa slowed disease progression, another was that the 2-week washout period was too short, allowing for residual effects of levodopa on symptoms, suggested Dr. Bressman and Dr. Saunders-Pullman.
The randomized LEAP study now shows not only that there were no differences in UPDRS scores when using a delayed start trial design – which implies that there was no disease-modifying effect – but also that starting levodopa early did not have negative effects, the editorial authors wrote.
In particular, the researchers showed no differences in rates of dyskinesia or levodopa-related fluctuations in those started early versus those started later.
“The results of the current trial, taken together with those of other trials, support treatment that is guided by clinical need and that uses the lowest dose that provides a satisfactory clinical effect,” wrote the editorial’s authors.
Dr. Bressman and Dr. Saunders‑Pullman are with the Icahn School of Medicine at Mt. Sinai, New York. Their editorial appears in the New England Journal of Medicine (2019;380:389-90). Dr. Bressman reported disclosures related to Denali Therapeutics, the Michael J. Fox Foundation, and Prevail Therapeutics, while Dr. Saunders-Pullman reported disclosures with Denali Therapeutics, the National Institutes of Health, Genzyme Sanofi, and the Bigglesworth Family Foundation.
This trial supports current clinical practice in two ways, according to Susan Bressman, MD, and Rachel Saunders‑Pullman, MD, MPH. On one hand, the study provides no evidence to suggest that levodopa slows Parkinson’s disease progression, Dr. Bressman and Dr. Saunders-Pullman wrote in an editorial accompanying the study. On the other hand, they added, it provides no evidence that clinicians should delay therapy when it is clinically indicated.
The LEAP trial (Levodopa in Early Parkinson’s Disease) was designed to resolve uncertainty over the potential effects of levodopa on disease progression, they noted. This was necessary because of the results of the placebo-controlled ELLDOPA trial, which was published about 14 years ago and suggested that patients randomized to 40 weeks of levodopa did not deteriorate clinically to the degree that was observed in patients randomized to placebo.
The primary end point of that trial was Unified Parkinson’s Disease Rating Scale (UPDRS) scores after a 2-week washout period.
While one interpretation of the UPDRS results from ELLDOPA was that levodopa slowed disease progression, another was that the 2-week washout period was too short, allowing for residual effects of levodopa on symptoms, suggested Dr. Bressman and Dr. Saunders-Pullman.
The randomized LEAP study now shows not only that there were no differences in UPDRS scores when using a delayed start trial design – which implies that there was no disease-modifying effect – but also that starting levodopa early did not have negative effects, the editorial authors wrote.
In particular, the researchers showed no differences in rates of dyskinesia or levodopa-related fluctuations in those started early versus those started later.
“The results of the current trial, taken together with those of other trials, support treatment that is guided by clinical need and that uses the lowest dose that provides a satisfactory clinical effect,” wrote the editorial’s authors.
Dr. Bressman and Dr. Saunders‑Pullman are with the Icahn School of Medicine at Mt. Sinai, New York. Their editorial appears in the New England Journal of Medicine (2019;380:389-90). Dr. Bressman reported disclosures related to Denali Therapeutics, the Michael J. Fox Foundation, and Prevail Therapeutics, while Dr. Saunders-Pullman reported disclosures with Denali Therapeutics, the National Institutes of Health, Genzyme Sanofi, and the Bigglesworth Family Foundation.
investigators reported. The disease course was not significantly different for patients who had a full 80 weeks of levodopa/carbodopa therapy, compared with that seen with those who started treatment after a 40-week delay, according to the investigators.
“These findings imply that levodopa had no disease-modifying effect on Parkinson’s disease over the period of the trial,” wrote investigator Rob M. A. de Bie, MD, PhD, professor of movement disorders at the University of Amsterdam, and his colleagues in the New England Journal of Medicine.
By contrast, results of an earlier randomized, placebo-controlled trial suggested that levodopa had disease-modifying effects, though the findings of that study were inconclusive, according to authors of an editorial (see Views on the News).
In the current multicenter trial, known as LEAP (Levodopa in Early Parkinson’s Disease) a total of 445 patients with early Parkinson’s disease were randomized to either 80 weeks of levodopa and carbodopa or to 40 weeks of placebo followed by 40 weeks of levodopa/carbodopa.
Levodopa was dosed at 100 mg three times per day, and carbodopa at 25 mg three times per day, according to the report.
There was no significant difference between the early and delayed treatment groups for primary outcome of the trial, which was change in the Unified Parkinson’s Disease Rating Scale (UPDRS) from baseline to week 80.
The mean change in UPDRS was –1.0 in the group of patients who had the full 80 weeks of levodopa/carbodopa and –2.0 for those who had delayed therapy, for a difference of 1 point (P = .44). Higher scores on the UPDRS signify worse disease.
