User login
Official Newspaper of the American College of Surgeons
VIDEO: Counseling patients considering contralateral prophylactic mastectomy
MIAMI – The number of women with ipsilateral breast cancer seeking a contralateral mastectomy to reduce their future risk and, essentially, for peace of mind, is increasing. Dr. Anees Chagpar director of the Breast Center, Smilow Cancer Hospital at Yale-New Haven (Conn.), suggests what doctors can include in discussions with these patients.
Presenting patients with a complete picture of risks and benefits promotes shared decision-making. Consider the absolute risk reduction provided by this type of surgery, particularly in older patients who are not BRCA 1 or 2 carriers, Dr. Chagpar said at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
Differences between unilateral and bilateral surgery go beyond operative time, duration of hospital stay, and risk of complications, Dr. Chagpar said, and should include a discussion about patient values and what is driving their consideration of this surgery.
Dr. Chagpar had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MIAMI – The number of women with ipsilateral breast cancer seeking a contralateral mastectomy to reduce their future risk and, essentially, for peace of mind, is increasing. Dr. Anees Chagpar director of the Breast Center, Smilow Cancer Hospital at Yale-New Haven (Conn.), suggests what doctors can include in discussions with these patients.
Presenting patients with a complete picture of risks and benefits promotes shared decision-making. Consider the absolute risk reduction provided by this type of surgery, particularly in older patients who are not BRCA 1 or 2 carriers, Dr. Chagpar said at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
Differences between unilateral and bilateral surgery go beyond operative time, duration of hospital stay, and risk of complications, Dr. Chagpar said, and should include a discussion about patient values and what is driving their consideration of this surgery.
Dr. Chagpar had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MIAMI – The number of women with ipsilateral breast cancer seeking a contralateral mastectomy to reduce their future risk and, essentially, for peace of mind, is increasing. Dr. Anees Chagpar director of the Breast Center, Smilow Cancer Hospital at Yale-New Haven (Conn.), suggests what doctors can include in discussions with these patients.
Presenting patients with a complete picture of risks and benefits promotes shared decision-making. Consider the absolute risk reduction provided by this type of surgery, particularly in older patients who are not BRCA 1 or 2 carriers, Dr. Chagpar said at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
Differences between unilateral and bilateral surgery go beyond operative time, duration of hospital stay, and risk of complications, Dr. Chagpar said, and should include a discussion about patient values and what is driving their consideration of this surgery.
Dr. Chagpar had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM MBCC
Review: Use wider margins for DCIS surgery without radiotherapy
MIAMI – A wider margin width for women undergoing breast-conserving surgery without radiotherapy for ductal carcinoma in situ (DCIS) may be better for women than the 2-mm or greater margin width for women undergoing radiotherapy that was recently recommended in a draft consensus statement.
The draft consensus statement is currently under review by the Society of Surgical Oncology, the American Society for Radiation Oncology, the American Society of Clinical Oncology, and the American Society of Breast Surgeons, Dr. Kimberly Van Zee, who participated in the November consensus conference, reported at the annual Miami Breast Cancer Conference, held by the Physicians’ Education Resource.
The draft consensus statement does not address margin width in those who are not receiving radiotherapy because data are lacking in that population, but in her own retrospective review of nearly 3,000 cases, Dr. Van Zee found that “wider margin width is associated with a lower risk of recurrence among women not undergoing radiation.”
Her review, published in October (Ann Surg. 2015;262:623-31) and considered in the development of the draft consensus statement, included 2,996 consecutive women who underwent breast conserving surgery between 1978 and 2010. Of those, 363 experienced recurrence; 732 of the women were followed for at least 10 years, and the median follow-up period was 75 months, said Dr. Van Zee, a surgical oncologist at Memorial Sloan Kettering Cancer Center, New York.
After controlling for age, family history, clinical vs. radiologic presentation, nuclear grade, number of excisions, radiotherapy, endocrine therapy, and year of surgery, margin width was shown to be significantly associated with recurrence, she noted.
Women with larger negative margins had a significantly lower risk of recurrence vs. those with positive margins, she said.
An interaction between radiation therapy and margin width was significant, which indicates that the effect of margin width differs by use of radiation therapy, she noted.
Stratification by radiation therapy use demonstrated that the association of recurrence with margin width was significant in those not receiving radiation therapy, but not in those receiving radiation therapy.
Among those not receiving radiation therapy, a margin width of greater than 10 mm was associated with about a 60% reduction in recurrence, compared with those with negative margins of 2 mm or less.
The findings are important, because while DCIS has minimal mortality, recurrence rates after breast-conserving surgery are significant, and about half of recurrences are invasive, she explained.
“We know that negative margins are clearly a factor that’s associated with a lower risk of recurrence; the problem with all of our randomized trials and many retrospective studies is that margins have been categorized as positive or negative, so that doesn’t help us in determining what the optimal negative margin is,” she said.
Importantly, while radiation is known to reduce the rate of recurrence, that reduction is proportional.
“In every subset, radiation reduces risk by about half,” she said, noting that in patients with low risk, a 50% reduction may not be worth it.
Conference chair Dr. Patrick I. Borgen of Maimonides Medical Center in Brooklyn, N.Y., praised Dr. Van Zee’s work, saying that “without any question, that review will significantly impact the meta-analysis as we go forward and try to make some sense of what to do with our patients with DCIS.”
Dr. Van Zee reported having no disclosures. Dr. Borgen is on speakers bureaus for Genomic Health and NanoString Technologies.
MIAMI – A wider margin width for women undergoing breast-conserving surgery without radiotherapy for ductal carcinoma in situ (DCIS) may be better for women than the 2-mm or greater margin width for women undergoing radiotherapy that was recently recommended in a draft consensus statement.
The draft consensus statement is currently under review by the Society of Surgical Oncology, the American Society for Radiation Oncology, the American Society of Clinical Oncology, and the American Society of Breast Surgeons, Dr. Kimberly Van Zee, who participated in the November consensus conference, reported at the annual Miami Breast Cancer Conference, held by the Physicians’ Education Resource.
The draft consensus statement does not address margin width in those who are not receiving radiotherapy because data are lacking in that population, but in her own retrospective review of nearly 3,000 cases, Dr. Van Zee found that “wider margin width is associated with a lower risk of recurrence among women not undergoing radiation.”
Her review, published in October (Ann Surg. 2015;262:623-31) and considered in the development of the draft consensus statement, included 2,996 consecutive women who underwent breast conserving surgery between 1978 and 2010. Of those, 363 experienced recurrence; 732 of the women were followed for at least 10 years, and the median follow-up period was 75 months, said Dr. Van Zee, a surgical oncologist at Memorial Sloan Kettering Cancer Center, New York.
After controlling for age, family history, clinical vs. radiologic presentation, nuclear grade, number of excisions, radiotherapy, endocrine therapy, and year of surgery, margin width was shown to be significantly associated with recurrence, she noted.
Women with larger negative margins had a significantly lower risk of recurrence vs. those with positive margins, she said.
An interaction between radiation therapy and margin width was significant, which indicates that the effect of margin width differs by use of radiation therapy, she noted.
Stratification by radiation therapy use demonstrated that the association of recurrence with margin width was significant in those not receiving radiation therapy, but not in those receiving radiation therapy.
Among those not receiving radiation therapy, a margin width of greater than 10 mm was associated with about a 60% reduction in recurrence, compared with those with negative margins of 2 mm or less.
The findings are important, because while DCIS has minimal mortality, recurrence rates after breast-conserving surgery are significant, and about half of recurrences are invasive, she explained.
