User login
CIPN persists in female cancer survivors

Photo courtesy of NIH
SAN FRANCISCO—A study of female cancer survivors indicates that many still have chemotherapy-induced peripheral neuropathy (CIPN) symptoms years after completing cancer treatment.
In addition, CIPN was associated with worse physical functioning, poorer mobility, and a higher risk of falls.
Although more research is needed, investigators believe these findings may inform rehabilitation and fall prevention interventions for people with CIPN.
The findings were presented at the 2016 Cancer Survivorship Symposium (abstract 130*).
“We can’t dismiss neuropathy as a treatment side effect that goes away because symptoms persist for years in nearly half of women,” said Kerri M. Winters-Stone, PhD, of Oregon Health and Science University in Portland.
“While there are no effective treatments for this side effect, rehabilitative exercise programs may preserve physical functioning and mobility in the presence of neuropathy to help prevent falls and resulting injuries.”
For this study, Dr Winters-Stone and her colleagues assessed data from 512 women enrolled in exercise intervention trials designed to address fractures and falls in female cancer survivors. Most of the women had breast cancer, but there were also cases of lung, colorectal, ovarian, and hematologic cancers.
At an average of 6 years post-cancer diagnosis, 46% of the women (n=238) still reported some symptoms of CIPN, such as loss of feeling in their hands and feet.
The investigators noted significant relationships (P<0.01) between CIPN severity and gait speed, Physical Performance Battery score, self-reported physical functioning, and self-reported disability.
The team also compared measures of physical functioning in the women with CIPN to measures in women without CIPN (n=274). This analysis was adjusted for cancer type and time since diagnosis.
There was a significant difference (P<0.01) between the groups in one measure of lower-extremity fitness but not another. Namely, it took CIPN-positive women significantly longer to rise out of a chair (tested 5 times each). But women in both groups fared similarly on a test measuring maximal leg press strength.
The investigators also tested the women on mobility and physical functioning. The CIPN-positive women fared significantly worse than CIPN-negative women (P<0.01) when it came to walking speed, step number, stride length, percentage of gait cycle in double support, and Physical Performance Battery score. However, there was no significant difference between the groups with regard to base of support.
Finally, CIPN-positive women were significantly more likely than CIPN-negative women to report poor physical function and disability (P<0.01 for both). And CIPN-positive women had a higher rate of falls in the last year (P<0.01).
The investigators said women with CIPN have specific underlying impairments that put them at risk for falls, which may be different from the impairments that occur with other conditions or old age.
For example, CIPN does not cause muscle weakness, but it has a distinct effect on movement and gait patterns.
The team noted that the women with CIPN had difficulty rising from a chair, possibly because their brains do not get enough information from their feet about how quickly or forcefully to stand up.
Based on these findings, the investigators argued that commonly recommended exercise, such as walking, may be safer for women with CIPN when done on a treadmill with handrails because their altered gait puts them at an increased risk of falling.
The team also said that machine-based resistance training may not be beneficial because neuropathy does not appear to decrease leg strength. Instead, rehabilitation efforts should focus on improving balance during upright movement and specific gait training.
Furthermore, the investigators believe that, if the symptoms of CIPN are detected early, cancer treatments could potentially be changed to prevent these debilitating problems or early rehabilitation interventions could be started.
In addition, Dr Winters-Stone and her research team are developing a smartphone-driven device that patients can use to detect and quantify symptoms of neuropathy, such as gait and balance impairments. ![]()
*Data in the abstract differ from the presentation.

Photo courtesy of NIH
SAN FRANCISCO—A study of female cancer survivors indicates that many still have chemotherapy-induced peripheral neuropathy (CIPN) symptoms years after completing cancer treatment.
In addition, CIPN was associated with worse physical functioning, poorer mobility, and a higher risk of falls.
Although more research is needed, investigators believe these findings may inform rehabilitation and fall prevention interventions for people with CIPN.
The findings were presented at the 2016 Cancer Survivorship Symposium (abstract 130*).
“We can’t dismiss neuropathy as a treatment side effect that goes away because symptoms persist for years in nearly half of women,” said Kerri M. Winters-Stone, PhD, of Oregon Health and Science University in Portland.
“While there are no effective treatments for this side effect, rehabilitative exercise programs may preserve physical functioning and mobility in the presence of neuropathy to help prevent falls and resulting injuries.”
For this study, Dr Winters-Stone and her colleagues assessed data from 512 women enrolled in exercise intervention trials designed to address fractures and falls in female cancer survivors. Most of the women had breast cancer, but there were also cases of lung, colorectal, ovarian, and hematologic cancers.
At an average of 6 years post-cancer diagnosis, 46% of the women (n=238) still reported some symptoms of CIPN, such as loss of feeling in their hands and feet.
The investigators noted significant relationships (P<0.01) between CIPN severity and gait speed, Physical Performance Battery score, self-reported physical functioning, and self-reported disability.
The team also compared measures of physical functioning in the women with CIPN to measures in women without CIPN (n=274). This analysis was adjusted for cancer type and time since diagnosis.
There was a significant difference (P<0.01) between the groups in one measure of lower-extremity fitness but not another. Namely, it took CIPN-positive women significantly longer to rise out of a chair (tested 5 times each). But women in both groups fared similarly on a test measuring maximal leg press strength.
The investigators also tested the women on mobility and physical functioning. The CIPN-positive women fared significantly worse than CIPN-negative women (P<0.01) when it came to walking speed, step number, stride length, percentage of gait cycle in double support, and Physical Performance Battery score. However, there was no significant difference between the groups with regard to base of support.
Finally, CIPN-positive women were significantly more likely than CIPN-negative women to report poor physical function and disability (P<0.01 for both). And CIPN-positive women had a higher rate of falls in the last year (P<0.01).
The investigators said women with CIPN have specific underlying impairments that put them at risk for falls, which may be different from the impairments that occur with other conditions or old age.
For example, CIPN does not cause muscle weakness, but it has a distinct effect on movement and gait patterns.
The team noted that the women with CIPN had difficulty rising from a chair, possibly because their brains do not get enough information from their feet about how quickly or forcefully to stand up.
Based on these findings, the investigators argued that commonly recommended exercise, such as walking, may be safer for women with CIPN when done on a treadmill with handrails because their altered gait puts them at an increased risk of falling.
The team also said that machine-based resistance training may not be beneficial because neuropathy does not appear to decrease leg strength. Instead, rehabilitation efforts should focus on improving balance during upright movement and specific gait training.
Furthermore, the investigators believe that, if the symptoms of CIPN are detected early, cancer treatments could potentially be changed to prevent these debilitating problems or early rehabilitation interventions could be started.
In addition, Dr Winters-Stone and her research team are developing a smartphone-driven device that patients can use to detect and quantify symptoms of neuropathy, such as gait and balance impairments. ![]()
*Data in the abstract differ from the presentation.

Photo courtesy of NIH
SAN FRANCISCO—A study of female cancer survivors indicates that many still have chemotherapy-induced peripheral neuropathy (CIPN) symptoms years after completing cancer treatment.
In addition, CIPN was associated with worse physical functioning, poorer mobility, and a higher risk of falls.
Although more research is needed, investigators believe these findings may inform rehabilitation and fall prevention interventions for people with CIPN.
The findings were presented at the 2016 Cancer Survivorship Symposium (abstract 130*).
“We can’t dismiss neuropathy as a treatment side effect that goes away because symptoms persist for years in nearly half of women,” said Kerri M. Winters-Stone, PhD, of Oregon Health and Science University in Portland.
“While there are no effective treatments for this side effect, rehabilitative exercise programs may preserve physical functioning and mobility in the presence of neuropathy to help prevent falls and resulting injuries.”
For this study, Dr Winters-Stone and her colleagues assessed data from 512 women enrolled in exercise intervention trials designed to address fractures and falls in female cancer survivors. Most of the women had breast cancer, but there were also cases of lung, colorectal, ovarian, and hematologic cancers.
At an average of 6 years post-cancer diagnosis, 46% of the women (n=238) still reported some symptoms of CIPN, such as loss of feeling in their hands and feet.
The investigators noted significant relationships (P<0.01) between CIPN severity and gait speed, Physical Performance Battery score, self-reported physical functioning, and self-reported disability.
The team also compared measures of physical functioning in the women with CIPN to measures in women without CIPN (n=274). This analysis was adjusted for cancer type and time since diagnosis.
There was a significant difference (P<0.01) between the groups in one measure of lower-extremity fitness but not another. Namely, it took CIPN-positive women significantly longer to rise out of a chair (tested 5 times each). But women in both groups fared similarly on a test measuring maximal leg press strength.
The investigators also tested the women on mobility and physical functioning. The CIPN-positive women fared significantly worse than CIPN-negative women (P<0.01) when it came to walking speed, step number, stride length, percentage of gait cycle in double support, and Physical Performance Battery score. However, there was no significant difference between the groups with regard to base of support.
Finally, CIPN-positive women were significantly more likely than CIPN-negative women to report poor physical function and disability (P<0.01 for both). And CIPN-positive women had a higher rate of falls in the last year (P<0.01).
The investigators said women with CIPN have specific underlying impairments that put them at risk for falls, which may be different from the impairments that occur with other conditions or old age.
For example, CIPN does not cause muscle weakness, but it has a distinct effect on movement and gait patterns.
The team noted that the women with CIPN had difficulty rising from a chair, possibly because their brains do not get enough information from their feet about how quickly or forcefully to stand up.
Based on these findings, the investigators argued that commonly recommended exercise, such as walking, may be safer for women with CIPN when done on a treadmill with handrails because their altered gait puts them at an increased risk of falling.
The team also said that machine-based resistance training may not be beneficial because neuropathy does not appear to decrease leg strength. Instead, rehabilitation efforts should focus on improving balance during upright movement and specific gait training.
Furthermore, the investigators believe that, if the symptoms of CIPN are detected early, cancer treatments could potentially be changed to prevent these debilitating problems or early rehabilitation interventions could be started.
In addition, Dr Winters-Stone and her research team are developing a smartphone-driven device that patients can use to detect and quantify symptoms of neuropathy, such as gait and balance impairments. ![]()
*Data in the abstract differ from the presentation.
How malaria fools the immune system

