User login
Intervention helps kids stay active after cancer treatment
ORLANDO—Results of a pilot study suggest a web-based, reward-driven intervention can motivate adolescent cancer survivors to stay physically active.
Time spent performing moderate-to-vigorous physical activity (MVPA) increased by an average of 5 minutes a week for subjects who were randomized to the intervention.
For control subjects, MVPA decreased by an average of 24 minutes a week.
These findings were presented at the 2018 Cancer Survivorship Symposium (abstract 102).
“Compared to the general population, childhood cancer survivors have an increased risk for obesity and metabolic syndrome, conditions that can lead to heart disease, stroke, and diabetes, so it is really important that they are physically active,” said study investigator Carrie R. Howell, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“By intervening in this young age group, we hope to help kids develop healthy exercise habits for life.”
Dr Howell and her colleagues studied cancer survivors, ages 11 to 15, who were no longer receiving cancer treatment and were physically active less than 60 minutes a day.
The subjects were randomized to the intervention or to a control group. Controls received a wearable activity monitor and an educational handout with information about the importance of physical activity and examples of activities.
The intervention group received the handout and activity monitor but also had access to an interactive website. On at least a weekly basis, subjects would connect their monitor to a computer and log their activity through the website. Upon achieving certain thresholds of activity, they received rewards, such as T-shirts and gift cards by mail.
At the beginning and end of the study, participants visited St. Jude for an assessment of their physical fitness (strength, flexibility, and endurance) and neurocognitive measures (attention and memory), as well as health-related quality of life (assessed using the Pediatric Quality of Life Inventory questionnaire).
Results
Seventy-eight cancer survivors completed the 24-week study, 53 of them in the intervention group and 25 in the control group.
MVPA increased by an average of 4.7 minutes per week in the intervention group and decreased by an average of 24.3 minutes per week in the control group.
“In this age group, it is common to see a decrease in physical activity over time, even among healthy kids,” Dr Howell said. “Therefore, we are encouraged that our intervention was successful at maintaining physical activity levels, but a longer program may be needed to create lasting exercise habits.”
In addition to increases in MVPA, the intervention group had the following improvements in fitness:
- Increase in hand grip strength from an average of 19.9 kg to 21.0 kg
- Increase in number of push-ups from an average of 15 to 18
- Increase in number of sit-ups from an average of 11 to 14.
Furthermore, subjects in the intervention group saw their verbal fluency z-score increase by an average of 0.13 points and their general cognition z-score increase by an average of 0.23 points.
Their quality of life scores increased as well. Both overall quality of life and physical-function-related quality of life scores increased from an average of 74.2 to 78.0.
Control subjects had no significant changes in fitness, neurocognitive measures, or quality of life.
This study was supported by the National Cancer Institute, the American Lebanese Syrian Associated Charities, and HopeLab.
Based on the results of this study, the investigators have designed a larger trial (ALTE1631) to test a web-based physical activity intervention. They hope to enroll 384 survivors of childhood acute lymphoblastic leukemia at institutions across the US. The intervention will last a year, with follow-up at 18 months.
Further down the line, the investigators plan to explore the relationship between physical activity and cognition.
ORLANDO—Results of a pilot study suggest a web-based, reward-driven intervention can motivate adolescent cancer survivors to stay physically active.
Time spent performing moderate-to-vigorous physical activity (MVPA) increased by an average of 5 minutes a week for subjects who were randomized to the intervention.
For control subjects, MVPA decreased by an average of 24 minutes a week.
These findings were presented at the 2018 Cancer Survivorship Symposium (abstract 102).
“Compared to the general population, childhood cancer survivors have an increased risk for obesity and metabolic syndrome, conditions that can lead to heart disease, stroke, and diabetes, so it is really important that they are physically active,” said study investigator Carrie R. Howell, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“By intervening in this young age group, we hope to help kids develop healthy exercise habits for life.”
Dr Howell and her colleagues studied cancer survivors, ages 11 to 15, who were no longer receiving cancer treatment and were physically active less than 60 minutes a day.
The subjects were randomized to the intervention or to a control group. Controls received a wearable activity monitor and an educational handout with information about the importance of physical activity and examples of activities.
The intervention group received the handout and activity monitor but also had access to an interactive website. On at least a weekly basis, subjects would connect their monitor to a computer and log their activity through the website. Upon achieving certain thresholds of activity, they received rewards, such as T-shirts and gift cards by mail.
At the beginning and end of the study, participants visited St. Jude for an assessment of their physical fitness (strength, flexibility, and endurance) and neurocognitive measures (attention and memory), as well as health-related quality of life (assessed using the Pediatric Quality of Life Inventory questionnaire).
Results
Seventy-eight cancer survivors completed the 24-week study, 53 of them in the intervention group and 25 in the control group.
MVPA increased by an average of 4.7 minutes per week in the intervention group and decreased by an average of 24.3 minutes per week in the control group.
“In this age group, it is common to see a decrease in physical activity over time, even among healthy kids,” Dr Howell said. “Therefore, we are encouraged that our intervention was successful at maintaining physical activity levels, but a longer program may be needed to create lasting exercise habits.”
In addition to increases in MVPA, the intervention group had the following improvements in fitness:
- Increase in hand grip strength from an average of 19.9 kg to 21.0 kg
- Increase in number of push-ups from an average of 15 to 18
- Increase in number of sit-ups from an average of 11 to 14.
Furthermore, subjects in the intervention group saw their verbal fluency z-score increase by an average of 0.13 points and their general cognition z-score increase by an average of 0.23 points.
Their quality of life scores increased as well. Both overall quality of life and physical-function-related quality of life scores increased from an average of 74.2 to 78.0.
Control subjects had no significant changes in fitness, neurocognitive measures, or quality of life.
This study was supported by the National Cancer Institute, the American Lebanese Syrian Associated Charities, and HopeLab.
Based on the results of this study, the investigators have designed a larger trial (ALTE1631) to test a web-based physical activity intervention. They hope to enroll 384 survivors of childhood acute lymphoblastic leukemia at institutions across the US. The intervention will last a year, with follow-up at 18 months.
Further down the line, the investigators plan to explore the relationship between physical activity and cognition.
ORLANDO—Results of a pilot study suggest a web-based, reward-driven intervention can motivate adolescent cancer survivors to stay physically active.
Time spent performing moderate-to-vigorous physical activity (MVPA) increased by an average of 5 minutes a week for subjects who were randomized to the intervention.
For control subjects, MVPA decreased by an average of 24 minutes a week.
These findings were presented at the 2018 Cancer Survivorship Symposium (abstract 102).
“Compared to the general population, childhood cancer survivors have an increased risk for obesity and metabolic syndrome, conditions that can lead to heart disease, stroke, and diabetes, so it is really important that they are physically active,” said study investigator Carrie R. Howell, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“By intervening in this young age group, we hope to help kids develop healthy exercise habits for life.”
Dr Howell and her colleagues studied cancer survivors, ages 11 to 15, who were no longer receiving cancer treatment and were physically active less than 60 minutes a day.
The subjects were randomized to the intervention or to a control group. Controls received a wearable activity monitor and an educational handout with information about the importance of physical activity and examples of activities.
The intervention group received the handout and activity monitor but also had access to an interactive website. On at least a weekly basis, subjects would connect their monitor to a computer and log their activity through the website. Upon achieving certain thresholds of activity, they received rewards, such as T-shirts and gift cards by mail.
At the beginning and end of the study, participants visited St. Jude for an assessment of their physical fitness (strength, flexibility, and endurance) and neurocognitive measures (attention and memory), as well as health-related quality of life (assessed using the Pediatric Quality of Life Inventory questionnaire).
Results
Seventy-eight cancer survivors completed the 24-week study, 53 of them in the intervention group and 25 in the control group.
MVPA increased by an average of 4.7 minutes per week in the intervention group and decreased by an average of 24.3 minutes per week in the control group.
“In this age group, it is common to see a decrease in physical activity over time, even among healthy kids,” Dr Howell said. “Therefore, we are encouraged that our intervention was successful at maintaining physical activity levels, but a longer program may be needed to create lasting exercise habits.”
In addition to increases in MVPA, the intervention group had the following improvements in fitness:
- Increase in hand grip strength from an average of 19.9 kg to 21.0 kg
- Increase in number of push-ups from an average of 15 to 18
- Increase in number of sit-ups from an average of 11 to 14.
Furthermore, subjects in the intervention group saw their verbal fluency z-score increase by an average of 0.13 points and their general cognition z-score increase by an average of 0.23 points.
Their quality of life scores increased as well. Both overall quality of life and physical-function-related quality of life scores increased from an average of 74.2 to 78.0.
Control subjects had no significant changes in fitness, neurocognitive measures, or quality of life.
This study was supported by the National Cancer Institute, the American Lebanese Syrian Associated Charities, and HopeLab.