At week 40, there was a change in UPDRS favoring the early-initiation strategy, which reflected the effects of levodopa on disease symptoms, investigators added.
Nausea was more common in the early-start group during the first 40 weeks of the trial. However, there were no differences between groups in other adverse events of particular interest, including dyskinesias and motor fluctuations related to levodopa, Dr. de Bie and his colleagues reported.
Taken together, these results suggest no beneficial or detrimental disease-modifying effect for an early treatment strategy, although further trials are warranted to evaluate other strategies, such as higher levodopa doses, longer administration, or starting the drug at later stages of disease, they wrote.
Dr. de Bie reported grants from ZonMw, Parkinson Vereniging, and Stichting Parkinsonfonds during the conduct of the study, as well as grants from GE Health and Medtronic outside the submitted work. Study authors provided disclosures related to Netherlands Organization for Scientific Research, Michael J. Fox Foundation, UCB, AbbVie, Boston Scientific, Biogen, Merck, and others.
SOURCE: Verschuur CVM et al. N Engl J Med. 2019;380:315-24.
investigators reported. The disease course was not significantly different for patients who had a full 80 weeks of levodopa/carbodopa therapy, compared with that seen with those who started treatment after a 40-week delay, according to the investigators.
“These findings imply that levodopa had no disease-modifying effect on Parkinson’s disease over the period of the trial,” wrote investigator Rob M. A. de Bie, MD, PhD, professor of movement disorders at the University of Amsterdam, and his colleagues in the New England Journal of Medicine.
By contrast, results of an earlier randomized, placebo-controlled trial suggested that levodopa had disease-modifying effects, though the findings of that study were inconclusive, according to authors of an editorial (see Views on the News).
In the current multicenter trial, known as LEAP (Levodopa in Early Parkinson’s Disease) a total of 445 patients with early Parkinson’s disease were randomized to either 80 weeks of levodopa and carbodopa or to 40 weeks of placebo followed by 40 weeks of levodopa/carbodopa.
Levodopa was dosed at 100 mg three times per day, and carbodopa at 25 mg three times per day, according to the report.
There was no significant difference between the early and delayed treatment groups for primary outcome of the trial, which was change in the Unified Parkinson’s Disease Rating Scale (UPDRS) from baseline to week 80.
The mean change in UPDRS was –1.0 in the group of patients who had the full 80 weeks of levodopa/carbodopa and –2.0 for those who had delayed therapy, for a difference of 1 point (P = .44). Higher scores on the UPDRS signify worse disease.
At week 40, there was a change in UPDRS favoring the early-initiation strategy, which reflected the effects of levodopa on disease symptoms, investigators added.
Nausea was more common in the early-start group during the first 40 weeks of the trial. However, there were no differences between groups in other adverse events of particular interest, including dyskinesias and motor fluctuations related to levodopa, Dr. de Bie and his colleagues reported.
Taken together, these results suggest no beneficial or detrimental disease-modifying effect for an early treatment strategy, although further trials are warranted to evaluate other strategies, such as higher levodopa doses, longer administration, or starting the drug at later stages of disease, they wrote.
Dr. de Bie reported grants from ZonMw, Parkinson Vereniging, and Stichting Parkinsonfonds during the conduct of the study, as well as grants from GE Health and Medtronic outside the submitted work. Study authors provided disclosures related to Netherlands Organization for Scientific Research, Michael J. Fox Foundation, UCB, AbbVie, Boston Scientific, Biogen, Merck, and others.
SOURCE: Verschuur CVM et al. N Engl J Med. 2019;380:315-24.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Levodopa did not have any significant disease-modifying effects in patients with early Parkinson’s disease.
Major finding: Change in the Unified Parkinson’s Disease Rating Scale (UPDRS) was –1.0 after 80 weeks of levodopa/carbodopa versus –2.0 for 40 weeks of placebo followed by 40 weeks of treatment (P = .44).
Study details: A delayed-start trial including 445 patients with early Parkinson’s disease randomized to 80 weeks of treatment or 40 weeks of placebo plus 40 weeks of treatment.
Disclosures: Study authors reported disclosures related to Netherlands Organization for Scientific Research, Michael J. Fox Foundation, UCB, AbbVie, Boston Scientific, Biogen, Merck, and others.
Source: Verschuur CVM et al. N Engl J Med. 2019;380:315-324.
Nuedexta mainly prescribed for dementia, Parkinson’s
Only 15% of patients prescribed dextromethorphan hydrobromide plus quinidine sulfate had pseudobulbar affect due to multiple sclerosis or amyotrophic lateral sclerosis, the condition for which this drug is labeled, according to an analysis of two national commercial insurance claims databases published online Jan. 7 in JAMA Internal Medicine.