infecting a red blood cell
Image courtesy of St. Jude
Children’s Research Hospital
Researchers have reconstructed how malaria parasite proteins bind to the antibodies that act as the first line of defense against the parasite.
The team described the binding of immunoglobulin M (IgM) to Plasmodium falciparum erythrocyte membrane protein-1 (PfEMP1).
They said their findings, published in Cell Reports, may provide valuable knowledge for the design of antimalarial drugs.
One strategy the malaria parasite Plasmodium falciparum uses to amplify its probability of spreading is the formation of rosette-shaped clusters of uninfected red blood cells (RBCs) surrounding a malaria-infected RBC.
Since the parasite in the central cell of the rosette can easily infect the surrounding cells, the rosette enhances the infection. Rosetting is associated with severe malaria and high fever.
One of the key players in the formation of the rosette is PfEMP1. PfEMP1 sticks out of the infected RBC and deceives one of the first defenses against malaria—IgM antibodies.
IgMs bind to the parasite or parasite-infected cells and call other immune molecules, like the complement system, for backup.
With the current study, researchers have shown that IgMs bind 1 or 2 PfEMP1 proteins, forming a bouquet-type shape on the surface of the infected cells.
Plasmodium falciparum exploits these IgMs to its own advantage because the bouquet attracts more RBCs, facilitating the formation of rosettes. Moreover, the IgMs in the bouquet are not able to bind the complement system and destroy the infected cell.
“The bond between PfEMP1s and IgMs is like the perfect Velcro—not too loose, not too strong,” said Ulf Skoglund, PhD, of Okinawa Institute for Science and Technology Graduate University in Japan.
“It is devilishly engineered to fool our immune system.”
The technique Dr Skoglund and his colleagues used to assess this bond allowed them to have a unique view of the proteins’ conformation.
“We have seen that PfEMP1 is a stiff, C-shaped protein,” he said. “Being stiff is an advantage. If it was floppy, it would not work so well. IgM, instead, assume 3 conformations: extended, bell, and turtle shape.”
Dr Skoglund and his colleagues believe that having this 3D structural model of the PfEMP1 and IgM complex can help scientists design antimalarial treatments that can break down or wash out malaria rosettes without hurting the patient. ![]()

infecting a red blood cell
Image courtesy of St. Jude
Children’s Research Hospital
Researchers have reconstructed how malaria parasite proteins bind to the antibodies that act as the first line of defense against the parasite.
The team described the binding of immunoglobulin M (IgM) to Plasmodium falciparum erythrocyte membrane protein-1 (PfEMP1).
They said their findings, published in Cell Reports, may provide valuable knowledge for the design of antimalarial drugs.
One strategy the malaria parasite Plasmodium falciparum uses to amplify its probability of spreading is the formation of rosette-shaped clusters of uninfected red blood cells (RBCs) surrounding a malaria-infected RBC.
Since the parasite in the central cell of the rosette can easily infect the surrounding cells, the rosette enhances the infection. Rosetting is associated with severe malaria and high fever.
One of the key players in the formation of the rosette is PfEMP1. PfEMP1 sticks out of the infected RBC and deceives one of the first defenses against malaria—IgM antibodies.
IgMs bind to the parasite or parasite-infected cells and call other immune molecules, like the complement system, for backup.
With the current study, researchers have shown that IgMs bind 1 or 2 PfEMP1 proteins, forming a bouquet-type shape on the surface of the infected cells.
Plasmodium falciparum exploits these IgMs to its own advantage because the bouquet attracts more RBCs, facilitating the formation of rosettes. Moreover, the IgMs in the bouquet are not able to bind the complement system and destroy the infected cell.
“The bond between PfEMP1s and IgMs is like the perfect Velcro—not too loose, not too strong,” said Ulf Skoglund, PhD, of Okinawa Institute for Science and Technology Graduate University in Japan.
“It is devilishly engineered to fool our immune system.”
The technique Dr Skoglund and his colleagues used to assess this bond allowed them to have a unique view of the proteins’ conformation.
“We have seen that PfEMP1 is a stiff, C-shaped protein,” he said. “Being stiff is an advantage. If it was floppy, it would not work so well. IgM, instead, assume 3 conformations: extended, bell, and turtle shape.”
Dr Skoglund and his colleagues believe that having this 3D structural model of the PfEMP1 and IgM complex can help scientists design antimalarial treatments that can break down or wash out malaria rosettes without hurting the patient. ![]()

infecting a red blood cell
Image courtesy of St. Jude
Children’s Research Hospital
Researchers have reconstructed how malaria parasite proteins bind to the antibodies that act as the first line of defense against the parasite.
The team described the binding of immunoglobulin M (IgM) to Plasmodium falciparum erythrocyte membrane protein-1 (PfEMP1).
They said their findings, published in Cell Reports, may provide valuable knowledge for the design of antimalarial drugs.
One strategy the malaria parasite Plasmodium falciparum uses to amplify its probability of spreading is the formation of rosette-shaped clusters of uninfected red blood cells (RBCs) surrounding a malaria-infected RBC.
Since the parasite in the central cell of the rosette can easily infect the surrounding cells, the rosette enhances the infection. Rosetting is associated with severe malaria and high fever.
One of the key players in the formation of the rosette is PfEMP1. PfEMP1 sticks out of the infected RBC and deceives one of the first defenses against malaria—IgM antibodies.
IgMs bind to the parasite or parasite-infected cells and call other immune molecules, like the complement system, for backup.
With the current study, researchers have shown that IgMs bind 1 or 2 PfEMP1 proteins, forming a bouquet-type shape on the surface of the infected cells.
Plasmodium falciparum exploits these IgMs to its own advantage because the bouquet attracts more RBCs, facilitating the formation of rosettes. Moreover, the IgMs in the bouquet are not able to bind the complement system and destroy the infected cell.
“The bond between PfEMP1s and IgMs is like the perfect Velcro—not too loose, not too strong,” said Ulf Skoglund, PhD, of Okinawa Institute for Science and Technology Graduate University in Japan.
“It is devilishly engineered to fool our immune system.”
The technique Dr Skoglund and his colleagues used to assess this bond allowed them to have a unique view of the proteins’ conformation.
“We have seen that PfEMP1 is a stiff, C-shaped protein,” he said. “Being stiff is an advantage. If it was floppy, it would not work so well. IgM, instead, assume 3 conformations: extended, bell, and turtle shape.”
Dr Skoglund and his colleagues believe that having this 3D structural model of the PfEMP1 and IgM complex can help scientists design antimalarial treatments that can break down or wash out malaria rosettes without hurting the patient. ![]()
Monitoring drug release with nanoparticles