Based on the results of this study, the investigators have designed a larger trial (ALTE1631) to test a web-based physical activity intervention. They hope to enroll 384 survivors of childhood acute lymphoblastic leukemia at institutions across the US. The intervention will last a year, with follow-up at 18 months.
Further down the line, the investigators plan to explore the relationship between physical activity and cognition.
Study reveals lack of sexual aids for cancer survivors
ORLANDO—A new study suggests many US cancer centers do not have therapeutic aids for patients who experience sexual dysfunction after cancer treatment.
Of 25 cancer centers polled, 80% said they had no sexual aids available on site for men, and 64% said they had no such aids for women.
Sharon Bober, PhD, of the Dana-Farber Cancer Institute in Boston, Massachusetts, and her colleagues presented this research at the 2018 Cancer Survivorship Symposium (abstract 134*).
“[P]roviding sexual aids is one step toward treating sexual health like any other aspect of survivorship care,” Dr Bober said.
“It should be no different than providing wigs and head coverings to women who have lost their hair due to chemotherapy. It’s important to give patients the message that regaining sexual health is a perfectly valid and life-affirming aspect of regaining overall quality of life.”
Dr Bober and her colleagues conducted this study to determine the availability of sexual aids at 25 National Cancer Institute-designated cancer centers.
The researchers called these centers posing as a spouse, adult child, or sibling of a patient. The team made separate calls to ask about sexual aids for women and those for men.
Women’s sexual aids
Twenty-four percent of cancer centers (n=6) said they had sexual aids for women, 64% (n=16) did not, and 12% of centers were unreachable (n=3).
The most common aids were personal lubrication, vaginal moisturizer, and vaginal dilators—all of which were available at 5 centers.
Three centers had vibrators, 2 had books/pamphlets, 2 had pelvic floor exercisers, and 2 had product lists.
Men’s sexual aids
Twelve percent of cancer centers (n=3) said they had sexual aids for men, 80% (n=20) did not, and 8% (n=2) were unreachable.
Two centers said they had personal lubrication available for men, 2 had penile support rings, 1 had vacuum erection devices, and 1 had books/pamphlets.
Next steps
Now, Dr Bober and her colleagues hope to query the other 44 National Cancer Institute-designated cancer centers to see what products they are selling and perhaps conduct patient surveys to find out what types of resources are most useful for cancer survivors.
“What we really need to do is go to the centers that are successfully providing sexual health products and find out how they promote and provide resources to their patients,” Dr Bober said.
“We can’t keep the conversation at the 10,000-foot level. We need to talk concretely about how to partner with providers to make sexual health resources, including sexual health aids, available so cancer survivors can get the help that they need.”
*Information presented differs from the abstract.
ORLANDO—A new study suggests many US cancer centers do not have therapeutic aids for patients who experience sexual dysfunction after cancer treatment.
Of 25 cancer centers polled, 80% said they had no sexual aids available on site for men, and 64% said they had no such aids for women.
Sharon Bober, PhD, of the Dana-Farber Cancer Institute in Boston, Massachusetts, and her colleagues presented this research at the 2018 Cancer Survivorship Symposium (abstract 134*).
“[P]roviding sexual aids is one step toward treating sexual health like any other aspect of survivorship care,” Dr Bober said.
“It should be no different than providing wigs and head coverings to women who have lost their hair due to chemotherapy. It’s important to give patients the message that regaining sexual health is a perfectly valid and life-affirming aspect of regaining overall quality of life.”
Dr Bober and her colleagues conducted this study to determine the availability of sexual aids at 25 National Cancer Institute-designated cancer centers.
The researchers called these centers posing as a spouse, adult child, or sibling of a patient. The team made separate calls to ask about sexual aids for women and those for men.
Women’s sexual aids
Twenty-four percent of cancer centers (n=6) said they had sexual aids for women, 64% (n=16) did not, and 12% of centers were unreachable (n=3).
The most common aids were personal lubrication, vaginal moisturizer, and vaginal dilators—all of which were available at 5 centers.
Three centers had vibrators, 2 had books/pamphlets, 2 had pelvic floor exercisers, and 2 had product lists.
Men’s sexual aids
Twelve percent of cancer centers (n=3) said they had sexual aids for men, 80% (n=20) did not, and 8% (n=2) were unreachable.
Two centers said they had personal lubrication available for men, 2 had penile support rings, 1 had vacuum erection devices, and 1 had books/pamphlets.
Next steps
Now, Dr Bober and her colleagues hope to query the other 44 National Cancer Institute-designated cancer centers to see what products they are selling and perhaps conduct patient surveys to find out what types of resources are most useful for cancer survivors.
“What we really need to do is go to the centers that are successfully providing sexual health products and find out how they promote and provide resources to their patients,” Dr Bober said.
“We can’t keep the conversation at the 10,000-foot level. We need to talk concretely about how to partner with providers to make sexual health resources, including sexual health aids, available so cancer survivors can get the help that they need.”
*Information presented differs from the abstract.
ORLANDO—A new study suggests many US cancer centers do not have therapeutic aids for patients who experience sexual dysfunction after cancer treatment.
Of 25 cancer centers polled, 80% said they had no sexual aids available on site for men, and 64% said they had no such aids for women.
Sharon Bober, PhD, of the Dana-Farber Cancer Institute in Boston, Massachusetts, and her colleagues presented this research at the 2018 Cancer Survivorship Symposium (abstract 134*).
“[P]roviding sexual aids is one step toward treating sexual health like any other aspect of survivorship care,” Dr Bober said.
“It should be no different than providing wigs and head coverings to women who have lost their hair due to chemotherapy. It’s important to give patients the message that regaining sexual health is a perfectly valid and life-affirming aspect of regaining overall quality of life.”
Dr Bober and her colleagues conducted this study to determine the availability of sexual aids at 25 National Cancer Institute-designated cancer centers.
The researchers called these centers posing as a spouse, adult child, or sibling of a patient. The team made separate calls to ask about sexual aids for women and those for men.
Women’s sexual aids
Twenty-four percent of cancer centers (n=6) said they had sexual aids for women, 64% (n=16) did not, and 12% of centers were unreachable (n=3).
The most common aids were personal lubrication, vaginal moisturizer, and vaginal dilators—all of which were available at 5 centers.
Three centers had vibrators, 2 had books/pamphlets, 2 had pelvic floor exercisers, and 2 had product lists.
Men’s sexual aids
Twelve percent of cancer centers (n=3) said they had sexual aids for men, 80% (n=20) did not, and 8% (n=2) were unreachable.
Two centers said they had personal lubrication available for men, 2 had penile support rings, 1 had vacuum erection devices, and 1 had books/pamphlets.
Next steps
Now, Dr Bober and her colleagues hope to query the other 44 National Cancer Institute-designated cancer centers to see what products they are selling and perhaps conduct patient surveys to find out what types of resources are most useful for cancer survivors.
“What we really need to do is go to the centers that are successfully providing sexual health products and find out how they promote and provide resources to their patients,” Dr Bober said.
“We can’t keep the conversation at the 10,000-foot level. We need to talk concretely about how to partner with providers to make sexual health resources, including sexual health aids, available so cancer survivors can get the help that they need.”
*Information presented differs from the abstract.
ASCO, NCCN release guidelines on checkpoint inhibitors
Two cancer organizations have released guidelines for managing the side effects of immune checkpoint inhibitors.
The American Society of Clinical Oncology (ASCO) and National Comprehensive Cancer Network® (NCCN) developed these guidelines because patients who receive immune checkpoint inhibitors experience unique side effects that can be severe, irreversible, and life-threatening.
Given that checkpoint inhibitors have entered the clinic fairly recently, clinicians may need guidance in recognizing and treating these side effects.
“With rapidly increasing use of immune checkpoint inhibitors, it is imperative that clinicians are knowledgeable about their unique toxicity profiles,” said ASCO Chief Executive Officer Clifford A. Hudis, MD.
“These new guidelines from ASCO and NCCN will help our community continue to provide the highest quality of care to all patients as they incorporate these agents into routine care.”
To the develop their guidelines, ASCO and NCCN convened multidisciplinary panels with representation from hematology, oncology, dermatology, gastroenterology, rheumatology, pulmonology, endocrinology, urology, neurology, emergency medicine, and nursing, as well as patient advocacy experts.
The clinical recommendations are based on a systematic review of the literature and an informal consensus process. The recommendations pertain only to checkpoint inhibitors currently approved in the US—pembrolizumab, nivolumab, atezolizumab, avelumab, ipilimumab, and durvalumab.
Key recommendations from the guidelines include:
- In general, checkpoint inhibitors can be continued with close monitoring if patients experience grade 1 toxicities, with the exception of some neurologic, cardiac, and hematologic toxicities.
