User login
Die not yet cast for lymphazurin and methylene blue dye
CHICAGO – Two commonly used dyes produced mixed results in sentinel lymph node mapping of early stage breast cancer in what was described as the highest-powered study to date.
The average number of sentinel lymph nodes identified per person was significantly higher with 1% methylene blue dye than with 1% lymphazurin (2.89 vs. 2.22; P less than .001).
Although there is extensive support for methylene blue as a safe and efficacious alternative to lymphazurin, this finding on the number of sentinel nodes identified is not replicated in any other study, Dr. Vaishali Patel said at the annual clinical congress of the American College of Surgeons. The study was conducted at the McLaren Flint (Mich.) Medical Center. Dr. Sukamal Saha was principal investigator.
On the other hand, lymphazurin identified significantly more additional lymph nodes than methylene blue (mean 4.48 vs. 2.84; P less than .001).
Nodal positivity was also significantly higher with lymphazurin than methylene blue (14.93% vs. 8.85%; P less than .001), which also has not been reported in other trials.
“We think this does offer a true comparison between the two dyes,” Dr. Patel of Detroit Medical Center Sinai-Grace Hospital said. “The volume of dye and technique were consistent for all 651 patients. … with one surgeon performing the injections and one surgeon performing the procedures.” The 651 consecutive patients were randomly assigned based on agent availability to a preoperative injection of lymphazurin (half intraparenchymal and half subareolar in the upper outer quadrant) or an intraoperative injection of methylene blue over 5 minutes (3 ccs intraparenchymal, 1 cc subareolar, and 1 cc intradermal).
The lymphazurin and methylene blue groups were also similar in number (298 patients vs. 353 patients), age (mean 61.6 years vs. 63.5 years), and T stage (in situ 12% vs. 17.8%; T1 64% vs. 65%; T2 23% vs. 17.5%).
In contrast, three smaller, well-established studies that came to different conclusions used four different surgeons and novel techniques to inject their radiocolloid and supervised residents for lymphatic mapping, she noted.
The radiocolloid lymphazurin first demonstrated superiority over methylene blue in 1990, but alternatives continue to be investigated due to frequent nonavailability and a host of adverse events including blue hives, blue discoloration or tattooing, and anaphylaxis.
Lymphazurin also costs 10-12 times more than methylene blue, which was reflected in the study in an average per patient cost of $815 vs. $75 for methylene blue, Dr. Patel said.
The American Society of Breast Surgeons, however, recommends dual-agent mapping using blue dye and a radioisotope in breast cancer to further improve the success in identifying the sentinel lymph nodes. The improvement is likely because of the dual mechanism at play: radiocolloids become entrapped within the lymph node, whereas certain blue dyes bind to interstitial albumin and are taken up by lymphatics, she explained.
The higher number of sentinel lymph nodes in the methylene blue group may be due to its particle size, which is smaller, weighs less, and diffused faster, Dr. Patel suggested.
The higher number of additional lymph nodes captured with lymphazurin may be because of the higher frequency of nodal dissection in this group than in the methylene blue group (25% vs. 16%).
The finding of greater nodal positivity in the lymphazurin group may be related to mechanism of action or the high percentage of patients with T1 disease enrolled in the study. Still, nodal positivity was higher with lymphazurin than methylene blue regardless of T stage, she said.
The lymphazurin group had higher rates than the methylene blue group of pseudohypoxemia (10% vs. 0%; P less than .0001), but blue hives (1.34% vs. 0%; P = .043) and anaphylaxis (.67% vs. 0%; P = .20) were kept in check. Patients were premedicated and early in the series, the surgeon began excising the area of injected blue skin during the primary surgery, Dr. Patel observed.
Despite being diluted, methylene blue was associated with higher rates of seroma (3.4% vs. 1.7%; P = .005) and skin necrosis (2.55% vs. 9%; P = .005).
Discussant Dr. Alyssa Throckmorton of Baptist Memorial Health Care in Memphis pointed out that more recent data show radiocolloid mapping alone is comparable to dual-agent mapping, suggesting that blue dye may not be needed. That said, there have been national shortages of methylene blue as well as lymphazurin.
“I think in surgeons who are going to use blue dye, with the way drug shortages have become in the last few years, you are going to have to be facile and familiar with both types of dye if you are going to use that as part of your clinical practice,” she said.
CHICAGO – Two commonly used dyes produced mixed results in sentinel lymph node mapping of early stage breast cancer in what was described as the highest-powered study to date.
The average number of sentinel lymph nodes identified per person was significantly higher with 1% methylene blue dye than with 1% lymphazurin (2.89 vs. 2.22; P less than .001).
Although there is extensive support for methylene blue as a safe and efficacious alternative to lymphazurin, this finding on the number of sentinel nodes identified is not replicated in any other study, Dr. Vaishali Patel said at the annual clinical congress of the American College of Surgeons. The study was conducted at the McLaren Flint (Mich.) Medical Center. Dr. Sukamal Saha was principal investigator.
On the other hand, lymphazurin identified significantly more additional lymph nodes than methylene blue (mean 4.48 vs. 2.84; P less than .001).
Nodal positivity was also significantly higher with lymphazurin than methylene blue (14.93% vs. 8.85%; P less than .001), which also has not been reported in other trials.
“We think this does offer a true comparison between the two dyes,” Dr. Patel of Detroit Medical Center Sinai-Grace Hospital said. “The volume of dye and technique were consistent for all 651 patients. … with one surgeon performing the injections and one surgeon performing the procedures.” The 651 consecutive patients were randomly assigned based on agent availability to a preoperative injection of lymphazurin (half intraparenchymal and half subareolar in the upper outer quadrant) or an intraoperative injection of methylene blue over 5 minutes (3 ccs intraparenchymal, 1 cc subareolar, and 1 cc intradermal).
The lymphazurin and methylene blue groups were also similar in number (298 patients vs. 353 patients), age (mean 61.6 years vs. 63.5 years), and T stage (in situ 12% vs. 17.8%; T1 64% vs. 65%; T2 23% vs. 17.5%).
In contrast, three smaller, well-established studies that came to different conclusions used four different surgeons and novel techniques to inject their radiocolloid and supervised residents for lymphatic mapping, she noted.
The radiocolloid lymphazurin first demonstrated superiority over methylene blue in 1990, but alternatives continue to be investigated due to frequent nonavailability and a host of adverse events including blue hives, blue discoloration or tattooing, and anaphylaxis.
Lymphazurin also costs 10-12 times more than methylene blue, which was reflected in the study in an average per patient cost of $815 vs. $75 for methylene blue, Dr. Patel said.
The American Society of Breast Surgeons, however, recommends dual-agent mapping using blue dye and a radioisotope in breast cancer to further improve the success in identifying the sentinel lymph nodes. The improvement is likely because of the dual mechanism at play: radiocolloids become entrapped within the lymph node, whereas certain blue dyes bind to interstitial albumin and are taken up by lymphatics, she explained.
The higher number of sentinel lymph nodes in the methylene blue group may be due to its particle size, which is smaller, weighs less, and diffused faster, Dr. Patel suggested.
The higher number of additional lymph nodes captured with lymphazurin may be because of the higher frequency of nodal dissection in this group than in the methylene blue group (25% vs. 16%).
The finding of greater nodal positivity in the lymphazurin group may be related to mechanism of action or the high percentage of patients with T1 disease enrolled in the study. Still, nodal positivity was higher with lymphazurin than methylene blue regardless of T stage, she said.
The lymphazurin group had higher rates than the methylene blue group of pseudohypoxemia (10% vs. 0%; P less than .0001), but blue hives (1.34% vs. 0%; P = .043) and anaphylaxis (.67% vs. 0%; P = .20) were kept in check. Patients were premedicated and early in the series, the surgeon began excising the area of injected blue skin during the primary surgery, Dr. Patel observed.
Despite being diluted, methylene blue was associated with higher rates of seroma (3.4% vs. 1.7%; P = .005) and skin necrosis (2.55% vs. 9%; P = .005).
Discussant Dr. Alyssa Throckmorton of Baptist Memorial Health Care in Memphis pointed out that more recent data show radiocolloid mapping alone is comparable to dual-agent mapping, suggesting that blue dye may not be needed. That said, there have been national shortages of methylene blue as well as lymphazurin.
“I think in surgeons who are going to use blue dye, with the way drug shortages have become in the last few years, you are going to have to be facile and familiar with both types of dye if you are going to use that as part of your clinical practice,” she said.
CHICAGO – Two commonly used dyes produced mixed results in sentinel lymph node mapping of early stage breast cancer in what was described as the highest-powered study to date.
The average number of sentinel lymph nodes identified per person was significantly higher with 1% methylene blue dye than with 1% lymphazurin (2.89 vs. 2.22; P less than .001).
Although there is extensive support for methylene blue as a safe and efficacious alternative to lymphazurin, this finding on the number of sentinel nodes identified is not replicated in any other study, Dr. Vaishali Patel said at the annual clinical congress of the American College of Surgeons. The study was conducted at the McLaren Flint (Mich.) Medical Center. Dr. Sukamal Saha was principal investigator.
On the other hand, lymphazurin identified significantly more additional lymph nodes than methylene blue (mean 4.48 vs. 2.84; P less than .001).
Nodal positivity was also significantly higher with lymphazurin than methylene blue (14.93% vs. 8.85%; P less than .001), which also has not been reported in other trials.
“We think this does offer a true comparison between the two dyes,” Dr. Patel of Detroit Medical Center Sinai-Grace Hospital said. “The volume of dye and technique were consistent for all 651 patients. … with one surgeon performing the injections and one surgeon performing the procedures.” The 651 consecutive patients were randomly assigned based on agent availability to a preoperative injection of lymphazurin (half intraparenchymal and half subareolar in the upper outer quadrant) or an intraoperative injection of methylene blue over 5 minutes (3 ccs intraparenchymal, 1 cc subareolar, and 1 cc intradermal).
The lymphazurin and methylene blue groups were also similar in number (298 patients vs. 353 patients), age (mean 61.6 years vs. 63.5 years), and T stage (in situ 12% vs. 17.8%; T1 64% vs. 65%; T2 23% vs. 17.5%).
In contrast, three smaller, well-established studies that came to different conclusions used four different surgeons and novel techniques to inject their radiocolloid and supervised residents for lymphatic mapping, she noted.
The radiocolloid lymphazurin first demonstrated superiority over methylene blue in 1990, but alternatives continue to be investigated due to frequent nonavailability and a host of adverse events including blue hives, blue discoloration or tattooing, and anaphylaxis.
Lymphazurin also costs 10-12 times more than methylene blue, which was reflected in the study in an average per patient cost of $815 vs. $75 for methylene blue, Dr. Patel said.
The American Society of Breast Surgeons, however, recommends dual-agent mapping using blue dye and a radioisotope in breast cancer to further improve the success in identifying the sentinel lymph nodes. The improvement is likely because of the dual mechanism at play: radiocolloids become entrapped within the lymph node, whereas certain blue dyes bind to interstitial albumin and are taken up by lymphatics, she explained.
The higher number of sentinel lymph nodes in the methylene blue group may be due to its particle size, which is smaller, weighs less, and diffused faster, Dr. Patel suggested.
The higher number of additional lymph nodes captured with lymphazurin may be because of the higher frequency of nodal dissection in this group than in the methylene blue group (25% vs. 16%).
The finding of greater nodal positivity in the lymphazurin group may be related to mechanism of action or the high percentage of patients with T1 disease enrolled in the study. Still, nodal positivity was higher with lymphazurin than methylene blue regardless of T stage, she said.
The lymphazurin group had higher rates than the methylene blue group of pseudohypoxemia (10% vs. 0%; P less than .0001), but blue hives (1.34% vs. 0%; P = .043) and anaphylaxis (.67% vs. 0%; P = .20) were kept in check. Patients were premedicated and early in the series, the surgeon began excising the area of injected blue skin during the primary surgery, Dr. Patel observed.
Despite being diluted, methylene blue was associated with higher rates of seroma (3.4% vs. 1.7%; P = .005) and skin necrosis (2.55% vs. 9%; P = .005).
Discussant Dr. Alyssa Throckmorton of Baptist Memorial Health Care in Memphis pointed out that more recent data show radiocolloid mapping alone is comparable to dual-agent mapping, suggesting that blue dye may not be needed. That said, there have been national shortages of methylene blue as well as lymphazurin.
“I think in surgeons who are going to use blue dye, with the way drug shortages have become in the last few years, you are going to have to be facile and familiar with both types of dye if you are going to use that as part of your clinical practice,” she said.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Contrary to prior studies, lymph node positivity was higher with lymphazurin than methylene blue in patients with early breast cancer.
Major finding: Nodal positivity was 14.93% with lymphazurin vs. 8.85% with methylene blue (P less than .001).
Data source: Prospective study in 651 patients undergoing lymphatic mapping for breast cancer.
Disclosures: Dr. Patel and Dr. Throckmorton reported having no relevant conflicts.
Readmission after esophagectomy raises mortality
About one in five patients who have surgery to remove part or all of the esophagus return to the hospital for complications within 30 days, and when they do their chance of death increases fivefold, compared with those who don’t return to the hospital, investigators at the University of Virginia Health System reported in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1254-60).
“Early recognition of life-threatening readmission diagnoses is essential in order to provide optimal care,” said lead author Dr. Yinin Hu and colleagues. Esophageal cancer is the fastest-growing cancer in the United States, so the study investigators set out to closely examine the reasons for readmissions and death after surgery.
The study identified 1,688 patients in the Surveillance, Epidemiology, and End Results (SEER)-Medicare database aged 66 or older who had surgery for esophageal cancer from 2000 to 2009. The overall 30-day mortality was 6.9%, and the 90-day mortality was 13.9%.