Conversely, 57% of patients prescribed dextromethorphan-quinidine (Nuedexta) had a diagnosis of Parkinson’s disease or dementia. Furthermore, according to Medicare Part D data, prescriptions for dextromethorphan-quinidine rose 15-fold during a recent 6-year period, with a concurrent 50-fold rise in reimbursement. “In response to findings such as ours, further attention should be paid to educating prescribers about the actual benefits and risks of this costly drug combination,” Michael Fralick, MD, and his associates at Brigham and Women’s Hospital and Harvard Medical School, Boston, wrote in their paper.
The Food and Drug Administration approved Nuedexta in 2010 for the treatment of pseudobulbar affect after it produced modest improvements in laughing or crying episodes in a 12-week, placebo-controlled trial of patients with multiple sclerosis (MS) or amyotrophic lateral sclerosis (ALS). The initial FDA label noted: “Nuedexta has not been shown to be safe or effective in other types of emotional lability that can commonly occur, for example, in Alzheimer’s disease and other dementias.” Then, in 2015, patients with Alzheimer’s disease showed modest improvements in agitation scores when they received dextromethorphan-quinidine in a 10-week, placebo-controlled, industry-designed and sponsored trial. Although the dextromethorphan-quinidine arm also had higher rates of falls, urinary tract infections, and serious adverse events, the prescribing information was updated in 2015 to remove the statement about patients with dementia.
To assess real-world prescribing patterns for dextromethorphan-quinidine, Dr. Fralick and his associates analyzed data from 12,858 patients who filled a prescription for this medication between 2010 and 2017 and were recorded in the Optum Clinformatics Data Mart or Truven Health MarketScan databases. Only 8.4% of patients had a diagnosis of MS and only 6.8% had ALS, while 57% had dementia and/or Parkinson’s disease and 28% had an unknown diagnosis. The number of patients prescribed dextromethorphan-quinidine rose from nearly 3,300 in 2011 to more than 50,000 in 2016, while spending on this medication by the Centers for Medicare & Medicaid Services increased from $3.9 million to $200.4 million during the same time period.
Current treatments for behavioral symptoms of dementia “are largely ineffective, and thus clinicians may want to prescribe dextromethorphan-quinidine to see if it helps their patients,” the researchers wrote. “Yet the absence of data showing efficacy, coupled with the demonstrated risks of falls and possible cardiac effects, calls this strategy into question.
“Further studies should be required to evaluate the safety and effectiveness of this medication as it is currently being used,” the authors suggested.
Study funders included the Laura and John Arnold Foundation, the Harvard Program in Therapeutic Science, the Engelberg Foundation, and the University of Toronto Clinician Scientist Training Program. One author disclosed grants from the Food and Drug Administration Office of Generic Drugs and Division of Health Communication unrelated to the study topic.
SOURCE: Fralick M et al. JAMA Inter Med. 2019 Jan 7. doi: 10.1001/jamainternmed.2018.6112
Only 15% of patients prescribed dextromethorphan hydrobromide plus quinidine sulfate had pseudobulbar affect due to multiple sclerosis or amyotrophic lateral sclerosis, the condition for which this drug is labeled, according to an analysis of two national commercial insurance claims databases published online Jan. 7 in JAMA Internal Medicine.
Conversely, 57% of patients prescribed dextromethorphan-quinidine (Nuedexta) had a diagnosis of Parkinson’s disease or dementia. Furthermore, according to Medicare Part D data, prescriptions for dextromethorphan-quinidine rose 15-fold during a recent 6-year period, with a concurrent 50-fold rise in reimbursement. “In response to findings such as ours, further attention should be paid to educating prescribers about the actual benefits and risks of this costly drug combination,” Michael Fralick, MD, and his associates at Brigham and Women’s Hospital and Harvard Medical School, Boston, wrote in their paper.
The Food and Drug Administration approved Nuedexta in 2010 for the treatment of pseudobulbar affect after it produced modest improvements in laughing or crying episodes in a 12-week, placebo-controlled trial of patients with multiple sclerosis (MS) or amyotrophic lateral sclerosis (ALS). The initial FDA label noted: “Nuedexta has not been shown to be safe or effective in other types of emotional lability that can commonly occur, for example, in Alzheimer’s disease and other dementias.” Then, in 2015, patients with Alzheimer’s disease showed modest improvements in agitation scores when they received dextromethorphan-quinidine in a 10-week, placebo-controlled, industry-designed and sponsored trial. Although the dextromethorphan-quinidine arm also had higher rates of falls, urinary tract infections, and serious adverse events, the prescribing information was updated in 2015 to remove the statement about patients with dementia.
To assess real-world prescribing patterns for dextromethorphan-quinidine, Dr. Fralick and his associates analyzed data from 12,858 patients who filled a prescription for this medication between 2010 and 2017 and were recorded in the Optum Clinformatics Data Mart or Truven Health MarketScan databases. Only 8.4% of patients had a diagnosis of MS and only 6.8% had ALS, while 57% had dementia and/or Parkinson’s disease and 28% had an unknown diagnosis. The number of patients prescribed dextromethorphan-quinidine rose from nearly 3,300 in 2011 to more than 50,000 in 2016, while spending on this medication by the Centers for Medicare & Medicaid Services increased from $3.9 million to $200.4 million during the same time period.