- For grade 2 toxicities, checkpoint inhibitors should be held until symptoms and/or lab values revert to grade 1 levels or lower. Corticosteroids may be offered.
- For grade 3 toxicities, patients should receive high-dose corticosteroids for at least 6 weeks. Extreme caution is recommended when restarting immunotherapy after grade 3 toxicity, if it is restarted at all.
- In general, grade 4 toxicities necessitate stopping checkpoint inhibitor therapy permanently.
Consult the guidelines for specific recommendations.
ASCO’s guidelines, “Management of Immune-Related Adverse Events in Patients Treated With Immune Checkpoint Inhibitor Therapy: American Society of Clinical Oncology Clinical Practice Guideline,” have been published in the Journal of Clinical Oncology.
NCCN’s guidelines, “Management of Immunotherapy-Related Toxicities (Immune Checkpoint Inhibitor-Related Toxicities),” are available on the NCCN website.
Two cancer organizations have released guidelines for managing the side effects of immune checkpoint inhibitors.
The American Society of Clinical Oncology (ASCO) and National Comprehensive Cancer Network® (NCCN) developed these guidelines because patients who receive immune checkpoint inhibitors experience unique side effects that can be severe, irreversible, and life-threatening.
Given that checkpoint inhibitors have entered the clinic fairly recently, clinicians may need guidance in recognizing and treating these side effects.
“With rapidly increasing use of immune checkpoint inhibitors, it is imperative that clinicians are knowledgeable about their unique toxicity profiles,” said ASCO Chief Executive Officer Clifford A. Hudis, MD.
“These new guidelines from ASCO and NCCN will help our community continue to provide the highest quality of care to all patients as they incorporate these agents into routine care.”
To the develop their guidelines, ASCO and NCCN convened multidisciplinary panels with representation from hematology, oncology, dermatology, gastroenterology, rheumatology, pulmonology, endocrinology, urology, neurology, emergency medicine, and nursing, as well as patient advocacy experts.
The clinical recommendations are based on a systematic review of the literature and an informal consensus process. The recommendations pertain only to checkpoint inhibitors currently approved in the US—pembrolizumab, nivolumab, atezolizumab, avelumab, ipilimumab, and durvalumab.
Key recommendations from the guidelines include:
- In general, checkpoint inhibitors can be continued with close monitoring if patients experience grade 1 toxicities, with the exception of some neurologic, cardiac, and hematologic toxicities.
- For grade 2 toxicities, checkpoint inhibitors should be held until symptoms and/or lab values revert to grade 1 levels or lower. Corticosteroids may be offered.
- For grade 3 toxicities, patients should receive high-dose corticosteroids for at least 6 weeks. Extreme caution is recommended when restarting immunotherapy after grade 3 toxicity, if it is restarted at all.
- In general, grade 4 toxicities necessitate stopping checkpoint inhibitor therapy permanently.
Consult the guidelines for specific recommendations.
ASCO’s guidelines, “Management of Immune-Related Adverse Events in Patients Treated With Immune Checkpoint Inhibitor Therapy: American Society of Clinical Oncology Clinical Practice Guideline,” have been published in the Journal of Clinical Oncology.
NCCN’s guidelines, “Management of Immunotherapy-Related Toxicities (Immune Checkpoint Inhibitor-Related Toxicities),” are available on the NCCN website.
Two cancer organizations have released guidelines for managing the side effects of immune checkpoint inhibitors.
The American Society of Clinical Oncology (ASCO) and National Comprehensive Cancer Network® (NCCN) developed these guidelines because patients who receive immune checkpoint inhibitors experience unique side effects that can be severe, irreversible, and life-threatening.
Given that checkpoint inhibitors have entered the clinic fairly recently, clinicians may need guidance in recognizing and treating these side effects.
“With rapidly increasing use of immune checkpoint inhibitors, it is imperative that clinicians are knowledgeable about their unique toxicity profiles,” said ASCO Chief Executive Officer Clifford A. Hudis, MD.
“These new guidelines from ASCO and NCCN will help our community continue to provide the highest quality of care to all patients as they incorporate these agents into routine care.”
To the develop their guidelines, ASCO and NCCN convened multidisciplinary panels with representation from hematology, oncology, dermatology, gastroenterology, rheumatology, pulmonology, endocrinology, urology, neurology, emergency medicine, and nursing, as well as patient advocacy experts.
The clinical recommendations are based on a systematic review of the literature and an informal consensus process. The recommendations pertain only to checkpoint inhibitors currently approved in the US—pembrolizumab, nivolumab, atezolizumab, avelumab, ipilimumab, and durvalumab.
Key recommendations from the guidelines include:
- In general, checkpoint inhibitors can be continued with close monitoring if patients experience grade 1 toxicities, with the exception of some neurologic, cardiac, and hematologic toxicities.
- For grade 2 toxicities, checkpoint inhibitors should be held until symptoms and/or lab values revert to grade 1 levels or lower. Corticosteroids may be offered.
- For grade 3 toxicities, patients should receive high-dose corticosteroids for at least 6 weeks. Extreme caution is recommended when restarting immunotherapy after grade 3 toxicity, if it is restarted at all.
- In general, grade 4 toxicities necessitate stopping checkpoint inhibitor therapy permanently.
Consult the guidelines for specific recommendations.
ASCO’s guidelines, “Management of Immune-Related Adverse Events in Patients Treated With Immune Checkpoint Inhibitor Therapy: American Society of Clinical Oncology Clinical Practice Guideline,” have been published in the Journal of Clinical Oncology.
NCCN’s guidelines, “Management of Immunotherapy-Related Toxicities (Immune Checkpoint Inhibitor-Related Toxicities),” are available on the NCCN website.
Child’s cancer diagnosis can affect mother’s income long-term
A study conducted in Sweden revealed that social benefits can ease financial burdens for parents of children recently diagnosed with cancer.
However, the study also showed that mothers experienced persistently lower income after benefits diminished.
Ayako Hiyoshi, PhD, of Örebro University in Örebro, Sweden, and her colleagues detailed these findings in Cancer.
The researchers gathered information from Swedish national registers and examined the trajectories of parents’ income from different sources.
Parents of children with cancer diagnosed between 2004 and 2009 were identified and matched with parents of children without cancer (reference parents).
In total, 20,091 families were followed from the year before cancer diagnosis to a maximum of 8 years.
The researchers noted that, around the time of a child’s cancer diagnosis, total income (from all sources) was, on average, higher in mothers of children with cancer than in reference mothers.
The ratio of mean total income for mothers of children with cancer, compared to reference mothers, was 1.032 at 1 year prior to the child’s diagnosis and 1.064 the year of diagnosis.
For fathers of children with cancer, total income was slightly lower than reference fathers’ income. The ratios were 0.987 at 1 year prior to diagnosis and 0.995 the year of diagnosis.
The researchers also noted that parents’ income from work was at its lowest around the time of a child’s cancer diagnosis but increased with time.
At cancer diagnosis, the ratio of mean income from work was 0.642 for mothers and 0.858 for fathers. One year later, the ratios were 0.786 and 0.956, respectively. At 3 years, the ratios were 0.876 and 0.986, respectively. At 6 years, the ratios were 0.856 and 1.058, respectively.
The researchers pointed out that sickness and childcare-related benefits, which compensated for income loss, were greater for parents of children with cancer than for reference parents. However, social benefits diminished over time.
One year prior to cancer diagnosis, the ratio of sickness benefits was 3.495 for mothers and 5.213 for fathers. The year of diagnosis, the ratios were 4.785 and 5.795, respectively. At 3 years, the ratios were 1.404 and 1.339, respectively. And at 6 years, the ratios were 0.931 and 1.421, respectively.
One year prior to cancer diagnosis, the ratio of childcare-related benefits was 2.830 for mothers and 3.514 for fathers. The year of diagnosis, the ratios were 4.553 and 4.930, respectively. At 3 years, the ratios were 2.225 and 1.948, respectively. And at 6 years, the ratios were 1.272 and 1.095, respectively.
The decline of social benefits over time meant that cancer mothers’ total income became lower than that of reference mothers, and this difference persisted over the period studied. This was not the case for cancer fathers, however.
The ratio of income from all sources for cancer mothers compared to reference mothers was 1.064 the year of diagnosis, 0.985 at 2 years, 0.966 at 4 years, and 0.934 at 6 years.
The ratio of income from all sources for cancer fathers compared to reference fathers was 0.995 the year of diagnosis, 0.993 at 2 years, 0.998 at 4 years, and 1.029 at 6 years.
“A significant and unexpected finding was that, although income from employment stayed lower for several years for mothers, total income was higher for mothers of children with cancer around the time of the child’s cancer diagnosis when the compensation from social benefits were included,” Dr Hiyoshi said.