Image courtesy of PNAS
Researchers say they have devised a system that allows for real-time monitoring of drug release.
The team created a luminescent nanoparticle and attached it to the anticancer drug doxorubicin, which allowed them to visualize the drug’s arrival in cancer cells.
Thus far, the team has only tested this system in vitro, but animal studies are currently underway.
“We really want to see what’s going on when we give chemo drugs, and this work paves the way for the exciting endeavor,” said Mingjun Zhang, PhD, of The Ohio State University in Columbus.
He and his colleagues described their work in Nature Nanotechnology.
The researchers noted that peptide nanoparticles with fluorescence properties are highly sought after because they are biodegradable and considered safe. However, peptides have limited intrinsic optical properties and therefore don’t make effective imaging probes.
In an attempt to overcome the imaging problem without compromising safety, the researchers created tryptophan–phenylalanine dipeptide nanoparticles (DNPs).
“Composed of natural amino acids, the nanoparticle is inherently biocompatible,” Dr Zhang said. “Our biological machines can easily take care of it.”
In addition, the DNPs proved photostable and could maintain their luminescence for extended periods of time.
To test the imaging capabilities of the DNPs, the researchers modified the nanoparticles with MUC1 aptamers so they would recognize the overexpressed MUC1 proteins on A549 human carcinoma epithelial cells.
Experiments showed these DNP/aptamer conjugates could effectively target and light up the cancer cells.
The researchers then tested the DNPs’ ability to monitor drug release by hitching the nanoparticles to doxorubicin. In experiments with A549 cells, the team was able to visualize the doxorubicin inside the cells.
Dr Zhang and his colleagues said the DNPs could be effective with other drugs as well. In fact, the team hopes this method might one day provide patients and their doctors with information on how well and how quickly a medication is working. ![]()

Image courtesy of PNAS
Researchers say they have devised a system that allows for real-time monitoring of drug release.
The team created a luminescent nanoparticle and attached it to the anticancer drug doxorubicin, which allowed them to visualize the drug’s arrival in cancer cells.
Thus far, the team has only tested this system in vitro, but animal studies are currently underway.
“We really want to see what’s going on when we give chemo drugs, and this work paves the way for the exciting endeavor,” said Mingjun Zhang, PhD, of The Ohio State University in Columbus.
He and his colleagues described their work in Nature Nanotechnology.
The researchers noted that peptide nanoparticles with fluorescence properties are highly sought after because they are biodegradable and considered safe. However, peptides have limited intrinsic optical properties and therefore don’t make effective imaging probes.
In an attempt to overcome the imaging problem without compromising safety, the researchers created tryptophan–phenylalanine dipeptide nanoparticles (DNPs).
“Composed of natural amino acids, the nanoparticle is inherently biocompatible,” Dr Zhang said. “Our biological machines can easily take care of it.”
In addition, the DNPs proved photostable and could maintain their luminescence for extended periods of time.
To test the imaging capabilities of the DNPs, the researchers modified the nanoparticles with MUC1 aptamers so they would recognize the overexpressed MUC1 proteins on A549 human carcinoma epithelial cells.
Experiments showed these DNP/aptamer conjugates could effectively target and light up the cancer cells.
The researchers then tested the DNPs’ ability to monitor drug release by hitching the nanoparticles to doxorubicin. In experiments with A549 cells, the team was able to visualize the doxorubicin inside the cells.
Dr Zhang and his colleagues said the DNPs could be effective with other drugs as well. In fact, the team hopes this method might one day provide patients and their doctors with information on how well and how quickly a medication is working. ![]()

Image courtesy of PNAS
Researchers say they have devised a system that allows for real-time monitoring of drug release.
The team created a luminescent nanoparticle and attached it to the anticancer drug doxorubicin, which allowed them to visualize the drug’s arrival in cancer cells.
Thus far, the team has only tested this system in vitro, but animal studies are currently underway.
“We really want to see what’s going on when we give chemo drugs, and this work paves the way for the exciting endeavor,” said Mingjun Zhang, PhD, of The Ohio State University in Columbus.
He and his colleagues described their work in Nature Nanotechnology.
The researchers noted that peptide nanoparticles with fluorescence properties are highly sought after because they are biodegradable and considered safe. However, peptides have limited intrinsic optical properties and therefore don’t make effective imaging probes.
In an attempt to overcome the imaging problem without compromising safety, the researchers created tryptophan–phenylalanine dipeptide nanoparticles (DNPs).
“Composed of natural amino acids, the nanoparticle is inherently biocompatible,” Dr Zhang said. “Our biological machines can easily take care of it.”
In addition, the DNPs proved photostable and could maintain their luminescence for extended periods of time.
To test the imaging capabilities of the DNPs, the researchers modified the nanoparticles with MUC1 aptamers so they would recognize the overexpressed MUC1 proteins on A549 human carcinoma epithelial cells.
Experiments showed these DNP/aptamer conjugates could effectively target and light up the cancer cells.
The researchers then tested the DNPs’ ability to monitor drug release by hitching the nanoparticles to doxorubicin. In experiments with A549 cells, the team was able to visualize the doxorubicin inside the cells.
Dr Zhang and his colleagues said the DNPs could be effective with other drugs as well. In fact, the team hopes this method might one day provide patients and their doctors with information on how well and how quickly a medication is working. ![]()
NICE releases guideline on sepsis

Photo courtesy of the CDC
The National Institute for Health and Care Excellence (NICE) has published a new draft guideline to help healthcare professionals recognize sepsis and provide early treatment.
Although treatable in many cases, sepsis can be difficult to recognize and diagnose.
A recent study* of more than 3000 patients treated at UK hospitals revealed delays in identifying sepsis in more than a third of cases.
“There are around 123,000 cases of sepsis in England every year, and, unfortunately, thousands of people die after developing the condition,” said Mark Baker, director of the centre for clinical practice at NICE.
“Many of these deaths might be prevented if sepsis was recognized quickly and treatment started early. We know that when hospitals are well-prepared, clinicians do better at responding to patients with sepsis. However, recent reports have revealed that a third of hospitals have no formal protocols for recognizing and responding to sepsis.”
NICE created its draft guidance with that in mind. The guidance provides recommendations to aid in the recognition, diagnosis, and early management of sepsis, including:
- What signs and symptoms to look out for
- How to identify patients at high risk of developing sepsis
- Which tests to use to diagnose and monitor patients
- How to care for people with suspected sepsis outside of the hospital
- When patients should be referred for emergency care
- Appropriate use of antibiotics and other supportive treatments, such as fluids and oxygen
- The type of information that should be given to patients, families, and caregivers.
“We want all healthcare professionals to see sepsis as an immediate, life-threatening condition and make sure there are systems in place across the NHS for it to be recognized and treated as an emergency,” Baker said.
“This new guideline will be the first to provide evidence-based best practice advice on how to quickly identify and treat people with sepsis. We now urge all healthcare professionals and organizations with an interest in this area to comment on the proposed recommendations.”
The draft version of this guideline has been published for consultation. Organizations can register as a stakeholder on the NICE website and have until February 22, 2016, to submit their comments. Individuals are advised to pass comments through a registered stakeholder organization that most closely represents them. ![]()
*Published in “Just Say Sepsis!”—a report by the National Confidential Enquiry into Patient Outcome and Death.

Photo courtesy of the CDC
The National Institute for Health and Care Excellence (NICE) has published a new draft guideline to help healthcare professionals recognize sepsis and provide early treatment.
Although treatable in many cases, sepsis can be difficult to recognize and diagnose.
A recent study* of more than 3000 patients treated at UK hospitals revealed delays in identifying sepsis in more than a third of cases.
“There are around 123,000 cases of sepsis in England every year, and, unfortunately, thousands of people die after developing the condition,” said Mark Baker, director of the centre for clinical practice at NICE.
“Many of these deaths might be prevented if sepsis was recognized quickly and treatment started early. We know that when hospitals are well-prepared, clinicians do better at responding to patients with sepsis. However, recent reports have revealed that a third of hospitals have no formal protocols for recognizing and responding to sepsis.”
NICE created its draft guidance with that in mind. The guidance provides recommendations to aid in the recognition, diagnosis, and early management of sepsis, including:
- What signs and symptoms to look out for
- How to identify patients at high risk of developing sepsis
- Which tests to use to diagnose and monitor patients
- How to care for people with suspected sepsis outside of the hospital
- When patients should be referred for emergency care
- Appropriate use of antibiotics and other supportive treatments, such as fluids and oxygen
- The type of information that should be given to patients, families, and caregivers.
“We want all healthcare professionals to see sepsis as an immediate, life-threatening condition and make sure there are systems in place across the NHS for it to be recognized and treated as an emergency,” Baker said.
“This new guideline will be the first to provide evidence-based best practice advice on how to quickly identify and treat people with sepsis. We now urge all healthcare professionals and organizations with an interest in this area to comment on the proposed recommendations.”
The draft version of this guideline has been published for consultation. Organizations can register as a stakeholder on the NICE website and have until February 22, 2016, to submit their comments. Individuals are advised to pass comments through a registered stakeholder organization that most closely represents them. ![]()
*Published in “Just Say Sepsis!”—a report by the National Confidential Enquiry into Patient Outcome and Death.