“We know that negative margins are clearly a factor that’s associated with a lower risk of recurrence; the problem with all of our randomized trials and many retrospective studies is that margins have been categorized as positive or negative, so that doesn’t help us in determining what the optimal negative margin is,” she said.
Importantly, while radiation is known to reduce the rate of recurrence, that reduction is proportional.
“In every subset, radiation reduces risk by about half,” she said, noting that in patients with low risk, a 50% reduction may not be worth it.
Conference chair Dr. Patrick I. Borgen of Maimonides Medical Center in Brooklyn, N.Y., praised Dr. Van Zee’s work, saying that “without any question, that review will significantly impact the meta-analysis as we go forward and try to make some sense of what to do with our patients with DCIS.”
Dr. Van Zee reported having no disclosures. Dr. Borgen is on speakers bureaus for Genomic Health and NanoString Technologies.
MIAMI – A wider margin width for women undergoing breast-conserving surgery without radiotherapy for ductal carcinoma in situ (DCIS) may be better for women than the 2-mm or greater margin width for women undergoing radiotherapy that was recently recommended in a draft consensus statement.
The draft consensus statement is currently under review by the Society of Surgical Oncology, the American Society for Radiation Oncology, the American Society of Clinical Oncology, and the American Society of Breast Surgeons, Dr. Kimberly Van Zee, who participated in the November consensus conference, reported at the annual Miami Breast Cancer Conference, held by the Physicians’ Education Resource.
The draft consensus statement does not address margin width in those who are not receiving radiotherapy because data are lacking in that population, but in her own retrospective review of nearly 3,000 cases, Dr. Van Zee found that “wider margin width is associated with a lower risk of recurrence among women not undergoing radiation.”
Her review, published in October (Ann Surg. 2015;262:623-31) and considered in the development of the draft consensus statement, included 2,996 consecutive women who underwent breast conserving surgery between 1978 and 2010. Of those, 363 experienced recurrence; 732 of the women were followed for at least 10 years, and the median follow-up period was 75 months, said Dr. Van Zee, a surgical oncologist at Memorial Sloan Kettering Cancer Center, New York.
After controlling for age, family history, clinical vs. radiologic presentation, nuclear grade, number of excisions, radiotherapy, endocrine therapy, and year of surgery, margin width was shown to be significantly associated with recurrence, she noted.
Women with larger negative margins had a significantly lower risk of recurrence vs. those with positive margins, she said.
An interaction between radiation therapy and margin width was significant, which indicates that the effect of margin width differs by use of radiation therapy, she noted.
Stratification by radiation therapy use demonstrated that the association of recurrence with margin width was significant in those not receiving radiation therapy, but not in those receiving radiation therapy.
Among those not receiving radiation therapy, a margin width of greater than 10 mm was associated with about a 60% reduction in recurrence, compared with those with negative margins of 2 mm or less.
The findings are important, because while DCIS has minimal mortality, recurrence rates after breast-conserving surgery are significant, and about half of recurrences are invasive, she explained.
“We know that negative margins are clearly a factor that’s associated with a lower risk of recurrence; the problem with all of our randomized trials and many retrospective studies is that margins have been categorized as positive or negative, so that doesn’t help us in determining what the optimal negative margin is,” she said.
Importantly, while radiation is known to reduce the rate of recurrence, that reduction is proportional.
“In every subset, radiation reduces risk by about half,” she said, noting that in patients with low risk, a 50% reduction may not be worth it.
Conference chair Dr. Patrick I. Borgen of Maimonides Medical Center in Brooklyn, N.Y., praised Dr. Van Zee’s work, saying that “without any question, that review will significantly impact the meta-analysis as we go forward and try to make some sense of what to do with our patients with DCIS.”
Dr. Van Zee reported having no disclosures. Dr. Borgen is on speakers bureaus for Genomic Health and NanoString Technologies.
AT MBCC
Key clinical point: A 2-mm or greater margin is optimal in women undergoing breast-conserving surgery and radiotherapy for ductal carcinoma in situ, according to the conclusion of a recent consensus conference, but wider margins may be needed in the absence of radiotherapy.
Major finding: Among those not receiving radiation therapy, a margin width of greater than 10 mm was associated with about a 60% reduction in recurrence, compared with those with negative margins of 2 mm or less.
Data source: A retrospective review of 2,996 cases
Disclosures: Dr. Van Zee reported having no disclosures. Dr. Borgen is on speakers bureaus for Genomic Health and NanoString Technologies.
VIDEO: Breast cancer surgery choice depends on the individual
MIAMI – In addition to a thorough discussion of the risks and benefits of breast-conserving therapy and mastectomy, physicians need to address the individual concerns that each patient will have before choosing a procedure, Dr. Patrick Borgen, chair of the department of surgery at Maimonides Medical Center in Brooklyn, N.Y., said.
The facts do not support the superiority of one procedure over another for all women, Dr. Borgen said at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource. When discussing the options, each individual patient will have unique concerns and quality of life issues that need to be factored into a collaborative decision about the choice of procedure.
Not including mastectomy in the conversation could be a disservice to the patient, Dr. Borgen said. Quality of life over time, patient anxiety, and “the price of vigilance” are additional factors that patients consider when weighing their surgical options.
Dr. Borgen had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MIAMI – In addition to a thorough discussion of the risks and benefits of breast-conserving therapy and mastectomy, physicians need to address the individual concerns that each patient will have before choosing a procedure, Dr. Patrick Borgen, chair of the department of surgery at Maimonides Medical Center in Brooklyn, N.Y., said.
The facts do not support the superiority of one procedure over another for all women, Dr. Borgen said at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource. When discussing the options, each individual patient will have unique concerns and quality of life issues that need to be factored into a collaborative decision about the choice of procedure.
Not including mastectomy in the conversation could be a disservice to the patient, Dr. Borgen said. Quality of life over time, patient anxiety, and “the price of vigilance” are additional factors that patients consider when weighing their surgical options.
Dr. Borgen had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MIAMI – In addition to a thorough discussion of the risks and benefits of breast-conserving therapy and mastectomy, physicians need to address the individual concerns that each patient will have before choosing a procedure, Dr. Patrick Borgen, chair of the department of surgery at Maimonides Medical Center in Brooklyn, N.Y., said.
The facts do not support the superiority of one procedure over another for all women, Dr. Borgen said at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource. When discussing the options, each individual patient will have unique concerns and quality of life issues that need to be factored into a collaborative decision about the choice of procedure.
Not including mastectomy in the conversation could be a disservice to the patient, Dr. Borgen said. Quality of life over time, patient anxiety, and “the price of vigilance” are additional factors that patients consider when weighing their surgical options.
Dr. Borgen had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT MBCC
Late-week discharges to home after CRC surgery prone to readmission
BOSTON – The day of the week a patient is discharged from the hospital may have an impact the likelihood of readmission.
Patients discharged home from the hospital on a Thursday after colorectal cancer surgery are more likely to be readmitted within 30 days than those discharged on any other day of the week, investigators found.
In contrast, there were no significant day-dependent differences in readmission rates among patients discharged to a skilled nursing facility or acute rehabilitation program, although patients admitted to clinical facilities had higher overall readmission rates, reported Anna Gustin and coinvestigators at the Levine Cancer Institute at the Carolinas Medical Center in Charlotte, N.C.
“For a patient discharged on a Thursday, if you’re going to get an infection, it’s going to be probably during the weekend, when it’s difficult to contact your primary physician, and when other resources are not as readily available,” said Ms. Gustin, who conducts epidemiologic research at Levine Cancer Center and is also a pre-med student and Japanese major at Wake Forest University in Winston-Salem, N.C.