“The persistently lower income from employment for mothers of children with cancer compared with mothers of cancer-free children implies potential long-term consequences for the mothers of children with cancer, including their career and future pension in old age.” ![]()
A study conducted in Sweden revealed that social benefits can ease financial burdens for parents of children recently diagnosed with cancer.
However, the study also showed that mothers experienced persistently lower income after benefits diminished.
Ayako Hiyoshi, PhD, of Örebro University in Örebro, Sweden, and her colleagues detailed these findings in Cancer.
The researchers gathered information from Swedish national registers and examined the trajectories of parents’ income from different sources.
Parents of children with cancer diagnosed between 2004 and 2009 were identified and matched with parents of children without cancer (reference parents).
In total, 20,091 families were followed from the year before cancer diagnosis to a maximum of 8 years.
The researchers noted that, around the time of a child’s cancer diagnosis, total income (from all sources) was, on average, higher in mothers of children with cancer than in reference mothers.
The ratio of mean total income for mothers of children with cancer, compared to reference mothers, was 1.032 at 1 year prior to the child’s diagnosis and 1.064 the year of diagnosis.
For fathers of children with cancer, total income was slightly lower than reference fathers’ income. The ratios were 0.987 at 1 year prior to diagnosis and 0.995 the year of diagnosis.
The researchers also noted that parents’ income from work was at its lowest around the time of a child’s cancer diagnosis but increased with time.
At cancer diagnosis, the ratio of mean income from work was 0.642 for mothers and 0.858 for fathers. One year later, the ratios were 0.786 and 0.956, respectively. At 3 years, the ratios were 0.876 and 0.986, respectively. At 6 years, the ratios were 0.856 and 1.058, respectively.
The researchers pointed out that sickness and childcare-related benefits, which compensated for income loss, were greater for parents of children with cancer than for reference parents. However, social benefits diminished over time.
One year prior to cancer diagnosis, the ratio of sickness benefits was 3.495 for mothers and 5.213 for fathers. The year of diagnosis, the ratios were 4.785 and 5.795, respectively. At 3 years, the ratios were 1.404 and 1.339, respectively. And at 6 years, the ratios were 0.931 and 1.421, respectively.
One year prior to cancer diagnosis, the ratio of childcare-related benefits was 2.830 for mothers and 3.514 for fathers. The year of diagnosis, the ratios were 4.553 and 4.930, respectively. At 3 years, the ratios were 2.225 and 1.948, respectively. And at 6 years, the ratios were 1.272 and 1.095, respectively.
The decline of social benefits over time meant that cancer mothers’ total income became lower than that of reference mothers, and this difference persisted over the period studied. This was not the case for cancer fathers, however.
The ratio of income from all sources for cancer mothers compared to reference mothers was 1.064 the year of diagnosis, 0.985 at 2 years, 0.966 at 4 years, and 0.934 at 6 years.
The ratio of income from all sources for cancer fathers compared to reference fathers was 0.995 the year of diagnosis, 0.993 at 2 years, 0.998 at 4 years, and 1.029 at 6 years.
“A significant and unexpected finding was that, although income from employment stayed lower for several years for mothers, total income was higher for mothers of children with cancer around the time of the child’s cancer diagnosis when the compensation from social benefits were included,” Dr Hiyoshi said.
“The persistently lower income from employment for mothers of children with cancer compared with mothers of cancer-free children implies potential long-term consequences for the mothers of children with cancer, including their career and future pension in old age.” ![]()
A study conducted in Sweden revealed that social benefits can ease financial burdens for parents of children recently diagnosed with cancer.
However, the study also showed that mothers experienced persistently lower income after benefits diminished.
Ayako Hiyoshi, PhD, of Örebro University in Örebro, Sweden, and her colleagues detailed these findings in Cancer.
The researchers gathered information from Swedish national registers and examined the trajectories of parents’ income from different sources.
Parents of children with cancer diagnosed between 2004 and 2009 were identified and matched with parents of children without cancer (reference parents).
In total, 20,091 families were followed from the year before cancer diagnosis to a maximum of 8 years.
The researchers noted that, around the time of a child’s cancer diagnosis, total income (from all sources) was, on average, higher in mothers of children with cancer than in reference mothers.
The ratio of mean total income for mothers of children with cancer, compared to reference mothers, was 1.032 at 1 year prior to the child’s diagnosis and 1.064 the year of diagnosis.
For fathers of children with cancer, total income was slightly lower than reference fathers’ income. The ratios were 0.987 at 1 year prior to diagnosis and 0.995 the year of diagnosis.
The researchers also noted that parents’ income from work was at its lowest around the time of a child’s cancer diagnosis but increased with time.
At cancer diagnosis, the ratio of mean income from work was 0.642 for mothers and 0.858 for fathers. One year later, the ratios were 0.786 and 0.956, respectively. At 3 years, the ratios were 0.876 and 0.986, respectively. At 6 years, the ratios were 0.856 and 1.058, respectively.
The researchers pointed out that sickness and childcare-related benefits, which compensated for income loss, were greater for parents of children with cancer than for reference parents. However, social benefits diminished over time.
One year prior to cancer diagnosis, the ratio of sickness benefits was 3.495 for mothers and 5.213 for fathers. The year of diagnosis, the ratios were 4.785 and 5.795, respectively. At 3 years, the ratios were 1.404 and 1.339, respectively. And at 6 years, the ratios were 0.931 and 1.421, respectively.
One year prior to cancer diagnosis, the ratio of childcare-related benefits was 2.830 for mothers and 3.514 for fathers. The year of diagnosis, the ratios were 4.553 and 4.930, respectively. At 3 years, the ratios were 2.225 and 1.948, respectively. And at 6 years, the ratios were 1.272 and 1.095, respectively.
The decline of social benefits over time meant that cancer mothers’ total income became lower than that of reference mothers, and this difference persisted over the period studied. This was not the case for cancer fathers, however.
The ratio of income from all sources for cancer mothers compared to reference mothers was 1.064 the year of diagnosis, 0.985 at 2 years, 0.966 at 4 years, and 0.934 at 6 years.
The ratio of income from all sources for cancer fathers compared to reference fathers was 0.995 the year of diagnosis, 0.993 at 2 years, 0.998 at 4 years, and 1.029 at 6 years.
“A significant and unexpected finding was that, although income from employment stayed lower for several years for mothers, total income was higher for mothers of children with cancer around the time of the child’s cancer diagnosis when the compensation from social benefits were included,” Dr Hiyoshi said.
“The persistently lower income from employment for mothers of children with cancer compared with mothers of cancer-free children implies potential long-term consequences for the mothers of children with cancer, including their career and future pension in old age.” ![]()
Team recommends changes to trial guidelines
Researchers have recommended changes to international guidelines used in the development of clinical trials.
The group’s goal is to improve the use of patient-reported outcomes (PROs)—feedback from patients about how the clinical trial has affected their overall health and quality of life.
“Patient-reported outcome data from clinical trials can provide valuable evidence to inform shared-decision making, pharmaceutical labeling claims, clinical guidelines, and health policy,” said Melanie Calvert, PhD, of the University of Birmingham in Edgbaston, Birmingham, England.
“However, clinical trial protocols often lack important information regarding the collection of quality of life and symptom data. Working in collaboration with international stakeholders, we have developed consensus-based, PRO-specific protocol guidance to help ensure high-quality data to inform patient-centered care.”
Dr Calvert and her colleagues published the guidance in JAMA.
The guidance is known as the SPIRIT-PRO Extension. The SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) statement, which was published in 2013, was intended to improve trial protocols by providing evidence-based recommendations for the minimum set of items to be addressed.
To add a PRO component to SPIRIT, Dr Calvert and her colleagues conducted a systematic review of existing PRO-specific protocol guidance. A taskforce used this data to compile a list of potential PRO-specific protocol items.
The review revealed 162 PRO-specific protocol recommendations, and the task force reduced this to 56. After 138 international stakeholders and 99 Delphi panelists weighed in, the final recommendations were agreed upon by 29 participants at a consensus meeting.
The final recommendations include 11 extensions and 5 elaborations to the SPIRIT checklist. The recommendations focus on PRO-specific issues relating to objectives, eligibility criteria, data collection, monitoring, and other aspects of trials.
“While this guidance has been developed for trials where PROs are a primary or key secondary outcome, we are actively encouraging protocol writers to consider use of this guidance in all trials or clinical research studies where PROs are collected,” Dr Calvert said.
“The guidance does not aim to be prescriptive, but instead to encourage and facilitate careful planning of PRO components of trials and thereby improve PRO trial design, which we hope will help staff and patients understand the rationale for PRO assessment, improve PRO data completeness and quality, facilitate high-quality analysis and reporting, and ultimately improve the quality of the global PRO evidence base.” ![]()
Researchers have recommended changes to international guidelines used in the development of clinical trials.
