User login
Paste may reduce radiation-induced fibrosis

woman for radiation
Photo by Rhoda Baer
A topical paste can reduce fibrosis caused by radiation therapy, according to preclinical research published in The FASEB Journal.
The study addressed a type of fibrosis called radiation dermatitis, in which radiation applied to the skin causes the buildup of fibrotic tissue and skin thickening.
To test their topical paste, researchers mimicked the development of radiation dermatitis in mice.
They exposed the mice’s skin to a single dose of 40 Gy, an amount of radiation similar to what patients undergoing anticancer radiation typically receive over 5 weeks.
Some of the irradiated animals were wild-type mice, while others were genetically engineered to lack the A2A receptor (A2AR). The researchers had previously shown that occupancy of A2AR induces collagen production.
The wild-type mice went on to receive placebo or daily treatment with ZM241385, a paste made with the research team’s patented A2AR blocker. The paste contains 2.5 milligrams of active ingredient per milliliter of 3% carboxymethyl cellulose, a gum “binder.”
A month after exposure, wild-type mice that received placebo had a nearly 2-fold increase in the amount of collagen and skin thickness. These mice also experienced epithelial hyperplasia.
On the other hand, mice treated with ZM241385 accumulated only 10% more skin-thickening collagen. ZM241385 treatment reduced the number of myofibroblasts, collagen fibrils, proliferating keratinocytes, and angiogenesis when compared to placebo. And the paste prevented epithelial hyperplasia.
Like ZM241385-treated mice, A2AR knockout mice did not have the excessive collagen production and skin thickening observed in placebo-treated wild-type mice. The knockout mice also exhibited reductions in myofibroblast content, angiogenesis, and epithelial hyperplasia.
The researchers noted that radiation-induced changes in the dermis and epidermis were accompanied by an infiltrate of T cells, which was prevented in both ZM241385-treated and A2AR knockout mice.
“Our latest study is the first to demonstrate that blocking or deleting the A2A receptor can be useful in reducing radiation-induced scarring in skin,” said study author Bruce Cronstein, MD, of New York University School of Medicine in New York, New York.
“The study also suggests that adenosine A2A receptor antagonists may have broad applications as drug therapies for preventing fibrosis and scarring, not just in the liver but also in the skin.”
If further experiments prove successful, Dr Cronstein said, clinicians treating early stage cancers with radiation could eventually prescribe an A2AR inhibitor paste to prevent fibrosis. He said his team next plans to study the mechanism underlying A2AR’s role in fibrosis. ![]()

woman for radiation
Photo by Rhoda Baer
A topical paste can reduce fibrosis caused by radiation therapy, according to preclinical research published in The FASEB Journal.
The study addressed a type of fibrosis called radiation dermatitis, in which radiation applied to the skin causes the buildup of fibrotic tissue and skin thickening.
To test their topical paste, researchers mimicked the development of radiation dermatitis in mice.
They exposed the mice’s skin to a single dose of 40 Gy, an amount of radiation similar to what patients undergoing anticancer radiation typically receive over 5 weeks.
Some of the irradiated animals were wild-type mice, while others were genetically engineered to lack the A2A receptor (A2AR). The researchers had previously shown that occupancy of A2AR induces collagen production.
The wild-type mice went on to receive placebo or daily treatment with ZM241385, a paste made with the research team’s patented A2AR blocker. The paste contains 2.5 milligrams of active ingredient per milliliter of 3% carboxymethyl cellulose, a gum “binder.”
A month after exposure, wild-type mice that received placebo had a nearly 2-fold increase in the amount of collagen and skin thickness. These mice also experienced epithelial hyperplasia.
On the other hand, mice treated with ZM241385 accumulated only 10% more skin-thickening collagen. ZM241385 treatment reduced the number of myofibroblasts, collagen fibrils, proliferating keratinocytes, and angiogenesis when compared to placebo. And the paste prevented epithelial hyperplasia.
Like ZM241385-treated mice, A2AR knockout mice did not have the excessive collagen production and skin thickening observed in placebo-treated wild-type mice. The knockout mice also exhibited reductions in myofibroblast content, angiogenesis, and epithelial hyperplasia.
The researchers noted that radiation-induced changes in the dermis and epidermis were accompanied by an infiltrate of T cells, which was prevented in both ZM241385-treated and A2AR knockout mice.
“Our latest study is the first to demonstrate that blocking or deleting the A2A receptor can be useful in reducing radiation-induced scarring in skin,” said study author Bruce Cronstein, MD, of New York University School of Medicine in New York, New York.
“The study also suggests that adenosine A2A receptor antagonists may have broad applications as drug therapies for preventing fibrosis and scarring, not just in the liver but also in the skin.”
If further experiments prove successful, Dr Cronstein said, clinicians treating early stage cancers with radiation could eventually prescribe an A2AR inhibitor paste to prevent fibrosis. He said his team next plans to study the mechanism underlying A2AR’s role in fibrosis. ![]()

woman for radiation
Photo by Rhoda Baer
A topical paste can reduce fibrosis caused by radiation therapy, according to preclinical research published in The FASEB Journal.
The study addressed a type of fibrosis called radiation dermatitis, in which radiation applied to the skin causes the buildup of fibrotic tissue and skin thickening.
To test their topical paste, researchers mimicked the development of radiation dermatitis in mice.
They exposed the mice’s skin to a single dose of 40 Gy, an amount of radiation similar to what patients undergoing anticancer radiation typically receive over 5 weeks.
Some of the irradiated animals were wild-type mice, while others were genetically engineered to lack the A2A receptor (A2AR). The researchers had previously shown that occupancy of A2AR induces collagen production.
The wild-type mice went on to receive placebo or daily treatment with ZM241385, a paste made with the research team’s patented A2AR blocker. The paste contains 2.5 milligrams of active ingredient per milliliter of 3% carboxymethyl cellulose, a gum “binder.”
A month after exposure, wild-type mice that received placebo had a nearly 2-fold increase in the amount of collagen and skin thickness. These mice also experienced epithelial hyperplasia.
On the other hand, mice treated with ZM241385 accumulated only 10% more skin-thickening collagen. ZM241385 treatment reduced the number of myofibroblasts, collagen fibrils, proliferating keratinocytes, and angiogenesis when compared to placebo. And the paste prevented epithelial hyperplasia.
Like ZM241385-treated mice, A2AR knockout mice did not have the excessive collagen production and skin thickening observed in placebo-treated wild-type mice. The knockout mice also exhibited reductions in myofibroblast content, angiogenesis, and epithelial hyperplasia.
The researchers noted that radiation-induced changes in the dermis and epidermis were accompanied by an infiltrate of T cells, which was prevented in both ZM241385-treated and A2AR knockout mice.
“Our latest study is the first to demonstrate that blocking or deleting the A2A receptor can be useful in reducing radiation-induced scarring in skin,” said study author Bruce Cronstein, MD, of New York University School of Medicine in New York, New York.
“The study also suggests that adenosine A2A receptor antagonists may have broad applications as drug therapies for preventing fibrosis and scarring, not just in the liver but also in the skin.”
If further experiments prove successful, Dr Cronstein said, clinicians treating early stage cancers with radiation could eventually prescribe an A2AR inhibitor paste to prevent fibrosis. He said his team next plans to study the mechanism underlying A2AR’s role in fibrosis. ![]()
Why cancer cells thrive when blood sugar is high

Photo by Andre Karwath
New research has revealed a mechanism that allows cancer cells to respond and grow rapidly when blood sugar levels rise.
This may help to explain why people who develop conditions in which they have chronically high blood sugar levels, such as obesity, also have an increased risk of developing certain cancers.
Susumu Hirabayashi, PhD, of Imperial College London in the UK, and Ross Cagan, PhD, of Mount Sinai Hospital in New York, New York, described the mechanism in eLife.
In a study published 2 years ago, the pair engineered fruit flies (Drosophila melanogaster) to activate the genes Ras and Src, which are activated in a range of malignancies.
The researchers activated Ras and Src in the flies’ developing eye tissue. Flies that were fed a normal diet grew small, benign tumors. But when flies were fed a high-sugar diet, they developed large, malignant tumors.
In flies fed a high-sugar diet, the normal cells became insulin-resistant, but the tumor cells didn’t. The tumor cells actually became more sensitive to insulin because they turned on a metabolic switch that triggered them to produce extra receptors for insulin. But this study did not explain how the tumor cells turned on this metabolic switch.
Now, after studying the same flies in more detail, Drs Hirabayashi and Cagan have found the tumor cells detect glucose availability indirectly, through a protein called salt-inducible kinase (SIK). When glucose levels are high, SIK sends a signal along the Hippo signaling pathway.
The Hippo signaling pathway is known to play a role in controlling cell growth. When it’s turned on, it keeps cell growth under control, but if it’s turned off, the cell can continue growing and may ultimately develop into a tumor.
Drs Hirabayashi and Cagan found that SIK acts like a sugar sensor, turning the Hippo signaling pathway off in response to raised glucose levels. This allows the tumor cells to continue to grow.
“Ras and Src co-activated tumors use SIK to sense that there’s lots of glucose available outside of their cells and to tell the cells to take advantage of that,” Dr Hirabayashi said. “Together, Ras and Src co-activated tumors use SIK to efficiently respond to glucose availability and ensure the tumors grow in nutrient-rich conditions such as obesity. We still don’t know if tumors caused by other genes respond to sugar in the same way.”
“Our results suggest that if we can develop drugs to target SIK, and stop it from alerting cancer cells in this way, then we may be able to stop cancer cells from thriving in an insulin-resistant environment and break the connection between obesity and cancer.” ![]()