In a study presented in a poster session at the annual Society of Surgical Oncology Cancer Symposium, Ms. Gustin and her coauthors looked at factors influencing readmission rates among patients undergoing surgery for primary, nonmetastatic colorectal cancer resections.
They drew on the to evaluate outcomes for 93,04 SEER-(Surveillance, Epidemiology, and End Results) Medicare database seven patients aged 66 years and older treated for primary colorectal cancer from 1998 through 2009.
They looked at potential contributing factors such as patient demographics, socioeconomic status, length of stay, days of admission and discharge, and discharge setting (home or clinical facility).
They use multivariate logistic regression models to analyze readmission rates at 14 and 30 days after initial discharge.
Focusing on home discharges, they found that as the week progressed, there was a significant likelihood that a patient discharged home would be readmitted (P less then .001 by chi-square and Cochran-Armitage tests). As noted before, the highest rate of readmission was for patients discharged on Thursday, at 12.4%, compared with 10.1% for patients discharged on Sunday, the discharge day least likely to be associated with rehospitalization.
In multivariate analysis, factors significantly associated with risk for 30-day readmission included male vs. female (hazard ratio, 1.16), black vs. other race (HR, 1.22), length of stay 5, 6-7, or 8-10 vs. 12 or more days (HR, 0.48, 0.59, 0.77, respectively), Charlson comorbidity index score 0, 1 or 3 vs. 3 (HR, 0.59, 0.73, 0.82, respectively), and home discharge vs. other (HR, 0.66; all above comparisons significant as shown by 95% confidence intervals).
The authors concluded that although home discharge itself reduces the likelihood of readmission, “improvements in preparing patients for discharge to home are needed. Additional outpatient interventions could rescue patients from readmission.”
They also suggested reexamining staffing policies and weekend availability of resources for patients, and call for addressing disparities in readmissions based on race, sex, length of stay, and comorbidities.
The study was internally supported. The authors reported having no relevant disclosures.
BOSTON – The day of the week a patient is discharged from the hospital may have an impact the likelihood of readmission.
Patients discharged home from the hospital on a Thursday after colorectal cancer surgery are more likely to be readmitted within 30 days than those discharged on any other day of the week, investigators found.
In contrast, there were no significant day-dependent differences in readmission rates among patients discharged to a skilled nursing facility or acute rehabilitation program, although patients admitted to clinical facilities had higher overall readmission rates, reported Anna Gustin and coinvestigators at the Levine Cancer Institute at the Carolinas Medical Center in Charlotte, N.C.
“For a patient discharged on a Thursday, if you’re going to get an infection, it’s going to be probably during the weekend, when it’s difficult to contact your primary physician, and when other resources are not as readily available,” said Ms. Gustin, who conducts epidemiologic research at Levine Cancer Center and is also a pre-med student and Japanese major at Wake Forest University in Winston-Salem, N.C.
In a study presented in a poster session at the annual Society of Surgical Oncology Cancer Symposium, Ms. Gustin and her coauthors looked at factors influencing readmission rates among patients undergoing surgery for primary, nonmetastatic colorectal cancer resections.
They drew on the to evaluate outcomes for 93,04 SEER-(Surveillance, Epidemiology, and End Results) Medicare database seven patients aged 66 years and older treated for primary colorectal cancer from 1998 through 2009.
They looked at potential contributing factors such as patient demographics, socioeconomic status, length of stay, days of admission and discharge, and discharge setting (home or clinical facility).
They use multivariate logistic regression models to analyze readmission rates at 14 and 30 days after initial discharge.
Focusing on home discharges, they found that as the week progressed, there was a significant likelihood that a patient discharged home would be readmitted (P less then .001 by chi-square and Cochran-Armitage tests). As noted before, the highest rate of readmission was for patients discharged on Thursday, at 12.4%, compared with 10.1% for patients discharged on Sunday, the discharge day least likely to be associated with rehospitalization.
In multivariate analysis, factors significantly associated with risk for 30-day readmission included male vs. female (hazard ratio, 1.16), black vs. other race (HR, 1.22), length of stay 5, 6-7, or 8-10 vs. 12 or more days (HR, 0.48, 0.59, 0.77, respectively), Charlson comorbidity index score 0, 1 or 3 vs. 3 (HR, 0.59, 0.73, 0.82, respectively), and home discharge vs. other (HR, 0.66; all above comparisons significant as shown by 95% confidence intervals).
The authors concluded that although home discharge itself reduces the likelihood of readmission, “improvements in preparing patients for discharge to home are needed. Additional outpatient interventions could rescue patients from readmission.”
They also suggested reexamining staffing policies and weekend availability of resources for patients, and call for addressing disparities in readmissions based on race, sex, length of stay, and comorbidities.
The study was internally supported. The authors reported having no relevant disclosures.
BOSTON – The day of the week a patient is discharged from the hospital may have an impact the likelihood of readmission.
Patients discharged home from the hospital on a Thursday after colorectal cancer surgery are more likely to be readmitted within 30 days than those discharged on any other day of the week, investigators found.
In contrast, there were no significant day-dependent differences in readmission rates among patients discharged to a skilled nursing facility or acute rehabilitation program, although patients admitted to clinical facilities had higher overall readmission rates, reported Anna Gustin and coinvestigators at the Levine Cancer Institute at the Carolinas Medical Center in Charlotte, N.C.
“For a patient discharged on a Thursday, if you’re going to get an infection, it’s going to be probably during the weekend, when it’s difficult to contact your primary physician, and when other resources are not as readily available,” said Ms. Gustin, who conducts epidemiologic research at Levine Cancer Center and is also a pre-med student and Japanese major at Wake Forest University in Winston-Salem, N.C.
In a study presented in a poster session at the annual Society of Surgical Oncology Cancer Symposium, Ms. Gustin and her coauthors looked at factors influencing readmission rates among patients undergoing surgery for primary, nonmetastatic colorectal cancer resections.
They drew on the to evaluate outcomes for 93,04 SEER-(Surveillance, Epidemiology, and End Results) Medicare database seven patients aged 66 years and older treated for primary colorectal cancer from 1998 through 2009.
They looked at potential contributing factors such as patient demographics, socioeconomic status, length of stay, days of admission and discharge, and discharge setting (home or clinical facility).
They use multivariate logistic regression models to analyze readmission rates at 14 and 30 days after initial discharge.
Focusing on home discharges, they found that as the week progressed, there was a significant likelihood that a patient discharged home would be readmitted (P less then .001 by chi-square and Cochran-Armitage tests). As noted before, the highest rate of readmission was for patients discharged on Thursday, at 12.4%, compared with 10.1% for patients discharged on Sunday, the discharge day least likely to be associated with rehospitalization.
In multivariate analysis, factors significantly associated with risk for 30-day readmission included male vs. female (hazard ratio, 1.16), black vs. other race (HR, 1.22), length of stay 5, 6-7, or 8-10 vs. 12 or more days (HR, 0.48, 0.59, 0.77, respectively), Charlson comorbidity index score 0, 1 or 3 vs. 3 (HR, 0.59, 0.73, 0.82, respectively), and home discharge vs. other (HR, 0.66; all above comparisons significant as shown by 95% confidence intervals).
The authors concluded that although home discharge itself reduces the likelihood of readmission, “improvements in preparing patients for discharge to home are needed. Additional outpatient interventions could rescue patients from readmission.”
They also suggested reexamining staffing policies and weekend availability of resources for patients, and call for addressing disparities in readmissions based on race, sex, length of stay, and comorbidities.