The group’s goal is to improve the use of patient-reported outcomes (PROs)—feedback from patients about how the clinical trial has affected their overall health and quality of life.
“Patient-reported outcome data from clinical trials can provide valuable evidence to inform shared-decision making, pharmaceutical labeling claims, clinical guidelines, and health policy,” said Melanie Calvert, PhD, of the University of Birmingham in Edgbaston, Birmingham, England.
“However, clinical trial protocols often lack important information regarding the collection of quality of life and symptom data. Working in collaboration with international stakeholders, we have developed consensus-based, PRO-specific protocol guidance to help ensure high-quality data to inform patient-centered care.”
Dr Calvert and her colleagues published the guidance in JAMA.
The guidance is known as the SPIRIT-PRO Extension. The SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) statement, which was published in 2013, was intended to improve trial protocols by providing evidence-based recommendations for the minimum set of items to be addressed.
To add a PRO component to SPIRIT, Dr Calvert and her colleagues conducted a systematic review of existing PRO-specific protocol guidance. A taskforce used this data to compile a list of potential PRO-specific protocol items.
The review revealed 162 PRO-specific protocol recommendations, and the task force reduced this to 56. After 138 international stakeholders and 99 Delphi panelists weighed in, the final recommendations were agreed upon by 29 participants at a consensus meeting.
The final recommendations include 11 extensions and 5 elaborations to the SPIRIT checklist. The recommendations focus on PRO-specific issues relating to objectives, eligibility criteria, data collection, monitoring, and other aspects of trials.
“While this guidance has been developed for trials where PROs are a primary or key secondary outcome, we are actively encouraging protocol writers to consider use of this guidance in all trials or clinical research studies where PROs are collected,” Dr Calvert said.
“The guidance does not aim to be prescriptive, but instead to encourage and facilitate careful planning of PRO components of trials and thereby improve PRO trial design, which we hope will help staff and patients understand the rationale for PRO assessment, improve PRO data completeness and quality, facilitate high-quality analysis and reporting, and ultimately improve the quality of the global PRO evidence base.” ![]()
Researchers have recommended changes to international guidelines used in the development of clinical trials.
The group’s goal is to improve the use of patient-reported outcomes (PROs)—feedback from patients about how the clinical trial has affected their overall health and quality of life.
“Patient-reported outcome data from clinical trials can provide valuable evidence to inform shared-decision making, pharmaceutical labeling claims, clinical guidelines, and health policy,” said Melanie Calvert, PhD, of the University of Birmingham in Edgbaston, Birmingham, England.
“However, clinical trial protocols often lack important information regarding the collection of quality of life and symptom data. Working in collaboration with international stakeholders, we have developed consensus-based, PRO-specific protocol guidance to help ensure high-quality data to inform patient-centered care.”
Dr Calvert and her colleagues published the guidance in JAMA.
The guidance is known as the SPIRIT-PRO Extension. The SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) statement, which was published in 2013, was intended to improve trial protocols by providing evidence-based recommendations for the minimum set of items to be addressed.
To add a PRO component to SPIRIT, Dr Calvert and her colleagues conducted a systematic review of existing PRO-specific protocol guidance. A taskforce used this data to compile a list of potential PRO-specific protocol items.
The review revealed 162 PRO-specific protocol recommendations, and the task force reduced this to 56. After 138 international stakeholders and 99 Delphi panelists weighed in, the final recommendations were agreed upon by 29 participants at a consensus meeting.
The final recommendations include 11 extensions and 5 elaborations to the SPIRIT checklist. The recommendations focus on PRO-specific issues relating to objectives, eligibility criteria, data collection, monitoring, and other aspects of trials.
“While this guidance has been developed for trials where PROs are a primary or key secondary outcome, we are actively encouraging protocol writers to consider use of this guidance in all trials or clinical research studies where PROs are collected,” Dr Calvert said.
“The guidance does not aim to be prescriptive, but instead to encourage and facilitate careful planning of PRO components of trials and thereby improve PRO trial design, which we hope will help staff and patients understand the rationale for PRO assessment, improve PRO data completeness and quality, facilitate high-quality analysis and reporting, and ultimately improve the quality of the global PRO evidence base.” ![]()
Interim trial results may be misleading
Interim results from randomized trials may be misleading at times, according to research published in JAMA.
Researchers compared interim and final publications on randomized trials and found that, 21% of the time, results changed significantly.
“Changes between interim and final publication matter because clinicians and the public could have been misled about whether an intervention was beneficial, harmful, or ineffective,” said study author Lisa Schwartz, MD, of Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, New Hampshire.
She and her colleagues searched PubMed for randomized trials from 2006 to 2015 with “interim,” “not mature,” or “immature” in the title or abstract.
To identify final publications, they searched PubMed, ClinicalTrials.gov, and Web of Science through 2016. The team emailed authors of interim reports when no final publication was identified.
For interim and final publications reporting the same efficacy and or safety outcome, the researchers compared trial characteristics and prominence. They also categorized abstract conclusions (not different, beneficial, or harmful) and compared changes between interim and final publications.
Findings
Interim results were reported in 613 of 1267 screened publications.
Of those publications, 72% reported on trials stopped early (for benefit, harm, futility, or other problems). The remaining 171 ongoing trials (mostly in oncology, surgery, or cardiology) reported interim efficacy or safety results.
Forty-one percent of the publications stated that the interim analysis was specified in the protocol, but half provided no reason for the interim publication.
Final results were published for 98 of the 160 trials (61%) that were more than 1 year beyond the completion date.
The researchers compared 73 interim and final publications reporting the same efficacy or safety outcome. And they found that interim and final publications had similar prominence.
In most cases (79%), the abstract conclusions did not change from the interim publication to the final publication. However, for 21% of trials, there were significant changes.
For 4 trials, the conclusions changed from “no difference” between randomized to treatments to the study treatment being “beneficial.” In 3 trials, the conclusions changed from “not different” to “harmful or possibly harmful.”
In 6 trials, the conclusions changed from “beneficial” to “not different.” One trial changed from “beneficial” to “harmful,” and another changed from “inconclusive” to “noninferior.”
Dr Schwartz and her colleagues concluded that while most interim and final publications reached similar conclusions, frequent non-publication of final results can lead to confusion or unfounded assumptions with true treatment effects remaining unknown.
To safeguard against any such confusion, the researchers recommended routinely adding the word “interim” in the title and justifying the reason in the publication. (Many interim publications reported analyses without any justification.)
“Most importantly, journals, authors, and funders should commit to making final results accessible by linking interim publications to final reports whenever available,” said study author Steven Woloshin, MD, of Dartmouth Institute for Health Policy and Clinical Practice. ![]()
Interim results from randomized trials may be misleading at times, according to research published in JAMA.
Researchers compared interim and final publications on randomized trials and found that, 21% of the time, results changed significantly.
“Changes between interim and final publication matter because clinicians and the public could have been misled about whether an intervention was beneficial, harmful, or ineffective,” said study author Lisa Schwartz, MD, of Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, New Hampshire.
She and her colleagues searched PubMed for randomized trials from 2006 to 2015 with “interim,” “not mature,” or “immature” in the title or abstract.
To identify final publications, they searched PubMed, ClinicalTrials.gov, and Web of Science through 2016. The team emailed authors of interim reports when no final publication was identified.
For interim and final publications reporting the same efficacy and or safety outcome, the researchers compared trial characteristics and prominence. They also categorized abstract conclusions (not different, beneficial, or harmful) and compared changes between interim and final publications.
Findings
Interim results were reported in 613 of 1267 screened publications.
Of those publications, 72% reported on trials stopped early (for benefit, harm, futility, or other problems). The remaining 171 ongoing trials (mostly in oncology, surgery, or cardiology) reported interim efficacy or safety results.
Forty-one percent of the publications stated that the interim analysis was specified in the protocol, but half provided no reason for the interim publication.
Final results were published for 98 of the 160 trials (61%) that were more than 1 year beyond the completion date.
The researchers compared 73 interim and final publications reporting the same efficacy or safety outcome. And they found that interim and final publications had similar prominence.
In most cases (79%), the abstract conclusions did not change from the interim publication to the final publication. However, for 21% of trials, there were significant changes.
For 4 trials, the conclusions changed from “no difference” between randomized to treatments to the study treatment being “beneficial.” In 3 trials, the conclusions changed from “not different” to “harmful or possibly harmful.”
In 6 trials, the conclusions changed from “beneficial” to “not different.” One trial changed from “beneficial” to “harmful,” and another changed from “inconclusive” to “noninferior.”
Dr Schwartz and her colleagues concluded that while most interim and final publications reached similar conclusions, frequent non-publication of final results can lead to confusion or unfounded assumptions with true treatment effects remaining unknown.
To safeguard against any such confusion, the researchers recommended routinely adding the word “interim” in the title and justifying the reason in the publication. (Many interim publications reported analyses without any justification.)