After excluding in-hospital deaths, the investigators’ readmission analysis included 1,543 patients. In this group, overall 90-day mortality following discharge was 6.4%, and the readmission rate within 30 days of discharge was 20.7%
The 90-day mortality for patients who were readmitted was more than four times that for those who were not readmitted, 16.3% vs. 3.8%; their in-hospital mortality was 8.8%. About one-third of readmissions were to facilities different from where patients had the index esophagectomy, and those patients were about seven times more likely to be transferred after readmission than patients admitted to the same facility, 15% vs. 1.9%. Risk-adjusted mortality did not vary significantly across providers.
The most frequent reasons for readmission were pneumonia (11.8%), malnutrition/dehydration (8.1%), pleural effusion (97.5%), and aspiration pneumonitis (6.8%). “Notably, more than one in five patients readmitted with a pulmonary diagnosis subsequently died within 90 days of the operation,” Dr. Hu and coauthors said, indicating that readmissions for pulmonary complications carried the worst prognosis.
This is the first study to demonstrate the gravity of pulmonary readmissions within 30 days of discharge, Dr. Hu and coauthors said. “Patients with nonspecific dyspneic symptoms or small pleural effusions should receive aggressive care upon readmission, as more than 20% will not survive the next few months,” Dr. Hu and coauthors said. “These results reinforce the notion that a fairly benign readmitting diagnosis is often an indicator of a much more severe root process.”
Among nonpulmonary reasons for readmission, dehydration and malnutrition carried the highest risk for death. “While there are many interventions that can promote postoperative nutrition, a readmission due to poor dietary tolerance often indicates other complications such as infection, stenosis, or anastomotic leak,” Dr. Hu and coauthors said. They suggested a thorough root-cause analysis should be part of every readmission.
The study also analyzed the hospital length of stay (LOS) as a predictor for readmission. The median LOS was 13 days, but the most common LOS was 9 days. “In general, the probability of readmission increases with increasing postoperative LOS,” Dr. Hu and colleagues said.
The authors reported no disclosures. Dr. Yinin Hu received funding from the National Institutes of Health and coauthor Dr. Benjamin Kozower received funding from the Agency for Healthcare Research and Quality.
The findings of this study may indicate that patients who stay in the hospital longer have underlying issues that did not surface during their admission for the operation, Dr. Anthony W. Kim of Yale University, New Haven, Conn., said in his invited commentary (J Thorac Cardiovasc Surg. 2015;150:1030-1). “Therefore, rather than employing a prevention of a failure-to-rescue strategy during a readmission, it may be worthwhile to enact a prevention-of-readmission strategy triggered by a longer than typical [length of stay],” Dr. Kim said. He suggested the root-cause analysis should begin in the hospital on the day after the patient exceeds the median length of stay.

|
Dr. Anthony W. Kim |
But citing the law of unintended consequences, Dr. Kim warns against using readmission as a quality metric as well a instrument to dictate reimbursement. “The law of unintended consequences dictates that when a readmission is taken out of context, using this measure raises the potential conflict of interest between doing what is right for the patient and achieving a specific milestone that may not be in the best interest of an individual patient,” he said. “Discharging a patient early perhaps to the exclusion of adequately addressing inpatient issues for the purposes of achieving a target [length of stay] is perhaps the prime example of these conflicting interests.”
Because of the difficult recovery course after esophagectomy, some readmissions are “necessary, beneficial and, unequivocally, the right decision,” Dr. Kim said. “Ironically, one of the unintended consequences of this article may be that it exposes the fact that until a better system of recording and scrutinizing readmissions exists, governing organizations should exercise considerable caution when assessing a surgeon, hospital, or system and their readmissions,” he said.
To paraphrase the sociologist Robert K. Merton, who devised the law of unintended consequences, the existing state of knowledge limits one’s ability to anticipate the consequences of action. The authors of this study “have added immensely to a body of knowledge that is still growing and deserves ongoing study if policy is to be based upon it,” Dr. Kim said.
Dr. Kim had no disclosures.
The findings of this study may indicate that patients who stay in the hospital longer have underlying issues that did not surface during their admission for the operation, Dr. Anthony W. Kim of Yale University, New Haven, Conn., said in his invited commentary (J Thorac Cardiovasc Surg. 2015;150:1030-1). “Therefore, rather than employing a prevention of a failure-to-rescue strategy during a readmission, it may be worthwhile to enact a prevention-of-readmission strategy triggered by a longer than typical [length of stay],” Dr. Kim said. He suggested the root-cause analysis should begin in the hospital on the day after the patient exceeds the median length of stay.

|
Dr. Anthony W. Kim |
But citing the law of unintended consequences, Dr. Kim warns against using readmission as a quality metric as well a instrument to dictate reimbursement. “The law of unintended consequences dictates that when a readmission is taken out of context, using this measure raises the potential conflict of interest between doing what is right for the patient and achieving a specific milestone that may not be in the best interest of an individual patient,” he said. “Discharging a patient early perhaps to the exclusion of adequately addressing inpatient issues for the purposes of achieving a target [length of stay] is perhaps the prime example of these conflicting interests.”
Because of the difficult recovery course after esophagectomy, some readmissions are “necessary, beneficial and, unequivocally, the right decision,” Dr. Kim said. “Ironically, one of the unintended consequences of this article may be that it exposes the fact that until a better system of recording and scrutinizing readmissions exists, governing organizations should exercise considerable caution when assessing a surgeon, hospital, or system and their readmissions,” he said.
To paraphrase the sociologist Robert K. Merton, who devised the law of unintended consequences, the existing state of knowledge limits one’s ability to anticipate the consequences of action. The authors of this study “have added immensely to a body of knowledge that is still growing and deserves ongoing study if policy is to be based upon it,” Dr. Kim said.
Dr. Kim had no disclosures.
The findings of this study may indicate that patients who stay in the hospital longer have underlying issues that did not surface during their admission for the operation, Dr. Anthony W. Kim of Yale University, New Haven, Conn., said in his invited commentary (J Thorac Cardiovasc Surg. 2015;150:1030-1). “Therefore, rather than employing a prevention of a failure-to-rescue strategy during a readmission, it may be worthwhile to enact a prevention-of-readmission strategy triggered by a longer than typical [length of stay],” Dr. Kim said. He suggested the root-cause analysis should begin in the hospital on the day after the patient exceeds the median length of stay.

|
Dr. Anthony W. Kim |
But citing the law of unintended consequences, Dr. Kim warns against using readmission as a quality metric as well a instrument to dictate reimbursement. “The law of unintended consequences dictates that when a readmission is taken out of context, using this measure raises the potential conflict of interest between doing what is right for the patient and achieving a specific milestone that may not be in the best interest of an individual patient,” he said. “Discharging a patient early perhaps to the exclusion of adequately addressing inpatient issues for the purposes of achieving a target [length of stay] is perhaps the prime example of these conflicting interests.”
Because of the difficult recovery course after esophagectomy, some readmissions are “necessary, beneficial and, unequivocally, the right decision,” Dr. Kim said. “Ironically, one of the unintended consequences of this article may be that it exposes the fact that until a better system of recording and scrutinizing readmissions exists, governing organizations should exercise considerable caution when assessing a surgeon, hospital, or system and their readmissions,” he said.
To paraphrase the sociologist Robert K. Merton, who devised the law of unintended consequences, the existing state of knowledge limits one’s ability to anticipate the consequences of action. The authors of this study “have added immensely to a body of knowledge that is still growing and deserves ongoing study if policy is to be based upon it,” Dr. Kim said.
Dr. Kim had no disclosures.
About one in five patients who have surgery to remove part or all of the esophagus return to the hospital for complications within 30 days, and when they do their chance of death increases fivefold, compared with those who don’t return to the hospital, investigators at the University of Virginia Health System reported in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1254-60).
“Early recognition of life-threatening readmission diagnoses is essential in order to provide optimal care,” said lead author Dr. Yinin Hu and colleagues. Esophageal cancer is the fastest-growing cancer in the United States, so the study investigators set out to closely examine the reasons for readmissions and death after surgery.
The study identified 1,688 patients in the Surveillance, Epidemiology, and End Results (SEER)-Medicare database aged 66 or older who had surgery for esophageal cancer from 2000 to 2009. The overall 30-day mortality was 6.9%, and the 90-day mortality was 13.9%.
After excluding in-hospital deaths, the investigators’ readmission analysis included 1,543 patients. In this group, overall 90-day mortality following discharge was 6.4%, and the readmission rate within 30 days of discharge was 20.7%
The 90-day mortality for patients who were readmitted was more than four times that for those who were not readmitted, 16.3% vs. 3.8%; their in-hospital mortality was 8.8%. About one-third of readmissions were to facilities different from where patients had the index esophagectomy, and those patients were about seven times more likely to be transferred after readmission than patients admitted to the same facility, 15% vs. 1.9%. Risk-adjusted mortality did not vary significantly across providers.
The most frequent reasons for readmission were pneumonia (11.8%), malnutrition/dehydration (8.1%), pleural effusion (97.5%), and aspiration pneumonitis (6.8%). “Notably, more than one in five patients readmitted with a pulmonary diagnosis subsequently died within 90 days of the operation,” Dr. Hu and coauthors said, indicating that readmissions for pulmonary complications carried the worst prognosis.
This is the first study to demonstrate the gravity of pulmonary readmissions within 30 days of discharge, Dr. Hu and coauthors said. “Patients with nonspecific dyspneic symptoms or small pleural effusions should receive aggressive care upon readmission, as more than 20% will not survive the next few months,” Dr. Hu and coauthors said. “These results reinforce the notion that a fairly benign readmitting diagnosis is often an indicator of a much more severe root process.”
Among nonpulmonary reasons for readmission, dehydration and malnutrition carried the highest risk for death. “While there are many interventions that can promote postoperative nutrition, a readmission due to poor dietary tolerance often indicates other complications such as infection, stenosis, or anastomotic leak,” Dr. Hu and coauthors said. They suggested a thorough root-cause analysis should be part of every readmission.
The study also analyzed the hospital length of stay (LOS) as a predictor for readmission. The median LOS was 13 days, but the most common LOS was 9 days. “In general, the probability of readmission increases with increasing postoperative LOS,” Dr. Hu and colleagues said.
The authors reported no disclosures. Dr. Yinin Hu received funding from the National Institutes of Health and coauthor Dr. Benjamin Kozower received funding from the Agency for Healthcare Research and Quality.
About one in five patients who have surgery to remove part or all of the esophagus return to the hospital for complications within 30 days, and when they do their chance of death increases fivefold, compared with those who don’t return to the hospital, investigators at the University of Virginia Health System reported in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1254-60).
“Early recognition of life-threatening readmission diagnoses is essential in order to provide optimal care,” said lead author Dr. Yinin Hu and colleagues. Esophageal cancer is the fastest-growing cancer in the United States, so the study investigators set out to closely examine the reasons for readmissions and death after surgery.
The study identified 1,688 patients in the Surveillance, Epidemiology, and End Results (SEER)-Medicare database aged 66 or older who had surgery for esophageal cancer from 2000 to 2009. The overall 30-day mortality was 6.9%, and the 90-day mortality was 13.9%.
After excluding in-hospital deaths, the investigators’ readmission analysis included 1,543 patients. In this group, overall 90-day mortality following discharge was 6.4%, and the readmission rate within 30 days of discharge was 20.7%
The 90-day mortality for patients who were readmitted was more than four times that for those who were not readmitted, 16.3% vs. 3.8%; their in-hospital mortality was 8.8%. About one-third of readmissions were to facilities different from where patients had the index esophagectomy, and those patients were about seven times more likely to be transferred after readmission than patients admitted to the same facility, 15% vs. 1.9%. Risk-adjusted mortality did not vary significantly across providers.
The most frequent reasons for readmission were pneumonia (11.8%), malnutrition/dehydration (8.1%), pleural effusion (97.5%), and aspiration pneumonitis (6.8%). “Notably, more than one in five patients readmitted with a pulmonary diagnosis subsequently died within 90 days of the operation,” Dr. Hu and coauthors said, indicating that readmissions for pulmonary complications carried the worst prognosis.
This is the first study to demonstrate the gravity of pulmonary readmissions within 30 days of discharge, Dr. Hu and coauthors said. “Patients with nonspecific dyspneic symptoms or small pleural effusions should receive aggressive care upon readmission, as more than 20% will not survive the next few months,” Dr. Hu and coauthors said. “These results reinforce the notion that a fairly benign readmitting diagnosis is often an indicator of a much more severe root process.”
Among nonpulmonary reasons for readmission, dehydration and malnutrition carried the highest risk for death. “While there are many interventions that can promote postoperative nutrition, a readmission due to poor dietary tolerance often indicates other complications such as infection, stenosis, or anastomotic leak,” Dr. Hu and coauthors said. They suggested a thorough root-cause analysis should be part of every readmission.
The study also analyzed the hospital length of stay (LOS) as a predictor for readmission. The median LOS was 13 days, but the most common LOS was 9 days. “In general, the probability of readmission increases with increasing postoperative LOS,” Dr. Hu and colleagues said.
The authors reported no disclosures. Dr. Yinin Hu received funding from the National Institutes of Health and coauthor Dr. Benjamin Kozower received funding from the Agency for Healthcare Research and Quality.
Key clinical point: Patients readmitted after esophagectomy are at a greater than fourfold higher risk of death than patients who do not need readmission.
Major finding: The 90-day mortality for patients who were readmitted was greater than four times that for those who were not readmitted, 16.3% vs. 3.8%.
Data source: Analysis of 1,688 patients in the SEER-Medicare database aged 66 or older who had surgery for esophageal cancer from 2000 to 2009.
Disclosures: The authors had no disclosures. Lead author Dr. Yinin Hu received funding from the National Institutes of Health and coauthor Dr. Benjamin Kozower received funding from the Agency for Healthcare Research and Quality.