The study was internally supported. The authors reported having no relevant disclosures.
Key clinical point: Patients discharged home on a Thursday following surgery for primary colorectal cancer are more likely to be readmitted with 30 days than are patients discharged home on any other day of the week.
Major finding: The highest rate of readmission was for patients discharged on Thursday, at 12.4%, compared with lowest rate of 10.1% for patients discharged on Sunday.
Data source: Retrospective SEER-Medicare database review of records on 93,047 patients treated for colorectal cancer.
Disclosures: The study was internally supported. The authors reported having no relevant disclosures.
VIDEO: Dr. Ann Partridge discusses counseling young breast cancer patients
MIAMI BEACH – Despite significant improvements in detection and treatment of contralateral breast cancer, there’s a “huge increase” in the number of women choosing to undergo bilateral mastectomy, Dr. Ann Partridge of Dana-Farber Cancer Institute in Boston said.
Physicians can counsel patients that the risk of cancer recurrence in the body elsewhere is more of a concern than a new breast cancer, Dr. Partridge said, and provide a realistic picture of the side effects and potential complications of bilateral versus unilateral surgery. Conversations between physicians and patients regarding the pros and cons of more aggressive therapy are essential, she said in a video interview at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
Some ethical considerations arise when counseling younger women with a genetic mutation that raises the risk of breast cancer (for example, BRCA1 or BRCA2), especially when they plan to undergo in vitro fertilization and pre-implantation embryo analysis. Dr. Partridge shares advice on how to help these women make the best decision for them.
Many women diagnosed with breast cancer before age 40 wonder if it’s safe to have a baby, Dr. Partridge said. Ask about intentions to get pregnant at the first visit, she advised, and share data from retrospective outcome comparisons when guiding these women on their options.
Dr. Partridge had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MIAMI BEACH – Despite significant improvements in detection and treatment of contralateral breast cancer, there’s a “huge increase” in the number of women choosing to undergo bilateral mastectomy, Dr. Ann Partridge of Dana-Farber Cancer Institute in Boston said.
Physicians can counsel patients that the risk of cancer recurrence in the body elsewhere is more of a concern than a new breast cancer, Dr. Partridge said, and provide a realistic picture of the side effects and potential complications of bilateral versus unilateral surgery. Conversations between physicians and patients regarding the pros and cons of more aggressive therapy are essential, she said in a video interview at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
Some ethical considerations arise when counseling younger women with a genetic mutation that raises the risk of breast cancer (for example, BRCA1 or BRCA2), especially when they plan to undergo in vitro fertilization and pre-implantation embryo analysis. Dr. Partridge shares advice on how to help these women make the best decision for them.
Many women diagnosed with breast cancer before age 40 wonder if it’s safe to have a baby, Dr. Partridge said. Ask about intentions to get pregnant at the first visit, she advised, and share data from retrospective outcome comparisons when guiding these women on their options.
Dr. Partridge had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MIAMI BEACH – Despite significant improvements in detection and treatment of contralateral breast cancer, there’s a “huge increase” in the number of women choosing to undergo bilateral mastectomy, Dr. Ann Partridge of Dana-Farber Cancer Institute in Boston said.
Physicians can counsel patients that the risk of cancer recurrence in the body elsewhere is more of a concern than a new breast cancer, Dr. Partridge said, and provide a realistic picture of the side effects and potential complications of bilateral versus unilateral surgery. Conversations between physicians and patients regarding the pros and cons of more aggressive therapy are essential, she said in a video interview at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
Some ethical considerations arise when counseling younger women with a genetic mutation that raises the risk of breast cancer (for example, BRCA1 or BRCA2), especially when they plan to undergo in vitro fertilization and pre-implantation embryo analysis. Dr. Partridge shares advice on how to help these women make the best decision for them.
Many women diagnosed with breast cancer before age 40 wonder if it’s safe to have a baby, Dr. Partridge said. Ask about intentions to get pregnant at the first visit, she advised, and share data from retrospective outcome comparisons when guiding these women on their options.
Dr. Partridge had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM MBCC
VIDEO: Physicians must counsel women on mastectomy misperceptions
MIAMI BEACH – Although many women with breast cancer who choose a mastectomy believe they will lower their risk for recurrence, compared with breast conservation therapy, physicians should counsel them about this misperception for most instances, Dr. Mike Dixon said in a video interview at the annual Miami Breast Cancer Conference.
Multiple factors suggest that the risk of cancer recurrence with breast conservation therapy have declined over time. When combined with advances in imaging and gains in systemic therapy and radiation therapy, offering women with early breast cancer a choice between mastectomy and breast conservation may no longer make sense, said Dr. Dixon, professor of surgery at the University of Edinburgh.
More favorable patient outcomes and lower overall costs also favor breast conservation therapy over mastectomy for most women, he explained.
The conference was held by Physicians’ Education Resource. Dr. Dixon has no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MIAMI BEACH – Although many women with breast cancer who choose a mastectomy believe they will lower their risk for recurrence, compared with breast conservation therapy, physicians should counsel them about this misperception for most instances, Dr. Mike Dixon said in a video interview at the annual Miami Breast Cancer Conference.
Multiple factors suggest that the risk of cancer recurrence with breast conservation therapy have declined over time. When combined with advances in imaging and gains in systemic therapy and radiation therapy, offering women with early breast cancer a choice between mastectomy and breast conservation may no longer make sense, said Dr. Dixon, professor of surgery at the University of Edinburgh.
More favorable patient outcomes and lower overall costs also favor breast conservation therapy over mastectomy for most women, he explained.
The conference was held by Physicians’ Education Resource. Dr. Dixon has no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MIAMI BEACH – Although many women with breast cancer who choose a mastectomy believe they will lower their risk for recurrence, compared with breast conservation therapy, physicians should counsel them about this misperception for most instances, Dr. Mike Dixon said in a video interview at the annual Miami Breast Cancer Conference.
Multiple factors suggest that the risk of cancer recurrence with breast conservation therapy have declined over time. When combined with advances in imaging and gains in systemic therapy and radiation therapy, offering women with early breast cancer a choice between mastectomy and breast conservation may no longer make sense, said Dr. Dixon, professor of surgery at the University of Edinburgh.
More favorable patient outcomes and lower overall costs also favor breast conservation therapy over mastectomy for most women, he explained.
The conference was held by Physicians’ Education Resource. Dr. Dixon has no relevant disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM MBCC
VIDEO: How to navigate value-based care payer contracts
AUSTIN, TEX. – The shift from volume- to value-based care has become a regular hot topic among the medical community. But one rarely discussed question is how quality-based care will impact physician contracts with health plans, according to Bloomfield Hills, Mich., health law attorney Mark S. Kopson.
In a video interview at an American Health Lawyers Association meeting, Mr. Kopson discusses how to navigate payer contracts when operating within value-based care models. He addresses ideal terms to include in quality-based care contracts and how to mitigate legal risks with health plans.
“The contract language that works in volume-based contracts doesn’t work in value-based contracts,” Mr. Kopson explains. “We have to make a distinction between the two and recognize that there are risks and issues that have to be addressed in value-based arrangements.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
AUSTIN, TEX. – The shift from volume- to value-based care has become a regular hot topic among the medical community. But one rarely discussed question is how quality-based care will impact physician contracts with health plans, according to Bloomfield Hills, Mich., health law attorney Mark S. Kopson.
In a video interview at an American Health Lawyers Association meeting, Mr. Kopson discusses how to navigate payer contracts when operating within value-based care models. He addresses ideal terms to include in quality-based care contracts and how to mitigate legal risks with health plans.