“Most importantly, journals, authors, and funders should commit to making final results accessible by linking interim publications to final reports whenever available,” said study author Steven Woloshin, MD, of Dartmouth Institute for Health Policy and Clinical Practice. ![]()
Interim results from randomized trials may be misleading at times, according to research published in JAMA.
Researchers compared interim and final publications on randomized trials and found that, 21% of the time, results changed significantly.
“Changes between interim and final publication matter because clinicians and the public could have been misled about whether an intervention was beneficial, harmful, or ineffective,” said study author Lisa Schwartz, MD, of Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, New Hampshire.
She and her colleagues searched PubMed for randomized trials from 2006 to 2015 with “interim,” “not mature,” or “immature” in the title or abstract.
To identify final publications, they searched PubMed, ClinicalTrials.gov, and Web of Science through 2016. The team emailed authors of interim reports when no final publication was identified.
For interim and final publications reporting the same efficacy and or safety outcome, the researchers compared trial characteristics and prominence. They also categorized abstract conclusions (not different, beneficial, or harmful) and compared changes between interim and final publications.
Findings
Interim results were reported in 613 of 1267 screened publications.
Of those publications, 72% reported on trials stopped early (for benefit, harm, futility, or other problems). The remaining 171 ongoing trials (mostly in oncology, surgery, or cardiology) reported interim efficacy or safety results.
Forty-one percent of the publications stated that the interim analysis was specified in the protocol, but half provided no reason for the interim publication.
Final results were published for 98 of the 160 trials (61%) that were more than 1 year beyond the completion date.
The researchers compared 73 interim and final publications reporting the same efficacy or safety outcome. And they found that interim and final publications had similar prominence.
In most cases (79%), the abstract conclusions did not change from the interim publication to the final publication. However, for 21% of trials, there were significant changes.
For 4 trials, the conclusions changed from “no difference” between randomized to treatments to the study treatment being “beneficial.” In 3 trials, the conclusions changed from “not different” to “harmful or possibly harmful.”
In 6 trials, the conclusions changed from “beneficial” to “not different.” One trial changed from “beneficial” to “harmful,” and another changed from “inconclusive” to “noninferior.”
Dr Schwartz and her colleagues concluded that while most interim and final publications reached similar conclusions, frequent non-publication of final results can lead to confusion or unfounded assumptions with true treatment effects remaining unknown.
To safeguard against any such confusion, the researchers recommended routinely adding the word “interim” in the title and justifying the reason in the publication. (Many interim publications reported analyses without any justification.)
“Most importantly, journals, authors, and funders should commit to making final results accessible by linking interim publications to final reports whenever available,” said study author Steven Woloshin, MD, of Dartmouth Institute for Health Policy and Clinical Practice. ![]()
Trial protocols redacted by industry sponsors
New research has revealed a lack of public information regarding protocols for industry-sponsored, randomized drug trials in Denmark.
First, researchers found it difficult to obtain protocols for commercially sponsored trials, with some sponsors taking legal action in an attempt to keep protocols private.
When the researchers did receive protocols, many had widespread redactions.
The researchers reported these findings in the Journal of the Royal Society of Medicine.
“We wished to compare the information in the protocols with the information provided to the patients in order to evaluate whether the trials were ethical and necessary and whether essential information about the benefits and the harms of the drugs had been hidden from the patients,” said study author Peter Gøtzsche, MD, director of the Nordic Cochrane Centre in Copenhagen, Denmark.
To that end, Dr Gøtzsche and his colleagues used the Danish Freedom of Information Act to request access to 78 protocols for randomized trials that were approved by a research ethics committee from October 2012 to March 2013.
The researchers said several companies refused to provide protocols and involved their lawyers. In fact, Sanofi-Aventis sued the National Committee on Health Research Ethics but lost.
Three years after this project was started, the researchers were able to obtain all the protocols they had requested. Eight protocols were excluded from analysis because they did not meet the research inclusion criteria.
Seventeen of 34 protocols for commercially sponsored trials were unredacted, compared to 34 of 36 non-commercially sponsored trials.
The researchers said the redactions “were most widespread in those sections of the protocol where there is empirical evidence of substantial problems with the trustworthiness of published drug trials.”
This includes data analysis, the handling of missing data, the detection/analysis of adverse events, the definition of patient outcomes, interim analyses and premature study termination, the sponsor’s access to incoming data while the study is ongoing, ownership of the data, and investigators’ publication rights.
“The amount of redactions in the protocols we received was so vast that it made them rather useless for assessing the ethical justification for the studies and to identify discrepancies with subsequent publications,” Dr Gøtzsche said.
“We could not identify any legitimate rationale for the redactions. The current mistrust in industry-sponsored drug trials can only change if the industry offers unconditional access to its trial protocols and other relevant documents and data.” ![]()
New research has revealed a lack of public information regarding protocols for industry-sponsored, randomized drug trials in Denmark.
First, researchers found it difficult to obtain protocols for commercially sponsored trials, with some sponsors taking legal action in an attempt to keep protocols private.
When the researchers did receive protocols, many had widespread redactions.
The researchers reported these findings in the Journal of the Royal Society of Medicine.
“We wished to compare the information in the protocols with the information provided to the patients in order to evaluate whether the trials were ethical and necessary and whether essential information about the benefits and the harms of the drugs had been hidden from the patients,” said study author Peter Gøtzsche, MD, director of the Nordic Cochrane Centre in Copenhagen, Denmark.
To that end, Dr Gøtzsche and his colleagues used the Danish Freedom of Information Act to request access to 78 protocols for randomized trials that were approved by a research ethics committee from October 2012 to March 2013.
The researchers said several companies refused to provide protocols and involved their lawyers. In fact, Sanofi-Aventis sued the National Committee on Health Research Ethics but lost.
Three years after this project was started, the researchers were able to obtain all the protocols they had requested. Eight protocols were excluded from analysis because they did not meet the research inclusion criteria.
Seventeen of 34 protocols for commercially sponsored trials were unredacted, compared to 34 of 36 non-commercially sponsored trials.
The researchers said the redactions “were most widespread in those sections of the protocol where there is empirical evidence of substantial problems with the trustworthiness of published drug trials.”
This includes data analysis, the handling of missing data, the detection/analysis of adverse events, the definition of patient outcomes, interim analyses and premature study termination, the sponsor’s access to incoming data while the study is ongoing, ownership of the data, and investigators’ publication rights.
“The amount of redactions in the protocols we received was so vast that it made them rather useless for assessing the ethical justification for the studies and to identify discrepancies with subsequent publications,” Dr Gøtzsche said.
“We could not identify any legitimate rationale for the redactions. The current mistrust in industry-sponsored drug trials can only change if the industry offers unconditional access to its trial protocols and other relevant documents and data.” ![]()
New research has revealed a lack of public information regarding protocols for industry-sponsored, randomized drug trials in Denmark.
First, researchers found it difficult to obtain protocols for commercially sponsored trials, with some sponsors taking legal action in an attempt to keep protocols private.
When the researchers did receive protocols, many had widespread redactions.
The researchers reported these findings in the Journal of the Royal Society of Medicine.
“We wished to compare the information in the protocols with the information provided to the patients in order to evaluate whether the trials were ethical and necessary and whether essential information about the benefits and the harms of the drugs had been hidden from the patients,” said study author Peter Gøtzsche, MD, director of the Nordic Cochrane Centre in Copenhagen, Denmark.
To that end, Dr Gøtzsche and his colleagues used the Danish Freedom of Information Act to request access to 78 protocols for randomized trials that were approved by a research ethics committee from October 2012 to March 2013.
The researchers said several companies refused to provide protocols and involved their lawyers. In fact, Sanofi-Aventis sued the National Committee on Health Research Ethics but lost.
Three years after this project was started, the researchers were able to obtain all the protocols they had requested. Eight protocols were excluded from analysis because they did not meet the research inclusion criteria.
Seventeen of 34 protocols for commercially sponsored trials were unredacted, compared to 34 of 36 non-commercially sponsored trials.
The researchers said the redactions “were most widespread in those sections of the protocol where there is empirical evidence of substantial problems with the trustworthiness of published drug trials.”
This includes data analysis, the handling of missing data, the detection/analysis of adverse events, the definition of patient outcomes, interim analyses and premature study termination, the sponsor’s access to incoming data while the study is ongoing, ownership of the data, and investigators’ publication rights.
“The amount of redactions in the protocols we received was so vast that it made them rather useless for assessing the ethical justification for the studies and to identify discrepancies with subsequent publications,” Dr Gøtzsche said.