Decision model shows prophylactic double mastectomy more costly to patients
CHICAGO – Contralateral prophylactic mastectomy is more expensive and provides a lower quality of life than unilateral mastectomy in younger women with sporadic breast cancer, a cost-effectiveness analysis shows.
“Unilateral mastectomy dominated contralateral prophylactic mastectomy in the treatment of unilateral, sporadic breast cancer,” Robert C. Keskey said at the annual clinical congress of the American College of Surgeons.
Among these women without a family history of breast cancer, unilateral mastectomy (UM) with 20 years of routine surveillance cost an average of $5,583 less than contralateral prophylactic mastectomy (CPM) ($13,703 vs. $19,286).
Women who chose UM also gained 0.21 quality adjusted life-years (QALYs), or about 2-3 months in perfect health (21.75 vs. 21.54).
Despite a decline in contralateral breast cancers, the national rate of CPM has risen from 9.7% to 24% in women 45 years of age or younger, due in part to the Angelina Jolie effect.
CPM reduces the risk of contralateral breast cancer by up to 95%, but has not been proven to provide a survival advantage and increases complications, Mr. Keskey of the University of Louisville (Ky.) said.
Discussant Dr. Judy Boughey of the Mayo Clinic in Rochester, Minn., observed that this is the third model to tackle this important issue and that all three came up with different results and conclusions.
“This probably highlights that our models are highly dependent on the assumptions made and the costs that are involved in building the model,” she said.
The first model developed at the Mayo Clinic by Dr. Boughey and others, reported that CPM is cost effective for women younger than 70 years. However, it did not take into account reconstruction and complications (J Clin Oncol. 2011;29:2993-3000), Mr. Keskey said during his talk.
The second model showed that CPM is cost saving, but provides a lower quality of life than UM in women younger than 50 years (Ann Surg Oncol. 2014 Jul;21:2209-17). This study only provided 10-year follow-up and overestimated reconstruction and complication rates, he said.
Dr. Boughey observed that the new model did not include symmetry, which was shown to be a big driver of CPM in a separate University of Michigan survey presented during the same session.
In addition, the quality-of-life assumptions used are the same as those in the second model, but significantly different from those in the Mayo model. In that analysis, if a patient felt that their quality of life was improved by a CPM, then the CPM was clearly cost effective, Dr. Boughey noted.
“So for a patient you see in the clinic who feels their quality of life is better with a CPM than without a CPM, does this model really apply?” she asked.
Mr. Keskey replied, “I think it still does in terms of the patient understanding what they’re going to face financially. It’s an important component of the puzzle. If they’re okay spending that money because they feel that either psychologically they are going to have a better quality of life or they feel their outcomes will be positive no matter what, then I think it’s important to understand this difference in cost and use that to make their decision.”
Study details
The investigators, led by Dr. Nicolas Ajkay, also of Louisville, created a decision tree using TreeAge Pro 2015 software to analyze the long-term costs of CPM vs. UM with routine surveillance in women aged 45 years and younger with sporadic breast cancer. The model included 16 event probabilities taken from the recent literature including complications with and without reconstruction, 5- and 10-year contralateral breast cancer risk, cancer stage, and hormone-receptor status.
Effectiveness was measured by QALYs taken from surveyed breast cancer patients. Medical costs were obtained from the 2014 Medicare physician fee schedule.
Because the physician fee schedule is not all inclusive, the investigators compared CPM and UM using costs from the Healthcare Cost and Utilization Project (HCUP), which contain total costs on hospital discharge after a procedure. When this was done, CPM cost an average of $15,425 more than UM and provided a lower quality of life, Mr. Keskey said.
The investigators also replaced yearly mammography in the unilateral mastectomy group with more expensive surveillance using breast magnetic resonance imaging. In this model, CPM actually saved about $300 ($19,286 vs. $19,560), but again provided a lower quality of life (21.54 vs. 21.75), he said. It resulted in a savings of $1,300 per QALY lost, which is not enough to be deemed cost effective.
“So even using a more expensive surveillance method, contralateral prophylactic mastectomy was still not cost effective,” Mr. Keskey said.
Finally, reconstruction rates were varied to see whether this would impact outcomes. The national reconstruction rate following unilateral mastectomy is about 28%, which resulted in a lifetime cost in the initial analysis model of about $13,703.
In order to make CPM less expensive than UM, the reconstruction rate following CPM would have to be dropped to 0% ($12,580) from the national rate of 75% ($19,286), he said. Further, even if the UM reconstruction rate was hiked to 100%, the lifetime costs associated with a unilateral mastectomy were cheaper at $19,275.
Limitations of the model include the subjective nature of QALYs, the cost-effectiveness analysis is a theoretical model, and its costs need to be validated against real-world numbers, Mr. Keskey said.
During a discussion of the study, however, an attendee expressed concern that the data will be used to deny insurance coverage for women seeking a prophylactic contralateral mastectomy.
The decision to undergo prophylactic mastectomy is very personal and needs to be individualized, despite the suggestion of increased cost and less quality of life in the study, according to senior author and colleague Dr. Nicolas Ajkay.
“For some patients, the thought of repeating breast cancer treatment, though a low probability, may be unacceptable; for others, imaging surveillance may not be a reasonable option; and a patient with preexisting breast asymmetry may consider bilateral mastectomy as a way to achieve symmetry and better cosmesis,” he said in an interview. “Our objective from the inception of the study, even before analyzing the results, was that this information could be part of a patient-physician discussion, never the main factor in the decision-making process.”
The authors and Dr. Boughey reported no conflicts of interest.
CHICAGO – Contralateral prophylactic mastectomy is more expensive and provides a lower quality of life than unilateral mastectomy in younger women with sporadic breast cancer, a cost-effectiveness analysis shows.
“Unilateral mastectomy dominated contralateral prophylactic mastectomy in the treatment of unilateral, sporadic breast cancer,” Robert C. Keskey said at the annual clinical congress of the American College of Surgeons.
Among these women without a family history of breast cancer, unilateral mastectomy (UM) with 20 years of routine surveillance cost an average of $5,583 less than contralateral prophylactic mastectomy (CPM) ($13,703 vs. $19,286).
Women who chose UM also gained 0.21 quality adjusted life-years (QALYs), or about 2-3 months in perfect health (21.75 vs. 21.54).
Despite a decline in contralateral breast cancers, the national rate of CPM has risen from 9.7% to 24% in women 45 years of age or younger, due in part to the Angelina Jolie effect.
CPM reduces the risk of contralateral breast cancer by up to 95%, but has not been proven to provide a survival advantage and increases complications, Mr. Keskey of the University of Louisville (Ky.) said.
Discussant Dr. Judy Boughey of the Mayo Clinic in Rochester, Minn., observed that this is the third model to tackle this important issue and that all three came up with different results and conclusions.
“This probably highlights that our models are highly dependent on the assumptions made and the costs that are involved in building the model,” she said.
The first model developed at the Mayo Clinic by Dr. Boughey and others, reported that CPM is cost effective for women younger than 70 years. However, it did not take into account reconstruction and complications (J Clin Oncol. 2011;29:2993-3000), Mr. Keskey said during his talk.
The second model showed that CPM is cost saving, but provides a lower quality of life than UM in women younger than 50 years (Ann Surg Oncol. 2014 Jul;21:2209-17). This study only provided 10-year follow-up and overestimated reconstruction and complication rates, he said.
Dr. Boughey observed that the new model did not include symmetry, which was shown to be a big driver of CPM in a separate University of Michigan survey presented during the same session.
In addition, the quality-of-life assumptions used are the same as those in the second model, but significantly different from those in the Mayo model. In that analysis, if a patient felt that their quality of life was improved by a CPM, then the CPM was clearly cost effective, Dr. Boughey noted.
“So for a patient you see in the clinic who feels their quality of life is better with a CPM than without a CPM, does this model really apply?” she asked.
Mr. Keskey replied, “I think it still does in terms of the patient understanding what they’re going to face financially. It’s an important component of the puzzle. If they’re okay spending that money because they feel that either psychologically they are going to have a better quality of life or they feel their outcomes will be positive no matter what, then I think it’s important to understand this difference in cost and use that to make their decision.”
Study details
The investigators, led by Dr. Nicolas Ajkay, also of Louisville, created a decision tree using TreeAge Pro 2015 software to analyze the long-term costs of CPM vs. UM with routine surveillance in women aged 45 years and younger with sporadic breast cancer. The model included 16 event probabilities taken from the recent literature including complications with and without reconstruction, 5- and 10-year contralateral breast cancer risk, cancer stage, and hormone-receptor status.
Effectiveness was measured by QALYs taken from surveyed breast cancer patients. Medical costs were obtained from the 2014 Medicare physician fee schedule.
Because the physician fee schedule is not all inclusive, the investigators compared CPM and UM using costs from the Healthcare Cost and Utilization Project (HCUP), which contain total costs on hospital discharge after a procedure. When this was done, CPM cost an average of $15,425 more than UM and provided a lower quality of life, Mr. Keskey said.
The investigators also replaced yearly mammography in the unilateral mastectomy group with more expensive surveillance using breast magnetic resonance imaging. In this model, CPM actually saved about $300 ($19,286 vs. $19,560), but again provided a lower quality of life (21.54 vs. 21.75), he said. It resulted in a savings of $1,300 per QALY lost, which is not enough to be deemed cost effective.
“So even using a more expensive surveillance method, contralateral prophylactic mastectomy was still not cost effective,” Mr. Keskey said.
Finally, reconstruction rates were varied to see whether this would impact outcomes. The national reconstruction rate following unilateral mastectomy is about 28%, which resulted in a lifetime cost in the initial analysis model of about $13,703.
In order to make CPM less expensive than UM, the reconstruction rate following CPM would have to be dropped to 0% ($12,580) from the national rate of 75% ($19,286), he said. Further, even if the UM reconstruction rate was hiked to 100%, the lifetime costs associated with a unilateral mastectomy were cheaper at $19,275.
Limitations of the model include the subjective nature of QALYs, the cost-effectiveness analysis is a theoretical model, and its costs need to be validated against real-world numbers, Mr. Keskey said.
During a discussion of the study, however, an attendee expressed concern that the data will be used to deny insurance coverage for women seeking a prophylactic contralateral mastectomy.
The decision to undergo prophylactic mastectomy is very personal and needs to be individualized, despite the suggestion of increased cost and less quality of life in the study, according to senior author and colleague Dr. Nicolas Ajkay.
“For some patients, the thought of repeating breast cancer treatment, though a low probability, may be unacceptable; for others, imaging surveillance may not be a reasonable option; and a patient with preexisting breast asymmetry may consider bilateral mastectomy as a way to achieve symmetry and better cosmesis,” he said in an interview. “Our objective from the inception of the study, even before analyzing the results, was that this information could be part of a patient-physician discussion, never the main factor in the decision-making process.”
The authors and Dr. Boughey reported no conflicts of interest.
CHICAGO – Contralateral prophylactic mastectomy is more expensive and provides a lower quality of life than unilateral mastectomy in younger women with sporadic breast cancer, a cost-effectiveness analysis shows.
“Unilateral mastectomy dominated contralateral prophylactic mastectomy in the treatment of unilateral, sporadic breast cancer,” Robert C. Keskey said at the annual clinical congress of the American College of Surgeons.
Among these women without a family history of breast cancer, unilateral mastectomy (UM) with 20 years of routine surveillance cost an average of $5,583 less than contralateral prophylactic mastectomy (CPM) ($13,703 vs. $19,286).
Women who chose UM also gained 0.21 quality adjusted life-years (QALYs), or about 2-3 months in perfect health (21.75 vs. 21.54).
Despite a decline in contralateral breast cancers, the national rate of CPM has risen from 9.7% to 24% in women 45 years of age or younger, due in part to the Angelina Jolie effect.
CPM reduces the risk of contralateral breast cancer by up to 95%, but has not been proven to provide a survival advantage and increases complications, Mr. Keskey of the University of Louisville (Ky.) said.
Discussant Dr. Judy Boughey of the Mayo Clinic in Rochester, Minn., observed that this is the third model to tackle this important issue and that all three came up with different results and conclusions.
“This probably highlights that our models are highly dependent on the assumptions made and the costs that are involved in building the model,” she said.
The first model developed at the Mayo Clinic by Dr. Boughey and others, reported that CPM is cost effective for women younger than 70 years. However, it did not take into account reconstruction and complications (J Clin Oncol. 2011;29:2993-3000), Mr. Keskey said during his talk.
The second model showed that CPM is cost saving, but provides a lower quality of life than UM in women younger than 50 years (Ann Surg Oncol. 2014 Jul;21:2209-17). This study only provided 10-year follow-up and overestimated reconstruction and complication rates, he said.
Dr. Boughey observed that the new model did not include symmetry, which was shown to be a big driver of CPM in a separate University of Michigan survey presented during the same session.
In addition, the quality-of-life assumptions used are the same as those in the second model, but significantly different from those in the Mayo model. In that analysis, if a patient felt that their quality of life was improved by a CPM, then the CPM was clearly cost effective, Dr. Boughey noted.
“So for a patient you see in the clinic who feels their quality of life is better with a CPM than without a CPM, does this model really apply?” she asked.
Mr. Keskey replied, “I think it still does in terms of the patient understanding what they’re going to face financially. It’s an important component of the puzzle. If they’re okay spending that money because they feel that either psychologically they are going to have a better quality of life or they feel their outcomes will be positive no matter what, then I think it’s important to understand this difference in cost and use that to make their decision.”
Study details
The investigators, led by Dr. Nicolas Ajkay, also of Louisville, created a decision tree using TreeAge Pro 2015 software to analyze the long-term costs of CPM vs. UM with routine surveillance in women aged 45 years and younger with sporadic breast cancer. The model included 16 event probabilities taken from the recent literature including complications with and without reconstruction, 5- and 10-year contralateral breast cancer risk, cancer stage, and hormone-receptor status.