Current treatments for behavioral symptoms of dementia “are largely ineffective, and thus clinicians may want to prescribe dextromethorphan-quinidine to see if it helps their patients,” the researchers wrote. “Yet the absence of data showing efficacy, coupled with the demonstrated risks of falls and possible cardiac effects, calls this strategy into question.
“Further studies should be required to evaluate the safety and effectiveness of this medication as it is currently being used,” the authors suggested.
Study funders included the Laura and John Arnold Foundation, the Harvard Program in Therapeutic Science, the Engelberg Foundation, and the University of Toronto Clinician Scientist Training Program. One author disclosed grants from the Food and Drug Administration Office of Generic Drugs and Division of Health Communication unrelated to the study topic.
SOURCE: Fralick M et al. JAMA Inter Med. 2019 Jan 7. doi: 10.1001/jamainternmed.2018.6112
Only 15% of patients prescribed dextromethorphan hydrobromide plus quinidine sulfate had pseudobulbar affect due to multiple sclerosis or amyotrophic lateral sclerosis, the condition for which this drug is labeled, according to an analysis of two national commercial insurance claims databases published online Jan. 7 in JAMA Internal Medicine.
Conversely, 57% of patients prescribed dextromethorphan-quinidine (Nuedexta) had a diagnosis of Parkinson’s disease or dementia. Furthermore, according to Medicare Part D data, prescriptions for dextromethorphan-quinidine rose 15-fold during a recent 6-year period, with a concurrent 50-fold rise in reimbursement. “In response to findings such as ours, further attention should be paid to educating prescribers about the actual benefits and risks of this costly drug combination,” Michael Fralick, MD, and his associates at Brigham and Women’s Hospital and Harvard Medical School, Boston, wrote in their paper.
The Food and Drug Administration approved Nuedexta in 2010 for the treatment of pseudobulbar affect after it produced modest improvements in laughing or crying episodes in a 12-week, placebo-controlled trial of patients with multiple sclerosis (MS) or amyotrophic lateral sclerosis (ALS). The initial FDA label noted: “Nuedexta has not been shown to be safe or effective in other types of emotional lability that can commonly occur, for example, in Alzheimer’s disease and other dementias.” Then, in 2015, patients with Alzheimer’s disease showed modest improvements in agitation scores when they received dextromethorphan-quinidine in a 10-week, placebo-controlled, industry-designed and sponsored trial. Although the dextromethorphan-quinidine arm also had higher rates of falls, urinary tract infections, and serious adverse events, the prescribing information was updated in 2015 to remove the statement about patients with dementia.
To assess real-world prescribing patterns for dextromethorphan-quinidine, Dr. Fralick and his associates analyzed data from 12,858 patients who filled a prescription for this medication between 2010 and 2017 and were recorded in the Optum Clinformatics Data Mart or Truven Health MarketScan databases. Only 8.4% of patients had a diagnosis of MS and only 6.8% had ALS, while 57% had dementia and/or Parkinson’s disease and 28% had an unknown diagnosis. The number of patients prescribed dextromethorphan-quinidine rose from nearly 3,300 in 2011 to more than 50,000 in 2016, while spending on this medication by the Centers for Medicare & Medicaid Services increased from $3.9 million to $200.4 million during the same time period.
Current treatments for behavioral symptoms of dementia “are largely ineffective, and thus clinicians may want to prescribe dextromethorphan-quinidine to see if it helps their patients,” the researchers wrote. “Yet the absence of data showing efficacy, coupled with the demonstrated risks of falls and possible cardiac effects, calls this strategy into question.
“Further studies should be required to evaluate the safety and effectiveness of this medication as it is currently being used,” the authors suggested.
Study funders included the Laura and John Arnold Foundation, the Harvard Program in Therapeutic Science, the Engelberg Foundation, and the University of Toronto Clinician Scientist Training Program. One author disclosed grants from the Food and Drug Administration Office of Generic Drugs and Division of Health Communication unrelated to the study topic.
SOURCE: Fralick M et al. JAMA Inter Med. 2019 Jan 7. doi: 10.1001/jamainternmed.2018.6112
FROM JAMA INTERNAL MEDICINE
Key clinical point:
Major finding: Only 8.4% of patients had a diagnosis of multiple sclerosis and only 6.8% had amyotrophic lateral sclerosis, while 57% had dementia and/or Parkinson’s disease and 28% had an unknown diagnosis.
Study details: Population-based cohort study of 12,858 patients prescribed dextromethorphan-quinidine between 2010 and 2017.