Photo by Andre Karwath
New research has revealed a mechanism that allows cancer cells to respond and grow rapidly when blood sugar levels rise.
This may help to explain why people who develop conditions in which they have chronically high blood sugar levels, such as obesity, also have an increased risk of developing certain cancers.
Susumu Hirabayashi, PhD, of Imperial College London in the UK, and Ross Cagan, PhD, of Mount Sinai Hospital in New York, New York, described the mechanism in eLife.
In a study published 2 years ago, the pair engineered fruit flies (Drosophila melanogaster) to activate the genes Ras and Src, which are activated in a range of malignancies.
The researchers activated Ras and Src in the flies’ developing eye tissue. Flies that were fed a normal diet grew small, benign tumors. But when flies were fed a high-sugar diet, they developed large, malignant tumors.
In flies fed a high-sugar diet, the normal cells became insulin-resistant, but the tumor cells didn’t. The tumor cells actually became more sensitive to insulin because they turned on a metabolic switch that triggered them to produce extra receptors for insulin. But this study did not explain how the tumor cells turned on this metabolic switch.
Now, after studying the same flies in more detail, Drs Hirabayashi and Cagan have found the tumor cells detect glucose availability indirectly, through a protein called salt-inducible kinase (SIK). When glucose levels are high, SIK sends a signal along the Hippo signaling pathway.
The Hippo signaling pathway is known to play a role in controlling cell growth. When it’s turned on, it keeps cell growth under control, but if it’s turned off, the cell can continue growing and may ultimately develop into a tumor.
Drs Hirabayashi and Cagan found that SIK acts like a sugar sensor, turning the Hippo signaling pathway off in response to raised glucose levels. This allows the tumor cells to continue to grow.
“Ras and Src co-activated tumors use SIK to sense that there’s lots of glucose available outside of their cells and to tell the cells to take advantage of that,” Dr Hirabayashi said. “Together, Ras and Src co-activated tumors use SIK to efficiently respond to glucose availability and ensure the tumors grow in nutrient-rich conditions such as obesity. We still don’t know if tumors caused by other genes respond to sugar in the same way.”
“Our results suggest that if we can develop drugs to target SIK, and stop it from alerting cancer cells in this way, then we may be able to stop cancer cells from thriving in an insulin-resistant environment and break the connection between obesity and cancer.” ![]()

Photo by Andre Karwath
New research has revealed a mechanism that allows cancer cells to respond and grow rapidly when blood sugar levels rise.
This may help to explain why people who develop conditions in which they have chronically high blood sugar levels, such as obesity, also have an increased risk of developing certain cancers.
Susumu Hirabayashi, PhD, of Imperial College London in the UK, and Ross Cagan, PhD, of Mount Sinai Hospital in New York, New York, described the mechanism in eLife.
In a study published 2 years ago, the pair engineered fruit flies (Drosophila melanogaster) to activate the genes Ras and Src, which are activated in a range of malignancies.
The researchers activated Ras and Src in the flies’ developing eye tissue. Flies that were fed a normal diet grew small, benign tumors. But when flies were fed a high-sugar diet, they developed large, malignant tumors.
In flies fed a high-sugar diet, the normal cells became insulin-resistant, but the tumor cells didn’t. The tumor cells actually became more sensitive to insulin because they turned on a metabolic switch that triggered them to produce extra receptors for insulin. But this study did not explain how the tumor cells turned on this metabolic switch.
Now, after studying the same flies in more detail, Drs Hirabayashi and Cagan have found the tumor cells detect glucose availability indirectly, through a protein called salt-inducible kinase (SIK). When glucose levels are high, SIK sends a signal along the Hippo signaling pathway.
The Hippo signaling pathway is known to play a role in controlling cell growth. When it’s turned on, it keeps cell growth under control, but if it’s turned off, the cell can continue growing and may ultimately develop into a tumor.
Drs Hirabayashi and Cagan found that SIK acts like a sugar sensor, turning the Hippo signaling pathway off in response to raised glucose levels. This allows the tumor cells to continue to grow.
“Ras and Src co-activated tumors use SIK to sense that there’s lots of glucose available outside of their cells and to tell the cells to take advantage of that,” Dr Hirabayashi said. “Together, Ras and Src co-activated tumors use SIK to efficiently respond to glucose availability and ensure the tumors grow in nutrient-rich conditions such as obesity. We still don’t know if tumors caused by other genes respond to sugar in the same way.”
“Our results suggest that if we can develop drugs to target SIK, and stop it from alerting cancer cells in this way, then we may be able to stop cancer cells from thriving in an insulin-resistant environment and break the connection between obesity and cancer.” ![]()
Studies reveal lack of transparency and poor reporting of research

Photo by Bill Branson
Two new studies suggest biomedical research may be hindered by poor reporting and a lack of transparency.
In one study, researchers analyzed more than 400 biomedical science articles and found the papers rarely provided full protocol information, complete data, and the necessary level of transparency to verify or replicate the work.
In the other study, researchers analyzed more than 500 preclinical experiments and found that most didn’t contain sufficient information on the animals used.
Both studies were published in PLOS Biology.
For the first study, Shareen Iqbal, PhD, of Emory University in Atlanta, Georgia, and her colleagues analyzed papers published between 2000 and 2014.
The team set out to determine the extent to which researchers report key information necessary for properly evaluating and replicating published research, including availability of protocols, data, and the frequency of published novel or replication studies.
Out of 441 articles drawn from across the biomedical literature, only 1 paper provided a full protocol, and none of the papers made all the data available. The majority of studies didn’t state funding or conflicts of interest, and replication studies were very rare.
Dr Iqbal and her colleagues said they hope their study will further sensitize scientists, funders, journals, and other science-related stakeholders about the need to improve these indicators.
For the second study, Ulrich Dirnagl, MD, of Charité Universitätsmedizin in Berlin, Germany, and his colleagues examined 100 papers describing preclinical research on stroke and cancer. These papers contained accounts of 316 experiments on infarct volume and 206 experiments on tumor shrinkage.
The vast majority of the reports didn’t contain sufficient information on how many animals were used in the experiments. What’s more, in many papers, animals “vanished” over the course of the study.
Using a computer model, the researchers simulated the effects of such animal loss on the validity of the experiments. They found that the more animals lost or removed, the shakier or more biased the experimental conclusions.
“The study began with an attempt to look at the robustness of findings in a handful of preclinical papers, but the sheer number of missing animals stopped us in our tracks,” said author Constance Holman, a graduate student at Charité Universitätsmedizin.
Researchers from both studies believe their findings add to the list of concerns about bias and reporting in research, but the results also establish ways in which research can become more transparent and potentially more reproducible. ![]()

Photo by Bill Branson
Two new studies suggest biomedical research may be hindered by poor reporting and a lack of transparency.
In one study, researchers analyzed more than 400 biomedical science articles and found the papers rarely provided full protocol information, complete data, and the necessary level of transparency to verify or replicate the work.
In the other study, researchers analyzed more than 500 preclinical experiments and found that most didn’t contain sufficient information on the animals used.
Both studies were published in PLOS Biology.
For the first study, Shareen Iqbal, PhD, of Emory University in Atlanta, Georgia, and her colleagues analyzed papers published between 2000 and 2014.
The team set out to determine the extent to which researchers report key information necessary for properly evaluating and replicating published research, including availability of protocols, data, and the frequency of published novel or replication studies.
Out of 441 articles drawn from across the biomedical literature, only 1 paper provided a full protocol, and none of the papers made all the data available. The majority of studies didn’t state funding or conflicts of interest, and replication studies were very rare.
Dr Iqbal and her colleagues said they hope their study will further sensitize scientists, funders, journals, and other science-related stakeholders about the need to improve these indicators.
For the second study, Ulrich Dirnagl, MD, of Charité Universitätsmedizin in Berlin, Germany, and his colleagues examined 100 papers describing preclinical research on stroke and cancer. These papers contained accounts of 316 experiments on infarct volume and 206 experiments on tumor shrinkage.
The vast majority of the reports didn’t contain sufficient information on how many animals were used in the experiments. What’s more, in many papers, animals “vanished” over the course of the study.
Using a computer model, the researchers simulated the effects of such animal loss on the validity of the experiments. They found that the more animals lost or removed, the shakier or more biased the experimental conclusions.
“The study began with an attempt to look at the robustness of findings in a handful of preclinical papers, but the sheer number of missing animals stopped us in our tracks,” said author Constance Holman, a graduate student at Charité Universitätsmedizin.
Researchers from both studies believe their findings add to the list of concerns about bias and reporting in research, but the results also establish ways in which research can become more transparent and potentially more reproducible. ![]()