Photo courtesy of the CDC
The National Institute for Health and Care Excellence (NICE) has published a new draft guideline to help healthcare professionals recognize sepsis and provide early treatment.
Although treatable in many cases, sepsis can be difficult to recognize and diagnose.
A recent study* of more than 3000 patients treated at UK hospitals revealed delays in identifying sepsis in more than a third of cases.
“There are around 123,000 cases of sepsis in England every year, and, unfortunately, thousands of people die after developing the condition,” said Mark Baker, director of the centre for clinical practice at NICE.
“Many of these deaths might be prevented if sepsis was recognized quickly and treatment started early. We know that when hospitals are well-prepared, clinicians do better at responding to patients with sepsis. However, recent reports have revealed that a third of hospitals have no formal protocols for recognizing and responding to sepsis.”
NICE created its draft guidance with that in mind. The guidance provides recommendations to aid in the recognition, diagnosis, and early management of sepsis, including:
- What signs and symptoms to look out for
- How to identify patients at high risk of developing sepsis
- Which tests to use to diagnose and monitor patients
- How to care for people with suspected sepsis outside of the hospital
- When patients should be referred for emergency care
- Appropriate use of antibiotics and other supportive treatments, such as fluids and oxygen
- The type of information that should be given to patients, families, and caregivers.
“We want all healthcare professionals to see sepsis as an immediate, life-threatening condition and make sure there are systems in place across the NHS for it to be recognized and treated as an emergency,” Baker said.
“This new guideline will be the first to provide evidence-based best practice advice on how to quickly identify and treat people with sepsis. We now urge all healthcare professionals and organizations with an interest in this area to comment on the proposed recommendations.”
The draft version of this guideline has been published for consultation. Organizations can register as a stakeholder on the NICE website and have until February 22, 2016, to submit their comments. Individuals are advised to pass comments through a registered stakeholder organization that most closely represents them. ![]()
*Published in “Just Say Sepsis!”—a report by the National Confidential Enquiry into Patient Outcome and Death.
A new tool for studying sepsis

Photo by Ingela Björck
Researchers have reported using mass spectrometry to measure hundreds of proteins in a single blood sample.
And they used the resulting protein patterns to determine the severity of sepsis in animal models. They were also able to determine which organs had been damaged in these mice.
The researchers said they’ve been able to map the majority of proteins found in vital organs and list which proteins are specific to each organ.
“If you see in a blood sample that the amount of proteins from a specific organ increases, it indicates damage to this organ,” explained study author Erik Malmström, of Lund University in Sweden.
“The method provides an understanding of the molecular events that take place during the course of a disease and the possibility, using the same analysis, to study how different organs are affected.”
The researchers described this work in Nature Communications.
The group believes their study of hundreds of different proteins could eventually be used to select other important proteins that can serve as biomarkers for different aspects of sepsis.
First and foremost, however, they think their method will be an important research tool.
“There is so much we don’t know about sepsis,” Malmström said. “Why do not all patients react the same way? Why do some organs suffer the most damage in some patients and not in others? Do different bacteria cause the disease to progress? Can you divide patients into different subgroups, or bacteria, or does each new combination of patients and bacteria lead to a specific form of sepsis?”
The current study was conducted in animals, but the researchers are now moving on to human tissue. They have obtained samples of healthy tissue from various organs and are comparing protein patterns of these samples with patterns in corresponding tissues from sepsis patients. ![]()

Photo by Ingela Björck
Researchers have reported using mass spectrometry to measure hundreds of proteins in a single blood sample.
And they used the resulting protein patterns to determine the severity of sepsis in animal models. They were also able to determine which organs had been damaged in these mice.
The researchers said they’ve been able to map the majority of proteins found in vital organs and list which proteins are specific to each organ.
“If you see in a blood sample that the amount of proteins from a specific organ increases, it indicates damage to this organ,” explained study author Erik Malmström, of Lund University in Sweden.
“The method provides an understanding of the molecular events that take place during the course of a disease and the possibility, using the same analysis, to study how different organs are affected.”
The researchers described this work in Nature Communications.
The group believes their study of hundreds of different proteins could eventually be used to select other important proteins that can serve as biomarkers for different aspects of sepsis.
First and foremost, however, they think their method will be an important research tool.
“There is so much we don’t know about sepsis,” Malmström said. “Why do not all patients react the same way? Why do some organs suffer the most damage in some patients and not in others? Do different bacteria cause the disease to progress? Can you divide patients into different subgroups, or bacteria, or does each new combination of patients and bacteria lead to a specific form of sepsis?”
The current study was conducted in animals, but the researchers are now moving on to human tissue. They have obtained samples of healthy tissue from various organs and are comparing protein patterns of these samples with patterns in corresponding tissues from sepsis patients. ![]()

Photo by Ingela Björck
Researchers have reported using mass spectrometry to measure hundreds of proteins in a single blood sample.
And they used the resulting protein patterns to determine the severity of sepsis in animal models. They were also able to determine which organs had been damaged in these mice.
The researchers said they’ve been able to map the majority of proteins found in vital organs and list which proteins are specific to each organ.
“If you see in a blood sample that the amount of proteins from a specific organ increases, it indicates damage to this organ,” explained study author Erik Malmström, of Lund University in Sweden.
“The method provides an understanding of the molecular events that take place during the course of a disease and the possibility, using the same analysis, to study how different organs are affected.”
The researchers described this work in Nature Communications.
The group believes their study of hundreds of different proteins could eventually be used to select other important proteins that can serve as biomarkers for different aspects of sepsis.
First and foremost, however, they think their method will be an important research tool.
“There is so much we don’t know about sepsis,” Malmström said. “Why do not all patients react the same way? Why do some organs suffer the most damage in some patients and not in others? Do different bacteria cause the disease to progress? Can you divide patients into different subgroups, or bacteria, or does each new combination of patients and bacteria lead to a specific form of sepsis?”
The current study was conducted in animals, but the researchers are now moving on to human tissue. They have obtained samples of healthy tissue from various organs and are comparing protein patterns of these samples with patterns in corresponding tissues from sepsis patients. ![]()
Fewer doses of malaria drug just as effective

Photo by Sarah Mattison
A trial of African children suggests that 3 doses of artesunate can be just as effective as 5 doses for treating severe malaria.
A 3-dose intramuscular (IM) artesunate regimen proved noninferior to 5 doses of IM artesunate.
However, a 3-dose intravenous (IV) artesunate regimen was not as effective.
Peter Kremsner, MD, of Eberhard Karls Universität Tübingen in Germany, and his colleagues reported these results in PLOS Medicine.
The World Health Organization recommends that patients with severe malaria be given a 5-dose regimen of IV or IM artesunate at the time of admission (0 hours) and at 12, 24, 48, and 72 hours. However, in resource-limited settings, administering 5 doses on schedule can be challenging.
So Dr Kremsner and his colleagues wanted to determine if 3 doses of artesunate would be just as effective. They conducted an open-label, randomized, controlled trial investigating the efficacy of 3-dose IV or IM artesunate at 0, 24, and 48 hours.
The researchers enrolled 1047 children (0.5 to 10 years of age) who had severe malaria and were treated at 7 different sites in 5 African countries. The children were randomized to receive a total artesunate dose of 12 mg/kg as a control regimen of 5 IM injections (n=348) or 3 injections of 4 mg/kg either IM (n=348) or IV (n=351).
Of these children, 1002 received treatment per-protocol—331 in the 5-dose group, 338 in the 3-dose IM group, and 333 in the 3-dose IV group.
Seventy-eight percent of patients in the 3-dose IM group had about 99% parasite clearance at 24 hours, as did 79% of patients in the 5-dose IM group, a result that met a preset criterion for noninferiority (P=0.02).
However, the 3-dose IV regimen did not meet the noninferiority criterion. Seventy-four percent of these children had about 99% parasite clearance at 24 hours (P=0.24).
Twenty-two percent of the entire study population developed delayed anemia, but there was no difference in the incidence of this adverse event between the treatment arms.
The researchers said further studies are needed to clarify whether treatment with artesunate or the malaria infection itself was responsible for the delayed anemia. And patients receiving the drug should be monitored for this complication.
The team also said their findings suggest a 3-dose IM artesunate regimen can be effective against severe malaria in children, but this study did have limitations. For instance, due to practical constraints, the primary endpoint was parasite clearance at 24 hours rather than survival. ![]()