Effectiveness was measured by QALYs taken from surveyed breast cancer patients. Medical costs were obtained from the 2014 Medicare physician fee schedule.
Because the physician fee schedule is not all inclusive, the investigators compared CPM and UM using costs from the Healthcare Cost and Utilization Project (HCUP), which contain total costs on hospital discharge after a procedure. When this was done, CPM cost an average of $15,425 more than UM and provided a lower quality of life, Mr. Keskey said.
The investigators also replaced yearly mammography in the unilateral mastectomy group with more expensive surveillance using breast magnetic resonance imaging. In this model, CPM actually saved about $300 ($19,286 vs. $19,560), but again provided a lower quality of life (21.54 vs. 21.75), he said. It resulted in a savings of $1,300 per QALY lost, which is not enough to be deemed cost effective.
“So even using a more expensive surveillance method, contralateral prophylactic mastectomy was still not cost effective,” Mr. Keskey said.
Finally, reconstruction rates were varied to see whether this would impact outcomes. The national reconstruction rate following unilateral mastectomy is about 28%, which resulted in a lifetime cost in the initial analysis model of about $13,703.
In order to make CPM less expensive than UM, the reconstruction rate following CPM would have to be dropped to 0% ($12,580) from the national rate of 75% ($19,286), he said. Further, even if the UM reconstruction rate was hiked to 100%, the lifetime costs associated with a unilateral mastectomy were cheaper at $19,275.
Limitations of the model include the subjective nature of QALYs, the cost-effectiveness analysis is a theoretical model, and its costs need to be validated against real-world numbers, Mr. Keskey said.
During a discussion of the study, however, an attendee expressed concern that the data will be used to deny insurance coverage for women seeking a prophylactic contralateral mastectomy.
The decision to undergo prophylactic mastectomy is very personal and needs to be individualized, despite the suggestion of increased cost and less quality of life in the study, according to senior author and colleague Dr. Nicolas Ajkay.
“For some patients, the thought of repeating breast cancer treatment, though a low probability, may be unacceptable; for others, imaging surveillance may not be a reasonable option; and a patient with preexisting breast asymmetry may consider bilateral mastectomy as a way to achieve symmetry and better cosmesis,” he said in an interview. “Our objective from the inception of the study, even before analyzing the results, was that this information could be part of a patient-physician discussion, never the main factor in the decision-making process.”
The authors and Dr. Boughey reported no conflicts of interest.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Unilateral mastectomy costs less and provides better quality of life than contralateral prophylactic mastectomy in younger women with sporadic breast cancer.
Major finding: Unilateral mastectomy with routine surveillance cost on average $5,583 less than prophylactic contralateral mastectomy.
Data source: Cost-effectiveness analysis of contralateral prophylactic mastectomy.
Disclosures: The authors and Dr. Boughey reported no conflicts of interest.
Tomotherapy may decrease radiation-induced bowel toxicity in cervical cancer
SAN ANTONIO – Interim results of an ongoing phase III trial show that women who have undergone surgical resection for cervical cancer may be less likely to experience late-onset bowel toxicity if they receive tomotherapy rather than conventionally delivered adjuvant radiotherapy.
In the PARCER trial, grade III or higher radiation-induced bowel toxicity occurred in just 3.2% of women who had adjuvant image-guided intensity-modulated radiation therapy (IG-IMRT) vs. 17.8% of those who received three-dimensional conformal radiation therapy (3D-CRT) at a median of 20 months. The 14.6% absolute difference was statistically significant (P = .02) but this was an exploratory endpoint.
The primary endpoint of late grade II or higher bowel toxicity was not statistically significant, but also showed around a 14% absolute difference between the arms, at 11.4% in the IG-IMRT- and 25% in the 3D-CRT–treated women (P = .13).
Nevertheless, the results are clinically relevant and the trial continues accrual to a target of 240 patients. The stopping rules were not met and there is the potential for the results to become statistically significant with longer follow-up, said Dr. Supriya Chopra of Tata Memorial Centre in Mumbai, India.
Speaking at a press briefing held during the annual meeting of the American Society for Radiation Oncology, she said: “Although this trial was done for cervical cancer, the trial results would impact practice for all endometrial cancer patients as well who would undergo postoperative radiation, and prostate cancer patients.”
“There was a substantial reduction in serious toxicities, something that justifies the added labor intensity and the added resource utilization of the more sophisticated approaches and still adds value to patients because there is a reduction in hospitalization and there is a reduction in the cost of downstream side effects,” said Dr. Brian Kavanagh of the University of Colorado at Denver, Aurora, and president-elect of the ASTRO Board of Directors, in an interview.
Data on 120 patients randomized to date were presented, of whom 58 had received conventional 3D-CRT, and 62 who had undergone IG-IMRT and received 50 Gy of radiation given in 24 fractions over 5 weeks. Patients also received weekly cisplatin (50 mg/m2) and two additional 6 Gy doses of pelvic radiation delivered via brachytherapy. In the IG-IMRT arm, investigators were careful to ensure that very little radiation reached the small bowel. Toxicity was assessed using the Common Toxicity Criteria for Adverse Events version 3.0.
Bowel toxicity can affect a substantial number of women after pelvic irradiation, and it tends to evolve over time, Dr. Chopra said.
“Most of the patients would be continually bothered about having chronic diarrhea or having abdominal bloating sensation which cannot be cured by anything, or just having some lower abdominal pain, which definitely affects their quality of life,” she explained.
The trial thus aimed to see if using the latest radiation technology could help to reduce these side effects.
“These early results are very encouraging but not robust enough to change practice at the moment,” Dr. Chopra said. If the trial is positive, however, she added that IMRT could become the new standard of care.
Final analyses will be undertaken after accrual has been completed and at a median follow-up of 3 years, so potentially by the end of 2018, she said.
SAN ANTONIO – Interim results of an ongoing phase III trial show that women who have undergone surgical resection for cervical cancer may be less likely to experience late-onset bowel toxicity if they receive tomotherapy rather than conventionally delivered adjuvant radiotherapy.
In the PARCER trial, grade III or higher radiation-induced bowel toxicity occurred in just 3.2% of women who had adjuvant image-guided intensity-modulated radiation therapy (IG-IMRT) vs. 17.8% of those who received three-dimensional conformal radiation therapy (3D-CRT) at a median of 20 months. The 14.6% absolute difference was statistically significant (P = .02) but this was an exploratory endpoint.
The primary endpoint of late grade II or higher bowel toxicity was not statistically significant, but also showed around a 14% absolute difference between the arms, at 11.4% in the IG-IMRT- and 25% in the 3D-CRT–treated women (P = .13).
Nevertheless, the results are clinically relevant and the trial continues accrual to a target of 240 patients. The stopping rules were not met and there is the potential for the results to become statistically significant with longer follow-up, said Dr. Supriya Chopra of Tata Memorial Centre in Mumbai, India.
Speaking at a press briefing held during the annual meeting of the American Society for Radiation Oncology, she said: “Although this trial was done for cervical cancer, the trial results would impact practice for all endometrial cancer patients as well who would undergo postoperative radiation, and prostate cancer patients.”
“There was a substantial reduction in serious toxicities, something that justifies the added labor intensity and the added resource utilization of the more sophisticated approaches and still adds value to patients because there is a reduction in hospitalization and there is a reduction in the cost of downstream side effects,” said Dr. Brian Kavanagh of the University of Colorado at Denver, Aurora, and president-elect of the ASTRO Board of Directors, in an interview.
Data on 120 patients randomized to date were presented, of whom 58 had received conventional 3D-CRT, and 62 who had undergone IG-IMRT and received 50 Gy of radiation given in 24 fractions over 5 weeks. Patients also received weekly cisplatin (50 mg/m2) and two additional 6 Gy doses of pelvic radiation delivered via brachytherapy. In the IG-IMRT arm, investigators were careful to ensure that very little radiation reached the small bowel. Toxicity was assessed using the Common Toxicity Criteria for Adverse Events version 3.0.
Bowel toxicity can affect a substantial number of women after pelvic irradiation, and it tends to evolve over time, Dr. Chopra said.
“Most of the patients would be continually bothered about having chronic diarrhea or having abdominal bloating sensation which cannot be cured by anything, or just having some lower abdominal pain, which definitely affects their quality of life,” she explained.
The trial thus aimed to see if using the latest radiation technology could help to reduce these side effects.
“These early results are very encouraging but not robust enough to change practice at the moment,” Dr. Chopra said. If the trial is positive, however, she added that IMRT could become the new standard of care.
Final analyses will be undertaken after accrual has been completed and at a median follow-up of 3 years, so potentially by the end of 2018, she said.
SAN ANTONIO – Interim results of an ongoing phase III trial show that women who have undergone surgical resection for cervical cancer may be less likely to experience late-onset bowel toxicity if they receive tomotherapy rather than conventionally delivered adjuvant radiotherapy.
In the PARCER trial, grade III or higher radiation-induced bowel toxicity occurred in just 3.2% of women who had adjuvant image-guided intensity-modulated radiation therapy (IG-IMRT) vs. 17.8% of those who received three-dimensional conformal radiation therapy (3D-CRT) at a median of 20 months. The 14.6% absolute difference was statistically significant (P = .02) but this was an exploratory endpoint.
The primary endpoint of late grade II or higher bowel toxicity was not statistically significant, but also showed around a 14% absolute difference between the arms, at 11.4% in the IG-IMRT- and 25% in the 3D-CRT–treated women (P = .13).
Nevertheless, the results are clinically relevant and the trial continues accrual to a target of 240 patients. The stopping rules were not met and there is the potential for the results to become statistically significant with longer follow-up, said Dr. Supriya Chopra of Tata Memorial Centre in Mumbai, India.
Speaking at a press briefing held during the annual meeting of the American Society for Radiation Oncology, she said: “Although this trial was done for cervical cancer, the trial results would impact practice for all endometrial cancer patients as well who would undergo postoperative radiation, and prostate cancer patients.”
“There was a substantial reduction in serious toxicities, something that justifies the added labor intensity and the added resource utilization of the more sophisticated approaches and still adds value to patients because there is a reduction in hospitalization and there is a reduction in the cost of downstream side effects,” said Dr. Brian Kavanagh of the University of Colorado at Denver, Aurora, and president-elect of the ASTRO Board of Directors, in an interview.
Data on 120 patients randomized to date were presented, of whom 58 had received conventional 3D-CRT, and 62 who had undergone IG-IMRT and received 50 Gy of radiation given in 24 fractions over 5 weeks. Patients also received weekly cisplatin (50 mg/m2) and two additional 6 Gy doses of pelvic radiation delivered via brachytherapy. In the IG-IMRT arm, investigators were careful to ensure that very little radiation reached the small bowel. Toxicity was assessed using the Common Toxicity Criteria for Adverse Events version 3.0.
Bowel toxicity can affect a substantial number of women after pelvic irradiation, and it tends to evolve over time, Dr. Chopra said.
“Most of the patients would be continually bothered about having chronic diarrhea or having abdominal bloating sensation which cannot be cured by anything, or just having some lower abdominal pain, which definitely affects their quality of life,” she explained.
The trial thus aimed to see if using the latest radiation technology could help to reduce these side effects.
“These early results are very encouraging but not robust enough to change practice at the moment,” Dr. Chopra said. If the trial is positive, however, she added that IMRT could become the new standard of care.
Final analyses will be undertaken after accrual has been completed and at a median follow-up of 3 years, so potentially by the end of 2018, she said.
AT THE ASTRO ANNUAL MEETING
Blacks receive inferior care for localized prostate cancer
Black patients with localized prostate cancer who underwent radical prostatectomy received inferior surgical care, compared with whites, as evidenced by fewer lymph node dissections and longer delays from diagnosis to treatment, among other indicators, researchers reported.
The time from diagnosis to treatment was longer in blacks than whites (79 vs. 71 days, P = .001). Overall, 57.7% of blacks had surgery without adjuvant therapy, compared with 61.3% of whites (P = .001). Blacks were less likely to undergo lymph node dissection (52.8% vs. 61.5%, P less than .001). The difference persisted but was not significant when the lymph node dissection analysis was restricted to patients with intermediate- and high-risk disease. Blacks were more likely to visit the emergency department within 30 days (P = .04) and beyond 30 days (P = .006) (JAMA Oncol. 2015 Oct 22. doi: 10.1001/jamaoncol/2015.3384).
When the lymph node dissection analysis was adjusted for geographic location (health service area), there were no differences between groups, which suggests that geographic variation in quality of care is tightly linked to racial disparities and may account for a large proportion of the differences.
The retrospective analysis of Medicare billing records evaluated 26,482 patients (2,020 blacks [7.6%] and 24,462 non-Hispanic whites [92.4%]) who underwent radical prostatectomy from 1992 through 2009.
Prostate cancer–specific mortality was not significantly different between blacks and whites. Unadjusted overall mortality was increased in blacks, but after adjustment for geographic location, overall mortality was similar between groups.
“Despite important constellations of poor quality of care for blacks undergoing [radical prostatectomy], we did not detect significant differences in overall and cancer-specific survival,” wrote Dr. Marianne Schmid of Brigham and Women’s Hospital, Harvard Medical School, Boston, and her colleagues. Furthermore, the research revealed no regional variation in cancer-specific mortality among patients who underwent surgery.
“A possible interpretation of our findings is that the biological differences in tumor aggressiveness among blacks may have been exaggerated, and that the perceived gap in survival is a result of lack of access or cultural perceptions with regard to surgical care for [prostate cancer] or other factors that differentiate who makes it to the operating table,” the researchers noted.