Photo by Bill Branson
Two new studies suggest biomedical research may be hindered by poor reporting and a lack of transparency.
In one study, researchers analyzed more than 400 biomedical science articles and found the papers rarely provided full protocol information, complete data, and the necessary level of transparency to verify or replicate the work.
In the other study, researchers analyzed more than 500 preclinical experiments and found that most didn’t contain sufficient information on the animals used.
Both studies were published in PLOS Biology.
For the first study, Shareen Iqbal, PhD, of Emory University in Atlanta, Georgia, and her colleagues analyzed papers published between 2000 and 2014.
The team set out to determine the extent to which researchers report key information necessary for properly evaluating and replicating published research, including availability of protocols, data, and the frequency of published novel or replication studies.
Out of 441 articles drawn from across the biomedical literature, only 1 paper provided a full protocol, and none of the papers made all the data available. The majority of studies didn’t state funding or conflicts of interest, and replication studies were very rare.
Dr Iqbal and her colleagues said they hope their study will further sensitize scientists, funders, journals, and other science-related stakeholders about the need to improve these indicators.
For the second study, Ulrich Dirnagl, MD, of Charité Universitätsmedizin in Berlin, Germany, and his colleagues examined 100 papers describing preclinical research on stroke and cancer. These papers contained accounts of 316 experiments on infarct volume and 206 experiments on tumor shrinkage.
The vast majority of the reports didn’t contain sufficient information on how many animals were used in the experiments. What’s more, in many papers, animals “vanished” over the course of the study.
Using a computer model, the researchers simulated the effects of such animal loss on the validity of the experiments. They found that the more animals lost or removed, the shakier or more biased the experimental conclusions.
“The study began with an attempt to look at the robustness of findings in a handful of preclinical papers, but the sheer number of missing animals stopped us in our tracks,” said author Constance Holman, a graduate student at Charité Universitätsmedizin.
Researchers from both studies believe their findings add to the list of concerns about bias and reporting in research, but the results also establish ways in which research can become more transparent and potentially more reproducible. ![]()
Docs’ body language may convey racial bias

Doctors may convey racial bias with their body language, according to research published in The Journal of Pain and Symptom Management.
In this small study, a group of physicians, most of whom were white males, gave less compassionate nonverbal cues when interacting with black actors portraying seriously ill patients than when interacting with white actors portraying seriously ill patients.
“Although we found that physicians said the same things to their black and white patients, communication is not just the spoken word. It also involves nonverbal cues, such as eye contact, body positioning, and touch,” said study author Amber Barnato, MD, of the University of Pittsburg in Pennsylvania.
“Poor nonverbal communication—something the physician may not even be aware he or she is doing—could explain why many black patients perceive discrimination in the healthcare setting.”
For this study, Dr Barnato and her colleagues recruited 33 hospital-based attending emergency medicine physicians, hospitalists, and intensivists from Allegheny County, Pennsylvania, and put them in realistic simulations where actors portrayed dying black and white patients accompanied by a family member.
The actors portrayed comparable medical conditions—plummeting vital signs related to either metastatic gastric or pancreatic cancer—and read from matching scripts. The physicians were unaware of what the trial was testing.
The majority of the physicians were white men, so the researchers could not derive any statistically significant conclusions about whether a physician’s race impacted his or her actions.
Physicians were scored on a point system for both their verbal and nonverbal communication skills when interacting with the patient and family member. The physicians averaged 7% lower scores for their nonverbal interactions with the black patients than with the white patients.
“When explaining what was happening and what the next steps for care could be, with the white patients, the physicians were more likely to stand right at the patient’s bedside and touch them in a sympathetic manner,” Dr Barnato said.
She explained that something as simple as a physician staying near the door and holding a binder in front of his body could be perceived by the patient and family as defensive or disengaged. This could lead to a cascade of misunderstandings that result in patients and their families requesting extraordinary life-saving measures because they don’t trust the doctor has their best interests in mind when suggesting gentler, end-of-life care options.
“When you survey people in the community about their feelings on end-of-life care, blacks are only slightly more likely than whites to say they want aggressive, life-sustaining measures when terminally ill,” Dr Barnato said.
“However, blacks are much more likely than whites to request such care when they are faced with making the decision in the hospital. Body language is a significant tool in building trust—or mistrust—and physicians need to ensure that their body language isn’t contributing to that decision.”
“To help black patients and their families feel welcome and encouraged to be partners in medical decision-making, it is critical that doctors be aware of their verbal and nonverbal communication and any unintentional biases.” ![]()

Doctors may convey racial bias with their body language, according to research published in The Journal of Pain and Symptom Management.
In this small study, a group of physicians, most of whom were white males, gave less compassionate nonverbal cues when interacting with black actors portraying seriously ill patients than when interacting with white actors portraying seriously ill patients.
“Although we found that physicians said the same things to their black and white patients, communication is not just the spoken word. It also involves nonverbal cues, such as eye contact, body positioning, and touch,” said study author Amber Barnato, MD, of the University of Pittsburg in Pennsylvania.
“Poor nonverbal communication—something the physician may not even be aware he or she is doing—could explain why many black patients perceive discrimination in the healthcare setting.”
For this study, Dr Barnato and her colleagues recruited 33 hospital-based attending emergency medicine physicians, hospitalists, and intensivists from Allegheny County, Pennsylvania, and put them in realistic simulations where actors portrayed dying black and white patients accompanied by a family member.
The actors portrayed comparable medical conditions—plummeting vital signs related to either metastatic gastric or pancreatic cancer—and read from matching scripts. The physicians were unaware of what the trial was testing.
The majority of the physicians were white men, so the researchers could not derive any statistically significant conclusions about whether a physician’s race impacted his or her actions.
Physicians were scored on a point system for both their verbal and nonverbal communication skills when interacting with the patient and family member. The physicians averaged 7% lower scores for their nonverbal interactions with the black patients than with the white patients.
“When explaining what was happening and what the next steps for care could be, with the white patients, the physicians were more likely to stand right at the patient’s bedside and touch them in a sympathetic manner,” Dr Barnato said.
She explained that something as simple as a physician staying near the door and holding a binder in front of his body could be perceived by the patient and family as defensive or disengaged. This could lead to a cascade of misunderstandings that result in patients and their families requesting extraordinary life-saving measures because they don’t trust the doctor has their best interests in mind when suggesting gentler, end-of-life care options.
“When you survey people in the community about their feelings on end-of-life care, blacks are only slightly more likely than whites to say they want aggressive, life-sustaining measures when terminally ill,” Dr Barnato said.
“However, blacks are much more likely than whites to request such care when they are faced with making the decision in the hospital. Body language is a significant tool in building trust—or mistrust—and physicians need to ensure that their body language isn’t contributing to that decision.”
“To help black patients and their families feel welcome and encouraged to be partners in medical decision-making, it is critical that doctors be aware of their verbal and nonverbal communication and any unintentional biases.” ![]()