“The contract language that works in volume-based contracts doesn’t work in value-based contracts,” Mr. Kopson explains. “We have to make a distinction between the two and recognize that there are risks and issues that have to be addressed in value-based arrangements.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
AUSTIN, TEX. – The shift from volume- to value-based care has become a regular hot topic among the medical community. But one rarely discussed question is how quality-based care will impact physician contracts with health plans, according to Bloomfield Hills, Mich., health law attorney Mark S. Kopson.
In a video interview at an American Health Lawyers Association meeting, Mr. Kopson discusses how to navigate payer contracts when operating within value-based care models. He addresses ideal terms to include in quality-based care contracts and how to mitigate legal risks with health plans.
“The contract language that works in volume-based contracts doesn’t work in value-based contracts,” Mr. Kopson explains. “We have to make a distinction between the two and recognize that there are risks and issues that have to be addressed in value-based arrangements.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @legal_med
EXPERT ANALYSIS FROM THE PHYSICIANS AND HOSPITALS LAW INSTITUTE
Neoadjuvant chemo reduces extent of axillary dissection in some breast cancers
BOSTON – The majority of patients with hormone receptor–negative breast cancer in the United States get chemotherapy in the adjuvant setting, but neoadjuvant chemotherapy is gaining in use, and is associated with a higher likelihood of breast-conserving surgery for some women with advanced disease, as well as less extensive axillary node dissection.
A review of data on more than 130,000 patients with breast tumors negative for both estrogen and progesterone receptors (ER–/PR–) showed that among patients with clinical stage T3 disease, 26% of those who had received neoadjuvant chemotherapy were able to have breast-conserving surgery, compared with 20% of patients who had received adjuvant chemotherapy, reported Dr. Carlos A. Puig and his colleagues from the Mayo Clinic in Rochester, Minn.
“Patients treated with neoadjuvant chemotherapy have less extensive axillary surgery and a lower rate of nodal positivity,” he added at the annual Society of Surgical Oncology Cancer Symposium.
The data showed that nearly a third of all patients with clinically node-positive disease (cN1-3) who received neoadjuvant chemotherapy had pathologically node-negative disease at the end of therapy.
The aggressive biology of ER–/PR– tumors makes them suitable targets for chemotherapy in the neoadjuvant setting, Dr. Puig said. Overall survival among patients with ER–/PR– who receive neoadjuvant chemotherapy is comparable to that of patients who receive chemotherapy in the adjuvant setting. Neoadjuvant regimens can also downstage tumors before surgery, and a pathologic complete response to chemotherapy delivered prior to surgery is prognostic for outcomes.
Trends in chemotherapy
Dr. Puig and his colleagues combed through the National Cancer Data Base, looking for trends in national practice patterns of use of neoadjuvant chemotherapy in ER–/PR– breast cancer from 2004 through 2012.
They identified a total of 108,128 patients with invasive ER–/PR– breast cancer who received adjuvant chemotherapy, and 24,848 who received neoadjuvant chemo; an additional 43,969 patients who did not receive chemotherapy were excluded from the analysis.
Factors significantly associated with the choice to administer neoadjuvant chemotherapy included age younger than 50, no comorbidities vs. one or two comorbidities on the Charlson/Deyo index, academic/research center vs. community cancer program, higher clinical T stage, and higher clinical N stage.
There was a gradual increase in the use of neoadjuvant chemotherapy over time, from 14.2% in 2004 to 22.3% of all patients in 2012 (P less than .001).
The overall breast-conserving surgery rates were lower among patients who had chemotherapy in the neoadjuvant setting – 33.2% vs. 54.7% (P less than .001). The rates of conservative surgery increased over time, from 32% in 2004 to 36% in 2012 (P less than .001), but decreased over the same period in patients who had adjuvant chemotherapy, from 58% to 51%, respectively.
In a breakdown of surgery type by clinical T stage, mastectomy was more frequently performed in patients who had undergone neoadjuvant treatment, compared with adjuvant therapy, except for stage T3 disease. A higher percentage of those with T3 tumors who had neoadjuvant therapy had breast-conserving surgery in comparison with women who had T3 tumors and adjuvant therapy (26.2% vs. 20.2%, respectively; P less than .001).
To identify the extent of axillary surgery, the authors considered one to five nodes removed to be a surrogate for sentinel lymph node biopsy, and six or more nodes as a surrogate for axillary lymph node dissection.
They found that among patients with clinical stage N1 through N3 who received neoadjuvant chemotherapy, 31.8% converted to pathologically node-negative status.
Dr. Puig noted that the study was limited by the retrospective design and the lack of data on HER2 receptor status, making it impossible to distinguish between ER–/PR– and triple-negative tumors. In addition, they did not have data on genetic testing that could affect surgical choices, such as the presence of BRCA1 or BRCA2.
Following Dr. Puig’s presentation, Dr. Monica Morrow, chief of breast surgery at Memorial Sloan-Kettering Cancer Center, New York, commented that the study put together “patients in whom we would consider there to be an absolute indication for neoadjuvant chemotherapy – meaning T4, N2-N3 – and patients where it’s optional.” The study results suggested that not all patients who should receive neoadjuvant therapy were getting it “which is a little disturbing,” Dr. Morrow said.
She also noted that the decrease in the use of axillary lymph node dissection began prior to publication of studies suggesting that it might be safe to do so.
Dr. Puig and Dr. Morrow had no relevant disclosures.
BOSTON – The majority of patients with hormone receptor–negative breast cancer in the United States get chemotherapy in the adjuvant setting, but neoadjuvant chemotherapy is gaining in use, and is associated with a higher likelihood of breast-conserving surgery for some women with advanced disease, as well as less extensive axillary node dissection.
A review of data on more than 130,000 patients with breast tumors negative for both estrogen and progesterone receptors (ER–/PR–) showed that among patients with clinical stage T3 disease, 26% of those who had received neoadjuvant chemotherapy were able to have breast-conserving surgery, compared with 20% of patients who had received adjuvant chemotherapy, reported Dr. Carlos A. Puig and his colleagues from the Mayo Clinic in Rochester, Minn.
“Patients treated with neoadjuvant chemotherapy have less extensive axillary surgery and a lower rate of nodal positivity,” he added at the annual Society of Surgical Oncology Cancer Symposium.
The data showed that nearly a third of all patients with clinically node-positive disease (cN1-3) who received neoadjuvant chemotherapy had pathologically node-negative disease at the end of therapy.
The aggressive biology of ER–/PR– tumors makes them suitable targets for chemotherapy in the neoadjuvant setting, Dr. Puig said. Overall survival among patients with ER–/PR– who receive neoadjuvant chemotherapy is comparable to that of patients who receive chemotherapy in the adjuvant setting. Neoadjuvant regimens can also downstage tumors before surgery, and a pathologic complete response to chemotherapy delivered prior to surgery is prognostic for outcomes.
Trends in chemotherapy
Dr. Puig and his colleagues combed through the National Cancer Data Base, looking for trends in national practice patterns of use of neoadjuvant chemotherapy in ER–/PR– breast cancer from 2004 through 2012.
They identified a total of 108,128 patients with invasive ER–/PR– breast cancer who received adjuvant chemotherapy, and 24,848 who received neoadjuvant chemo; an additional 43,969 patients who did not receive chemotherapy were excluded from the analysis.
Factors significantly associated with the choice to administer neoadjuvant chemotherapy included age younger than 50, no comorbidities vs. one or two comorbidities on the Charlson/Deyo index, academic/research center vs. community cancer program, higher clinical T stage, and higher clinical N stage.