Median total calculated costs were lower for blacks ($13,015 vs. $15,758), but surgical treatment was associated with higher incremental annual costs, with the top 50% spending $1,185 more. Increased costs are likely due to the higher prevalence of radiotherapy and androgen deprivation therapy, and increased rates of emergency department visits, rather than the use of newer, more expensive technologies.
The research indicates that unfavorable quality of care for black patients did not translate to worse overall survival and cancer-specific survival. Rather, lower survival among black patients with prostate cancer may result from barriers to definitive treatment, according to the investigators.
Dr. Schmid reported having no relevant financial disclosures. Several of her coauthors reported financial ties to several industry sources.
The findings of the study by Dr. Schmid and her colleagues point to racial health inequalities in the United States and are applicable to medical care of the American population in general, not just to men with prostate cancer.

|
Dr. Otis Brawley |
Despite the fact that black patients in this study had insurance and access to care and were considered healthy enough for surgery, there was still a disparity in quality of care. Interestingly, there were no differences between the groups in all-cause or cancer-specific mortality. This is hard evidence that the biology of prostate cancer is similar for black and white men with localized disease.
Is the disparity in quality of care due to racism on the part of physicians? Probably not. More likely, a higher proportion of black men have physicians who do not routinely perform radical prostatectomies, and a higher proportion of blacks are treated at hospitals that have a low volume of prostate surgery.
Even though a significant proportion of blacks received inferior treatment, similar outcomes for the two groups suggests that some patients with localized prostate cancer are overtreated, and the medical community should be more discerning in who receives treatment.
Dr. Otis Brawley is the chief medical officer for the American Cancer Society and professor of hematology, oncology, medicine, and epidemiology at Emory University, Atlanta. These remarks were part of an editorial accompanying the report (JAMA Oncol. 2015 Oct 22. doi: 10.1001/jamaoncol/2015.3384). Dr. Brawley reported having no relevant financial disclosures.
The findings of the study by Dr. Schmid and her colleagues point to racial health inequalities in the United States and are applicable to medical care of the American population in general, not just to men with prostate cancer.

|
Dr. Otis Brawley |
Despite the fact that black patients in this study had insurance and access to care and were considered healthy enough for surgery, there was still a disparity in quality of care. Interestingly, there were no differences between the groups in all-cause or cancer-specific mortality. This is hard evidence that the biology of prostate cancer is similar for black and white men with localized disease.
Is the disparity in quality of care due to racism on the part of physicians? Probably not. More likely, a higher proportion of black men have physicians who do not routinely perform radical prostatectomies, and a higher proportion of blacks are treated at hospitals that have a low volume of prostate surgery.
Even though a significant proportion of blacks received inferior treatment, similar outcomes for the two groups suggests that some patients with localized prostate cancer are overtreated, and the medical community should be more discerning in who receives treatment.
Dr. Otis Brawley is the chief medical officer for the American Cancer Society and professor of hematology, oncology, medicine, and epidemiology at Emory University, Atlanta. These remarks were part of an editorial accompanying the report (JAMA Oncol. 2015 Oct 22. doi: 10.1001/jamaoncol/2015.3384). Dr. Brawley reported having no relevant financial disclosures.
The findings of the study by Dr. Schmid and her colleagues point to racial health inequalities in the United States and are applicable to medical care of the American population in general, not just to men with prostate cancer.

|
Dr. Otis Brawley |
Despite the fact that black patients in this study had insurance and access to care and were considered healthy enough for surgery, there was still a disparity in quality of care. Interestingly, there were no differences between the groups in all-cause or cancer-specific mortality. This is hard evidence that the biology of prostate cancer is similar for black and white men with localized disease.
Is the disparity in quality of care due to racism on the part of physicians? Probably not. More likely, a higher proportion of black men have physicians who do not routinely perform radical prostatectomies, and a higher proportion of blacks are treated at hospitals that have a low volume of prostate surgery.
Even though a significant proportion of blacks received inferior treatment, similar outcomes for the two groups suggests that some patients with localized prostate cancer are overtreated, and the medical community should be more discerning in who receives treatment.
Dr. Otis Brawley is the chief medical officer for the American Cancer Society and professor of hematology, oncology, medicine, and epidemiology at Emory University, Atlanta. These remarks were part of an editorial accompanying the report (JAMA Oncol. 2015 Oct 22. doi: 10.1001/jamaoncol/2015.3384). Dr. Brawley reported having no relevant financial disclosures.
Black patients with localized prostate cancer who underwent radical prostatectomy received inferior surgical care, compared with whites, as evidenced by fewer lymph node dissections and longer delays from diagnosis to treatment, among other indicators, researchers reported.
The time from diagnosis to treatment was longer in blacks than whites (79 vs. 71 days, P = .001). Overall, 57.7% of blacks had surgery without adjuvant therapy, compared with 61.3% of whites (P = .001). Blacks were less likely to undergo lymph node dissection (52.8% vs. 61.5%, P less than .001). The difference persisted but was not significant when the lymph node dissection analysis was restricted to patients with intermediate- and high-risk disease. Blacks were more likely to visit the emergency department within 30 days (P = .04) and beyond 30 days (P = .006) (JAMA Oncol. 2015 Oct 22. doi: 10.1001/jamaoncol/2015.3384).
When the lymph node dissection analysis was adjusted for geographic location (health service area), there were no differences between groups, which suggests that geographic variation in quality of care is tightly linked to racial disparities and may account for a large proportion of the differences.
The retrospective analysis of Medicare billing records evaluated 26,482 patients (2,020 blacks [7.6%] and 24,462 non-Hispanic whites [92.4%]) who underwent radical prostatectomy from 1992 through 2009.
Prostate cancer–specific mortality was not significantly different between blacks and whites. Unadjusted overall mortality was increased in blacks, but after adjustment for geographic location, overall mortality was similar between groups.
“Despite important constellations of poor quality of care for blacks undergoing [radical prostatectomy], we did not detect significant differences in overall and cancer-specific survival,” wrote Dr. Marianne Schmid of Brigham and Women’s Hospital, Harvard Medical School, Boston, and her colleagues. Furthermore, the research revealed no regional variation in cancer-specific mortality among patients who underwent surgery.
“A possible interpretation of our findings is that the biological differences in tumor aggressiveness among blacks may have been exaggerated, and that the perceived gap in survival is a result of lack of access or cultural perceptions with regard to surgical care for [prostate cancer] or other factors that differentiate who makes it to the operating table,” the researchers noted.
Median total calculated costs were lower for blacks ($13,015 vs. $15,758), but surgical treatment was associated with higher incremental annual costs, with the top 50% spending $1,185 more. Increased costs are likely due to the higher prevalence of radiotherapy and androgen deprivation therapy, and increased rates of emergency department visits, rather than the use of newer, more expensive technologies.
The research indicates that unfavorable quality of care for black patients did not translate to worse overall survival and cancer-specific survival. Rather, lower survival among black patients with prostate cancer may result from barriers to definitive treatment, according to the investigators.
Dr. Schmid reported having no relevant financial disclosures. Several of her coauthors reported financial ties to several industry sources.
Black patients with localized prostate cancer who underwent radical prostatectomy received inferior surgical care, compared with whites, as evidenced by fewer lymph node dissections and longer delays from diagnosis to treatment, among other indicators, researchers reported.
The time from diagnosis to treatment was longer in blacks than whites (79 vs. 71 days, P = .001). Overall, 57.7% of blacks had surgery without adjuvant therapy, compared with 61.3% of whites (P = .001). Blacks were less likely to undergo lymph node dissection (52.8% vs. 61.5%, P less than .001). The difference persisted but was not significant when the lymph node dissection analysis was restricted to patients with intermediate- and high-risk disease. Blacks were more likely to visit the emergency department within 30 days (P = .04) and beyond 30 days (P = .006) (JAMA Oncol. 2015 Oct 22. doi: 10.1001/jamaoncol/2015.3384).
When the lymph node dissection analysis was adjusted for geographic location (health service area), there were no differences between groups, which suggests that geographic variation in quality of care is tightly linked to racial disparities and may account for a large proportion of the differences.
The retrospective analysis of Medicare billing records evaluated 26,482 patients (2,020 blacks [7.6%] and 24,462 non-Hispanic whites [92.4%]) who underwent radical prostatectomy from 1992 through 2009.
Prostate cancer–specific mortality was not significantly different between blacks and whites. Unadjusted overall mortality was increased in blacks, but after adjustment for geographic location, overall mortality was similar between groups.
“Despite important constellations of poor quality of care for blacks undergoing [radical prostatectomy], we did not detect significant differences in overall and cancer-specific survival,” wrote Dr. Marianne Schmid of Brigham and Women’s Hospital, Harvard Medical School, Boston, and her colleagues. Furthermore, the research revealed no regional variation in cancer-specific mortality among patients who underwent surgery.
“A possible interpretation of our findings is that the biological differences in tumor aggressiveness among blacks may have been exaggerated, and that the perceived gap in survival is a result of lack of access or cultural perceptions with regard to surgical care for [prostate cancer] or other factors that differentiate who makes it to the operating table,” the researchers noted.
Median total calculated costs were lower for blacks ($13,015 vs. $15,758), but surgical treatment was associated with higher incremental annual costs, with the top 50% spending $1,185 more. Increased costs are likely due to the higher prevalence of radiotherapy and androgen deprivation therapy, and increased rates of emergency department visits, rather than the use of newer, more expensive technologies.
The research indicates that unfavorable quality of care for black patients did not translate to worse overall survival and cancer-specific survival. Rather, lower survival among black patients with prostate cancer may result from barriers to definitive treatment, according to the investigators.
Dr. Schmid reported having no relevant financial disclosures. Several of her coauthors reported financial ties to several industry sources.
FROM JAMA ONCOLOGY
Key clinical point: Compared with whites, black patients with localized prostate cancer received lower quality of care.
Major finding: Blacks were less likely to undergo lymph node dissection than whites (52.8% vs. 61.5%; OR, 0.76; P less than .001), and had more postoperative complications, emergency department visits, and readmissions (P less than .05 for all comparisons).
Data source: A retrospective analysis of Medicare billing records of 26,482 patients (7.6% blacks and 92.4% non-Hispanic whites) who underwent radical prostatectomy from 1992 through 2009.
Disclosures: Dr. Schmid reported having no relevant financial disclosures. Several of her coauthors reported financial ties to several industry sources.
Delayed diagnosis tops breast cancer malpractice claims
The majority of medical malpractice lawsuits involving breast cancer result from delayed-diagnosis allegations, but a significant portion also stem from alleged poor management of breast cancer patients, a study showed.
In a review of 562 breast cancer malpractice claims from 2009 to 2014, 61% related to alleged delays in diagnosing breast cancer, and 39% stemmed from purported negligent treatment of patients, according to a joint analysis by medical liability insurers the Doctors Co. and CRICO.
“It was a big surprise to us to see that almost 40% of our cases involved patients who had already been diagnosed and were already receiving treatment,” said study coauthor Darrell Ranum, vice president of patient safety and risk management for the Doctors Co. “Breast cancer has been studied primarily from the angle of the diagnosis issues. We looked at our data, and we discovered there [was] really another very sizable bucket of claims involving breast cancer cases that involved treatment and management of breast cancer.”
The Doctors Co. and CRICO Strategies, a division of CRICO, pooled their databases of claims to conduct the study. Of the 562 breast cancer cases identified, 342 related to alleged delays in diagnosis, and 220 involved the management of breast cancer patients.
Nearly half of the delayed-diagnosis cases involved radiology (48%). But cases involving radiology did not necessarily result from a radiologist’s negligence. In some cases, primary care physicians or other clinicians may have misread or misinterpreted a radiologist’s report, Mr. Ranum said.
Physician offices/clinical care settings accounted for 39% of the delayed-diagnosis cases with family medicine and gynecology being the most common office settings in which cases originated. Common contributing factors to delayed-diagnosis lawsuits were inadequate patient assessment, such as misinterpretation of diagnostic studies. Delay in ordering diagnostic tests or failure to order them also topped contributing factors.
The vast majority of patients who had a delayed diagnosis of breast cancer were seriously harmed, with 70% of cases resulting in very severe outcomes, including 43 patient deaths, according to the report.
Of the 220 breast cancer management claims, 42% were surgery-related allegations. Patients often claimed poor performance of the initial surgery to remove a malignancy, or negligent performance of subsequent surgeries to reconstruct the breast, the study found.
Additional surgical allegations related to patient dissatisfaction with preoperative or postoperative management. The remaining nonsurgical cases related to medication management and minor procedures during the treatment course. The outcome of breast cancer claims involving surgical treatment were primarily of medium severity, with outcomes such as postoperative hematomas, injury to adjacent organs, and postoperative infections.
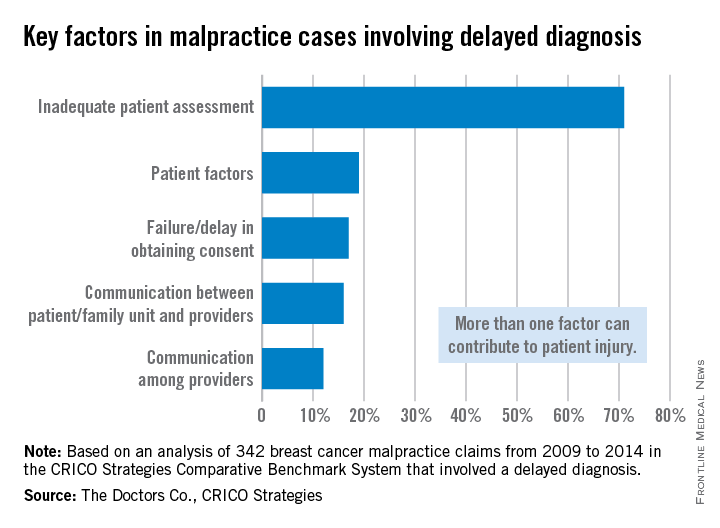
The analysis highlights opportunities for physicians to improve their care of breast cancer patients, both in the timely diagnosis of the disease and the ongoing management of care, Mr. Ranum said. He stressed that obtaining a timely and accurate diagnosis, including a complete history and interpretation of diagnostic studies, is critical. Equally important is the ongoing management of patients once an accurate diagnosis is made. Physicians should also implement processes, including documentation forms, that support and assist clinicians in providing a comprehensive informed consent process and better alignment of patients’ expectations.