Doctors may convey racial bias with their body language, according to research published in The Journal of Pain and Symptom Management.
In this small study, a group of physicians, most of whom were white males, gave less compassionate nonverbal cues when interacting with black actors portraying seriously ill patients than when interacting with white actors portraying seriously ill patients.
“Although we found that physicians said the same things to their black and white patients, communication is not just the spoken word. It also involves nonverbal cues, such as eye contact, body positioning, and touch,” said study author Amber Barnato, MD, of the University of Pittsburg in Pennsylvania.
“Poor nonverbal communication—something the physician may not even be aware he or she is doing—could explain why many black patients perceive discrimination in the healthcare setting.”
For this study, Dr Barnato and her colleagues recruited 33 hospital-based attending emergency medicine physicians, hospitalists, and intensivists from Allegheny County, Pennsylvania, and put them in realistic simulations where actors portrayed dying black and white patients accompanied by a family member.
The actors portrayed comparable medical conditions—plummeting vital signs related to either metastatic gastric or pancreatic cancer—and read from matching scripts. The physicians were unaware of what the trial was testing.
The majority of the physicians were white men, so the researchers could not derive any statistically significant conclusions about whether a physician’s race impacted his or her actions.
Physicians were scored on a point system for both their verbal and nonverbal communication skills when interacting with the patient and family member. The physicians averaged 7% lower scores for their nonverbal interactions with the black patients than with the white patients.
“When explaining what was happening and what the next steps for care could be, with the white patients, the physicians were more likely to stand right at the patient’s bedside and touch them in a sympathetic manner,” Dr Barnato said.
She explained that something as simple as a physician staying near the door and holding a binder in front of his body could be perceived by the patient and family as defensive or disengaged. This could lead to a cascade of misunderstandings that result in patients and their families requesting extraordinary life-saving measures because they don’t trust the doctor has their best interests in mind when suggesting gentler, end-of-life care options.
“When you survey people in the community about their feelings on end-of-life care, blacks are only slightly more likely than whites to say they want aggressive, life-sustaining measures when terminally ill,” Dr Barnato said.
“However, blacks are much more likely than whites to request such care when they are faced with making the decision in the hospital. Body language is a significant tool in building trust—or mistrust—and physicians need to ensure that their body language isn’t contributing to that decision.”
“To help black patients and their families feel welcome and encouraged to be partners in medical decision-making, it is critical that doctors be aware of their verbal and nonverbal communication and any unintentional biases.” ![]()
Cancer drug discovery database goes 3D

Photo by Rhoda Baer
Researchers have updated the canSAR database, a tool designed to aid cancer drug discovery, by adding 3D structures of faulty proteins and maps of cancer’s communication networks.
The canSAR database brings together biological, chemical, and pharmacological data.
The goal of the database is to make these data accessible to researchers worldwide to help with hypothesis generation and support drug discovery decisions.
Users can search canSAR using text queries, protein/gene name searches, any keyword searches, chemical structure searches, and sequence similarity searches. Users can also explore and filter chemical compound sets, view experimental data, and produce summary plots.
The canSAR database was launched in 2011 with the goal of using Big Data approaches to build a detailed picture of how the majority of known human molecules behave.
The database has already collated billions of experimental measurements, mapping the actions of 1 million drugs and chemicals on human proteins, and it has combined these data with genetic information and results from clinical trials.
The updated version of canSAR uses artificial intelligence to identify nooks and crannies on the surface of faulty cancer-causing molecules as a key step in designing new drugs to block them. It also allows researchers to identify communication lines that can be intercepted within tumor cells, opening up potential new approaches for cancer treatment.
The growing database now holds the 3D structures of almost 3 million cavities on the surface of nearly 110,000 molecules.
“Our database is constantly growing with information and is the largest of its kind, with more than 140,000 users from over 175 countries,” said Bissan Al-Lazikani, PhD, of The Institute of Cancer Research in London, UK.
“And we regularly develop new artificial intelligence technologies that help scientists make predictions and design experiments. Our aim is that cancer scientists will be armed with the data they need to carry out life-saving research into the most exciting drugs of the future.”
“Scientists need to find all the information there is about a faulty gene or protein to understand whether a new drug might work. These data are vast and scattered, but the canSAR database brings them together and adds value by identifying hidden links and presenting the key information easily.”
Details on the updates to canSAR have been published in Nucleic Acid Research. The database is available online at https://cansar.icr.ac.uk/. ![]()

Photo by Rhoda Baer
Researchers have updated the canSAR database, a tool designed to aid cancer drug discovery, by adding 3D structures of faulty proteins and maps of cancer’s communication networks.
The canSAR database brings together biological, chemical, and pharmacological data.
The goal of the database is to make these data accessible to researchers worldwide to help with hypothesis generation and support drug discovery decisions.
Users can search canSAR using text queries, protein/gene name searches, any keyword searches, chemical structure searches, and sequence similarity searches. Users can also explore and filter chemical compound sets, view experimental data, and produce summary plots.
The canSAR database was launched in 2011 with the goal of using Big Data approaches to build a detailed picture of how the majority of known human molecules behave.
The database has already collated billions of experimental measurements, mapping the actions of 1 million drugs and chemicals on human proteins, and it has combined these data with genetic information and results from clinical trials.
The updated version of canSAR uses artificial intelligence to identify nooks and crannies on the surface of faulty cancer-causing molecules as a key step in designing new drugs to block them. It also allows researchers to identify communication lines that can be intercepted within tumor cells, opening up potential new approaches for cancer treatment.
The growing database now holds the 3D structures of almost 3 million cavities on the surface of nearly 110,000 molecules.
“Our database is constantly growing with information and is the largest of its kind, with more than 140,000 users from over 175 countries,” said Bissan Al-Lazikani, PhD, of The Institute of Cancer Research in London, UK.
“And we regularly develop new artificial intelligence technologies that help scientists make predictions and design experiments. Our aim is that cancer scientists will be armed with the data they need to carry out life-saving research into the most exciting drugs of the future.”
“Scientists need to find all the information there is about a faulty gene or protein to understand whether a new drug might work. These data are vast and scattered, but the canSAR database brings them together and adds value by identifying hidden links and presenting the key information easily.”
Details on the updates to canSAR have been published in Nucleic Acid Research. The database is available online at https://cansar.icr.ac.uk/. ![]()

Photo by Rhoda Baer
Researchers have updated the canSAR database, a tool designed to aid cancer drug discovery, by adding 3D structures of faulty proteins and maps of cancer’s communication networks.
The canSAR database brings together biological, chemical, and pharmacological data.
The goal of the database is to make these data accessible to researchers worldwide to help with hypothesis generation and support drug discovery decisions.
Users can search canSAR using text queries, protein/gene name searches, any keyword searches, chemical structure searches, and sequence similarity searches. Users can also explore and filter chemical compound sets, view experimental data, and produce summary plots.
The canSAR database was launched in 2011 with the goal of using Big Data approaches to build a detailed picture of how the majority of known human molecules behave.
The database has already collated billions of experimental measurements, mapping the actions of 1 million drugs and chemicals on human proteins, and it has combined these data with genetic information and results from clinical trials.
The updated version of canSAR uses artificial intelligence to identify nooks and crannies on the surface of faulty cancer-causing molecules as a key step in designing new drugs to block them. It also allows researchers to identify communication lines that can be intercepted within tumor cells, opening up potential new approaches for cancer treatment.
The growing database now holds the 3D structures of almost 3 million cavities on the surface of nearly 110,000 molecules.
“Our database is constantly growing with information and is the largest of its kind, with more than 140,000 users from over 175 countries,” said Bissan Al-Lazikani, PhD, of The Institute of Cancer Research in London, UK.
“And we regularly develop new artificial intelligence technologies that help scientists make predictions and design experiments. Our aim is that cancer scientists will be armed with the data they need to carry out life-saving research into the most exciting drugs of the future.”
“Scientists need to find all the information there is about a faulty gene or protein to understand whether a new drug might work. These data are vast and scattered, but the canSAR database brings them together and adds value by identifying hidden links and presenting the key information easily.”
Details on the updates to canSAR have been published in Nucleic Acid Research. The database is available online at https://cansar.icr.ac.uk/. ![]()
Identifying druggable proteins

Photo by Darren Baker
A computer model that employs techniques used to analyze social networks could aid the development of new cancer treatments, according to researchers.
The model analyzes the unique behaviors of cancer-causing proteins, spotting what makes them different from normal proteins and mapping out molecular targets for drugs that could potentially be developed to treat cancers.
The researchers described this model in PLOS Computational Biology.
Bissan Al-Lazikani, PhD, of The Institute of Cancer Research in London, UK, and her colleagues compared proteins to members of an enormous social network, mapping the ways they interact. This allowed the team to predict which proteins might be most effectively targeted with drugs.
Cancer-causing proteins that have already been successfully targeted tended to have particular “social” characteristics that differed from non-cancer proteins. “Hub-like” proteins that were shown to “communicate” with lots of other proteins were more likely to cause cancers.
The researchers said this suggests that previously unexplored cancer proteins with similar characteristics could make good drug targets.
“Our study is the first to identify the rules of social behavior of cancer proteins and use it to predict new targets for potential cancer drugs,” Dr Al-Lazikani said.
“It shows that cancer drug targets behave very differently from normal proteins and often have a complex web of social interactions. Finding new targets is one of the most important steps in drug discovery, but it can be a lengthy, expensive process.”
“The map that we’ve made will help researchers design better new drugs, more quickly, saving time and money. It also sheds light on how resistance to treatments may occur and, in just a few years, could help doctors choose the best drug combinations to suit individual patients.”
All of the researchers’ target predictions are available on the canSAR website. The underlying data and tools are also available on the site. ![]()