Disclosures: Study funders included the Laura and John Arnold Foundation, the Harvard Program in Therapeutic Science, the Engelberg Foundation, and the University of Toronto Clinician Scientist Training Program. One author disclosed grants from the Food and Drug Administration Office of Generic Drugs and Division of Health Communication unrelated to the study topic.
Source: Fralick M et al. JAMA Intern Med. 2019 Jan 7. doi: 10.1001/jamainternmed.2018.6112.
Neurologic Disease Eventually Affects Half of Women and One-Third of Men
Findings strengthen the call for prioritizing the focus on preventive interventions at the population level.
Around one-half of women and one-third of men will develop dementia, stroke, or parkinsonism during their lifetime, according to a study published online ahead of print October 2 in the Journal of Neurology, Neurosurgery & Psychiatry.
The population-based Rotterdam study involved 12,102 individuals (57.7% women) who were ages 45 or older and free of neurologic disease at baseline. This cohort was followed for 26 years. Silvan Licher, a PhD student in the Department of Epidemiology at Erasmus MC University Medical Center Rotterdam in the Netherlands, and colleagues found that a 45-year-old woman had a 48.2% overall remaining lifetime risk of developing dementia, stroke, or parkinsonism, while a 45-year-old man had a 36.3% lifetime risk.
“There are currently no disease-modifying drugs available for dementia and most causes of parkinsonism, and prevention of stroke is hampered by suboptimal adherence to effective preventive strategies or unmet guideline thresholds,” the authors wrote. “Yet a delay in onset of these common neurologic diseases by merely a few years could reduce the population burden of these diseases substantially.”
Women age 45 had a significantly higher lifetime risk than men of developing dementia (31.4% vs 18.6%, respectively) and stroke (21.6% vs 19.3%), but the risk of parkinsonism was similar between the sexes. Women also had a significantly greater lifetime risk of developing more than one neurologic disease, compared with men (4% vs 3.1%), largely because of the overlap between dementia and stroke.
At age 45, women had the greatest risk of dementia, but as men and women aged, their remaining lifetime risk of dementia increased relative to other neurologic diseases. After age 85, 66.6% of first diagnoses in women and 55.6% in men were dementia. By comparison, first manifestation of stroke was the greatest threat to men age 45. Men also were at a significantly higher risk for stroke at a younger age—before age 75—than were women (8.4% vs 5.8%, respectively). In the case of parkinsonism, the lifetime risk peaked earlier than it did for dementia and stroke and was relatively low after age 85, with no significant differences in risk between men and women.
The authors considered what effect a delay in disease onset and occurrence might have on remaining lifetime risk for neurologic disease. They found that a one-, two-, or three-year delay in the onset of all neurologic disease was associated with a 20% reduction in lifetime risk in individuals age 45 or older, and a greater than 50% reduction in risk in the oldest. A three-year delay in the onset of dementia reduced the lifetime risk by 15% for men and women age 45 and conveyed a 30% reduction in risk to those age 45 or older.
The Rotterdam study is supported by Erasmus MC and Erasmus University Rotterdam; the Netherlands Organization for Scientific Research; the Netherlands Organization for Health Research and Development; the Research Institute for Diseases in the Elderly; the Netherlands Genomics Initiative; the Ministry of Education, Culture, and Science; the Ministry of Health, Welfare, and Sports; the European Commission and the Municipality of Rotterdam; the Netherlands Consortium for Healthy Aging; and the Dutch Heart Foundation.
—Bianca Nogrady
Suggested Reading
Licher S, Darweesh SKL, Wolters FJ, et al. Lifetime risk of common neurological diseases in the elderly population. J Neurol Neurosurg Psychiatry. 2018 Oct 2 [Epub ahead of print].
Findings strengthen the call for prioritizing the focus on preventive interventions at the population level.
Findings strengthen the call for prioritizing the focus on preventive interventions at the population level.
Around one-half of women and one-third of men will develop dementia, stroke, or parkinsonism during their lifetime, according to a study published online ahead of print October 2 in the Journal of Neurology, Neurosurgery & Psychiatry.
The population-based Rotterdam study involved 12,102 individuals (57.7% women) who were ages 45 or older and free of neurologic disease at baseline. This cohort was followed for 26 years. Silvan Licher, a PhD student in the Department of Epidemiology at Erasmus MC University Medical Center Rotterdam in the Netherlands, and colleagues found that a 45-year-old woman had a 48.2% overall remaining lifetime risk of developing dementia, stroke, or parkinsonism, while a 45-year-old man had a 36.3% lifetime risk.
“There are currently no disease-modifying drugs available for dementia and most causes of parkinsonism, and prevention of stroke is hampered by suboptimal adherence to effective preventive strategies or unmet guideline thresholds,” the authors wrote. “Yet a delay in onset of these common neurologic diseases by merely a few years could reduce the population burden of these diseases substantially.”