“Systems need to be in place and systems need to be tested to make sure they don’t fail so that the information gets to where it needs to go,” Mr. Ranum said. “Our hope is that physicians will take a look at their own internal processes and track a patient from the time the physician says, ‘We need for you to have a mammogram,’ all the way through every step in that process.”
On Twitter @legal_med
The majority of medical malpractice lawsuits involving breast cancer result from delayed-diagnosis allegations, but a significant portion also stem from alleged poor management of breast cancer patients, a study showed.
In a review of 562 breast cancer malpractice claims from 2009 to 2014, 61% related to alleged delays in diagnosing breast cancer, and 39% stemmed from purported negligent treatment of patients, according to a joint analysis by medical liability insurers the Doctors Co. and CRICO.
“It was a big surprise to us to see that almost 40% of our cases involved patients who had already been diagnosed and were already receiving treatment,” said study coauthor Darrell Ranum, vice president of patient safety and risk management for the Doctors Co. “Breast cancer has been studied primarily from the angle of the diagnosis issues. We looked at our data, and we discovered there [was] really another very sizable bucket of claims involving breast cancer cases that involved treatment and management of breast cancer.”
The Doctors Co. and CRICO Strategies, a division of CRICO, pooled their databases of claims to conduct the study. Of the 562 breast cancer cases identified, 342 related to alleged delays in diagnosis, and 220 involved the management of breast cancer patients.
Nearly half of the delayed-diagnosis cases involved radiology (48%). But cases involving radiology did not necessarily result from a radiologist’s negligence. In some cases, primary care physicians or other clinicians may have misread or misinterpreted a radiologist’s report, Mr. Ranum said.
Physician offices/clinical care settings accounted for 39% of the delayed-diagnosis cases with family medicine and gynecology being the most common office settings in which cases originated. Common contributing factors to delayed-diagnosis lawsuits were inadequate patient assessment, such as misinterpretation of diagnostic studies. Delay in ordering diagnostic tests or failure to order them also topped contributing factors.
The vast majority of patients who had a delayed diagnosis of breast cancer were seriously harmed, with 70% of cases resulting in very severe outcomes, including 43 patient deaths, according to the report.
Of the 220 breast cancer management claims, 42% were surgery-related allegations. Patients often claimed poor performance of the initial surgery to remove a malignancy, or negligent performance of subsequent surgeries to reconstruct the breast, the study found.
Additional surgical allegations related to patient dissatisfaction with preoperative or postoperative management. The remaining nonsurgical cases related to medication management and minor procedures during the treatment course. The outcome of breast cancer claims involving surgical treatment were primarily of medium severity, with outcomes such as postoperative hematomas, injury to adjacent organs, and postoperative infections.
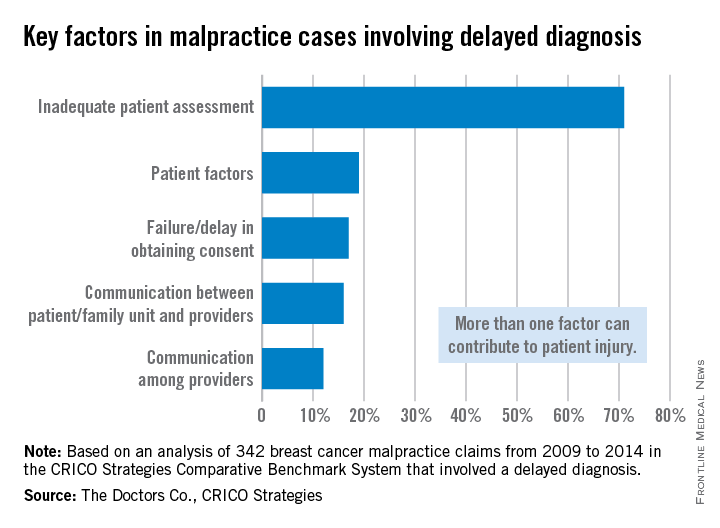
The analysis highlights opportunities for physicians to improve their care of breast cancer patients, both in the timely diagnosis of the disease and the ongoing management of care, Mr. Ranum said. He stressed that obtaining a timely and accurate diagnosis, including a complete history and interpretation of diagnostic studies, is critical. Equally important is the ongoing management of patients once an accurate diagnosis is made. Physicians should also implement processes, including documentation forms, that support and assist clinicians in providing a comprehensive informed consent process and better alignment of patients’ expectations.
“Systems need to be in place and systems need to be tested to make sure they don’t fail so that the information gets to where it needs to go,” Mr. Ranum said. “Our hope is that physicians will take a look at their own internal processes and track a patient from the time the physician says, ‘We need for you to have a mammogram,’ all the way through every step in that process.”
On Twitter @legal_med
The majority of medical malpractice lawsuits involving breast cancer result from delayed-diagnosis allegations, but a significant portion also stem from alleged poor management of breast cancer patients, a study showed.
In a review of 562 breast cancer malpractice claims from 2009 to 2014, 61% related to alleged delays in diagnosing breast cancer, and 39% stemmed from purported negligent treatment of patients, according to a joint analysis by medical liability insurers the Doctors Co. and CRICO.
“It was a big surprise to us to see that almost 40% of our cases involved patients who had already been diagnosed and were already receiving treatment,” said study coauthor Darrell Ranum, vice president of patient safety and risk management for the Doctors Co. “Breast cancer has been studied primarily from the angle of the diagnosis issues. We looked at our data, and we discovered there [was] really another very sizable bucket of claims involving breast cancer cases that involved treatment and management of breast cancer.”
The Doctors Co. and CRICO Strategies, a division of CRICO, pooled their databases of claims to conduct the study. Of the 562 breast cancer cases identified, 342 related to alleged delays in diagnosis, and 220 involved the management of breast cancer patients.
Nearly half of the delayed-diagnosis cases involved radiology (48%). But cases involving radiology did not necessarily result from a radiologist’s negligence. In some cases, primary care physicians or other clinicians may have misread or misinterpreted a radiologist’s report, Mr. Ranum said.
Physician offices/clinical care settings accounted for 39% of the delayed-diagnosis cases with family medicine and gynecology being the most common office settings in which cases originated. Common contributing factors to delayed-diagnosis lawsuits were inadequate patient assessment, such as misinterpretation of diagnostic studies. Delay in ordering diagnostic tests or failure to order them also topped contributing factors.
The vast majority of patients who had a delayed diagnosis of breast cancer were seriously harmed, with 70% of cases resulting in very severe outcomes, including 43 patient deaths, according to the report.
Of the 220 breast cancer management claims, 42% were surgery-related allegations. Patients often claimed poor performance of the initial surgery to remove a malignancy, or negligent performance of subsequent surgeries to reconstruct the breast, the study found.
Additional surgical allegations related to patient dissatisfaction with preoperative or postoperative management. The remaining nonsurgical cases related to medication management and minor procedures during the treatment course. The outcome of breast cancer claims involving surgical treatment were primarily of medium severity, with outcomes such as postoperative hematomas, injury to adjacent organs, and postoperative infections.
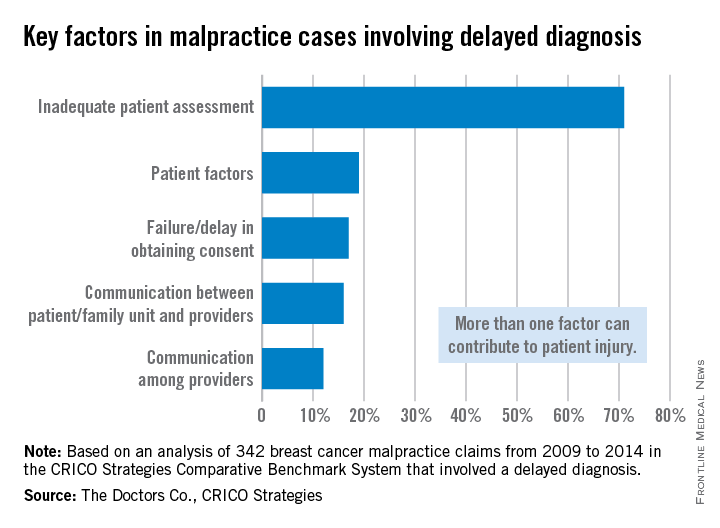
The analysis highlights opportunities for physicians to improve their care of breast cancer patients, both in the timely diagnosis of the disease and the ongoing management of care, Mr. Ranum said. He stressed that obtaining a timely and accurate diagnosis, including a complete history and interpretation of diagnostic studies, is critical. Equally important is the ongoing management of patients once an accurate diagnosis is made. Physicians should also implement processes, including documentation forms, that support and assist clinicians in providing a comprehensive informed consent process and better alignment of patients’ expectations.
“Systems need to be in place and systems need to be tested to make sure they don’t fail so that the information gets to where it needs to go,” Mr. Ranum said. “Our hope is that physicians will take a look at their own internal processes and track a patient from the time the physician says, ‘We need for you to have a mammogram,’ all the way through every step in that process.”
On Twitter @legal_med
Self-assessed mental health scores tied to radical cystectomy complications
Patients with bladder cancer and low scores on self-assessed mental health testing had more high-grade complications after radical cystectomy than their peers with better scores, even though their physical health was comparable, according to research published in the Journal of Urology.
The retrospective study mirrors past work linking preoperative mental disorders to adverse outcomes after major abdominal surgery, bariatric surgery, cardiac surgery, and kidney transplantation, said Dr. Pranav Sharma and his associates at Moffitt Cancer Center in Tampa. This study is the first to examine the association for bladder cancer patients who undergo radical cystectomy, according to the researchers.
They examined 30-day rates of Clavien grade IIIa or greater complications among 274 patients who filled out the Short Form 12 self-assessment of health status less than 6 months before surgery as part of a “new patient” questionnaire (J Urol. 2015. doi:10.1016/j.juro.2015.07.095). This included only 58% of radical cystectomy patients treated at Moffitt, and these patients had higher rates of positive soft-tissue margins and more aggressive pathology than did radical cystectomy patients who did not fill out the SF-12, the researchers said.
In all, 17% of patients experienced at least one high-grade complication within 30 days of their surgery. The median mental health composite score among patients with high-grade complications was 44.8 on a 100-point scale – significantly lower than the 49.8 score for patients who did not experience 30-day high-grade complications (P = .004). Physical composite scores did not significantly differ among patients who did and did not experience 30-day high-grade complications (median, 39.2 for patients with complications vs. 43.8 for those without; P = .06), the investigators said.
A model that incorporated known risk factors for postoperative complications – including age, body mass index, age-adjusted Charlson Comorbidity Index, American Society of Anesthesiologists score, preoperative albumin, and pathologic tumor stage – was not significantly linked with 30-day high-grade complications, even after including the SF-12 physical composite score (P = .14), Dr. Sharma and his associates reported. The association, however, became significant after they added the mental health composite score to the model (odds ratio, 0.96; 95% confidence interval, 0.93-0.99; P = .01).
“Although there is responder subjectivity associated with survey-based health-related [quality of life] measures, this finding suggests that measuring baseline mental health before surgery may provide additional information that can improve the risk stratification of patients undergoing radical cystectomy,” they wrote.
The study might have lacked statistical power to detect some associations, and the small sample size precluded the researchers from testing associations between self-reported health and specific types of complications, they noted. Also, “since we evaluated patients retrospectively, only a non-causal association between preoperative SF-12 mental composite score and high-grade 30-day complications after radical cystectomy can be suggested,” they cautioned.
The research was partly supported by the Collaborative Data Services Core at the H. Lee Moffitt Cancer Center & Research Institute. The investigators declared no conflicts of interest.
Patients with bladder cancer and low scores on self-assessed mental health testing had more high-grade complications after radical cystectomy than their peers with better scores, even though their physical health was comparable, according to research published in the Journal of Urology.
The retrospective study mirrors past work linking preoperative mental disorders to adverse outcomes after major abdominal surgery, bariatric surgery, cardiac surgery, and kidney transplantation, said Dr. Pranav Sharma and his associates at Moffitt Cancer Center in Tampa. This study is the first to examine the association for bladder cancer patients who undergo radical cystectomy, according to the researchers.
They examined 30-day rates of Clavien grade IIIa or greater complications among 274 patients who filled out the Short Form 12 self-assessment of health status less than 6 months before surgery as part of a “new patient” questionnaire (J Urol. 2015. doi:10.1016/j.juro.2015.07.095). This included only 58% of radical cystectomy patients treated at Moffitt, and these patients had higher rates of positive soft-tissue margins and more aggressive pathology than did radical cystectomy patients who did not fill out the SF-12, the researchers said.
In all, 17% of patients experienced at least one high-grade complication within 30 days of their surgery. The median mental health composite score among patients with high-grade complications was 44.8 on a 100-point scale – significantly lower than the 49.8 score for patients who did not experience 30-day high-grade complications (P = .004). Physical composite scores did not significantly differ among patients who did and did not experience 30-day high-grade complications (median, 39.2 for patients with complications vs. 43.8 for those without; P = .06), the investigators said.