Photo by Darren Baker
A computer model that employs techniques used to analyze social networks could aid the development of new cancer treatments, according to researchers.
The model analyzes the unique behaviors of cancer-causing proteins, spotting what makes them different from normal proteins and mapping out molecular targets for drugs that could potentially be developed to treat cancers.
The researchers described this model in PLOS Computational Biology.
Bissan Al-Lazikani, PhD, of The Institute of Cancer Research in London, UK, and her colleagues compared proteins to members of an enormous social network, mapping the ways they interact. This allowed the team to predict which proteins might be most effectively targeted with drugs.
Cancer-causing proteins that have already been successfully targeted tended to have particular “social” characteristics that differed from non-cancer proteins. “Hub-like” proteins that were shown to “communicate” with lots of other proteins were more likely to cause cancers.
The researchers said this suggests that previously unexplored cancer proteins with similar characteristics could make good drug targets.
“Our study is the first to identify the rules of social behavior of cancer proteins and use it to predict new targets for potential cancer drugs,” Dr Al-Lazikani said.
“It shows that cancer drug targets behave very differently from normal proteins and often have a complex web of social interactions. Finding new targets is one of the most important steps in drug discovery, but it can be a lengthy, expensive process.”
“The map that we’ve made will help researchers design better new drugs, more quickly, saving time and money. It also sheds light on how resistance to treatments may occur and, in just a few years, could help doctors choose the best drug combinations to suit individual patients.”
All of the researchers’ target predictions are available on the canSAR website. The underlying data and tools are also available on the site. ![]()

Photo by Darren Baker
A computer model that employs techniques used to analyze social networks could aid the development of new cancer treatments, according to researchers.
The model analyzes the unique behaviors of cancer-causing proteins, spotting what makes them different from normal proteins and mapping out molecular targets for drugs that could potentially be developed to treat cancers.
The researchers described this model in PLOS Computational Biology.
Bissan Al-Lazikani, PhD, of The Institute of Cancer Research in London, UK, and her colleagues compared proteins to members of an enormous social network, mapping the ways they interact. This allowed the team to predict which proteins might be most effectively targeted with drugs.
Cancer-causing proteins that have already been successfully targeted tended to have particular “social” characteristics that differed from non-cancer proteins. “Hub-like” proteins that were shown to “communicate” with lots of other proteins were more likely to cause cancers.
The researchers said this suggests that previously unexplored cancer proteins with similar characteristics could make good drug targets.
“Our study is the first to identify the rules of social behavior of cancer proteins and use it to predict new targets for potential cancer drugs,” Dr Al-Lazikani said.
“It shows that cancer drug targets behave very differently from normal proteins and often have a complex web of social interactions. Finding new targets is one of the most important steps in drug discovery, but it can be a lengthy, expensive process.”
“The map that we’ve made will help researchers design better new drugs, more quickly, saving time and money. It also sheds light on how resistance to treatments may occur and, in just a few years, could help doctors choose the best drug combinations to suit individual patients.”
All of the researchers’ target predictions are available on the canSAR website. The underlying data and tools are also available on the site. ![]()
Factors predict low accrual in cancer clinical trials

for a clinical trial
Photo by Esther Dyson
Twelve factors may predict low patient accrual in cancer clinical trials, according to research published in JNCI.
Many studies have been conducted to investigate the perceived barriers to clinical trial accrual from the patient or provider perspective.
However, researchers have rarely taken a trial-level view and investigated why certain trials are able to accrue patients faster than expected while others fail to attract even a fraction of the intended number of participants.
Caroline S. Bennette, PhD, of the University of Washington in Seattle, and her colleagues conducted their study to do just that.
They analyzed information on 787 phase 2/3 clinical trials sponsored by the National Clinical Trials Network (NCTN; formerly the Cooperative Group Program) launched between 2000 and 2011.
After excluding trials that closed because of toxicity or interim results, the researchers found that 145 (18%) NCTN trials closed with low accrual or were accruing at less than 50% of target accrual 3 years or more after opening.
The team identified potential risk factors from the literature and interviews with clinical trial experts and found multiple trial-level factors that were associated with poor accrual to NCTN trials, such as increased competition for patients from currently ongoing trials, planning to enroll a higher proportion of the available patient population, and not evaluating a new investigational agent or targeted therapy.
The researchers then developed a multivariable prediction model of low accrual using 12 trial-level risk factors. The team said these factors had good agreement between predicted and observed risks of low accrual in a preliminary validation using 46 trials opened between 2012 and 2013.
Those 12 risk factors are:
- The number of competing trials per 10,000 eligible patients per year (odds ratio [OR]=1.88)
- Phase 3 vs phase 2 trial (OR=1.86)
- Enrollment as percentage of eligible population for targeted therapy (OR=0.57)
- Enrollment as percentage of eligible population for radiation therapy (OR=1.81)
- Annual incidence of clinical condition(s) per 10,000 (OR=0.99)
- Tissue sample required to assess eligibility (OR=1.26)
- Investigational new drug (OR=0.34)
- Metastatic setting (OR=1.46)
- Sample size per 100 (OR=0.95)
- More than one condition evaluated (OR=1.98)
- Common solid cancer (prostate, breast, lung, or colon) vs liquid or rare solid cancers (OR=2.32)
- Interaction term (phase 3 x investigational new drug, OR=2.47).
The researchers concluded that systematically considering the overall influence of these risk factors could aid in the design and prioritization of future clinical trials. ![]()

for a clinical trial
Photo by Esther Dyson
Twelve factors may predict low patient accrual in cancer clinical trials, according to research published in JNCI.
Many studies have been conducted to investigate the perceived barriers to clinical trial accrual from the patient or provider perspective.
However, researchers have rarely taken a trial-level view and investigated why certain trials are able to accrue patients faster than expected while others fail to attract even a fraction of the intended number of participants.
Caroline S. Bennette, PhD, of the University of Washington in Seattle, and her colleagues conducted their study to do just that.
They analyzed information on 787 phase 2/3 clinical trials sponsored by the National Clinical Trials Network (NCTN; formerly the Cooperative Group Program) launched between 2000 and 2011.
After excluding trials that closed because of toxicity or interim results, the researchers found that 145 (18%) NCTN trials closed with low accrual or were accruing at less than 50% of target accrual 3 years or more after opening.
The team identified potential risk factors from the literature and interviews with clinical trial experts and found multiple trial-level factors that were associated with poor accrual to NCTN trials, such as increased competition for patients from currently ongoing trials, planning to enroll a higher proportion of the available patient population, and not evaluating a new investigational agent or targeted therapy.
The researchers then developed a multivariable prediction model of low accrual using 12 trial-level risk factors. The team said these factors had good agreement between predicted and observed risks of low accrual in a preliminary validation using 46 trials opened between 2012 and 2013.
Those 12 risk factors are:
- The number of competing trials per 10,000 eligible patients per year (odds ratio [OR]=1.88)
- Phase 3 vs phase 2 trial (OR=1.86)
- Enrollment as percentage of eligible population for targeted therapy (OR=0.57)
- Enrollment as percentage of eligible population for radiation therapy (OR=1.81)
- Annual incidence of clinical condition(s) per 10,000 (OR=0.99)
- Tissue sample required to assess eligibility (OR=1.26)
- Investigational new drug (OR=0.34)
- Metastatic setting (OR=1.46)
- Sample size per 100 (OR=0.95)
- More than one condition evaluated (OR=1.98)
- Common solid cancer (prostate, breast, lung, or colon) vs liquid or rare solid cancers (OR=2.32)
- Interaction term (phase 3 x investigational new drug, OR=2.47).
The researchers concluded that systematically considering the overall influence of these risk factors could aid in the design and prioritization of future clinical trials. ![]()