There was a gradual increase in the use of neoadjuvant chemotherapy over time, from 14.2% in 2004 to 22.3% of all patients in 2012 (P less than .001).
The overall breast-conserving surgery rates were lower among patients who had chemotherapy in the neoadjuvant setting – 33.2% vs. 54.7% (P less than .001). The rates of conservative surgery increased over time, from 32% in 2004 to 36% in 2012 (P less than .001), but decreased over the same period in patients who had adjuvant chemotherapy, from 58% to 51%, respectively.
In a breakdown of surgery type by clinical T stage, mastectomy was more frequently performed in patients who had undergone neoadjuvant treatment, compared with adjuvant therapy, except for stage T3 disease. A higher percentage of those with T3 tumors who had neoadjuvant therapy had breast-conserving surgery in comparison with women who had T3 tumors and adjuvant therapy (26.2% vs. 20.2%, respectively; P less than .001).
To identify the extent of axillary surgery, the authors considered one to five nodes removed to be a surrogate for sentinel lymph node biopsy, and six or more nodes as a surrogate for axillary lymph node dissection.
They found that among patients with clinical stage N1 through N3 who received neoadjuvant chemotherapy, 31.8% converted to pathologically node-negative status.
Dr. Puig noted that the study was limited by the retrospective design and the lack of data on HER2 receptor status, making it impossible to distinguish between ER–/PR– and triple-negative tumors. In addition, they did not have data on genetic testing that could affect surgical choices, such as the presence of BRCA1 or BRCA2.
Following Dr. Puig’s presentation, Dr. Monica Morrow, chief of breast surgery at Memorial Sloan-Kettering Cancer Center, New York, commented that the study put together “patients in whom we would consider there to be an absolute indication for neoadjuvant chemotherapy – meaning T4, N2-N3 – and patients where it’s optional.” The study results suggested that not all patients who should receive neoadjuvant therapy were getting it “which is a little disturbing,” Dr. Morrow said.
She also noted that the decrease in the use of axillary lymph node dissection began prior to publication of studies suggesting that it might be safe to do so.
Dr. Puig and Dr. Morrow had no relevant disclosures.
BOSTON – The majority of patients with hormone receptor–negative breast cancer in the United States get chemotherapy in the adjuvant setting, but neoadjuvant chemotherapy is gaining in use, and is associated with a higher likelihood of breast-conserving surgery for some women with advanced disease, as well as less extensive axillary node dissection.
A review of data on more than 130,000 patients with breast tumors negative for both estrogen and progesterone receptors (ER–/PR–) showed that among patients with clinical stage T3 disease, 26% of those who had received neoadjuvant chemotherapy were able to have breast-conserving surgery, compared with 20% of patients who had received adjuvant chemotherapy, reported Dr. Carlos A. Puig and his colleagues from the Mayo Clinic in Rochester, Minn.
“Patients treated with neoadjuvant chemotherapy have less extensive axillary surgery and a lower rate of nodal positivity,” he added at the annual Society of Surgical Oncology Cancer Symposium.
The data showed that nearly a third of all patients with clinically node-positive disease (cN1-3) who received neoadjuvant chemotherapy had pathologically node-negative disease at the end of therapy.
The aggressive biology of ER–/PR– tumors makes them suitable targets for chemotherapy in the neoadjuvant setting, Dr. Puig said. Overall survival among patients with ER–/PR– who receive neoadjuvant chemotherapy is comparable to that of patients who receive chemotherapy in the adjuvant setting. Neoadjuvant regimens can also downstage tumors before surgery, and a pathologic complete response to chemotherapy delivered prior to surgery is prognostic for outcomes.
Trends in chemotherapy
Dr. Puig and his colleagues combed through the National Cancer Data Base, looking for trends in national practice patterns of use of neoadjuvant chemotherapy in ER–/PR– breast cancer from 2004 through 2012.
They identified a total of 108,128 patients with invasive ER–/PR– breast cancer who received adjuvant chemotherapy, and 24,848 who received neoadjuvant chemo; an additional 43,969 patients who did not receive chemotherapy were excluded from the analysis.
Factors significantly associated with the choice to administer neoadjuvant chemotherapy included age younger than 50, no comorbidities vs. one or two comorbidities on the Charlson/Deyo index, academic/research center vs. community cancer program, higher clinical T stage, and higher clinical N stage.
There was a gradual increase in the use of neoadjuvant chemotherapy over time, from 14.2% in 2004 to 22.3% of all patients in 2012 (P less than .001).
The overall breast-conserving surgery rates were lower among patients who had chemotherapy in the neoadjuvant setting – 33.2% vs. 54.7% (P less than .001). The rates of conservative surgery increased over time, from 32% in 2004 to 36% in 2012 (P less than .001), but decreased over the same period in patients who had adjuvant chemotherapy, from 58% to 51%, respectively.
In a breakdown of surgery type by clinical T stage, mastectomy was more frequently performed in patients who had undergone neoadjuvant treatment, compared with adjuvant therapy, except for stage T3 disease. A higher percentage of those with T3 tumors who had neoadjuvant therapy had breast-conserving surgery in comparison with women who had T3 tumors and adjuvant therapy (26.2% vs. 20.2%, respectively; P less than .001).
To identify the extent of axillary surgery, the authors considered one to five nodes removed to be a surrogate for sentinel lymph node biopsy, and six or more nodes as a surrogate for axillary lymph node dissection.
They found that among patients with clinical stage N1 through N3 who received neoadjuvant chemotherapy, 31.8% converted to pathologically node-negative status.
Dr. Puig noted that the study was limited by the retrospective design and the lack of data on HER2 receptor status, making it impossible to distinguish between ER–/PR– and triple-negative tumors. In addition, they did not have data on genetic testing that could affect surgical choices, such as the presence of BRCA1 or BRCA2.
Following Dr. Puig’s presentation, Dr. Monica Morrow, chief of breast surgery at Memorial Sloan-Kettering Cancer Center, New York, commented that the study put together “patients in whom we would consider there to be an absolute indication for neoadjuvant chemotherapy – meaning T4, N2-N3 – and patients where it’s optional.” The study results suggested that not all patients who should receive neoadjuvant therapy were getting it “which is a little disturbing,” Dr. Morrow said.
She also noted that the decrease in the use of axillary lymph node dissection began prior to publication of studies suggesting that it might be safe to do so.
Dr. Puig and Dr. Morrow had no relevant disclosures.
Key clinical point: Neoadjuvant chemotherapy can benefit some patients with advanced hormone receptor–negative breast cancer.
Major finding: Among patients with cT3 disease, 26% who had neoadjuvant chemotherapy were able to have breast-conserving surgery, compared with 20% of patients who had received adjuvant chemotherapy.
Data source: Retrospective review of data on 132,976 patients with invasive ER–/PR– breast cancer.
Disclosures: Dr. Puig and Dr. Morrow had no relevant disclosures.
Historic Cleveland Clinic uterus transplant fails
Surgeons at the Cleveland Clinic had to remove the transplanted uterus of a 26-year-old woman who was the first patient in a groundbreaking U.S.-based study aimed at achieving pregnancy in women with uterine factor infertility.
Removal of the uterus, which was announced March 9, came after the patient experienced a sudden complication. The study was originally slated to include 10 women and is still ongoing, according to a statement from the Cleveland Clinic.
“At this time, the circumstance of the complication is under review and more information will be shared as it becomes available,” according to a statement. “There is a known risk in solid organ transplantation that the transplanted organ may have to be removed should a complication arise. The medical team took all necessary precautions and measures to ensure the safety of our patient.”