Photo by Sarah Mattison
A trial of African children suggests that 3 doses of artesunate can be just as effective as 5 doses for treating severe malaria.
A 3-dose intramuscular (IM) artesunate regimen proved noninferior to 5 doses of IM artesunate.
However, a 3-dose intravenous (IV) artesunate regimen was not as effective.
Peter Kremsner, MD, of Eberhard Karls Universität Tübingen in Germany, and his colleagues reported these results in PLOS Medicine.
The World Health Organization recommends that patients with severe malaria be given a 5-dose regimen of IV or IM artesunate at the time of admission (0 hours) and at 12, 24, 48, and 72 hours. However, in resource-limited settings, administering 5 doses on schedule can be challenging.
So Dr Kremsner and his colleagues wanted to determine if 3 doses of artesunate would be just as effective. They conducted an open-label, randomized, controlled trial investigating the efficacy of 3-dose IV or IM artesunate at 0, 24, and 48 hours.
The researchers enrolled 1047 children (0.5 to 10 years of age) who had severe malaria and were treated at 7 different sites in 5 African countries. The children were randomized to receive a total artesunate dose of 12 mg/kg as a control regimen of 5 IM injections (n=348) or 3 injections of 4 mg/kg either IM (n=348) or IV (n=351).
Of these children, 1002 received treatment per-protocol—331 in the 5-dose group, 338 in the 3-dose IM group, and 333 in the 3-dose IV group.
Seventy-eight percent of patients in the 3-dose IM group had about 99% parasite clearance at 24 hours, as did 79% of patients in the 5-dose IM group, a result that met a preset criterion for noninferiority (P=0.02).
However, the 3-dose IV regimen did not meet the noninferiority criterion. Seventy-four percent of these children had about 99% parasite clearance at 24 hours (P=0.24).
Twenty-two percent of the entire study population developed delayed anemia, but there was no difference in the incidence of this adverse event between the treatment arms.
The researchers said further studies are needed to clarify whether treatment with artesunate or the malaria infection itself was responsible for the delayed anemia. And patients receiving the drug should be monitored for this complication.
The team also said their findings suggest a 3-dose IM artesunate regimen can be effective against severe malaria in children, but this study did have limitations. For instance, due to practical constraints, the primary endpoint was parasite clearance at 24 hours rather than survival. ![]()

Photo by Sarah Mattison
A trial of African children suggests that 3 doses of artesunate can be just as effective as 5 doses for treating severe malaria.
A 3-dose intramuscular (IM) artesunate regimen proved noninferior to 5 doses of IM artesunate.
However, a 3-dose intravenous (IV) artesunate regimen was not as effective.
Peter Kremsner, MD, of Eberhard Karls Universität Tübingen in Germany, and his colleagues reported these results in PLOS Medicine.
The World Health Organization recommends that patients with severe malaria be given a 5-dose regimen of IV or IM artesunate at the time of admission (0 hours) and at 12, 24, 48, and 72 hours. However, in resource-limited settings, administering 5 doses on schedule can be challenging.
So Dr Kremsner and his colleagues wanted to determine if 3 doses of artesunate would be just as effective. They conducted an open-label, randomized, controlled trial investigating the efficacy of 3-dose IV or IM artesunate at 0, 24, and 48 hours.
The researchers enrolled 1047 children (0.5 to 10 years of age) who had severe malaria and were treated at 7 different sites in 5 African countries. The children were randomized to receive a total artesunate dose of 12 mg/kg as a control regimen of 5 IM injections (n=348) or 3 injections of 4 mg/kg either IM (n=348) or IV (n=351).
Of these children, 1002 received treatment per-protocol—331 in the 5-dose group, 338 in the 3-dose IM group, and 333 in the 3-dose IV group.
Seventy-eight percent of patients in the 3-dose IM group had about 99% parasite clearance at 24 hours, as did 79% of patients in the 5-dose IM group, a result that met a preset criterion for noninferiority (P=0.02).
However, the 3-dose IV regimen did not meet the noninferiority criterion. Seventy-four percent of these children had about 99% parasite clearance at 24 hours (P=0.24).
Twenty-two percent of the entire study population developed delayed anemia, but there was no difference in the incidence of this adverse event between the treatment arms.
The researchers said further studies are needed to clarify whether treatment with artesunate or the malaria infection itself was responsible for the delayed anemia. And patients receiving the drug should be monitored for this complication.
The team also said their findings suggest a 3-dose IM artesunate regimen can be effective against severe malaria in children, but this study did have limitations. For instance, due to practical constraints, the primary endpoint was parasite clearance at 24 hours rather than survival. ![]()
Microcapsules could provide targeted drug delivery
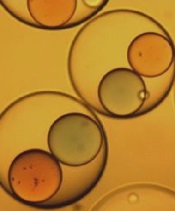
Image courtesy of Ronald Xu
& The Ohio State University
Researchers say they have developed a quick and controllable method for getting 2 or more ingredients into the same tiny drug capsule and having them mix only when triggered by a signal like vibrations or heat.
This work was inspired by the search for targeted drug delivery options to treat cancers.
The idea with this multi-ingredient capsule is that the ingredients must be mixed for the drug to work, and the mixing could be triggered in targeted areas of the body, thereby boosting drug efficiency while reducing side effects.
While the researchers found they could use their technique to create multi-ingredient microcapsules, they have not yet used it to encapsulate cancer treatments.
They described their work in Applied Physics Letters.
“One of the limitations of chemotherapy is that less than 5% of the drugs typically get to the tumor, while the rest can be absorbed by other organs,” said study author Ronald Xu, PhD, of The Ohio State University in Columbus.
He and his colleagues thought one possible way to address this problem could be to make the drugs non-toxic when injected into the body and trigger mixing that would produce a toxic product only near the tumor site.
The researchers knew that, for such drugs to work on a large scale, there must be a way to quickly, controllably, and cost-effectively produce capsules with 2 or more active ingredients. If the drugs are to be injected and spread through the body via the bloodstream, the capsules should also be small.
With that in mind, Dr Xu and his colleagues developed a device that can produce tiny capsules approximately 100 microns across with multiple inner ingredients.
The device works by funneling different ingredients through 2 inner needles. These needles run parallel to each other and are both enclosed in a larger outer needle, which contains an ingredient for making the outer shell of the capsule.
As all the ingredients exit the needles through a single nozzle, a high-speed gas forces the liquids into a narrow stream that breaks into individual droplets. An electric field stabilizes the flow so that uniform droplets are created.
Depending on the relative flow rates, each droplet may contain 2 or more smaller inner droplets made from the ingredients in the inner needles.
The researchers tested their device with colored paraffin wax—red in one needle and blue in the other. The outer shell was made from sodium alginate, a material extracted from seaweed that turned gelatinous when the droplets fell into a calcium chloride solution.
Depending on the experimental conditions, the team was able to produce between 1000 and 100,000 capsules per second, and nearly 100% of the inner liquids were incorporated into the capsules without any waste.
Once encapsulated, the 2 colors of wax did not mix because of surface tension. But the researchers found they could force the red and blue wax to merge by vibrating the capsules. The team also discovered they could release the inner droplets by dissolving the outer shell.
The key features of the new device are its high efficiency and yield, and the fact that the size of the droplets can be uniformly controlled, Dr Xu said.
He added that, by further fine-tuning the device’s operation, the team could make capsules that are 3-5 microns across, about the size of a red blood cell. The process can also be scaled up by building an array of nozzles and could be modified to encapsulate 3 or more active ingredients by adding additional inner needles.
While Dr Xu and his colleagues were motivated by drug delivery, they believe their device might also find wider use in a range of applications that require controlled reactions, such as regenerative medicine and nuclear and chemical engineering. ![]()
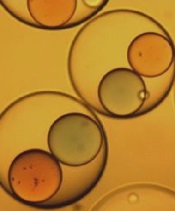
Image courtesy of Ronald Xu
& The Ohio State University
Researchers say they have developed a quick and controllable method for getting 2 or more ingredients into the same tiny drug capsule and having them mix only when triggered by a signal like vibrations or heat.
This work was inspired by the search for targeted drug delivery options to treat cancers.
The idea with this multi-ingredient capsule is that the ingredients must be mixed for the drug to work, and the mixing could be triggered in targeted areas of the body, thereby boosting drug efficiency while reducing side effects.
While the researchers found they could use their technique to create multi-ingredient microcapsules, they have not yet used it to encapsulate cancer treatments.
They described their work in Applied Physics Letters.
“One of the limitations of chemotherapy is that less than 5% of the drugs typically get to the tumor, while the rest can be absorbed by other organs,” said study author Ronald Xu, PhD, of The Ohio State University in Columbus.
He and his colleagues thought one possible way to address this problem could be to make the drugs non-toxic when injected into the body and trigger mixing that would produce a toxic product only near the tumor site.
The researchers knew that, for such drugs to work on a large scale, there must be a way to quickly, controllably, and cost-effectively produce capsules with 2 or more active ingredients. If the drugs are to be injected and spread through the body via the bloodstream, the capsules should also be small.
With that in mind, Dr Xu and his colleagues developed a device that can produce tiny capsules approximately 100 microns across with multiple inner ingredients.
The device works by funneling different ingredients through 2 inner needles. These needles run parallel to each other and are both enclosed in a larger outer needle, which contains an ingredient for making the outer shell of the capsule.
As all the ingredients exit the needles through a single nozzle, a high-speed gas forces the liquids into a narrow stream that breaks into individual droplets. An electric field stabilizes the flow so that uniform droplets are created.
Depending on the relative flow rates, each droplet may contain 2 or more smaller inner droplets made from the ingredients in the inner needles.
The researchers tested their device with colored paraffin wax—red in one needle and blue in the other. The outer shell was made from sodium alginate, a material extracted from seaweed that turned gelatinous when the droplets fell into a calcium chloride solution.
Depending on the experimental conditions, the team was able to produce between 1000 and 100,000 capsules per second, and nearly 100% of the inner liquids were incorporated into the capsules without any waste.
Once encapsulated, the 2 colors of wax did not mix because of surface tension. But the researchers found they could force the red and blue wax to merge by vibrating the capsules. The team also discovered they could release the inner droplets by dissolving the outer shell.
The key features of the new device are its high efficiency and yield, and the fact that the size of the droplets can be uniformly controlled, Dr Xu said.
He added that, by further fine-tuning the device’s operation, the team could make capsules that are 3-5 microns across, about the size of a red blood cell. The process can also be scaled up by building an array of nozzles and could be modified to encapsulate 3 or more active ingredients by adding additional inner needles.
While Dr Xu and his colleagues were motivated by drug delivery, they believe their device might also find wider use in a range of applications that require controlled reactions, such as regenerative medicine and nuclear and chemical engineering. ![]()
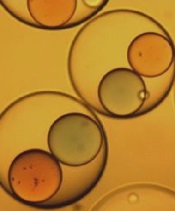
Image courtesy of Ronald Xu
& The Ohio State University
Researchers say they have developed a quick and controllable method for getting 2 or more ingredients into the same tiny drug capsule and having them mix only when triggered by a signal like vibrations or heat.
This work was inspired by the search for targeted drug delivery options to treat cancers.
The idea with this multi-ingredient capsule is that the ingredients must be mixed for the drug to work, and the mixing could be triggered in targeted areas of the body, thereby boosting drug efficiency while reducing side effects.
While the researchers found they could use their technique to create multi-ingredient microcapsules, they have not yet used it to encapsulate cancer treatments.
They described their work in Applied Physics Letters.
“One of the limitations of chemotherapy is that less than 5% of the drugs typically get to the tumor, while the rest can be absorbed by other organs,” said study author Ronald Xu, PhD, of The Ohio State University in Columbus.
He and his colleagues thought one possible way to address this problem could be to make the drugs non-toxic when injected into the body and trigger mixing that would produce a toxic product only near the tumor site.
The researchers knew that, for such drugs to work on a large scale, there must be a way to quickly, controllably, and cost-effectively produce capsules with 2 or more active ingredients. If the drugs are to be injected and spread through the body via the bloodstream, the capsules should also be small.
With that in mind, Dr Xu and his colleagues developed a device that can produce tiny capsules approximately 100 microns across with multiple inner ingredients.
The device works by funneling different ingredients through 2 inner needles. These needles run parallel to each other and are both enclosed in a larger outer needle, which contains an ingredient for making the outer shell of the capsule.
As all the ingredients exit the needles through a single nozzle, a high-speed gas forces the liquids into a narrow stream that breaks into individual droplets. An electric field stabilizes the flow so that uniform droplets are created.
Depending on the relative flow rates, each droplet may contain 2 or more smaller inner droplets made from the ingredients in the inner needles.
The researchers tested their device with colored paraffin wax—red in one needle and blue in the other. The outer shell was made from sodium alginate, a material extracted from seaweed that turned gelatinous when the droplets fell into a calcium chloride solution.
Depending on the experimental conditions, the team was able to produce between 1000 and 100,000 capsules per second, and nearly 100% of the inner liquids were incorporated into the capsules without any waste.
Once encapsulated, the 2 colors of wax did not mix because of surface tension. But the researchers found they could force the red and blue wax to merge by vibrating the capsules. The team also discovered they could release the inner droplets by dissolving the outer shell.
The key features of the new device are its high efficiency and yield, and the fact that the size of the droplets can be uniformly controlled, Dr Xu said.
He added that, by further fine-tuning the device’s operation, the team could make capsules that are 3-5 microns across, about the size of a red blood cell. The process can also be scaled up by building an array of nozzles and could be modified to encapsulate 3 or more active ingredients by adding additional inner needles.
While Dr Xu and his colleagues were motivated by drug delivery, they believe their device might also find wider use in a range of applications that require controlled reactions, such as regenerative medicine and nuclear and chemical engineering.
Study confirms resistant malaria in Cambodia