for a clinical trial
Photo by Esther Dyson
Twelve factors may predict low patient accrual in cancer clinical trials, according to research published in JNCI.
Many studies have been conducted to investigate the perceived barriers to clinical trial accrual from the patient or provider perspective.
However, researchers have rarely taken a trial-level view and investigated why certain trials are able to accrue patients faster than expected while others fail to attract even a fraction of the intended number of participants.
Caroline S. Bennette, PhD, of the University of Washington in Seattle, and her colleagues conducted their study to do just that.
They analyzed information on 787 phase 2/3 clinical trials sponsored by the National Clinical Trials Network (NCTN; formerly the Cooperative Group Program) launched between 2000 and 2011.
After excluding trials that closed because of toxicity or interim results, the researchers found that 145 (18%) NCTN trials closed with low accrual or were accruing at less than 50% of target accrual 3 years or more after opening.
The team identified potential risk factors from the literature and interviews with clinical trial experts and found multiple trial-level factors that were associated with poor accrual to NCTN trials, such as increased competition for patients from currently ongoing trials, planning to enroll a higher proportion of the available patient population, and not evaluating a new investigational agent or targeted therapy.
The researchers then developed a multivariable prediction model of low accrual using 12 trial-level risk factors. The team said these factors had good agreement between predicted and observed risks of low accrual in a preliminary validation using 46 trials opened between 2012 and 2013.
Those 12 risk factors are:
- The number of competing trials per 10,000 eligible patients per year (odds ratio [OR]=1.88)
- Phase 3 vs phase 2 trial (OR=1.86)
- Enrollment as percentage of eligible population for targeted therapy (OR=0.57)
- Enrollment as percentage of eligible population for radiation therapy (OR=1.81)
- Annual incidence of clinical condition(s) per 10,000 (OR=0.99)
- Tissue sample required to assess eligibility (OR=1.26)
- Investigational new drug (OR=0.34)
- Metastatic setting (OR=1.46)
- Sample size per 100 (OR=0.95)
- More than one condition evaluated (OR=1.98)
- Common solid cancer (prostate, breast, lung, or colon) vs liquid or rare solid cancers (OR=2.32)
- Interaction term (phase 3 x investigational new drug, OR=2.47).
The researchers concluded that systematically considering the overall influence of these risk factors could aid in the design and prioritization of future clinical trials.
Why it’s hard to develop immunity against malaria

Diana Hansen, PhD
Photo courtesy of the Walter
and Eliza Hall Institute
Results of preclinical research appear to explain how the malaria parasite Plasmodium falciparum causes an inflammatory reaction that sabotages the body’s ability to protect itself from malaria.
Researchers found evidence to suggest that the same inflammatory molecules that drive the immune response in clinical and severe malaria also prevent the body from developing protective antibodies against the parasite.
They said this discovery opens up the possibility of improving new or existing malaria vaccines by boosting immune cells needed for long-lasting immunity.
Diana Hansen, PhD, of the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia, and her colleagues described this work in Cell Reports.
Dr Hansen said this is the first time scientists have pinpointed why the immune system fails to develop immunity during malaria infection.
“With many infections, a single exposure to the pathogen is enough to induce production of antibodies that will protect you for the rest of your life,” she explained. “However, with malaria, it can take up to 20 years for someone to build up sufficient immunity to be protected.”
The fact that the body is not good at developing long-lasting immunity to the parasite has hampered vaccine development, Dr Hansen added.
“This was complicated by the fact that we didn’t know whether it was the malaria parasite itself or the inflammatory reaction to malaria that was actually inhibiting the ability to develop protective immunity,” she said.
“We have now shown that it was a double-edged sword. The strong inflammatory reaction that accompanies and, in fact, drives severe clinical malaria is also responsible for silencing the key immune cells needed for long-term protection against the parasite.”
Dr Hansen and her colleagues conducted experiments in mouse models of malaria and found that inflammatory molecules released by the body to fight the infection were preventing protective antibodies from being made.
“Specialized immune cells called helper T cells join forces with B cells to generate these protective antibodies,” said Axel Kallies, PhD, of the Walter and Eliza Hall Institute of Medical Research.
“However, we showed that, during malaria infection, critical inflammatory molecules actually arrest development of helper T cells, and, therefore, the B cells don’t get the necessary instructions to make antibodies.”
Specifically, the researchers found that severe malaria infection inhibited the establishment of germinal centers in the spleens of the mice. And malaria infection induced high frequencies of T-follicular-helper cell precursors but resulted in impaired T-follicular-helper cell differentiation.
Precursor T-follicular-helper cells induced during infection had low levels of PD-1 and CXCR5 and co-expressed Th1-associated molecules such as T-bet and CXCR3.
However, when the researchers blocked the inflammatory cytokines TNF and IFN-γ or deleted T-bet, they were able to restore T-follicular-helper cell differentiation and germinal center responses to infection.
Dr Hansen said these findings could lead to new avenues in the search for effective malaria vaccines.
“This research opens the door to therapeutic approaches to accelerate development of protective immunity to malaria and improve efficacy of malaria vaccines,” she said.
“Until now, malaria vaccines have had disappointing results. We can now see a way of improving these responses by tailoring or augmenting the vaccine to boost development of helper T cells that will enable the body to make protective antibodies that target the malaria parasites.”

Diana Hansen, PhD
Photo courtesy of the Walter
and Eliza Hall Institute
Results of preclinical research appear to explain how the malaria parasite Plasmodium falciparum causes an inflammatory reaction that sabotages the body’s ability to protect itself from malaria.
Researchers found evidence to suggest that the same inflammatory molecules that drive the immune response in clinical and severe malaria also prevent the body from developing protective antibodies against the parasite.
They said this discovery opens up the possibility of improving new or existing malaria vaccines by boosting immune cells needed for long-lasting immunity.
Diana Hansen, PhD, of the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia, and her colleagues described this work in Cell Reports.
Dr Hansen said this is the first time scientists have pinpointed why the immune system fails to develop immunity during malaria infection.
“With many infections, a single exposure to the pathogen is enough to induce production of antibodies that will protect you for the rest of your life,” she explained. “However, with malaria, it can take up to 20 years for someone to build up sufficient immunity to be protected.”
The fact that the body is not good at developing long-lasting immunity to the parasite has hampered vaccine development, Dr Hansen added.
“This was complicated by the fact that we didn’t know whether it was the malaria parasite itself or the inflammatory reaction to malaria that was actually inhibiting the ability to develop protective immunity,” she said.
“We have now shown that it was a double-edged sword. The strong inflammatory reaction that accompanies and, in fact, drives severe clinical malaria is also responsible for silencing the key immune cells needed for long-term protection against the parasite.”
Dr Hansen and her colleagues conducted experiments in mouse models of malaria and found that inflammatory molecules released by the body to fight the infection were preventing protective antibodies from being made.
“Specialized immune cells called helper T cells join forces with B cells to generate these protective antibodies,” said Axel Kallies, PhD, of the Walter and Eliza Hall Institute of Medical Research.
“However, we showed that, during malaria infection, critical inflammatory molecules actually arrest development of helper T cells, and, therefore, the B cells don’t get the necessary instructions to make antibodies.”
Specifically, the researchers found that severe malaria infection inhibited the establishment of germinal centers in the spleens of the mice. And malaria infection induced high frequencies of T-follicular-helper cell precursors but resulted in impaired T-follicular-helper cell differentiation.
Precursor T-follicular-helper cells induced during infection had low levels of PD-1 and CXCR5 and co-expressed Th1-associated molecules such as T-bet and CXCR3.
However, when the researchers blocked the inflammatory cytokines TNF and IFN-γ or deleted T-bet, they were able to restore T-follicular-helper cell differentiation and germinal center responses to infection.
Dr Hansen said these findings could lead to new avenues in the search for effective malaria vaccines.
“This research opens the door to therapeutic approaches to accelerate development of protective immunity to malaria and improve efficacy of malaria vaccines,” she said.
“Until now, malaria vaccines have had disappointing results. We can now see a way of improving these responses by tailoring or augmenting the vaccine to boost development of helper T cells that will enable the body to make protective antibodies that target the malaria parasites.”