On Feb. 24, a transplant team at the Cleveland Clinic made history by performing the first uterus transplant in the United States. Prior to that, there had been nine successful uterus transplants performed at the University of Gothenburg in Sweden, with the first posttransplant baby born in 2014.
The Cleveland Clinic transplant recipient, known as “Lindsey” to protect her privacy, was selected from more than 250 applicants to undergo the 9-hour procedure involving transplantation of a uterus from a deceased organ donor of reproductive age.
If the transplant had been a successful, Lindsey was set to undergo a year of antirejection treatment followed by in vitro fertilization. Under the study protocol, the uterus transplant would be temporary and the uterus would be removed after a patient had delivered one or two babies.
Officials at the Cleveland Clinic said Lindsey was doing well and recovering after the removal of the transplanted uterus.
“I just wanted to take a moment to express my gratitude toward all of my doctors,” Lindsey and her husband said in a statement. “They acted very quickly to ensure my health and safety. Unfortunately, I did lose the uterus to complications. However, I am doing okay and appreciate all of your prayers and good thoughts.”
On Twitter @maryellenny
Surgeons at the Cleveland Clinic had to remove the transplanted uterus of a 26-year-old woman who was the first patient in a groundbreaking U.S.-based study aimed at achieving pregnancy in women with uterine factor infertility.
Removal of the uterus, which was announced March 9, came after the patient experienced a sudden complication. The study was originally slated to include 10 women and is still ongoing, according to a statement from the Cleveland Clinic.
“At this time, the circumstance of the complication is under review and more information will be shared as it becomes available,” according to a statement. “There is a known risk in solid organ transplantation that the transplanted organ may have to be removed should a complication arise. The medical team took all necessary precautions and measures to ensure the safety of our patient.”
On Feb. 24, a transplant team at the Cleveland Clinic made history by performing the first uterus transplant in the United States. Prior to that, there had been nine successful uterus transplants performed at the University of Gothenburg in Sweden, with the first posttransplant baby born in 2014.
The Cleveland Clinic transplant recipient, known as “Lindsey” to protect her privacy, was selected from more than 250 applicants to undergo the 9-hour procedure involving transplantation of a uterus from a deceased organ donor of reproductive age.
If the transplant had been a successful, Lindsey was set to undergo a year of antirejection treatment followed by in vitro fertilization. Under the study protocol, the uterus transplant would be temporary and the uterus would be removed after a patient had delivered one or two babies.
Officials at the Cleveland Clinic said Lindsey was doing well and recovering after the removal of the transplanted uterus.
“I just wanted to take a moment to express my gratitude toward all of my doctors,” Lindsey and her husband said in a statement. “They acted very quickly to ensure my health and safety. Unfortunately, I did lose the uterus to complications. However, I am doing okay and appreciate all of your prayers and good thoughts.”
On Twitter @maryellenny
Surgeons at the Cleveland Clinic had to remove the transplanted uterus of a 26-year-old woman who was the first patient in a groundbreaking U.S.-based study aimed at achieving pregnancy in women with uterine factor infertility.
Removal of the uterus, which was announced March 9, came after the patient experienced a sudden complication. The study was originally slated to include 10 women and is still ongoing, according to a statement from the Cleveland Clinic.
“At this time, the circumstance of the complication is under review and more information will be shared as it becomes available,” according to a statement. “There is a known risk in solid organ transplantation that the transplanted organ may have to be removed should a complication arise. The medical team took all necessary precautions and measures to ensure the safety of our patient.”
On Feb. 24, a transplant team at the Cleveland Clinic made history by performing the first uterus transplant in the United States. Prior to that, there had been nine successful uterus transplants performed at the University of Gothenburg in Sweden, with the first posttransplant baby born in 2014.
The Cleveland Clinic transplant recipient, known as “Lindsey” to protect her privacy, was selected from more than 250 applicants to undergo the 9-hour procedure involving transplantation of a uterus from a deceased organ donor of reproductive age.
If the transplant had been a successful, Lindsey was set to undergo a year of antirejection treatment followed by in vitro fertilization. Under the study protocol, the uterus transplant would be temporary and the uterus would be removed after a patient had delivered one or two babies.
Officials at the Cleveland Clinic said Lindsey was doing well and recovering after the removal of the transplanted uterus.
“I just wanted to take a moment to express my gratitude toward all of my doctors,” Lindsey and her husband said in a statement. “They acted very quickly to ensure my health and safety. Unfortunately, I did lose the uterus to complications. However, I am doing okay and appreciate all of your prayers and good thoughts.”
On Twitter @maryellenny
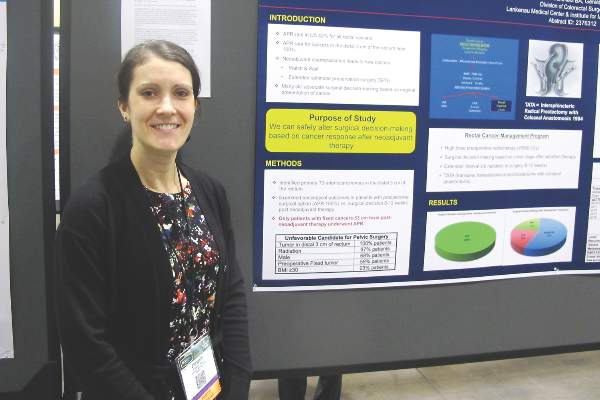
Hold rectal surgery decision until neoadjuvant chemo is done
BOSTON – Good results come to those who wait, suggest the findings of a study of optimal timing of surgical decisions in patients with advanced stage cancers in the distal rectum.
When surgeons waited 8 to 12 weeks after the completion of neoadjuvant chemoradiation to decide whether to proceed with radical sphincter preservation surgery (SPS) or abdominoperineal resection (APR) in patients with T3 cancers of the distal third of the rectum, they were able to avoid creating a colostomy with no adverse oncologic outcomes in 79% of patients, reported Dr. Elizabeth A. Myers and her colleagues from the Lankenau Medical Center and Institute for Medical Research in Wynnewood, Pennsylvania.
“An interesting thing, but still quite controversial, is the timing of when you do surgery,” Dr. Myers said in an interview during a poster session at the annual Society of Surgical Oncology Cancer Symposium.
“There is a large school of thought that still believes you should base your surgical plan on the tumor at its presentation, versus making the decision once the patient has undergone neoadjuvant chemoradiation treatment. The purpose of our study is to show with our data that you can safely alter your decision making based on what the cancer presents as following neoadjuvant chemoradiation,” she said.
The investigators looked at 192 consecutive patients with T3 cancers of the distal third of the rectum who were included in a prospectively maintained database. At the time of presentation, all of the patients would have met criteria for requiring APR and colostomy, due to unfavorable factors for pelvic surgery such as prior radiation (97%), male sex (68%), preoperative fixed tumor (59%), or obesity (23%).
The patients underwent neoadjuvant radiation given at a mean of dose of 5,580 cGy, consisting of a 4,500 cGy standard dose and a 1,080 cGy boost to the area of tumor. Most (87%) also received concurrent 5-fluorauracil-based chemotherapy.
“We have found that this helps to downgrade the tumor quite well,” Dr. Myers said.
Following the completion of therapy, they waited for 8 to 12 additional weeks before planning surgery to allow for the maximum benefit of radiation.
All patients, except those who at the end of neoadjuvant chemotherapy still had a fixed cancer at the 3 cm level or below, were offered SPS. The mean time from completion of chemotherapy to surgery was 11 weeks.