Women age 45 had a significantly higher lifetime risk than men of developing dementia (31.4% vs 18.6%, respectively) and stroke (21.6% vs 19.3%), but the risk of parkinsonism was similar between the sexes. Women also had a significantly greater lifetime risk of developing more than one neurologic disease, compared with men (4% vs 3.1%), largely because of the overlap between dementia and stroke.
At age 45, women had the greatest risk of dementia, but as men and women aged, their remaining lifetime risk of dementia increased relative to other neurologic diseases. After age 85, 66.6% of first diagnoses in women and 55.6% in men were dementia. By comparison, first manifestation of stroke was the greatest threat to men age 45. Men also were at a significantly higher risk for stroke at a younger age—before age 75—than were women (8.4% vs 5.8%, respectively). In the case of parkinsonism, the lifetime risk peaked earlier than it did for dementia and stroke and was relatively low after age 85, with no significant differences in risk between men and women.
The authors considered what effect a delay in disease onset and occurrence might have on remaining lifetime risk for neurologic disease. They found that a one-, two-, or three-year delay in the onset of all neurologic disease was associated with a 20% reduction in lifetime risk in individuals age 45 or older, and a greater than 50% reduction in risk in the oldest. A three-year delay in the onset of dementia reduced the lifetime risk by 15% for men and women age 45 and conveyed a 30% reduction in risk to those age 45 or older.
The Rotterdam study is supported by Erasmus MC and Erasmus University Rotterdam; the Netherlands Organization for Scientific Research; the Netherlands Organization for Health Research and Development; the Research Institute for Diseases in the Elderly; the Netherlands Genomics Initiative; the Ministry of Education, Culture, and Science; the Ministry of Health, Welfare, and Sports; the European Commission and the Municipality of Rotterdam; the Netherlands Consortium for Healthy Aging; and the Dutch Heart Foundation.
—Bianca Nogrady
Suggested Reading
Licher S, Darweesh SKL, Wolters FJ, et al. Lifetime risk of common neurological diseases in the elderly population. J Neurol Neurosurg Psychiatry. 2018 Oct 2 [Epub ahead of print].
Around one-half of women and one-third of men will develop dementia, stroke, or parkinsonism during their lifetime, according to a study published online ahead of print October 2 in the Journal of Neurology, Neurosurgery & Psychiatry.
The population-based Rotterdam study involved 12,102 individuals (57.7% women) who were ages 45 or older and free of neurologic disease at baseline. This cohort was followed for 26 years. Silvan Licher, a PhD student in the Department of Epidemiology at Erasmus MC University Medical Center Rotterdam in the Netherlands, and colleagues found that a 45-year-old woman had a 48.2% overall remaining lifetime risk of developing dementia, stroke, or parkinsonism, while a 45-year-old man had a 36.3% lifetime risk.
“There are currently no disease-modifying drugs available for dementia and most causes of parkinsonism, and prevention of stroke is hampered by suboptimal adherence to effective preventive strategies or unmet guideline thresholds,” the authors wrote. “Yet a delay in onset of these common neurologic diseases by merely a few years could reduce the population burden of these diseases substantially.”
Women age 45 had a significantly higher lifetime risk than men of developing dementia (31.4% vs 18.6%, respectively) and stroke (21.6% vs 19.3%), but the risk of parkinsonism was similar between the sexes. Women also had a significantly greater lifetime risk of developing more than one neurologic disease, compared with men (4% vs 3.1%), largely because of the overlap between dementia and stroke.
At age 45, women had the greatest risk of dementia, but as men and women aged, their remaining lifetime risk of dementia increased relative to other neurologic diseases. After age 85, 66.6% of first diagnoses in women and 55.6% in men were dementia. By comparison, first manifestation of stroke was the greatest threat to men age 45. Men also were at a significantly higher risk for stroke at a younger age—before age 75—than were women (8.4% vs 5.8%, respectively). In the case of parkinsonism, the lifetime risk peaked earlier than it did for dementia and stroke and was relatively low after age 85, with no significant differences in risk between men and women.
The authors considered what effect a delay in disease onset and occurrence might have on remaining lifetime risk for neurologic disease. They found that a one-, two-, or three-year delay in the onset of all neurologic disease was associated with a 20% reduction in lifetime risk in individuals age 45 or older, and a greater than 50% reduction in risk in the oldest. A three-year delay in the onset of dementia reduced the lifetime risk by 15% for men and women age 45 and conveyed a 30% reduction in risk to those age 45 or older.
The Rotterdam study is supported by Erasmus MC and Erasmus University Rotterdam; the Netherlands Organization for Scientific Research; the Netherlands Organization for Health Research and Development; the Research Institute for Diseases in the Elderly; the Netherlands Genomics Initiative; the Ministry of Education, Culture, and Science; the Ministry of Health, Welfare, and Sports; the European Commission and the Municipality of Rotterdam; the Netherlands Consortium for Healthy Aging; and the Dutch Heart Foundation.