Image by Ute Frevert
and Margaret Shear
Results of a new study confirm that dihydroartemisinin-piperaquine, the first-line treatment for Plasmodium falciparum malaria infection in Cambodia, has failed in certain provinces due to parasite resistance to both artemisinin and piperaquine.
Dihydroartemisinin-piperaquine is an artemisinin combination therapy (ACT) that combines fast-acting artemisinin with a long-acting partner drug, piperaquine.
Resistance to artemisinin in parts of Southeast Asia is well-documented, but, until now, only a few studies have presented clear evidence of piperaquine resistance.
Additional results from this study suggest that artesunate, a form of artemisinin, plus mefloquine, a different long-acting partner drug, should be the first-line ACT in areas where dihydroartemisinin-piperaquine treatment has failed.
Chanaki Amaratunga, PhD, of the National Institute of Allergy and Infectious Diseases in Rockville, Maryland, and colleagues reported these results in The Lancet Infectious Diseases.
The researchers assessed the efficacy of dihydroartemisinin-piperaquine treatment in 241 malaria-afflicted participants ages 2 to 65. The subjects lived in 3 different Cambodian provinces with varying levels of artemisinin resistance.
After monitoring parasite levels in the blood for 63 days, the researchers found that parasites had reemerged despite initial clearance in 45.7% of participants in Pursat, 15.9% of participants in Preah Vihear, and 1.67% of participants in Ratanakiri.
The results indicate the ACT is failing in Pursat and Preah Vihear, where artemisinin resistance is common, but remains highly efficacious in Ratanakiri, where resistance is uncommon.
Laboratory tests showed the parasites from dihydroartemisinin-piperaquine failures contained a genetic marker of artemisinin resistance and had a decreased susceptibility to piperaquine, demonstrating that both artemisinin and piperaquine resistance contributed to treatment failures.
However, the parasites also showed an increased susceptibility to mefloquine and completely lacked the molecular marker for mefloquine resistance.
These findings informed new World Health Organization guidelines reinstating artesunate plus mefloquine as the first-line ACT in Cambodia where dihydroartemisinin-piperaquine treatment has failed.
The researchers said the findings also provide evidence to initiate surveillance programs to track the spread of piperaquine resistance and clinical trials to test alternative combination therapies.