“We could not identify any legitimate rationale for the redactions. The current mistrust in industry-sponsored drug trials can only change if the industry offers unconditional access to its trial protocols and other relevant documents and data.” ![]()
Zika vaccine candidate receives fast track designation
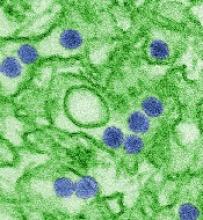
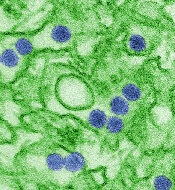
The US Food and Drug Administration (FDA) has granted fast track designation to TAK-426, a candidate vaccine for Zika virus.
TAK-426 is a purified, inactivated, alum-adjuvanted, whole Zika virus vaccine candidate being developed by Takeda Pharmaceutical Company Limited with the aid of federal funding.
TAK-426 is currently being studied in a phase 1 trial, ZIK-101 (NCT03343626).
This randomized, placebo-controlled, double-blind trial was designed to evaluate the safety and immunogenicity of TAK-426 in 240 male and female subjects between the ages of 18 and 49.
The trial is taking place in the continental US and US territories. It is being conducted under a US Investigational New Drug application.
Takeda says that, if initial data from ZIK-101 are supportive, the company will work to progress into phase 2 development as soon as possible.
Takeda’s Zika program is supported by federal funds from the Biomedical Advanced Research and Development Authority (BARDA) within the Office of the Assistant Secretary for Preparedness and Response in the US Department of Health and Human Services (contract No. HHSO100201600015C).
“We recognize the public health threat posed by the Zika virus,” said Laurence De Moerlooze, PhD, lead of the global Zika program at Takeda.
“As soon as Takeda received funding from BARDA, we mobilized a team and prioritized development of this vaccine candidate, initiating a phase 1 trial within 15 months of contract signature. With fast track designation, the ongoing support of BARDA, and the abilities of our organization, we are confident that we will continue to make expedient progress.”
About fast track designation
The FDA’s fast track designation is a process designed to facilitate the development and expedite the review of drugs and vaccines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
The fast track process allows for more frequent interactions with the FDA, rolling reviews of a product application, and eligibility for priority review if relevant criteria are met. The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months. ![]()
The US Food and Drug Administration (FDA) has granted fast track designation to TAK-426, a candidate vaccine for Zika virus.
TAK-426 is a purified, inactivated, alum-adjuvanted, whole Zika virus vaccine candidate being developed by Takeda Pharmaceutical Company Limited with the aid of federal funding.
TAK-426 is currently being studied in a phase 1 trial, ZIK-101 (NCT03343626).
This randomized, placebo-controlled, double-blind trial was designed to evaluate the safety and immunogenicity of TAK-426 in 240 male and female subjects between the ages of 18 and 49.
The trial is taking place in the continental US and US territories. It is being conducted under a US Investigational New Drug application.
Takeda says that, if initial data from ZIK-101 are supportive, the company will work to progress into phase 2 development as soon as possible.
Takeda’s Zika program is supported by federal funds from the Biomedical Advanced Research and Development Authority (BARDA) within the Office of the Assistant Secretary for Preparedness and Response in the US Department of Health and Human Services (contract No. HHSO100201600015C).
“We recognize the public health threat posed by the Zika virus,” said Laurence De Moerlooze, PhD, lead of the global Zika program at Takeda.
“As soon as Takeda received funding from BARDA, we mobilized a team and prioritized development of this vaccine candidate, initiating a phase 1 trial within 15 months of contract signature. With fast track designation, the ongoing support of BARDA, and the abilities of our organization, we are confident that we will continue to make expedient progress.”
About fast track designation
The FDA’s fast track designation is a process designed to facilitate the development and expedite the review of drugs and vaccines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
The fast track process allows for more frequent interactions with the FDA, rolling reviews of a product application, and eligibility for priority review if relevant criteria are met. The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months. ![]()
The US Food and Drug Administration (FDA) has granted fast track designation to TAK-426, a candidate vaccine for Zika virus.
TAK-426 is a purified, inactivated, alum-adjuvanted, whole Zika virus vaccine candidate being developed by Takeda Pharmaceutical Company Limited with the aid of federal funding.
TAK-426 is currently being studied in a phase 1 trial, ZIK-101 (NCT03343626).
This randomized, placebo-controlled, double-blind trial was designed to evaluate the safety and immunogenicity of TAK-426 in 240 male and female subjects between the ages of 18 and 49.
The trial is taking place in the continental US and US territories. It is being conducted under a US Investigational New Drug application.
Takeda says that, if initial data from ZIK-101 are supportive, the company will work to progress into phase 2 development as soon as possible.
Takeda’s Zika program is supported by federal funds from the Biomedical Advanced Research and Development Authority (BARDA) within the Office of the Assistant Secretary for Preparedness and Response in the US Department of Health and Human Services (contract No. HHSO100201600015C).
“We recognize the public health threat posed by the Zika virus,” said Laurence De Moerlooze, PhD, lead of the global Zika program at Takeda.
“As soon as Takeda received funding from BARDA, we mobilized a team and prioritized development of this vaccine candidate, initiating a phase 1 trial within 15 months of contract signature. With fast track designation, the ongoing support of BARDA, and the abilities of our organization, we are confident that we will continue to make expedient progress.”
About fast track designation
The FDA’s fast track designation is a process designed to facilitate the development and expedite the review of drugs and vaccines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
The fast track process allows for more frequent interactions with the FDA, rolling reviews of a product application, and eligibility for priority review if relevant criteria are met. The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months. ![]()
Treatment costs threaten cancer program growth
Treatment costs are the greatest threat to the growth of cancer programs, according to a survey of nearly 300 cancer program administrators and providers.
Sixty-eight percent of survey respondents said treatment costs were among the biggest threats to future cancer program growth at their organization.
Other top threats to growth included physician alignment around services and program goals—cited by 47% of respondents—and changes in healthcare coverage—cited by 46%.
This survey—the “2017 Trending Now in Cancer Care Survey”—was conducted by the Association of Community Cancer Centers (ACCC) and Advisory Board’s Oncology Roundtable. It was supported by Pfizer Oncology.
The survey was distributed via email on July 24, 2017. Respondents included 293 cancer program administrators and providers from 209 institutions. They submitted responses over 6 weeks.
Respondents identified the following “biggest threats” to cancer program growth:
- Cost of drugs and/or new treatment modalities—68%
- Physician alignment around services and program goals—47%
- Changes in healthcare coverage—46%
- Cuts to fee-for-service reimbursement—44%
- Shifting reimbursement to value-based care—43%
- Marketplace competition—35%
- Workforce planning (eg, managing staff shortages)—34%
- Network strategy and integration—33%
- Site of care policies issued by private payers—27%
- Access to capital—26%
- Quality reporting requirements—22%
- Health information technology—21%
- Other—6%.
When asked to identify their greatest opportunities for cost savings, respondents overwhelmingly pointed toward clinical standardization (63%) and drugs (62%).
Other opportunities included:
- Supplies—28%
- Capital expenses (eg, imaging technology)—24%
- Non-clinical staff (eg, billing and coding specialists)—22%
- Technology maintenance—20%
- Clinical staff—16%
- Retail pharmacy—14%
- Clinical research—10%
- Support services (eg, acupuncture)—9%
- Other—4%.
Respondents also said the investments most likely to yield a return for their cancer program were:
- Increasing the number of sub-specialists (eg, breast surgeons)—59%
- Marketing—41%
- Specialty pharmacy—36%
- Increasing the number of general oncology physicians—34%
- Screening services (eg, mobile screening unit)—29%
- Capital investments—24%
- Clinical research—16%
- Support services—15%
- Retail pharmacy—14%
- Building upgrades—14%.
More details on the “2017 Trending Now in Cancer Care Survey” can be found on the ACCC website. ![]()
Treatment costs are the greatest threat to the growth of cancer programs, according to a survey of nearly 300 cancer program administrators and providers.
Sixty-eight percent of survey respondents said treatment costs were among the biggest threats to future cancer program growth at their organization.
Other top threats to growth included physician alignment around services and program goals—cited by 47% of respondents—and changes in healthcare coverage—cited by 46%.
This survey—the “2017 Trending Now in Cancer Care Survey”—was conducted by the Association of Community Cancer Centers (ACCC) and Advisory Board’s Oncology Roundtable. It was supported by Pfizer Oncology.
The survey was distributed via email on July 24, 2017. Respondents included 293 cancer program administrators and providers from 209 institutions. They submitted responses over 6 weeks.
Respondents identified the following “biggest threats” to cancer program growth:
- Cost of drugs and/or new treatment modalities—68%
- Physician alignment around services and program goals—47%
- Changes in healthcare coverage—46%
- Cuts to fee-for-service reimbursement—44%
- Shifting reimbursement to value-based care—43%
- Marketplace competition—35%
- Workforce planning (eg, managing staff shortages)—34%
- Network strategy and integration—33%
- Site of care policies issued by private payers—27%
- Access to capital—26%
- Quality reporting requirements—22%
- Health information technology—21%
- Other—6%.