A model that incorporated known risk factors for postoperative complications – including age, body mass index, age-adjusted Charlson Comorbidity Index, American Society of Anesthesiologists score, preoperative albumin, and pathologic tumor stage – was not significantly linked with 30-day high-grade complications, even after including the SF-12 physical composite score (P = .14), Dr. Sharma and his associates reported. The association, however, became significant after they added the mental health composite score to the model (odds ratio, 0.96; 95% confidence interval, 0.93-0.99; P = .01).
“Although there is responder subjectivity associated with survey-based health-related [quality of life] measures, this finding suggests that measuring baseline mental health before surgery may provide additional information that can improve the risk stratification of patients undergoing radical cystectomy,” they wrote.
The study might have lacked statistical power to detect some associations, and the small sample size precluded the researchers from testing associations between self-reported health and specific types of complications, they noted. Also, “since we evaluated patients retrospectively, only a non-causal association between preoperative SF-12 mental composite score and high-grade 30-day complications after radical cystectomy can be suggested,” they cautioned.
The research was partly supported by the Collaborative Data Services Core at the H. Lee Moffitt Cancer Center & Research Institute. The investigators declared no conflicts of interest.
Patients with bladder cancer and low scores on self-assessed mental health testing had more high-grade complications after radical cystectomy than their peers with better scores, even though their physical health was comparable, according to research published in the Journal of Urology.
The retrospective study mirrors past work linking preoperative mental disorders to adverse outcomes after major abdominal surgery, bariatric surgery, cardiac surgery, and kidney transplantation, said Dr. Pranav Sharma and his associates at Moffitt Cancer Center in Tampa. This study is the first to examine the association for bladder cancer patients who undergo radical cystectomy, according to the researchers.
They examined 30-day rates of Clavien grade IIIa or greater complications among 274 patients who filled out the Short Form 12 self-assessment of health status less than 6 months before surgery as part of a “new patient” questionnaire (J Urol. 2015. doi:10.1016/j.juro.2015.07.095). This included only 58% of radical cystectomy patients treated at Moffitt, and these patients had higher rates of positive soft-tissue margins and more aggressive pathology than did radical cystectomy patients who did not fill out the SF-12, the researchers said.
In all, 17% of patients experienced at least one high-grade complication within 30 days of their surgery. The median mental health composite score among patients with high-grade complications was 44.8 on a 100-point scale – significantly lower than the 49.8 score for patients who did not experience 30-day high-grade complications (P = .004). Physical composite scores did not significantly differ among patients who did and did not experience 30-day high-grade complications (median, 39.2 for patients with complications vs. 43.8 for those without; P = .06), the investigators said.
A model that incorporated known risk factors for postoperative complications – including age, body mass index, age-adjusted Charlson Comorbidity Index, American Society of Anesthesiologists score, preoperative albumin, and pathologic tumor stage – was not significantly linked with 30-day high-grade complications, even after including the SF-12 physical composite score (P = .14), Dr. Sharma and his associates reported. The association, however, became significant after they added the mental health composite score to the model (odds ratio, 0.96; 95% confidence interval, 0.93-0.99; P = .01).
“Although there is responder subjectivity associated with survey-based health-related [quality of life] measures, this finding suggests that measuring baseline mental health before surgery may provide additional information that can improve the risk stratification of patients undergoing radical cystectomy,” they wrote.
The study might have lacked statistical power to detect some associations, and the small sample size precluded the researchers from testing associations between self-reported health and specific types of complications, they noted. Also, “since we evaluated patients retrospectively, only a non-causal association between preoperative SF-12 mental composite score and high-grade 30-day complications after radical cystectomy can be suggested,” they cautioned.
The research was partly supported by the Collaborative Data Services Core at the H. Lee Moffitt Cancer Center & Research Institute. The investigators declared no conflicts of interest.
FROM THE JOURNAL OF UROLOGY
Key clinical point: Measuring baseline mental health before surgery may provide additional information that can improve the risk stratification of patients undergoing radical cystectomy.
Major finding: The median mental health composite score among patients with high-grade complications was 44.8 on a 100-point scale – significantly lower than the 49.8 median score for patients with no 30-day high-grade complications (P = .004).
Data source: Single-center retrospective study of patients who completed the Short Form 12 less than 6 months before undergoing surgery.
Disclosures: The research was partly supported by the Collaborative Data Services Core at the H. Lee Moffitt Cancer Center and Research Institute. The investigators declared no conflicts of interest.
VIDEO: Tomosynthesis soon to be standard of care for breast cancer screening
CHICAGO – The uptake of tomosynthesis has been fairly brisk among the nation’s breast cancer screening centers.
There are good reasons for that. In an interview at the annual clinical congress of the American College of Surgeons, Dr. Sarah Friedewald, division chief of breast and women’s imaging at Northwestern University, Chicago, explained the procedure; its pluses and minuses; and why it’s likely to be the standard of care for breast cancer screening within 5 years.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – The uptake of tomosynthesis has been fairly brisk among the nation’s breast cancer screening centers.
There are good reasons for that. In an interview at the annual clinical congress of the American College of Surgeons, Dr. Sarah Friedewald, division chief of breast and women’s imaging at Northwestern University, Chicago, explained the procedure; its pluses and minuses; and why it’s likely to be the standard of care for breast cancer screening within 5 years.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – The uptake of tomosynthesis has been fairly brisk among the nation’s breast cancer screening centers.
There are good reasons for that. In an interview at the annual clinical congress of the American College of Surgeons, Dr. Sarah Friedewald, division chief of breast and women’s imaging at Northwestern University, Chicago, explained the procedure; its pluses and minuses; and why it’s likely to be the standard of care for breast cancer screening within 5 years.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE ACS CLINICAL CONGRESS
VIDEO: Immediate breast reconstruction results reassuring in select patients
CHICAGO – Immediate breast reconstruction did not dramatically increase adverse outcomes in women undergoing mastectomy, a SCOAP database analysis found.
The popularity of immediate breast reconstruction is on the rise. Uptake rates, however, vary considerably across the country, prompting some to question whether concerns about adverse outcomes may be putting some surgeons and patients off the procedure.
Using the Surgical Clinical Outcomes Assessment Program database, researchers examined three key outcomes – 30-day readmissions, surgical complications, and surgical site infections – in 757 women who did or did not undergo breast reconstruction within 30 days of mastectomy for stage 0-3 breast cancer.
The results were reassuring, but should be interpreted within the context that those undergoing immediate reconstruction were a select group of women who were more likely to be nonsmokers and less likely to be obese or to be diagnosed with invasive cancer, observed study author Dr. Meghan Flanagan of the University of Washington in Seattle.
Click here to hear our interview with Dr. Flanagan at the annual clinical congress of the American College of Surgeons, where the data were formally presented.
Dr. Flanagan reported no relevant conflicts of interest.
CHICAGO – Immediate breast reconstruction did not dramatically increase adverse outcomes in women undergoing mastectomy, a SCOAP database analysis found.
The popularity of immediate breast reconstruction is on the rise. Uptake rates, however, vary considerably across the country, prompting some to question whether concerns about adverse outcomes may be putting some surgeons and patients off the procedure.
Using the Surgical Clinical Outcomes Assessment Program database, researchers examined three key outcomes – 30-day readmissions, surgical complications, and surgical site infections – in 757 women who did or did not undergo breast reconstruction within 30 days of mastectomy for stage 0-3 breast cancer.
The results were reassuring, but should be interpreted within the context that those undergoing immediate reconstruction were a select group of women who were more likely to be nonsmokers and less likely to be obese or to be diagnosed with invasive cancer, observed study author Dr. Meghan Flanagan of the University of Washington in Seattle.
Click here to hear our interview with Dr. Flanagan at the annual clinical congress of the American College of Surgeons, where the data were formally presented.
Dr. Flanagan reported no relevant conflicts of interest.
CHICAGO – Immediate breast reconstruction did not dramatically increase adverse outcomes in women undergoing mastectomy, a SCOAP database analysis found.
The popularity of immediate breast reconstruction is on the rise. Uptake rates, however, vary considerably across the country, prompting some to question whether concerns about adverse outcomes may be putting some surgeons and patients off the procedure.
Using the Surgical Clinical Outcomes Assessment Program database, researchers examined three key outcomes – 30-day readmissions, surgical complications, and surgical site infections – in 757 women who did or did not undergo breast reconstruction within 30 days of mastectomy for stage 0-3 breast cancer.
The results were reassuring, but should be interpreted within the context that those undergoing immediate reconstruction were a select group of women who were more likely to be nonsmokers and less likely to be obese or to be diagnosed with invasive cancer, observed study author Dr. Meghan Flanagan of the University of Washington in Seattle.
Click here to hear our interview with Dr. Flanagan at the annual clinical congress of the American College of Surgeons, where the data were formally presented.
Dr. Flanagan reported no relevant conflicts of interest.
AT THE ACS ANNUAL CONGRESS
Better outcomes with open surgery vs. laparoscopic for rectal cancer
Two randomized studies of rectal cancer surgeries using highly qualified surgeons were not able to show that laparoscopic procedures produce results equal to open ones.
The studies, published online in JAMA, each enrolled slightly under 500 patients at multiple sites, randomized them to open pelvic dissection or laparoscopic dissection, and selected surgeons with exceptional skills.
Both studies found rates of pathologist-determined adequate surgical dissection to be slightly lower for patients undergoing the laparoscopic procedures.
The North American study was carried out under the American College of Surgeons Oncology Group and led by Dr. James Fleshman of Baylor University Medical Center, Dallas. The study, which took place at 35 surgical centers, enrolled 486 patients with stage II or III rectal cancer within 12 cm of the anal verge who were randomized after neoadjuvant therapy to minimally invasive (n = 240) or open proctectomy (n=222) (JAMA. 2015;314[13]:1346-55).
Success was measured by pathologic oncologic markers related to quality of the rectal specimen: a composite of circumferential radial margin greater than 1 mm, distal margin without tumor, and completeness of total mesorectal excision. A 6% noninferiority margin was chosen according to clinical relevance estimations for this patient group.
Successful resection occurred in 82% of laparoscopic resection cases (95% confidence interval, 76.8%-86.6%) and 87% of open cases (95% CI, 82.5%-91.4%). The results did not support noninferiority for laparoscopic procedures (P = .41).
The finding came as a surprise, Dr. Fleshman and colleagues wrote in their analysis, not least because of the skill level of the surgeons participating in the study. A group of “highly motivated, credentialed, expert laparoscopic rectal surgeons was ideal to test this hypothesis,” they wrote. Moreover, only 11% of patients assigned laparoscopy had to be converted to open procedures, “so the learning curve cannot be invoked to explain our results because conversion rates were reasonable.”
More likely, they wrote, “the technique itself, along with the current methodology available, must be questioned if motivated experts cannot produce a quality specimen defined by this novel combined metric.”
Proctectomy is always challenging, Dr. Fleshman and colleagues wrote, “and it can be even more difficult to work in the deep pelvis with in-line rigid instruments from angles that require complicated maneuvers to reach the extremes of the pelvis. It is possible that modification of instruments or a different platform such as robotics will improve efficacy of minimally invasive techniques.”
The Australian study, carried out by the Australasian Gastro-Intestinal Trials Group network and led by Dr. Andrew R. L. Stevenson of the University of Queensland and Royal Brisbane and Women’s Hospital, Brisbane, Australia, enrolled 475 patients with T1-3 rectal tumors less than 15 cm from the anal verge and randomized them to laparoscopic (n = 238) or open (n = 235) pelvic dissection. Half of patients had received radiotherapy before the operations. Some 26 surgeons operated at 24 sites in Australia and New Zealand. (JAMA. 2015;314[13]:1356-63).
For this trial, successful resection was defined as complete total mesorectal excision, a clear circumferential margin of at least 1 mm, and a clear distal resection margin of 1 mm or more. The prescribed noninferiority margin for this patient group was 8%. As in the North American study, pathologists were blinded to the method of surgery.
Successful resection occurred in 194 patients (82%) in the laparoscopic group and 208 (89%) in the open surgery group, not reaching noninferiority for the laparoscopic approach (P = 0.38 for noninferiority). Conversion to open dissection occurred in 9% of the laparoscopy-assigned patients.
“Even though our trial was not designed to demonstrate whether one method of rectal dissection was superior to the other, the inability to establish noninferiority suggests that surgeons should be cautious when considering the suitability of a laparoscopic approach for a patient with rectal cancer,” Dr. Stevenson and colleagues wrote in their analysis.
“Subgroup analyses raise the possibility that laparoscopic surgery might be less successful than open surgery in patients who have received neoadjuvant therapy, have larger T3 tumors, or have higher BMIs. However, our study was underpowered to show significant differences in proportions of lower success rates for laparoscopic surgery vs. open surgery.”
The North American trial was funded by the National Cancer Institute, the American Society of Colon and Rectal Surgeons, the Society of American Gastrointestinal and Endoscopic Surgeons, and the Covidien Company. Dr. Fleshman reported no conflicts, while several coauthors disclosed financial relationships with surgical device manufacturers, including Covidien.
The Australasian trial was funded by the Colorectal Surgical Society of Australia and New Zealand and the National Health and Medical Research Council. No conflicts of interest were reported.
The studies by Fleshman et al. and Stevenson et al. have set a standard for surgeons performing these complex operations and the surgical expertise that must be ensured when conducting randomized clinical trials. In both studies, only surgeons accredited after video review of relevant operations were allowed to participate, and the primary outcome was defined as the adequacy of surgical dissection as assessed by completeness of the total mesorectal excision, uninvolved CRM, and uninvolved distal resection margin. The technical quality of surgery in both trials was high as demonstrated by few laparoscopic conversions, high sphincter preservation rates, and low rates of anastomotic leakage and other complications in these study groups that included high-risk overweight patients, the majority of whom were male. Likewise, the composite pathologic success rate based on meeting all three surgical dissection criteria was very high. However, in both studies, the adequacy of surgical dissection tended to be lower in the minimally invasive group, compared with the open resection group despite comparable low rates of distal margin involvement. Although several nonrandomized studies with inherent selection bias have described the overall advantages of a minimally invasive approach for patients with rectal cancer or complicated diverticulitis, these large, randomized, multicenter trials substantiate recent findings from similar randomized trials. A laparoscopic resection may not be oncologically justified in many patients requiring proctectomy for rectal cancer. The studies do not signal a moratorium on laparoscopic approaches, but surgeons must proceed in a judicious manner to ensure that patients are informed about the benefits and risks associated with minimally invasive and open operations.