Image by Ute Frevert
and Margaret Shear
Results of a new study confirm that dihydroartemisinin-piperaquine, the first-line treatment for Plasmodium falciparum malaria infection in Cambodia, has failed in certain provinces due to parasite resistance to both artemisinin and piperaquine.
Dihydroartemisinin-piperaquine is an artemisinin combination therapy (ACT) that combines fast-acting artemisinin with a long-acting partner drug, piperaquine.
Resistance to artemisinin in parts of Southeast Asia is well-documented, but, until now, only a few studies have presented clear evidence of piperaquine resistance.
Additional results from this study suggest that artesunate, a form of artemisinin, plus mefloquine, a different long-acting partner drug, should be the first-line ACT in areas where dihydroartemisinin-piperaquine treatment has failed.
Chanaki Amaratunga, PhD, of the National Institute of Allergy and Infectious Diseases in Rockville, Maryland, and colleagues reported these results in The Lancet Infectious Diseases.
The researchers assessed the efficacy of dihydroartemisinin-piperaquine treatment in 241 malaria-afflicted participants ages 2 to 65. The subjects lived in 3 different Cambodian provinces with varying levels of artemisinin resistance.
After monitoring parasite levels in the blood for 63 days, the researchers found that parasites had reemerged despite initial clearance in 45.7% of participants in Pursat, 15.9% of participants in Preah Vihear, and 1.67% of participants in Ratanakiri.
The results indicate the ACT is failing in Pursat and Preah Vihear, where artemisinin resistance is common, but remains highly efficacious in Ratanakiri, where resistance is uncommon.
Laboratory tests showed the parasites from dihydroartemisinin-piperaquine failures contained a genetic marker of artemisinin resistance and had a decreased susceptibility to piperaquine, demonstrating that both artemisinin and piperaquine resistance contributed to treatment failures.
However, the parasites also showed an increased susceptibility to mefloquine and completely lacked the molecular marker for mefloquine resistance.
These findings informed new World Health Organization guidelines reinstating artesunate plus mefloquine as the first-line ACT in Cambodia where dihydroartemisinin-piperaquine treatment has failed.
The researchers said the findings also provide evidence to initiate surveillance programs to track the spread of piperaquine resistance and clinical trials to test alternative combination therapies.

Image by Ute Frevert
and Margaret Shear
Results of a new study confirm that dihydroartemisinin-piperaquine, the first-line treatment for Plasmodium falciparum malaria infection in Cambodia, has failed in certain provinces due to parasite resistance to both artemisinin and piperaquine.
Dihydroartemisinin-piperaquine is an artemisinin combination therapy (ACT) that combines fast-acting artemisinin with a long-acting partner drug, piperaquine.
Resistance to artemisinin in parts of Southeast Asia is well-documented, but, until now, only a few studies have presented clear evidence of piperaquine resistance.
Additional results from this study suggest that artesunate, a form of artemisinin, plus mefloquine, a different long-acting partner drug, should be the first-line ACT in areas where dihydroartemisinin-piperaquine treatment has failed.
Chanaki Amaratunga, PhD, of the National Institute of Allergy and Infectious Diseases in Rockville, Maryland, and colleagues reported these results in The Lancet Infectious Diseases.
The researchers assessed the efficacy of dihydroartemisinin-piperaquine treatment in 241 malaria-afflicted participants ages 2 to 65. The subjects lived in 3 different Cambodian provinces with varying levels of artemisinin resistance.
After monitoring parasite levels in the blood for 63 days, the researchers found that parasites had reemerged despite initial clearance in 45.7% of participants in Pursat, 15.9% of participants in Preah Vihear, and 1.67% of participants in Ratanakiri.
The results indicate the ACT is failing in Pursat and Preah Vihear, where artemisinin resistance is common, but remains highly efficacious in Ratanakiri, where resistance is uncommon.
Laboratory tests showed the parasites from dihydroartemisinin-piperaquine failures contained a genetic marker of artemisinin resistance and had a decreased susceptibility to piperaquine, demonstrating that both artemisinin and piperaquine resistance contributed to treatment failures.
However, the parasites also showed an increased susceptibility to mefloquine and completely lacked the molecular marker for mefloquine resistance.
These findings informed new World Health Organization guidelines reinstating artesunate plus mefloquine as the first-line ACT in Cambodia where dihydroartemisinin-piperaquine treatment has failed.
The researchers said the findings also provide evidence to initiate surveillance programs to track the spread of piperaquine resistance and clinical trials to test alternative combination therapies.
Cutting costs for cancer pts with comorbidities

Photo courtesy of the CDC
Patients with incurable cancer and multiple comorbidities who consulted with a palliative care team within 2 days of hospitalization had significant savings in hospital costs, according to a new study.
The study also showed that the higher number of comorbidities a patient had, the greater the reduction in direct hospital costs with early palliative care as opposed to standard care.
Previous studies have shown a link between palliative care and lower costs, but this is the first to examine whether the effect of palliative care consultation varies by the number of co-existing chronic conditions.
“We already know that coordinated, patient-centered palliative care improves care quality, enhances survival, and reduces costs for persons with cancer,” said R. Sean Morrison, MD, of the Icahn School of Medicine at Mount Sinai in New York, New York.
“Our latest research now shows the strong association between cost and the number of co-occurring conditions. Among patients with advanced cancer and other serious illnesses, aggressive treatments are often inconsistent with patients’ wishes and are associated with worse quality of life compared to other treatments. It is imperative that policymakers act to expand access to palliative care.”
Dr Morrison and his colleagues described their research in Health Affairs.
The study included 906 patients with advanced cancer and multiple comorbidities who were treated at 6 hospitals. One hundred and ninety-three patients were seen by a palliative care team within 2 days of hospitalization, while the remaining 713 patients received usual care.
Patients from the palliative care group had significantly lower total direct hospital costs if they had multimorbidity. For patients with a comorbidity score of 0–1, the estimated mean treatment effect was not significant.
However, patients with a comorbidity score of 2–3 had a 22% reduction in costs, or a reduction of $2321. Patients with a score of 4 or higher had a cost reduction of 32%, or $3515.
“The fact that we found greater cost savings for cancer patients with more comorbidities than for those with fewer comorbidities raises the question of whether similar results would be observed in patients with other serious illnesses and multimorbidity,” said Peter May, of Trinity College Dublin in Ireland.
“Future research is also needed to determine when in the course of illness palliative care is most cost-effective.”

Photo courtesy of the CDC
Patients with incurable cancer and multiple comorbidities who consulted with a palliative care team within 2 days of hospitalization had significant savings in hospital costs, according to a new study.
The study also showed that the higher number of comorbidities a patient had, the greater the reduction in direct hospital costs with early palliative care as opposed to standard care.
Previous studies have shown a link between palliative care and lower costs, but this is the first to examine whether the effect of palliative care consultation varies by the number of co-existing chronic conditions.
“We already know that coordinated, patient-centered palliative care improves care quality, enhances survival, and reduces costs for persons with cancer,” said R. Sean Morrison, MD, of the Icahn School of Medicine at Mount Sinai in New York, New York.
“Our latest research now shows the strong association between cost and the number of co-occurring conditions. Among patients with advanced cancer and other serious illnesses, aggressive treatments are often inconsistent with patients’ wishes and are associated with worse quality of life compared to other treatments. It is imperative that policymakers act to expand access to palliative care.”
Dr Morrison and his colleagues described their research in Health Affairs.
The study included 906 patients with advanced cancer and multiple comorbidities who were treated at 6 hospitals. One hundred and ninety-three patients were seen by a palliative care team within 2 days of hospitalization, while the remaining 713 patients received usual care.
Patients from the palliative care group had significantly lower total direct hospital costs if they had multimorbidity. For patients with a comorbidity score of 0–1, the estimated mean treatment effect was not significant.
However, patients with a comorbidity score of 2–3 had a 22% reduction in costs, or a reduction of $2321. Patients with a score of 4 or higher had a cost reduction of 32%, or $3515.
“The fact that we found greater cost savings for cancer patients with more comorbidities than for those with fewer comorbidities raises the question of whether similar results would be observed in patients with other serious illnesses and multimorbidity,” said Peter May, of Trinity College Dublin in Ireland.
“Future research is also needed to determine when in the course of illness palliative care is most cost-effective.”