Of the 192 patients, 41 underwent APR, 109 had radical SPS, including 107 receiving transanal transabdominal proctocolectomy with coloanal anastomosis (TATA), and 2 receiving low anterior resection. The remaining patients had local excision with either a transanal technique (TAE; 15 patients) or transanal endoscopic microsurgery (TEM, 27 patients).
After a mean follow-up of 55.4 months (range, 1-242 months) the 5-year stoma-free survival rate was 79%. Kaplan-Meier 5-year actuarial survival rates were 98% for all patients who underwent radical SPS, 100% for those who had local excision with TEM, 82% for those who had local excision with TAE (combined SPS procedures, 95%), and 72% for patients who underwent APR.
Local recurrences occurred in 6.6% of all patients who underwent SPS, compared with 7.3% of those who underwent APR. Distant metastases occurred in 22.5% and 24.4%, respectively.
“Holding surgical decision-making until after completion of neoadjuvant therapy allows for increased sphincter preservation with good oncologic outcomes in rectal cancer patients,” the investigators concluded.
BOSTON – Good results come to those who wait, suggest the findings of a study of optimal timing of surgical decisions in patients with advanced stage cancers in the distal rectum.
When surgeons waited 8 to 12 weeks after the completion of neoadjuvant chemoradiation to decide whether to proceed with radical sphincter preservation surgery (SPS) or abdominoperineal resection (APR) in patients with T3 cancers of the distal third of the rectum, they were able to avoid creating a colostomy with no adverse oncologic outcomes in 79% of patients, reported Dr. Elizabeth A. Myers and her colleagues from the Lankenau Medical Center and Institute for Medical Research in Wynnewood, Pennsylvania.
“An interesting thing, but still quite controversial, is the timing of when you do surgery,” Dr. Myers said in an interview during a poster session at the annual Society of Surgical Oncology Cancer Symposium.
“There is a large school of thought that still believes you should base your surgical plan on the tumor at its presentation, versus making the decision once the patient has undergone neoadjuvant chemoradiation treatment. The purpose of our study is to show with our data that you can safely alter your decision making based on what the cancer presents as following neoadjuvant chemoradiation,” she said.
The investigators looked at 192 consecutive patients with T3 cancers of the distal third of the rectum who were included in a prospectively maintained database. At the time of presentation, all of the patients would have met criteria for requiring APR and colostomy, due to unfavorable factors for pelvic surgery such as prior radiation (97%), male sex (68%), preoperative fixed tumor (59%), or obesity (23%).
The patients underwent neoadjuvant radiation given at a mean of dose of 5,580 cGy, consisting of a 4,500 cGy standard dose and a 1,080 cGy boost to the area of tumor. Most (87%) also received concurrent 5-fluorauracil-based chemotherapy.
“We have found that this helps to downgrade the tumor quite well,” Dr. Myers said.
Following the completion of therapy, they waited for 8 to 12 additional weeks before planning surgery to allow for the maximum benefit of radiation.
All patients, except those who at the end of neoadjuvant chemotherapy still had a fixed cancer at the 3 cm level or below, were offered SPS. The mean time from completion of chemotherapy to surgery was 11 weeks.
Of the 192 patients, 41 underwent APR, 109 had radical SPS, including 107 receiving transanal transabdominal proctocolectomy with coloanal anastomosis (TATA), and 2 receiving low anterior resection. The remaining patients had local excision with either a transanal technique (TAE; 15 patients) or transanal endoscopic microsurgery (TEM, 27 patients).
After a mean follow-up of 55.4 months (range, 1-242 months) the 5-year stoma-free survival rate was 79%. Kaplan-Meier 5-year actuarial survival rates were 98% for all patients who underwent radical SPS, 100% for those who had local excision with TEM, 82% for those who had local excision with TAE (combined SPS procedures, 95%), and 72% for patients who underwent APR.
Local recurrences occurred in 6.6% of all patients who underwent SPS, compared with 7.3% of those who underwent APR. Distant metastases occurred in 22.5% and 24.4%, respectively.
“Holding surgical decision-making until after completion of neoadjuvant therapy allows for increased sphincter preservation with good oncologic outcomes in rectal cancer patients,” the investigators concluded.
BOSTON – Good results come to those who wait, suggest the findings of a study of optimal timing of surgical decisions in patients with advanced stage cancers in the distal rectum.
When surgeons waited 8 to 12 weeks after the completion of neoadjuvant chemoradiation to decide whether to proceed with radical sphincter preservation surgery (SPS) or abdominoperineal resection (APR) in patients with T3 cancers of the distal third of the rectum, they were able to avoid creating a colostomy with no adverse oncologic outcomes in 79% of patients, reported Dr. Elizabeth A. Myers and her colleagues from the Lankenau Medical Center and Institute for Medical Research in Wynnewood, Pennsylvania.
“An interesting thing, but still quite controversial, is the timing of when you do surgery,” Dr. Myers said in an interview during a poster session at the annual Society of Surgical Oncology Cancer Symposium.
“There is a large school of thought that still believes you should base your surgical plan on the tumor at its presentation, versus making the decision once the patient has undergone neoadjuvant chemoradiation treatment. The purpose of our study is to show with our data that you can safely alter your decision making based on what the cancer presents as following neoadjuvant chemoradiation,” she said.
The investigators looked at 192 consecutive patients with T3 cancers of the distal third of the rectum who were included in a prospectively maintained database. At the time of presentation, all of the patients would have met criteria for requiring APR and colostomy, due to unfavorable factors for pelvic surgery such as prior radiation (97%), male sex (68%), preoperative fixed tumor (59%), or obesity (23%).
The patients underwent neoadjuvant radiation given at a mean of dose of 5,580 cGy, consisting of a 4,500 cGy standard dose and a 1,080 cGy boost to the area of tumor. Most (87%) also received concurrent 5-fluorauracil-based chemotherapy.
“We have found that this helps to downgrade the tumor quite well,” Dr. Myers said.
Following the completion of therapy, they waited for 8 to 12 additional weeks before planning surgery to allow for the maximum benefit of radiation.
All patients, except those who at the end of neoadjuvant chemotherapy still had a fixed cancer at the 3 cm level or below, were offered SPS. The mean time from completion of chemotherapy to surgery was 11 weeks.
Of the 192 patients, 41 underwent APR, 109 had radical SPS, including 107 receiving transanal transabdominal proctocolectomy with coloanal anastomosis (TATA), and 2 receiving low anterior resection. The remaining patients had local excision with either a transanal technique (TAE; 15 patients) or transanal endoscopic microsurgery (TEM, 27 patients).
After a mean follow-up of 55.4 months (range, 1-242 months) the 5-year stoma-free survival rate was 79%. Kaplan-Meier 5-year actuarial survival rates were 98% for all patients who underwent radical SPS, 100% for those who had local excision with TEM, 82% for those who had local excision with TAE (combined SPS procedures, 95%), and 72% for patients who underwent APR.
Local recurrences occurred in 6.6% of all patients who underwent SPS, compared with 7.3% of those who underwent APR. Distant metastases occurred in 22.5% and 24.4%, respectively.
“Holding surgical decision-making until after completion of neoadjuvant therapy allows for increased sphincter preservation with good oncologic outcomes in rectal cancer patients,” the investigators concluded.
FROM SSO 2016
Key clinical point: Waiting 8-12 weeks following neoadjuvant chemoradiation in patients with T3 distal rectal cancers improves chances for sphincter preservation.
Major finding: The 5-year stoma-free survival rate was 79% in patients initially considered candidates for APR and colostomy.
Data source: Retrospective review of 192 patients in a prospectively maintained database.
Disclosures: The study was internally supported. Dr. Myers reported having no conflicts of interest.