—Bianca Nogrady
Suggested Reading
Licher S, Darweesh SKL, Wolters FJ, et al. Lifetime risk of common neurological diseases in the elderly population. J Neurol Neurosurg Psychiatry. 2018 Oct 2 [Epub ahead of print].
New brain circuitry found with Parkinson’s disease gene therapy
A gene therapy for Parkinson’s disease, focusing on the subthalamic nucleus, appears to lead to the formation of unique brain circuitry that correlates with clinical improvement.
In a paper published online Nov. 28 in Science Translational Medicine, researchers describe the findings of a metabolic imaging study to explore the mechanism underlying benefits seen in a phase 2, blinded, sham-controlled clinical trial of the gene therapy.
The therapy in question used an adeno-associated viral vector to deliver the gene for glutamic acid decarboxylase into the subthalamic nucleus – a region of the brain known to be overactivated in Parkinson’s disease – which was intended to have an inhibitory effect on the neurons in that region.
Martin Niethammer, MD, PhD, of the Center for Neurosciences at The Feinstein Institute for Medical Research in New York, and his coauthors used 18F-fluorodeoxyglucose positron emission tomography at baseline, 6, and 12 months in 15 gene-therapy patients and 21 sham-treated patients, which revealed the development of new brain circuits in patients treated with the gene therapy.
The circuits, which researchers called the glutamic acid decarboxylase-related pattern, or GADRP, presented with increased metabolism in the premotor region – which also extended into the adjacent motor cortex – and in the supramarginal gyrus. There was also decreased metabolic activity in the caudate, anterior putamen, and adjacent globus pallidus; the ventral anterior and medial dorsal thalamic nuclei; and in the inferior frontal gyrus.
All 15 patients who received the gene therapy showed significant trends in GADRP expression after the treatment, compared with patients who underwent the sham procedure. Furthermore, these correlated significantly with improved clinical outcomes.
The imaging also revealed increased connectivity between regions in the GADRP space among patients who received the gene therapy, with researchers noting five new intrahemispheric node-to-node connections in these patients that were not seen in the sham procedure group.
These included connection linking the left caudate nucleus to the left superior frontal node, the right superior frontal node to the right supramarginal gyrus, and linking the left anterior putamen and globus pallidus with the ipsilateral thalamic node.
The authors also found that overall connectivity in the network rose to “abnormal” levels in the 12 months after gene therapy, while no similar increases were seen in the sham group.
Given that deep brain stimulation for Parkinson’s disease also targets the subthalamic nucleus, researchers looked at changes to the GADRP network in these patients, compared with those who received sham therapy and those who received gene therapy.
They saw that changes in GADRP expression were significantly different between the gene therapy-treated patients and those treated with deep brain stimulation and sham surgery. However, the differences between deep brain stimulation and sham surgery were not significant.
“The current study indicates that customized networks can be characterized using functional imaging data acquired in randomized, controlled phase 2 clinical trials and, if validated, could be used as quantitative outcome measures in more definitive, later-stage clinical trials,” the authors wrote.
The study was supported by Neurologix. Two authors were consultants and stockholders of MeiraGTx.
SOURCE: Niethammer N et al. Sci Transl Med. 2018 Nov 28. doi: 10.1126/scitranslmed.aau0713.
A gene therapy for Parkinson’s disease, focusing on the subthalamic nucleus, appears to lead to the formation of unique brain circuitry that correlates with clinical improvement.
In a paper published online Nov. 28 in Science Translational Medicine, researchers describe the findings of a metabolic imaging study to explore the mechanism underlying benefits seen in a phase 2, blinded, sham-controlled clinical trial of the gene therapy.
The therapy in question used an adeno-associated viral vector to deliver the gene for glutamic acid decarboxylase into the subthalamic nucleus – a region of the brain known to be overactivated in Parkinson’s disease – which was intended to have an inhibitory effect on the neurons in that region.
Martin Niethammer, MD, PhD, of the Center for Neurosciences at The Feinstein Institute for Medical Research in New York, and his coauthors used 18F-fluorodeoxyglucose positron emission tomography at baseline, 6, and 12 months in 15 gene-therapy patients and 21 sham-treated patients, which revealed the development of new brain circuits in patients treated with the gene therapy.
The circuits, which researchers called the glutamic acid decarboxylase-related pattern, or GADRP, presented with increased metabolism in the premotor region – which also extended into the adjacent motor cortex – and in the supramarginal gyrus. There was also decreased metabolic activity in the caudate, anterior putamen, and adjacent globus pallidus; the ventral anterior and medial dorsal thalamic nuclei; and in the inferior frontal gyrus.