Photo courtesy of the CDC
Patients with incurable cancer and multiple comorbidities who consulted with a palliative care team within 2 days of hospitalization had significant savings in hospital costs, according to a new study.
The study also showed that the higher number of comorbidities a patient had, the greater the reduction in direct hospital costs with early palliative care as opposed to standard care.
Previous studies have shown a link between palliative care and lower costs, but this is the first to examine whether the effect of palliative care consultation varies by the number of co-existing chronic conditions.
“We already know that coordinated, patient-centered palliative care improves care quality, enhances survival, and reduces costs for persons with cancer,” said R. Sean Morrison, MD, of the Icahn School of Medicine at Mount Sinai in New York, New York.
“Our latest research now shows the strong association between cost and the number of co-occurring conditions. Among patients with advanced cancer and other serious illnesses, aggressive treatments are often inconsistent with patients’ wishes and are associated with worse quality of life compared to other treatments. It is imperative that policymakers act to expand access to palliative care.”
Dr Morrison and his colleagues described their research in Health Affairs.
The study included 906 patients with advanced cancer and multiple comorbidities who were treated at 6 hospitals. One hundred and ninety-three patients were seen by a palliative care team within 2 days of hospitalization, while the remaining 713 patients received usual care.
Patients from the palliative care group had significantly lower total direct hospital costs if they had multimorbidity. For patients with a comorbidity score of 0–1, the estimated mean treatment effect was not significant.
However, patients with a comorbidity score of 2–3 had a 22% reduction in costs, or a reduction of $2321. Patients with a score of 4 or higher had a cost reduction of 32%, or $3515.
“The fact that we found greater cost savings for cancer patients with more comorbidities than for those with fewer comorbidities raises the question of whether similar results would be observed in patients with other serious illnesses and multimorbidity,” said Peter May, of Trinity College Dublin in Ireland.
“Future research is also needed to determine when in the course of illness palliative care is most cost-effective.”
Cardiac abnormalities among childhood cancer survivors

Photo by Bill Branson
A new study has provided additional insight into the development of cardiac abnormalities in adult survivors of childhood cancer.
Researchers analyzed more than 1800 cancer survivors who were exposed to cardiotoxic therapies as children.
The team said they found evidence of cardiac abnormalities in a substantial number of these subjects, many of whom were younger and did not exhibit symptoms of abnormalities.
Daniel A. Mulrooney, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and his colleagues reported these findings in Annals of Internal Medicine.
The team assessed cardiac outcomes among 1853 subjects who were 18 and older and had received cancer-related cardiotoxic therapy at least 10 years earlier.
The subjects were pretty evenly split along gender lines (52.3% male), their median age at cancer diagnosis was 8 (range, 0 to 24), and their median age at evaluation was 31 (range, 18 to 60).
At evaluation, 7.4% of subjects had cardiomyopathy (newly identified in 4.7%), 3.8% had coronary artery disease (newly identified in 2.2%), 28% had valvular regurgitation or stenosis (newly identified in 24.8%), and 4.4% had conduction or rhythm abnormalities (newly identified in 1.4%). All but 5 subjects were asymptomatic.
Multivariable analysis suggested the odds of developing cardiomyopathy were significantly associated with being male (odds ratio [OR]=1.9), receiving anthracycline doses of 250 mg/m2 or greater (OR=2.7), having cardiac radiation exposure greater than 1500 cGy (OR=1.9), and having hypertension (OR=3.0).
Being younger at diagnosis was associated with higher odds of valvular disease. The ORs were 1.5 for patients who were 0 to 4 years of age at diagnosis and 1.3 for patients who were 5 to 9 at diagnosis.
Receiving higher radiation doses was associated with higher odds of valvular disease as well. But associations between radiation and valvular disease varied according to a patient’s anthracycline exposure (interaction P<0.001). The highest odds were among survivors with the highest doses of radiation exposure and any anthracycline exposure (OR=4.5).
The researchers also noted a reduction in the OR for valvular disease among obese patients (OR=0.4) and those with dyslipidemia (OR=0.7).
The team said there were not enough cases of coronary artery disease and conduction or rhythm abnormalities to support a fully adjusted multivariable model. However, it seemed these outcomes were more common with older age (≥40 years) and among patients with cardiac radiation doses of 1500 cGy or greater.
The researchers said this study revealed “considerable cardiovascular disease” in a large cohort of adult survivors of childhood cancer, which suggests a substantial future healthcare burden.
The team believes their findings could guide stratification of risk factors, screening practices, health counseling, and potential therapeutic measures aimed at changing the disease trajectory in this young adult population.

Photo by Bill Branson
A new study has provided additional insight into the development of cardiac abnormalities in adult survivors of childhood cancer.
Researchers analyzed more than 1800 cancer survivors who were exposed to cardiotoxic therapies as children.
The team said they found evidence of cardiac abnormalities in a substantial number of these subjects, many of whom were younger and did not exhibit symptoms of abnormalities.
Daniel A. Mulrooney, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and his colleagues reported these findings in Annals of Internal Medicine.
The team assessed cardiac outcomes among 1853 subjects who were 18 and older and had received cancer-related cardiotoxic therapy at least 10 years earlier.
The subjects were pretty evenly split along gender lines (52.3% male), their median age at cancer diagnosis was 8 (range, 0 to 24), and their median age at evaluation was 31 (range, 18 to 60).
At evaluation, 7.4% of subjects had cardiomyopathy (newly identified in 4.7%), 3.8% had coronary artery disease (newly identified in 2.2%), 28% had valvular regurgitation or stenosis (newly identified in 24.8%), and 4.4% had conduction or rhythm abnormalities (newly identified in 1.4%). All but 5 subjects were asymptomatic.
Multivariable analysis suggested the odds of developing cardiomyopathy were significantly associated with being male (odds ratio [OR]=1.9), receiving anthracycline doses of 250 mg/m2 or greater (OR=2.7), having cardiac radiation exposure greater than 1500 cGy (OR=1.9), and having hypertension (OR=3.0).
Being younger at diagnosis was associated with higher odds of valvular disease. The ORs were 1.5 for patients who were 0 to 4 years of age at diagnosis and 1.3 for patients who were 5 to 9 at diagnosis.
Receiving higher radiation doses was associated with higher odds of valvular disease as well. But associations between radiation and valvular disease varied according to a patient’s anthracycline exposure (interaction P<0.001). The highest odds were among survivors with the highest doses of radiation exposure and any anthracycline exposure (OR=4.5).
The researchers also noted a reduction in the OR for valvular disease among obese patients (OR=0.4) and those with dyslipidemia (OR=0.7).
The team said there were not enough cases of coronary artery disease and conduction or rhythm abnormalities to support a fully adjusted multivariable model. However, it seemed these outcomes were more common with older age (≥40 years) and among patients with cardiac radiation doses of 1500 cGy or greater.
The researchers said this study revealed “considerable cardiovascular disease” in a large cohort of adult survivors of childhood cancer, which suggests a substantial future healthcare burden.
The team believes their findings could guide stratification of risk factors, screening practices, health counseling, and potential therapeutic measures aimed at changing the disease trajectory in this young adult population.

Photo by Bill Branson
A new study has provided additional insight into the development of cardiac abnormalities in adult survivors of childhood cancer.
Researchers analyzed more than 1800 cancer survivors who were exposed to cardiotoxic therapies as children.
The team said they found evidence of cardiac abnormalities in a substantial number of these subjects, many of whom were younger and did not exhibit symptoms of abnormalities.
Daniel A. Mulrooney, MD, of St. Jude Children’s Research Hospital in Memphis, Tennessee, and his colleagues reported these findings in Annals of Internal Medicine.
The team assessed cardiac outcomes among 1853 subjects who were 18 and older and had received cancer-related cardiotoxic therapy at least 10 years earlier.
The subjects were pretty evenly split along gender lines (52.3% male), their median age at cancer diagnosis was 8 (range, 0 to 24), and their median age at evaluation was 31 (range, 18 to 60).
At evaluation, 7.4% of subjects had cardiomyopathy (newly identified in 4.7%), 3.8% had coronary artery disease (newly identified in 2.2%), 28% had valvular regurgitation or stenosis (newly identified in 24.8%), and 4.4% had conduction or rhythm abnormalities (newly identified in 1.4%). All but 5 subjects were asymptomatic.
Multivariable analysis suggested the odds of developing cardiomyopathy were significantly associated with being male (odds ratio [OR]=1.9), receiving anthracycline doses of 250 mg/m2 or greater (OR=2.7), having cardiac radiation exposure greater than 1500 cGy (OR=1.9), and having hypertension (OR=3.0).
Being younger at diagnosis was associated with higher odds of valvular disease. The ORs were 1.5 for patients who were 0 to 4 years of age at diagnosis and 1.3 for patients who were 5 to 9 at diagnosis.
Receiving higher radiation doses was associated with higher odds of valvular disease as well. But associations between radiation and valvular disease varied according to a patient’s anthracycline exposure (interaction P<0.001). The highest odds were among survivors with the highest doses of radiation exposure and any anthracycline exposure (OR=4.5).
The researchers also noted a reduction in the OR for valvular disease among obese patients (OR=0.4) and those with dyslipidemia (OR=0.7).
The team said there were not enough cases of coronary artery disease and conduction or rhythm abnormalities to support a fully adjusted multivariable model. However, it seemed these outcomes were more common with older age (≥40 years) and among patients with cardiac radiation doses of 1500 cGy or greater.
The researchers said this study revealed “considerable cardiovascular disease” in a large cohort of adult survivors of childhood cancer, which suggests a substantial future healthcare burden.
The team believes their findings could guide stratification of risk factors, screening practices, health counseling, and potential therapeutic measures aimed at changing the disease trajectory in this young adult population.