When asked to identify their greatest opportunities for cost savings, respondents overwhelmingly pointed toward clinical standardization (63%) and drugs (62%).
Other opportunities included:
- Supplies—28%
- Capital expenses (eg, imaging technology)—24%
- Non-clinical staff (eg, billing and coding specialists)—22%
- Technology maintenance—20%
- Clinical staff—16%
- Retail pharmacy—14%
- Clinical research—10%
- Support services (eg, acupuncture)—9%
- Other—4%.
Respondents also said the investments most likely to yield a return for their cancer program were:
- Increasing the number of sub-specialists (eg, breast surgeons)—59%
- Marketing—41%
- Specialty pharmacy—36%
- Increasing the number of general oncology physicians—34%
- Screening services (eg, mobile screening unit)—29%
- Capital investments—24%
- Clinical research—16%
- Support services—15%
- Retail pharmacy—14%
- Building upgrades—14%.
More details on the “2017 Trending Now in Cancer Care Survey” can be found on the ACCC website. ![]()
Treatment costs are the greatest threat to the growth of cancer programs, according to a survey of nearly 300 cancer program administrators and providers.
Sixty-eight percent of survey respondents said treatment costs were among the biggest threats to future cancer program growth at their organization.
Other top threats to growth included physician alignment around services and program goals—cited by 47% of respondents—and changes in healthcare coverage—cited by 46%.
This survey—the “2017 Trending Now in Cancer Care Survey”—was conducted by the Association of Community Cancer Centers (ACCC) and Advisory Board’s Oncology Roundtable. It was supported by Pfizer Oncology.
The survey was distributed via email on July 24, 2017. Respondents included 293 cancer program administrators and providers from 209 institutions. They submitted responses over 6 weeks.
Respondents identified the following “biggest threats” to cancer program growth:
- Cost of drugs and/or new treatment modalities—68%
- Physician alignment around services and program goals—47%
- Changes in healthcare coverage—46%
- Cuts to fee-for-service reimbursement—44%
- Shifting reimbursement to value-based care—43%
- Marketplace competition—35%
- Workforce planning (eg, managing staff shortages)—34%
- Network strategy and integration—33%
- Site of care policies issued by private payers—27%
- Access to capital—26%
- Quality reporting requirements—22%
- Health information technology—21%
- Other—6%.
When asked to identify their greatest opportunities for cost savings, respondents overwhelmingly pointed toward clinical standardization (63%) and drugs (62%).
Other opportunities included:
- Supplies—28%
- Capital expenses (eg, imaging technology)—24%
- Non-clinical staff (eg, billing and coding specialists)—22%
- Technology maintenance—20%
- Clinical staff—16%
- Retail pharmacy—14%
- Clinical research—10%
- Support services (eg, acupuncture)—9%
- Other—4%.
Respondents also said the investments most likely to yield a return for their cancer program were:
- Increasing the number of sub-specialists (eg, breast surgeons)—59%
- Marketing—41%
- Specialty pharmacy—36%
- Increasing the number of general oncology physicians—34%
- Screening services (eg, mobile screening unit)—29%
- Capital investments—24%
- Clinical research—16%
- Support services—15%
- Retail pharmacy—14%
- Building upgrades—14%.
More details on the “2017 Trending Now in Cancer Care Survey” can be found on the ACCC website. ![]()
Health systems plan to produce drugs themselves
A group of US health systems is planning to form a not-for-profit generic drug company with the goal of ending drug shortages and reducing prices for patients.
The company will either directly manufacture generic drugs or subcontract manufacturing to organizations it deems reputable.
“For people in the United States, there is a dangerous gap today between the demand and supply of affordable prescription drugs,” said Richard J. Gilfillan, MD, chief executive officer of Trinity Health, one of the health systems involved in this project.
“If the only way to provide our communities with affordable drugs is to produce them ourselves, then that is what we will do. We look forward to more healthcare systems around the country joining this people-centered effort.”
The organizations involved in this project include Intermountain Healthcare, Ascension, SSM Health, and Trinity Health, as well as the US Department of Veterans Affairs (although the department has not provided financial support for the project).
The 5 organizations represent more than 450 hospitals around the US, and other health systems are set to join the initiative as well.
“It’s an ambitious plan, but healthcare systems are in the best position to fix the problems in the generic drug market,” said Marc Harrison, MD, president and chief executive officer of Intermountain Healthcare.
“We witness, on a daily basis, how shortages of essential generic medications or egregious cost increases for those same drugs affect our patients. We are confident we can improve the situation for our patients by bringing much-needed competition to the generic drug market.”
The formation of this not-for-profit generic drug company will be guided by an advisory committee, which will include:
- Madhu Balachandran, retired executive vice-president of Global Operations, Amgen
- Don Berwick, MD, president emeritus and senior fellow, Institute for Healthcare Improvement; former Centers for Medicare & Medicaid Services administrator
- Clayton Christensen, professor at Harvard Business School and founder of Innosight
- Bob Kerrey, managing director, Allen & Company; former Nebraska governor and US senator
- Martin VanTrieste, retired senior vice-president and chief quality officer, Amgen
- Senior-level leaders from the organizations founding the company.

A group of US health systems is planning to form a not-for-profit generic drug company with the goal of ending drug shortages and reducing prices for patients.
The company will either directly manufacture generic drugs or subcontract manufacturing to organizations it deems reputable.
“For people in the United States, there is a dangerous gap today between the demand and supply of affordable prescription drugs,” said Richard J. Gilfillan, MD, chief executive officer of Trinity Health, one of the health systems involved in this project.
“If the only way to provide our communities with affordable drugs is to produce them ourselves, then that is what we will do. We look forward to more healthcare systems around the country joining this people-centered effort.”
The organizations involved in this project include Intermountain Healthcare, Ascension, SSM Health, and Trinity Health, as well as the US Department of Veterans Affairs (although the department has not provided financial support for the project).
The 5 organizations represent more than 450 hospitals around the US, and other health systems are set to join the initiative as well.
“It’s an ambitious plan, but healthcare systems are in the best position to fix the problems in the generic drug market,” said Marc Harrison, MD, president and chief executive officer of Intermountain Healthcare.
“We witness, on a daily basis, how shortages of essential generic medications or egregious cost increases for those same drugs affect our patients. We are confident we can improve the situation for our patients by bringing much-needed competition to the generic drug market.”
The formation of this not-for-profit generic drug company will be guided by an advisory committee, which will include:
- Madhu Balachandran, retired executive vice-president of Global Operations, Amgen
- Don Berwick, MD, president emeritus and senior fellow, Institute for Healthcare Improvement; former Centers for Medicare & Medicaid Services administrator
- Clayton Christensen, professor at Harvard Business School and founder of Innosight
- Bob Kerrey, managing director, Allen & Company; former Nebraska governor and US senator
- Martin VanTrieste, retired senior vice-president and chief quality officer, Amgen
- Senior-level leaders from the organizations founding the company.

A group of US health systems is planning to form a not-for-profit generic drug company with the goal of ending drug shortages and reducing prices for patients.
The company will either directly manufacture generic drugs or subcontract manufacturing to organizations it deems reputable.
“For people in the United States, there is a dangerous gap today between the demand and supply of affordable prescription drugs,” said Richard J. Gilfillan, MD, chief executive officer of Trinity Health, one of the health systems involved in this project.
“If the only way to provide our communities with affordable drugs is to produce them ourselves, then that is what we will do. We look forward to more healthcare systems around the country joining this people-centered effort.”
The organizations involved in this project include Intermountain Healthcare, Ascension, SSM Health, and Trinity Health, as well as the US Department of Veterans Affairs (although the department has not provided financial support for the project).
The 5 organizations represent more than 450 hospitals around the US, and other health systems are set to join the initiative as well.
“It’s an ambitious plan, but healthcare systems are in the best position to fix the problems in the generic drug market,” said Marc Harrison, MD, president and chief executive officer of Intermountain Healthcare.
“We witness, on a daily basis, how shortages of essential generic medications or egregious cost increases for those same drugs affect our patients. We are confident we can improve the situation for our patients by bringing much-needed competition to the generic drug market.”
The formation of this not-for-profit generic drug company will be guided by an advisory committee, which will include:
- Madhu Balachandran, retired executive vice-president of Global Operations, Amgen
- Don Berwick, MD, president emeritus and senior fellow, Institute for Healthcare Improvement; former Centers for Medicare & Medicaid Services administrator
- Clayton Christensen, professor at Harvard Business School and founder of Innosight
- Bob Kerrey, managing director, Allen & Company; former Nebraska governor and US senator
- Martin VanTrieste, retired senior vice-president and chief quality officer, Amgen
- Senior-level leaders from the organizations founding the company.