Diana Hansen, PhD
Photo courtesy of the Walter
and Eliza Hall Institute
Results of preclinical research appear to explain how the malaria parasite Plasmodium falciparum causes an inflammatory reaction that sabotages the body’s ability to protect itself from malaria.
Researchers found evidence to suggest that the same inflammatory molecules that drive the immune response in clinical and severe malaria also prevent the body from developing protective antibodies against the parasite.
They said this discovery opens up the possibility of improving new or existing malaria vaccines by boosting immune cells needed for long-lasting immunity.
Diana Hansen, PhD, of the Walter and Eliza Hall Institute of Medical Research in Parkville, Victoria, Australia, and her colleagues described this work in Cell Reports.
Dr Hansen said this is the first time scientists have pinpointed why the immune system fails to develop immunity during malaria infection.
“With many infections, a single exposure to the pathogen is enough to induce production of antibodies that will protect you for the rest of your life,” she explained. “However, with malaria, it can take up to 20 years for someone to build up sufficient immunity to be protected.”
The fact that the body is not good at developing long-lasting immunity to the parasite has hampered vaccine development, Dr Hansen added.
“This was complicated by the fact that we didn’t know whether it was the malaria parasite itself or the inflammatory reaction to malaria that was actually inhibiting the ability to develop protective immunity,” she said.
“We have now shown that it was a double-edged sword. The strong inflammatory reaction that accompanies and, in fact, drives severe clinical malaria is also responsible for silencing the key immune cells needed for long-term protection against the parasite.”
Dr Hansen and her colleagues conducted experiments in mouse models of malaria and found that inflammatory molecules released by the body to fight the infection were preventing protective antibodies from being made.
“Specialized immune cells called helper T cells join forces with B cells to generate these protective antibodies,” said Axel Kallies, PhD, of the Walter and Eliza Hall Institute of Medical Research.
“However, we showed that, during malaria infection, critical inflammatory molecules actually arrest development of helper T cells, and, therefore, the B cells don’t get the necessary instructions to make antibodies.”
Specifically, the researchers found that severe malaria infection inhibited the establishment of germinal centers in the spleens of the mice. And malaria infection induced high frequencies of T-follicular-helper cell precursors but resulted in impaired T-follicular-helper cell differentiation.
Precursor T-follicular-helper cells induced during infection had low levels of PD-1 and CXCR5 and co-expressed Th1-associated molecules such as T-bet and CXCR3.
However, when the researchers blocked the inflammatory cytokines TNF and IFN-γ or deleted T-bet, they were able to restore T-follicular-helper cell differentiation and germinal center responses to infection.
Dr Hansen said these findings could lead to new avenues in the search for effective malaria vaccines.
“This research opens the door to therapeutic approaches to accelerate development of protective immunity to malaria and improve efficacy of malaria vaccines,” she said.
“Until now, malaria vaccines have had disappointing results. We can now see a way of improving these responses by tailoring or augmenting the vaccine to boost development of helper T cells that will enable the body to make protective antibodies that target the malaria parasites.”
Education may increase clinical trial participation

Photo courtesy of NCI
and Matthews Media Group
A new study suggests that educating cancer patients about clinical trials—with either a general or patient-specific program—increases the likelihood that patients will enroll in such trials.
After completing either type of educational program, 21% of the cancer patients studied chose to enroll in clinical trials.
Traditionally, less than 5% of cancer patients decide to participate in trials, according to the American Cancer Society.
“Unfortunately, although clinical trials are critical for advancing cancer treatment and ultimately serve as the basis for new standards of care, very few patients participate,” said Neal J. Meropol, MD, of Case Western Reserve University School of Medicine in Cleveland, Ohio.
“We want to close the patient knowledge gap and positively affect their attitudes toward clinical trials.”
Dr Meropol and his colleagues described their effort to do just that in the Journal of Clinical Oncology.
The researchers compared a tailored video education program on clinical trials, PRE-ACT (Preparatory Education about Clinical Trials), to educational information delivered as written text.
PRE-ACT is an intervention in which patients access a website to take an online survey. The survey gauges the individual patient’s knowledge and attitudes about clinical trials, and then, based on that patient’s answers, video clips are presented addressing his or her specific concerns.
For example, patients may worry they will receive a placebo rather than active treatment, so one video clip explains how placebos are used ethically in cancer studies, and the fact that very few studies will include a placebo without any active treatment. The videos also help patients clarify their preferences in terms of quality of life or length of life.
Results
Dr Meropol and his colleagues enrolled 1255 cancer patients in the study. Half of them participated in the PRE-ACT program, and the other half received written information about clinical trials that was not specifically chosen based on their survey responses.
Both interventions improved patients’ knowledge and attitudes regarding clinical trials when compared with baseline (all P<0.001).
Patients in both arms said they felt more prepared to consider enrolling in a clinical trial after completing their assigned educational program (P<0.001), but there was a trend favoring the PRE-ACT arm (P<0.09).
Patients in the PRE-ACT arm also showed a significantly greater increase in knowledge (P<0.001) and a significantly greater decrease in attitudinal barriers (P<0.001) than patients in the text-only arm. And PRE-ACT was associated with greater patient satisfaction.
Financial concerns
During the course of this research, Dr Meropol and his colleagues made a surprising discovery. Video clips meant to address concerns about the costs of clinical trial treatment actually caused a spike in worries about the out-of-pocket costs of clinical trials.
These financial concerns generated yet another paper that appeared in the same edition of the Journal of Clinical Oncology.
“What was a surprise is that giving people information about costs in general terms made them more anxious,” Dr Meropol said. “It was not surprising to us that these concerns actually affect distress, add to decisional conflict, and interfere with decision-making.”
“This finding highlighted for us that communication about costs is both necessary and challenging. It indicates that we need to be sensitive to patients’ cost concerns as they navigate decisions about cancer care.”
The researchers are now planning to develop tools to assist patients with financial navigation. The team is also developing a web-based educational program for oncology nurses to help them discuss clinical trial participation with patients.

Photo courtesy of NCI
and Matthews Media Group
A new study suggests that educating cancer patients about clinical trials—with either a general or patient-specific program—increases the likelihood that patients will enroll in such trials.
After completing either type of educational program, 21% of the cancer patients studied chose to enroll in clinical trials.
Traditionally, less than 5% of cancer patients decide to participate in trials, according to the American Cancer Society.
“Unfortunately, although clinical trials are critical for advancing cancer treatment and ultimately serve as the basis for new standards of care, very few patients participate,” said Neal J. Meropol, MD, of Case Western Reserve University School of Medicine in Cleveland, Ohio.
“We want to close the patient knowledge gap and positively affect their attitudes toward clinical trials.”
Dr Meropol and his colleagues described their effort to do just that in the Journal of Clinical Oncology.
The researchers compared a tailored video education program on clinical trials, PRE-ACT (Preparatory Education about Clinical Trials), to educational information delivered as written text.
PRE-ACT is an intervention in which patients access a website to take an online survey. The survey gauges the individual patient’s knowledge and attitudes about clinical trials, and then, based on that patient’s answers, video clips are presented addressing his or her specific concerns.
For example, patients may worry they will receive a placebo rather than active treatment, so one video clip explains how placebos are used ethically in cancer studies, and the fact that very few studies will include a placebo without any active treatment. The videos also help patients clarify their preferences in terms of quality of life or length of life.
Results
Dr Meropol and his colleagues enrolled 1255 cancer patients in the study. Half of them participated in the PRE-ACT program, and the other half received written information about clinical trials that was not specifically chosen based on their survey responses.
Both interventions improved patients’ knowledge and attitudes regarding clinical trials when compared with baseline (all P<0.001).
Patients in both arms said they felt more prepared to consider enrolling in a clinical trial after completing their assigned educational program (P<0.001), but there was a trend favoring the PRE-ACT arm (P<0.09).
Patients in the PRE-ACT arm also showed a significantly greater increase in knowledge (P<0.001) and a significantly greater decrease in attitudinal barriers (P<0.001) than patients in the text-only arm. And PRE-ACT was associated with greater patient satisfaction.
Financial concerns
During the course of this research, Dr Meropol and his colleagues made a surprising discovery. Video clips meant to address concerns about the costs of clinical trial treatment actually caused a spike in worries about the out-of-pocket costs of clinical trials.
These financial concerns generated yet another paper that appeared in the same edition of the Journal of Clinical Oncology.
“What was a surprise is that giving people information about costs in general terms made them more anxious,” Dr Meropol said. “It was not surprising to us that these concerns actually affect distress, add to decisional conflict, and interfere with decision-making.”
“This finding highlighted for us that communication about costs is both necessary and challenging. It indicates that we need to be sensitive to patients’ cost concerns as they navigate decisions about cancer care.”
The researchers are now planning to develop tools to assist patients with financial navigation. The team is also developing a web-based educational program for oncology nurses to help them discuss clinical trial participation with patients.