Dr. Scott A. Strong and Dr. Nathaniel J. Soper are with Northwestern University Feinberg School of Medicine, Chicago. Dr. Strong and Dr. Soper declared no conflicts of interest. These remarks were excerpted from an accompanying editorial (JAMA. 2015 Oct 6. doi: 10.1001/jama.2015.11454).
The studies by Fleshman et al. and Stevenson et al. have set a standard for surgeons performing these complex operations and the surgical expertise that must be ensured when conducting randomized clinical trials. In both studies, only surgeons accredited after video review of relevant operations were allowed to participate, and the primary outcome was defined as the adequacy of surgical dissection as assessed by completeness of the total mesorectal excision, uninvolved CRM, and uninvolved distal resection margin. The technical quality of surgery in both trials was high as demonstrated by few laparoscopic conversions, high sphincter preservation rates, and low rates of anastomotic leakage and other complications in these study groups that included high-risk overweight patients, the majority of whom were male. Likewise, the composite pathologic success rate based on meeting all three surgical dissection criteria was very high. However, in both studies, the adequacy of surgical dissection tended to be lower in the minimally invasive group, compared with the open resection group despite comparable low rates of distal margin involvement. Although several nonrandomized studies with inherent selection bias have described the overall advantages of a minimally invasive approach for patients with rectal cancer or complicated diverticulitis, these large, randomized, multicenter trials substantiate recent findings from similar randomized trials. A laparoscopic resection may not be oncologically justified in many patients requiring proctectomy for rectal cancer. The studies do not signal a moratorium on laparoscopic approaches, but surgeons must proceed in a judicious manner to ensure that patients are informed about the benefits and risks associated with minimally invasive and open operations.
Dr. Scott A. Strong and Dr. Nathaniel J. Soper are with Northwestern University Feinberg School of Medicine, Chicago. Dr. Strong and Dr. Soper declared no conflicts of interest. These remarks were excerpted from an accompanying editorial (JAMA. 2015 Oct 6. doi: 10.1001/jama.2015.11454).
The studies by Fleshman et al. and Stevenson et al. have set a standard for surgeons performing these complex operations and the surgical expertise that must be ensured when conducting randomized clinical trials. In both studies, only surgeons accredited after video review of relevant operations were allowed to participate, and the primary outcome was defined as the adequacy of surgical dissection as assessed by completeness of the total mesorectal excision, uninvolved CRM, and uninvolved distal resection margin. The technical quality of surgery in both trials was high as demonstrated by few laparoscopic conversions, high sphincter preservation rates, and low rates of anastomotic leakage and other complications in these study groups that included high-risk overweight patients, the majority of whom were male. Likewise, the composite pathologic success rate based on meeting all three surgical dissection criteria was very high. However, in both studies, the adequacy of surgical dissection tended to be lower in the minimally invasive group, compared with the open resection group despite comparable low rates of distal margin involvement. Although several nonrandomized studies with inherent selection bias have described the overall advantages of a minimally invasive approach for patients with rectal cancer or complicated diverticulitis, these large, randomized, multicenter trials substantiate recent findings from similar randomized trials. A laparoscopic resection may not be oncologically justified in many patients requiring proctectomy for rectal cancer. The studies do not signal a moratorium on laparoscopic approaches, but surgeons must proceed in a judicious manner to ensure that patients are informed about the benefits and risks associated with minimally invasive and open operations.
Dr. Scott A. Strong and Dr. Nathaniel J. Soper are with Northwestern University Feinberg School of Medicine, Chicago. Dr. Strong and Dr. Soper declared no conflicts of interest. These remarks were excerpted from an accompanying editorial (JAMA. 2015 Oct 6. doi: 10.1001/jama.2015.11454).
Two randomized studies of rectal cancer surgeries using highly qualified surgeons were not able to show that laparoscopic procedures produce results equal to open ones.
The studies, published online in JAMA, each enrolled slightly under 500 patients at multiple sites, randomized them to open pelvic dissection or laparoscopic dissection, and selected surgeons with exceptional skills.
Both studies found rates of pathologist-determined adequate surgical dissection to be slightly lower for patients undergoing the laparoscopic procedures.
The North American study was carried out under the American College of Surgeons Oncology Group and led by Dr. James Fleshman of Baylor University Medical Center, Dallas. The study, which took place at 35 surgical centers, enrolled 486 patients with stage II or III rectal cancer within 12 cm of the anal verge who were randomized after neoadjuvant therapy to minimally invasive (n = 240) or open proctectomy (n=222) (JAMA. 2015;314[13]:1346-55).
Success was measured by pathologic oncologic markers related to quality of the rectal specimen: a composite of circumferential radial margin greater than 1 mm, distal margin without tumor, and completeness of total mesorectal excision. A 6% noninferiority margin was chosen according to clinical relevance estimations for this patient group.
Successful resection occurred in 82% of laparoscopic resection cases (95% confidence interval, 76.8%-86.6%) and 87% of open cases (95% CI, 82.5%-91.4%). The results did not support noninferiority for laparoscopic procedures (P = .41).
The finding came as a surprise, Dr. Fleshman and colleagues wrote in their analysis, not least because of the skill level of the surgeons participating in the study. A group of “highly motivated, credentialed, expert laparoscopic rectal surgeons was ideal to test this hypothesis,” they wrote. Moreover, only 11% of patients assigned laparoscopy had to be converted to open procedures, “so the learning curve cannot be invoked to explain our results because conversion rates were reasonable.”
More likely, they wrote, “the technique itself, along with the current methodology available, must be questioned if motivated experts cannot produce a quality specimen defined by this novel combined metric.”
Proctectomy is always challenging, Dr. Fleshman and colleagues wrote, “and it can be even more difficult to work in the deep pelvis with in-line rigid instruments from angles that require complicated maneuvers to reach the extremes of the pelvis. It is possible that modification of instruments or a different platform such as robotics will improve efficacy of minimally invasive techniques.”
The Australian study, carried out by the Australasian Gastro-Intestinal Trials Group network and led by Dr. Andrew R. L. Stevenson of the University of Queensland and Royal Brisbane and Women’s Hospital, Brisbane, Australia, enrolled 475 patients with T1-3 rectal tumors less than 15 cm from the anal verge and randomized them to laparoscopic (n = 238) or open (n = 235) pelvic dissection. Half of patients had received radiotherapy before the operations. Some 26 surgeons operated at 24 sites in Australia and New Zealand. (JAMA. 2015;314[13]:1356-63).
For this trial, successful resection was defined as complete total mesorectal excision, a clear circumferential margin of at least 1 mm, and a clear distal resection margin of 1 mm or more. The prescribed noninferiority margin for this patient group was 8%. As in the North American study, pathologists were blinded to the method of surgery.
Successful resection occurred in 194 patients (82%) in the laparoscopic group and 208 (89%) in the open surgery group, not reaching noninferiority for the laparoscopic approach (P = 0.38 for noninferiority). Conversion to open dissection occurred in 9% of the laparoscopy-assigned patients.
“Even though our trial was not designed to demonstrate whether one method of rectal dissection was superior to the other, the inability to establish noninferiority suggests that surgeons should be cautious when considering the suitability of a laparoscopic approach for a patient with rectal cancer,” Dr. Stevenson and colleagues wrote in their analysis.
“Subgroup analyses raise the possibility that laparoscopic surgery might be less successful than open surgery in patients who have received neoadjuvant therapy, have larger T3 tumors, or have higher BMIs. However, our study was underpowered to show significant differences in proportions of lower success rates for laparoscopic surgery vs. open surgery.”
The North American trial was funded by the National Cancer Institute, the American Society of Colon and Rectal Surgeons, the Society of American Gastrointestinal and Endoscopic Surgeons, and the Covidien Company. Dr. Fleshman reported no conflicts, while several coauthors disclosed financial relationships with surgical device manufacturers, including Covidien.
The Australasian trial was funded by the Colorectal Surgical Society of Australia and New Zealand and the National Health and Medical Research Council. No conflicts of interest were reported.
Two randomized studies of rectal cancer surgeries using highly qualified surgeons were not able to show that laparoscopic procedures produce results equal to open ones.
The studies, published online in JAMA, each enrolled slightly under 500 patients at multiple sites, randomized them to open pelvic dissection or laparoscopic dissection, and selected surgeons with exceptional skills.
Both studies found rates of pathologist-determined adequate surgical dissection to be slightly lower for patients undergoing the laparoscopic procedures.
The North American study was carried out under the American College of Surgeons Oncology Group and led by Dr. James Fleshman of Baylor University Medical Center, Dallas. The study, which took place at 35 surgical centers, enrolled 486 patients with stage II or III rectal cancer within 12 cm of the anal verge who were randomized after neoadjuvant therapy to minimally invasive (n = 240) or open proctectomy (n=222) (JAMA. 2015;314[13]:1346-55).
Success was measured by pathologic oncologic markers related to quality of the rectal specimen: a composite of circumferential radial margin greater than 1 mm, distal margin without tumor, and completeness of total mesorectal excision. A 6% noninferiority margin was chosen according to clinical relevance estimations for this patient group.
Successful resection occurred in 82% of laparoscopic resection cases (95% confidence interval, 76.8%-86.6%) and 87% of open cases (95% CI, 82.5%-91.4%). The results did not support noninferiority for laparoscopic procedures (P = .41).
The finding came as a surprise, Dr. Fleshman and colleagues wrote in their analysis, not least because of the skill level of the surgeons participating in the study. A group of “highly motivated, credentialed, expert laparoscopic rectal surgeons was ideal to test this hypothesis,” they wrote. Moreover, only 11% of patients assigned laparoscopy had to be converted to open procedures, “so the learning curve cannot be invoked to explain our results because conversion rates were reasonable.”
More likely, they wrote, “the technique itself, along with the current methodology available, must be questioned if motivated experts cannot produce a quality specimen defined by this novel combined metric.”
Proctectomy is always challenging, Dr. Fleshman and colleagues wrote, “and it can be even more difficult to work in the deep pelvis with in-line rigid instruments from angles that require complicated maneuvers to reach the extremes of the pelvis. It is possible that modification of instruments or a different platform such as robotics will improve efficacy of minimally invasive techniques.”
The Australian study, carried out by the Australasian Gastro-Intestinal Trials Group network and led by Dr. Andrew R. L. Stevenson of the University of Queensland and Royal Brisbane and Women’s Hospital, Brisbane, Australia, enrolled 475 patients with T1-3 rectal tumors less than 15 cm from the anal verge and randomized them to laparoscopic (n = 238) or open (n = 235) pelvic dissection. Half of patients had received radiotherapy before the operations. Some 26 surgeons operated at 24 sites in Australia and New Zealand. (JAMA. 2015;314[13]:1356-63).
For this trial, successful resection was defined as complete total mesorectal excision, a clear circumferential margin of at least 1 mm, and a clear distal resection margin of 1 mm or more. The prescribed noninferiority margin for this patient group was 8%. As in the North American study, pathologists were blinded to the method of surgery.
Successful resection occurred in 194 patients (82%) in the laparoscopic group and 208 (89%) in the open surgery group, not reaching noninferiority for the laparoscopic approach (P = 0.38 for noninferiority). Conversion to open dissection occurred in 9% of the laparoscopy-assigned patients.
“Even though our trial was not designed to demonstrate whether one method of rectal dissection was superior to the other, the inability to establish noninferiority suggests that surgeons should be cautious when considering the suitability of a laparoscopic approach for a patient with rectal cancer,” Dr. Stevenson and colleagues wrote in their analysis.
“Subgroup analyses raise the possibility that laparoscopic surgery might be less successful than open surgery in patients who have received neoadjuvant therapy, have larger T3 tumors, or have higher BMIs. However, our study was underpowered to show significant differences in proportions of lower success rates for laparoscopic surgery vs. open surgery.”
The North American trial was funded by the National Cancer Institute, the American Society of Colon and Rectal Surgeons, the Society of American Gastrointestinal and Endoscopic Surgeons, and the Covidien Company. Dr. Fleshman reported no conflicts, while several coauthors disclosed financial relationships with surgical device manufacturers, including Covidien.
The Australasian trial was funded by the Colorectal Surgical Society of Australia and New Zealand and the National Health and Medical Research Council. No conflicts of interest were reported.
FROM JAMA
Key clinical point: Two studies evaluating resection results failed to show laparoscopic surgeries for colorectal cancer as noninferior to open procedures.
Major finding: Among patients with stage III or IV rectal cancers, successful resection occurred in 81.7% of laparoscopic resection cases (95% CI, 76.8%-86.6%) and 86.9% of open resection cases (95% CI, 82.5%-91.4%), not supporting noninferiority for laparoscopic procedures (P = .41 for noninferiority). Similarly, among patients with T1-3 rectal tumors, 82% assigned laparoscopic surgery and 89% in the open surgery group saw adequate resections (P = .38 for noninferiority).
Data source: Randomized trials of slightly under 500 patients each at multiple study sites in North America, Australia, and New Zealand.
Disclosures: Australian-led study was publicly and institutionally funded with no investigator disclosures; U.S.-led study had support from a device manufacturer and several coauthors disclosed support from this and other manufacturers.