All 15 patients who received the gene therapy showed significant trends in GADRP expression after the treatment, compared with patients who underwent the sham procedure. Furthermore, these correlated significantly with improved clinical outcomes.
The imaging also revealed increased connectivity between regions in the GADRP space among patients who received the gene therapy, with researchers noting five new intrahemispheric node-to-node connections in these patients that were not seen in the sham procedure group.
These included connection linking the left caudate nucleus to the left superior frontal node, the right superior frontal node to the right supramarginal gyrus, and linking the left anterior putamen and globus pallidus with the ipsilateral thalamic node.
The authors also found that overall connectivity in the network rose to “abnormal” levels in the 12 months after gene therapy, while no similar increases were seen in the sham group.
Given that deep brain stimulation for Parkinson’s disease also targets the subthalamic nucleus, researchers looked at changes to the GADRP network in these patients, compared with those who received sham therapy and those who received gene therapy.
They saw that changes in GADRP expression were significantly different between the gene therapy-treated patients and those treated with deep brain stimulation and sham surgery. However, the differences between deep brain stimulation and sham surgery were not significant.
“The current study indicates that customized networks can be characterized using functional imaging data acquired in randomized, controlled phase 2 clinical trials and, if validated, could be used as quantitative outcome measures in more definitive, later-stage clinical trials,” the authors wrote.
The study was supported by Neurologix. Two authors were consultants and stockholders of MeiraGTx.
SOURCE: Niethammer N et al. Sci Transl Med. 2018 Nov 28. doi: 10.1126/scitranslmed.aau0713.
A gene therapy for Parkinson’s disease, focusing on the subthalamic nucleus, appears to lead to the formation of unique brain circuitry that correlates with clinical improvement.
In a paper published online Nov. 28 in Science Translational Medicine, researchers describe the findings of a metabolic imaging study to explore the mechanism underlying benefits seen in a phase 2, blinded, sham-controlled clinical trial of the gene therapy.
The therapy in question used an adeno-associated viral vector to deliver the gene for glutamic acid decarboxylase into the subthalamic nucleus – a region of the brain known to be overactivated in Parkinson’s disease – which was intended to have an inhibitory effect on the neurons in that region.
Martin Niethammer, MD, PhD, of the Center for Neurosciences at The Feinstein Institute for Medical Research in New York, and his coauthors used 18F-fluorodeoxyglucose positron emission tomography at baseline, 6, and 12 months in 15 gene-therapy patients and 21 sham-treated patients, which revealed the development of new brain circuits in patients treated with the gene therapy.
The circuits, which researchers called the glutamic acid decarboxylase-related pattern, or GADRP, presented with increased metabolism in the premotor region – which also extended into the adjacent motor cortex – and in the supramarginal gyrus. There was also decreased metabolic activity in the caudate, anterior putamen, and adjacent globus pallidus; the ventral anterior and medial dorsal thalamic nuclei; and in the inferior frontal gyrus.
All 15 patients who received the gene therapy showed significant trends in GADRP expression after the treatment, compared with patients who underwent the sham procedure. Furthermore, these correlated significantly with improved clinical outcomes.
The imaging also revealed increased connectivity between regions in the GADRP space among patients who received the gene therapy, with researchers noting five new intrahemispheric node-to-node connections in these patients that were not seen in the sham procedure group.
These included connection linking the left caudate nucleus to the left superior frontal node, the right superior frontal node to the right supramarginal gyrus, and linking the left anterior putamen and globus pallidus with the ipsilateral thalamic node.
The authors also found that overall connectivity in the network rose to “abnormal” levels in the 12 months after gene therapy, while no similar increases were seen in the sham group.
Given that deep brain stimulation for Parkinson’s disease also targets the subthalamic nucleus, researchers looked at changes to the GADRP network in these patients, compared with those who received sham therapy and those who received gene therapy.
They saw that changes in GADRP expression were significantly different between the gene therapy-treated patients and those treated with deep brain stimulation and sham surgery. However, the differences between deep brain stimulation and sham surgery were not significant.
“The current study indicates that customized networks can be characterized using functional imaging data acquired in randomized, controlled phase 2 clinical trials and, if validated, could be used as quantitative outcome measures in more definitive, later-stage clinical trials,” the authors wrote.
The study was supported by Neurologix. Two authors were consultants and stockholders of MeiraGTx.
SOURCE: Niethammer N et al. Sci Transl Med. 2018 Nov 28. doi: 10.1126/scitranslmed.aau0713.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point:
Major finding: Gene therapy for Parkinson’s disease was associated with increased brain connectivity.
Study details: A phase 2, blinded, sham-controlled study of 36 patients with Parkinson’s disease.
Disclosures: The study was supported by Neurologix. Two authors were consultants and stockholders of MeiraGTx.
Source: Niethammer N et al. Sci Transl Med. 2018 Nov 28. doi: 10.1126/scitranslmed.aau0713.