Photo courtesy of NCI
and Matthews Media Group
A new study suggests that educating cancer patients about clinical trials—with either a general or patient-specific program—increases the likelihood that patients will enroll in such trials.
After completing either type of educational program, 21% of the cancer patients studied chose to enroll in clinical trials.
Traditionally, less than 5% of cancer patients decide to participate in trials, according to the American Cancer Society.
“Unfortunately, although clinical trials are critical for advancing cancer treatment and ultimately serve as the basis for new standards of care, very few patients participate,” said Neal J. Meropol, MD, of Case Western Reserve University School of Medicine in Cleveland, Ohio.
“We want to close the patient knowledge gap and positively affect their attitudes toward clinical trials.”
Dr Meropol and his colleagues described their effort to do just that in the Journal of Clinical Oncology.
The researchers compared a tailored video education program on clinical trials, PRE-ACT (Preparatory Education about Clinical Trials), to educational information delivered as written text.
PRE-ACT is an intervention in which patients access a website to take an online survey. The survey gauges the individual patient’s knowledge and attitudes about clinical trials, and then, based on that patient’s answers, video clips are presented addressing his or her specific concerns.
For example, patients may worry they will receive a placebo rather than active treatment, so one video clip explains how placebos are used ethically in cancer studies, and the fact that very few studies will include a placebo without any active treatment. The videos also help patients clarify their preferences in terms of quality of life or length of life.
Results
Dr Meropol and his colleagues enrolled 1255 cancer patients in the study. Half of them participated in the PRE-ACT program, and the other half received written information about clinical trials that was not specifically chosen based on their survey responses.
Both interventions improved patients’ knowledge and attitudes regarding clinical trials when compared with baseline (all P<0.001).
Patients in both arms said they felt more prepared to consider enrolling in a clinical trial after completing their assigned educational program (P<0.001), but there was a trend favoring the PRE-ACT arm (P<0.09).
Patients in the PRE-ACT arm also showed a significantly greater increase in knowledge (P<0.001) and a significantly greater decrease in attitudinal barriers (P<0.001) than patients in the text-only arm. And PRE-ACT was associated with greater patient satisfaction.
Financial concerns
During the course of this research, Dr Meropol and his colleagues made a surprising discovery. Video clips meant to address concerns about the costs of clinical trial treatment actually caused a spike in worries about the out-of-pocket costs of clinical trials.
These financial concerns generated yet another paper that appeared in the same edition of the Journal of Clinical Oncology.
“What was a surprise is that giving people information about costs in general terms made them more anxious,” Dr Meropol said. “It was not surprising to us that these concerns actually affect distress, add to decisional conflict, and interfere with decision-making.”
“This finding highlighted for us that communication about costs is both necessary and challenging. It indicates that we need to be sensitive to patients’ cost concerns as they navigate decisions about cancer care.”
The researchers are now planning to develop tools to assist patients with financial navigation. The team is also developing a web-based educational program for oncology nurses to help them discuss clinical trial participation with patients.
Team explains how artemisinin kills malaria parasite
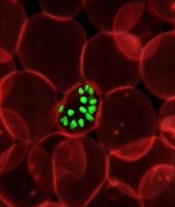
infecting a red blood cell
Photo courtesy of St. Jude
Children’s Research Hospital
Researchers say they have gained a better understanding of how the antimalarial drug artemisinin kills the Plasmodium falciparum parasite.
A chemical proteomics analysis revealed more than 120 protein targets of artemisinin and the mechanism that activates its killing effect.
Given the emergence of artemisinin resistance, the team believes their findings could aid the design of new treatments against drug-resistant parasites.
They reported the findings in Nature Communications.
Previously, only 2 targets of artemisinin had been identified, and their correlation with the parasite-killing effect of the drug had been questioned.
Lin Qingsong, PhD, of the National University of Singapore, and his colleagues identified 124 protein targets of artemisinin in P falciparum. Many of these newly identified protein targets are involved in essential biological processes in the parasite, thus explaining artemisinin’s potent killing effect.
The research suggests that, through its promiscuous targeting mechanism, artemisinin targets the blood-eating nature of the malaria parasite, binding to a broad spectrum of targets simultaneously and fatally disrupting the biochemistry of the parasite.
The study also showed that the main activator of artemisinin is heme, an iron-containing compound that is either biosynthesized by the parasite at its early developmental ring stage or derived from hemoglobin digestion in the later stages.
The drug activation level was found to be much lower in ring-stage parasites, given that artemisinin activation requires heme, which is of much lower abundance and is biosynthesized by the parasite.
In comparison, during the late stages of its life cycle, the parasite actively digests the hemoglobin in infected blood cells as its primary energy source. This releases large amounts of heme, and the drug is able to specifically respond to parasite-infected cells and effectively attack the disease-causing parasites.
“The current findings not only provide a more complete picture of how artemisinin and its derivatives work but also suggest new ways of using the drug,” Dr Lin said. “For instance, to improve drug activation at ring stage, we can explore enhancing the level of heme biosynthesis in the parasite.”
“By understanding that hemoglobin digestion releases huge amounts of heme, which brings about the effective killing mechanism in the later stages, we can also consider prolonging the treatment time to ensure that the drug can effectively kill the parasite through multiple cycles.”
In addition, the researchers are planning to develop novel artemisinin analogues with more specific targeting properties.
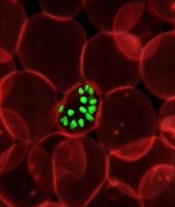
infecting a red blood cell
Photo courtesy of St. Jude
Children’s Research Hospital
Researchers say they have gained a better understanding of how the antimalarial drug artemisinin kills the Plasmodium falciparum parasite.
A chemical proteomics analysis revealed more than 120 protein targets of artemisinin and the mechanism that activates its killing effect.
Given the emergence of artemisinin resistance, the team believes their findings could aid the design of new treatments against drug-resistant parasites.
They reported the findings in Nature Communications.
Previously, only 2 targets of artemisinin had been identified, and their correlation with the parasite-killing effect of the drug had been questioned.
Lin Qingsong, PhD, of the National University of Singapore, and his colleagues identified 124 protein targets of artemisinin in P falciparum. Many of these newly identified protein targets are involved in essential biological processes in the parasite, thus explaining artemisinin’s potent killing effect.
The research suggests that, through its promiscuous targeting mechanism, artemisinin targets the blood-eating nature of the malaria parasite, binding to a broad spectrum of targets simultaneously and fatally disrupting the biochemistry of the parasite.
The study also showed that the main activator of artemisinin is heme, an iron-containing compound that is either biosynthesized by the parasite at its early developmental ring stage or derived from hemoglobin digestion in the later stages.
The drug activation level was found to be much lower in ring-stage parasites, given that artemisinin activation requires heme, which is of much lower abundance and is biosynthesized by the parasite.
In comparison, during the late stages of its life cycle, the parasite actively digests the hemoglobin in infected blood cells as its primary energy source. This releases large amounts of heme, and the drug is able to specifically respond to parasite-infected cells and effectively attack the disease-causing parasites.
“The current findings not only provide a more complete picture of how artemisinin and its derivatives work but also suggest new ways of using the drug,” Dr Lin said. “For instance, to improve drug activation at ring stage, we can explore enhancing the level of heme biosynthesis in the parasite.”
“By understanding that hemoglobin digestion releases huge amounts of heme, which brings about the effective killing mechanism in the later stages, we can also consider prolonging the treatment time to ensure that the drug can effectively kill the parasite through multiple cycles.”
In addition, the researchers are planning to develop novel artemisinin analogues with more specific targeting properties.
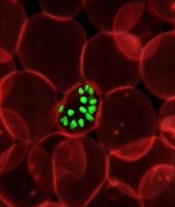
infecting a red blood cell
Photo courtesy of St. Jude
Children’s Research Hospital
Researchers say they have gained a better understanding of how the antimalarial drug artemisinin kills the Plasmodium falciparum parasite.
A chemical proteomics analysis revealed more than 120 protein targets of artemisinin and the mechanism that activates its killing effect.
Given the emergence of artemisinin resistance, the team believes their findings could aid the design of new treatments against drug-resistant parasites.
They reported the findings in Nature Communications.
Previously, only 2 targets of artemisinin had been identified, and their correlation with the parasite-killing effect of the drug had been questioned.
Lin Qingsong, PhD, of the National University of Singapore, and his colleagues identified 124 protein targets of artemisinin in P falciparum. Many of these newly identified protein targets are involved in essential biological processes in the parasite, thus explaining artemisinin’s potent killing effect.
The research suggests that, through its promiscuous targeting mechanism, artemisinin targets the blood-eating nature of the malaria parasite, binding to a broad spectrum of targets simultaneously and fatally disrupting the biochemistry of the parasite.
The study also showed that the main activator of artemisinin is heme, an iron-containing compound that is either biosynthesized by the parasite at its early developmental ring stage or derived from hemoglobin digestion in the later stages.
The drug activation level was found to be much lower in ring-stage parasites, given that artemisinin activation requires heme, which is of much lower abundance and is biosynthesized by the parasite.
In comparison, during the late stages of its life cycle, the parasite actively digests the hemoglobin in infected blood cells as its primary energy source. This releases large amounts of heme, and the drug is able to specifically respond to parasite-infected cells and effectively attack the disease-causing parasites.
“The current findings not only provide a more complete picture of how artemisinin and its derivatives work but also suggest new ways of using the drug,” Dr Lin said. “For instance, to improve drug activation at ring stage, we can explore enhancing the level of heme biosynthesis in the parasite.”
“By understanding that hemoglobin digestion releases huge amounts of heme, which brings about the effective killing mechanism in the later stages, we can also consider prolonging the treatment time to ensure that the drug can effectively kill the parasite through multiple cycles.”
In addition, the researchers are planning to develop novel artemisinin analogues with more specific targeting properties.